Abstract
Purpose of review:
Chronic cough is the most common presenting complaint in a pediatric aerodigestive clinic. The etiology of chronic cough is varied and often includes more than one organ system. This review aims to summarize the current literature for a multidisciplinary approach when evaluating a child with chronic cough.
Recent findings:
There is very little medical literature focused on a multidisciplinary approach to chronic cough. In the limited data available, multidisciplinary clinics have been shown to be more cost-efficient for the families of children with complex medical problems, and also increase the likelihood of successfully obtaining a diagnosis.
Summary:
There is no consensus in the literature on how to work-up a child with chronic cough presenting to an aerodigestive clinic. Current studies from these clinics have shown improved outcomes related to cost-effectiveness and identifying definitive diagnoses. Future studies evaluating clinical outcomes are necessary to help delineate the utility of testing routinely performed, and to demonstrate the impact of interventions from each specialty on quality of life and specific functional outcome measures.
Keywords: aerodigestive, multidisciplinary clinic, chronic cough, pediatrics
Introduction
Historically, multidisciplinary clinics were formed to improve the care of complex patients, as well as the quality of life of their parents, by decreasing hospital expenses, length of stay, and the burden of keeping several appointments with multiple subspecialists (1–3). With the advancement in medicine, the number of surviving extremely premature patients has increased. This created a large population of pediatric patients with complex medical problems who are technology-dependent and require care from multiple specialists (4). These multidisciplinary clinics aim to increase communication across disciplines, to reduce fragmentation of care, consolidate delivery of care, and coordinate resources (5).
In the last twenty years, pediatric aerodigestive programs have emerged as a model for delivering multidisciplinary care for patients with issues breathing, feeding, and growing (4). The first aerodigestive program was established at Cincinnati Children’s Hospital Medical Center in 1999. In 2018, we now have 50 additional centers located throughout the country, spanning 32 states (5). While an overall general framework for clinical flow exists (Figure 1), there is a heterogeneity among aerodigestive programs that is largely based on local infrastructure, resources, and limitations of sponsoring institutions (4). The 2018 Consensus Statement by Boesch et al. named essential core members of the care team to be a care coordinator, gastroenterology, otolaryngology, pulmonology, speech language pathology, and nursing (5).
Figure 1.
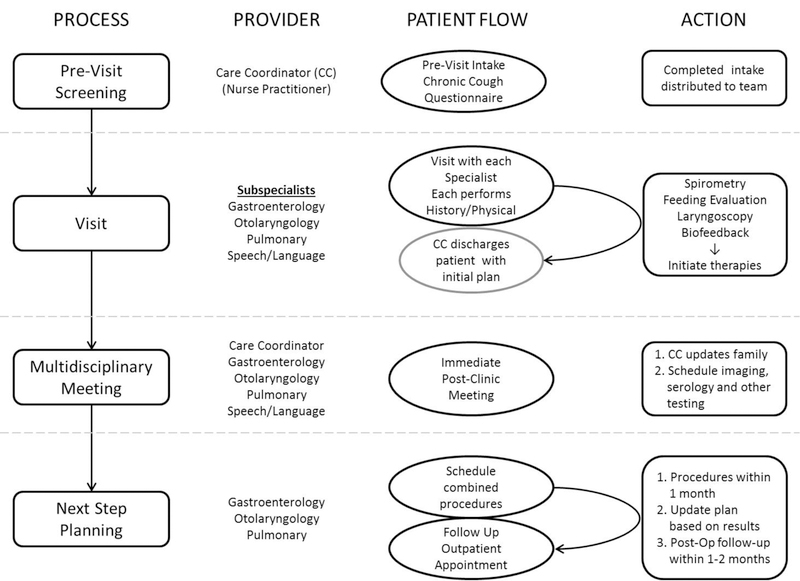
Conceptual overview of aerodigestive program core components involved in a patient encounter. General aspects to streamline centralized patient flow consist of 1) key providers including a care coordinator; 2) sharing of patient clinical information before/during clinic visits; 3) multidisciplinary discussion to develop a comprehensive plan that is then shared with the patient/family; and then 4) planning future steps including objective testing, procedures and follow up visits. Actual implementation of these core components will vary between aerodigestive programs based on local and institutional resources.
One of the most common complaints encountered in the aerodigestive clinic is chronic cough (6). Chronic cough in pediatrics was described by the American College of Chest Physicians (ACCP) as a cough lasting more than 4 weeks (7, 8); whereas, it was defined by the British Thoracic Society (BTS) as a cough lasting more than 8 weeks (9). In the last few years, the ACCP has produced two systematic reviews regarding pediatric chronic cough. The first described the etiologies of chronic cough in children and how it differs from that in adults (8). The second focused on determining the most effective treatments for chronic wet cough (10). Neither review addressed the use of a multidisciplinary approach.
In this article, we will present the last five years of literature related to the aerodigestive approach to chronic cough, and highlight the most important references. We will also provide expert opinions where data is lacking. Our aim is to outline a comprehensive approach to evaluating and managing a child with chronic cough from a multidisciplinary perspective.
