Abstract
Purpose:
To determine whether there were temporal differences in the rates of first stroke hospitalizations and 30-day mortality after stroke between black and white Medicare enrollees.
Methods:
We used a 20% sample of Medicare beneficiaries aged ≥65 years and described the annual rate of first hospitalization for ischemic and hemorrhagic strokes from years 1988 to 2013, as well as 30-day mortality after stroke hospitalization. We used linear tests of trend to determine whether stroke rates changed over time, and tested the interaction term between race and year to determine whether trends differed by race.
Results:
We identified 1,009,057 incident hospitalizations for ischemic strokes and 147,817 for hemorrhagic strokes. Annual stroke hospitalizations decreased significantly over time for both blacks and whites, and in both stroke subtypes (p values for trend all <0.001). Reductions in stroke rates were comparable between blacks and whites: among men, the OR for the interaction term for race by year was 1.008 [1.004–1.012] for ischemic and 1.002 (95% CI 0.999–1.004) for hemorrhagic; for women, it was 1.000 [0.997–1.004] for ischemic and 1.003 (95% CI 1.001–1.006) for hemorrhagic. Both black men and women experienced greater improvements over time in terms of 30-day mortality after strokes.
Conclusions:
Rates of incident hospitalizations for ischemic and hemorrhagic strokes fell significantly over a 25 year period for both black and white Medicare enrollees. Black men and women experienced greater improvements in 30-day mortality after both ischemic and hemorrhagic stroke.
Background
Stroke remains a leading cause of death in the United States, but its incidence and mortality have declined considerably over the past few decades(1–4). These improvements in outcomes coincide with an era of quality improvement initiatives, the development of stroke centers of excellence, the decline in tobacco smoking, and the increased use of risk-modifying medications(1, 4–6).
Progress, however, may not be equally distributed amongst individuals of different racial categories. Stroke risk in black Americans, for example, have consistently exceeded the risk observed in white Americans(4, 7). A wider prevalence of contributing clinical factors, such as hypertension, smoking, and diabetes, in addition to disparities in clinical management and socioeconomic factors, may contribute to this increased observed risk(8–11). Whether the disparities in stroke risk have changed over time is still in question, with studies finding conflicting results. Some data show that declines in stroke incidence have been similar between blacks and whites(4). Others have found that the improvements in stroke risk amongst blacks lags behind whites(7, 12). Whether there are differences in stroke-related mortality, too, is unclear(8, 13, 14).
Our study’s objective was to describe temporal trends over a 25-year period in the US with regard to stroke hospitalization and short-term mortality after stroke hospitalization, comparing trends between black and white Medicare enrollees. We separately report data on the two major stroke subtypes, ischemic and hemorrhagic strokes.
Methods
Because there was no single nationally-representative database that contained comprehensive information on stroke events, clinical risk factors for stroke, and medication prevalence over time, our approach was to obtain relevant data from three separate databases that collected nationally-representative data from Medicare enrollees during the time period of interest. Specifically, we obtained data on stroke hospitalizations and 30-day mortality after hospitalizations from the Medicare Provider Analysis and Review (MedPAR) database, a 20% sample of fee-for service Medicare beneficiaries aged 65 years or older(15). Demographic information in the Medicare claims files come from the Medicare Enrollment Database maintained at the Center for Medicare and Medicaid Services Data Center. The variable “race” comes from the Master Beneficiary Record of the Social Security Administration, which beneficiaries complete at the time of registration using pre-defined options. To identify the population prevalence of risk factors for stroke in the US black and white Medicare enrollees, we used data from the nationally-representative Third National Health and Nutrition Examination Survey (NHANES) surveys, restricted to people aged 65 years or older and with Medicare coverage. Finally, to assess the prevalence of prescribed medications used to modify stroke risk, we used data from the Medicare Current Beneficiary Survey (MCBS), a nationally-representative survey of patients enrolled in Medicare
Identification of stroke events
Stroke hospitalizations occurring between 1988 and 2013 were identified by searching the MedPAR database for hospitalizations with a primary International Classification of Diseases 9th Revision, Clinical Modification (ICD-9) discharge diagnosis code for stroke, and stratified as ischemic (ICD-9 codes 434.x and 436.x) or hemorrhagic (ICD-9 codes 430.x and 431.x). We excluded subjects living outside of the United States (n=13,392) or who were enrolled in a Medicare health maintenance organization (n=168,132), for which Medicare utilization data may be incomplete. Information on subject demographics (age, sex, race), region of residence (Midwest, Northeast, South, or West), and vital status were obtained from Medicare denominator files. Only subjects whose race was categorized as “white” or “black” were included in this study, as coding for other race categories was less reliable in these records(16). We also searched for specific ICD-9 discharge diagnosis codes documented during the hospitalization for medical conditions related to stroke outcomes and mortality, including the variables used to calculate a Charlson comorbidity risk score.
