Abstract
Introduction:
Oil spill response and cleanup (OSRC) workers had potentially stressful experiences during mitigation efforts following the 2010 Deepwater Horizon disaster. Smelling chemicals; skin or clothing contact with oil; heat stress; handling oily plants/wildlife or dead animal recovery; and/or being out of regular work may have posed a risk to worker respiratory health through psychological stress mechanisms.
Objective:
To evaluate the association between six potentially stressful oil spill experiences and lung function among OSRC workers 1-3 years following the Deepwater Horizon disaster, while controlling for primary oil spill inhalation hazards and other potential confounders.
Methods:
Of 6,811 GuLF STUDY participants who performed OSRC work and completed a quality spirometry test, 4,806 provided information on all exposures and confounders. We carried out complete case analysis and used multiple imputation to assess risk among the larger sample. Potentially stressful work experiences were identified from an earlier study of these workers. The lung function parameters of interest include the forced expiratory volume in 1 second (FEV1, mL), the forced vital capacity (FVC, mL) and the ratio (FEV1/FVC, %).
Results:
On average, participants in the analytic sample completed spirometry tests 1.7 years after the spill. Among workers with at least 2 acceptable FEV1 and FVC curves, workers with jobs that involved oily plants/wildlife or dead animal recovery had lower values of FEV1 (Mean difference: −53 mL, 95% CI: −84, −22), FVC (Mean difference: −45 mL, 95% CI: −81, −9) and FEV1/FVC (Mean difference: −0.44%, 95% CI: −0.80, −0.07) compared to unexposed workers in analyses using multiple imputation.
Conclusions:
Workers involved in handling oily plants/wildlife or dead animal recovery had lower lung function than unexposed workers after accounting for other OSRC inhalation hazards.
Keywords: Lung function, spirometry, nonchemical stressors, oil spill, Deepwater Horizon
Introduction
Tens of thousands of oil spill response and cleanup (OSRC) workers performed activities offshore and on land in the US Gulf of Mexico and adjacent states to help mitigate the environmental impacts of the 2010 Deepwater Horizon (DWH) disaster [1]. During the oil spill mitigation effort, OSRC workers were exposed to mental health stressors [2, 3] and chemical and physical hazards [2, 4]. OSRC workers smelled oil chemicals, had skin or clothing contact with oil/tar/oily water, handled oily plants/wildlife or dead animal recovery, worked under physically demanding conditions such as high heat [2], and faced disruption of regular work due to the closure of coastal fisheries during and after the disaster [3, 5]. Specific OSRC work experiences may have induced psychological stress or related adverse mental health sequelae [3] posing a risk to workers’ respiratory health.
Psychological stress can induce neuroendocrine-induced immunological changes that can lead to inflammation and bronchoconstriction [6-8] and has been linked to adverse respiratory outcomes including reduced lung function. In a general population setting, exposure to trauma and post-traumatic stress disorder has been associated with reduced lung function, asthma, and COPD [9]. In disaster settings, post-traumatic stress disorder was associated with asthma symptoms among first responders of the World Trade Center terrorist attack and incident asthma among older adults exposed to war-related stressors [10-12].
Adverse mental health outcomes have been observed in communities affected by prior oil spills including Exxon Valdez [13, 14], Sea Empress [15, 16], Hebei Spirit [17], and Prestige [18]. Adverse mental health outcomes have also been observed among affected communities following the DWH disaster, and is associated with being a coastal fisher [19] as well as with disruption of participants’ lives, work, family and social engagements [20]. Additionally, increased prevalence of depression and post-traumatic stress symptoms were associated with specific experiences among DWH OSRC workers. These experiences included smelling chemicals; stopping work due to heat; and working as a commercial fisher before the spill [3].
Prior studies also have identified adverse respiratory health in relation to oil spill work exposures. Transient lung function decrements were also identified in oil spill cleanup workers following the Tasman Spirit but were not identified at 1-year follow up [21]. After the Prestige oil spill, although lung function was not found to be associated with cleanup work, markers of lung inflammation were elevated in exposed versus unexposed among non-smokers 2 years after the spill [22]. We previously examined associations between primary inhalation hazards and lung function 1-3 years following the DWH disaster [23, 24]. Among workers, lung function was inversely associated with high potential exposure to burning oil/gas and decontamination work [23], but was not associated with ordinal estimates of total hydrocarbons (THC) levels, used as a general marker of oil spill chemical exposures [24]. Although prior studies suggest acute adverse respiratory health outcomes, none have explored risks unique to DWH OSRC work experiences that may have been stressful. The objective of this study is to evaluate the relationship between six previously identified unique oil spill experiences [3] and lung function among OSRC workers 1-3 years following the 2010 DWH disaster, while accounting for other indicators of chemical exposures from the spill.
