Abstract
Mitochondrial dihydrolipoamide dehydrogenase (DLDH) is a redox enzyme involved in decarboxylation of pyruvate to form acetyl-CoA during the cascade of glucose metabolism and mitochondrial adenine triphosphate (ATP) production. Depending on physiological or pathophysiological conditions, DLDH can either enhance or attenuate the production of reactive oxygen species (ROS) and reactive nitrogen species. Recent research in our laboratory has demonstrated that inhibition of DLDH induced antioxidative responses and could serve as a protective approach against oxidative stress in stroke injury. In this perspective article, we postulated that chronic inhibition of DLDH could also attenuate oxidative stress in type 2 diabetes. We discussed DLDH-involving mitochondrial metabolic pathways and metabolic intermediates that could accumulate upon DLDH inhibition and their corresponding roles in abrogating oxidative stress in diabetes. We also discussed a couple of DLDH inhibitors that could be tested in animal models of type 2 diabetes. It is our belief that DLDH inhibition could be a novel approach to fighting type 2 diabetes.
Keywords: diabetes mellitus, dihydrolipoamide dehydrogenase, mitochondria, oxidative stress, reactive oxygen species
1. Introduction
Adult-onset diabetes mellitus, also known as type 2 diabetes, is caused by insulin resistance followed by β-cell dysfunction [1,2,3]. The hallmark of this metabolic disorder is persistent hyperglycemia in the blood induced by dysregulation of glucose metabolism [4,5,6]. While pathogenesis of type 2 diabetes is multifactorial, oxidative stress has been thought to be the converging event leading to development and progression of type 2 diabetes [7,8,9,10]. As sources of reactive oxygen species-induced oxidative stress are usually endogenous in type 2 diabetes [11,12], managing diabetic oxidative stress by stimulating endogenous antioxidation pathways may provide a novel approach to fighting diabetes.
2. Oxidative Stress and Diabetes
When blood glucose is constantly high, there can be a variety of pathophysiological consequences. These include non-enzymatic modifications of proteins by glucose through a process known as glycation [13,14,15], elevated levels of reactive oxygen species (ROS) [15,16] that can cause oxidative damage to proteins, DNA, and lipids [17,18,19,20], and upregulation of metabolic and signaling pathways that can have detrimental effects on glucose metabolism [21,22,23,24,25]. With respect to elevated ROS production, it has been established that nearly all the identified pathways that are upregulated by persistent hyperglycemia can induce or contribute to redox imbalance and ROS production [12,26]. These include the polyol pathway, the protein kinase C activation pathway, the hexosamine pathway, the advanced glycation end products pathway, and the glyceraldehyde autoxidation pathway [8,10]. In addition, upregulation of the poly adenine diphosphate ADP ribosylation pathway and down regulation of the sirtuin 3 pathway have also been implicated in diabetic oxidative stress that accentuates diabetes and its complications [16,27]. Therefore, we believe that stimulation and reinforcement of cellular antioxidation pathways are promising strategies for attenuating diabetic oxidative stress and ameliorating diabetes.
In this article, we postulate that chronic inhibition of mitochondrial dihydrolipomide dehydrogenase (DLDH) can be explored to manage diabetic oxidative stress in diabetic conditions
3. Mitochondrial Dihydrolipomide Dehydrogenase (DLDH)
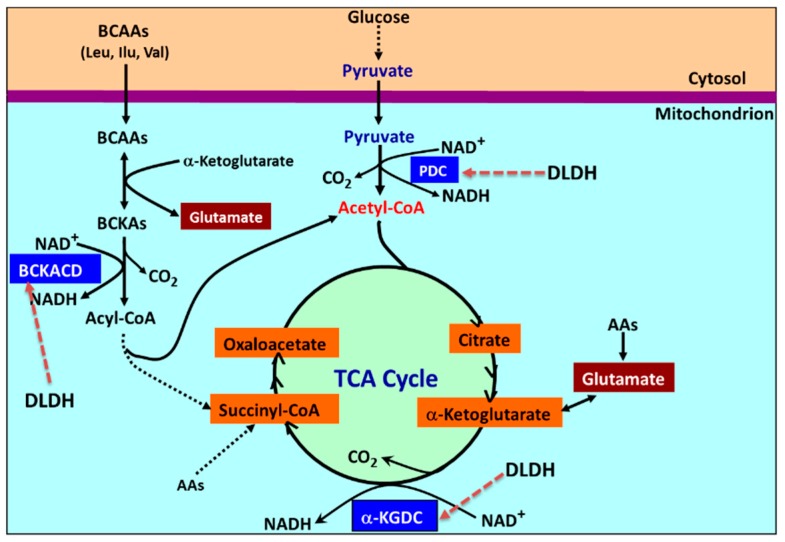
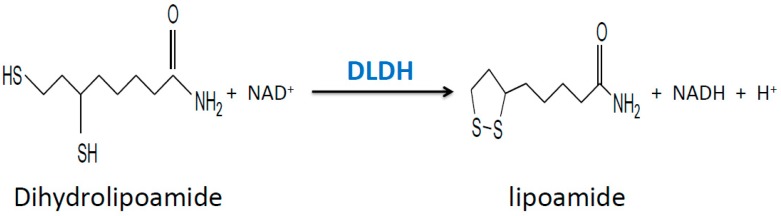
Mitochondrial dihydrolipomide dehydrogenase (DLDH) is a flavin adenine dinucleotide (FAD)-containing, nicotinamide adenine dinucleotide (NAD)-dependent disulfide-implicated redox enzyme [28,29,30,31]. DLDH participates in three mitochondrial enzyme complexes, namely pyruvate dehydrogenase complex, α-keto glutarate dehydrogenase complex, and branched chain amino acid dehydrogenase complex (Figure 1). DLDH is also involved in the glycine cleavage system. In the three dehydrogenase complexes, DLDH catalyzes the same reactions that oxidizes dihydrolipoamide to lipoamide (Figure 2) so that the overall enzymatic reactions can continue.
