Introduction
Cardiovascular disease (CVD) remains a highly prevalent cause of morbidity and mortality, both in the United States and worldwide. In parallel with the development of new and improved therapies for established CVD such as coronary artery disease or heart failure (HF), there has been an increased focus on modification of cardiovascular risk factors for both primary and secondary prevention, reflecting an evolving understanding of CVD as a systemic process with numerous determinants.
Obstructive sleep apnea (OSA) has been associated with many different forms of CVD including hypertension, stroke, HF, coronary artery disease, and atrial fibrillation (AF).1 Adults with OSA not only have an increased risk of developing comorbid CVD but also have worse outcomes related to CVD. OSA is highly prevalent, estimated to affect 34% of men and 17% of women in the general population2 and 40% to 60% of patients with CVD.3, 4 Furthermore, the prevalence is increasing, with these figures representing a 30% increase over the previous 2 decades,2 likely related to the obesity epidemic as well as an aging population.
Despite the clear association between CVD and OSA, randomized trials have failed to demonstrate that treatment of sleep apnea improves hard cardiovascular outcomes in patients with established CVD.5 Nevertheless, this area remains controversial, as randomized trials performed to date remain limited in number as well as design, highlighting the need for further study.6 Furthermore, the current literature suggests that the impact of diagnosing and treating OSA varies between specific CVD processes, implying the need for a more sophisticated understanding and nuanced clinical approach to this issue. In this article we review the literature pertaining to OSA in patients with CVD. Additionally, we offer a practical clinical approach to the evaluation and management of known or suspected OSA in patients with CVD consisting of recommendations integrated from several separate societal practice guidelines combined with several of our own suggestions on issues not addressed by current guidelines, based on our own clinical experience and best available literature.
Overview of Sleep Apnea
Definition
Sleep apnea is characterized by repetitive episodes of apnea occurring during sleep. An apnea is defined as a cessation of inspiratory airflow lasting 10 seconds or more, while the term hypopnea refers to a reduction in inspiratory airflow (by at least 30%) lasting 10 seconds or more with an associated drop in oxygen saturation or arousal from sleep.7 The steps required for a successful inspiratory cycle include activation of a signal from the regulatory brainstem center, transmission of the signal via peripheral nerves, activation of respiratory muscles to produce negative intrathoracic pressure, and a patent airway. The mechanism for apneas or hypopneas can be either obstructive, in which airflow cessation results despite inspiratory effort because of blockage within the upper airways, or central, in which both airflow and inspiratory efforts are absent. The term sleep‐disordered breathing (SDB) encompasses OSA, central (CSA), and mixed apnea, the latter of which shows absent respiratory effort initially and clear effort with obstruction and the end of mixed apnea.
Important risk factors for OSA include obesity, craniofacial or oropharyngeal anatomic abnormalities, male sex, and smoking.8 During sleep, there is a reduction in tone of the dilator muscles involved in maintaining airway patency. In particular, relaxation of the genioglossus muscle allows the tongue to fall posteriorly within the pharynx, facilitating obstruction in susceptible individuals.9 Anatomic factors including obesity that result in relative narrowing of the airway lumen increase the likelihood of obstruction. The observation that OSA also affects nonobese patients without identifiable anatomic abnormalities indicates that nonanatomic mechanisms are important as well. Examples of these include ventilatory control instability10 and reduced sleep arousal threshold.11 The relative contribution from these processes varies between individual patients, with potential therapeutic implications. A better understanding of the mechanisms underlying OSA could facilitate more personalized therapeutic strategies in the future.
CSA results from transient failure of respiratory control centers in the medulla to trigger inspiration. The primary mechanism is thought to be abnormal regulation of the apneic threshold, the partial pressure of CO2 below which respiration is suppressed, although depending on the underlying cause CSA patients can be either hypercapnic, eucapnic, or hypocapnic.9 HF is one of the leading causes of CSA, associated in particular with Cheyne‐Stokes breathing, which is characterized by cyclic crescendo‐decrescendo respiratory efforts and hypocapnia.12
Evaluation and Diagnosis
The evaluation for sleep apnea begins with a comprehensive sleep assessment, which includes a thorough clinical history documenting signs or symptoms, such as excessive daytime sleepiness, morning headaches, snoring, witnessed apnea, or difficulty concentrating, a physical examination, and a review of the medical history for relevant comorbidities and other risk factors13 (Table 1). Patients with suspected sleep apnea following this assessment should undergo diagnostic testing, the criterion standard of which is polysomnography. Treatment of OSA is generally reserved for those individuals with an apnea–hypopnea index (AHI; the number of apneas and hypopneas observed per hour) ≥5 measured during sleep study in patients with either signs/symptoms of sleep apnea or associated medical conditions (including hypertension, HF, coronary artery disease, significant arrhythmias, and other forms of CVD). Alternatively, an AHI ≥15 is often treated as OSA even in the absence of signs, symptoms, or associated medical conditions.14 Severity is also determined using the AHI, with 5 to 14 considered mild, 15 to 30 moderate, and >30 severe disease. Significant night‐to‐night variability of AHI has been observed in studies of consecutive night polysomnography, with 7% to 25% of patients meeting diagnostic criteria for moderate‐to‐severe OSA the second night despite a negative result the previous evening.15 Current guidelines therefore recommend repeating polysomnography in patients with a negative initial study when clinical suspicion of OSA remains high.16
Table 1.
Signs and Symptoms of Obstructive Sleep Apnea
| Snoring |
| Witnessed apneas by sleep partner |
| Episodes of gasping or choking during sleep |
| Insomnia with repeated awakenings |
| Excessive daytime sleepiness |
| Nonrefreshing sleep |
| Morning headaches |
| Difficulty concentrating |
| Memory impairment |
| Irritability and/or mood changes |
| Nocturia |
| Decreased libido and/or erectile dysfunction |
Home sleep apnea testing (HSAT) using a portable monitoring device is a reasonable alternative testing strategy. Several HSAT devices exist, all of which measure heart rate and oximetry with some also measuring nasal pressure, chest and abdominal plethysmography, and/or peripheral arterial tonometry. Compared with polysomnography, the diagnostic accuracy of HSAT is lower and, importantly, varies depending on the population studied and diagnostic criteria used.17, 18, 19 Despite these caveats, HSAT represents a viable alternative to polysomnography in select circumstances and is recommended for diagnosis of OSA in uncomplicated patients with an increased risk of moderate‐to‐severe OSA.7 Given its limited sensitivity and the potential consequences of false‐negative results, negative or nondiagnostic studies should be followed up with polysomnography. Furthermore, patients at risk for central or mixed sleep apnea (significant cardiopulmonary disease, chronic opioid use, history of stroke, or neuromuscular disorders with potential respiratory muscle involvement) or other nonrespiratory sleep disorders requiring evaluation should undergo polysomnography rather than HSAT,16 because the diagnostic accuracy of the latter for central apneas has not been validated.
Because a single night of HSAT is less resource intensive than a single full night of polysomnography, reduced cost has been cited as a potential benefit of increasing HSAT use in diagnosing OSA. Several economic analyses comparing the cost effectiveness of HSAT with full‐ or split‐night polysomnography in adults with suspected moderate to severe OSA instead found full‐night polysomnography to be the preferred testing modality.20, 21 Increased costs related to repeat testing and false‐negative HSAT results account for these findings. A major caveat of these analyses is the potential for error related to imprecisions of modeling a clinical diagnostic pathway and limitations in the quality of real‐world data available to calibrate their models. Only 1 study published to date has analyzed relative cost effectiveness of various diagnostic modalities using measurement of real‐world resource utilization in the context of a randomized controlled trial (RCT). Using data from the HomePAP trial, Kim et al found that in 373 patients at risk for moderate‐to‐severe OSA, a home‐based testing pathway resulted in significantly lower costs to the payer than a laboratory‐based polysomnography pathway ($1575 versus $1840, P=0.02).22 Therefore, use of HSAT in appropriately selected patients with suspected OSA may have the potential to reduce costs; however, providers must recognize that extending HSAT use to other populations, in particular low‐risk patients, may actually increase overall costs because of more frequent follow‐up testing.
Several clinical questionnaires and prediction tools have been developed to aid in the evaluation of OSA, such as the STOP‐BANG questionnaire, the Epworth Sleepiness Scale, and the Berlin Questionnaire (Table 2). These clinical tools were designed to provide a standardized assessment approach that can be performed relatively quickly in the outpatient setting, either in sleep centers or in primary care clinics. While offering the advantage of being quick, convenient, and inexpensive, studies evaluating the diagnostic accuracy of such clinical tools in comparison with polysomnography or HSAT have demonstrated inadequate sensitivity and specificity.7 Accordingly, clinical assessment prediction tools are not currently recommended for the diagnosis of OSA in the absence of polysomnography or HSAT. They can, however, play a useful role as adjunctive tools in the screening process or aid in assessment of treatment efficacy during long‐term follow‐up of patients with OSA.
Table 2.
Summary of Clinical Obstructive Sleep Apnea Questionnaires
| Questionnaire | Summary of Questionnaire Contents | Diagnostic Accuracy Compared With AHI (>15 events/h)16 |
|---|---|---|
| Berlin Questionnaire |
10 questions pertaining to the following 3 symptoms/signs:
Patients classified by score as having low risk or high risk of OSA |
|
| STOP Questionnaire |
4 questions regarding the following signs/symptoms:
|
|
| STOP‐BANG Questionnaire |
4 questions regarding signs/symptoms plus 4 clinical attributes:
Patients classified as low, intermediate, or high risk for OSA |
|
| Epworth Sleepiness Scale |
8 questions asking patients to rate the likelihood of falling asleep in various daytime contexts Patients classified as having normal sleep, average sleepiness, or severe and possibly pathologic sleepiness |
|
AHI indicates apnea–hypopnea index; BMI, body mass index; OSA, obstructive sleep apnea.
Treatment
Effective management of OSA requires a comprehensive assessment of each individual patient's phenotype as well as long‐term follow‐up and monitoring. Behavioral, medical, dental, and surgical options exist for treatment of sleep apnea.
Positive airway pressure (PAP) therapy is a first‐line therapy for all patients diagnosed with obstructive sleep apnea and has been shown to both reduce the AHI23 and improve self‐reported sleepiness and quality of life.24 It is cost effective, with an estimated incremental cost‐effectiveness ratio of $15 915 per quality‐adjusted life year gained.20 The therapeutic mechanism of PAP is pneumatic splinting of the upper airway, thereby reducing airflow obstruction and apneic events. The 2 major PAP delivery modes are continuous positive airway pressure (CPAP) and bi‐level positive airway pressure. CPAP is the preferred first‐line modality in most patients with OSA, while bi‐level positive airway pressure is generally reserved for patients with OSA accompanied by hypoventilation syndromes, although it can also be used in patients with OSA alone who fail to tolerate CPAP and in some cases of CSA. The optimal settings are ideally determined via manual titration of PAP during full‐night polysomnography to a pressure that eliminates upper airway obstruction and remains tolerable to the patient. Alternatively, some patients undergo a split‐night study in which PAP titration is performed following the diagnostic portion of polysomnography. A split‐night study requires that a conclusive diagnosis of moderate‐to‐severe OSA be made with at least 3 hours remaining in the test to conduct PAP titration.
