Abstract
PURPOSE
Hypertension trials often exclude patients with complex health problems and lack generalizability. We aimed to determine if systolic blood pressure (SBP) in patients undergoing antihypertensive treatment is associated with 1-year changes in cognitive/daily functioning or quality of life (QoL) in persons aged ≥75 years with or without complex health problems.
METHODS
We analyzed data from a population-based prospective cohort study (Integrated Systematic Care for Older Persons [ISCOPE]) with a 1-year follow-up. Stratified by SBP level in the year before baseline, we used mixed-effects linear regression models to evaluate the change from baseline to 1-year follow-up in outcome measures (Mini-Mental State Examination [MMSE], Groningen Activity Restriction Scale [GARS], and EQ-5D-3L). We adjusted for age, sex, and baseline MMSE/GARS/EQ-5D-3L scores and stratified for complex health problems as a proxy for frailty.
RESULTS
Participant (n = 1,266) age averaged 82.4 (SD 5) years, and 874 (69%) were women. For participants undergoing antihypertensive therapy (1,057; 83.5%) and with SBP <130 mm Hg, crude cognitive decline was 0.90 points MMSE, whereas in those with SBP >150 mm Hg, it was 0.14 points MMSE (ie, 0.76-point less decline; P for trend = .013). Complex health problems modified the association of SBP with cognition; the association was seen in those with antihypertensive treatment (P for trend <.001), not in those without (P for trend = .13). Daily functioning/QoL did not differ across the strata of SBP or antihypertensive treatment.
CONCLUSIONS
Participants aged ≥75 years undergoing antihypertensive treatment, with SBP ≥130 mm Hg compared to <130 mm Hg, showed less cognitive decline after 1 year, without loss of daily functioning or QoL. This effect was strongest in participants with complex health problems. More studies should be conducted to determine if there is a causal relation and to understand the mechanism of the association observed.
Key words: hypertension, old age, cognitive function, daily functioning, quality of life
INTRODUCTION
Hypertension guidelines recommend lowering systolic blood pressure (SBP) in older patients, but cohort studies have raised concern that lowering SBP too much might harm these patients by, for example, accelerating cognitive decline.1–11 A recent network meta-analysis of 17 hypertension trials proved the effectiveness and safety of lowering SBP to <130 mm Hg in patients with hypertension,12 spurring the American College of Cardiology/American Heart Association to update their guidelines to recommend lowering SBP to <130 mm Hg for noninstitutionalized older patients.13 Hypertension trials, however, often exclude older, frail patients and those with complex health problems,14 and many have questioned the generalizability and applicability of the results of these studies.15,16 In an earlier study, we reported in a population-based Dutch cohort of persons aged 85 years (n = 570) that low SBP was associated with increased all-cause mortality risk and cognitive decline but only in frail patients who were undergoing antihypertensive therapy.17
In the present study, we set out to determine if low SBP and cognitive decline are similarly associated in a relatively younger cohort of persons aged ≥75 years in the primary care setting and with or without antihypertensive treatment. We also tested for an association between SBP and daily functioning and quality of life (QoL).
METHODS
Study Design
This was a prospective cohort study based on data from the Integrated Systematic Care for Older Persons (ISCOPE) study, a cluster-randomized trial.
Data From the ISCOPE Trial
In the ISCOPE study, 560 family physicians (FPs) were approached, and 104 FPs included participants from 2009 to 2010 in Leiden, the Netherlands.18 The inclusion criterion was age ≥75 years; terminal illness and life expectancy of <3 months were the only exclusion criteria. Participants were randomized to either an integrated care plan with a functional geriatric approach or usual care.18 Of 11,476 patients in the target population, 7,285 (63.5%) answered a screening questionnaire. A random sample of 1,921 patients was selected for a 1-year follow-up. Of these, 106 (5.5%) died.
Population
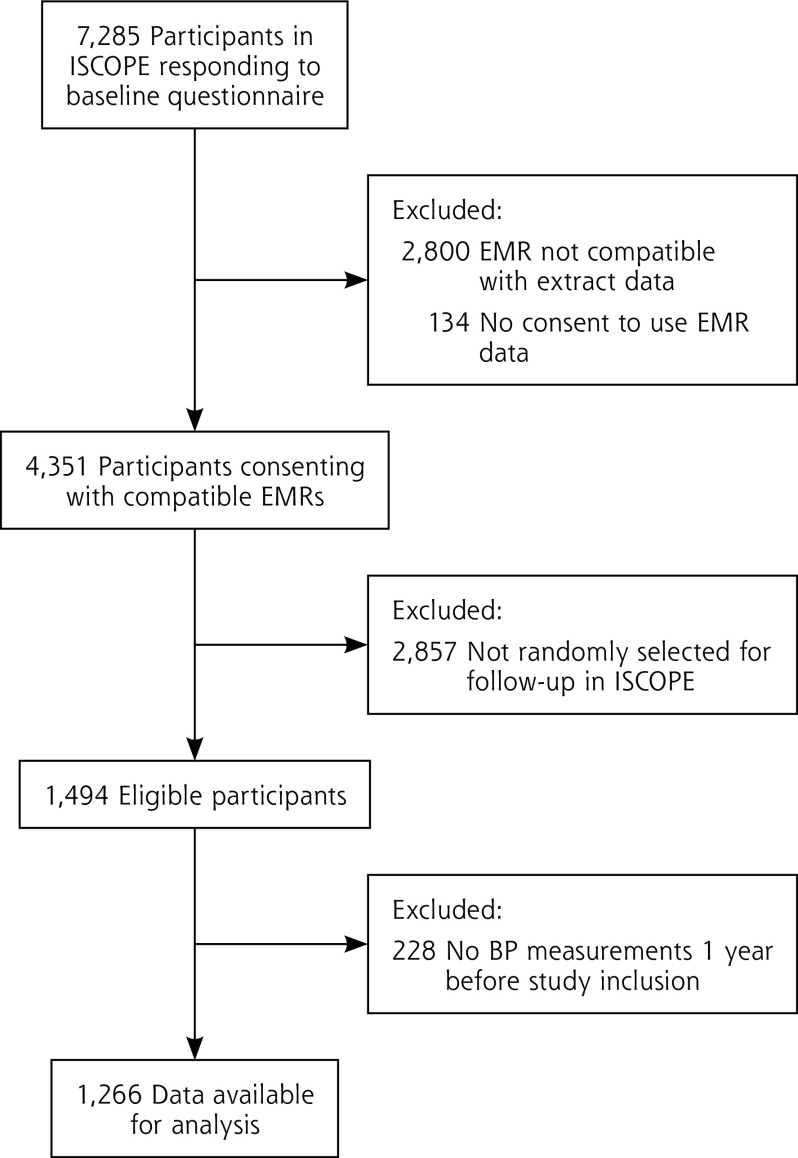
