Abstract
The purpose of this survey was to determine the association of parents’ attitudes and behaviors toward children's visual care with myopia risk in school-aged children.
A total of 894 parents of school-aged children were investigated in primary and middle schools in the central and noncentral urban area in Wuhan through stratified cluster random sampling on July, 2015. We analyzed the association by the generalized linear mixed model.
The results indicated that children with parents’ high expectations of 1.5 or higher on their vision exhibited a decreased risk of myopia compared with 1.0 and 0.5 or lower (OR = 0.49, 95%CI = 0.36–0.67). Children whose parents only paid attention to their vision in junior and senior school and in primary school had an increased myopia risk than that in preschool (OR = 2.12, 95%CI = 1.01–4.45, and OR = 3.11, 95%CI = 1.28–7.58, respectively). Children whose parents ensured for their sufficient sleep had a decreased myopia risk (OR = 0.45, 95%CI = 0.24–0.85). Compared with children whose parents who never adjusted electronic devices’ parameters, the odds ratio of sometimes was 0.49 (95%CI = 0.31–0.79), often 0.53 (95%CI = 0.33–0.85), and always 0.44 (95%CI = 0.26–0.75), respectively.
Parents’ attitudes and behaviors toward children's visual care are significantly associated with the myopia risk in school-aged children. Consequently, efforts should be made to educate parents on how they protect children's vision and reduce their risk of myopia.
Keywords: myopia, parents’ attitudes and behaviors, school-aged children, visual care
1. Introduction
Myopia is a worldwide health problem leading to pathological ocular complications and visual impairment.[1] The prevalence of myopia in Asia has been reported to be higher than in other parts of the world.[2] In China, the prevalence of myopia in children aged 7 to 18 years has been reported to increase from 47.5% in 2005 to 55.5% in 2010, and to 57.1% in 2014.[3] Myopia has a higher prevalence in school-aged teenagers[4–7] and the age of onset shows a younger tendency.[8]
Myopia is a complex condition of which the onset and development is associated with genetic[9,10] and environmental factors.[11] It was reported that children with parental myopia exhibited a higher risk of myopia than those whose parents were emmetropic.[5,12–14] However, it was indicated that the rapid change in the prevalence of myopia may result from the dominant impact of environmental factors.[15] For environmental factors, some studies have shown that near work and outdoor activities are potential factors associated with the myopia risk.[14,16–19]
Parents are generally the sole guardians of children. Traditionally in China, school-aged children are always inclined to agree to parents’ arrangements. What is more, previous studies revealed that parental attitudes and behaviors had an important influence on children's physical activities and screen time.[20,21] Thus, we hypothesized parents’ attitudes and behaviors toward children's visual care have a significant influence on children's myopia risk. However, the association, to the best of our knowledge, has rarely been reported. Our study focused on parents’ attitudes and behaviors toward children's visual care to evaluate their association with children's myopia risk.
2. Methods
2.1. Participants
A total of 1004 parents of school-aged children were recruited in our study by stratified cluster sampling on July, 2015. They came from different districts of Wuhan, in which the Hongshan, East-West Lake, and Jiangan districts were randomly selected within the central urban area, and the Huangpi and Xinzhou districts within the noncentral urban area. Two primary schools and 2 middle schools were chosen randomly from every district. Children in grade 1, grade 3, and grade 5 were selected from the primary school, grade 1 from the junior high school (described as grade 7 in the following text), and grade 1 from the senior high school (described as grade 10 in the following text), respectively. In each cluster, children meeting the following criteria were recruited: informed consent form signed by parents and no history or current severe disease. Children were excluded if they have the history of intra ocular surgery or ocular trauma, and if children's parents did not know whether they were myopic. Children's parents in these classes were asked to complete the questionnaire.
2.2. Ethics statement
The study was approved by the Medical Ethics Committee of Tongji Medical College, Huazhong University of Science and Technology, and followed the guidelines of the Declaration of Helsinki. The nature of the study was explained to parents and school students, and written informed consent was obtained from the parents of all participating students.
