Abstract
Background
Activating mutations of the receptor tyrosine kinase KIT are early events in the development of most gastrointestinal stromal tumors (GISTs). Although GISTs generally remain dependent on oncogenic KIT during tumor progression, KIT mutations alone are insufficient to induce malignant behavior. This is evidenced by KIT-mutant micro-GISTs, which are present in up to one-third of normal individuals, but virtually never progress to malignancy.
Methods
We performed whole exome sequencing on 29 tumors obtained from 21 patients with high grade or metastatic KIT-mutant GIST (discovery set). We further validated the frequency and potential prognostic significance of aberrations in CDKN2A/B, RB1, and TP53 in an independent series of 71 patients with primary GIST (validation set).
Results
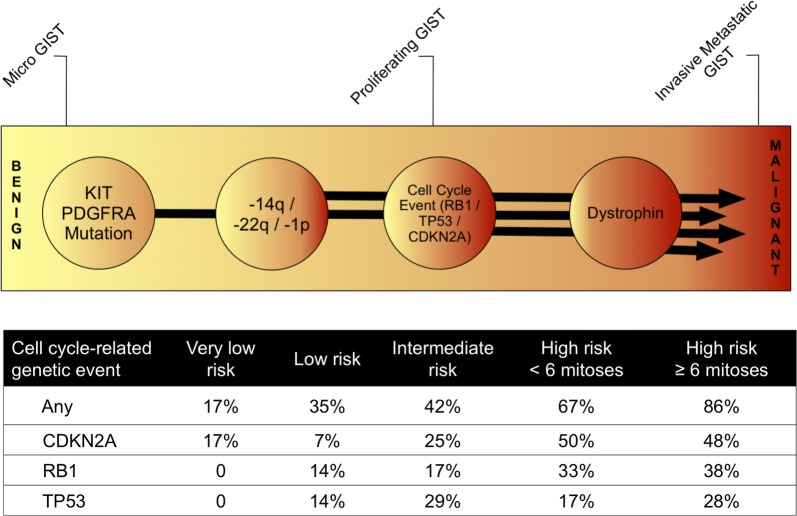
Using whole exome sequencing we found significant enrichment of genomic aberrations in cell cycle-associated genes (Fisher’s Exact p = 0.001), most commonly affecting CDKN2A/B, RB1, and TP53 in our discovery set. We found a low mutational tumor burden in these 29 advanced GIST samples, a finding with significant implications for the development of immunotherapy for GIST. In addition, we found mutation of spliceosome genes in a minority of cases, implicating dysregulation of splicing as a potential cancer promoting mechanism in GIST. We next assessed the prognostic significance of CDKN2A, RB1 or TP53 mutation/copy loss in an independent cohort of 71 patients with primary GIST. Genetic events (mutation, deletion, and/or LOH) involving at least one of the three genes examined were found in 17% of the very low-risk, 36% of the low-risk, 42% of the intermediate risk, 67% of the high-risk/low mitotic-count, and in 86% of the high-risk/high mitotic-count group. The presence of cell cycle-related events was associated with a significantly shorter relapse-free survival (median 67 months versus not reached; p < 0.0001) and overall survival (Log Rank, p = 0.042).
Conclusion
Our results demonstrate that genomic events targeting cell cycle-related genes are associated with GIST progression to malignant disease. Based on this data, we propose a model for molecular pathogenesis of malignant GIST.
Electronic supplementary material
The online version of this article (10.1186/s13569-019-0112-7) contains supplementary material, which is available to authorized users.
Keywords: GI stromal tumor, Sarcoma, Cell cycle, KIT, TP53, RB1, CDKN2A, Spliceosome
Introduction
Gastrointestinal stromal tumors (GISTs) are the most common mesenchymal tumors of the gastrointestinal tract. The vast majority of these tumors have activating mutations of the KIT or PDGFRA receptor tyrosine kinases that are considered to be initiating oncogenic events [1, 2]. GISTs lacking KIT or PDGFRA mutations comprise 10–15% of the cases. Alternative oncogenic events in these tumors include activating mutations of BRAF or KRAS or inactivating mutations of NF1 or genes encoding the succinate dehydrogenase (SDH) complex [3–5]. The oncogenic reliance of GISTs upon mutated KIT/PDGFRA is emphasized by their sensitivity to imatinib mesylate (IM), a tyrosine kinase inhibitor (TKI) that targets both KIT and PDGFRA kinase activity, leading to substantial tumor shrinkage with durable responses in most patients [6, 7].
However, IM is not a cure for GIST. Most patients will eventually experience tumor progression despite continuous IM treatment [8, 9]. Resistance to IM often arises due to secondary mutations within KIT or PDGFRA. Such mutations are commonly found in tumors removed from patients with clinical IM resistance. Additional kinase inhibitors target these secondary mutations and are used as second-line or later treatment for IM-resistant GISTs [10, 11]. Nevertheless, the progression-free survival with these salvage tyrosine kinase inhibitors is limited, and most patients experience progression from these agents within 6–12 months [6, 12].
Numerous studies have reported small incidental GISTs, less than a centimeter in diameter, that are identified during gastrectomy or at autopsy [13–16]. Many of these lesions harbor KIT mutations identical to those identified in larger malignant lesions, indicating that additional genetic events are necessary to transform these micro-GISTs into malignant tumors. Detection of genomic events associated with the development of malignant GISTs could therefore identify patients at high risk of recurrence after curative-intent resection of a primary tumor. Here we report that genomic alterations in key cell cycle regulators are recurrent abnormalities in patients with advanced GIST.
Methods
Patients and tumor tissues
De-identified samples analyzed by whole exome sequencing (WES) were obtained from participating institutions (Oregon Health and Science University, University of Duisburg-Essen, Brigham and Women`s Hospital and Katholieke Universiteit Leuven and University Hospitals Leuven). This study was approved by the institutional review boards at each of the participating sites. For whole exome sequencing approach, we selected 21 patients with high-risk GISTs, including 20 patients who presented with or eventually developed metastatic disease (discovery set). All tumor samples were obtained from frozen tissues except for one (19A), which was obtained from formalin-fixed paraffin embedded (FFPE) tissue. Paired normal DNA was extracted from frozen normal tissue (32%, 7/22), blood (63%, 14/22), or FFPE tissue (5%, 1/22).
Targeted sequence analysis was performed on a second group of 71 GIST samples representing an independent cohort of clinically characterized patients from prospectively maintained databases of participating institutions (University of Duisburg-Essen, Brigham and Women`s Hospital, and Oregon Health and Science University) and from the Life Raft Group patient database (validation data set) [17]. This cohort study was approved by the institutional review boards at each of the participating sites.
Progression-free survival (PFS) was calculated as the length of time from diagnosis of localized disease to the date of documented recurrence or death from any cause, whichever occurred first. Overall survival (OS) was defined as the length of time from the time of diagnosis of localized disease to death from any cause. PFS and OS estimates and standard errors determined using the Kaplan–Meier method and statistical comparisons were performed using the log-rank test. Two-sided p values less than 0.05 were considered to be statistically significant. The statistical analyses were performed using SPSS 19.0 and R 2.15.2 (http://www.r-project.org/). We conducted a multivariate analysis for PFS using three covariates (mitotic count, size and cell-cycle-related genomic events) using SAS software 9.4 (SAS Institute Inc., Cary, NC, USA).
Whole exome sequencing
The experimental and computational details of these experiments are included in additional methods.
Ion torrent targeted-exome genomic sequencing
In an independent validation cohort of 71 patients, targeted sequence analysis was performed with a custom AmpliSeq panel (Life Technologies, Grand Island, NY) that includes 24 genes (AKT1, AKT2, AKT3, ATM, BRAF, CDKN2A, HRAS, KIT, KRAS, MAP2K1, NF1, NRAS, PDGFRA, PIK3CA, PTEN, PTPN11, RB1, SDHA, SDHAF1, SDHAF2, SDHB, SDHC, SDHD, TP53). Sequencing was carried out on an Ion Torrent PGM instrument (Thermo Fisher Scientific, Inc., Waltham, MA), and Torrent Suite Software v3.2 was used for sequence alignment and variant calling.
Interphase FISH on tumor sections
To detect deletions affecting the CDKN2A/B/9p21.3, RB1/13q14 and TP53/17p13 genes, cut sections (4 µm thick) from paraffin-embedded tumor tissues from 42 patients were subjected to separate interphase FISH assays. FISH assays were performed using the commercially available dual-color probes LSI CDKN2A/B (9p21)-Spectrum Orange (SO)/CEP9-Spectrum Green (SG), LSI RB1-SO/CEPX-SG and LSI TP53-SO/CEP17-SG cocktails (all from Abbott Laboratories, Des Plaines, IL). Probe hybridization and detection were carried out according to standard methods. Slides were analyzed blinded from the clinical data, using a Zeiss microscope (Axioplan 2, Jena, Germany) equipped with the appropriate filters. The numbers of differentially labeled hybridization signals representing the investigated gene and reference centromere chromosomal regions were individually recorded for 100 non-overlapping interphase nuclei in at least two different areas of the section. Zero to 1 green centromeric (green) signals per nucleus in > 60% of cells were defined as a whole chromosome loss. In addition, the ratio of red to green signals was calculated. Heterozygous or homozygous losses were delineated by ratios < 0.6 and < 0.3, respectively.