Auto‐titrating CPAP (APAP) is another option that offers the advantage of performing titration at home rather than in a sleep laboratory. In APAP, the clinician programs a pressure range, and the level of administered PAP is automatically adjusted throughout the night to the lowest pressure required to maintain upper airway patency using proprietary event‐detection software. Several randomized trials comparing fixed CPAP with APAP showed either no difference or, in some cases, a small advantage of APAP with respect to adherence rate, reduction in AHI, and improvement in sleepiness in cohorts with uncomplicated OSA.25, 26 Notably, patients with HF, chronic obstructive pulmonary disease or other form of significant lung disease, obesity hypoventilation syndrome, and SDB related to neuromuscular disease were excluded from these studies, and current guidelines recommend against use of APAP for either pressure titration or therapy in these patients.27
PAP therapy is an efficacious treatment of OSA; however, effectiveness can be limited by patient nonadherence, which is not uncommon and can be caused by a variety of factors.28 Strategies that may be effective for some patients in improving adherence with therapy include changing the mask interface (superior tolerability of the nasal interface has been suggested), adding humidification to the PAP circuit (effectiveness may be limited to those with nasal congestion), adding a chinstrap to the mask interface (which also appears to reduce air leak and residual AHI),29 and utilizing an APAP mode.24 Cognitive behavioral therapy aimed at improving patients’ self‐efficacy with respect to their health has been shown to increase adherence in several studies.28 Early assessment and prompt troubleshooting of any problems is extremely important following treatment initiation, because use during the first 2 weeks predicts long‐term adherence to therapy.23
Behavioral therapies for sleep apnea include weight loss, positional therapy, and avoidance of alcohol or other sedating agents (Table 3). Weight loss reduces the severity of OSA in most overweight patients, with a significant correlation between the magnitude of weight loss and the reduction in AHI.30, 31, 32 Weight loss can be either medical or surgical.33 Intensive lifestyle modifications and weight loss may reduce the risk of future cardiovascular events including mortality in overweight/obese patients via mechanisms unrelated to OSA34, 35 and therefore should be recommended to all such patients with OSA in addition to other therapies.36 Bariatric surgery is efficacious in terms of both weight loss and reduction in AHI and therefore should be considered in select obese patients with OSA.37 Although weight loss can reduce AHI, most patients will require some form of additional OSA therapy, because only 10% to 30% of patients have achieved an AHI <5 in medical or surgical weight loss trials.33
Table 3.
Behavioral Therapies for Obstructive Sleep Apnea
| Treatment | Patient Selection |
|---|---|
| Weight loss | All overweight or obese patients should be encouraged to lose weight, as adjunct to primary therapy |
| Positional therapy |
Can be used as either a secondary or adjunctive therapy in patients with significant reduction in nonsupine position as compared with supine Can be considered as primary therapy in select cases when normalization of AHI in a nonsupine position has been demonstrated by polysomnography and adherence can be assured |
| Avoidance of alcohol or other substances |
Patients should be encouraged to minimize alcohol intake Physicians should monitor for and avoid prescribing medications with potential to exacerbate sleep apnea, such as benzodiazepines, opiates, or other central nervous system depressants |
AHI indicates apnea–hypopnea index.
Positional therapy involves use of a positioning device to maintain a position other than supine during sleep, as supine positioning is associated with greater reductions in airway dimensions.38 The role of positional therapy is predominantly secondary, but it can be used as a supplemental primary therapy in patients demonstrated as having a low‐AHI when in a nonsupine position.39 It is estimated that >50% of all patients with an AHI >5 events/h have a positional component to their sleep apnea.40
Oral appliances, such as a mandibular advancement device and tongue‐retaining devices, work by mechanically enlarging the upper airway by displacing the tongue forward and reducing its collapsibility during sleep,41 mimicking the Jaw‐Thrust technique used by anesthesiologists to open the airway in sedated patients. Both the mandibular advancement device and tongue‐retaining devices increase cross‐sectional area of the airway at the level of the velopharynx and oropharynx, although the change in diameter is greater with tongue‐retaining devices than with the mandibular advancement device.42 Oral appliances are effective in reducing AHI in patients with OSA43 but are less efficacious than PAP therapy.41, 43 Baseline AHI ≥30 and maximum therapeutic CPAP pressure >12 mm Hg are predictive of oral appliance treatment failure (success defined by achieving either AHI <5, or 5≤ AHI <10 with >50% reduction from baseline), and thus these clinical features should be considered when selecting patients for oral appliance therapy.44 Oral appliances are recommended for treatment of primary snoring without OSA, and in mild‐to‐moderate OSA in cases where the patient strongly prefers to try an appliance over PAP therapy. They are also preferable compared with no therapy for primary snoring without OSA, or OSA of any severity in patients who are intolerant to or unwilling to try PAP therapy.43
Upper airway surgery is designed to address anatomic airway obstruction in the upper airway and consists of a variety of different techniques. Individual surgical procedures may be classified as nasal, upper pharyngeal, lower pharyngeal, or global upper airway depending on the anatomic level at which obstruction is targeted. Many patients have obstructive anatomy at multiple sites and require multilevel surgical correction, in which several procedures are performed either simultaneously or in a staged manner. Surgery can be considered as primary therapy for patients with primary snoring with OSA, in patients with mild‐to‐moderate OSA where they may supersede oral appliances, and in cases of obstructive anatomy where surgery would be considered highly effective, and as secondary therapy for patients with OSA who experience inadequate response to or cannot tolerate PAP therapy.39
Surgery is an effective management option for the treatment of OSA, with reported polysomnographic success rates (generally defined as a ≥50% reduction in AHI to an AHI value ≤20) of 35% to 83% in the literature.45, 46, 47, 48, 49 Limitations of the reported efficacy in the literature include significant heterogeneity of surgical technique as well as patient selection based on individual anatomic characteristics and surgeon preference. An overview of the different types of surgical procedures used to treat OSA along with reported efficacy of each technique is presented in Table 4.50 One particular form of surgery, hypoglossal nerve stimulation, has a growing body of literature supporting its efficacy. The STAR (Stimulation Treatment for Apnea Reduction) trial enrolled 126 patients with moderate‐to‐severe OSA who had difficulty adhering to CPAP and surgically implanted hypoglossal simulators.51 After 18 months, there was a 68% reduction in median AHI as well as improved scores on the Epworth Sleepiness Scale and Functional Outcomes of Sleep Questionnaire with only 2 serious adverse events reported throughout the trial.52
Table 4.
Overview of Surgical Procedures for Obstructive Sleep Apnea
| Anatomic Region | Specific Procedures | Outcomes |
|---|---|---|
| Nasal |
|
Significant 2.66 cm H2O reduction in required CPAP pressure (95% CI 1.67–3.65; P<0.00001) reported in meta‐analysis following nasal surgeries45
Average nightly CPAP use increased from 3.0±3.1 h preoperatively to 5.5±2.0 h following surgery |
| Upper pharyngeal |
|
Pooled polysomnographic success rate 50%a for UPPP in meta‐analyses; however, results from individual studies vary significantly, with success rates up to 83% in more selective cohorts50 |
| Lower pharyngeal |
|
Polysomnographic success rate ranges from 35% to 62% across studies of various hypopharyngeal procedures48 |
| Global upper airway procedures |
|
Pooled efficacy results from meta‐analyses of each procedure type: |
AHI indicates apnea–hypopnea index; CPAP, continuous positive airway pressure; MMA, maxillomandibular advancement; OSA, obstructive sleep apnea; UPPP, uvulopalatopharyngoplasty.
Polysomnographic success defined as ≥50% reduction from baseline AHI and postsurgical AHI <20 events/h.
Cure rate defined as postsurgical AHI <5 events/h.
Risks of upper airway surgery include those inherent to any surgical procedure such as bleeding, infection, and complications related to anesthesia. The latter category as well as perioperative cardiovascular complications are known to be higher in patients with OSA as compared with the general surgical population.53, 54 Additional risks vary according to the specific procedural technique utilized and include, but are not limited to, airway compromise, dysphagia, local anesthesia or paresis, vocal changes, globus sensation, and taste changes.55
Cardiovascular Conditions Associated With OSA
Resistant Hypertension
Of all the cardiovascular disease processes associated with OSA, the relationship with hypertension is the best established. Multiple observational studies have demonstrated this association,56, 57 and an influential study by Peppard et al, which followed 709 patients in the Wisconsin Sleep Cohort, found a linear, dose‐dependent relationship between the severity of OSA at baseline and the relative risk of developing hypertension during follow‐up.58 The relationship is particularly strong between OSA and resistant hypertension, commonly defined as inability to adequately control blood pressure despite use of 3 antihypertensive agents including a diuretic or adequate blood pressure control requiring ≥4 agents. For example, 1 study found the prevalence of OSA to be 71% in patients with resistant hypertension versus 38% in those with essential hypertension.59
Several randomized controlled trials have demonstrated a reduction in systemic blood pressure in patients treated with CPAP. A recent meta‐analysis of 5 randomized trials enrolling 457 total patients found a significant reduction in 24‐hour ambulatory blood pressure (4.78 mm Hg [95% CI, 1.61–7.95] systolic and 2.95 mm Hg [95% CI, 0.53–5.37] diastolic) as well as a mean nocturnal diastolic blood pressure (1.53 mm Hg [95% CI, 0–3.07]) in patients treated with CPAP.60 While the magnitude of this reduction was relatively modest, it has been shown that even small reductions in blood pressure confer reduced risk of adverse cardiovascular events.61 Based on these data, we believe that diagnostic testing is reasonable in all patients with resistant hypertension, including those without clear signs or symptoms of OSA.
Pulmonary Hypertension
OSA is strongly associated with pulmonary hypertension (PH) and may play a causative role in its pathophysiology. Whereas ≈10% to 20% of patients with moderate‐to‐severe OSA have coexisting PH,62 the prevalence of OSA in patients with PH diagnosed by right heart catheterization has been estimated to be 70% to 80%.63 Both hypercapnia and nocturnal episodes of hypoxia can trigger pulmonary arteriolar constriction leading to acute, reversible elevation in pulmonary artery pressures. Signaling pathways implicated in hypoxic vasoconstriction in PH include nitric oxide, endothelin, angiopoietin‐1, serotonin, and NADPH‐oxidase.64 Chronic hypoxia activates additional inflammatory pathways resulting in pulmonary vascular remodeling and, eventually, irreversible increases in pulmonary vascular resistance.65 Additional postulated mechanisms contributing to PH include increased right‐sided preload resulting from negative transthoracic pressure during periods of airway obstruction, generation of reactive oxygen species as well as endothelial dysfunction within the pulmonary vasculature.66 Echocardiographic evidence of right ventricular remodeling and dysfunction has been observed in association with OSA as well.67 In addition to direct mechanisms involving the pulmonary vasculature, OSA can lead to PH indirectly via contributing to left HF with associated postcapillary PH such as in patients with refractory hypertension.
Pulmonary hypertension resulting solely from OSA is generally mild; however, OSA can further exacerbate elevations in pulmonary artery pressures and pulmonary vascular resistance when superimposed on PH associated with other underlying causes. Importantly, the presence of OSA in patients found to have severe PH has been associated with increased mortality.68 Regarding the effects of OSA treatment in patients with PH, the current literature, while limited by small sample size and paucity of randomized trials, does suggest a benefit. Observational studies have demonstrated reduction in pulmonary vascular resistance in patients treated with CPAP.69 In the 1 randomized trial to date, treatment of OSA with CPAP was associated with a significant reduction in pulmonary artery systolic pressure (28.9 mm Hg versus 24 mm Hg) when compared with a sham device.70 Given the detrimental effects of sleep apnea in patients with PH and limited evidence suggesting a beneficial effect of CPAP, we recommend clinical screening of all PH patients for sleep apnea with a comprehensive sleep assessment. In addition, we believe that performing some form of diagnostic sleep testing in all patients with PH is reasonable. We generally perform overnight oximetry testing in patients felt to be at low risk of sleep apnea following comprehensive sleep assessment to exclude nocturnal hypoxemia. Patients with suspected sleep apnea based on the presence of SDB symptoms or risk factors, as well as patients found to have nocturnal hypoxemia on home testing, should be referred for formal polysomnography. This approach is in agreement with the recommendations provided by the ACCF/AHA 2009 Expert Consensus Document on Pulmonary Hypertension71 as well as the 2015 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension.72
Heart Failure
Sleep apnea is highly prevalent in patients with HF, with studies indicating a prevalence between 50% and 70%.73, 74 Notably, CSA accounts for approximately two thirds of the sleep apnea observed in this population, while OSA comprises a significant minority. An inverse relationship exists between the prevalence of CSA and both left ventricular ejection fraction and the clinical severity of HF.73 While CSA and OSA coexist in a significant proportion of cases, one acts as the dominant phenotype in the majority of patients.73 Because HSAT devices have not been validated to diagnose CSA, current guidelines recommend polysomnography as the preferred diagnostic modality for patients with HF.16 A single study of 53 inpatients with decompensated HF found a high concordance between AHI, classified as either obstructive or central, measured during concurrent polysomnography and HSAT monitoring, with correlation coefficients of 0.91 (95% CI, 0.84–0.95) and 0.98 (95% CI, 0.96–0.99), respectively,75 suggesting the potential of HSAT for a role in evaluating patients at risk for complicated SDB in the future pending further investigation.
