Abstract
BACKGROUND:
Different methods have been developed and employed with variable degrees of success in pre-operative templating for total hip arthroplasty. Preoperative templating, especially digital templating, has been claimed to have increased the effectiveness of total hip arthroplasty by improving the precision of prediction of prosthetic implant size.
AIMS:
The overall aim of this systematic review is to identify whether the use of pre-operative templating in total hip arthroplasty procedures has resulted in increased accuracy, reliability and precision of the procedure. Various methods of templating, like traditional acetate overlay and digital method of templating that includes a single radiographic marker and double radiographic marker methods, have been compared to establish the most reliable method of templating.
METHODS:
We searched the PubMed, Google Scholar Cochrane Central Register of Controlled Trials (CENTRAL), and MEDLINE (1966 to present), EMBASE (1980 to present), CINAHL (1982 to present), Psych INFO (1967 to present) and Clinical Trials Gov.
CONCLUSION:
The results of this systemic review suggest that preoperative templating is resulting in an enormous increase in the accuracy of total hip arthroplasty and among various methods, King Mark is the most reliable method.
Keywords: total hip arthroplasty, digital templating, prosthetic implant size
Introduction
Hip arthroplasty, also called hip replacement, is a surgical technique which involves the replacement of the diseased hip joint with a prosthetic implant. People with severe hip joint damage have gained a lot of benefit from this procedure. Hemiarthroplasty is another procedure that involves the replacement of only one half the joints with the prosthesis while the other half of the joint is left unaltered. However, researchers have shown that total hip arthroplasty shows better results than hemiarthroplasty [1]. The prosthetic implant used in this technique has 3 parts:
A femoral stem and head: This portion of the prosthesis is in one piece and is made of stainless steel
Acetabulum: This is made of polyethene.
Bone cement: Its major composition is acrylic.
The major aim while selecting for the composition of the implant is that it should be biocompatible and must not elicit an immune reaction in the body which would otherwise lead to rejection of the implant. Moreover, these implants must also resist corrosion and degradation so that they may last in the body for the longest period.
The most common indication of total hip replacement is osteoarthritis. A displaced fracture of the femoral neck that occurs in younger patients is also an important indication [2]. Other major indications include juvenile rheumatoid arthritis, ankylosing spondylitis, hip fractures, bone tumours (benign and malignant) and arthritis that is associated with Paget’s disease. Total hip arthroplasty is also recommended for the management of unreduced traumatic dislocation of the hip joint that is very common in developing countries [3]. There are several techniques of carrying out arthroplasty; the major being posterior, lateral anterolateral and anterior approaches.
In modern times, hip arthroplasty has been used extensively for managing severe hip damage. According to a review of peer-reviewed articles related to the experience of Rothman Institute, hip arthroplasty is a very safe, reliable and efficient procedure with a 10-year survival rate of the implant being greater than 99%. This remarkable rate of success has been attributed largely to the use of modern nonmetal implants [4]. Previously, metal on metal implants was used for hip joint replacement procedures, but their failure has been reported on numerous occasions [5]. So implants have now been replaced with a newer and more reliable prosthesis that has a higher success rate.
Like any other procedure, hip arthroplasty also has its complications. Dislocation is the most common complication, and it arises because the hip ball can get dislocated from its socket during the first 2 to 3 months after the operation. Venous thrombosis following hip replacement is a major problem that haunts the surgeons. However, this can be dealt with by the use of thromboprophylaxis in these patients [6]. Metal sensitivity is another complication that can lead to implant failure in patients receiving a metal prosthesis, and this should be suspected in patients who show the cutaneous signs of allergy after implantation of a metal device [7]. Sciatic nerve palsy, osteolysis and the difference between the lengths of the two legs are among other complications that are worth mentioning [8], [9].
Preoperative planning plays an important role in the success of any surgical procedure. Same is the case with hip arthroplasty in which preoperative assessment of various aspects of the procedure is of utmost importance. Researches have shown that unplanned hip replacement procedures have lower success rates than elective procedures. A prospective study was carried out at the University of Pennsylvania, and it depicted that unplanned and urgent hip arthroplasty resulted in a longer hospital stay of the patient and increase in the cost of the surgery with greater financial burden [10].
One of the important features in pre-operative planning of hip arthroplasty is the appropriate determination of the size of the prosthesis that has to be used in the procedure [11]. Preoperative templating ensures a greater degree of success of hip implant procedures. It has a profound effect on increasing the accuracy of the hip replacement procedure [12]. Accurately determining the size of the template also increases the precision of the procedure [13]. Preoperative templating also reduces the probability that the implanted prosthesis might loosen over time [14], [15]. Moreover, accurate templating before performing arthroplasty has also an important impact in decreasing the complications of the procedure among which leg length inequality and peri-prosthetic fractures are most notable [16], [17], [18], [19], [20], [21], [22], [23]. For this purpose, templates of both the acetabular and the femoral components are taken [24]. Many studies have shown that placement of the acetabular component of accurate size is of vital importance in determining how much successful the operation would be. But the major problem that the surgeons encounter in this regard is the accurate magnification of the radiograph to get the hard copy template of the radiograph for total hip arthroplasty. Accurately determining the magnification of hip radiograph and its correct application to find the exact size of the template has been the topic of interest for many years and this target, if achieved, can drastically increase the efficiency and accuracy of the hip replacement operation. For this purpose, several methods have been employed until now with variable degrees of success.
Previously, the process of templating was done by conventional methods which involved the use of drawings on transparencies of magnified implants [25]. Nowadays, digital radiography is used for this purpose.
In Digital radiography, computer programs are used to calculate the x-ray magnification and the templates are adjusted according to the magnification. The template and the radiograph are scaled in digital radiograph templating method to obtain the correct magnification. There are four basic steps in the process of templating from hip radiographs [26].
To identify the significant anatomical landmarks in the radiograph
To ascertain the quality of the radiograph.
The identification of various mechanical references, for example, femoral offset, acetabular offset, leg length discrepancy etc.
To optimise the position of the implant so that hip biomechanics are re-established.
In one study, one to one relationship was applied to assess the scaling to determine hip magnification. An object of known size, called the reference object, was placed adjacent to the hip to determine hip magnification. This technique was successful in establishing accurate templating for hip arthroplasty as the magnification of the reference object was equivalent to the magnification of the hip. However, it was found that for the method to be successful, it was compulsory that distance of the reference object and that of the centre of rotation of the hip should be at the same distance from the detector [27]. In another technique, a ten-penny coin was used as a marker in the process of scaling for magnification. Another method called two digital-line methods was also used for this purpose [28].
All the methods that are described above for digital templating have been designed in such a way that they use a single radiographic marker ball or disc whose diameter is known. However, for this method to be accurate, the marker has to be placed in the coronal plane of the hips so that the accurate magnification of the hip may be obtained. If the marker is not properly positioned in the mentioned manner, the results of templating become inaccurate and the process becomes useless. For this purpose, the scientists felt a need to devise a new method of radiographic calibration that may provide more accurate results than the traditional single marker metal ball method of templating. Moreover, the condition that the radiographic marker should be positioned very precisely was also very annoying for the orthopaedic surgeons and in the course of developing a new device for templating; it was kept in mind that the new method must free the surgeons of this limitation. This lead to the new invention KING MARK by the University of Warwick and University Hospitals Coventry and Warwickshire (UHCW) which has revolutionised the whole procedure of digital templating and radiographic magnification for prosthetic implants. This technique has been claimed to be superior to the traditional metal ball method in many respects. King Mark is a double calibration device that is used for radiographic magnification. In King Mark, two markers are used for calibrating the template size. One marker is placed behind the pelvis, and the other marker is placed in front of the pelvis. The marker that is placed behind the pelvis is a pad that is radiolucent. Steel rods are embedded in it. The marker that is placed anteriorly is a strap that has radio-opaque balls secured in it. In this way, two markers are used for appropriate calibration. The King Mark is placed in the midline and if it is not placed in the midline, it appears on the radiographs that the markers are not properly positioned and this saves the surgeons from positioning mistakes that were encountered in the traditional single ball marker. One of the greatest advantages of this technique is that while single markers were not easy to use with very large patients, King Mark is easy to use in patients of all sizes. The method is non-intrusive and its accuracy and efficiency has been validated by a number of renowned institutions that are currently using it as part of the templating for total hip arthroplasty. Previously, in the UK, the sizes of the prosthesis for hip replacement were estimated correctly only in approximately 30% of the cases. With this new invention, the condition is expected to improve a lot and the inventors believe that it will go a long way in ensuring that the future total hip arthroplasty procedures are more successful at a much higher rate than they are currently. Professor of Trauma and Orthopaedic Surgery at Warwick Medical School, Professor Damian Griffin said:
“King Mark has removed all of the uncertainty about scaling digital radiographs for hip replacement. Our radiographers find it easy to use, and I can be confident that the measurements I make on scaled radiographs are correct. It is now unusual for my pre-operative templating not to be exactly right.”