Figure 1.
Mitochondrial metabolic pathways involving dihydrolipomide dehydrogenase (DLDH), which include the pyruvate to acetyl-CoA pathway, the α-ketoglutarate to succinyl-CoA pathway, and the branched chain amino acids (leucine, isoleucine, and valine) to acyl-CoA pathway. The glycine cleavage pathway that also involves DLDH is not shown here. DLDH-involved complexes are indicated by dotted red arrows on the figure. BCAA: branched chain amino acids; NAD+: nicotinamide adenine dinucleotide; NADH: reduced form of NAD+; AAs: amino acids; α-KGDC: alpha ketoglutarate dehydrogenase complex; TCA: tricarboxylic acid; BCKA: branched chain keto acid; BCKACD: branched chain alpha keto acid dehydrogenase complex; PDC: pyruvate dehydrogenase complex.
Figure 2.
The chemical reaction catalyzed by DLDH. Dihydrolipoamide is oxidized to lipoamide at the expense of NAD+. Hence the DLDH-catalyzed reaction produces NADH that feeds into the electron transport chain in the inner mitochondrial membrane.
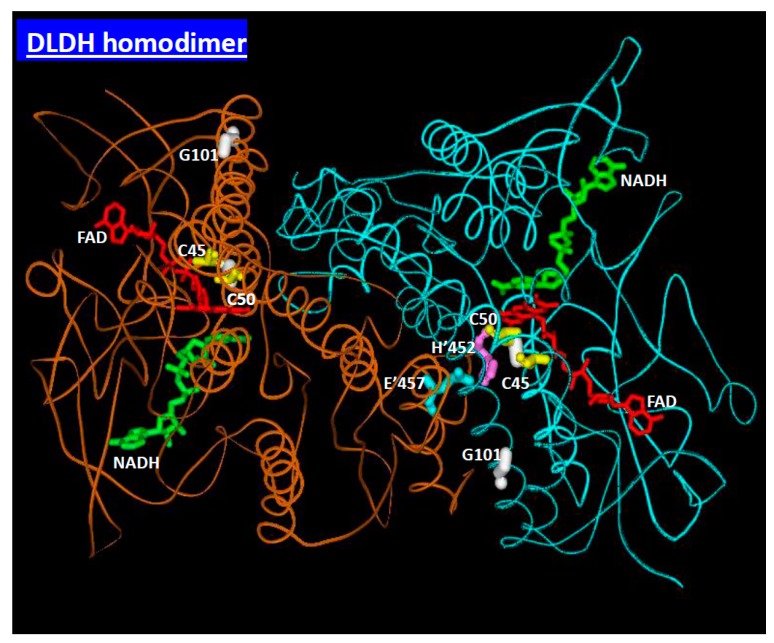
DLDH is a multifunctional protein. In rat, the brain and the testis appear to have the highest DLDH activity while the lung gives the lowest DLDH activity [31]. When it exists as a homodimer in the above mentioned dehydrogenase complexes, it is a classical redox-dependent enzyme that converts dihydrolipoamide to lipoamide using two cysteine residues at its active center as a redox relay system (Figure 3). However, the enzyme, when it exists as a monomer, can have a moonlighting function, for example acting as a protease [32]. DLDH can either enhance or attenuate production of reactive oxygen species (ROS), depending on experimental or pathophysiological conditions [29,33,34,35,36,37,38]. In particular, DLDH has two redox-reactive cysteine residues at its active center [39,40] that may scavenge reactive oxygen or reactive nitrogen species, thereby bearing the brunt of oxidative attack and sparing other macromolecules from oxidative damage.
Figure 3.
Structure of a DLDH homodimer. Each monomer contributes amino acid residues involved in enzyme activities. Each monomer contains a tightly bound flavin adenine dinucleotide (FAD) molecule, an NAD molecule and two cysteine residues (C45 and C50 in the figure) at the active center. The two cysteines form a disulfide bond (yellow) during catalysis. Electrons from the substrate dihydrolipoamide are eventually transported to NAD via the two cysteine residues and the FAD molecule. This image was created using MDL Chime [41]. Data were derived from the Protein Data Bank (PDB ID: 1ZMC) [42].