Methods
Study design and population
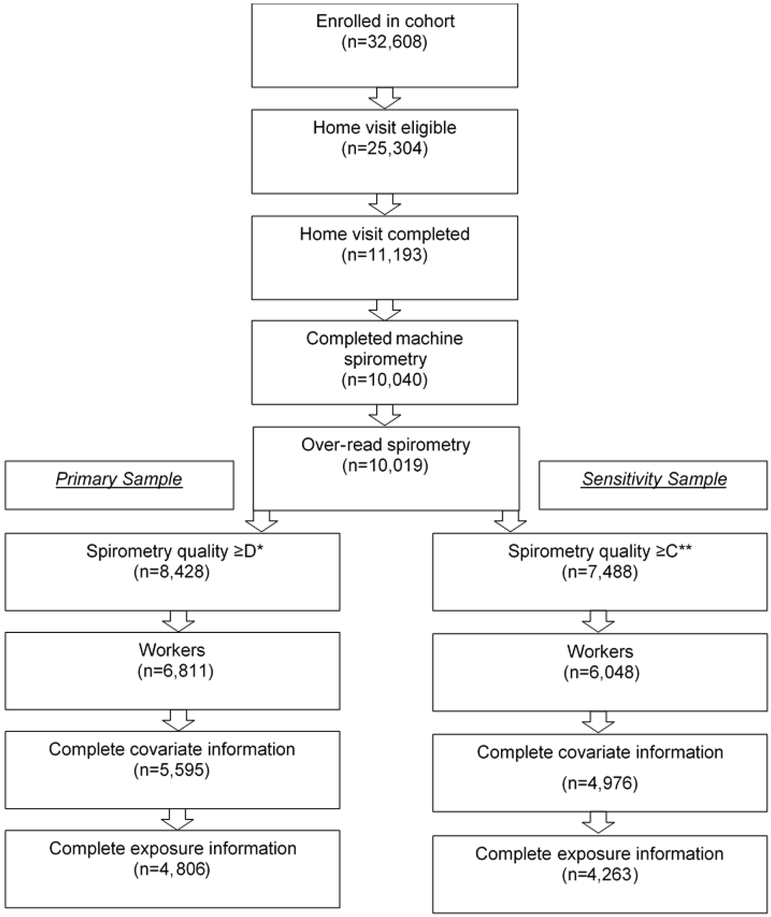
The Gulf Long-Term Follow-up Study (GuLF STUDY), is a large prospective cohort study of the health effects of the DWH disaster. The study includes 32,608 adults who participated in the oil spill response and cleanup (workers) or received safety training but did not work (non-workers) [25, 26]. All participants were first administered an enrollment questionnaire by telephone (March 2011-May 2013). During enrollment, participants who worked at least 1 day on any OSRC activity (workers) provided work histories detailing OSRC jobs and tasks. A subgroup of participants who lived in a US Gulf state (Alabama, Louisiana, Mississippi, Florida, or Texas) and spoke English or Spanish were eligible for a home visit (N=25,304). During the home visit (May 2011-May 2013) examiners coached participants (N=11,193) to perform spirometry and collected anthropometric measurements including height and weight. Participants also completed an additional questionnaire that collected more detail on OSRC and other work history information, demographics, lifestyle, and health. Of the 10,040 home visit participants who completed a spirometry test, 10,019 received expert over-reading scores. Our primary analysis included those who met spirometry quality criteria (see Lung function) and had complete information on exposures and covariates (N=4,806) (Figure 1).
Figure 1.
Participant eligibility.
*Spirometry quality≥D: 2 acceptable curves with no reproducibility requirement.
**Spirometry quality ≥C: 3 acceptable curves with ≤150 mL between the highest and second highest curves or equivalent as deemed by pulmonary function expert.
*n=1 participant has an FVC of 26 mL so we excluded this curve and assigned the participants next highest curve
Ethical approval
The Institutional Review Board of the National Institute of Environmental Health Sciences approved the study procedures. Home visit participants provided written informed consent.
Lung function
Our analysis focused on OSRC workers as the exposures of interest were only relevant to those who worked at least one day in response and cleanup efforts following the disaster. Ultrasonic spirometers were used to collect the lung function measurements (Easy on-PC; ndd Medical Technologies, Andover, MA). Participants were seated with a nose-clip and performed spirometry until they achieved either three acceptable or a maximum of eight maneuvers. To increase data quality control, an expert reviewed machine-read spirometry quality scores. The expert was able to recover valid spirometry tests that were excluded by a stricter computer interpretation of quality criteria. We defined meeting quality spirometry two ways: Those with spirometry quality ≥ D defined as two FEV1 and two FVC curves that met within-maneuver acceptability criteria and those with spirometry quality ≥ C defined as three acceptable curves with ≤150 mL difference between the largest and second largest curve for FEV1 or FVC or those deemed to have met comparable spirometry quality based on over-reading expert review [27]. We used the former definition to maximize sample size and to address potential selection bias and the latter stricter definition to determine whether using the less-strict definition of quality affected point estimates and 95% confidence intervals. Measures of lung function included the forced expiratory volume in 1 second (FEV1; mL), the forced vital capacity (FVC; mL), and the ratio (FEV1/FVC%). For each participant, we analyzed the best FEV1 curve and best FVC curve among available acceptable curves. Following American Thoracic Society/European Respiratory Society standards, we calculated the FEV1/FVC ratio from these parameters.
Oil spill response and cleanup experiences
We assessed six oil spill experiences that were previously identified as potentially stressful and examined in relation to mental health outcomes (Supplemental Figure 1) [3]. Oil spill experiences were derived from the enrollment and home visit questionnaires. Participants were defined as exposed if they responded positively to the related question on ever participated in the particular DWH spill-related experience, and unexposed if they responded negatively to the same question. These experiences included jobs that involved smelling chemicals; skin or clothing contact with oil/tar/oily water; body or clothing ever became wet with chemicals; ever had to stop working because of heat; and worked any job involving oily plants/wildlife or dead animal recovery; and potentially being out of regular work. Participants were classified separately for each oil spill experience, such that participants could be classified as exposed for one experience and unexposed for another.
Covariates
Potential confounders were selected based on a minimally sufficient adjustment set from a directed acyclic graph that was previously described [23]. Considerations of inclusion of basic adjustments for lung function (gender, race, ethnicity, age, height, and height squared) were based on prior literature describing spirometric reference values for US adults [28]. Body mass index was required to meet the adjustment set, so we included weight because height squared was already included in the model. All study participants were asked questions about demographics, lifestyle, and health during the telephone enrollment interview and home visit. Identified confounders included: age at home visit (years), height (inches), height2, weight (pounds), gender (male, female), Hispanic ethnicity (yes, no), race (white, black, other), annual household income (less than or equal to $20,000, $20,001 to $50,000, more than $50,000), highest level of educational attainment (<high school/equivalent, high school diploma/General Education Diploma, some college/2 year degree, 4 year college graduate or more), employment status at the time of enrollment (employed, unemployed, other), pre-spill lung disease (bronchitis, asthma, or emphysema) (yes, no), pre-spill diabetes (yes, no), previous oil industry experience (yes, no), previous oil spill cleanup work (yes, no), residential proximity to the US Gulf Coast (living on a coastal county, living adjacent to a coastal county, other Gulf state residence), smoking status at enrollment (never, former, light current (<20 cigarettes/day), heavy current (≥20 cigarettes/day)), and exposure to passive smoke at the time of the home visit defined as having a regular smoker in the home (yes, no).