2.3. Investigated variables
The questionnaire focused on demographic information and parents’ attitudes and behaviors toward children's visual care. The demographic information included the age, gender, education, occupation, place of residence, and eyesight status of the parents and children's characteristics such as gender, age, grade, and vision. Questions were asked concerning parents’ attention to children's vision, including when they began to pay attention to their children's vision. The questionnaire evaluated parents’ behaviors toward children's visual care by the following questions: whether they reminded children to relax their eyes after using them for a long time; whether they provided their children with foods with vision-protecting properties; whether they educate their children about vision-protecting knowledge; whether they adjusted the parameters of electronic devices (i.e., brightness, contrast, and softness); whether they pay attention to children's visual hygiene; whether they stopped their children using electronic screen devices in dim light; how frequently they rectified their children's sitting and pen-holding postures when doing homework; how frequently they took their children to outdoor activities, and whether they ensured that their children got sufficient sleep. Most of the questions were multiple-choice: never, sometimes, often, and always. Parents’ attitudes to children's visual care were also investigated, which included their expectations on their children's vision, and the attitude to children's lower vision.
2.4. Methods of myopia diagnosis
We screened children's vision in primary and middle school in Wuhan every year, which was required by the Wuhan bureau of education. Two steps were taken to diagnose children's myopia. First, noncycloplegic refraction was measured by the auto-refractor (TOPCON ACP-8). The DK-10 phoropter was used to test for ametropia in each naked eye. Second, if myopia was suspected in the children, their parents were required to take them to eyesight examinations using cycloplegic refraction. Cycloplegia was achieved by using 1% cyclopentolate eye drops. Three drops of cyclopentolate were administered at 5-minute intervals and the cycloplegic refraction was measured about 30 minutes after the last application. With the cycloplegic refraction, myopia was defined as spherical equivalent (SE) of refractive error of less than –0.5 diopters (D).[22]
2.5. Statistical methodology
Statistical analyses were performed by using SPSS version 12.0. The continuous variables were presented as the mean ± SD; categorical variables were presented as n (percentage). The chi-square analysis was performed to assess the differences in the characteristic of the categorical variables and t-test analysis for continuous variables. After univariate analysis of potential associations, we performed the generalized liner mixed model with children's eyesight as the dependent variable and all parameters as fixed effect variables which showed a significant association with children's myopia risk in univariate analysis and clusters of school as the random effect variable. The generalized linear mixed model was used to identify the independent risk factors for myopia and explore the association between myopia of school-aged children and parents’ attitudes and behaviors toward their children's visual care. P < .05 was considered to be statistically significant. Odds ratios (OR) and 95% confidence intervals (95%CI) were calculated for risk factors that were independently associated with myopia in this population.
3. Results
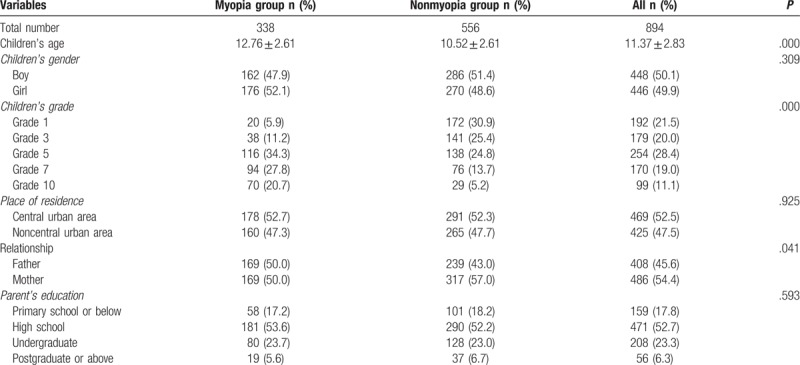
Of the 1004 parents recruited in this study, 45 invalid questionnaires and 65 questionnaires in which the parents did not know whether their children were myopic or not have been excluded. As a result, a total of 894 parents were included in our study. Table 1 showed the demographic characteristics of parents and children. Among these, 54.4% of respondents were mothers. More than half of the parents’ education background was above high school, and 6.3% parents with the lowest percentage had been educated to a postgraduate or higher level. 52.5% of families lived in the central urban area, compared with 47.5% in the noncentral urban area. The mean age of the total children was 11.37 ± 2.83. Among these, the nonmyopia group was younger than the myopia group (t = –12.451, P = .000). More children in grade 1 and 3 were not myopic in contrast to children in grade 5, 7, and 10. There were no significant differences in these characteristics between the myopia and nonmyopia groups, except the children's age and grade (P = .000).