Using this technique, calibrations determined via digital templating will become more accurate and cost-effective. An orthopedic surgeon at UHCW Mr Steve Krikler said:
“Since changing to King Mark system, I have found the acetabular cup size to be very accurately predicted from the template, and the femoral size is also much more accurately predicted. I am now much more confident in choosing the stem offset and other parameters which are within my control, I always template my arthroplasties in TraumaCad, and I will only accept pre-operative images which include King Mark.”
Given all this, it is expected that in the future, King Mark may also be used in other joint replacement procedures as well in addition to the hip arthroplasty.
Figure 1.
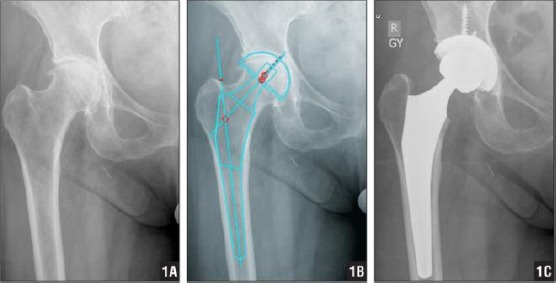
Preoperative hip radiograph (A), preoperative digital template using the traditional metal ball method of templating (B), and postoperative hip radiograph (C) of a patient who received a Right Total Hip Replacement
A small metal ball of known size can be seen at the left edge of the picture to help in identifying the magnification of x-ray
Figure 2.
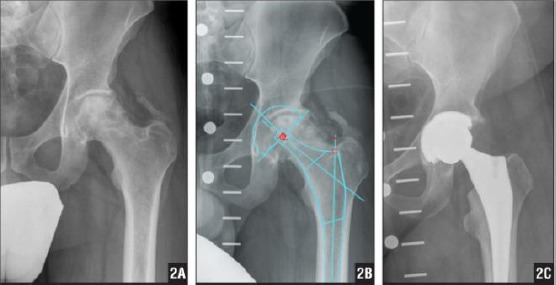
Preoperative hip radiograph (A), preoperative digital template using the newly designed KingMark (Double Markers) method of templating (B), and postoperative hip radiograph (C) of a patient who received a Left Total Hip Replacement
The overall aim of this systematic review is to identify whether the use of preoperative templating in total hip arthroplasty procedures has resulted in increased accuracy, reliability and precision of the procedure. The study also aims at assessing the effects of pre-operative templating on cost-effectiveness of total hip arthroplasty. Various methods of templating including traditional acetate overlay and digital method of templating that include a single radiographic marker, and double radiographic marker methods have been compared to establish the most reliable method of templating. The aims also include assessment of the extent to which pre-operative templating has reduced post-operative complications of the procedure.
Methods
Criteria for considering studies for this review
Type of studies
Both prospective and retrospective studies have been selected for this review. Moreover, both conventional parallel designs and cross over type designs were included.
Type of participants
Studies included in this review only involved participants who had total hip arthroplasty, whether cemented or uncemented. Studies in which hemiarthroplasty procedures are performed were not considered.
Type of interventions
Study procedures that involve the following interventions will be considered.
- Total hip arthroplasty
- Digital templating for total hip arthroplasty
- Computed tomography-based templating for total hip arthroplasty
- Metal ball method of templating for total hip arthroplasty.
- Double radiographic method or King Mark method of templating for total hip arthroplasty
Primary outcomes
- Increased or decreased intra and inter observer reliability of templating procedure
- Increased or decreased accuracy or precision of total hip arthroplasty using the templating procedure.
- Decrease or increase in the cost-effectiveness of total hip arthroplasty after using templating
Secondary outcome
- Increased or decreased post-operative complications in patients with total hip arthroplasty after the use of templating technique.
Search strategy
We searched the PubMed, Google Scholar Cochrane Central Register of Controlled Trials (CENTRAL), and MEDLINE (1966 to present), EMBASE (1980 to present), CINAHL (1982 to present), Psych INFO (1967 to present) and Clinical Trials Gov exhaustively and comprehensively. In our search, we used descriptors like the accuracy of total hip arthroplasty following pre-operative templating, leg length discrepancy, leg length inequality, metal ball method of pre-operative templating, templating for total hip arthroplasty, THA, King Mark, a single radiographic marker for templating, a double radiographic marker for templating. We first searched for PubMed. Subsequent search strategies were derived from the MEDLINE strategy and Adapted for each database. A detailed description of the database outputs is shown in Tables 1 and 2, and Figure 1).
Table 1.
Keywords used in the research strategy. Initial searches were performed by using keywords, alternate keywords combined with Boolean logic (OR). They were then combined using the Boolean logic (AND) to ensure that all the required terms for research will be included in the studies.
| Search | Keywords |
|---|---|
| 1 | hip OR hip joint |
| 2 | hip prosthesis OR hip replacement OR hip arthroplasty OR total hip arthroplasty OR total hip replacement OR total joint replacement OR THA |
| 4 | King mark OR metal on metal implant OR non-metal implant OR metal ball method OR |
| 5. | Preoperative templating OR leg length discrepancy |
| 6. | 1 AND 2 AND 3 AND 4 AND 5 |
Table 2.
The number of articles and databases
| Databases | CINAHL FULLTEXT | MEDLINE | Pubmed | Cochrane | Embase | Psycho info. |
|---|---|---|---|---|---|---|
| Search 1 | 4524 | 1,314 | 13,847 | 3086 | 4930 | 5,277 |
| Search 2 | 2458 | 854 | 5247 | 1014 | 2637 | 3,252 |
| Search 3 | 852 | 524 | 325 | 626 | 1352 | 512 |
| Search 4 | 354 | 303 | 101 | 352 | 462 | 405 |
| Search 5 | 25 | 19 | 10 | 11 | 9 | 13 |
Figure 1.
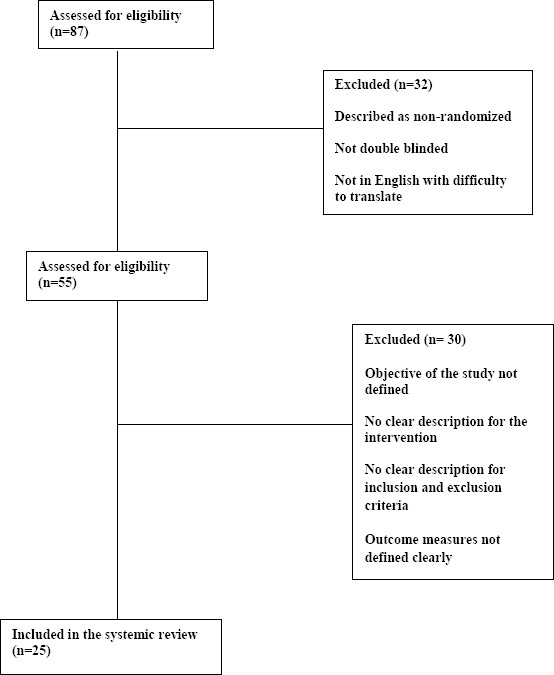
Consort diagram for the search strategy used
As shown in Table 1, different databases were searched with the help of keywords and Boolean logic ‘AND’,’OR’. A group of 87 articles were retrieved in total out of which 25 were included in the systematic review. The flowchart below gives the process of article selection regarding the inclusion and exclusion criteria.
Reference list
Reference list of articles that the authors know has been searched. Other reviews that are found during the process of the search were not included.
Grey literature
We tried to contact authors of included studies to acquire other data that may either be unpublished, informally published or ongoing and is related to pre-operative templating for total hip arthroplasty.
Selection of studies
Review authors had independently screened and selected studies for possible inclusion in the study.
The titles and abstracts of trials identified from the search were independently reviewed and pooled for further screening.
Each review author independently examined the full text of all trials that were identified from the title and abstract screens.
Each reviewer compiled a list of studies that meet the inclusion criteria.
The contents of each review author’s list were compared, and any disagreement was resolved by discussion and consensus between all of the review authors.
