Abstract
Myeloid cells, are critical for orchestrating regulated inflammation during wound healing. Toll-like receptors (TLRs), particularly TLR4 and its downstream signaling MyD88 pathway, play an important role in regulating myeloid-mediated inflammation. Since an initial inflammatory phase is vital for tissue repair, we investigated the role of TLR4 regulated myeloid-mediated inflammation in wound healing. In a cutaneous tissue injury murine model, we found that TLR4 expression is dynamic in wound myeloid cells during the course of normal wound healing. We identified that changes in myeloid TLR4 during tissue repair correlated with increased expression of the histone methyltransferase, Mix-lineage leukemia-1 (MLL1) that specifically trimethylates the histone 3 lysine 4 (H3K4me3) position of the TLR4 promoter. Furthermore, we used a myeloid-specific Mll1 knockout (Mll1f/fLyz2Cre+) to determine MLL1 drives Tlr4 expression during wound healing. To understand the critical role of myeloid-specific TLR4 signaling, we used mice deficient in Tlr4 (Tlr4−/−), Myd88 (Myd88−/−), and myeloid-specific Tlr4 (Tlr4f/fLyz2Cre+) to demonstrate delayed wound healing at early time points post-injury. Furthermore, in vivo wound myeloid cells isolated from Tlr4−/− and Myd88−/− wounds demonstrated decreased inflammatory cytokine production. Importantly, adoptive transfer of monocyte/macrophages from wild-type mice trafficked to wounds with restoration of normal healing and myeloid cell function in Tlr4-deficient mice. These results define a role for myeloid-specific, MyD88-dependent TLR4 signaling in the inflammatory response following cutaneous tissue injury and suggest that MLL1 regulates TLR4 expression in wound myeloid cells.
Keywords: Toll-like receptor, wound, mechanism, inflammation
INTRODUCTION
Wound healing is a complex, but well-orchestrated biological event, with interplay between a number of resident and infiltrating cell types (1, 2). The recruitment of circulating blood myeloid to the site of tissue injury plays an important role in tissue repair. These recruited myeloid are critical for the regulated inflammatory response that is necessary for progression through the healing cascade. The precise timing of both the initiation and resolution of inflammation is essential for restoring tissue integrity. The first phase of the inflammatory response is destructive to the tissue and promotes clearance of invading pathogens, while the second phase is a resolution phase where tissue repair ensues (3, 4). For this reason, inflammation is an adaptive process that is necessary to maintain tissue homeostasis (5). In the absence of precise, programmed inflammation, pathologic non-healing ensues. A common characteristic of poorly healing wounds is an impaired initial immune response to injury and/or a sustained period of inflammation. During the first part of the inflammatory phase of wound healing, myeloid cells, particularly monocytes/macrophages, exist in a pro-inflammatory state, where they release inflammatory cytokines and mediators, recruit leukocytes, and promote tissue and pathogen destruction (6). After this early inflammatory phase, macrophages undergo a phenotype switch and begin secreting anti-inflammatory mediators as well as growth factors to promote tissue repair and wound resolution (7).
Accumulating evidence suggests that epigenetic regulation of gene expression influences immune cell phenotypes (8, 9). At present, a paucity of data exists on epigenetic-based mechanisms that regulate wound myeloid cell plasticity. Mixed-lineage leukemia 1 (MLL1) is a histone methyltransferase with site specificity for lysine 4 on histone H3 (H3K4) (10, 11). H3K4 trimethylation (H3K4me3) of gene promoter regions is associated with active gene expression (12). In mammals, H3K4me3 is controlled by the SET1-MLL family of enzymes (13). Although the role of MLL1 in oncogenesis has been investigated, few studies have examined the role of MLL1 in innate immunity (10, 14, 15). We have recently identified that MLL1 may regulate macrophage cytokine expression, however the role of MLL1 in regulating upstream signaling pathways remains poorly defined (16).
One receptor-signaling pathway that has been shown to be instrumental in the regulation of innate immunity, specifically macrophages, neutrophils, and dendritic cells, are the Toll-like receptors (TLRs). TLRs are a family of evolutionarily conserved receptors, which have a key role in host defense by regulating both innate and adaptive immune responses (17). TLR2 recognizes the peptidoglycan and lipopeptide in the cell walls of Gram-positive bacteria, while TLR4 recognizes lipopolysaccharide (LPS), which is an integral component of the outer membranes of Gram-negative bacteria. Importantly, Gram negative bacteria are common organisms found in diabetic wounds (18). Following ligand binding, TLR4 elicits immune response through coupling with intracellular adapter proteins including, MyD88 (myeloid differentiation factor 88), Mal (MyD88 adaptor-like), TRIF (TIR domain–containing adaptor inducing IFN-β), and TRAM (TRIF-related adaptor molecule). Ultimately, TLR signaling pathways regulate gene expression of cytokines, costimulatory molecules, and adhesion molecules. Recent studies suggest that TLR4 plays an important role in sterile inflammation, tissue repair, and response to a variety of injuries. For example, studies in animal models have demonstrated that TLR4 plays key roles during inflammation following ischemia/reperfusion injury, neurodegenerative disease, and thermal injury (19–21). Despite the importance of TLR4 in the regulation of cytokines, there remains a paucity of data on the role of TLR4 and MyD88 in cutaneous wound healing. Of the limited literature, it focuses primarily on early wound healing in keratinocytes (22) and thus the in vivo role of TLR4 in myeloid cells during the course of healing remains unknown.
Given the importance of TLR4 on immune cell function, particularly macrophage function, we investigated the role of MLL1 in regulating TLR4/MyD88 in cutaneous wound healing. Here, we show that MLL1, and hence, H3K4 trimethylation, directs dynamic Tlr4 expression in wound myeloid cells during the course of normal wound healing. Using TLR4 knockout (Tlr4−/−) and MyD88 knockout (Myd88−/−) mice, we demonstrate that TLR4 and MyD88 signaling are critical for the inflammatory response and that the absence of TLR4 or MyD88 decreases the necessary early inflammatory cytokine response and impairs wound healing. Further, using a myeloid-specific TLR4 knockout (Tlr4f/fLyz2Cre+), we demonstrate that myeloid-specific TLR4 is necessary for an adequate early inflammatory response in normal wound healing. Lastly, early adoptive transfer of wild-type monocytes/macrophages after tissue injury was sufficient to rescue wound healing with restoration of the inflammatory response. Taken together, our findings suggest that MLL1 regulates Tlr4 expression during normal tissue repair and that TLR4/MyD88 signaling plays an integral role in myeloid cell-mediated inflammation during wound repair.
MATERIALS AND METHODS
Mice
Mice were maintained in the University of Michigan pathogen-free animal facility, and all protocols were approved by and in accordance with the guidelines established by the Institutional Animal Care and Use Committee (UCUCA). Male and female C57BL/6 (Tlr4+/+), CD45.1, CD45.2, Tlr4−/−, and Myd88−/− mice maintained on a normal chow diet (ND) (13.5% kcal fat; LabDiet) were purchased at 20 weeks from The Jackson Laboratory (Bar Harbor, ME). Mice with the Mll1 or Tlr4 gene deleted in myeloid cells were generated by mating Mll1f/f (16) or Tlr4f/f (kind gift from Timothy Billiar University of Pittsburgh) mice with LysM-Cre mice (The Jackson Laboratory). Animals underwent all procedures at 20–24 weeks of age. Body weights were determined prior to experimentation.
Wound Healing Assessment
Before wounding, mice were anesthetized, hair was removed with Veet (Reckitt Benckiser), and skin was cleaned with sterile water. Full-thickness back wounds were created by 4-mm punch biopsy with or without wound splinting as previously described (23, 24). Initial wound surface area was recorded and digital photographs were obtained daily using an Olympus digital camera. Photographs contained an internal scale to allow for standard measurement calibration. Wound area was quantified using ImageJ software (National Institutes of Health, Bethesda, MD) and was expressed as the percentage of original wound size over time.
