Abstract
Social support is used to determine transplant eligibility despite lack of an evidence base and vague regulatory guidance. It is unknown how many patients are disqualified from transplantation due to inadequate support, and whether providers feel confident using these subjective criteria to determine eligibility. Transplant providers (n = 551) from 202 centers estimated that, on average, 9.6% (standard deviation = 9.4) of patients evaluated in the prior year were excluded due to inadequate support. This varied significantly by United Network for Organ Sharing region (7.6%−12.2%), and by center (21.7% among top quartile). Significantly more providers used social support in listing decisions than believed it ought to be used (86.3% vs 67.6%). Nearly 25% believed that using social support in listing determinations was unfair or were unsure; 67.3% felt it disproportionately impacted patients of low socioeconomic status. Overall, 42.4% were only somewhat or not at all confident using social support to determine transplant suitability. Compared to surgical/medical transplant providers, psychosocial providers had 2.13 greater odds of supporting the criteria (P = .03). Furthermore, 69.2% supported revised guidelines for use of social support in listing decisions. Social support criteria should be reconsidered in light of the limited evidence, potential for disparities, practice variation, low provider confidence, and desire for revised guidelines.
Keywords: clinical decision-making, ethics, ethics and public policy, guidelines, health services and outcomes research, kidney transplantation/nephrology, organ transplantation in general, patient characteristics, recipient selection, social sciences
1 |. INTRODUCTION
Organ transplantation remains the only lifesaving treatment for most patients with organ failure. Yet, for over 30 years, patients who are socioeconomically disadvantaged, living in rural areas, and racial/ethnic minorities remain less likely to be listed for transplantation, despite disproportionate need.1–6 The social support requirement presents an important and understudied barrier to the waitlist that is not evidence based, with meta- analyses repeatedly unable to demonstrate a relationship between social support and posttransplant adherence among published studies.7,8 It is unclear how frequently patients are disqualified from transplantation due to inadequate social support, and whether social support criteria disproportionately impact vulnerable populations. Vulnerable groups may face greater difficulty demonstrating social support due to challenges bringing caregivers to healthcare appointments and inability to self- finance home-based assistance.4,9–16 Lack of clear guidelines for defining and evaluating social support may also contribute to significant variation across transplant centers, resulting in unequal access to the waitlist. Moreover, subjective criteria such as social support are especially susceptible to implicit bias, exacerbating concerns about inconsistent use and disparities.17,18 As such, countries including Canada and the European Union have recently removed social support considerations from the list of transplant eligibility criteria.19,20 Yet in the United States, inadequate social support remains a contraindication to transplantation.
It remains unclear how much providers rely upon social support in listing determinations, how much variation exists in use of social support, and whether providers perceive social support criteria as fair. Providers’ perceptions that social support is used inconsistently in listing decisions (procedural justice concerns) or that some groups of patients face disproportionate difficulty meeting these criteria (distributive justice concerns) may increase variation in its use among providers.21,22 Clinical factors can also affect the perceived legitimacy of the criteria and providers’ reliance on social support.21,23 Factors shown to affect perceived legitimacy include tradition (experience using social support at their center), expertise (confidence in using the criteria to determine eligibility), and legality (clarity of the federal mandate Centers for Medicare and Medicaid Services [CMS] guidelines for social support evaluation).24,25 Taken together, differences in clinicians’ attitudes towards the criteria may partly explain variation in use of social support criteria and subsequent inequalities in access to the waitlist.
Social support criteria remain controversial and may undermine consistency, transparency, and equity in the evaluation process. Consequently, providers may differ in their attitudes towards social support criteria. Yet, no studies have estimated its impact or providers’ attitudes towards social support criteria. The objective of this national study of transplant providers was to examine how frequently social support criteria affect waitlisting decisions and whether certain patient groups are disproportionately affected by these criteria. We also examine providers’ perceptions of fairness and legitimacy of social support criteria and desire for improved clarity. Understanding the impact of social support is critical for ensuring that patients are held to clear, uniform standards, and for upholding transparency and equity in access to transplantation.
2 |. METHODS
2.1 |. Survey design and administration
A 35-item survey instrument was developed following a meta- analysis and literature review,7 in- depth interviews about experiences using social support criteria and survey domains with transplant surgeons (kidney, liver, and heart), nephrologists, and transplant social workers (n = 6), and in consultation with a multidisciplinary group of transplant experts (surgeon, psychologist, social scientists, ethicists, and social workers). The instrument was revised following input from the American Society of Transplantation, American Society of Transplant Surgeons, and Society for Transplant Social Workers. Questions addressed clinicians’ rationale for evaluating social support, perceived impact of social support on access to the waitlist, perceived evidence for these criteria, and beliefs about its fairness and legitimacy. The survey included questions, “Generally, patients with low social support should be evaluated less favorably for transplantation than similar patients with greater social support” [legitimacy] and “Using social support to determine transplant eligibility is fair” [fairness]. These measures are consistent with those widely used in prior studies.25–27 Because socioeconomic status has consistently been associated with disparities in access to transplant, respondents were asked whether patients of lower socioeconomic status were as able as those of higher socioeconomic status to demonstrate adequate social support.1,2,28 Responses ranged from strongly disagree to strongly agree on a 5- point Likert scale. To ensure validity and interpretability, the survey was pretested using cognitive interviews asking respondents to “think aloud” about the questions and response options (n = 6), resulting in revised questions, response options, and inclusion of open- ended questions.29 The survey was then pilot tested to confirm the feasibility and estimate time to completion.29 The study was approved by the Tufts University Institutional Review Board.
