Abstract
This study aims to compare the impact of early and late post-discharge cardiopulmonary rehabilitation on the outcomes of intensive care unit (ICU) survivors.
The retrospective, cohort study used a sub-database of the Taiwan National Health Insurance Research Database (NHIRD) that contained information of all patients had ICU admission between 2000 and 2012. Early group was defined if patients had received cardiopulmonary rehabilitation within 30 days after ICU discharge, and late group was define as if patients had received cardiopulmonary rehabilitation between 30 days and 1 year after ICU discharge. The end points were mortality and re-admission during the 3-year follow-up.
Among 2136 patients received cardiopulmonary rehabilitation after ICU discharge, 994 was classified early group and other 1142 patients were classified as late group. Overall, early group had a lower mortality rate (6.64% vs. 10.86%, P = .0006), and a lower ICU readmission rate (47.8% vs. 57.97%, P < 0.0001) than late group after 3-year follow-up. Kaplan-Meier analysis showed that early group had significantly lower mortality (P = .0009) and readmission rate (P < .0001) than late group. In multivariate analysis, the risk of ICU readmission was found to be independently associated with late group (hazard ratio, [HR], 1.28; 95% confidence intervals, [CI], 1.13–1.47).
Early post-discharge cardiopulmonary rehabilitation among ICU survivors has the long-term survival benefit and significantly decreases the readmission rate.
Keywords: early cardiopulmonary rehabilitation, intensive care unit, mortality, readmission
Key points
Among patients received cardiopulmonary rehabilitation after ICU discharge, early group (within 30 days after ICU discharge) had a lower mortality and ICU readmission rate than late group (between 30 days and 1 year after ICU discharge) after 3-year follow-up.
After multivariate analysis, the risk of ICU readmission was found to be independently associated with late group
Early post-discharge cardiopulmonary rehabilitation among ICU survivors has the long-term survival benefit and significantly decreases the readmission rate.
1. Introduction
Intensive care unit (ICU) is an important place for resuscitation and saving life of critically ill patients. However, the process of critical care during ICU stay may also bring several complications, such as nosocomial infections, ventilator-associated lung injury, adverse drug effects, venous thromboembolism, delirium, and stress ulcers related gastrointestinal tract bleeding.[1–3] Even for the patients with survive after ICU discharges, some of patients may be left with exercise limitation, physical disability, psychological dysfunction, and decreased physical quality of life for a long time.[4–7] Moreover, these functional disabilities and impairment of physical performance due to muscle wasting and sarcopenia are associated with mortality.[8–11]
To decrease the negative impact of muscle wasting and functional disability after ICU discharge, rehabilitation may be a resolution for this clinical problem. For stroke patients, cardiorespiratory and mixed training, involving walking, within post-stroke rehabilitation programs was demonstrated to improve the functional activity.[12] For patients with chronic obstructive pulmonary disease, supervised exercise programs after primary pulmonary rehabilitation is more effective than usual care for preserving exercise capacity than usual care.[13] For the patients receiving coronary artery bypass graft surgery, 10-year all-cause mortality can be reduced after cardiac rehabilitation.[14] For ICU survivors of sepsis, the long term outcome can be improved by post-discharge rehabilitation.[15] For critically ill patients in ICU, inpatients Physical therapy can improve the short-term outcomes – including improving quality of life, physical function, enhancing muscle strength, increasing decreasing ventilator-free days, and decreasing length of stay in ICU and hospital.[16] However, the appropriate timing of introducing rehabilitation program for ICU patients remains unclear. Most of studies focus on the early rehabilitation for the critically ill patients during ICU stay, and the effect seems to be controversy.[17–19] In this study, we hypotheses that the ICU survivor would be in a relative stable status and cardiopulmonary rehabilitation in the early stage after ICU discharge may provide some benefit. Thus, this study is conducted to compare the effect of early and late post-discharge cardiopulmonary rehabilitation on the outcomes of ICU survivors.
2. Methods
2.1. Data source
The retrospective, cohort study used a sub-database of the Taiwan National Health Insurance Research Database (NHIRD) that contains information of all patients had ICU admission between 2000 and 2012. Detailed information including outpatient and inpatient medical care, diagnoses, surgical procedures, and prescribed medications for each insured patient was obtained, including diagnostic codes according to the clinical modification of the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) code. The study was approved by the Institutional Review Board (IRB) at Chi Mei Medical Center. The data used in this study are de-identified, and released to the public for research purposes; therefore, the IRB waived informed consent from the enrolled patients (IRB no: 10707-E01).