Statistical Analysis
We calculated frequencies and percentages for dichotomous and categorical variables and means and standard deviations for continuous variables. We used multivariable linear regression models to estimate adjusted mean differences and 95% confidence intervals in FEV1 (mL), FVC (mL), and FEV1/FVC (%) between exposed and unexposed groups, for each oil spill experience. We adjusted for identified confounders as well as other OSRC chemical exposures. To adjust for THC exposures, we categorized the maximum ordinal estimated THC exposure level across all jobs held as: ≤0.29 ppm; 0.30-0.99 ppm; 1.00-2.99 ppm; ≥3.00 ppm [29]. To adjust for burning oil/gas (none, low/medium, high) and dispersant exposures (no, yes), we used self-reported data from work histories that were classified by industrial hygienists [29]. We calculated Spearman’s correlation coefficients to examine correlations among the six potentially stressful oil spill experiences and among the OSRC work inhalation exposures.
We conducted a complete case analysis among workers with complete information on exposure and confounders. In our primary analytic sample, 30% of participants were excluded due to missing information on either exposures or the model covariates. To address potential bias that could arise from excluding these participants, we analyzed associations among OSRC workers with data imputed for missing exposure and covariates [30, 31]. Multiple imputation was conducted 10 times using the fully conditioned specification (FCS) [32]. Models used to impute missing covariates included all exposure, outcome, and covariates terms in the multivariable models. Statistical analyses were conducted in SAS 9.4 (Cary, NC).
Sensitivity analyses
We performed several sensitivity analyses to address potential bias and assess effect modification in our sample. To assess the impact of using the above less-strict spirometry quality definition, we repeated complete case and imputed analyses among those who met stricter quality spirometry of ≥C (N=4,263; N=6,048, respectively). We repeated analyses among those without pre-spill lung disease (N=4,151) to determine the impact of having included participants with prior lung disease. Separately, we examined associations among OSRC workers with no previous oil industry or oil spill cleanup experience (N=3,716) because these workers might experience greater stress in response to seeing and smelling oil. We also repeated analyses restricted to never-smokers (N=2,010) to assess potential bias from residual confounding by smoking status. We explored effect measure modification by gender to test potential differences in physiologic responses to environmental stressors suggested in prior research [33, 34]. We also stratified by time elapsed between participants’ last day of OSRC work and spirometry test to assess whether any lung function differences were stronger closer in time to spill exposures. Finally, we evaluated individual interview items that comprised the experience of handling oily plants/wildlife or dead animal recovery by separately estimating the effect of performing tasks related to handling plants (“Did you cut, collect, or put oily plants, sargassum weed or grass, or garbage into bags or containers for disposal?”) and handling wildlife (“Did you handle any wildlife, whether alive or dead, during the cleanup?”) to further explore the impact of witnessing environmental degradation.
Results
Selected population characteristics among OSRC workers with a spirometry quality score of ≥ D are presented in Table 1. The analytic sample was predominately men (80%), Non-Hispanic (94%), and white (54%). Thirty-nine percent of participants had an annual household income less than or equal to $20,000 per year. Correlation coefficients among the oil experiences or among exposures were generally low (−0.01-0.36) (Supplemental Table 1 and 2).
Table 1.
Selected population characteristics of oil spill response and cleanup workers with ≥D spirometry quality scores* (N=4,806)
| Characteristic | Mean (SD) |
|---|---|
| Age, years | 43 (13) |
| Height, m | 1.74 (0.09) |
| Weight, kg | 91 (21) |
| Time elapsed between last day of OSRC work and spirometry, years | 17 (0.5) |
| FEV1, mL | 3,197 (791) |
| FVC, mL | 4,084 (955) |
| FEV1/FVC% | 78.31 (7.08) |
| N (%) | |
| Gender | |
| Male | 3867 (80) |
| Female | 939 (20) |
| Hispanic ethnicity | |
| Non-Hispanic | 4496 (94) |
| Hispanic | 310 (6) |
| Race | |
| White | 2614 (54) |
| Black | 1701 (35) |
| Asian/Other | 491 (10) |
| Annual household income | |
| More than $50,000 | 1264 (26) |
| $20,001 to $50,000 | 1666 (35) |
| Less than or equal to $20,000 | 1876 (39) |
| Highest level of educational attainment | |
| 4-Year College Graduate or More | 619 (13) |
| Some College/2-Year Degree | 1537 (32) |
| High School Diploma/GED | 1710 (36) |
| Less than High School/Equivalent | 940 (20) |
| Employment at the time of enrollment | |
| Employed | 2672 (56) |
| Unemployed/looking for work | 1325 (28) |
| Other | 809 (17) |
| Pre-spill lung disease | |
| No | 4151 (86) |
| Yes | 655 (14) |
| Pre-spill diabetes | |
| No | 4560 (95) |
| Yes | 246 (5) |
| Previous oil industry experience | |
| No | 3976 (83) |
| Yes | 830 (17) |
| Previous oil spill cleanup experience | |
| No | 4406 (92) |
| Yes | 400 (8) |
| Residential proximity to the Gulf Coast† | |
| Direct contact | 3503 (73) |
| Indirect contact | 337 (7) |
| Other Gulf state residence | 966 (20) |
| Smoking status at enrollment | |
| Never smoker | 2010 (42) |
| Former smoker | 949 (20) |
| Light current smoker | 1223 (25) |
| Heavy current smoker | 624 (13) |
| Secondhand smoke at home visit | |
| No | 3356 (70) |
| Yes | 1450 (30) |
| Maximum ordinal total hydrocarbons (THC) level | |
| ≤0.29 ppm | 502 (10) |
| 0.30-0.99 ppm | 1910 (40) |
| 1.00-2.99 ppm | 1655 (34) |
| ≥3.00 ppm | 739 (15) |
| Potential exposure to dispersants | |
| No | 4135 (86) |
| Yes | 671 (14) |
| Potential exposure to burning oil/gas | |
| Unexposed | 4347 (90) |
| Low/Medium | 403 (8) |
| High | 56 (1) |
| Smelled oil, dispersants, or cleaning chemicals | |
| No | 2014 (42) |
| Yes | 2972 (58) |
| Skin or clothing in contact with oil/tar/oily water | |
| No | 1695 (35) |
| Yes | 3111 (65) |
| Body or clothing ever became wet with chemicals | |
| No | 3163 (66) |
| Yes | 1643 (34) |
| Ever had to stop working because you were hot | |
| No | 2777 (58) |
| Yes | 2029 (42) |
| Worked any job involving oily plants/wildlife or dead animal recovery | |
| No | 2832 (59) |
| Yes | 1974 (41) |
| Ever worked as a commercial fisherman | |
| No | 3996 (83) |
| Yes | 810 (17) |
SD, standard deviation; FEV1, forced expiratory volume in 1 second; FVC, forced vital capacity,
Quality ≥D defined having at least two curves that meet the 2005 American Thoracic Society/European Respiratory society inter-maneuver criteria for both FEV1 and FVC or expert deemed equivalent score,
Residential proximity to the coast is defined as: living in a county directly adjacent to the Gulf of Mexico (direct), living in a county adjacent to coastal counties (indirect), or living in another Gulf state county.