Sleep apnea is prevalent in patients with asymptomatic left ventricular dysfunction as well as those with clinically overt HF, with 1 study diagnosing moderate‐to‐severe sleep apnea in 66% of patients with the former.76 Coexisting sleep apnea has been associated with increased risk of adverse outcomes, including mortality, in patients with HF.77, 78 Several pathophysiologic processes that result directly from apneic events may explain this association, including activation of the sympathetic nervous system79 as well as increased preload and afterload resulting from perturbation of intrathoracic pressure while attempting to inspire against occluded airways.80 Additional mechanisms by which sleep apnea may worsen outcomes in patients with HF include exacerbating systemic hypertension,81 increased risk of arrhythmias including sudden cardiac death,82 and an elevated risk of coronary events.83
Studies investigating the potential benefits of PAP therapy with respect to underlying heart failure in this patient population have been conflicting and ultimately disappointing. Several studies looking at surrogate end points suggested beneficial effects associated with PAP therapy in sleep apnea patients with HF. Reductions in sympathetic nervous system signaling have been observed in patients with both OSA and CSA treated with CPAP.84, 85 CPAP also reduces the pro‐arrhythmic state associated with OSA, having been shown to decrease ventricular ectopy86 as well as the risk of recurrent AF.87, 88 Furthermore, CPAP results in favorable hemodynamic effects, including improved left ventricular systolic89 and diastolic function90 in OSA patients with high wedge pressures.
These promising early studies prompted larger RCT looking at hard clinical end points, particularly in patients with predominant CSA. The CANPAP (Canadian Continuous Positive Airway Pressure for Patients with Central Sleep Apnea and Heart Failure) trial investigated the effect of CPAP treatment in patients with HF and CSA. No benefit was seen in the patients treated with CPAP; however, a post hoc analysis suggested a reduction in mortality among patients for whom CPAP therapy resulted in a significant improvement in AHI (to <15 events/h).91 While CPAP is effective in relieving obstructive events, many patients with HF have persistent central apneas and hypopneas despite therapy with appropriately titrated CPAP. Adaptive servoventilation (ASV) is a form of bi‐level positive airway pressure therapy in which the degree of pressure support (difference between inspiratory and expiratory pressures) varies between respiratory cycles in order to maintain stable minute ventilation. A backup rate is programmed to trigger breaths during periods of central apnea. This mode therefore offers a theoretic advantage in HF patients with Cheyne‐Stokes breathing, which is characterized by periods of hyperventilation, hypoventilation, and central apnea.92
The SAVIOR‐C (Study of the Effects of Adaptive Servo‐ventilation Therapy on Cardiac Function and Remodeling in Patients with Chronic Heart Failure) trial failed to show an improvement in ejection fraction or brain natriuretic peptide (BNP) level after 24 weeks of ASV therapy in patients with HF and CSA but did reveal improvements in quality of life and clinical status.93 The SERVE‐HF (Treatment of Sleep‐Disordered Breathing with Predominant Central Sleep Apnea by Adaptive Servo Ventilation in Patients with Heart Failure) trial was designed to test the effect of ASV on mortality in patients with left ventricular ejection fraction ≤45% and predominantly central sleep apnea. Despite effectively reducing the AHI, ASV failed to confer a survival benefit, and actually was associated with an increase in cardiovascular mortality (29.9% versus 24%).94 Postulated mechanisms for this finding include reductions in cardiac output related to the higher levels of PAP delivered in ASV mode, as well as the hypothesis that CSA is actually a compensatory mechanism in patients with severe HF with beneficial properties that were attenuated by ASV treatment. Additionally, the proprietary algorithm used in SERVE‐HF has been shown to induce episodes of significant hyperventilation in some patients, which some suspect may have been related to the increase in mortality.95 The question of whether SERVE‐HF's findings represent a class effect of ASV versus that of 1 specific algorithm may be answered by the ongoing ADVENT‐HF (Effect of Adaptive Servo Ventilation on Survival and Hospital Admissions in Heart Failure) trial, which is investigating the effect of ASV therapy on mortality and morbidity in HF patients (left ventricular ejection fraction ≤45%) with SDB using an updated algorithm.96
Given these results, treatment of ASV is contraindicated in patients with HF and CSA. In contrast to CSA, large randomized trials looking at the effect of CPAP therapy on hard end points in HF patients with predominantly obstructive sleep apnea are lacking. Given the beneficial effect of CPAP on surrogate end points discussed above, in context of the observed increase in adverse events including mortality associated with OSA as well as the absence of studies suggesting harm, we suggest diagnostic testing in HF patients with suspected sleep apnea based on nocturnal symptoms and/or risk factors discovered during a comprehensive sleep assessment.
Atrial Fibrillation
Similar to OSA, AF is common in the general population, with a prevalence of 1% to 2%.97 In patients with OSA, the prevalence of AF is ≈5%,98 while notably the prevalence of OSA in patients diagnosed with AF has been reported as high as 32% to 39%.99, 100, 101 A significant independent association between the 2 disorders exists even after controlling for confounding conditions such as systemic hypertension, obesity, and HF.101 While multiple mechanisms have been postulated to explain this association, the most important appear to be nocturnal surges in sympathetic tone, systemic hypertension, and structural remodeling, particularly of the atria. Alterations in both sympathetic and parasympathetic system regulation have been observed in association with OSA.79 During an apneic episode, vagal efferent output is enhanced, causing transient bradycardia as well as shortened atrial effective refractory period with resultant susceptibility to excitatory stimuli, an effect that can be reversed with atropine or vagotomy. In animal models of OSA, episodic hypoxemia results in surges of sympathetic nervous system output as well as activation of the renin–angiotensin system, reducing the threshold for AF induction.102 The observation that renal denervation and sympathetic ganglion block provide significant but incomplete protection against apnea‐associated AF induction suggests that additional mechanisms beyond neurohormonal activation are relevant.103, 104, 105 Over time, OSA promotes structural remodeling of both the ventricles and atria, providing an additional pro‐arrhythmic mechanism. Exaggerated swings in intrathoracic pressure, as are seen during apneic events, have been shown to cause acute atrial dilation as well as increased frequency of premature beats even in healthy subjects.106, 107 Chronic repetitive apneic events are associated with progressive left atrial dilation and fibrosis108, 109 as well as left ventricular hypertrophy and diastolic dysfunction.110 Electrophysiologic studies of dilated left atria following repetitive apneic events have revealed slowed atrial conduction, reduced electrogram amplitudes, and complex fractionated atrial electrograms providing mechanistic support for atrial remodeling in AF related to OSA.109 Significant slowing of atrial conduction also occurs during hypercapnia, even in the absence of hypoxia.111 The susceptibility to AF among patients with OSA likely reflects the combined effects of these various mechanisms, with neurohormonal activation and hypercapnia triggered by acute apneic events superimposed on the vulnerable substrate of a remodeled heart.
Beyond the apparent epidemiologic association between the 2 conditions, there is a growing body of evidence to suggest a significant role of OSA in recurrent and/or treatment‐refractory AF. In the ORBIT‐AF (Outcomes Registry for Better Informed Treatment of Atrial Fibrillation), which included >10 000 patients with AF, those with coexisting OSA had significantly worse AF symptoms and were more likely to be on rhythm control therapy.87 An increased risk of recurrent AF following an incident episode88 and worse outcomes after catheter ablation112, 113, 114 have been observed in patients with OSA. Importantly, there is evidence that treatment of OSA may modify these risks. In the ORBIT‐AF cohort, OSA patients treated with CPAP were significantly less likely to progress to permanent AF as compared with OSA patients not receiving CPAP.87 Furthermore, multiple observational studies have demonstrated a significant reduction in the risk of recurrent AF following catheter ablation among OSA patients treated with CPAP as compared with OSA patients not receiving treatment.112, 115, 116, 117 A meta‐analysis of these studies found that in OSA patients treated with CPAP, the AF recurrence risk following catheter ablation was not significantly different from a control population without OSA, whereas OSA patients not treated with CPAP had a statistically significant 57% increased risk of recurrence (P<0.001).113 Important limitations of these studies include observational design, diagnosis of sleep apnea via clinical history and/or standardized questionnaires in lieu of formal sleep testing in the majority of cases, and determination of CPAP use via self‐reporting.
Overall, the current body of literature in this area suggests a possible benefit of treating OSA with CPAP with respect to AF burden and risk of recurrence during rhythm control, particularly following catheter ablation. On the basis of these data, we suggest diagnostic testing with either HSAT or polysomnography in patients with suspected sleep apnea following comprehensive sleep assessment based on nocturnal symptoms and/or risk factors when catheter ablation is planned. This recommendation is consistent with the 2017 Heart Rhythm Society Expert Consensus Statement on catheter and surgical ablation of AF.118 Furthermore, we believe it is reasonable for clinicians to consider diagnostic testing in select patients with suspected sleep apnea managed via rhythm control strategies other than ablation, although there is currently insufficient evidence to provide specific clinical criteria guiding selection from within this large and heterogeneous group of patients. Providers must therefore apply individualized clinical judgment in selecting patients for HSAT or polysomnography testing, keeping in mind that patients with higher‐risk features (history of recurrent AF after cardioversion, anti‐arrhythmic drug failure, etc) are more likely to benefit from detection and treatment of OSA. Patients with AF found to have symptoms of SDB and at risk for moderate‐to‐severe OSA during comprehensive sleep assessment should be referred for diagnostic testing, similar to patients without comorbid AF.
Other Arrhythmias
Beyond AF, OSA has been linked with a spectrum of other cardiac rhythm disturbances as well as sudden cardiac death. Simantirakis et al reported a 22% prevalence of prolonged pauses and bradycardia in patients with moderate‐to‐severe OSA who received long‐term monitoring with an implanted loop recorder.119 Patients are considered to have the “tachy‐brady syndrome” when such bradyarrhythmias alternate with AF or other forms of supraventricular tachycardia. The risk of ventricular arrhythmias also appears to be higher among patients with OSA. Mehra et al found a significantly higher prevalence of nonsustained ventricular tachycardia (5.3% versus 1.2%, P=0.004) among patients with severe OSA compared with controls.98 Similarly, severe OSA was associated with a significantly higher overall risk of complex ventricular ectopy, defined as nonsustained ventricular tachycardia, bigeminy, trigeminy, or quadrigeminy (25% versus 14.5%, P=0.002). Importantly, an increased risk of sudden cardiac death has been reported in patients with severe OSA, particularly among those observed to have nocturnal oxygen desaturation to <78%.120 There are limited data suggesting a beneficial effect of CPAP therapy on reducing rhythm disturbances in patients with OSA119, 121, 122; however, additional study is necessary given the small size and predominantly observational nature of these trials.
Coronary Artery Disease, Cerebrovascular Disease, or Patients Without Established CVD Who Are at High Risk for Future Adverse Cardiovascular Events
Associations have been identified between OSA and other forms of CVD in addition to those described above, in particular coronary artery disease (CAD)58, 123 and cerebrovascular disease.124 Among the pathophysiologic mechanisms linking OSA with CAD and cerebrovascular disease are some of those described above as involved in other forms of CVD, including increased sympathetic nervous system activity, oxidative stress, and predilection to poorly controlled and/or resistant hypertension. Additional mechanisms have been identified as well, including endothelial dysfunction,125, 126 promotion of a procoagulable state,127 and metabolic dysregulation characterized by insulin resistance.128, 129 Treatment of OSA with CPAP has been shown to mitigate these processes,127, 130, 131 offering a plausible mechanism by which treating OSA could influence cardiovascular outcomes.