Data extraction and management
Two review authors had independently extracted data using specially developed data extraction forms. Information collection was based on:
Participant characteristics (age, sex, number of participants, indications for total hip arthroplasty, the type of method used in templating for total hip arthroplasty)
Intervention details (traditional method use of pre-operative templating, digital method, metal ball method, single radiographic method, King Mark method, double radiographic marker method)
Outcome measures (description of the measures used, continuous/dichotomous nature etc.)
Dealing with missing data
For missing data, the authors of the studies will be contacted. This would be done during the eligibility assessment and data abstraction. Moreover, the missing data will also be sought from secondary publications of the same study. However, if data are only available in the graphic format, we will impute approximations of the mean.
Publication bias
We assessed the risk of bias for each included study by an adapted Cochrane Collaboration “Risk of bias” assessment tool, including sequence generation, allocation concealment, blinding, incomplete outcome data/loss to follow-up, selective outcome reporting and other issues.
The response options for the quality assessment are defined as: yes (criteria applied and described appropriately or acknowledged in the study), no (criteria inappropriately applied) and unclear (criteria not described and impossible to obtain from the study). Each study has been classified into one of the categories below.
- High risk of bias: one or more criteria not applied/met.
- Moderate risk of bias: one or more criteria unclear.
- Low risk of bias: all criteria applied/met.
The review authors will discuss any disagreement in the assessment of the risk of bias to reach a consensus.
Assessment of quality of evidence across studies
We assessed the quality of evidence in this systematic review using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) tool with GRADE profiler (GRADEpro) version 3.6 software, defining the quality of evidence for each outcome as the extent to which one can be confident that an estimate of effect or relation is close to the quantity of specific interest. The GRADE system rates the quality of evidence across studies as one of four levels: very low, low, moderate and high.
Sensitivity analysis
We hypothesize that pre-operative templating for total hip arthroplasty is less effective in increasing the reliability of templating hip arthroplasty in studies with a high risk of bias and in studies with short duration (that is, less than six months), thus we carried out sensitivity analyses by excluding studies classified as having high risk of bias and removing those having short duration. Also, the fixed-effects model was conducted for sensitivity analysis.
Assessment of reporting biases
We constructed a funnel plot to investigate the potential for publication bias for the primary outcomes relating to the accuracy and reliability of various methods of templating for hip replacement procedures.
Discussion
Several types of research have been carried out throughout the world to find out whether pre-operative templating for total hip replacement is effective or not, to determine what methods of templating are more reliable. Most of the studies that were done on the effectiveness of templating concluded that the role of pre-operative is certainly very important in estimating the success of the procedure. It was found that pre-operative is templating certainly increased the accuracy of total hip arthroplasty, increase in long term survival of the prosthetic implants in the body, a greater degree of patient satisfaction, decrease in post-operative complications of the procedure and better cost-effectiveness. Regarding the fact that what method of templating was more reliable, most of the studies revealed that the new digital method of pre-operative templating is clinically more significant than the traditional and conventional methods which had larger mean errors. Digital methods of templating comprise of single radiographic marker methods (metal ball methods) and the newly invented King Mark method which is a double marker technique. King Mark was found superior to the standard metal ball method.
Regarding the effectiveness of pre-operative templating research concluded that preoperative templating resulted in accurate planning of the size of prosthetic implants in 98% of the cases and hence it was recommended that templating must be done preoperatively in all cases of total hip replacement to make the process more reliable [29].
In a study, the digital method of templating was compared with a conventional method of templating for hip arthroplasty. Eighteen patients have included in the study, and all of them underwent uncemented total hip replacement procedures. The conventional templating was performed by using hard copy radiographic films and hard copy prosthetic overlays on a radiographic view box. The digital templating involved using computer-based software. Moreover, intra-observer and inter-observer variations were also assessed in all cases. The results of the study depicted that there was no significant difference between the conventional and the digital templating methods in determining the size of the actual prosthesis to be used in the procedure. Moreover, intra and interobserver variability were also found to be approximately the same for both conventional and digital methods. However, the basic limitation of this trial was that they included uncemented hip arthroplasties in their trial and so it is expected that carrying out the trial with the cemented templating hip arthroplasty might reveal some differences between the conventional and digital methods [30].
In another study, the standard acetate method was compared with the digital method of templating. It was found that while using the standard acetate method, the accuracy of the template for the acetabular component was 67% and was found to be 82% of the femoral component. In contrast, the accuracies for the acetabular and femoral components were found to be 78% and 90% respectively when the digital method was used thus reflecting the superiority of digital method of templating for the hip replacement procedure [31].
In another randomized control trial, it was found that the digital method was superior to the conventional methods both in accuracy and in long term survival of the implant [32].
Another study that focused on determining the reliability of digitally assessed magnification of hip radiographs for estimating the correct implant size stressed that the results of pro-operative templating must be verified once again intra-operatively to ensure the success of the procedure [33].
It has also been found that the accuracy of the templating procedure does not entirely depend upon the method of templating but is also determined by the efficiency and the experience of the physician. In a study, the implant sizes were determined using the same digital method of templating by two groups. One of the groups consisted if orthopaedic residents and the other group included experienced orthopedic surgeons. The results of the accuracy of the implants were compared afterwards. The group consisting of orthopedic residents accurately predicted the acetabular component size in 63% of cases and the femoral component size in 87% of the cases. On the other hand, the group of experienced surgeons accurately predicted the acetabular component measurements in 88% cases and the femoral component in 97% cases. These figures certainly stressed that an experienced hand also has a significant role to play inaccurate pre-operative templating [34]. Similarly, it has been found training and experience level of the attending surgeon has no effect on the accuracy of acetabular component templates, but these factors do have a serious impact in determining the accuracy and precision of the femoral component template [35].
In a study, the templates developed by the same digital method of templating by a group of orthopaedic residents and by another group consisting of orthopaedic surgeons were compared. It was found that the accuracy of the templates developed by the orthopaedic residents was 63% of the acetabular implants and 89% of the femoral implants. Using the same method of templating, the orthopaedic surgeons correctly templates the acetabular component in 89% cases and the femoral component in 97% cases. This validated the statement that for the digital templating method to be accurate and reliable, it must be performed by an experienced hand rather than by untrained and unskilled personnel [36].
The conclusion of another study stated that digital templating predicts the size of the prosthetic implant with a high degree of precision and accuracy both for total hip arthroplasty and for short- stem hip arthroplasty and hence can cause a significant reduction in the postoperative complications and the failure of the surgical intervention [37]. Another study that assessed the accuracy of digital templating for uncemented hip arthroplasty revealed that digital templating predicted the size of the prosthetic implant accurately in 50% of the cases. However, when implants with two sizes of the template were used, the accuracy reached 100%. It was also found that the training level of the surgeon also affected the accuracy of the procedure. The Less experienced investigator had an accuracy rate of 82% while the more experienced ones had the accuracy rate of around 95% [38].
Another study stressed that although digital templating is a very reliable method for pre-operative detection of prosthetic implant size yet, it has been found that when implants are selected only from pre-operative templating, there is an increased risk that fractures may occur during the insertion of the implants [39]. Another study concluded that digital templating is very useful inaccurate correction of leg length in total hip arthroplasty [40].
Another study was done with the aim of assessing the reliability and accuracy of the digital method of templating. During the process, templates were made both for the acetabular component and the femoral component. The study also stressed as another one described previously, that all the implants that are selected by pre-operative digital templating must be verified intra-operatively to make the total hip arthroplasty procedure more efficient and reliable [41].
In other research, three methods of templating were compared with one another to find out which one of them was more reliable. One of the methods was analogue hard copy templating method, and the rest of the two were digital methods of templating. In addition to determining the accuracy of the method, the researchers were also interested in finding out whether these methods of templating were reproducible or not. In the study, both cemented, and uncemented implants were used to carry out total hip arthroplasty. The process of determining the best templating method was done using a retrospective study. The study included 33 patients out which 16 patients underwent cemented total hip arthroplasties, and 17 patients underwent cemented total hip arthroplasties. In the analogue hard copy method of templating, transparent sheets were taken, and the contours of the prosthesis were depicted on it. In this way, all the total hip arthroplasties were templated by analogue hard copy method. Digital Method 1 was performed with IMPAX™ ES Orthopaedic Application planning software, and the diameter of the reference object was used to determine template size. The digital method 2 was performed identically as the digital method 1. The main difference was that instead of using the diameter of the reference object as such, the corrected diameter of the reference object (that was determined by applying the linear relationship between magnifications of the reference objected the hip) was used. The results showed that digital method 2 was superior to the other 2 methods. Moreover, the reproducibility of all three methods was found to be moderate [42].
