Abstract
In French Polynesia, arthropod-borne diseases are major public health problems. From the mid-1940s, the four serotypes of dengue virus (DENV-1 to -4) have caused 15 epidemics of variable severity. In 2013, for the first time, a sustained co-circulation of two different DENV serotypes (DENV-1 and -3) was reported. The same year, Zika virus (ZIKV) caused the largest outbreak ever recorded at that time. Severe neurologic complications in adults, including Guillain-Barré syndrome and central nervous system malformations in newborns and foeteuses, such as microcephaly, were reported, and a causal link with ZIKV infection was established. In addition to mosquito-borne transmission, the potential for perinatal, sexual and blood-transfusion transmission of ZIKV was demonstrated. In 2014, chikungunya virus (CHIKV) caused an explosive outbreak. Series of Guillain-Barré syndrome temporally associated with the CHIKV epidemic were reported. Except for DENV, ZIKV and CHIKV, no other arboviruses have been detected so far, but serologic evidence suggested the past silent circulation of Ross River virus. From May 2015 DENV-1 has been the only arbovirus transmitted in French Polynesia, but the reemergence of DENV-2 is highly expected since the detection of two autochthonous cases of DENV-2 infection in June 2018.
Keywords: Arbovirus, chikungunya, dengue, French Polynesia, Pacific, Ross River, Zika
Introduction
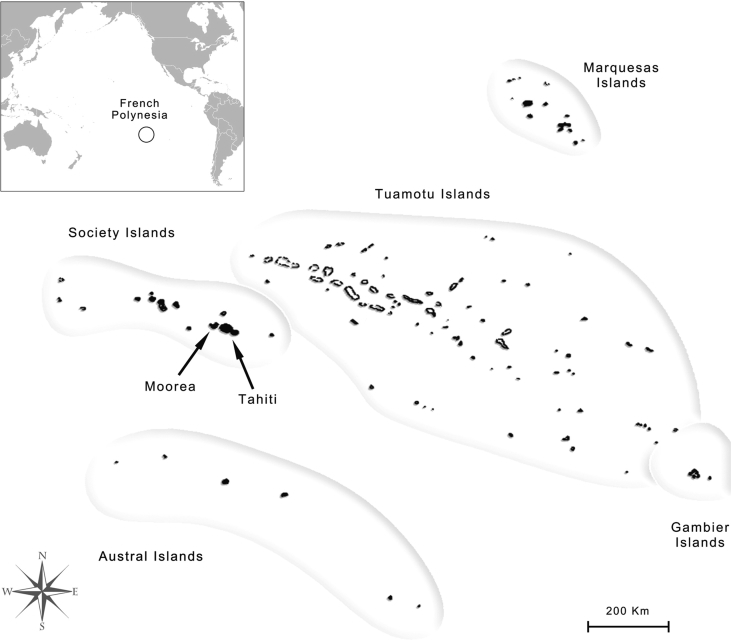
French Polynesia (FP) is a French overseas collectivity in the Southeast Pacific (Fig. 1). The population is ∼276 000 inhabitants living on 74 islands distributed among five archipelagos (Society, Tuamotu, Marquesas, Australs and Gambier). The most populated islands are Tahiti and Moorea (Windward Islands, Society archipelago) with ∼190 000 and ∼17 000 inhabitants, respectively (2017 census; http://www.ispf.pf/docs/default-source/rp2017/repart_poplegale_iles_2017_v3.pdf?sfvrsn=2). Arthropod-borne viruses (arboviruses) are transmitted to vertebrate hosts by haematophagous insects such as mosquitoes. In FP, the four serotypes of dengue virus (DENV-1 to -4; family Flaviviridae, genus Flavivirus) were the only known mosquito-borne viruses causing outbreaks until the emergence of Zika virus (ZIKV; family Flaviviridae, genus Flavivirus) and chikungunya virus (CHIKV; family Togaviridae, genus Alphavirus) [1], [2], [3]. Serologic evidence also suggested an undetected transmission of Ross River virus (RRV; family Togaviridae, genus Alphavirus) [4], [5].
Fig. 1.
Map of French Polynesia. Five archipelagos of French Polynesia are delineated by grey lines. Islands of Tahiti and Moorea are indicated by arrows. Inset map at upper left shows location of French Polynesia in Pacific Ocean (black circle).
Here we review knowledge from the literature about the epidemiologic characteristics, clinical features and modes of transmission of arboviruses in FP.