Multiplex ligation-dependent probe amplification (MLPA)
Gene dosage ratios for 12 CDKN2A/CDKN2B loci and 11 other chromosome 9p genes were determined using the 9p21 MLPA kit (ME024-B1 MRC-Holland, Amsterdam, Netherlands). The probe-mix contains 21 different probes for the CDKN2A/B genes. In addition, it contains 2 probes each for MTAP, CDKN2B-AS1, PAX5 and MIR31, and 4 probes between the MIR31 gene and the 9p telomere. Two digestion control probes and 12 reference probes were included for data analysis. In each set of experiments, one negative control sample (no DNA) and 6 normal control samples (DNA isolated from paraffin sections of normal human intestines from different individuals) were included. Briefly, 50 ng of extracted tumor DNA was denatured and target gene probes were hybridized to the target DNA prior to probe ligation in the presence of Ligase-65 (MRC-Holland). The ligation products were subjected to polymerase chain reaction (PCR) amplification performed on a GeneAmp PCR System 9700 Thermal Cycler (Applied Biosystems, Warrington, UK) with a hot-start PCR program. MLPA fragments were visualized on an ABI 3130XL Automated DNA Sequencer (Applied Biosystems). Peak detection analysis has been automated using ABI PRISM Genescan® Analysis software version 3.1 (Applied Biosystems) and GeneMarker software (Softgenetics, State College, PA, USA).
CDKN2A copy number variation assessment using SNP arrays
CDKN2A homozygous deletions were identified by Affymetrix 250 K Nsp1 SNP arrays (Thermo Fisher Scientific). High-molecular-weight genomic DNA was isolated using the QIAamp DNA Mini kit (Qiagen). DNA was digested with Nsp1, and linkers were ligated to the restriction fragments to permit PCR amplification. PCR products were purified and fragmented by treatment with DNase I, and fragments were then labeled and hybridized to microarray chips. The positions and intensities of fluorescence emissions were analyzed using Chip software. Array intensity values were normalized to the value for the array with median intensity.
Results
Clinical characteristics of GIST patients analyzed by whole exome sequencing (discovery set)
We analyzed 29 high-risk GIST lesions paired with normal tissue obtained from 21 patients (Discovery Set, Table 1). Twenty of these patients presented with, or developed, metastatic disease, and thirteen of these patients had one to ten metastatic lesions that were surgically removed after clinical resistance to one or more tyrosine kinase inhibitors (median of one lesion). Seventeen of the 21 patients had tumor samples collected after one or more lines of TKI therapy. Secondary KIT mutations were identified in 18 of the 25 tumors harvested after TKI therapy (72%). In the other seven tumors, only a primary KIT gain-of-function mutation was identified. As expected, only a primary KIT mutation was found in samples from the four patients whose tumors were collected prior to TKI therapy.
Table 1.
Clinicopathological features of the discovery set (21 patients, 29 samples)
| ID | Genotype | Gender | Age at Diagnosis | Site of Primary Tumor | Sample type | Metastatic disease | Therapies prior to sample harvest | |
|---|---|---|---|---|---|---|---|---|
| 1 | 1A | KIT exon 9 insertion AY502–503; exon 13 N655S; exon 17 N822 K | Male | 45 | Small intestine | Metastasis | Y | IM, SU |
| 1B | KIT exon 9 insertion AY502–503; exon 17 N822K | Male | 45 | Small intestine | Metastasis | Y | IM, SU | |
| 1C | KIT exon 9 insertion AY502–503, exon 13 N655S; exon 17 N822K | Male | 45 | Small intestine | Metastasis | Y | IM, SU | |
| 2 | 2A | KIT exon 9 insertion AY502–503; exon 17 D816H | Male | 56 | Small intestine | Metastasis | Y | IM, SU |
| 2B | KIT exon 9 insertion AY502–503; exon 17 D820E | Male | 56 | Small intestine | Metastasis | Y | IM, SU | |
| 3 | 3A | KIT exon 11 deletion W557-V559 | Male | 60 | Small intestine | Metastasis | Y | IM |
| 4 | 4A | KIT exon 11 deletion VQWKV 555–559; exon 13 V654A | Male | 50 | Stomach | Metastasis | Y | IM |
| 5 | 5A | KIT exon 9 insertion AY502–503; exon 17 Y823D | Female | 33 | Small intestine | Metastasis | Y | IM, SU, NI, SO, IM + LBH, DA |
| 5B | KIT exon 9 insertion AY502–503; exon 17 D820E; exon 18 S840 N | Female | 33 | Small intestine | Metastasis | Y | IM, SU, NI, SO, IM + LBH, SO + RAP, DA, DOX + GEM, PA | |
| 6 | 6A | KIT exon 11 deletion D579 | Male | 65 | Small intestine | Metastasis | Y | IM |
| 7 | 7A | KIT exon 11 deletion W557-K558 | Female | 39 | Small intestine | Metastasis | Y | IM |
| 8 | 8A | KIT exon 11 V559D | Male | 65 | Rectum | Primary tumor | Y | IM |
| 9 | 9A | KIT exon 11 deletion K550-K558; KIT exon 17 D820G | Male | 65 | Stomach | Primary tumor | Y | IM |
| 10 | 10A | KIT exon 11 deletion K550–558 (starts intron 10); exon 17 D820Y | Female | 43 | Small intestine | Metastasis | Y | IM, SU, RE |
| 10B | KIT exon 11 deletion K550–558 (starts intron 10); exon 17 D820Y | Female | 43 | Small intestine | Metastasis | Y | IM, SU, RE | |
| 11 | 11A | KIT exon 11 deletion E554-D572; exon 13 V654A | Male | 45 | Small intestine | Metastasis | Y | IM |
| 12 | 12A | KIT exon 11 deletion N567-L576 | Male | 56 | Small intestine | Metastasis | Y | IM |
| 13 | 13A | KIT exon 9 S476I | Male | 40 | Small intestine | Metastasis | Y | IM, SU |
| 14 | 14A | KIT exon 11 deletion G554-V559; Exon 17 N822 K | Male | 28 | Small intestine | Metastasis | Y | IM, SU, NI, SO, DA |
| 14B | KIT exon 11 deletion G554-V559; Exon 17 N822 K | Male | 28 | Small intestine | Metastasis | Y | IM, SU, NI, SO, DA | |
| 14C | KIT exon 11 deletion G554-V559; Exon 17 N822 K | Male | 28 | Small intestine | Metastasis | Y | IM | |
| 15 | 15A | KIT exon 11 deletion Y553-K558; exon 17 N822 K | Male | 42 | Stomach | Metastasis | Y | IM |
| 16 | 16A | KIT exon 11 deletion W557-K558; exon 17 D816G | Male | 45 | Small intestine | Metastasis | Y | IM |
| 16B | KIT exon 11 deletion W557-K558; exon 17 Y823D | Male | 45 | Small intestine | Metastasis | Y | IM | |
| 17 | 17A | KIT exon 11 deletion 551_554PMYE > Q | Male | 65 | Small intestine | Primary tumor | Y | None |
| 18 | 18A | KIT exon 9 insertion AY502–503 | Female | 41 | Small intestine | Primary tumor | Y | None |
| 19 | 19A | KIT exon 11 V559D | Female | 65 | Stomach | Metastasis | Y | None |
| 20 | 20A | KIT exon 13 K642E | Female | 62 | Small intestine | Primary tumor | N | None |
| 21 | 21A | KIT exon 11 deletion W557-K558 | Male | 74 | Stomach | Metastasis | Y | IM |
DA dasatinib, DOX doxorubicin, GEM gemcitabine, IM imatinib, LBH LBH-589, panbinostat, NI nilotinib, PA pazopanib, RAP rapamycin, RE regorafenib, SU sunitinib, SO sorafenib, Y/N (yes/no)
Whole exome sequencing
The average whole exome sequencing read depth for each tumor sample was 88X (75X median) (Additional file 1: Figure S1). Only 4 of the 21 patients had samples with coverage less than 50×, with a 40–49× average (41–48× median) coverage over the targeted panel. Given the high purity of GIST samples (80–90% tumor cells), coverage was deemed adequate for identifying somatic variants of interest and only mutations with a read depth of at least 20 reads were included in our analysis. Across the entire cohort of GIST specimens, we identified a total of 4303 exonic or splice-site, non-synonymous somatic mutations including 1278 missense, 123 nonsense, 82 splice site, and 4 read-through mutations. In addition, we identified 157 deletion and 35 insertion mutations (Additional file 1: Table S1) [18].
It is well established that detection of larger insertion/deletion mutations (“indels”) by next-generation sequencing is challenging. Therefore, we used Sanger sequencing to identify or verify primary KIT insertion/deletion mutations, especially for KIT exon 9 and 11 mutations. Known primary insertion/deletion mutations not called by our indel detector were verified by visual inspection of whole exome sequencing reads.
