Abstract
Objectives:
The conceptual models underlying physical activity interventions have been based largely on differences between more and less active people. Yet physical activity is a dynamic behavior, and such models are not sensitive to factors that regulate behavior at a momentary level or how people respond to individual attempts at intervening. We demonstrate how a control systems engineering approach can be applied to develop personalized models of behavioral responses to an intensive text message-based intervention.
Design & Method:
To establish proof-of-concept for this approach, 10 adults wore activity monitors for 16 weeks and received five text messages daily at random times. Message content was randomly selected from three types of messages designed to target (1) social-cognitive processes associated with increasing physical activity, (2) social-cognitive processes associated with reducing sedentary behavior, or (3) general facts unrelated to either physical activity or sedentary behavior. A dynamical systems model was estimated for each participant to examine the magnitude and timing of responses to each type of text message.
Results:
Models revealed heterogeneous responses to different message types that varied between people and between weekdays and weekends.
Conclusions:
This proof-of-concept demonstration suggests that parameters from this model can be used to develop personalized algorithms for intervention delivery. More generally, these results demonstrate the potential utility of control systems engineering models for optimizing physical activity interventions.
Keywords: precision medicine, short message service (SMS), computational model, system identification
The widespread availability of mobile technology, such as smartphones with messaging capability, has created new possibilities for intervening on health behaviors in the natural context of individuals’ daily lives. This technology can expand the reach of physical activity interventions to address the widespread physical inactivity worldwide (Hallal et al., 2012). These tools have created, for the first time ever, the potential to adapt and personalize interventions to address the needs of individuals in the dynamic contexts of their daily lives (Heron & Smyth, 2010; Nahum-Shani, Hekler, & Spruijt-Metz, 2015). One of the major barriers to realizing the vision of personalized physical activity messaging interventions is that theories of physical activity determinants have been vague about the dynamics of those processes (Riley et al., 2011). In this paper, we shift the focus from physical activity determinants (e.g., goals, efficacy beliefs) to the idiosyncratic nature of treatment responses to a theoretically-guided text message intervention. This manuscript demonstrates an application of methods from the field of control systems engineering to identify these treatment responses as a step toward developing personalized physical activity messaging interventions. The focus is conceptual rather than technical in an attempt to bridge the concepts and tools from behavioral science and engineering.
Behavioral Intervention via Technology
Text messages (i.e., short message service [SMS]) and app-driven notifications have been used to deliver mobile physical activity interventions. These asynchronous message interventions have been widely implemented because this mode of communication is device agnostic, easy to use, inexpensive, and capable of reaching large segments of the population (Cole-Lewis & Kershaw, 2010). The most recent meta-analysis of text message intervention effects on preventive health behaviors concluded that “text message interventions are capable of producing positive change” (Armanasco, Miller, Fjeldsoe, & Marshall, 2017, p. 391). Most of the available evidence in that review involved interventions for smoking cessation or physical activity promotion. The overall pooled effect size for text message interventions was small (d = 0.24) but trended slightly larger for physical activity interventions (d = 0.35) (Armanasco et al., 2017). This effect compared favorably with the average effect of in-person interventions on physical activity in healthy adults (d = 0.19; Conn, Hafdahl, & Mehr, 2011). But text message interventions have typically been implemented as blunt instruments with theory guiding message content but lacking a strong empirical or theoretical basis for the selection or timing of messages.
Physical activity is a dynamic behavior. It varies throughout the day and from day to day (Martin et al., 2014). Over half of the variance in daily physical activity appears to lie within individuals from one day to the next (e.g., Conroy, Elavsky, Maher, & Doerksen, 2013). These momentary and daily behavioral fluctuations can inform our understanding of physical activity dynamics. Selecting and timing interventions to coincide with opportunities for physical activity should improve intervention outcomes by reducing attempts at intervention when participants are unable or unlikely to respond. Yet the physical activity motivation theories that frequently underlie messaging interventions rarely address time-varying contexts or psychological processes to guide intervention selection or timing. Indeed, few health behavior theories used to guide mHealth intervention development have explicitly addressed the dynamics of either health behavior or its underlying motivation (Riley et al., 2011). This silence stands in contrast to the increasing availability of sensors to measure physical activity passively which have created new possibilities for just-in-time interventions (Riley, Martin, & Rivera, 2014).
To illustrate, social-cognitive theory has arguably been one of the most influential theories of physical activity motivation and has provided the conceptual roots for many interventions with a variety of populations (McAuley & Blissmer, 2000; Rhodes & Nigg, 2011; Young, Plotnikoff, Collins, Callister, & Morgan, 2014). It is the most frequently cited theory in content creation for text message interventions for physical activity (Armanasco et al., 2017). Briefly, this theory proposes that physical activity is directly influenced by self-efficacy beliefs and goals, and that each of those constructs have their own determinants (Bandura, 1997, 2004). Scores of cross-sectional and prospective studies have provided evidence in support of these propositions (Young et al., 2014). The theory also proposes strategies that can be used to modify these cognitions. Yet the theory does not clearly specify when these cognitions should be changed or how much they should be changed to regulate ongoing behavior. Consequently, interventions developed based on social-cognitive theory have relied on a black box model that requires assumptions about the timing and magnitude of the processes outlined in the conceptual model.
Computational models based on social-cognitive theory have been proposed to formalize some of these dynamic processes (Hekler, Michie, et al., 2016; Martín et al., 2014; Pirolli, 2016; Riley et al., 2016, 2014; Spruijt-Metz et al., 2015; Timms, Martin, Rivera, Hekler, & Riley, 2014). These models often use a fluid analogy to describe the ebb and flow of motivation across systems of inputs and outputs. Modeling and simulation work illustrates the value of these models but they have yet to realize their intended impact on intervention development and public health. This computational approach holds tremendous promise for elaborating and refining theory. Computational approaches can also be applied differently to model dynamic behavioral responses to periodic interventions, such as individual text messages (Ashour et al., 2016). Although this black-box approach would not allow us to understand the psychological dynamics related to an intervention, it would provide a mathematical foundation for optimizing interventions by adapting the selection and timing of messages to produce desired effects on behavior.
One Size May Not Fit All
Three widely-used strategies to adapt (i.e., customize) interventions for groups or individuals involve targeting, tailoring, and personalizing (Armanasco et al., 2017; Fjeldsoe, Marshall, & Miller, 2009; Kreuter & Skinner, 2000; Napolitano & Marcus, 2002; Schmid, Rivers, Latimer, & Salovey, 2008). Targeting involves creating specific message content to be used by specific groups (e.g., obese adults, breast cancer survivors). Tailoring involves creating specific message content based on user data (e.g., feedback on goal accomplishment from step counts). Personalizing involves adding static, user-specific information ‒ such as someone’s name ‒ to a message. This strategy has a history in health messaging interventions that is distinct from the emergent area of personalized medicine. Critically, none of these strategies consistently increases text message intervention effect sizes on physical activity (Armanasco et al., 2017). One reason these strategies have not had their intended impact may be that they all assume that treatment responses are relatively uniform across participants regardless of what specific intervention content was delivered or how it was timed. In many cases, treatment responses vary between people, across different days, and as a function of message content or timing. This heterogeneity is likely when theories emphasize between-person differences and are often silent or vague about temporal processes or within-person change (Borsboom, Mellenbergh, & van Heerden, 2003; Dunton & Atienza, 2009; Riley et al., 2011). Heterogeneous response patterns may be unavoidable when intervening on outcomes such as health behaviors which have multiple, interacting determinants across multiple levels and time scales (Sallis, Owen, & Fisher, 2008).