The survey was administered via Qualtrics in October to November 2016 to the American Society of Transplant Surgeons (ASTS) and Society of Transplant Social Workers (STSW) membership. This represents diverse perspectives present in transplant listing meetings, including: surgeons and other medical providers (eg, nephrologists, hepatologists, etc.) who sometimes lead listing meetings and psychosocial providers who present social support evaluations. Respondents received an email containing the study description, consent form, and anonymous survey link, and were offered a $5 Starbucks gift card in appreciation.
2.2 |. Statistical analyses
We conducted bivariate analyses using Pearson χ2 tests to describe respondents’ beliefs and preferences related to social support criteria, by organ type (eg, abdominal vs thoracic) and clinical role (eg, psychosocial providers versus medical/surgical providers).
Logistic regression models examined variation in providers’ attitudes towards social support criteria, based on ethical and sociological theories of perceived legitimacy.22,23,25 Dependent variables were constructed from the questions: “Generally, patients with low social support should be evaluated less favorably for transplantation than similar patients with greater social support” [legitimacy] and “Using social support to determine transplant eligibility is fair” [fairness]. Response options were dichotomized to measure disagreement. Models examined whether providers’ concerns about fairness and legitimacy were linked to modifiable clinical procedural factors, including (1) clear and consistent center policies, (2) impartial and neutral evaluations of social support, and (3) transparency in informing patients when social support contributes to negative listing decisions (transparency); or to societal distributive factors including (1) disproportionate impact of low socioeconomic status; (2) patient lifestyle or health behaviors, and (3) patients’ ability to modify social support. Models examining perceived legitimacy included ethical beliefs (utility and fairness), tradition using social support (percentage of patients at respondent’s center excluded due to social support during prior year); expertise (confidence in using social support), and perceived clarity of CMS’s guidelines for social support evaluation. To facilitate logistic models, we coded the neutral response as “agree” on the premise that respondents with neutral opinions would default towards current transplant guidelines in favor of using social support.
All models were adjusted for organ type (eg, thoracic vs abdominal transplant), clinical role (psychosocial provider vs medical/surgical provider), and United Network for Organ Sharing (UNOS) region. Analyses were performed using the statistical analysis software Stata, version 15 (StataCorp, College Station, TX). Sensitivity analyses compared the results of the full and reduced- form models, removing covariates with strong correlations. Second, we ran regressions on a subsample (N = 452) for whom we had data on number of years in practice to account for potential effects of experience with transplant decision- making. Finally, we re- ran all models, excluding the neutral category. These changes did not significantly alter the results.
3 |. RESULTS
Overall, 604 clinicians from 202 transplant centers completed the survey (41% response rate), of whom 551 had complete information and were included in the analysis. This response rate is considered high for a sample of clinicians.26, 27 A nonresponse analysis comparing late respondents (those responding after a third reminder) revealed no significant differences. Respondents’ characteristics are shown in Table 1. Nearly half (47%) were psychosocial providers; 53% were surgical/medical providers (surgeons, nephrologists, hepatologists, etc.). Most were involved in kidney transplantation (72.6%), followed by liver (53%), pancreas (39.9%), heart (13.4%), and lung (7.8%); 87% were involved in multiple organ programs. Respondents had an average of 16.6 (SD = 11.3) years in practice (Table 1). There were 82 instances in which respondents reported being from the same medical center, though in 64 of these instances, fewer than 5 represented the same medical center. Only 5 centers had multiple participants from the same medical center within same organ transplant program, ranging from 5 to 9 participants.
TABLE 1.
Sample characteristics
| N | % | Avg | SD | |
|---|---|---|---|---|
| Organ programa | ||||
| Kidney | 400 | 72.6 | ||
| Liver | 292 | 53.0 | ||
| Pancreas | 220 | 39.9 | ||
| Heart | 74 | 13.4 | ||
| Lung | 43 | 7.8 | ||
| Other | 52 | 9.4 | ||
| Psychosocial expertise, training, and demographics | ||||
| Conducts psychosocial evaluation | 259 | 47.0 | ||
| Y in practice | 16.6 | 11.3 | ||
| Male | 243 | 53.2 | ||
| Respondents per UNOS region | ||||
| Region 1 | 46 | 10.4 | ||
| Region 2 | 52 | 11.7 | ||
| Region 3 | 24 | 5.4 | ||
| Region 4 | 35 | 7.9 | ||
| Region 5 | 58 | 13.1 | ||
| Region 6 | 21 | 4.7 | ||
| Region 7 | 40 | 9.0 | ||
| Region 8 | 30 | 6.8 | ||
| Region 9 | 28 | 6.3 | ||
| Region 10 | 46 | 10.4 | ||
| Region 11 | 63 | 14.2 | ||
| Total respondents | 551 | |||
SD, standard deviation; UNOS, United Network for Organ Sharing.
Total may exceed 100% because respondents indicated multiple options if applicable.
3.1 |. Impact of the social support criteria and lack of transparency
Transplant providers estimated that, on average, 9.6% (standard deviation [SD] = 9.4) of candidates evaluated during the prior year were ruled out due to inadequate social support. Centers varied significantly, with the top quartile of respondents reporting that their centers excluded >20% of patients during the prior year due to inadequate social support. Estimated deferral rates varied by UNOS region from 7.62% (SD = 5.86) in Region 6% to 12.23% (SD = 10.83) in Region 8. Providers overwhelmingly (86.3%) agreed or strongly agreed that, in their experience, patients with inadequate support are evaluated less favorably for transplantation than similar patients with greater support. While 88.7% had used inadequate social support along with other factors when arriving at negative listing decisions (relative contraindication), nearly half (45.3%) reported having relied primarily on social support in negative listing decisions (absolute contraindication). Figure 1 shows respondents’ beliefs about and use of social support criteria. Appendices 1 and 2 show these beliefs stratified by organ and highest degree of specialty, respectively. Perceived deferral rates did not differ significantly by organ, or between organs with replacement therapies (kidney dialysis and heart left ventricular assist device) compared to other organs.