Wound Histology
On day 3 post-wounding, whole wounds were excised using a 6mm punch biopsy. Wound sections were fixed in 10% formalin overnight before embedding in paraffin. 5 μm sections were stained with hematoxylin and eosin for evaluation of re-epithelialization and with Masson’s Trichrome stain for collagen deposition. Images were captured using Olympus BX43 microscope and Olympus cell Sens Dimension software. Percent re-epithelialization was calculated by measuring distance traveled by epithelial tongues on both sides of wound divided by total distance needed for full re-epithelialization
Wound Digestion
Following sacrifice, wounds were collected from the backs of the mice postmortem following CO2 asphyxiation using a 6 mm wound biopsy. Sharp scissors were used to excise the full thickness dermis with a 1–2mm margin around the wound ensuring collection of granulation tissue and wounds were placed in RPMI. Wounds were then carefully minced with sharp scissors and digested by incubating in a 50 mg/ml Liberase TM (Roche) and 20U/ml DNaseI (Sigma-Aldrich) solution. Wound cell suspensions were then gently plunged and filtered through a 100μm filter to yield a single cell suspension. Cells were then either magnetic-activated cell sorted (MACs) for CD3−, CD19−, Ly6G−, CD11b+ cells for RNA studies or cultured ex-vivo for application of GolgiStop and subsequent staining for intracellular flow cytometry (25).
Wound Myeloid Cell Isolation and Magnetic-Activated Cell Sorting
Wounds were digested as described above. Single cell suspensions were incubated with fluorescein isothiocyanate–labeled anti-CD3, anti-CD19, and anti-Ly6G (BioLegend) followed by anti–fluorescein isothiocyanate microbeads (Miltenyi Biotec). Flow-through was then incubated with anti-CD11b microbeads (Miltenyi Biotec) to isolate the non-neutrophil, non-lymphocyte, CD11b+ cells. Cells were saved in Trizol (Invitrogen) for quantitative RT-PCR analyses.
ChIP Assay
Chromatin immunoprecipitation (ChIP) assay was performed as described previously (26). Briefly, cells fixed in paraformaldehyde were lysed and sonicated to generate 100–300bp fragments. To immunoprecipitate, samples were incubated in anti-H3K4trimethyl antibody (Abcam) or isotype control (rabbit polyclonal IgG) (Millipore) in parallel samples overnight followed by addition of proteinA Sepharose beads (Thermo-Fisher). Bound DNA was eluted and purified using Phenol:Chloroform:Isoamyl alcohol extraction and ethanol precipitation. Primers were designed using the Ensembl genome browser to search the TLR4 promoter and then NCBI Primer-BLAST was used to design primers that flank this site.
Adoptive Transfer
CD3−CD11c−CD19−Ly6G−NK1.1−CD11b+ single-cell suspensions were isolated by magnetic-activated cell sorting (MACS) from spleens of Tlr4−/− and Tlr4+/+ mice as described above. One million cells were injected intravenously via tail vein into wounded mice within twohours of wounding. Wound healing was monitored over time and wound area was calculated using NIH ImageJ Software (National Institute of Heath, Bethesda, MD). Initial wound size was calculated immediately after wounding, and wound closure was assessed over time as a percent of initial wound area.
Flow Cytometry
Single cell suspensions were collected and washed two times with cold PBS and filtered into a 96-well plate for surface staining. Cells were initially stained with pacific orange LIVE/DEAD fixable viability dye (Thermofisher) and then washed two times with cold PBS. Cells were then resuspended in Flow Buffer (PBS, FBS, NaN3, and Hepes Buffer) and Fc-Receptors were blocked with anti-CD16/32 (Biolegend) prior to surface staining. Biotinylated monoclonal antibodies used for surface staining included: Anti-CD3, Anti-CD19, Anti-CD45.1, Anti-CD45.2, Anti-Ter-119, Anti-NK1.1, Anti-CD11b, Anti-Ly6G, and Anti-Ly6C (Biolegend). Following surface staining, cells were washed twice, and biotinylated antibodies were labeled with streptavidin APC-Cy7. Next, cells were either washed and acquired for surface-only flow cytometry, or were fixed with 2% formaldehyde and then washed/permeabilized with BD perm/wash buffer (BD Biosciences) for intra-cellular flow cytometry. After permeablilization, intra-cellular stains included: anti-IL1β (mature IL1β, BD Biosciences), anti-TNF-α (Biolegend), anti-iNOS (affymetrix). After washing, samples were then acquired on a 3-Laser Novocyte Flow Cytometer (Acea Biosciences, Inc.). Data were analyzed using FlowJo software version 10.0 (Treestar, Inc.) and data were compiled using Prism software (GraphPad, Inc.). To verify gating and purity, all populations were routinely back-gated.
Cell Culture and Cytokine Analysis
Bone marrow (BM) cells were collected by flushing mouse femurs and tibias with RPMI. BM-derived MΦs (BMDMs) were cultured as previously detailed (26). On day 6, the cells were replated, and after resting for 24 h, they were incubated with or without LPS (100 ng/mL; Sigma (L2880) purified by phenol extraction <3% impurities) for 2–6 hours after which cells were placed in Trizol (Invitrogen) for RNA analysis.
RNA Analysis
Total RNA extraction was performed using Trizol (Invitrogen) according to manufacturer’s instructions. RNA was then reversed transcribed to cDNA using iScript (Biorad). PCR was performed with 2X Taqman PCR mix using the 7500 Real-Time PCR System. Primers for Il1b (Mm00434228_m10), Tnfa (Mm00443258_m1), Mll1 (Mm01179235_m1), Cd44 (Mm0 1277164-m1), Tlr4 (Mm00445273_m1) were purchased (Applied Biosystems). 18S was used as the internal control. Data were then analyzed relative to 18s ribosomal RNA (2ΔCt). All samples were assayed in triplicate. The threshold cycle values were used to plot a standard curve. Data were compiled in Microsoft Excel and presented using Prism software (GraphPad).
Statistical Analysis
Data were analyzed using GraphPad Prism software version 6. We expressed the results as means ±SEM. The statistical significance of differences between two groups was determined using Student t tests for data that passed a normality test; otherwise a non-parametric Mann-Whitney test was used. Differences between more than two groups were evaluated by one-way analysis of variance followed by post hoc analysis (Bonferroni test) for data that passed tests for normality and equal variance (Bartlett’s test); otherwise, a non-parametric Kruskal-Wallis test followed by Dunn’s post hoc analysis was used. P values <0.05 were considered significant.
RESULTS
TLR4 is dynamic during normal wound repair and is regulated by histone methylation
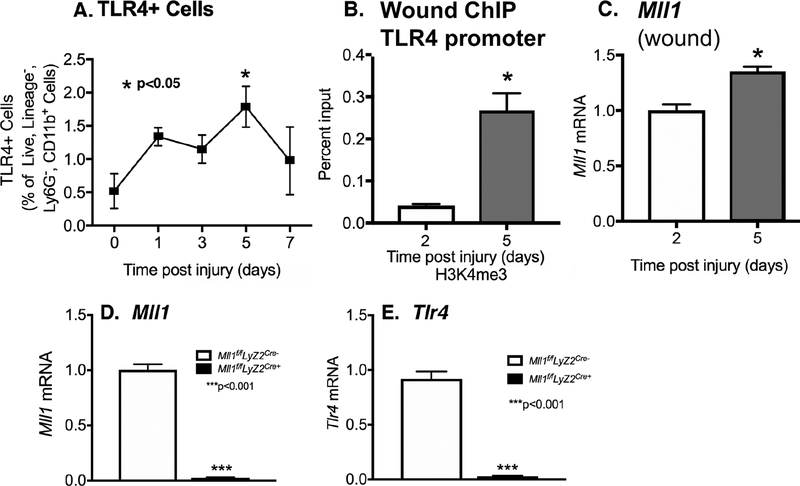
Increasing evidence suggests that proper wound healing requires the establishment of a regulated inflammatory response mediated by macrophages (8, 27, 28). The mechanisms responsible for macrophage phenotype in wound repair are incompletely understood. TLR4 is a major receptor that initiates a downstream signaling cascade that promotes inflammation, mostly through MyD88-dependent pathway and NF-κB expression. Further, TLR4 has been shown to play a vital role in the innate immune response to various sterile injuries. In order to examine the role of TLR4 in vivo in myeloid cells during wound repair, C57BL/6 mice were subjected to 4-mm full thickness wounds as previously described(8), and myeloid cells (CD11b+[CD3−CD19−Ly6G−]) were isolated from wounds by cell sorting at early time points (days 1–5) post injury. Expression of TLR4 was significantly upregulated in early wound myeloid cells after injury (Figure 1A).
