Abstract
Background
Primary cardiac lymphoma (PCL) is a very rare disease and is most commonly found among immunocompromised patients. Its cardiac manifestations are non-specific, leading to delayed diagnosis and poor prognosis. However, chemotherapy could improve survival, which makes early and prompt diagnosis very crucial. This is a report of a rare case of PCL found on a 73-year-old man who benefit from early debulking surgery.
Case Summary
A 73-year-old man presented with worsening dyspnoea over the last 2 months. A 7.2 × 10.2 cm intramural tumour was found extending from the right atrium to the right ventricle. It was considered that the tumour could cause sudden death due to its size and extension. Therefore, surgical debulking with biopsy and valve repair was done. Cytology examination from the resected specimen demonstrated diffuse large B-cell lymphoma non-germinal centre B-cell like type. He was discharged 2 weeks after the surgery in stable condition and referred to internal medicine department for chemotherapy. However, he chose palliative home care and died 44 days after surgery.
Discussion
In cases of PCL with concerning tumour size and symptoms due to cardiac obstruction, early surgical debulking could improve haemodynamics, prevent sudden death, and confirm immunopathological diagnosis needed in determining further chemotherapy, which is proven to improve survival.
Keywords: Case report, Cardiac tumour, Primary cardiac lymphoma, Cardiac surgery, Surgical debulking
Learning points
Early diagnosis is crucial in primary cardiac lymphoma (PCL) cases as its non-specific symptoms often lead to delayed diagnosis and poor prognosis.
Early surgical debulking should be considered to improve symptoms, prevent sudden death, and confirm diagnosis in PCL cases with concerning tumour size and symptoms due to cardiac obstruction.
Introduction
Primary cardiac lymphoma (PCL) is extra-nodal lymphoma involving only the heart and/or the pericardium.1 It is rare, accounting only for 1.6% of malignant cardiac tumours which only account for 30% of cardiac tumours.2 Primary cardiac lymphoma is more commonly found among immunocompromised patients with median age of 63 years and male predominance. Its non-specific cardiac manifestations often lead to delayed diagnosis and poor prognosis.3,4
Timeline
| Time | Events |
|---|---|
| 2 months ago | The patient developed worsening dyspnoea on exertion |
| 1 month ago | Patient lost weight (10 kg) |
| 1 week ago | Patient had two episodes of syncope |
| Admission | Patient presented with worsening dyspnoea on exertion for 2 months. Transthoracic echocardiography showed intracardiac tumour extending from the right atrium to the right ventricle making tricuspid valve (TV) hard to evaluate, mild mitral and aortic regurgitation, mild aortic stenosis, and large pericardial effusion with preserved ejection fraction. A 12 lead electrocardiography showed left axis deviation, low QRS voltage in lead V1–V2, 1st grade atrioventricular (AV) block, and P mitrale. Multi slice computed tomography coronary angiogram showed four-vessel cardiovascular disease, intramural tumour at right AV region affecting the TV, right coronary artery irregularity, multiple mediastinal lymphadenopathy on stations 4L, 5, and 6, and pericardial effusion. |
| Day 6 | Surgical biopsy, debulking, and TV repair was performed |
| Day 20 | Patient was discharged for further oncological treatment, but later decided to choose palliative home care instead |
| Day 50 | Patient passed away |
Case summary
A 73-year-old man presented with worsening dyspnoea on exertion for 2 months. No orthopnoea was reported. He also had lost 10 kg of body weight and had two episodes of syncope. He had no history of smoking. There was no complaint of fever, night sweats, chronic cough, or chest pain. Previous lung disease was denied.
Patient had history of stroke 4 years before. He also had three-vessel cardiovascular disease, Type 2 diabetes mellitus, and hypertension since 3 years before. He had undergone catheterization and was regularly consuming aspirin, metformin, bisoprolol, candesartan, and atorvastatin.
Physical examinations showed muffled heart sounds and pansystolic murmur at mitral valve. Complete blood count showed anaemia with Hb of 11.7 g/dL (13.0–16.0) slight leucocytosis with leucocyte of 10.210 × 103/μL (5–10), and erythrocyte sedimentation rate of 12 mm/h (0–20). Blood glucose was 162 mg/dL (<140) and HbA1c was 6.3% (<5.6). Anti-HIV test result was negative.