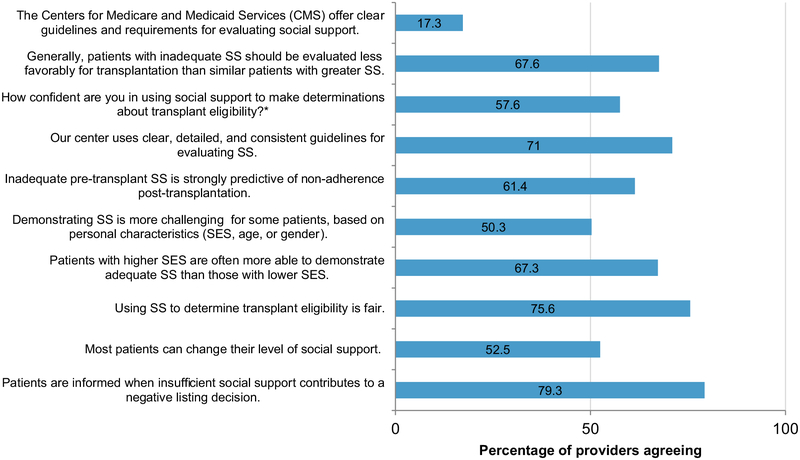
FIGURE 1.
Attitudes regarding use of social support criteria in waitlisting determinations from a national sample of transplant providers (n = 551). Social support is abbreviated as “SS.” Response categories for “How confident are you in using SS to make determinations about transplant eligibility?” are extremely/very confident, somewhat confident, not at all confident. SES, socioeconomic status
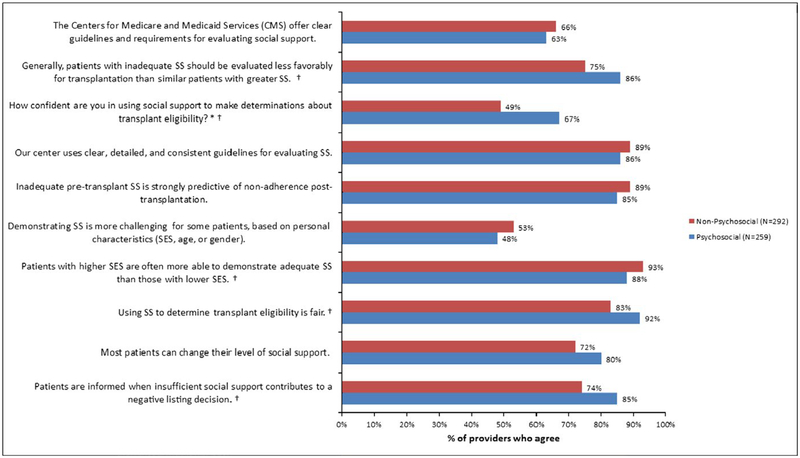
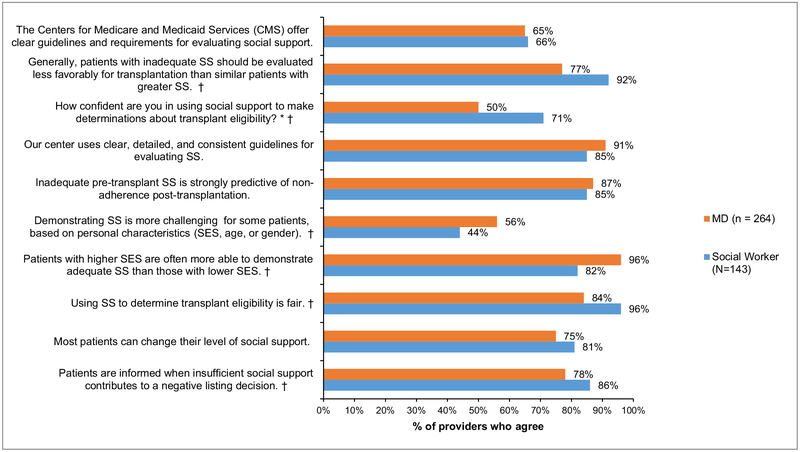
Patients were not universally informed that they were ruled out due to inadequate support, even when this occurred. Although most (79.3%) providers perceived that patients were informed when insufficient social support contributes to a negative listing decision, one fifth (21.6%) did not. Psychosocial providers were significantly more likely to report that patients were informed when social support contributed to negative listing decisions than medical/surgical providers (85.3% vs 73.9%, P = .002).
3.2 |. Disparities in meeting social support criteria
Two thirds of clinicians (67.3%) agreed that patients with higher socioeconomic status were more often able to demonstrate adequate social support than those with lower socioeconomic status. Half (50.3%) thought that demonstrating social support is more challenging for some patients based on socioeconomic status, age, or sex, and only one third (33.5%) disagreed with that statement. Most respondents (85.5%) thought that patients’ lifestyle choices and health behaviors, such as prior history of substance use, determine their ability to demonstrate adequate social support. Importantly, only half of respondents (52.5%) believed that social support was modifiable. Though most viewed it as fair (75.6%), one fifth of respondents (19.3%) did not believe that the process of evaluating patients’ social support at their center was impartial or neutral. Psychosocial providers were significantly less likely than medical/surgical providers to perceive the evaluation process as impartial (79.8% vs 81.5%, P = .025).