Table 1.
Demographic characteristics of parents and children.
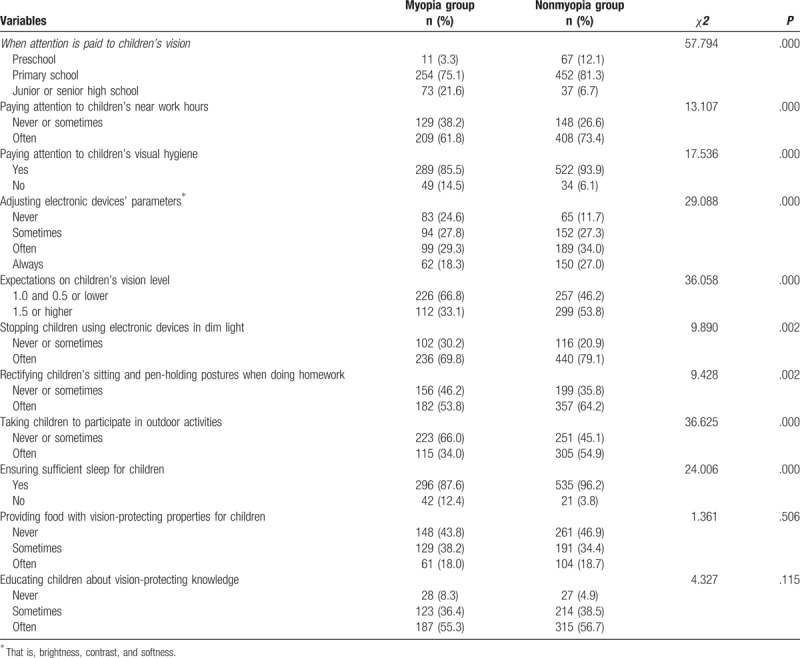
The chi-square analysis of the parents’ attitudes and behaviors associated with children's myopia risk is shown in Table 2. There was a significant difference in the time when attention was paid to children's vision (χ2 = 57.794, P < .001), and the time in the myopia group was comprised of preschool (3.3%), primary school (75.1%), and junior or senior school (21.6%) whereas that in the non-myopia group was made up of preschool(12.1%), primary school (81.3%), and junior or senior school (6.7%). Paying attention to children's near work hours was significantly different (χ2 = 13.107, P < .001) between the myopia group with never or sometimes (38.2%), often (61.8%) and the nonmyopia group with never or sometimes (26.6%) and often (73.4%). Whether parents paid attention to children's visual hygiene was significantly different (χ2 = 17.536, P < .001). “Yes” in the myopia group was 85.5% compared with 93.9% in the nonmyopia group. As for the adjustment of the parameters of their children's electronic devices, never and sometimes were selected more frequently in the myopia group than in the nonmyopia group. However, often and always were less frequently chosen (χ2 = 29.088, P < .001). Parents’ expectations on children's vision between the myopia group and the nonmyopia group were significantly different (χ2 = 36.058, P < .001) with 1.5 or higher in the nonmyopia group at 53.8% and only 33.1% in the myopia group. When asked if they stopped their children using electronic screen devices in dim light, 69.8% of parents in the myopia group chose “always” in contrast to 79.1% in the nonmyopia group with a significant difference (χ2 = 9.890, P = .002). In answer to the question how frequently they rectified their children's sitting and pen-holding postures when doing homework, the percentage of parents (53.8%) in the myopia group who indicated that they always paid attention was significantly different from that of the nonmyopia group (64.2%)(χ2 = 9.428, P = .002). More parents often took their children to participate in outdoor activities in the nonmyopia group (54.9%) than in the myopia group (34.0%) with a significant difference (χ2 = 36.625, P < .001). 96.2% of parents in the nonmyopia group ensured that their children had sufficient sleep compared with 87.6% in the myopia group with a significant difference (χ2 = 24.006, P < .001).