We needed electronic medical record (EMR) data to extract SBP measurements and identify antihypertensive drugs according to Anatomic Therapeutic Chemical (ATC) codes. We thus selected participants based on the following 4 criteria: (1) they consented for us to analyze their EMR data; (2) we could link their EMR data to the data set; (3) they were selected for 1 year of follow-up in ISCOPE; and (4) their SBP measurements were recorded for the year before they were included in ISCOPE (Figure 1).
Figure 1.
Study flowchart
BP = blood pressure; EMR = electronic medical record; ISCOPE = Integrated Systematic Care for Older Persons study.
Ethical Approval
Informed consent was obtained from each patient. The study protocol conformed to the ethical guidelines of the 1975 Declaration of Helsinki. The Ethics Committee of the Leiden University Medical Center (Leiden, The Netherlands [P09.096]) approved the ISCOPE study, registered in the Netherlands Trial Register (NTR1946).
Exposures
We averaged SBP values for up to 5 of the most recent measurements taken the year before baseline from the EMR. We grouped participants into 3 SBP categories (<130, 130-150, >150 mm Hg). Those with SBP <130 mm Hg were the reference group. We also used EMR data at baseline to determine which participants were undergoing antihypertensive treatment.
Outcome Measurements
In ISCOPE, research nurses made home visits at baseline and at 1-year follow-up.18 Measures included the Mini-Mental State Examination (MMSE), which measures cognitive function on a scale of 0 to 30 points (higher score indicates better function),19 and the Groningen Activity Restriction Scale (GARS) questionnaire, which measures basic and instrumental activities of daily living. The combined score for GARS ranges from 18 to 72 points (higher score indicates greater disability).20 Quality of life was assessed with the EQ-5D-3L index; participants rated their health status in 5 dimensions (mobility; self-care; usual activities; pain and discomfort; anxiety and depression) and at 3 levels (no, some, extreme),21 and we converted the values to a weighted index according to the EuroQoL Group (full health has a value of 1, death has a value of 0).22
Confounders
We a priori selected age, sex, and either MMSE, GARS, or EQ-5D-3L at baseline, depending on the outcome, as confounders. We took a causal modeling approach to identifying other potential confounders by examining change (±10%) between our crude and adjusted models for the following: living situation; income; education; diabetes; cardiovascular disease (CVD) (myocardial infarction, angina pectoris, intermittent claudication, other ischemic heart disease, stroke, transient ischemic attack, heart failure); and noncardiovascular comorbidities (cancer, diabetes, depression). None of these covariates met these confounder criteria, and the model was adjusted for as prespecified.
To identify participants with complex health problems, we used scores from a validated questionnaire covering 4 domains (functional, somatic, mental, social),18 for which each contained 4 to 9 questions. If a participant reported problems for ≥2 questions in a domain, the score was 1 for that domain; if they reported no problems, the score was 0. Participants with a score of 1 for 3 or 4 of the domains were classified as having complex problems. Details regarding scoring and grouping are described elsewhere.18
Statistical Analysis
By descriptive analysis, we compared baseline characteristics for participants with and without SBP measurements in the EMR to determine selection bias, and we then compared participants with and without antihypertensive treatment. We used the χ2 test for categorical data, t test for normally distributed data, and Wilcoxon rank sum test for nonnormally distributed continuous data.
In a primary analysis, we assessed associations between SBP category (<130, 130-150, >150 mm Hg) stratified by antihypertensive therapy (yes or no)and change in function in old age (MMSE, GARS, EQ-5D-3L) from baseline to 1-year follow-up. We estimated the change in function and 95% CIs in a crude mixed-effects regression model that only accounted for the correlated nature of data for participants with or without antihypertensive treatment by the same FP. We calculated P for trend to test a linear trend across categories of SBP and antihypertensive therapy (yes or no). We then adjusted the mixed-effects regression model for sex, age, and baseline values for MMSE, GARS, or EQ-5D-3L, depending on the outcome. Linear assumptions were tested and valid for all outcomes.
