Abstract
Background:
In 2006, our healthcare system created a hospital Evidence-based Practice Center (EPC) to support the local delivery of high quality, safe and high value patient care. Since then, the importance of healthcare staff work life has also been highlighted, and together these four elements form the Quadruple Aim framework. Synergistic to this Aim, the Magnet® program promotes and recognizes organizational nursing excellence.
Objective:
To examine the EPC’s work to inform nursing policy and practice in support of the goals of the Quadruple Aim framework and Magnet® designation.
Methods:
Methods used included: (a) descriptive analysis of the hospital EPC’s database of rapid reviews; and (b) administration of a 40-item electronic questionnaire to nurses who requested an EPC review during fiscal years (FY) 2015 and 2016.
Results:
Of 308 rapid reviews completed in the EPC’s first 10 years, 59 (19%) addressed nursing topics. The proportion of reviews relevant to nursing increased from 5% (2/39) in the center’s first 2 years to 44% (25/60) in FY 2015–2016. The majority of nursing reviews (39/59) examined processes of care. Of 23 nurses eligible to participate in the survey, 21 responded (91%). Nurses with administrative or managerial responsibilities requested 70% of reviews; clinical nurse specialists and bedside nurses requested 17% and 9%, respectively. Reviews were used to support clinical program development (48%), provide clinical guidance (33%), update nursing policies or procedures (24%) and develop training and curricula (24%). Nurses were satisfied with the hospital EPC reviews (mean; 4.7/5), and 95% indicated they were likely to request a future review.
Linking Evidence to Action:
A dedicated hospital EPC in partnership with nursing offers a unique mechanism for promoting a culture of evidence-based practice. Nurses at all organizational levels, use the services of a hospital EPC to inform nursing policy and practice, and are highly satisfied with the process, supporting the Quadruple Aim and Magnet® designation.
Keywords: Evidence-based nursing, evidence-based practice, evidence-based practice center, rapid reviews, quality improvement
Introduction
Evidence-based practice (EBP) is widely accepted as a core tenet of high-quality cost-effective patient care. The Institute of Medicine’s Roundtable on Evidence Based Practice recommends that, by the year 2020, 90% of clinical decisions should be evidence-based (Institutes of Medicine, 2009). This emphasis on evidence-based care operationalizes the Triple Aim initiative, which sets three overarching goals for healthcare delivery: (a) improving population health, (b) improving the patient experience, and (c) reducing per capita cost of care (Berwick, Nolan, & Whittington, 2008). Challenges in pursuing the Triple Aim have subsequently highlighted the need to support the health care workforce. Thus, the Triple Aim has expanded to become the Quadruple Aim with the inclusion of a focus on improving the work life of health care providers and staff (Bodenheimer & Sinsky, 2014; Ruddy, Thomas-Hemak, & Meede, 2016; Sikka, Morath, & Leape, 2015). These overarching strategies are used to frame health care policy in the United States and internationally (e.g., in Canada; Liddy & Keely, 2018; and Australia (Productivity Commission, 2017).
One mechanism for addressing issues of safety, effectiveness and cost of health technologies is through the use of health technology assessment (HTA; Gagnon, Desmartis, Poder, & Witteman, 2014[. Often, HTA is conducted by or for national or international organizations (Gagnon, 2014). With growing awareness of the importance of institutional context, however, HTA is increasingly being conducted at the hospital level (Gagnon, 2014).
In 2006, the University of Pennsylvania Health System (UPHS) created an Evidence-based Practice Center (EPC), an HTA unit, to support the integration of the best available evidence into institutional decision-making in order to strengthen the quality and safety of individual-level patient care and optimize the value of care provided across the health system (Jayakumar et al., 2016; Umscheid, Williams, & Brennan, 2010). Our healthcare system-based EPC is interprofessional and provides rapid systematic reviews of the scientific literature to inform the development of local policies and practices, as well as education on EBP to faculty and staff (Jayakumar et al., 2016).