Behavioral intervention approaches have become more sophisticated in recent years (Goldstein et al., 2017; Kumar et al., 2013; Nahum-Shani et al., 2016, 2015; Nilsen et al., 2012; Riley et al., 2011; Spruijt-Metz et al., 2015; Thomas & Bond, 2015). Examples include stepped care and just-in-time adaptive interventions (JITAIs). Stepped care increases the intensity/cost of treatment when patients’ exhibit sub-optimal responses to treatment after a prescribed interval. For example, Jakicic et al. (2012) delivered a stepped care weight loss intervention based on increasing physical activity and reducing caloric intake. Participants initially received a monthly group counseling session with a behavioral lesson delivered via mail. Every three months, participants who failed to meet planned weight loss goals received an intensified (i.e., stepped up) counseling frequency, mode, or strategies. These steps involved progressively adding telephone counseling sessions, individual sessions, and meal replacements in a standardized sequence. Stepped care approaches for weight loss have proven to be more cost effective than standard behavioral interventions (Brownell, 1986; Jakicic et al., 2012). New research designs, such as the sequential multiple assignment randomized trial (SMART) design, provide a tool for optimizing stepped care algorithms (Lei, Nahum-Shani, Lynch, Oslin,& Murphy, 2012; Sherwood et al., 2016).
JITAIs, on the other hand, involve context-sensitive decision rules for triggering interventions at moments of vulnerability/opportunity (Nahum-Shani et al., 2016, 2015). JITAIs are newer and have attracted great attention in the context of preventing lapses in behavior change once vulnerability is detected (e.g., during smoking cessation or weight loss attempts) (Goldstein et al., 2017; Kumar et al., 2015). JITAIs have also been developed to reduce sedentary behavior in obese adults and information workers (Luo et al., 2018; Thomas & Bond, 2015). JITAIs specify decision points, tailoring variables, decision rules, and intervention options to deliver treatment at specific times that coincide with vulnerability or opportunity (NahumShani et al., 2016, 2015). For example, the HeartSteps intervention for physical activity promotion delivers up to five daily contextually-relevant suggestions (intervention options: take a walk vs take a break from sitting) tailored to the user’s context (i.e., time of day, location, day of week) (Klasnja et al., 2015). The microrandomized trial has emerged as a new research design for optimizing decision rules and timing intervention delivery based on the user’s context (Klasnja et al., 2015).
Stepped care and JITAIs are sophisticated intervention approaches that can tailor interventions based on treatment response or contextual factors. Both can adapt the selection and timing of treatments (albeit at different timescales), and both rely on fixed, pre-specified tailoring variables and decision rules. Decision rules are typically informed by clinical experience, literature reviews, behavioral theory or empirical tests (e.g., using SMART or microrandomized trial designs) but, critically, these rules are developed for the typical participant (Lagoa, Bekiroglu, Lanza, & Murphy, 2014; Riley et al., 2011). That is, the same decision rule is applied for all patients.
With the availability of intensive longitudinal data on behavior, it may be possible to develop computational models that enable personalized selection and timing of treatments for maximum effect and minimal burden and fatigue. This approach may increase the likelihood of delivering interventions when individuals can respond as desired. Another advantage of personalizing decision rules based on a computational model is that, by modeling the persistence of treatment responses, new treatments can be withheld until a prior treatment response has likely run its complete course. This computational approach for personalizing adaptive interventions could reduce user burden and treatment fatigue, thereby supporting the level of extended participant engagement needed to improve distal health outcomes (Heckman, Mathew, & Carpenter, 2015).
Control Systems Engineering Tools
Control systems engineering tools provide a systematic approach for designing personalized adaptive interventions using intensive longitudinal data. Control systems engineering capitalizes on feedback to adapt responses dynamically in the service of achieving a goal. Control systems are common in everyday life. For example, thermostats in homes and cruise control in automobiles both involve setting a goal (i.e., set point for temperature or speed) and intervening as needed to minimize discrepancies between periodic real-time assessments and the goal. Control systems are also used to regulate complex, dynamic systems such as aircraft navigation. Flight, like human behavior, is complex and multiply determined. More precisely, what works to control flight/action under one set of conditions may not work similarly under other conditions and control systems are designed to take into account both present and past states to determine the “right action” to achieve the desired objectives. This paper extends that approach to develop personalized adaptive interventions for health behavior change.
Control systems engineering tools are already being applied to problems such as smoking cessation and managing gestational weight gain (Dong, Deshpande, Rivera, Downs, & Savage, 2014; Guo, Rivera, Downs, & Savage, 2016; Savage, Downs, Dong, & Rivera, 2014; Timms, Rivera, Collins, & Piper, 2013, 2014; Timms, Rivera, Piper, & Collins, 2014). For example, system identification and model predictive control were applied in a proof-of-concept study for designing a personalized adaptive smoking cessation intervention (Lagoa et al., 2014). An intensive longitudinal dataset was simulated to resemble published smoking cessation studies (Shiffman et al., 2000; Shiffman, Hickcox, et al., 1996; Shiffman, Paty, Gnys, Kassel, & Hickcox, 1996). The simulated data involved 150 participants who completed 3 measures/day for 50 days with interventions delivered on half of those occasions. Models were fit for each variable in this dynamic system. Urge was modeled as a function of urge at the last two measurement occasions, negative affect at the last two measurement occasions, self-efficacy at the last two measurement occasions, and a residual variance term. Similar models were estimated for negative affect (using prior data on negative affect, urge and self-efficacy) and self-efficacy (using data on prior self-efficacy, urge, and negative affect). In other words, a multidimensional model was obtained that described the dynamic interactions among the measured variables. Contemporary methods of model predictive control were applied to the system identified based on the simulated data on subjective urges to smoke, negative affect, and self-efficacy (Wang & Rivera, 2008; Wang, Rivera, & Kempf, 2007). The resulting controller adapted to the state of the participant, providing treatment only when it was predicted to be effective. That is, the model led to personalized decision rules for optimized treatment allocation that were more efficient because they limited treatment to moments when participants were expected to respond based on their historical individual patterns of responses. The controller-based treatment was shown to be more effective and less burdensome than conventional static treatments.
Physical activity is another excellent use case for applying computational modeling approaches from control systems engineering because it is possible to passively collect intensive longitudinal data about physical activity over extended periods of time (Riley et al., 2014). As noted above, others have proposed dynamical expressions of social-cognitive theory as computational models of physical activity (Hekler, Klasnja, et al., 2016; Martín et al., 2014; Riley et al., 2016, 2014; Spruijt-Metz et al., 2015; Timms, Martin, et al., 2014). The socialcognitive variables used as inputs in those models are generally assessed using self-reports which can be burdensome for users. This may limit their use to slower timescales of change (e.g., daily or weekly). These approaches have also been applied to adapt the level of daily step goals and incentives for achieving those goals (Korinek et al., 2017). Instead of using socialcognitive variables as inputs and outputs, we propose that text message treatment delivery can be used as an input to predict dynamic behavioral responses to treatments based on historical responses to different types of treatments and recent behavior (Ashour et al., 2016). These inputs provide a foundation for developing a computational model of physical activity at a faster timescale ‒ minutes or hours ‒ than has been done previously.
