Abstract
Background:
The risk of falls among adults with knee osteoarthritis (OA) has been documented, yet, to our knowledge no studies have examined knee OA and medically treated injurious falls (hereafter injurious falls) (overall and by sex), an outcome of substantial clinical and public health relevance.
Methods:
Using data from the Health ABC Knee Osteoarthritis Substudy, a community-based study of white and black older adults, we tested associations between knee OA status and the risk of injurious falls among 734 participants with a mean (SD) age of 74.7 (2.9) years. Knee radiographic osteoarthritis (ROA) was defined as having a Kellgren-Lawrence grade of ≥2 in at least one knee. Knee symptomatic ROA (sROA) was defined as having both ROA and pain symptoms in the same knee. Injurious falls were defined using a validated diagnoses code algorithm from linked Medicare Fee-for-Service claims. Cox regression modeling was used to estimate hazard ratios (HRs) and 95% confidence intervals (CIs).
Results:
The mean (SD) follow-up time was 6.59 (3.12) years. Of the 734 participants, 255 (34.7%) had an incident injurious fall over the entire study period. In the multivariate model, compared with those without ROA or pain, individuals with sROA (HR=1.09; 95% CI: 0.73, 1.65) did not have a significantly increased risk of injurious falls. Compared with men without ROA or pain, men with sROA (HR=2.57; 95% CI: 1.12, 5.91) had a significantly higher risk of injurious falls. No associations were found for women or by injurious fall type.
Conclusion:
Knee sROA was independently associated with an increased risk of injurious falls in older men, but not in older women.
Keywords: radiographic and symptomatic knee osteoarthritis, pain, incidence, injurious falls
Introduction
Knee osteoarthritis (OA) is a common and disabling chronic condition among older adults (ages ≥65 years) (1). In the US, the prevalence of knee radiographic OA (ROA) and symptomatic ROA (sROA) among adults aged ≥60 years was 37.4% and 12.1%, respectively, thus, about 1 in 3 adults with knee OA report pain. (2). The prevalence of knee ROA is significantly higher in women versus men, 42.1% vs 31.2%, but knee sROA prevalence did not differ by sex. (2). Furthermore, the lifetime risk to age 85 years of knee sROA was estimated to be about 45% and did not vary by sex (3). Knee OA may lead to reduced quality of life (4) and early retirement (5). Major health outcomes associated with knee OA include expensive joint replacement (620,000 OA-attributable knee replacements in the U.S. in 2010) (6), and possibly an increased risk of mortality (7, 8).
Falls are the leading cause of injury-related morbidity and mortality among older adults, with more than one in four older adults falling each year(9), resulting in direct medical costs of about $32 billion in 2015 (10). Major fall-related injuries among older adults, including hip fractures and brain injuries, are associated with a decline in functional abilities and reductions in social and physical activities (11).
In a systematic review of 12 studies, 17% of the falls were attributed to gait/balance disorders or weakness as the most likely cause, common characteristics of adults with knee OA (11). A fairly recent study, among adults with knee OA, showed that lower knee extension muscle strength and lower knee flexion muscle strength were associated with increased falls(12). Moreover, poor or declining physical function are risk factors for fractures, 95% of which occur because of a fall (13–16). Multiple cross-sectional studies have examined the association between knee OA and falls yielding primarily null associations (17–19). Several studies have examined the association between baseline knee OA and risk of incident falls with some indicating an increase in the risk of falls (20–22) and others finding a null result (23, 24). Knee OA severity appears to impact the risk of falls with greater severity linked to a higher rate of falls. (25) Other knee OA related outcomes such as knee arthroplasty and knee instability have been examined in regards to falls. Interestingly, adults with knee arthroplasty do not appear to have an increased risk of falls compared with adults without knee arthroplasty(26, 27), whereas knee instability has been shown to be associated with a greater prevalence of recurrent falls(28). Yet, injurious falls are an outcome of greater clinical and public health relevance (29). Two cross-sectional studies found higher prevalence of injurious falls among adults with doctor-diagnosed arthritis (two times greater) (30) and lower limb arthritis (about 1.3 times greater) (31). A longitudinal study of community-dwelling older adults showed a 40% increased risk of self-reported injurious falls among adults with arthritis or rheumatism (32). However, to our knowledge, the association between knee OA and incident injurious falls has not been examined. If risk of injurious falls is higher among older adults with knee OA, targeted therapy/programs which would modify function and/or pain for those with elevated risk, would be beneficial to reduce morbidity and mortality from falls.
To address this substantial knowledge gap, we examined the association between knee OA (for both ROA and sROA) and treated incident injurious falls among community-dwelling white and black older men and women, from the Health Aging and Body Composition (Health ABC) Knee Osteoarthritis Substudy.
Furthermore, we also performed a priori secondary analyses stratified by sex and by injurious falls type (fracture versus non-fracture). Because of sex differences in pain threshold, reporting of pain, pain impacts on behavior, and overall risk behavior, it was important to examine these associations in men and women, separately. Moreover, it is important to stratify by sex as there is evidence that sex hormones influence the development of osteoarthritis and osteoporosis/fracture risk, practically via the reduction of estrogen levels in post-menopausal women (33).
Methods
Study Population
The parent Health ABC study enrolled 3,075 women and men, aged 70–79, from two field centers, Pittsburgh, PA and Memphis, TN at visit 1 (baseline, 1997–1998). Participants had to report no difficulty walking at least 1/4 mile and or climbing a flight of stairs to be eligible to participate. White participants were identified from a random sample of white Medicare beneficiaries. Black subjects were identified as age-eligible community residents from designated ZIP code areas surrounding Pittsburgh PA and Memphis TN. Exclusion criteria included reported difficulty performing basic activities of daily living, obvious cognitive impairment, inability to communicate with the interviewer, intention of moving within 3 years, or participation in a trial involving a lifestyle intervention. There were 3,044 enrollees that remained at visit 2 (1998–1999).