Nurses and midwives comprise nearly half of the healthcare workforce globally (World Health Organization, 2016), and nursing is the largest segment of the health care workforce in the US (U.S. Department of Labor, 2015). The Magnet® program is one mechanism hospitals used to invest in their nursing personnel. Emanating from a study investigating the ability of certain hospitals to retain and attract nurses during an acute nursing shortage in the 1980s in the US, the Magnet® program embraces 14 organizational traits that affect nursing care and patient outcomes (Lash & Munroe, 2005). Magnet designated organizations create supportive, multidisciplinary environments where nurses are encouraged to develop professionally and use EBP to provide high-quality care and improve patient outcomes. More recently, the Magnet® designation has also been awarded to hospitals internationally. Currently, hospitals in five other countries besides the US have achieved Magnet® status: Australia, Belgium, Canada, Lebanon, and Saudi Arabia (American Nurses Credentialing Center, 2018).
Despite the growth of Magnet®, a recent survey found a low rate of EBP implementation in several U.S. healthcare settings (Melnyk, Gallagher-Ford, Zellefrow, Tucker, Van Dromme et al., 2018) and that nurses were not yet competent in many EBP skills (Melnyk, Gallagher-Ford, L., Zellefrow, Tucker, Thomas et al., 2018). This is consistent with Asian studies of nurses which suggested limited exposure to and knowledge of EBP (Wilson et al., 2016). A limited number of strategies for increasing the use of EBP by hospital-based nurses have been described in the literature to date. U.S.-based strategies include: Academic-service partnerships in which nurse scientists from schools of nursing are embedded in academic hospital settings and participate in population-specific EBP committees (e.g., perioperative; Duffy, Stroups, Culp, Lucke-Wold, & Sand-Jecklin, 2016) or work individually with direct care nurses or teams of nurses leading either EBP or research projects (Hinic, Kowalski, & Silverstein, 2017); EBP “nurse consultants” employed in community hospitals to advise and guide bedside nurses (Brockopp, Corley, Moe, & Schreiber, 2013); and clinical inquiry specialists, doctoral-level nurse scholars who work with nurses in outpatient oncology centers (Boucher, Underhill, Roper, & Berry, 2013). Internationally, 10–14 week academic EBP courses have been held in acute care settings (Wu, Brettle, Zhou, Ou, Wang, & Wang, 2018.
In this article, we demonstrate how a health system-based EPC supports nursing to promote professional development, provide high quality, cost-effective care, and develop policies and practices to improve patient outcomes, as well as positive work life for staff.
Methods
Setting
The UPHS is an integrated health care delivery network serving the greater Philadelphia area. In FY 2016, UPHS included four acute care hospitals with a total of 1,916 beds, as well as facilities specializing in acute rehabilitation, skilled nursing, long-term acute care, and hospice. In addition, the network offers homecare services and outpatient primary and specialty care. Combined, these sites reported 85,488 adult inpatient admissions, 187,391 emergency department visits, and 2.56 million outpatient visits in FY16. Each of our system’s acute care hospitals is Magnet® designated, and the system is regularly recognized among the top-ranking academic healthcare systems in the United States.
In FY 2016, the health system EPC was codirected by two physicians with clinical and administrative responsibilities, and staffed by three full-time research analysts with diverse professional backgrounds. The EPC also includes an administrative coordinator, biostatistics and health economics consultants, library liaisons, and medical and nursing liaisons who bring relevant referrals to the EPC and disseminate completed EPC reports back to their respective facilities. One research analyst and one librarian are RNs with extensive clinical backgrounds. Total staff for the EPC equals 5.5 full time equivalents; all are supported by the health system Chief Medical Officer’s budget.
The process for requesting reports from the EPC is informal. Health system stakeholders, including physicians, nurses, other clinical leaders, and health system administrators, may reach out to either of the physician leaders or any of the analysts or liaisons via email or through in-person conversation. All EPC requests are discussed at the weekly departmental meeting. Topics aligning with health system priorities, as well as processes that impact multiple units or entities, are typically prioritized in the EPC work queue by the Director. Topics that do not align with health system priorities or are too narrow are typically not accepted as an EPC project, though we offer referrals to sources of information (e.g., biomedical librarian, medical society or organizational publications). When research analysts complete a report, the Director assigns them another. The analyst then develops a research protocol or plan in collaboration with the report requestor. Stakeholders are informed that the average request takes 8–12 weeks to fulfill. At times, decisions need to be made sooner and so project priorities and analyst responsibilities are reassigned.
