Abstract
Background
Mobile phone apps capable of monitoring arrhythmias and heart rate (HR) are increasingly used for screening, diagnosis, and monitoring of HR and rhythm disorders such as atrial fibrillation (AF). These apps involve either the use of (1) photoplethysmographic recording or (2) a handheld external electrocardiographic recording device attached to the mobile phone or wristband.
Objective
This review seeks to explore the current state of mobile phone apps in cardiac rhythmology while highlighting shortcomings for further research.
Methods
We conducted a narrative review of the use of mobile phone devices by searching PubMed and EMBASE from their inception to October 2018. Potentially relevant papers were then compared against a checklist for relevance and reviewed independently for inclusion, with focus on 4 allocated topics of (1) mobile phone monitoring, (2) AF, (3) HR, and (4) HR variability (HRV).
Results
The findings of this narrative review suggest that there is a role for mobile phone apps in the diagnosis, monitoring, and screening for arrhythmias and HR. Photoplethysmography and handheld electrocardiograph recorders are the 2 main techniques adopted in monitoring HR, HRV, and AF.
Conclusions
A number of studies have demonstrated high accuracy of a number of different mobile devices for the detection of AF. However, further studies are warranted to validate their use for large scale AF screening.
Keywords: mobile phone apps, atrial fibrillation, heart rate, arrhythmia, photoplethysmography, electrocardiography, mobile health
Introduction
Over the past years, there has been a significant increase in the number of mobile phone apps focusing on cardiovascular diseases. These apps are designed to monitor cardiovascular risk factors such as obesity, smoking, sedentary lifestyle, diabetes, and hypertension as well as to prevent and manage chronic conditions such as atrial fibrillation (AF) [1-5]. There are currently more than 100,000 available mobile health apps on iTunes and Google Play as well as more than 400 wearable activity monitors [6]. Approximately 64% of adults possess a mobile phone in the United States, and 62% of mobile phone owners use their phones to access health information and obtain education about diseases and health conditions [6]. Previous research has reported the benefits of using mobile health in modifying behavior to improve cardiovascular health through dietary management, physical activity promotion, smoking cessation, weight control, blood pressure control, cholesterol management, and blood sugar measurement [7-12]. However, there remains some ambiguity when it comes to the use of such apps in heart rate (HR) and HR variability (HRV) because of the lack of reliable statistical tests used in studies and the lack of standardized recommendations from professional bodies in terms of screening and monitoring of these parameters, as highlighted by Pecchia et al recently [13].
Currently, mobile phone–based photoplethysmography (PPG) and handheld electrocardiograph (ECG) recorders are the 2 main concepts adopted in monitoring HR, HRV, and AF [14,15]. PPG is an optical technique that detects heartbeats by analyzing changes in skin color and light absorption. Using a mobile app, the PPG sensor detects variations in light intensity via transmission through or reflection from the tissue (the reflectance and transmittance model). The variations in the light intensity are related to changes in the blood perfusion of the tissue, and based on these changes, heart-related information can be retrieved [14,16]. Similarly, the handheld ECG recorder is also based primarily on a mobile phone and mobile phone app interface. However, an additional external component, an ECG sensor unit, is required for the app to function adequately. This will then allow for a standard lead I ECG to be recorded [15]. For the purpose of this review, the term handheld ECG recorder will refer specifically to the mobile phone app involving an external ECG sensor component, which is not required by the PPG approach.
Studies have been conducted using mobile phone apps, such as AliveCor, to detect arrhythmias such as AF [17-19], atrial flutter, atrial and ventricular premature beats, bundle branch blocks, and ST-segment abnormalities [20]. As the use of mobile phone apps in cardiovascular care is a rapidly evolving field, this literature review seeks to act as a checkpoint, encapsulating the current state of mobile phone–based PPG and ECG recorders in monitoring HR, HRV, and AF. This will put into perspective what has been effective and applicable along with the relevant challenges encountered to better navigate future research projects into this niche.
Methods
Overview
A PubMed and EMBASE search that primarily concerned the use of mobile phone apps for monitoring HR, HRV, and AF was conducted. The following search string was employed: (“mobile applications” OR “smartphone” OR “digital health”) AND (“atrial fibrillation” OR “heart rate”). The search period was determined as beginning from the earliest available publications in the databases to October 14, 2018. No language restrictions were included.
The search results were subsequently transferred to Microsoft Excel (Microsoft Corp, Redmond WA), and all potentially relevant reports were retrieved as complete manuscripts and abstracts and assessed for compliance with relevance to the 4 core principles of this narrative review: (1) mobile phone apps, (2) HR, (3) HRV, and (4) AF. Overall, 3 authors (CL, FW, and TT) independently reviewed each publication and report, and findings were agreed upon by consensus with input from 2 senior researchers (BY and GT). A total of 1006 papers were found, and 822 publications were excluded after screening due to irrelevance and noncompliance with principles explored. Thus, 124 papers were used for this narrative review (Multimedia Appendix 1).
Results
Atrial Fibrillation and Other Arrhythmias
Atrial Fibrillation—KardiaMobile App
The KardiaMobile app, developed by AliveCor [21], is a commonly used device in studies investigating the monitoring of AF. The equipment comprises a finger pad sensor for the left and right hands, which is attached to the mobile phone, and an app that receives the transmitted information. A 2017 study by Tu et al gives a detailed account of the technology used by the device [22]. When fingers are placed on the sensors, recording begins. Using a 19,000 Hz center frequency and a modulation index of 200 Hz/mV, electrical activity is transmitted to the mobile phone via ultrasound signal frequency modulation to obtain the ECG trace. The frequency and modulation index signal that is transmitted to the microphone of the mobile phone are digitized at 44.1 kHz and 24-bit resolution, respectively. The app is then able to produce an ECG trace from the received signal (300 samples/second, 16-bit resolution), which can either be viewed as it is produced or be stored as a PDF file for later viewing. On the basis of the absence of P waves and irregularity of the RR (R wave to R wave) interval, the associated algorithm within the app produces a potential AF diagnosis [22].
The Lau et al study [23] took a group of 109 patients, 39 of which were in AF, and used the AliveCor algorithm to analyze the rhythms, obtaining a sensitivity of 87% and specificity of 97% when compared with interpretation by a cardiologist. The algorithm was then altered by increasing the weighting of absent P waves in the diagnostic process, and recordings were conducted on this same set of patients. The optimized algorithm was found to have a sensitivity of 100% and specificity of 96%. A second set of 204 patients, with 48 having known AF, were then analyzed by the optimized algorithm, which obtained a sensitivity of 98% and specificity of 97% in this second dataset. Other studies have largely found the sensitivity of the AliveCor device to be in the region of 90% to 98%, with specificity values ranging from 29.2% to 99% in various studies [24-29]. However, a study on the use of AliveCor in inpatients in cardiology and geriatric wards only found a sensitivity of 54.5% and 78.9%, respectively, for these groups [26], whereas another study published in 2017 used the AliveCor algorithm as a control and found a sensitivity of 71.4% for AliveCor [30]. A study of 13,222 patients identified 101 participants to have previously undiagnosed AF, with 65.3% of these patients reporting no symptoms before this diagnosis [24]. Within the field of pediatrics, accurate single-lead ECG tracings were also obtained in both healthy children and children with arrhythmic abnormalities [31]. The device is generally well tolerated, and patients report that it is easy to use [27]. Implementation of the AliveCor in community health care settings has also been investigated. Patients generally responded positively to the suggestion of an ECG being conducted by a pharmacist while they were attending the pharmacy for other purposes [32]. However, some patients were unwilling to have this conducted for the fear of discovering something was wrong. In a primary care setting, the use of AliveCor was well received by patients, but the staff had some reservations about being involved because of a self-perceived lack of knowledge [33]. Patients also report that they felt more confident in managing their AF by using the app [27,34]. The AliveCor device [18,35-37] has also been incorporated with patient education to increase the knowledge of the patients about AF [38]. Mobile apps have been extended to monitor paroxysmal AF for intermittent anticoagulation [39]. This evidently raises public health issues of systematic and opportunistic screening. In a recent evaluation of the European Heart Rhythm Association Consensus on screening AF, opportunistic screening was recommended for individuals aged above 65 years and younger patients at high risk of stroke [40]. As such, it is important to understand local screening guidelines before systematic or opportunistic screenings commence as large number of false positives yields unnecessary, expensive, and potentially harmful follow-ups that might affect patients’ mental health.
Atrial Fibrillation—CardiioRhythm App
The detection of AF by analysis of finger and facial PPG signals using the CardiioRhythm mobile phone app has been tested in 2 recent studies. In the study by Chan et al [30], finger PPG waveforms of 20-seconds duration were captured 3 times using an iPhone 4S equipped with the CardiioRhythm app and compared with the AliveCor single-lead ECG as referenced. Finger PPG waveforms were captured using the light emitting diode flash of the iPhone and the camera, which detected reflected light to measure the arterial pulsation. These waveforms were recorded at 30 Hz, with the duration of each recording being 17.1 seconds, and were filtered with a bandpass filter using a range of 0.7 Hz to 4.0 Hz. AF was diagnosed from this if 2 of the 3 PPG recordings were irregular. This was defined as a lack of repeating pattern, using a Support Vector Machine to classify the waveforms as similar or nonsimilar to other waveforms. Analysis of the diagnoses put forward by the CardiioRhythm app in this study showed a sensitivity of 92.9% and specificity of 97.7% in detecting AF compared with a sensitivity of 71.4% for the AliveCor device that was obtained by this study. This study found the specificities for the 2 devices to be comparable. The first prospective, international, 2-center, clinical validation study (DETECT AF PRO) based on similar finger PPG technology was also conducted recently to demonstrate the feasibility of such apps alone with a 5-min sensitivity and specificity of 91.5% and 99.6%, respectively [41].
In another study by Yan et al, the CardiioRhythm app was used to analyze facial PPG signals in 217 patients recorded using the front camera of an iPhone 6S without physical contact (Figure 1) [42]. Overall, 3 successive 20-second recordings were acquired per patient. Pulse irregularity in 1 or more PPG readings or 3 uninterpretable PPG readings were considered a positive AF screening result. The CardiioRhythm facial PPG app demonstrated a sensitivity of 94.7% and specificity of 95.8%. The positive and negative predictive values were 92.2% and 97.1%, respectively.
Figure 1.