Among workers with a less strict spirometry test quality scores ≥ D who had complete exposure and covariate information (N=4,806), those who smelled chemicals had higher FEV1 (Mean difference: 31 mL; 95% CI: −3, 64), and FVC (Mean difference: 30 mL, 95% CI: −9, 69) values than unexposed workers (Table 2). However, these associations were weaker after including workers with imputed data (N=6,811). Additionally, workers who had jobs that involved oily plants/wildlife or dead animal recovery had a significantly lower FEV1 (Mean difference: −70 mL, 95% CI: −105, −34), FVC (Mean difference: −56 mL, 95% CI: −97, −15) and FEV1/FVC (Mean difference: −0.60%, 95% CI: −1.02, −0.19) compared to unexposed. These associations were similar but attenuated for workers with imputed data for FEV1 (Mean difference: −53 mL, 95% CI: −84, −22), FVC (Mean difference: −45 mL, 95% CI: −81, −9), and FEV1/FVC ratio (Mean difference: −0.44%, 95% CI: −0.80, −0.07). Lung function parameters were not associated with any other oil spill experiences that we evaluated. Analyses restricted to workers who achieved stricter spirometry test quality scores ≥ C with complete exposure and covariate information (N=4,263) did not change the main finding, however the association between oily plants/wildlife or dead animal recovery was slightly attenuated (Table 3).
Table 2.
Oil spill experiences and lung function among oil spill response and cleanup workers with quality spirometry ≥ D*
| Complete case (N=4,806) |
Imputed (N=6,811) |
||
|---|---|---|---|
| N(%) | Mean Difference (95% CI)† |
Mean Difference (95% CI)† |
|
| Smelled oil, dispersants, or cleaning chemicals | |||
| FEV1(mL) | 2792 (58) | 31 (−3, 64) | 17 (−13, 46) |
| FVC(mL) | 30 (−9, 69) | 25 (−8, 59) | |
| FEV1/FVC% | 0.22 (−0.17, 0.62) | −0.009 (−0.36, 0.34) | |
| Skin or clothing in contact with oil/tar/oily water | |||
| FEV1(mL) | 3111 (65) | −23 (−58, 12) | −17 (−48, 13) |
| FVC(mL) | −18 (−59, 23) | −4 (−40, 31) | |
| FEV1/FVC% | −0.13 (−0.55, 0.28) | −0.22 (−0.59, 0.14) | |
| Body or clothing ever became wet with chemicals | |||
| FEV1(mL) | 1643 (34) | 17 (−18, 52) | 26 (−5, 56) |
| FVC(mL) | 4 (−37, 44) | 21 (−15, 56) | |
| FEV1/FVC% | 0.39 (−0.02, 0.79) | 0.27 (−0.09, 0.63) | |
| Ever had to stop working because you were hot | |||
| FEV1(mL) | 2029 (42) | −16 (−49, 18) | −14 (−43, 15) |
| FVC(mL) | −23 (−62, 16) | −17 (−51, 17) | |
| FEV1/FVC% | 0.14 (−0.25, 0.54) | 0.08 (−0.27, 0.42) | |
| Jobs that involved oily plants/wildlife or dead animal recovery | |||
| FEV1(mL) | 1974 (41) | −70 (−105, −34) | −53 (−84, −22) |
| FVC(mL) | −56 (−97, −15) | −45 (−81, −9) | |
| FEV1/FVC% | −0.60 (−1.02, −0.19) | −0.44 (−0.80, −0.07) | |
| Worked as a commercial fisherman full-time, part-time or seasonally | |||
| FEV1(mL) | 810 (17) | 28 (−19, 75) | 20 (−20, 60) |
| FVC(mL) | 34 (−21, 89) | 25 (−22, 72) | |
| FEV1/FVC% | 0.15 (−0.40, 0.71) | 0.02 (−0.46, 0.49) | |
Abbreviations: CI, confidence interval; N(%), number of participants exposed in the complete case sample; FEV1, forced expiratory volume in 1 second; FVC, forced vital capacity, mL, milliliters.
Quality ≥ D is defined having at least two acceptable curves that meet the 2005 American Thoracic Society/European Respiratory society intermaneuver criteria,
Adjusted for: Maximum ordinal total hydrocarbon exposure levels, potential exposure to burning oil/gas, potential dispersant exposure, age, height, height2, weight, gender, ethnicity, race, pre-spill diabetes, pre-spill lung disease, income, education, employment at time of enrollment, previous oil industry experience, previous oil spill cleanup work, residential proximity to coast, smoking, secondhand smoke.