Another study was done with the aim of comparing the conventional method of templating with a new CT based method. The results of the study showed that the new CT based method of templating was much more accurate and easier than the conventional one. The new method was also found to be reproducible and easier to use even for the less experienced practitioners [43].
Another study compared the analogue and digital methods for total hip and knee arthroplasties. The results of the study, strikingly, were in favor of the analogue method of templating for hip arthroplasties. It was calculated by statistical analysis that analogue templates were accurate in 73% and 89% cases for cemented cups and stems and were 64% and 52% accurate for uncemented cups and stems respectively. Regarding the digital method, the accuracy of templates for cemented total hip arthroplasties was calculated to be 72% and 79% for cement cup and stem respectively and 52% and 66% for uncemented cups and stems respectively [44].
In another study, the accuracy and reliability of digital templating were assessed in uncemented hip replacement procedures. Orthoview software was used for this procedure. The accuracy in templating for femoral component was calculated to be 75% with 0.5 sizes and approximately 98% within 1 size. Head length templates were accurate in about 62% of the cases. The Acetabular component template was found to be accurate to 2 mm in 80% cases and with 4 mm in 98% cases. The results surely validated the efficiency of digital templating [45].
In a research procedure, validity, inter-observer reliability and intra-observer reproducibility of Mdesk, a digital method of pre-operative templating, were assessed. It was found that the validity of the system was good. The inter-observer reliability was found to be fair, and the intra-observer reproducibility was found to be excellent. By the observations, it was recommended that the pre-operative templating and the operation for the insertion of the implants must be done by the same surgeon to assure the success of total hip replacement [46].
Pre-operatively predicted prosthesis for total hip arthroplasty were compared in a study with the sizes of the original implants that were used in the surgical procedure afterwards. The mode of templating was digital. The researchers found that the pre-operatively predicted implants were of exact sizes as that of the original prosthesis used in hip replacement in 36% cases for femoral component and 33.7% cases for the acetabular component. The template size was with 1 size above or below of the originally used size in 77.5% cases for an acetabular cup and 82.3% cases for the femoral stem. This showed that digital preoperative templating was highly reliable and accurate. However, a difference of more than 2 sizes above or below the corrected size was found in a few cases, and so it was recommended that intraoperative X-rays must be used to verify the size of the prosthesis predicted by digital templating to ensure the successful hip arthroplasty [47].
A study in which metal ball method for templating was used to depict that the method accurately predicted the prosthesis size in 58.5% cases for total hip arthroplasty and approximately 93% of the templates were about +/- 1 size of the original implants. Moreover, none of the templates taken by digital metal ball method of templating was beyond 2 sizes of the originally implanted prosthesis, i.e. approximately all of the cases of templating hip arthroplasty were sized correctly. Metal sphere also correctly estimated the femoral head size in 100 % cases [48].
A study for the assessment of the reliability of digital templating in carrying out total hip arthroplasty in patients with Crowe type 2 and 3 dysplastic hips was done. Two groups of patients were assessed. One of the groups had Crowe type 2, and 3 dysplastic hips and the other group had other primary hip diseases. Total hip arthroplasty was to be done in both the groups and hence templates of the prostheses were prepared using digital templating. In patients with Crowe type 1 and 2 dysplastic hips, the accuracy of digital templating was 48.8% for acetabular component and 73.2% of the femoral component. On the other hand, in patients with other primary diseases, the results of digital templating to carry out hip arthroplasty were quite encouraging, and the accurate prediction of the acetabular component was achieved in 70.8% cases and 79.2% cases for the femoral component. Nevertheless, digital templating is still useful in patients with Crowe type 1 and 2 dysplastic hips [49].
Striking evidence in favour of manual methods of templating and against the digital method was provided in a study. It showed that the manual acetate method accurately predicted the femoral prosthetic component in 75% cases and that of the acetabular component in 83.3% cases. The digital method, on the other hand, was accurate in 41.6% cases about femoral component and in 75% cases for the acetabular component. The manual method of templating was much cheaper than the digital method of templating. Moreover, manual templating was also proved to be faster than the digital templating technique [50].
Four different methods of digital templating were compared in research. In two methods, metal balls were used for calibration. In method 1, the ball was placed laterally, and in method 2, the ball was placed medially. In method 3, the fixed magnification of 121% was applied and in method 4, object-film distance was applied. The results of templating were then compared and revealed that method 1 and 2 were associated with mean errors of 2.55% and 2.04% respectively. Mean error for method 3 was 1.42% and for method 4 it was 1.57%. The greater degree of errors in methods 1 and 2 was mostly due to the high degree of precision with which the balls have to be placed in order to get correct magnification for templating. Methods 3 and 4 proved to be more clinical significance [51].
In another similar study, computer based digital templating in uncemented total hip arthroplasty was compared with standard templating techniques. Digital templating again proved to be of better significance and reliability than standard templating technique. Good intra observer and inter observer reliability was found with the use of digital method of hip magnification for total hip arthroplasty. The Infraclass correlation coefficient was calculated to 0.7. There were significant differences in the accuracy of these two procedures. Using the digital templating technique, the size of femoral stem was predicted accurately to within 1 size in 85% cases and that of acetabular component in 80% cases. The only standard technique, however, was much less accurate especially in the prediction of acetabular component size. The accuracy was only 60% to within 1 sizes. This validated the superiority of digital computer-based method of templating over the standard only templating [52].
The usual method of performing digital templating is by the use of radiographic markers. However, hip magnification can also be calculated without the use of a radiographic marker. This can be done by measuring the distance from the x-ray focal spot to the object and the distance from the x-ray focal spot to the radiological cassette or image receptor. These two methods of digital templating were compared in research. Medical records were taken, and the original size of the femoral head was obtained that was used in the surgical intervention. The methods mentioned above were then used to find out hip magnification and predict the size of the femoral head prosthesis. The accuracy of these methods was compared with each other afterwards. It was observed that both the methods had an almost equal accuracy. The radiographic marker method had a mean error of 2.6%, and non-marker methods had a mean error of 2.8%. However, the distance method was expected to be more acceptable to the patients and the technician. The distance method was also less complicated as there was no compulsion of the accurate placement of the radiographic marker for obtaining an accurate calibration of the prosthetic implant [53].
Another study investigated the utility of computer software based digital templating and also compared it with a traditional method in which magnification of 115-120% was assumed in the development of templates. The results of the study suggested that if magnification is assumed to be 115%, then the prosthesis size is not accurately determined and we get an over-sized magnification by 6 mm. So the use of digital templating was recommended [54].
To calculate magnification for templating, the object that is being used for templating must be placed at its centre and lack of fulfilment of this condition frequently leads to an error in determining accurate template for hip replacement. In a study, a new method was devised to alleviate this compulsion, and a planar disc was introduced. This disc was placed in the radiographic cassette and predicted magnification was obtained afterwards. The researchers concluded that the use of planar disc was associated with a greater degree of accuracy in predicting the correct magnification than the sphere. It was also noted that the technique was cost-effective and hence the use of planar disc instead of the sphere was recommended [55].
It has been declared by research work that to minimise the complaints of leg length discrepancy in patients who undergo total hip arthroplasty, pre-operative digital templating fooled by an Intraoperative x-ray is much helpful. By using this method of pre-operative and intraoperative assessment, the mean postoperative leg length inequality was reduced to 0.33 mm in contrast to greater than 6 mm that is usually encountered with the use of digital templating [56].
A prospective trial was done to identify accurate calibration methods of the digital radiograph to be used in pre-operative templating for total hip arthroplasty. One method involved positioning a coin between the patient’s thighs and another method involved the use of callipers to measure the width of the pelvis. Their accuracy was then determined by comparing predicted sizes of the head of implants with the size of originally used implants. Coin method was found to more accurate clinically than calliper method [57].
Another prospective study compared analogue and digital techniques of pre-operative templating. Digital templating was found to be less accurate than analogue templating. For uncemented acetabular and femoral components, accuracy for the digital method was 52% and 66% respectively, and for cemented components, accuracy was 72% and 79% respectively. The accuracy of the analogue method for cemented acetabular and femoral component was 73% and 79& and for uncemented components was 64% and 52%. However, limitations of the study were that digital templates were not developed by experienced surgeons and analogue templates were planned by skilled surgeons and that might have resulted in bias [58].