Pediatric Pulmonologist Perspective
Chronic cough has been described but not studied intensively in the recent literature. In our multidisciplinary clinic, most of the patients with chronic cough have been seen by at least 1 specialist, and have failed a treatment trial before being seen (6). Cough can be seen as being caused by inflammation, increased secretions, or extra-respiratory causes (9). In general, chronic cough symptoms may be considered to be from one or a combination of any of the following (Table 1): upper airway; lower airway; GI tract, or other organ systems (cardiac, immune, or rheumatologic conditions) (8, 11, 12). Due to the complexity of the patients seen, the failure of treatment, and the broad differential diagnosis, a thorough history and physical exam is crucial to narrow down the possible etiologies and to decide whether further evaluation is needed.
Table 1.
Lower Airway and Other Conditions Associated with Chronic Cough
| Condition | Other Sign/Symptoms | Diagnostic Evaluation | Other Considerations |
|---|---|---|---|
| Lower Airway | |||
| Pulmonary Eosinophilia | Wheezing, Non-responsive to asthma therapy |
2-view Chest x-ray Spirometry |
FeNO |
| Refractory Asthma | Chest CT | ||
| Chronic Suppurative Bronchitis | Wet cough | Flexible bronchoscopy with BAL |
|
| Bronchiectasis | Recurrent pneumonia | ||
| Bronchomalacia | Fixed cough, not responsive to therapy |
||
| Vascular Sling/Ring | |||
| Complete Ring | Dyspnea | ||
| Mass | |||
| Genetic | |||
| Cystic Fibrosis | GI symptoms, poor weight gain | Sweat Test | Genetic Testing |
| Primary Ciliary Dyskinesia | Recurrent pneumonia, digital clubbing, nasal polyps Sino-pulmonary infections |
Nasal Nitric Oxide | Ciliary Biopsy |
| Immunologic | |||
| Hyper-IgE Syndromes | Atopy, non-responsive to asthma therapy |
CBC with Differential | Immunology Referral |
| Eosinophilic Syndromes | Immunoglobulin Studies | ||
| IgA Deficiency | Sino-pulmonary infections | Vaccine Response Titers | |
| Other Immunodeficiency | Skin infections | Oxidative burst | |
| Rheumatologic Conditions | Pleural effusion | Rheumatology referral | |
| Joint pain, swelling |
FeNO: Fractional exhaled nitric oxide
BAL: Bronchoalveolar lavage
CT: Computed Tomography
History of cough should include the onset, duration and description of the cough, and sputum production. Ameliorating and exacerbating factors, triggers, whether it is associated with feeds, and the presence of cough with sleep or other activities, are essential factors to include as well (9). It is also important to ask about birth history, as the cause of cough in a premature patient may be different than a patient who is born at term; medical problems that cause developmental delays thus predisposing the child to have increased risk of aspiration; and genetic disorders associated with airway abnormalities such as VACTERL syndrome. In children, protracted bacterial bronchitis caused by Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis is described to be very common, so asking about the treatments tried and duration of those treatments is recommended (7, 13). Treatment failure could be due to lack of compliance, inadequate course or inaccurate diagnosis.
With respect to physical examination, observation can be very instructive; check for facial features suggestive of genetic disorders, signs of atopy or digital clubbing (9). Observation should include the chest; examining for deformities, including but not limited to scoliosis, pectus excavatum or carinatum, increased antero-posterior diameter or chest asymmetry. An increased diameter of the chest along with digital clubbing can indicate the chronic nature of the cough and prompt further workup. Auscultation of the chest is important in narrowing the differential diagnosis, especially if abnormal.
There are multiple studies that can be performed to aid in evaluating children presenting with cough. Functional studies, such as spirometry, can be performed in aerodigestive clinic for patient 5 years and older to further understand the nature of the disease (restrictive or obstructive) (14, 15). Furthermore, it may help indicate whether the problem is intra (lower airway) or extra-thoracic (upper airway) in nature. It is a non-invasive test that may be very informative and may avoid further invasive testing. Patients with an obstructive pattern that responds to bronchodilators may be treated for asthma (16), particularly if they have a history consistent with atopy.
Chest radiography should be considered as an initial study (17) if chronic lung changes are suspected such as patients with chronic aspiration, recurrent pneumonia, or retained foreign body. Moreover, it can be obtained if gross abnormalities need to be ruled out, for instance, compression on the trachea or main bronchi by a mass or abnormal vasculature. A radiograph with no obvious abnormal findings, however, may not rule out other conditions affecting the airways (9). Chest computed tomography (CT) scan can be pursued if a higher definition study is needed (17). More specifically, high resolution chest CT should be considered to evaluate for bronchiectasis in children with productive cough outside of viral illnesses, or with positive respiratory cultures, that is non-responsive to traditional antibiotic and asthma therapies (18).
Serum studies may be considered to help delineate a specific line of thinking. For example, a complete blood count with differential (elevated eosinophils) and total immunoglobulin E (IgE) may be helpful to identify allergy-mediated conditions. Additionally, if a history of chronic infections is elicited, obtaining immunoglobulins levels and vaccine titers may be helpful in identifying humoral vs. immune mediated deficiencies, or hyper-immunoglobulin syndromes such as hyper-IgE mediated conditions. If there is a concern about recurrent lung infections with GI symptoms, screening tests such as a sweat test and fecal elastase may suggest cystic fibrosis as an etiology. Furthermore, if sino-pulmonary infections are present, then nasal nitric oxide testing and video microscopy may help screen for primary ciliary dyskinesia (19).