Support for efficacy of OSA treatment on improving cardiovascular outcomes came from early observational studies. A prospective analysis of 54 patients with known CAD and OSA found a significant reduction in the composite end point of cardiovascular death, acute coronary syndrome, hospitalization for HF, or need for coronary revascularization (hazard ratio 0.24; 95% CI, 0.09–0.62; P<0.01) among patients treated for OSA with either CPAP or upper airway surgery; however, these results may have been subject to significant bias because the untreated arm consisted of patients who had refused treatment despite a recommendation from their provider.132 An observational study that followed 223 patients for 5 years after a stroke found an increased risk of mortality in patients unable to tolerate CPAP versus those who tolerated CPAP (hazard ratio 1.58; 95% CI, 1.01–2.49; P=0.04).133 Similarly, a 444 patient cohort that included patients treated with CPAP, weight loss, or surgery found a significant reduction in mortality associated with each individual treatment modality as compared with untreated patients. When compared with the general population using census‐derived survival data, untreated patients had a significantly higher mortality rate, whereas mortality did not differ significantly between the treated patients and general population.134
Disappointingly though, no randomized trials investigating the impact of PAP therapy on cardiovascular outcomes have shown a clear benefit with respect to hard cardiovascular outcomes. In patients with a history of stroke, Hsu et al found no reduction in recurrent cerebrovascular events in patients with OSA treated with PAP therapy.135 Peker et al randomized 244 nonsleepy patients with CAD following revascularization and moderate‐to‐severe OSA to APAP versus no PAP therapy and found no difference in the composite cardiovascular event outcome after a median of 57 months follow‐up.136
The SAVE (Sleep Apnea Cardiovascular Endpoints) trial was the largest RCT designed to investigate the question of whether treating OSA with CPAP may improve cardiovascular outcomes in patients with established CVD.5 SAVE randomized 2717 patients with moderate‐to‐severe OSA and either CAD or cerebrovascular disease to CPAP plus usual care or usual care alone and followed them for a mean period of 3.7 years. The trial failed to demonstrate a significant reduction in the primary end point (a composite of cardiovascular death, myocardial infarction, stroke, hospitalization for unstable angina, HF, or transient ischemic attack) among patients treated with CPAP in addition to usual care (hazard ratio 1.10; 95% CI, 0.91–1.32; P=0.34). Among secondary end points, CPAP was associated with significant reductions in snoring and daytime sleepiness, improvement in health‐related quality of life and mood, and fewer days off work because of poor health.
While these studies included patients with established CVD, the role of PAP therapy for primary prevention in OSA patients without established CVD has also been queried. Barbé et al enrolled 725 nonsleepy patients with moderate‐to‐severe OSA but no prior history of CVD and randomized them to CPAP versus no therapy. After a median of 4 years, there was no difference in the incidence of systemic hypertension or cardiovascular events including cardiovascular death, nonfatal MI or stroke, TIA, or HF.137 A 2017 meta‐analysis of 10 RCTs (of which 6 required established CVD for enrollment) by Yu et al showed no association between PAP therapy and major cardiovascular events (hazard ratio 0.77; 95% CI, 0.53–1.13; P=0.19).138
While PAP therapy appears to be effective in reducing symptoms of OSA, the results of these randomized trials do not support its efficacy in reducing the risk of adverse cardiovascular events in patients with OSA. Several potential limitations to the available evidence have been cited.6 First, suboptimal PAP adherence was common, with a median duration of <4 hours/night reported in 6 of the 10 RCTs included in the meta‐analysis.138 In SAVE, by far the largest of all these trials, the median duration of PAP use was 3.3 hours per night, and fewer than half (42%) of those in the CPAP arm achieved “good adherence,” defined as ≥4 hours of CPAP use per night.5 Yu's meta‐analysis revealed that in the 4 RCTs achieving median adherence >4 hours/night, PAP therapy was associated with a significantly lower risk of adverse cardiovascular events (relative risk 0.58; 95% CI, 0.34–0.99); however, the implication of this finding is uncertain given the absence of a similar association on a subgroup analysis of patients from all 10 RCTs with good PAP adherence using meta‐regression, possible confounding because of nonrandomized differences between adherent and nonadherent patients, and the inherent limitations of post‐hoc, subgroup analysis findings. Secondly, patients with severe sleep apnea symptoms (commonly defined by Epworth Sleepiness Scale (ESS) >10) were excluded from several of the randomized trials, and some authors have hypothesized that benefits of PAP therapy on preventing adverse cardiovascular outcomes may be limited to these higher‐risk patients with severe OSA. Third, all patients enrolled in the SAVE trial were diagnosed with OSA using HSAT, despite guidelines recommending polysomnography to be used for patients with established significant cardiopulmonary disease, which was one of the inclusion criteria for entry into this study. Therefore, there is the possibility that a significant percentage of the enrolled population may have been affected by Cheyne‐Stokes breathing or other forms of mixed apneas that would not have experienced the same benefit from PAP therapy as in patients with strictly obstructive apneas.6
Although these limitations may serve as topics of interest for future investigations, the best available evidence does not support the use of PAP therapy specifically for the purpose of reducing the risk of future adverse events at this time. Therefore, we suggest diagnostic testing for patients with established CAD, cerebrovascular disease, or elevated cardiovascular risk in whom sleep apnea is clinically suspected because of signs or symptoms uncovered during clinical sleep assessment.
Perioperative Risk
Comorbid OSA is relevant to the perioperative management of patients with CVD planning to undergo surgery. OSA not only increases the risk of respiratory complications, but some studies have reported an increased risk of postoperative AF and other cardiac complications.53 The high prevalence of undiagnosed OSA combined with the observation that perioperative complications are more common in patients with undiagnosed OSA139 has prompted many centers to incorporate screening for OSA as a routine component of preoperative assessment. Various sleep questionnaires have been utilized in this role, with STOP‐BANG being the most validated in the surgical patient population. A STOP‐BANG score ≥3 identifies patients at risk of OSA and has been independently associated with an increased risk of perioperative complications.54 In patients with previously diagnosed OSA, preoperative evaluation should include a review of prior sleep study results to confirm the type and severity of sleep apnea as well as assessment of their compliance with PAP and/or other therapies.
Identifying patients with an established diagnosis or high risk for OSA during preoperative assessment provides an opportunity for targeted interventions that may reduce the risk of perioperative cardiopulmonary complications. Specific management issues that warrant consideration include determining the need for additional preoperative cardiopulmonary evaluation and optimization, selection of an appropriate anesthetic strategy, the intensity and duration of postoperative monitoring, and the provision of PAP therapy postoperatively. The 2016 Society of Anesthesia and Sleep Medicine Guidelines on Preoperative Screening and Assessment of Adult Patients with Obstructive Sleep Apnea offers guidance with respect to these questions.53 A preoperative assessment algorithm reflecting these guidelines is displayed in Figure 1.
Figure 1.
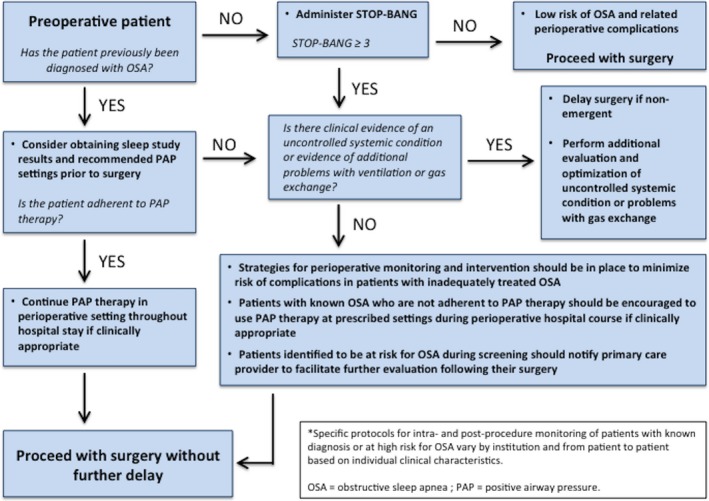
Algorithm for preoperative OSA evaluation. Specific protocols for intra‐ and postprocedure monitoring of patients with known diagnosis or at high risk for OSA vary by institution and from patient to patient based on individual clinical characteristics. OSA indicates obstructive sleep apnea; PAP, positive airway pressure.
Summary of Proposed Recommendations
-
Evaluation
-
Given the high prevalence of sleep apnea in patients with known CVD, we recommend that clinicians perform routine screening for symptoms of SDB in patients with established CVD.
Reasonable strategies for screening include focused questioning performed by the provider as well as use of standardized questionnaires such as STOP‐BANG, the ESS, or the Berlin questionnaire.
Patients reporting any symptoms should undergo a comprehensive sleep assessment.
Screening for OSA should be incorporated into routine preoperative assessment, and in particular we suggest using tools such as STOP‐BANG for this purpose.
-
Our approach to selecting patients for diagnostic sleep testing following a comprehensive sleep assessment varies based upon the underlying cardiovascular comorbidity (Figure 2):
-
We suggest diagnostic testing for all patients, including those without symptoms of SDB, with the following forms of CVD:
Resistant hypertension, defined as inadequately controlled blood pressure despite therapy with ≥3 oral antihypertensive agents including a diuretic, or adequate blood pressure control requiring ≥4 agents.
Pulmonary hypertension.
Recurrent AF following either cardioversion or ablation.
-
We suggest diagnostic testing for patients with established or at risk for CVD in whom sleep apnea is suspected following a comprehensive sleep assessment:
Symptomatic HF (New York Heart Association Class II‐IV) or asymptomatic (New York Heart Association Class I) left ventricular dysfunction (ejection fraction <40%).
AF, particularly in patients who are persistently symptomatic, challenging to pharmacologically rate control, or in whom a rhythm control strategy will be pursued.
Sick sinus syndrome.
Tachy‐brady syndrome.
Ventricular tachycardia or frequent ventricular ectopy.
Survivors of sudden cardiac death.
Coronary artery disease.
Cerebrovascular disease.
Patients at elevated risk for future cardiovascular events.
Routine screening for nocturnal symptoms of SDB should be repeated at defined intervals during long‐term follow‐up in patients with CVD or other significant risk factors who are not referred for diagnostic testing following their initial comprehensive sleep assessment.
Figure 2.
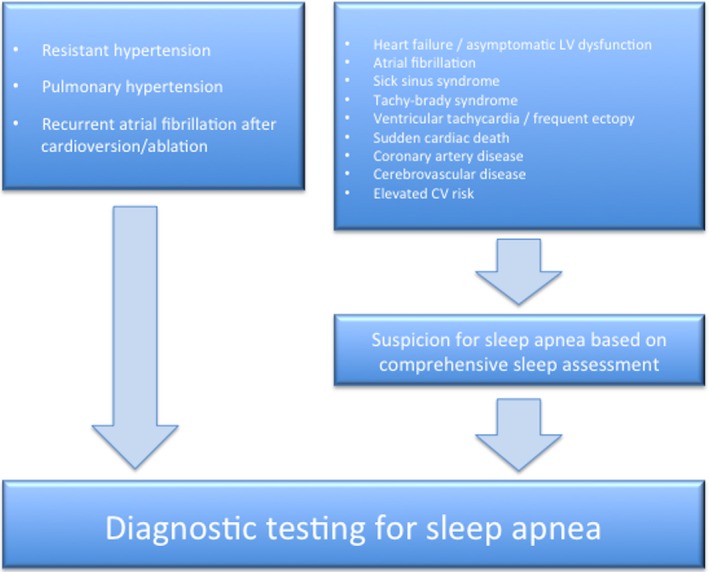 Proposed algorithm to select patients for formal diagnostic sleep testing based on underlying cardiovascular condition. CV indicates cardiovascular; LV, left ventricular.
Proposed algorithm to select patients for formal diagnostic sleep testing based on underlying cardiovascular condition. CV indicates cardiovascular; LV, left ventricular. -
-
Diagnostic testing strategy: We agree with the following recommendations from the 2017 American Academy of Sleep Medicine regarding diagnosing OSA:
Clinical tools, questionnaires, and prediction algorithms should not be used to diagnose OSA in the absence of performing polysomnography or HSAT.
-
Either polysomnography or HSAT may be used to diagnose OSA in uncomplicated patients.
Those with a negative or inconclusive HSAT should undergo polysomnography.
For those with a high pretest probability and negative polysomnography, a repeat polysomnography may be considered.
Polysomnography should be used rather than HSAT in complicated patients, defined as those with significant underlying cardiopulmonary disease, potential respiratory muscle weakness caused by neuromuscular disorders, documented awake hypoventilation or suspected sleep‐related hypoventilation, chronic opioid use, stroke, severe insomnia, or suspected sleep‐related movement disorder such as restless leg syndrome.
