Abstract
Background:
Over 90% of women experience pain during breastfeeding initiation and lack strategies to self-manage breast and nipple pain. Guided by the Individual and Family Self-Management Theory (IFSMT), a Breastfeeding Self-Management (BSM) intervention targeted women’s knowledge, beliefs, and social facilitation to manage their breast and nipple pain and achieve their breastfeeding goals.
Objectives:
The purpose of this longitudinal pilot randomized control trial (RCT) was to test the preliminary efficacy of the BSM intervention on general and specific pain related to breastfeeding.
Method:
Sixty women intending to breastfeed were approached within 48 hours of delivery to participate in this pilot RCT (30 randomized to BSM intervention and 30 to control group). All participants provided baseline data before discharge, and pain and breastfeeding measures at 1, 2, and 6 weeks. Participants in the BSM intervention group received educational modules addressing breast and nipple pain, biweekly, text-based, nurse coaching, and completed a daily breastfeeding journal.
Results:
Women in the BSM intervention group reported significantly less breast and nipple pain at 1 and 2 weeks using a visual analogue scale (VAS), p < 0.014, and p < 0.006, and at 2 weeks using the Brief Pain Inventory intensity scale, p < .029, but no difference in breastfeeding duration.
Discussion:
The BSM intervention pilot demonstrates a positive effect on breastfeeding specific and overall generalized pain. Future investigation is needed to identify at-risk women of ongoing breastfeeding pain, and develop precision interventions to sustain this beneficial health behavior for mothers and infants.
Keywords: breastfeeding, pain, self-management
Breast milk obtained during breastfeeding is a natural source of precision nutrition (American Academy of Pediatrics, 2012). Researchers postulate that the changing composition of breast milk responds to the nutritional and immunological needs of the preterm and full-term infants (Bobiński, Mikulska, Mojska, & Simon, 2013; Gardner et al., 2017; Khan et al., 2013). Although no study has directly tested the precise adaptation of breast milk to the infant’s needs, the studies do lend support that breast milk should be considered a precise nutrition for infants. The optimal length of exclusive breast milk nutrition is until 6 months. However, the average number of exclusively breastfeeding women declines from 81% at initiation, 59% at 1 month, 52.2% at 2 months, to 23% at 6 months, costing the United States $13 billion per year in infant health-related expenditures (Bartick & Reinhold, 2010; Center for Disease Control and Prevention, 2018). A critical window of opportunity to prevent breastfeeding cessation occurs as breastfeeding is established and during the first month following birth (Center for Disease Control, 2018). The development of personalized interventions to promote breastfeeding during this important period could lead to improved health outcomes for mother and baby.
Breastfeeding pain is a major reason for early cessation of breastfeeding for approximately 35% of women (McCann, Baydar, & Williams, 2007; Wagner, Chantry, Dewey, & Nommsen-Rivers, 2013). Although 90% of women report acute breast and nipple pain during the first week of breastfeeding initiation, this pain is considered to be clinical normative and/or related to the mechanics of breastfeeding (ankyloglossia, infection, or engorgement) (Lucas & McGrath, 2016; Morland-Schultz & Hill, 2005). Thus, most clinical interventions target mechanical or positional triggers of pain (Lucas & McGrath, 2016). However, 30% of women who continue to breastfeed at 2 weeks after birth report persistent breast and nipple pain (Kent et al., 2015). Of the women with persistent pain who seek professional support, 43% continue to have persistent pain (Kent et al., 2015). Currently, standard clinical lactation education does not routinely provide knowledge and skills to self-manage breast and nipple pain during breastfeeding (Lucas & McGrath, 2016). In addition, few clinical interventions to promote breastfeeding consider the influence of each woman’s personal, genetic, social and environmental breastfeeding characteristics, on breastfeeding pain self-management (Amir, Jones, & Buck, 2015; Ryan & Sawin, 2009).
As little attention has been given to addressing breastfeeding pain, women rarely receive adequate knowledge and skills to address self-management of their breastfeeding-related pain (Amir et al., 2015). Pain self-management strategies of distraction, cognitive reframing, relaxation, and breathing have been effective for reducing pain (Davis, Zautra, Wolf, Tennen, & Yeung, 2015; Litt & Tennen, 2015). Many women are familiar with cognitive behavioral interventions focused on relaxation, breathing, and use of guided imagery for labor-related pain and anxiety (Smith, Levett, Collins, & Crowther, 2011). In the postpartum period, cognitive behavioral therapy is effective in treating postpartum mood disorders in both inpatient and outpatient settings, which often has a positive downstream effect of extending breastfeeding duration (Spinelli, Endicott, & Goetz, 2013; Taylor, Cavanagh, & Strauss, 2016). One study reported increasing breastfeeding duration through support provided by community healthcare workers (Sikander et al., 2015). However, to date, no studies have investigated the efficacy of cognitive behavioral self-management intervention for women experiencing acute and persistent breast and nipple pain while breastfeeding. The purpose of this study was to test the efficacy of novel Breastfeeding Self-Management (BSM) intervention on the primary outcome of pain intensity and interference, and secondarily on breastfeeding duration.
Theoretical Model
For this study, a BSM intervention was developed for breastfeeding women and was guided by the Individual & Family Self-Management Theory (IFSMT; Supplement Figure 1). The IFSMT is grounded in the self-management literature and proposes that an individual’s health condition must be understood within the context of their overall health, their family, and social environment. For women experiencing pain during breastfeeding, their condition-specific health behavior characteristics (health history, genetic, psychological, and somatosensory), physical and social environment (hospital as baby-friendly, access to lactation healthcare professional), and individual and family characteristics (income, personal, and family history of breastfeeding and infant demographics) must be taken into account (Ryan & Sawin, 2009). Based on these characteristics, the BSM intervention was designed to provide timely knowledge and skills regarding breastfeeding and strategies for women to modify their breastfeeding behaviors by increasing pain self-efficacy and access to instrumental support (Ryan & Sawin, 2009).
