Abstract
Background:
Although there is extensive research on falls prevention, most of this knowledge is from western countries, and this may limit its usefulness when implementing in countries with different culture and healthcare systems.
Objective:
This study evaluated the feasibility and effectiveness of a falls prevention intervention programme for older people in Thailand.
Methods:
Two hundred and seventy-seven community-dwelling older people were randomized to either an intervention programme which included an education about falls risk management plus a home-based balance exercise delivered by a physiotherapist for four-month duration or control group. Falls, balance, physical activity, and other falls risk factors were measured at baseline and after programme completion.
Results:
About 90% of the participants in the intervention group completed the programme, with very high adherence to the exercise programme, though poor compliance with the suggestions of other falls risks management. There were no falls or injuries related to the exercise programme reported. There was no significant difference in falls rate between the two groups.
Conclusion:
This falls prevention program was not effective in reducing falls in community-dwelling older people in Thailand. However, the study provided encouraging evidence that home-based balance exercise could be practically implemented in older people living in communities in Thailand.
Keywords: Exercise, falls prevention, older people, Thailand
Introduction
Falling is a well-recognized health issue in older people, with one in three people aged over 65, living in the community, falling each year.1,2 There have been extensive research in falls in older people including several systematic reviews conducted with the aim to find out which fall prevention interventions are effective for older people living in the community including older people with a high falls risk. Evidence-based interventions are available to prevent falls. The evidence for the effectiveness of falls prevention interventions for community-dwelling older people has been previously summarized in a systematic review3 and updated up to the year 2012.4 The recent review reported that an exercise programme as a single intervention, as well as multifactorial programmes (a combination of single interventions targeted an individual person’s identified falls risk factors), were the most common interventions studied.4 The meta-analysis revealed that two types of single intervention: (1) multi-component exercise programme and (2) home safety modification found to be effective in reducing falls risk and falls rate in older people. The effectiveness of the combination exercise programmes in reducing risk of falling has also been affirmed by two systematic reviews and meta-analyses by Sherrington and team.5,6 Regarding the effectiveness of multifactorial intervention programmes, the recent systematic review by Gillespie et al. in 2012 also supported that multifactorial intervention programmes could also minimize falls rate; however, this would not have an effect on the falls risk level.4 Even though these systematic reviews3-6 demonstrated the evidence of several intervention programmes effectively preventing falls for community-dwelling older people, in different countries, falls by older people could be recognized and then managed in different ways depending upon the various factors in particular culture, living standards, as well as the healthcare and social welfare systems of each country. These could be factors influencing feasibility and also effectiveness of falls prevention intervention programmes to be implemented in each country.
In Thailand, there have been only a limited number of studies of falls prevention interventions. A review of Thai research of falls prevention programmes in 20077 identified only three published research studies in which two quasi-experimental studies were mainly educational interventions and the other one was a randomized controlled trial providing a falls prevention booklet combined with clinical assessment. Since then, there has been another study which was a qualitative study of older people’s opinion and preferences on fall prevention programmes for Thai community-dwelling older people.8 As such, there is little research evidence to guide falls prevention practice for Thai older people living in the community.7
As older population in Thailand is rising and is expected to reach 14%, 19.8% and 30% in 2015, 2025, and 2050, respectively,9 and since we could anticipate consequences of falls as one of the health problems in the population, there is a clear need for studies to investigate the effect of falls prevention intervention focusing on exercise programmes specifically in community-dwelling older people in Thailand.
The aim of this study is to provide evidence of the effectiveness of a home-based falls prevention programme, focusing on balance exercise programmes on falls and falls risk factors including physical performance in community-dwelling older people in Thailand.
Methods
Study design
The study was a single-blinded randomized controlled trial. The study protocol was approved by the Human Research Ethics Committees, Thammasat University (Project No. 044/2556). The written informed consent was obtained from each participant.
Participants
People aged 60 and over who had been living in the community were eligible for inclusion in this study if they satisfied all the following criteria: (i) ability to walk outdoors with no more support than a single point stick; (ii) having no other serious orthopedic condition (e.g., recent lower limb surgery, severe arthritis of a lower limb) or major neurological disorder (e.g., stroke with unilateral or bilateral paresis or Parkinson disease) that could restrict functional mobility. Those who had a severe level of cognitive impairment that could limit participation would be excluded.