-
-
Treatment: We agree with the recommendations from the 2009 Adult Obstructive Sleep Apnea Task Force of the American Academy of Sleep Medicine regarding treatment of OSA:
Clinical correlation is necessary to determine whether CPAP‐intolerant patients should be referred for upper airway surgery or oral appliance therapy. A multidisciplinary approach to the management of OSA should be used as appropriate for each individual patient, including involvement of physicians trained in sleep medicine, otolaryngology–head and neck surgery, cardiology, maxillofacial surgery, and dentists trained in sleep dentistry.
All patients with diagnosed OSA should be offered treatment.
Follow‐up sleep testing should be performed to assess efficacy of non‐PAP therapies as part of a routine follow‐up plan in addition to assessment of symptoms and other clinical parameters.
For patients with difficulty tolerating CPAP, attempts at modifying the treatment should be made to improve compliance.
ASV mode should not be used in patients with HF and low ejection fraction, in whom there is evidence of harm.
-
Oral appliances (OAs): We agree with the 2015 recommendations from the AASM and AADSM regarding OAs.
OAs may be offered as primary therapy in primary snoring without sleep apnea.
OAs may be offered as primary therapy in patients with mild‐to‐moderate OSA who strongly prefer to avoid CPAP therapy.
Patients who do not respond to/tolerate PAP can be considered for OAs.
OAs may be considered as adjunctive to PAP in selected cases.
Custom OAs provided by a qualified dentist are preferred to noncustomized OAs whenever feasible. Patients treated with OAs should have routine qualified dental follow‐up and monitoring for assessment of effectiveness and potential side effects.
-
Upper airway surgery
Upper airway surgery may be offered as primary therapy in primary snoring without sleep apnea.
Patients who do not respond to/tolerate PAP can be considered for upper airway surgery.
Upper airway surgery may be considered as adjunctive to PAP or OAs in selected cases.
Weight loss: All overweight and obese patients with OSA should be encouraged to lose weight. Patients with comorbid CVD stand to gain even greater benefit from weight loss and should be referred to a formal weight loss program, resource permitting.
Disclosures
Dr Kezirian has received research funding from Inspire Medical System and served on the advisory boards of Nyxoah, ReVENT Medical, Pillar Palatal, Cognition Life Science, Gerard Scientific, and Berendo Scientific. Dr De Marco has received research funding from Pfizer, honoraria from Novartis, and served as a consultant for Boston Scientific, Actelion, and Bellerophon. Dr Mirzayan owns and operates apnea‐centric facilities that treat CPAP‐intolerant patients with oral appliances; in addition, he receives payment to provide lectures and training to dentists on the subject of screening and treatment of sleep apnea in the dental practice context. Dr Goldberg has served as a consultant and has minor ownership interest in Siesta Medical. The remaining authors have no disclosures to report.
J Am Heart Assoc. 2019;8:e010440 DOI: 10.1161/JAHA.118.010440.
References
- 1. Shahar E, Whitney CW, Redline S, Lee ET, Newman AB, Nieto FJ, O'Connor GT, Boland LL, Schwartz JE, Samet JM. Sleep‐disordered breathing and cardiovascular disease: cross‐sectional results of the Sleep Heart Health Study. Am J Respir Crit Care Med. 2001;163:19–25. [DOI] [PubMed] [Google Scholar]
- 2. Peppard PE, Young T, Barnet JH, Palta M, Hagen EW, Hla KM. Increased prevalence of sleep‐disordered breathing in adults. Am J Epidemiol. 2013;177:1006–1014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Johnson KG, Johnson DC. Frequency of sleep apnea in stroke and TIA patients: a meta‐analysis. J Clin Sleep Med. 2010;6:131–137. [PMC free article] [PubMed] [Google Scholar]
- 4. Worsnop CJ, Naughton MT, Barter CE, Morgan TO, Anderson AI, Pierce RJ. The prevalence of obstructive sleep apnea in hypertensives. Am J Respir Crit Care Med. 1998;157:111–115. [DOI] [PubMed] [Google Scholar]
- 5. McEvoy RD, Antic NA, Heeley E, Luo Y, Ou Q, Zhang X, Mediano O, Chen R, Drager LF, Liu Z, Chen G, Du B, McArdle N, Tripathi M, Billot L, Li Q, Lorenzi‐Filho G, Barbe F, Redline S, Wang J, Arima H, Neal B, White DP, Grunstein RR, Zhong N, Anderson CS. CPAP for prevention of cardiovascular events in obstructive sleep apnea. N Engl J Med. 2016;375:919–931. [DOI] [PubMed] [Google Scholar]
- 6. Bahammam AS, Pandi‐Perumal SR, Spence DW, Moscovitch A, Streiner DL. The SAVE Trial: has the importance of CPAP for preventing cardiovascular events been discounted? Sleep Vigil. 2017;1:47–48. [Google Scholar]
- 7. Bibbins‐Domingo K, Grossman DC, Curry SJ, Davidson KW, Epling JW, Garcia FA, Herzstein J, Kemper AR, Krist AH, Kurth AE, Landefeld CS, Mangione CM, Phillips WR, Phipps MG, Pignone MP, Silverstein M, Tseng CW. Screening for obstructive sleep apnea in adults: US Preventive Services Task Force recommendation statement. JAMA. 2017;317:407–414. [DOI] [PubMed] [Google Scholar]
- 8. Jordan AS, McSharry DG, Malhotra A. Adult obstructive sleep apnoea. Lancet. 2014;383:736–747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Dempsey JA, Veasey SC, Morgan BJ, O'Donnell CP. Pathophysiology of sleep apnea. Physiol Rev. 2010;90:47–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Wellman A, Jordan AS, Malhotra A, Fogel RB, Katz ES, Schory K, Edwards JK, White DP. Ventilatory control and airway anatomy in obstructive sleep apnea. Am J Respir Crit Care Med. 2004;170:1225–1232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Eckert DJ, Owens RL, Kehlmann GB, Wellman A, Rahangdale S, Yim‐Yeh S, White DP, Malhotra A. Eszopiclone increases the respiratory arousal threshold and lowers the apnoea/hypopnoea index in obstructive sleep apnoea patients with a low arousal threshold. Clin Sci. 2011;120:505–514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Javaheri S, Barbe F, Campos‐Rodriguez F, Dempsey JA, Khayat R, Malhotra A, Martinez‐Garcia MA, Mehra R, Pack AI, Polotsky VY, Redline S, Somers VK. Sleep apnea: types, mechanisms, and clinical cardiovascular consequences. J Am Coll Cardiol. 2017;69:841–858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Malhotra A, White DP. Obstructive sleep apnoea. Lancet. 2002;360:237–245. [DOI] [PubMed] [Google Scholar]
- 14. Sateia MJ. International classification of sleep disorders‐third edition: highlights and modifications. Chest. 2014;146:1387–1394. [DOI] [PubMed] [Google Scholar]
- 15. Ahmadi N, Shapiro GK, Chung SA, Shapiro CM. Clinical diagnosis of sleep apnea based on single night of polysomnography vs. two nights of polysomnography. Sleep Breath. 2009;13:221–226. [DOI] [PubMed] [Google Scholar]
- 16. Kapur VK, Auckley DH, Chowdhuri S, Kuhlmann DC, Mehra R, Ramar K, Harrod CG. Clinical practice guideline for diagnostic testing for adult obstructive sleep apnea: an American Academy of Sleep Medicine clinical practice guideline. J Clin Sleep Med. 2017;13:479–504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Zeidler MR, Santiago V, Dzierzewski JM, Mitchell MN, Santiago S, Martin JL. Predictors of obstructive sleep apnea on polysomnography after a technically inadequate or normal home sleep test. J Clin Sleep Med. 2015;11:1313–1318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Rosen CL, Auckley D, Benca R, Foldvary‐Schaefer N, Iber C, Kapur V, Rueschman M, Zee P, Redline S. A multisite randomized trial of portable sleep studies and positive airway pressure autotitration versus laboratory‐based polysomnography for the diagnosis and treatment of obstructive sleep apnea: the HomePAP study. Sleep. 2012;35:757–767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. de Oliveira ACT, Martinez D, Vasconcelos LFT, Cadaval Gonçalves S, do Carmo Lenz M, Costa Fuchs S, Gus M, de Abreu‐Silva EO, Beltrami Moreira L, Danni Fuchs F. Diagnosis of obstructive sleep apnea syndrome and its outcomes with home portable monitoring. Chest. 2009;135:330–336. [DOI] [PubMed] [Google Scholar]
- 20. Pietzsch JB, Garner A, Cipriano LE, Linehan JH. An integrated health‐economic analysis of diagnostic and therapeutic strategies in the treatment of moderate‐to‐severe obstructive sleep apnea. Sleep. 2011;34:695–709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Deutsch PA, Simmons MS, Wallace JM. Cost‐effectiveness of split‐night polysomnography and home studies in the evaluation of obstructive sleep apnea syndrome. J Clin Sleep Med. 2006;2:145–153. [PubMed] [Google Scholar]
- 22. Kim RD, Kapur VK, Redline‐Bruch J, Rueschman M, Auckley DH, Benca RM, Foldvary‐Schafer NR, Iber C, Zee PC, Rosen CL, Redline S, Ramsey SD. An economic evaluation of home versus laboratory‐based diagnosis of obstructive sleep apnea. Sleep. 2015;38:1027–1037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Gay P, Weaver T, Loube D, Iber C; Positive Airway Pressure Task Force . Evaluation of positive airway pressure treatment for sleep related breathing disorders in adults. Sleep. 2006;29:381–401. [DOI] [PubMed] [Google Scholar]
- 24. Kushida CA, Littner MR, Hirshkowitz M, Morgenthaler TI, Alessi CA, Bailey D, Boehlecke B, Brown TM, Coleman J, Friedman L, Kapen S, Kapur VK, Kramer M, Lee‐Chiong T, Owens J, Pancer JP, Swick TJ, Wise MS. Practice parameters for the use of continuous and bilevel positive airway pressure devices to treat adult patients with sleep‐related breathing disorders. Sleep. 2006;29:375–380. [DOI] [PubMed] [Google Scholar]
- 25. Xu T, Li T, Wei D, Feng Y, Xian L, Wu H, Xu J. Effect of automatic versus fixed continuous positive airway pressure for the treatment of obstructive sleep apnea: an up‐to‐date meta‐analysis. Sleep Breath. 2012;16:1017–1026. [DOI] [PubMed] [Google Scholar]
- 26. Bloch KE, Huber F, Furian M, Latshang TD, Lo Cascio CM, Nussbaumer‐Ochsner Y, Senn O, Russi EW, Kohler M, Schoch OD, Turk A, Imhof E, Laube I, Matthews F, Thurnheer R. Autoadjusted versus fixed CPAP for obstructive sleep apnoea: a multicentre, randomised equivalence trial. Thorax. 2018;73:174–184. [DOI] [PubMed] [Google Scholar]
- 27. Morgenthaler TI, Aurora RN, Brown T, Zak R, Alessi C, Boehlecke B, Chesson AL, Friedman L, Kapur V, Maganti R, Owens J, Pancer J, Swick TJ; Standards of Practice Committee of the American Academy of Sleep Medicine . Practice parameters for the use of autotitrating continuous positive airway pressure devices for titrating pressures and treating adult patients with obstructive sleep apnea syndrome: an update for 2007. An American Academy of Sleep Medicine report. Sleep. 2008;31:141–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Wozniak DR, Lasserson TJ, Smith I. Educational, supportive and behavioural interventions to improve usage of continuous positive airway pressure machines in adults with obstructive sleep apnoea. Cochrane Database Syst Rev. 2014:CD007736. [DOI] [PubMed] [Google Scholar]