In our recent studies, we have found that DLDH can be inactivated by mitochondrial ROS or by reactive nitrogen species (RNS) [38,43,44]. These studies, on the other hand, would indicate that DLDH could serve as an antioxidant enzyme under stress or pathophysiological conditions. As age-related metabolic stress involves reactive oxygen or nitrogen species [45,46], we reason that enhancing DLDH’s ability to scavenge ROS or RNS may serve as approaches for retardation of development of age related metabolic syndrome including diabetes; and such enhancement may be achieved by chronic inhibition of DLDH in vivo, which should be designed not to pose any toxicity but to lend the benefits of anti-oxidation property of a chronically inhibited DLDH [44]. Below we will discuss what happens when DLDH is chronically inhibited. Please note that we will not cover acute inhibition of DLDH activity, as such an approach may pose toxicity to experimental subjects.
4. Accumulation of Dihydrolipoamide
A direct consequence of DLDH inhibition is the blockade of dihydrolipoamide conversion to lipoamide. This would induce accumulation of dihydrolipoamide in the cell [47]. As dihydrolipoamide contains two free sulfhydryl groups, it has a strong antioxidation ability [39,48,49,50,51]. Therefore, accumulation of dihydrolipoamide upon chronic inhibition of DLDH may give cells the ability to eliminate more reactive oxygen or nitrogen species under diabetic conditions.
It should be noted that in mouse studies, loss of 50% DLDH activity does not yield any diseased phenotypes [52,53]. This demonstrates that partial inhibition of DLDH is feasible and does not impair thriving of the DLDH-deficient animals. Nonetheless, benefits resulting from chronic DLDH inhibition in diabetic rodent models have yet to be evaluated.
5. Accumulation of Pyruvate
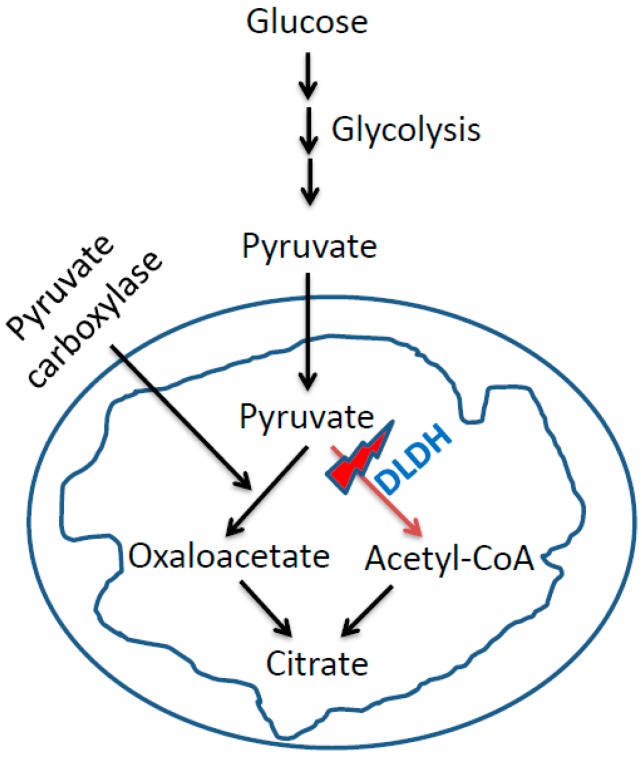
Chronic inhibition of DLDH may also induce accumulation of pyruvate in a cell (Figure 4). Pyruvate, as has been established, is an antioxidant that could be neuroprotective or cardiac protective [54,55,56,57,58]. Nonetheless, whether pyruvate is accumulated following chronic DLDH inhibition in diabetic subjects needs to be investigated.
Figure 4.
DLDH inhibition could divert pyruvate to the pathway of oxaloacetate formation, which could be further channeled into the anaplerotic pathway.
Another possibility of pyruvate accumulation is the shift of pyruvate towards oxaloacetate (OAA) production that is catalyzed by pyruvate carboxylase. This reaction is involved in anaplerotic metabolism and production of NADPH [59] that may also be explored to fight oxidative stress in diabetes because NADPH is involved in maintaining cellular redox balance and glutathione metabolism [60,61,62,63].
6. DLDH Chronic Inhibition and Activation of Nrf2 Signaling Pathway
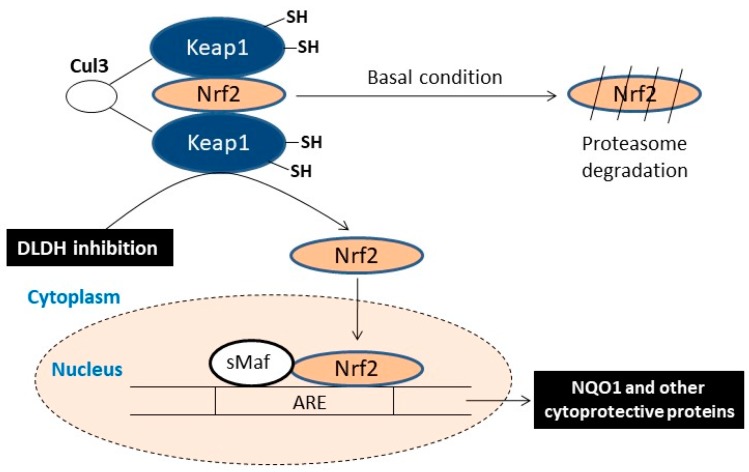
We have found that in stroke neuroprotection studies, inhibition of DLDH by 5-methoxyindole-2-carboxylic acid (MICA) was able to activate the Nrf2 signaling pathway that leads to NAD(P)H quinone dehydrogenase 1 (NQO1) upregulation [44,64]. This pathway was clearly demonstrated in both preconditioning and postconditioning in rat brain by MICA treatment, demonstrating that chronic inhibition of DLDH could be used as a potential approach for targeting oxidative stress in metabolic diseases (as shown in Figure 5). Studies by others also indicate the involvement of DLDH in the activation of the Nrf2 signaling pathways [65,66]. More recently, DLDH inhibition by MICA has also been shown to yield beneficial effects in Alzheimer’s disease [67,68].