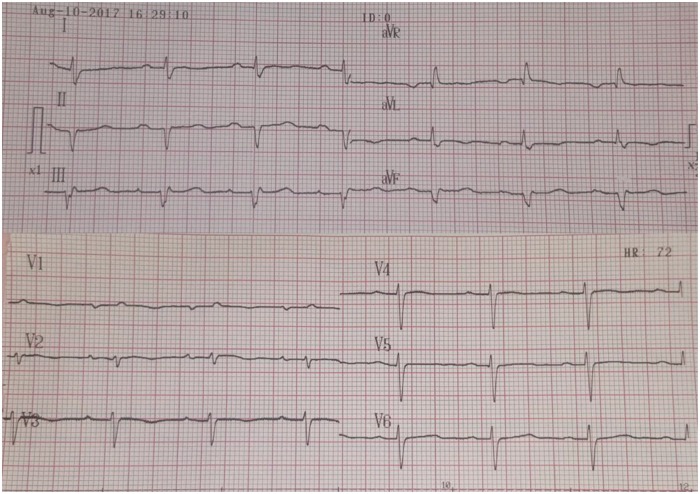
A 12 lead electrocardiogram showed left axis deviation and low QRS voltage in lead V1–V2 with first grade atrioventricular (AV) block and P mitrale (Figure 1).
Figure 1.
Preoperative electrocardiogram showing left axis deviation, low QRS voltage in V1–V2, 1st grade atrioventricular block, and P mitrale.
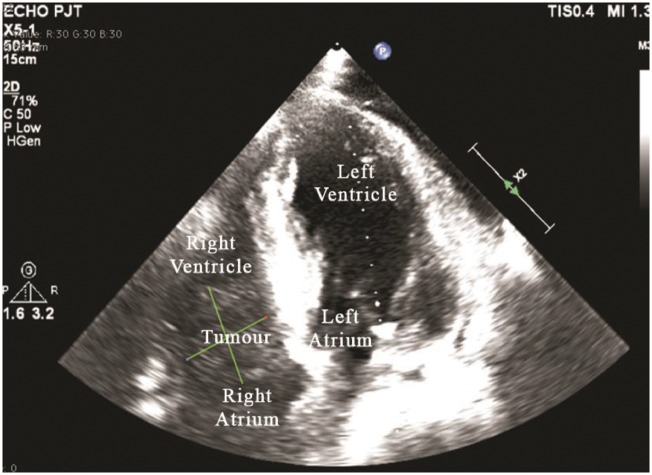
Chest radiograph revealed cardiomegaly and elongated, calcified aorta. Transthoracic echocardiography showed sessile intracardiac tumour extending from the right atrium to the right ventricle (RV), causing blood flow through tricuspid valve (TV) hard to evaluate (Figure 2). There were mild mitral (MR) and aortic regurgitation (AR), mild aortic stenosis, and large pericardial effusion (21.6 mm). However, the effusion was not haemodynamically significant. There was no ventricular or atrial collapse, no apparent transmitral respiratory variation, and the ejection fraction was preserved (ejection fraction 59.1%).
Figure 2.
Echocardiography showing tumour extending from right atrium to right ventricle through the tricuspid valve.