- 29. Knowles SR, O'Brien DT, Zhang S, Devara A, Rowley JA. Effect of addition of chin strap on PAP compliance, nightly duration of use, and other factors. J Clin Sleep Med. 2014;10:377–383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Johansson K, Hemmingsson E, Harlid R, Trolle Lagerros Y, Granath F, Rössner S, Neovius M. Longer term effects of very low energy diet on obstructive sleep apnoea in cohort derived from randomised controlled trial: prospective observational follow‐up study. BMJ. 2011;342:d3017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Foster GD, Borradaile KE, Sanders MH, Millman R, Zammit G, Newman AB, Wadden TA, Kelley D, Wing RR, Pi‐Sunyer FX, Reboussin D, Kuna ST. A randomized study on the effect of weight loss on obstructive sleep apnea among obese patients with type 2 diabetes: the Sleep AHEAD study. Arch Intern Med. 2009;169:1619–1626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Kuna ST, Reboussin DM, Borradaile KE, Sanders MH, Millman RP, Zammit G, Newman AB, Wadden TA, Jakicic JM, Wing RR, Pi‐Sunyer FX, Foster GD; Sleep AHEAD Research Group . Long‐term effect of weight loss on obstructive sleep apnea severity in obese patients with type 2 diabetes. Sleep. 2013;36:641–649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Greenburg DL, Lettieri CJ, Eliasson AH. Effects of surgical weight loss on measures of obstructive sleep apnea: a meta‐analysis. Am J Med. 2009;122:535–542. [DOI] [PubMed] [Google Scholar]
- 34. Horvath K, Jeitler K, Siering U, Stich AK, Skipka G, Gratzer TW, Siebenhofer A. Long‐term effects of weight‐reducing interventions in hypertensive patients: systematic review and meta‐analysis. Arch Intern Med. 2008;168:571–580. [DOI] [PubMed] [Google Scholar]
- 35. Poobalan AS, Aucott LS, Smith WC, Avenell A, Jung R, Broom J. Long‐term weight loss effects on all cause mortality in overweight/obese populations. Obes Rev. 2007;8:503–513. [DOI] [PubMed] [Google Scholar]
- 36. Morgenthaler TI, Kapen S, Lee‐Chiong T, Alessi C, Boehlecke B, Brown T, Coleman J, Friedman L, Kapur V, Owens J, Pancer J, Swick T; Standards of Practice Parameters of the American Academy of Sleep Medicine . Practice parameters for the medical therapy of obstructive sleep apnea. Sleep. 2006;29:1031–1035. [PubMed] [Google Scholar]
- 37. Ashrafian H, Toma T, Rowland SP, Harling L, Tan A, Efthimiou E, Darzi A, Athanasiou T. Bariatric surgery or non‐surgical weight loss for obstructive sleep apnoea? A systematic review and comparison of meta‐analyses. Obes Surg. 2015;25:1239–1250. [DOI] [PubMed] [Google Scholar]
- 38. Pevernagie DA, Stanson AW, Sheedy PF, Daniels BK, Shepard JW. Effects of body position on the upper airway of patients with obstructive sleep apnea. Am J Respir Crit Care Med. 1995;152:179–185. [DOI] [PubMed] [Google Scholar]
- 39. Epstein LJ, Kristo D, Strollo PJ, Friedman N, Malhotra A, Patil SP, Ramar K, Rogers R, Schwab RJ, Weaver EM, Weinstein MD; Adult Obstructive Sleep Apnea Task Force of the American Academy of Sleep Medicine . Clinical guideline for the evaluation, management and long‐term care of obstructive sleep apnea in adults. J Clin Sleep Med. 2009;5:263–276. [PMC free article] [PubMed] [Google Scholar]
- 40. Ravesloot MJL, White D, Heinzer R, Oksenberg A, Pépin JL. Efficacy of the new generation of devices for positional therapy for patients with positional obstructive sleep apnea: a systematic review of the literature and meta‐analysis. J Clin Sleep Med. 2017;13:813–824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Ferguson KA, Cartwright R, Rogers R, Schmidt‐Nowara W. Oral appliances for snoring and obstructive sleep apnea: a review. Sleep. 2006;29:244–262. [DOI] [PubMed] [Google Scholar]
- 42. Sutherland K, Deane SA, Chan AS, Schwab RJ, Ng AT, Darendeliler MA, Cistulli PA. Comparative effects of two oral appliances on upper airway structure in obstructive sleep apnea. Sleep. 2011;34:469–477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Ramar K, Dort LC, Katz SG, Lettieri CJ, Harrod CG, Thomas SM, Chervin RD. Clinical practice guideline for the treatment of obstructive sleep apnea and snoring with oral appliance therapy: an update for 2015. J Clin Sleep Med. 2015;11:773–827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Storesund A, Johansson A, Bjorvatn B, Lehmann S. Oral appliance treatment outcome can be predicted by continuous positive airway pressure in moderate to severe obstructive sleep apnea. Sleep Breath. 2018;22:385–392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Camacho M, Riaz M, Capasso R, Ruoff CM, Guilleminault C, Kushida CA, Certal V. The effect of nasal surgery on continuous positive airway pressure device use and therapeutic treatment pressures: a systematic review and meta‐analysis. Sleep. 2015;38:279–286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Camacho M, Certal V, Brietzke SE, Holty JE, Guilleminault C, Capasso R. Tracheostomy as treatment for adult obstructive sleep apnea: a systematic review and meta‐analysis. Laryngoscope. 2014;124:803–811. [DOI] [PubMed] [Google Scholar]
- 47. Certal VF, Zaghi S, Riaz M, Viera AS, Pinheiro CT, Kushida C, Capasso R, Camacho M. Hypoglossal nerve stimulation in the treatment of obstructive sleep apnea: a systematic review and meta‐analysis. Laryngoscope. 2015;125:1254–1264. [DOI] [PubMed] [Google Scholar]
- 48. Kezirian EJ, Goldberg AN. Hypopharyngeal surgery in obstructive sleep apnea: an evidence‐based medicine review. Arch Otolaryngol Head Neck Surg. 2006;132:206–213. [DOI] [PubMed] [Google Scholar]
- 49. Holty JE, Guilleminault C. Maxillomandibular advancement for the treatment of obstructive sleep apnea: a systematic review and meta‐analysis. Sleep Med Rev. 2010;14:287–297. [DOI] [PubMed] [Google Scholar]
- 50. Stuck BA, Ravesloot MJL, Eschenhagen T, de Vet HCW, Sommer JU. Uvulopalatopharyngoplasty with or without tonsillectomy in the treatment of adult obstructive sleep apnea—a systematic review. Sleep Med. 2018;50:152–165. [DOI] [PubMed] [Google Scholar]
- 51. Strollo PJ, Soose RJ, Maurer JT, de Vries N, Cornelius J, Froymovich O, Hanson RD, Padhya TA, Steward DL, Gillespie MB, Woodson BT, Van de Heyning PH, Goetting MG, Vanderveken OM, Feldman N, Knaack L, Strohl KP; STAR Trial Group . Upper‐airway stimulation for obstructive sleep apnea. N Engl J Med. 2014;370:139–149. [DOI] [PubMed] [Google Scholar]
- 52. Strollo PJ, Gillespie MB, Soose RJ, Maurer JT, de Vries N, Cornelius J, Hanson RD, Padhya TA, Steward DL, Woodson BT, Verbraecken J, Vanderveken OM, Goetting MG, Feldman N, Chabolle F, Badr MS, Randerath W. Upper airway stimulation for obstructive sleep apnea: durability of the treatment effect at 18 months. Sleep. 2015;38:1593–1598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Chung F, Memtsoudis SG, Ramachandran SK, Nagappa M, Opperer M, Cozowicz C, Patrawala S, Lam D, Kumar A, Joshi GP, Fleetham J, Ayas N, Collop N, Doufas AG, Eikermann M, Gali B, Gay P, Hernandez AV, Kaw R, Kezirian EJ, Malhotra A, Mokhlesi B, Parthasarathy S, Stierer T, Wappler F, Hillman DR, Auckley D. Society of anesthesia and sleep medicine guidelines on preoperative screening and assessment of adult patients with obstructive sleep apnea. Anesth Analg. 2016;123:452–473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Corso RM, Petrini F, Buccioli M, Nanni O, Carretta E, Trolio A, De Nuzzo D, Pigna A, Di Giacinto I, Agnoletti V, Gambale G. Clinical utility of preoperative screening with STOP‐Bang questionnaire in elective surgery. Minerva Anestesiol. 2014;80:877–884. [PubMed] [Google Scholar]
- 55. MacKay SG, Chan L. Surgical approaches to obstructive sleep apnea. Sleep Med Clin. 2016;11:331–341. [DOI] [PubMed] [Google Scholar]
- 56. Nieto FJ, Young TB, Lind BK, Shahar E, Samet JM, Redline S, D'Agostino RB, Newman AB, Lebowitz MD, Pickering TG. Association of sleep‐disordered breathing, sleep apnea, and hypertension in a large community‐based study. Sleep Heart Health Study. JAMA. 2000;283:1829–1836. [DOI] [PubMed] [Google Scholar]
- 57. Marin JM, Agusti A, Villar I, Forner M, Nieto D, Carrizo SJ, Barbé F, Vicente E, Wei Y, Nieto FJ, Jelic S. Association between treated and untreated obstructive sleep apnea and risk of hypertension. JAMA. 2012;307:2169–2176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Peppard PE, Young T, Palta M, Skatrud J. Prospective study of the association between sleep‐disordered breathing and hypertension. N Engl J Med. 2000;342:1378–1384. [DOI] [PubMed] [Google Scholar]
- 59. Gonçalves SC, Martinez D, Gus M, de Abreu‐Silva EO, Bertoluci C, Dutra I, Branchi T, Moreira LB, Fuchs SC, de Oliveira AC, Fuchs FD. Obstructive sleep apnea and resistant hypertension: a case‐control study. Chest. 2007;132:1858–1862. [DOI] [PubMed] [Google Scholar]
- 60. Liu L, Cao Q, Guo Z, Dai Q. Continuous positive airway pressure in patients with obstructive sleep apnea and resistant hypertension: a meta‐analysis of randomized controlled trials. J Clin Hypertens (Greenwich). 2016;18:153–158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Turnbull F; Collaboration BPLTT . Effects of different blood‐pressure‐lowering regimens on major cardiovascular events: results of prospectively‐designed overviews of randomised trials. Lancet. 2003;362:1527–1535. [DOI] [PubMed] [Google Scholar]
- 62. Yamakawa H, Shiomi T, Sasanabe R, Hasegawa R, Ootake K, Banno K, Wakayama H, Katada M, Kobayashi T. Pulmonary hypertension in patients with severe obstructive sleep apnea. Psychiatry Clin Neurosci. 2002;56:311–312. [DOI] [PubMed] [Google Scholar]
- 63. Jilwan FN, Escourrou P, Garcia G, Jaïs X, Humbert M, Roisman G. High occurrence of hypoxemic sleep respiratory disorders in precapillary pulmonary hypertension and mechanisms. Chest. 2013;143:47–55. [DOI] [PubMed] [Google Scholar]
- 64. Kholdani C, Fares WH, Mohsenin V. Pulmonary hypertension in obstructive sleep apnea: is it clinically significant? A critical analysis of the association and pathophysiology. Pulm Circ. 2015;5:220–227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Weitzenblum E. Chronic cor pulmonale. Heart. 2003;89:225–230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Wong HS, Williams AJ, Mok Y. The relationship between pulmonary hypertension and obstructive sleep apnea. Curr Opin Pulm Med. 2017;23:517–521. [DOI] [PubMed] [Google Scholar]
- 67. Sajkov D, McEvoy RD. Obstructive sleep apnea and pulmonary hypertension. Prog Cardiovasc Dis. 2009;51:363–370. [DOI] [PubMed] [Google Scholar]