System identification uses data on historical responses to treatment (and other inputs) to develop a dynamic model of participant response to treatment. This process involves identifying both the number of sub-models needed, and their parameters based on noisy, potentially fragmented input data provided by heterogeneous inputs, such as message delivery logs and activity monitors. This step of system identification also provides characterizations of probability distributions on the identification error that can be used in a subsequent control synthesis stage when personalized decision rules are formalized in algorithms. System identification provides the mathematical foundation for applying probabilistic robust control synthesis to develop “controllers” that can optimize treatment delivery. Following, we present an illustration of system identification methods applied to model text message (input) effects on changes in physical activity (output). For this illustration, we use real data from a small study designed to establish proof-of-concept for applying this method to modeling how physical activity responds to a text message intervention grounded in social-cognitive theory.
Methods
Participants and Procedures
Adults (n=10) who did not meet federally recommended levels of aerobic physical activity but had no contraindications to physical activity were recruited via advertisements posted in the community to participate in a 16-week text message intervention study. Interested participants completed a telephone screening and eligible participants were scheduled for a lab visit. Participants had a mean age of 34.4 years (SD = 9.0, range = 22–47). Most were female (90%), employed full-time (80%), and parents (60%). Many were single (50%) but some were married (40%) or divorced (10%). Educational attainments varied from a high school diploma to a doctoral degree, and most had at least a bachelor’s degree (60%). Most were White (90%; 10% Asian American) and none were Hispanic or Latino.
During an initial lab visit for onboarding, a research assistant taught participants how to wear the activPAL3 activity monitor. These monitors were waterproofed in a nitrile sleeve and attached to the thigh with Hypafix tape. Participants were instructed to wear the monitor continuously and to remove it only when the device would be submerged in water (e.g., while bathing/swimming). Participants were given a paper log to document wake/sleep times each day and any non-wear time. Participants provided their mobile phone number for message delivery (intervention) over the next 16 weeks. For the 16 week intervention period, participants visited the lab at the end of each week to exchange their activity monitors and paper logs for charged monitors with full storage capacity and new paper logs.
Intervention
Over the next 16 weeks, participants received five text messages daily between 8:00am and 8:00pm (total of 5598 messages delivered). Messages were distributed on a random schedule within equal-sized segments of the day using SurveySignal (www.SurveySignal.com). A minimum inter-message interval of 1 hr was specified to limit pileup and distribute messages across the day. Messages were drawn randomly from content pools defined by one of three themes: “move more” (101 messages), “sit less” (101 messages), and general facts/trivia unrelated to either physical activity or sedentary behavior (254 messages). Message content for the physical activity and sedentary behavior pools was written based on social-cognitive theory to be consistent with prior text message interventions and our team’s prior research (Armanasco et al., 2017; Conroy, Elavsky, et al., 2013; Conroy, Maher, Elavsky, Hyde, & Doerksen, 2013). These messages involved (a) raising risk awareness and prompting planning (e.g., “Take it easy on your heart. By being inactive you are more likely to suffer from high blood pressure. Plan out your activity for today”), (b) enhancing outcome expectancies and prompting planning (e.g., “Don’t let extra pounds pack on! Regular physical activity can keep you lean. Take a moment to plan out how you will be active today”), (c) efficacy-building affirmations (e.g., “There are many people just like you that make the choice to be active every day”), (d) highlighting social support (e.g., “The people that care about you want you to engage in regular physical activity”), and (e) evoking anticipated reward/regret (e.g., “You don’t want to be a couch potato. Imagine how lazy you will feel if you do not participate in 30 minutes of physical activity today”).
Participants were asked to confirm message receipt with a reply message (even a single character sufficed for confirmation). Treatment fidelity was incentivized by $15 weekly payments for responding to 75% of delivered messages. Additionally, participants who responded to at least 75% of messages within two minutes were entered into a monthly drawing for a $100 bonus. Overall, 98.3% of messages were confirmed, and 67% were confirmed within two minutes (Conroy, Yang, Smyth, Lanza, & Lagoa, 2018). The time of both message delivery and receipt confirmation were recorded. The former was used as a model input because it can be manipulated by an intervention controller; any variability in message receipt delays contributes to the estimate of model uncertainty.
Data Processing and Analysis
Data processing and analysis took place in four stages. First, in the data processing stage, the time spent stepping in each 15-sec epoch output from the activPAL monitors was aggregated into 15-min epochs across the 24-hr day to create a discrete outcome in a computationally-efficient model. Sleep time activity data were excluded based on participants’ logs. Variables also were created to represent the type of message (“move more,” “sit less,” or general facts/trivia). Next, in the mathematical modeling stage, a personalized mathematical model of stepping time (output) was created for each participant using the three types of messages and prior behavior as inputs and stepping time as the output. This model is described in the Appendix. Briefly, each model was specified as a 5th order dynamical affine model, meaning that each input variable was entered for the last five 15-min epochs. Models also included a sparse perturbation (error or unexplained variance) term for each participant, and an uncertainty (noise) term for the general model.
In the third stage, system identification, separate models were optimized for weekday and weekend treatment responses because physical activity differs significantly across these two periods (Martin et al., 2014). This model is called a switch model. The parameters of the models were identified using a least absolute shrinkage and selection operator (LASSO) approach where the objective is to simultaneously minimize the error between observed stepping time and predicted stepping and, at the same time, minimize the number of time instants where the sparse perturbation is not zero (Kukreja, Löfberg, & Brenner, 2006). In mathematical terms, as in traditional LASSO approaches, the model minimized an objective function containing the sum of squares of the errors at the measured time instants and the sum of the magnitudes of the perturbations. In the final stage, simulation, treatment responses for each participant were estimated using the system identified in step 3. The effects of “move more” and “sit less” messages were interpreted relative to the effects of general facts/trivia messages.
Results
A control system for physical activity was identified using a piecewise 5th order dynamical affine model. This model was selected because it offered the best compromise between accuracy (size of the error) and complexity; higher-order models improved accuracy but increased the risk of overfitting the data. The models revealed heterogeneous responses to different message types that varied between people and between weekdays and weekends. Responses to text messages were estimated using the identified models and plotted for two cases to illustrate the diversity of treatment responses across time and message content. Figure 1 presents simulated impulse response curves. These curves depict the expected timing of peak responses to different types of messages on weekends (left panel) and weekdays (right panel). In these curves, the x-axis represents time since message delivery, and the y-axis represents predicted unit impulse changes in movement time during each 15-min epoch (i.e., the predicted person-specific change in the percentage of movement time during each 15-min epoch compared to the estimated movement time had the intervention not been delivered). For the participant represented in the top panel, peak responses occurred around 45–75 min after “move more” message delivery on weekends and there was not a distinct behavioral response to messages on weekdays. For the participant represented in the bottom panel, peak responses occurred around 75–90 min after “sit less” message delivery on weekends and there was not a distinct behavioral response to messages on weekdays. These peak responses for individual messages are informative but can be misleading because they do not represent the cumulative response to each message. That information is needed to understand the overall magnitude of responses.