Flexible bronchoscopy with bronchoalveolar lavage (BAL), a minimally invasive procedure requiring anesthesia, is reserved for patients who have an unclear diagnosis, a suspected infection, chronic inflammation that failed to improve with treatment trial, or if BAL pathology will be informative in achieving a diagnosis (20). In the aerodigestive setting, it is usually done in combination with other endoscopies to avoid multiple anesthesia, thus decreasing morbidity (6). The timing of bronchoscopy in relation to recent antibiotic or systemic steroid use should be considered when interpreting results, particularly if trying to establish a baseline or response to specific therapies. If trying to establish a baseline, recent use of these therapies may lead to false negative BAL results and affect findings on direct visualization. Ultimately the window of time after steroid or antibiotic treatment to perform bronchoscopy for baseline results has not been clearly identified within the current literature. It is also important to evaluate the lower airway during spontaneous breathing. This will allow for evaluation of airway dynamics for more appropriate diagnosis of abnormal anatomy and adequate assessment of conditions such as bronchomalacia (20).
When considering treatment, asthma therapies, including inhaled steroids and bronchodilators, are often started as asthma is the most common lower airway diagnosis for chronic cough. Due to its prevalence in the general pediatric population, it is also a common co-morbid condition for children with other lower airway disorders or extra-pulmonary conditions that may be the primary source of chronic cough. If a child has a spirometry with an obstructive pattern (unless too young to perform spirometry), demonstrates clinical response to bronchodilator, and/or has symptoms suggestive of asthma (cough, wheeze, shortness of breath), asthma therapy may be initiated per national guidelines (21, 22).
Additionally, upper airway secretions secondary to rhinitis and gastroesophageal reflux are common co-morbid conditions with asthma. For this reason it is common to clinically treat rhinitis (topical nasal steroids, antihistamines) and/or reflux (H2-blockers, proton pump inhibitors), as indicated, during the same time period based on presenting symptoms. If symptoms improve, each medication can be removed systematically and symptoms monitored to determine the most effective treatment option. However, when evaluating these co-morbidities as etiologies of chronic cough, a short course of these treatments should not be considered a method of diagnosis, and may need to be stopped prior to performing further studies.
Pediatric Otolaryngologist Perspective
The otolaryngologist-aerodigestive specialist’s role in evaluating a patient with chronic cough entails a careful evaluation of the airway from the nose to the tracheobronchial tree. The differential diagnosis of pediatric chronic cough is broad. While there is significant overlap with the pulmonologist and gastroenterologist evaluation for chronic cough, there are specific upper airway conditions that should be systematically worked up in the outpatient clinical setting (Table 2). This consists of a thorough history and examination, often including a flexible nasopharyngoscopy and laryngoscopy.
Table 2.
Upper Airway Conditions Associated with Chronic Cough
| Condition | Other Sign/Symptoms | Diagnostic Evaluation | Other Considerations |
|---|---|---|---|
| Rhinitis | Non-purulent drainage | Flexible nasopharyngoscopy | Lateral Neck x-ray |
| Adenoidal Hypertrophy | Snoring, mouth breathing, feeding difficulty, |
Flexible Laryngoscopy | |
| Tonsillar Hypertrophy | Sinus CT | ||
| Adenoiditis | Headaches, purulent nasal drainage |
Direct Laryngobronchoscopy | |
| Chronic Rhinosinusitis | |||
| Paradoxical Vocal Cord Motion | Non-responsive to asthma therapy |
||
| Neurogenic cough | |||
| Laryngomalacia | Feeding difficulties | ||
| Tracheomalacia | Positional change in cough | ||
| Mass/Foreign body |
CT: Computed Tomography
At the nasal level, allergic rhinitis (AR) leading to post-nasal drainage is a relatively common cause of chronic cough. Depending on the allergen, symptoms may be seasonal or year round, and physical examination often shows pale, enlarged turbinates. Allergy medications including antihistamines and nasal steroid sprays are often started empirically, but allergy testing may be warranted. AR itself can make patients more susceptible to chronic rhinosinusitis (CRS), another cause of chronic cough. Diagnosis is made based on symptoms of purulent rhinorrhea, nasal obstruction, facial pressure, facial pain, or cough, in addition to endoscopic findings and/or changes on CT scan (23). CRS is an exacerbating co-morbid condition in children with asthma, and children with CRS with nasal polyposis should be evaluated for cystic fibrosis. CT imaging of the sinuses is the gold standard for diagnosing CRS. It should be done 4–6 weeks after antibiotic therapy, when the child is in a healthy state, to determine medical failures and appropriately select surgical candidates. Adenoiditis is an important contributing factor to CRS, especially in children under six, and adenoidectomy should be considered first line surgical therapy in these patients regardless of adenoid size (23). Adenoid hypertrophy alone can be the cause of chronic cough, particularly if the adenoids appear large upon nasopharyngeal endoscopy.
Oropharyngeal causes of chronic cough are relatively uncommon but include tonsillar hypertrophy. Enlarged pharyngeal or lingual tonsils impinging on the posterior pharyngeal wall or epiglottis, respectively, (24) can cause reflexive cough. Interestingly, chronic cough from tonsillar hypertrophy can occur in the absence of obstructive sleep symptoms.