A study was done to analyse the reliability and efficiency of the computed tomography-based method of pre-operative templating and compared it the traditionally used methods. Patients selected for this study were those who underwent uncemented total hip arthroplasty. It was suggested that except for a few cases in which combined femoral neck anteversion and external rotational contracture of the hip is less than 15 degrees, computed tomography-based computer software generated templates were more reliable, accurate and precise in determining prosthesis size both for a femoral and acetabular component in total hip arthroplasty [59].
Accuracy of pre-operative templating for uncemented total hip arthroplasty. The results of the trial depicted that the template size of femoral stem was exactly accurate only in 50% cases. However, the accuracy of templating was increased to greater than 85% when the femoral component implant was used with +/- 1 size of the template size. Accuracy rose to almost 100% when the femoral prosthesis within two sizes above or below the template size was used in operation. The experience level of the attending surgeon also greatly affected the precision of templating. Cases involving acute femoral neck fractures and proximal bone deformity were particularly difficult to template accurately [60].
To analyze whether the advent of templating techniques by digital methods has resulted in any positive impact on the success of total hip arthroplasty in orthopaedic procedures, a study was done and concluded that as digital methods have resulted in mean magnification of 97%, therefore, templating by digital methods might result in improper selection of prosthetic implants for total hip arthroplasty as most of the manufacturing industries assume magnification to be 115-120% [61].
Assessment of precision, accuracy, reliability and utility of digital and analogue pre-operative templating procedures in determining the success of total hip arthroplasty was done in a prospective study. The accuracy of the analogue method in predicting the acetabular component size was 97%, and that of the digital method was 81%. In the case of the femoral component, the accuracy of the analogue method was found to be 98%, and that of the digital method was found to be 81%. Analogue method of templating was found to be more accurate than digital methods especially in estimating the size of the acetabular component. It was concluded that a large error in digitally predicted prosthesis template sizes was due to inaccurate positioning of the radiographic marker because for digital templating to be accurate, it is necessary that the radiographic marker should be appropriately positioned [62].
In other research, the accuracy of pre-operative templating in cementless total hip arthroplasties was calculated. A total of 109 surgical cases was included in the study. For an acetabular component of the prosthesis, accuracy of the predicted template was only 42.2%. In the case of the femoral stem, the accuracy of the predicted template was found to be 68.8%. However, when implants within 1 or 2 sizes of the template implants were used, the accuracy of templating rose to greater than 90% both for femoral and acetabular components. It was also noticed that if the patient had undergone total hip arthroplasty in the contralateral hip and it was used as an aid in predicting the size of the prosthesis, accuracy of templating increased even further but only for the femoral stem [63].
As mentioned earlier, leg length discrepancy is a common complaint among patients who undergo total hip arthroplasty. Preoperative templating has been noticed to play a major role in alleviating this complaint a great deal. A study was done with the aim of verifying this and concluded that in patients in whom the size of acetabular and femoral implants was determined preoperatively by templating, incidence of leg length inequality was reduced to almost nil and hence it was concluded that pre-operative templating is a reliable method for achieving leg length equality in patients who undergo total hip arthroplasty [64].
A study was carried out with the aim of assessing the degree of accuracy and reliability of the digital method of templating by comparing it with the traditional acetate method. Templating was done by using both methods one by one and the sizes of these templates were then compared with the size of original implants that were used in surgical procedures. About safety, digital templating was noted to be safer than traditional templating. About accuracy, the value of absolute error indicated that digital method was less accurate than acetate-based methods because the digital method underestimated the size of the femoral component and overestimated the size of the acetabular component [65].
Researchers tried to establish the most reliable position for placing the radiographic marker so that accurate template may be obtained for total hip arthroplasty. After carefully evaluating 106 patients, they concluded that the most reliable position for placing a radiographic marker to increase the accuracy and reliability of templating is at greater trochanter without skin overlap [66].
Similarly, it has been found that digital templating is very useful in total hip arthroplasties and is much more reliable than traditionally used acetate overlays that are prone to errors in magnification [67].
The studies mentioned above represent the analysis of digital templating methods using single radiographic markers. As mentioned previously, the single radiographic marker usage was associated with some complications in the procedure, and so, the King Mark method which uses two separate radiographic markers for hip magnification was devised. Although the method has been claimed to remove the major difficulties that were encountered using single marker templating methods and has been praised by the orthopaedic surgeons throughout the world, a new series of research and analysis has now begun to unfold various aspects of this new invention. Several researchers have compared the new method with the previous single radiographic marker method.
In a study, researchers investigated the double radiographic marker method of hip magnification for pre-operative templating and compared it with the normally used single marker method. In both cases, the calculation of magnification of the radiograph and its calibration was done by using Traumacad. The statistical analysis of the study revealed that the median error using double marker method of radiographic magnification was only 1.14% while using the single radiographic marker, the median error was estimated to be approximately 6%. The study concluded that the double marker method is certainly more accurate and reliable than the single marker method to template for hip arthroplasty procedure [68].
University Hospitals Coventry and Warwickshire NHS Trust in the UK also carried out a similar study in which they compared the single radiographic marker method with the recently invented double radiographic marker method. The predicted magnification of the hip radiograph was calculated by both the methods for the acetabular and femoral components of the prosthetic implant, and the true magnification of these components was also determined. The researchers then compared the single and double marker methods. It was found that for the single marker method, the correlation between the true and predicted magnification was moderate for a single marker. The values were calculated to be r = 0.5 and n = 63. For the double radiographic marker, the values were r = 0.90 and n = 74, and so the correlation was good. Median error for the single marker method was 4.8%, and for the double marker, method was 1.1%. The intraclass correlation coefficient was 0.89 for the double marker method and 0.32 for the single marker procedure. So the validity of the double marker method was excellent. All these results proved that the double marker method was better than the single marker method [69].
Similarly, another study for the assessment of the accuracy and reliability of King Mark double radiographic marker and to compare it with the standard metal ball method was done in The Centre for Hip Surgery, Wrightington Hospital, UK. During the study, radiographic magnification was used by both methods to predict the size of the femoral head prosthesis and was then compared separately to the actual sizes of the prosthetic femoral head that were used in the surgical procedure. It was estimated that the median error was 1.02 mm for King Mark and 2.05 mm for the standard metal ball method. The intra-class Correlation coefficient was 0.83 for King Mark method and 0.76 for the metal ball method. So the ICC was better for King Mark. However, the analysis showed that the interobserver agreement was not very encouraging for both methods. The research concluded that King Mark was much more accurate and efficient than the standard metal ball method in templating for the size of the femoral head while on the other hand, the metal ball method might overestimate the template size [70].
Conclusion
Total hip arthroplasty is a very useful procedure that has played a really important role in the rehabilitation of patients suffering from various debilitating diseases of the hip and has saved a large number of patients from getting crippled for the lifetime. Thousands of total hip replacements are carried out throughout the world. Given this, it is very important that the prosthetic implants that have to be used in arthroplasty must be chosen precisely to avoid a large number of complications that may occur as a result of improper selection of the implant size. By discussion mentioned above, we conclude that preoperative templating for the process of hip arthroplasty has increased the success rates of templating hip arthroplasty throughout the world.
It has been observed that pre-operative templating has increased the success of total hip arthroplasty to almost 98%. By comparison between the accuracy of various methods of templating, it has been found that the digital method of templating is superior to all the other conventional and traditional methods in all respects. The mean error in predicting the size of the femoral and acetabular components of the implants is much lesser for the digital method as compared to the traditional methods. The incidence of postoperative failure of total hip arthroplasty has greatly reduced since the advent of digital techniques. Moreover, the risk of postoperative complications has also been minimised by the accurate use of digital methods. The problem of leg length discrepancy that previously was much more prevalent in patients who underwent hip replacement has been solved to a large extent using digital methods. The intra and interobserver reliability is also much better for digital methods than for the traditional methods. The ICC coefficient is also significantly greater for digital methods, and this provides the evidence of the reliability of digital methods. However, it has been found that the precision and accuracy of templating is not solely dependent upon the method of templating used but also depends on the skills and experience of the performing surgeon. The results of templating in predicting the size of the prosthesis accurately to be used in the original procedure also depend upon the level of training and experience of the personnel and the process of templating if performed by an adept surgeon increases the probability of accurate prediction of the implant size. It is also recommended that pre-operative templating and total hip arthroplasty should be performed by the same surgeon as it has been proved by several research procedures that this plays an important role in improving the success rate of hip replacement procedures.