3.3 |. Low provider confidence and desire for improved guidelines
Widespread use of social support criteria did not correspond with high levels of confidence in it. Nearly half of respondents (42.4%) were only somewhat or not at all confident in using social support to determine transplant suitability, with 57.6% being confident (Figure 1). Medical/surgical providers (compared to psychosocial providers) and providers in abdominal transplant programs (versus thoracic) were less confident in using social support (32.8% vs 51.3%; P < .001; and 28.2% vs 45.2%; P = .004, respectively). Only 17.3% of providers considered CMS’ guidelines for evaluating and using social support in transplant decisions to be clear. Moreover, while 71% agreed that their center used clear, detailed, and consistent guidelines for evaluating social support, 29% disagreed or were unsure. Overall, 70% supported the development of a more uniform approach to social support evaluation.
3.4 |. Fairness and perceived legitimacy of social support criteria
One quarter of providers (24.3%) thought using social support to determine transplant eligibility was unfair or were unsure about its fairness (Figure 1). Medical/surgical providers were more than twice as likely as psychosocial providers to perceive use of social support as unfair (P = .006). In multivariate logistic regression models, distributive factors (related to disproportionate impact on vulnerable populations) and procedural concerns (related to the uniformity, impartiality, and transparency) were significantly associated with perceived fairness of social support criteria (Table 2). Respondents who believed that demonstrating social support is more challenging based on age, sex, or socioeconomic status were significantly less likely to perceive social support criteria as fair (odds ratio 0.32, P = .002) (distributive factor). Those who believed that social support was modifiable were 1.89 more likely to view social support as fair (P = .055). Respondents who perceived their center’s policies for evaluating social support were clear and consistent were 2.29 (P < .05) times more likely to perceive the criteria as fair. Moreover, respondents at centers that always informed patients when social support contributes to negative listing decisions had 2.34 greater odds of perceiving the criteria as fair (P = .017). Taken together, concerns about disparities, patients’ control over their level of social support, and opaque clinical practices explained 20% of the variation in perceived fairness of the criteria.
TABLE 2.
Modifiable clinical factors (procedural) and societal factors (distributive) associated with providers’ perception that using social support (SS) in listing decisions is fair
| Belief that using SS to determine eligibility for transplant is fair (odds ratios) | |||
|---|---|---|---|
| Societal factors: distributive concerns | Modifiable clinical factors: procedural concerns | Combined model | |
| Distributive factors | |||
| Demonstrating SS is more challenging for some patients, based on personal characteristics such as age, SES, or sex | 0.31*** (0.17, 0.59) | 0.32*** (0.16, 0.65) | |
| Lifestyle choices (eg, substance use) influence adequacy of patients’ SS | 1.61 (0.51, 5.09) | 1.36 (0.37, 4.97) | |
| Most patients can change their level of SS | 2.56*** (1.42, 4.62) | 1.89* (0.99, 3.61) | |
| Patients with high SES are more often able to demonstrate adequate SS than patients with low SES | 0.69 (0.19, 2.55) | 0.69 (0.18, 2.68) | |
| Modifiable clinical factors procedural factors | |||
| Evaluation of SS is based on clear, detailed, consistent center policy | 3.04*** (1.42, 6.53) | 2.29** (1.00, 5.25) | |
| Process of assessing SS at center is unbiased and impartial | 2.82** (1.11, 7.23) | 2.20 (0.84, 5.74) | |
| Patients are always informed if denial is due to lack of SS | 1.89* (0.98–3.63) | 2.34** (1.17, 4.68) | |
| Respondent characteristics | |||
| Psychosocial providers | 2.15** (1.14, 4.03) | 2.94*** (1.48, 5.82) | 2.54** (1.24, 5.22) |
| Involved in thoracic organ program | 1.16 (0.44, 3.06) | 0.99 (0.38, 2.59) | 0.89 (0.32, 2.45) |
| N = 496, R2 = 0.14 | N = 482, R2 = 0.14 | N = 468, R2 = 0.20 | |
Logistic regression models predict the probability of agreeing or strongly agreeing that it is fair to use social support to determine patient eligibility for transplant. Indicators for respondent United Network for Organ Sharing Region were included in the model but did not achieve significance. Full questions and complete results, including 95% confidence intervals, are available upon request. SES, socioeconomic status.
P < .10,
P < .05,
P < .01.
Respondents were divided over whether social support should be used for determining transplant eligibility (legitimacy). While 86.3% of respondents agreed that patients with inadequate support were less likely to be listed, only 67.6% believed that this should be the case. While 71.4% perceived social support was important for preventing organ waste (utility), respondents were less sure about the evidence for this. Only 61.4% believed that lack of social support was strongly predictive of medication nonadherence posttransplant (Figure 1).
Multivariate models identified factors associated with perceived legitimacy of social support criteria (Table 3). Beliefs that social support criteria were important for preventing organ waste (utility) and were fair were associated with 10.54 (P < .0001) and 9.24 (P < .0001) greater odds of perceiving the criteria as legitimate (ie, that social support should influence listing decisions). These factors remained significant when controlling for the percent of patients excluded during the past year at the respondent’s center (experience), respondents’ confidence in using the criteria (expertise), and perceived clarity of CMS guidelines regarding social support (legality). UNOS region and clinical role were also included in the model. Psychosocial providers were twice as likely as medical/surgical providers to support use of social support criteria in listing decisions (P < .03). Taken together, ethical beliefs and clinical role account for over a quarter of the variation in perceived legitimacy of social support criteria (adjusted R2 = 0.26).
