Abstract
Background:
A majority of reports in the past decade have demonstrated that perioperative hypothermia increases susceptibility to surgical site infection (SSI). However, in recent years, an increasing number of studies did not find an association between hypothermia and the risk of SSI. These contradictory results have given rise to a conflicting issue on whether perioperative hypothermia is associated with SSI risk in surgical patients.
Methods:
We examined the association between perioperative hypothermia and SSI incidence and then integrated available evidence by searching the databases, such as PubMed, Web of Science, Embase, and Cochrane library for potential papers from inception to April 2018. We included studies that reported original data or odds ratio (OR) with 95% confidence intervals (CIs) of the associations. Using fixed-effects models combined the OR with 95% CIs, randomized controlled trials and observational studies were analyzed, respectively, and cohort studies were further analyzed. Sensitivity analyses were performed by omitting each study iteratively, and publication bias was detected using Begg's tests.
Results:
We screened 384 studies, and identified 8 eligible studies, including 2 randomized controlled trials and 6 observational studies (1 case–control study and 5 cohort studies). The pooled OR results in the randomized controlled studies showed that perioperative hypothermia could increase the risk of SSI without heterogeneity (OR, 1.60; 95% CI, 1.14–2.23; I2 = 0.0%, P = .845). The fixed-effect meta-analysis indicated no association between perioperative hypothermia and SSI risk in observational studies (OR, 0.98; 95% CI, 0.96–1.01; I2 = 53.2%, P = .058). Furthermore, cohort studies were performed to pool OR by using the fixed-effect model, and the incorporated results also suggested a similar relationship (OR, 1.13; 95% CI, 0.97–1.33; I2 = 46.4%, P = .113).
Conclusion:
The meta-analysis suggests that perioperative hypothermia is not associated with SSI in surgical patients. However, the 8 eligible studies were mostly cohort studies. Thus, further randomized controlled trials are required to confirm this finding.
Keywords: meta-analysis, perioperative hypothermia, surgical site infection
1. Introduction
Body temperature is vital in maintaining normal human activities. However, factors, such as the use of anesthetic drugs, cold operating theater, skin antisepsis, and cold irrigation of a patient with the body uncovered, and the use of intravenous solutions during surgery, can lead to a low body temperature in the anesthetic–surgical procedure. Hypothermia occurs when the core temperature of an organism is <36°C, commonly affecting up to 70% of surgical patients perioperatively.[1] Anesthesiology studies have shown that perioperative hypothermia is associated with numerous adverse outcomes, including triggered myocardial ischemia, prolonged recovery, impaired immunity, increased blood loss, delayed wound healing, and increased risk of surgical site infection (SSI).[2,3]
SSI is possibly the most common postoperative complication, affecting up to 30% of surgical patients,[4] lengthening the hospital duration by 1 week and considerably increasing the cost of the health care.[5] Besides, data have revealed that antibiotic resistance patterns exists in more than half of the isolated microorganisms from infected surgical wounds.[6]
Considering the high incidence and potential preventability of SSI, risk factors during the perioperative period contributing to the risk of SSI are emphasized generally. There is concern regarding the link between perioperative hypothermia and the risk of SSI. The study of Kurz et al[7] observed that the incidence of SSI increases thrice, when a patient's body temperature is 2°C lower than the normal temperature. However, Geiger et al[8] showed that low intraoperative temperatures are related to low SSI rates. Furthermore, the new study by Baucom et al[9] did not find an association between hypothermia and SSI. These contradictory results have given rise to a conflicting issue on whether perioperative hypothermia is associated to SSI risk in surgical patients. A meta-analysis may be necessary in integrating available evidence. Therefore, we assessed the evidence on the association between perioperative hypothermia and SSI by conducting a meta-analysis of published studies.
2. Materials and methods
2.1. Searching strategy
Related articles were identified and selected from PubMed, Web of Science, Embase, and Cochrane Library by using search terms: (perioperative hypothermia or intraoperative hypothermia or hypothermia) and (surgical wound infection or surgical wound infection or surgical site infection or site infection or wound infection). The search in each electronic database was limited to studies concerning humans that were published before April 2018. Reference lists were also reviewed, and related references were hand-searched to obtain potentially eligible papers. Two independent authors screened abstracts and citations. The included articles were reviewed further for full-text reports. Figure 1 shows the literature search procedure in detail. No ethical approval was needed in this study.