2.2. Patient selection
Throughout the study period, a total of 49,185 patients with ICU admission ever received cardiopulmonary rehabilitation. If patients had multiple ICU admissions, we only enrolled the first time ICU admission. Overall, there were 2136 patients received rehabilitation of cardiopulmonary training after ICU discharge. The cardiopulmonary rehabilitation was identified from the claiming medical expenditure claim applications. Among them, 994 patients had received cardiopulmonary rehabilitation within 30 days after ICU discharge, and were classified as early group. Another 1142 patients had received cardiopulmonary rehabilitation between 30 days and 1 year after ICU discharge, and were classified as late group (Fig. 1).
Figure 1.
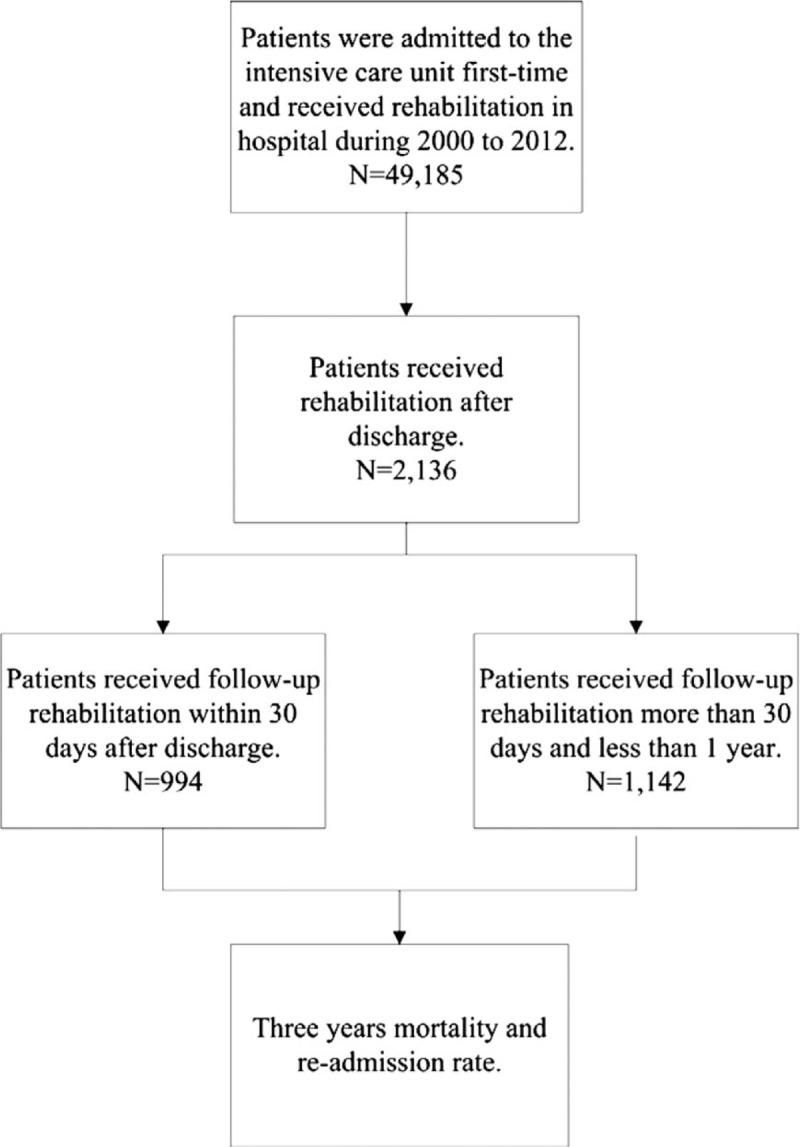
Flow chart of patient selection.
2.3. Baseline variables and outcome measurement
Demographic and clinical characteristics, including age, gender, comorbidities, and Charlson Comorbidity Index (CCI) score, length of ICU stay were collected. The comorbidities, including of chronic obstructive pulmonary diseases (COPD; ICD-9-CM: 490–496), diabetes mellitus (DM; ICD-9-CM: 250), dementia (ICD-9-CM: 290, 294, 331), congestive heart failure (ICD-9-CM: 428), cerebrovascular disease (ICD-9-CM: 430–438), myocardial infarction (ICD-9-CM: 410–412), and malignancy (ICD-9-CM: 140–208), was defined as the records from one-year before the date of ICU admission. The end points were mortality and re-admission during the 3-year follow-up.