Epidemiology
Dengue viruses
The earliest dengue-like outbreaks in FP were reported during the 19th century, in 1852, 1870, 1885 and 1902 [6], [7], [8]. In 1944, concomitant with World War II, which caused a massive movement of people and the spread of mosquito vectors across the Pacific region, the first DENV outbreak of known serotype was reported (Table 1). DENV-1 was identified as the aetiologic agent of the epidemic by the serologic analysis of serum samples collected in 1951 and 1952 [9]. Then, probably as a result of the geographical isolation and small size of the population, the disease disappeared from FP until the occurrence of two consecutive outbreaks in 1964–1965 [10], [11] and 1969 [12] (Table 1). Serologic tests performed on convalescent sera showed that the viruses involved in those outbreaks were more closely related to DENV-3 [11], [12]. During the interepidemic period, only one case of infection was detected in 1968, suggesting either that the same DENV-3 strain has been silently circulating during the whole period or that multiple virus importations occurred [12]. From the 1960s, the construction of the international airport on Tahiti that increased human exchanges with DENV hyperendemic areas, accelerated urbanization, increase in population and lack of mosquito control contributed to the increasing number of DENV outbreaks due to DENV-2 in 1971, DENV-1 in 1975–1976, DENV-4 in 1979, DENV-1 in 1988–1989, DENV-3 in 1989–1990, DENV-2 in 1996–1997, DENV-1 in 2001 and then in 2006–2007, DENV-4 in 2009 and DENV-1 concomitantly with DENV-3 in 2013 [13], [14], [15], [16], [17], [18], [19], [20], [21], [22] (Table 1). Phylogenetic evidence supported that the epidemics in FP resulted from introduction of DENV strains either from the Caribbean, South America, Southeast Asia or other Pacific island countries and territories [1], [2], [3], [21], [22], [23], [24], [25] (Table 1).
Table 1.
Characteristics of dengue, Zika and chikungunya virus infection outbreaks and circulation in French Polynesia, 1944–2018
| Arbovirus | Period of outbreak | Period of circulation | No. of infections estimated during outbreak | No. of infections confirmed during outbreak | No. of hospitalizations during outbreak | No. of deaths during outbreak | Probable area of virus importation | Source |
|---|---|---|---|---|---|---|---|---|
| DENV-1 | 1944 | NA | 26 000a | NA | NA | NA | NA | [9], [18] |
| DENV-3 | Aug 1964–May 1965 | Aug 1964–Dec 1965 | NA | 7 | NA | 0 | Caribbean | [10], [11], [24] |
| DENV-3 | Jun 1969–Oct 1969 | Jun 1969–Oct 1969 | NA | NA | NA | NA | Caribbean | [12], [24] |
| DENV-2 | May 1971–Sep 1971 | May 1971–May 1975 | 42 200a | >50 | 33 | 3 | Caribbean | [13], [18], [24] |
| DENV-1 | Jul 1975–Mar 1976 | Mar 1975–Mar 1979 | 34 100a | 694 | 0 | 0 | Southeast Asia | [14], [18], [23] |
| DENV-4 | Jan 1979–May 1979 | Jan 1979–May 1988 | 37 500a | 630 | 50 | 1 | Southeast Asia | [15], [16], [18], [21] |
| Mar 1985–Jul 1985 | NA | 92 | NA | NA | ||||
| DENV-1 | Dec 1988–Jun 1989 | Nov 1988–Nov 1989 | 35 100a | 1976 | 0 | 0 | South America | [17], [18], [25] |
| DENV-3 | Aug 1989–Jun 1990 | Apr 1989–Dec 1996 | 49 500a | 1357 | 401 | 11 | Oceania | [18], [24] |
| DENV-2 | Aug 1996–Apr 1997 | Aug 1996–Dec 2000 | 43 500a | 2027 | 232 | 1 | Southeast Asia | [1], [18] |
| DENV-1 | Jan 2001–Nov 2001 | Jan 2001–Jul 2009 | 33 800 | ∼2400 | 1379 | 8 | Southeast Asia | [19], [20], [25] |
| Aug 2006–Nov 2007 | NA | 2262 | 241 | 1 | ||||
| DENV-4 | Feb 2009–Sep 2009 | Jan 2009–Dec 2010 | 24 500 | 2473 | 105 | 0 | Oceania | [20], [21] |
| DENV-3 | Feb 2013–Dec 2013 | Feb 2013–Dec 2014 | 11 000–22 000b | 1434b | 115b | 1b | South America | [22], [34] |
| DENV-1 | Feb 2013–Dec 2014 | Feb 2013–Ongoing | NA | 3678c | ∼340c | 1c | NA | [22], [26], [34] |
| ZIKV | Oct 2013–Apr 2014 | Oct 2013–Apr 2014 | 32 000 | 383 | 69 | 2 | Southeast Asia | [2], [29], [30], [31], [41] |
| CHIKV | Sep 2014–Mar 2015 | Sep 2014–Apr 2015 | 69 000 | 4443 | 844 | 18 | Caribbean | [3], [34], [44], [46], [47] |
CHIKV, chikungunya virus; DENV-1, dengue virus serotype 1; DENV-2, dengue virus serotype 2; DENV-3, dengue virus serotype 3; DENV-4, dengue virus serotype 4; NA, data not available; ZIKV, Zika virus.
Data available only for Windward Islands.
No. of estimated DENV infections, of infections confirmed by serologic and/or molecular testing, of hospitalizations and deaths reported during period of co-circulation of both DENV-1 and DENV-3 from February to December 2013.