Study Design
The first part of our study involved descriptive analysis of data from an internally-maintained database of systematic reviews performed by our center, housed on a password-protected, limited-access health system shared drive. The second part of our study involved the administration of a 40-item web-based survey to nurse stakeholders who received an EPC report during the most recent 2 fiscal years, in order to determine the ways in which reports influenced nurse decision making, the level of satisfaction, and obtain suggestions on how to improve reports to meet nursing needs. This project was reviewed and determined to qualify as Quality Improvement by the University of Pennsylvania’s Institutional Review Board (Protocol #825748, August 19, 2016).
Database Analysis
Variables of the rapid reviews we examined included: report characteristics (e.g., technology reviewed, clinical specialty examined, completion time, and performance of meta-analyses and GRADE [Grading of Recommendations Assessment, Development and Evaluation] analyses; Guyatt et al., 2008); report use (e.g., integration of report into clinical decision support [CDS] interventions); and dissemination beyond UPHS (e.g., submission to Center for Reviews and Dissemination [CRD] Health Technology Assessment [HTA] database; [Booth, Wright, & Outhwaite, 2010] and to peer-reviewed journals). Report completion time was measured from the time the project was opened by the Research Analyst to the time the final draft report was sent to the requestor. The technology categorization scheme was adapted from that provided by Goodman and the UK National Institute for Health Research HTA Programme and has been previously described (Jayakumar et al., 2016). We systematically assigned the technology reviewed in each report to one of eight mutually exclusive categories. The clinical specialty examined in each report was determined using a previously reported algorithm (Jayakumar et al., 2016). Database results were analyzed in Microsoft Excel (Microsoft Corp., Redmond, WA).
Survey Sample and Administration
Eligible survey participants were the 23 Registered Nurses (RNs) who received an EPC report between July 1, 2014 and June 30, 2016 (i.e., FY 15 and FY16). Participation was voluntary; no incentives were offered.
A 40-item electronic survey was distributed by email in Fall 2016 to the eligible RNs (Supplementary information). Questions included in the survey were adapted from similar surveys reported previously (Jayakumar et al, 2016; Peterson, Floyd, Ferguson, Christensen, & Helfand, 2016). Five-point Likert scales were employed to assess report usability and impact, and requestor satisfaction (scale of 1–5, with greater numbers reflecting greater agreement). The survey was administered using REDCap electronic data capture tools (Harris et al., 2009). One week prior to dissemination of the survey, email notification about the planned survey and a copy of the most recently requested report was sent to each nurse requestor by the first author (JGL). All subsequent communication with study participants was performed by the survey administrator (KJ), who is neither employed by the hospital EPC nor involved in any aspect of the production of EPC reports. Individual responses were kept confidential and participant identities were known only to the survey administrator. Approximately one week after nursing stakeholders were notified about the survey, an invitation to participate and a secure link were sent via individual email to each nurse requestor. A second invitation was extended to those participants who did not respond within one week. A final invitation was extended to those participants who did not respond within four weeks of the initial invite. To minimize the potential for bias, we surveyed those nurses who requested multiple reports on only the most recent report requested. Survey results were imported into Microsoft Excel (Microsoft Corp, Redmond, WA) for descriptive analysis.
Results
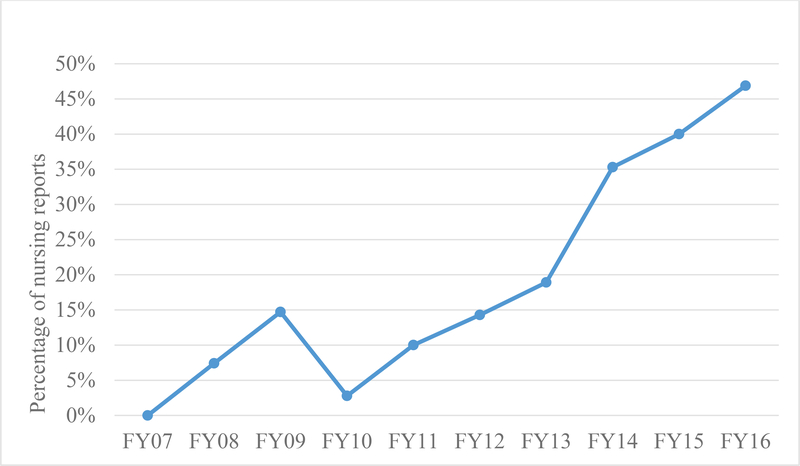
Three hundred and eight rapid reviews were completed for our health system in the first 10 years of the hospital EPC (FY2007–2016). Of these, 19% (59/308) addressed nursing topics. The number of EPC reports requested by nurses or related directly to nursing practice increased over time, from 2/39 (5%) in the center’s first 2 fiscal years (FY 2007–2008) to 25/57 (44%) in the 2 most recent fiscal years (FY 2015–2016; see Figure 1). Overall, 51 individual nurses served as co-authors on 57 different reports. The majority of nursing reports (n = 39) addressed process of care issues (e.g., strategies to reduce violence in the emergency department); other reports examined device effectiveness (n = 10; e.g., disinfecting caps for central lines), policy issues (n = 6; e.g., critical incident debriefing programs to reduce nurse stress), diagnostic tests (n = 3; e.g., postpartum mood disorder screening), and pharmaceuticals (n = 1; locking solutions for central venous catheters). Table 1 provides an overview of HTA categories, with examples of nursing report titles by category. Original meta-analyses of study data were conducted in three nursing reports; GRADE analyses were employed in 16 reports (27%); and 14 reports (24%) informed or were integrated into the health system’s computerized clinical decision support tools. Nursing reports were completed in a mean of 53 days (median 58, range, 15 – 140). Forty-four reports (75%) were submitted to—and are posted on—the international Health Technology Assessment (HTA) database.