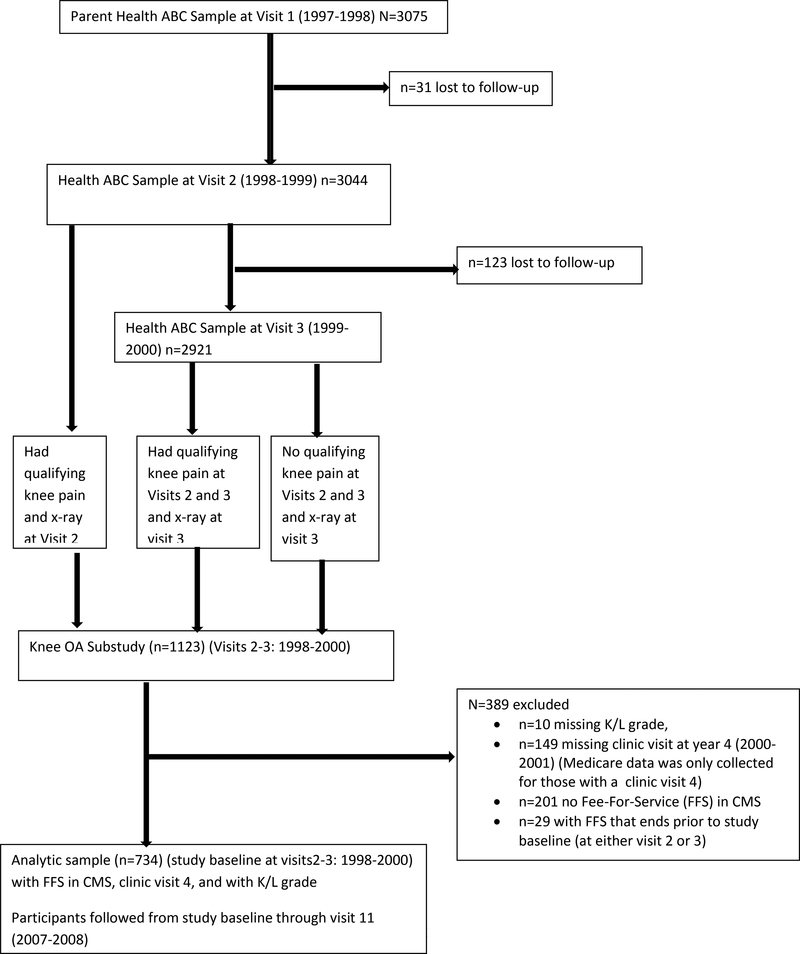
The Health ABC Knee Osteoarthritis Substudy included 1123 participants from visits 2 (1998–1999) or 3 (1999–2000) (Figure). Participants were included in the knee Osteoarthritis Substudy at visit 2 if they had qualifying knee pain and knee x-ray. Cases with qualifying knee pain were identified if they had “knee pain, aching, or stiffness on most days for at least 1 month” at some point over the previous year or if they reported moderate or worse knee pain during the previous month in association with at least one activity on the Western Ontario and McMaster Universities Arthritis Index (WOMAC) knee pain scale (34). Additional participants with qualifying pain were added at visit 3 if they had qualifying knee pain at both visits 2 and 3, and knee x-ray at visit 3. Finally, a random set of 270 controls (with no qualifying pain at either visit 2 or 3) with knee x-ray at visit 3 were selected from 1798 participants for inclusion in the knee Osteoarthritis Substudy (35).
Figure:
Flow chart for creating the analytic sample
Participants included in the analytic sample (n=734) were those that were followed after study baseline (i.e., visits 2 or 3 in 1998–2000), with a clinic visit 4 (Medicare data was only collected for those with a clinic visit 4 (2000–2001)), did not have a missing K/L grade reading of their knee x-ray, and had Medicare fee-for-service (FFS) in CMS (to ascertain injurious falls status) that extended beyond study baseline enrollment date (1998–2000) (Figure). Participants in the analytic study were followed from study baseline (1998–2000) until the occurrence of an injurious fall, the loss of FFS, loss to follow-up, death, or through visit 11 (2007–2008) (when Medicare claims were last collected for this study). Injurious fall status was assessed during this time period of FFS in the CMS dataset. The institutional review board at each center approved the study protocol, and written informed consent was obtained from all the participants.
Exposure Variable of Knee OA and Pain
At both visits 2 and 3, expert readers assessed posterior-anterior and skyline projection knee x-rays to assess Kellgren-Lawrence (K/L) grade based on individual radiographic features (joint space narrowing, osteophytes, subchondral attrition, cysts and sclerosis) and scored using the Osteoarthritis Research Society International atlas in the medial and lateral compartment of the tibio-femoral joint and the patello-femoral joint (36). Participants had x-rays at either visits 2 or 3. Follow-up began at either V2 or V3 depending on when the x-ray was taken. Inter-rater reliability was excellent (weighted kappa 0.87 for K/L grade). Knee ROA was defined as a K/L grade ≥ 2.
Adults were categorized into 4 mutually exclusive groups: knee sROA, knee ROA without pain, knee pain without ROA, and no ROA or pain. During the clinic visit when knee imaging was completed, participants were asked if they had, “knee pain on most days in the past 30 days”. Knee pain was defined as having pain symptoms (during the majority of the last 30 days) in at least one knee. Knee ROA was defined as having a Kellgren-Lawrence grade of ≥2 in at least one knee. Knee sROA was defined as having both ROA and pain symptoms in the same knee.
Injurious Falls
Incident injurious falls were ascertained from outpatient and inpatient Medicare claims and defined using a diagnosis code algorithm from linked Medicare claims. All injuries captured in Medicare claims are included, which includes any outpatient care billed by any type of provider. Any unique event with an ICD-9 fall code (E880–888) plus non-fracture injury, a vertebral fracture code (805–806) with a fall code, or any non-vertebral fracture code (800–804, 807–829) with/without a fall code was considered an injurious fall as an estimated 80% of non-vertebral fractures are attributed to falls (37). All traumatic injuries (e.g. motor vehicle accidents), intentional injuries and pathologic injuries were not considered to meet the definition of an injurious fall.