No. of DENV infections confirmed by serologic and/or molecular testing, of hospitalizations and deaths reported during period of co-circulation of both DENV-1 and DENV-3 from February 2013 to December 2014.
Until the early 2000s, the epidemiology of DENV in FP was characterized by the alternating transmission of each DENV serotype, with a period of co-circulation of two different serotypes not exceeding 5 months (Table 1). Between February 2013 and April 2014, for the first time, a long-term simultaneous transmission of two different DENV serotypes (DENV-1 and -3) was observed [22]. Even though the delay from the previous circulation period was longer for DENV-3 (1989–1996) than for DENV-1 (2001–2009), DENV-3 rapidly disappeared while DENV-1 continued being transmitted and was still circulating as of 30 December 2018 [26].
In February 2017, while DENV-2 was actively circulating in several Pacific island countries and territories, three travelers returning from Vanuatu to participate in a soccer contest in Tahiti were confirmed as experiencing a DENV-2 infection [1]. No additional cases were reported until June 2018, when autochthonous DENV-2 infections were detected 2 weeks apart in two residents from the same island (Raiatea, Society Islands) who had not recently travelled abroad [26]. Vector control measures were immediately implemented to prevent the spread of the virus, and no other case of DENV-2 infection was reported during the following months. Nevertheless, because of the low level of herd immunity against this serotype, FP is still at high risk for a DENV-2 outbreak to occur. Indeed, serosurveys conducted in adult blood donors from Tahiti between 2011 and 2013 [27], in the general population from the five archipelagos and in schoolchildren from Tahiti in 2014 [28] and in the inhabitants from the Windward Islands in 2015 [28] confirmed that prevalence rates of immunoglobulin G (IgG) antibodies against DENV-2 (respectively 49%, 51%, 0 and 18%) were lower than against the other DENV serotypes (respectively 65%, 88%, 50% and 80% for DENV-1, 60%, 67%, 15% and 55% for DENV-3 and 60%, 61%, 14% and 42% for DENV-4).
Zika virus
The first reported outbreak of ZIKV in the Pacific region occurred in Yap Island (Federated States of Micronesia) in 2007 [29]. In October 2013, concomitant with the co-circulation of DENV-1 and DENV-3, a cluster of patients from Tahiti presenting with an exanthematous illness resembling dengue was recorded [2], [29], [30], [31]. ZIKV was identified by molecular testing in the serum of a patient who tested negative for DENV. From October 2013 to April 2014, ZIKV caused the largest outbreak ever recorded at that time, with approximately 32 000 clinical cases (11.5% of the population) reported (Table 1). Phylogenetic analysis of ZIKV strains showed that the closest strain to the viruses isolated in FP had been collected in Cambodia in 2010 [2]. The serosurvey conducted in blood donors before the first detection of ZIKV found that the proportion of participants that had IgG against this virus was very low (0.8%), confirming that ZIKV did not circulate in FP before the occurrence of the outbreak [27]. After the emergence of ZIKV, 49% of the participants recruited in the five archipelagos of FP were seropositive for anti-ZIKV IgG [32].
Chikungunya virus
CHIKV infection was first reported in the Pacific in New Caledonia in 2011 [3], [33]. In FP, CHIKV infection was detected for the first time in May 2014 in a resident returning from Guadeloupe (Caribbean), where an outbreak was ongoing [33]. Vector control measures were immediately implemented, and no secondary case of CHIKV infection was detected during the following months. From September 2014, an increasing number of patients with dengue-like illness who tested negative for both DENV and ZIKV were recorded in Tahiti, and autochthonous CHIKV infection was confirmed in seven patients [3]. Until the end of the outbreak in March 2015, it was estimated that ∼69 000 patients (25% of the population) sought medical care for CHIKV infection [34] (Table 1). Phylogenetic studies suggested that the CHIKV strain involved in the outbreak had probably been introduced from the Caribbean, although the virus was actively circulating in other Pacific island countries and territories at the time the first autochthonous cases of infection were detected [3]. The low seroprevalence of CHIKV (≤3%) found in serosurveys conducted before the outbreak in FP confirmed that the virus had not previously circulated in the population [4], [28]. After the end of the outbreak, 76% of the participants from the Windward Islands were seropositive for anti-CHIKV IgG [28].
Ross River virus
RRV is endemic to Australia and caused outbreaks between 1979 and 1980 in several Pacific island countries and territories (Fiji, Cook Islands, American Samoa, New Caledonia and Wallis and Futuna), but not in FP [4]. Although RRV infections have never been reported in FP, serosurveys conducted among blood donors during 2011–2013 and then among the general population from the five archipelagos in 2014 showed that respectively 34% and 35% of the participants had anti-RRV IgG, suggesting an undetected circulation of this arbovirus [4], [5]. Nevertheless, the analysis of blood samples collected from schoolchildren aged under 16 years in 2014 revealed that only 1% of them were seropositive for anti-RRV IgG, suggesting that RRV had not recently circulated in FP [5].