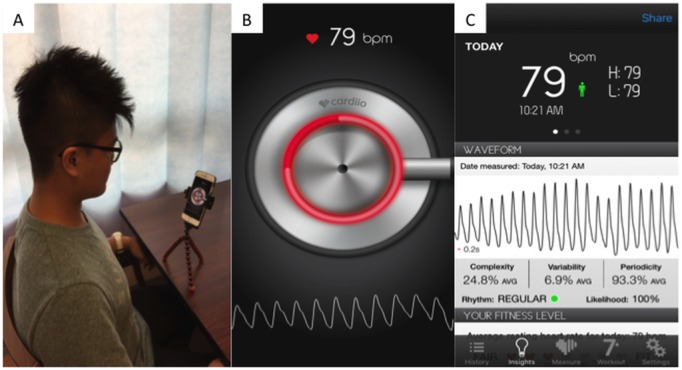
(A) Patient setup; (B) cardiioRhythm app facial photoplethysmography analysis interface; and (C) complete facial photoplethysmography signals report.
Atrial Fibrillation—FibriCheck App
A recent study conducted by Mortelmans et al [43] used the PPG app FibriCheck. The patient places the left index finger over the flashlight and camera, holding their finger horizontally and keeping the finger in place for 1 min. To ensure an accurate reading, the screen becomes red when appropriate contact has been made, and the practitioner manually commences the measurement. The amount of light that is reflected onto the camera is then captured and used to calculate the variation in local arteriole blood volume pulse variation. The rhythm of the pulse is then identified based on the RR interval. The app in the mobile phone then judges the quality of the signal based on the detection of the pulse. If the detection was masked with noise, or beats were absent, these recordings were not included in the app’s analysis. When measurements were detected as a good signal, these data were interpreted by the AF algorithm.
Concurrently with the PPG measurement, a single-lead ECG was taken and analyzed by the FibriCheck app. Selection of the data took place based on quality, and good quality measurements were analyzed by the AF algorithm using variability between RR intervals to detect irregularities. The FibriCheck app was used on an iPhone 5S. With 242 participants, this study found a sensitivity of 98%, specificity of 88%, and accuracy of 93% for the FibriCheck algorithm when the data were obtained via PPG. Interpretation by the app of the single-lead ECG performed better, yielding a sensitivity of 98%, specificity of 90%, and accuracy of 94% when compared with standard ECG. When comparing the 2 methods by false-positive results, when analyzed by FibriCheck, 8 false positives were produced from a trace obtained by PPG measurement and 11 false positives were produced from a trace obtained by a single-lead ECG.
Atrial Fibrillation—Other Methods of Detection
Some studies have looked at the use of the inertial measurement unit, using modern microelectromechanical (MEMS) sensors already present in mobile phones, to detect AF [44]. The patient is advised to lie supine and place the mobile phone on their chest. The accelerometer of the mobile phone, which detects the orientation of the phone, can detect cardiogenic movements of the chest. The movements detected are those caused by the opening of the aortic valve, and so, the interval between each successive valve opening is recorded and considered to determine the presence of AF. This yielded a sensitivity of 93.8% and specificity of 100% in the detection of AF. A similar study used the MEMS sensors of mobile phones to obtain measurements, which when analyzed by machine learning methods found a sensitivity of 98.5% and specificity of 95.2% in its best performing method [45].
The feasibility of producing a wearable sensor that records HR and transmits information to a mobile phone app was examined [46]. The way this app identifies AF is similar to the FibriCheck app. As an example, a 42-year-old male admitted with new-onset AF of undetermined duration was deemed appropriate for electrocardioversion because of his FitBit Charge HR device recording the time at which increased HR was observed, allowing the onset of AF to be identified [47]. In a study by Yan et al, the diagnostic accuracy of the CardiioDeepRhythm app, a deep convolutional neural network for detecting AF from the PPG signal acquired using an off-the-shelf wrist-worn device (Empatica E4, Milan, Italy), was tested in 51 in-hospital patients reporting a sensitivity and specificity of 93% and 94%, respectively [48]. These findings demonstrate the promising value of PPG sensors for ambulatory AF monitoring. Krivoshei et al [49] conducted a study investigating the use of PPG in AF, with a view to implementing the technology in a smartwatch; the protocol for this trial was published as an abstract during a conference [50]. Table 1 summarizes the sensitivities and specificities of the apps in AF detection. Despite some studies conducting direct comparisons between different technological modalities [30], it is still done with reference to the gold standard of a conventional 12-lead ECG within a short period. This is especially important because none of the new app technologies have been properly integrated into the wider health care network as compared with the 12-lead ECG, which is a validated instrument commonly available within primary and secondary care settings.
Table 1.
Sensitivities and specificities for the 5 main technologies applied in atrial fibrillation detection.
| Modalities | Sensitivity (%) | Specificity (%) |
| Original AliveCor algorithm (finger pad sensor) | 54.5-98.0 | 29.2-99.0 |
| Optimized AliveCor algorithm (finger pad sensor) | 98-100 | 96-97 |
| CardiioRhythm (finger PPGa) | 92.6-92.9 | 94.8-97.7 |
| CardiioRhythm (facial PPG) | 94.7 | 95.8 |
| CardiioRhythm (wristband PPG) | 93 | 94 |
| FibriCheck (finger PPG) | 98 | 88-90 |
| Inertial measurement unit (chest accelerometer) | 93.8-98.5 | 95.2-100 |
aPPG: photoplethysmography.
Heart Rate and Heart Rate Variability
Heart Rate
There has been considerable innovation in the use of mobile phone apps for the purpose of HR monitoring in adults. In particular, numerous studies have investigated the potential of 2 specific methods—seismocardiogram (SCG) and PPG—in producing accurate HR measurements. Landreani et al, for instance, described the application of SCG and ballistocardiogram (BCG) signals for HR monitoring apps in mobile phone–embedded accelerometers [51]. This is achieved by determining the RR interval of sufficient amplitude and subsequently detecting the fiducial peak from the SCG and BCG signals. In PPG, the accuracy of this method was also demonstrated in a study by Alaleef et al, who found a 99.7% accuracy and maximum absolute error of 0.4 beats/min [52]. The accuracy and feasibility of PPG signals from mobile phone apps also varied between different types of PPG apps. In Parpinel et al’s study, higher feasibilities and accuracies were found for contact PPG–based apps compared with the noncontact PPG–based ones [53]. Koenig et al [54] found that their algorithm using PPG to assess HR had a consistent accuracy when compared with ECG (correlation index R>.99).
Gold Standards and Validation of Mobile Phone Heart Rate Apps
Although there is currently no consensus on the gold standard for the validation of HR apps, Vanderberk et al suggested the comparison of the HR on mobile phone apps with an ECG system via RR intervals. With regard to the actual accuracy of these mobile phone apps, there was no significant difference (P=.92) found between the interval measurements of the HR app and the ECG system, suggesting that the HR apps have a comparable accuracy with ECGs [55]. This is further supported by a recent comparison of 3 HR apps against simultaneous standard ECG monitoring, which found an acceptable correlation. However, accuracy became questionable in specific cases of irregular rhythms such as AF [56].
Heart Rate Apps in Different Fields
The use of HR apps has been tested in different clinical settings. In a specific app reviewed by Chaudhry et al, named Unique Heart Rate Monitor, PPG was used for the measurement and categorization of workout intensity. It also allows subjects to check their HR in response to medical therapy [57]. The clinical use of HR apps during exercise was also assessed by numerous studies. In particular, some studies noted that the measurement accuracy tended to differ at different exercise intensities. In 1 study, the app had higher measurement errors at increased exercise intensities when compared with Holter echocardiography monitors; however, it had similar accuracy to the Holter monitor at resting and recovery stages [58]. Yan et al presented similar findings, although the correlations between the facial PPG–estimated HR and ECG HR had smaller variations (r=.997 on resting compared with r=.982 with postmoderate intensity exercise) [59]. Furthermore, it was also found that both iOS and Android operating systems, with the same HR app, had concurrent validity with an FT7 Polar HR monitor at rest and at postexercise time points [60]. Although many studies reported the use of mobile phones as the media for measuring and interpreting HRs, some studies used mobile phone apps as a feedback system rather than the actual HR sensor. By using Bluetooth communication, subjects had their HR measured by a specially devised HR sensor at different exercise intensities, and this information was transferred via Bluetooth back to the mobile phone for analysis based on existing information during the pre-exercise period [61]. In addition, some cardiac HR monitors have a built-in alert system with real-time bradycardia and tachycardia arrhythmia detection. In the study by Golzar et al, users reported almost zero delays with data transmission and a 91.62% performance accuracy in comparison with regular ECG monitoring [62].
Apart from using HR apps for exercise HR monitoring, other studies also investigated the potential use of HR monitoring to reduce the exercise-induced risk of hypoglycemia. This is done within the context of control-to-range closed-loop artificial pancreas systems. By integrating HR as part of the feedback system in the Android app, it was found that the inclusion of HR monitoring better controlled blood glucose decline during exercise (P=.02) and resulted in fewer hypoglycemic events during exercise (P=.16 for none vs 2 events) [63].
The use of camera-based PPG has also been suggested for use in other age groups, including infants and newborns. Although the method has reported inaccuracies because of subject movements throughout the day, Kevat et al found that this method of HR measurement had increased clarity and precision in neonates receiving phototherapy [64]. Although this specific application of PPG may have potential use in pediatric patients, the inaccuracies of this method remain. Thus, when PPG is compared with normal ECG monitoring, different phone apps had lower accuracies for HR measurements using the finger or toe but higher accuracies at the earlobes. HR measurements were inaccurate above 120 bpm [65]. These results suggest that the technique is still evolving and requires considerable research before implementing it as a standard alternative to regular ECG HR monitoring for pediatric populations.
Apart from HR measurements in neonates and children, Android-based HR apps have also been developed to track and increase adherence to certain activities such as breathing awareness meditation. In the study by Gregoski et al, a tension tamer HR app used PPG via phone camera lens to transmit time-stamped HRs back to the hospital server for real-time adherence collection [66]. However, the very small sample size prevents definite conclusions to be drawn. The inaccuracies of these mobile phone apps were also found in the context of fetal HR monitoring by Soffer et al, who reviewed 30 unique apps and found that over 33% of the apps did not put disclaimers and/or provided false medical information [67].
Although PPG has been widely investigated, the use of mobile phones to generate phonocardiograms (PCGs) has been reviewed by many investigators such as Chen et al, who used iPhone 4S to record heart sounds from subjects at rest or postexercise and used these sounds for HR calculation in PCGs via the peak-based detection method [68]. Although the use of this Web-based PCG-template extraction and matching was found to be accurate, further research needs to be done to validate this finding.
Heart Rate Variability
Apart from HR, HRV measurements in mobile phone apps have also been extensively researched. Sometimes coined as the RR interval, HRV is the measure of the variation in time intervals between heartbeats, usually with reference to ventricular contraction. Classically, HRV is measured using the ECG using mainly the time-domain and frequency-domain approaches introduced in 1996 [69,70].