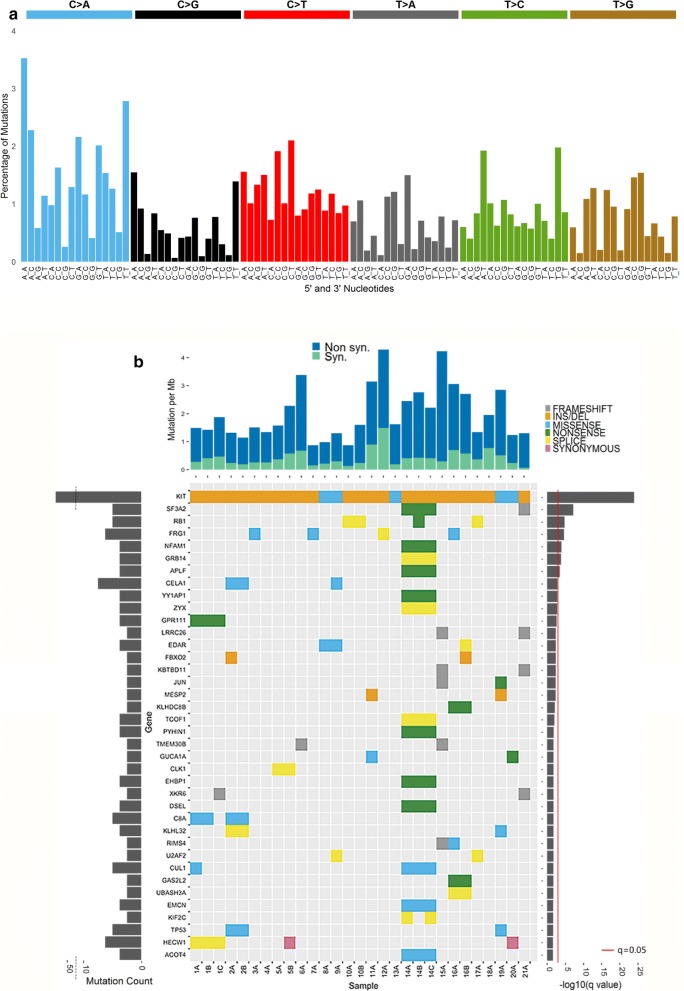
GIST mutational signature
An average of 122 somatic mutations were identified in the 29 KIT-mutant GIST samples (Additional file 1: Table S1). Genetic significance was determined based on the frequency of somatic variants with MutSigCV 1.4, which accounts for heterogeneity in mutational rate across the genome [19]. The mutation pattern of KIT-mutant GISTs consists largely of CpG transversions to A/T mutations, occurring at a relative rate of approximately 3.3 mutations per megabase (Mb) (Additional file 1: Table S2) [20]. The mutation signature was assessed by incorporating the sequence context of bases immediately 5′ and 3′ to the mutated base [21]. Percentages of mutations were normalized using the trinucleotide frequency in the human exome to the genome, leading to a decrease of C > T mutations occurring in NpCpG trinucleotides from 3 to 4% to 2% (Fig. 1a). The normalized signature show similarities to several COSMIC Signatures of Mutational Processes in Human Cancer, including Signature 5 (transcriptional strand bias for T > C substitutions at ApTpN context) and Signature 18 (neuroblastoma, breast and stomach carcinoma) [22]. The high frequencies of transition mutations at CpG in GIST are consistent with results of mutation rates of other gastrointestinal malignancies, including colorectal carcinoma, as previously reported [19]. Overall, the tumor mutation burden in these tumors was low (Additional file 1: Table S2), a finding with implications for the development of immunotherapy for GIST [23]. Ranked by q-value (lowest q-value first), the ten most commonly mutated genes in our collection of KIT-mutant GIST were KIT, SF3A2, RB1, FRG1, NFAM1, GRB14, APLF, CELA1, YY1AP1, and ZYX (Fig. 1b).
Fig. 1.
Mutational signature of 29 KIT-mutant GIST. a Average sequence context of somatic coding mutations for 40 GIST samples from WES. Signature displayed is according to the 96-substitution classification defined by the flanking 5′ and 3′ sequence adjacent to the mutated base. The mutation types are on the horizontal axis, vertical axis is the percentage of mutations attributed to each mutation type. Mutation signatures were normalized to the trinucleotide frequency of whole human genome. b Significantly mutated genes with q-value < 0.2 (corresponding p-value 0.0003) in KIT mutant GISTs. Main panel, variant type of significantly mutated genes found in each sample of our cohort of samples. Left panel represents the number of mutations of each gene. Right panel indicates the negative log10 of the q-value. Top panel represents the mutations per megabase (Mb) of the total coverage for each sample
Somatic copy number alterations
Various recurrent cytogenetic events have been described in GIST including deletions of chromosomes 14q, 22q, 15q, 1p, 9p and gains of chromosome 8q [24–28]. Large copy number events affecting more than 20% of a chromosomal arm were computationally identified using sequencing data (Table 2, Additional file 1: Table S3). Consistent with the above-cited literature, 23 out of 29 samples (16/21 patients) exhibited heterozygous loss of the long arm of chromosome 22q, and 24 of 29 samples (17/21 patients) had heterozygous copy number loss of the long arm of chromosome 14q (encompassing RBM25, HSP90AA1, and MAX).
Table 2.
Regions of large-scale, chromosomal copy number variation in 29 KIT-mutant GIST (discovery set)
| Genomic location | Event | Number of patients 21 total patients |
Number of samples with CNV 29 total samples |
Number of Genes with somatic SNV within CNV | Mean fraction of chromosomal arm | Fraction GIST samples with CNV | SNV mutated Genes from Cell Cycle (and others) pathways found in regions of large scale CNV. Bolded gene names indicated genes mutated in more than one sample |
|---|---|---|---|---|---|---|---|
| 14q | LOSS | 16 | 25 | 24 | 0.929948779 | 0.862068966 | ACOT4, ADAM20, BCL11B, COCH, DTD2, DYNC1H1, FLVCR2, HSP90AA1, KCNH5, LTBP2, MYH7, NGB, OR4M1, OR4N2, PSMB11, RBM25, SERPINA1, SERPINA9, TMEM30B |
| 1p | LOSS | 16 | 25 | 43 | 0.838940558 | 0.862068966 | ABCA4, ALDH4A1, B4GALT2, C8A, CCDC24, CD2, CDCP2, CROCC, CSDE1, CYP2J2, ELTD1, FBXO2, GADD45A, GJB5, GPR153, GRIK3, HSPG2, IGSF3, JUN, KIF2C, NBPF1, PALMD, RAP1GAP, RBMXL1, RERE, SF3A3, SRRM1, SZT2, TNFRSF8, TRIM45, TTC39A, WRAP73, ZMYM4, ZNF326 |
| 22q | LOSS | 17 | 23 | 17 | 0.878011687 | 0.793103448 | BCR, CHADL, GTPBP1, HDAC10, LZTR1, MLC1, NFAM1, NUP50, PEX26, RBFOX2, SOX10, TTC28 |
| 15q | LOSS | 13 | 21 | 29 | 0.940300484 | 0.724137931 | ANKRD34C, CHRNA5, CSPG4, FAM169B, IGF1R, IQGAP1, MAN2A2, MAP1A, MESP2, MGA, MORF4L1, MYO5C, NEO1, RFX7, RMDN3, RNF111, RYR3, SKOR1, SPINT1, SPTBN5, STARD5, TBC1D2B, TCF12, TJP1, TP53BP1, USP3 |
| 13q | LOSS | 12 | 20 | 13 | 0.888207393 | 0.689655172 | DACH1, LACC1, MYCBP2, PARP4, RB1, SHISA2, TPP2, ZC3H13 |
| 5p | GAIN | 10 | 14 | 10 | 0.928171594 | 0.482758621 | ADAMTS16, CDH10, CDH6, DAB2, OXCT1, PLEKHG4B, PRDM9 |
| 5q | GAIN | 9 | 9 | 25 | 0.924167057 | 0.310344828 | ACSL6, AGGF1, ARSI, CCNB1, CLINT1, DDX46, EBF1, FAM71B, FAT2, GNB2L1, MSH3, NDUFAF2, PCDHA1, PCDHB16, PCDHB7, PCDHGB6, PCSK1, RASGRF2, RBM27, TCOF1, TMCO6 |
| 7q | GAIN | 6 | 8 | 17 | 0.74250744 | 0.275862069 | CCDC136, CEP41, CUL1, FKBP6, MET, NOM1, OPN1SW, PCLO, PON1, TMEM168, TMEM176A, TRPV5, ZNF425, ZNF727 |
| 8q | GAIN | 7 | 8 | 11 | 0.818582114 | 0.275862069 | AGO2, COL14A1, EPPK1, NCOA2, PLEC, TNFRSF11B, TRPA1, ZFPM2 |
Additional heterozygous large chromosomal copy number losses were detected for a large region of chromosome 1p (encompassing SF3A3, RBMXL1, and MAD2L2) in 25/29 tumors (18/21 patients), chromosome 15q in 21/29 tumors (13/21 patients), and chromosome 13q (including RB1) in 20/29 tumors (11/21 patients), respectively. These results are consistent with prior studies [29–31].