Figure 1.
Nursing reports, by fiscal year.
Table 1.
Nursing Reports, by Type of Technology Reviewed
| Category/type of technology | Definition*:A report primarily examining… | N nursing reports (59) | % nursing reports | Examples of report titles |
|---|---|---|---|---|
| Process of care | …a clinical pathway or a clinical practice guideline… [involving] elements of prevention, diagnosis, and/or treatment or significantly incorporates two or more (of the other) technology categories. | 39 | 66% |
Patient-related outcomes: • Nursing double checks of high-alert intravenous medications to prevent errors in the acute care setting • Nurse directed dietary advancement for patients in the acute care setting • Interventions to reduce social isolation among oncology patients with extended hospital stays • Patient transfer from the postanesthesia care unit to an inpatient medical surgical unit • Routine replacement of peripheral intravenous catheters; an update • aPTT collection practices for patients receiving intravenous heparin infusion Nurse/staff-related outcomes: • Interventions to reduce stress among nurses caring for patients with sickle cell disease • Post-event debriefing for nurses and other hospital staff |
| Device, equipment, supplies | … the efficacy/effectiveness, safety, appropriate use, or cost of an instrument, apparatus, implement, machine … which is intended for use in the prevention, diagnosis, or treatment of disease and does not achieve its primary intended purposes through chemical action or metabolism. | 10 | 17% | • Disinfecting caps and antimicrobial locks for reducing blood stream infections associated with central venous catheters • Use of bispectral index monitoring for patients receiving therapeutic hypothermia |
| Policy or organizational/ managerial system | … the laws or regulations; the organization, financing, or delivery of care, including settings of care; or health care providers. | 6 | 10% | • Shared governance for nursing assistants and other ancillary medical staff in the hospital setting • Career advancement for advance practice providers • Geriatric consultation teams/assessments in acute care hospitals: effect on patient outcomes |
| Test, scale, or risk factor | … the efficacy/effectiveness, safety, appropriate use, or cost of a test intended to screen for, diagnose, classify, or monitor the progression of a disease. | 3 | 5% | • Postpartum mood disorder screening |
| Drug | … the efficacy/effectiveness, safety, appropriate use, or cost of a pharmacologic agent. | 1 | 2% | • Locking solutions for central venous catheters |
Definitions adapted from Jayakumar (2016).
Across the last 2 fiscal years, 19 nurses initiated a single request for an EBP report; four additional nurses requested more than one report. Thus, our survey sample consisted of 23 nurses. The overall response rate was 91% (21/23).