Clinical Features
DENV infections
Until the early 1970s in FP, DENV infections caused mild clinical symptoms, mostly including sudden and high fever, myalgia, arthralgia, retro-ocular headache and maculopapular rash [10], [12]. During the DENV-3 outbreak in 1964–1965, haemorrhagic symptoms (digestive, cutaneous, mucosal and genital haemorrhages) were frequently reported but without causing severe disease [10]. The DENV-2 outbreak in 1971 was characterized for the first time by the occurrence of severe haemorrhagic symptoms requiring hospitalization for 33 patients, three of whom died [13] (Table 1). Since then FP has been hit by DENV epidemics of variable severity, with DENV infection–related hospitalizations and deaths frequently recorded in children [18], [19]. Severe manifestations of the disease mostly included haemorrhage and organ impairment [19]. Neurologic complications such as acute encephalitis and Guillain-Barré syndrome (GBS) were also reported during outbreaks of DENV-1 in 2001 [19] and DENV-4 in 2009 [35].
It has been suggested that the history of exposure of the population to other DENV serotypes could have been associated to the severity of the DENV-2 outbreak in 1971 [36] and the DENV-1 outbreak in 2001 [37] through the mechanism of antibody-dependent enhancement. However, the observation that severe cases were as frequent in primary as in secondary DENV infection suggested that severe DENV epidemics could be related to the increased virulence of some virus strains [38].
ZIKV infections
Clinical symptoms of ZIKV infection in FP were estimated having occurred in 57% of patients [32] and included maculopapular rash, fatigue, fever, arthralgia, nonpurulent conjunctivitis, hand or foot oedemas, headache and myalgia [30], [31]. None of the ZIKV-infected patients developed severe symptoms that required hospitalization during the acute phase of the disease, but neurologic or autoimmune complications occurred later in 69 patients (Table 1). In November 2013, a first case of probable ZIKV infection complicated by GBS was described [39]. Until February 2014, a total of 42 cases of GBS were observed in adults, while the mean annual number of GBS in FP was five between 2009 and 2012 [30], [31], [40]. Twenty-one additional cases of neurologic complications were recorded, including nine encephalitis and meningoencephalitis, and four myelitis and other neurologic disorders (paresthesia, facial paralysis, vestibulitis) [30]. Moreover, four cases of immune thrombocytopenic purpura, one of optic neuritis and one of papillitis were diagnosed. A retrospective case–control study conducted in FP demonstrated for the first time the association between GBS and ZIKV infection, with neutralizing antibodies against ZIKV detected in the blood samples collected from all patients with GBS [40]. For the other cases of neurologic complications, the causal link could not be established, although ZIKV infection was confirmed by molecular testing for four patients and by serologic testing for six other patients [30].
After the ZIKV epidemic, an unusual increase in annual congenital cerebral malformations (twofold), brainstem dysfunction (31-fold) and severe microcephaly (14-fold) was observed among children born to women who were pregnant during the outbreak [41]. A retrospective review of congenital cerebral malformations and dysfunction, detected in a prenatal and neonatal population in FP from March 2014 to May 2015, identified 19 cases, including eight of major brain lesions and severe microcephaly, six of severe cerebral lesions without microcephaly and five of brainstem dysfunction without visible malformations. Medical termination of pregnancy was performed in 11 cases, and two infants died within the first months after birth (Table 1). It was estimated that the number of microcephaly cases associated with ZIKV infection was 95 (95% confidence interval, 34–191) per 10 000 women infected in FP during the first trimester of pregnancy [42]. A retrospective case–control study confirmed the association between maternal ZIKV infection and central nervous system malformations in newborns and foeteuses whose gestation occurred during the ZIKV outbreak in FP [43]. However, a cross-sectional study conducted among children born without birth defects after the ZIKV outbreak did not provide evidence that congenital ZIKV infection had a major negative effect on the early stages of childhood development [43]. Because this study was performed on a small case series of infants recruited shortly after the end of the ZIKV outbreak, larger cohorts of children followed over a longer period of time are needed to detect potential developmental and learning delays.
CHIKV infections
Symptomatic CHIKV infection was estimated to occur in 87% of the patients in FP [28]. In addition to the symptoms regularly reported (fever, arthralgia, myalgia and maculopapular rash) [3], [44], a case of uveitis associated to CHIKV infection was also documented [45]. A total of 844 patients were hospitalized for more than 24 hours [46] (Table 1), including 64 patients with confirmed CHIKV infection who were admitted to the intensive care unit for complications such as encephalitis, myocarditis and GBS [47]. From November 2014 to February 2015, nine cases of GBS were detected [44]. GBS incidence was increased fourfold to ninefold during this period, suggesting a causal relationship between CHIKV infection and GBS. Moreover, 21 infants developed symptoms related to CHIKV infection during the first days after birth, including two severe cases [46]. Eighteen CHIKV infection–related deaths were recorded, mostly in patients with comorbidities [44], [47] (Table 1).