- 68. Minai OA, Ricaurte B, Kaw R, Hammel J, Mansour M, McCarthy K, Golish JA, Stoller JK. Frequency and impact of pulmonary hypertension in patients with obstructive sleep apnea syndrome. Am J Cardiol. 2009;104:1300–1306. [DOI] [PubMed] [Google Scholar]
- 69. Sajkov D, Wang T, Saunders NA, Bune AJ, Mcevoy RD. Continuous positive airway pressure treatment improves pulmonary hemodynamics in patients with obstructive sleep apnea. Am J Respir Crit Care Med. 2002;165:152–158. [DOI] [PubMed] [Google Scholar]
- 70. Arias MA, García‐Río F, Alonso‐Fernández A, Martínez I, Villamor J. Pulmonary hypertension in obstructive sleep apnoea: effects of continuous positive airway pressure: a randomized, controlled cross‐over study. Eur Heart J. 2006;27:1106–1113. [DOI] [PubMed] [Google Scholar]
- 71. McLaughlin VV, Archer SL, Badesch DB, Barst RJ, Farber HW, Linder JR, Mathier MA, McGoon MD, Park MH, Rosenson RS, Rubin LJ, Tapson VF, Varga J. ACCF/AHA 2009 expert consensus document on pulmonary hypertension a report of the American College of Cardiology Foundation Task Force on Expert Consensus Documents and the American Heart Association developed in collaboration with the American College of Chest Physicians; American Thoracic Society, Inc.; and the Pulmonary Hypertension Association. J Am Coll Cardiol. 2009;53:1573–1619. [DOI] [PubMed] [Google Scholar]
- 72. Galiè N, Humbert M, Vachiery JL, Gibbs S, Lang I, Torbicki A, Simonneau G, Peacock A, Vonk Noordegraaf A, Beghetti M, Ghofrani A, Gomez Sanchez MA, Hansmann G, Klepetko W, Lancellotti P, Matucci M, McDonagh T, Pierard LA, Trindade PT, Zompatori M, Hoeper M. 2015 ESC/ERS guidelines for the diagnosis and treatment of pulmonary hypertension. Eur Heart J. 2016;69:177. [DOI] [PubMed] [Google Scholar]
- 73. Oldenburg O, Lamp B, Faber L, Teschler H, Horstkotte D, Töpfer V. Sleep‐disordered breathing in patients with symptomatic heart failure: a contemporary study of prevalence in and characteristics of 700 patients. Eur J Heart Fail. 2007;9:251–257. [DOI] [PubMed] [Google Scholar]
- 74. Oldenburg O, Teerlink JR. Screening for sleep‐disordered breathing in patients hospitalized for heart failure. JACC Heart Fail. 2015;3:732–733. [DOI] [PubMed] [Google Scholar]
- 75. Aurora RN, Patil SP, Punjabi NM. Portable sleep monitoring for diagnosing sleep apnea in hospitalized patients with heart failure. Chest. 2018;154:91–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Lanfranchi PA, Somers VK, Braghiroli A, Corra U, Eleuteri E, Giannuzzi P. Central sleep apnea in left ventricular dysfunction: prevalence and implications for arrhythmic risk. Circulation. 2003;107:727–732. [DOI] [PubMed] [Google Scholar]
- 77. Oldenburg O, Wellmann B, Buchholz A, Bitter T, Fox H, Thiem U, Horstkotte D, Wegscheider K. Nocturnal hypoxaemia is associated with increased mortality in stable heart failure patients. Eur Heart J. 2016;37:1695–1703. [DOI] [PubMed] [Google Scholar]
- 78. Khayat R, Jarjoura D, Porter K, Sow A, Wannemacher J, Dohar R, Pleister A, Abraham WT. Sleep disordered breathing and post‐discharge mortality in patients with acute heart failure. Eur Heart J. 2015;36:1463–1469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Leung RS. Sleep‐disordered breathing: autonomic mechanisms and arrhythmias. Prog Cardiovasc Dis. 2009;51:324–338. [DOI] [PubMed] [Google Scholar]
- 80. Bradley TD, Hall MJ, Ando S, Floras JS. Hemodynamic effects of simulated obstructive apneas in humans with and without heart failure. Chest. 2001;119:1827–1835. [DOI] [PubMed] [Google Scholar]
- 81. Logan AG, Tkacova R, Perlikowski SM, Leung RS, Tisler A, Floras JS, Bradley TD. Refractory hypertension and sleep apnoea: effect of CPAP on blood pressure and baroreflex. Eur Respir J. 2003;21:241–247. [DOI] [PubMed] [Google Scholar]
- 82. Gami AS, Olson EJ, Shen WK, Wright RS, Ballman KV, Hodge DO, Herges RM, Howard DE, Somers VK. Obstructive sleep apnea and the risk of sudden cardiac death: a longitudinal study of 10,701 adults. J Am Coll Cardiol. 2013;62:610–616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Peker Y, Carlson J, Hedner J. Increased incidence of coronary artery disease in sleep apnoea: a long‐term follow‐up. Eur Respir J. 2006;28:596–602. [DOI] [PubMed] [Google Scholar]
- 84. Usui K, Bradley TD, Spaak J, Ryan CM, Kubo T, Kaneko Y, Floras JS. Inhibition of awake sympathetic nerve activity of heart failure patients with obstructive sleep apnea by nocturnal continuous positive airway pressure. J Am Coll Cardiol. 2005;45:2008–2011. [DOI] [PubMed] [Google Scholar]
- 85. Hall AB, Ziadi MC, Leech JA, Chen SY, Burwash IG, Renaud J, de Kemp RA, Haddad H, Mielniczuk LM, Yoshinaga K, Huo A, Chen L, Walter O, Garrard L, Da Silva JN, Floras JS, Beanlands RS. Effects of short‐term continuous positive airway pressure on myocardial sympathetic nerve function and energetics in patients with heart failure and obstructive sleep apnea: a randomized study. Circulation. 2014;130:892–901. [DOI] [PubMed] [Google Scholar]
- 86. Javaheri S. Effects of continuous positive airway pressure on sleep apnea and ventricular irritability in patients with heart failure. Circulation. 2000;101:392–397. [DOI] [PubMed] [Google Scholar]
- 87. Holmqvist F, Guan N, Zhu Z, Kowey PR, Allen LA, Fonarow GC, Hylek EM, Mahaffey KW, Freeman JV, Chang P, Holmes DN, Peterson ED, Piccini JP, Gersh BJ; ORBIT‐AF Investigators . Impact of obstructive sleep apnea and continuous positive airway pressure therapy on outcomes in patients with atrial fibrillation—results from the Outcomes Registry for Better Informed Treatment of Atrial Fibrillation (ORBIT‐AF). Am Heart J. 2015;169:647–654.e642. [DOI] [PubMed] [Google Scholar]
- 88. Kanagala R, Murali NS, Friedman PA, Ammash NM, Gersh BJ, Ballman KV, Shamsuzzaman AS, Somers VK. Obstructive sleep apnea and the recurrence of atrial fibrillation. Circulation. 2003;107:2589–2594. [DOI] [PubMed] [Google Scholar]
- 89. Kaneko Y, Floras JS, Usui K, Plante J, Tkacova R, Kubo T, Ando S, Bradley TD. Cardiovascular effects of continuous positive airway pressure in patients with heart failure and obstructive sleep apnea. N Engl J Med. 2003;348:1233–1241. [DOI] [PubMed] [Google Scholar]
- 90. Arias MA, García‐Río F, Alonso‐Fernández A, Mediano O, Martínez I, Villamor J. Obstructive sleep apnea syndrome affects left ventricular diastolic function: effects of nasal continuous positive airway pressure in men. Circulation. 2005;112:375–383. [DOI] [PubMed] [Google Scholar]
- 91. Bradley TD, Logan AG, Kimoff RJ, Sériès F, Morrison D, Ferguson K, Belenkie I, Pfiefer M, Fleetham J, Hanly P, Smilovitch M, Tomlinson G, Floras JS; CANPAP Investigators . Continuous positive airway pressure for central sleep apnea and heart failure. N Engl J Med. 2005;353:2025–2033. [DOI] [PubMed] [Google Scholar]
- 92. Sharma BK, Bakker JP, McSharry DG, Desai AS, Javaheri S, Malhotra A. Adaptive servoventilation for treatment of sleep‐disordered breathing in heart failure: a systematic review and meta‐analysis. Chest. 2012;142:1211–1221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Momomura S, Seino Y, Kihara Y, Adachi H, Yasumura Y, Yokoyama H, Wada H, Ise T, Tanaka K; SAVIOR‐C Investigators . Adaptive servo‐ventilation therapy for patients with chronic heart failure in a confirmatory, multicenter, randomized, controlled study. Circ J. 2015;79:981–990. [DOI] [PubMed] [Google Scholar]
- 94. Cowie MR, Woehrle H, Wegscheider K, Angermann C, d'Ortho MP, Erdmann E, Levy P, Simonds AK, Somers VK, Zannad F, Teschler H. Adaptive servo‐ventilation for central sleep apnea in systolic heart failure. N Engl J Med. 2015;373:1095–1105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Javaheri S, Brown LK, Randerath W, Khayat R. SERVE‐HF: more questions than answers. Chest. 2016;149:900–904. [DOI] [PubMed] [Google Scholar]
- 96. Lyons OD, Floras JS, Logan AG, Beanlands R, Cantolla JD, Fitzpatrick M, Fleetham J, John Kimoff R, Leung RS, Lorenzi Filho G, Mayer P, Mielniczuk L, Morrison DL, Ryan CM, Series F, Tomlinson GA, Woo A, Arzt M, Parthasarathy S, Redolfi S, Kasai T, Parati G, Delgado DH, Bradley TD; ADVENT‐HF Investigators . Design of the effect of adaptive servo‐ventilation on survival and cardiovascular hospital admissions in patients with heart failure and sleep apnoea: the ADVENT‐HF trial. Eur J Heart Fail. 2017;19:579–587. [DOI] [PubMed] [Google Scholar]
- 97. Go AS, Hylek EM, Phillips KA, Chang Y, Henault LE, Selby JV, Singer DE. Prevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention: the AnTicoagulation and Risk Factors in Atrial Fibrillation (ATRIA) Study. JAMA. 2001;285:2370–2375. [DOI] [PubMed] [Google Scholar]
- 98. Mehra R, Benjamin EJ, Shahar E, Gottlieb DJ, Nawabit R, Kirchner HL, Sahadevan J, Redline S. Association of nocturnal arrhythmias with sleep‐disordered breathing: the Sleep Heart Health Study. Am J Respir Crit Care Med. 2006;173:910–916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Albuquerque FN, Calvin AD, Sert Kuniyoshi FH, Konecny T, Lopez‐Jimenez F, Pressman GS, Kara T, Friedman P, Ammash N, Somers VK, Caples SM. Sleep‐disordered breathing and excessive daytime sleepiness in patients with atrial fibrillation. Chest. 2012;141:967–973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Bitter T, Langer C, Vogt J, Lange M, Horstkotte D, Oldenburg O. Sleep‐disordered breathing in patients with atrial fibrillation and normal systolic left ventricular function. Dtsch Arztebl Int. 2009;106:164–170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Gami AS, Pressman G, Caples SM, Kanagala R, Gard JJ, Davison DE, Malouf JF, Ammash NM, Friedman PA, Somers VK. Association of atrial fibrillation and obstructive sleep apnea. Circulation. 2004;110:364–367. [DOI] [PubMed] [Google Scholar]
- 102. May AM, Van Wagoner DR, Mehra R. OSA and cardiac arrhythmogenesis: mechanistic insights. Chest. 2017;151:225–241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Ghias M, Scherlag BJ, Lu Z, Niu G, Moers A, Jackman WM, Lazzara R, Po SS. The role of ganglionated plexi in apnea‐related atrial fibrillation. J Am Coll Cardiol. 2009;54:2075–2083. [DOI] [PubMed] [Google Scholar]
- 104. Linz D, Mahfoud F, Schotten U, Ukena C, Neuberger HR, Wirth K, Böhm M. Renal sympathetic denervation suppresses postapneic blood pressure rises and atrial fibrillation in a model for sleep apnea. Hypertension. 2012;60:172–178. [DOI] [PubMed] [Google Scholar]
- 105. Linz D, Hohl M, Khoshkish S, Mahfoud F, Ukena C, Neuberger HR, Wirth K, Böhm M. Low‐level but not high‐level baroreceptor stimulation inhibits atrial fibrillation in a pig model of sleep apnea. J Cardiovasc Electrophysiol. 2016;27:1086–1092. [DOI] [PubMed] [Google Scholar]