We performed several sensitivity analyses for the primary analysis as follows: (1) restricting the sample to participants with no history of CVD at baseline; (2) including the ISCOPE trial arm as a confounder, although the ISCOPE trial did not show that the integrated care plan increased QoL or daily function or changed health care use; (3) restricting the sample to participants aged <85 years; (4) excluding those with SBP <120 mm Hg.
In a secondary analysis, we took the same approach, but we stratified for participants with and without complex health problems. A 2-sided P of .05 was considered statistically significant. We used STATA 15.1 (StataCorp LP) for all analyses.
RESULTS
Study Population
Of 7,285 participants who responded to the screening questionnaire in ISCOPE, we excluded 2,934 (40.3%) because they did not consent to providing a link to their EMR data (n = 134; 1.8%) or their EMR data could not be linked with ISCOPE data (n = 2,800; 38.4%) (Figure 1). Of the 4,351 who remained, 1,494 (34.3%) were followed up for 1 year in ISCOPE. Of those, we excluded 228 (15.3%) because they had no EMR SBP measurements. Those we excluded for lack of SBP measurements were healthier overall than the study participants; they had less CVD (21% vs 40%; P <.001), less antihypertensive therapy (49% vs 84%; P <.001), less diabetes (15% vs 22%; P = .030), lower GARS score (27 vs 31; P <.001), higher EQ-5D-3L score (0.81 vs 0.77; P <.001), higher MMSE score (28 [27-29] vs 28 [26-29]; P = .019), and less complex health problems (39% vs 53%; P >.001) (Supplemental Table 1, available at http://www.AnnFamMed.org/content/17/2/100/suppl/DC1/).
The final data set comprised 1,266 participants. The average age was 82.4 years (SD 5 years) (Table 1), and 379 (30%) participants were aged ≥85 years. Most (83.5%) were undergoing antihypertensive treatment. At baseline, the sociodemographic characteristics of participants with or without antihypertensive treatment were similar, but participants with antihypertensive treatment more often had an SBP >150 mm Hg (35% vs 23%; P = .004), more CVD (48% vs 4%; P <.001), more diabetes (23% vs 15%; P = .013), higher GARS score (33.3 vs 31.2; P = .019), and lower QoL (EQ-5D-3L 0.66 vs 0.71; P = .031). Supplemental Table 2 compares baseline characteristics across SBP categories (Supplemental Table 2, available at http://www.AnnFamMed.org/content/17/2/100/suppl/DC1/).
Table 1.
Baseline Characteristics of Participants Overall and Grouped by Antihypertensive Treatment (n = 1,266)
| Characteristic | Overall (n = 1,266) |
Antihypertensive Treatment
|
P Valuea |
|
|---|---|---|---|---|
| Yes (n = 1,057) |
No (n = 209) |
|||
| Sociodemographic data | ||||
| Female, n (%) | 874 (69) | 728 (69) | 146 (70) | .72 |
| Age, years (SD) | 82.4 (5) | 82.5 (5) | 82.3 (5) | .59 |
| Primary school only, n (%) | 656 (52) | 541 (51) | 115 (55) | .33 |
| Low incomeb, n (%) | 197 (16) | 166 (16) | 31 (15) | .72 |
| Residential home, n (%) | 101 (8) | 83 (8) | 18 (9) | .72 |
| Systolic blood pressure, n (%) | ||||
| <130 mm Hg | 237 (19) | 197 (19) | 40 (19) | |
| 130-150 mm Hg | 613 (48) | 493 (47) | 120 (57) | .004 |
| >150 mm Hg | 416 (33) | 367 (35) | 49 (23) | |
| Comorbidity, n (%) | ||||
| CVDc | 511 (40) | 503 (48) | 8 (4) | <.001 |
| Diabetes mellitus | 274 (22) | 242 (23) | 32 (15) | .013 |
| Depression | 182 (14) | 148 (14) | 34 (16) | .42 |
| Cancer | 159 (13) | 134 (13) | 25 (12) | .75 |
| Complex health problemsd | 674 (53) | 571 (54) | 103 (49) | .23 |
| Baseline function, mean (SD) | ||||
| MMSEe score | 27.2 (3.1) | 27.2 (3.0) | 27.0 (3.5) | .31 |
| GARSf score | 33.0 (11.5) | 33.3 (11.4) | 31.2 (11.7) | .019 |
| EQ-5D-3Lg index values | 0.70 (0.27) | 0.66 (0.27) | 0.71 (0.26) | .031 |
CVD = cardiovascular disease; EUR = euro; GARS = Groningen Activities Restriction Scale; MMSE = Mini-Mental State Examination.
P value from χ2 test for categorical data and t test for normally distributed continuous data.
Defined as state pension only (~EUR 750 monthly).
CVD included myocardial infarction, angina pectoris, intermittent claudication, other ischemic heart disease, stroke, transient ischemic attack, and heart failure.
Defined as patients having problems in 3 or more of 4 domains (functional, somatic, mental, social).
MMSE on a scale of 0 to 30 points (higher scores indicate better cognitive function).
GARS; score ranges from 18 to 72 (higher scores indicate greater disability).
Quality of life (EQ-5D-3L index values; full health has a value of 1, dead a value of 0).