Figure 1.
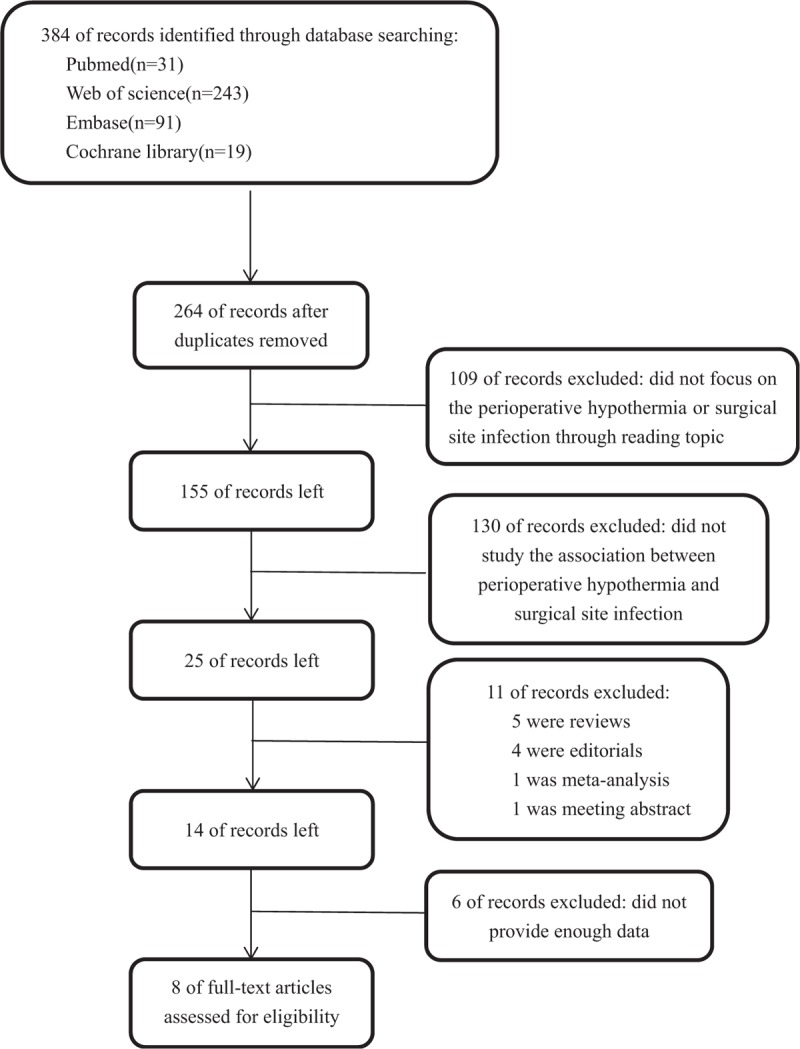
The detailed procedures for the literature search.
2.2. Inclusion and exclusion criteria
The inclusion criteria for this meta-analysis were: studies assessing the correlation between perioperative hypothermia and SSI; studies including the incidence number or odds ratio (OR) of SSI and hypothermia in a control group with 95% confidence intervals (95% CIs); studies selected for clinical trial research; and studies containing a reference group. Studies irrelevant to hypothermia, editorials, comments, letters, review articles, and papers lacking pertinent statistical information for calculating effect estimates were excluded from the meta-analysis.