Determining the population prevalence of stroke risk factors
Population-level prevalence of risk factors for stroke in the 65 years or older Medicare population were obtained by analyzing data from the NHANES surveys from 1988 to 1994 as well as from the continuous NHANES survey from years 2001–2008 and 2011–2014. NHANES questionnaires were completed by non-institutionalized individuals from the civilian population and contain detailed information obtained through direct patient interview as well as physiologic assessments(17). In addition to reporting the prevalence of individual risk factors, we also calculated the estimated stroke risk for the population during that time period, using the Framingham stroke risk score. The Framingham stroke risk score estimates 10-year stroke risk(18) in men and women based on age, systolic blood pressure, antihypertensive treatment, diabetes mellitus, smoking status, cardiovascular disease, left ventricular hypertrophy(LVH), and atrial fibrillation. The Framingham stroke risk score was developed to predict all strokes (e.g., a combination of ischemic and hemorrhagic stroke subtypes). With the exception of LVH and atrial fibrillation, all variables used to calculate the Framingham risk score were available in NHANES. The prevalence of LVH was obtained from electrocardiograms obtained on NHANES participants from years 1988–1994 and for later years, extrapolated from the scientific literature(19, 20). Atrial fibrillation prevalence for each time period was calculated by using the published population prevalence in the Medicare population from years 1992–2002 and then imputing the estimated prevalence of atrial fibrillation for years outside of this time window assuming a linear trend(1, 12, 21). Although ischemic and hemorrhagic strokes have several overlapping risk factors, including advancing age, hypertension, and smoking, there are additional risk factors distinct to hemorrhagic stroke, such as traumatic injury, anticoagulant exposure, and brain aneurysms, data which were lacking in our study.
Determining the population prevalence of medication use
Several medications, namely, statins, antihypertensive drugs, and antiplatelet agents are known to play a role in modifying stroke risk. To obtain information on the prevalence of medication use among Medicare enrollees, we used the MCBS from years 1992 to 2012. The MCBS is a nationally-representative survey of patients enrolled in Medicare that contains self-reported information on prescription medications, pharmacy receipts, and medication containers provided to the interviewers, supplemented by Medicare Part D prescription data from years 2006–2012(22). We calculated the percent Medicare enrollees ≥65 years each year who reported taking antihypertensive medications (angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, beta-blockers, calcium channel blockers, diuretics, and other antihypertensive agents), statins, and non-aspirin antiplatelet medications (clopidogrel, ticlopidine). Because aspirin was available without prescription, its use was not fully captured by the MCBS and not included in this study.
Statistical Analysis
The primary outcomes of the study were first hospitalization for stroke after age 65 and 30-day mortality after stroke hospitalization. The primary predictor was race (black versus white). Only the first hospitalization for stroke per subject was considered in the analysis in order to focus on incident stroke. Annual hospitalization rates for first stroke, stratified by gender, were calculated as the number of strokes per 100,000 Medicare beneficiaries per year, with crude rates standardized to the age and sex distribution of the year 2000 population. The age-adjusted risk of stroke between blacks and whites was compared first using simple logistic regression. Next, a linear regression model was developed to determine whether the annual rate of first stroke hospitalization changed significantly over time, incorporating year as a quadratic function. Finally, to test whether the temporal change in stroke hospitalization rate differed by race, we tested the interaction term between race and year. This approach was next applied to the analysis of 30-day mortality after stroke hospitalization, using multivariable logistic regression to adjust for co-existing factors that may be associated with 30-day mortality. Variables included in the models of mortality were those plausibly related to stroke-mortality: age, region, comorbid conditions related to stroke (myocardial infarction, congestive heart failure, hypertension, diabetes mellitus, atrial fibrillation, vascular disease, hyperlipidemia), and mean Charlson comorbidity index(23).
To describe the population prevalence of specific risk factors for stroke and preventive medication use, we used the NHANES and MCBS. The prevalence of stroke risk factors, stratified by race, was obtained during four time periods: 1988–1994, 2001–2004, 2005–2008, and 2011–2014. The proportion of Medicare enrollees reporting use of statins, antihypertensive, and antiplatelet medications was calculated for each year between 1992 and 2012. Comparisons of categorical variables were performed using Chi-squared tests and comparisons of means were performed using t-tests.