Table 3.
Oil spill experiences and lung function among oil spill response and cleanup workers with spirometry quality ≥ grade C*
| Complete case (N=4,263) |
Imputation (N=6,048) |
||
|---|---|---|---|
| N(%) | Mean Difference (95% CI)† |
Mean Difference (95% CI)† |
|
| Smelled oil, dispersants, or cleaning chemicals | |||
| FEV1(mL) | 2479 (58) | 35 (−0.34, 70) | 19 (−12, 49) |
| FVC(mL) | 32 (−9, 73) | 25 (−10, 61) | |
| FEV1/FVC% | 0.31 (−0.10, 0.71) | 0.06 (−0.29, 0.42) | |
| Skin or clothing in contact with oil/tar/oily water | |||
| FEV1(mL) | 2741 (64) | −18 (−55, 19) | −16 (−47, 16) |
| FVC(mL) | −13 (−56, 30) | −2 (−39, 35) | |
| FEV1/FVC% | −0.13 (−0.55, 0.30) | −0.24 (−0.61, 0.13) | |
| Body or clothing ever became wet with chemicals | |||
| FEV1(mL) | 1453 (34) | 14 (−22, 50) | 22 (−10, 54) |
| FVC(mL) | 3 (−40, 46) | 22 (−16, 59) | |
| FEV1/FVC% | 0.31 (−0.11, 0.73) | 0.17 (−0.20, 0.54) | |
| Ever had to stop working because you were hot | |||
| FEV1(mL) | 1788 (42) | −8 (−43, 27) | −9 (−39, 22) |
| FVC(mL) | −17 (−58, 24) | −15 (−, 21) | |
| FEV1/FVC% | 0.21 (−0.19, 0.62) | 0.13 (−0.22, 0.49) | |
| Job involving oily plants/wildlife or dead animal recovery | |||
| FEV1(mL) | 1739 (41) | −60 (−97, −23) | −49 (−81, −16) |
| FVC(mL) | −44 (−88, −1) | −37 (−74, 1) | |
| FEV1/FVC% | −0.58 (−1.01, −0.15) | −0.46 (−0.84, −0.08) | |
| Worked as a commercial fisherman full-time, part-time or seasonally | |||
| FEV1(mL) | 716 (17) | 25 (−24, 75) | 12 (−30, 54) |
| FVC(mL) | 25 (−33, 84) | 9 (−40, 59) | |
| FEV1/FVC% | 0.25 (−0.32. 0.82) | 0.10 (−0.39. 0.59) | |
Abbreviations: CI, confidence interval; N(%), number of participants exposed in the complete case sample; FEV1, forced expiratory volume in 1 second; FVC, forced vital capacity, mL, milliliters.
Quality ≥C is defined as having three acceptable curves that meet the American Thoracic Society/ European Respiratory Society inter-maneuver criteria and between-maneuver criteria with reproducibility of ≤150mL or equivalent deemed by a spirometry expert.
Adjusted for: Maximum ordinal total hydrocarbon exposure levels, potential exposure to burning oil/gas, potential dispersant exposure, age, height, height2, weight, gender, ethnicity, race, pre-spill diabetes, pre-spill lung disease, income, education, employment at time of enrollment, previous oil industry experience, previous oil spill cleanup work, residential proximity to coast, smoking, secondhand smoke.
In sensitivity analyses, associations between jobs involving oily plants/wildlife, or dead animal recovery and lung function remained among both those spirometry test quality scores ≥ D without pre-spill lung disease (Supplemental Table 3) and among those with no previous oil industry or oil spill cleanup experience (Supplemental Table 4). Among never-smokers, associations between jobs that involved oily wildlife, plants, or dead animal recovery and FEV1 and FVC measures were slightly stronger than comparable associations found in primary analyses: FEV1 (Mean difference: −90 mL, 95% CI; −142, −37), FVC (Mean difference: −86 mL, 95% CI: −147, −24) (Supplemental Table 5).
More women (48%) than men (39%) worked a job involving oily plants/wildlife or dead animal recovery. In gender stratified analyses, the associations between jobs involving oily plants/wildlife or dead animal recovery and FEV1 and FVC were slightly stronger in men than women. The association between this experience and the FEV1/FVC ratio in men was similar to, but slightly weaker than the association in women (Supplemental Table 6).
In analyses stratified by time elapsed between participants’ last day of OSRC work and spirometry test, associations between working any job involving oily plants/wildlife, or dead animal recovery and lung function measures were similar across time (≤ 1 year, >1 year and ≤ 2 years, and >2 years since last day of work) (Supplemental Table 7).
In analyses among workers with spirometry test quality scores ≥ D that assessed the individual components of the composite job of oily plants/wildlife or dead animal recovery, workers who handled wildlife or dead animals had no significant differences for FEV1 (Mean difference: 11 mL; 95% CI: −90, 113), FVC (Mean difference: 46 mL; 95% CI: −72, 164), or FEV1/FVC (Mean difference: −0.50%, 95% CI: −1.69, 0.68). Workers who cut, collected, or put oily plants, sargassum weed or grass, or garbage into bags or containers for disposal had a lower FEV1 (Mean difference: −73 mL, 95% CI: −111, −34), FVC (Mean difference: −70 mL, 95% CI: −115, −26), and FEV1/FVC ratio (Mean difference: −0.45%, 95% CI: −0.90, 0.01) compared to unexposed workers.