2.3. Data extraction
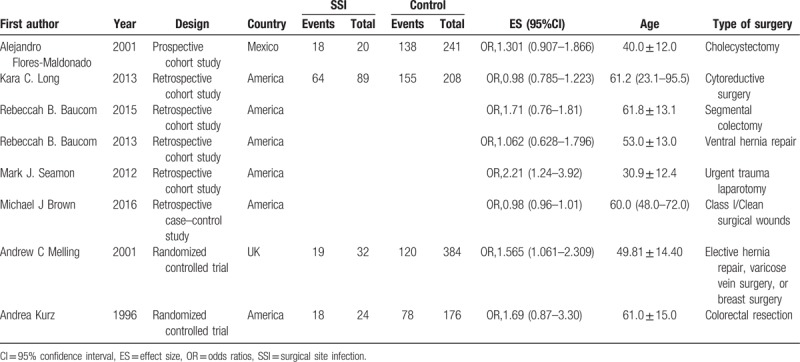
Data from each eligible paper were screened and abstracted independently by 2 investigators by using a preparative standardized data form. Disagreements were resolved through detailed discussions or consultations with the third author until a consensus was reached. The data included the first author's surname, authors’ countries, year of publication, method of the study, number in case and control groups, adjusted OR with 95% CIs, age, and type of surgery (Table 1).
Table 1.
Characteristics of studies included in the meta-analysis.
2.4. Data synthesis and analysis
This meta-analysis was performed by calculating OR with 95% CIs to reflect the relationship between hypothermia and SSI risk. The chi-squared-based Q test and I2 statistics were used to assess heterogeneity among included studies, and the fixed-effect model or random-effect model was applied depending on heterogeneity assumption.[10] The random-effect model was used to calculate the pooled OR in the presence of significant heterogeneity (P < .05 and I2 > 50%); otherwise, a fixed-effect model was performed.[11] Sensitivity analysis was conducted by excluding one study at a time to estimate the stability of the pooled results. Besides, we utilized Begg's test (rank correlation method)[12] to evaluate potential publication bias, where P < .1 was considered as representative of significant statistical publication bias. All statistical analyses were performed using Stata version 12.0 software (StataCorp, College Station, TX). Statistical significance was considered if P < .05.
3. Results
3.1. Search results
The search identified 384 potentially relevant articles in different electronic databases. Among these articles, 120 duplicate datasets were excluded. Subsequently, 240 articles not focusing on the association between perioperative hypothermia and SSI were removed. After thoroughly screening the remaining articles, 5 articles not providing detailed data for the meta-analysis were excluded, and 11 others were removed for other reasons. A final set of 8 eligible articles was used in the meta-analysis after extraction.[7,9,13–18]Figure 1 presents the detailed flowchart of the procedure for study selection.
3.2. Characteristics of studies
Among the 8 datasets, 2 were randomized controlled trials,[7,16] 1 was a case–control study,[17] and 5 were cohort studies.[9,13–15,18] The year of publication ranged from 1996 to 2017. Among the included studies, 6 were performed in the United States,[7,9,14,15,17,18] 1 was conducted in Mexico,[13] and 1 was performed in the United Kingdom.[16] The main characteristics of the individual studies are summarized in Table 1.
3.3. Meta-analysis results
The meta-analysis was conducted to explore the potential relationship between perioperative hypothermia and SSI risk in the 8 studies. Figure 2 shows that the pooled OR results in the randomized controlled studies that showed that perioperative hypothermia could increase the risk of SSI without heterogeneity (OR, 1.60; 95% CI, 1.14–2.23; I2 = 0.0%, P = .845). The fixed-effect meta-analysis indicated no association between perioperative hypothermia and SSI risk in observational studies (OR, 0.98; 95% CI, 0.96–1.01; I2 = 53.2%, P = .058). Furthermore, cohort studies were performed further to pool OR by using a fixed-effect model, and the incorporated results also suggested a similar relationship (OR, 1.13; 95% CI, 0.97–1.33; I2 = 46.4%, P = .113) (Fig. 3).
Figure 2.