Figure 1.
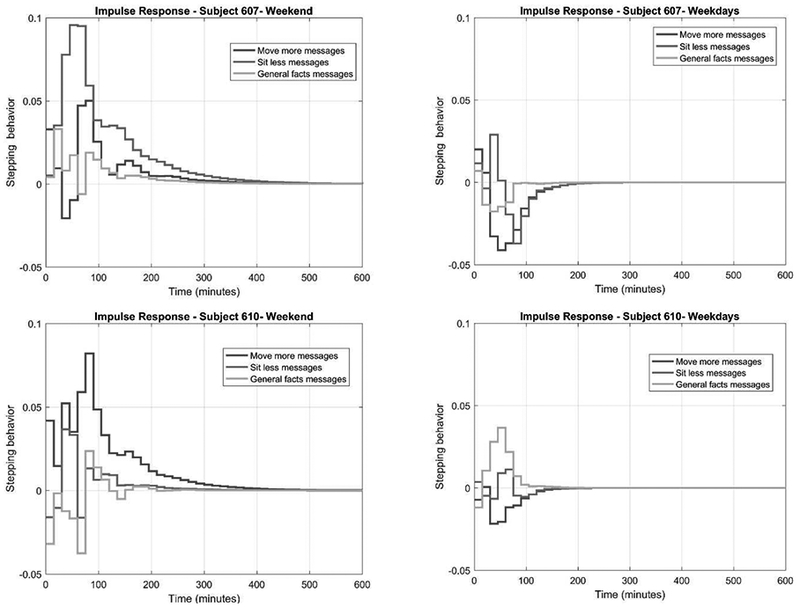
Simulated impulse response curves for participants #607 (top panel) and #610 (bottom panel) on weekends (left panel) and weekdays (right panel).
Figures 2 and 3 depict cumulative response curves following a single message (if multiple messages are received, their effects would accumulate). These curves represent the predicted cumulative behavior change (y-axis) as a function of the time following message delivery (x-axis) and the type of message (line) on weekends (left panel) and weekdays (right panel). Figure 2 shows that, for one participant, weekend stepping time (left panel) increased following “move more” messages, but not in response to messages focused on “sit less” or general facts/trivia. Weekday responses (right panel) to all three message types were negligible. For this participant, four weekend messages to “move more” should lead to a 40-min increase in stepping time each week. Figure 3 shows that, for another participant, weekend movement time (left panel) increased following “sit less” messages but not in response to messages focused on “move more” or general facts/trivia. Weekday responses (right panel) to all three message types were negligible. For this participant, five weekend messages to “sit less” should lead to a 40-min increase in stepping time each week. Thus, these two participants increased their physical activity in response to different message content (i.e., “move more” vs “sit less”), demonstrating the potential value of personalized message selection algorithms.
Figure 2.
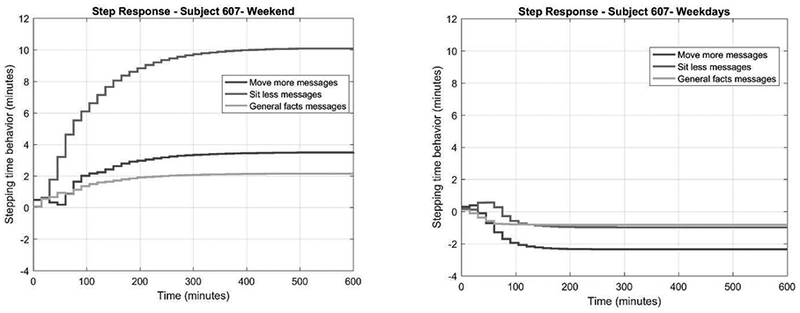
Simulated treatment responses for participant #607 on weekends (left panel) and weekdays (right panel). These curves depict the predicted cumulative change in stepping time following receipt of different types of text message.
Figure 3.
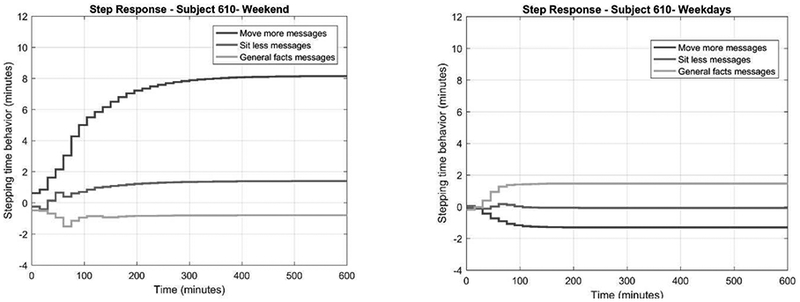
Simulated treatment responses for participant #610 on weekends (left panel) and weekdays (right panel). These curves depict the predicted cumulative change in stepping time following receipt of different types of text message.
Patterns that emerge across personalized models may also inform understanding of more generalized behavioral responses to intervention. In this study, inspection of the individual impulse and cumulative response curves for the 10 participants in this study led to three general observations. First, half of the sample had more pronounced behavioral responses to text messages on weekends than weekdays. The other half of the sample had similar behavioral responses to text messages on weekends and weekdays. Second, 4 out of 10 participants showed clear signs of behavior change following a text message; the remaining six participants had limited responses. Finally, among the responders, half increased their stepping time in response to “move more” messages, and half increased their stepping time in response to “sit less” messages.
Discussion
This study demonstrated the feasibility of applying control systems engineering tools to develop personalized models of behavioral responses to text message interventions. The systems identified provide a basis for developing controllers that can adapt text message delivery based on time-varying inputs (in this case, recent behavior and historical responses to messages) to generate desired outputs (in this case, changes in physical activity).
This application of system identification extends prior efforts to develop a computational formulation of the social-cognitive processes that motivate physical activity (Korinek et al., 2017; Martín et al., 2014; Riley et al., 2016; Spruijt-Metz et al., 2015; Timms, Martin, et al., 2014). Those models have frequently used a fluid analogy model to depict how changes in each construct are associated with changes in motivational - and ultimately behavioral - sequelae. In contrast, the present approach did not attempt to model psychological mechanisms of change as inputs so the dynamics of those psychological processes effectively remain inside a black box. Instead, the present approach modeled behavior change as a function of inputs that included recent physical activity and text message delivery. This model is likely simplistic for a complex behavior such as physical activity. It could be enriched - and model uncertainty reduced - by including momentary information such as location (e.g., work, home), time of day, weather, built environment features or other easily-classified determinants (Owen et al., 2011; Seefeldt, Malina, & Clark, 2002). Message features could also be coded and modeled on a more granular level based on their content, valence and temporal framing (e.g., motivational vs volitional, approach vs avoidance, immediate vs delayed behavioral initiation). It may even be possible to include subjective states (e.g., stress) as perturbations; however, that will be easier if those states can be detected using personal sensing to avoid burdening users. Collectively, these efforts could help move the field from relatively static theories of physical activity to more dynamic explanations of the contexts, interventions, and psychological processes that promote (or inhibit) physical activity.