SAS 9.2 statistical package (SAS Institute Inc, Cary, NC) was used for data analyses. This study was approved by the institutional review board of the University of California, San Francisco and waiver of informed consent was granted due to the nature of the study.
Results
Incidence and outcomes of ischemic stroke
We identified 1,009,057 hospitalizations for first ischemic stroke between 1988–2013, with 116,351 occurring among blacks and 892,706 among whites. The clinical characteristics of hospitalized patients with ischemic stroke are presented in eTables 1 and 2. A greater proportion of ischemic strokes came from the Southern region compared to other regions. Cardiovascular risk factors were common amongst patients with ischemic stroke, including hypertension, heart failure, diabetes mellitus, atrial fibrillation, and hyperlipidemia, particularly in more recent years (eTables 1 and 2).
Overall, black enrollees were at higher risk for ischemic stroke than whites, with an age-adjusted odds ratio (OR) of 1.36 (95% confidence interval [CI], 1.30–1.43) for black men compared to white men, and OR 1.47 (95% CI, 1.41–1.53) for black women compared to white women. The annual rate of first ischemic stroke hospitalizations declined significantly over time for both blacks and whites (p values for trend <0.001, Figure 1a). The reductions in stroke rates were slightly greater for black men: OR for the interaction term of race by year 1.008 [1.004–1.012] for men and 1.000 [0.997–1.004] for women.
Figure 1.
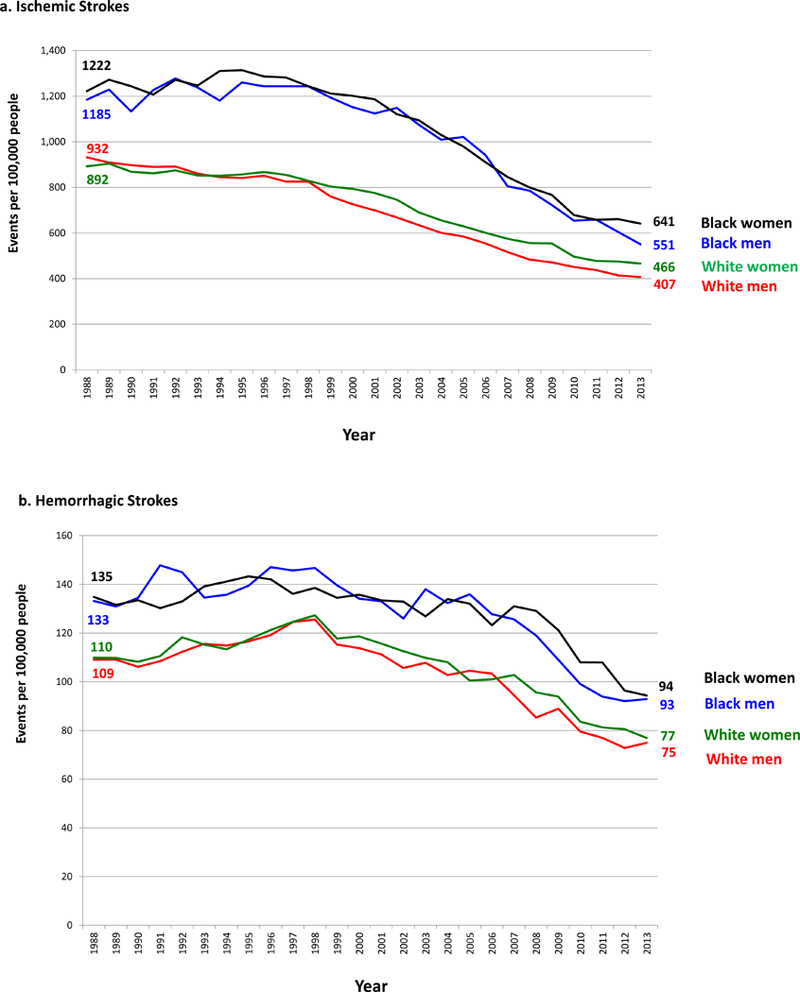
Age-adjusted Rates of First Hospitalization for (a) Ischemic and (b) Hemorrhagic Stroke in the US Medicare Population aged ≥ 65 years, 1988–2013.
Both blacks and whites also experienced improvements in 30-day mortality after hospitalization for ischemic stroke (Figure 2). Both black men and black women experienced slightly greater improvements in 30-day mortality after ischemic stroke: for white men, ischemic stroke mortality fell from 16.4% in 1988 to 11.8% in 2013 and from 16.1% to 8.1% for black men (p values for trend <0.001, OR of the interaction term of black race by year 0.986 [95% CI, 0.982 – 0.990]). For women: ischemic stroke mortality declined from 16.0% to 14.8% in white women and 13.8% to 8.7% in black women (p values for trend <0.001, OR for interaction term 0.981 [95% CI, 0.977 – 0.986]).