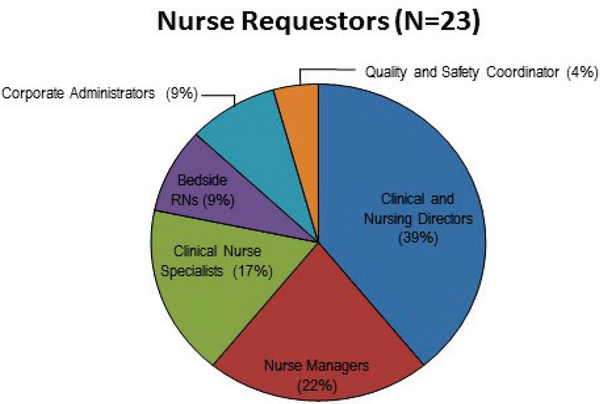
Nurses whose primary responsibilities were administrative or managerial (i.e., corporate administrators, clinical and nursing directors, nurse managers) requested 70% of the reports. Clinical nurse specialists, bedside nurses, and nurses with a primary role in quality and safety (i.e., quality improvement advisors) also requested reports (Figure 2). Clinical and Nursing Directors with overarching responsibilities for Advance Practice, nursing education, research, patient safety and quality, women’s health, and perioperative services, represented the majority of nurse requestors (39%). Nurse Managers with responsibility for specific clinical areas (e.g., medical-surgical units, cardiovascular care, oncology, labor and delivery, and psychiatry) comprised the second largest group of nurse requestors (22%).
Figure 2.
Roles or job titles of nurses requesting rapid reviews.
Most nurses were referred to the EPC by colleagues (11/21; 52%), although over a third had an existing relationship or had personally met EPC faculty and staff (38%); the remainder learned about the EPC from a presentation on the Center’s activities. An overwhelming majority of respondents (90%) indicated that the EPC’s ability to identify and synthesize evidence was the reason for requesting a report. Other factors that influenced nurses to request a report from the EPC include personal time constraints (40%), colleague recommendation (35%), EPC’s objectivity (35%), and the inability to identify meaningful evidence on his or her own (5%). Of note, 81% of nurse requestors reported conducting literature searches prior to contacting the EPC. If the EPC were unable to undertake the project, 81% of nurses indicated they would be unlikely or extremely unlikely to take action without a literature review; 71% would be likely or extremely likely to conduct a review themselves; 52% of nurses would be extremely likely to ask an individual nursing expert (e.g., CNS, CNE, Committee Chair) to conduct a review; and 43% would be likely or extremely likely to ask a committee or task force to conduct a review.
Nurses reported they used the reviews to support clinical program development (48%); provide clinical guidance (33%); update nursing policies and procedures (24%); develop training and curricula (24%); inform resource allocation decisions (19%); and inform research proposals (10%). EPC reports confirmed the perspective of 81% of requestors, changed the perspective of 15%, and had no effect on the remaining 5%. Ninety-one percent of nurse requestors strongly agreed or agreed with the findings of the EPC report.
Reviews were used to inform decision-making soon after completion, with 57% of respondents reporting that they used the information within a month of receiving it and 29% reporting use within 3 months of receipt. Only a single report was not used at all; this was due to an organizational restructure that occurred after the report was completed which rendered the report’s findings immaterial. Overall, nurse requestors were highly satisfied with EPC reports (mean: 4.7 on a 5-point Likert scale). All respondents (100%) strongly agreed or agreed that EPC reports concisely presented information and were easy to understand, 95% strongly agreed or agreed that EPC reports answered the questions posed and were easy to request; mean scores ranged from 4.7 – 4.8. Almost all of the nurses (95%) indicated they were likely to request a future review and all (100%) would recommend the EPC to health system colleagues.
Discussion
Our findings suggest that, within the context of a health care organization that formally promotes EBP, nurses at all organizational levels (from senior administrators to frontline clinicians) are increasingly using the services of a health system EPC to inform nursing policy and practice decisions. Performing high quality EBP reviews is time intensive, which can often limit nurses’ efficient use of the best evidence. Reviews completed by a hospital EPC can overcome this barrier and help expedite policy changes and practice decisions by nursing. Overall, nurses who requested a review were highly satisfied with both the hospital EPC and the rapid reviews it produces, and actively used this information to initiate organizational changes that affect patient and family outcomes as well as support the healthcare system and improve work life balance, all essential parts of the Quadruple Aim.