Sample size was calculated for the study, based on the data from the pilot study, with an estimated effect size of 0.5, indicating 138 participants per group (276 participants in total) would be required for power of 80% and alpha of 0.05, assuming a loss to follow up of 15%.
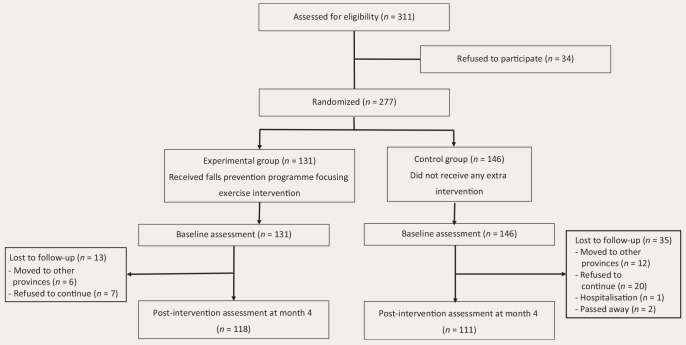
Participants were recruited from a previous study on balance and falls risk in older people in Thailand. After baseline assessment, each participant was randomized into either (1) the control or (2) the intervention programmes, using a concealed randomization procedure. A random number table with group allocation was computer-generated and packed in an opaque-sealed envelope by a staff member independent of the current research team. After baseline assessment, the next numbered envelope was opened by a research assistant who was not involved in assessments or interventions. The research assistant then contacted a physiotherapist who was delivering the intervention programme, but was not involved in assessment (single blind randomized controlled trial). The CONSORT diagram is presented Fig. 1.
Fig. 1.
CONSORT diagram of the study.
Procedure
A baseline assessment was carried out, which included measures of falls rate, a comprehensive series of clinical measures of balance and mobility performance as well as level of physical activity, and measures of common falls risk factors, and then repeated after the intervention programme was completed (four months). All measurements on both assessment occasions were undertaken by trained assessors blind to group allocation.
Outcome measures
Measures of falls: The number of falls in the preceding 12 months (self-report, based on information from the participant and their falls calendars) was recorded.
Measures of balance and mobility performance, physical activity level and frequency of exercises:
-
(i)
Functional Reach (FR) test,10 a test of the maximum distance11 that participants can reach forward with their dominant arm raised to 90∘.
-
(ii)
Step Test (ST),12 a test that measures the number of times the participant steps with one foot fully on and then off a 7.5 cm-block as quickly as possible in 15 s was recorded. Each leg was tested separately, and performance on the side with a poorer score was recorded.
-
(iii)
Timed Chair Stand (TCS),13 a test measuring the speed of standing up/sitting down as fast as possible five times from a 45 cm-high chair.
-
(iv)
Timed Up and Go (TUG) test,14 an assessment that measures speed in standing up from a standard chair, walking 3 m at usual speed, turning, then returning to sit again in the chair (s). This task was reassessed under dual task conditions, with a secondary cognitive task (counting backwards by 3 s while performing the TUG), and with a secondary motor task (carrying a full cup of water while performing the TUG).15
-
(v)
A Thai-translated version of the physical activity level assessment, modified from the Physical Activity Scale for the Elderly (PASE).16
Measures of other falls risk factors consisted of the following:
-
(i)
Fear of falling: a Thai-translated version of the Modified Falls Efficacy Scale, which is a self-reported questionnaire to determine how confidently participants feel that they are able to perform each of 14 common activities in daily life.
-
(ii)
Visual problems and treatment were reported by each participant.
-
(iii)
Home environmental hazards were assessed by observation in/at walkways, bedrooms, kitchens, bathrooms, and stairs.
-
(iv)Appropriate footwear was assessed by observation using the checklist described as follows:
-
–Poorly-fitting footwear/slippers.
-
–Unstable footwear.
-
–Slippery footwear.
-
–Footwear with heels higher than one inch.
-
–Worn-out footwear.
-
–
Participants were randomized to either the intervention group (received fall prevention programme focusing on balance exercise) or control group. Participants in both groups continued with their usual care and other activities while participating in this study.
Intervention
Falls prevention programme focusing on balance exercise.