Table 2.
Distribution of risk factors of the children's myopia.
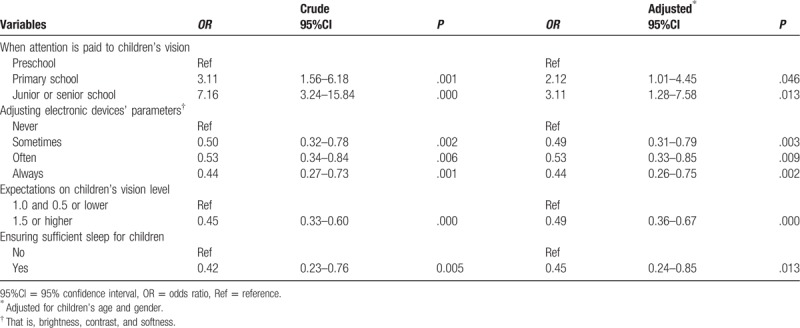
The results of the generalized linear mixed model of parents’ attitudes and behaviors associated with their children's myopia risk are shown in Table 3. After adjusting for the potential confounders of children's age and gender, the following 4 factors associated with children's myopia risk were found. Compared with preschool, children whose parents only began to pay attention to their vision when they were in junior or senior school had the highest risk of myopia (OR = 3.11, 95%CI = 1.28–7.58, P < .05), followed by those when they were in primary school (OR = 2.12, 95%CI = 1.01–4.45, P < .05). Children whose parents expected their children to have vision of at least 1.5 had a significantly decreased risk of myopia (OR = 0.49, 95%CI = 0.36–0.67, P < .001), compared with 1.0 and 0.5 or lower. Compared with never, parents who adjusted the parameters of their children's electronic devices sometimes (OR = 0.49, 95%CI = 0.31–0.79, P = .003), often (OR = 0.53, 95%CI = 0.33–0.85, P = .009), and always (OR = 0.44, 95%CI = 0.26–0.75, P = .002) decreased the risk of myopia significantly. Children who were ensured sufficient sleep had a significantly decreased risk of myopia (OR = 0.45, 95%CI = 0.24–0.85, P < .05). However, no significant association between parents’ behaviors of taking children to participate in outdoor activities and their children's myopia risk was observed after adjusting for the potential confounders (OR = 0.74, 95%CI = 0.53–1.04, P = .081).
Table 3.
Parents’ attitudes and behaviors with children's myopia risk.
4. Discussion
Prevalence of myopia is associated with heredity[9,10] and environment.[11] Wojciechowski's study[23] indicated that the myopia “epidemic” was considered to be related with the environmental and behavioral factors. For the environmental factor, most attention was paid to the near work and to outdoor activities.[14,16–19] Studies have reported that children's health is significantly associated with parents’ attitudes and behaviors.[24–26] However, the influence of parents’ attitudes and behaviors on children's myopia risk was rarely reported. Our study has found that parents’ attitudes and behaviors toward children's visual care can influence the myopia risk of school-aged children to a large extent.