With the use of PPG, Bolkovsky et al used both Android and iPhone mobile phones to obtain RR intervals and subsequently deduce HRV via complex HRV algorithms. Although the results were statistically same as the ECG gold standard, the main issue was the insufficient sampling rate in both phones (20 Hz in Android and 30 Hz in iPhone), which was below the suggested rate of 250 Hz [71]. mobile phone PPG has also been advocated by Plews et al, who reported almost perfect correlations of PPG with the ECGs (R=.99), with an acceptable technical error of estimates and trivial differences in standardized differences [72]. The accuracy and reliability of mobile phone PPGs have also been validated in other studies; in some cases, mobile phone PPGs were found to have comparable accuracies with commonly used HRV computer software programs (R=.92) [73]. Other methods of HRV measurement have also been studied, such as seismocardiography. Although sampling frequency from mobile phone devices accounted for a significant source of error, RR series measurements differed by less than 10 ms in some studies, suggesting the comparable accuracy of this measuring technique [74].
Although many studies support mobile phone PPG, common errors in using this low-cost technology include frequent noise and artifacts in measurement. To reduce the impact of noise, however, Huang et al proposed the use of a continuous wavelet transform denoising technique to extract the pulse signal and subsequently deduce the RR intervals in the denoised signal. The experiments showed low mean absolute errors of only 3.53 ms, highlighting the efficacy of this proposed method in reducing mobile phone PPG errors. The use of this technique for error reduction should thus be investigated further [75].
Although methods have been proposed to reduce the impact of noise and artifacts in HRV measurement, other studies have investigated the effect of mobile phone models on the SD of beat-to-beat error measurement (SDE) of HRV indices. In 1 study, 2 different mobile phone models (Samsung S5 and Motorola) showed significant device influence in the supine posture measurement, with the Motorola model having a higher SDE than the Samsung S5 [76].
Application of Heart Rate Variability
In 1 case report, Lai et al reported the potential use of HRV measurement analysis in monitoring concussed athletes as well as assessing their capacity to return-to-play [77]. Via an AliveCor mobile phone ECG app, HRV parameters were statistically significant in symptomatic and recovered concussed athletes. However, the study noted that this difference was affected by the severity of traumatic brain injury, whereas other similar studies reported no difference in HRV parameters [78,79]. Other studies also proposed the potential use of mobile phone–derived HRV in athletic training programs; for instance, collection of daily HRV data on mobile phones using ultrashort HRV measures provides trainers with numerical indicators on athlete coping and adaptation [80]. Similar studies by Flatt et al also found that measuring the log-transformed root mean square of successive RR intervals (RMSSD) multiplied by 20 (lnRMSSDx20) obtained by mobile phone apps were sensitive markers to the changes in training load in soccer team’s training program [81].
HRV by mobile phone apps have also been used as an accurate predictor of acute mountain sickness (AMS) at high altitudes. In 1 study, Mellor et al reported lower HRV scores in those with mild and severe AMS compared with those without AMS (P=.007) and found that a reduction in HRV greater than 5 had an 83% sensitivity and 60% specificity of identifying severe AMS. As this is the first study of its kind, further studies should be conducted to confirm these findings [82].
HRV measurement by mobile phone apps was also investigated with regard to the autonomic nervous system and mental health. For instance, Heathers et al found that pulse rate variability (PRV) could be measured by mobile phone substitutes with accuracies ranging from 2% to 5% for low- and high-frequency spectral power, respectively [83]. Mobile phone apps, thus, may play a future role in psychophysiological research. In addition, mobile phones have also been used in stress classification via the use of night-time HRV data and as a monitoring tool for mental stress in different psychological settings [84,85]. The drawbacks of these studies, however, are the fairly low accuracies (59%) and that the HRV measurements were confined to ultra-short periods. The potential for long-term measurement should thus be investigated [85].
Other Arrhythmias
Although a large proportion of the research has investigated the use of mobile apps to detect AF, other arrhythmias have been investigated. A study presented in abstract in 2016 by Dimarco et al [86] used the AliveCor device to investigate 148 patients who had reported palpitations for arrhythmias. The device was used as an alternative to ambulatory monitoring.
An ECG trace was obtained using the device, and the trace was then interpreted by a cardiologist. The traces obtained were of suitable quality to diagnose arrhythmias, with diagnoses of supraventricular or ventricular ectopy in 27.4% of patients, sinus tachycardia in 18.6%, AF in 7.1%, and supraventricular tachycardia in 5.3%, which could be managed appropriately. In the remaining 41.6%, they could be reassured that they remained in sinus rhythm.
When the AliveCor device was used to measure corrected QT (Q wave to T wave) interval in those with sinus rhythm and antiarrhythmic drugs, results suggested that it was comparable with 12-lead ECG [87]. With a sensitivity of 64% and specificity of 97%, this suggested that the device could be used to monitor those with arrhythmias. A study comparing the AliveCor device with a 14-day event monitor found that the device was equivalent to the event monitor in detecting AF and premature atrial contractions (PAC) but was slightly less effective in identifying episodes of premature ventricular contractions (PVC) [88].
The Smartphone Pediatric ElectrocARdiogram trial [89] investigated the use of the AliveCor device in pediatric patients with known paroxysmal arrhythmias. The device produced a trace, which was then reviewed by a cardiologist. Of the 240 traces recorded by 20 patients, 231 were suitable for diagnostic purposes. A total of 35 patients were initially included in the trial; 15 of these patients did not transmit ECGs. Of the suitable traces, sinus rhythm was detected in 43% of the traces. Moreover, 29% displayed sinus tachycardia, supraventricular tachycardia was present in 16%, and AF was present in 8%. Furthermore, 98% of parents of patients involved in the trial reported greater comfort in managing their child’s arrhythmia, with 93% expressing a desire to continue using the device.
A study by Mc et al [90] assessed whether the Pulse Waveform Analysis app could distinguish sinus rhythm and AF from PAC and PVC. The patient covered the camera and lamp of an iPhone 4S with their finger for 2 min, allowing a pulse waveform to be recorded and a video of blood flow to be recorded. A total of 3 statistical techniques were then used in combination—RMSSD, Poincare plot, and Shannon Entropy (ShE)—to distinguish AF from ectopic beats. Results for each of the arrhythmias were as follows: for AF, a sensitivity of 97%, specificity of 93.5%, and accuracy of 95.1%; for PAC, a sensitivity of 66.7%, specificity of 98%, and accuracy of 95.5%; and for PVC, a sensitivity of 73.3%, specificity of 97.6%, and accuracy of 96%. A similar study assessed the use of a mobile phone app identifying PVC using RR intervals, finding a sensitivity of 90.13% and specificity of 82.52% [91]. A study using similar methods found that the best results were obtained when RMSSD and ShE were combined to analyze the trace. When these 2 techniques were combined in a study of 76 participants, the results were 100% accurate for detecting AF and 96.05% accurate for detecting sinus rhythm [92]. Using simulated ECG signals from the Massachusetts Institute of Technology–Beth Israel Hospital arrhythmia database, a study tested the ability of an Android program to detect arrhythmias from ECG traces [93]. The analog ECG traces were converted to a digital format and then made available for transmission via Bluetooth. The Pan-Tompkins algorithm [94] was then used to identify RR intervals to determine the heartbeat. The algorithm produced an accuracy of 98.98% at detecting sinus rhythm and an average accuracy of 98.34% at detecting 7 different possible heart rhythms.
Discussion
Limitations
The main limitations of this narrative review are the lack of focus on more specific arrhythmias beyond normal sinus rhythm and AF. However, normal sinus rhythm and AF are epidemiologically the most common types of heart rhythm; hence, it is important to establish a strong foundation for these apps with these rhythms first. Second, it is common for narrative reviews to circumvent important criteria to mitigate bias because of the lack of a rigorous evidence-based methodology. This inevitably leads to selection bias based on expert opinions. This bias was addressed in this narrative review by adapting the Preferred Reporting Items for Systematic Reviews and Meta-Analyses criteria to select relevant publications. In doing so, all evidence pertaining to the issues discussed in this review has been considered to provide a balanced understanding and discussion.
Photoplethysmography
Despite being effective in accessing HR and HRV, the applications of PPG monitoring are limited by multiple confounders such as finger pressure, skin tone, light intensities, and user movement leading to artefactual measurements [95,96]. As such, this will have an impact on the feasibility and reliability of mobile phone–based PPG within clinical practice. A minimum sampling rate is necessary for clinically accurate measurements—30 Hz for HR and 200 Hz for HRV measurements [97,98]. However, the frame rate of mobile phones usually operates around 30 Hz, which is a major limitation identified by Bolkhovsky et al [71]. It was proposed that using cubic interpolation, the second derivative, and the zero-crossing algorithm instead of minima detection would overcome this limitation and allow for better HR detection [99-102]. A filter is required to remove artifacts without compromising the original signal when conducting a time-domain analysis to evaluate small variations occurring in normal-to-normal intervals [103]. Examples of filters are independent component analysis using accelerometer data to remove artifacts [104] or employing a fourth-order bandpass filter [99,101]. A heating problem was also noticed by Garcia-Agundez et al when testing their algorithm, which resulted in complaints about the discomfort of holding the mobile phone [102]. Furthermore, although the SCG accelerometers could be used without supporting ECG signals, HR detection was only possible if patients were motionless and supine, leading to considerable variability in data collection because of different measurement positions. There were also difficulties encountered in setting appropriate R-peak thresholds and in comparing the data with simultaneous ECG signals (the gold standard technique) [105,106]. Another area to consider is the use of PP (P wave to P wave) intervals and PRV instead of the RR interval and HRV. Although most studies use RR and HRV approaches with supporting literature that time domain, frequency domain, and Poincare plot HRV parameters computed using RR interval and PP interval methods showed no significant differences, the PP variability was found to be accurate (0.1 ms) compared with RR variability [107]. Furthermore, most studies usually compare between normal sinus rhythm and AF. However, a simple ectopic will be able to derange specificity to unacceptable levels. In this respect, more research needs to done to evaluate the impact of short-term arrhythmic abnormalities on PPG-based and single-lead ECG–based AF detection modalities.
