Abstract
Dementia-related behavioral symptoms are challenging clinical features occurring across etiologies and disease progression. They are associated with increased healthcare utilization, nursing home placement, family upset and burden. Families typically manage behavioral symptoms without requisite knowledge, skills and guidance. We designed WeCareAdvisor™ as an easy-to-use, evidence-informed web-based platform. It provides families knowledge about dementia, daily tips, and a systematic approach to describe behaviors, investigate modifiable contributors, create treatment plans (WeCareAdvisor™ Prescription) consisting of management tips tailored to symptom presentation, and evaluate effectiveness. WeCareAdvisor™ is being tested in a randomized trial to assess acceptability, usability and immediate impact on caregiver confidence managing and upset with behavioral symptoms, and secondarily, frequency of behavioral occurrences. Fifty-seven caregivers will be enrolled from communities and medical clinics at two sites (University of Michigan; Johns Hopkins University). Families reporting behavioral symptoms in a telephone screen are consented and interviewed at home. Following the interview, an envelope is opened by interviewers to reveal group assignment (immediate vs one-month delayed treatment group). Those receiving WeCareAdvisor™ immediately are provided an iPad and instruction in its use; those in the delayed treatment group are informed of next study steps. All caregivers are reassessed at home one month from baseline. The delayed treatment group then receives iPad instructions and are re-interviewed one month thereafter. During treatment phase, participants receive 3 weekly check-in calls to encourage tool use and troubleshoot. Key outcomes include number of times using WeCareAdvisor™ and for which behaviors, self-efficacy and upset managing behavioral symptoms, and frequency of behavioral occurrences.
Clinical trial registration #: NCT02420535.
Keywords: Alzheimer’s disease and related disorders, dementia care, neuropsychiatric symptoms, family caregiving, nonpharmacological strategies
1. Introduction
Over five million people in the US have dementia with most living at home and cared for by family caregivers [1]. Behavioral symptoms, a core clinical feature, dominate disease presentation, occurring across disease etiologies and stages [2–4]. Untreated, clinically significant behavioral symptoms may lead to rapid disease progression and conversion from mild cognitive impairment to dementia [5–7]. Other negative consequences include poor life quality, hospitalizations, residential placement, staff burnout, need for caregiver oversight, caregiver distress, and higher out-of-pocket costs to families [8–12].
Families are typically on their own to learn about behaviors and their management [13,14]. While some caregiver interventions show reductions in behavioral occurrences and caregiver distress, they are time-consuming, labor-intensive and provide decision support and strategies for a limited time [15–17]. Additionally, few proven interventions are available in real-world contexts leaving most families without access to evidence-based behavioral management techniques [18].
As families need information for behavior(s) they are managing in real time, technology may provide on-demand support [14]. Prior studies using technology to reinforce knowledge and behavioral management skills were costly and not amenable to wide-scale dissemination [15]. Alternately, online platforms have been useful to families managing other complex health conditions (cancer, cardiovascular disease, smoking cessation, weight management, depression, asthma) [19–21]. The approach however, has not been applied in dementia care and evaluated for impact on behavioral symptom management.
To help families understand behavioral symptoms and identify management strategies, we designed WeCareAdvisor™, as an online platform [14]. We describe here the rationale for the tool and randomized trial design that we will employ to evaluate its feasibility, usability and outcomes.
1.1. Rationale for and design of the tool
Although it is unclear why behavioral symptoms occur, current thought is that behaviors may be due in part to the confluence of multiple, interacting yet modifiable factors [22]. These factors may be related to the person with dementia, caregiver or environment [23]. Factors related to the person living with dementia include untreated pain or infection, inappropriate medications or dosage, boredom, feelings of insecurity, fatigue or an underlying unmet need such as hunger, thirst, or being too hot or cold. Factors may also be related to the caregiver and include communications that are too complex, poor health or being too stressed and overwhelmed. Finally, factors may be related to the physical environment such as if it is too hot or cold, overstimulating, or complex. With disease progression and decrements in information processing and executive functioning, persons with dementia may become more vulnerable to these factors resulting in behavioral expressions [24].
Box 1 presents a case scenario that typifies the challenges families confront when managing behavioral symptoms and which we sought to address in the design of the WeCareAdvisor™ tool.
Box 1. Case scenario.
Frank is an 81-year old man who lives with his 71-year old wife, Dot. Frank was diagnosed with dementia 5 years ago after displaying significant short-term memory loss. More recently, Frank has been getting verbally aggressive with Dot when angry or stressed. He has never hurt Dot physically, but the new behavior scares her. Dot often feels like she is “walking on eggshells” with Frank and overall, she feels very stressed, overburdened, and exhausted. Dot told Frank’s primary care physician (PCP) about the behavior at his last appointment, and that she “wasn’t sure how much longer” she could handle Frank at home. The PCP recommended antipsychotic treatment, but Dot was concerned because Frank had experienced side effects with such medications in the past when he was hospitalized for surgery and became delirious. The PCP was not aware of an approach to assess the potential underlying medical, environmental, or social factors contributing to Frank’s behavior, so he could not teach the family about specific nonpharmacologic (behavioral or environmental) strategies to prevent and minimize the behavior. Dot would benefit from learning communication techniques and home environmental simplifications to decrease the triggers that may contribute to Frank’s episodes of anger and verbal aggression.