2.4. Statistical analyses
The baseline characteristics, including age, gender, comorbidities, group of CCI score, length of ICU stay, and outcomes (mortality and ICU readmission), are presented as frequency with percentage, and the differences between early and late cardiopulmonary rehabilitation were evaluated using Pearson χ2 test for these categorical variables. Kaplan-Meier curves were used to plot the cumulative incidence rates of mortality and ICU readmission among study subjects, and a log-rank test was used to compare the risk differences between early and late cardiopulmonary rehabilitation. In addition, the relative risk ratio of mortality and ICU readmission between the patients receiving cardiopulmonary training rehabilitation post-ICU discharge within 30 days and more than 30 days within 1-year during the follow-up period was estimated using Cox proportional hazard regression. SAS 9.4 (SAS Institute, Cary, NC) was used for all statistical analyses. Significance was set at P < .05 (2-sided). Kaplan-Meier curves were plotted using Stata 12 (Stata Corp., College Station, TX).
3. Results
3.1. Comparison between early and late rehabilitation groups
Among 2136 patients received cardiopulmonary rehabilitation after ICU discharge, 994 received early rehabilitation within 30 days after discharge, and other 1142 patients receive late rehabilitation between 30 days and 1 year after discharge (Fig. 1). Table 1 summarized their demographics and clinical characteristics. The distribution of age was different between early and late group (P = .0164). Early group had less COPD, CHF, cerebrovascular disease, and malignancy than late group. In contrast, early group had more myocardial infarction than late group. Early group also had higher rate of ICU stay <15 days, and fewer patients with CCI > 2. Overall, early group had a lower mortality rate (6.64% vs. 10.86%, P = .0006), and a lower ICU readmission rate (47.8% vs. 57.97%, P < .0001) than late group. Late group had a longer length of ICU stay than early rehabilitation group (P < .0001).
Table 1.
Demographics and clinical characteristics of patients with rehabilitation after ICU discharge.
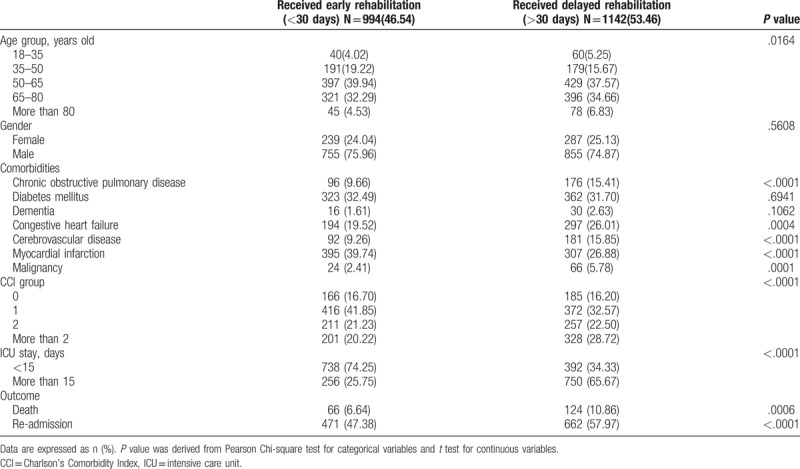
Table 2.
Risk factor of 3-year mortality in patients with rehabilitation after ICU discharge.
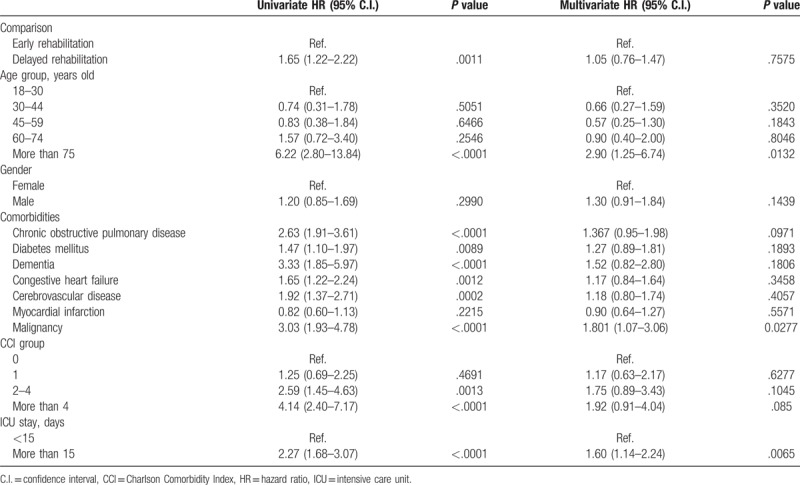
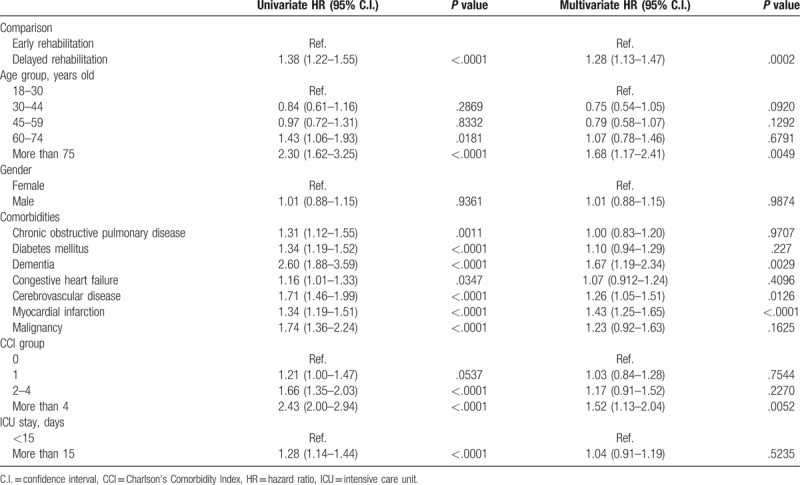
Table 3.