Crude 1-Year Changes in Cognitive Function, Daily Function, and Quality of Life
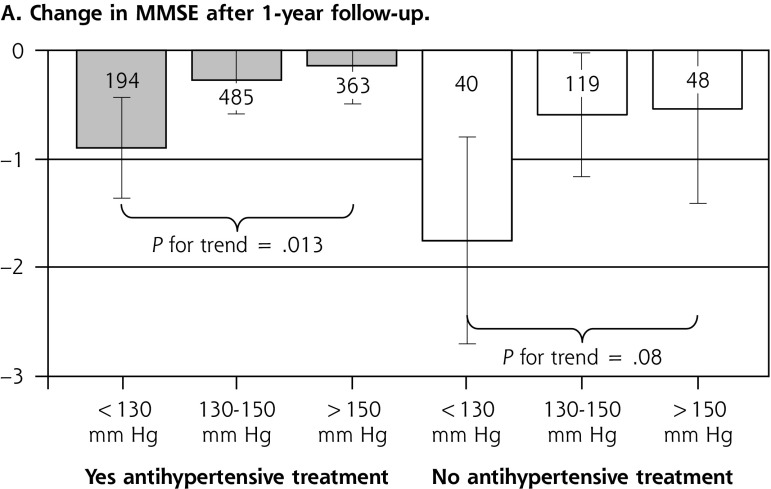
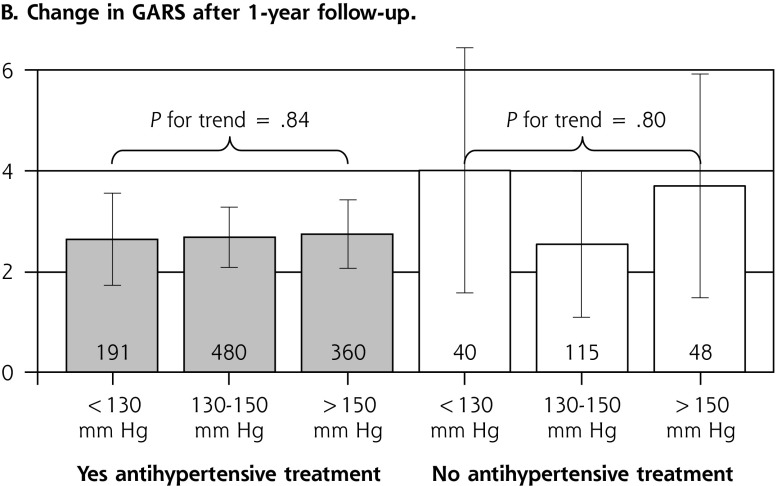
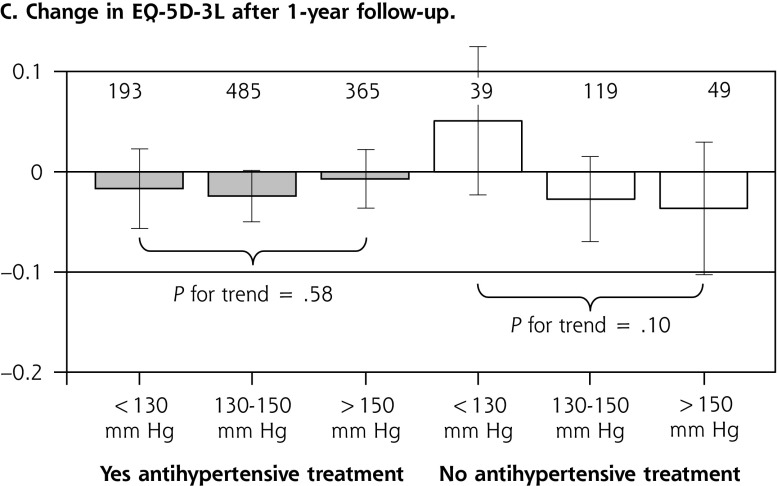
Figure 2 shows the crude estimates of changes from baseline to 1-year follow-up in cognitive function (MMSE) (A), daily functioning (GARS) (B), and QoL (EQ-5D-3L) (C). For participants undergoing antihypertensive treatment, we found a clear trend across categories of SBP; with lower SBP, cognitive decline worsened (measured by MMSE)at 1-year follow-up (P for trend .013). For participants undergoing antihypertensive treatment and with SBP <130 mm Hg, cognitive decline in1 year averaged 0.90 points MMSE (95% CI, 0.43-1.36 points), whereas it was 0.14 points MMSE (95% CI, 0.21-0.49 points) for those with SBP >150 mm Hg (a 0.76-pointless decline in participants with SBP >150 mm Hg than in those with SBP <130 mm Hg). For participants without antihypertensive treatment, we observed a similar trend, but it was not statistically significant (1.75 points, 95% CI, 0.80-2.70 points for SBP <130 mm Hg vs 0.54 points, 95% CI, 0.43-1.41 points for SBP >150 mm Hg; P for trend .08). We found no association between SBP and daily functioning or QoL for participants with or without antihypertensive therapy.
Figure 2.
Associations between systolic blood pressure, antihypertensive treatment, and change in function after a 1-year follow-up.
GARS = Groningen Activity Restriction Scale; MMSE = Mini-Mental State Examination.
Note: Numbers in or above bars equal number of participants.
Estimates, 95% CI, and P for trend from crude mixed-effects linear regression accounting for clustering within family physicians. A. Cognitive function measured by MMSE (fewer points = cognitive decline). B. Daily functioning measured by GARS (more points = more disability). C. Quality of life measured by EQ-5D-3L (fewer points = lower quality of life).