Figure 1. TLR4 and MLL1 is upregulated in myeloid cells in the early inflammatory phase of wound healing.
A: Wounds were created by 4-mm punch biopsy on C57BL/6 mice. Wounds were harvested on days 0, 1, 3, 5, and 7. Wound myeloid cells CD11b+[CD3−CD19−Ly6G−] were isolated and single cell suspensions were processed for flow cytometry with pseudocolor plots. Data analysis of TLR4+ cells as a percentage of live, lineage−, Ly6−, CD11b+ cells (n = 5). B: Wound myeloid cells were isolated at day 2 and 5 postinjury by MACS for CD11b+[CD3−CD19−Ly6G−] cells. ChIP analysis for H3K4me3 at TLR4 promoter on day 2 and day 5 in cells isolated from the wounds was performed (n = 15). For all ChIP experiments, isotype control antibody to IgG was run in parallel. C: Wound myeloid cells CD11b+[CD3−CD19−Ly6G−] were isolated and Mll1 expression was quantified using qPCR (n=10). D-E: Wound myeloid cells CD11b+[CD3−CD19−Ly6G−] were isolated from Mll1f/fLyz2Cre+ and Mll1f/fLyz2Cre- and Mll1 or Tlr4 expression was quantified using qPCR. Data are presented as the mean±SEM. Data are representative of 2–3 independent experiments. Data were first analyzed for normal distribution and if data passed normality test, 2-tailed Student t test was used.
Increasingly, evidence suggests that epigenetic regulation (e.g., DNA methylation, histone modification) of gene expression plays a key role in influencing inflammatory phenotypes (8, 29). In addition, previous studies have suggested that the histone methyltransferase MLL1 drives inflammatory gene expression in myeloid cells (16, 30). To evaluate if the increased TLR4 expression in wound myeloid cells is due to epigenetic regulation of the TLR4 gene, we examined several histone methylation marks associated with gene activation. We found that H3K4me3 was significantly increased on the Tlr4 promoter in wound myeloid cells at day 5 as compared to earlier timepoints (day 2) (Figure 1B). The H3K4me3 methylation mark maintains the chromatin in a conformation so specific genes are effectively activated. Since the methyltransferase, MLL1, specifically methylates H3K4 (12, 31) we examined the expression of Mll1 and found it significantly increased at day 5 following tissue injury which corresponds to the increased TLR4 levels (Figure 1C). We have previously shown that myeloid-specific deficiency of Mll1 results in impaired cutaneous wound healing (32). To evaluate the ability of MLL1 to regulate Tlr4 expression, we generated mice deficient in Mll1 in cells of the myeloid lineage with lysosomes (monocytes, macrophages, granulocytes) by using the Cre-lox system. Myeloid-specific depletion of Mll1 was confirmed by examining MACS splenic monocyte/macrophages from Mll1f/fLyz2Cre+ mice and littermate controls (Mll1f/fLyz2Cre-) (Figure 1D). To determine whether Mll1 alters Tlr4 expression, myeloid cells were isolated on day 5 post wounding from Mll1f/fLyz2Cre+ mice and littermate controls. Mll1-deficient wound myeloid cells demonstrated significant decrease in Tlr4 expression in the Mll1f/fLyz2Cre+ compared to littermate controls (Figure 1E). These data suggest MLL1-derived H3K4me3 methylation may increase Tlr4 gene expression in wound myeloid cells following injury and that this may control, at least in part, the regulated inflammatory response during tissue repair.
TLR4 deficiency impairs cutaneous wound healing
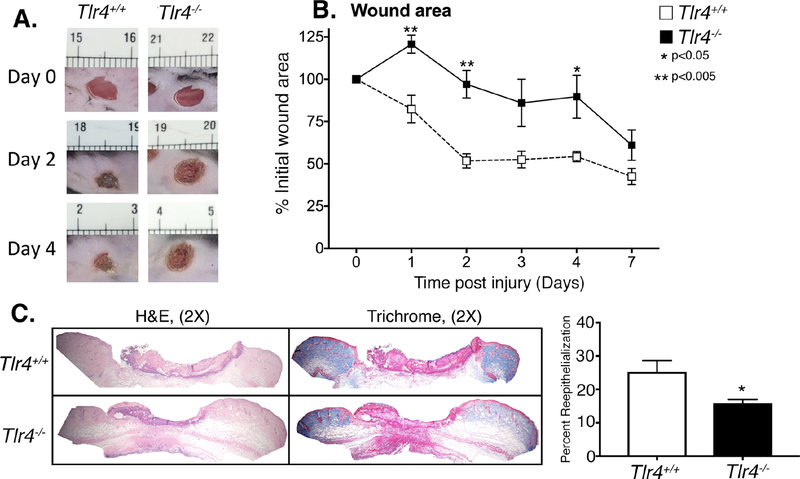
Given the dynamic changes in TLR4 expression in wound myeloid cells during healing, we examined if TLR4 is critical for cutaneous wound repair. To determine if the early increase in TLR4 in wound MΦs is necessary for healing, we wounded Tlr4−/− and control mice and monitored healing daily. Tlr4−/− mice had impaired healing throughout the entire wound course compared with controls (Figure 2A, B). When we examined wounds with histology, Tlr4−/− mice demonstrated impaired epithelialization and decreased collagen content compared with controls (Figure 2C). There was no difference in the expression of other toll-like receptors or the CD44 co-receptor in Tlr4−/− and control mice (Supplemental Figure 1A-C). Herein, these findings suggest that upregulation of TLR4 is necessary for normal wound closure.
Figure 2. TLR4 deficient mice exhibit delayed wound healing and decreased reepithelization.
A: Wounds were created in Tlr4−/− and control mice. Representative photographs of the wounds of Tlr4−/− mice and controls on days 0 and 4 post injury are shown. B: The change in wound area was recorded daily by blinded observer and analyzed with ImageJ software (n = 5). C: Wounds were harvested on day 3, paraffin embedded and sectioned. 5 μM sections were stained with hematoxylin and eosin and with Masson’s Trichrome stain. Percent re-epithelialization was calculated by measuring distance traveled by epithelial tongues on both sides of wound divided by total distance for full re-epithelialization. Representative images are shown in 2X magnification (*P < 0.05; n=5; repeated 1X). Data are presented as the mean±SEM. Data are representative of 2–3 independent experiments. Data were first analyzed for normal distribution and if data passed normality test, 2-tailed Student t test was used.