The control systems engineering approach complements and extends existing approaches - particularly tailoring and just-in-time interventions - used to make text message intervention less generic and more effective. Similar to tailoring, it uses participant data to inform messaging (Kreuter & Skinner, 2000; Schmid et al., 2008); however, it enriches existing tailoring approaches by developing individual mathematical models of behavior and treatment responses to guide message selection and timing. In that way, it is similar to applications of system identification to adapt daily step goals and incentives (Korinek et al., 2017). By personalizing and periodically updating individual treatment algorithms, instead of simply message content, it is possible to reduce the threat of treatment fatigue by selecting and timing messages so participants only receive the minimal dose needed to achieve desired behavior change. For example, the participant whose data are presented in Figure 2 received 35 messages/week but only needed four “move more” messages at least five hours apart on weekends to achieve a 40 minutes/week increase in physical activity. Treatment fatigue is an important consideration for these models because fatigue can blunt intervention effects on behavior and health outcomes over time (Bekiroglu, Lagoa, Murphy, & Lanza, 2017; Heckman et al., 2015).
Similar to just-in-time interventions, this approach can contextualize intervention delivery once a model is trained. The model identified in this paper revealed different response patterns on weekends versus weekdays. Whereas just-in-time adaptive interventions specify a fixed decision rule for using participant data to guide treatment delivery (Nahum-Shani et al., 2016), the piecewise affine model reported here included sub-models for these different contexts to provide the basis for personalized, context-specific decision rules. Different sub-models could be estimated if other information was included. For example, physical activity varies as a function of precipitation so one might envision the possibility of different sub-models for rainy versus dry days (Chan & Ryan, 2009).
Any number of possible sub-models could be generated using existing data streams on smartphones, including self-reports (although self-report data increases user burden and therefore may not be possible to collect as intensively as sensor-based data). Hybrid interventions may be possible by combining established approaches to tailoring messages using a generalized decision rule and a computational approach based on a personalized mathematical model (and decision rule). For example, user’s reports about their motivation or affective experience on a given day could be used to determine relevant sub-models for controlling intervention delivery.
Text message intervention responses were quite idiosyncratic. Some people increased their movement time in response to messages to “move more;” others increased their movement time in response to messages to “sit less.” Some individuals responded quickly; others responded slowly or not at all. The size and duration of responses also varied. To the best of our knowledge, these idiosyncratic response patterns have been treated as error variance in prior models of text message interventions. System identification provides a new method for revealing individual response patterns. This information can be used to guide the selection and timing of interventions.
Future work should extend this system identification work by applying robust control tools for effective control design in the presence of uncertainty. The models identified in the first stage (system identification) along with the uncertainty descriptions can used to design controllers that maximize the probability of achieving a desired goal while avoiding unsafe or ineffective operating regions. Given that the model obtained is piecewise linear, these controllers will be piecewise linear or non-linear (i.e., separate sub-models of control for weekend and weekday physical activity). For a physical activity controller, the unsafe/ineffective operating regions would be defined as states where exercise might be unsafe or where one is very far from the objectives and at the same time treatment is ineffective (e.g., times when goal discrepancies are large and necessary intervention burden would be excessive, or when participants are simply unlikely to respond to intervention, such as during work hours). Tradeoffs between performance and computational complexity of the resulting controller should be studied in order to develop a controller that is effective and can be deployed without unduly impacting user experience. For example, elaborate controllers could detract from user experience by consuming excessive memory on mobile devices, slowing their processors and draining batteries rapidly (Kim, Agrawal, & Ungureanu, 2012). Users could also be unsettled by overly personalized messages that are construed as privacy violations (John, Kim, & Barasz, 2018). Future work will need to investigate the optimal model complexity for reducing uncertainty in the model while maintaining an acceptable user experience.
If a generic system identification model is used to develop a controller for intervention delivery, the controller could be refined as participants’ responses are observed. This process of adaptation involves using newly-collected data to update the models and the corresponding controller. The initial controller deployed provides a “warm start” for intervention based on the model identified from data based on a similar population-based sample in the previous stages. Being a population-based model, it will fit the behavior of some participants better than others. The purpose of adaptation is to progressively refine the intervention (i.e., controller) as the system learns participant responses to treatment and adapts to changes in behavior (including changes due to participants habituating to certain messages or become fatigued with messaging in general). Thus, periodic (e.g., monthly) updates to the controller could reflect the refined and increasingly personalized models over time. Throughout this process, it is imperative to evaluate acceptability and feasibility of more and less aggressive adaptation strategies by comparing their impact on user experience.
The ethical implications of using rich, potentially identifiable information to develop personalized models of physical activity warrants careful consideration. The model in this paper was relatively simple but future applications may draw on a person’s location, audio samples, communication logs, social media traces or other identifiable information. Digital tools for health and wellness promotion have a poor record of protecting user privacy with even simple steps such as data encryption (Huckvale, Prieto, Tilney, Benghozi, & Car, 2015). Without careful handling, this information may have unintended consequences for participants or members of their social networks. The policies of many institutional review boards have not kept pace with the emerging applications of mobile technologies for health behavior interventions; thus, researchers bear a special responsibility for considering the ethical dimension of mobile health interventions. Fortunately, resources are emerging (such as the Connected and Open Research Ethics initiative) to assist researchers and administrators navigate the emerging ethical and regulatory challenges in this work (Torous & Nebeker, 2017).
Control systems engineering is a relatively new influence on behavioral intervention design. These tools may help to realize the vision of precision medicine for lifestyle behavior change. Yet this approach is still very much in a proof-of-concept phase. Feasibility of the approach needs to be evaluated with larger and more diverse samples. Efficacy needs to be evaluated against appropriate control groups (e.g., interventions for unrelated behaviors, generic physical activity messaging interventions on a fixed- or random-schedule). If results are promising, the computational approach will need to be compared with other adaptive intervention approaches (e.g., tailored messages based on user-reported preferences for message content or timing; see Smyth & Heron, 2016). Model complexity will be an important consideration in this work. It will be important to identify the necessary and sufficient set of information for developing personalized interventions that outperform less sophisticated tailoring approaches. Some people may respond to a generic or established tailoring approach as well as or better than they do to a sophisticated, computationally-intensive tailoring approach. For such people, it would be quite appropriate to use approaches that do not require learning or adaptation to achieve peak effects. If participant characteristics that predict which tailoring approach will be most effective can be identified, then those characteristics could be used to recommend optimal intervention approaches. Benefit-cost analyses will also be an important part of these evaluations. Finally, it is possible that personalized interventions should be implemented differently in worksite health programs compared to direct-to-consumer wearable devices. Factors that influence effective dissemination and implementation of interventions developed using this approach will need to be identified.
The approach demonstrated in this paper provides a new tool with unique potential for improving mobile physical activity interventions. It also has important limitations. First, the study demonstrated proof-of-concept only. It did not evaluate the efficacy of the intervention, and it is not clear that this approach is more efficacious that simpler approaches with ad hoc decision rules. Second, the sample that provided study data was small and not representative of the broader population. It is not clear that treatment responses will be as heterogeneous in specific populations (e.g., patients with chronic disease) or for users in different social ecologies. Third, the model was relatively simple and characterized by high levels of uncertainty. Future work should expand the range of inputs (factors that can be manipulated, e.g., message delivery) and include better assessments of perturbations (factors that cannot be manipulated, e.g., weather) to reduce uncertainty. Fourth, messages were delivered at an unusually high frequency in this study; message pile-up was not factored into the system identification model so estimates of cumulative responses may be inflated. Finally, the focus here was on movement time and different models should be considered for other measures, such as step counts or intensityspecific duration (e.g., moderate-to-vigorous physical activity) and other behaviors (e.g., diet, smoking).