Multivariable Models for Cognitive Function, Daily Functioning, and Quality of Life
Table 2 shows changes in function for the reference group (<130 mm Hg) stratified by antihypertensive treatment for each outcome (MMSE, GARS, EQ-5D-3L). Compared to the reference group, participants with antihypertensive therapy showed less cognitive decline after 1 year by 0.71 points MMSE (95% CI, 0.20-1.22 points; P = .007) when SBP was 130-150 mm Hg and by 1.01 points MMSE (95% CI, 0.47-1.55; P <.001) when SBP was >150 mm Hg (P for trend <.001). For participants without antihypertensive therapy, the trend was in the same direction but not significant (P for trend .07). For outcomes of daily functioning and QoL, there was no association with SBP category or antihypertensive therapy (yes/no).
Table 2.
Associations Between Baseline Systolic Blood Pressure and Antihypertensive Treatment With Change in Cognitive/Daily Function and Quality of Life After 1-year Follow-Up (n = 1,266)
| Characteristic | Antihypertensive Treatment
|
|||||||
|---|---|---|---|---|---|---|---|---|
| Yes (n = 1,057) | No (n = 209) | |||||||
|
| ||||||||
| No. | Change (95% CI) | P Value | P Trend | No. | Change (95% CI) | P Value | P Trend | |
| Cognitive function | ||||||||
| <130 mm Hg | 194 | Reference | … | <.001 | 40 | Reference | … | .07 |
| 130-150 mm Hg | 485 | 0.71 (0.20-1.22) | .007 | … | 118 | 1.04 (−0.04 to 2.12) | .06 | … |
| >150 mm Hg | 362 | 1.01 (0.47-1.55) | <.001 | … | 48 | 1.22 (−0.03 to 2.47) | .06 | … |
| Daily function | ||||||||
| <130 mm Hg | 191 | Reference | … | .47 | 40 | Reference | … | .70 |
| 130-150 mm Hg | 480 | −0.08 (−1.11 to 0.96) | .88 | … | 114 | −1.73 (−4.54 to 1.10) | .42 | … |
| >150 mm Hg | 359 | −0.37 (−1.47 to 0.74) | .51 | … | 48 | −0.75 (−4.02 to 2.52) | .65 | … |
| Quality of life | ||||||||
| <130 mm Hg | 193 | Reference | … | .17 | 39 | Reference | … | .14 |
| 130-150 mm Hg | 484 | 0 (−0.04 to 0.04) | .98 | … | 118 | −0.06 (−0.14 to 0.02) | .13 | … |
| >150 mm Hg | 364 | 0.03 (−0.02 to 0.07) | .24 | … | 49 | −0.07 (−0.16 to 0.02) | .12 | … |
GARS = Groningen Activities Restriction Scale; MMSE = Mini-Mental State Examination; Reference = <130 mm Hg; SBP = systolic blood pressure.
Note: Multivariable mixed-effects regression model adjusted for age, sex, baseline MMSE/GARS/EQ-5D-3L and accounting for clustering within family physicians.
Reading example: Patients undergoing antihypertensive treatment and with a baseline SBP >150 mm Hg had 1.01 points MMSE (95% CI, 0.47-1.55 points) less cognitive decline compared to patients undergoing antihypertensive therapy and with a baseline SBP <130 mm Hg (Reference).
Sensitivity Analyses
The findings remained robust when we restricted the sample to participants with no history of CVD at baseline (Supplemental Table 3, available at http://www.AnnFamMed.org/content/17/2/100/suppl/DC1/). All other sensitivity analyses, including adding the ISCOPE trial arm as a confounder, restricting the sample to participants aged <85 years (n = 887), and excluding participants with SBP <120 mm Hg (n = 70), showed similar results (data not shown).
Secondary Analysis for Complex Health Problems
For participants with complex health problems (n = 674; 53%), we found the same association (Table 3). Compared to the reference group (SBP <130 mm Hg), participants showed less cognitive decline after 1 year by 0.99 points MMSE (95% CI, 0.32-1.66 points; P = .004) when SBP was 130-150 mm Hg and by 1.39 points MMSE (95% CI, 0.68-2.11 points; P <.001) when SBP was >150 mm Hg (P for trend <.001). This association was not found for participants without complex health problems (P for trend .35) (Supplemental Table 4, available at http://www.AnnFamMed.org/content/17/2/100/suppl/DC1/). Complex health problems did not modify the effect on daily functioning or QoL.
Table 3.
Subgroup Analysis Restricted to Patients With Complex Health Problems (n = 674)
| Characteristic | Antihypertensive Treatment
|
|||||||
|---|---|---|---|---|---|---|---|---|
| Yes (n = 571) | No (n = 103) | |||||||
|
| ||||||||
| No. | Change (95% CI) | P Value | P Trend | No. | Change (95% CI) | P Value | P Trend | |
| Cognitive function | ||||||||
| <130 mm Hg | 117 | Reference | … | < .001 | 20 | Reference | … | .13 |
| 130-150 mm Hg | 258 | 0.99 (0.32-1.66) | .004 | … | 60 | 1.90 (0.05-3.75) | .044 | … |
| >150 mm Hg | 189 | 1.39 (0.68-2.11) | <.001 | … | 22 | 1.78 (−0.42 to 3.98) | .11 | … |
| Daily function | ||||||||
| <130 mm Hg | 115 | Reference | … | .59 | 20 | Reference | … | .65 |
| 130-150 mm Hg | 254 | −0.18 (−1.57 to 1.20) | .79 | … | 57 | −2.02 (−6.14 to 2.10) | .34 | … |
| >150 mm Hg | 188 | −0.40 (−1.88 to 1.09) | .60 | … | 22 | −1.20 (−6.11 to 3.72) | .63 | … |
| Quality of life | ||||||||
| <130 mm Hg | 117 | Reference | … | .61 | 19 | Reference | … | .19 |
| 130-150 mm Hg | 257 | −0.03 (−0.08 to 0.03) | .21 | … | 60 | −0.11 (−0.23 to 0.01) | .08 | … |
| >150 mm Hg | 190 | 0.01 (−0.05 to 0.07) | .99 | … | 22 | −0.10 (−0.24 to 0.04) | .16 | … |
GARS = Groningen Activities Restriction Scale; MMSE = Mini-Mental State Examination; Reference = <130 mm Hg; SBP = systolic blood pressure.