Figure 5.
Scheme showing that inhibition of DLDH could activate the Nrf2 signaling pathway, resulting in upregulation of antioxidant enzymes including NAD(P)H quinone dehydrogenase 1 (NQO1) and heme-oxygenase-1 as well as other antioxidant enzymes.
7. Potential DLDH Inhibitors
Currently, there are two DLDH inhibitors that have been studied. One is MICA [69], and the other is valproic acid (VPA) metabolites. As we have covered MICA in above discussions, we would now discuss VPA metabolites. VPA is an antiepileptic drug [70]. It has been reported that derivatives of VPA such as valproyl-CoA and valproyl-dephospho-CoA can directly inhibit DLDH activity [71], leading to impairment of mitochondrial function reflected by decreased oxygen consumption and decreased ATP synthesis [71]. These derivatives, together with MICA and its derivatives, should also be tested for their antioxidative effects in type 2 diabetes. It should be noted that whether VPA inhibition of DLDH could also lead to activation of the Nrf2 signaling pathway remains unknown. It should also be noted that while arsenite inhibits overall DLDH-catalyzed reaction, arsenite should not be tested in the context of diabetes as this chemical will conjugate with dihydrolipoamide [47,72] rather than the enzyme DLDH itself, leading to less dihydrolipoamide that could be available for antioxidative purposes. It should be pointed out that while arsenite is not suitable to develop in diabetic research, many other natural product(s) or nutrients could be good DLDH inhibitors that will need to be identified for managing diabetic oxidative stress.
8. Conclusions
Oxidative stress is a major pathological mechanism of type 2 diabetes. DLDH, as a redox-sensitive enzyme, plays a central role in glucose metabolism. As inhibition of DLDH could induce antioxidative responses and enhance cellular antioxidation capacity in oxidative stress conditions, we propose that chronic DLDH inhibition could serve as a protective approach against oxidative stress in type 2 diabetes, thereby leading to diabetes remission. In this sense, DLDH inhibition may elicit antioxidative effects similar to those induced by treatment with antioxidant-like natural products and/or nutrients.
Author Contributions
Conceptualization, X.Y., J.S., and L.-J.Y.; original draft preparation, X.Y., J.S., and L.-J.Y.; review and editing, L.-J.Y..
Funding
Liang-Jun Yan (L.-J.Y.) was supported in part by University of North Texas Health Science Center (HSC) intramural grants RI 10015 and RI10039 and by the National Institutes of Health grant R01NS079792.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Cernea S., Dobreanu M. Diabetes and beta cell function: From mechanisms to evaluation and clinical implications. Biochem. Med. 2013;23:266–280. doi: 10.11613/BM.2013.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Alzaid A., Rizza R.A. Insulin resistance and its role in the pathogenesis of impaired glucose tolerance and non-insulin-dependent diabetes mellitus: Perspectives gained from in vivo studies. In: Moller D.E., editor. Insulin Resistance. John Wiley & Sons Ltd.; New York, NY, USA: 1993. pp. 143–186. [Google Scholar]
- 3.Barnett A.H. Type 2 Diabetes. 2rd ed. Oxford University Press; Oxford, UK: 2012. p. 162. [Google Scholar]
- 4.Tuch B., Dunlop M., Proietto J. Diabetes Research: A Guide for Postgraduates. Harwood Academic Publishers; Reading, UK: 2000. [Google Scholar]
- 5.Abdul-Ghani M.A., DeFronzo R.A. Oxidative stress in type 2 diabetes. In: Miwa S., Beckman K.B., Muller F.L., editors. Oxidative Stress in Aging. Humana Press; New York, NY, USA: 2008. pp. 191–212. [Google Scholar]
- 6.DeFronzo R.A. Pathogenesis of type 2 diabetes mellitus. Med. Clin. N. Am. 2004;88:787–835. doi: 10.1016/j.mcna.2004.04.013. [DOI] [PubMed] [Google Scholar]
- 7.Wu J., Jin Z., Zheng H., Yan L.J. Sources and implications of nadh/nad (+) redox imbalance in diabetes and its complications. Diabetes Metab. Syndr. Obes. 2016;9:145–153. doi: 10.2147/DMSO.S106087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yan L.J. Pathogenesis of chronic hyperglycemia: From reductive stress to oxidative stress. J. Diabetes Res. 2014;2014:137919. doi: 10.1155/2014/137919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rosen P., Nawroth P.P., King G., Moller W., Tritschler H.J., Packer L. The role of oxidative stress in the onset and progression of diabetes and its complications: A summary of a congress series sponsored by unesco-mcbn, the american diabetes association and the german diabetes society. Diabetes Metab. Res. Rev. 2001;17:189–212. doi: 10.1002/dmrr.196. [DOI] [PubMed] [Google Scholar]