Transmission
Mosquito-borne transmission
In FP, the transmission of DENV, ZIKV and CHIKV is related to two diurnal mosquito species belonging to the genus Aedes, subgenus Stegomyia: the worldwide distributed Ae. aegypti and the indigenous Ae. polynesiensis [48], [49], [50]. The silent circulation of RRV may have been supported by these same vectors but also by potential vectors from the Culex genus distributed in the region: Cx. annulirostris, Cx. sitiens and Cx. quinquefasciatus [51]. The mosquito vectors of arboviruses in FP are reviewed in a article devoted to this topic entitled ‘Mosquito vectors of arboviruses in French Polynesia,’ published in the special issue about infections in FP in this journal (New Microbes and New Infections).
Non–vector-borne transmission
Non–mosquito-borne transmission of CHIKV has not been described in FP. For DENV, perinatal infections were observed during the outbreaks of DENV-3 in 1989–1990 and DENV-1 in 2001, respectively in five and three infants born from mothers experiencing a dengue-like illness just before or during delivery [19], [52]. The potential for maternofoetal and blood transfusion transmission of ZIKV was first described in FP and was later confirmed when the virus emerged in Brazil [31]. Indeed, two cases of perinatal transmission of ZIKV were recorded in 2013 and 2014, with high ZIKV RNA loads detected in both mothers’ breast milk [53]. Even though no replicative virus particles were detected in the milk after inoculation onto mammalian cells, it has been suggested that ZIKV transmission by breast-feeding should be considered. The potential for ZIKV transmission through blood transfusion was demonstrated, with 42 (2.8%) of 1505 blood donors, although asymptomatic at the time of blood donation, found to be positive by molecular testing, including 11 who developed a Zika fever–like syndrome within 3 to 10 days after donation [54]. However, posttransfusion ZIKV infection was not documented in blood transfusion recipients in FP. Finally, ZIKV transmission by sexual intercourse, suspected for the first time in a US citizen in 2008, was also suggested in FP, as high virus RNA loads and replicative particles were detected in two semen samples collected 3 days apart from a patient who sought treatment for haematospermia [55].
Conclusion
The epidemiology of arboviruses has recently changed in FP from an alternating transmission of each of the four DENV serotypes [1] to the sustained co-circulation of two different serotypes [22] along with the emergence of viruses not previously reported in the country [2], [3]. Except for DENV, ZIKV and CHIKV, no other arboviruses have been isolated in FP so far, but serologic evidence strongly suggested the past undetected transmission of RRV [4], [5]. The existence of air links between FP and other countries where different arboviruses circulate, the presence of several potential mosquito vectors and the absence of herd immunity against those arboviruses may allow the introduction and local transmission of new mosquito-borne viruses, as previously happened with ZIKV and CHIKV [56]. However, FP can be a hub to emergence of arboviruses in other countries, as illustrated by the exported cases of ZIKV infection detected in neighbouring Pacific island countries and territories, in Europe and in the United States; phylogenetic evidence also suggests that the ZIKV strain responsible for the outbreak in Brazil had been imported from the Pacific region, including FP [31], [57]. The experience of FP with the emergence of ZIKV and CHIKV and the occurrence of severe neurologic disorders after infection [39], [40], [41], [42] demonstrated that the clinical impact of arboviruses should not be underestimated. As a result of the high risk of reemergence of DENV-2 and the constant threat of introduction of new viruses, effective surveillance of arboviruses is crucial in FP.
Conflict of Interest
None declared.