In the adjudication of our diagnoses code algorithm as previously detailed (38), a subset of Medicare fall injuries were compared to the self-reported fall injuries with medical records. The injuries adjudicated were included due to potential uncertainty of particular diagnoses codes to classify a primary injurious fall: concurrent stroke code; fall code with uncertain injury; fracture code that was not in 1st or 2nd position (i.e., not listed as the 1st or 2nd reason for visit/hospitalization billing); vertebral column/rib fracture without a fall code. Overall, the injurious fall adjudication showed an excellent agreement, except for vertebral fractures where only 50% of vertebral fractures were confirmed. We revised the initial diagnoses code algorithm to exclude vertebral fractures without concurrent fall codes.
Covariates Evaluated for Inclusion in Models
All covariates evaluated for inclusion in models were measured once at either visit 1 or 2. Potential covariates associated with the exposure or outcome at p<0.1 were included in the full multivariate adjusted model. If covariates were available at both visits the visit one measurement was used. These potential covariates were selected based on documented associations with knee OA and falls. Demographic variables included self-report of age, sex, race (white or black), and education (<high school (HS), HS graduate, or postsecondary), and study site (Memphis or Pittsburgh). Weight was measured on a standard balance beam scale to the nearest 0.1 kg. Height was measured by a stadiometer to the nearest 0.1 cm. The anthropometric measure of BMI (kg/m2) was calculated using the formula weight (kg)/height2 (m2).
Lifestyle factors included self-report of smoking (never, past smoker, current smoker) and physical activity (kcal/kg/wk). Physical activity was determined using the caloric expenditure in the past week for self-reported duration of walking, climbing stairs, and exercise (39).
Several medical characteristics were considered for the analysis. Participants self-reported their current health status (fair/poor/very poor versus good/very good/excellent) and history of falls in the past 12 months, depression, poor vision, myocardial infarction, and stroke. Diabetes was defined using fasting glucose (≥126 mg/dl), self-report, or hypoglycemic medication use. Diagnosed and/or treated hypertension (hypertension hereafter) was defined via self-report or antihypertensive medication use. To assess supplementary intake for vitamin D and calcium, and medication use such as non-steroidal anti-inflammatory drugs (NSAIDs), statins, steroid use, and antidepressants, participants were asked to bring all prescription and over the counter medications, which were coded based on the Iowa Drug Information System (40). Total number of other medications was assessed using number of other prescription medications (excluding steroids & antidepressants).
Statistical Analysis
Chi-square tests were used to evaluate proportion differences for incident injurious falls across study covariates. Two-sample t-tests (Wilcoxon rank-sum test for non-normally distributed data) were used to examine mean differences in continuous covariates by incident injurious falls status. To compare baseline knee OA status by study covariates chi-square tests were performed to assess proportion differences. Fisher’s exact test was performed for all tests of proportion if the expected value for any cell was <5. To compare mean differences in continuous covariates by baseline knee OA status ANOVA (Kruskal-Wallis test for non-normally distributed data) was performed.
Cox proportional-hazards models were used to estimate hazard ratios (HRs) with 95% confidence intervals (CIs) and compare the time from the visits 2 or 3 (depending on when x-ray was taken) to incident injurious falls by baseline knee OA status (knee sROA, knee pain without ROA, knee ROA without pain groups compared with reference group (no ROA or pain)), while controlling for potential confounders. Participants were right censored if they did not have the event of interest by the time they were lost to follow-up, their follow-up ended, or by the time of their death. Individuals with missing covariate data were dropped from the multivariate analyses. Furthermore, we performed a priori secondary analyses stratified by sex and by injurious falls type (fracture versus non-fracture). The proportional hazards assumption was assessed by testing (1) the interaction of knee OA indicator variables (sROA, ROA without pain, or pain without ROA, vs. no ROA/no pain) with log(time) and (2) the knee OA indicator variables using the Supremum test based on Schoenfeld residuals, in full multivariate adjusted models. The proportional hazards assumption was considered violated if p<0.05 for the knee OA indicator variables*log(time) interaction terms or knee OA indicator variables. Knee OA did not violate the proportional hazards assumption in the full multivariate adjusted overall, sex-stratified and injury type-stratified models.
All analyses were performed using the Statistical Analysis System (SAS, version 9.3; SAS Institute, Cary, NC, USA). Statistical significance for all analyses was determined at the α<0.05 level.
Results
Overall
The mean (SD) follow-up time was 6.59 (3.12) years. The mean (SD) age of the participants was 74.7 (2.9) years. There were 249 participants with sROA, 32 had ROA without pain, 306 had pain without ROA, and 147 without pain or ROA in either knee. Of the 734 participants, 255 (34.7%) had an incident injurious fall over the entire study period. The average annual incidence rate of injurious falls across 11 years (from 1998 through 2008) was 4.84 per 100 person-years (p-yrs). The incidence rate per 100 p-yrs of injurious falls by year was 0.7 (1998), 3.0 (1999), 4.0 (2000), 5.8 (2001), 5.2 (2002), 3.7 (2003), 4.8 (2004), 5.4 (2005), 3.2 (2006), 6.8 (2007), and 10.3 (2008). Table 1 shows the distributions of baseline knee OA status and incident injurious falls by baseline characteristics. Baseline knee OA status differed significantly by race, site, health status, history of falls, hypertension status, NSAID use, or steroid use (Table 1). Women, whites, those who had higher education, never smoked, better health, or no heart disease, or those who took calcium or vitamin D supplements, anti-depressants, or steroids were significantly more likely to have an incident injurious fall by end of follow-up (Table 1). Mean age and BMI varied significantly by knee OA status (p<0.01 for both). Baseline mean age was higher (75.1 vs. 74.5 years, p=0.01) and baseline mean BMI was lower (27.3 vs. 28.3 kg/m2, p=0.01) among adults with an incident injurious fall by end of follow-up. Median physical activity did not significantly differ by knee ROA status (p=0.35). Baseline median physical activity was 2.4 kcal/kg/week for those with an incident injurious fall and 2.2 kcal/kg/week for those without an incident injurious by end of follow-up, p=0.09. Number of other prescription medications (excluding steroids & antidepressants) differed by knee OA status (knee sROA=3.64, knee ROA without pain=2.81, pain with knee ROA=3.74, no knee pain or ROA=2.51, p<0.01) and was borderline significantly higher among adults with an injurious fall (3.61 vs. 3.18, p=0.05).
Table 1.