- 10.Luo X., Li R., Yan L.J. Roles of pyruvate, nadh, and mitochondrial complex i in redox balance and imbalance in β cell function and dysfunction. J. Diabetes Res. 2015;2015 doi: 10.1155/2015/512618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ruskovska T., Bernlohr D.A. Oxidative stress and protein carbonylation in adipose tissue—Implications for insulin resistance and diabetes mellitus. J. Proteom. 2013;92:323–334. doi: 10.1016/j.jprot.2013.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Robertson R.P. Chronic oxidative stress as a central mechanism for glucose toxicity in pancreatic islet beta cells in diabetes. J. Biol. Chem. 2004;279:42351–42354. doi: 10.1074/jbc.R400019200. [DOI] [PubMed] [Google Scholar]
- 13.Aragno M., Mastrocola R. Dietary sugars and endogenous formation of advanced glycation endproducts: Emerging mechanisms of disease. Nutrients. 2017;9:385. doi: 10.3390/nu9040385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lovestone S., Smith U. Advanced glycation end products, dementia, and diabetes. Proc. Natl. Acad. Sci. USA. 2014;111:4743–4744. doi: 10.1073/pnas.1402277111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rosca M.G., Mustata T.G., Kinter M.T., Ozdemir A.M., Kern T.S., Szweda L.I., Brownlee M., Monnier V.M., Weiss M.F. Glycation of mitochondrial proteins from diabetic rat kidney is associated with excess superoxide formation. Am. J. Physiol. Ren. Physiol. 2005;289:F420–F430. doi: 10.1152/ajprenal.00415.2004. [DOI] [PubMed] [Google Scholar]
- 16.Wu J., Jin Z., Yan L.J. Redox imbalance and mitochondrial abnormalities in the diabetic lung. Redox Biol. 2017;11:51–59. doi: 10.1016/j.redox.2016.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Beckman K.B., Ames B.N. Oxidative decay of DNA. J. Biol. Chem. 1997;272:19633–19636. doi: 10.1074/jbc.272.32.19633. [DOI] [PubMed] [Google Scholar]
- 18.Yan L.J., Lodge J.K., Traber M.G., Packer L. Apolipoprotein b carbonyl formation is enhanced by lipid peroxidation during copper-mediated oxidation of human low-density lipoproteins. Arch. Biochem. Biophys. 1997;339:165–171. doi: 10.1006/abbi.1996.9867. [DOI] [PubMed] [Google Scholar]
- 19.Yan L.J. Analysis of oxidative modification of proteins. Curr. Protoc. Protein Sci. 2009;56:14.4.1–14.4.28. doi: 10.1002/0471140864.ps1404s56. [DOI] [PubMed] [Google Scholar]
- 20.Yan L.J., Sohal R.S. Gel electrophoretic quantitation of protein carbonyls derivatized with tritiated sodium borohydride. Anal. Biochem. 1998;265:176–182. doi: 10.1006/abio.1998.2868. [DOI] [PubMed] [Google Scholar]
- 21.Pieper A.A., Brat D.J., Krug D.K., Watkins C.C., Gupta A., Blackshaw S., Verma A., Wang Z.Q., Snyder S.H. Poly(adp-ribose) polymerase-deficient mice are protected from streptozotocin-induced diabetes. Proc. Natl. Acad. Sci. USA. 1999;96:3059–3064. doi: 10.1073/pnas.96.6.3059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pacher P., Liaudet L., Soriano F.G., Mabley J.G., Szabo E., Szabo C. The role of poly(adp-ribose) polymerase activation in the development of myocardial and endothelial dysfunction in diabetes. Diabetes. 2002;51:514–521. doi: 10.2337/diabetes.51.2.514. [DOI] [PubMed] [Google Scholar]
- 23.Chung S.S., Ho E.C., Lam K.S., Chung S.K. Contribution of polyol pathway to diabetes-induced oxidative stress. J. Am. Soc. Nephrol. 2003;14:S233–S236. doi: 10.1097/01.ASN.0000077408.15865.06. [DOI] [PubMed] [Google Scholar]
- 24.Li Q., Hwang Y.C., Ananthakrishnan R., Oates P.J., Guberski D., Ramasamy R. Polyol pathway and modulation of ischemia-reperfusion injury in type 2 diabetic bbz rat hearts. Cardiovasc. Diabetol. 2008;7:33. doi: 10.1186/1475-2840-7-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Oates P.J. Polyol pathway and diabetic peripheral neuropathy. Int. Rev. Neurobiol. 2002;50:325–392. doi: 10.1016/s0074-7742(02)50082-9. [DOI] [PubMed] [Google Scholar]