Cognitive behavioral therapy is effective within a therapeutic relationship; however, a face-to-face interaction during the first weeks after delivery is burdensome. Several studies found interactive texting using a script was effective in maintaining exclusive breastfeeding and increasing breastfeeding duration (Gallegos, Russell-Bennett, Previte, & Parkinson, 2014; Poorman, Gazmararian, Parker, Yang, & Elon, 2015). The BSM intervention leveraged the universal use of smartphones in childbearing adults and used texting for all study communication (Fox & Duggan, 2012). The BSM intervention included nurse-led instrumental support texting, emailed study measures, hyperlinks to educational modules addressing breast and nipple pain, a daily breastfeeding journal, and reminders to complete study documents. All of these activities were targeted to support women to increase their knowledge and skills regarding breast and nipple pain, as well as their ability to manage breastfeeding challenges.
Methods
Design
A pilot RCT with 60 women was designed to test the efficacy of the BSM intervention on breast and nipple pain and general pain in breastfeeding women compared to routine postpartum care and limited breastfeeding support. Data were collected from April 2017 to November 2017. The study was approved by the University of Connecticut institutional review board and registered with Clinical Trials.gov (NCT03392675).
Sample and Setting
Women were recruited at two tertiary care academic hospitals delivering 2,280 infants annually with in-hospital and outpatient lactation support. Eligibility criteria for women were: (a) 18–45 years of age; (b) within 48 hours of having given birth; (c) antenatal intention to breastfeed; (d) access to texting; (e) access to a computer; (f) fluency to read and write English; (g) singleton infant > 37 weeks gestational age admitted to newborn nursery; and (h) evaluated by an International Board Certified Lactation Consultant (IBCLC) during their in-hospital stay. Exclusion criteria for women were: (a) < 18 years of age; (b) delivered infant with congenital anomalies; (c) history of mental health disorder (i.e., schizophrenia, bipolar disorder); (d) health condition that would alter pain sensorium (i.e., sickle cell anemia, diabetes, history of seizures); and (e) eczema, rash, or dermatographism on nondominant forearm which could interfere with experimental pain testing.
Sample Size.
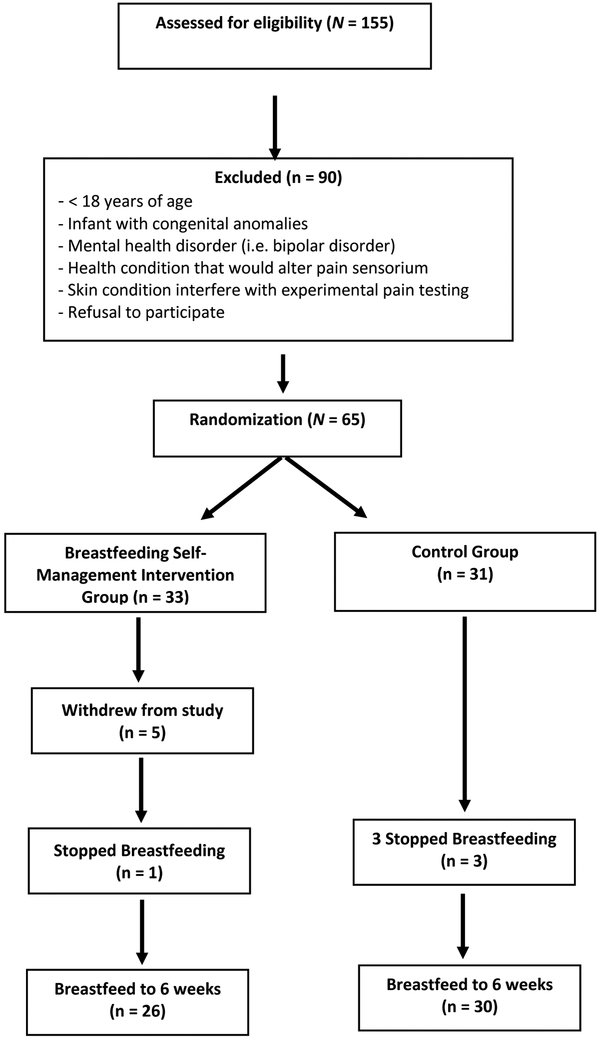
Based on a two-group study with an alpha of 0.05 80% power will be achieved with a total sample size of 60 women, with 30 women per group, with a 10-point difference in mean pain intensity on the visual analog scale (Erdfelder, Faul, & Buchner, 1996). The sample size is similar to other feasibility studies (Billingham, Whitehead, & Julious, 2013) and the results will inform the effect size for a forthcoming larger study. Figure 1 (CONSORT diagram) reflects eligibility, randomization, and retention of participations.
Figure 1.
Consort Diagram
Breastfeeding Self-Management Intervention
The BSM intervention incorporated educational modules that covered information to address breastfeeding challenges and skills to manage breastfeeding pain, text-based instrumental support for self-managing breastfeeding pain duration, a daily journal and nurse coaching for women experiencing breast and nipple pain during breastfeeding at 1, 2, and 6 weeks.
Biweekly texting.
After discharge home, a nurse-lead team member contacted women in the intervention group biweekly for 6 weeks. The primary investigator (PI) and the team’s IBCLC-adapted MumBubConnect study texting scripts (Gallegos et al., 2014) were used to create standardized text responses addressing breastfeeding concerns women encounter during the first 6 weeks of breastfeeding. For example, nipple soreness due to the initiation of feeding during the first week, breast soreness due to engorgement occurring throughout the study, or cluster feeding in the second and third week. Biweekly, women were texted and asked about their breastfeeding experience and given five optional text responses: “happy,” “average,” “sore,” “engorged,” or “always (feeding).” The study team’s texted response provided strategies to address pain, soreness, engorgement, and if the strategies were not working, to encourage women to contact the study team or the hospital provided IBCLC (Poorman et al., 2015). If breastfeeding was going well after the first two weeks, the texts changed to an educational response to reinforce the health and cognitive benefit their infant was receiving from breastfeeding. Otherwise, the texts were focused on providing instrumental support to facilitate problem-solving and pain self-efficacy.