Risk factor of readmission in patients with rehabilitation after ICU discharge.
3.2. Risk of mortality
Using univariate analysis, late group was associated with higher risk of mortality than early group (hazard ratio, [HR], 1.65, 95% CI, 1.22–2.22). Kaplan-Meier analysis showed that early group had a lower mortality rate than late rehabilitation (P = .0009) (Fig. 2). Patients older than 75 years had higher mortality than the patients younger than 30 years (HR, 6.22; 95% confidence intervals, [CI], 2.80–13.84). Patients with COPD, DM, dementia, CHF, cerebrovascular and malignancy had higher risk of mortality than patients without underlying comorbidity (all P < .005). Patients had CCI scores more than 2 had higher risk of mortality than the patients with CCI score of 0. Patients with length of ICU stay more than 15 days had higher risk of death than those with less than 15 days (HR, 2.27, 95% CI, 1.68–3.07). After multivariate analysis, the risk of mortality was found to be independently associated with old age (≥75 yeas) (HR, 2.90; 95% CI, 1.25–6.74), malignancy (HR, 1.80; 95% CI, 1.07–3.06), and prolong ICU stay (more than 15 days) (HR, 1.60; 95% CI, 1.14–2.24).
Figure 2.
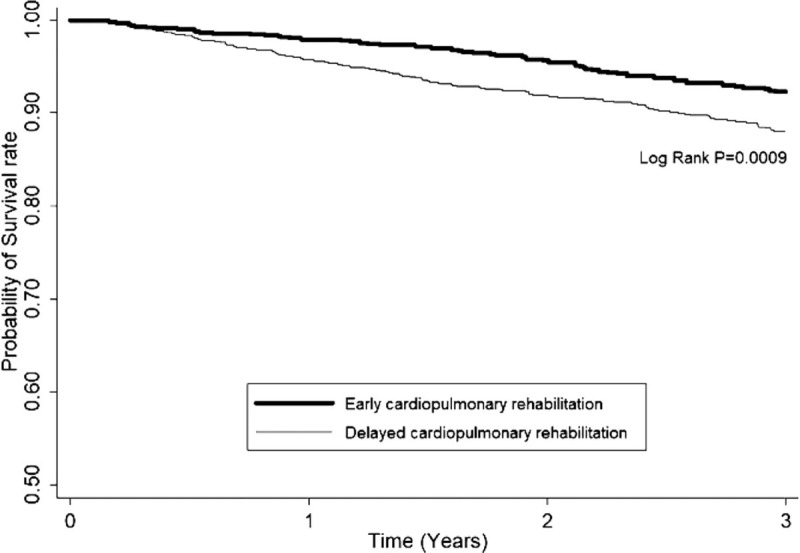
Probability of survival rate among early and later rehabilitation group.