Participants randomized to the intervention programme were provided with a four-month multifactorial falls prevention programme which focused on a balance training exercise. The intervention programme consisted of the following:
-
(1)
An individualized home-based balance exercise programme was developed and monitored by a physiotherapist. The programme focused on lower extremity strengthening exercises and balance training. The programme was based on an existing home exercise programme (the Otago programme, http://www.acc.co.nz/PRD_EXT_CSMP/groups/external_providers/documents/publications_promotion/prd_ctrb118334.pdf) that has been shown to be effective in reducing falls in older people. The length of the programme and number of visits were modified from the originally described randomized trial (from 4 to 5 visits during 6 to 12 months to be a couple of visits during the 4-month period of the programme) to increase feasibility of the programme (due to the limited support both in terms of expenses and staff). However, frequency of exercises per week was modified to be increased from three days/week in original programme to be at least four days/week. Each participant was also provided with an exercise booklet with illustrations and instructions so that the participant could continue the exercises at home.
Two follow-up phone calls in between visits were also provided in order to ensure that there were no negative effects from the exercises and to gauge that the participant had done the exercises correctly. The participants were provided with the physiotherapist’s contact phone details and were able to contact the physiotherapist if necessary.
Data on adherence to the exercise programme were collected by participants completing monthly exercise recording sheets, which were retrieved and reviewed by the physiotherapist during the subsequent home visits and phone calls.
-
(2)
A booklet of falls risk management strategies based on common falls risk factors reported in community-dwelling older people was provided, together with advice for each participant about how to deal with their falls risk factors identified from the pre-intervention assessment (e.g., suggestion for taking medications review, eye check, and home environmental hazard modifications).
-
(3)
A handrail (to be installed in the bathroom or toilet) or a walking-assistive device was provided for the participants who needed it (need was based on the pre-intervention assessment results).
Control
Participants randomized to the control group received usual care and continued their usual activities without any of the limitation from being participated in the study.
Statistical analysis
All analyses were conducted using the intention-to-treat principle that included all randomized participants. To manage missing data associated with participants dropping out from the study during the four months of intervention, Last Observation Carried Forward Method was used.17
To evaluate the effectiveness of the intervention programme, we used the generalized linear models (SPSS advance statistics 17.0), with group allocation as the factor (predictor) variable. Variables which are commonly recognized as falls risk factors as well as the variables which were found to be different between the intervention and control groups at the baseline assessment were considered as covariates for the first run of model of each outcome measure analyzed. Only variables with a significant level at the tests of model effects were included as covariates in the final model of each variable analysis. The final model of each outcome measure also contained baseline performance on the outcome as another covariate. Each outcome measure was analyzed by a separate model in which the type of model was selected based on the nature of the outcome measure and its distribution (Table 1).
Table 1.
Type of model selected for each outcome measure.
| Generalized linear models | |||
|---|---|---|---|
| Outcome | Measure | Distribution | Link function |
| Number of falls in the previous year | Count | Poisson | Log |
| Fallers: non-Fallers | Binary | Binomial | Logistic |
| Number of medical conditions 4 | Binary | Binomial | Logistic |
| Number of medications 4 | Binary | Binomial | Logistic |
| Normal eyesight: Abnormal eyesight, (%) | Binary | Binomial | Logistic |
| Using bifocal or multifocal eyeglasses, (%) | Binary | Binomial | Logistic |
| Other eye conditionsa (treatment: non-treatment), (%non-treatment) | Nominal | Multinomial | Cumulative Logit |
| Appropriate footwear: Inappropriate footwear,b (%inappropriate footwear) | Binary | Binomial | Logistic |
| Having 4 home hazard environments, (%) | Binary | Binomial | Logistic |
| Regularly go to toilet at night 2 times, (%) | Binary | Binomial | Logistic |
| Regularly go to toilet at night 4 times, (%) | Binary | Binomial | Logistic |
| Number of medical conditions | Quantitative | Gamma | Identity |
| Number of medications | Quantitative | Gamma | Identity |
| Functional Reach test | Quantitative | Normal | Identity |
| Step Test (worst side) | Quantitative | Normal | Identity |
| Timed Up and Go test (TUG) | Quantitative | Gamma | Identity |
| TUG (secondary manual task) | Quantitative | Gamma | Identity |
| TUG (secondary cognitive task) | Quantitative | Gamma | Identity |
| Timed Chair Stand | Quantitative | Gamma | Identity |
| Hand reaction time | Quantitative | Gamma | Identity |
| Modified PASEc score | Quantitative | Gamma | Identity |
| Exercise frequency (times/week) | Quantitative | Gamma | Identity |
| Total exercise time (hours/week) | Quantitative | Gamma | Identity |
| Modified Falls Efficacy Scale | Quantitative | Gamma | Identity |
| MMSEd | Quantitative | Gamma | Identity |
| Number of home environmental hazards | Quantitative | Gamma | Identity |
aOther eye conditions including cataract, glaucoma, Pterygium, Pinguecula; bInappropriate footwear including poorly fitted shoes/slippers, unstable shoes, slippery shoes, shoes with 1 inch high-heel, worn-out footwear; cModified PASE (hours/week); dMini-Mental State Examination (Thai version).