Myeloid cells from wounds of TLR4-deficient mice demonstrate decreased inflammatory cytokine expression
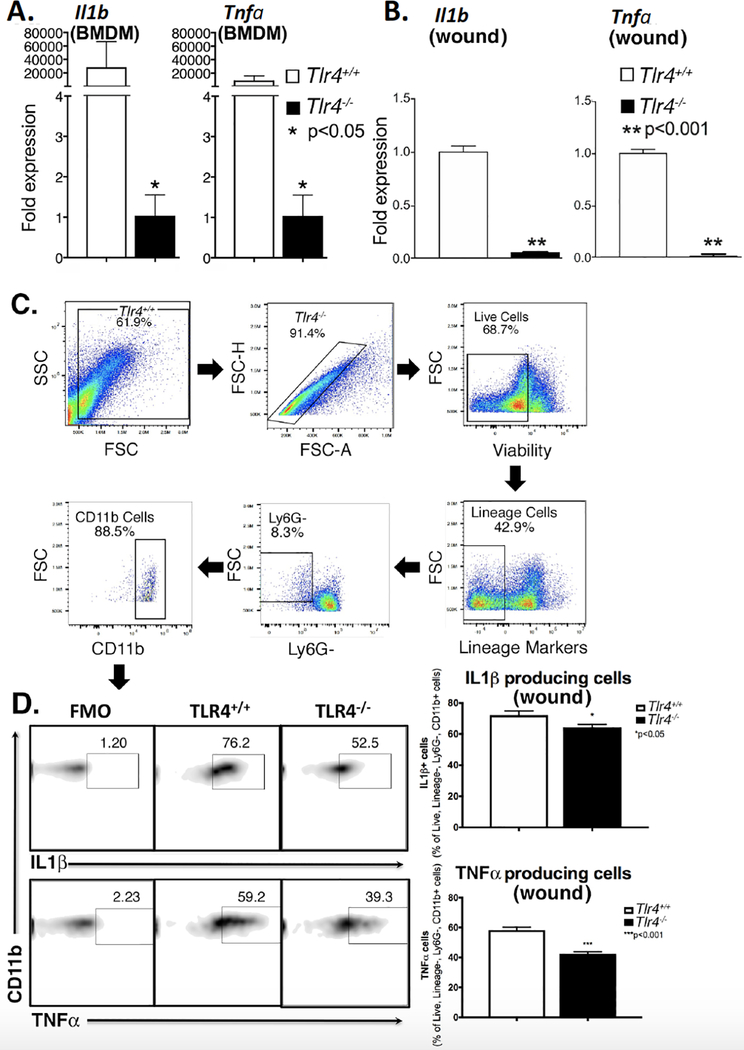
Since TLR4 is upregulated in wound myeloid cells and TLR4 is associated with NF-kβ–mediated initiation of the inflammatory response, we examined the role in vivo of TLR4 in wound myeloid cell-mediated inflammation (33). This is important since it is well established that regulated inflammation is critical for tissue repair (34, 35). To study this first in vitro, bone marrow derived macrophages (BMDMs) from Tlr4−/−and control mice were stimulated with LPS and analyzed for expression of inflammatory genes known to be important in wound healing, including Ilb and Tnfa (8). This demonstrated significantly decreased Il1b and Tnfa expression in the Tlr4−/− BMDMs compared with controls (Figure 3A). To determine whether the in vitro findings translate in vivo, we examined both inflammatory gene expression and cytokine production by qPCR and flow cytometry, respectively, on wound myeloid cells (live, lineage−, Ly6G−, CD11b+) isolated from Tlr4−/− and control wounds. We examined day 3 post-wounding to allow circulating monocytes adequate time to enter the tissues, transform into macrophages or dendritic cells, and assume a functional role (36, 37). Previous studies suggest that recruited inflammatory cell numbers are at their highest levels on day 3 post-wounding (38). There was no difference in the CD11b+ cells or neutrophils present within wound tissue at day 3 in Tlr4−/− and control wounds (Supplemental Figure 2A,B). However, examination of inflammatory cytokines known to play a major role in healing demonstrated that Il1b and Tnfa were significantly reduced at both the gene expression and protein level in the Tlr4−/− wound myeloid cells (Figure 3B-D). Taken together, these results suggest that TLR4 plays an important role in initiating the early inflammatory response critical for normal healing.
Figure 3. Decreased inflammatory cytokine expression in TLR4-deficient macrophages in vitro and in vivo.
A: Bone marrow derived macrophages (BMDMs) harvested from Tlr4−/− mice and controls were stimulated with LPS (100 ng/mL) for 2 hours after which they were collected for analysis. Il1b and Tnfa gene expression was quantified by qPCR (n = 5). B: Wound myeloid cells CD11b+[CD3−CD19−Ly6G−] were isolated and Il1b and Tnfa expression was quantified using qPCR (n=5). C: Tlr4−/−and control wound cell isolates were processed for intracellular flow cytometry. The gating strategy used for intracellular flow cytometry selecting live, lineage−, Ly6G−, CD11b+ cells is shown. D: Flow cytometry quantification of IL1β and TNFα in wounds (n = 10). Data are presented as the mean±SEM. Data are representative of 2–3 independent experiments. Data were first analyzed for normal distribution and if data passed normality test, 2-tailed Student t test was used. FMO, fluorescence minus one; FSC, forward scatter; FSC-A, forward scatter area; FSC-H, forward scatter height; SSC, side scatter.
MyD88 deficiency impairs cutaneous wound healing and decreases inflammatory cytokine expression
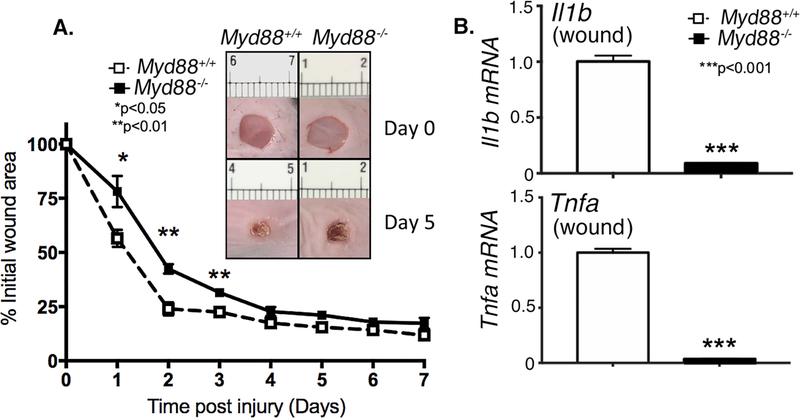
In response to ligand stimulation, TLR4 triggers downstream signaling via both MyD88-dependent and MyD88-independent pathways (39). The MyD88-dependent pathway ultimately leads to the activation of NF-κB and transcription of prominent inflammatory genes (40). To determine if this downstream pathway is instrumental to impaired wound healing in TLR4 deficiency, we wounded Myd88−/− and control mice and monitored healing daily. Myd88−/− mice had impaired healing compared with controls throughout the wound course consistent with Tlr4−/−mice (Figure 4A). We also examined sorted wound myeloid cells (CD3−CD19−Ly6G−CD11b+) and found that Il1b and Tnfa were significantly reduced in Myd88−/− wound myeloid cells in comparison to controls (Figure 4B). These findings suggest that upregulation of the TLR4-MyD88 signaling pathway is necessary for early inflammation and normal wound closure.
Figure 4. MyD88-deficient mice exhibit delayed wound healing and decreased inflammatory cytokine expression.
A: Wounds were created in Myd88−/− and control mice. Representative photographs of the wounds of Myd88−/− mice and controls on days 0 and 3 post injury are shown. The change in wound area was recorded daily by blinded observer and analyzed with NIH ImageJ software (n = 4, repeated 2X). B: Wound myeloid cells CD11b+[CD3−CD19−Ly6G−] were isolated and Il1b and Tnfa expression was quantified using qPCR (n=5). Data are presented as the mean±SEM. Data are representative of 2–3 independent experiments. Data were first analyzed for normal distribution and if data passed normality test, 2-tailed Student t test was used.