Note: Associations of baseline systolic blood pressure and antihypertensive treatment with change in cognitive/daily function and quality of life after 1-year follow-up (n = 1,266). Multivariable mixed-effects regression model adjusted for sex, age, baseline MMSE/GARS/EQ-5D-3L, and accounting for clustering within family physicians.
Reading example: Patients undergoing antihypertensive treatment and with a baseline SBP >150 mm Hg had 1.39 points MMSE (95% CI, 0.68-2.11 points) less cognitive decline compared to patients undergoing antihypertensive therapy and with a baseline SBP <130 mm Hg (Reference).
DISCUSSION
In this large Dutch primary-care cohort of persons aged ≥75 years, those undergoing antihypertensive treatment had less cognitive decline if their SBP in the year before baseline was ≥130 mm Hg. The association was strongest in those with complex health problems. Daily functioning and QoL were the same across the strata of SBP and antihypertensive treatment. Sensitivity analyses excluding participants with CVD or including the trial arm of the ISCOPE trial in the model supported these findings.
Comparison With Previous Studies
We interpret the differences in MMSE scores (0.71-1.39 per year depending on SBP category) to be statistically significant as well as clinically meaningful. The literature suggests a decline of 3 to 5 points over 5 years to be clinically relevant.23,24 Based on our earlier study, in which we followed an older cohort over a period of5 years, we found no evidence that this decline would stop after 1 year or regress to the mean.17 Our present study builds on a study by Mosello and Simoni25 but is much larger (1,266 vs 172 participants) and was conducted in a different setting (primary care vs outpatient memory clinics). Mosello and Simoni25 included only patients with dementia or mild cognitive impairment. Our study included participants often excluded from trials because they are sicker and have complex health problems. We found the same associations but also demonstrated that complex health problems changed the association. These findings are consistent with those of other studies reporting that associations changed with frailty.26,27 Studies of older patients which did not stratify according to antihypertensive treatment found either no association28 or an association between higher SBP, better cognition, and lower risk of dementia.29 The present study helps to explain this difference by showing that in participants without complex health problems as a proxy for frailty, low SBP is not as clearly associated with cognitive decline30 as in those with complex health problems.
We also found no evidence that SBP is associated with changes in daily function in participants with antihypertensive therapy, though prior studies identified both positive and negative associations.3,31,32 A cohort study of 35 centenarians in Poland found at follow-up that higher SBP benefitted daily activity.3 The Leiden 85-plus Study found that higher SBP was associated with lower activities of daily living disability over 5 years.31 In contrast, a US longitudinal cohort study of approximately 600 persons aged 75 years found that high SBP was associated with declining physical function (measured by gait speed) over 10 years of follow-up.32 This diametric association might be explained by age; there was evidence that high SBP was associated with physical function at age 75 years, but that high SBP increased physical function in those aged >85 years and aged >100 years. Most studies that assessed the association between SBP and function in old age did not assess QoL. A Polish study of approximately 11,500 elderly patients found that those treated for hypertension (especially those on multiple antihypertensive medications) had optimal QoL with higher SBP,33 but our present results suggest no association between SBP and 1-year change in daily function or QoL.
Strengths and Limitations
Strengths of the present study include the large number of older participants recruited by a large group of FPs and the extensive measurements that consider cognitive function, daily functioning, and QoL. The study also has the following limitations: it was observational; therefore, we cannot exclude residual confounding. However, the strength of the associations we identified, consistency with prior studies, dose-response relation, and temporal relation of SBP measurements and outcome assessments all point toward a causal interpretation. We do not have data for participants whose family physicians were using an incompatible EMR. Incompatible EMRs at the level of FPs is unlikely to introduce selection bias, nor is the random selection of participants for a 1-year follow-up. Participants excluded because of no SBP measurements recorded in the year before the start of the study were even healthier, and they did not otherwise differ from responders. The latter limitation can also be considered a strength because we included sicker, older participants with a high incidence of CVD and undergoing antihypertensive treatment, and this ever-increasing group is often excluded from trials.