Educational modules and online resources.
Women were texted to access the seven 5-minute education modules via REDCap: A secure web application for building and managing online surveys and databases (https://www.project-redcap.org/), during weeks 1 and 2 of the study. Using REDCap, the study team was notified when women accessed the educational modules. Up to three reminders were sent to women to view the modules using text and email. Each module provided the women with strategies to manage breast and nipple pain. The educational modules addressed the neurophysiological basis of pain, common triggers for breast and nipple pain, breastfeeding challenges, strategies to address breast and nipple pain and other breastfeeding challenges, general lactation support, pain catastrophizing, stress reactivity, therapeutic breathing, and guided imagery. Each of the modules also provided hyperlinks to additional online resources.
Daily breastfeeding journal.
The intervention participants were provided a bound breastfeeding journal to evaluate six sessions a day of breastfeeding during weeks 1 and 2 and one session a day of breastfeeding during weeks 3, 4, 5, and 6. Each journal entry asked the participant to rate their infant’s temperament, infant latch, suction pattern, and a visual analogue scale (0–100) of breast and nipple pain for each session of breastfeeding. In addition, women assessed their infants’ breastfeeding effort using the Maternal Assessment of Infant Breastfeeding Behaviors–Revised (MAIBB-R) (Lucas et al., 2015). The systematic evaluation of their infants’ latch and suction pattern was included to facilitate women reflecting on when breast and nipple pain or breastfeeding challenges occurred and what strategy worked to resolve the challenge (Bandura, 2005). The self-reflection and self-management of these issues was designed to decrease negative coping mechanisms such as anticipatory catastrophizing of breast and nipple pain. A prepaid envelope was provided to women to return the journal after the study was completed at 6 weeks.
Control Group
Women in the control group were contacted by text at 1, 2, and 6 weeks to check their email to complete their data measures via a REDCap link. Members of the study team were notified via REDCap when women completed the data measures. Up to three text and email reminders were sent to the women to complete the data measures.
Procedure
The clinical partner at each hospital site screened for potential participants routinely during the week. Women were approached within 48 hours of delivery by a member of the study team to assess eligibility. Interested women who met eligibility criteria met with a member of the research team to provide informed consent. A written consent to participate was obtained from each participant. Following study consent, women completed baseline measures, provided their email addresses and phone numbers for the study team to follow-up. Women were randomized to the intervention or control using a computer-generated, randomization scheme generated by the study statistician (S.W.). All study personnel involved in data collection remained blinded to the group assignment of participants.
During weeks 1, 2, and 6 after discharge, a study team member texted all women to check their email to complete the study measures via REDCap link. The follow-up measures contained questions regarding breastfeeding challenges, strategies to address breast and nipple pain, social support to problem solve breastfeeding challenges and breast and nipple pain, Brief Pain Inventory (BPI), the Visual Analogue Scale (VAS) of breast and nipple pain, and the duration of breastfeeding. The study protocol followed the University of Connecticut’s REDCap recommendations for maintaining de-identified data.
Measurements
Sociodemographics.
At baseline, women completed the BRICS Demographics (NINR common data elements) including age, education, income, race/ethnicity, marital and employment status (available online at: https://cde.nlm.nih.gov/cde/search?selectedOrg=NINR).
Maternal and Infant Breastfeeding History.
General breastfeeding history, knowledge, belief, and social environment was collected by a self-report form created by the PI for earlier pilot studies (Lucas et al., 2015). Women reported their breastfeeding context factors of maternal height, weight (BMI), parity, route of delivery, history of breastfeeding, inverted or flat maternal nipples, breast surgery, chronic medical conditions, pregnancy medical condition, and mental health history. Additional information was collected on access to an IBCLC, use of a nipple shield or of a pump, and professional intervention for infant health which required artificial milk supplementation. The context factor for women’s social environment of family included a familial history of breastfeeding, family capital (income and resources), family structure (family members in the home); and infant characteristics of weight, length, gender. The IFSMT process factors collected were antenatal intention and preparation to breastfeed, and antenatal knowledge of breast and nipple pain (American Academy of Pediatrics, 2012).
Ongoing Breastfeeding Assessment Survey (OBAS).
The OBAS was adapted from a semistructured interview guide the PI created for earlier pilot studies (Lucas et al., 2015). The OBAS uses Likert-type and multiple-choice questions to obtain IFSMT breastfeeding context variable which emerged after discharge such as engorgement, breast infection and infant diagnosis of ankyloglossia (Kent et al., 2015; Lucas & McGrath, 2016). Women completed questions regarding social facilitation factors addressing paternal, familial, and social media support (friends texting, Facebook, etc.); breastfeeding knowledge and beliefs factors of maternal perception of breastfeeding experience and perception of adequate milk supply; IFSMT proximal outcomes questions measured use of nonpharmacological therapies (e.g., galactagogues, heat), frequency of breastfeeding sessions, frequency of breastfeeding management interventions; and frequency of accessing lactation healthcare professionals; and the distal outcomes of health status of breastfeeding exclusivity and duration (Ryan & Sawin, 2009).
Maternal Assessment of Infant Breastfeeding Behaviors Revised (MAIBB-R).
The MAIBB-R is the PI’s adapted version of Barnes, Lecthin, Jackson, and Shea’s (1953) (Barnes, Lethin, Jackson, & Shea, 1953)maternal self-report indicator of eight infant latch, suction, and pause patterns. Based on the results of earlier studies, the PI identified that the indicator: (a) used adultomorphic description which influenced women’s choices; (b) women combined latch and suction patterns to describe infant latch and suction patterns 30% of the time; and (c) at the time of the indicator’s development, normal milk ejection physiology was unknown and was not one of the eight descriptors (Lucas, McGrath, Diallo, & Brandon, 2016). Women who reported their infant demonstrated a vigorous suction pattern were more likely to report nipple pain (Lucas et al., 2015).
Breastfeeding Algorithm.