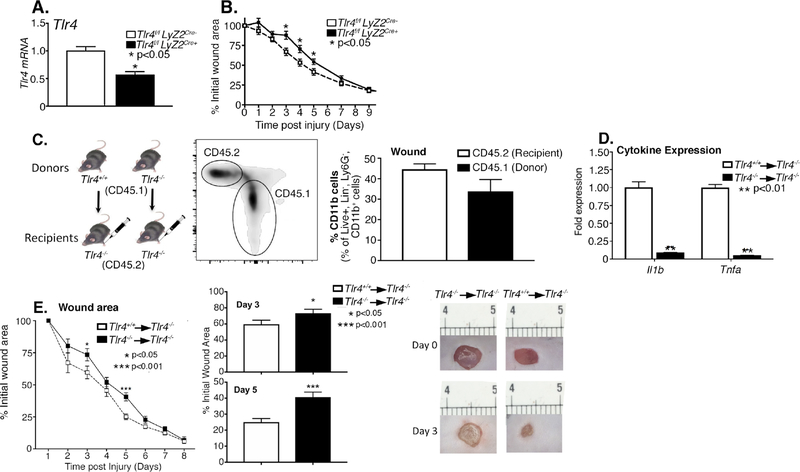
Myeloid-specific TLR4 is sufficient to rescue wound healing
In order to confirm the importance of myeloid-specific TLR4 in cutaneous wound healing, we generated mice deficient in Tlr4 in cells of the myeloid lineage with lysosomes (monocytes, macrophages, granulocytes) by using the Cre-lox system. Myeloid-specific depletion of Tlr4 was confirmed by examining MACS splenic monocyte/macrophages from Tlr4f/fLyz2Cre+ mice and littermate controls (Tlr4f/fLyz2Cre-) (Figure 5A). Wounds were generated in the Tlr4f/fLyz2Cre+ mice and their littermate controls, and wound closure was analyzed daily. Wound closure was markedly delayed at early time points in the Tlr4f/fLyz2Cre+ mice (Figure 5B). Additionally, to determine if TLR4+ monocytes/macrophages can restore healing, we performed an congenic adoptive transfer. Monocyte/macrophages (CD3−, CD19−, Ly6G−, NK1.1−, CD11c−, CD11b+) were isolated from Tlr4+/+ mice expressing CD45.1 and injected into the peripheral blood of wounded (day 1) Tlr4−/− mice expression CD45.2. To confirm the transferred monocytes appropriately tracked to the cutaneous wound, on day 4 post-injury (day 3 post-transfer) wound myeloid cells (CD3−CD19−Ly6G−CD11b+) were analyzed for CD45.1 and CD45.2 expression. A marked percentage of wound myeloid cells were found to express CD45.1 (Figure 5C) indicating transferred myeloid cells appropriately tracked to the cutaneous wound in agreement with our previous publications (32, 41, 42). To confirm these cells were functional, we also analyzed cytokine expression and found Tlr4+/+→Tlr4−/− wound myeloid cells displayed increased cytokine expression in comparison to Tlr4−/−→Tlr4−/− (Figure 5D). Importantly, wound healing was significantly improved in Tlr4+/+→Tlr4−/− in comparison Tlr4+/+→Tlr4−/− (Figure 5E). These results suggest that myeloid-specific TLR4 was sufficient to partially rescue wound healing in these mice, likely by restoring the initial inflammatory phase necessary for proper wound healing.
Figure 5. Myeloid-specific TLR4 was sufficient to rescue wound healing in Tlr4−/−mice.
A: Myeloid depletion of Tlr54 was examined by qPCR in MACS splenic myeloid cells CD11b+[CD3−CD19−Ly6G−] from Tlr4f/fLyz2Cre+ mice and littermate controls (Tlr4f/fLyz2Cre-) (n= 10). B: Wounds were created by 4-mm punch biopsy on the backs of Tlr4f/fLyz2Cre+ mice and littermate control mice. The change in wound area was recorded daily with ImageJ software until complete healing was observed (n=10). C: CD3−CD11c−CD19−Ly6G−NK1.1−CD11b+ single cell suspensions were isolated from Tlr4−/−and Tlr4+/+ spleens expressing CD45.1 by MACS. Cells (1 × 106) were injected intravenously in wounded (day 1) Tlr4−/− mice expressing CD45.2. Tracking of CD45.1 cells to the wounds was identified by the previously mentioned gating strategy and quantified as shown above. D: Wound myeloid cells CD11b+[CD3−CD19−Ly6G−] were isolated and Il1b and Tnfa expression was quantified using qPCR on day 4 post-wound (day 3 post-transfer) (n=3). E: Wound closure was measured in recipient mice daily by blinded observers with ImageJ software (n = 15) (n=15). B: Representative images are shown from Tlr4−/−→ Tlr4−/− and Tlr4+/+→ Tlr4−/− mice on days 0 and 3. Data are presented as the mean±SEM. Data are representative of 2–3 independent experiments. Data were first analyzed for normal distribution and if data passed normality test, 2-tailed Student t test was used.
DISCUSSION
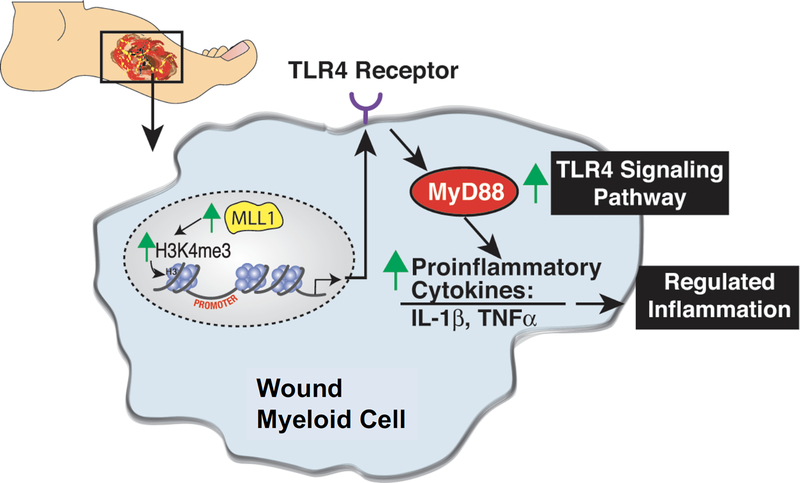
Herein, we identify that TLR4 expression is significantly elevated in tissue myeloid cells following cutaneous tissue injury and remains elevated during the wound healing course. The increased TLR4 expression is in part due to increased expression of the histone methyltransferase, MLL1, and its resulting methylation at the activating H3K4 site on the TLR4 promoter. Additionally, our results show that global TLR4 and MyD88 deficiency as well as myeloid-specific TL4 deficiency results in impaired wound healing as well as decreased expression of well-established proinflammatory mediators that are critical for normal tissue repair. Furthermore, when myeloid-specific TLR4 was replenished via adoptive transfer, wound healing was restored, suggesting that myeloid-specific TLR4 was both necessary and sufficient to partially rescue wound healing (Figure 6).
Figure 6.
Schematic of regulation of TLR4/MyD88 in normal wound healing.