Conclusions and Future Directions
Our present findings suggest the importance of close blood pressure monitoring for patients undergoing antihypertensive treatment, to maintain optimal cognition especially in those with complex health problems, those for whom we observed the strongest effect. More studies should be conducted to examine whether there is a causal relation and to understand the mechanism of the association observed. Early trials, such as the Dutch Discontinuation of Antihypertensive Treatment in Elderly People (DANTE) study, asked if deprescribing antihypertensive medication improved cognitive function in older patients with mild cognitive impairment but found no evidence of effect after 16 weeks of follow-up.34 The long-term effects of deprescribing antihypertensive drugs are still uncertain, but a recent Cochrane review found that withdrawing from antihypertensive therapy in old age did not increase mortality.35 We encourage researchers to conduct new randomized trials to test the long-term effectiveness and safety of deprescribing antihypertensive drugs to raise SBP, especially in frail older patients. Until the results of these new trials are available, clinicians must decide daily on the appropriate treatment for hypertension in older patients, with limited evidence.15,16 Antihypertensive treatment is intended to reduce the risk of cardiovascular events and to preserve cognitive/daily function and QoL in older people. However, our results show that SBP <130 mm Hg with antihypertensive treatment is associated with additional cognitive decline. Our results suggest that SBP thresholds for treatment should be redefined, especially for frail older persons.36 Because older patients are more likely to be frail and experience accelerated cognitive decline, clinicians are advised to be cautious about lowering SBP too much.
Acknowledgments
The authors wish to thank David A. Leon, PhD, for providing input in the early stages of analysis and Kali Tal, PhD, for editorial assistance.
Footnotes
Conflicts of interest: authors report none.
Funding support: Professor Streit’s research was supported by grants (P2BEP3_165353) from the Swiss National Science Foundation (SNF) and the Gottfried and Julia Bangerter-Rhyner Foundation, Switzerland. The original ISCOPE study was funded by ZonMw, the Netherlands, Organization for Health Research and Development (ZonMw No. 311060201). The funding source had no role in the design or conduct of the study; the collection, management, analysis, or interpretation of the data; the preparation, review, or approval of the manuscript; or the decision to submit the manuscript for publication.
Supplemental Materials: Available at http://www.AnnFamMed.org/content/17/2/100/suppl/DC1/.
References
- 1.Yeung SE, Thornton WL. Age-related effects of blood pressure on everyday cognitive function in community-dwelling women. Neuropsychol Dev Cogn B Aging Neuropsychol Cogn. 2011; 18(6): 733–755. [DOI] [PubMed] [Google Scholar]
- 2.van Vliet P, Sabayan B, Wijsman LW, et al. NT-proBNP, blood pressure, and cognitive decline in the oldest old: the Leiden 85-plus Study. Neurology. 2014; 83(13): 1192–1199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Szewieczek J, Dulawa J, Gminski J, et al. Better cognitive and physical performance is associated with higher blood pressure in centenarians. J Nutr Health Aging. 2011; 15(8): 618–622. [DOI] [PubMed] [Google Scholar]
- 4.Pieraccioli MC, Mossello E, Nesti N, et al. Low ambulatory blood pressure as predictor of cognitive decline in older subjects with dementia or mild cognitive impairment. Eur Geriatr Med. 2012; 3(1): S141. [Google Scholar]
- 5.Oveisgharan S, Solomon A, Kivipelto M, Hachinski V. Blood pressure, memory, and executive function changes in late-life. Alzheimer’s and Dementia. 2012; (1): P88. [Google Scholar]
- 6.Nilsson SE, Read S, Berg S, Johansson B, Melander A, Lindblad U. Low systolic blood pressure is associated with impaired cognitive function in the oldest old: longitudinal observations in a population-based sample 80 years and older. Aging Clin Exp Res. 2007; 19(1): 41–47. [DOI] [PubMed] [Google Scholar]
- 7.Mossello E, Pieraccioli M, Nesti N, et al. Effects of low blood pressure in cognitively impaired elderly patients treated with antihypertensive drugs. JAMA Intern Med. 2015; 175(4): 578–585. [DOI] [PubMed] [Google Scholar]
- 8.Molander L, Lövheim H, Norman T, Nordström P, Gustafson Y. Lower systolic blood pressure is associated with greater mortality in people aged 85 and older. J Am Geriatr Soc. 2008; 56(10): 1853–1859. [DOI] [PubMed] [Google Scholar]
- 9.Lv YB, Zhu PF, Yin ZX, et al. A U-shaped association between blood pressure and cognitive impairment in Chinese elderly. J Am Med Dir Assoc. 2017; 18(2): 193.e7–193.e13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Corrada MM, Hayden KM, Paganini-Hill A, et al. Age of onset of hypertension and risk of dementia in the oldest-old: the 90+ Study. Alzheimers Dement. 2017; 13(2): 103–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Duarte PO, Duarte MGF, Pelichek A, et al. Cardiovascular risk factors and inflammatory activity among centenarians with and without dementia. Aging Clin Exp Res. 2017; 29(3): 411–417. [DOI] [PubMed] [Google Scholar]
- 12.Bangalore S, Toklu B, Gianos E, et al. Optimal systolic blood pressure target after SPRINT: insights from a network meta-analysis of randomized trials. Am J Med. 2017; 130(6): 707–19 e8. [DOI] [PubMed] [Google Scholar]