Figure 2.
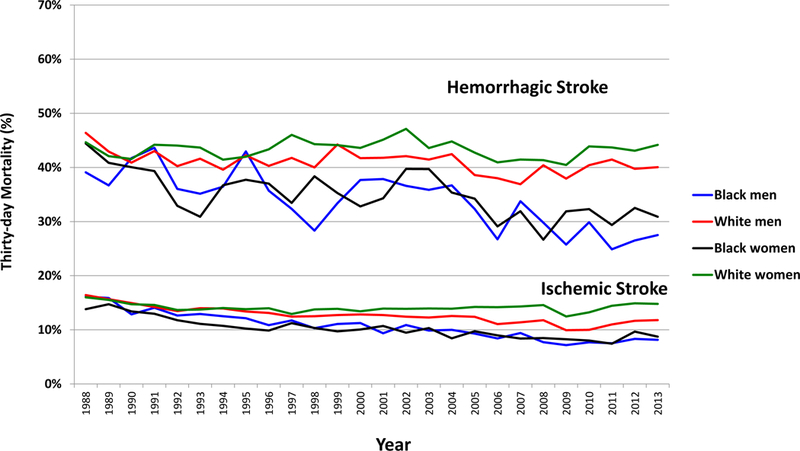
Risk-adjusted 30-day Mortality after Hospitalization for Ischemic and Hemorrhagic Stroke in the US Medicare Population aged ≥ 65 years, 1988–2013.
Incidence and outcomes of hemorrhagic stroke
We identified 147,817 hospitalizations for first hemorrhagic stroke over the time period, 14,237 occurring among blacks and 133,580 among whites. Clinical characteristics of hospitalized patients with hemorrhagic stroke are presented in eTables 3 and 4. Similar to ischemic strokes, a greater proportion of hemorrhagic strokes came from the Southern region of the US and several cardiovascular risk factors, including hypertension, hypertension, diabetes mellitus, and hyperlipidemia were commonly diagnosed (eTables 3 and 4).
Black enrollees were at higher risk for hemorrhagic stroke than whites, with an OR of 1.21 (95% CI, 1.17–1.26) for black men and 1.15 (95% CI, 1.11–1.20) for black women. As with ischemic stroke, the annual rate of first hospitalization for hemorrhagic stroke declined over time for both blacks and whites (p for trends <0.001, Figure 1b). The decline in stroke rate was similar between blacks and whites, with black women experiencing a marginally smaller decline (OR for the interaction between black race and year 1.002 (95% CI 0.999–1.004) for men and 1.003 (95% CI 1.001–1.006) for women).
The 30-day mortality after hospitalization for hemorrhagic stroke was considerably higher than after ischemic stroke. Blacks had lower 30-day stroke mortality than whites (Figure 2). Risk-adjusted hemorrhagic stroke mortality improved over time and more prominently for blacks. Hemorrhagic stroke mortality decreased in black men from 39.1% in 1988 to 27.5% in 2013, and from 46.4% to 40.0% in white men (p value for trends <0.001, OR for interaction term of race by year 0.988 [95% CI, 0.983 – 0.993]). Among women, mortality in black women decreased from 44.4% to 30.9% and from 44.6% to 44.2% for white women (p value for trends <0.001, OR for interaction term of race by year 0.99 [95% CI, 0.985– 0.994]).
Stroke risk factor prevalence and medication use in the general US population
In the general US Medicare population, the prevalence of several risk factors for stroke decreased over time, notably, smoking, mean systolic blood pressure, and mean total cholesterol level (eTables 5 and 6). Other factors, such as diabetes mellitus and obesity, increased in the population over time.
Black men were more likely than white men to be active smokers (p<0.01), although the prevalence of smoking declined over time in both races: 23.2% of black men and 14.3% of white men in 1988–1994 reported smoking, declining to 15.6% of black men and 6.9% of white men by 2011–2014 (eTable 5). Among women, the differences in smoking were not statistically different between blacks and whites (p=0.91, eTable 6).
The mean systolic blood pressure in the population declined over time, for both men and women (eTable 5 and 6). Reductions in blood pressure and cholesterol occurred during a period of time when there occurred dramatic increases in the use of antihypertensive medications and statins in the Medicare population (Figure 3).
Figure 3.