The role of TLR4 in wound healing has previously been investigated in other models, but these have failed to identify regulators of the TLR4 expression following tissue injury and lack the importance of cell specificity with downstream TLR4 signaling pathways. Within the context of thermal burn injury, TLR4 has been shown to provide an important role in leukocyte adhesion and cytokine release (43). Similarly within diabetes, TLR4 expression and signaling are significantly increased in diabetic patients and db/db mice (44). Knockdown of TLR4 in diabetic mice resulted in attenuated inflammation as measured by circulating chemokines and improved wound healing suggesting that sustained TLR4 activation may be detrimental in diabetic wounds (45, 46). In contrast to the detrimental effects of TLR4 in diabetic wound healing, in nondiabetic wound healing, TLR4 signaling may be instrumental in the early phase as demonstrated in our current study with TLR4 deficient mice displaying markedly prolonged wound healing associated with decreased inflammatory gene expression. Previous work has demonstrated that wounds in Tlr2−/−, Tlr4−/−, and double-knockout Tlr2−/−/Tlr4−/− mice, exhibited attenuated healing and decreased global wound Tgfβ and Ccl5 expression relative to wild-type animals (47). However, the dynamic epigenetic regulation of TLR4 expression, as well as cell specificity has not previously been examined. Additionally, other studies have not interrogated the specific contributions of downstream adapter proteins, such as MyD88-dependent signaling, and their contribution to inflammation and wound healing. MyD88 is the most common adaptor molecule involved in most TLR signaling, with the exception of TLR3, which uses TRIF/TRAM. However, TLR4 has also been shown to signal through noncanonical intracellular pathways which may partially explain why the MyD88 deficient mice had a less robust delay in wound closure in comparison to the TLR4 knockout. Indeed, there is growing evidence of “noncanonical” toll-like receptor 4 (TLR4) signaling effectors (e.g., phosphatase and tensin homolog, integrins and the epidermal growth factor receptor) as important downstream participants (48).
Another murine model that has been recently used is the C3H/HeJ mice that have a genetic deficiency of TLR4. This model demonstrated delayed wound healing accompanied by elevated global levels of Tlr2, Tgfβ, and fibrosis in the wounded skin (22). While the findings in this study corroborate our own findings regarding the importance of TLR4 in wound healing, the Ch3H/HeJ represents an imprecise system to analyze the sole effect of TLR4 (49, 50). The C3H/HeJ mice have a spontaneous mutation resulting in loss of the TLR4 gene, but also have chromosomal inversion of Chromosome 6, which could lead to unknown abnormalities other than TLR4. Despite the lack of exogenous mouse mammary tumor virus, virgin and breeding females may still develop some mammary tumors later in life. Thus, C3H/HeJ mice have several immunological abnormalities, which may affect the function of TLR4.
The precise timing of both the initiation and resolution of inflammation is essential for restoring tissue integrity following injury. The first phase of wound healing is an inflammatory response which is characterized by tissue destruction and clearance of invading pathogens. In contrast, the second phase involves resolution of inflammation and tissue repair (3, 4). Healing of cutaneous wounds is a complex biological event that results from the interplay of a large number of resident cells, fibroblasts and keratinocytes, as well as infiltrating cell types, including leukocytes, monocytes/macrophages, and dendritic cells. Given the influential role of TLRs in wound healing, studies have attempted to identify the specific cell type expressing TLR4 vital for wound repair. However this has been complicated as there is a lack of consensus in distinguishing monocytes, dendritic cells, and macrophages within the skin during periods of wound healing using surface markers (51, 52). Previous studies have investigated the role of TLR4 in wound healing but have focused on fibroblasts and CD19 B lymphocytes cells (22, 53). Within the current study, through a novel myeloid-specific TLR4 deficient murine model and adoptive transfer, we demonstrated that myeloid-specific TLR4 and its downstream MyD88 signaling is necessary for sterile wound healing. The importance of myeloid-specific TLR4 is likely driven by the notion that the TLR4 pathway is critical for the initial inflammatory phase of wound healing as myeloid cells are predominately responsible for initial cytokine release during the first phase of wound healing and in turn play a key role in the orchestration of subsequent phases (35, 54).
Accumulating evidence suggests that epigenetic regulation of gene expression influences immune cell phenotypes within both disease states, such as diabetes, as well as the normal response to injury (8, 26, 32). At present, a paucity of data exists on epigenetic-based mechanisms that regulate wound macrophage plasticity. Within the current study we demonstrate that wound myeloid cells display increased expression of Mll1 and increased methylation at the lysine 4 on histone 3 (H3K4) of the TLR4 promoter resulting in dynamic TLR4 expression during the wound healing course. The dependence of TLR4 on MLL1 was further supported when analyzing mice deficient in MLL1 in the myeloid-specific lineage (Mll1f/fLyz2Cre+) where wounds from these mice showed significantly decreased Tlr4 expression. H3K4 trimethylation (H3K4me3) of gene promoter regions is associated with active gene expression (12) and we have previously shown that H3K4 trimethylation is involved in the regulation of inflammatory cytokine production in diabetic wound macrophages through the actions of the epigenetic methyltransferase MLL1 (32). The dynamic epigenetic regulation of TLR4 is important as previous studies have shown that immune cell phenotypes are continuing evolving during the course of wound healing and aberrances in this process can lead to delayed tissue repair (41). The role of epigenetic modifications on TLRs has previously been investigated in the regulation of TLR2 within diabetic wound healing demonstrating that altered CpG methylation status on the TLR2 promoter may correlate with diabetic foot ulcer severity (55). However, to date no studies have investigated the role of epigenetic modification of the TLR4 promoter pathway in nondiabetic wound healing.
Although this study produces insight into the mechanism behind TLR4 and myeloid inflammation in cutaneous wound healing, some limitations must be addressed. Myeloid cells play an important role in tissue repair following injury however, there is evidence that TLR4 is also expressed in keratinocytes, fibroblasts, and B cells (53, 56). This may partially explain why the adoptive transfer of myeloid-specific TLR4 cells partially restores wound healing as TLR4 may also regulate other cell types including epithelial cells. Further, there are multiple ligands that stimulate TLR4 dependent response, and at this time we are unable to determine which specific ligand is involved during cutaneous injury but it likely represents a combination of ligands including hylauron and skin microbiota. Lastly, although H3K4 trimethylation suggests a potential mechanism for increased TLR4 expression in wound MΦs, we acknowledge that other epigenetic modifications may play a role in TLR4 production. Indeed, other epigenetic enzymes have been shown to play a role in aberrant myeloid cell function in pathological states (55, 57, 58). Thus, further studies assessing the role of other specific epigenetic enzymes in the regulation of TLR4 signaling would be useful.
In summary, we showed myeloid-specific TLR4 is important for normal inflammation during tissue repair and is epigenetically driven by MLL1. Activating the TLR4 and MyD88 specific signaling, at least early in the wound healing course, may be a reasonable therapeutic strategy for regulating the initial inflammatory response in pathologic conditions that impair wound healing.
Supplementary Material
Acknowledgements:
We thank Robin Kunkel for her assistance with the graphical illustrations.
Funding Sources: This work is supported in part by National Institutes of Health grants R01-HL137919 (KG), K08-DK102357 (KG), F32-DK117545 (FD), American College of Surgeons Resident Fellowship (FD), T32-HL076123 (AK) and the Wolfe Foundation.