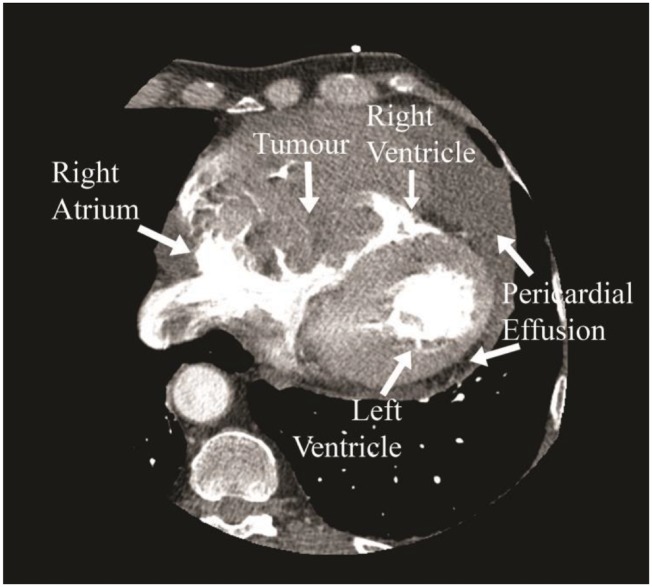
Multi slice computed tomography coronary angiogram showed calcified plaque in left anterior descending artery, right coronary artery, left main coronary artery, and left circumflex artery. A 7.2 × 10.2 cm intramural tumour with tissue density and a few necrotic areas were seen at right AV region, affecting the TV and dominantly protruding intracavitary to the atrium area (Figure 3) with visible right coronary artery irregularity, without extension to the superior vena cava or inferior vena cava. Multiple lymphadenopathy on stations 4L, 5, and 6, and pericardial effusion (25 mm) were also seen. To investigate for other tumour or metastases, abdominal CT scan was done but showed no other tumour. No other examination was done.
Figure 3.
Multi slice computed tomography showing a tumour at right atrioventricular region.
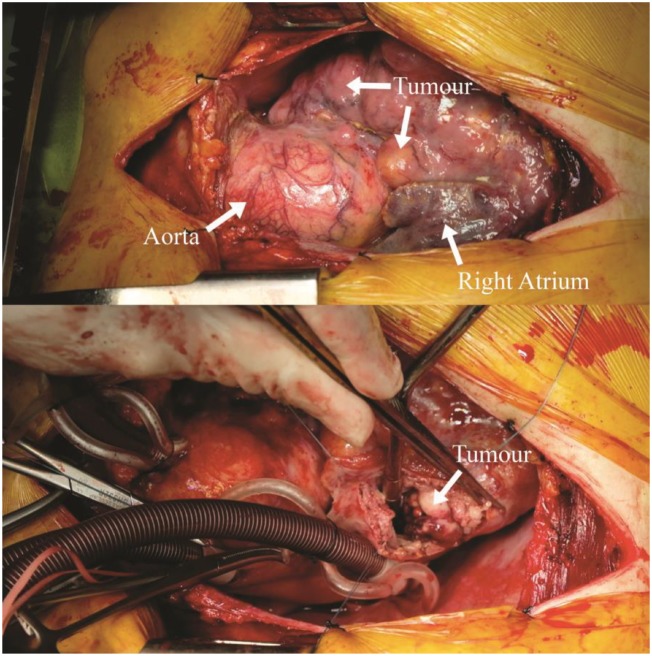
Our team decided to do surgical debulking and biopsy. After mid sternotomy, cardiopulmonary bypass machine was established. Right atrium was opened and a globular, yellowish white tumour with unclear border which did not bleed easily was seen (Figure 4). Debulking was performed until the TV became visible. The annulus appeared dilated and the chordae were ruptured. Valve repair was done using anterior-septal commisuroplasty and De Vega's procedure.
Figure 4.
Intraoperative pictures of the tumour.
Post-operative transoesophageal echocardiography showed leftover tumour on septal area of the RV. Opening of TV was good with mean pressure gradient of 0.5 mmHg and maximum velocity of 54.2 cm/s. There was no stenosis, but a mild tricuspid regurgitation (TR), AR, and MR were found.
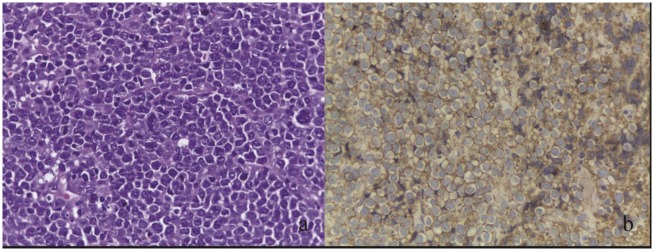
Histopathology and immunohistochemistry examination of the resected specimen demonstrated diffuse large B-cell lymphoma (DLBCL) non-germinal centre B-cell like type, which were Ki67 90% positive for CD3, CD20, MUM1, BCL6, and negative for CD10, BCL2, TdT (Figure 5A and B). According to the Ann Arbor staging of non-Hodgkin lymphomas, the patient was classified as stage IV-B DLBCL.