Handheld Electrocardiograph Recorders
Handheld single-lead ECG recorders, which correspond to the standard lead I, do not cater to potential positional variability. For example, in cases where the heart is positioned more vertically, the amplitude of the QRS complexes may be reduced and comparable with the amplitude of artifacts [15]. Furthermore, a single recorded lead I ECG also does not allow for differentiation between types of narrow and wide complex QRS tachycardia [15]. Although small studies have been conducted to show that it is plausible to use a single-lead ECG to diagnose the ST-segment elevation acute coronary syndrome [108], it is not sufficient to warrant routine clinical use. In some situations, new materials and sensors (eg, biopatches) have allowed these ECGs to be recorded from atypical places (eg, mastoid area) [109] and under different environmental conditions such as after immersion in water or in areas with magnetic fields between 1.5 and 3 T (during magnetic resonance imaging) [110-113]. Novel biopatches have also allowed other parameters such as respiratory rate, body position, temperature, and quality of sleep or physical activity to be monitored, which aids in excluding ST depression caused by increased physical activity or changes in body position [19,114,115]. However, when this is coupled with fewer leads, not only will there be suboptimal signal-to-noise ratio but signals generated might also be different from those produced by standard ECG leads [15]. Furthermore, the utility of biopatches comes with a drawback of having a short intersensor distance, which could potentially compromise the quality of the P wave recorded [15].
Health Care Infrastructural Implementation
Despite being a promising concept, there are currently clear limitations to the use of mobile phone apps for HR, HRV, and AF monitoring. Looking beyond the technological drawbacks, there is little evidence as to how mobile phone monitoring will be matched with health care infrastructural changes to allow for such data to sync with the electronic medical record [116,117]. Furthermore, not all patients will have the same device or mobile phone, which may result in different recorded results. Special clinical attention also has to be given to incidental findings of ECG abnormalities such as ventricular and supraventricular tachycardia in asymptomatic low-risk patients [15]. The impact of app use on health care services is also not to be underestimated. The necessity for a health care professional to confirm arrhythmias detected by these apps will result in a significant burden on services. Given the transient nature of some arrhythmias, an app with a high specificity is likely to be more beneficial to avoid over investigation and treatment of patients, reducing the impact on existing services.
A recent large-scale community AF screening program on more than 10,000 patients aged above of 65 years was conducted, proving the feasibility of integrating this technological within-health care services to identify with new AF [118]. The main drawback illustrated by this study is the lack of downstream management pathways. This raises the medico-legal aspect of introducing mobile phone apps. First, there must be an understanding as to how these apps will support decision making or purport to intervene in clinical decisions. This, in turn, will lay the foundation for a robust government framework to evaluate its effect on clinical outcomes and potential unintended consequences [119,120]. A deeper engagement in this respect was raised in January 2016 when 2 class action lawsuits were filed against such manufacturers, calling into question the reliability and accuracy of these devices and apps [121]. Perhaps the issue is in classifying these devices and apps as certified medical devices. Despite the intuitive need for medical devices to be of high quality, local regulations for medical devices have to be followed. Such regulations range from the Medical Devices Framework concept of intended purpose to the risk-based case-by-case approach employed by the US Food and Drug Administration [122].
Looking specifically at the European regulations, the Medical Device Directive was replaced by the new Medical Device Regulation. Although the new regulatory framework still revolves around intended purpose, the bar for medical device classification has been lowered because of a broader definition assigned to the term medical purpose. In short, despite the undisputed potential of such apps in the detection of arrhythmias, adhering to appropriate laws and regulations remains a significant hurdle to address [123].
Conclusions and Future Directions
In this study, we conducted a narrative review of the literature surrounding the usage of mobile phone apps in the monitoring of HR and rhythm. The findings of this narrative review suggest that there is a role for mobile phone app in the diagnosis, monitoring, and screening of arrhythmias and HR. The usage of apps in specific situations, such as during and following exercise or to measure corrected QT interval following the administration of medications, has also shown a role for the apps in more specific scenarios. Although the majority of literature reviewed focused on adult patients, the use of PPG apps in pediatric and neonatal patient populations requires further studies.
Some problems identified with the use of these devices have included patient movement resulting in artifact and in positional variability in patient usage affecting results. This has been demonstrated in studies investigating both adult and pediatric patients [89]. There is also an issue regarding consistency and availability of mobile phones, with variation in the devices used. Within the context of HR monitoring and AF detection, given the impressive degree of sensitivity (>90%) and specificity (>90%) in most cases or apps, neither sensitivity nor specificity is more important than the other. Instead, it is important for both sensitivity and specificity to be maintained at a high level or be on par with the standard ECG, especially in patients with pacemakers or implantable cardioverter defibrillators [124]. Therefore, further studies are required to address these issues before they can be routinely implemented. As such, there are little implications for current practice at this point.
Moving forward, further large-scale validation studies looking beyond normal sinus rhythm and AF are required. For example, it is important for these apps to not mistake malignant ventricular ectopics as sinus rhythm or AF as it will be potentially harmful to patients. With regard to AF detection, multiple studies have been conducted to validate its feasibility. Perhaps it would be best to start conducting large-scale AF screening programs. Doing so will help address the following points: (1) the medico-legal aspect of implementing these apps as valid medical devices for systematic and opportunistic screening nationally, (2) the cost-effectiveness of identifying new AF patients through such a screening program, and (3) refinement of a suitable management pathway for new AF patients identified through this process. Such an initiative has the potential to reduce AF burden internationally and increase the efficiency of picking up AF in the community. Within the clinical setting, apps used by patients can prompt clinicians to perform further investigations such as a confirmatory ECG.
Acknowledgments
GT would like to thank the Croucher Foundation of Hong Kong for their support. BY would like to acknowledge the Hong Kong Research Grants Council–General Research Fund for their support (reference number 14118314). The International Research Mentorship Programme organized by the Newcastle University Cardiovascular Society supported FW and TT.
Abbreviations
- AF
atrial fibrillation
- AMS
acute mountain sickness
- BCG
ballistocardiogram
- ECG
electrocardiograph
- HR
heart rate
- HRV
heart rate variability
- MEMS
microelectromechanical sensors
- PAC
premature atrial contractions
- PCG
phonocardiogram
- PP
P wave to P wave
- PPG
photoplethysmography
- PRV
pulse rate variability
- PVC
premature ventricular contractions
- QT
Q wave to T wave
- RMSSD
Root Mean Square of Successive Difference
- RR
R wave to R wave
- SCG
seismocardiogram
- SDE
SD of beat-to-beat error measurement
- ShE
Shannon Entropy
A description outlining the search process of papers.
Footnotes
Authors' Contributions: KL, TL, MW, GT, and BY designed and conceptualized the study. FW and TT were responsible for the data collection and literature screening. KL, FW, and TT drafted the manuscript. FW, MW, AJ, and AB revised the manuscript. BY contributed to critical revision of this manuscript. All authors reviewed the manuscript and approved for publication.
Conflicts of Interest: None declared.
References
- 1.Artinian NT, Fletcher GF, Mozaffarian D, Kris-Etherton P, Van Horn L, Lichtenstein AH, Kumanyika S, Kraus WE, Fleg JL, Redeker NS, Meininger JC, Banks J, Stuart-Shor EM, Fletcher BJ, Miller TD, Hughes S, Braun LT, Kopin LA, Berra K, Hayman LL, Ewing LJ, Ades PA, Durstine JL, Houston-Miller N, Burke LE, American Heart Association Prevention Committee of the Council on Cardiovascular Nursing Interventions to promote physical activity and dietary lifestyle changes for cardiovascular risk factor reduction in adults: a scientific statement from the American Heart Association. Circulation. 2010 Jul 27;122(4):406–41. doi: 10.1161/CIR.0b013e3181e8edf1. http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=20625115 .CIR.0b013e3181e8edf1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Moerenhout T, Devisch I, Cornelis GC. E-health beyond technology: analyzing the paradigm shift that lies beneath. Med Health Care Philos. 2018 Mar;21(1):31–41. doi: 10.1007/s11019-017-9780-3.10.1007/s11019-017-9780-3 [DOI] [PubMed] [Google Scholar]