- 26.Yan L.J. Redox imbalance stress in diabetes mellitus: Role of the polyol pathway. Anim. Model Exp. Med. 2018;1:7–13. doi: 10.1002/ame2.12001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hirschey M.D., Shimazu T., Jing E., Grueter C.A., Collins A.M., Aouizerat B., Stancakova A., Goetzman E., Lam M.M., Schwer B., et al. Sirt3 deficiency and mitochondrial protein hyperacetylation accelerate the development of the metabolic syndrome. Mol. Cell. 2011;44:177–190. doi: 10.1016/j.molcel.2011.07.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Williams C.H., Jr. Lipoamide dehydrogenase, glutathione reductase, thioredoxin reductase, and mercuric ion reductase-a family of flavoenzyme transhydrogenases. In: Muller F., editor. Chemistry and Biochemistry of Flavoenzymes. Volume III. CRC Press; Boca Raton, FL, USA: 1992. pp. 121–212. [Google Scholar]
- 29.Yan L.J., Thangthaeng N., Forster M.J. Changes in dihydrolipoamide dehydrogenase expression and activity during postnatal development and aging in the rat brain. Mech. Ageing Dev. 2008;129:282–290. doi: 10.1016/j.mad.2008.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yan L.J., Thangthaeng N., Sumien N., Forster M.J. Serum dihydrolipoamide dehydrogenase is a labile enzyme. J. Biochem. Pharmacol. Res. 2013;1:30–42. [PMC free article] [PubMed] [Google Scholar]
- 31.Yan L.J., Yang S.H., Shu H., Prokai L., Forster M.J. Histochemical staining and quantification of dihydrolipoamide dehydrogenase diaphorase activity using blue native page. Electrophoresis. 2007;28:1036–1045. doi: 10.1002/elps.200600574. [DOI] [PubMed] [Google Scholar]
- 32.Babady N.E., Pang Y.P., Elpeleg O., Isaya G. Cryptic proteolytic activity of dihydrolipoamide dehydrogenase. Proc. Natl. Acad. Sci. USA. 2007;104:6158–6163. doi: 10.1073/pnas.0610618104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Quinlan C.L., Goncalves R.L., Hey-Mogensen M., Yadava N., Bunik V.I., Brand M.D. The 2-oxoacid dehydrogenase complexes in mitochondria can produce superoxide/hydrogen peroxide at much higher rates than complex i. J. Biol. Chem. 2014 doi: 10.1074/jbc.M113.545301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Xia L., Bjornstedt M., Nordman T., Eriksson L.C., Olsson J.M. Reduction of ubiquinone by lipoamide dehydrogenase. An antioxidant regenerating pathway. Eur. J. Biochem. 2001;268:1486–1490. doi: 10.1046/j.1432-1327.2001.02013.x. [DOI] [PubMed] [Google Scholar]
- 35.Sreider C.M., Grinblat L., Stoppani A.O. Catalysis of nitrofuran redox-cycling and superoxide anion production by heart lipoamide dehydrogenase. Biochem. Pharmacol. 1990;40:1849–1857. doi: 10.1016/0006-2952(90)90366-S. [DOI] [PubMed] [Google Scholar]
- 36.Ambrus A., Torocsik B., Tretter L., Ozohanics O., Adam-Vizi V. Stimulation of reactive oxygen species generation by disease-causing mutations of lipoamide dehydrogenase. Hum. Mol. Genet. 2011;20:2984–2995. doi: 10.1093/hmg/ddr202. [DOI] [PubMed] [Google Scholar]
- 37.Chen H.J., Chen Y.M., Chang C.M. Lipoyl dehydrogenase catalyzes reduction of nitrated DNA and protein adducts using dihydrolipoic acid or ubiquinol as the cofactor. Chem. Biol. Interact. 2002;140:199–213. doi: 10.1016/S0009-2797(02)00019-4. [DOI] [PubMed] [Google Scholar]
- 38.Yan L.J., Sumien N., Thangthaeng N., Forster M.J. Reversible inactivation of dihydrolipoamide dehydrogenase by mitochondrial hydrogen peroxide. Free Radic. Res. 2013;47:123–133. doi: 10.3109/10715762.2012.752078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Patel M.S., Hong Y.S. Lipoic acid as an antioxidant: The role of dihydrolipoamide dehydrogenase. In: Armstrong D., editor. Free Radical and Antioxidant Protocols. Humana Press; Totowa, NJ, USA: 1998. pp. 337–346. [DOI] [PubMed] [Google Scholar]
- 40.Jentoft J.E., Shoham M., Hurst D., Patel M.S. A structural model for human dihydrolipoamide dehydrogenase. Proteins. 1992;14:88–101. doi: 10.1002/prot.340140110. [DOI] [PubMed] [Google Scholar]
- 41.Tong J.C., Kong L., Tan T.W., Ranganathan S. Mpid-t: Database for sequence-structure-function information on t-cell receptor/peptide/mhc interactions. Appl. Bioinform. 2006;5:111–114. doi: 10.2165/00822942-200605020-00005. [DOI] [PubMed] [Google Scholar]