In summary, this paper provided proof-of-concept for the application of control systems engineering methods – specifically system identification – to develop personalized models of behavioral responses to text messages. This model included a limited number of inputs so model uncertainty is larger than desired. Future work should enrich this model by incorporating additional inputs to reduce uncertainty while using new methods (e.g., using the concept of sparsity to determine low complexity models that describe behavior) to safeguard against overfitting. These models provide a foundation for developing controllers that can select and time messages to achieve behavior change goals more efficiently. These controllers can also be adapted over time to create personalized treatment policies.
Highlights.
Customizing messaging interventions has not increased effects on physical activity.
Tools from control systems engineering can be applied to model behavior change.
Behavioral responses to physical activity messages are largely idiosyncratic.
Different decision rules can trigger different interventions for different people.
Acknowledgments
Funding for this research was made possible by grants from the Penn State Social Science Research Institute, the National Science Foundation (CNS 1329422), and the National Institutes of Health (P50 DA039838). The content is solely the responsibility of the authors and does not necessarily represent the official views of the Social Science Research institute, the National Science Foundation or the National Institutes of Health. The authors have no conflicts to disclose.
Appendix: Dynamic Modelling of Stepping Time as a Function of Messaging
In this paper, we have argued that stepping time behavior is dynamic. To model such a type of behavior we used affine time difference equations. These equations provide a mathematical model for the fact that stepping behavior is not “instantaneous” and that interventions can have a delayed onset, a prolonged effect, or both.
In this appendix, a mathematical description of this model is provided. All modeling was performed using MATLAB (MathWorks®, Natick, MA). The models used are individual models so we concentrate on how to determine a model for a specific participant. Moreover, for simplicity, we only show how to determine the model for weekdays’ stepping behavior. Computing the model for weekend behavior can be done in a similar way. The weekend and weekday models can then be combined to describe the participant’s behavioral patterns across the week. The following notation is used throughout this appendix
| T | Time interval size equal to 15 minutes |
|---|---|
| S(t) | Percentage of time spent stepping by the participant in the time interval between t and t + T, where this time interval is assumed to be in a weekday |
| TxtMM(t) | Equal to one if move more text message is received by the participant in the time interval between t and t + T. Zero otherwise |
| TxtSL(t) | Equal to one if sit less text message is received by the participant in the time interval between t and t + T. Zero otherwise |
| TxtGEN(t) | Equal to one if general facts text message is received by the participant in the time interval between t and t + T. Zero otherwise |
The time-difference model used in this paper is of the form
where ϵ(t) is the error in the model assumed to be zero mean Gaussian with unknown variance and a0,…, a5, b0,…, b5, c0l…, c5l d0,…, d5 are coefficients to be determined from the data collected. Note that the model above is of order 5. The choice of the model order was done by performing a careful trade-off between model complexity and size of the model error.
determine the coefficients of the model, we started by defining error function Err(a0,…, a5, b0, …, b5, c0, …, c5, d0, …, d5)
where the sum above is taken over values of t for which there are five consecutive measures of stepping time available. Then, the coefficients a0,…, a5, b0,…, b5, c0,…, c5, d0,…, d5 were found
by minimizing the above Err function.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
David E. Conroy, Department of Kinesiology and Human Development and Family Studies, The Pennsylvania State University; Department of Preventive Medicine, Northwestern University
Sarah Hojjatinia, Department of Electrical Engineering, The Pennsylvania State University.
Constantino M. Lagoa, Department of Electrical Engineering, The Pennsylvania State University
Chih-Hsiang Yang, Department of Kinesiology, The Pennsylvania State University; Department of Preventive Medicine, University of Southern California.
Stephanie T. Lanza, Department of Biobehavioral Health, The Pennsylvania State University
Joshua M. Smyth, Department of Biobehavioral Health, The Pennsylvania State University
References
- Armanasco AA, Miller YD, Fjeldsoe BS, & Marshall AL (2017). Preventive health behavior change text message interventions: A meta-analysis. American Journal of Preventive Medicine, 52(3), 391–402. 10.1016/j.amepre.2016.10.042 [DOI] [PubMed] [Google Scholar]
- Ashour M, Bekiroglu K, Yang CH, Lagoa C, Conroy D, Smyth J, & Lanza S (2016). On the mathematical modeling of the effect of treatment on human physical activity In 2016 IEEE Conference on Control Applications (CCA) (pp. 1084–1091). 10.1109/CCA.2016.7587951 [DOI] [Google Scholar]
- Bandura A (1997). Self-efficacy: The exercise of control (1st edition). New York: Worth Publishers. [Google Scholar]
- Bandura A (2004). Health promotion by social cognitive means. Health Education & Behavior, 31(2), 143–164. 10.1177/1090198104263660 [DOI] [PubMed] [Google Scholar]
- Bekiroglu K, Lagoa C, Murphy SA, & Lanza ST (2017). Control engineering methods for the design of robust behavioral treatments. IEEE Transactions on Control Systems Technology, 25(3), 979–990. 10.1109/TCST.2016.2580661 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borsboom D, Mellenbergh GJ, & van Heerden J (2003). The theoretical status of latent variables. Psychological Review, 110(2), 203–219. [DOI] [PubMed] [Google Scholar]
- Brownell KD (1986). Public health approaches to obesity and its management. Annual Review of Public Health, 7, 521–533. 10.1146/annurev.pu.07.050186.002513 [DOI] [PubMed] [Google Scholar]
- Chan CB, & Ryan DA (2009). Assessing the effects of weather conditions on physical activity participation using objective measures. International Journal of Environmental Research and Public Health, 6(10), 2639–2654. 10.3390/ijerph6102639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cole-Lewis H, & Kershaw T (2010). Text messaging as a tool for behavior change in disease prevention and management. Epidemiologic Reviews, 32(1), 56–69. 10.1093/epirev/mxq004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conn VS, Hafdahl AR, & Mehr DR (2011). Interventions to increase physical activity among healthy adults: Meta-analysis of outcomes. American Journal of Public Health, 101(4), 751–758. 10.2105/AJPH.2010.194381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conroy DE, Elavsky S, Maher JP, & Doerksen SE (2013). A daily process analysis of intentions and physical activity in college students. Journal of Sport & Exercise Psychology, 35, 493–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conroy DE, Maher JP, Elavsky S, Hyde AL, & Doerksen SE (2013). Sedentary behavior as a daily process regulated by habits and intentions. Health Psychology, 32(11), 1149–1157. 10.1037/a0031629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conroy DE, Yang C-H, Smyth JM, Lanza ST, & Lagoa CM (2018). Temporal dynamics of treatment receipt in a text message intervention for physical activity Unpublished manuscript, University Park, PA: The Pennsylvania State University. [Google Scholar]