TABLE 3.
Factors associated with transplant providers’ perception that social support (SS) should influence listing decisions (perceived legitimacy)
| Belief that SS criteria should influence patient prospects for listing (odds ratio) | |
|---|---|
| SS is important to listing to avoid organ waste | 10.54*** (4.12, 26.94) |
| Using SS to determine transplant eligibility is fair | 9.24*** (4.06, 21.02) |
| Percent of patients at center denied access due to SS in past year | 1.20 (0.83, 1.75) |
| Confidence in use of SS to determine patient suitability for transplant | 0.94 (0.47, 1.89) |
| CMS states clear use guidelines for SS in listing | 0.68 (0.35, 1.32) |
| Respondent characteristics | |
| Psychosocial provider | 2.13** (0.47, 1.89) |
| Involvement in thoracic organ program | 0.56 (0.24, 1.33) |
| N = 445, R2 = 0.26 |
Logistic regression models predict the probability of agreeing or strongly agreeing that patients with less SS ought to be evaluated less favorably for transplant. Indicators for respondent United Network for Organ Sharing Region were included in the model but did not achieve significance. Full questions and complete results, including 95% confidence intervals, are available upon request. CMS, Centers for Medicare and Medicaid Services.
P < .05,
P < .01.
4 |. DISCUSSION
Despite federal guidelines mandating equitable access to scarce organs,30 significant disparities remain in access to the waitlist.11, 28 Our findings demonstrate that social support represents an influential and understudied source of disparities in access to transplantation. This national study of transplant providers found that an estimated 10%−22% of transplant candidates were excluded due to inadequate support last year. Furthermore, 67% of providers believed use of social support disproportionately impacted patients of lower socioeconomic status and only 52% believed that social support was modifiable. Significantly more providers used the social support criteria in decision- making than believed they ought to be used (86% vs 68%). A sizable minority (25%) believed that using social support criteria in listing determinations was unfair, or they were unsure. There is substantial discomfort with the social support criteria: only 42% of respondents were only somewhat or not at all confident in using social support to determine transplant suitability. These data show, for the first time, that providers perceive that a significant proportion of patients are excluded from transplant waitlists because of social support, even though many providers lack confidence in current social support criteria and believe their use is unfair and disproportionately affects poorer patients.
Recent scrutiny of similar eligibility criteria, such as cognitive impairment and sobriety periods, has resulted in lawsuits and state laws prohibiting use of cognitive impairment as an eligibility criterion.31 The social support criteria are susceptible to similar concerns due to their tenuous evidence base and potential for increasing disparities among socially vulnerable patients.32 Our findings clarify a need and an opportunity for the transplant community to revise and standardize social support criteria to avoid similar public outcry and to address concerns of transplant providers, 70% of whom favored revising CMS criteria. Worldwide, clarifying use of social support in transplant evaluations is a growing priority for the transplant community. These changes, along with our findings of limited provider confidence in social support criteria and a desire for revised guidelines, present a backdrop for improving social support criteria in the United States. Consensus conferences supported by professional societies, including the American Society of Transplantation, ASTS, and the STSW33 and guideline development following a systematic approach, such as Grades of Recommendation Assessment, Development, and Evaluation (GRADE), can ensure that the strength of recommendations correspond to the quality of existing evidence.34 This is necessary to ensure that transplant candidates are evaluated fairly and consistently using evidence- based measures.
Subjective and ambiguously defined criteria may facilitate implicit bias towards stigmatized populations, including people with cognitive disabilities, history of substance use, and those with few friends or family. Vague guidelines leave providers susceptible to acting unsystematically, responding to intuitions and personal experiences instead of relying on evidence.35–39 Indeed, we found that despite absence of strong evidence indicating a relationship between social support and posttransplant adherence, 61.4% of providers believed that inadequate pretransplant social support was predictive of nonadherence and 71.4% believed that social support was important to avoid wasting organs, indicating either un-substantiated beliefs or potential implicit bias towards unsupported patients. Prior studies clarify how implicit attitudes may explain well- intentioned clinicians sometimes treating marginalized patients worse.40–42 In the transplant context, research has revealed biases in clinician’s interactions with disadvantaged patients, including in assessing patient preferences and commitment to transplantation, estimating their likelihood of completing evaluations or adhering to treatment, and determining the expected commitment of their social supports.3,38,39,43,44 Similarly, reliance on ambiguously defined criteria such as social support may unintentionally amplify existing bias towards patients of low socioeconomic status or patients of color.
Improving transparency by communicating the reasons that candidates are not listed for transplant is a second necessary step to ensuring trust and equity in transplant evaluations. Nearly a quarter (22%) of providers believed patients were not always informed by their center when inadequate social support contributed to a negative listing decision. Yet, transparency was an important predictor of perceived fairness of social support criteria. Providers who reported that their centers always informed patients had 2.34 greater odds of perceiving the criteria as fair (P = .017). Principles of informed consent require that patients be informed of any reason, medical or otherwise, bearing on their ability to receive lifesaving treatment. Upholding the ethical principles of autonomy, beneficence, and justice requires that transplant teams inform patients when social support contributes to a negative listing decision.45 When properly informed, patients and care teams can best determine future steps, including bolstering or better demonstrating existing social support.46 Future studies should also examine whether processes exist for patients to appeal judgments about their social support or obtain a second opinion in cases of disagreement.