- 3.Appelboom G, LoPresti M, Reginster JY, Sander Connolly E, Dumont EP. The quantified patient: a patient participatory culture. Curr Med Res Opin. 2014 Dec;30(12):2585–7. doi: 10.1185/03007995.2014.954032. [DOI] [PubMed] [Google Scholar]
- 4.Martin SS, Feldman DI, Blumenthal RS, Jones SR, Post WS, McKibben RA, Michos ED, Ndumele CE, Ratchford EV, Coresh J, Blaha MJ. mActive: a randomized clinical trial of an automated mHealth intervention for physical activity promotion. J Am Heart Assoc. 2015 Nov 9;4(11) doi: 10.1161/JAHA.115.002239. http://jaha.ahajournals.org/cgi/pmidlookup?view=long&pmid=26553211 .JAHA.115.002239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dower GE, Yakush A, Nazzal SB, Jutzy RV, Ruiz CE. Deriving the 12-lead electrocardiogram from four (EASI) electrodes. J Electrocardiol. 1988;21 Suppl:S182–7. doi: 10.1016/0022-0736(88)90090-8. [DOI] [PubMed] [Google Scholar]
- 6.Kelli HM, Witbrodt B, Shah A. The future of mobile health applications and devices in cardiovascular health. Euro Med J Innov. 2017 Jan 10;2017:92–7. http://europepmc.org/abstract/MED/28191545 . [PMC free article] [PubMed] [Google Scholar]
- 7.Wing RR, Tate DF, Gorin AA, Raynor HA, Fava JL. A self-regulation program for maintenance of weight loss. N Engl J Med. 2006 Oct 12;355(15):1563–71. doi: 10.1056/NEJMoa061883.355/15/1563 [DOI] [PubMed] [Google Scholar]
- 8.Franz MJ, VanWormer JJ, Crain AL, Boucher JL, Histon T, Caplan W, Bowman JD, Pronk NP. Weight-loss outcomes: a systematic review and meta-analysis of weight-loss clinical trials with a minimum 1-year follow-up. J Am Diet Assoc. 2007 Oct;107(10):1755–67. doi: 10.1016/j.jada.2007.07.017.S0002-8223(07)01483-6 [DOI] [PubMed] [Google Scholar]
- 9.Burke LE, Wang J, Sevick MA. Self-monitoring in weight loss: a systematic review of the literature. J Am Diet Assoc. 2011 Jan;111(1):92–102. doi: 10.1016/j.jada.2010.10.008. http://europepmc.org/abstract/MED/21185970 .S0002-8223(10)01644-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jospe MR, Fairbairn KA, Green P, Perry TL. Diet app use by sports dietitians: a survey in five countries. JMIR Mhealth Uhealth. 2015 Jan 22;3(1):e7. doi: 10.2196/mhealth.3345. http://mhealth.jmir.org/2015/1/e7/ v3i1e7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Turner-McGrievy GM, Beets MW, Moore JB, Kaczynski AT, Barr-Anderson DJ, Tate DF. Comparison of traditional versus mobile app self-monitoring of physical activity and dietary intake among overweight adults participating in an mHealth weight loss program. J Am Med Inform Assoc. 2013 May 1;20(3):513–8. doi: 10.1136/amiajnl-2012-001510. http://jamia.oxfordjournals.org/cgi/pmidlookup?view=long&pmid=23429637 .amiajnl-2012-001510 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ghorai K, Akter S, Khatun F, Ray P. mHealth for smoking cessation programs: a systematic review. J Pers Med. 2014 Jul 18;4(3):412–23. doi: 10.3390/jpm4030412. http://www.mdpi.com/resolver?pii=jpm4030412 .jpm4030412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pecchia L, Castaldo R, Montesinos L, Melillo P. Are ultra-short heart rate variability features good surrogates of short-term ones? State-of-the-art review and recommendations. Healthc Technol Lett. 2018 Mar 14;5(3):94–100. doi: 10.1049/htl.2017.0090. http://europepmc.org/abstract/MED/29922478 .HTL.2017.0090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Allen J. Photoplethysmography and its application in clinical physiological measurement. Physiol Meas. 2007 Mar;28(3):R1–39. doi: 10.1088/0967-3334/28/3/R01.S0967-3334(07)14869-3 [DOI] [PubMed] [Google Scholar]
- 15.Guzik P, Malik M. ECG by mobile technologies. J Electrocardiol. 2016;49(6):894–901. doi: 10.1016/j.jelectrocard.2016.07.030.S0022-0736(16)30108-X [DOI] [PubMed] [Google Scholar]
- 16.Kamal AA, Harness JB, Irving G, Mearns AJ. Skin photoplethysmography--a review. Comput Methods Programs Biomed. 1989 Apr;28(4):257–69. doi: 10.1016/0169-2607(89)90159-4.0169-2607(89)90159-4 [DOI] [PubMed] [Google Scholar]
- 17.Lowres N, Neubeck L, Salkeld G, Krass I, McLachlan AJ, Redfern J, Bennett AA, Briffa T, Bauman A, Martinez C, Wallenhorst C, Lau JK, Brieger DB, Sy RW, Freedman SB. Feasibility and cost-effectiveness of stroke prevention through community screening for atrial fibrillation using iPhone ECG in pharmacies. The SEARCH-AF study. Thromb Haemost. 2014 Jun;111(6):1167–76. doi: 10.1160/TH14-03-0231.14-03-0231 [DOI] [PubMed] [Google Scholar]
- 18.Hickey KT, Hauser NR, Valente LE, Riga TC, Frulla AP, Masterson Creber R, Whang W, Garan H, Jia H, Sciacca RR, Wang DY. A single-center randomized, controlled trial investigating the efficacy of a mHealth ECG technology intervention to improve the detection of atrial fibrillation: the iHEART study protocol. BMC Cardiovasc Disord. 2016 Jul 16;16:152. doi: 10.1186/s12872-016-0327-y. https://bmccardiovascdisord.biomedcentral.com/articles/10.1186/s12872-016-0327-y .10.1186/s12872-016-0327-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shih CM, Lin CW, Clinciu DL, Jian WS, Kuo TB, Nguyen PA, Iqbal U, Hsu CK, Owili PO, Li YC. Managing mass events and competitions with difficult-to-access locations using mobile electrocardiac monitoring. Comput Methods Programs Biomed. 2015 Sep;121(2):109–15. doi: 10.1016/j.cmpb.2015.04.014.S0169-2607(15)00112-1 [DOI] [PubMed] [Google Scholar]
- 20.Le Page P, MacLachlan H, Anderson L, Penn LA, Moss A, Mitchell AR. The efficacy of a smartphone ECG application for cardiac screening in an unselected island population. Br J Cardiol. 2015;22:31–3. doi: 10.5837/bjc.2015.009. [DOI] [Google Scholar]
- 21.AliveCor. [2018-12-12]. KardiaMobile https://shop.gb.alivecor.com/products/kardiamobile .
- 22.Tu HT, Chen Z, Swift C, Churilov L, Guo R, Liu X, Jannes J, Mok V, Freedman B, Davis SM, Yan B. Smartphone electrographic monitoring for atrial fibrillation in acute ischemic stroke and transient ischemic attack. Int J Stroke. 2017 Oct;12(7):786–9. doi: 10.1177/1747493017696097. [DOI] [PubMed] [Google Scholar]
- 23.Lau JK, Lowres N, Neubeck L, Brieger DB, Sy RW, Galloway CD, Albert DE, Freedman SB. iPhone ECG application for community screening to detect silent atrial fibrillation: a novel technology to prevent stroke. Int J Cardiol. 2013 Apr 30;165(1):193–4. doi: 10.1016/j.ijcard.2013.01.220.S0167-5273(13)00280-5 [DOI] [PubMed] [Google Scholar]
- 24.Chan NY, Choy CC. Screening for atrial fibrillation in 13 122 Hong Kong citizens with smartphone electrocardiogram. Heart. 2017 Dec 1;103(1):24–31. doi: 10.1136/heartjnl-2016-309993.heartjnl-2016-309993 [DOI] [PubMed] [Google Scholar]
- 25.Chan PH, Wong CK, Pun L, Wong YF, Wong MM, Chu DW, Siu CW. Head-to-head comparison of the AliveCor heart monitor and Microlife WatchBP Office AFIB for atrial fibrillation screening in a primary care setting. Circulation. 2017 Jan 3;135(1):110–2. doi: 10.1161/CIRCULATIONAHA.116.024439. http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=28028066 .CIRCULATIONAHA.116.024439 [DOI] [PubMed] [Google Scholar]
- 26.Desteghe L, Raymaekers Z, Lutin M, Vijgen J, Dilling-Boer D, Koopman P, Schurmans J, Vanduynhoven P, Dendale P, Heidbuchel H. Performance of handheld electrocardiogram devices to detect atrial fibrillation in a cardiology and geriatric ward setting. Europace. 2017 Jan;19(1):29–39. doi: 10.1093/europace/euw025.euw025 [DOI] [PubMed] [Google Scholar]
- 27.Lowres N, Mulcahy G, Gallagher R, Ben Freedman S, Marshman D, Kirkness A, Orchard J, Neubeck L. Self-monitoring for atrial fibrillation recurrence in the discharge period post-cardiac surgery using an iPhone electrocardiogram. Eur J Cardiothorac Surg. 2016 Jul;50(1):44–51. doi: 10.1093/ejcts/ezv486.ezv486 [DOI] [PubMed] [Google Scholar]
- 28.Orchard J, Lowres N, Freedman SB, Ladak L, Lee W, Zwar N, Peiris D, Kamaladasa Y, Li J, Neubeck L. Screening for atrial fibrillation during influenza vaccinations by primary care nurses using a smartphone electrocardiograph (iECG): a feasibility study. Eur J Prev Cardiol. 2016 Oct;23(2 suppl):13–20. doi: 10.1177/2047487316670255.23/2_suppl/13 [DOI] [PubMed] [Google Scholar]
- 29.Koltowski L, Balsam P, Glowczynska R, Peller M, Maksym J, Blicharz L, Niedziela M, Maciejewski K, Opolsk G, Grabowski M. Comparison of Kardia Mobile (one lead ECGs records) with 12-lead ECGs in 100 consecutive patients with various cardiovascular disorders. EP Europace. 2017 Jun;19(3):iii353. doi: 10.1093/ehjci/eux158.263. [DOI] [Google Scholar]
- 30.Chan PH, Wong CK, Poh YC, Pun L, Leung WW, Wong YF, Wong MM, Poh MZ, Chu DW, Siu CW. Diagnostic performance of a smartphone-based photoplethysmographic application for atrial fibrillation screening in a primary care setting. J Am Heart Assoc. 2016 Jul 21;5(7) doi: 10.1161/JAHA.116.003428. http://www.ahajournals.org/doi/full/10.1161/JAHA.116.003428?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed .JAHA.116.003428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gropler MRF, Dalal AS, Van Hare GF, Silva JNA. Can smartphone wireless ECGs be used to accurately assess ECG intervals in pediatrics? A comparison of mobile health monitoring to standard 12-lead ECG. PLoS One. 2018 Sep 27;13(9):e0204403. doi: 10.1371/journal.pone.0204403. http://dx.plos.org/10.1371/journal.pone.0204403 .PONE-D-18-00822 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lowres N, Krass I, Neubeck L, Redfern J, McLachlan AJ, Bennett AA, Freedman SB. Atrial fibrillation screening in pharmacies using an iPhone ECG: a qualitative review of implementation. Int J Clin Pharm. 2015 Dec;37(6):1111–20. doi: 10.1007/s11096-015-0169-1.10.1007/s11096-015-0169-1 [DOI] [PubMed] [Google Scholar]