Distributions of baseline knee OA status and incident injurious falls by baseline characteristics (N=734)a
| Knee sROA (K/L≥2 + symptoms) (n=249) |
Knee ROA without pain (K/L≥2) (n=32) |
Pain without knee ROA (n=306) |
No knee pain or ROA (n=147) |
P-value for characteristics by knee OA status |
Injurious fall (n=255) |
P-value for characteristics by injurious falls status | |
|---|---|---|---|---|---|---|---|
| Overall | 33.9 | 4.4 | 41.7 | 20.0 | - | 34.7 | - |
| Demographic Characteristics | |||||||
| Sex | 0.32 | <0.01 | |||||
| Men | 31.3 | 4.2 | 41.3 | 23.3 | 26.7 | ||
| Women | 35.7 | 4.5 | 41.9 | 17.9 | 39.9 | ||
| Race | <0.01 | <0.01 | |||||
| Whites | 29.3 | 2.1 | 47.4 | 21.2 | 42.7 | ||
| Blacks | 40.3 | 7.4 | 33.9 | 18.4 | 23.9 | ||
| Site | 0.01 | 0.10 | |||||
| Pittsburgh | 40.3 | 3.1 | 36.8 | 19.8 | 38.1 | ||
| Memphis | 29.1 | 5.3 | 45.4 | 20.2 | 32.2 | ||
| Education | 0.28 | <0.01 | |||||
| <High school | 37.4 | 6.6 | 37.4 | 18.5 | 26.1 | ||
| High school graduate | 29.9 | 3.6 | 45.7 | 20.8 | 32.6 | ||
| Postsecondary | 34.8 | 3.3 | 41.5 | 20.4 | 42.8 | ||
| Lifestyle Characteristics | |||||||
| Smoking | 0.19 | 0.04 | |||||
| Never | 37.2 | 4.3 | 40.1 | 18.5 | 37.2 | ||
| Past smoker | 33.0 | 4.4 | 43.2 | 19.4 | 35.0 | ||
| Current smoker | 20.6 | 4.8 | 44.4 | 30.2 | 20.6 | ||
| Health status | 0.04 | 0.04 | |||||
| Fair/poor/very poor | 41.9 | 5.7 | 40.3 | 12.1 | 26.6 | ||
| Good/very good/excellent | 32.3 | 4.1 | 42.0 | 21.6 | 36.4 | ||
| Medical Characteristics | |||||||
| History of Falls last 12 months | 0.02 | 0.22 | |||||
| Yes | 31.9 | 2.7 | 50.8 | 14.6 | 38.4 | ||
| No | 34.6 | 4.8 | 38.8 | 21.9 | 33.5 | ||
| Diabetes | 0.59 | 0.08 | |||||
| Yes | 33.3 | 5.3 | 44.4 | 17.0 | 29.2 | ||
| No | 34.1 | 4.1 | 40.9 | 21.0 | 36.4 | ||
| Hypertension | 0.02 | 0.45 | |||||
| Yes | 38.1 | 4.8 | 40.4 | 16.8 | 33.5 | ||
| No | 29.1 | 3.8 | 43.2 | 23.8 | 36.2 | ||
| Stroke | 0.20 | 0.89 | |||||
| Yes | 25.0 | 8.3 | 33.3 | 33.3 | 33.3 | ||
| No | 34.2 | 4.2 | 42.1 | 19.5 | 34.8 | ||
| Myocardial infarction | 0.42 | 0.02 | |||||
| Yes | 32.4 | 7.4 | 36.8 | 23.5 | 22.1 | ||
| No | 34.3 | 4.1 | 42.2 | 19.5 | 36.1 | ||
| Depression | 0.61 | 0.34 | |||||
| Yes | 39.1 | 2.2 | 45.7 | 13.0 | 41.3 | ||
| No | 33.5 | 4.6 | 41.5 | 20.4 | 34.4 | ||
| Poor vision | 0.33 | 0.22 | |||||
| Yes | 35.2 | 3.6 | 42.9 | 18.3 | 36.6 | ||
| No | 32.3 | 5.3 | 40.1 | 22.3 | 32.3 | ||
| Calcium supplement | 0.38 | <0.01 | |||||
| Yes | 29.7 | 3.5 | 47.1 | 19.8 | 45.9 | ||
| No | 35.3 | 4.5 | 40.1 | 20.1 | 31.2 | ||
| Vitamin D supplement | 0.81 | 0.02 | |||||
| Yes | 35.6 | 2.3 | 40.2 | 21.8 | 46.0 | ||
| No | 33.8 | 4.5 | 42.0 | 19.8 | 33.1 | ||
| Antidepressant use | 0.50 | 0.03 | |||||
| Yes | 26.1 | 4.4 | 56.5 | 13.0 | 56.5 | ||
| No | 34.2 | 4.2 | 41.3 | 20.2 | 34.0 | ||
| Statin use | 0.84 | 0.25 | |||||
| Yes | 30.6 | 5.1 | 43.9 | 20.4 | 39.8 | ||
| No | 34.5 | 4.1 | 41.5 | 19.9 | 33.9 | ||
| NSAID use | <0.01 | 0.09 | |||||
| Yes | 46.4 | 4.1 | 43.8 | 5.7 | 39.7 | ||
| No | 29.5 | 4.3 | 41.0 | 25.2 | 32.8 | ||
| Steroid use | 0.04 | 0.01 | |||||
| Yes | 23.8 | 4.8 | 61.9 | 9.5 | 54.8 | ||
| No | 34.5 | 4.3 | 40.5 | 20.7 | 33.5 | ||
| Knee OA status | - | 0.15 | |||||
| sROA | - | - | - | - | 35.3 | ||
| ROA | - | - | - | - | 28.1 | ||
| Pain without ROA | - | - | - | - | 38.2 | ||
| No pain or ROA | - | - | - | - | 27.9 |
Abbreviations: SD, standard deviation; BMI, body mass index; IQR, interquartile range; NSAID, nonsteroidal anti-inflammatory drug
Data from the Health Aging and Body Composition (Health ABC) study, a US cohort study of 3,075 women and men, aged 70–79
Among Men
There were a total of 77 injurious falls out of 288 (26.7%) men, and the cumulative incidence varied by knee OA status. The cumulative incidence of injurious falls by knee OA group was 33.3% for sROA, 16.7% for ROA without pain, 29.4% for pain without ROA, and 14.9% for no ROA or pain.