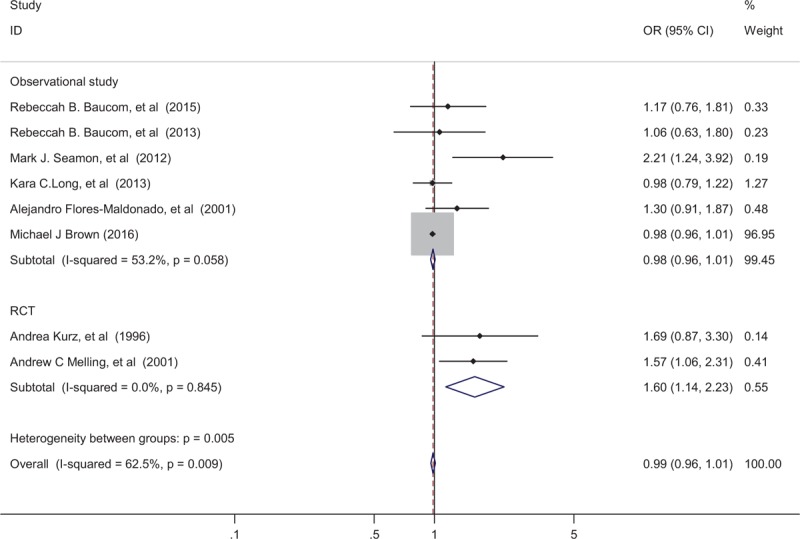
Odds ratio (OR) for the association between the perioperative hypothermia and surgical site infection in 2 RCT studies and 6 observational studies. The diamond denotes the incorporated OR. Shaded rectangles suggest the OR in each study, with sizes inversely proportional to the SE of the OR. Horizontal lines indicate the 95% confidence interval (CI). CI = confidence interval, OR = odds ratio, SE = standard error.
Figure 3.
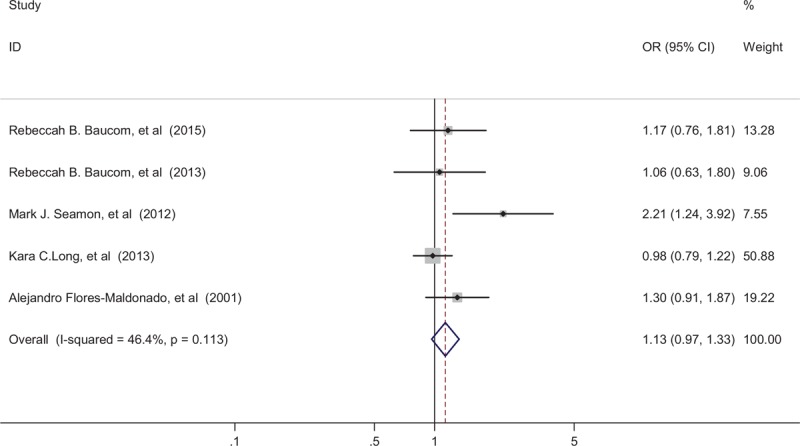
Odds ratio (OR) for the association between the perioperative hypothermia and surgical site infection in 5 cohort studies. The diamond denotes the incorporated OR. Shaded rectangles suggest the OR in each study, with sizes inversely proportional to the SE of the OR. Horizontal lines indicate the 95% confidence interval (CI). CI = confidence interval, OR = odds ratio, SE = standard error.
3.4. Sensitivity analysis
A sensitivity analysis was conducted by sequentially excluding each individual study at a time to estimate the stability of the pooled results in observational studies and cohort studies respectively. The analysis results demonstrated that no individual study significantly affected the pooled ORs (Figs. 4 and 5).
Figure 4.
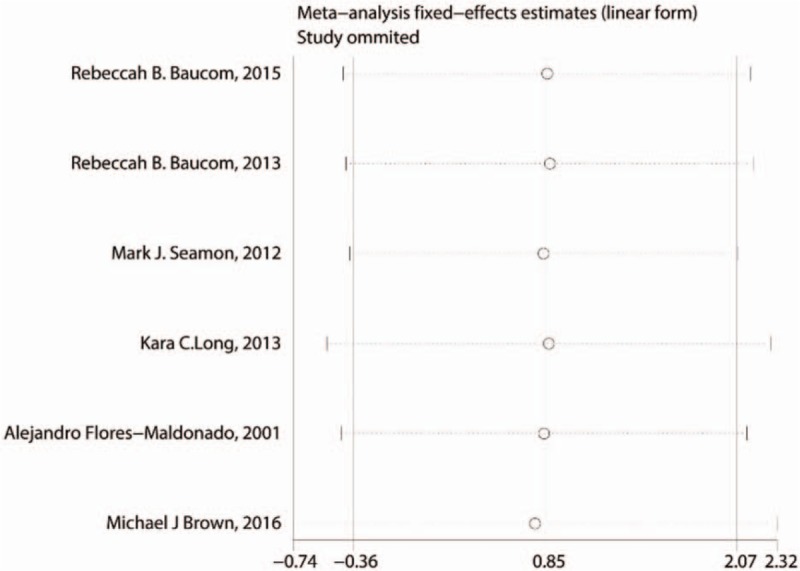
Sensitivity analysis plots of the included observational studies focusing on the association between the perioperative hypothermia and surgical site infection risk.