Based on previous pilot work, the PI adapted the LATCH scale into a maternal self-report algorithm (Jensen, Wallance, & Kelsay, 1994). The algorithm expands the LATCH scale descriptions of infant latch and sucking behaviors that might cause pain. Women evaluated infant awake/sleep state, cue of hunger (hand swipe, rooting, lip smacking), number of latch attempts, latch strength, suction strength, pattern of pauses and suction, length (minutes) of feeding, and VAS (0–100) of breast and nipple pain which occurred during breastfeeding.
Brief Pain Inventory (BPI) Short Form.
The BPI is a self-report questionnaire originally developed to assess cancer pain but is now a generic pain questionnaire. The BPI short form has nine items: two items on pain relief treatment or medication; four items about pain intensity (worst pain, least pain, average pain, pain right now); and one item on pain interference with a seven subitems (general activity, mood, walking ability, normal walk, relations with other people, sleep, and enjoyment of life). The pain relief item is scored by percentage of relief and treatment by a list of medication.
Each item on the pain intensity is rated from 0 = no pain to 10 = extreme pain. Each item on the pain interference subscale is rated from 0 = no interference to 10 = completely interferes. The pain interference scale is calculated by adding all of the seven subitem scores and dividing by 7. Both the pain severity and pain interference scores range from 0 to 10 (Cleeland, 2009). Test-retest reliability has been assessed for malignant pain and shows good reliability for pain intensity (r = 0.8) and pain interference (r = 0.8) (Poquet & Lin, 2016). The BPI has a Cronbach’s α internal consistency coefficients ranges from 0.77 to 0.91 (Cleeland, 2009; Poquet & Lin, 2016). A truncated pain interference subscale using general activity, mood, sleep, and breastfeeding, has been used to assess trauma-based and persistent breast and nipple pain (McClellan, Kent, Hepworth, Hartmann, & Geddes, 2015).
Data Analysis
Sample characteristics were described with frequencies and percentages, or means and standard deviations and continuous variables were evaluated for normality. Association of sample characteristics between BSM intervention and control groups were assessed using two sample t-test on continuous demographic variables and Pearson chi-square test to verify the nonsignificant difference of discrete characteristics.
The BPI intensity, BPI interference, and VAS of breast and nipple pain severity scales were used to measure women’s report of pain during breastfeeding at 1, 2, and 6 weeks. The BPI and VAS measures were described using, range, mean and standard deviation and two sample t-test at each timepoint were used to compare the difference of mean scores between the BSM intervention and the control groups. For those datasets without normal distribution in pain severity and BPI intensity, Box-Cox transformation was used to transform the data and meet the normality assumption of the two-sample t-test. For BPI interference, a permutation test was to normalize the empirical and normal distribution to compare the mean between the two groups. Notched boxplots and graphs with nonparametric regression smoothing line were generated for each pain measurement and their means using ggplot package in R 3.4.3. A linear mixed model (LMM) was applied on each pain measurement and a likelihood ratio test (LRT) was used to test the main effect of the BSM intervention in reducing pain in the intervention group. The model contained pain scores as dependent variables at 1, 2 and 6 weeks. The fixed covariate was baseline pain score, time, and intervention condition with subject as a random term. If the LRT show a significant main effect of the BSM intervention, then the interaction effect of BSM intervention by time was tested further. All regression analyses used lme4 package in R 3.4.3.
Results
Demographic Characteristics
Sixty-five women were recruited in the study, five women dropped out of the study before 2 weeks for a total of 60 women (27 intervention, 33 control) who completed the study. From the control group, two women stopped breastfeeding at 1 week and one woman stopped breastfeeding at 2 weeks. In comparison, in the BSM intervention group, only one woman stopped breastfeeding at 6 weeks. All women were subsequently withdrawn from study participation; however, the BSM intervention group were more likely to breastfeed to 6 weeks. There was no significant difference in demographic characteristics between women who dropped out of the study, stopped breastfeeding, or provided breastfeeding data at 1, 2, and 6 weeks. As shown in Table 1, the demographic characteristics and breastfeeding duration showed no significant difference between the BSM intervention group and the control group. Demographic characteristics of the 56 women (26 intervention, 30 control) used in the analysis reported a mean age of 30.38, (SD = 4.85) and were predominantly Caucasian (76.8%) or identified as Latina (12.5%), reported college or greater education (78.5%), income > $75,000 (66.1%), being married (66.1%), working (82.1%) and delivered vaginally (80.4). Less than half reported that this was their first child and their first experience breastfeeding (46.4%). Over half of the infants were male (57.1%).
Table 1.
Demographic Characteristics by Intervention Condition
| Characteristic | BSM (n = 26) | Control (n = 30) | Testa | ||
|---|---|---|---|---|---|
| M | SD | M | SD | p-value | |
| Age | 30.04 | 4.67 | 30.67 | 5.08 | .632 |
| n | % | n | % | ||
| Race | .910 | ||||
| White | 22 | 84.6 | 21 | 70.0 | |
| Asian | 2 | 7.7 | 1 | 3.3 | |
| Black or African American | 2 | 7.7 | 4 | 13.3 | |
| Not reported | 0 | 0.0 | 4 | 13.3 | |
| Ethnicity | .967 | ||||
| Hispanic or Latino | 3 | 11.5 | 4 | 13.3 | |
| Not Hispanic or Latino | 20 | 76.9 | 23 | 76.7 | |
| Unknown or Not Reported | 3 | 11.5 | 3 | 10.0 | |
| Education | .680 | ||||
| High school or below | 6 | 23.1 | 6 | 20.2 | |
| College | 10 | 38.5 | 15 | 50.0 | |
| Graduate School | 10 | 38.5 | 9 | 30.0 | |
| Family Income | .889 | ||||
| Less than $50,000 | 6 | 23.0 | 8 | 26.7 | |
| $51,000 - $75,000 | 3 | 11.5 | 2 | 6.7 | |
| $76,000 - $100,000 | 8 | 30.8 | 8 | 26.7 | |
| Greater than $100,000 | 9 | 34.6 | 12 | 40.0 | |
| Marital Status | .992 | ||||
| Single | 8 | 30.8 | 9 | 30.0 | |
| Married | 17 | 65.4 | 20 | 66.7 | |
| Not Reported | 1 | 3.8 | 1 | 33.3 | |
| Working (Yes) | 20 | 76.9 | 26 | 86.7 | .343 |
| # of BF (1 = Yes) | 11 | 42.3 | 15 | 50.0 | .565 |
| Parity (1 = Yes) | 10 | 38.5 | 13 | 43.3 | .717 |
| Gender of Infant (Male) | 13 | 50.0 | 19 | 63.3 | .315 |
| Delivery (Vaginal) | 20 | 76.9 | 25 | 83.3 | .547 |
| Breastfeeding Duration (n=60 for total sample) | |||||
| 1 Week | 27 | 100 | 31 | 93.9 | .497* |
| 2 Weeks | 27 | 100 | 30 | 90.9 | .245 |
| 6 Weeks | 26 | 96 | 30 | 90.9 | .620 |
Note.