- 42.Brautigam C.A., Chuang J.L., Tomchick D.R., Machius M., Chuang D.T. Crystal structure of human dihydrolipoamide dehydrogenase: Nad+/nadh binding and the structural basis of disease-causing mutations. J. Mol. Biol. 2005;350:543–552. doi: 10.1016/j.jmb.2005.05.014. [DOI] [PubMed] [Google Scholar]
- 43.Yan L.J., Liu L., Forster M.J. Reversible inactivation of dihydrolipoamide dehydrogenase by angeli’s salt. Acta Biophys. Sin. (Sheng Wu Wu Li Hsueh Bao) 2012;28:341–350. [PMC free article] [PubMed] [Google Scholar]
- 44.Wu J., Li R., Li W., Ren M., Thangthaeng N., Sumien N., Liu R., Yang S., Simpkins J.W., Forster M.J., et al. Administration of 5-methoxyindole-2-carboxylic acid that potentially targets mitochondrial dihydrolipoamide dehydrogenase confers cerebral preconditioning against ischemic stroke injury. Free Radic. Biol. Med. 2017;113:244–254. doi: 10.1016/j.freeradbiomed.2017.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Jackson M.J., Papa S., Bolanos J., Bruckdorfer R., Carlsen H., Elliott R.M., Flier J., Griffiths H.R., Heales S., Holst B., et al. Antioxidants, reactive oxygen and nitrogen species, gene induction and mitochondrial function. Mol. Asp. Med. 2002;23:209–285. doi: 10.1016/S0098-2997(02)00018-3. [DOI] [PubMed] [Google Scholar]
- 46.Son S.M. Reactive oxygen and nitrogen species in pathogenesis of vascular complications of diabetes. Diabetes Metab. J. 2012;36:190–198. doi: 10.4093/dmj.2012.36.3.190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Alzahrani S., Ebert P.R. Oxygen and arsenite synergize phosphine toxicity by distinct mechanisms. Toxicol. Sci. 2018 doi: 10.1093/toxsci/kfy248. [DOI] [PubMed] [Google Scholar]
- 48.Haramaki N., Han D., Handelman G.J., Tritschler H.J., Packer L. Cytosolic and mitochondrial systems for nadh- and nadph-dependent reduction of alpha-lipoic acid. Free Radic. Biol. Med. 1997;22:535–542. doi: 10.1016/S0891-5849(96)00400-5. [DOI] [PubMed] [Google Scholar]
- 49.Bast A., Haenen G.R. Lipoic acid: A multifunctional antioxidant. In: Pompella A., Banhegyi G., Wellman-Rousseau M., editors. Thiol Metabolism and Redox Regulation of Cellular Function. IOS Press; Amsterdam, The Netherlands: 2002. pp. 230–237. [Google Scholar]
- 50.Packer L., Tritschler H.J., Wessel K. Neuroprotection by the metabolic antioxidant alpha-lipoic acid. Free Radic. Biol. Med. 1997;22:359–378. doi: 10.1016/S0891-5849(96)00269-9. [DOI] [PubMed] [Google Scholar]
- 51.Panigrahi M., Sadguna Y., Shivakumar B.R., Kolluri S.V., Roy S., Packer L., Ravindranath V. Alpha-lipoic acid protects against reperfusion injury following cerebral ischemia in rats. Brain Res. 1996;717:184–188. doi: 10.1016/0006-8993(96)00009-1. [DOI] [PubMed] [Google Scholar]
- 52.Johnson M.T., Yang H.S., Magnuson T., Patel M.S. Targeted disruption of the murine dihydrolipoamide dehydrogenase gene (dld) results in perigastrulation lethality. Proc. Natl. Acad. Sci. USA. 1997;94:14512–14517. doi: 10.1073/pnas.94.26.14512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Klivenyi P., Starkov A.A., Calingasan N.Y., Gardian G., Browne S.E., Yang L., Bubber P., Gibson G.E., Patel M.S., Beal M.F. Mice deficient in dihydrolipoamide dehydrogenase show increased vulnerability to mptp, malonate and 3-nitropropionic acid neurotoxicity. J. Neurochem. 2004;88:1352–1360. doi: 10.1046/j.1471-4159.2003.02263.x. [DOI] [PubMed] [Google Scholar]
- 54.Ryou M.G., Liu R., Ren M., Sun J., Mallet R.T., Yang S.H. Pyruvate protects the brain against ischemia-reperfusion injury by activating the erythropoietin signaling pathway. Stroke. 2012;43:1101–1107. doi: 10.1161/STROKEAHA.111.620088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Knott E.M., Sun J., Lei Y., Ryou M.G., Olivencia-Yurvati A.H., Mallet R.T. Pyruvate mitigates oxidative stress during reperfusion of cardioplegia-arrested myocardium. Ann. Thorac. Surg. 2006;81:928–934. doi: 10.1016/j.athoracsur.2005.08.046. [DOI] [PubMed] [Google Scholar]
- 56.Sharma A.B., Barlow M.A., Yang S.H., Simpkins J.W., Mallet R.T. Pyruvate enhances neurological recovery following cardiopulmonary arrest and resuscitation. Resuscitation. 2008;76:108–119. doi: 10.1016/j.resuscitation.2007.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Mallet R.T., Sun J., Knott E.M., Sharma A.B., Olivencia-Yurvati A.H. Metabolic cardioprotection by pyruvate: Recent progress. Exp. Biol. Med. 2005;230:435–443. doi: 10.1177/153537020523000701. [DOI] [PubMed] [Google Scholar]