In clinic, the larynx is evaluated with flexible fiberoptic laryngoscopy (FFL) and approximately 50% of all aerodigestive clinic patients warrant this procedure (6). Pediatric chronic cough is often attributed to laryngopharyngeal reflux (LPR) or gastroesophageal reflux. Coughing may arise in direct relationship to reflux events from irritation of vagal sensory nerve endings in the distal esophagus (25) or may arise from chronic laryngeal irritation (26). FFL can show signs suggestive of LPR, including edema and erythema of the arytenoid and posterior glottis, and laryngeal ventricle obliteration (26). However, these findings are non-specific and often erroneously attributed to reflux disease (6). Although typically 67% of patients referred to our aerodigestive clinic for chronic cough report a previous trial of anti-reflux medications, reflux is ultimately implicated to cause or exacerbate chronic cough in only 10% of patients (6). Others have also contested correlation of laryngeal findings to reflux disease in pediatric patients (27). Chronic aspiration can be seen with decreased laryngeal sensation and pooling of secretions. Laryngeal cleft should also be considered, and requires a direct laryngoscopy in the operating room with palpation of the inter-arytenoid space. Type 1 cleft, which is defined as incomplete formation of the inter-arytenoid muscles extending to the level of the true vocal cords, may present in a delayed fashion with cough, especially with feeding (28). Average inter-arytenoid height in non-aspirating patients is 3 mm (29); however, aspirating children with this height may still benefit from inter-arytenoid injection (28).
Methodical airway evaluation in the OR is also indicated to exclude subglottic and tracheal pathology. Patients that present with recurrent croup raise concern for an underlying airway abnormality, such as subglottic stenosis or tracheobronchomalacia (30). Anomalies of the great vessels, like innominate artery compression, retro-esophageal subclavian artery, pulmonary sling, or double aortic arch, may also present with cough that is often accompanied by apnea spells, recurrent pneumonia, or dysphagia. Depending on the age of the patient, chronic airway foreign bodies should also be considered. They most often present with a chronic, non-productive cough in children less than three years old (31). Usually, there is no witnessed aspiration event which clouds the picture. In rare instances, chronic foreign bodies have been found in teens misdiagnosed with reactive airway disease since early childhood. Younger children with eosinophilic esophagitis may present with airway symptoms, including chronic cough, in the absence of dysphagia (32). Tracheoesophageal fistulas can also occur, and require careful exam of the posterior tracheal mucosa. Primary ciliary dyskinesia should be considered in a child with a history of cough, sinusitis, and otitis media. This should prompt a ciliary biopsy. This can be done via nasal ciliary brushings, which are easy to obtain. However, the yield is lower than in tracheal biopsies, particularly if a child has had frequent viral illnesses, or has been exposed to noxious inhaled agents such as cigarette smoke. Cricopharyngeal achalasia is a rare cause of cough in infants and is accompanied by feeding difficulties.
Other uncommon causes of chronic cough may be identified on a thorough head and neck exam. Chiari malformation may show subtle findings of other cranial nerve involvement on flexible laryngoscopy, and head and neck exam, prompting MRI scan and eventual diagnosis (33). In rare cases, hairs or foreign bodies on the tympanic membrane may cause chronic cough via the Arnold nerve reflex mediated through the auricular branch of the vagus nerve, that innervates a portion of the EAC (34).
Speech-Language Pathologist Perspective
Speech-language pathologists are knowledgeable in the anatomical structures involved with chronic cough, as they overlap with those involved in the function of voice and swallowing (35). Some of the vocal characteristics found in patients with chronic cough include breathy, rough, strain and glottal fry qualities. Patients with chronic cough may present with coexisting laryngeal dysfunction, or voice disorders such as paradoxical vocal fold movement, muscle tension dysphonia, and laryngeal trauma (36). Chronic cough can also cause hard glottal attacks that may result in laryngeal trauma (37). Overall, there is limited information on the management of chronic cough by speech-language pathologists in the pediatric population. Therefore, clinicians base their treatment on information provided in studies completed within the adult population.
Prior to initiating speech therapy for chronic cough, patients should complete assessment and treatment for any medical conditions that may trigger the cough (38). Speech therapy for the treatment of chronic cough includes educating and training the patient on identifying cough triggers, cough suppression techniques, vocal hygiene techniques, and breathing exercises (39).
One study, that showed improvement in health-related quality of life and cough frequency used physiotherapy, speech and language therapy intervention (PSALTI) (36). In this study, participants were randomized to four one-on-one therapy sessions across 1 month on either PSALTI or the control group. PSALTI components included education, laryngeal hygiene and hydration, teaching cough control, and psychoeducation counseling. Subjects in the PSALTI group, as compared to the control group, showed improvement in health-related quality of life and cough (36). Further research is needed on the duration and number of treatment sessions. This treatment should also be considered as an adjunct to medical treatment.
In aerodigestive clinic, patients will typically complete a flexible fiberoptic laryngoscopy with the otolaryngologist to assess the anatomy of the larynx and any possible vocal trauma secondary to coughing. The speech-language pathologist may also train the patients in breathing exercise with the scope in place to provide biofeedback on abduction of the vocal cords during the exercises. If a child demonstrates impaired vocal quality, a referral is made to the voice clinic, where they are further evaluated using stroboscopy, and vocal parameters are taken using software such as Visi-Pitch (Pentax Medical), a medical acoustic product that supplements standard speech therapy with real-time processing for immediate visual and auditory biofeedback.