Among Women
There were 178 injurious falls out of 446 (39.9%) participants, and the cumulative incidence did not vary by knee OA status. The cumulative incidence of injurious falls by knee OA group was 36.5% for sROA, 35.0% for ROA without pain, 43.9% for pain without ROA, and 38.8% for no ROA or pain.
Multivariate Analyses
In the multivariate model with men and women combined, compared with those without ROA or pain, individuals with sROA (HR=1.09; 95% CI: 0.73, 1.65), ROA without pain (HR=1.01; 95% CI: 0.46, 2.20), and pain without ROA (HR=1.08; 95% CI: 0.74, 1.57) did not have a significantly increased risk of injurious falls (Table 2). Among men only, and compared with men without ROA or pain, those with sROA (HR=2.57; 95% CI: 1.12, 5.91) had a significantly higher risk of injurious falls (Table 2). No significant association existed between knee OA and injurious falls in women. The 4*2 interaction term predicting injurious falls between knee OA and sex was not statistically significant (p>0.05); however, interpretation of this result should be viewed with caution as this analysis was likely underpowered as a result of the low number of adults with ROA and no pain. The association between knee OA and injurious falls did not differ by injurious fall type (fracture versus non-fracture) (Table 3).
Table 2.
Adjusted risk of injurious falls associated with knee sROA, knee ROA without pain, and knee pain without ROA, overall and by sex
| Number with injurious falls | Knee sROAa HR (95% CI) |
Knee ROA without Paina HR (95% CI) |
Knee pain without ROAa HR (95% CI) |
|
|---|---|---|---|---|
| Overallb | ||||
| Age-adjusted (N=734) | 255 | 1.05 (0.72, 1.52) | 0.91 (0.44, 1.87) | 1.15 (0.80, 1.64) |
| Full MV model (n=714) | 249 | 1.09 (0.73, 1.64) | 1.11 (0.51, 2.44) | 1.05 (0.72, 1.54) |
| Menb | ||||
| Age-adjusted (N=288) | 77 | 1.86 (0.91, 3.83) | 0.93 (0.20, 4.25) | 1.73 (0.85, 3.50) |
| Full MV model (n=278) | 75 | 2.59 (1.13, 5.98) | 1.19 (0.25, 5.68) | 2.03 (0.94, 4.37) |
| Womenb | ||||
| Age-adjusted (N=446) | 178 | 0.76 (0.49, 1.18) | 0.83 (0.36, 1.88) | 0.91 (0.60, 1.38) |
| Full MV model (n=436) | 174 | 0.88 (0.54, 1.43) | 1.13 (0.44, 2.87) | 0.86 (0.56, 1.34) |
Abbreviations: ROA, radiographic osteoarthritis; sROA, Symptomatic ROA; HR, hazard ratio; CI, confidence intervals; MV, multivariate model
The reference group comprises participants without ROA or pain in a knee
Adjusted for age, sex, race education, BMI, physical activity, smoking, health status, history of falls in past 12 months, diabetes, hypertension, myocardial infarction, steroid use, NSAID use, antidepressant use, calcium supplement use, Vitamin D supplement use and total number of other prescription medications (excluding steroid use and antidepressant use)
Excluded participants with no incident injurious falls after x-ray date, but with injurious falls prior to x-ray date
Table 3.
Adjusted risk of fracture and non-fracture injurious falls associated with knee sROA, knee ROA without pain, and knee pain without ROA, overall
| Injurious Fall | Number with injurious falls | Knee sROAa HR (95% CI) |
Knee ROA without paina HR (95% CI) |
Knee pain without ROAa HR (95% CI) |
|---|---|---|---|---|
| Fractureb | ||||
| Age-adjusted (N-667) | 188 | 1.08 (0.70, 1.69) | 1.19 (0.56, 2.51) | 1.18 (0.78, 1.81) |
| Full MV model (n=649) | 184 | 1.18 (0.73, 1.90) |
1.70 (0.75, 3.83) |
1.06 (0.68, 1.66) |
| Non-Fractureb | ||||
| Age-adjusted (N=546) | 67 | 0.99 (0.49, 2.01) | * | 1.18 (0.61, 2.30) |
| Full MV model (n=530) | 65 | 1.08 (0.49, 2.38) | * | 1.22 (0.59, 2.52) |
Abbreviations: ROA, radiographic osteoarthritis; sROA, Symptomatic ROA; HR, hazard ratio; CI, confidence intervals; MV, multivariate model
No non-fracture injuries occurred among participants with knee ROA without pain
The reference group comprises participants without ROA or pain in a knee
Adjusted for age, race, sex, education, BMI, physical activity, smoking, health status, history of falls in past 12 months, diabetes, hypertension, myocardial infarction, steroid use, NSAID use, antidepressant use, calcium supplement use, Vitamin D supplement use and total number of other prescription medications (excluding steroid use and antidepressant use)
Discussion
To our knowledge this is the first study to examine knee OA and risk of treated incident injurious falls. We showed that knee sROA was associated with an increased risk of injurious falls among older community-dwelling men independent of many potential confounders. Knee OA was not a predictor of injurious falls overall, among women, or by injurious fall type (fracture versus non-fracture). Our findings suggest that knee sROA is a risk factor for injurious falls in men, but not women. Fall prevention efforts that target men with knee sROA are need to reduce injurious falls risk.
Men with sROA had a 2.6 fold increased hazard rate of injurious falls compared with men who had no pain or ROA in either knee. In contrast, there was no significant association in women. It is unclear why this association was observed in men only. One potential explanation for this observation is that men are more likely to fall than women under similar conditions of health (e.g., OA) and balance (41). This may be the result of several factors, for instance, women who report pain are more likely to limit their activity than men (42), and men with similar conditions of health are more likely to put themselves in a hazardous situation than women (41). Women may have a lower pain threshold and men are more likely to only report severe pain (43). A recent longitudinal study of three years using data from the Swedish National Study on Aging and Care in Kungsholmen showed that among men with the presence of pain or pain that limited their daily activities there was an increased risk of injurious falls, but for women these associations were null (44). Previous longitudinal studies have not to our knowledge examined knee OA using objectively measured radiographic data and related these to injurious falls treated in Medicare.