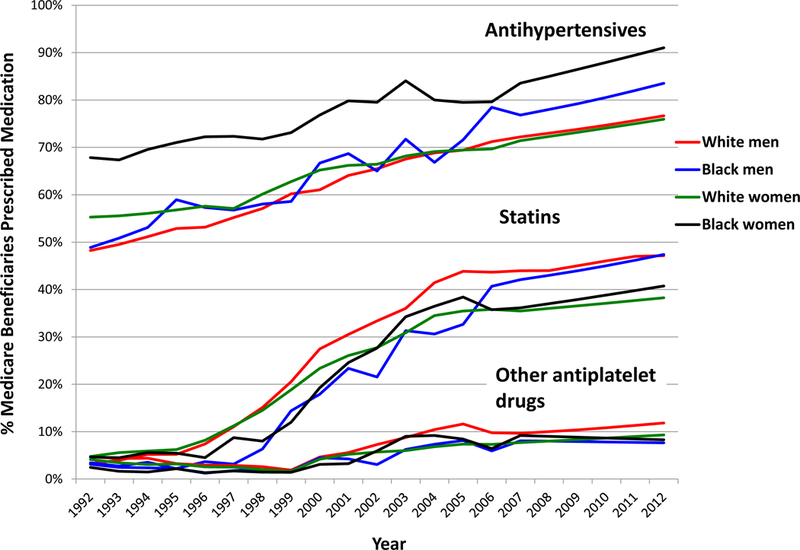
Prevalence of Antihypertensive Medications, Statins, and Non-aspirin Antiplatelet Drugs among Medicare Enrollees aged ≥ 65 years, 1992–2012.
In contrast to blood pressure and cholesterol, the population prevalence of diabetes mellitus and obesity (body mass index ≥ 30 kg/m2) increased over time. Black enrollees were more likely than whites to have diabetes or obesity (p<0.01, both). However among women, the proportion of white women with obesity steadily increased, approaching the prevalence of obesity amongst black women (eTable 6).
Discussion
Our study of evolving US trends in stroke found that both black and white Medicare enrollees experienced considerable improvements over time with regard to stroke hospitalizations. Improvements in 30-day mortality after stroke hospitalizations were also observed. Although black men and women continued to be at higher risk for stroke overall, the improvements in stroke hospitalization rates and mortality were comparable for both blacks and whites. In fact, black men and women experienced slightly greater improvements than whites in terms of 30-day mortality for both stroke subtypes.
The higher risk for stroke amongst black Americans is likely multifactorial. Our study, like others, found that the prevalence of individual risk factors for stroke varied by race and that black enrollees had, overall, a higher calculated population-risk for stroke based on stroke risk factors(24). Diagnosed hypertension at the time of stroke, for example, was significantly more prevalent amongst black men and women compared to whites. There were also several notable improvements in modifiable risk factors that occurred over time. The proportion of people in the general population who reported being a current smoker has fallen for both men and women, blacks and whites. Two additional risk factors that are modifiable – systolic blood pressure and total cholesterol level – have also improved over time. This occurred in conjunction with increased use of antihypertensive medications and statins and it is likely that more widespread use of these medications combined with reductions in smoking use have contributed to these improvements. If so, this represents a significant success in public health and one that has been shared by both races.
Nevertheless there remain areas of concern that may should alert clinicians, policy makers, and researchers on further opportunities to reduce the burden of stroke in the US. Smoking prevalence, for example, although declining continues to be unacceptably high and disproportionately higher amongst black men. Diabetes and overweight/obesity continue to be a worsening epidemic in the US. These conditions, in contrast to high blood pressure and hyperlipidemia, which have more targeted pharmacologic treatments, may require more multifaceted approaches to management including behavioral and lifestyle modifications, in addition to medical therapy.
In addition to differences in the prevalence of comorbid conditions, regional and socioeconomic factors may also contribute to disparities in observed stroke outcomes(11). Other studies have noted that a combination of medical, socioeconomic, and behavioral factors contribute to a disproportionate burden of stroke in the Southern US region, sometimes called the “Stroke Belt”(25).
Our study found that 30-day mortality after stroke hospitalization has improved significantly over time, and was more pronounced among black enrollees than whites. The exact reason for this observation is not clear. Because our study focused on the ≥65 year old population, we were not able to determine whether differing rates of stroke at younger ages might have contributed to this finding. It is possible that blacks were more likely to have severe strokes at younger ages(26), potentially leading to survivor bias in the population we observed. The shared reduction in stroke-related mortality in both racial categories may also represent improvements in acute stroke care nationwide(27, 28).