Figure 5.
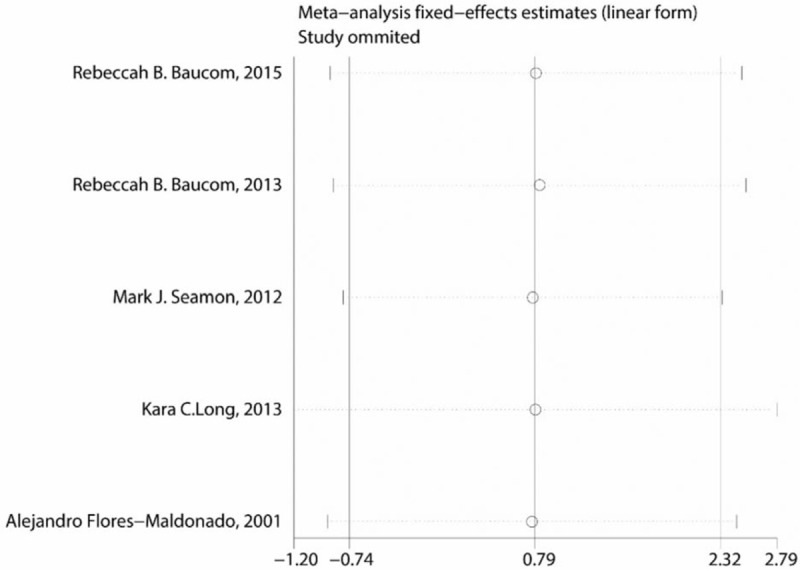
Sensitivity analysis plots of the included cohort studies focusing on the association between the perioperative hypothermia and surgical site infection risk.
3.5. Publication bias
Begg's test with funnel plot asymmetry was used to assess potential bias in the observational studies and cohort studies and identify small study effects on the association between perioperative hypothermia and SSI risk. The funnel plot (P = .133, .462, respectively), which is shown in Figures 6 and 7, did not reveal marked deviations from symmetry, thus indicating a low probability of publication/selection bias.
Figure 6.
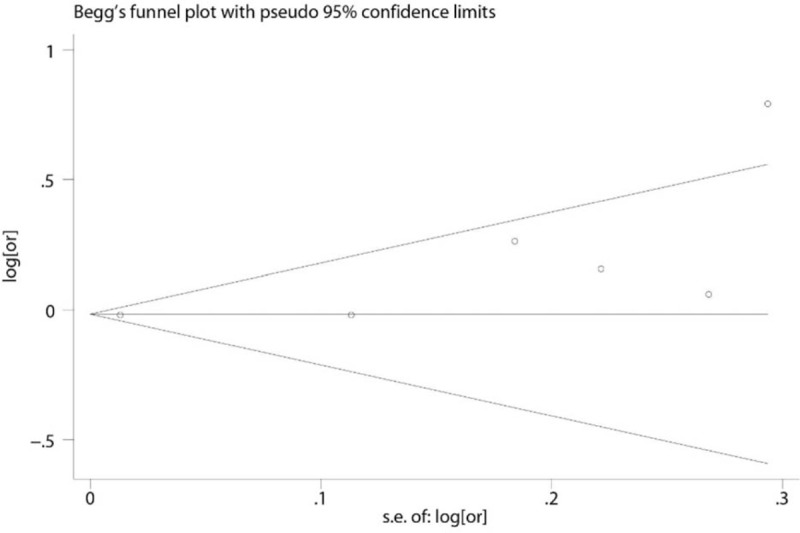
Funnel plot of studies evaluating the association the association between the perioperative hypothermia and surgical site infection risk in the observational studies. The Begg regression asymmetry test (P = .133).