- 106. Orban M, Bruce CJ, Pressman GS, Leinveber P, Romero‐Corral A, Korinek J, Konecny T, Villarraga HR, Kara T, Caples SM, Somers VK. Dynamic changes of left ventricular performance and left atrial volume induced by the mueller maneuver in healthy young adults and implications for obstructive sleep apnea, atrial fibrillation, and heart failure. Am J Cardiol. 2008;102:1557–1561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Camen G, Clarenbach CF, Stöwhas AC, Rossi VA, Sievi NA, Stradling JR, Kohler M. The effects of simulated obstructive apnea and hypopnea on arrhythmic potential in healthy subjects. Eur J Appl Physiol. 2013;113:489–496. [DOI] [PubMed] [Google Scholar]
- 108. Drager LF, Bortolotto LA, Pedrosa RP, Krieger EM, Lorenzi‐Filho G. Left atrial diameter is independently associated with arterial stiffness in patients with obstructive sleep apnea: potential implications for atrial fibrillation. Int J Cardiol. 2010;144:257–259. [DOI] [PubMed] [Google Scholar]
- 109. Dimitri H, Ng M, Brooks AG, Kuklik P, Stiles MK, Lau DH, Antic N, Thorton A, Saint DA, McEvoy D, Antic R, Kalman JM, Sanders P. Atrial remodeling in obstructive sleep apnea: implications for atrial fibrillation. Heart Rhythm. 2012;9:321–327. [DOI] [PubMed] [Google Scholar]
- 110. Cioffi G, Russo TE, Stefenelli C, Selmi A, Furlanello F, Cramariuc D, Gerdts E, de Simone G. Severe obstructive sleep apnea elicits concentric left ventricular geometry. J Hypertens. 2010;28:1074–1082. [DOI] [PubMed] [Google Scholar]
- 111. Stevenson IH, Roberts‐Thomson KC, Kistler PM, Edwards GA, Spence S, Sanders P, Kalman JM. Atrial electrophysiology is altered by acute hypercapnia but not hypoxemia: implications for promotion of atrial fibrillation in pulmonary disease and sleep apnea. Heart Rhythm. 2010;7:1263–1270. [DOI] [PubMed] [Google Scholar]
- 112. Naruse Y, Tada H, Satoh M, Yanagihara M, Tsuneoka H, Hirata Y, Ito Y, Kuroki K, Machino T, Yamasaki H, Igarashi M, Sekiguchi Y, Sato A, Aonuma K. Concomitant obstructive sleep apnea increases the recurrence of atrial fibrillation following radiofrequency catheter ablation of atrial fibrillation: clinical impact of continuous positive airway pressure therapy. Heart Rhythm. 2013;10:331–337. [DOI] [PubMed] [Google Scholar]
- 113. Li L, Wang ZW, Li J, Ge X, Guo LZ, Wang Y, Guo WH, Jiang CX, Ma CS. Efficacy of catheter ablation of atrial fibrillation in patients with obstructive sleep apnoea with and without continuous positive airway pressure treatment: a meta‐analysis of observational studies. Europace. 2014;16:1309–1314. [DOI] [PubMed] [Google Scholar]
- 114. Ng CY, Liu T, Shehata M, Stevens S, Chugh SS, Wang X. Meta‐analysis of obstructive sleep apnea as predictor of atrial fibrillation recurrence after catheter ablation. Am J Cardiol. 2011;108:47–51. [DOI] [PubMed] [Google Scholar]
- 115. Fein AS, Shvilkin A, Shah D, Haffajee CI, Das S, Kumar K, Kramer DB, Zimetbaum PJ, Buxton AE, Josephson ME, Anter E. Treatment of obstructive sleep apnea reduces the risk of atrial fibrillation recurrence after catheter ablation. J Am Coll Cardiol. 2013;62:300–305. [DOI] [PubMed] [Google Scholar]
- 116. Neilan TG, Farhad H, Dodson JA, Shah RV, Abbasi SA, Bakker JP, Michaud GF, van der Geest R, Blankstein R, Steigner M, John RM, Jerosch‐Herold M, Malhotra A, Kwong RY. Effect of sleep apnea and continuous positive airway pressure on cardiac structure and recurrence of atrial fibrillation. J Am Heart Assoc. 2013;2:e000421 DOI: 10.1161/JAHA.113.000421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. Patel D, Mohanty P, Di Biase L, Shaheen M, Lewis WR, Quan K, Cummings JE, Wang P, Al‐Ahmad A, Venkatraman P, Nashawati E, Lakkireddy D, Schweikert R, Horton R, Sanchez J, Gallinghouse J, Hao S, Beheiry S, Cardinal DS, Zagrodzky J, Canby R, Bailey S, Burkhardt JD, Natale A. Safety and efficacy of pulmonary vein antral isolation in patients with obstructive sleep apnea: the impact of continuous positive airway pressure. Circ Arrhythm Electrophysiol. 2010;3:445–451. [DOI] [PubMed] [Google Scholar]
- 118. Calkins H, Hindricks G, Cappato R, Kim YH, Saad EB, Aguinaga L, Akar JG, Badhwar V, Brugada J, Camm J, Chen PS, Chen SA, Chung MK, Nielsen JC, Curtis AB, Davies DW, Day JD, d'Avila A, de Groot NMSN, Di Biase L, Duytschaever M, Edgerton JR, Ellenbogen KA, Ellinor PT, Ernst S, Fenelon G, Gerstenfeld EP, Haines DE, Haissaguerre M, Helm RH, Hylek E, Jackman WM, Jalife J, Kalman JM, Kautzner J, Kottkamp H, Kuck KH, Kumagai K, Lee R, Lewalter T, Lindsay BD, Macle L, Mansour M, Marchlinksi FE, Michaud GF, Makagawa H, Natale A, Nattel S, Okumura K, Packer D, Pokushalov E, Reynolds MR, Sanders P, Scanavacca M, Schilling R, Tondo C, Tsao HM, Verma A, Wilber DJ, Yamane T. 2017 HRS/EHRA/ECAS/APHRS/SOLAECE expert consensus statement on catheter and surgical ablation of atrial fibrillation: executive summary. J Arrhythm. 2017;33:369–409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119. Simantirakis EN, Schiza SI, Marketou ME, Chrysostomakis SI, Chlouverakis GI, Klapsinos NC, Siafaksas NS, Vardas PE. Severe bradyarrhythmias in patients with sleep apnoea: the effect of continuous positive airway pressure treatment: a long‐term evaluation using an insertable loop recorder. Eur Heart J. 2004;25:1070–1076. [DOI] [PubMed] [Google Scholar]
- 120. Patel N, Donahue C, Shenoy A, Patel A, El‐Sherif N. Obstructive sleep apnea and arrhythmia: a systemic review. Int J Cardiol. 2017;228:967–970. [DOI] [PubMed] [Google Scholar]
- 121. Grimm W, Koehler U, Fus E, Hoffmann J, Menz V, Funck R, Peter JH, Maisch B. Outcome of patients with sleep apnea‐associated severe bradyarrhythmias after continuous positive airway pressure therapy. Am J Cardiol. 2000;86:688–692, A689. [DOI] [PubMed] [Google Scholar]
- 122. Ryan CM, Usui K, Floras JS, Bradley TD. Effect of continuous positive airway pressure on ventricular ectopy in heart failure patients with obstructive sleep apnoea. Thorax. 2005;60:781–785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123. Gottlieb DJ, Yenokyan G, Newman AB, O'Connor GT, Punjabi NM, Quan SF, Redline S, Resnick HE, Tong EK, Diener‐West M, Shahar E. Prospective study of obstructive sleep apnea and incident coronary heart disease and heart failure: the Sleep Heart Health Study. Circulation. 2010;122:352–360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124. Redline S, Yenokyan G, Gottlieb DJ, Shahar E, O'Connor GT, Resnick HE, Diener‐West M, Sanders MH, Wolf PA, Geraghty EM, Ali T, Lebowitz M, Punjabi NM. Obstructive sleep apnea‐hypopnea and incident stroke: the Sleep Heart Health Study. Am J Respir Crit Care Med. 2010;182:269–277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125. Patt BT, Jarjoura D, Haddad DN, Sen CK, Roy S, Flavahan NA, Khayat RN. Endothelial dysfunction in the microcirculation of patients with obstructive sleep apnea. Am J Respir Crit Care Med. 2010;182:1540–1545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126. Phillips SA, Olson EB, Morgan BJ, Lombard JH. Chronic intermittent hypoxia impairs endothelium‐dependent dilation in rat cerebral and skeletal muscle resistance arteries. Am J Physiol Heart Circ Physiol. 2004;286:H388–H393. [DOI] [PubMed] [Google Scholar]
- 127. Phillips CL, McEwen BJ, Morel‐Kopp MC, Yee BJ, Sullivan DR, Ward CM, Tofler GH, Grunstein RR. Effects of continuous positive airway pressure on coagulability in obstructive sleep apnoea: a randomised, placebo‐controlled crossover study. Thorax. 2012;67:639–644. [DOI] [PubMed] [Google Scholar]
- 128. Ip MS, Lam B, Ng MM, Lam WK, Tsang KW, Lam KS. Obstructive sleep apnea is independently associated with insulin resistance. Am J Respir Crit Care Med. 2002;165:670–676. [DOI] [PubMed] [Google Scholar]
- 129. Botros N, Concato J, Mohsenin V, Selim B, Doctor K, Yaggi HK. Obstructive sleep apnea as a risk factor for type 2 diabetes. Am J Med. 2009;122:1122–1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130. Schwarz EI, Puhan MA, Schlatzer C, Stradling JR, Kohler M. Effect of CPAP therapy on endothelial function in obstructive sleep apnoea: a systematic review and meta‐analysis. Respirology. 2015;20:889–895. [DOI] [PubMed] [Google Scholar]
- 131. Iftikhar IH, Hoyos CM, Phillips CL, Magalang UJ. Meta‐analyses of the association of sleep apnea with insulin resistance, and the effects of CPAP on HOMA‐IR, adiponectin, and visceral adipose fat. J Clin Sleep Med. 2015;11:475–485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132. Milleron O, Pillière R, Foucher A, de Roquefeuil F, Aegerter P, Jondeau G, Raffstin BG, Dubourg O. Benefits of obstructive sleep apnoea treatment in coronary artery disease: a long‐term follow‐up study. Eur Heart J. 2004;25:728–734. [DOI] [PubMed] [Google Scholar]
- 133. Martínez‐García MA, Soler‐Cataluña JJ, Ejarque‐Martínez L, Soriano Y, Román‐Sánchez P, Illa FB, Canal JM, Durán‐Cantolla J. Continuous positive airway pressure treatment reduces mortality in patients with ischemic stroke and obstructive sleep apnea: a 5‐year follow‐up study. Am J Respir Crit Care Med. 2009;180:36–41. [DOI] [PubMed] [Google Scholar]
- 134. Marti S, Sampol G, Muñoz X, Torres F, Roca A, Lloberes P, Sagalés T, Quesada P, Morell F. Mortality in severe sleep apnoea/hypopnoea syndrome patients: impact of treatment. Eur Respir J. 2002;20:1511–1518. [DOI] [PubMed] [Google Scholar]
- 135. Hsu CY, Vennelle M, Li HY, Engleman HM, Dennis MS, Douglas NJ. Sleep‐disordered breathing after stroke: a randomised controlled trial of continuous positive airway pressure. J Neurol Neurosurg Psychiatry. 2006;77:1143–1149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136. Peker Y, Glantz H, Eulenburg C, Wegscheider K, Herlitz J, Thunström E. Effect of positive airway pressure on cardiovascular outcomes in coronary artery disease patients with nonsleepy obstructive sleep apnea. The RICCADSA randomized controlled trial. Am J Respir Crit Care Med. 2016;194:613–620. [DOI] [PubMed] [Google Scholar]
- 137. Barbé F, Durán‐Cantolla J, Sánchez‐de‐la‐Torre M, Martínez‐Alonso M, Carmona C, Barceló A, Chiner E, Masa JF, Gonzalez M, Marín JM, Garcia‐Rio F, Diaz de Atauri J, Terán J, Mayos M, de la Peña M, Monasterio C, del Camp F, Montserrat JM; Spanish Sleep and Breathing Network . Effect of continuous positive airway pressure on the incidence of hypertension and cardiovascular events in nonsleepy patients with obstructive sleep apnea: a randomized controlled trial. JAMA. 2012;307:2161–2168. [DOI] [PubMed] [Google Scholar]
- 138. Yu J, Zhou Z, McEvoy RD, Anderson CS, Rodgers A, Perkovic V, Neal B. Association of positive airway pressure with cardiovascular events and death in adults with sleep apnea: a systematic review and meta‐analysis. JAMA. 2017;318:156–166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139. Kaw R, Michota F, Jaffer A, Ghamande S, Auckley D, Golish J. Unrecognized sleep apnea in the surgical patient: implications for the perioperative setting. Chest. 2006;129:198–205. [DOI] [PubMed] [Google Scholar]