However, a few studies have examined radiographically measured knee OA and incident self-reported falls by sex, or in one sex (21, 23, 24). One study among adults followed <3 years showed that knee OA was a significant predictor of falls in women, but not men (21), whereas two others found no association in either sex (23, 24). Further studies using radiographically measured knee OA and injurious falls are needed, based on our initial findings. Comparing these studies is arduous due to the heterogeneity of the study populations and exposures and outcomes.
The mechanism regarding the association between knee OA and injurious falls in men appears to be perceived pain. Among men with knee sROA or pain without ROA there was an over two-fold increased risk of injurious falls when compared with men without ROA or pain. Men with ROA but without pain had a similar incidence of injurious falls as men without ROA or pain. This is not surprising as pain has been shown to be associated with falls in a meta-analysis of 21 studies (45).
History of falls has been shown to be predictor of incident falls(46). In our study, history of falls varied significantly by knee OA status with 50% of adults with pain without ROA having a history of a fall in the last 12 months. However, history of falls did not significantly predict incidence injurious falls in both the univariate and multivariate analyses, suggesting that injurious falls (a proxy for severe falls) may have non-overlapping risk factors when compared with the outcome of falls.
In view of the heterogeneity in the association of knee OA with fall outcomes across studies, it is prudent to consider non-pharmacologic therapies that might help reduce falls risk in older adults, particularly older men with knee OA by improving physical function. For example, EnhanceFitness is an evidence-based community-delivered physical activity program, recommended by the CDC for adults with arthritis and disseminated by many YMCA recreational facilities across the U.S., has been shown to produce substantial improvements (18 to 35%) in function (e.g., muscle strength and balance) (47, 48) and showed that consistent EnhanceFitness users had a 26% reduced risk of falls requiring medical care (49). Increased implementation of this intervention or other physical activity interventions (50) may reduce the risk of injurious falls among adults with knee OA, though further studies are needed.
Our study has notable strengths, including being the first to examine radiographic knee OA and the risk of incident injurious falls. Furthermore, fall injuries were determined from both outpatient and inpatient Medicare claims which allowed outcomes to be collected even if participants did not attend subsequent Heath ABC clinic visits. Medicare includes all potentially relevant health services provided for injurious falls for adults ≥65 years, though would not capture health services provided by the VA which for this age group may affect missingness of health services data in men more than women. These adjudicated injurious falls from Medicare claims may provide a more a complete assessment of injurious falls and also when they occurred versus relying solely on self-reported injurious falls, which are likely subject to recall bias. Moreover, we examined both non-fracture and fracture fall injuries. Finally, we adjusted for many potential confounders, and over a long follow-up period (median over 6.5 years). However, our study has several potential limitations. First, we measured knee OA at baseline only and radiographic and pain changes may occur over time. Second, self-report of certain potential confounders may bias findings (e.g., physical activity). Third, the low prevalence of adults with knee ROA and no pain in this sample may have reduced our power to detect associations with injurious falls in this group. Fourth, the 389 participants taken from the Knee Osteoarthritis Substudy and excluded from the analytic sample varied slightly from the analytic sample, which may impact the generalizability of the findings. Although knee OA, age, sex, and BMI did not differ by group, those excluded were more likely to be black and slightly more educated. In addition, our sample comes from a non-disabled well-functioning population at baseline, which may also affect generalizability. Finally, we adjusted for many potential confounders, but residual confounding is a limitation of all observational studies.
In summary, in a cohort of older men and women, knee sROA was independently associated with a 2.6 fold increased risk of incident injurious falls in men only. More studies are needed to confirm this initial finding and explore why this association was limited to men. Studies with a larger cohort of participants with radiographic evidence of knee OA but no pain are needed to better understand the independent impact of knee OA without pain on injurious falls.
Significant & Innovations.
To our knowledge, no studies have examined the association between knee osteoarthritis and medically treated injurious falls an outcome of substantial clinical and public health relevance.
Compared with men without radiographic osteoarthritis or pain, men with symptomatic radiographic osteoarthritis (Hazard Ratio=2.57; 95% Confidence Interval: 1.12, 5.91) had a significantly higher risk of injurious falls. No association was found for women.
Non-pharmacologic therapies (e.g., physical activity interventions) may help reduce falls risk in older adults, particularly older men with knee OA, by improving physical function. For example, EnhanceFitness is an evidence-based community-delivered physical activity program, recommended by the CDC for adults with arthritis and disseminated by many YMCA recreational facilities across the U.S., has been shown to produce substantial improvements in function (e.g., muscle strength and balance) and may reduce the risk of a medically treated injurious fall.
Acknowledgments
Funding:This work was supported by the National Institute on Aging (NIA) Contracts N01-AG-6–2101; N01-AG-6–2103; N01-AG-6–2106; NIA grant R01-AG028050 (to E.S.S.), and National Institute of Nursing Research grant R01-NR12459. This research was supported in part by the Intramural Research Program of the National Institute of Health, NIA, the University of Pittsburgh Claude D. Pepper Older Americans Independence Center (P30-AG024827) Pilot Grant (to E.S.S.), and National Institute on Aging Training Grant T32-AG000181 (to A.B.N.). In 2016, a preliminary version of this work was presented at the American College of Rheumatology Conference and the American Society for Bone Research Conference.