- 13.Whelton PK, Carey RM, Aronow WS, et al. ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. Hypertension. 2018; 71(6): 1269–1324. [DOI] [PubMed] [Google Scholar]
- 14.Messerli FH, Sulicka J, Gryglewska B. Treatment of hypertension in the elderly. N Engl J Med. 2008; 359(9): 972–973, author reply 973–974. [PubMed] [Google Scholar]
- 15.Lonn EM, Yusuf S. Should patients with cardiovascular risk factors receive intensive treatment of hypertension to <120/80 mm Hg target? An antagonist view from the HOPE-3 trial (Heart Outcomes Evaluation-3). Circulation. 2016; 134(18): 1311–1313. [DOI] [PubMed] [Google Scholar]
- 16.Oparil S, Lewis CE. Should patients with cardiovascular risk factors receive intensive treatment of hypertension to <120/80 mm Hg target? A protagonist view from the SPRINT trial (Systolic Blood Pressure Intervention Trial). Circulation. 2016; 134(18): 1308–1310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Streit S, Poortvliet RKE, Gussekloo J. Lower blood pressure during antihypertensive treatment is associated with higher all-cause mortality and accelerated cognitive decline in the oldest-old-data from the Leiden 85-plus Study [published online ahead of print May 8, 2018] Age Ageing. 10.1093/ageing/afy072. [DOI] [PubMed] [Google Scholar]
- 18.Blom J, den Elzen W, van Houwelingen AH, et al. Effectiveness and cost-effectiveness of a proactive, goal-oriented, integrated care model in general practice for older people. A cluster randomised controlled trial: Integrated Systematic Care for older People—the ISCOPE study. Age Ageing. 2016; 45(1): 30–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975; 12(3): 189–198. [DOI] [PubMed] [Google Scholar]
- 20.Kempen GI, Miedema I, Ormel J, Molenaar W. The assessment of disability with the Groningen Activity Restriction Scale. Conceptual framework and psychometric properties. Soc Sci Med. 1996; 43(11): 1601–1610. [DOI] [PubMed] [Google Scholar]
- 21.EuroQol Group. EuroQol—a new facility for the measurement of health-related quality of life. Health Policy. 1990; 16(3): 199–208. [DOI] [PubMed] [Google Scholar]
- 22.EuroQoL Group. EQ-5D–3L user guide. https://euroqol.org/wp-content/uploads/2016/09/EQ-5D-3L_UserGuide_2015.pdf. Published April 2015 Accessed January 4, 2019.
- 23.Tombaugh TN. Test-retest reliable coefficients and 5-year change scores for the MMSE and 3MS. Arch Clin Neuropsychol. 2005; 20(4): 485–503. [DOI] [PubMed] [Google Scholar]
- 24.Schmand B, Lindeboom J, Launer L, Dinkgreve M, Hooijer C, Jonker C. What is a significant score change on the mini-mental state examination? Int J Geriatr Psychiatry. 1995; 10(5): 411–414. [Google Scholar]
- 25.Mossello E, Simoni D. High blood pressure in older subjects with cognitive impairment. Monaldi Arch Chest Dis. 2016; 84(1–2): 730. [DOI] [PubMed] [Google Scholar]
- 26.Odden MC, Wu C, Shlipak MG, et al. ; Health ABC Study. Blood pressure trajectory, gait speed, and outcomes: the Health, Aging, and Body Composition study. J Gerontol A Biol Sci Med Sci. 2016; 71(12): 1688–1694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Odden MC, Peralta CA, Haan MN, Covinsky KE. Rethinking the association of high blood pressure with mortality in elderly adults: the impact of frailty. Arch Intern Med. 2012; 172(15): 1162–1168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Johnson KC, Margolis KL, Espeland MA, et al. ; Women’s Health Initiative Memory Study and Women’s Health Initiative Investigators. A prospective study of the effect of hypertension and baseline blood pressure on cognitive decline and dementia in postmenopausal women: the Women’s Health Initiative Memory Study. J Am Geriatr Soc. 2008; 56(8): 1449–1458. [DOI] [PubMed] [Google Scholar]
- 29.Kivipelto M, Helkala EL, Laakso MP, et al. Midlife vascular risk factors and Alzheimer’s disease in later life: longitudinal, population based study. BMJ. 2001; 322(7300): 1447–1451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Williamson JD, Supiano MA, Applegate WB, et al. ; SPRINT Research Group. Intensive vs standard blood pressure control and cardiovascular disease outcomes in adults aged ≥75 years: a randomized clinical trial. JAMA. 2016; 315(24): 2673–2682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sabayan B, Oleksik AM, Maier AB, et al. High blood pressure and resilience to physical and cognitive decline in the oldest old: the Leiden 85-plus Study. J Am Geriatr Soc. 2012; 60(11): 2014–2019. [DOI] [PubMed] [Google Scholar]
- 32.Rosano C, Longstreth WT, Jr, Boudreau R, et al. High blood pressure accelerates gait slowing in well-functioning older adults over 18-years of follow-up. J Am Geriatr Soc. 2011; 59(3): 390–397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zygmuntowicz M, Owczarek A, Elibol A, Olszanecka-Glinianowicz M, Chudek J. Blood pressure for optimal health-related quality of life in hypertensive patients. J Hypertens. 2013; 31(4): 830–839. [DOI] [PubMed] [Google Scholar]
- 34.Moonen JE, Foster-Dingley JC, de Ruijter W, et al. Effect of discontinuation of antihypertensive treatment in elderly people on cognitive functioning–the DANTE Study Leiden: a randomized clinical trial. JAMA Intern Med. 2015; 175(10): 1622–1630. [DOI] [PubMed] [Google Scholar]
- 35.Jongstra S, Harrison JK, Quinn TJ, Richard E. Antihypertensive withdrawal for the prevention of cognitive decline. Cochrane Database Syst Rev. 2016; 11: CD011971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Benetos A, Rossignol P, Cherubini A, et al. Polypharmacy in the aging patient: management of hypertension in octogenarians. JAMA. 2015; 314(2): 170–180. [DOI] [PubMed] [Google Scholar]