Results
Participant characteristics
Two hundred and seventy-seven participants were randomized to the intervention (131) or the control (146) groups.
Baseline characteristics and possible falls risk factors for the total 277 participants are shown in Table 2. The mean age standard deviation of the participants in the control and intervention programmes were 72.92 5.63 and 72.18 5.41, respectively. Participants were predominantly female in both groups. At baseline, performance on the balance and mobility tests, and other falls risk factors between the two groups were similar on most outcome measures. However, there were several outcome measures significantly different between the two groups at baseline including the number of medical conditions, amount of prescribed medications taken, time to perform TCS test, score of physical activity level measured by PASE, and number of home environmental hazards. In general, the intervention group had better health conditions and mobility performance compared to the control at the baseline; however, the intervention group also had a greater number of home environmental hazards than the control group.
Table 2.
Characteristics and falls risk factors of the participants at baseline ().
| Characteristics and Falls risk factors | Intervention group () | Control group () |
|---|---|---|
| Age, mean SD | 72.2 5.4 | 72.9 5.6 |
| Gender (M:F), n | 34:97 | 40:106 |
| MMSEa score, mean SD | 25.2 4.3 | 24.6 4.5 |
| Number of medical conditions, mean SD | 2.0 1.1 | 2.4 1.2* |
| Number of medical condition greater than 4, (%) | 11 (8.4%) | 25 (17.1%) |
| Number of medications, mean SD | 1.8 1.7 | 2.2 1.7* |
| Taken greater than 4 medications, (%) | 17 (13%) | 31 (21.2%) |
| Falls in previous year, mean SD | 0.3 0.8 | 0.3 0.9 |
| Fallers: non-fallers, (% fallers) | 26:104 (19.9%) | 28:118 (19.2%) |
| Functional Reach test (distance_cm), mean SD | 22.1 6.6 | 20.9 6.1 |
| Step Test (number of steps_worse side), mean SD | 10.5 3.4 | 10.2 2.7 |
| Timed Up and Go test (TUG) score (s), mean SD | 13.3 5.6 | 13.3 3.9 |
| TUG (secondary manual task) (s), mean SD | 13.1 5.2 | 13.9 4.4 |
| TUG (secondary cognitive task) (s), mean SD | 16.5 7.1 | 16.8 5.5 |
| Timed Chair Stand (s), mean SD | 10.7 4.5 | 11.4 3.6* |
| Hand reaction time (ms) | 1.4 0.5 | 1.3 0.7 |
| Modified PASEb score (hours/week) | 34.0 7.9 | 32.2 8.9* |
| Modified Falls Efficacy Scale | 119.9 23.5 | 122.0 18.6 |
| Normal eyesight: Abnormal eyesight, (%non-normal eyesight) | 35:96 (73.3%) | 39:107 (73.3%) |
| Using bifocal or multifocal eyeglasses, (%) | 11 (8.4%) | 18 (12.3%) |
| Other eye conditionsc treatment: non-treatment, (%non-treatment) | 48:18 (27.3%) | 59:22 (27.2%) |
| Appropriate footwear: Inappropriate footwear,d (% inappropriate footwear) | 101:30 (22.9%) | 99:47 (32.2%) |
| Number of home environmental hazards, mean SD | 4.0 2.1 | 3.7 2.6* |
| Having home hazard environment 4, (%) | 63 (48.1%) | 58 (39.7%) |
; aMini-Mental State Examination (Thai version); bModified PASE (hours/week); cOther eye conditions including cataract, glaucoma, Pterygium, Pinguecula; dInappropriate footwear including poorly fitted shoes/slippers, unstable shoes, slippery shoes, shoes with inch high-heel, worn-out footwear.
Intention to treat outcome analysis
One hundred and eighteen of the 131 participants in the intervention group completed the programme. In the control group, 111 of the 146 participants in the control group completed the study. The combined discontinuing rate of this study was 17.33%.