KIT-mutant GISTs had heterozygous copy number gains affecting more than 20% of chromosomes arms 5p (14/29 tumors, 10/21 patients), 8q (10/29 tumors, 7/21 patients), and 7q (8/29 tumors, 6/21 patients) [31]. Heterozygous copy number gains affecting chromosome 5q (including CCNB1, DDX46) were observed in 8/29 GIST samples (6/21 patients; Table 2).
Enrichment for Somatic Mutation of Cell Cycle Pathway-Related Genes in GISTs
Pathway analysis using the list of genes associated with exonic/splice site, non-silent somatic mutations in the KIT-mutant GISTs was performed using KEGGREST v1.8.1. This analysis not only showed significant enrichment in cancer-related pathways and other KIT-associated pathways, but also enrichment for the KEGG cell cycle pathway (hsa04110; Fisher’s Exact p = 0.001, Additional file 2: Table S4) [32]. In addition, gene set enrichment analysis (GSEA) of somatic mutations using MutSigCV against a gene enrichment database, Molecular Signatures Database (MsigDB) v5.1, showed enrichment of genes associated with the cell cycle pathway (Reactome, M543, p = 0.011, Additional file 3: Table S5).
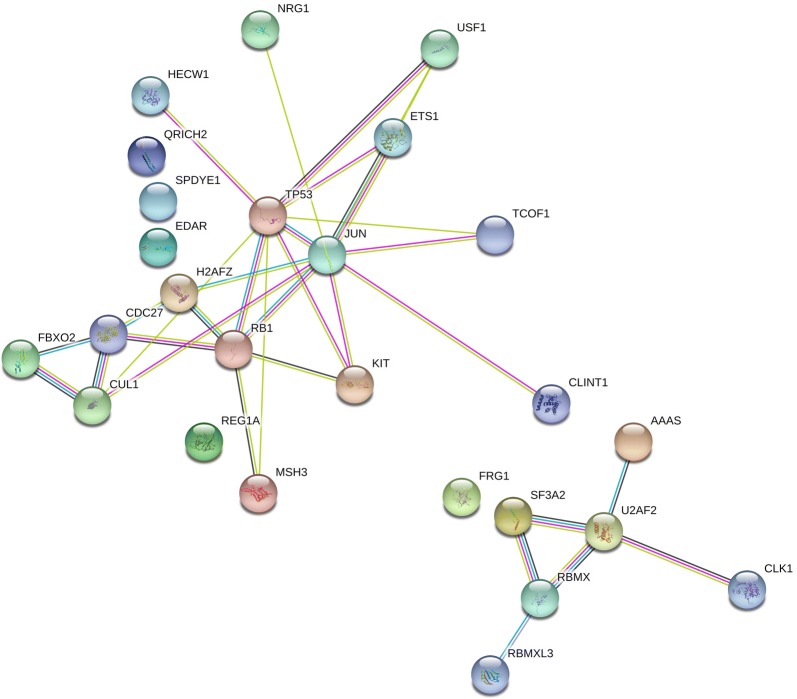
A total of ten KEGG cell cycle-associated genes were found to be significantly mutated by MutSigCV (nominal p < 0.05) in the entire cohort of GIST patients (Additional file 4: Tables S6, Additional file 5: Tables S7) [19]. These mutated cell cycle-related genes had 14 unique somatic exonic or splice site-related non-synonymous point mutation events that were filtered by variant allelic fraction greater than 0.2 to eliminate potential false positive results due to the presence of pseudogenes. The significantly mutated cell cycle genes in our cohort of KIT-mutant GISTs consisted of eight genes: RB1 (p = 1.3e−6), CUL1 (p = 3.1e−4), TP53 (p = 3.7e−4), CDC27 (p = 2.0e−3), ANAPC1 (7.4e−3), E2F3 (2.2e−2), GADD45A (p = 4.9e−2), and MAD2L2 (p = 0.05) (Table 3). Evaluation using STRINGv10 of significantly mutated genes showed significant enrichment for the cell cycle pathway (p = 0.0007) and spliceosome-related genes (p = 0.0008) in KIT-mutant GISTs (Fig. 2) [33].
Table 3.
Significant exonic or splice site non-synonymous mutations of KEGG cell cycle genes by MutSigCV in KIT mutant GIST samples
| Hugo symbol | Number of patients | Samples | Variant classification | Variant type | Genome_change | Exon | Codon change | Protein change | Gene p value | Mean VAF | Range VAF |
|---|---|---|---|---|---|---|---|---|---|---|---|
| RB1 | 1 | 17A | Splice_Site | DEL | g.chr13:48953728_48953729delAG | 14 | c.e14-1 | 1.31E−06 | 0.50 | 0.50 | |
| RB1 | 1 | 10A, 10B | Splice_Site | SNV | g.chr13:49030485G > A | 19 | c.(1960–1962)Gtg > Atg | p.V654 M | 1.31E−06 | 0.52 | 0.18–0.86 |
| RB1 | 1 | 14B | Nonsense_Mutation | SNV | g.chr13:48954195G > T | 15 | c.(1396–1398)Gaa > Taa | p.E466* | 1.31E−06 | 1.00 | 1 |
| CUL1 | 1 | 14A, 14B, 14C | Missense_Mutation | SNV | g.chr7:148451142C > T | 3 | c.(214–216)tCg > tTg | p.S72L | 3.11E−04 | 0.54 | 0.41–0.54 |
| TP53 | 1 | 2A, 2B | Missense_Mutation | SNV | g.chr17:7577548C > T | 7 | c.(733–735)Ggc > Agc | p.G245S | 3.66E−04 | 0.92 | 0.89–0.92 |
| TP53 | 1 | 20A | Missense_Mutation | SNV | g.chr17:7573984A > G | 10 | c.(1042–1044)tTg > tCg | p.L348S | 3.66E−04 | 0.50 | 0.5 |
| TP53 | 1 | 20A | Missense_Mutation | SNV | g.chr17:7577548C > A | 7 | c.(733–735)Ggc > Tgc | p.G245C | 3.66E−04 | 0.41 | 0.41 |
| CDC27 | 1 | 8A | Missense_Mutation | SNV | g.chr17:45266534G > A | 1 | c.(4–6)aCg > aTg | p.T2 M | 2.00E−03 | 0.33 | 0.33 |
| ANAPC1 | 1 | 15A | Frame_Shift_Del | DEL | g.chr2:112622408_112622409delCA | 8 | c.(805–807)tggfs | p.W269 fs | 7.36E−03 | 0.50 | 0.5 |
| E2F3 | 1 | 10A, 10B | Missense_Mutation | SNV | g.chr6:20486985T > C | 5 | c.(949–951)gTt > gCt | p.V317A | 2.23E−02 | 0.34 | 0.19–0.49 |
| GADD45A | 1 | 21A | Missense_Mutation | SNV | g.chr1:68153434G > A | 4 | c.(475–477)Gtg > Atg | p.V159 M | 4.88E−02 | 0.42 | 0.42 |
| MAD2L2 | 1 | 15A | Missense_Mutation | SNV | g.chr1:11735761G > C | 9 | c.(454–456)aCg > aGg | p.T152R | 4.97E−02 | 0.77 | 0.77 |
Fig. 2.