According to the chi-square analysis, our study found that parents’ behaviors such as paying attention to children's near work hours and visual hygiene, adjusting the parameters of electronic devices, stopping children using electronic screen devices in dim light, rectifying children's sitting and pen-holding postures when doing homework, taking children to participate in outdoor activities, and ensuring sufficient sleep for their children could all decrease the myopia risk. Our study also found that the time at which parents paid attention to their children's vision and parents’ expectations on their children's vision were both associated with the myopia risk.
The results of the generalized linear mixed model indicated that paying attention to children's vision early, parents’ high expectations on their children's vision, frequent adjustment of the parameters of electronic devices, and ensuring sufficient sleep for their children had all protected children from myopia.
Our study has found that if parents pay attention to children's vision early, the risk of children's myopia will be decreased. It has been reported that the preschool period is crucial for the development of eyesight, besides, children can achieve the best possible eyesight before puberty.[27] So if intervenes can be taken during preschool period, school-aged children will have a lower risk of myopia. In terms of the relationship between attitudes and behaviors, attitudes can contribute to the behavior intention and finally to the relevant behaviors. Besides, stable and accessible attitudes have a strong association with future behaviors,[28] and parents’ positive attitudes can result in effective behaviors toward their children's eyesight. Parents pay attention to their children's vision at an early stage and consequently intervene by, for example, restricting the number of hours their children spend doing near work and by increasing outdoor activities which are considered as factors protecting against myopia.[14,16–19] So the time when parents pay attention to children's vision may be associated with the time of parents’ behaviors in protecting their children's vision, and consequently influences children's myopic development.
Our study found a lower risk of myopia if parents had higher expectations on their children's vision. Parents with higher expectations on their children's vision may pay more attention to their children's vision and take more measures to prevent children from myopia. According to the expectancy effect,[29] parent's expectations on children's vision may also have an influence on children's relevant attitudes and behaviors in regard to visual care, and then children may develop healthy habits to prevent myopia onset or development.
Fernández -Montero's study[30] found that longer computer usage times increased the risk of myopia development or progression. Our study indicated that parents’ adjustment of the parameters of their children's electronic devices (i.e., brightness, contrast, and softness) frequently has a protective effect on the myopia risk. In terms of Shen's finding [31] that human visual comfort was associated with the balanced screen-background luminance ratio by varying background luminance, we can also mediate the screen luminance in order to enhance visual comfort. So when children use electronic screen devices, attention should be paid not only to the time, but also to the devices’ parameters.
By ensuring sufficient sleep for their children, parents can also reduce the risk of children's myopia. The result is in line with Gong's finding [14] that children who slept for shorter periods of time were significantly more likely to have myopic refractions. Jee's study[32] also found that myopia had an inverse relationship with sleep duration. The reason cannot be explained completely at present. Regular sleep is a crucial part of circadian rhythms which guarantee normal growth and development, but the ocular rhythms disturbed by deficient sleep have a negative influence on eye growth.[33] According to animal experiments, deprivation of sleep in mouse could result in the refractive error,[34] and studies has found the significant role of dopamine on the onset and development of myopia,[35] both of which play an indicating role in human myopia. So the appropriate sleeping time of school-aged children should be guaranteed to help prevent them from developing myopia.
Although some surveys have reported the association between outdoor activities and myopia, this issue remains controversial. In the current study, the frequency of taking children to participate in outdoor activities is not associated with children's myopia risk after adjusting for the confounders. It is consistent with Lin's finding,[19] but contrasts with other studies.[16,17]
In conclusion, parents’ attitudes and behaviors have an influence on children's myopia risk. This may not only make children conscious of the importance of protecting their vision, but also rectify children's unhealthy visual habits to prevent myopia. In the future, it is important to take more measures to educate parents on how to protect children's vision, and efforts can be made in the following aspects: print some brochures about healthy habits with eyes and distribute them to parents; regularly held parents’ meeting to carry out health education about eyesight protection; establish the record of health management on eyesight to warn parents early. As a consequence, the incidence of children's myopia can be decreased as a result of parents’ positive attitudes and behaviors toward children's visual care.