- 33.Orchard J, Freedman SB, Lowres N, Peiris D, Neubeck L. iPhone ECG screening by practice nurses and receptionists for atrial fibrillation in general practice: the GP-SEARCH qualitative pilot study. Aust Fam Physician. 2014 May;43(5):315–9. http://www.racgp.org.au/afp/2014/may/iphone-ecg-screening/ [PubMed] [Google Scholar]
- 34.Kropp C, Ellis J, Nekkanti R, Sears S. Monitoring patients with implantable cardioverter defibrillators using mobile phone electrocardiogram: case study. JMIR Cardio. 2018;2(1):e5. doi: 10.2196/cardio.8710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Treskes RW, Gielen W, Wermer MJ, Grauss RW, van Alem AP, Dehnavi RA, Kirchhof CJ, van der Velde ET, Maan AC, Wolterbeek R, Overbeek OM, Schalij MJ, Trines SA. Mobile phones in cryptogenic strOke patients Bringing sIngle Lead ECGs for Atrial Fibrillation detection (MOBILE-AF): study protocol for a randomised controlled trial. Trials. 2017 Aug 29;18(1):402. doi: 10.1186/s13063-017-2131-0. https://trialsjournal.biomedcentral.com/articles/10.1186/s13063-017-2131-0 .10.1186/s13063-017-2131-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gwynne K, Flaskas Y, O'Brien C, Jeffries TL, McCowen D, Finlayson H, Martin T, Neubeck L, Freedman B. Opportunistic screening to detect atrial fibrillation in Aboriginal adults in Australia. BMJ Open. 2016 Nov 15;6(11):e013576. doi: 10.1136/bmjopen-2016-013576. http://bmjopen.bmj.com/cgi/pmidlookup?view=long&pmid=27852724 .bmjopen-2016-013576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Soni A, Karna S, Patel H, Fahey N, Raithatha S, Handorf A, Bostrom J, Bashar S, Talati K, Shah R, Goldberg RJ, Thanvi S, Phatak AG, Allison JJ, Chon K, Nimbalkar SM, McManus DD. Study protocol for Smartphone Monitoring for Atrial fibrillation in Real-Time in India (SMART-India): a community-based screening and referral programme. BMJ Open. 2017 Dec 14;7(12):e017668. doi: 10.1136/bmjopen-2017-017668. http://bmjopen.bmj.com/cgi/pmidlookup?view=long&pmid=29247089 .bmjopen-2017-017668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Guhl EN, Schlusser CL, Henault LE, Bickmore TW, Kimani E, Paasche-Orlow MK, Magnani JW. Rationale and design of the Atrial Fibrillation health Literacy Information Technology Trial: (AF-LITT) Contemp Clin Trials. 2017 Nov;62:153–8. doi: 10.1016/j.cct.2017.09.005. http://europepmc.org/abstract/MED/28923492 .S1551-7144(17)30355-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Stavrakis S, Stoner JA, Kardokus J, Garabelli PJ, Po SS, Lazzara R. Intermittent vs. Continuous Anticoagulation theRapy in patiEnts with Atrial Fibrillation (iCARE-AF): a randomized pilot study. J Interv Card Electrophysiol. 2017 Jan;48(1):51–60. doi: 10.1007/s10840-016-0192-8. http://europepmc.org/abstract/MED/27696012 .10.1007/s10840-016-0192-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Özcan EE, Görenek B. Lessons from the current European Heart Rhythm Association consensus document on screening for atrial fibrillation. Anatol J Cardiol. 2018 Mar;19(3):222–4. doi: 10.14744/AnatolJCardiol.2018.37043. http://www.anatoljcardiol.com/linkout/?PMID=29521317 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Brasier N, Raichle CJ, Dörr M, Becke A, Nohturfft V, Weber S, Bulacher F, Salomon L, Noah T, Birkemeyer R, Eckstein J. Detection of atrial fibrillation with a smartphone camera: first prospective, international, two-centre, clinical validation study (DETECT AF PRO) Europace. 2018 Jul 31; doi: 10.1093/europace/euy176.5062933 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Yan BP, Lai WHS, Chan CKY, Chan SC, Chan L, Lam KM, Lau HW, Ng CM, Tai LY, Yip KW, To OTL, Freedman B, Poh YC, Poh MZ. Contact-free screening of atrial fibrillation by a smartphone using facial pulsatile photoplethysmographic signals. J Am Heart Assoc. 2018 Apr 5;7(8) doi: 10.1161/JAHA.118.008585. http://jaha.ahajournals.org/cgi/pmidlookup?view=long&pmid=29622592 .JAHA.118.008585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mortelmans C, Van Haelst R, Van Der Auwera J, Grieten L, Vandervoort P, Vaes B. Validation of a new smartphone application for the diagnosis of atrial fibrillation in primary care. EP Europace. 2017 Jun 1;19(3):iii16. doi: 10.1093/ehjci/eux136.008. [DOI] [Google Scholar]
- 44.Lahdenoja O, Hurnanen T, Iftikhar Z, Nieminen S, Knuutila T, Saraste A, Kiviniemi T, Vasankari T, Airaksinen J, Pankaala M, Koivisto T. Atrial fibrillation detection via accelerometer and gyroscope of a smartphone. IEEE J Biomed Health Inform. 2018 Jan;22(1):108–18. doi: 10.1109/JBHI.2017.2688473. [DOI] [PubMed] [Google Scholar]
- 45.Koivisto T, Lahdenoja O, Hurnanen T, Knuutila T, Vasankari T, Kiviniemi T, Saraste A, Airaksinen J, Pankaala M. Detecting atrial fibrillation via existing smartphones without any add-ons. ESC Congress; August 27-31, 2016; Rome. 2016. [Google Scholar]
- 46.Rincon F, Grassi PR, Khaled N, Atienza D, Sciuto D. Automated real-time atrial fibrillation detection on a wearable wireless sensor platform. 2012 Annual International Conference of the IEEE Engineering in Medicine and Biology Society; August 28-September 1, 2012; San Diego, CA, USA. 2012. [DOI] [PubMed] [Google Scholar]
- 47.Rudner J, McDougall C, Sailam V, Smith M, Sacchetti A. Interrogation of patient smartphone activity tracker to assist arrhythmia management. Ann Emerg Med. 2016 Sep;68(3):292–4. doi: 10.1016/j.annemergmed.2016.02.039.S0196-0644(16)00143-8 [DOI] [PubMed] [Google Scholar]
- 48.Yan BP, Lai HS, Fong AH, Lai PS, Cheng OW, Chan CK, Chan WM, To OT, Poh YC, Poh MZ. Validation of a deep convolutional network for detecting atrial fibrillation with a wrist-worn wearable device. Heart Rhythm Society's Annual Scientific Sessions; May 9-12, 2018; Boston, MA. 2018. https://static1.squarespace.com/static/58334ce08419c209d6bf1882/t/5b9abc3fcd8366c8440de450/1536867391780/HRS-Boston-2018-Cardiio.pdf . [Google Scholar]
- 49.Krivoshei L, Weber S, Burkard T, Maseli A, Brasier N, Kühne M, Conen D, Huebner T, Seeck A, Eckstein J. Smart detection of atrial fibrillation†. Europace. 2017 May 1;19(5):753–7. doi: 10.1093/europace/euw125. http://europepmc.org/abstract/MED/27371660 .euw125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Doerr M, Koenig N, Seeck A, Stoeckli R, Rhinisperger M, Djurdjevic A, Birkemeyer R, Eckstein J. Trial design of the WATCH AF trial - SmartWATCHes for detection of atrial fibrillation. EP Europace. 2017 Jun 1;19(3):iii41. doi: 10.1093/ehjci/eux141.014. [DOI] [Google Scholar]
- 51.Landreani F, Caiani EG. Smartphone accelerometers for the detection of heart rate. Expert Rev Med Devices. 2017 Nov 26;14(12):935–48. doi: 10.1080/17434440.2017.1407647. [DOI] [PubMed] [Google Scholar]
- 52.Alafeef M. Smartphone-based photoplethysmographic imaging for heart rate monitoring. J Med Eng Technol. 2017 Jul;41(5):387–95. doi: 10.1080/03091902.2017.1299233. [DOI] [PubMed] [Google Scholar]
- 53.Parpinel M, Scherling L, Lazzer S, Della Mea V. Reliability of heart rate mobile apps in young healthy adults: exploratory study and research directions. J Innov Health Inform. 2017 Jun 30;24(2):921. doi: 10.14236/jhi.v24i2.921. [DOI] [PubMed] [Google Scholar]
- 54.Koenig N, Seeck A, Eckstein J, Mainka A, Huebner T, Voss A, Weber S. Validation of a new heart rate measurement algorithm for fingertip recording of video signals with smartphones. Telemed J E Health. 2016 Aug;22(8):631–6. doi: 10.1089/tmj.2015.0212. [DOI] [PubMed] [Google Scholar]
- 55.Vandenberk T, Stans J, Mortelmans C, Van Haelst R, Van Schelvergem G, Pelckmans C, Smeets CJ, Lanssens D, De Cannière H, Storms V, Thijs IM, Vaes B, Vandervoort PM. Clinical validation of heart rate apps: mixed-methods evaluation study. JMIR Mhealth Uhealth. 2017 Aug 25;5(8):e129. doi: 10.2196/mhealth.7254. http://mhealth.jmir.org/2017/8/e129/ v5i8e129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Pipitprapat W, Harnchoowong S, Suchonwanit P, Sriphrapradang C. The validation of smartphone applications for heart rate measurement. Ann Med. 2018 Nov 17;:1–7. doi: 10.1080/07853890.2018.1531144. [DOI] [PubMed] [Google Scholar]
- 57.Chaudhry BM. Heart rate monitoring mobile applications. Mhealth. 2016 Apr 22;2:17. doi: 10.21037/mhealth.2016.04.01. doi: 10.21037/mhealth.2016.04.01.mh-02-2016.04.01 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lee ES, Lee JS, Joo MC, Kim JH, Noh SE. Accuracy of heart rate measurement using smartphones during treadmill exercise in male patients with ischemic heart disease. Ann Rehabil Med. 2017 Feb;41(1):129–37. doi: 10.5535/arm.2017.41.1.129. http://e-arm.org/journal/view.php?doi=10.5535/arm.2017.41.1.129 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Yan BP, Chan CK, Li CK, To OT, Lai WH, Tse G, Poh YC, Poh MZ. Resting and postexercise heart rate detection from fingertip and facial photoplethysmography using a smartphone camera: a validation study. JMIR Mhealth Uhealth. 2017 Mar 13;5(3):e33. doi: 10.2196/mhealth.7275. http://mhealth.jmir.org/2017/3/e33/ v5i3e33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Mitchell K, Graff M, Hedt C, Simmons J. Reliability and validity of a smartphone pulse rate application for the assessment of resting and elevated pulse rate. Physiother Theory Pract. 2016 Aug;32(6):494–9. doi: 10.1080/09593985.2016.1203046. [DOI] [PubMed] [Google Scholar]