Pediatric Gastroenterologist Perspective
There are multiple gastrointestinal conditions that can lead to chronic cough as a primary symptom (Table 3). Gastroesophageal reflux disease (GERD) is the most frequent gastrointestinal disorder that can present with chronic cough. Other gastrointestinal causes of chronic cough include esophageal anatomic abnormality, esophageal dysmotility, and eosinophilic esophagitis (EoE). The symptoms of GERD can be nonspecific in young children. They can present with abdominal pain, regurgitation, vomiting, and poor feeding. In older children (age >8 years) and adolescents, GERD classically manifests with heartburn and regurgitation. Extra-esophageal symptoms of GERD include chronic cough and laryngeal disorders (40).
Table 3.
Gastrointestinal Conditions Associated with Chronic Cough
| Condition | Other Sign/Symptoms | Diagnostic Evaluation | Other Considerations |
|---|---|---|---|
| Gastroesophageal Reflux | Irritability, Feeding aversion, dysphagia |
EGD with biopsy | Upper GI Series |
| Eosinophilic Esophagitis | Impedance study | Swallow Study | |
| Esophageal Dysmotility | Recurrent pneumonia | Swallow evaluation pH probe |
Pepsin-A (BAL) |
| Recurrent Aspiration | |||
| Anatomic Abnormality |
EGD: Esophagogastroduodenoscopy
BAL: Bronchoalveolar Lavage
GERD develops secondary to excessive transient lower esophageal sphincter relaxation. The stimulation of the vagus nerve by the refluxate in the esophagus and microaspiration of refluxed contents into the airway contributes to chronic cough. GERD can be mediated by acid or non-acid contents in the refluxate. Bile and pepsin have been implicated in non-acid reflux disease. Acid suppression precipitates bile and can cause more inflammation (41). The acid reduction may also result in microaspiration of gastric fluid, which contains pathogens. This has been implicated as another mechanism of worsening airway disease and cough.
The diagnostic evaluation of extra-esophageal reflux involves a comprehensive history and physical examination. Barium radiographs can evaluate for anatomical abnormalities, such as tracheoesophageal fistula and esophageal stasis, which can increase the risk of aspiration. An esophagogastroduodenoscopy (EGD) with biopsies can reveal the presence of microscopic esophagitis. This has been identified in a third of pediatric patients who present with only extra-esophageal symptoms of reflux. Furthermore, up to 8% of patients with EoE can present with cough or respiratory symptoms as their primary problem (42, 43). It can also reveal the presence of candida esophagitis, which can be seen in patients on inhaled steroids. An endoscopy can also be used to relieve an obstruction of the esophageal outlet in patients with a fundoplication or achalasia. Another test commonly employed is a combined pH and multichannel intraluminal impedance (pH-MII) test, which has the advantage of evaluating for acid and non- acid reflux, and can help associate symptoms like cough with reflux episodes. Pepsin-A has been evaluated as a biomarker for gastroesophageal reflux since it is exclusively produced in the stomach (44). Salivary pepsin has shown promise as a biomarker for GERD (45). Nevertheless, there has not been significant correlation between pepsin obtained during a BAL and extra-esophageal reflux (41). The short term use of PPI therapy as a diagnostic test for cough is not recommended (46).
Treatment involves conservative measures. In infants, thickening feeds and a 2–4 week trial of an extensively hydrolyzed or amino-acid based formula may be considered. In children, elevation of the head and left lateral positioning is beneficial. In patients with acid reflux, 4–8 weeks of therapy with a PPI is recommended. If PPI treatment trial fails to alleviate symptoms, long term treatment with PPI is not recommended (22). There is a paucity of pharmacotherapy to treat non acid reflux. Prokinetics may be used in select patients, as they enhance esophageal and gastric motility. Erythromycin, a macrolide antibiotic, enhances motility in the proximal part of the gut via motilin receptors, and is one of the most common prokinetics. Metoclopramide, a dopamine antagonist, is not used frequently due to its association with tardive dyskinesia and other dystonic reactions. Transpyloric feeds can be considered in patients who are dependent on gastrostomy feeds. Laparoscopic Nissen fundoplication is usually reserved for patients with no response to the above treatment options (46). Neuromodulation with amitriptyline or gabapentin has demonstrated success in modifying the cough response in adults (47).
Conclusion
The development of pediatric aerodigestive programs is still in its early stages, particularly in terms of producing outcomes based studies that can subsequently help improve upon the current aerodigestive model. Recent studies have shown the benefits of such programs including improved length of inpatient stay, reduced hospitalization rates and total cost, and improvement of patient care and family satisfaction (5, 48). Referring patients to an aerodigestive clinic for common complaints such as chronic cough can be valuable for improved diagnosis, decreased frequency of anesthesia and successful treatment. As we have already mentioned, the differential diagnosis of chronic cough includes different systems and having simultaneous evaluation by different subspecialists can eliminate unnecessary testing. In general, further studies focused on improving the evaluation performed, comparison of different treatment modalities initiated in aerodigestive clinics, as well as impact on quality of life for both the patient and their families, are warranted.
Key Points.