KIT mutant GISTs have enrichment for KEGG cell cycle pathway (p = 0.0007) and spliceosome pathway (p = 0.0008) using STRING v10 clustering of significantly somatic mutated genes (p < 0.003). The left cluster represents the cell cycle genes CDC27, CUL1, TP53, RB1 and closely related mutated genes. The cluster on the right represents genes involved in spliceosome regulation, SF3A2, U2AF2, RBMX and other closely related genes
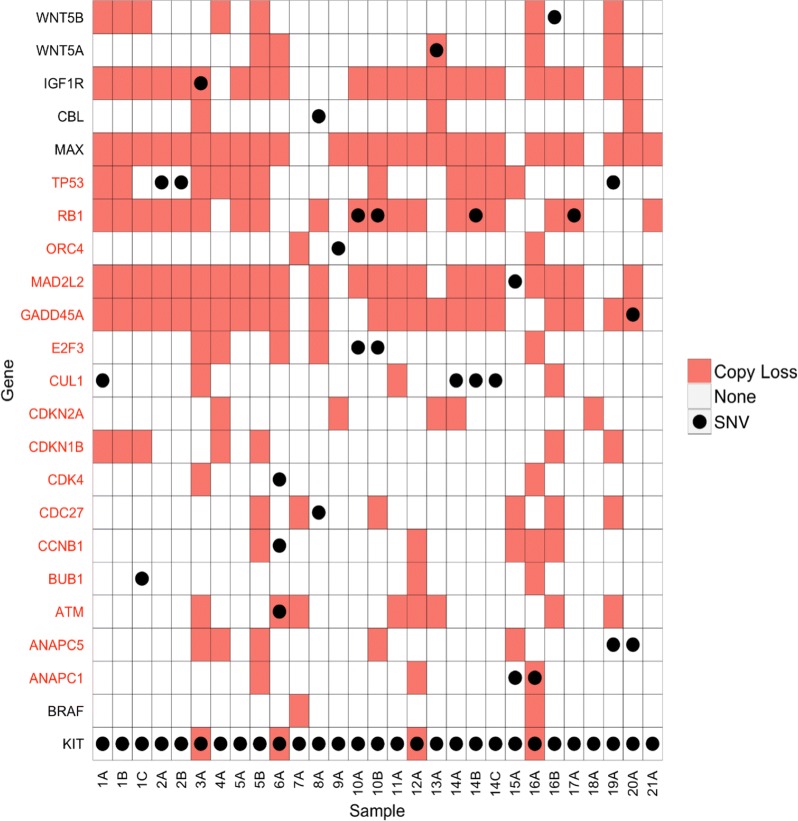
Integrated mutation and copy number analysis of cell cycle genes
To delineate the spectrum of molecular mechanisms that inactivate cell cycle genes in advanced GIST, we integrated the data from the somatic variant analysis with the inferred copy number variation data from the sequencing analysis. As shown in Fig. 3, TP53 (9/21 patients, 14/29 tumors), RB1 (12/21 cases, 19/29 tumors), CDKN2A (5/22 cases, 5/29 tumors), and MAX (17/21 patients, 25/29 tumors) were frequently altered by somatic mutation and/or copy number variation. Hemizyous/homozygous inactivating single nucleotide mutations of MAX were previously reported in 8/76 (10.5%) of GIST [34]. We did not any identify any inactivating MAX mutations in our series; this difference may be due to our smaller sample size. As noted above, large heterozygous deletions of chromosome 14 that included MAX were found in 17/21 (81%) patients in our WES cohort. Homozygous inactivation of MAX was previously reported to decrease expression of CDKN2A in GIST [34]. Based on our results, we speculate that haplo insufficiency of MAX may be enough to provide early dysregulation of the cell cycle (CDKN2A) during GIST pathogenesis.
Fig. 3.
Integrated genomic analysis of somatic mutation and copy number variations of KEGG pathway cell cycle genes in KIT-mutant GIST. The integrated results from genomic copy number loss and somatic mutation analyses are shown. Genes with a deleterious single nucleotide variant* (●) in a gene within the cell cycle pathway (red font on left) or cancer pathways (black font on left) are shown with the corresponding copy number variation for the same gene (red boxes). *Exonic, non-synonymous or splicing
Somatic cell cycle mutations are conserved between individual tumors resected from the same patient
In general, any somatic cell cycle mutation found in one metastasis from a given patient was also found in the other metastases analyzed from that patient. For example, all three metastases analyzed of Patient 1 had the same CDKN2A homozygous deletion, as identified by Affymetrix array. Similarly, both metastases analyzed from Patient 2 had the same TP53 c.(733–735) Ggc > Agc, p.G245S mutation at allelic fractions that were essentially homozygous (0.92 and 0.89, respectively; samples 2A and 2B, Table 3).
Dystrophin
Deletion of dystrophin (DMD), a tumor suppressor gene in human cancers with a myogenic program, has been reported as a late genetic event associated with the development of metastatic potential in GIST [35]. In our cohort, DMD copy loss was observed in eleven of the 29 lesions of KIT-mutant GIST (8/21 patients). The majority of the DMD copy loss events occurred in exons 1 through 32 which impacts Dp427 myogenic dystrophin but preserves a ubiquitously-expressed Dp71 dystrophin, as reported previously [35]. Among the patients with multiple tumors sequenced (patients 1, 2, 10, 14, and 16), no DMD copy loss was found in samples from patients 10, 14, or 16. Samples from patient 1 (3 samples) and patient 2 (2 samples) had identical DMD deletions in all analyzed samples.
Loss-of-heterozygosity (LOH) and targeted sequencing of CDKN2A, RB1 and TP53 in a cohort of 71 patients with well-defined GIST (validation data set)
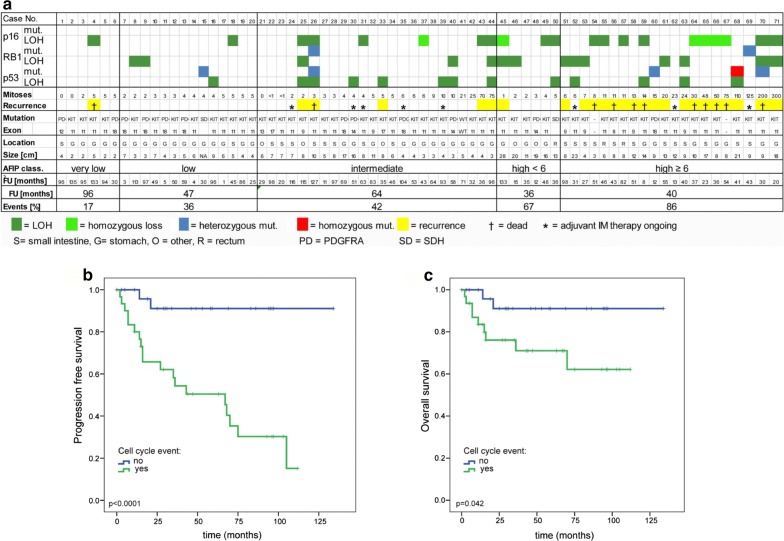
Based on the whole exome sequencing results, we expanded our study to perform a focused genetic screen for mutations and/or LOH of the cell cycle regulators CDKN2A/B, RB1 and TP53 using a combination of a clinically validated next generation sequencing panel, MLPA, and FISH in a cohort of 71 GIST patients from well-defined clinical risk groups with annotated clinical follow up. MAX was excluded from these analyses as we viewed this as an early event that was unlikely to influence prognosis [34]. In addition to the AFIP (Armed Forces Institute of Pathology) criteria for risk of GIST recurrence, we further divided the high-risk group into patients with lower (< 6 mitoses/50 high power fields [HPF]) and those with higher mitotic counts (≥ 6 mitoses/50HPF). Genetic events (mutation, deletion, and/or LOH) involving at least one of the three genes examined (CDKN2A/B, RB1, TP53) were found in 17% (1/6) of the very low-risk, 36% (5/14) of the low-risk, 42% (10/24) of the intermediate risk, 67% (4/6) of the high-risk/low mitotic-count and in 86% (18/21) of the high-risk/high mitotic-count group (Fig. 4a). The presence of cell cycle-related events was associated with a significantly shorter relapse-free survival (median 67 months versus not reached; p < 0.0001; Fig. 4b) and overall survival (Log Rank, p = 0.042; Fig. 4C) in the univariate analysis. Patients who were receiving ongoing adjuvant imatinib treatment were excluded from our analyses. In a multivariate analysis, the proportional hazards assumption was fulfilled for all covariates, and Cox regression analysis revealed a hazard ratio of 3.9, 7.3 and 4.5 for cell cycle-related events, mitotic count, and tumor size, respectively (p = 0.0775; Additional file 6: Table S8).
Fig. 4.
a Systematic screen for cell cycle-related genetic events in GIST with very low, low, intermediate and high risk of relapse according to the AFIP classification using Ion Torrent sequencing, MLPA and FISH analyses. Kaplan–Meier curves showing relapse-free (b) and overall survival (c) for patients with (green line) or without (blue line) a cell cycle-related event involving either TP53, CDKN2A, or RB1
Discussion
The dependency of most GIST on oncogenic KIT mutations is indisputable. Consistent with this statement, our current whole exome sequencing studies revealed secondary KIT mutations in 18/29 tumors obtained from 21 patients with malignant KIT-mutant GIST (Table 1). Other recurrent molecular causes of TKI resistance such as acquired mutations of downstream signaling effectors (e.g., KRAS or PIK3CA) were not identified in our discovery sample set. We conclude that secondary KIT mutations are found in most cases of KIT-mutant GIST with acquired resistance to kinase inhibitors. These results are in agreement with prior sequencing studies that analyzed the frequency of secondary kinase mutations in TKI-resistant, KIT-mutant GIST [30, 36].
However, additional events besides primary KIT mutations are needed for GIST cells to evolve into metastatic or resistant disease, as evidenced by similar or identical KIT mutations in cases of micro-GISTs and metastatic tumors [25]. In this study, we provide evidence that mutational dysregulation of the cell cycle is a crucial mechanism in progression from low-risk to malignant GIST. Whole exome sequencing of a set of high grade or metastatic GIST specimens showed significant enrichment of mutations of cell cycle pathway-related genes (Fisher’s Exact p = 0.001). We found further evidence of genomic inactivation of cell cycle control genes when analyzing copy number loss using the whole exome sequencing data. Overall, the most common recurrently copy number loss events were found in MAX (17/21 patients) and the cell cycle-related genes RB1 (13/22 patients), TP53 (12/21 patients), CDKN1B (5/21 cases), and CDKN2A/B (5/21 cases). Samples with somatic mutations of cell cycle genes and/or copy number losses of these same genes are summarized in Fig. 3.