Figure 7.
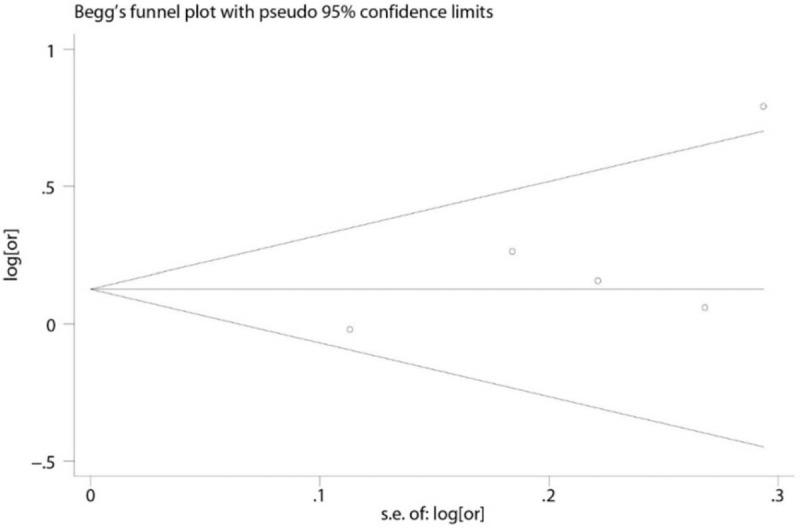
Funnel plot of studies evaluating the association the association between the perioperative hypothermia and surgical site infection risk in cohort studies. The Begg regression asymmetry test (P = .462).
4. Discussion
In the current meta-analysis, we evaluated the association between perioperative hypothermia and SSI risk. Eight published articles, namely, 2 randomized controlled trials, one case–control study, and 5 cohort studies, were selected. Randomized controlled trials and observational studies were performed respectively. Because the number of randomized controlled trials was low, their results were consistent. Hence, the power of pooled OR results in the randomized controlled studies was little. We found evidence from observational studies that suggested no association between perioperative hypothermia and SSI risk in the surgical population.
Because the first report on hypothermia and its association with SSI was published in 1996,[7] numerous clinical trials have been conducted on perioperative hypothermia and the risk of wound infection. In investigations on the link between perioperative hypothermia and the risk of SSI, similar results were obtained by previous studies.[9,14,15,17,19] Baucom et al[15] indicated no correlation between perioperative hypothermia and 30-day SSI in patients who underwent ventral hernia repair. The new study of this team further explored the association between perioperative hypothermia and SSI by using accurate perioperative temperature measurements and 4 definitions of perioperative hypothermia among patients who underwent elective segmental colectomy. The results indicated that perioperative hypothermia was independent of SSI.[9] Another study using continuously intraoperative temperature measurements to examine 1008 colorectal surgery patients also found no correlation between perioperative hypothermia and SSI.[19] Meanwhile, Geiger et al[8] retrospectively collected data on the same surgical population and demonstrated that low intraoperative temperatures were related to low SSI rates. Their results were similar to those of Edwards et al[20] who reported that women who did not develop postcesarean infections have lower mean temperatures than those who developed such infections during cesarean delivery. Moreover, recent data on a plastic surgery population obtained using multivariate models demonstrated that perioperative hypothermia was not associated with wound complications.[21] These studies demonstrated that the clinical importance of the effect the temperature on SSI risk might seem low. Other factors, such as surgery duration, surgery complexity, and patient frailty, seem to be greatly indicative of the decreased incidence of SSI .[22]
By contrast, the result from Kurz et al[7] showed that the incidence of wound infection increases 3 times when the body temperature is 2°C lower than the normal temperature. The underlying mechanism might be that hypothermia directly affecting the immunity of antibodies and cells and indirectly decreasing oxygenation due to local tissue vasoconstriction, thereby increasing the susceptibility to SSI.[23] Based on this randomized study, active perioperative warming was recommended to reduce the rate of SSI. However, this study has several limitations. Given that the subjects in the hypothermia group had a higher volume of blood transfusions intraoperatively, they had a greater risk of SSI than those in the normothermic group. Moreover, the number of patients who underwent SSI was relatively small in the normothermic group. Subsequently, several other studies obtained similar conclusions.[16,18] By contrast, these studies using various definitions of hypothermia and single temperature measurement time points as variables to explore the association with SSI revealed an association between hypothermia and SSI.[17] Meanwhile, forced-air warming devices might interfere ultraclean operating room airflow, thus potentially contaminating the surgical site and further increasing the susceptibility to SSI.[24–26]