References
- 1.Aubry M., Teissier Y., Mapotoeke M., Teissier A., Giard M., Musso D. High risk of dengue type 2 outbreak in French Polynesia, 2017. Euro Surveill. 2017;22:30505. doi: 10.2807/1560-7917.ES.2017.22.14.30505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cao-Lormeau V.M., Roche C., Teissier A., Robin E., Berry A.L., Mallet H.P. Zika virus, French Polynesia, South Pacific, 2013. Emerg Infect Dis. 2014;20:1085–1086. doi: 10.3201/eid2006.140138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Aubry M., Teissier A., Roche C., Richard V., Yan A.S., Zisou K. Chikungunya outbreak, French Polynesia, 2014. Emerg Infect Dis. 2015;21:724–726. doi: 10.3201/eid2104.141741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Aubry M., Finke J., Teissier A., Roche C., Broult J., Paulous S. Silent circulation of Ross River virus in French Polynesia. Int J Infect Dis. 2015;37:19–24. doi: 10.1016/j.ijid.2015.06.005. [DOI] [PubMed] [Google Scholar]
- 5.Aubry M., Teissier A., Huart M., Merceron S., Vanhomwegen J., Roche C. Ross River virus seroprevalence, French Polynesia, 2014–2015. Emerg Infect Dis. 2017;23:1751–1753. doi: 10.3201/eid2310.170583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chassaniol D. Lettre de Mr le Chef de Service de la Santé à Mr le Directeur de l’Intérieur. Bull Soc Etudes Océaniennes EFO, Numéro spécial 231. 1885;19:218. [Google Scholar]
- 7.Buisson Les Marquises et les marquisiens. Ann Hyg Colon. 1903;6:535–551. [Google Scholar]
- 8.Hodée P. Archeveche De Papeete/Editions Saint Paul; Papeete: 1983. Tahiti 1834–1984, 150 ans de vie chrétienne en église. Papeete, French Polynesia. [Google Scholar]
- 9.Rosen L. Dengue antibodies in residents of the Society Islands, French Ocenia. Am J Trop Med Hyg. 1958;7:403–405. doi: 10.4269/ajtmh.1958.7.403. [DOI] [PubMed] [Google Scholar]
- 10.Laigret J., Rosen L., Scholammer G. Sur une épidémie de dengue survenue à Tahiti en 1964. Relations avec les ‘fièvres hémorragiques’ du Sud-Est Asiatique. Bull Soc Pathol Exot Filiales. 1967;60:339–353. [PubMed] [Google Scholar]
- 11.Rosen L. A recent outbreak of dengue in French Polynesia. Jpn J Med Sci Biol. 1967;20(Suppl):67–69. [PubMed] [Google Scholar]
- 12.Saugrain J., Rosen L., Outin-Fabre D., Moreau J.P. Une récente épidémie d’arbovirose du type dengue à Tahiti. Comparaisons avec l’épidémie de 1964. Bull Soc Pathol Exot Filiales. 1970;63:636–642. [PubMed] [Google Scholar]
- 13.Moreau J.P., Rosen L., Saugrain J., Lagraulet J. An epidemic of dengue on Tahiti associated with hemorrhagic manifestations. Am J Trop Med Hyg. 1973;22:237–241. doi: 10.4269/ajtmh.1973.22.237. [DOI] [PubMed] [Google Scholar]
- 14.Kaeuffer H., Pichon G., Merlin M., Carme B., Riviere F., Rosen L. A propos d’une épidémie contrôlée de dengue en Polynésie française. Bilan séro-épidémiologique. Med Trop. 1976;36:455–459. [Google Scholar]
- 15.Parc F., Pichon G., Tetaria C., Louis F., Laigret J. La dengue due au virus de type 4 en Polynésie française. I. Epidémiologie générale—aspects cliniques particuliers. Med Trop. 1981;41:93–96. [PubMed] [Google Scholar]
- 16.Chungue E., Boutin J.P., Roux J. Dengue surveillance in French Polynesia: an attempt to use the excess number of laboratory requests for confirmation of dengue diagnosis as an indicator of dengue activity. Eur J Epidemiol. 1991;7:616–620. doi: 10.1007/BF00218671. [DOI] [PubMed] [Google Scholar]
- 17.Chungue E., Burucoa C., Boutin J.P., Philippon G., Laudon F., Plichart R. Dengue 1 epidemic in French Polynesia, 1988–1989: surveillance and clinical, epidemiological, virological and serological findings in 1752 documented clinical cases. Trans R Soc Trop Med Hyg. 1992;86:193–197. doi: 10.1016/0035-9203(92)90568-w. [DOI] [PubMed] [Google Scholar]
- 18.Chungue E., Deparis X., Murgue B. Dengue in French Polynesia: major features, surveillance, molecular epidemiology and current situation. Pac Health Dialog. 1998;5:154–162. [Google Scholar]
- 19.Hubert B. Epidémie de dengue 1 en Polynésie française—2001. http://www.hygiene-publique.gov.pf/IMG/pdf/Dengue2001-PolynesieFrancaise.pdf Available at:
- 20.Daudens E., Lastère S., Hirschauer C., Cao-Lormeau V.M., Louette R., Roche C. Epidémiologie de la dengue et stratégies de lutte en Polynésie française, 2006–2008. Bull Epidemiol Hebd. 2009;48–50:499–503. [Google Scholar]