Understanding whether transplant providers perceive the social support criteria as legitimate and fair is critical to understanding variation in clinical practice and ensuring equitable treatment of patients. Although most providers thought the social support criteria were fair, a sizable minority (25%) believed they were unfair. Although the distributive concerns are difficult to address, procedural fairness can be remedied through process improvements.22 Beyond transparency when patients are ruled out due to social support, requiring better data collection and reporting of factors that contribute to negative waitlisting decisions is also crucial to understanding the impact of social support on access to the waitlist, including for vulnerable populations. Although the Organ Procurement and Transplantation Network only collects data about waitlisted and transplanted patients, expanding data collection to including prelisting factors should be considered to ensure equitable access to the transplant waitlist. In recent years in an effort to improve uniformity, some centers have adopted quantitative, validated measures of social support (eg, the Stanford Integrated Psychosocial Assessment for Transplant). While quantitative measures are useful in standardizing assessments, the evidence linking these measures to adherence or posttransplant outcomes is limited and more research is needed before recommending their widespread use.47,48
As with all surveys, our study was subject to nonsampling error, including nonresponse bias. However, results of a nonresponse analysis reveal that nonresponders did not differ on demographic or center characteristics, and the attitudes of late responders did not differ significantly from others. Moreover, when calculating the response rate based on the membership list, we attempted to remove members practicing exclusively internationally and in pediatric settings and who were therefore ineligible. Due to limitations identifying all such persons, our denominator is likely larger than the population eligible to participate, reducing our response rate. Our sample included diverse members of the transplant team, but future studies should include additional patient and provider perspectives by partnering with additional professional organizations representing members of the transplant community. It is also possible that reported practices do not perfectly reflect actual practices, and that individuals within a center may have different perceptions. Given the small number of cases of multiple respondents from a single center and transplant program, we were unable to sufficiently explore correlation of beliefs within a center. Future qualitative studies should examine actual practices by observing how transplant teams use social support in listing decisions and report decisions to patients. Finally, while socioeconomic status is a key determinant of disparities in access to transplant and may inhibit patients’ ability to pay for a caregiver, future studies should also examine the impact of race and ethnicity. Strengths of our study include a sample representing nearly all transplant centers in the United States and diverse representation by geography, center size, and clinical role.
5 |. CONCLUSIONS
Providers estimate that inadequate social support excludes up to 20% of transplant candidates needing an organ transplant. A majority of transplant providers believed that social support criteria disproportionately impacted patients of low socioeconomic status, and nearly half of providers lacked confidence in current social support criteria. These data suggest a need to better define and determine how social support should be used in listing decisions to reduce disparities in access to transplantation.
ACKNOWLEDGMENTS
The authors gratefully acknowledge the support and assistance of the American Society of Transplant Surgeons and the Society for Transplant Social Work in fielding the survey and for comments during the development of the survey. The authors also gratefully acknowledge the dedicated and skilled research assistance of Meghan Olsen and statistical guidance from Jennifer Perloff.
Funding information
This study was funded by the Greenwall Foundation through their “Making a Difference” grants (PI Ladin) and the Greenwall Faculty Scholars Program (Ladin). Dr. Ladin gratefully acknowledges support by the National Center for Advancing Translational Sciences, National Institutes of Health, Award Number KL2TR001063. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Abbreviations:
- ASTS
American Society of Transplant Surgeons
- CMS
Centers for Medicare and Medicaid Services
- STSW
Society of Transplant Social Work
- UNOS
United Network for Organ Sharing
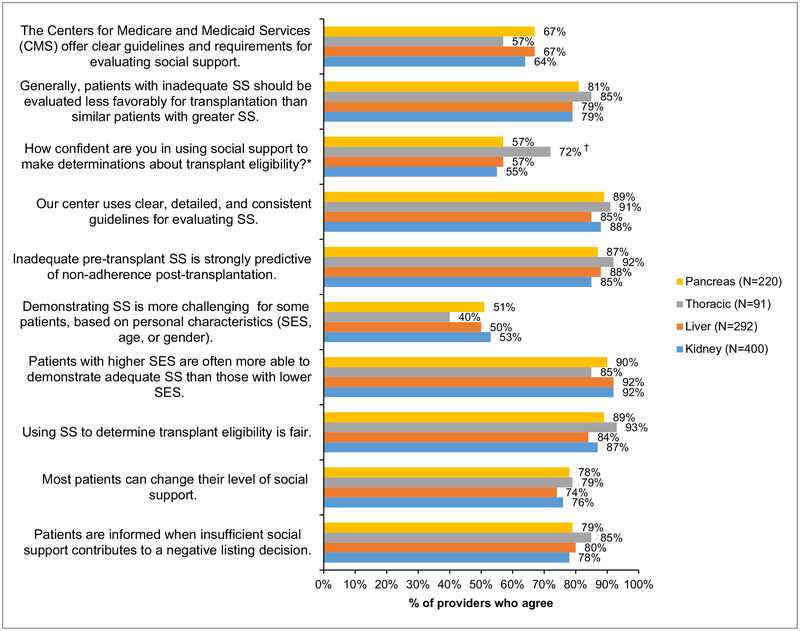
APPENDIX 1. Attitudes regarding use of social support criteria in waitlisting determinations from a national sample of transplant providers, stratified by provider’s transplant organ
SS = Social support. Organ of transplant is not mutually exclusive.
* Response categories for “How confident are you in using SS to make determinations about transplant eligibility?” are Extremely/Very Confident, Somewhat Confident, Not At All Confident.
† Indicates statistically significant difference between groups in % of providers who agree, at P < .05.
APPENDIX 2A. Attitudes regarding use of social support criteria in waitlisting determinations from a national sample of transplant providers, psychosocial providers (social workers, psychologists, psychiatrists) versus medical/surgical providers
SS = Social support.