The study also has some limitations. First, parents’ attitudes and behaviors were obtained from questionnaires, which could be subject to recall bias. In addition, as a case-control study, the cause or effect of parents’ attitudes and behaviors toward their children's myopia development was not clear. So the future cohort study with a larger sample size is required to demonstrate the association between parents’ attitudes and behaviors and children's myopia risk.
Footnotes
Abbreviations: 95%CI = 95% confidence interval, D = diopters, OR = odds ratio, SD = standard deviation, SE = spherical equivalent.
Authorship: MXL and LHY conceived and designed the research study; SZ and DDD extracted the data; SZ and SQW analyzed the data; SZ wrote the paper; XXL and TX performed the research study; BLL and HXW reviewed and edited the manuscript. All authors read and approved the manuscript.
Funding: This work was supported by NKTRDP of Wuhan (200760423157) and the Fundamental Research Funds for the Central Universities, HUST (2172012ZHYX004).
The authors have no conflicts of interest to disclose.
References
- [1].Foster PJ, Jiang Y. Epidemiology of myopia. Eye 2014;28:202–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Pan CW, Ramamurthy D, Saw SM. Worldwide prevalence and risk factors for myopia. Ophthalmic Physiol Opt 2012;32:3–16. [DOI] [PubMed] [Google Scholar]
- [3].Dong YH, Liu HB, Wang ZH, et al. Prevalence of myopia and increase trend in children and adolescents aged 7-18 years in Han ethnic group in China, 2005–2014. Zhonghua Liu Xing Bing Xue Za Zhi 2017;38:583–7. [DOI] [PubMed] [Google Scholar]
- [4].Wu JF, Bi HS, Wang SM, et al. Refractive error, visual acuity and causes of vision loss in children in Shandong, China. The Shandong Children Eye Study. PLoS One 2013;8:e82763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Guo L, Yang J, Mai J, et al. Prevalence and associated factors of myopia among primary and middle school-aged students: a school-based study in Guangzhou. Eye 2016;30:796–804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Lyu Y, Zhang H, Gong Y, et al. Prevalence of and factors associated with myopia in primary school students in the Chaoyang District of Beijing, China. Jpn J Ophthalmol 2015;59:421–9. [DOI] [PubMed] [Google Scholar]
- [7].Guo K, Yang DY, Wang Y, et al. Prevalence of myopia in schoolchildren in Ejina: the Gobi Desert Children Eye StudyMyopia in the Gobi Desert Children Eye Study. Invest Ophthalmol Vis Sci 2015;56:1769–74. [DOI] [PubMed] [Google Scholar]
- [8].Holden B, Sankaridurg P, Smith E, et al. an underrated global challenge to vision: where the current data takes us on myopia control. Eye 2014;28:142–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Zhang Q. Genetics of refraction and myopia. Prog Mol Biol Transl Sci 2015;134:269–79. [DOI] [PubMed] [Google Scholar]
- [10].Wojciechowski R. Nature and nurture: the complex genetics of myopia and refractive error. Clinical Genet 2011;79:301–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Ramamurthy D, Lin Chua SY, Saw S. A review of environmental risk factors for myopia during early life, childhood and adolescence. Clin Exp Ophthalmol 2015;98:497–506. [DOI] [PubMed] [Google Scholar]
- [12].Xiang F, He M, Morgan IG. The impact of parental myopia on myopia in Chinese children: population-based evidence. Optom Vis Sci 2012;89:1487–96. [DOI] [PubMed] [Google Scholar]
- [13].Zhang X, Qu X, Zhou X. Association between parental myopia and the risk of myopia in a child. Exp Ther Med 2015;9:2420–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Gong Y, Zhang X, Tian D, et al. Parental myopia, near work, hours of sleep and myopia in Chinese children. Health 2014;6:64–70. [Google Scholar]