Two sample t-test for continuous demographics variables,.
Pearson chi-square for discrete demographic variables, Fisher’s exact test for breastfeeding duration.
Pain Measurements Over Time Between Groups
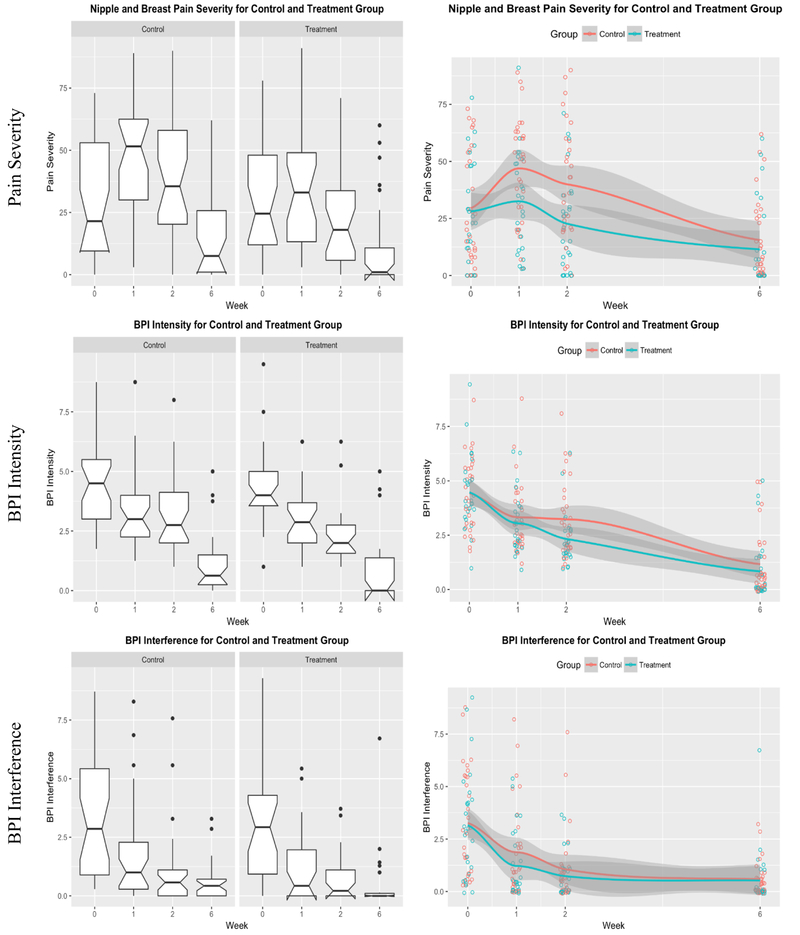
The mean and standard deviation of the VAS breast and nipple pain scale, and BPI intensity and interference measures are reported in Supplement Table 1. There were significant differences in reported pain measurements between the two groups at several timepoints. In the BSM intervention group, women reported significantly lower breast and nipple pain severity at week 1 (p = .014) and week 2 (p = .006) and for BPI intensity at week 2 (p = .029). No significant difference for BPI interference was found at any timepoint.
The pain measurement trends for the breast and nipple pain severity and BPI intensity were graphed and nonparametric regression plots (Figure 2). In the nonparametric regression plots, the predicted pain measurement mean and confidence interval are graphed. The nipple and breast pain severity scores for both groups peaked at week 1 and decreased afterwards and were compared using a two sample t-test conditions. There was a significant difference in the breast and nipple pain mean scores for the control group were 47.0 (SD = 22.7) and BSM intervention group were 32.5 (SD = 21.7), p < 0.014 at 1 week, and at 2 weeks, the control groups mean scores were 40.0 (SD = 25.3) and BSM intervention were 22.7 (SD = 21.0), p < 0.006. At 2 weeks, the BPI intensity mean scores by the control group were 3.23 (SD = 1.78) and the BSM intervention groups mean scores were 2.33 (SD = 1.20), p < 0.029 (Figure 2 and Supplement Table 1). For the BPI interference scores, there was no significant difference between groups at any timepoint.
Figure 2.
Graphs of Pain Measurements between Groups
Linear Mixed Model of Pain Measurements
Table 2 presents the findings of the LRT between the model with BSM intervention and the model without the BSM intervention with each pain measurement. If the main effect of the BSM intervention is significant, then the interaction term of the intervention by time was tested. For the breast and nipple pain findings, the BSM intervention had a significant main effect (p = .014) and interaction effect of reported pain severity by time (p = .005). The estimated coefficient of BSM intervention group is −14.17 which means the BSM group reported 14.17 less breast and nipple pain compared to the control group (Table 3). The BSM intervention reduced pain severity the greatest at week 1 and week 2 with decreasing effect in week 6. However, no significant main effect was found for general pain as measured by the BPI intensity (p = .088) and BPI interference (p = .271).
Table 2.