Because the whole exome sequencing results in our present series underscored the importance of genomic inactivation of cell cycle regulator genes in GIST, we performed focused testing of the genomic status (mutation, copy number variation, and LOH) of three of these genes (CDKN2A, RB1, and TP53) in an independent group of GIST patients with annotated long-term clinical follow up (validation data set). We found that mutations and/or copy loss of these cell cycle regulator genes were associated with an increased risk of metastatic recurrence. In this second group of patients, we noted a significantly lower percentage of TP53, CDKN2A/B or RB1 genomic alterations in low-risk compared to high-risk GIST (Fig. 4). All but two of the patients who later experienced recurrence had at least one genomic alteration involving CDKN2A/B, RB1, or TP53. Notably, cell cycle-related genetic events were associated with higher number of mitoses in primary GISTs (Fig. 4a), a well-recognized risk factor for the development of metastatic disease.
Patients with intermediate-risk GISTs are clinically challenging, because there are currently no reliable biomarkers to identify the patients in this risk category who have a higher risk of relapse and might benefit from adjuvant imatinib therapy. Among the 24 intermediate-risk GISTs in our second cohort, ten (42%) had cell cycle-related genetic events. Notably, among these ten patients, seven did not receive adjuvant imatinib and five patients experienced a recurrence of their GIST. By contrast, none of the 14 patients with intermediate-risk GIST lacking a genomic cell cycle event had a recurrence (2-sample proportion test, p = 0.002). Overall, a cell cycle-related genetic event was strongly associated with poor progression-free survival in patients with GIST (p < 0.0001). Notably, the only patient with metastatic relapse in the very low-risk group of six patients had LOH of the CDKN2A/B locus in his gastric primary tumor.
In a multivariate analysis, both mitotic count and tumor size were highly significant prognostic factors. Due to the limitations of sample size, primary tumor site was excluded from the analysis. Nonetheless, multivariate analysis for recurrence-free survival revealed a hazard ratio of 3.9 for GISTs with a cell cycle-related genetic event (p = 0.078) even against the background of a relatively small group of patients. Further assessment of the clinical validity of these genetic events as prognostic factors will require larger numbers of patients with annotated long-term clinical follow-up. Our results are generally concordant with other studies that correlated cell cycle events and risk of GIST recurrence. However, these studies used a variety of techniques, including immunohistochemistry, to identify cell cycle gene dysregulation [37–40]. As shown in our studies, analysis of both specific cell cycle gene mutation status and CNV are necessary to identify a more complete spectrum of genomic events targeting RB1, CDN2A/B, and TP53 genes. Our experimental methods may not detect all intragenic deletions (e.g. microdeletions). In addition, in some cases of malignant GIST, CDKN2A is inactivated by promoter hypermethylation [41, 42]. Further studies are needed to identify the optimal diagnostic techniques needed to identify all mechanisms of inactivation of cell cycle genes in GIST. If validated in subsequent studies, these cell cycle markers could be used for prognostication in conjunction with standard pathological features that are known to correlate with risk.
In addition to the recurrent genomic events targeting cell cycle control genes, we also discovered evidence for dysregulation of mRNA splicing in the biology of metastatic GIST. Gene set enrichment analysis found KIT-mutant GISTs to also be enriched for mutations of genes involved in spliceosome regulation (p value = 0.026), including SF3A2 (q < 0.001), U2AF2, RBMX, RBMXL3, PRPF18, SNRP200 that were significantly mutated in KIT-mutant GISTs with p < 0.05. SF3A2 and U2AF2 are both associated with spliceosome component U2 small nuclear ribonucleotide proteins (snRNP) [43]. Three lesions from a single patient (samples 14A, 14B, 14C) contained the identical SF3A2 nonsense mutation E177*. Two other tumors from different patients (9A and 17A) contained identical somatic U2AF2 splice site mutations. The remaining mutated genes involved in spliceosome assembly with p < 0.001 were identified in nine other samples from eight different patients. In addition, four KIT-mutant samples contained somatic single nucleotide variants in FRG1 (q < 0.01), a cancer driver gene in follicular thyroid cancer [44].
Notably, mutations of SF3A2 and FRG1 ranked as the first and third most common somatic mutations (after KIT), respectively in KIT-mutant GIST (Fig. 1b). SF3A2 is part of the U2 snRNP, and another member of this complex (SF3B1) is recurrently mutated in myelodysplastic syndrome, acute myeloid leukemia, and chronic lymphocytic leukemia [45]. We also identified loss of the SF3A3 gene, located on 1p, to be a frequent event in our series (17/21 patients, 25/29 samples). Like SF3A2, the SF3A3 gene encodes a component of the splicing factor 3a complex. In addition, we found mutations of U2AF2, a component of the U2AF complex. U2AF2 mutations leading to spliceosome dysfunction have been reported in other cancers [46]. Notably, mutation of the other member of the U2AF complex (U2AF1) has been reported in the same hematologic malignancies associated with SF3B1 mutations [47]. Further studies are needed to understand how dysregulation of the spliceosome contributes to GIST biology.
Taken together, our study provides evidence that mutational dysregulation of the cell cycle is a crucial mechanism in progression from low-risk to malignant GIST. Based on these observations we propose a model of genetic progression leading to malignant, invasive and metastatic GIST as shown in Fig. 5. Our model depicts chromosome 14q and 22q deletions as early events in GIST progression. KIT-mutant asymptomatic and innocuous micro-GISTs have been found in approximately one-third of the general population. These tumors rarely progress to malignancy, presumably because they require additional mutations to become clinically aggressive. Cytogenetic studies support this hypothesis, demonstrating that early GISTs typically harbor KIT or PDGFRA mutations, often accompanied by chromosome 14q and 22q deletions, but do not yet show evidence of chromosome 9p deletions that potentially target CDKN2A/B [26]. In contrast, inactivation of dystrophin is a late event in GIST progression (Fig. 5). Dystrophin has been shown to behave as a tumor suppressor, and in a large series of GISTs genomic mechanisms of dystrophin inactivation were present in 96% of metastatic GIST, but absent in low-risk GIST [36]. We therefore propose that cell cycle-related events are ubiquitous, intermediate steps in the progression of GIST. Our observations also suggest that clinical assessment of genetic events involving CDKN2A/B, RB1 or TP53 may be a useful addition to existing risk assessment models, with implications for selection of patients for adjuvant treatment and intensified surveillance schedules.
Fig. 5.
Model of genetic progression of GIST from benign to invasive/metastatic tumors
Conclusions
Our studies show that cell cycle dysregulation due to genomic inactivation of cell cycle regulatory genes is a ubiquitous mechanism during the transition from low-risk to high-risk/metastatic GIST. These events might sensitize cells to KIT-independent treatment approaches such as CDK4 or MDM2 inhibitors. Based on this data, we propose a model for molecular pathogenesis of malignant GIST. Further studies are needed to confirm these genomic observations as potential predictors of clinical behavior and to examine the efficacy of imatinib combination therapy with cell cycle inhibitors in GIST. In addition, further studies are needed to understand the role of spliceosome mutations in malignant GIST biology.
Additional files
Additional file 1. Additional methods for genomic studies. Figure S1. Comparison of WES read depth (blue bars) and SNV frequency (orange bars). Table S1. Mutation type frequency in 29 KIT-mutant GIST. Table S2. Breakdown of mutation rates per category discovered for this individual set. Table S3. Regions of large copy number variations affecting greater than 20% of the bases of a given chromosome arm. The numbers represent proportion of bases in the specified chromosomal arm that exhibit copy number variation.
Additional file 2: Table S4. KEGG pathways enrichment analysis results.
Additional file 3: Table S5. Gene set enrichment analyses for significant mutations according to Mutsig assessment.
Additional file 4: Table S6. MutSig analysis results. All mutations-sample codes match manuscript numbering.
Additional file 5: Table S7. All somatic mutations. Sample codes match manuscript numbering (e.g. 1A, 1B, etc.).
Additional file 6: Table S8. Multi-variate analysis of clinically characterized GIST.
Authors’ contributions
Study design: MCH, JP, MD-R, CLC, AD, BR, TO, MvdR, JC, JAF, SB. Initial draft: MCH, JP, JAF, SB. Provision of tumor samples: MCH, MvDR, CLC, CPR, MvdR, AD, JC, JAF, SB. Data analysis: MCH, JP, CB, JAF, SB. Writing, editing, and final approval of manuscript: all authors. All authors read and approved the final manuscript.
Acknowledgements
None.
Competing interests
MCH: Novartis consulting and expert testimony, Molecular MD consulting and equity interest, patent on treatment of GIST. SB: Research support from Novartis, Blueprint Medicines, Ariad; Consultant for GSK, Novartis, Pfizer, Bayer, Fresenius, Lilly, Blueprint Medicines, Deciphera; Honoraria (CME) from Pharmamar, GSK, Pfizer, Bayer; Travel support from Pharmamar, Bayer.