The WeCareAdvisor™ tool is being developed over three interrelated phases. In Phase I, in-depth qualitative data were collected from providers and caregivers to inform the style, “look and feel” and content of the platform [25]. Then in Phase II, iterative cycles of programming, testing and refinement, combined with the clinical, behavioral, technological and design expertise of the study team, translated evidence-based treatment and knowledge into an efficient and easy-to-use tool. Phase III, the focus of this protocol paper, involves testing the completed version of WeCareAdvisor™ in a pilot randomized trial with family caregivers to gauge its usability and immediate impact on care-giver upset and efficacy managing behaviors, and secondarily, the occurrence of behavioral symptoms.
The tool design embraces eight key principles, described in Table 1, that were identified as important characteristics by end users in Phase I and Phase II. It consists of three components: “daily tips”, basic information about dementia and behaviors (the “Caregiver Survival Guide™”), and an algorithm (DICE – Describe, Investigate, Create, Evaluate) to help families identify contributors to behavioral symptoms from which to create a treatment plan.
Table 1.
Principles underlying development of WeCareAdvisor™.
| Principle | Explanation |
|---|---|
| Easy-to-use | Although some familiarity with an electronic device is needed, tool is designed for simplicity in accessing information and responding to queries |
| On demand | Available to user any time when needed and on any electronic device |
| Opportunity for repeated use | User can access any section of tool repeatedly including obtaining strategies for the same behavioral symptoms |
| Attention to health literac | Material is presented at an 8th grade level with easy-to-understand definitions provided |
| Buddy system | Based on demographic characteristics (race, age, gender), a patient navigator is provided with similar characteristics who helps the user walk through the steps of DICE |
| Addresses the range of behaviors that may occur at any one time and over course of disease | For each behavioral symptom cluster, an explanation of specific behaviors are provided |
| Include strategies customized to a specific behavioral symptom and context in which it occurs | Strategies are selected based upon caregiver input from over 1000 strategies contained in the tool |
| Generate a treatment plan reflecting varied potential contributors to the behavioral symptoms from medical or medication concerns, sleep disturbances to caregiver and environmental factors | The WeCareAdvisor™ Prescription provides specific strategies that form a treatment plan the family can follow |
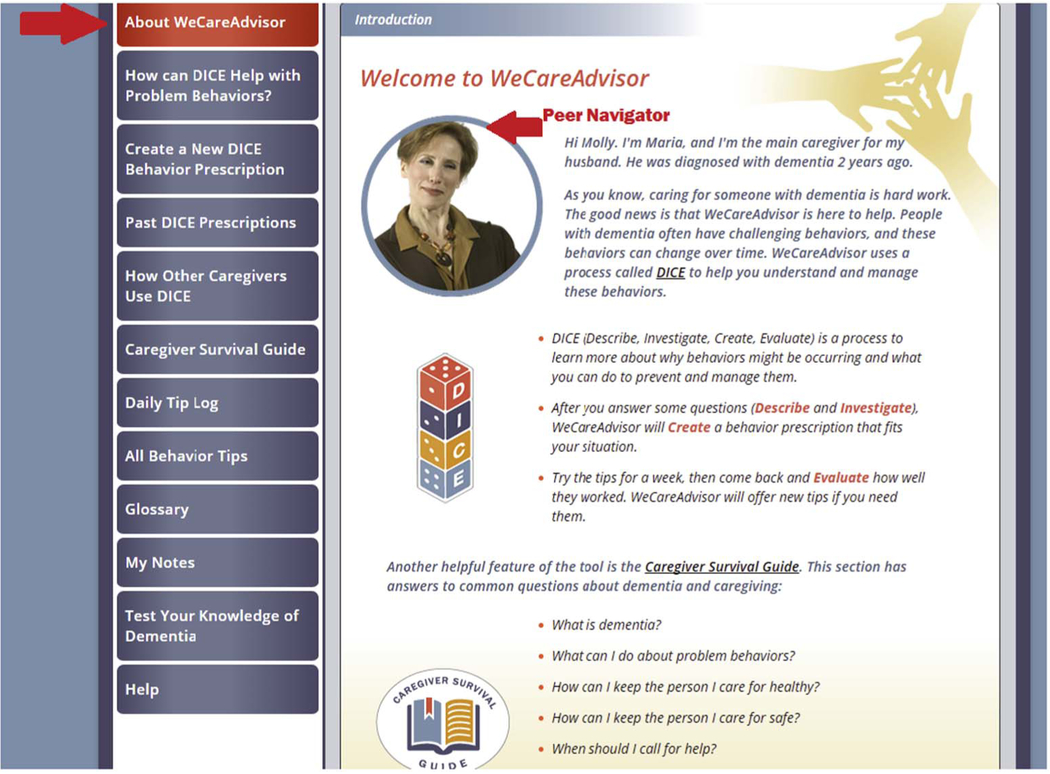
Table 2 shows the landing page along with a sample of a personal navigator who reflects the basic characteristics of a caregiver based on the information he/she provides when setting up the tool.