Discussion
We observed lower lung function associated with jobs that involved oily plants/wildlife or dead animal recovery and suggestively better lung function associated with smelling oil spill chemicals. We did not observe associations between any other oil spill experience evaluated and lung function in our primary sample. The inverse association between jobs involving oily plants/wildlife or dead animal recovery and lung function was robust to inclusion of participants with imputed data on exposure and covariate information and to multiple sensitivity analyses, i.e. using a stricter definition of quality spirometry, although the association was slightly attenuated for both types of analyses. Findings for this oil spill experience were also robust to sensitivity analyses that restricted to those participants with no previous respiratory disease, with no previous oil industry/spill experience and among never smokers, although differences observed varied slightly depending on the analytic subpopulation. We also evaluated individual components of the composite experience of jobs involving handling of oily plants/wildlife or dead animal recovery by assessing just those who handled oily plants and separately, those who handed wildlife. Results suggest that handling oily plants might be driving the observed association.
The magnitude of the association observed between oily wildlife/plants or dead animal recovery and FEV1 ranged from −70 mL to −49 mL among primary analytic subgroups. This is larger than the expected age-related decline in FEV1 for adults (age 35-40 years) which is estimated as 25-30 mL/year [35]. In addition to normal age-related FEV1 loss, the functional relevance of the magnitude of associations observed in our study can be better understood in the context of lung function impacts of other known respiratory irritants. For example, short-term ambient air pollution (PM2.5) exposure has been associated with ~20 mL lower FEV1 and FVC among nonsmoking adults [36], whereas long-term air pollution (PM2.5) has also been associated with an additional ~11 mL in FEV1 annual decline above expected age-related decline [37]. Further, current cigarette smoking habit has been associated with declines of 12.6 mL/year per pack/day in FEV1 for men, and 7.2 mL/ year per pack/day in FEV1 for women [38].
We initially hypothesized that certain oil spill experiences induced psychological stress or related sequalae, which may have reduced OSRC workers’ lung function. Prior work showed that adverse mental health outcomes associated with cleanup work may have persisted 1-3 years following the cleanup efforts of the DWH spill [3]. Psychological stress, anger, and negative emotions have been associated with reduced lung function and other adverse respiratory outcomes [11, 12, 39-41], including asthma [11] and reduced lung function [42]. Stress can induce changes in neuroendocrine pathways and in the immune response that can lead to airway inflammation [6]. In GuLF STUDY OSRC workers, Kwok et al. did not observe an association between jobs that involved oily plants/wildlife or dead animal recovery and either post-traumatic stress (prevalence ratio (PR): 1.17, 95% CI: 0.95, 1.44) or depression (PR: 0.96, 95% CI: 0.87, 1.07). But, it is possible that exposed OSRC workers with jobs that involved oily plants/wildlife or dead animal recovery experienced stress that was not detected by these mental health indicators but that still may have led to reduced lung function. Workers with jobs that involved oily plants/wildlife or dead animal recovery may have had lower lung function due to the stress of witnessing or seeing environmental pollution and degradation firsthand. Alternatively, the inverse association may be due to other chemical exposures (e.g., due to accidental ingestion) resulting from close contact with oiled plants or wildlife or findings may have been due to chance.
Smelling chemicals was suggestively associated with better lung function in the complete case analyses and in analyses with imputed data. Higher lung function in this group may suggest that a healthy worker effect for those sensitized to smelling spill chemicals may be present in analyses. It is important to note that we hypothesized that smelling odors would be associated with perceived stress, which in turn may have induced adverse effects on lung function. The experience of smelling chemicals itself is not indicative of chemical exposure and is, in fact, a poor surrogate of exposure and can be misleading. Odor thresholds for the major components of oil, benzene, toluene, ethylbenzene, xylene, and n-hexane (BTEX-H) [43-47] are 10-100 times higher than the exposure levels encountered by the GuLF STUDY workers. Similarly, odor thresholds for the components of oil spill dispersants are at least 10 times higher than the exposure encountered in our study [4]. Any odor associated with the oil is likely due to minor non-BTEX-H components. The cleaning agents had some components that had an odor at the exposure levels encountered by workers.
Overall, we did not observe reduced lung function associated with the oil spill experiences that were found to be associated with adverse mental health indicators by Kwok et al. [3]. For example, while Kwok et al. observed that workers who smelled oil, dispersants, or cleaning chemicals, had to stop work because of heat, or who worked as a commercial fisherman prior to the spill had higher prevalence of depression and post-traumatic stress, we found no effect of these experiences on lung function.
Several study limitations need to be considered. One primary limitation is that the oil spill experiences evaluated do not measure stress directly and represent a heterogenous mixture of exposures including stress, and/or chemical exposures. Our analysis does not shed light on the possible reasons why lung function is lower in oily plants group, or if differences are attributable to stress or toxic contaminants or both. However, it is not clear what contaminants could be causing this effect. Estimated exposure to THC is a crude indicator of the oil spill experience and does not reflect actual exposures to its components of BTEX-H and other compounds. However, the categorical exposure levels to THC components (very low, low, medium, or high) and dispersants (yes, no) may also result in misclassification. Such misclassification may lead to potential residual confounding in associations observed. We also know of no other chemical exposures to this group of workers. In addition, if exposures like THC and burning are highly correlated with stress it may be difficult to adjust for these factors. Further, exposures were defined as “ever”/ “never”, which did not account for how much time a worker was exposed to each experience. There may have been other oil spill experiences that the oily plant workers and the OSRC workers as a whole had that were not assessed by Kwok et al., that may have also been stressful. Finally, use of a one-time measurement of lung function 1-3 years after the spill limits our ability to make causal inferences, because we lack the ability to compare this measure to a baseline measure preceding the oil spill.
This study is the first to assess the potential impact on lung function of oil spill experiences independent of indicators of chemical exposure. This type of analysis was not possible in studies of prior oil spills due to the lack of detailed information on experiences and on chemical exposures. We took advantage of the GuLF STUDY’s unique dataset, which allowed for exploration of OSRC work experiences impact on lung function, separate from the primary chemical exposures of interest. Previous studies of oil spills assessing lung function among oil spill cleanup workers were not able to study these experiences independent of inhalation exposure estimates. Additionally, the sample of OSRC workers with measured lung function is also large compared to existing studies on prior spills. Finally, our study controlled for multiple potential confounders, was robust to multiple sensitivity analyses, and used objective measures of lung function that are clinically meaningful.