Table 3 demonstrates the comparison of outcome measures assessed at pre- and post-intervention time points between the intervention and control groups. Also, (coefficient) values are presented which represent the average values of the outcome measures of the exercise group compared with the control group, after adjusting for the effects of all other factors and/or covariate (s) in the models selected for analysis (the relevant values are reported). A negative value means that the average value of the outcome of the intervention group is higher than the control group when analyses contained baseline performance and other falls risk factors as covariates.
Table 3.
Outcome analysis.a
| Intervention group | Control group | |||||
|---|---|---|---|---|---|---|
| Outcome measures | Baseline performance | Post-intervention performance | Baseline performance | Post-intervention performance | IRR/OR (95% CI) | value |
| Falls in the previous year, mean SD | 0.3 0.8 | 0.3 0.7 | 0.3 0.9 | 0.3 0.7 | IRR 0.008 (0.40–0.42) | 0.971 |
| Fallers: non-fallers, (% fallers) | 26:104 (19.9%) | 31:100 (23.7%) | 28:118 (19.2%) | 35:111 (24.0%) | OR 0.046 (0.81–0.72) | 0.907 |
| Number of medical conditions 4 | 11 (8.4%) | 11 (8.40%) | 25 (17.1%) | 18 (12.3%) | OR 0.371 (0.62–1.36) | 0.462 |
| Number of medications 4 | 17 (13.0%) | 16 (12.2%) | 31 (21.2%) | 26 (17.8%) | OR 0.060 (1.01–0.89) | 0.900 |
| Normal eyesight: Abnormal eyesight, (%) | 35:96 (73.3%) | 38:93 (71.0%) | 39:107 (73.3%) | 45:101 (69.2%) | OR 0.121 (0.57–0.81) | 0.729 |
| Using bifocal/multifocal eyeglasses, (%) | 11 (8.4%) | 22 (16.8%) | 18 (12.3%) | 25 (17.1%) | OR 0.117 (0.67–0.91) | 0.771 |
| Other eye conditionsb (treatment: non-treatment), (%non-treatment) | 48:18 (27.3%) | 52:17 (24.6%) | 59:22 (27.2%) | 58:24 (29.3%) | OR 0.105 (0.61–0.82) | 0.774 |
| Appropriate footwear: Inappropriate footwear,c (%inappropriate footwear) | 101:30 (22.9%) | 85:46 (35.1%) | 99.47 (32.2%) | 87:59 (40.1%) | OR 0.046 (0.59–0.50) | 0.870 |
| Having 4 home hazard environments, (%) | 63 (48.1%) | 60 (45.8%) | 58 (39.7%) | 55 (37.7%) | OR 0.046 (0.81–0.72) | 0.858 |
| Number of medical conditions | 2.0 1.1 | 1.9 1.3 | 2.4 1.2 | 2.1 1.2 | 0.023 (0.22–0.17) | 0.817 |
| Number of medications | 1.8 1.7 | 1.9 1.7 | 2.2 1.7 | 2.3 1.7 | 0.109 (0.33–0.11) | 0.328 |
| Functional Reach test11 | 22.1 6.6 | 23.4 6.9 | 20.9 6.1 | 22.8 6.8 | 0.416 (0.79–1.630) | 0.500 |
| Step Test (worse side) (steps) | 10.5 3.4 | 10.5 3.3 | 10.2 2.7 | 10.1 3.0 | 0.033 (0.50–0.43) | 0.889 |
| Timed Up and Go test (s) | 13.3 5.6 | 13.9 5.2 | 13.3 3.9 | 13.6 3.8 | 0.481 (0.93–[0.04]) | 0.034* |
| TUG (2nd task_manual task) (s) | 13.1 5.2 | 14.5 5.4 | 13.9 4.4 | 14.5 4.3 | 0.342 (0.84–0.16) | 0.181 |
| TUG (2nd task_cognitive task) (s) | 16.5 7.1 | 19.4 9.4 | 16.8 5.5 | 18.4 6.5 | 0.972 (2.04–0.10) | 0.075 |
| Timed Chair Stand (s) | 10.7 4.5 | 11.1 4.9 | 11.4 3.6 | 11.4 3.4 | 0.992 (1.42–[0.56]) | 0.000** |
| Hand reaction time | 1.4 0.5 | 1.3 0.5 | 1.3 0.7 | 1.2 0.6 | 0.053 (0.13–0.03) | 0.205 |
| Modified PASEd score (hours/week) | 34.0 7.9 | 34.4 9.7 | 32.2 8.9 | 34.4 11.7 | 0.995 (1.38–3.37) | 0.412 |
| Exercise frequency (times/week) | 3.7 3.4 | 6.0 2.3 | 3.3 3.4 | 3.7 3.3 | 0.466 (0.89–[0.04]) | 0.032* |
| Total exercise time (hours/week) | 13.2 15.1 | 20.5 13.1 | 12.5 15.0 | 14.0 16.2 | 1.382 (4.23–1.47) | 0.342 |
| Modified Falls Efficacy Scale | 119.9 23.5 | 119.4 26.5 | 122.0 18.6 | 121.1 21.4 | 0.362 (5.29–6.02) | 0.900 |
| MMSEe | 25.2 4.3 | 25.8 4.1 | 24.6 4.5 | 24.8 4.8 | 0.731 (1.32–[0.15]) | 0.014* |
| Number of home environmental hazards | 4.0 2.1 | 4.3 2.7 | 3.7 2.6 | 3.8 2.8 | 0.202 (0.43–0.03) | 0.084 |