Our study had several limitations. The data on stroke hospitalizations and mortality, as well as some of the clinical data, were administrative in nature and restricted to the ≥65 year old Medicare population. Hence, we could not be sure that the first stroke hospitalization in the MedPAR database actually represented the first stroke for that individual. Although it is likely that the majority of people with incident strokes present to hospitals, if there were systematic differences by race in terms of the age at presentation or likelihood of being hospitalized, our findings could be biased(13, 29). Finally, because we used data from three separate data sources, we were unable to make direct correlations between the stroke rates observed in one data set and changes in risk factors observed in another. We cannot claim that changes in stroke risk factors and medication use had a causal effect on the reductions in stroke hospitalizations. Regardless, our study illustrates the considerable advances in cardiovascular risk factor modification that have been shared by both blacks and whites.
In conclusion, although black Americans continued to experience higher rates of stroke hospitalizations than whites, there have been considerable improvements in stroke incidence and short-term stroke-related mortality over the past 25 years shared by both black and white Medicare enrollees.
Supplementary Material
Table 1.
Age-adjusted hospitalizations per 100,000 people for ischemic and hemorrhagic stroke, 1988–2013
| Ischemic Strokes per 100,000 | Hemorrhagic Strokes per 100,000 | |||||||
|---|---|---|---|---|---|---|---|---|
| Men | Women | Men | Women | |||||
| Year | Black | White | Black | White | Black | White | Black | White |
| 1988 | 1,185 | 932 | 1,222 | 892 | 133 | 109 | 135 | 110 |
| 1989 | 1,229 | 909 | 1,272 | 904 | 131 | 109 | 132 | 110 |
| 1990 | 1,133 | 898 | 1,244 | 869 | 134 | 106 | 133 | 108 |
| 1991 | 1,227 | 889 | 1,207 | 862 | 148 | 108 | 130 | 111 |
| 1992 | 1,278 | 892 | 1,272 | 875 | 145 | 112 | 133 | 118 |
| 1993 | 1,238 | 860 | 1,247 | 852 | 135 | 116 | 139 | 115 |
| 1994 | 1,181 | 845 | 1,310 | 851 | 136 | 115 | 141 | 113 |
| 1995 | 1,260 | 842 | 1,314 | 857 | 139 | 117 | 143 | 117 |
| 1996 | 1,243 | 851 | 1,287 | 868 | 147 | 119 | 142 | 121 |
| 1997 | 1,243 | 826 | 1,282 | 855 | 146 | 125 | 136 | 125 |
| 1998 | 1,243 | 826 | 1,244 | 829 | 147 | 126 | 139 | 127 |
| 1999 | 1,194 | 760 | 1,212 | 804 | 140 | 115 | 134 | 118 |
| 2000 | 1,152 | 726 | 1,201 | 794 | 134 | 114 | 136 | 119 |
| 2001 | 1,125 | 699 | 1,186 | 775 | 133 | 111 | 133 | 116 |
| 2002 | 1,148 | 668 | 1,121 | 746 | 126 | 106 | 133 | 113 |
| 2003 | 1,074 | 635 | 1,094 | 690 | 138 | 108 | 127 | 110 |
| 2004 | 1,009 | 601 | 1,030 | 656 | 132 | 103 | 134 | 108 |
| 2005 | 1,021 | 585 | 980 | 629 | 136 | 104 | 132 | 101 |
| 2006 | 942 | 555 | 911 | 601 | 128 | 103 | 123 | 101 |
| 2007 | 806 | 517 | 846 | 575 | 126 | 94 | 131 | 103 |
| 2008 | 785 | 483 | 799 | 556 | 119 | 85 | 129 | 96 |
| 2009 | 723 | 471 | 767 | 555 | 109 | 89 | 121 | 94 |
| 2010 | 654 | 451 | 679 | 496 | 99 | 80 | 108 | 84 |
| 2011 | 659 | 437 | 658 | 478 | 94 | 77 | 108 | 81 |
| 2012 | 605 | 414 | 661 | 475 | 92 | 73 | 96 | 81 |
| 2013 | 551 | 407 | 641 | 466 | 93 | 75 | 94 | 77 |
Table 2.