3.3. Risk of ICU readmission
Using univariate analysis, late group was associated with a higher risk of ICU readmission than early group (HR, 1.38, 95% CI, 1.22–1.55). Kaplan-Meier analysis showed that early rehabilitation group had a lower ICU readmission rate than late rehabilitation (P < .0001) (Fig. 3). Patients older than 60 years had a higher risk of ICU readmission than the patients younger than 30 years. Patients with COPD, DM, dementia, CHF, cerebrovascular, myocardial infraction, and malignancy had a higher risk of readmission than patients without underlying comorbidity (all P < .05). Patients had CCI scores more than 2 had a higher risk of readmission than the patients with CCI score of 0. Patients with length of ICU stay more than 15 days had a higher risk of ICU readmission than those with less than 15 days (HR, 2.27, 95% CI, 1.68–3.07). After multivariate analysis, the risk of ICU readmission was found to be independently associated with late rehabilitation (HR, 1.28; 95% CI, 1.13–1.47), old age (≥75 yeas) (HR, 1.68; 95% CI, 1.17–2.41), dementia (HR, 1.67; 95% CI, 1.19–2.34), cerebrovascular disease (HR, 1.26; 95% CI, 1.05–1.51), myocardial infraction (HR, 1.43, 95% CI, 1.25–1.65), and higher CCI scores (>4) (HR, 1.52; 95%, 1.13–2.04).
Figure 3.
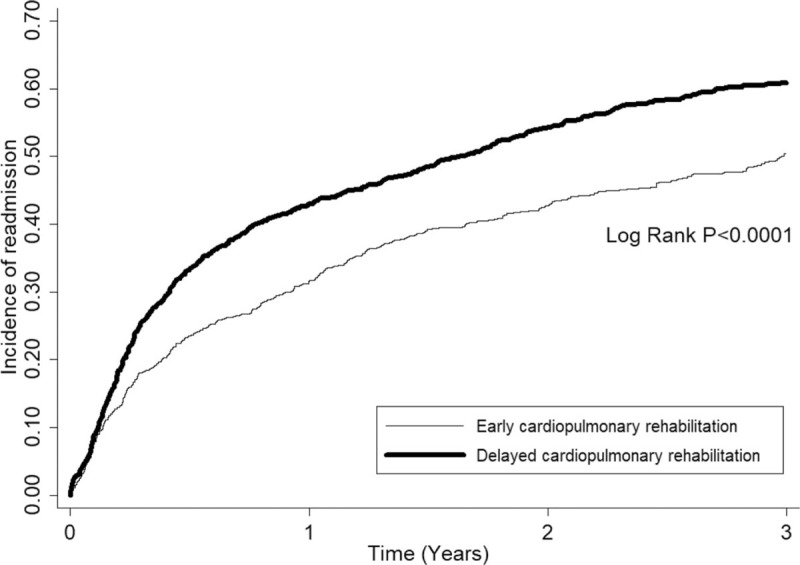
Cumulative incidences of readmission among early and later rehabilitation group.
4. Discussion
This study is the first population-based nationwide study to compare the effect of early and late post-discharge cardiopulmonary rehabilitation on the outcomes of ICU survivors. The results showed that early cardiopulmonary rehabilitation within 30 days post-discharge might decrease 3-year mortality and significantly decreased the readmission rate. Besides, the effect remained constant among some subgroups, as age >75 years, cancers co-morbidity and ICU stays >15 days had a survival benefit, and those whose age >75 years, co-morbidities of stroke and myocardial infarction and CCI > 4 had a less hospital readmission. While the critically ill patients survive discharge from ICU, they should just begin recovering from the energy loss, muscle weakness, and physical inactivity.[5,6] Thus, rehabilitation should be important for these patients. In a randomized controlled trial, Jones et al showed rehabilitation after critical illness can help improve Short-Form Health Survey physical function scores at 8 weeks and 6 months (P = .006).[20] Another study[15] showed that post-ICU discharge rehabilitation for the ICU survivor of sepsis was associated with a 5.6% risk reduction in mortality. In this study, we found that early rehabilitation for these patients can provide more outcome benefit than late rehabilitation, and it further expands our understanding of post-ICU discharge rehabilitation in terms of timing.
It is well known that patient compliance with post-discharge rehabilitation is lower than compliance in the ICU or other hospital wards, and early post-discharge rehabilitation may break this vicious cycle of functional disability and post-critical mortality by improving muscle strength and functional activity.[21] A recent systematic review and meta-analysis of hospital based inpatient geriatric rehabilitation, including exercise training, demonstrated that rehabilitation strategies cannot only restore functioning but also prevent disabilities.[22] Within 12 months of hospital discharge, Davidson et al reported elderly patients had lower hospital readmission rates in the rehabilitation group (relative risk: 0.63).[23] Besides, Chao et al displayed that critical ill survivors aged between 60 and 80 years with post-discharge rehabilitation had a lower mortality.[15] Our study also showed age >75 with early post-discharge rehabilitation had significantly lower mortality and readmission.