- [15].Rose KA, Morgan IG, Smith W, et al. High heritability of myopia does not preclude rapid changes in prevalence. Clin Exp Ophthalmol 2002;30:168–72. [DOI] [PubMed] [Google Scholar]
- [16].French AN, Ashby RS, Morgan IG, et al. Time outdoors and the prevention of myopia. Exp Eye Res 2013;114:58–68. [DOI] [PubMed] [Google Scholar]
- [17].Guggenheim JA, Northstone K, McMahon G, et al. Time outdoors and physical activity as predictors of incident myopia in childhood: a prospective cohort studytime outdoors and incident myopia in childhood. Invest Ophthalmol Vis Sci 2012;53:2856–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Lin Z, Vasudevan B, Jhanji V, et al. Near work, outdoor activity, and their association with refractive error. Optom Vis Sci 2014;91:376–82. [DOI] [PubMed] [Google Scholar]
- [19].Lin Z, Vasudevan B, Mao GY, et al. The influence of near work on myopic refractive change in urban students in Beijing: a three-year follow-up report. Graefes Arch Clin Exp Ophthalmol 2016;254:2247–55. [DOI] [PubMed] [Google Scholar]
- [20].Xu H, Wen LM, Rissel C. Associations of parental influences with physical activity and screen time among young children: a systematic review. J Obes 2015;2015:546925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].O’Connor TM, Chen T-A, Baranowski J, et al. Physical activity and screen-media-related parenting practices have different associations with children's objectively measured physical activity. Childhood Obesity 2013;9:446–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Morgan IG, Ohno-Matsui K, Saw S-M. Myopia. Lancet 2012;379:1739–48. [DOI] [PubMed] [Google Scholar]
- [23].Wojciechowski R, Hysi PG. Focusing in on the complex genetics of myopia. PLoS Genet 2013;9:e1003442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Case A, Paxson C. Parental behavior and child health. Health Affairs 2002;21:164–78. [DOI] [PubMed] [Google Scholar]
- [25].Szilagyi PG, Schor EL. The health of children. Health Services Res 1998;33(4 pt 2):1001–39. [PMC free article] [PubMed] [Google Scholar]
- [26].Wong ST. The relationship between parent emotion, parent behavior, and health status of young African American and Latino children. J Pediatr Nurs 2006;21:434–42. [DOI] [PubMed] [Google Scholar]
- [27].Warburg M. Development of sight. Ugeskr Laeger 1991;153:1571–5. [PubMed] [Google Scholar]
- [28].Glasman LR, Albarracin D. Forming attitudes that predict future behavior: a meta-analysis of the attitude-behavior relation. Psychol Bull 2006;132:778–822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Kohn PM. Relationships between expectations of teachers and performance of students. J Sch Health 1973;43:498–503. [DOI] [PubMed] [Google Scholar]
- [30].Fernández-Montero A, Olmo-Jimenez JM, Olmo N, et al. The impact of computer use in myopia progression: a cohort study in Spain. Prev Med 2015;71:67–71. [DOI] [PubMed] [Google Scholar]
- [31].Shen Y, Kuai S, Zhou W, et al. Study of preferred background luminance in watching computer screen in children. Chin Med J (Engl) 2014;127:2073–7. [PubMed] [Google Scholar]
- [32].Jee D, Morgan IG, Kim EC. Inverse relationship between sleep duration and myopia. Acta Ophthalmol 2016;94:e204–10. [DOI] [PubMed] [Google Scholar]
- [33].Nickla DL. Ocular diurnal rhythms and eye growth regulation: where we are 50 years after Lauber. Exp Eye Res 2013;114:25–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Tkatchenko TV, Shen Y, Tkatchenko AV. Mouse experimental myopia has features of primate myopia. Invest Ophthalmol Vis Sci 2010;51:1297–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Feldkaemper M, Schaeffel F. An updated view on the role of dopamine in myopia. Exp Eye Res 2013;114:106–19. [DOI] [PubMed] [Google Scholar]