* Response categories for “How confident are you in using SS to make determinations about transplant eligibility?” are Extremely/Very Confident, Somewhat Confident, Not At All Confident.
† Indicates statistically significant difference between groups in % of providers who agree, at P < .05.
APPENDIX 2B. Attitudes regarding use of social support criteria in waitlisting determinations from a national sample of transplant providers, stratified by provider’s highest degree of specialty
SS = Social support.
* Response categories for “How confident are you in using SS to make determinations about transplant eligibility?” are Extremely/Very Confident, Somewhat Confident, Not At All Confident.
† Indicates statistically significant difference between groups in % of providers who agree, at P < .05.
Footnotes
DISCLOSURE
The authors of this manuscript have no conflicts of interest to disclose as described by the American Journal of Transplantation.
REFERENCES
- 1.DePasquale EC, Kobashigawa JA. Socioeconomic disparities in heart transplantation: a universal fix? Circ Cardiovasc Qual Outcomes. 2016;9(6):693–694. [DOI] [PubMed] [Google Scholar]
- 2.Patzer RE, Perryman JP, Schrager JD, et al. The role of race and poverty on steps to kidney transplantation in the Southeastern United States. Am J Transplant. 2012;12(2):358–368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tong A, Howard K, Wong G, et al. Nephrologists’ perspectives on waitlisting and allocation of deceased donor kidneys for transplant. Am J Kidney Dis. 2011;58(5):704–716. [DOI] [PubMed] [Google Scholar]
- 4.Schold JD, Heaphy EL, Buccini LD, et al. Prominent impact of community risk factors on kidney transplant candidate processes and outcomes. Am J Transplant. 2013;13(9):2374–2383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Browne T, Amamoo A, Patzer RE, et al. Everybody needs a cheerleader to get a kidney transplant: a qualitative study of the patient barriers and facilitators to kidney transplantation in the Southeastern United States. BMC Nephrol. 2016;17(1):108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Flattau A, Olaywi M, Gaglio PJ, et al. Social barriers to listing for adult liver transplantation: their prevalence and association with program characteristics. Liver Transpl. 2011;17(10):1167–1175. [DOI] [PubMed] [Google Scholar]
- 7.Ladin K, Daniels A, Osani M, Bannuru R. Is social support associated with post- transplant medication adherence and outcomes? A systematic review and meta- analysis. Transplant Revs. 2017;32:16–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dew MA, DiMartini AF, De Vito DA, et al. Rates and risk factors for nonadherence to the medical regimen after adult solid organ transplantation. Transplantation. 2007;83(7):858–873. [DOI] [PubMed] [Google Scholar]
- 9.Ladin K, Hanto DW. Understanding disparities in transplantation: do social networks provide the missing clue? Am J Transplant. 2010;10(3):472–476. [DOI] [PubMed] [Google Scholar]
- 10.Salter ML, Orandi B, McAdams-DeMarco MA, et al. Patient- and provider- reported information about transplantation and subsequent waitlisting. J Am Soc Nephrol. 2014;25(12):2871–2877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ladin K, Rodrigue JR, Hanto DW. Framing disparities along the continuum of care from chronic kidney disease to transplantation: barriers and interventions. Am J Transplant. 2009;9(4):669–674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Johansen KL, Zhang R, Huang Y, Patzer RE, Kutner NG. Association of race and insurance type with delayed assessment for kidney transplantation among patients initiating dialysis in the United States. Clin J Am Soc Nephrol. 2012;7(9):1490–1497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schold JD, Gregg JA, Harman JS, Hall AG, Patton PR, Meier-Kriesche HU. Barriers to evaluation and wait listing for kidney transplantation. Clin J Am Soc Nephrol. 2011;6(7):1760–1767. [DOI] [PubMed] [Google Scholar]
- 14.Lehr CJ, Zaas DW. Candidacy for lung transplant and lung allocation. Thorac Surg Clin. 2015;25(1):1–15. [DOI] [PubMed] [Google Scholar]
- 15.Scholz U Predicting intentions and adherence behavior in the context of organ transplantation: gender differences of provided social support. J Psychosom Res. 2012;72:214–219. [DOI] [PubMed] [Google Scholar]
- 16.Browne T The relationship between social networks and pathways to kidney transplant parity: evidence from black Americans in Chicago. Soc Sci Med. 2011;73(5):663–667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Majeske R Transforming objectivity to promote equity in transplant candidate selection. Theor Med. 1996;17(1):45–59. [DOI] [PubMed] [Google Scholar]
- 18.Chapman EN, Kaatz A, Carnes M. Physicians and implicit bias: how doctors may unwittingly perpetuate health care disparities. J Gen Intern Med. 2013;28(11):1504–1510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Knoll G, Cockfield S, Blydt-Hansen T, et al. Canadian Society of Transplantation consensus guidelines on eligibility for kidney transplantation. Canad Med Assoc J. 2005;173(10):1181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Batabyal P, Chapman JR, Wong G, Craig JC, Tong A. Clinical practice guidelines on wait- listing for kidney transplantation: consistent and equitable? Transplantation. 2012;94(7):703–713. [DOI] [PubMed] [Google Scholar]