Essential core members of the aerodigestive clinic care team include a care coordinator, gastroenterology, otolaryngology, pulmonology, speech language pathology, and nursing (5).
In children, protracted bacterial bronchitis caused by Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis is described to be very common (13).
In children with protracted wet cough that is non-responsive to traditional antibiotic and asthma treatments, high resolution chest CT should be considered to evaluate for bronchiectasis (18).
Flexible bronchoscopy with bronchoalveolar lavage (BAL), a minimally invasive procedure requiring anesthesia, is reserved for patients who have an unclear diagnosis, a suspected infection, chronic inflammation that failed to improve with treatment trial, or if BAL pathology will be informative in achieving a diagnosis (20).
2/3 of ADC patients warrant single or combined endoscopy including flexible bronchoscopy, esophagogastroduodenoscopy and/or direct laryngoscopy and rigid bronchoscopy (6).
Patients with chronic cough may present with coexisting laryngeal dysfunction, or voice disorders such as paradoxical vocal fold movement, muscle tension dysphonia, and laryngeal trauma. These patients may demonstrate improvement in quality of life and cough frequency with physiotherapy, speech and language therapy intervention (36).
Extra-esophageal symptoms of GERD include chronic cough and laryngeal disorders (40).
Up to 8% of patients with EoE can present with cough or respiratory symptoms as their primary problem (42, 43).
Footnotes
Compliance with Ethical Standards
Conflict of Interest
Samira Naime, Suruchi K. Batra, Caitlin Fiorillo, Maura E. Collins, Meagan Gatti, Gina M. Krakovsky, Sona Sehgal, Nancy M. Bauman, and Dinesh K. Pillai declare that they have no conflict of interest.
Human and Animal Rights
This article does not contain any studies with human or animal subjects performed by any of the authors.
Papers of particular interest, published recently, have been highlighted as:
• Of importance
•• Of major importance
Contributor Information
Samira Naime, Department of Pulmonary and Sleep Medicine, Children’s National Health System, Washington, DC, USA. snaime2@childrensnational.org.
Suruchi K. Batra, Department of Gastroenterology, Hepatology, and Nutrition, Children’s National Health System, Washington, DC, USA. sbatra@childrensnational.org.
Caitlin Fiorillo, Department of Otolaryngology-Head and Neck Surgery, Children’s National Health System, Washington, DC, USA. cfiorillo2@childrensnational.org.
Maura E. Collins, Department of Hearing and Speech, Children’s National Health System, Washington, DC, USA. MaCollins@childrensnational.org.
Meagan Gatti, Department of Pulmonary and Sleep Medicine, Children’s National Health System, Washington, DC, USA. MGATTI@childrensnational.org.
Gina M. Krakovsky, Department of Otolaryngology-Head and Neck Surgery, Children’s National Health System, Washington, DC, USA. Krakovs@childrensnational.org.
Sona Sehgal, Department of Gastroenterology, Hepatology, and Nutrition, Children’s National Health System, Washington, DC, USA. SSehgal@childrensnational.org.
Nancy M. Bauman, Department of Otolaryngology-Head and Neck Surgery, Children’s National Health System, Washington, DC, USA. NBauman@childrensnational.org.
Dinesh K. Pillai, Department of Pulmonary and Sleep Medicine, Children’s National Health System, Washington, DC, USA..
References
- 1.Galligan MM, Bamat TW, Hogan AK, Piccione J. The Pediatric Aerodigestive Center as a Tertiary Care-Based Medical Home: A Proposed Model. Curr Probl Pediatr Adolesc Health Care 2018;48(4):104–10 [DOI] [PubMed] [Google Scholar]
- 2.Appachi S, Banas A, Feinberg L, Henry D, Kenny D, Kraynack N, et al. Association of Enrollment in an Aerodigestive Clinic With Reduced Hospital Stay for Children With Special Health Care Needs. JAMA Otolaryngol Head Neck Surg 2017;143(11):1117–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Collaco JM, Aherrera AD, Au Yeung KJ, Lefton-Greif MA, Hoch J, Skinner ML. Interdisciplinary pediatric aerodigestive care and reduction in health care costs and burden. JAMA Otolaryngol Head Neck Surg 2015;141(2):101–5. [DOI] [PubMed] [Google Scholar]
- 4.Piccione J, Boesch RP. The Multidisciplinary Approach to Pediatric Aerodigestive Disorders. Curr Probl Pediatr Adolesc Health Care 2018;48(3):66–70. [DOI] [PubMed] [Google Scholar]
- 5.●Boesch RP, Balakrishnan K, Acra S, Benscoter DT, Cofer SA, Collaco JM, et al. Structure and Functions of Pediatric Aerodigestive Programs: A Consensus Statement. Pediatrics 2018.This consensus statement highlights the crucial parties involved in an aerodigestive clinic and their specific responsibilites/role.
- 6.●Rotsides JM, Krakovsky GM, Pillai DK, Sehgal S, Collins ME, Noelke CE, et al. Is a Multidisciplinary Aerodigestive Clinic More Effective at Treating Recalcitrant Aerodigestive Complaints Than a Single Specialist? Ann Otol Rhinol Laryngol 2017;126(7):537–43.This longitudinal observational study shows the success rate of forming a diagnosis and successfully treat patients that failed to improve after seeing at least one subspecialist.