Figure 5.
(A) Histopathology revealed round, uniform tumour cells with coarse chromatin by haematoxylin and eosin stain and (B) immunostaining showed CD20+ neoplastic lymphoid cells.
The patient was moved to the intensive care unit and extubated after 2 days. No dyspnoea was reported. Two weeks after surgery, he was discharged in stable condition and referred to internal medicine department for chemotherapy. Unfortunately, data from the internal medicine department showed that the patient refused further treatment and chose palliative home care instead. He died 44 days after surgery.
Discussion
Primary cardiac lymphoma is a rare malignant cardiac tumour, which is more commonly found among immunocompromised patients with male predominance and usually affects the right chambers of the heart.3,4 These characteristics correspond with our patient's. The non-specific cardiac manifestations of PCL often lead to delayed diagnosis and poor prognosis.3,4 Therefore, early diagnosis is crucial.
Due to the tumour's size and extension, our team that consisted of cardiologist, cardiac surgeons, and oncologist decided to do surgical debulking, as debulking has shown to improve haemodynamics and prevent sudden death due to arrhythmia or tumour emboli.5 The surgery successfully improved our patient's symptoms and diagnosis of DLBCL was confirmed through histology examination of the resected specimen.
To improve patient's prognosis, chemotherapy with main regimen of cyclophosphamide, doxorubicin, vincristine, and prednisone could be used, while total surgical resection for PCL is difficult and is not proven to increase patient's survival3,4,6 Therefore, we referred our patient to the internal medicine department for further oncologic therapy.
Conclusion
Primary cardiac lymphoma is a rare disease. Its unspecific symptoms and poor prognosis make early diagnosis crucial. In cases of PCL with concerning tumour size and symptoms due to cardiac obstruction, early surgical debulking should be considered as a method to improve haemodynamics, prevent sudden death, and confirm immunopathological diagnosis needed in determining further chemotherapy which is proven to improve survival.
Acknowledgements
The authors would like to thank Ismail Dilawar for his contributions to this case report.
Slide sets: A fully edited slide set detailing this case and suitable for local presentation is available online as Supplementary data.
Consent: The author/s confirm that written consent for submission and publication of this case report including image(s) and associated text has been obtained from the patient in line with COPE guidance.
Conflict of interest: none declared.
Supplementary Material
References
- 1. Travis WD, Marx A, Brambilla E, Nicholson A, Burke A.. WHO Classification of Tumours of the Lung, Pleura, Thymus and Heart. Lyon: IARC; 2015. p340–1. [DOI] [PubMed] [Google Scholar]
- 2. Amano J, Nakayama J, Yoshimura Y, Ikeda U.. Clinical classification of cardiovascular tumors and tumor-like lesions, and its incidences. Gen Thorac Cardiovasc Surg 2013;61:435–447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Miguel CE, Bestetti RB.. Primary cardiac lymphoma. Int J Cardiol 2011;149:358–363. [DOI] [PubMed] [Google Scholar]
- 4. Petrich A, Cho SI, Billett H.. Primary cardiac lymphoma an analysis of presentation, treatment, and outcome patterns. Cancer 2011;117:581–589. [DOI] [PubMed] [Google Scholar]
- 5. Habertheuer A, Ehrlich M, Wiedemann D, Mora B, Rath C, Kocher A.. A rare case of primary cardiac B cell lymphoma. J Cardiothorac Surg 2014;9:14.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Yanase Y, Yamauchi A, Uehara M, Tachibana K, Muraki S, Takagi N, Higami T.. Surgical resection of primary cardiac lymphoma presenting as a huge mass: report of two cases. Gen Thorac Cardiovasc Surg 2012;60:494–497. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.