LRT p-value for different Pain Measurements
| Pain Measurement | LRT p-value of main effect | LRT p-value of interaction term of BSM intervention by time |
|---|---|---|
| Nipple and Breast Pain Severity | .0136 | .0051 |
| BPI Intensity | .0884 | |
| BPI Interference | .2714 |
Note. LRT = Likelihood Ratio Test
Table 3.
Estimated Coefficients of Pain Severity Model
| Fixed Covariate | Estimate | Std. Error |
|---|---|---|
| Intercept | 41.58 | 4.75 |
| Baseline pain severity | 0.18 | 0.10 |
| Week 2 | −7.00 | 3.60 |
| Week 6 | −31.43 | 3.60 |
| BSM Intervention Group | −14.17 | 5.52 |
| Week 2 BSM Intervention Group | −2.84 | 5.28 |
| Week 6 BSM Intervention Group | 10.36 | 5.28 |
Discussion
The BSM intervention positively affected women’s self-report of breast and nipple pain during the early stages of breastfeeding when the rate of breastfeeding cessation is typically highest. In addition to reducing breast and nipple pain, women reported lower general pain compared to the control group at 2 weeks postpartum. However, in comparison to the control group, the intervention did not significantly increase breastfeeding duration.
The BSM intervention utilizing a text-based communication module, targeting the behavior change of decreasing pain and sustaining breastfeeding duration was effective. Text-based intervention studies are effective for providing reminders for infant vaccination, managing diabetes, healthy eating, and weight management (Kao & Liebovitz, 2017; McCarroll, Eyles, & Ni Mhurchu, 2017; Overdijkink et al., 2018). For women participating in interventions to sustain breastfeeding duration, studies using text-based communication is reported as supportive, but not invasive (Gallegos et al., 2014; Poorman et al., 2015). We found both groups follow-up on the text to complete study measures study using the REDCap interface. However, women were less likely to complete or use the paper-based journal and we were not able to obtain daily assessment of breast and nipple pain. Based on their positive responses to texting, in future studies we will adapt the paper journal to a text-based, daily breastfeeding algorithm. The texted-based intervention was also effective in following up with women who identified concerns with breastfeeding and accessing lactation healthcare professionals.
The importance of breastfeeding is well understood and yet breastfeeding cessation has not been evaluated through a lens of precision health. Each woman has a unique clinical history and personal report for continuing or ceasing breastfeeding. For women struggling with breastfeeding challenges and breast and nipple pain, preventive care that identifies the triggers for breast and nipple pain but also integrates knowledge of a women’s genetic predisposition for chronic pain could lead to the development of more personalized interventions. Women’s mental health of depression, anxiety, fatigue, and sleep deprivation also influence their ability to self-regulate their behaviors and manage their breast and nipple pain (Brown, Rance, & Bennett, 2016; Stuebe, Grewen, & Meltzer-Brody, 2013). Future analysis will evaluate participants who had continuing pain associated with issues with latch, underlying medical issues, differences in somatosensory status or the presence of a genetic polymorphisms that place the women at risk for continuing pain.
Women in the BSM intervention group also reported a significant reduction in general postpartum pain at week 2 after giving birth. The nonpharmacological management of pain using cognitive behavioral therapy has not been explored specifically for postpartum pain (Kainu, Halmesmäki, Korttila, & Sarvela, 2016). Several recent reports have presented the management of postpartum, breast and nipple pain with an emphasis on pharmacological interventions (ACOG, 2018; Berens, Eglash, Malloy, & Steube, 2016). Each of these reports do not incorporate the importance of nonpharmacological interventions and effect of targeted support of health behavior. In our study, several women reported other areas of the body where they were experiencing pain. Their pain scores were significantly reduced in the intervention group. Our future larger study will also include overall generalized postpartum pain (Declercq, Sakala, Corry, Applebaum, & Herrlich, 2014).
The generalizability of the pilot RCT is limited due to the small sample size. The strong positive trends and receptive response to the text-based intervention merits a larger study. A therapeutic study based on texting seems to be positive to women, where there is limited participant burden of a face-to-face interaction or travel to a lactation professional, and yet women do not feel alone during the first few weeks at home.
Limitations
Although women reported the type of analgesic, anti-inflammatory or nonpharmacological intervention they were using during the study, we did not ask dosages or frequency and could not include this variable in the study analysis. Based on the pilot study, we identified that our baseline data collection protocol was perceived as intensive to women and clinical staff. In future studies, we will need to prioritize our baseline and weekly measures to decrease participant burden. We plan to work closely with the clinical staff to coordinate clinical care with data collection to decrease the time burden for participants, clinical staff, and our study team.
Conclusion
The results of this randomized controlled pilot study support a positive effect of the BSM intervention on decreasing breast and nipple pain among breastfeeding women, particularly over the first few weeks when the rate of cessation is typically highest. Women responded positively to the text-based communication and educational modules, which is a less time intensive and costly therapeutic intervention than face-to-face contact. Future study needs to replicate this study in a larger population to verify the clinical significance of this intervention and to expand the evaluation of pain by including postpartum pain assessment.
Supplementary Material
Supplement Figure 1. Model of Breast and Nipple Pain Self-Management. Adapted from Individual and Family Self-Management Theory, by P. A. Ryan and K. J. Sawin retrieved from www.nursing.uwm.edu/smsc. Copyright 2009, 2014 by Ryan and Sawin. Adapted with permission.
Supplement Table 1. Pain Measurements Comparison between Groups
Acknowledgement:
Research reported in this publication was supported by the National Institute of Nursing Research of the National Institutes of Health (NIH-NINR), Grant number: NIH-NINR P20NR016605. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The authors thank Dr. Deborah McDonald, RN, PhD, for her support and advice.
Footnotes
The authors have no conflicts of interest to report.
Ethical Conduct of Research: The authors confirm that any aspects of the work reported in this manuscript has been conducted by the ethical conduct of research and approved by the University of Connecticut Institutional Review Board.