Footnotes
Disclosures: The authors have no conflicts of interest
References
- 1.Singer AJ, and Clark RA 1999. Cutaneous wound healing. N. Engl. J. Med 341: 738–46. [DOI] [PubMed] [Google Scholar]
- 2.WERNER S, and GROSE R 2003. Regulation of Wound Healing by Growth Factors and Cytokines. Physiol. Rev 83: 835–870. [DOI] [PubMed] [Google Scholar]
- 3.Italiani P, and Boraschi D 2014. From Monocytes to M1/M2 Macrophages: Phenotypical vs. Functional Differentiation. Front. Immunol 5: 514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wynn TA, and Vannella KM 2016. Macrophages in Tissue Repair, Regeneration, and Fibrosis. Immunity 44: 450–462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Medzhitov R 2008. Origin and physiological roles of inflammation. Nature 454: 428–35. [DOI] [PubMed] [Google Scholar]
- 6.Snyder RJ, Lantis J, Kirsner RS, Shah V, Molyneaux M, and Carter MJ 2016. Macrophages: A review of their role in wound healing and their therapeutic use. Wound Repair Regen. 24: 613–29. [DOI] [PubMed] [Google Scholar]
- 7.Boniakowski AE, Kimball AS, Jacobs BN, Kunkel SL, and Gallagher KA 2017. Macrophage-Mediated Inflammation in Normal and Diabetic Wound Healing. J. Immunol 199: 17–24. [DOI] [PubMed] [Google Scholar]
- 8.Gallagher K. a., Joshi A, Carson WF, Schaller M, Allen R, Mukerjee S, Kittan N, Feldman EL, Henke PK, Hogaboam C, Burant CF, and Kunkel SL 2015. Epigenetic changes in bone marrow progenitor cells influence the inflammatory phenotype and alter wound healing in type 2 diabetes. Diabetes 64: 1420–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ishii M, Wen H, Corsa CAS, Liu T, Coelho AL, Allen RM, Carson WF, Cavassani KA, Li X, Lukacs NW, Hogaboam CM, Dou Y, and Kunkel SL 2009. Epigenetic regulation of the alternatively activated macrophage phenotype. Blood 114: 3244–3254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schaller M, Ito T, Allen RM, Kroetz D, Kittan N, Ptaschinski C, Cavassani K, Carson WF, Godessart N, Grembecka J, Cierpicki T, Dou Y, and Kunkel SL 2015. Epigenetic regulation of IL-12-dependent T cell proliferation. J. Leukoc. Biol 98: 601–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yamashita M, Hirahara K, Shinnakasu R, Hosokawa H, Norikane S, Kimura MY, Hasegawa A, and Nakayama T 2006. Crucial role of MLL for the maintenance of memory T helper type 2 cell responses. Immunity 24: 611–22. [DOI] [PubMed] [Google Scholar]
- 12.Bernstein BE, Kamal M, Lindblad-Toh K, Bekiranov S, Bailey DK, Huebert DJ, McMahon S, Karlsson EK, Kulbokas EJ, Gingeras TR, Schreiber SL, and Lander ES 2005. Genomic maps and comparative analysis of histone modifications in human and mouse. Cell 120: 169–81. [DOI] [PubMed] [Google Scholar]
- 13.Wang X, Zhu K, Li S, Liao Y, Du R, Zhang X, Shu H-B, Guo A-Y, Li L, and Wu M 2012. MLL1, a H3K4 methyltransferase, regulates the TNFα-stimulated activation of genes downstream of NF-κB. J. Cell Sci 125: 4058–66. [DOI] [PubMed] [Google Scholar]
- 14.Vedadi M, Blazer L, Eram MS, Barsyte-Lovejoy D, Arrowsmith CH, and Hajian T 2017. Targeting human SET1/MLL family of proteins. Protein Sci. 26: 662–676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Carson WF, Cavassani KA, Soares EM, Hirai S, Kittan NA, Schaller MA, Scola MM, Joshi A, Matsukawa A, Aronoff DM, Johnson CN, Dou Y, Gallagher KA, and Kunkel SL 2017. The STAT4/MLL1 Epigenetic Axis Regulates the Antimicrobial Functions of Murine Macrophages. J. Immunol 199: 1865–1874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kimball A, Joshi A, Carson WF, Boniakowski A, Davis F, Schaller M, Allen R, Bermick J, Henke PK, Burant CF, Kunkel SL, and Gallagher KA 2017. The Histone Methyltransferase, MLL1, Directs Macrophage-Mediated Inflammation in Wound Healing and is Altered in a Murine Model of Obesity and Type 2 Diabetes. Diabetes db170194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Janeway CA, and Medzhitov R 2002. I NNATE I MMUNE R ECOGNITION. Annu. Rev. Immunol 20: 197–216. [DOI] [PubMed] [Google Scholar]
- 18.Rastogi A, Sukumar S, Hajela A, Mukherjee S, Dutta P, Bhadada SK, and Bhansali A 2017. The microbiology of diabetic foot infections in patients recently treated with antibiotic therapy: A prospective study from India. J. Diabetes Complications 31: 407–412. [DOI] [PubMed] [Google Scholar]
- 19.Breslin JW, Wu MH, Guo M, Reynoso R, and Yuan SY 2008. Toll-like receptor 4 contributes to microvascular inflammation and barrier dysfunction in thermal injury. Shock 29: 349–55. [DOI] [PubMed] [Google Scholar]
- 20.Molteni M, Gemma S, and Rossetti C 2016. The Role of Toll-Like Receptor 4 in Infectious and Noninfectious Inflammation. Mediators Inflamm. 2016: 6978936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Maung AA, Fujimi S, Miller ML, MacConmara MP, Mannick JA, and Lederer JA 2005. Enhanced TLR4 reactivity following injury is mediated by increased p38 activation. J. Leukoc. Biol 78: 565–573. [DOI] [PubMed] [Google Scholar]
- 22.Chen L, Guo S, Ranzer MJ, and DiPietro LA 2013. Toll-Like Receptor 4 Has an Essential Role in Early Skin Wound Healing. J. Invest. Dermatol 133: 258–267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Galiano RD, Michaels V J, Dobryansky M, Levine JP, and Gurtner GC 2004. Quantitative and reproducible murine model of excisional wound healing. Wound Repair Regen. 12: 485–492. [DOI] [PubMed] [Google Scholar]
- 24.Gallagher K. a., Joshi a., Carson WF, Schaller M, Allen R, Mukerjee S, Kittan N, Feldman EL, Henke PK, Hogaboam C, Burant CF, and Kunkel SL 2014. Epigenetic Changes in Bone Marrow Progenitor Cells Influence the Inflammatory Phenotype and Alter Wound Healing in Type 2 Diabetes. Diabetes 64: 1420–1430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mirza RE, Fang MM, Ennis WJ, and Koh TJ 2013. Blocking Interleukin-1 Induces a Healing-Associated Wound Macrophage Phenotype and Improves Healing in Type 2 Diabetes. Diabetes 62: 2579–2587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ishii M, Wen H, Corsa CAS, Liu T, Coelho AL, Allen RM, Carson WF, Cavassani KA, Li X, Lukacs NW, Hogaboam CM, Dou Y, and Kunkel SL 2009. Epigenetic regulation of the alternatively activated macrophage phenotype. Blood 114: 3244–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wood S, Jayaraman V, Huelsmann EJ, Bonish B, Burgad D, Sivaramakrishnan G, Qin S, DiPietro LA, Zloza A, Zhang C, and Shafikhani SH 2014. Pro-inflammatory chemokine CCL2 (MCP-1) promotes healing in diabetic wounds by restoring the macrophage response. PLoS One 9: e91574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Koh TJ, and DiPietro LA 2011. Inflammation and wound healing: the role of the macrophage. Expert Rev. Mol. Med 13: e23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hirahara K, Vahedi G, Ghoreschi K, Yang X-P, Nakayamada S, Kanno Y, O’Shea JJ, and Laurence A 2011. Helper T-cell differentiation and plasticity: insights from epigenetics. Immunology 134: 235–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kittan NA, Allen RM, Dhaliwal A, Cavassani KA, Schaller M, Gallagher KA, Carson WF, Mukherjee S, Grembecka J, Cierpicki T, Jarai G, Westwick J, Kunkel SL, and Hogaboam CM 2013. Cytokine induced phenotypic and epigenetic signatures are key to establishing specific macrophage phenotypes. PLoS One 8: e78045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yang W, and Ernst P 2017. SET/MLL family proteins in hematopoiesis and leukemia. Int. J. Hematol. 105: 7–16. [DOI] [PubMed] [Google Scholar]