Clinical practice guidelines recommend rehabilitation evaluation and treatment as soon as possible after hospital admission.[24] Freburger et al found that compared to those who received no therapy, individuals who received rehabilitation in the first 30 days after discharge home after stroke were less likely to be readmitted to the hospital in the subsequent 30 days.[25] The present study displayed that early post-discharge rehabilitation among ICU survivors with stroke could prevent further readmission.
Shannon et al described that 1569 Cardiac rehabilitation participants after hospital discharge had lower all-cause readmission (HR 0.75), cardiovascular readmission (HR 0.80), non-cardiovascular readmission (HR 0.72), and mortality (HR 0.58) risk, and most of them (>90%) received rehabilitation program within 30 days.[26] Our study also displayed early post-discharge rehabilitation could decrease readmission among patients with myocardial infarction.
As cancer survivorship is increasing, but physical, cognitive and emotional sequelae post life-saving treatments often leave people with activity and participation limitations. Hauken et al displayed a rehabilitation program tailored for cancer patients seemed to build positive health outcomes and physical capacity in a long-term perspective.[27] Our study also evidenced a survival benefit of early rehabilitation for critically ill survivors with cancer.
A study on rehabilitation cohort comprised 15,535 ICU sepsis survivors received post-discharge rehabilitation within 3 months showed that CCI > 3, ICU stays ≥7 days and hospital stays ≥21 days significantly decreased the risk of mortality relative to the control cohort.[15] Our study also showed that early post-discharge rehabilitation had a significant mortality reduction among patients with ICU stay more than 15 days, and also had a lower readmission rate among those who had a CCI > 4.
Our findings can be explained by several mechanisms. First, cardiovascular and respiratory failures are the most common dysfunctional organs in ICUs; therefore, cardiopulmonary rehabilitation can help recovery of the patients just survived through the critical illness. Second, cardiopulmonary rehabilitation has been proven its effect in improving ventilator efficiency and VO2 kinetics for patients with coronary artery disease,[28] in enhancing functional capacity, and quality of life for patients with heart failure,[29] in relieving dyspnea and improving exercise capacity for patients with chronic obstructive pulmonary diseases.[30,31] Third, the time frame of introducing rehabilitation is post-ICU discharge, not in the acute stage in the ICU. Thus, the concern about wasting patients’ energy against the disease, increasing risk of rehabilitation associated side effect in the unstable conditions, frequent interruption of rehabilitation due to many examinations and treatment in the ICU,[32] may be minimized.
4.1. Study strength and limitations
Our study has some strength. This is the first study with a 12-year nationwide cohort survey to investigate whether early post-discharge rehabilitation is associated with improved long-term survival and decreased hospital re-admission in ICU survivors. Additionally, this study has several limitations. First, from the NHIRD database, we cannot obtain the data of patients’ physical performance, muscle strength, functional status, and quality of life. We just can measure the definite and solid outcomes, such as all-cause mortality and readmission. Second, we cannot avoid selection bias. The implementation of rehabilitation program depends on the physicians’ judgement and patient's clinical condition. Therefore, we did not try to compare the outcome of patients with or without rehabilitation. In addition, we choose the post-ICU discharge stage for study. In this study, these ICU survivors should recover from the acute stage and remain in a relative stable status. Thus, the effect of selection bias can be minimized. Third, this study is not randomized controlled trial, so we cannot perfectly match the each study group. However, our findings are based on the real world's situation, and can be generalized to other hospitals. Finally, this was an observational study. We observed that patients who underwent cardiopulmonary rehabilitation <30 days from hospital discharge had lower mortality and lower readmission rates, but there is not enough data to determine cause or effect. Specifically, the factors that led to some patients receiving rehabilitation <30 days remain unknown and include the possibility that patients with higher severity of illness (higher CCI, longer ICU stay) were not considered by their doctors to be appropriate candidates for cardiopulmonary rehabilitation within 30 days after hospital discharge.
5. Conclusions
The present study showed that early post-discharge (within 30 days) rehabilitation among ICU survivors might have the long-term survival benefit and significantly decreases the readmission rate. Elderly, more co-morbidities (including cancer, stroke, and myocardial infarction) and longer ICU stays may be a target subpopulation likely to benefit most from post-discharge rehabilitation.
Acknowledgments
We thank the staff of the Taiwan Bureau of National Health Insurance, Bureau of Health Promotion, and Department of Health. This research was funded by grant CMFHR10788 from Chi-Mei Medical Center.