Conclusions
In the present study, we examined the associations between six unique oil spill experiences related to OSRC activities identified as potentially stressful for a previous study [3], and lung function 1-3 years following the DWH disaster. OSRC workers with jobs that involved oily plants/wildlife or dead animal recovery had lower lung function than unexposed OSRC workers, independent of estimated THC exposure levels and surrogates of potential exposure to dispersant, and burning oil/gas. It is unclear whether this association reflects stress related to this cleanup job or other exposures. The evaluation of stress measures such as psychosocial instruments, is needed to further elucidate the relationship between stress related to oil spill cleanup work-related activities and lung function. Additionally, the prospective assessment of stress and follow-up lung function measurements will provide an understanding of whether these effects are transient or persistent in this population.
Supplementary Material
Highlights.
Oil spill response and cleanup (OSRC) workers involved with the Deepwater Horizon disaster had potentially stressful work experiences that may have posed a risk to respiratory health.
In this study, we examined potentially stressful OSRC experiences in relation to lung function parameters forced expiratory volume in one second (FEV1), forced vital capacity (FVC), and the FEV1/FVC ratio.
Jobs that involved handling oily plants/wildlife or dead animal recovery were associated with lower FEV1, FVC, and FEV1/FVC after accounting for OSRC work inhalation exposures.
This large study is the first to examine lung function in relation to potentially stressful work experiences during the DWH disaster response and clean-up effort.
Acknowledgments
Funding source: This research was funded by the Intramural Research Program of the NIH, the National Institute of Environmental Health Sciences (Z01 ES 102945), and the NIH Common Fund.
Footnotes
Conflicts of interest: Patricia Stewart reports personal fees from Stewart Exposure Assessments, LLC. Mark Stenzel reports personal fees from Exposure Assessment Applications, LLC, during the conduct of the study. No other authors report any conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.King BS and Gibbins JD, Health hazard evaluation of Deepwater Horizon response workers. 2011: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health, Health Hazard Evaluation Program. [Google Scholar]
- 2.King BS, Gibbins John D., Health Hazard Evaluation of Deepwater Horizon Response Workers. 2011, National Institute for Occupational Safety and Heatlh. [Google Scholar]
- 3.Kwok RK, et al. , Mental health indicators associated with oil spill response and clean-up: cross-sectional analysis of the GuLF STUDY cohort. Lancet Public Health, 2017. 2(12): p. e560–e567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stewart PA, et al. , Development of a total hydrocarbon ordinal job-exposure matrix for workers responding to the Deepwater Horizon disaster: The GuLF STUDY. J Expo Sci Environ Epidemiol, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ylitalo GM, et al. , Federal seafood safety response to the Deepwater Horizon oil spill. Proceedings of the National Academy of Sciences, 2012. 109(50): p. 20274–20279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wright RJ, Rodriguez M, and Cohen S, Review of psychosocial stress and asthma: an integrated biopsychosocial approach. Thorax, 1998. 53(12): p. 1066–1074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kullowatz A, et al. , Stress effects on lung function in asthma are mediated by changes in airway inflammation. Psychosom Med, 2008. 70(4): p. 468–75. [DOI] [PubMed] [Google Scholar]
- 8.Wright RJ, Cohen RT, and Cohen S, The impact of stress on the development and expression of atopy. Curr Opin Allergy Clin Immunol, 2005. 5(1): p. 23–9. [DOI] [PubMed] [Google Scholar]
- 9.Spitzer C, et al. , Association of airflow limitation with trauma exposure and post-traumatic stress disorder. European Respiratory Journal, 2011. 37(5): p. 1068–1075. [DOI] [PubMed] [Google Scholar]
- 10.Brackbill RM, et al. , Asthma and posttraumatic stress symptoms 5 to 6 years following exposure to the World Trade Center terrorist attack. Jama, 2009. 302(5): p. 502–516. [DOI] [PubMed] [Google Scholar]
- 11.Wright RJ, et al. , War-related stressors are associated with asthma risk among older Kuwaitis following the 1990 Iraqi invasion and occupation. J Epidemiol Community Health, 2010. 64(7): p. 630–5. [DOI] [PubMed] [Google Scholar]
- 12.Turyk ME, et al. , Stressful life events and asthma in adolescents. Pediatr Allergy Immunol, 2008. 19(3): p. 255–63. [DOI] [PubMed] [Google Scholar]
- 13.Palinkas LA, et al. , Community patterns of psychiatric disorders after the Exxon Valdez oil spill. Am J Psychiatry, 1993. 150(10): p. 1517–23. [DOI] [PubMed] [Google Scholar]
- 14.Palinkas LA, et al. , Ethnic differences in stress, coping, and depressive symptoms after the Exxon Valdez oil spill. J Nerv Ment Dis, 1992. 180(5): p. 287–95. [DOI] [PubMed] [Google Scholar]
- 15.Gallacher J, et al. , Symptomatology attributable to psychological exposure to a chemical incident: a natural experiment. Journal of Epidemiology and Community Health, 2007. 61(6): p. 506–512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lyons RA, et al. , Acute health effects of the Sea Empress oil spill. J Epidemiol Community Health, 1999. 53(5): p. 306–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sim MS, Jo IJ, and Song HG, Acute health problems related to the operation mounted to clean the Hebei Spirit oil spill in Taean, Korea. Mar Pollut Bull, 2010. 60(1): p. 51–7. [DOI] [PubMed] [Google Scholar]
- 18.Sabucedo JM, et al. , Symptomatic profile and health-related quality of life of persons affected by the Prestige catastrophe. Disasters, 2010. 34(3): p. 809–20. [DOI] [PubMed] [Google Scholar]