- 21.Cao-Lormeau V.M., Roche C., Aubry M., Teissier A., Lastère S., Daudens E. Recent emergence of dengue virus serotype 4 in French Polynesia results from multiple introductions from other South Pacific Islands. PLoS One. 2011;6:e29555. doi: 10.1371/journal.pone.0029555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cao-Lormeau V.M., Roche C., Musso D., Mallet H.P., Dalipanda T., Dofai A. Dengue virus type 3, South Pacific Islands, 2013. Emerg Infect Dis. 2014;20:1034–1036. doi: 10.3201/eid2006.131413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chungue E. Molecular epidemilogy of dengue viruses. In: Saluzzo J., Dodet B., editors. Factors in the emergence of arbovirus diseases. Elsevier; Paris: 1997. pp. 93–101. [Google Scholar]
- 24.Chungue E., Deubel V., Cassar O., Laille M., Martin P.M. Molecular epidemiology of dengue 3 viruses and genetic relatedness among dengue 3 strains isolated from patients with mild or severe form of dengue fever in French Polynesia. J Gen Virol. 1993;74:2765–2770. doi: 10.1099/0022-1317-74-12-2765. [DOI] [PubMed] [Google Scholar]
- 25.Laille M., Roche C. Comparison of dengue-1 virus envelope glycoprotein gene sequences from French Polynesia. Am J Trop Med Hyg. 2004;71:478–484. [PubMed] [Google Scholar]
- 26.Direction de la Santé de la Polynésie française Communiqué de presse du bulletin de surveillance sanitaire. https://www.service-public.pf/dsp/surveillance-veille-sanitaire/ Available at:
- 27.Aubry M., Finke J., Teissier A., Roche C., Broult J., Paulous S. Seroprevalence of arboviruses among blood donors in French Polynesia, 2011–2013. Int J Infect Dis. 2015;41:11–12. doi: 10.1016/j.ijid.2015.10.005. [DOI] [PubMed] [Google Scholar]
- 28.Aubry M., Teissier A., Huart M., Merceron S., Vanhomwegen J., Mapotoeke M. Seroprevalence of dengue and chikungunya virus antibodies, French Polynesia, 2014–2015. Emerg Infect Dis. 2018;24:558–561. doi: 10.3201/eid2403.171149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Musso D., Gubler D.J. Zika virus. Clin Microbiol Rev. 2016;29:487–524. doi: 10.1128/CMR.00072-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mallet H.P., Vial A.L., Musso D. Bilan de l’épidémie à virus Zika survenue en Polynésie française entre octobre 2013 et mars 2014. De la description de l’épidémie aux connaissances acquises après l’évènement. Bull Epidemiol Hebd. 2016;20–21:367–373. [Google Scholar]
- 31.Musso D., Bossin H., Mallet H.P., Besnard M., Broult J., Baudouin L. Zika virus in French Polynesia, 2013–14: anatomy of a completed outbreak. Lancet Infect Dis. 2018;18:e172–e182. doi: 10.1016/S1473-3099(17)30446-2. [DOI] [PubMed] [Google Scholar]
- 32.Aubry M., Teissier A., Huart M., Merceron S., Vanhomwegen J., Roche C. Zika virus seroprevalence, French Polynesia, 2014–2015. Emerg Infect Dis. 2017;23:669–672. doi: 10.3201/eid2304.161549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nhan T.X., Claverie A., Roche C., Teissier A., Colleuil M., Baudet J.M. Chikungunya virus imported into French Polynesia, 2014. Emerg Infect Dis. 2014;20:1773–1774. doi: 10.3201/eid2010.141060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Direction de la santé de la Polynésie française Bulletins de surveillance sanitaire en Polynésie française et documents associés. http://www.hygiene-publique.gov.pf/spip.php?article120 Available at:
- 35.Oehler E., Le Henaff O., Larre P., Ghawche F. Syndrome de Guillain-Barré compliquant une dengue de type 4 en Polynésie. Med Trop. 2011;71:203–204. [PubMed] [Google Scholar]
- 36.Saugrain J., Moreau J.P., Rosen L. L’épidémie de dengue de Tahiti en 1971. Evolution de la tendance hémorragique et comparaisons avec des épidémies précédentes. Bull Soc Pathol Exot Filiales. 1973;66:381–385. [PubMed] [Google Scholar]
- 37.Hubert B., Halstead S.B. Dengue 1 virus and dengue hemorrhagic fever, French Polynesia, 2001. Emerg Infect Dis. 2009;15:1265–1270. doi: 10.3201/eid1508.081500. [DOI] [PubMed] [Google Scholar]
- 38.Deparis X., Roche C., Murgue B., Chungue E. Possible dengue sequential infection: dengue spread in a neighbourhood during the 1996/97 dengue-2 epidemic in French Polynesia. Trop Med Int Health. 1998;3:866–871. doi: 10.1046/j.1365-3156.1998.00330.x. [DOI] [PubMed] [Google Scholar]
- 39.Oehler E., Watrin L., Larre P., Leparc-Goffart I., Lastère S., Valour F. Zika virus infection complicated by Guillain-Barré syndrome—case report, French Polynesia, December 2013. Euro Surveill. 2014;19:20720. doi: 10.2807/1560-7917.es2014.19.9.20720. [DOI] [PubMed] [Google Scholar]