Although our study did not suggest an association between perioperative hypothermia and SSI in patients who underwent surgery, the effect of perioperative temperature on clinical outcomes was reasonably important because hypothermia had been associated with other adverse outcomes. However, in the present era of precision medicine, we need to identify and minimize the efforts that produce costs without achieving improvements. Besides, under the state of anesthesia, body temperatures mildly <36°C might be protective,[8] owing to the decrease in the body's metabolism. Therefore, the optimal timing of active warming in surgical patients should be accurately reflected to minimize waste of health resources,[9] and the percentage of duration time of the temperature nadir warrants further exploration regarding its potential significance to clinical outcomes.[15]
The limitations of the current meta-analysis are as follows. First, only 5 cohort studies were performed mainly because the number of randomized controlled trials was low. Second, a subgroup analysis for exploring the influence of variables, such as the types of surgery and the types of infection, on the risk of SSI was not performed due to the limited articles and unavailability of variables.
In conclusion, our study suggests that perioperative hypothermia is not associated with the risk of SSI in observational studies. However, evidence from randomized controlled studies was not found to confirm this association owing to only 2 studies were included in this meta-analysis. Therefore, this result should be interpreted with caution, and considerably more work should be done. Large-scale, randomized-controlled, prospective clinical trials involving the duration and degree of hypothermia should be performed. A cut-off point for temperature under conditions of anesthesia might also be explored.
Author contributions
Ning Bu and Wei Gao designed this study; Enfa Zhao and Yuan Gao collected and collated case data; Sha Zhao and Bo Wang extracted and confirmed the data; Ning Bu and Zhidong Kong analyzed data; Ning Bu and Enfa Zhao wrote the manuscript; Qiang Wang and Wei Gao edited the manuscript.
Conceptualization: Ning Bu.
Data curation: Yuan Gao, Sha Zhao, Wang Bo, Zhidong Kong.
Formal analysis: Ning Bu, Enfa Zhao.
Project administration: Qiang Wang.
Software: Ning Bu, Enfa Zhao.
Validation: Qiang Wang.
Writing – original draft: Ning Bu, Enfa Zhao.
Writing – review & editing: Qiang Wang, Wei Gao.
Footnotes
Abbreviations: CI = confidence interval, ES = effect size, OR = odds ratio, SSI = surgical site infection.
Competing interests: The authors declare no competing financial interests.
The authors have no conflicts of interest to disclose.
References
- [1].Burger] L, Fitzpatrick J. Prevention of inadvertent perioperative hypothermia. Br J Nurs 2009;18:11141116-9. [DOI] [PubMed] [Google Scholar]
- [2].Sessler DI. Complications and treatment of mild hypothermia. Anesthesiology 2001;95:531–43. [DOI] [PubMed] [Google Scholar]
- [3].Sessler DI. Temperature monitoring and perioperative thermoregulation. Anesthesiology 2008;109:318–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Allegranzi B, Bischoff P, de Jonge S, et al. New WHO recommendations on preoperative measures for surgical site infection prevention: an evidence-based global perspective. Lancet Infect Dis 2016;16:e276–87. [DOI] [PubMed] [Google Scholar]
- [5].Belda FJ, Aguilera L, Garcia de la Asuncion J, et al. Supplemental perioperative oxygen and the risk of surgical wound infection: a randomized controlled trial. JAMA 2005;294:2035–42. [DOI] [PubMed] [Google Scholar]
- [6].Magill SS, Edwards JR, Bamberg W, et al. Multistate point-prevalence survey of health care-associated infections. N Engl J Med 2014;370:1198–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Kurz A, Sessler DI, Lenhardt R. Perioperative normothermia to reduce the incidence of surgical-wound infection and shorten hospitalization. Study of Wound Infection and Temperature Group. N Engl J Med 1996;334:1209–15. [DOI] [PubMed] [Google Scholar]