- 7.Kantar A Update on Pediatric Cough. Lung 2016;194(1):9–14. [DOI] [PubMed] [Google Scholar]
- 8.Chang AB, Oppenheimer JJ, Weinberger M, Grant CC, Rubin BK, Irwin RS, et al. Etiologies of Chronic Cough in Pediatric Cohorts: CHEST Guideline and Expert Panel Report. Chest 2017;152(3):607–17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shields MD, Doherty GM. Chronic cough in children. Paediatr Respir Rev 2013;14(2):100–5; quiz 6, 37–8. [DOI] [PubMed] [Google Scholar]
- 10.Chang AB, Oppenheimer JJ, Weinberger M, Rubin BK, Irwin RS. Children With Chronic Wet or Productive Cough--Treatment and Investigations: A Systematic Review. Chest 2016;149(1):120–42. [DOI] [PubMed] [Google Scholar]
- 11.Kantar A, Bernardini R, Paravati F, Minasi D, Sacco O. Chronic cough in preschool children. Early Hum Dev 2013;89 Suppl 3:S19–24. [DOI] [PubMed] [Google Scholar]
- 12.Karabel M, Kelekci S, Karabel D, Gurkan MF. The evaluation of children with prolonged cough accompanied by American College of Chest Physicians guidelines. Clin Respir J 2014;8(2):152–9. [DOI] [PubMed] [Google Scholar]
- 13.Di Filippo P, Scaparrotta A, Petrosino MI, Attanasi M, Di Pillo S, Chiarelli F, et al. An underestimated cause of chronic cough: The Protracted Bacterial Bronchitis. Ann Thorac Med 2018;13(1):7–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Quanjer PH, Weiner DJ. Interpretative consequences of adopting the Global Lungs 2012 reference equations for spirometry for children and adolescents. Pediatr Pulmonol 2014;49(2):118–25. [DOI] [PubMed] [Google Scholar]
- 15.Jat KR. Spirometry in children. Prim Care Respir J 2013;22(2):221–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Usta Guc B, Asilsoy S, Durmaz C. The assessment and management of chronic cough in children according to the British Thoracic Society guidelines: descriptive, prospective, clinical trial. Clin Respir J 2014;8(3):330–7. [DOI] [PubMed] [Google Scholar]
- 17.Douros K, Alexopoulou E, Nicopoulou A, Anthracopoulos MB, Fretzayas A, Yiallouros P, et al. Bronchoscopic and high-resolution CT scan findings in children with chronic wet cough. Chest 2011;140(2):317–23. [DOI] [PubMed] [Google Scholar]
- 18.Gallucci M, di Palmo E, Bertelli L, Camela F, Ricci G, Pession A. A pediatric disease to keep in mind: diagnostic tools and management of bronchiectasis in pediatric age. Ital J Pediatr 2017;43(1):117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shapiro AJ, Davis SD, Polineni D, Manion M, Rosenfeld M, Dell SD, et al. Diagnosis of Primary Ciliary Dyskinesia. An Official American Thoracic Society Clinical Practice Guideline. Am J Respir Crit Care Med 2018;197(12):e24–e39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Faro A, Wood RE, Schechter MS, Leong AB, Wittkugel E, Abode K, et al. Official American Thoracic Society technical standards: flexible airway endoscopy in children. Am J Respir Crit Care Med 2015;191(9):1066–80. [DOI] [PubMed] [Google Scholar]
- 21.National Asthma E, Prevention P. Expert Panel Report 3 (EPR-3): Guidelines for the Diagnosis and Management of Asthma-Summary Report 2007. J Allergy Clin Immunol 2007;120(5 Suppl):S94–138. [DOI] [PubMed] [Google Scholar]
- 22.Perotin JM, Launois C, Dewolf M, Dumazet A, Dury S, Lebargy F, et al. Managing patients with chronic cough: challenges and solutions. Ther Clin Risk Manag 2018;14:1041–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Brietzke SE, Shin JJ, Choi S, Lee JT, Parikh SR, Pena M, et al. Clinical consensus statement: pediatric chronic rhinosinusitis. Otolaryngol Head Neck Surg 2014;151(4):542–53. [DOI] [PubMed] [Google Scholar]
- 24.Gurgel RK, Brookes JT, Weinberger MM, Smith RJ. Chronic cough and tonsillar hypertrophy: a case series. Pediatr Pulmonol 2008;43(11):1147–9. [DOI] [PubMed] [Google Scholar]
- 25.Couto M, de Diego A, Perpini M, Delgado L, Moreira A. Cough reflex testing with inhaled capsaicin and TRPV1 activation in asthma and comorbid conditions. J Investig Allergol Clin Immunol 2013;23(5):289–301. [PubMed] [Google Scholar]
- 26.Venkatesan NN, Pine HS, Underbrink M. Laryngopharyngeal reflux disease in children. Pediatr Clin North Am 2013;60(4):865–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rosen R, Mitchell PD, Amirault J, Amin M, Watters K, Rahbar R. The Edematous and Erythematous Airway Does Not Denote Pathologic Gastroesophageal Reflux. J Pediatr 2017;183:127–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Johnston DR, Watters K, Ferrari LR, Rahbar R. Laryngeal cleft: evaluation and management. Int J Pediatr Otorhinolaryngol 2014;78(6):905–11. [DOI] [PubMed] [Google Scholar]