Clinical Trial Registration: The study was registered with Clinical Trials.gov (NCT03392675). Data were collected from April 2017 to November 2017. https://clinicaltrials.gov/ct2/.
Contributor Information
Ruth Lucas, University of Connecticut School of Nursing.
Yiming Zhang, University of Connecticut Department of Statistics.
Stephen J. Walsh, University of Connecticut School of Nursing, Storrs, CT..
Heather Evans, School of Interdisciplinary Health & Science, Department of Nursing, University of Saint Joseph, West Hartford, CT.
Erin Young, University of Connecticut School of Nursing, Storrs, CT..
Angela Starkweather, University of Connecticut School of Nursing, Storrs, CT..
References
- ACOG. (2018). ACOG committee opinion No. 742: Postpartum pain management. Obstetrics & Gynecology, 132(1), e35–e43. 10.1097/AOG.0000000000002683 [DOI] [PubMed] [Google Scholar]
- American Academy of Pediatrics. (2012). Breastfeeding and the use of human milk. Pediatrics, 129(3), e827–e841. 10.1542/peds.2011-3552 [DOI] [PubMed] [Google Scholar]
- Amir LH, Jones LE, & Buck ML (2015). Nipple pain associated with breastfeeding: Incorporating current neurophysiology into clinical reasoning. Australian Family Physician, 44(3), 127–132. [PubMed] [Google Scholar]
- Bandura A (2005). The primacy of self regulation in health promotion. Applied Psychology: An International Review, 54(2), 245–254. [Google Scholar]
- Barnes G, Lethin A, Jackson E, & Shea N (1953). Management of breast feeding. JAMA : The Journal of the American Medical Association, 151(3), 192–199. [PubMed] [Google Scholar]
- Bartick M, & Reinhold A (2010). The burden of suboptimal breastfeeding in the United States: A pediatric cost analysis. Pediatrics, 125(5), e1048–e1056. 10.1542/peds.2009-1616 [DOI] [PubMed] [Google Scholar]
- Berens P, Eglash A, Malloy M, & Steube AM (2016). ABM clinical protocol #26: persistent pain with breastfeeding. Breastfeeding Medicine, 11(2), 46–53. 10.1089/bfm.2016.29002.pjb [DOI] [PubMed] [Google Scholar]
- Billingham SAM, Whitehead AL, & Julious SA (2013). An audit of sample sizes for pilot and feasibility trials being undertaken in the United Kingdom registered in the United Kingdom Clinical Research Network database. BMC Medical Research Methodology, 13(1), 1 10.1186/1471-2288-13-104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bobiński R, Mikulska M, Mojska H, & Simon M (2013). Comparison of the fatty acid composition of transitional and mature milk of mothers who delivered healthy full-term babies, preterm babies and full-term small for gestational age infants. European Journal of Clinical Nutrition, 67(9), 966–971. 10.1038/ejcn.2013.96 [DOI] [PubMed] [Google Scholar]
- Brown A, Rance J, & Bennett P (2016). Understanding the relationship between breastfeeding and postnatal depression: The role of pain and physical difficulties. Journal of Advanced Nursing, 72(2), 273–282. 10.1111/jan.12832 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for Disease Control. (2018). Breastfeeding Report Card. Retrieved from https://www.cdc.gov/breastfeeding/data/reportcard.htm
- Center for Disease Control and Prevention. (2018). Breastfeeding among U.S. children born 2009–2015, CDC National Immunization Survey. [Google Scholar]
- Cleeland CS (2009). The Brief Pain Inventory User Guide. The Brief Pain Inventory, 3–4. Retrieved from http://www.mdanderson.org/education-and-research/departments-programs-and-labs/departments-and-divisions/symptom-research/symptom-assessment-tools/BPI_UserGuide.pdf [Google Scholar]
- Davis MC, Zautra AJ, Wolf LD, Tennen H, & Yeung EW (2015). Mindfulness and cognitive–behavioral interventions for chronic pain: Differential effects on daily pain reactivity and stress reactivity. Journal of Consulting and Clinical Psychology, 83(1), 24–35. 10.1037/a0038200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Declercq E, Sakala C, Corry M, Applebaum S, & Herrlich A (2014). Major Survey Findings of Listening to Mothers III: Pregnancy and Birth. Journal of Perinatal Education, 23(1), 9–16. 10.1891/1058-1243.23.1.9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erdfelder E, Faul F, & Buchner A (1996). GPOWER: A General Power Analysis Program. Behavior Researh Methods, Instruments, & Computers, 28, 1–11. [Google Scholar]
- Fox S, & Duggan M (2012). Mobile Health 2012 Pew Internet: Washington, D.C., 29 Retrieved from http://www.pewinternet.org/~/media//Files/Reports/2012/PIP_MobileHealth2012_FINAL.pdf [Google Scholar]
- Gallegos D, Russell-Bennett R, Previte J, & Parkinson J (2014). Can a text message a week improve breastfeeding? BMC Pregnancy and Childbirth, 14(1), 374 10.1186/s12884-014-0374-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gardner AS, Rahman IA, Lai CT, Hepworth A, Trengove N, Hartmann PE, & Geddes DT (2017). Changes in fatty acid composition of human milk in response to cold-like symptoms in the lactating mother and infant. Nutrients, 9(9), 1034 10.3390/nu9091034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jensen D, Wallance S, & Kelsay P (1994). LATCH: A breastfeeding charting system and documentation tool. JOGNN - Journal of Obstetric, Gynecologic, and Neonatal Nursing, 23(1), 27–32. [DOI] [PubMed] [Google Scholar]
- Kainu JP, Halmesmäki E, Korttila KT, & Sarvela PJ (2016). Persistent pain after cesarean delivery and vaginal delivery: A prospective cohort study. Anesthesia and Analgesia, 123(6), 1535–1545. 10.1213/ANE.0000000000001619 [DOI] [PubMed] [Google Scholar]
- Kao CK, & Liebovitz DM (2017). Consumer mobile health apps: Current state, barriers, and future directions. PM and R, 9(5), S106–S115. 10.1016/j.pmrj.2017.02.018 [DOI] [PubMed] [Google Scholar]