- Dong Y, Deshpande S, Rivera DE, Downs DS, & Savage JS (2014). Hybrid model predictive control for sequential decision policies in adaptive behavioral interventions. Proceedings of the American Control Conference, 2014, 4198–4203. 10.1109/ACC.2014.6859462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunton GF, & Atienza AA (2009). The need for time-intensive information in healthful eating and physical activity research: a timely topic. Journal of the American Dietetic Association, 109(1), 30–35. 10.1016/j.jada.2008.10.019 [DOI] [PubMed] [Google Scholar]
- Fjeldsoe BS, Marshall AL, & Miller YD (2009). Behavior change interventions delivered by mobile telephone short-message service. American Journal of Preventive Medicine, 36(2), 165–173. 10.1016/j.amepre.2008.09.040 [DOI] [PubMed] [Google Scholar]
- Goldstein SP, Evans BC, Flack D, Juarascio A, Manasse S, Zhang F, & Forman EM (2017). Return of the JITAI: Applying a just-in-time adaptive intervention framework to the development of m-Health solutions for addictive behaviors. International Journal of Behavioral Medicine. 10.1007/s12529-016-9627-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo P, Rivera DE, Downs DS, & Savage JS (2016). Semi-physical identification and state estimation of energy intake for interventions to manage gestational weight gain. Proceedings of the American Control Conference, 2016, 1271–1276. 10.1109/ACC.2016.7525092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hallal PC, Andersen LB, Bull FC, Guthold R, Haskell W, Ekelund U, & Lancet Physical Activity Series Working Group. (2012). Global physical activity levels: surveillance progress, pitfalls, and prospects. Lancet, 380(9838), 247–257. 10.1016/S0140-6736(12)60646-1 [DOI] [PubMed] [Google Scholar]
- Heckman BW, Mathew AR, & Carpenter MJ (2015). Treatment burden and treatment fatigue as barriers to health. Current Opinion in Psychology, 5, 31–36. 10.1016/j.copsyc.2015.03.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hekler EB, Klasnja P, Riley WT, Buman MP, Huberty J, Rivera DE, & Martin CA (2016). Agile science: Creating useful products for behavior change in the real world. Translational Behavioral Medicine, 6(2), 317–328. 10.1007/s13142-016-0395-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hekler EB, Michie S, Pavel M, Rivera DE, Collins LM, Jimison HB, Spruijt-Metz D (2016). Advancing models and theories for digital behavior change interventions. American Journal of Preventive Medicine, 51(5), 825–832. 10.1016/j.amepre.2016.06.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heron KE, & Smyth JM (2010). Ecological momentary interventions: Incorporating mobile technology into psychosocial and health behaviour treatments. British Journal of Health Psychology, 15(Pt 1), 1–39. 10.1348/135910709X466063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huckvale K, Prieto JT, Tilney M, Benghozi P-J, & Car J (2015). Unaddressed privacy risks in accredited health and wellness apps: A cross-sectional systematic assessment. BMC Medicine, 13 10.1186/s12916-015-0444-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jakicic JM, Tate DF, Lang W, Davis KK, Polzien K, Rickman AD, … Finkelstein EA (2012). Effect of a stepped-care intervention approach on weight loss in adults: A randomized clinical trial. JAMA, 307(24), 2617–2626. 10.1001/jama.2012.6866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- John LK, Kim T, & Barasz K (2018). Ads that don’t overstep. Harvard Business Review, 96(1), 62–69. [Google Scholar]
- Kim H, Agrawal N, & Ungureanu C (2012). Revisiting storage for smartphones. Trans. Storage, 8(4), 14:1–14:25. 10.1145/2385603.2385607 [DOI] [Google Scholar]
- Klasnja P, Hekler EB, Shiffman S, Boruvka A, Almirall D, Tewari A, & Murphy SA (2015). Microrandomized trials: An experimental design for developing just-in-time adaptive interventions. Health Psychology, 34 Suppl, 1220–1228. 10.1037/hea0000305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korinek EV, Phatak SS, Martin CA, Freigoun MT, Rivera DE, Adams MA, … Hekler EB (2017). Adaptive step goals and rewards: A longitudinal growth model of daily steps for a smartphone-based walking intervention. Journal of Behavioral Medicine. 10.1007/s10865-017-9878-3 [DOI] [PubMed] [Google Scholar]
- Kreuter MW, & Skinner CS (2000). Tailoring: What’s in a name? Health Education Research, 15(1), 1–4. [DOI] [PubMed] [Google Scholar]
- Kukreja SL, Löfberg J, & Brenner MJ (2006). A least absolute shrinkage and selection operator (LASSO) for nonlinear system identification. IFAC Proceedings Volumes, 39(1), 814–819. 10.3182/20060329-3-AU-2901.00128 [DOI] [Google Scholar]
- Kumar S, Abowd GD, Abraham WT, al’Absi M, Beck JG, Chau DH, … Wetter DW (2015). Center of excellence for mobile sensor data-to-knowledge (MD2K). Journal of the American Medical Informatics Association: JAMIA, 22(6), 1137–1142. 10.1093/jamia/ocv056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar S, Nilsen WJ, Abernethy A, Atienza A, Patrick K, Pavel M, … Swendeman D (2013). Mobile health technology evaluation: The mHealth evidence workshop. American Journal of Preventive Medicine, 45(2), 228–236. 10.1016/j.amepre.2013.03.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lagoa CM, Bekiroglu K, Lanza ST, & Murphy SA (2014). Designing adaptive intensive interventions using methods from engineering. Journal of Consulting and Clinical Psychology, 82(5), 868–878. 10.1037/a0037736 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lei H, Nahum-Shani I, Lynch K, Oslin D, & Murphy SA (2012). A “SMART” design for building individualized treatment sequences. Annual Review of Clinical Psychology, 8, 21–48. 10.1146/annurev-clinpsy-032511-143152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo Y, Lee B, Wohn DY, Rebar AL, Conroy DE, & Choe EK (2018). Time for break: Understanding information workers’ sedentary behavior through a break prompting system In Proceedings of the 2018 CHI Conference on Human Factors in Computing Systems (pp. 127:1–127:14). New York, NY, USA: ACM; 10.1145/3173574.3173701 [DOI] [Google Scholar]
- Martín CA, Rivera DE, Riley WT, Hekler EB, Buman MP, Adams MA, & King AC (2014). A dynamical systems model of social cognitive theory. Proceedings of the American Control Conference, 2407–2412. [Google Scholar]
- Martin KR, Koster A, Murphy RA, Van Domelen DR, Hung M, Brychta RJ, … Harris TB (2014). Changes in daily activity patterns with age in U.S. men and women: National Health and Nutrition Examination Survey 2003–04 and 2005–06. Journal of the American Geriatrics Society, 62(7), 1263–1271. 10.1111/jgs.12893 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McAuley E, & Blissmer B (2000). Self-efficacy determinants and consequences of physical activity. Exercise and Sport Sciences Reviews, 28(2), 85–88. [PubMed] [Google Scholar]