Furthermore, the intra operative verification of the prosthesis is also recommended as the implants that have been inserted solely on the basis of results of templating have resulted in subsequent failure much earlier than those that were carefully verified intra operatively. However, the use of single radiographic marker had its problems with that high degree of precision was required in positioning the marker. To get rid of this, inventors have developed a novel method of templating for hip arthroplasty which has proved to be much more accurate, reliable and easy to use than the single radiographic marker technique. However, several aspects of King Mark, the double radiographic marker method, are yet to be revealed and with the passage of time, researchers will be done to assess the further credibility of this method.
Limitations: Although great care has been taken, but this review may have some limitations. This is because many types of research and trials that have been selected for this systemic review might be associated with bias. Moreover, studies that were published in non-English language could not be translated and then included in the review procedure. If these studies were thoughtful and necessary for incorporation into our systematic review, then our review might be subjected to selection bias.
Footnotes
Funding: This research did not receive any financial support
Competing Interests: The authors have declared that no competing interests exist
Reference
- 1.Parker MJ, Gurusamy KS, Azegami S. Arthroplasties (with and without bone cement) for proximal femoral fractures in adults. The Cochrane database of systematic reviews. 2010;6:CD001706. doi: 10.1002/14651858.CD001706.pub4. https://doi.org/10.1002/14651858.CD001706.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Skala-Rosenbaum J, Cech O, Dzupa V. [Arthroplasty for intracapsular fractures of the femoral neck. Current concept review] Acta chirurgiae orthopaedicae et traumatologiae Cechoslovaca. 2012;79(6):484–92. PMid:23286679. [PubMed] [Google Scholar]
- 3.Garrett JC, Epstein HC, Harris WH, Harvey JP, Jr, Nickel VL. Treatment of unreduced traumatic posterior dislocations of the hip. J Bone Joint Surg Am. 1979;61:2–6. https://doi.org/10.2106/00004623-197961010-00002 PMid:759430. [PubMed] [Google Scholar]
- 4.Austin MS, Higuera CA, Rothman RH. Total hip arthroplasty at the rothman institute. HSS journal :the musculoskeletal journal of Hospital for Special Surgery. 2012;8(2):146–50. doi: 10.1007/s11420-012-9268-x. https://doi.org/10.1007/s11420-012-9268-x PMid:23874255 PMCid:PMC3715633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mikhael MM, Hanssen AD, Sierra RJ. Failure of metal-on-metal total hip arthroplasty mimicking hip infection. A report of two cases. The Journal of bone and joint surgery American volume. 2009;91(2):443–6. doi: 10.2106/JBJS.H.00603. https://doi.org/10.2106/JBJS.H.00603 PMid:19181991. [DOI] [PubMed] [Google Scholar]
- 6.Sobieraj DM, Lee S, Coleman CI, Tongbram V, Chen W, Colby J, et al. Prolonged versus standard-duration venous thromboprophylaxis in major orthopedic surgery:a systematic review. Annals of internal medicine. 2012;156(10):720–7. doi: 10.7326/0003-4819-156-10-201205150-00423. https://doi.org/10.7326/0003-4819-156-10-201205150-00423 PMid:22412039. [DOI] [PubMed] [Google Scholar]
- 7.Hallab N, Merritt K, Jacobs JJ. Metal sensitivity in patients with orthopaedic implants. The Journal of bone and joint surgery American volume. 2001;83-A(3):428–36. doi: 10.2106/00004623-200103000-00017. https://doi.org/10.2106/00004623-200103000-00017 PMid:11263649. [DOI] [PubMed] [Google Scholar]
- 8.Goldstein WM, Gordon A, Branson JJ. Leg length inequality in total hip arthroplasty. Orthopedics. 2005;28(9 suppl):s1037–s1040. doi: 10.3928/0147-7447-20050902-06. PMid:16190031. [DOI] [PubMed] [Google Scholar]
- 9.Rubash HE, Parvataneni HK. The pants too short, the leg too long:leg length inequality after THA. Orthopedics. 2007;30:764–765. doi: 10.3928/01477447-20070901-30. PMid:17899929. [DOI] [PubMed] [Google Scholar]
- 10.Kamath AF, Austin DC, Derman PB, Israelite CL. Unplanned Hip Arthroplasty Imposes Clinical and Cost Burdens on Treating Institutions. Clinical orthopaedics and related research. 2013 doi: 10.1007/s11999-013-3226-x. https://doi.org/10.1007/s11999-013-3226-x PMid:23928711 PMCid:PMC3825898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Crooijmans HJ, Laumen AM, van Pul C, van Mourik JB. A new digital preoperative planning method for total hip arthroplasties. Clinical orthopaedics and related research. 2009;467(4):909–16. doi: 10.1007/s11999-008-0486-y. https://doi.org/10.1007/s11999-008-0486-y PMid:18781367 PMCid:PMC2650039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Crooijmans HJ, Laumen AM, van Pul C, van Mourik JB. A new digital preoperative planning method for total hip arthroplasties. Clinical orthopaedics and related research. 2009;467(4):909–16. doi: 10.1007/s11999-008-0486-y. https://doi.org/10.1007/s11999-008-0486-y PMid:18781367 PMCid:PMC2650039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Blackley HR, Howell GE, Rorabeck CH. Planning and management of the difficult primary hip replacement:preoperative planning and technical considerations. Instr Course Lect. 2000;49:3–11. PMid:10829157. [PubMed] [Google Scholar]
- 14.Müller ME. Lessons of 30 years of total hip arthroplasty. Clin Orthop Relat Res. 1992;274:12–21. PMid:1728996. [PubMed] [Google Scholar]
- 15.Haddad FS, Masri BA, Garbuz DS, Duncan CP. The prevention of periprosthetic fractures in total hip and knee arthroplasty. The Orthopedic clinics of North America. 1999;30(2):191–207. doi: 10.1016/s0030-5898(05)70074-2. https://doi.org/10.1016/S0030-5898(05)70074-2. [DOI] [PubMed] [Google Scholar]
- 16.Cech O, Fassbender M, Kirschner P, Rozkydal Z. [Preoperative planning and surgical technic in achieving stability and leg length equality in total hip joint arthroplasty] (in Czech) Acta Chir Orthop Traumatol Cech. 2002;69:362–368. PMid:12587498. [PubMed] [Google Scholar]
- 17.Eggli S, Pisan M, Muller ME. The value of preoperative planning for total hip arthroplasty. J Bone Joint Surg Br. 1998;80:382–390. doi: 10.1302/0301-620x.80b3.7764. https://doi.org/10.1302/0301-620X.80B3.7764 PMid:9619923. [DOI] [PubMed] [Google Scholar]
- 18.Goldstein WM, Gordon A, Branson JJ. Review Leg length inequality in total hip arthroplasty. Orthopedics. 2005;28(9 Suppl):s1037–40. doi: 10.3928/0147-7447-20050902-06. PMid:16190031. [DOI] [PubMed] [Google Scholar]
- 19.Haddad FS, Masri BA, Garbuz DS, Duncan CP. Review The prevention of periprosthetic fractures in total hip and knee arthroplasty. Orthop Clin North Am. 1999;30(2):191–207. doi: 10.1016/s0030-5898(05)70074-2. https://doi.org/10.1016/S0030-5898(05)70074-2. [DOI] [PubMed] [Google Scholar]
- 20.Woolson ST. Leg length equalization during total hip replacement. Orthopedics. 1990;13:17–21. doi: 10.3928/0147-7447-19900101-05. PMid:2300514. [DOI] [PubMed] [Google Scholar]
- 21.Suh KT, Cheon SJ, Kim DW. Comparison of preoperative templating with postoperative assessment in cementless total hip arthroplasty. Acta Orthop Scand. 2004;75:40–44. doi: 10.1080/00016470410001708070. https://doi.org/10.1080/00016470410001708070 PMid:15022804. [DOI] [PubMed] [Google Scholar]