Author contributions
C.M. Chen, Willy Chou and K.C. Cheng is the guarantor of this manuscript, C.M. Chao, C.C. Lai, C.H. Ho and C.M. Chen contributed to the conception and design of the study, A.C. Cheng and C.H. Ho analysed and interpreted the data, C.C. Lai and C.M. Chen drafted the manuscript.
Conceptualization: Chih-Cheng Lai, Willy Chou, Chien-Ming Chao, Kuo-Chen Cheng, Chin-Ming Chen.
Data curation: Chih-Cheng Lai, Ai-Chin Cheng, Kuo-Chen Cheng, Chin-Ming Chen.
Formal analysis: Chung-Han Ho.
Investigation: Willy Chou, Chien-Ming Chao, Kuo-Chen Cheng.
Supervision: Kuo-Chen Cheng.
Writing – original draft: Chih-Cheng Lai.
Writing – review & editing: Chih-Cheng Lai, Chin-Ming Chen.
Footnotes
Abbreviations: CCI = Charlson Comorbidity Index, CI = confidence intervals, COPD = chronic obstructive pulmonary diseases, DM = diabetes mellitus, HR = hazard ratio, ICD-9-CM = International Classification of Diseases, Ninth Revision, Clinical Modification, ICU = intensive care unit, IRB = Institutional Review Board, NHIRD = National Health Insurance Research Database.
C-CL, WC and A-CC have contributed equally to this work.
This study was approved by the Institutional Review Board (IRB) at Chi Mei Medical Center. The data used in this study are de-identified, and released to the public for research purposes; therefore, the IRB waived informed consent from the enrolled patients (IRB no: 10707-E01). Also see attached file.
Informed consent has been obtained from all participants included in the analyzed studies, and the studies are being conducted in accordance with the Declaration of Helsinki.
All data generated or analysed during this study are included in this published article. The study used a sub-database of the Taiwan National Health Insurance Research Database-104–391 (NHIRD-104–391) that contains information of all patients had ICU admission between 2000 and 2012.
This research was funded by grant CMFHR10788 from Chi Mei Medical Center.
The authors declare that they have no conflicts of interests to disclose.
References
- [1].Wollschlager CM, Conrad AR, Khan FA. Common complications in critically ill patients. Dis Mon 1988;34:221–93. [DOI] [PubMed] [Google Scholar]
- [2].Kuchnicka K, Maciejewski D. Ventilator-associated lung injury. Anaesthesiol Intensive Ther 2013;45:164–70. [DOI] [PubMed] [Google Scholar]
- [3].Jones SF, Pisani MA. ICU delirium: an update. Curr Opin Crit Care 2012;18:146–51. [DOI] [PubMed] [Google Scholar]
- [4].Desai SV, Law TJ, Needham DM. Long-term complications of critical care. Crit Care Med 2011;39:371–9. [DOI] [PubMed] [Google Scholar]
- [5].Herridge MS, Tansey CM, Matte A, et al. Functional disability 5 years after acute respiratory distress syndrome. N Engl J Med 2011;364:1293–304. [DOI] [PubMed] [Google Scholar]
- [6].Iwashyna TJ, Ely EW, Smith DM, et al. Long-term cognitive impairment and functional disability among survivors of severe sepsis. JAMA 2010;304:1787–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Hopkins RO, Jackson JC. Long-term neurocognitive function after critical illness. Chest 2006;130:869–78. [DOI] [PubMed] [Google Scholar]
- [8].Strandberg TE, Stenholm S, Strandberg AY, et al. The “obesity paradox,” frailty, disability, and mortality in older men: a prospective, longitudinal cohort study. Am J Epidemiol 2013;178:1452–60. [DOI] [PubMed] [Google Scholar]
- [9].Roshanravan B, Robinson-Cohen C, Patel KV, et al. Association between physical performance and all-cause mortality in CKD. J Am Soc Nephrol 2013;24:822–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Arango-Lopera VE, Arroyo P, Gutierrez-Robledo LM, et al. Mortality as an adverse outcome of sarcopenia. J Nutr Health Aging 2013;17:259–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Montano-Loza AJ, Meza-Junco J, Prado CM, et al. Muscle wasting is associated with mortality in patients with cirrhosis. Clin Gastroenterol Hepatol 2012;10: 166-173, 173 e161. [DOI] [PubMed] [Google Scholar]
- [12].Saunders DH, Sanderson M, Hayes S, et al. Physical fitness training for stroke patients. Cochrane Database Syst Rev 2016;3:CD003316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Beauchamp MK, Evans R, Janaudis-Ferreira T, et al. Systematic review of supervised exercise programs after pulmonary rehabilitation in individuals with COPD. Chest 2013;144:1124–33. [DOI] [PubMed] [Google Scholar]