Footnotes
Conflict of Interest: All authors have no conflict of interest to declare
CDC Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention
References
- 1.Allen KD, Golightly YM. Epidemiology of osteoarthritis: state of the evidence. Current opinion in rheumatology. 2015;27(3):276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dillon CF, Rasch EK, Gu Q, Hirsch R. Prevalence of knee osteoarthritis in the United States: arthritis data from the Third National Health and Nutrition Examination Survey 1991–94. The Journal of rheumatology. 2006;33(11):2271–9. [PubMed] [Google Scholar]
- 3.Murphy L, Schwartz TA, Helmick CG, Renner JB, Tudor G, Koch G, et al. Lifetime risk of symptomatic knee osteoarthritis. Arthritis Care & Research. 2008;59(9):1207–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Salaffi F, Carotti M, Stancati A, Grassi W. Health-related quality of life in older adults with symptomatic hip and knee osteoarthritis: a comparison with matched healthy controls. Aging clinical and experimental research. 2005;17(4):255–63. [DOI] [PubMed] [Google Scholar]
- 5.Karpansalo M, Manninen P, Kauhanen J, Lakka TA, Salonen JT. Perceived health as a predictor of early retirement. Scandinavian journal of work, environment & health. 2004:287–92. [DOI] [PubMed] [Google Scholar]
- 6.Steiner C, Andrews R, Barrett M, Weiss A. HCUP Projections: mobility/orthopedic procedures 2011 to 2012. HCUP projections report. 2012;3:2012–03. [Google Scholar]
- 7.Liu Q, Niu J, Huang J, Ke Y, Tang X, Wu X, et al. Knee osteoarthritis and all-cause mortality: the Wuchuan Osteoarthritis Study. Osteoarthritis and Cartilage. 2015. [DOI] [PubMed] [Google Scholar]
- 8.Kluzek S, Sanchez-Santos M, Leyland K, Judge A, Spector T, Hart D, et al. Painful knee but not hand osteoarthritis is an independent predictor of mortality over 23 years follow-up of a population-based cohort of middle-aged women. Annals of the rheumatic diseases. 2015:annrheumdis-2015–208056. [DOI] [PubMed] [Google Scholar]
- 9.Falls Bergen G. and fall injuries among adults aged≥ 65 years—United States, 2014. MMWR Morbidity and mortality weekly report. 2016;65. [DOI] [PubMed] [Google Scholar]
- 10.Burns ER, Stevens JA, Lee R. The direct costs of fatal and non-fatal falls among older adults—United States. Journal of safety research. 2016;58:99–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rubenstein LZ, Josephson KR. Falls and their prevention in elderly people: what does the evidence show? Medical Clinics of North America. 2006;90(5):807–24. [DOI] [PubMed] [Google Scholar]
- 12.de Zwart AH, van der Esch M, Pijnappels MA, Hoozemans MJ, van der Leeden M, Roorda LD, et al. Falls associated with muscle strength in patients with knee osteoarthritis and self-reported knee instability. The Journal of rheumatology. 2015;42(7):1218–23. [DOI] [PubMed] [Google Scholar]
- 13.Barbour KE, Lui L-Y, McCulloch CE, Ensrud KE, Cawthon PM, Yaffe K, et al. Trajectories of lower extremity physical performance: effects on fractures and mortality in older women. Journals of Gerontology Series A: Biomedical Sciences and Medical Sciences. 2016;71(12):1609–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cawthon PM, Fullman RL, Marshall L, Mackey DC, Fink HA, Cauley JA, et al. Physical performance and risk of hip fractures in older men. Journal of Bone and Mineral Research. 2008;23(7):1037–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cummings SR, Nevitt MC, Browner WS, Stone K, Fox KM, Ensrud KE, et al. Risk factors for hip fracture in white women. New England journal of medicine. 1995;332(12):767–74. [DOI] [PubMed] [Google Scholar]
- 16.Lewis CE, Ewing SK, Taylor BC, Shikany JM, Fink HA, Ensrud KE, et al. Predictors of non‐spine fracture in elderly men: the MrOS study. Journal of Bone and Mineral Research. 2007;22(2):211–9. [DOI] [PubMed] [Google Scholar]
- 17.Mat S, Ng CT, Tan MP. Influence of hip and knee osteoarthritis on dynamic postural control parameters among older faller. Journal of rehabilitation medicine. 2017;49(3):258–63. [DOI] [PubMed] [Google Scholar]
- 18.Muraki S, Akune T, Oka H, En‐yo Y, Yoshida M, Nakamura K, et al. Prevalence of falls and the association with knee osteoarthritis and lumbar spondylosis as well as knee and lower back pain in Japanese men and women. Arthritis care & research. 2011;63(10):1425–31. [DOI] [PubMed] [Google Scholar]
- 19.Foley S, Lord SR, Srikanth V, Cooley H, Jones G. Falls risk is associated with pain and dysfunction but not radiographic osteoarthritis in older adults: Tasmanian Older Adult Cohort study. Osteoarthritis and cartilage. 2006;14(6):533–9. [DOI] [PubMed] [Google Scholar]
- 20.Doré AL, Golightly YM, Mercer VS, Shi XA, Renner JB, Jordan JM, et al. Lower‐Extremity Osteoarthritis and the Risk of Falls in a Community‐Based Longitudinal Study of Adults With and Without Osteoarthritis. Arthritis care & research. 2015;67(5):633–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Scott D, Blizzard L, Fell J, Jones G. Prospective study of self‐reported pain, radiographic osteoarthritis, sarcopenia progression, and falls risk in community‐dwelling older adults. Arthritis care & research. 2012;64(1):30–7. [DOI] [PubMed] [Google Scholar]
- 22.Tsonga T, Michalopoulou M, Malliou P, Godolias G, Kapetanakis S, Gkasdaris G, et al. Analyzing the history of falls in patients with severe knee osteoarthritis. Clinics in orthopedic surgery. 2015;7(4):449–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Arden NK, Crozier S, Smith H, Anderson F, Edwards C, Raphael H, et al. Knee pain, knee osteoarthritis, and the risk of fracture. Arthritis Care & Research. 2006;55(4):610–5. [DOI] [PubMed] [Google Scholar]
- 24.Muraki S, Akune T, Ishimoto Y, Nagata K, Yoshida M, Tanaka S, et al. Risk factors for falls in a longitudinal population-based cohort study of Japanese men and women: the ROAD Study. Bone. 2013;52(1):516–23. [DOI] [PubMed] [Google Scholar]