- Nahum-Shani I, Hekler EB, & Spruijt-Metz D (2015). Building health behavior models to guide the development of just-in-time adaptive interventions: A pragmatic framework. Health Psychology, 34, 1209–1219. 10.1037/hea0000306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nahum-Shani I, Smith SN, Spring BJ, Collins LM, Witkiewitz K, Tewari A, & Murphy SA (2016). Just-in-time adaptive interventions (JITAIs) in mobile health: Key components and design principles for ongoing health behavior support. Annals of Behavioral Medicine. 10.1007/s12160-016-9830-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Napolitano MA, & Marcus BH (2002). Targeting and tailoring physical activity information using print and information technologies. Exercise and Sport Sciences Reviews, 30(3), 122–128. [DOI] [PubMed] [Google Scholar]
- Nilsen W, Kumar S, Shar A, Varoquiers C, Wiley T, Riley WT, … Atienza AA (2012). Advancing the science of mHealth. Journal of Health Communication, 17 Suppl 1, 5–10. 10.1080/10810730.2012.677394 [DOI] [PubMed] [Google Scholar]
- Owen N, Sugiyama T, Eakin EE, Gardiner PA, Tremblay MS, & Sallis JF (2011). Adults’ sedentary behavior: Determinants and interventions. American Journal of Preventive Medicine, 41(2), 189–196. https://doi.org/10.1016Zj.amepre.2011.05.013 [DOI] [PubMed] [Google Scholar]
- Pirolli P (2016). A computational cognitive model of self-efficacy and daily adherence in mHealth. Translational Behavioral Medicine, 6(4), 496–508. 10.1007/s13142-016-0391-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhodes RE, & Nigg CR (2011). Advancing physical activity theory. Exercise and Sport Sciences Reviews, 39(3), 113–119. 10.1097/JES.0b013e31821b94c8 [DOI] [PubMed] [Google Scholar]
- Riley WT, Martin CA, & Rivera DE (2014). The importance of behavior theory in control system modeling of physical activity sensor data. Conference Proceedings of the Annual International Conference of the IEEE Engineering in Medicine and Biology Society, 2014, 6880–6883. 10.1109/EMBC.2014.6945209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riley WT, Martin CA, Rivera DE, Hekler EB, Adams MA, Buman MP, … King AC (2016). Development of a dynamic computational model of social cognitive theory. Translational Behavioral Medicine, 6(4), 483–495. 10.1007/s13142-015-0356-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riley WT, Rivera DE, Atienza AA, Nilsen W, Allison SM, & Mermelstein R (2011). Health behavior models in the age of mobile interventions: Are our theories up to the task? Translational Behavioral Medicine, 1(1), 53–71. 10.1007/s13142-011-0021-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sallis JF, Owen N, & Fisher EB (2008). Ecological models of health behavior In Health behavior and health education: Theory, research, and practice (4th ed.). San Francisco, CA: Jossey-Bass. [Google Scholar]
- Savage JS, Downs DS, Dong Y, & Rivera DE (2014). Control systems engineering for optimizing a prenatal weight gain intervention to regulate infant birth weight. American Journal of Public Health, 104(7), 1247–1254. 10.2105/AJPH.2014.301959 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmid KL, Rivers SE, Latimer AE, & Salovey P (2008). Targeting or tailoring? Maximizing resources to create effective health communications. Marketing Health Services, 28(1), 32–37. [PMC free article] [PubMed] [Google Scholar]
- Seefeldt V, Malina RM, & Clark MA (2002). Factors affecting levels of physical activity in adults. Sports Medicine, 32(3), 143–168. [DOI] [PubMed] [Google Scholar]
- Sherwood NE, Butryn ML, Forman EM, Almirall D, Seburg EM, Lauren Crain A, … Jeffery RW (2016). The BestFIT trial: A SMART approach to developing individualized weight loss treatments. Contemporary Clinical Trials, 47, 209–216. 10.1016/j.cct.2016.01.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiffman S, Balabanis MH, Paty JA, Engberg J, Gwaltney CJ, Liu KS, … Paton SM (2000). Dynamic effects of self-efficacy on smoking lapse and relapse. Health Psychology, 19(4), 315–323. [DOI] [PubMed] [Google Scholar]
- Shiffman S, Hickcox M, Paty JA, Gnys M, Kassel JD, & Richards TJ (1996). Progression from a smoking lapse to relapse: Prediction from abstinence violation effects, nicotine dependence, and lapse characteristics. Journal of Consulting and Clinical Psychology, 64(5), 993–1002. [DOI] [PubMed] [Google Scholar]
- Shiffman S, Paty JA, Gnys M, Kassel JA, & Hickcox M (1996). First lapses to smoking: Within-subjects analysis of real-time reports. Journal of Consulting and Clinical Psychology, 64(2), 366–379. [DOI] [PubMed] [Google Scholar]
- Smyth, & Heron. (2016). Is providing mobile interventions “just-in-time” helpful? An experimental proof of concept study of just-in-time intervention for stress management. In 2016 IEEE Wireless Health (WH) (pp. 1–7). 10.1109/WH.2016.7764561 [DOI] [Google Scholar]
- Spruijt-Metz D, Hekler E, Saranummi N, Intille S, Korhonen I, Nilsen W, … Pavel M (2015). Building new computational models to support health behavior change and maintenance: New opportunities in behavioral research. Translational Behavioral Medicine, 5(3), 335–346. 10.1007/s13142-015-0324-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas JG, & Bond DS (2015). Behavioral response to a just-in-time adaptive intervention (JITAI) to reduce sedentary behavior in obese adults: Implications for JITAI optimization. Health Psychology, 34 Suppl, 1261–1267. 10.1037/hea0000304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Timms KP, Martin CA, Rivera DE, Hekler EB, & Riley W (2014). Leveraging intensive longitudinal data to better understand health behaviors. Conference Proceedings of the Annual International Conference of the IEEE Engineering in Medicine and Biology Society, 2014, 6888–6891. 10.1109/EMBC.2014.6945211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Timms KP, Rivera DE, Collins LM, & Piper ME (2013). Control systems engineering for understanding and optimizing smoking cessation interventions. Proceedings of the American Control Conference, 1964–1969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Timms KP, Rivera DE, Collins LM, & Piper ME (2014). Continuous-time system identification of a smoking cessation intervention. International Journal of Control, 87(7), 1423–1437. 10.1080/00207179.2013.874080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Timms KP, Rivera DE, Piper ME, & Collins LM (2014). A hybrid model predictive control strategy for optimizing a smoking cessation intervention. Proceedings of the American Control Conference, 2014, 2389–2394. 10.1109/ACC.2014.6859466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torous J, & Nebeker C (2017). Navigating ethics in the digital age: Introducing Connected and Open Research Ethics (CORE), a tool for researchers and institutional review boards. Journal of Medical Internet Research, 19(2), e38 10.2196/jmir.6793 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang W, & Rivera DE (2008). Model predictive control for tactical decision-making in semiconductor manufacturing supply chain management. IEEE Transactions on Control Systems Technology, 16(5), 841–855. 10.1109/TCST.2007.916327 [DOI] [Google Scholar]
- Wang W, Rivera DE, & Kempf KG (2007). Model predictive control strategies for supply chain management in semiconductor manufacturing. International Journal of Production Economics, 107(1), 56–77. [Google Scholar]
- Young MD, Plotnikoff RC, Collins CE, Callister R, & Morgan PJ (2014). Social cognitive theory and physical activity: A systematic review and meta-analysis. Obesity Reviews, 15(12), 983–995. 10.1111/obr.12225 [DOI] [PubMed] [Google Scholar]