- [8].Geiger T, Horst S, Muldoon R, et al. Perioperative core body temperatures effect on outcome after colorectal resections. Dis Colon Rectum 2011;54:e44–5. [PubMed] [Google Scholar]
- [9].Baucom RB, Phillips SE, Ehrenfeld JM, et al. Association of perioperative hypothermia during colectomy with surgical site infection. JAMA Surg 2015;150:570–5. [DOI] [PubMed] [Google Scholar]
- [10].Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med 2002;21:1539–58. [DOI] [PubMed] [Google Scholar]
- [11].Higgins JP, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. BMJ 2003;327:557–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics 1994;50:1088–101. [PubMed] [Google Scholar]
- [13].Flores-Maldonado A, Medina-Escobedo CE, Rios-Rodriguez HM, et al. Mild perioperative hypothermia and the risk of wound infection. Arch Med Res 2001;32:227–31. [DOI] [PubMed] [Google Scholar]
- [14].Long KC, Tanner EJ, Frey M, et al. Intraoperative hypothermia during primary surgical cytoreduction for advanced ovarian cancer: risk factors and associations with postoperative morbidity. Gynecol Oncol 2013;131:525–30. [DOI] [PubMed] [Google Scholar]
- [15].Baucom RB, Phillips SE, Ehrenfeld JM, et al. Defining intraoperative hypothermia in ventral hernia repair. J Surg Res 2014;190:385–90. [DOI] [PubMed] [Google Scholar]
- [16].Melling AC, Ali B, Scott EM, et al. Effects of preoperative warming on the incidence of wound infection after clean surgery: a randomised controlled trial. Lancet 2001;358:876–80. [DOI] [PubMed] [Google Scholar]
- [17].Brown MJ, Curry TB, Hyder JA, et al. Intraoperative hypothermia and surgical site infections in patients with class i/clean wounds: a case-control study. J Am Coll Surg 2017;224:160–71. [DOI] [PubMed] [Google Scholar]
- [18].Seamon MJ, Wobb J, Gaughan JP, et al. The effects of intraoperative hypothermia on surgical site infection: an analysis of 524 trauma laparotomies. Ann Surg 2012;255:789–95. [DOI] [PubMed] [Google Scholar]
- [19].Melton GB, Vogel JD, Swenson BR, et al. Continuous intraoperative temperature measurement and surgical site infection risk: analysis of anesthesia information system data in 1008 colorectal procedures. Ann Surg 2013;258:606–12. discussion 612-603. [DOI] [PubMed] [Google Scholar]
- [20].Edwards RK, Madani K, Duff P. Is perioperative hypothermia a risk factor for post-cesarean infection? Infect Dis Obstet Gynecol 2003;11:75–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Constantine RS, Kenkel M, Hein RE, et al. The impact of perioperative hypothermia on plastic surgery outcomes: a multivariate logistic regression of 1062 cases. Aesth Surg J 2015;35:81–8. [DOI] [PubMed] [Google Scholar]
- [22].Korol E, Johnston K, Waser N, et al. A systematic review of risk factors associated with surgical site infections among surgical patients. PLoS One 2013;8:e83743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Cattaneo CG, Frank SM, Hesel TW, et al. The accuracy and precision of body temperature monitoring methods during regional and general anesthesia. Anesth Analg 2000;90:938–45. [DOI] [PubMed] [Google Scholar]
- [24].Albrecht M, Gauthier R, Leaper D. Forced-air warming: a source of airborne contamination in the operating room? Orthop Rev 2009;1:e28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Wood AM, Moss C, Keenan A, et al. Infection control hazards associated with the use of forced-air warming in operating theatres. J Hosp Infect 2014;88:132–40. [DOI] [PubMed] [Google Scholar]
- [26].McGovern PD, Albrecht M, Belani KG, et al. Forced-air warming and ultra-clean ventilation do not mix: an investigation of theatre ventilation, patient warming and joint replacement infection in orthopaedics. J Bone Joint Surg Br 2011;93:1537–44. [DOI] [PubMed] [Google Scholar]