Likely drivers of the increase in nursing requests we identified included a combination of internal and external factors. Internally, our EPC has more fully integrated nursing into the Center activities. In July 2011, we hired a Research Analyst with extensive experience as a clinical nurse as well as systematic review experience. Analysts not only have a role in performing rapid reviews, but also perform teaching and outreach functions. This is particularly so for the analyst with a background as a practicing nurse. This analyst provides an evidence-based practice didactic during the health system nursing orientation, more extensive instruction in EBP in the nursing residency program and critical care advanced practice provider fellowship, and leads an advance practice provider quarterly continuing education seminar in EBP. Moreover, in October 2011, we invited our first nurse liaison to attend our weekly Center meetings. In 2013, additional nurse liaisons were added from other entities across our health system. Also in 2013, the first cohort of nurse leaders (n = 7) were given support to receive external training in EBP (Wyer, Umscheid, Wright, Silva, & Lang, 2015). Reflecting continuing organizational support for nurse participation in EBP, an additional 29 nurses from our health system (primarily clinical nurse specialists) have attended the external EBP training in the 4 fiscal years that have followed. As a direct outcome of this training, two nurses spearheaded the creation of a system-wide EBP Nursing Leadership Council (EBP-NLC) in 2015. The goal of this council is to align clinical practice across the health system to promote seamless continuity of patient care, and create a unified foundation for quality, safety, and value. Council members identify and disseminate EBP recommendations, provide EBP continuing education, and promote the development of standardized structures for documenting evidence in practice (e.g., through policies, procedures, guidelines, protocols, and pathways).
Externally, the journey for all of the hospitals in our health system to attain Magnet® status has supported nurse engagement with our EPC, and has provided incentives to nursing leadership to support further EBP training. The reviews by the EPC have facilitated nurse led practice change projects supporting Magnet® redesignation. The Magnet® journey for our health system is supported by the mission of the EPC.
The advantages of our hospital EPC approach compared to previous strategies for increasing the use of EBP by nurses include recognition at the health system level of the importance of the use of EBP across disciplines to improve outcomes; so much so, that the Chief Medical Officer’s budget provides financial support for the EPC. In addition, the interprofessional team in the center goes beyond what an academic-service partnership (Duffy et al., 2016) can accomplish in population specific EBP committees. The EPC also can support more nurses in implementing EBP in their clinical setting than the work of one nurse scientist employed by a health system (Duffy et al., 2016). Nurse consultants (Brockopp et al., 2013) can guide and advise bedside nurses in evidence-based practice, but do not have the benefit of the EPC team to perform time sensitive rapid reviews on pressing clinical issues; clinical inquiry specialists (Boucher et al., 2013) also do not have the time to perform reviews that a team of reviewers can provide.
Our study has a number of limitations. First, the study involves a single healthcare system setting and the survey includes a relatively small sample size, which may impact the generalizability of our findings to other settings and to nurses more generally. In addition, seven of the 21 (33%) nurses who requested evidence reviews and participated in our survey also received training at TEACH, or are EBP-NLC members. Despite this, our survey participants reflect a broad array of nursing roles, departments, and clinical settings across our health system, which may improve the generalizability of our findings to other settings. A second limitation is that not all of the eligible nurse requestors responded to our survey. But our response rate of 91% compares well to other surveys published in medical journals (Asch, Jedrziewski, & Christakis, 1997). Third, our survey of impact is self-reported rather than an evaluation of actual decision making or patient outcomes. Thus, the survey relies on the accuracy of the responses. Fourth, recall bias must be considered, as some respondents were asked to evaluate reports that were greater than 1 year old. To reduce this bias, we asked respondents to consider the most recent report they requested, emailed that report to them just prior to the survey, and only surveyed those who requested reports in the most recent 2 fiscal years. Fifth, social desirability bias could have affected the survey responses in terms of how the request for participation was framed, though this bias was likely minimized by the promise of confidentiality, and the use of an individual not affiliated with the EPC to administer the survey.
Given the positive impact of the EPC on nursing practice and policy within our health system, our goals for the immediate future include further investments in the development and implementation of electronic health record nurse-driven EBP care pathways, and evidence-based interventions tailored to meet local patient and workforce needs.
Conclusions
In conclusion, a dedicated, interprofessional hospital EPC can empower nurses and support both the Quadruple Aim and Magnet® designation efforts across a health system. The synergy the EPC creates within the health system breaks down the barriers to nurses engaging in evidence-based practice by creating a process for nurses at all levels to request rapid evidence reviews that can inform and influence the local delivery of high quality, safe and high value care.
Supplementary Material
Linking Evidence to Action.
A dedicated hospital evidence practice center (EPC) can promote a culture of EBP and foster nursing professional development and interprofessional collaboration.
Evidence reviews conducted by a hospital EPC unit can be used by nurses at all organizational levels.