- 61.Lee H, Chung H, Ko H, Jeong C, Noh SE, Kim C, Lee J. Dedicated cardiac rehabilitation wearable sensor and its clinical potential. PLoS One. 2017 Oct 31;12(10):e0187108. doi: 10.1371/journal.pone.0187108. http://dx.plos.org/10.1371/journal.pone.0187108 .PONE-D-17-18930 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Golzar M, Fotouhi-Ghazvini F, Rabbani H, Zakeri FS. Mobile cardiac health-care monitoring and notification with real time tachycardia and bradycardia arrhythmia detection. J Med Signals Sens. 2017;7(4):193–202. http://www.jmss.mui.ac.ir/article.asp?issn=2228-7477;year=2017;volume=7;issue=4;spage=193;epage=202;aulast=Golzar . [PMC free article] [PubMed] [Google Scholar]
- 63.Breton MD, Brown SA, Karvetski CH, Kollar L, Topchyan KA, Anderson SM, Kovatchev BP. Adding heart rate signal to a control-to-range artificial pancreas system improves the protection against hypoglycemia during exercise in type 1 diabetes. Diabetes Technol Ther. 2014 Aug;16(8):506–11. doi: 10.1089/dia.2013.0333. http://europepmc.org/abstract/MED/24702135 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kevat AC, Bullen DV, Davis PG, Kamlin CO. A systematic review of novel technology for monitoring infant and newborn heart rate. Acta Paediatr. 2017 May;106(5):710–20. doi: 10.1111/apa.13786. [DOI] [PubMed] [Google Scholar]
- 65.Ho CL, Fu YC, Lin MC, Chan SC, Hwang B, Jan SL. Smartphone applications (apps) for heart rate measurement in children: comparison with electrocardiography monitor. Pediatr Cardiol. 2014 Apr;35(4):726–31. doi: 10.1007/s00246-013-0844-8. [DOI] [PubMed] [Google Scholar]
- 66.Gregoski MJ, Vertegel A, Shaporev A, Treiber FA. Tension Tamer: delivering meditation with objective heart rate acquisition for adherence monitoring using a smart phone platform. J Altern Complement Med. 2013 Jan;19(1):17–9. doi: 10.1089/acm.2011.0772. http://europepmc.org/abstract/MED/22967280 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Soffer M, Chen K. Identification and evaluation of fetal heart rate monitoring mobile applications [33I] Obstet Gynecol. 2017;129(5):101S. doi: 10.1097/01.AOG.0000514972.96123.fb. [DOI] [Google Scholar]
- 68.Chen YH, Chen HH, Chen TC, Chen LG. Robust heart rate measurement with phonocardiogram by on-line template extraction and matching. Conf Proc IEEE Eng Med Biol Soc. 2011;2011:1957–60. doi: 10.1109/IEMBS.2011.6090552. [DOI] [PubMed] [Google Scholar]
- 69.Guzik P, Piekos C, Pierog O, Fenech N, Krauze T, Piskorski J, Wykretowicz A. Classic electrocardiogram-based and mobile technology derived approaches to heart rate variability are not equivalent. Int J Cardiol. 2018 May 1;258:154–6. doi: 10.1016/j.ijcard.2018.01.056.S0167-5273(17)35439-6 [DOI] [PubMed] [Google Scholar]
- 70.- Heart rate variability: standards of measurement, physiological interpretation and clinical use. Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Circulation. 1996 Mar 1;93(5):1043–65. http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=8598068 . [PubMed] [Google Scholar]
- 71.Bolkhovsky JB, Scully CG, Chon KH. Statistical analysis of heart rate and heart rate variability monitoring through the use of smart phone cameras. Conf Proc IEEE Eng Med Biol Soc. 2012;2012:1610–3. doi: 10.1109/EMBC.2012.6346253. [DOI] [PubMed] [Google Scholar]
- 72.Plews DJ, Scott B, Altini M, Wood M, Kilding AE, Laursen PB. Comparison of heart-rate-variability recording with smartphone photoplethysmography, Polar H7 chest strap, and electrocardiography. Int J Sports Physiol Perform. 2017 Nov 1;12(10):1324–8. doi: 10.1123/ijspp.2016-0668. [DOI] [PubMed] [Google Scholar]
- 73.Perrotta AS, Jeklin AT, Hives BA, Meanwell LE, Warburton DER. Validity of the Elite HRV smartphone application for examining heart rate variability in a field-based setting. J Strength Cond Res. 2017 Aug;31(8):2296–302. doi: 10.1519/JSC.0000000000001841. [DOI] [PubMed] [Google Scholar]
- 74.Ramos-Castro J, Moreno J, Miranda-Vidal H, García-González MA, Fernández-Chimeno M, Rodas G, Capdevila L. Heart rate variability analysis using a seismocardiogram signal. Conf Proc IEEE Eng Med Biol Soc. 2012;2012:5642–5. doi: 10.1109/EMBC.2012.6347274. [DOI] [PubMed] [Google Scholar]
- 75.Huang RY, Dung LR. Measurement of heart rate variability using off-the-shelf smart phones. Biomed Eng Online. 2016 Jan 29;15:11. doi: 10.1186/s12938-016-0127-8. https://biomedical-engineering-online.biomedcentral.com/articles/10.1186/s12938-016-0127-8 .10.1186/s12938-016-0127-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Guede-Fernandez F, Ferrer-Mileo V, Ramos-Castro J, Fernandez-Chimeno M, Garcia-Gonzalez MA. Real time heart rate variability assessment from Android smartphone camera photoplethysmography: postural and device influences. Conf Proc IEEE Eng Med Biol Soc. 2015;2015:7332–5. doi: 10.1109/EMBC.2015.7320085. [DOI] [PubMed] [Google Scholar]
- 77.Lai E, Boyd K, Albert D, Ciocca M, Chung EH. Heart rate variability in concussed athletes: a case report using the smartphone electrocardiogram. HeartRhythm Case Rep. 2017 Sep 6;3(11):523–6. doi: 10.1016/j.hrcr.2017.08.009. https://linkinghub.elsevier.com/retrieve/pii/S2214-0271(17)30159-8 .S2214-0271(17)30159-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Gall B, Parkhouse W, Goodman D. Heart rate variability of recently concussed athletes at rest and exercise. Med Sci Sports Exerc. 2004 Aug;36(8):1269–74. doi: 10.1249/01.mss.0000135787.73757.4d.00005768-200408000-00001 [DOI] [PubMed] [Google Scholar]
- 79.La Fountaine MF, Heffernan KS, Gossett JD, Bauman WA, De Meersman RE. Transient suppression of heart rate complexity in concussed athletes. Auton Neurosci. 2009 Jun 15;148(1-2):101–3. doi: 10.1016/j.autneu.2009.03.001.S1566-0702(09)00077-0 [DOI] [PubMed] [Google Scholar]
- 80.Flatt AA, Esco MR. Evaluating individual training adaptation with smartphone-derived heart rate variability in a collegiate female soccer team. J Strength Cond Res. 2016 Feb;30(2):378–85. doi: 10.1519/JSC.0000000000001095. [DOI] [PubMed] [Google Scholar]
- 81.Flatt AA, Esco MR. Smartphone-derived heart-rate variability and training load in a women's soccer team. Int J Sports Physiol Perform. 2015 Nov;10(8):994–1000. doi: 10.1123/ijspp.2014-0556.2014-0556 [DOI] [PubMed] [Google Scholar]
- 82.Mellor A, Bakker-Dyos J, OʼHara J, Woods DR, Holdsworth DA, Boos CJ. Smartphone-enabled heart rate variability and acute mountain sickness. Clin J Sport Med. 2018 Jan;28(1):76–81. doi: 10.1097/JSM.0000000000000427. [DOI] [PubMed] [Google Scholar]
- 83.Heathers JA. Smartphone-enabled pulse rate variability: an alternative methodology for the collection of heart rate variability in psychophysiological research. Int J Psychophysiol. 2013 Sep;89(3):297–304. doi: 10.1016/j.ijpsycho.2013.05.017.S0167-8760(13)00169-4 [DOI] [PubMed] [Google Scholar]
- 84.Muaremi A, Arnrich B, Tröster G. Towards measuring stress with smartphones and wearable devices during workday and sleep. Bionanoscience. 2013;3:172–83. doi: 10.1007/s12668-013-0089-2. http://europepmc.org/abstract/MED/25530929 .89 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Salahuddin L, Cho J, Jeong MG, Kim D. Ultra short term analysis of heart rate variability for monitoring mental stress in mobile settings. Conf Proc IEEE Eng Med Biol Soc. 2007;2007:4656–9. doi: 10.1109/IEMBS.2007.4353378. [DOI] [PubMed] [Google Scholar]
- 86.Dimarco AD, Onwordi E, Walters E, Mullan N, Willis L, Tanner M. Diagnostic utility of smartphone ECG technology in the initial investigation of palpitations. EP Europace. 2017 Jun 1;19(3):iii102. doi: 10.1093/ehjci/eux141.184. [DOI] [Google Scholar]
- 87.Garabelli P, Stavrakis S, Albert M, Koomson E, Parwani P, Chohan J, Smith L, Albert D, Xie R, Xie Q, Reynolds D, Po S. Comparison of QT interval readings in normal sinus rhythm between a smartphone heart monitor and a 12-lead ECG for healthy volunteers and inpatients receiving sotalol or dofetilide. J Cardiovasc Electrophysiol. 2016 Jul;27(7):827–32. doi: 10.1111/jce.12976. [DOI] [PubMed] [Google Scholar]
- 88.Narasimha D, Curtis A. Smartphone based ECG recorder versus an event monitor for the evaluation of palpitations. Heart Rhythm Society's 37th Annual Scientific Sessions; May 4-7, 2016; San Francisco. 2016. [Google Scholar]
- 89.Nguyen HH, Van Hare GF, Rudokas M, Bowman T, Silva JN. SPEAR Trial: Smartphone Pediatric ElectrocARdiogram Trial. PLoS One. 2015 Aug 21;10(8):e0136256. doi: 10.1371/journal.pone.0136256. http://dx.plos.org/10.1371/journal.pone.0136256 .PONE-D-15-26592 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.McManus DD, Chong JW, Soni A, Saczynski JS, Esa N, Napolitano C, Darling CE, Boyer E, Rosen RK, Floyd KC, Chon KH. PULSE-SMART: pulse-based arrhythmia discrimination using a novel smartphone application. J Cardiovasc Electrophysiol. 2016 Jan;27(1):51–7. doi: 10.1111/jce.12842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Cuesta P, Lado MJ, Vila XA, Alonso R. Detection of premature ventricular contractions using the RR-interval signal: a simple algorithm for mobile devices. Technol Health Care. 2014;22(4):651–6. doi: 10.3233/THC-140818.Y4R83TH3R0678K0U [DOI] [PubMed] [Google Scholar]