Notes: Test scores reported are mean and standard deviation. *; **; aThe adjusted IRR, OR, coefficient (95% confidence interval (CI)), and values are based on generalized linear models in which the intervention group is compared with the control group; bOther eye conditions including cataract, glaucoma, Pterygium, Pinguecula; cInappropriate footwear including poorly fitted shoes/slippers, unstable shoes, slippery shoes, shoes with inch high-heel, worn-out footwear; dModified PASE (hours/week); eMini-Mental State Examination (Thai version).
At the post-intervention reassessment, the number of falls in the previous year of both the intervention and control groups did not change in comparison to the baseline, and were not significantly different between the two groups. As for the percentage of participants reporting one or more falls in the preceding year at the reassessment, the intervention group increased by approximately 4% which was similar with the control group.
No changes and no differences between the groups were found in the majority of the outcome measures. A significantly slower mobility during TUG and TCS tests was found in the intervention group compared with the control group. However, this was only a small change (mean value increased by less than 1 s). It was also found that the number of home environmental hazard had increased in the intervention group.
Safety and compliance to the intervention programme
Home-based balance exercise programme
There were no falls or injuries associated with performing the exercise programme. Only a few participants reported (mild) pain or bodily discomfort when a new exercise was introduced. However, those symptoms eased with continuing the exercises.
Full compliance (100%) was defined as a participant doing the exercises four days a week. The average of percentage of adherence of all participants who completed the exercise programme (4th month period) (118 of 131 participants) was 90%. Around 90 out of 118 participants had greater than 80% adherence, with 51 of them completing the exercise programme with 100% adherence. The common reasons for limited exercise-adherence of the participants were health conditions which could lead to hospitalization in some cases, being away from home.
Education and falls prevention booklet
Most suggestions about minimizing falls risk by managing falls risk factors in particular, such as number of medications used, visual problems, and in particular home hazard modification, could not be implemented in practice. For example, the provided handrail could not be installed in some participants’ bathrooms or toilets due to the limitations of house structure (e.g., wall built with corrugated sheets).
Discussion
This study is adding evidence that a falls-prevention advisory programme together with a booklet regarding falls risk factors, falls risk management and falls prevention guidelines, and in particular a home-based balance exercise programme delivered by a physiotherapist, can be implemented safely in older people living in communities in Thailand. However, the programme was not effective in terms of reducing occurrences of falling in the population. Referring to the understanding that falls often involve a mix of contributory intrinsic and extrinsic falls risk factors,18 the study hypothesized that a multifactorial intervention programme would effectively reduce falls in older people. However, the findings did not support our initial hypothesis that a multifactorial intervention programme which targeted identified falls risk factors would reduce falls rate and improve physical performance as several previous studies suggested.3,4 Main explanation for the lack of effectiveness of the programme could be a combination of several factors including the design of the programme especially the exercise programme, the way to implement the education intervention offering knowledge and suggestions of falls risk management strategies as well as some possible variations among participants included in the study.