- 21.Daniels N, Sabin JE. Limits to health care: fair procedures, democratic deliberation and the legitimacy problem for insurers. Philos Public Aff. 1997;26:303–350. [DOI] [PubMed] [Google Scholar]
- 22.Daniels N, Sabin JE. Accountability for reasonableness: an update. BMJ. 2008;337:a1850. [DOI] [PubMed] [Google Scholar]
- 23.Zelditch M Theories of legitimacy In: Jost J, Major B, eds. The Psychology of Legitimacy. Cambridge: Cambridge University Press; 2001:33–53. [Google Scholar]
- 24.Justice Buchanan A., Legitimacy, and Self-Determination: Moral Foundations For International Law. Oxford: Oxford University Press; 2004. [Google Scholar]
- 25.Levi M, Sacks A, Tyler T. Conceptualizing legitimacy, measuring legitimating beliefs. Am Behav Sci. 2009;53(3):354–375. [Google Scholar]
- 26.Johnson T, Wislar J. Response rates and nonresponse errors in surveys. J Am Med Assoc. 2012;307:1805–1806. [DOI] [PubMed] [Google Scholar]
- 27.Kellerman S, Herold J. Physician response to surveys. Am J Prevent Med. 2001;20(1):61–67. [DOI] [PubMed] [Google Scholar]
- 28.Axelrod DA, Dzebisashvili N, Schnitzler MA, et al. The interplay of socioeconomic status, distance to center, and interdonor service area travel on kidney transplant access and outcomes. Clin J Am Soc Nephrol. 2015;5(12):2276–2288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fowler F Survey Research Methods. Thousand Oaks, CA: SAGE Publications; 2009. [Google Scholar]
- 30.Organ Procurement and Transplantation Network. OPTN Strategic Plan 2015–2018. Washington, D.C.: Department of Health and Human Services; 2015. [Google Scholar]
- 31.Halpern SD, Goldberg D. Allocating organs to cognitively impaired patients. N Engl J Med. 2017;376(4):299–301. [DOI] [PubMed] [Google Scholar]
- 32.Anderson K, Cass A, Cunningham J, Snelling P, Devitt J, Preece C. The use of psychosocial criteria in Australian patient selection guidelines for kidney transplantation. Soc Sci Med. 2007;64(10):2107–2114. [DOI] [PubMed] [Google Scholar]
- 33.Martin P, DiMartini A, Feng S, Brown R Jr, Fallon M. Evaluation for liver transplantation in adults: 2013 practice guideline by the American Association for the Study of Liver Diseases and the American Society of Transplantation. Hepatology. 2014;59(3):1144–1165. [DOI] [PubMed] [Google Scholar]
- 34.Guyatt GH, Oxman AD, Vist GE, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336(7650):924–926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Haider AH, Schneider EB, Sriram N, et al. Unconscious race and class bias: its association with decision making by trauma and acute care surgeons. J Trauma Acute Care Surg. 2014;77(3):409–416. [DOI] [PubMed] [Google Scholar]
- 36.Haider AH, Schneider EB, Sriram N, et al. Unconscious race and social class bias among acute care surgical clinicians and clinical treatment decisions. JAMA Surg. 2015;150(5):457–464. [DOI] [PubMed] [Google Scholar]
- 37.Haider AH, Sexton J, Sriram N, et al. Association of unconscious race and social class bias with vignette- based clinical assessments by medical students. J Am Med Assoc. 2011;306(9):942–951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Epstein AM, Ayanian JZ, Keogh JH, et al. Racial disparities in access to renal transplantation–clinically appropriate or due to underuse or overuse? N Engl J Med. 2000;343(21):1537–1544, 1532 p preceding 1537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ayanian JZ, Cleary PD, Keogh JH, Noonan SJ, David-Kasdan JA, Epstein AM. Physicians’ beliefs about racial differences in referral for renal transplantation. Am J Kidney Dis. 2004;43(2): 350–357. [DOI] [PubMed] [Google Scholar]
- 40.Green AR, Carney DR, Pallin DJ, et al. Implicit bias among physicians and its prediction of thrombolysis decisions for black and white patients. J Gen Intern Med. 2007;22(9):1231–1238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hall WJ, Chapman MV, Lee KM, et al. Implicit racial/ethnic bias among health care professionals and its influence on health care outcomes: a systematic review. Am J Public Health. 2015;105(12):e60–e76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jensen NM. Physicians and implicit bias. J Gen Intern Med. 2014;29(5):707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Boulware L, Troll M, Wang N, Powe N. Perceived transparency and fairness of the organ allocation system and willingness to donate organs: a national study. Am J Transplant. 2007;7:1778–1787. [DOI] [PubMed] [Google Scholar]
- 44.Tong A, Hanson CS, Chapman JR, et al. The preferences and perspectives of nephrologists on patients’ access to kidney transplantation: a systematic review. Transplantation. 2014;98(7):682–691. [DOI] [PubMed] [Google Scholar]
- 45.Axelrod DA, Goold SD. Maintaining trust in the surgeon- patient relationship: challenges for the new millennium. Arch Surg. 2000;135(1):55–61. [DOI] [PubMed] [Google Scholar]
- 46.Lee SJ, Back AL, Block SD, Stewart SK. Enhancing physician- patient communication. Hematol Am Soc Hematol Educ Prog. 2002;1:464–483. [DOI] [PubMed] [Google Scholar]
- 47.Maldonado JR, Dubois HC, David EE, et al. The Stanford Integrated Psychosocial Assessment for Transplantation (SIPAT): a new tool for the psychosocial evaluation of pre- transplant candidates. Psychosomatics. 2012;53(2):123–132. [DOI] [PubMed] [Google Scholar]
- 48.Vandenbogaart E, Doering L, Chen B, et al. Evaluation of the SIPAT instrument to assess psychosocial risk in heart transplant candidates: a retrospective single center study. Heart Lung. 2017;46(4):273–279. [DOI] [PubMed] [Google Scholar]