- 92.McManus DD, Lee J, Maitas O, Esa N, Pidikiti R, Carlucci A, Harrington J, Mick E, Chon KH. A novel application for the detection of an irregular pulse using an iPhone 4S in patients with atrial fibrillation. Heart Rhythm. 2013 Mar;10(3):315–9. doi: 10.1016/j.hrthm.2012.12.001. http://europepmc.org/abstract/MED/23220686 .S1547-5271(12)01435-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Yen TH, Chang CY, Yu SN. A portable real-time ECG recognition system based on smartphone. 2013 35th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC); July 3-7, 2013; Osaka, Japan. 2013. [DOI] [PubMed] [Google Scholar]
- 94.Pan J, Tompkins WJ. A real-time QRS detection algorithm. IEEE Trans Biomed Eng. 1985 Mar;32(3):230–6. doi: 10.1109/TBME.1985.325532. [DOI] [PubMed] [Google Scholar]
- 95.Gregoski MJ, Mueller M, Vertegel A, Shaporev A, Jackson BB, Frenzel RM, Sprehn SM, Treiber FA. Development and validation of a smartphone heart rate acquisition application for health promotion and wellness telehealth applications. Int J Telemed Appl. 2012;2012:696324. doi: 10.1155/2012/696324. doi: 10.1155/2012/696324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Hassan MA, Malik AS, Saad N, Fofi D, Meriaudeau F. Effect of motion artifact on digital camera based heart rate measurement. Conf Proc IEEE Eng Med Biol Soc. 2017 Jul;2017:2851–4. doi: 10.1109/EMBC.2017.8037451. [DOI] [PubMed] [Google Scholar]
- 97.Polimeni G, Scarpino A, Barbé K, Lamonaca F, Grimaldi D. Evaluation of the number of PPG harmonics to assess smartphone effectiveness. 2014 IEEE International Symposium on Medical Measurements and Applications (MeMeA); June 11-12, 2014; Lisboa, Portugal. 2014. [DOI] [Google Scholar]
- 98.Voss A, Wessel N, Sander A, Malberg H, Dietz R. Influence of low sampling rate on heart rate variability analysis based on non-linear dynamics. Computers in Cardiology 1995; September 10-13, 1995; Vienna, Austria. 1995. [DOI] [Google Scholar]
- 99.Altini M, Amft O. HRV4Training: large-scale longitudinal training load analysis in unconstrained free-living settings using a smartphone application. Conf Proc IEEE Eng Med Biol Soc. 2016 Aug;2016:2610–3. doi: 10.1109/EMBC.2016.7591265. [DOI] [PubMed] [Google Scholar]
- 100.Elgendi M. Proceedings of the Third International Conference on Bio-inspired Systems and Signal Processing. Setúbal, Portugal: SciTePress; 2010. Heart Rate Variability Measurement Using the Second Derivative Photoplethysmogram; pp. 82–7. [Google Scholar]
- 101.Ferrer-Mileo V, Guede-Fernandez F, Fernandez-Chimeno M, Ramos-Castro J, Garcia-Gonzalez MA. Accuracy of heart rate variability estimation by photoplethysmography using an smartphone: processing optimization and fiducial point selection. Conf Proc IEEE Eng Med Biol Soc. 2015 Aug;2015:5700–3. doi: 10.1109/EMBC.2015.7319686. [DOI] [PubMed] [Google Scholar]
- 102.Garcia-Agundez A, Dutz T, Goebel S. Adapting smartphone-based photoplethysmograpy to suboptimal scenarios. Physiol Meas. 2017 Feb;38(2):219–32. doi: 10.1088/1361-6579/aa51db. [DOI] [PubMed] [Google Scholar]
- 103.Peng F, Zhang Z, Gou X, Liu H, Wang W. Motion artifact removal from photoplethysmographic signals by combining temporally constrained independent component analysis and adaptive filter. Biomed Eng Online. 2014 Apr 24;13:50. doi: 10.1186/1475-925X-13-50. https://biomedical-engineering-online.biomedcentral.com/articles/10.1186/1475-925X-13-50 .1475-925X-13-50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Fukushima H, Kawanaka H, Bhuiyan MS, Oguri K. Estimating heart rate using wrist-type photoplethysmography and acceleration sensor while running. Conf Proc IEEE Eng Med Biol Soc. 2012;2012:2901–4. doi: 10.1109/EMBC.2012.6346570. [DOI] [PubMed] [Google Scholar]
- 105.Friedrich D, Aubert XL, Fuhr H, Brauers A. Heart rate estimation on a beat-to-beat basis via ballistocardiography - a hybrid approach. Conf Proc IEEE Eng Med Biol Soc. 2010;2010:4048–51. doi: 10.1109/IEMBS.2010.5627626. [DOI] [PubMed] [Google Scholar]
- 106.Di Rienzo M, Vaini E, Castiglioni P, Merati G, Meriggi P, Parati G, Faini A, Rizzo F. Wearable seismocardiography: towards a beat-by-beat assessment of cardiac mechanics in ambulant subjects. Auton Neurosci. 2013 Nov;178(1-2):50–9. doi: 10.1016/j.autneu.2013.04.005.S1566-0702(13)00080-5 [DOI] [PubMed] [Google Scholar]
- 107.Selvaraj N, Jaryal A, Santhosh J, Deepak KK, Anand S. Assessment of heart rate variability derived from finger-tip photoplethysmography as compared to electrocardiography. J Med Eng Technol. 2008;32(6):479–84. doi: 10.1080/03091900701781317.795354184 [DOI] [PubMed] [Google Scholar]
- 108.Muhlestein JB, Le V, Albert D, Moreno FL, Anderson JL, Yanowitz F, Vranian RB, Barsness GW, Bethea CF, Severance HW, Ramo B, Pierce J, Barbagelata A, Muhlestein JB. Smartphone ECG for evaluation of STEMI: results of the ST LEUIS Pilot Study. J Electrocardiol. 2015;48(2):249–59. doi: 10.1016/j.jelectrocard.2014.11.005.S0022-0736(14)00444-0 [DOI] [PubMed] [Google Scholar]
- 109.Da He D, Winokur ES, Sodini CG. A continuous, wearable, and wireless heart monitor using head ballistocardiogram (BCG) and head electrocardiogram (ECG) Conf Proc IEEE Eng Med Biol Soc. 2011;2011:4729–32. doi: 10.1109/IEMBS.2011.6091171. [DOI] [PubMed] [Google Scholar]
- 110.Batchelor JC, Yeates SG, Casson AJ. Conformal electronics for longitudinal bio-sensing in at-home assistive and rehabilitative devices. Conf Proc IEEE Eng Med Biol Soc. 2016 Aug;2016:3159–62. doi: 10.1109/EMBC.2016.7591399. [DOI] [PubMed] [Google Scholar]
- 111.Kim DH, Lu N, Ma R, Kim YS, Kim RH, Wang S, Wu J, Won SM, Tao H, Islam A, Yu KJ, Kim TI, Chowdhury R, Ying M, Xu L, Li M, Chung HJ, Keum H, McCormick M, Liu P, Zhang YW, Omenetto FG, Huang Y, Coleman T, Rogers JA. Epidermal electronics. Science. 2011 Aug 12;333(6044):838–43. doi: 10.1126/science.1206157. http://www.sciencemag.org/cgi/pmidlookup?view=long&pmid=21836009 .333/6044/838 [DOI] [PubMed] [Google Scholar]
- 112.Reyes BA, Posada-Quintero HF, Bales JR, Clement AL, Pins GD, Swiston A, Riistama J, Florian JP, Shykoff B, Qin M, Chon KH. Novel electrodes for underwater ECG monitoring. IEEE Trans Biomed Eng. 2014 Jun;61(6):1863–76. doi: 10.1109/TBME.2014.2309293. [DOI] [PubMed] [Google Scholar]
- 113.Lobodzinski SS, Laks MM. New devices for very long-term ECG monitoring. Cardiol J. 2012;19(2):210–4. doi: 10.5603/cj.2012.0039. http://www.cardiologyjournal.org/en/darmowy_pdf.phtml?id=108&indeks_art=1571 . [DOI] [PubMed] [Google Scholar]
- 114.Engel JM, Chakravarthy BL, Rothwell D, Chavan A. SEEQ™ MCT wearable sensor performance correlated to skin irritation and temperature. Conf Proc IEEE Eng Med Biol Soc. 2015;2015:2030–3. doi: 10.1109/EMBC.2015.7318785. [DOI] [PubMed] [Google Scholar]
- 115.Jovanov E. Preliminary analysis of the use of smartwatches for longitudinal health monitoring. Conf Proc IEEE Eng Med Biol Soc. 2015 Aug;2015:865–8. doi: 10.1109/EMBC.2015.7318499. [DOI] [PubMed] [Google Scholar]
- 116.Goodloe JM, Arthur A, Rhodes T, Holder P, Winham J, Thomas S. Emergency medical technician-basic acquisition and transmission of 12-lead ECG using a novel device (Readylink™) J Am Coll Cardiol. 2013 Mar;61(10) doi: 10.1016/S0735-1097(13)60113-8. [DOI] [Google Scholar]
- 117.de Ruvo E, Sciarra L, Martino AM, Rebecchi M, Iulianella RV, Sebastiani F, Fagagnini A, Borrelli A, Scarà A, Grieco D, Tota C, Stirpe F, Calò L. A prospective comparison of remote monitoring systems in implantable cardiac defibrillators: potential effects of frequency of transmissions. J Interv Card Electrophysiol. 2016 Jan;45(1):81–90. doi: 10.1007/s10840-015-0067-4.10.1007/s10840-015-0067-4 [DOI] [PubMed] [Google Scholar]
- 118.Chan NY, Choy CC, Chan CK, Siu CW. Effectiveness of a nongovernmental organization-led large-scale community atrial fibrillation screening program using the smartphone electrocardiogram: an observational cohort study. Heart Rhythm. 2018 Sep;15(9):1306–11. doi: 10.1016/j.hrthm.2018.06.006.S1547-5271(18)30570-8 [DOI] [PubMed] [Google Scholar]
- 119.Charani E, Castro-Sánchez E, Moore LS, Holmes A. Do smartphone applications in healthcare require a governance and legal framework? It depends on the application! BMC Med. 2014 Feb 14;12:29. doi: 10.1186/1741-7015-12-29. http://www.biomedcentral.com/1741-7015/12/29 .1741-7015-12-29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Nicolas PT, Lindsay FW. Liability for mobile health and wearable technologies. Ann Health Law. 2016;25:62. https://papers.ssrn.com/sol3/papers.cfm?abstract_id=2725450 . [Google Scholar]
- 121.Lang M. Beyond Fitbit: a critical appraisal of optical heart rate monitoring wearables and apps, their current limitations and legal implications. ALB L J Sci & Tech. 2017:39. https://digitalcommons.chapman.edu/law_articles/226/ [Google Scholar]
- 122.Quinn P. The EU commission's risky choice for a non-risk based strategy on assessment of medical devices. CLSR. 2017;33(3):361–70. doi: 10.1016/j.clsr.2017.03.019. doi: 10.1016/j.clsr.2017.03.019. [DOI] [Google Scholar]
- 123.Lang M. Heart rate monitoring apps: information for engineers and researchers about the new European Medical Devices Regulation 2017/745. JMIR Biomed Eng. 2017 Aug 18;2(1):e2. doi: 10.2196/biomedeng.8179. [DOI] [Google Scholar]
- 124.White RD, Flaker G. Smartphone-based arrhythmia detection: should we encourage patients to use the ECG in their pocket? J Atr Fibrillation. 2017 Apr 30;9(6):1605. doi: 10.4022/jafib.1605. http://europepmc.org/abstract/MED/29250298 . [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
A description outlining the search process of papers.