Regarding the implementation of the education programme, one possible reason is that the falls risk management strategies suggested could not practically implemented by most of our participants, particularly the advice to modify home environmental hazards and inappropriate footwear. In addition, several falls risk factors identified could not be practically modified by the older people themselves, but required assistance from varied health care professionals as well as support from the healthcare system and government, for example, medications reviews, eye check-ups and treatment. These could be affirmed by the lack of differences in numbers of medications taken, untreated visual problem and home environmental hazards at the post-intervention assessment compared with the baseline in both the intervention and control groups. This finding emphasizes that a falls prevention intervention for older people in Thailand should be a multifactorial programme delivered by multidisciplinary team of health care professionals.
Focusing on the effect of the home-based balance exercise intervention programme, there was no improvement in balance or mobility performance or any falls outcome measures found in the intervention group after the completion of the programme. The findings were not consistent with the findings previously reported from a number of randomized controlled trials as well as several systematic reviews regarding the effectiveness of exercise intervention in reducing falls risk and falls rate in older people.3-6 The non-significant results might be explained by the design of the exercise programme in particular intensity, and challenges of the programme. In terms of intensity, the exercise programme in the present study was a four-month duration programme, which was less than the intensity recommended for exercise aiming to reduce falls by Sherrington et al.5,6 Additionally, the exercises prescribed in this study could be less challenging to postural and balance control systems in particular participants who were healthy and still living actively in the community.5,6 The mean age of participants of the study was approximately 70 s which was younger than participants (mean age 81.6 3.9 years) of several randomized controlled trails found effectiveness of the Otago exercise programme reported in a recent systematic review and meta-analysis.19 This could be affirmed by the findings that there was no significant improvement in physical performance outcomes such as strength and balance, and consequently the non-reduction in falls rate at post-intervention assessment. Future exercise programmes could be modified from the current one by increasing the duration of the programme to at least six months and increasing the intensity of each exercise session. In addition, exercises prescribed should effectively challenge healthy older people’s postural and balance control. Even though the exercise programme has not been found to be effective in this study, the programme achieved a very high level of adherence. This is an encouraging finding that a home-based exercise intervention programme aiming to increase balance and mobility performance and consequently reduce risk of falling could be practically implemented in community-dwelling older people in Thailand.
Issues related to variation among participants of the study and the potential for other physical activity programmes involved in both control and intervention groups may have partly contributed to the lack of significant effects of the exercise programme. Participants of the study were recruited from several communities in urban and suburban areas. This may result in variation in physical health (i.e., the number of medical conditions of the included participants varied from 0 to 7 conditions), as well as variation in some socioeconomic factors including access to medical care, family support and education. Variation among participants could influence how the prescribed exercise and falls management strategies could be implemented by the participants in real practice. Therefore, future study aiming to develop practical falls prevention intervention programme in particular multifactorial type programme should take into consideration the participant’s right to medical care and services.
There are limitations of the study. The lack of quantitative data is recorded on compliance of other falls risk management strategies apart from the exercise programme (e.g., home hazard modification, medications review, eye check). However, the results (number of home hazard environment, number of medications, number of participants using bifocal or multifocal eyeglasses, number of eye conditions and number of participants wearing inappropriate footwear) at the post-intervention which remained similar with those reported at the baseline assessment might assist in confirming the low compliance of the falls risk management strategies suggested for the study’s participants. Future study should consider collecting participant compliance in every item of intervention and this would be beneficial in improving future falls risk management programme. A further limitation of the study is the high number of outcome measures of the study which may result in significance of the findings by statistical chance. To account for multiple variables, significant level at might be considered. However, applying significant level at to the study did not change the current conclusion of study’s findings.
Conclusion
Falls prevention programme focusing exercise programme could be implemented safely in community-dwelling older people in Thailand. However, the lack of effectiveness of the programme might be addressed by increasing the intensity and challenge of the exercise programme as well as tailoring the falls prevention programme with participant’s right to medical care and services and delivering the programme by multidisciplinary team of health care professionals.
Conflict of Interest
The authors declare that there is no conflict of interest relevant to the study.
Funding/Support
The study was funded by the Health Systems Research Institute under the National Research Council of Thailand. We are grateful to all the participants of this study. We also acknowledge the assistance and support from the physiotherapists and staff from the Faculty of Allied Health Sciences, Thammasat University and the Faculty of Medicine Vajira Hospital, Bangkok.
Author Contributions
All authors contributed to the study concept and design. All project management aspects were mainly carried out by P. Suttanon. Data was collected by all authors. Data analysis and interpretation were mainly carried out by P. Suttanon with suggestions from all other authors. Drafting of the manuscript was conducted by P. Suttanon, with revision of the manuscript by all authors.