- 19.Cherry KE, et al. , Long-term psychological outcomes in older adults after disaster: relationships to religiosity and social support. Aging Ment Health, 2015. 19(5): p. 430–43. [DOI] [PubMed] [Google Scholar]
- 20.Osofsky HJ, Osofsky JD, and Hansel TC, Deepwater horizon oil spill: mental health effects on residents in heavily affected areas. Disaster Med Public Health Prep, 2011. 5(4): p. 280–6. [DOI] [PubMed] [Google Scholar]
- 21.Meo SA, et al. , Lung function in subjects exposed to crude oil spill into sea water. Marine Pollution Bulletin, 2008. 56(1): p. 88–94. [DOI] [PubMed] [Google Scholar]
- 22.Rodriguez-Trigo G, et al. , Health changes in fishermen 2 years after clean-up of the Prestige oil spill. Annals of Internal Medicine, 2010. 153(8): p. 489–98. [DOI] [PubMed] [Google Scholar]
- 23.Gam KB, et al. , Lung Function in Oil Spill Response Workers 1-3 Years After the Deepwater Horizon Disaster. Epidemiology, 2018. 29(3): p. 315–322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gam KB, et al. , Exposure to oil spill chemicals and lung function in Deepwater Horizon disaster response workers. J Occup Environ Med, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kwok RK, et al. , The GuLF STUDY: A Prospective Study of Persons Involved in the Deepwater Horizon Oil Spill Response and Clean-Up. Environ Health Perspect, 2017. 125(4): p. 570–578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Engel LS, et al. , The Gulf Long-Term Follow-Up Study (GuLF STUDY): Biospecimen collection at enrollment. Journal of Toxicology and Environmental Health, Part A, 2017. 80(4): p. 218–229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Miller MR, et al. , Standardisation of spirometry. European Respiratory Journal, 2005. 26(2): p. 319–338. [DOI] [PubMed] [Google Scholar]
- 28.Hankinson JL, Odencrantz JR, and Fedan KB, Spirometric reference values from a sample of the general U.S. population. American Journal of Respiratory and Critical Care Medicine, 1999. 159(1): p. 179–87. [DOI] [PubMed] [Google Scholar]
- 29.Stewart P, Stenzel Mark R, Ramachandran Gurumurthy, Banerhee Sudipto, Huynh Tran, Groth Caroline, Kwok Richard K., Blair Aaron, Engel Lawrence S., Sandler Dale P., Development of a total hydrocarbon ordinal job-exposure matrix for workers responding to the Deepwater Horizon disaster: the GuLF STUDY. Journal of Exposure Science and Environmental Epidemiology, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lee KJ and Carlin JB, Multiple imputation for missing data: fully conditional specification versus multivariate normal imputation. Am J Epidemiol, 2010. 171(5): p. 624–32. [DOI] [PubMed] [Google Scholar]
- 31.Allison PD, Imputation of categorical variables with PROC MI. SUGI 30 proceedings, 2005. 113(30): p. 1–14. [Google Scholar]
- 32.Graham JW, Olchowski AE, and Gilreath TD, How Many Imputations are Really Needed? Some Practical Clarifications of Multiple Imputation Theory. Prevention Science, 2007. 8(3): p. 206–213. [DOI] [PubMed] [Google Scholar]
- 33.Bale TL and Epperson CN, Sex differences and stress across the lifespan. Nat Neurosci, 2015. 18(10): p. 1413–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Clougherty JE, A growing role for gender analysis in air pollution epidemiology. Environ Health Perspect, 2010. 118(2): p. 167–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sharma G and Goodwin J, Effect of aging on respiratory system physiology and immunology. Clinical Interventions in Aging, 2006. 1(3): p. 253–260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rice MB, et al. , Short-term exposure to air pollution and lung function in the Framingham Heart Study. Am J Respir Crit Care Med, 2013. 188(11): p. 1351–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rice MB, et al. , Long-term exposure to traffic emissions and fine particulate matter and lung function decline in the Framingham heart study. Am J Respir Crit Care Med, 2015. 191(6): p. 656–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Xu X, et al. , Effects of cigarette smoking on rate of loss of pulmonary function in adults: a longitudinal assessment. Am Rev Respir Dis, 1992. 146(5 Pt 1): p. 1345–8. [DOI] [PubMed] [Google Scholar]
- 39.Ritz T and Kullowatz A, Effects of emotion and stress on lung function in health and asthma. Current Respiratory Medicine Reviews, 2005. 1(2): p. 209–218. [Google Scholar]
- 40.Ritz T, et al. , Exhaled Nitric Oxide Decreases during Academic Examination Stress in Asthma. Ann Am Thorac Soc, 2015. 12(11): p. 1638–45. [DOI] [PubMed] [Google Scholar]
- 41.Goodwin RD, et al. , Association between lung function and mental health problems among adults in the United States: Findings from the First National Health and Nutrition Examination Survey. Am J Epidemiol, 2007. 165. [DOI] [PubMed] [Google Scholar]
- 42.Ochs-Balcom HM, et al. , The association of depressive symptoms and pulmonary function in healthy adults. Psychosom Med, 2013. 75(8): p. 737–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.ATSDR. Toxicological Profile for Benzene. Agency for Toxic Substances and Disease Registry, U.S. Department of Health and Human Services; 2007. [PubMed] [Google Scholar]
- 44.ATSDR. Toxicological Profile for Toluene. Agency for Toxic Substances and Disease Registry, U.S. Department of Health and Human Services; 2017. [PubMed] [Google Scholar]
- 45.ATSDR. Toxicological Profile for Ethylbenzene. Agency for Toxic Substances and Disease Registry, U.S. Department of Health and Human Services; 2010. [PubMed] [Google Scholar]
- 46.ATSDR. Toxicological Profile for Xylene. Agency for Toxic Substances and Disease Registry, U.S. Department of Health and Human Services; 2007. [PubMed] [Google Scholar]
- 47.ATSDR. Toxicological Profile for n-hexane. Agency for Toxic Substances and Disease Registry, U.S. Department of Health and Human Services; 1999. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.