- 29.Smith RJ, Neville MB, Bauman NM. Interarytenoid notch height relative to the vocal folds. Pilot study. Ann Otol Rhinol Laryngol 1994;103(10):753–7. [DOI] [PubMed] [Google Scholar]
- 30.Hiebert JC, Zhao YD, Willis EB. Bronchoscopy findings in recurrent croup: A systematic review and meta-analysis. Int J Pediatr Otorhinolaryngol 2016;90:86–90. [DOI] [PubMed] [Google Scholar]
- 31.Martin A, van der Meer G, Blair D, Mahadevan M, Neeff M, Barber C, et al. Long-standing inhaled foreign bodies in children: Characteristics and outcome. Int J Pediatr Otorhinolaryngol 2016;90:49–53. [DOI] [PubMed] [Google Scholar]
- 32.Kubik M, Thottam P, Shaffer A, Choi S. The role of the otolaryngologist in the evaluation and diagnosis of eosinophilic esophagitis. Laryngoscope 2017;127(6):1459–64. [DOI] [PubMed] [Google Scholar]
- 33.Chambers KJ, Setlur J, Hartnick CJ. Chiari type I malformation: presenting as chronic cough in older children. Laryngoscope 2013;123(11):2888–91. [DOI] [PubMed] [Google Scholar]
- 34.Dicpinigaitis PV, Kantar A, Enilari O, Paravati F. Prevalence of Arnold Nerve Reflex in Adults and Children With Chronic Cough. Chest 2018;153(3):675–9. [DOI] [PubMed] [Google Scholar]
- 35.Hegland K, Sapienza CJPSSD. SLP’s role in evaluation and treatment of cough function 2013;22(3):85–93. [Google Scholar]
- 36.Murry T, Milstein CFJPotASIG. Laryngeal Movement Disorders and Their Management 2016;1(3). [Google Scholar]
- 37.Vertigan AE, Gibson PGJL. The role of speech pathology in the management of patients with chronic refractory cough 2012;190(1):35–40. [DOI] [PubMed] [Google Scholar]
- 38.Ruddy BH, Sandage MJJPotASIG. Treatment for Cough: Two Sides to the Story 2017;2(3). [Google Scholar]
- 39.Krakowiak K, Dąbrowska M, Buła F, Łobacz A, Rojek D, Grabczak EM, et al. Speech therapy—a non-pharmacological method to manage difficult-to-treat chronic cough 2017;85(2):116–20. [DOI] [PubMed] [Google Scholar]
- 40.Ciorba A, Bianchini C, Zuolo M, Feo CV. Upper aerodigestive tract disorders and gastro-oesophageal reflux disease. World J Clin Cases 2015;3(2):102–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Reder NP, Davis CS, Kovacs EJ, Fisichella PM. The diagnostic value of gastroesophageal reflux disease (GERD) symptoms and detection of pepsin and bile acids in bronchoalveolar lavage fluid and exhaled breath condensate for identifying lung transplantation patients with GERD-induced aspiration. Surg Endosc 2014;28(6):1794–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hill CA, Ramakrishna J, Fracchia MS, Sternberg D, Ojha S, Infusino S, et al. Prevalence of eosinophilic esophagitis in children with refractory aerodigestive symptoms. JAMA Otolaryngol Head Neck Surg 2013;139(9):903–6. [DOI] [PubMed] [Google Scholar]
- 43.Rosen R, Amirault J, Johnston N, Haver K, Khatwa U, Rubinstein E, et al. The utility of endoscopy and multichannel intraluminal impedance testing in children with cough and wheezing. Pediatr Pulmonol 2014;49(11):1090–6. [DOI] [PubMed] [Google Scholar]
- 44.Vaezi MF, Sifrim D. Assessing Old and New Diagnostic Tests for Gastroesophageal Reflux Disease. Gastroenterology 2018;154(2):289–301. [DOI] [PubMed] [Google Scholar]
- 45.Hayat JO, Gabieta-Somnez S, Yazaki E, Kang JY, Woodcock A, Dettmar P, et al. Pepsin in saliva for the diagnosis of gastro-oesophageal reflux disease. Gut 2015;64(3):373–80. [DOI] [PubMed] [Google Scholar]
- 46.Rosen R, Vandenplas Y, Singendonk M, Cabana M, DiLorenzo C, Gottrand F, et al. Pediatric Gastroesophageal Reflux Clinical Practice Guidelines: Joint Recommendations of the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition and the European Society for Pediatric Gastroenterology, Hepatology, and Nutrition. J Pediatr Gastroenterol Nutr 2018;66(3):516–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Johnston N, Ondrey F, Rosen R, Hurley BP, Gould J, Allen J, et al. Airway reflux. Ann N Y Acad Sci 2016;1381(1):5–13. [DOI] [PubMed] [Google Scholar]
- 48.●●Mudd PA, Silva AL, Callicott SS, Bauman NM. Cost Analysis of a Multidisciplinary Aerodigestive Clinic: Are Such Clinics Financially Feasible? Ann Otol Rhinol Laryngol 2017;126(5):401–6.This study increases clinician based knowledge and awareness of financial implications by showing a detailed breakdown of the costs in a multidisciplinary clinic at one hospital.