- 22.Wedemeyer C, Quitmann H, Xu J, Heep H, von Knoch M, Saxler G. Digital templating in total hip arthroplasty with the Mayo stem. Arch Orthop Trauma Surg. 2007 doi: 10.1007/s00402-007-0494-5. [DOI] [PubMed] [Google Scholar]
- 23.Haddad FS, Masri BA, Garbuz DS, Duncan CP. The prevention of periprosthetic fractures in total hip and knee arthroplasty. Orthop Clin North Am. 1999;30:191–207. doi: 10.1016/s0030-5898(05)70074-2. https://doi.org/10.1016/S0030-5898(05)70074-2. [DOI] [PubMed] [Google Scholar]
- 24.Schmalzried TP. Preoperative templating and biomechanics in total hip arthroplasty. Instr Course Lect. 2008;57:273–9. [PubMed] [Google Scholar]
- 25.Kosashvili Y, Shasha N, Olschewski E, Safir O, White L, Gross A, et al. Digital versus conventional templating techniques in preoperative planning for total hip arthroplasty. Canadian journal of surgery Journal canadien de chirurgie. 2009;52(1):6–11. [PMC free article] [PubMed] [Google Scholar]
- 26.Scheerlinck T. Primary hip arthroplasty templating on standard radiographs. A stepwise approach. Acta orthopaedica Belgica. 2010;76(4):432–42. PMid:20973347. [PubMed] [Google Scholar]
- 27.Gorski JM, Schwartz L. A device to measure x-ray magnification in preoperative planning for cementless arthroplasty. Clin Orthop Relat Res. 1986;202:302–306. https://doi.org/10.1097/00003086-198601000-00043. [PubMed] [Google Scholar]
- 28.Oddy M, Jones M, Pendegrass C, Pilling J, Wimhurst J. Assessment of reproducibility and accuracy in templating hybrid total hip arthroplasty using digital radiographs. J Bone Joint Surg Br. 2006;88:581–585. doi: 10.1302/0301-620X.88B5.17184. https://doi.org/10.1302/0301-620X.88B5.17184 PMid:16645101. [DOI] [PubMed] [Google Scholar]
- 29.Eggli S, Pisan M, Muller ME. The value of preoperative planning for total hip arthroplasty. The Journal of bone and joint surgery British volume. 1998;80(3):382–90. doi: 10.1302/0301-620x.80b3.7764. https://doi.org/10.1302/0301-620X.80B3.7764 PMid:9619923. [DOI] [PubMed] [Google Scholar]
- 30.Kosashvili Y, Shasha N, Olschewski E, Safir O, White L, Gross A, et al. Digital versus conventional templating techniques in preoperative planning for total hip arthroplasty. Canadian journal of surgery Journal canadien de chirurgie. 2009;52(1):6–11. [PMC free article] [PubMed] [Google Scholar]
- 31.Whiddon DR, Bono JV, Lang JE, Smith EL, Salyapongse AK. Accuracy of digital templating in total hip arthroplasty. Am J Orthop (Belle Mead NJ) 2011;40(8):395–8. PMid:22016868. [PubMed] [Google Scholar]
- 32.Phillips JH, Albregts AE, Kling TF, Jr, Cohen MJ. Digital radiography in pediatric orthopaedics:a prospective, controlled, and randomized trial. Journal of pediatric orthopedics. 1994;14(3):377–80. doi: 10.1097/01241398-199405000-00020. https://doi.org/10.1097/01241398-199405000-00020 PMid:8006173. [DOI] [PubMed] [Google Scholar]
- 33.Chen B, Xiao SX, Gu PC, Lin XJ. Personalized image-based templates for precise acetabular prosthesis placement in total hip arthroplasty:a pilot study. Journal of Zhejiang University Science B. 2010;11(9):673–80. doi: 10.1631/jzus.B1000066. https://doi.org/10.1631/jzus.B1000066 PMid:20803771 PMCid:PMC2932877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mittag F, Ipach I, Schaefer R, Meisner C, Leichtle U. THA. Predictive value of preoperative digital templating in THA depends on the surgical experience of the performing physician. Int Orthop. 2012;36(9):1767–72. doi: 10.3928/01477447-20120123-14. https://doi.org/10.3928/01477447-20120123-14. [DOI] [PubMed] [Google Scholar]
- 35.Jung S, Neuerburg C, Kappe T, Wernerus D, Reichel H, Bieger R. [Validity of digital templating in total hip arthroplasty:impact of stem design and planner's experience] Zeitschrift fur Orthopadie und Unfallchirurgie. 2012;150(4):404–8. doi: 10.1055/s-0031-1298386. PMid:22753126. [DOI] [PubMed] [Google Scholar]
- 36.Mittag F, Ipach I, Schaefer R, Meisner C, Leichtle U. Predictive value of preoperative digital templating in THA depends on the surgical experience of the performing physician. Orthopedics. 2012;35(2):e144–7. doi: 10.3928/01477447-20120123-14. https://doi.org/10.3928/01477447-20120123-14. [DOI] [PubMed] [Google Scholar]
- 37.Schmidutz F, Steinbrück A, Wanke-Jellinek L, Pietschmann M, Jansson V. The accuracy of digital templating:a comparison of short-stem total hip arthroplasty andconventional total hip arthroplasty. Fottner AiJ Arthroplasty. 1995;10(4):507–13. doi: 10.1007/s00264-012-1532-7. PMid:8523011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Carter LW, Stovall DO, Young TR. Determination of accuracy of preoperative templating of noncemented femoral prostheses. The Journal of arthroplasty. 1995;10(4):507–13. doi: 10.1016/s0883-5403(05)80153-6. https://doi.org/10.1016/S0883-5403(05)80153-6. [DOI] [PubMed] [Google Scholar]
- 39.Kosashvili Y, Shasha N, Olschewski E, Safir O, White L, Gross A, et al. Digital versus conventional templating techniques in preoperative planning for total hip arthroplasty. Canadian journal of surgery Journal canadien de chirurgie. 2009;52(1):6–11. [PMC free article] [PubMed] [Google Scholar]
- 40.Jassim SS, Ingham C, Keeling M, Wimhurst JA. Digital templating facilitates accurate leg length correction in total hip arthroplasty. Acta orthopaedica Belgica. 2012;78(3):344–9. PMid:22822575. [PubMed] [Google Scholar]
- 41.Olsen M, Gamble P, Chiu M, Tumia N, Boyle RA, Schemitsch EH. Assessment of accuracy and reliability in preoperative templating for hip resurfacingarthroplasty. J Zhejiang Univ Sci B. 2010;11(9):673–680. doi: 10.1016/j.arth.2009.01.022. [DOI] [PubMed] [Google Scholar]
- 42.Crooijmans HJ, Laumen AM, van Pul C, van Mourik JB. A new digital preoperative planning method for total hip arthroplasties. Clinical orthopaedics and related research. 2009;467(4):909–16. doi: 10.1007/s11999-008-0486-y. https://doi.org/10.1007/s11999-008-0486-y PMid:18781367 PMCid:PMC2650039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Viceconti M, Lattanzi R, Antonietti B, Paderni S, Olmi R, Sudanese A, et al. CT-based surgical planning software improves the accuracy of total hip replacement preoperative planning. Medical engineering & physics. 2003;25(5):371–7. doi: 10.1016/s1350-4533(03)00018-3. https://doi.org/10.1016/S1350-4533(03)00018-3. [DOI] [PubMed] [Google Scholar]
- 44.The B, Diercks RL, van Ooijen PM, van Horn JR. Comparison of analog and digital preoperative planning in total hip and knee arthroplasties. A prospective study of 173 hips and 65 total knees. Acta orthopaedica. 2005;76(1):78–84. doi: 10.1080/00016470510030364. https://doi.org/10.1080/00016470510030364 PMid:15788312. [DOI] [PubMed] [Google Scholar]
- 45.Shaarani SR, McHugh G, Collins DA. Accuracy of digital preoperative templating in 100 consecutive uncemented total hip arthroplasties:a single surgeon series. The Journal of arthroplasty. 2013;28(2):331–7. doi: 10.1016/j.arth.2012.06.009. https://doi.org/10.1016/j.arth.2012.06.009 PMid:22854351. [DOI] [PubMed] [Google Scholar]
- 46.Bertz A, Indrekvam K, Ahmed M, Englund E, Sayed-Noor AS. Validity and reliability of preoperative templating in total hip arthroplasty using a digital templating system. Skeletal radiology. 2012;41(10):1245–9. doi: 10.1007/s00256-012-1431-4. https://doi.org/10.1007/s00256-012-1431-4 PMid:22588597. [DOI] [PubMed] [Google Scholar]