EPC reviews can be used to update nursing policies and procedures, and inform clinical program development, resource allocation decisions, and future research proposals.
Nurses who use the services of a hospital EPC are highly satisfied with the process, supporting the Quadruple Aim and Magnet® designation.
Acknowledgments
We thank Fran Barg, PhD (Department of Family Medicine and Community Health, University of Pennsylvania Perelman School of Medicine) and Joel Betesh, MD (University of Pennsylvania Health System) for their contributions to developing the survey. They did not receive any compensation for their contributions.
Dr. Umscheid’s contribution was supported in part by the National Center for Research Resources, Grant UL1RR024134, which is now at the National Center for Advancing Translational Sciences, Grant UL1TR000003. The content of this paper is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
None of the funders had a role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Contributor Information
Julia G. Lavenberg, Research Analyst, Penn Medicine Center for Evidence-based Practice, Philadelphia, PA, USA.
Pamela Z. Cacchione, Nurse Scientist, Penn Presbyterian Medical Center, Associate Professor of Geropsychiatric Nursing, University of Pennsylvania, School of Nursing, Philadelphia, PA, USA.
Kishore L. Jayakumar, Transitional Year Resident, Department of Medicine, Crozer Chester Medical Center, Upland, PA, USA.
Brian F. Leas, Senior Research Analyst, Penn Medicine Center for Evidence-based Practice, Philadelphia, PA, USA.
Matthew D. Mitchell, Senior Research Analyst, Penn Medicine Center for Evidence-based Practice, Philadelphia, PA, USA.
Nikhil K. Mull, Co-Director, Penn Medicine Center for Evidence-based Practice and Assistant Professor of Clinical Medicine, Perelman School of Medicine, University of Pennsylvania, Philadelphia, PA, USA.
Craig A. Umscheid, Director, Penn Medicine Center for Evidence-based Practice, and Vice Chair, Quality and Safety, Department of Medicine, and Associate Professor of Medicine and Epidemiology, Perelman School of Medicine, University of Pennsylvania, Philadelphia, PA, USA.
References
- American Nurses Credentialing Center. (2017). ANCC Magnet Recognition Program®. Retrieved from https://www.nursingworld.org/organizational-programs/magnet/
- Asch DA, Jedrziewski MK, & Christakis NA (1997). Response rates to mail surveys published in medical journals. Journal of Clinical Epidemiology, 50(10),1129–1136. [DOI] [PubMed] [Google Scholar]
- Berwick DM, Nolan TW, & Whittington J (2008). The triple aim: Care, health and cost. Health Affairs, 27(3), 759–769. [DOI] [PubMed] [Google Scholar]
- Bodenheimer T, & Sinsky C (2014). From triple to quadruple aim: Care of the patient requires care of the provider. Annals of Family Medicine, 12(6), 573–576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Booth AM, Wright KE, & Outhwaite H (2010). Centre for Reviews and Dissemination databases: Value, content, and developments. International Journal of Technology Assessment in Health Care, 26(4), 470–472. [DOI] [PubMed] [Google Scholar]
- Boucher J, Underhill M, Roper K, & Berry D (2013). Science and practice aligned within nursing: Structure and process for evidence-based practice. Journal of Nursing Administration, 43(4), 229–234. [DOI] [PubMed] [Google Scholar]
- Brockopp DY, Corley D, Moe K, & Schreiber J (2013). The Baptist Health Lexington evidence-based practice model: A 5-year journey. Journal of Nursing Administration, 43(4), 187–93. [DOI] [PubMed] [Google Scholar]
- Duffy JR, Stroups L, Culp S, Lucke-Wold N, & Sand-Jecklin K (2016). Nurses’ research capacity, use of evidence, and research productivity in acute care: Year 1 findings from a partnership study. Journal of Nursing Administration, 46(1), 12–17. [DOI] [PubMed] [Google Scholar]
- Gagnon M-P (2014). Hospital-based health technology assessment: Developments to date. PharmacoEconomics, 32, 819–824. [DOI] [PubMed] [Google Scholar]
- Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, & Schünemann HJ (2008). GRADE: An emerging consensus on rating quality of evidence and strength of recommendations. British Medical Journal, 336(7650), 924–926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, & Conde JG (2009). Research electronic data capture (REDcap)—a metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics, 42(2), 377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hinic K, Kowalski MO, & Silverstein W (2017). Professor in residence: An innovative academic-practice partnership. Journal of Continuing Education in Nursing, 48(12), 552–556. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. (2009). Charter and vision statement In Institute of Medicine’s (U.S.) Roundtable on evidence-based medicine workshop summary, Leadership commitments to improve high value in healthcare: Finding common ground (pp. ix–x). Washington, DC: National Academies Press. [PubMed] [Google Scholar]
- Jayakumar KL, Lavenberg JA, Mitchell MD, Doshi JA, Leas B, Goldmann DR, … Umscheid CA (2016). Evidence synthesis activities of a hospital evidence-based practice center and impact on hospital decision making. Journal of Hospital Medicine, 11(3), 185–192. [DOI] [PubMed] [Google Scholar]
- Lash AA & Munroe DJ (2005). Magnet designation: A communiqué to the profession and the public about nursing excellence. MEDSURG Nursing, (Suppl), 7–12; quiz 13. [PubMed] [Google Scholar]
- Liddy C, & Keely E (2018). Using the Quadruple Aim framework to measure impact of health technology implementation: A case study of eConsult. Journal of the American Board of Family Medicine, 31, 445–455. [DOI] [PubMed] [Google Scholar]
- Melnyk BM, Gallagher-Ford L, Zellefrow C, Tucker S, Van Dromme L, & Thomas BK (2018a). Outcomes from the first Helene Fuld Health Trust National Institute for Evidence-Based Practice in Nursing and healthcare invitational expert forum. Worldviews on Evidence-Based Nursing, 15, 5–15. [DOI] [PubMed] [Google Scholar]
- Melnyk BM, Gallagher-Ford L, Zellefrow C, Tucker S, Thomas B, Sinnott LT, & Tan A (2018). The first U.S. study on nurses’ evidence-based practice competencies indicates major deficits that threaten healthcare quality, safety, and patient outcomes. Worldviews on Evidence-Based Nursing, 15, 16–25. [DOI] [PubMed] [Google Scholar]
- Peterson K, Floyd N, Ferguson L, Christensen V, & Helfand M (2016). User survey finds rapid evidence reviews increased uptake of evidence by Veterans Health Administration leadership to inform fast-paced health-system decision-making. Systematic Reviews, 5(1), 132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Productivity Commission. (2017). Impacts of health recommendations, Shifting the dial: 5 year productivity review. Supporting paper No. 6. Canberra, Australia: Commonwealth of Australia. [Google Scholar]
- Ruddy MP, Thomas-Hemak L, & Meede L (2016). Practice transformation: Professional development is personal. Academic Medicine, 5, 624–627. [DOI] [PubMed] [Google Scholar]
- Sikka R, Morath JM, & Leape L (2015). The quadruple aim: Care, health cost and meaning in work. BMJ Quality & Safety, 25, 608–610. [DOI] [PubMed] [Google Scholar]
- Umscheid CA, Williams K, & Brennan PJ (2010). Hospital-based comparative effectiveness centers: Translating research into practice to improve the quality, safety and value of patient care. Journal of General Internal Medicine, 25(12), 1352–1355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U. S. Department of Labor, Bureau of Labor Statistics. (2015, July 13). Registered nurses have highest employment in healthcare occupations; anesthesiologists earn the most. TED: The Economics Daily. Retrieved from https://www.bls.gov/opub/ted/2015/registered-nurses-have-highest-employment-in-healthcare-occupations-anesthesiologists-earn-the-most.htm
- Wilson L, Acharya R, Karki S, Budhwani H, Shrestha P, Chalise P, … Gautam K (2016). Evidence-based practice models to maximize nursing’s contributions to global health. Asian Journal of Nursing Education and Research, 6(1), 1–7. [Google Scholar]
- World Health Organization. (2016). Global strategic directions for Strengthening nursing and midwifery 2016–2020. Retrieved 2018 from http://www.who.int/hrh/nursing_midwifery/global-strategic-midwifery2016-2020.pdf [PubMed]
- Wyer PC, Umscheid CA, Wright S, Silva SA, & Lang E (2015). Teaching Evidence Assimilation for Collaborative Health Care (TEACH) 2009–2014: Building evidence-based capacity within health care provider organizations. eGEMS (Generating Evidence & Methods to improve patient outcomes), 3(2), 1165. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.