- Kent JC, Ashton E, Hardwick CM, Rowan MK, Chia ES, Fairclough KA, … Geddes DT (2015). Nipple pain in breastfeeding mothers: Incidence, causes and treatments. International Journal of Environmental Research and Public Health, 12(10), 12247–12263. 10.3390/ijerph121012247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khan S, Hepworth AR, Prime DK, Lai CT, Trengove NJ, & Hartmann PE (2013). Variation in fat, lactose, and protein composition in breast milk over 24 hours: Associations with infant feeding patterns. Journal of Human Lactation, 29(1), 81–89. 10.1177/0890334412448841 [DOI] [PubMed] [Google Scholar]
- Litt MD, & Tennen H (2015). What are the most effective coping strategies for managing chronic pain? Pain Management, 5(6), 403–406. 10.2217/pmt.15.45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lucas RF, Judge M, Sajdlowska J, Cong X, Mcgrath JM, & Brandon D (2015). Effect of maternal body mass index on infant breastfeeding behaviors and exclusive direct breastfeeding. JOGNN - Journal of Obstetric, Gynecologic, and Neonatal Nursing, 44(6), 772–783. 10.1111/1552-6909.12755 [DOI] [PubMed] [Google Scholar]
- Lucas RF, & McGrath JM (2016). Clinical assessment and management of breastfeeding pain. Topics in Clinical Nutrition, 32(3), 1–12. [Google Scholar]
- Lucas RF, McGrath JM, Diallo A, & Brandon D (2016). Validating the Maternal Assessment of Breastfeeding Behaviors Instrument - Revised (MAIBB-R) using maternal narrative of their infants’ latch and sucking patterns In International Congress of Infant Studies. New Orleans, LA. [Google Scholar]
- McCann MF, Baydar N, & Williams RL (2007). Breastfeeding attitudes and reported problems in a national sample of WIC participants. Journal of Human Lactation, 23(4), 314–324. 10.1177/0890334407307882 [DOI] [PubMed] [Google Scholar]
- McCarroll R, Eyles H, & Ni Mhurchu C (2017). Effectiveness of mobile health (mHealth) interventions for promoting healthy eating in adults: A systematic review. Preventive Medicine, 105(August), 156–168. 10.1016/j.ypmed.2017.08.022 [DOI] [PubMed] [Google Scholar]
- McClellan HL, Kent JC, Hepworth AR, Hartmann PE, & Geddes DT (2015). Persistent nipple pain in breastfeeding mothers associated with abnormal infant tongue movement. International Journal of Environmental Research and Public Health, 12(9), 10833–10845. 10.3390/ijerph120910833 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morland-Schultz K, & Hill PD (2005). Prevention of and therapies for nipple pain: A systematic review. Journal of Obstetric, Gynecologic & Neonatal Nursing, 34(4), 428–437. 10.1177/0884217505276056 [DOI] [PubMed] [Google Scholar]
- Overdijkink SB, Velu AV, Rosman AN, Van Beukering MDM, Kok M, & Steegers-Theunissen RPM (2018). The usability and effectiveness of mobile health technology-based lifestyle and medical intervention apps supporting health care during pregnancy: Systematic review. JMIR Mhealth Uhealth, 6(4), e109 10.2196/mhealth.8834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poorman E, Gazmararian J, Parker RM, Yang B, & Elon L (2015). Use of text messaging for maternal and infant health: A systematic review of the literature. Maternal and Child Health Journal, 19(5), 969–989. 10.1007/s10995-014-1595-8 [DOI] [PubMed] [Google Scholar]
- Poquet N, & Lin C (2016). The Brief Pain Inventory (BPI). Journal of Physiotherapy, 62(1), 52 10.1016/j.jphys.2015.07.001 [DOI] [PubMed] [Google Scholar]
- Ryan P, & Sawin KJ (2009). The Individual and Family Self-Management Theory: Background and perspectives on context, process, and outcomes. Nursing Outlook, 57(4), 217–225.e6. 10.1016/j.outlook.2008.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sikander S, Maselko J, Zafar S, Haq Z, Ahmad I, Ahmad M, … Rahman A (2015). Cognitive-behavioral counseling for exclusive breastfeeding in rural pediatrics: A cluster RCT. Pediatrics, 135(2), e424–e431. 10.1542/peds.2014-1628 [DOI] [PubMed] [Google Scholar]
- Smith CA, Levett KM, Collins CT, & Crowther CA (2011). Relaxation techniques for pain management in labour. Cochrane Database of Systematic Reviews (Online), 12(12), CD009514 10.1002/14651858.CD009514 [DOI] [PubMed] [Google Scholar]
- Spinelli MG, Endicott J, & Goetz RR (2013). Increased breastfeeding rates in black women after a treatment intervention. Breastfeeding Medicine, 8(6), 479–484. 10.1089/bfm.2013.0051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stuebe AM, Grewen K, & Meltzer-Brody S (2013). Association between maternal mood and oxytocin response to breastfeeding. Journal of Women’s Health, 22(4), 352–361. 10.1089/jwh.2012.3768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor BL, Cavanagh K, & Strauss C (2016). The effectiveness of mindfulness-based interventions in the perinatal period: A systematic review and meta-analysis. PLoS ONE, 11(5), 1–30. 10.1371/journal.pone.0155720 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagner EA, Chantry CJ, Dewey KG, & Nommsen-Rivers LA (2013). Breastfeeding Concerns at 3 and 7 Days Postpartum and Feeding Status at 2 Months. Pediatrics, 132(4), e865–e875. 10.1542/peds.2013-0724 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplement Figure 1. Model of Breast and Nipple Pain Self-Management. Adapted from Individual and Family Self-Management Theory, by P. A. Ryan and K. J. Sawin retrieved from www.nursing.uwm.edu/smsc. Copyright 2009, 2014 by Ryan and Sawin. Adapted with permission.
Supplement Table 1. Pain Measurements Comparison between Groups