- [14].Pack QR, Goel K, Lahr BD, et al. Participation in cardiac rehabilitation and survival after coronary artery bypass graft surgery: a community-based study. Circulation 2013;128:590–7. [DOI] [PubMed] [Google Scholar]
- [15].Chao PW, Shih CJ, Lee YJ, et al. Association of postdischarge rehabilitation with mortality in intensive care unit survivors of sepsis. Am J Respir Crit Care Med 2014;190:1003–11. [DOI] [PubMed] [Google Scholar]
- [16].Kayambu G, Boots R, Paratz J. Physical therapy for the critically ill in the ICU: a systematic review and meta-analysis. Crit Care Med 2013;41:1543–54. [DOI] [PubMed] [Google Scholar]
- [17].Castro-Avila AC, Seron P, Fan E, et al. Effect of early rehabilitation during intensive care unit stay on functional status: systematic review and meta-analysis. PLoS One 2015;10:e0130722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Doiron KA, Hoffmann TC, Beller EM. Early intervention (mobilization or active exercise) for critically ill adults in the intensive care unit. Cochrane Database Syst Rev 2018;3:CD010754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Lai CC, Chou W, Chan KS, et al. Early mobilization reduces duration of mechanical ventilation and intensive care unit stay in patients with acute respiratory failure. Arch Phys Med Rehabil 2017;98:931–9. [DOI] [PubMed] [Google Scholar]
- [20].Jones C, Skirrow P, Griffiths RD, et al. Rehabilitation after critical illness: a randomized, controlled trial. Crit Care Med 2003;31:2456–61. [DOI] [PubMed] [Google Scholar]
- [21].Vivodtzev I, Pepin JL, Vottero G, et al. Improvement in quadriceps strength and dyspnea in daily tasks after 1 month of electrical stimulation in severely deconditioned and malnourished COPD. Chest 2006;129:1540–8. [DOI] [PubMed] [Google Scholar]
- [22].Bachmann S, Finger C, Huss A, et al. Inpatient rehabilitation specifically designed for geriatric patients: systematic review and meta-analysis of randomised controlled trials. BMJ 2010;340:c1718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Davidson PM, Cockburn J, Newton PJ, et al. Can a heart failure-specific cardiac rehabilitation program decrease hospitalizations and improve outcomes in high-risk patients? Eur J Cardiovasc Prev Rehabil 2010;17:393–402. [DOI] [PubMed] [Google Scholar]
- [24].Pollock A, Baer G, Campbell P, et al. Physical rehabilitation approaches for the recovery of function and mobility following stroke. Cochrane Database Syst Rev 2014;4: 1-422 (CD001920). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Freburger JK, Li D, Fraher EP. Community use of physical and occupational therapy after stroke and risk of hospital readmission. Arch Phys Med Rehabil 2018;99: 26-34 e25. [DOI] [PubMed] [Google Scholar]
- [26].Dunlay SM, Pack QR, Thomas RJ, et al. Participation in cardiac rehabilitation, readmissions, and death after acute myocardial infarction. Am J Med 2014;127:538–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Hauken MA, Holsen I, Fismen E, et al. Working toward a good life as a cancer survivor: a longitudinal study on positive health outcomes of a rehabilitation program for young adult cancer survivors. Cancer Nurs 2015;38:3–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Popovic D, Kumar N, Chaudhry S, et al. Improvements in key cardiopulmonary exercise testing variables following cardiac rehabilitation in patients with coronary artery disease. J Cardiopulm Rehabil Prev 2018;38:E5–8. [DOI] [PubMed] [Google Scholar]
- [29].Chen YW, Wang CY, Lai YH, et al. Home-based cardiac rehabilitation improves quality of life, aerobic capacity, and readmission rates in patients with chronic heart failure. Medicine (Baltimore) 2018;97:e9629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].McCarthy B, Casey D, Devane D, et al. Pulmonary rehabilitation for chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2015;2: 1-212 (CD003793). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Puhan MA, Gimeno-Santos E, Cates CJ, et al. Pulmonary rehabilitation following exacerbations of chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2016;12:CD005305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Pawlik AJ, Kress JP. Issues affecting the delivery of physical therapy services for individuals with critical illness. Phys Ther 2013;93:256–65. [DOI] [PubMed] [Google Scholar]