Risk-adjusted 30-day mortality after ischemic and hemorrhagic stroke hospitalizations, 1988–2013
| Ischemic Stroke Mortality | Hemorrhagic Stroke Mortality | |||||||
|---|---|---|---|---|---|---|---|---|
| Men | Women | Men | Women | |||||
| Year | Black | White | Black | White | Black | White | Black | White |
| 1988 | 16% | 16% | 14% | 16% | 39% | 46% | 44% | 45% |
| 1989 | 16% | 16% | 15% | 16% | 37% | 43% | 41% | 42% |
| 1990 | 13% | 15% | 13% | 15% | 42% | 41% | 40% | 42% |
| 1991 | 14% | 14% | 13% | 15% | 44% | 43% | 39% | 44% |
| 1992 | 13% | 13% | 12% | 14% | 36% | 40% | 33% | 44% |
| 1993 | 13% | 14% | 11% | 14% | 35% | 42% | 31% | 44% |
| 1994 | 12% | 14% | 11% | 14% | 36% | 40% | 37% | 41% |
| 1995 | 12% | 13% | 10% | 14% | 43% | 42% | 38% | 42% |
| 1996 | 11% | 13% | 10% | 14% | 36% | 40% | 37% | 43% |
| 1997 | 12% | 12% | 11% | 13% | 32% | 42% | 33% | 46% |
| 1998 | 10% | 13% | 10% | 14% | 28% | 40% | 38% | 44% |
| 1999 | 11% | 13% | 10% | 14% | 33% | 44% | 35% | 44% |
| 2000 | 11% | 13% | 10% | 13% | 38% | 42% | 33% | 44% |
| 2001 | 9% | 13% | 11% | 14% | 38% | 42% | 34% | 45% |
| 2002 | 11% | 12% | 9% | 14% | 37% | 42% | 40% | 47% |
| 2003 | 10% | 12% | 10% | 14% | 36% | 41% | 40% | 44% |
| 2004 | 10% | 13% | 8% | 14% | 37% | 42% | 35% | 45% |
| 2005 | 9% | 12% | 10% | 14% | 32% | 39% | 34% | 43% |
| 2006 | 8% | 11% | 9% | 14% | 27% | 38% | 29% | 41% |
| 2007 | 9% | 11% | 8% | 14% | 34% | 37% | 32% | 41% |
| 2008 | 8% | 12% | 8% | 15% | 30% | 40% | 27% | 41% |
| 2009 | 7% | 10% | 8% | 12% | 26% | 38% | 32% | 40% |
| 2010 | 8% | 10% | 8% | 13% | 30% | 40% | 32% | 44% |
| 2011 | 8% | 11% | 7% | 14% | 25% | 41% | 29% | 44% |
| 2012 | 8% | 12% | 10% | 15% | 26% | 40% | 33% | 43% |
| 2013 | 8% | 12% | 9% | 15% | 27% | 40% | 31% | 44% |
Acknowledgments
Funding:
This research was supported by the National Institute on Aging of the National Institutes of Health under Award Numbers R37AG047312 and P01 AG031098 and the National Heart, Lung, and Blood Institute of the National Institutes of Health under Award Number K24HL141354.
Footnotes
Conflicts of interest: none of the authors have conflicts of interest related to this work
References
- 1.Fang MC, Coca Perraillon M, Ghosh K, et al. Trends in stroke rates, risk, and outcomes in the United States, 1988 to 2008. Am J Med 2014;127:608–615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Akushevich I, Kravchenko J, Ukraintseva S, et al. Time trends of incidence of age-associated diseases in the US elderly population: Medicare-based analysis. Age and ageing 2013;42:494–500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Krumholz HM, Normand SL, Wang Y. Trends in hospitalizations and outcomes for acute cardiovascular disease and stroke, 1999–2011. Circulation 2014;130:966–975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Koton S, Schneider AL, Rosamond WD, et al. Stroke incidence and mortality trends in US communities, 1987 to 2011. JAMA 2014;312:259–268 [DOI] [PubMed] [Google Scholar]
- 5.Xian Y, Holloway RG, Chan PS, et al. Association between stroke center hospitalization for acute ischemic stroke and mortality. Jama 2011;305:373–380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Song S, Fonarow GC, Olson DM, et al. Association of Get With The Guidelines-Stroke Program Participation and Clinical Outcomes for Medicare Beneficiaries With Ischemic Stroke. Stroke 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kleindorfer DO, Khoury J, Moomaw CJ, et al. Stroke Incidence Is Decreasing in Whites But Not in Blacks. Stroke 2010;41:1326–1331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mochari-Greenberger H, Mosca L. Racial/Ethnic differences in medication uptake and clinical outcomes among hospitalized cardiovascular patients with hypertension and diabetes. American journal of hypertension 2015;28:106–112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mochari-Greenberger H, Liao M, Mosca L. Racial and ethnic differences in statin prescription and clinical outcomes among hospitalized patients with coronary heart disease. Am J Cardiol 2014;113:413–417 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Howard G, Cushman M, Kissela BM, et al. Traditional risk factors as the underlying cause of racial disparities in stroke: lessons from the half-full (empty?) glass. Stroke 2011;42:3369–3375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bravata DM, Wells CK, Gulanski B, et al. Racial disparities in stroke risk factors: the impact of socioeconomic status. Stroke 2005;36:1507–1511 [DOI] [PubMed] [Google Scholar]