- 47.Efe T, El Zayat BF, Heyse TJ, Timmesfeld N, Fuchs-Winkelmann S, Schmitt J. Precision of preoperative digital templating in total hip arthroplasty. Acta orthopaedica Belgica. 2011;77(5):616–21. PMid:22187836. [PubMed] [Google Scholar]
- 48.Levine B, Fabi D, Deirmengian C. Digital templating in primary total hip and knee arthroplasty. Orthopedics. 2010;33(11):797. doi: 10.3928/01477447-20100924-04. https://doi.org/10.3928/01477447-20100924-04. [DOI] [PubMed] [Google Scholar]
- 49.Zhao X, Zhu ZA, Zhao J, Li MQ, Wang G, Yu DG, et al. The utility of digital templating in Total Hip Arthroplasty with Crowe type II and III dysplastic hips. International orthopaedics. 2011;35(5):631–8. doi: 10.1007/s00264-010-0991-y. https://doi.org/10.1007/s00264-010-0991-y PMid:20229268 PMCid:PMC3080488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Berstock JR, Webb JC, Spencer RF. A comparison of digital and manual templating using PACS images. Annals of the Royal College of Surgeons of England. 2010;92(1):73–4. doi: 10.1308/003588410X12518836440289a. https://doi.org/10.1308/rcsann.2010.92.1.73 PMid:20056068 PMCid:PMC3024623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Franken M, Grimm B, Heyligers I. A comparison of four systems for calibration when templating for total hip replacement with digital radiography. The Journal of bone and joint surgery British volume. 2010;92(1):136–41. doi: 10.1302/0301-620X.92B1.22257. https://doi.org/10.1302/0301-620X.92B1.22257 PMid:20044692. [DOI] [PubMed] [Google Scholar]
- 52.Gamble P, de Beer J, Petruccelli D, Winemaker M. The accuracy of digital templating in uncemented total hip arthroplasty. The Journal of arthroplasty. 2010;25(4):529–32. doi: 10.1016/j.arth.2009.04.011. https://doi.org/10.1016/j.arth.2009.04.011 PMid:19493647. [DOI] [PubMed] [Google Scholar]
- 53.Heinert G, Hendricks J, Loeffler MD. Digital templating in hip replacement with and without radiological markers. The Journal of bone and joint surgery British volume. 2009;91(4):459–62. doi: 10.1302/0301-620X.91B4.21730. https://doi.org/10.1302/0301-620X.91B4.21730 PMid:19336804. [DOI] [PubMed] [Google Scholar]
- 54.White SP, Bainbridge J, Smith EJ. Assessment of magnification of digital pelvic radiographs in total hip arthroplasty using templating software. Annals of the Royal College of Surgeons of England. 2008;90(7):592–6. doi: 10.1308/003588408X318101. https://doi.org/10.1308/003588408X318101 PMid:18831869 PMCid:PMC2728308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kulkarni A, Partington P, Kelly D, Muller S. Disc calibration for digital templating in hip replacement. The Journal of bone and joint surgery British volume. 2008;90(12):1623–6. doi: 10.1302/0301-620X.90B12.20238. https://doi.org/10.1302/0301-620X.90B12.20238 PMid:19043135. [DOI] [PubMed] [Google Scholar]
- 56.Hofmann AA, Bolognesi M, Lahav A, Kurtin S. Minimizing leg-length inequality in total hip arthroplasty:use of preoperative templating and an intraoperative x-ray. American journal of orthopedics. 2008;37(1):18–23. PMid:18309380. [PubMed] [Google Scholar]
- 57.Wimsey S, Pickard R, Shaw G. Accurate scaling of digital radiographs of the pelvis. A prospective trial of two methods. The Journal of bone and joint surgery British volume. 2006;88(11):1508–12. doi: 10.1302/0301-620X.88B11.18017. https://doi.org/10.1302/0301-620X.88B11.18017 PMid:17075099. [DOI] [PubMed] [Google Scholar]
- 58.The B, Diercks RL, van Ooijen PM, van Horn JR. Comparison of analog and digital preoperative planning in total hip and knee arthroplasties. A prospective study of 173 hips and 65 total knees. Acta orthopaedica. 2005;76(1):78–84. doi: 10.1080/00016470510030364. https://doi.org/10.1080/00016470510030364 PMid:15788312. [DOI] [PubMed] [Google Scholar]
- 59.Sugano N, Ohzono K, Nishii T, Haraguchi K, Sakai T, Ochi T. Computed-tomography-based computer preoperative planning for total hip arthroplasty. Computer aided surgery:official journal of the International Society for Computer Aided Surgery. 1998;3(6):320–4. doi: 10.1002/(SICI)1097-0150(1998)3:6<320::AID-IGS6>3.0.CO;2-O. https://doi.org/10.3109/10929089809148153 PMid:10379982. [DOI] [PubMed] [Google Scholar]
- 60.Carter LW, Stovall DO, Young TR. Determination of accuracy of preoperative templating of noncemented femoral prostheses. The Journal of arthroplasty. 1995;10(4):507–13. doi: 10.1016/s0883-5403(05)80153-6. https://doi.org/10.1016/S0883-5403(05)80153-6. [DOI] [PubMed] [Google Scholar]
- 61.White SP, Shardlow DL. Effect of introduction of digital radiographic techniques on pre-operative templating in orthopaedic practice. Annals of the Royal College of Surgeons of England. 2005;87(1):53–4. doi: 10.1308/1478708051540. https://doi.org/10.1308/1478708051540 PMid:15720909 PMCid:PMC1963834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Gonzalez Della Valle A, Comba F, Taveras N, Salvati EA. The utility and precision of analogue and digital preoperative planning for total hip arthroplasty. International orthopaedics. 2008;32(3):289–94. doi: 10.1007/s00264-006-0317-2. https://doi.org/10.1007/s00264-006-0317-2 PMid:17404731 PMCid:PMC2323429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Unnanuntana A, Wagner D, Goodman SB. The accuracy of preoperative templating in cementless total hip arthroplasty. The Journal of arthroplasty. 2009;24(2):180–6. doi: 10.1016/j.arth.2007.10.032. https://doi.org/10.1016/j.arth.2007.10.032 PMid:18534455. [DOI] [PubMed] [Google Scholar]
- 64.Goodman SB, Huene DS, Imrie S. Preoperative templating for the equalization of leg lengths in total hip arthroplasty. Contemporary orthopaedics. 1992;24(6):703–10. PMid:10149945. [PubMed] [Google Scholar]
- 65.Iorio R, Siegel J, Specht LM, Tilzey JF, Hartman A, Healy WL. A comparison of acetate vs digital templating for preoperative planning of total hip arthroplasty:is digital templating accurate and safe? The Journal of arthroplasty. 2009;24(2):175–9. doi: 10.1016/j.arth.2007.11.019. https://doi.org/10.1016/j.arth.2007.11.019 PMid:18534425. [DOI] [PubMed] [Google Scholar]
- 66.Bayne CO, Krosin M, Barber TC. Evaluation of the accuracy and use of x-ray markers in digital templating for total hip arthroplasty. The Journal of arthroplasty. 2009;24(3):407–13. doi: 10.1016/j.arth.2007.11.020. https://doi.org/10.1016/j.arth.2007.11.020 PMid:18534424. [DOI] [PubMed] [Google Scholar]
- 67.Whiddon DR, Bono JV. Digital templating in total hip arthroplasty. Instructional course lectures. 2008;57:273–9. PMid:18399591. [PubMed] [Google Scholar]
- 68.Baxter JA, Barlow T, Karthikeyan S, Mayo DJ, King RJ. The accuracy of automatic calibration of digital pelvic radiographs using two different scale markers:a comparative study. Hip international:the journal of clinical and experimental research on hip pathology and therapy. 2012;22(1):82–9. doi: 10.5301/HIP.2012.9044. https://doi.org/10.5301/HIP.2012.9044 PMid:22344481. [DOI] [PubMed] [Google Scholar]
- 69.King RJ, Makrides P, Gill JA, Karthikeyan S, Krikler SJ, Griffin DR. A novel method of accurately calculating the radiological magnification of the hip. The Journal of bone and joint surgery British volume. 2009;91(9):1217–22. doi: 10.1302/0301-620X.91B9.22615. https://doi.org/10.1302/0301-620X.91B9.22615 PMid:19721050. [DOI] [PubMed] [Google Scholar]
- 70.Alnahhal A, Sharma S, Hafez M, Tim Board. Accuracy of a new method of pelvic radiograph calibration:An independent comparative study. Med Eng Phys. 2003;25(5):371–7. [Google Scholar]