- 25.Khalaj N, Osman NAA, Mokhtar AH, Mehdikhani M, Abas WABW. Balance and risk of fall in individuals with bilateral mild and moderate knee osteoarthritis. PloS one. 2014;9(3):e92270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Riddle DL, Golladay GJ. A longitudinal comparative study of falls in persons with knee arthroplasty and persons with or at high risk for knee osteoarthritis. Age and ageing. 2016;45(6):794–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Smith T, Pearson M, Latham S. Are people following hip and knee arthroplasty at greater risk of experiencing a fall and fracture? Data from the Osteoarthritis Initiative. Archives of orthopaedic and trauma surgery. 2016;136(6):865–72. [DOI] [PubMed] [Google Scholar]
- 28.Nevitt MC, Tolstykh I, Shakoor N, Nguyen USD, Segal NA, Lewis C, et al. Symptoms of knee instability as risk factors for recurrent falls. Arthritis care & research. 2016;68(8):1089–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nevitt MC, Cummings SR, Hudes ES. Risk factors for injurious falls: a prospective study. Journal of gerontology. 1991;46(5):M164–M70. [DOI] [PubMed] [Google Scholar]
- 30.Barbour KE, Stevens JA, Helmick CG, Luo Y-H, Murphy LB, Hootman JM, et al. Falls and Fall Injuries Among Adults with Arthritis—United States, 2012. MMWR Morbidity and mortality weekly report. 2014;63(17):379–83. [PMC free article] [PubMed] [Google Scholar]
- 31.Sturnieks DL, Tiedemann A, Chapman K, Munro B, Murray SM, Lord SR. Physiological risk factors for falls in older people with lower limb arthritis. The Journal of Rheumatology. 2004;31(11):2272–9. [PubMed] [Google Scholar]
- 32.O’Loughlin JL, Robitaille Y, Boivin J-F, Suissa S. Incidence of and risk factors for falls and injurious falls among the community-dwelling elderly. American journal of epidemiology. 1993;137(3):342–54. [DOI] [PubMed] [Google Scholar]
- 33.Linn S, Murtaugh B, Casey E. Role of sex hormones in the development of osteoarthritis. PM&R. 2012;4(5):S169–S73. [DOI] [PubMed] [Google Scholar]
- 34.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. The Journal of rheumatology. 1988;15(12):1833–40. [PubMed] [Google Scholar]
- 35.Conroy MB, Kwoh CK, Krishnan E, Nevitt MC, Boudreau R, Carbone LD, et al. Muscle strength, mass, and quality in older men and women with knee osteoarthritis. Arthritis care & research. 2012;64(1):15–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Altman RD, Hochberg M, Murphy W Jr, Wolfe F, Lequesne M. Atlas of individual radiographic features in osteoarthritis. Osteoarthritis and cartilage/OARS, Osteoarthritis Research Society. 1995;3:3–70. [PubMed] [Google Scholar]
- 37.Schwartz AV, Nevitt MC, Brown BW Jr, Kelsey JL. Increased falling as a risk factor for fracture among older women: the study of osteoporotic fractures. American Journal of Epidemiology. 2005;161(2):180–5. [DOI] [PubMed] [Google Scholar]
- 38.Sagawa N MZ, Boudreau RM, Hanlon JT, Albert SM, O’Hare C, Satterfield S, Schwartz AV, Vinik AI, Cauley JA, Harris TB, Newman AB, Strotmeyer ES. . Low blood pressure levels for fall injuries in older adults: the Health, Aging and Body Composition Study. Eur J Ageing. 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ainsworth BE, Haskell WL, Whitt MC, Irwin ML, Swartz AM, Strath SJ, et al. Compendium of physical activities: an update of activity codes and MET intensities. Medicine and science in sports and exercise. 2000;32(9; SUPP/1):S498–S504. [DOI] [PubMed] [Google Scholar]
- 40.Pahor M, Chrischilles E, Guralnik J, Brown S, Wallace R, Carbonin P. Drug data coding and analysis in epidemiologic studies. European journal of epidemiology. 1994;10(4):405–11. [DOI] [PubMed] [Google Scholar]
- 41.Pereira CL, Baptista F, Infante P. Men older than 50 yrs are more likely to fall than women under similar conditions of health, body composition, and balance. American journal of physical medicine & rehabilitation. 2013;92(12):1095–103. [DOI] [PubMed] [Google Scholar]
- 42.Davison MJ, Ioannidis G, Maly MR, Adachi JD, Beattie KA. Intermittent and constant pain and physical function or performance in men and women with knee osteoarthritis: data from the osteoarthritis initiative. Clinical rheumatology. 2016;35(2):371–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Fillingim RB. Sex, gender, and pain: women and men really are different. Current Pain and Headache Reports. 2000;4(1):24–30. [DOI] [PubMed] [Google Scholar]
- 44.Welmer A-K, Rizzuto D, Calderón-Larrañaga A, Johnell K. Sex differences in the association between pain and injurious falls in older adults: a population-based longitudinal study. American journal of epidemiology. 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Stubbs B, Binnekade T, Eggermont L, Sepehry AA, Patchay S, Schofield P. Pain and the risk for falls in community-dwelling older adults: systematic review and meta-analysis. Archives of physical medicine and rehabilitation. 2014;95(1):175–87. e9. [DOI] [PubMed] [Google Scholar]
- 46.Deandrea S, Lucenteforte E, Bravi F, Foschi R, La Vecchia C, Negri E. Risk Factors for Falls in Community-dwelling Older People:” A Systematic Review and Meta-analysis”. Epidemiology. 2010:658–68. [DOI] [PubMed] [Google Scholar]
- 47.Wallace JI, Buchner DM, Grothaus L, Leveille S, Tyll L, LaCroix AZ, et al. Implementation and effectiveness of a community-based health promotion program for older adults. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences. 1998;53(4):M301–M6. [DOI] [PubMed] [Google Scholar]
- 48.Belza B, Shumway-Cook A, Phelan EA, Williams B, Snyder SJ, LoGerfo JP. The effects of a community-based exercise program on function and health in older adults: The EnhanceFitness Program. Journal of Applied Gerontology. 2006;25(4):291–306. [Google Scholar]
- 49.Greenwood-Hickman MA, Rosenberg DE, Phelan EA, Fitzpatrick AL. Peer Reviewed: Participation in Older Adult Physical Activity Programs and Risk for Falls Requiring Medical Care, Washington State, 2005–2011. Preventing chronic disease. 2015;12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Gillespie LD, Robertson MC, Gillespie WJ, Sherrington C, Gates S, Clemson LM, et al. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2012;9(11). [DOI] [PMC free article] [PubMed] [Google Scholar]