- 12.Shroff GR, Solid CA, Herzog CA. Atrial fibrillation, stroke, and anticoagulation in Medicare beneficiaries: trends by age, sex, and race, 1992–2010. Journal of the American Heart Association 2014;3:e000756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Volpp KG, Stone R, Lave JR, et al. Is thirty-day hospital mortality really lower for black veterans compared with white veterans? Health services research 2007;42:1613–1631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Towfighi A, Ovbiagele B, Saver JL. Therapeutic milestone: stroke declines from the second to the third leading organ- and disease-specific cause of death in the United States. Stroke 2010;41:499–503 [DOI] [PubMed] [Google Scholar]
- 15.National Center for Health Statistics Office of Analysis and Epidemiology. Analytic Issues in Using the Medicare Enrollment and Claims Data Linked to NCHS Surveys. Hyattsville, MD. 2012 [Google Scholar]
- 16.Zaslavsky AM, Ayanian JZ, Zaborski LB. The validity of race and ethnicity in enrollment data for Medicare beneficiaries. Health services research 2012;47:1300–1321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Centers for Disease Control and Prevention, National Center for Health Statistics. National Health and Nutrition Examination Survey 1988–1994, 1999–2000, 2001–2002, 2003–2004, 2005–2006, and 2007–2008 documentation files. Available at: http://www.cdc.gov/nchs/nhanes.htm. Accessed February 14, 2012,
- 18.Wolf P, D’Agostino R, Belanger A, et al. Probability of stroke: a risk profile from the Framingham Study. Stroke 1991;22:312–318 [DOI] [PubMed] [Google Scholar]
- 19.Carandang R, Seshadri S, Beiser A, et al. Trends in Incidence, Lifetime Risk, Severity, and 30-Day Mortality of Stroke Over the Past 50 Years. JAMA: The Journal of the American Medical Association 2006;296:2939–2946 [DOI] [PubMed] [Google Scholar]
- 20.Mosterd A, D’Agostino RB, Silbershatz H, et al. Trends in the prevalence of hypertension, antihypertensive therapy, and left ventricular hypertrophy from 1950 to 1989. The New England journal of medicine 1999;340:1221–1227 [DOI] [PubMed] [Google Scholar]
- 21.Lakshminarayan K, Solid CA, Collins AJ, et al. Atrial Fibrillation and Stroke in the General Medicare Population. Stroke 2006;37:1969–1974 [DOI] [PubMed] [Google Scholar]
- 22.Adler GS. A profile of the Medicare Current Beneficiary Survey. Health Care Finance Rev 1994;15:153–163 [PMC free article] [PubMed] [Google Scholar]
- 23.Klabunde CN, Potosky AL, Legler JM, et al. Development of a comorbidity index using physician claims data. Journal of clinical epidemiology 2000;53:1258–1267 [DOI] [PubMed] [Google Scholar]
- 24.Sacco RL, Boden-Albala B, Abel G, et al. Race-ethnic disparities in the impact of stroke risk factors: the northern Manhattan stroke study. Stroke 2001;32:1725–1731 [DOI] [PubMed] [Google Scholar]
- 25.Casper ML, Wing S, Anda RF, et al. The shifting stroke belt. Changes in the geographic pattern of stroke mortality in the United States, 1962 to 1988. Stroke 1995;26:755–760 [DOI] [PubMed] [Google Scholar]
- 26.Howard VJ, Kleindorfer DO, Judd SE, et al. Disparities in stroke incidence contributing to disparities in stroke mortality. Annals of Neurology 2011;69:619–627 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Xian Y, Holloway RG, Noyes K, et al. Racial differences in mortality among patients with acute ischemic stroke: an observational study. Ann Intern Med 2011;154:152–159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schwamm LH, Reeves MJ, Pan W, et al. Race/ethnicity, quality of care, and outcomes in ischemic stroke. Circulation 2010;121:1492–1501 [DOI] [PubMed] [Google Scholar]
- 29.Trivedi MM, Ryan KA, Cole JW. Ethnic differences in ischemic stroke subtypes in young-onset stroke: the Stroke Prevention in Young Adults Study. BMC neurology 2015;15:221. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