- 40.Cao-Lormeau V.M., Blake A., Mons S., Lastère S., Roche C., Vanhomwegen J. Guillain-Barré syndrome outbreak associated with Zika virus infection in French Polynesia: a case–control study. Lancet. 2016;387:1531–1539. doi: 10.1016/S0140-6736(16)00562-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Besnard M., Eyrolle-Guignot D., Guillemette-Artur P., Lastère S., Bost-Bezeaud F., Marcelis L. Congenital cerebral malformations and dysfunction in fetuses and newborns following the 2013 to 2014 Zika virus epidemic in French Polynesia. Euro Surveill. 2016;21:30181. doi: 10.2807/1560-7917.ES.2016.21.13.30181. [DOI] [PubMed] [Google Scholar]
- 42.Cauchemez S., Besnard M., Bompard P., Dub T., Guillemette-Artur P., Eyrolle-Guignot D. Association between Zika virus and microcephaly in French Polynesia, 2013–15: a retrospective study. Lancet. 2016;387:2125–2132. doi: 10.1016/S0140-6736(16)00651-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Subissi L., Dub T., Besnard M., Mariteragi-Helle T., Nhan T., Lutringer-Magnin D. Zika virus infection during pregnancy and early childhood development, French Polynesia, 2013–2016. Emerg Infect Dis. 2018;24:1850–1858. doi: 10.3201/eid2410.172079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Oehler E., Fournier E., Leparc-Goffart I., Larre P., Cubizolle S., Sookhareea C. Increase in cases of Guillain-Barré syndrome during a chikungunya outbreak, French Polynesia, 2014 to 2015. Euro Surveill. 2015;20:30079. doi: 10.2807/1560-7917.ES.2015.20.48.30079. [DOI] [PubMed] [Google Scholar]
- 45.Nhan T., Fallevoz T., Jean-Jacques D.P., Richard V., Musso D. Chikungunya virus uveitis during French Polynesia outbreak, 2014–2015. J Clin Case Rep. 2016;6:682. [Google Scholar]
- 46.Bompard P., Marcelis L., Musso D., Fleuré M., Lastère S., Mallet H.P. Fort de France; Martinique: 2015. Surveillance épidémiologique de l’épidémie de chikungunya en Polynésie française—2014–2015. 4ème journées interrégionales de veille sanitaire des Antilles Guyane. [Google Scholar]
- 47.Koeltz A., Lastère S., Jean-Baptiste S. Intensive care admissions for severe chikungunya virus infection, French Polynesia. Emerg Infect Dis. 2018;24:794–796. doi: 10.3201/eid2404.161536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Richard V., Paoaafaite T., Cao-Lormeau V.M. Vector competence of French Polynesian Aedes aegypti and Aedes polynesiensis for Zika virus. PLoS Negl Trop Dis. 2016;10:e0005024. doi: 10.1371/journal.pntd.0005024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Richard V., Paoaafaite T., Cao-Lormeau V.M. Vector competence of Aedes aegypti and Aedes polynesiensis populations from French Polynesia for chikungunya virus. PLoS Negl Trop Dis. 2016;10:e0004694. doi: 10.1371/journal.pntd.0004694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Vazeille-Falcoz M., Mousson L., Rodhain F., Chungue E., Failloux A.B. Variation in oral susceptibility to dengue type 2 virus of populations of Aedes aegypti from the islands of Tahiti and Moorea, French Polynesia. Am J Trop Med Hyg. 1999;60:292–299. doi: 10.4269/ajtmh.1999.60.292. [DOI] [PubMed] [Google Scholar]
- 51.Marie J., Bossin H.C. First record of Wyeomyia (Wyeomyia) mitchellii (Diptera: Culicidae) in French Polynesia. J Med Entomol. 2013;50:37–42. doi: 10.1603/me12170. [DOI] [PubMed] [Google Scholar]
- 52.Poli L., Chungue E., Soulignac O., Gestas P., Kuo P., Papouin-Rauzy M. Dengue materno-fœtale. A propos de 5 cas observés durant l’épidémie de Tahiti (1989) Bull Soc Pathol Exot. 1991;84:513–521. [PubMed] [Google Scholar]
- 53.Besnard M., Lastère S., Teissier A., Cao-Lormeau V., Musso D. Evidence of perinatal transmission of Zika virus, French Polynesia, December 2013 and February 2014. Euro Surveill. 2014;19:20751. [PubMed] [Google Scholar]
- 54.Musso D., Roche C., Robin E., Nhan T., Teissier A., Cao-Lormeau V.M. Potential sexual transmission of Zika virus. Emerg Infect Dis. 2015;21:359–361. doi: 10.3201/eid2102.141363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Musso D., Nhan T., Robin E., Roche C., Bierlaire D., Zisou K. Potential for Zika virus transmission through blood transfusion demonstrated during an outbreak in French Polynesia, November 2013 to February 2014. Euro Surveill. 2014;19:20761. doi: 10.2807/1560-7917.es2014.19.14.20761. [DOI] [PubMed] [Google Scholar]
- 56.Musso D., Rodriguez-Morales A.J., Levi J.E., Cao-Lormeau V.M., Gubler D.J. Unexpected outbreaks of arbovirus infections: lessons learned from the Pacific and tropical America. Lancet Infect Dis. 2018;18:e355–e361. doi: 10.1016/S1473-3099(18)30269-X. [DOI] [PubMed] [Google Scholar]
- 57.Cao-Lormeau V.M. Tropical islands as new hubs for emerging arboviruses. Emerg Infect Dis. 2016;22:913–915. doi: 10.3201/eid2205.150547. [DOI] [PMC free article] [PubMed] [Google Scholar]