- 58.Wang X., Perez E., Liu R., Yan L.J., Mallet R.T., Yang S.H. Pyruvate protects mitochondria from oxidative stress in human neuroblastoma sk-n-sh cells. Brain Res. 2007;1132:1–9. doi: 10.1016/j.brainres.2006.11.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Jitrapakdee S., Vidal-Puig A., Wallace J.C. Anaplerotic roles of pyruvate carboxylase in mammalian tissues. Cell. Mol. Life Sci. 2006;63:843–854. doi: 10.1007/s00018-005-5410-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ying W. Nad+/nadh and nadp+/nadph in cellular functions and cell death: Regulation and biological consequences. Antioxid. Redox Signal. 2008;10:179–206. doi: 10.1089/ars.2007.1672. [DOI] [PubMed] [Google Scholar]
- 61.Kirsch M., De Groot H. Nad(p)h, a directly operating antioxidant? FASEB J. 2001;15:1569–1574. doi: 10.1096/fj.00-0823hyp. [DOI] [PubMed] [Google Scholar]
- 62.Yan L.J., Christians E.S., Liu L., Xiao X., Sohal R.S., Benjamin I.J. Mouse heat shock transcription factor 1 deficiency alters cardiac redox homeostasis and increases mitochondrial oxidative damage. EMBO J. 2002;21:5164–5172. doi: 10.1093/emboj/cdf528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Yan L.J., Rajasekaran N.S., Sathyanarayanan S., Benjamin I.J. Mouse hsf1 disruption perturbs redox state and increases mitochondrial oxidative stress in kidney. Antioxid. Redox Signal. 2005;7:465–471. doi: 10.1089/ars.2005.7.465. [DOI] [PubMed] [Google Scholar]
- 64.Wu J., Jin Z., Yang X., Yan L.J. Post-ischemic administration of 5-methoxyindole-2-carboxylic acid at the onset of reperfusion affords neuroprotection against stroke injury by preserving mitochondrial function and attenuating oxidative stress. Biochem. Biophys. Res. Commun. 2018;497:444–450. doi: 10.1016/j.bbrc.2018.02.106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Sun Z., Park S.Y., Hwang E., Zhang M., Seo S.A., Lin P., Yi T.H. Thymus vulgaris alleviates uvb irradiation induced skin damage via inhibition of mapk/ap-1 and activation of nrf2-are antioxidant system. J. Cell. Mol. Med. 2017;21:336–348. doi: 10.1111/jcmm.12968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Sun Z., Du J., Hwang E., Yi T.H. Paeonol extracted from paeonia suffruticosa andr. Ameliorated uvb-induced skin photoaging via dld/nrf2/are and mapk/ap-1 pathway. Phytother. Res. 2018;32:1741–1749. doi: 10.1002/ptr.6100. [DOI] [PubMed] [Google Scholar]
- 67.Ahmad W. Dihydrolipoamide dehydrogenase suppression induces human tau phosphorylation by increasing whole body glucose levels in a c. Elegans model of alzheimer’s disease. Exp. Brain Res. 2018;236:2857–2866. doi: 10.1007/s00221-018-5341-0. [DOI] [PubMed] [Google Scholar]
- 68.Ahmad W., Ebert P.R. 5-methoxyindole-2-carboxylic acid (mica) suppresses abeta-mediated pathology in C. elegans. Exp. Gerontol. 2018;108:215–225. doi: 10.1016/j.exger.2018.04.021. [DOI] [PubMed] [Google Scholar]
- 69.Yan L.J. Reexploring 5-methoxyindole-2-carboxylic acid (mica) as a potential antidiabetic agent. Diabetes Metab. Syndr. Obes. 2018;11:183–186. doi: 10.2147/DMSO.S166485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Romoli M., Mazzocchetti P., D’Alonzo R., Siliquini S., Rinaldi V.E., Verrotti A., Calabresi P., Costa C. Valproic acid and epilepsy: From molecular mechanisms to clinical evidences. Curr. Neuropharmacol. 2018 doi: 10.2174/1570159X17666181227165722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Luis P.B., Ruiter J.P., Aires C.C., Soveral G., Tavares de Almeida I., Duran M., Wanders R.J., Silva M.F. Valproic acid metabolites inhibit dihydrolipoyl dehydrogenase activity leading to impaired 2-oxoglutarate-driven oxidative phosphorylation. Biochim. Biophys. Acta. 2007;1767:1126–1133. doi: 10.1016/j.bbabio.2007.06.007. [DOI] [PubMed] [Google Scholar]
- 72.Bergquist E.R., Fischer R.J., Sugden K.D., Martin B.D. Inhibition by methylated organo-arsenicals of the respiratory 2-oxo-acid dehydrogenases. J. Organomet. Chem. 2009;694:973–980. doi: 10.1016/j.jorganchem.2008.12.028. [DOI] [PMC free article] [PubMed] [Google Scholar]