References
- 1. Gill T, Taylor AW, Pengelly A. A population-based survey of factors relating to the prevalence of falls in older people. Gerontology 2005;51:340–5. [DOI] [PubMed] [Google Scholar]
- 2. Morris M, Osborne D, Hill K, et al. . Predisposing factors for occasional and multiple falls in older Australians who live at home. Aust J Physiother 2004;50:153–9. [DOI] [PubMed] [Google Scholar]
- 3. Gillespie LD, Robertson MC, Gillespie WJ, et al. . Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev 2009; 10.1002/14651858.CD007146.pub2. [DOI] [PubMed] [Google Scholar]
- 4. Gillespie LD, Robertson MC, Gillespie WJ, et al. . Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev 2012;2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Sherrington C, Whitney JC, Lord SR, Herbert RD, Cumming RG, Close JC. Effective exercise for the prevention of falls: A systematic review and meta-analysis. J Am Geriatr Soc 2008;56:2234–43. [DOI] [PubMed] [Google Scholar]
- 6. Sherrington C, Tiedemann A, Fairhall N, Close J, Lord SR. Exercise to prevent falls in older adults: An updated meta-analysis and best practice recommendations. N S W Public Health Bull 2011;22:78–83. [DOI] [PubMed] [Google Scholar]
- 7. Piphatvanitcha N, Kespichayawattana J, Aungsuroch Y, Magilvy JK. State of sciences: Falls prevention program in community-dwelling elders. Thai J Surg 2007;28:9097. [Google Scholar]
- 8. Jitramontree N, Chatchaisucha S, Thaweeboon T, Kutintara B, Intanasak S. Action research development of a fall prevention program for Thai community-dwelling older persons. Pac Rim Int J Nurs Res 2015;19:69–79. [Google Scholar]
- 9. Thailand U. Population Ageing in Thailand: Prognosis and Policy Response. Bangkok: United Nations Population Fund, 2006:2–3. [Google Scholar]
- 10. Duncan PW, Weiner DK, Chandler J, Studenski S. Functional Reach: A new clinical measure of balance. J Gerontol 1990;45:M192–M7. [DOI] [PubMed] [Google Scholar]
- 11. Kaufer DI, Cummings JL, Ketchel P, et al. . Validation of the NPI-Q, a brief clinical form of the Neuropsychiatric Inventory. J Neuropsychiatry Clin Neurosci 2000;12:233–9. [DOI] [PubMed] [Google Scholar]
- 12. Hill KD, Bernhardt J, McGann AM, Maltese D, Berkovits D. A new test of dynamic standing balance for stroke patients: Reliability, validity, and comparison with healthy elderly. Physiother Can 1996;48:257–62. [Google Scholar]
- 13. Whitney SL, Wrisley DM, Marchetti GF, Gee MA, Redfern MS, Furman JM. Clinical measurement of sit-to-stand performance in people with balance disorders: Validity of data for the Five-Times-Sit-to-Stand test. Phys Ther 2005;85:1034–45. [PubMed] [Google Scholar]
- 14. Podsiadlo D, Richardson S. The timed Up & Go: A test of basic functional mobility for frail elderly persons. J Am Geriatr Soc 1991;39:142–8. [DOI] [PubMed] [Google Scholar]
- 15. Shumway-Cook A, Brauer S, Woollacott M. Predicting the probability for falls in community-dwelling older adults using the Timed Up & Go test. Phys Ther 2000;80:896–903. [PubMed] [Google Scholar]
- 16. Washburn RA, Ficker JL. Physical activity scale for the elderly (PASE): The relationship with activity measured by a portable accelerometer. J Sports Med Phys Fitness 1999;39:336–40. [PubMed] [Google Scholar]
- 17. Teri L, Gibbons LE, McCurry SM, et al. . Exercise plus behavioral management in patients with Alzheimer disease: A randomized controlled trial. J Am Med Assoc 2003;250:2015–22. [DOI] [PubMed] [Google Scholar]
- 18. Lord SR, Sherrington C, Menz HB, Close JC. Falls in Older People: Risk Factors and Strategies for Prevention. 2nd ed. New York: Cambridge University Press, 2007. [Google Scholar]
- 19. Thomas S, Mackintosh S, Halbert J. Does the ‘Otago exercise programme’ reduce mortality and falls in older adults? A systematic review and meta-analysis. Age and Ageing 2010;39:681–7. [DOI] [PubMed] [Google Scholar]