Availability of data and materials
The dataset(s) supporting the conclusions of this article are included within the article and its additional file(s). Additional datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request. We are in the process of depositing all of the data in a publically available database.
Consent for publication
Does not apply (all samples were de-identified).
Ethics approval and consent to participate
De-identified samples analyzed by whole exome sequencing (WES) were obtained from participating institutions (Oregon Health and Science University, University of Duisburg-Essen, Brigham and Women`s Hospital and Katholieke Universiteit Leuven and University Hospitals Leuven). These samples included 29 samples from 21 different patients. This portion of our study was approved by the institutional review boards at each of the participating sites.
Targeted sequence analysis was performed on a second group of 71 GIST samples representing an independent cohort of clinically characterized patients from prospectively maintained databases of participating institutions (University of Duisburg-Essen, Brigham and Women`s Hospital, and Oregon Health and Science University) and from the Life Raft Group patient database. This cohort study was approved by the institutional review boards at each of the participating sites.
Funding
Life Raft Group (MCH, MD-R, CLC, AD, BR, TO, MvDR, JAF, SB), GIST Cancer Research Fund (MCH, CLC, AD), VA Merit Review Grant (MCH, 2I01BX000338-05), NIH Grant DK058185 (TO), Sarkomtour Fundraising Initiative (SB).
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Michael C. Heinrich, Email: heinrich@ohsu.edu
Janice Patterson, Email: patterja@ohsu.edu.
Carol Beadling, Email: beadling@ohsu.edu.
Yuexiang Wang, Email: yxwang76@sibs.ac.cn.
Maria Debiec-Rychter, Email: maria.debiec-rychter@kuleuven.be.
Barbara Dewaele, Email: barbara.dewaele@uzleuven.be.
Christopher L. Corless, Email: corlessc@ohsu.edu
Anette Duensing, Email: aduensin@pitt.edu.
Chandrajit P. Raut, Email: craut@bwh.harvard.edu
Brian Rubin, Email: rubinb2@ccf.org.
Tamas Ordog, Email: Ordog.Tamas@mayo.edu.
Matt van de Rijn, Email: mrijn@stanford.edu.
Jerry Call, Email: jcall@liferaftgroup.org.
Thomas Mühlenberg, Email: thomas.muehlenberg@uk-essen.de.
Jonathan A. Fletcher, Email: jfletcher@bwh.harvard.edu
Sebastian Bauer, Email: sebastian.bauer@uni-due.de.
References
- 1.Hirota S, Isozaki K, Moriyama Y, Hashimoto K, Nishida T, Ishiguro S, et al. Gain-of-function mutations of c-kit in human gastrointestinal stromal tumors. Science. 1998;279:577–580. doi: 10.1126/science.279.5350.577. [DOI] [PubMed] [Google Scholar]
- 2.Heinrich MC, Corless CL, Demetri GD, Blanke CD, von Mehren M, Joensuu H, et al. Kinase mutations and imatinib response in patients with metastatic gastrointestinal stromal tumor. J Clin Oncol. 2003;21:4342–4349. doi: 10.1200/JCO.2003.04.190. [DOI] [PubMed] [Google Scholar]
- 3.Corless CL. Gastrointestinal stromal tumors: what do we know now? Mod Pathol. 2014;27:S1–S16. doi: 10.1038/modpathol.2013.173. [DOI] [PubMed] [Google Scholar]
- 4.Liegl-Atzwanger B, Fletcher JA, Fletcher CDM. Gastrointestinal stromal tumors. Virchows Arch Int J Pathol. 2010;456:111–127. doi: 10.1007/s00428-010-0891-y. [DOI] [PubMed] [Google Scholar]
- 5.Agaram NP, Wong GC, Guo T, Maki RG, Singer S, Dematteo RP, et al. Novel V600E BRAF mutations in imatinib-naive and imatinib-resistant gastrointestinal stromal tumors. Genes Chromosomes Cancer. 2008;47:853–859. doi: 10.1002/gcc.20589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Demetri GD, von Mehren M, Blanke CD, Van den Abbeele AD, Eisenberg B, Roberts PJ, et al. Efficacy and safety of imatinib mesylate in advanced gastrointestinal stromal tumors. N Engl J Med. 2002;347:472–480. doi: 10.1056/NEJMoa020461. [DOI] [PubMed] [Google Scholar]
- 7.Fanta PT, Sicklick JK, Betz BL, Peterson MR. In vivo imatinib sensitivity in a patient with GI Stromal Tumor bearing a PDGFRA Deletion DIM842-844. J Clin Oncol. 2015;33:e41–e44. doi: 10.1200/JCO.2013.50.0082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Blanke CD, Demetri GD, von Mehren M, Heinrich MC, Eisenberg B, Fletcher JA, et al. Long-term results from a randomized phase II trial of standard- versus higher-dose imatinib mesylate for patients with unresectable or metastatic gastrointestinal stromal tumors expressing KIT. J Clin Oncol Off J Am Soc Clin Oncol. 2008;26:620–625. doi: 10.1200/JCO.2007.13.4403. [DOI] [PubMed] [Google Scholar]
- 9.Blay J-Y, Le Cesne A, Ray-Coquard I, Bui B, Duffaud F, Delbaldo C, et al. Prospective multicentric randomized phase III study of imatinib in patients with advanced gastrointestinal stromal tumors comparing interruption versus continuation of treatment beyond 1 year: the French Sarcoma Group. J Clin Oncol Off J Am Soc Clin Oncol. 2007;25:1107–1113. doi: 10.1200/JCO.2006.09.0183. [DOI] [PubMed] [Google Scholar]
- 10.Demetri GD, van Oosterom AT, Garrett CR, Blackstein ME, Shah MH, Verweij J, et al. Efficacy and safety of sunitinib in patients with advanced gastrointestinal stromal tumour after failure of imatinib: a randomised controlled trial. Lancet Lond Engl. 2006;368:1329–1338. doi: 10.1016/S0140-6736(06)69446-4. [DOI] [PubMed] [Google Scholar]
- 11.Demetri GD, Reichardt P, Kang Y-K, Blay J-Y, Rutkowski P, Gelderblom H, et al. Efficacy and safety of regorafenib for advanced gastrointestinal stromal tumours after failure of imatinib and sunitinib (GRID): an international, multicentre, randomised, placebo-controlled, phase 3 trial. Lancet Lond Engl. 2013;381:295–302. doi: 10.1016/S0140-6736(12)61857-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Heinrich MC, Marino-Enriquez A, Presnell A, Donsky RS, Griffith DJ, McKinley A, et al. Sorafenib inhibits many kinase mutations associated with drug-resistant gastrointestinal stromal tumors. Mol Cancer Ther. 2012;11:1770–1780. doi: 10.1158/1535-7163.MCT-12-0223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Agaimy A, Wünsch PH, Hofstaedter F, Blaszyk H, Rümmele P, Gaumann A, et al. Minute gastric sclerosing stromal tumors (GIST tumorlets) are common in adults and frequently show c-KIT mutations. Am J Surg Pathol. 2007;31:113–120. doi: 10.1097/01.pas.0000213307.05811.f0. [DOI] [PubMed] [Google Scholar]
- 14.Corless CL, McGreevey L, Haley A, Town A, Heinrich MC. KIT mutations are common in incidental gastrointestinal stromal tumors one centimeter or less in size. Am J Pathol. 2002;160:1567–1572. doi: 10.1016/S0002-9440(10)61103-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kawanowa K, Sakuma Y, Sakurai S, Hishima T, Iwasaki Y, Saito K, et al. High incidence of microscopic gastrointestinal stromal tumors in the stomach. Hum Pathol. 2006;37:1527–1535. doi: 10.1016/j.humpath.2006.07.002. [DOI] [PubMed] [Google Scholar]
- 16.Muenst S, Thies S, Went P, Tornillo L, Bihl MP, Dirnhofer S. Frequency, phenotype, and genotype of minute gastrointestinal stromal tumors in the stomach: an autopsy study. Hum Pathol. 2011;42:1849–1854. doi: 10.1016/j.humpath.2011.01.024. [DOI] [PubMed] [Google Scholar]
- 17.Call J, Walentas CD, Eickhoff JC, Scherzer N. Survival of gastrointestinal stromal tumor patients in the imatinib era: life raft group observational registry. BMC Cancer. 2012;12:90. doi: 10.1186/1471-2407-12-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Van der Auwera GA, Carneiro MO, Hartl C, Poplin R, Del Angel G, Levy-Moonshine A, et al. From FastQ data to high confidence variant calls: the genome analysis toolkit best practices pipeline. Curr Protoc Bioinforma Ed Board Andreas Baxevanis Al. 2013;43:1–33. doi: 10.1002/0471250953.bi1110s43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lawrence MS, Stojanov P, Polak P, Kryukov GV, Cibulskis K, Sivachenko A, et al. Mutational heterogeneity in cancer and the search for new cancer-associated genes. Nature. 2013;499:214–218. doi: 10.1038/nature12213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kandoth C, McLellan MD, Vandin F, Ye K, Niu B, Lu C, et al. Mutational landscape and significance across 12 major cancer types. Nature. 2013;502:333–339. doi: 10.1038/nature12634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Alexandrov LB, Nik-Zainal S, Wedge DC, Aparicio SAJR, Behjati S, Biankin AV, et al. Signatures of mutational processes in human cancer. Nature. 2013;500:415–421. doi: 10.1038/nature12477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.COSMIC: Signatures of Mutational Processes in Human Cancer. http://cancer.sanger.ac.uk/cosmic/signatures. Accessed 25 July 2016.