- 32.Kimball AS, Joshi A, Carson WF, Boniakowski AE, Schaller M, Allen R, Bermick J, Davis FM, Henke PK, Burant CF, Kunkel SL, and Gallagher KA 2017. The Histone Methyltransferase MLL1 Directs Macrophage-Mediated Inflammation in Wound Healing and Is Altered in a Murine Model of Obesity and Type 2 Diabetes. Diabetes 66: 2459–2471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Portou MJ, Baker D, Abraham D, and Tsui J 2015. The innate immune system, toll-like receptors and dermal wound healing: A review. Vascul. Pharmacol 71: 31–6. [DOI] [PubMed] [Google Scholar]
- 34.Davis FMFM, Kimball A, Boniakowski A, and Gallagher K 2018. Dysfunctional Wound Healing in Diabetic Foot Ulcers: New Crossroads. Curr. Diab. Rep 18: 2. [DOI] [PubMed] [Google Scholar]
- 35.Boniakowski AE, Kimball AS, Jacobs BN, Kunkel SL, and Gallagher KA 2017. Macrophage-Mediated Inflammation in Normal and Diabetic Wound Healing. J. Immunol 199: 17–24. [DOI] [PubMed] [Google Scholar]
- 36.Fathke C, Wilson L, Hutter J, Kapoor V, Smith A, Hocking A, and Isik F 2004. Contribution of bone marrow-derived cells to skin: collagen deposition and wound repair. Stem Cells 22: 812–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wu Y, Wang J, Scott PG, and Tredget EE 2007. Bone marrow-derived stem cells in wound healing: a review. Wound Repair Regen 15 Suppl 1: S18–26. [DOI] [PubMed] [Google Scholar]
- 38.Leibovich SJ, and Ross R 1975. The role of the macrophage in wound repair. A study with hydrocortisone and antimacrophage serum. Am. J. Pathol 78: 71–100. [PMC free article] [PubMed] [Google Scholar]
- 39.Di Gioia M, and Zanoni I 2015. Toll-like receptor co-receptors as master regulators of the immune response. Mol. Immunol 63: 143–52. [DOI] [PubMed] [Google Scholar]
- 40.Chen GY, and Nuñez G 2010. Sterile inflammation: sensing and reacting to damage. Nat. Rev. Immunol 10: 826–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kimball A, Schaller M, Joshi A, Davis FM, denDekker A, Boniakowski A, Bermick J, Obi A, Moore B, Henke PK, Kunkel SL, and Gallagher KA 2018. Ly6CHi Blood Monocyte/Macrophage Drive Chronic Inflammation and Impair Wound Healing in Diabetes Mellitus. Arterioscler. Thromb. Vasc. Biol 38: 1102–1114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Boniakowski AE, Kimball AS, Joshi A, Schaller M, Davis FM, denDekker A, Obi AT, Moore BB, Kunkel SL, and Gallagher KA 2018. Murine macrophage chemokine receptor CCR2 plays a crucial role in macrophage recruitment and regulated inflammation in wound healing. Eur. J. Immunol 48: 1445–1455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cairns BA, Barnes CM, Mlot S, Meyer AA, and Maile R 2008. Toll-like receptor 2 and 4 ligation results in complex altered cytokine profiles early and late after burn injury. J. Trauma 64: 1069–77; discussion 1077–8. [DOI] [PubMed] [Google Scholar]
- 44.Rosa Ramirez S, and Ravi Krishna Dasu M 2012. Toll-like receptors and diabetes complications: recent advances. Curr. Diabetes Rev. 8: 480–8. [DOI] [PubMed] [Google Scholar]
- 45.Devaraj S, Tobias P, and Jialal I 2011. Knockout of toll-like receptor-4 attenuates the pro-inflammatory state of diabetes. Cytokine 55: 441–5. [DOI] [PubMed] [Google Scholar]
- 46.Dasu MR, and Jialal I 2013. Amelioration in wound healing in diabetic toll-like receptor-4 knockout mice. J. Diabetes Complications 27: 417–421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Suga H, Sugaya M, Fujita H, Asano Y, Tada Y, Kadono T, and Sato S 2014. TLR4, rather than TLR2, regulates wound healing through TGF-β and CCL5 expression. J. Dermatol. Sci 73: 117–24. [DOI] [PubMed] [Google Scholar]
- 48.McKeown-Longo PJ, and Higgins PJ 2017. Integration of Canonical and Noncanonical Pathways in TLR4 Signaling: Complex Regulation of the Wound Repair Program. Adv. wound care 6: 320–329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Bettinger DA, Pellicane JV, Tarry WC, Yager DR, Diegelmann RF, Lee R, Cohen IK, and DeMaria EJ 1994. The role of inflammatory cytokines in wound healing: accelerated healing in endotoxin-resistant mice. J. Trauma 36: 810–3; discussion 813–4. [DOI] [PubMed] [Google Scholar]
- 50.Brancato SK, Thomay AA, Daley JM, Crane MJ, Reichner JS, Sabo E, and Albina JE 2013. Toll-like receptor 4 signaling regulates the acute local inflammatory response to injury and the fibrosis/neovascularization of sterile wounds. Wound Repair Regen. 21: 624–633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Tamoutounour S, Guilliams M, Montanana Sanchis F, Liu H, Terhorst D, Malosse C, Pollet E, Ardouin L, Luche H, Sanchez C, Dalod M, Malissen B, and Henri S 2013. Origins and functional specialization of macrophages and of conventional and monocyte-derived dendritic cells in mouse skin. Immunity 39: 925–38. [DOI] [PubMed] [Google Scholar]
- 52.Gautier EL, Shay T, Miller J, Greter M, Jakubzick C, Ivanov S, Helft J, Chow A, Elpek KG, Gordonov S, Mazloom AR, Ma’ayan A, Chua W-J, Hansen TH, Turley SJ, Merad M, Randolph GJ, and Immunological Genome Consortium. 2012. Gene-expression profiles and transcriptional regulatory pathways that underlie the identity and diversity of mouse tissue macrophages. Nat. Immunol 13: 1118–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Iwata Y, Yoshizaki A, Komura K, Shimizu K, Ogawa F, Hara T, Muroi E, Bae S, Takenaka M, Yukami T, Hasegawa M, Fujimoto M, Tomita Y, Tedder TF, and Sato S 2009. CD19, a response regulator of B lymphocytes, regulates wound healing through hyaluronan-induced TLR4 signaling. Am. J. Pathol 175: 649–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Davis FM, Kimball A, Boniakowski A, and Gallagher K 2018. Dysfunctional Wound Healing in Diabetic Foot Ulcers: New Crossroads. Curr. Diab. Rep 18. [DOI] [PubMed] [Google Scholar]
- 55.Singh KK, Agrawal NK, Gupta SK, Mohan G, Chaturvedi S, and Singh KK 2015. Genetic and epigenetic alterations in Toll like receptor 2 and wound healing impairment in type 2 diabetes patients. J. Diabetes Complications 29: 222–9. [DOI] [PubMed] [Google Scholar]
- 56.Cheng T-L, Lai C-H, Chen P-K, Cho C-F, Hsu Y-Y, Wang K-C, Lin W-L, Chang B-I, Liu S-K, Wu Y-T, Hsu C-K, Shi G-Y, and Wu H-L 2015. Thrombomodulin promotes diabetic wound healing by regulating toll-like receptor 4 expression. J. Invest. Dermatol 135: 1668–1675. [DOI] [PubMed] [Google Scholar]
- 57.Rafehi H, El-Osta A, and Karagiannis TC 2012. Epigenetic mechanisms in the pathogenesis of diabetic foot ulcers. J. Diabetes Complications 26: 554–61. [DOI] [PubMed] [Google Scholar]
- 58.Paneni F, Costantino S, Battista R, Castello L, Capretti G, Chiandotto S, Scavone G, Villano A, Pitocco D, Lanza G, Volpe M, Lüscher TF, and Cosentino F 2015. Adverse epigenetic signatures by histone methyltransferase Set7 contribute to vascular dysfunction in patients with type 2 diabetes mellitus. Circ. Cardiovasc. Genet 8: 150–8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.