- 23.Rizvi NA, Hellmann MD, Snyder A, Kvistborg P, Makarov V, Havel JJ, et al. Cancer immunology. Mutational landscape determines sensitivity to PD-1 blockade in non-small cell lung cancer. Science. 2015;348:124–128. doi: 10.1126/science.aaa1348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gunawan B, von Heydebreck A, Sander B, Schulten H-J, Haller F, Langer C, et al. An oncogenetic tree model in gastrointestinal stromal tumours (GISTs) identifies different pathways of cytogenetic evolution with prognostic implications. J Pathol. 2007;211:463–470. doi: 10.1002/path.2128. [DOI] [PubMed] [Google Scholar]
- 25.Corless CL, Barnett CM, Heinrich MC. Gastrointestinal stromal tumours: origin and molecular oncology. Nat Rev Cancer. 2011;11:865–878. doi: 10.1038/nrc3143. [DOI] [PubMed] [Google Scholar]
- 26.Yang J, Du X, Lazar AJF, Pollock R, Hunt K, Chen K, et al. Genetic aberrations of gastrointestinal stromal tumors. Cancer. 2008;113:1532–1543. doi: 10.1002/cncr.23778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ylipää A, Hunt KK, Yang J, Lazar AJF, Torres KE, Lev DC, et al. Integrative genomic characterization and a genomic staging system for gastrointestinal stromal tumors. Cancer. 2011;117:380–389. doi: 10.1002/cncr.25594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Heinrich MC, Rubin BP, Longley BJ, Fletcher JA. Biology and genetic aspects of gastrointestinal stromal tumors: kIT activation and cytogenetic alterations. Hum Pathol. 2002;33:484–495. doi: 10.1053/hupa.2002.124124. [DOI] [PubMed] [Google Scholar]
- 29.Heinrich MC, Corless CL, Duensing A, McGreevey L, Chen C-J, Joseph N, et al. PDGFRA activating mutations in gastrointestinal stromal tumors. Science. 2003;299:708–710. doi: 10.1126/science.1079666. [DOI] [PubMed] [Google Scholar]
- 30.Schoppmann SF, Vinatzer U, Popitsch N, Mittlböck M, Liebmann-Reindl S, Jomrich G, et al. Novel clinically relevant genes in gastrointestinal stromal tumors identified by exome sequencing. Clin Cancer Res Off J Am Assoc Cancer Res. 2013;19:5329–5339. doi: 10.1158/1078-0432.CCR-12-3863. [DOI] [PubMed] [Google Scholar]
- 31.El-Rifai W, Sarlomo-Rikala M, Andersson LC, Knuutila S, Miettinen M. DNA sequence copy number changes in gastrointestinal stromal tumors: tumor progression and prognostic significance. Cancer Res. 2000;60:3899–3903. [PubMed] [Google Scholar]
- 32.KEGGREST. Bioconductor. http://bioconductor.org/packages/KEGGREST/. Accessed 12 Mar 2016.
- 33.Szklarczyk D, Franceschini A, Wyder S, Forslund K, Heller D, Huerta-Cepas J, et al. STRING v10: protein-protein interaction networks, integrated over the tree of life. Nucleic Acids Res. 2015;43:D447–D452. doi: 10.1093/nar/gku1003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Schaefer I-M, Wang Y, Liang C, Bahri N, Quattrone A, Doyle L, et al. MAX inactivation is an early event in GIST development that regulates p16 and cell proliferation. Nat Commun. 2017;8:14674. doi: 10.1038/ncomms14674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wang Y, Marino-Enriquez A, Bennett RR, Zhu M, Shen Y, Eilers G, et al. Dystrophin is a tumor suppressor in human cancers with myogenic programs. Nat Genet. 2014;46:601–606. doi: 10.1038/ng.2974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wang Y, Fletcher JA. Cell cycle and dystrophin dysregulation in GIST. Cell Cycle. 2015;14:2713–2714. doi: 10.1080/15384101.2015.1064676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lartigue L, Neuville A, Lagarde P, Brulard C, Rutkowski P, Tos PD, et al. Genomic index predicts clinical outcome of intermediate-risk gastrointestinal stromal tumours, providing a new inclusion criterion for imatinib adjuvant therapy. Eur J Cancer. 2015;51:75–83. doi: 10.1016/j.ejca.2014.10.014. [DOI] [PubMed] [Google Scholar]
- 38.Sabah M, Cummins R, Leader M, Kay E. Altered expression of cell cycle regulatory proteins in gastrointestinal stromal tumors: markers with potential prognostic implications. Hum Pathol. 2006;37:648–655. doi: 10.1016/j.humpath.2006.01.023. [DOI] [PubMed] [Google Scholar]
- 39.Lagarde P, Pérot G, Kauffmann A, Brulard C, Dapremont V, Hostein I, et al. Mitotic checkpoints and chromosome instability are strong predictors of clinical outcome in gastrointestinal stromal tumors. Clin Cancer Res. 2012;18:826–838. doi: 10.1158/1078-0432.CCR-11-1610. [DOI] [PubMed] [Google Scholar]
- 40.Ihle MA, Huss S, Jeske W, Hartmann W, Merkelbach-Bruse S, Schildhaus H-U, et al. Expression of cell cycle regulators and frequency of TP53 mutations in high risk gastrointestinal stromal tumors prior to adjuvant imatinib treatment. PLoS ONE. 2018;13:e0193048. doi: 10.1371/journal.pone.0193048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.House MG, Guo M, Efron DT, Lillemoe KD, Cameron JL, Syphard JE, et al. Tumor suppressor gene hypermethylation as a predictor of gastric stromal tumor behavior. J Gastrointest Surg Off J Soc Surg Aliment Tract. 2003;7:1004–1014. doi: 10.1016/j.gassur.2003.08.002. [DOI] [PubMed] [Google Scholar]
- 42.Okamoto Y, Sawaki A, Ito S, Nishida T, Takahashi T, Toyota M, et al. Aberrant DNA methylation associated with aggressiveness of gastrointestinal stromal tumour. Gut. 2012;61:392–401. doi: 10.1136/gut.2011.241034. [DOI] [PubMed] [Google Scholar]
- 43.Lin P-C, Xu R-M. Structure and assembly of the SF3a splicing factor complex of U2 snRNP. EMBO J. 2012;31:1579–1590. doi: 10.1038/emboj.2012.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Erinjeri NJ, Nicolson NG, Deyholos C, Korah R, Carling T. Whole-exome sequencing identifies two discrete druggable signaling pathways in follicular thyroid cancer. J Am Coll Surg. 2018;226(950–959):e5. doi: 10.1016/j.jamcollsurg.2018.01.059. [DOI] [PubMed] [Google Scholar]
- 45.Chesnais V, Kosmider O, Damm F, Itzykson R, Bernard OA, Solary E, et al. Spliceosome mutations in myelodysplastic syndromes and chronic myelomonocytic leukemia. Oncotarget. 2012;3:1284–1293. doi: 10.18632/oncotarget.749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Glasser E, Agrawal AA, Jenkins JL, Kielkopf CL. Cancer-associated mutations mapped on high-resolution structures of the U2AF2 RNA recognition motifs. Biochemistry. 2017;56:4757–4761. doi: 10.1021/acs.biochem.7b00551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ilagan JO, Ramakrishnan A, Hayes B, Murphy ME, Zebari AS, Bradley P, et al. U2AF1 mutations alter splice site recognition in hematological malignancies. Genome Res. 2015;25:14–26. doi: 10.1101/gr.181016.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. Additional methods for genomic studies. Figure S1. Comparison of WES read depth (blue bars) and SNV frequency (orange bars). Table S1. Mutation type frequency in 29 KIT-mutant GIST. Table S2. Breakdown of mutation rates per category discovered for this individual set. Table S3. Regions of large copy number variations affecting greater than 20% of the bases of a given chromosome arm. The numbers represent proportion of bases in the specified chromosomal arm that exhibit copy number variation.
Additional file 2: Table S4. KEGG pathways enrichment analysis results.
Additional file 3: Table S5. Gene set enrichment analyses for significant mutations according to Mutsig assessment.
Additional file 4: Table S6. MutSig analysis results. All mutations-sample codes match manuscript numbering.
Additional file 5: Table S7. All somatic mutations. Sample codes match manuscript numbering (e.g. 1A, 1B, etc.).
Additional file 6: Table S8. Multi-variate analysis of clinically characterized GIST.
Data Availability Statement
The dataset(s) supporting the conclusions of this article are included within the article and its additional file(s). Additional datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request. We are in the process of depositing all of the data in a publically available database.