Table 2.
Landing page with sample personal navigator.
|
Daily tips are delivered each day to a user’s email. Users can also view all tips on the online platform. Tips were developed by the research team to reflect the best evidence for the common and daily challenges that caregivers experience. Messages concern tips for good dementia care or offer general support to caregivers. They are also designed to encourage the caregiver to interact with the WeCareAdvisor™ on their own on a regular basis to address behavioral symptoms as well as to support and motivate the caregivers. Select daily tips are shown in Table 3 to illustrate their brevity and messaging.
Table 3.
Sample tips provided daily via email to spouse caring for her husband (Marco).
| Here’s your daily tip from WeCareAdvisor™: |
| • Try to choose activities that relate to what Marco used to enjoy. For example, a person who used to enjoy sewing might like to string beads. Someone who used to pay the bills might enjoy sorting coins. |
| • Adjust activities as Marco’s dementia worsens. He may not be able to do the same things he could do last month, or even last week. |
| • Ignore mistakes whenever possible. As long as Marco and the people around him are safe, try to let mistakes go without making a big deal about them. |
| • Choose activities that are simple enough to be done in 1–2 steps. If something is too complicated, Marco is likely to get frustrated. |
| • Remember that when you’re feeling stressed, you’re not alone. Help is available 24/7 from the Alzheimer’s Association. The Helpline number is 800–272-39. |
Basic information about dementia and behavioral symptoms are provided in a section on the online platform referred to as the Caregiver Survival Guide™. The research team developed the content of the Guide based on the best evidence, education materials previously developed and tested in randomized trials, and clinical experience. The guide also includes over 1000 tips for managing behavioral symptoms culled from the literature and best practices evaluated in trials and used in clinical practices [26].
The heart of WeCareAdvisor™ is an algorithm for identifying behaviors and potential contributors from which a customized treatment plan is generated. The algorithm, referred to as DICE (Describe, Investigate, Create, Evaluate), was developed by a consensus panel of dementia care experts [22]. Iterations of this approach have been used in randomized trials providing families skills training [16], and clinical practice [27]. DICE has been described in detail elsewhere [22,23]. As applied in the tool, DICE involves the following steps. The first is to describe the behavior. This involves asking family caregivers to choose the most problematic behavioral category (e.g. agitation, aggression, depression, irritability) they wish to work on and then to respond to a series of questions concerning how often the targeted behavior occurs, if the behavior reflects sudden onset, if the caregiver or the person with dementia is in danger as a result of the behavior, how stressed the caregiver is as a result of the behavior and the context in which the behavior occurs (e.g. only at night? When too many people are around?). The second step, referred to as investigate, seeks to identify potential modifiable contributors to the targeted behavioral symptom. This involves the caregiver answering a series of questions concerning the person with dementia’s medication use, changes in medical status, safety, and pain, their living environment (e.g., is it overstimulating, is there sufficient light), as well as the caregiver’s own level of stress and wellbeing. In the third step, create, a customized “prescription” based on the information the caregiver provided in the previous steps is generated. As illustrated in Table 4, the “prescription” offers strategies in four areas: health and safety; for the person with dementia; for the caregiver; and for the environment. Caregivers are encouraged to print the prescriptions to share with their health providers and other family members. Caregivers are encouraged to try strategies for a week. After one week of use, caregivers receive an email reminder to use the tool to complete the final step of DICE by evaluating the effectiveness of each strategy in reducing or managing the targeted behavior. If the strategy was not effective, caregivers are asked a series of questions to help them problem solve possible reasons why (e.g., not enough time to try, just did not work). Caregivers are able to obtain additional strategies for the targeted behavior or choose a new behavior to work on at any time. Additionally, families can refer to the Caregiver Survival Guide™ to review all possible strategies whenever they choose.
Table 4.
Sample WeCareAdvisor™ prescription.

|
2. Trial design
We are testing WeCareAdvisor™ in a multi-site, randomized trial using a delayed treatment control group. The protocol received ethical approval from the Institutional Review Boards of each site (Gitlin and Lyketsos at Johns Hopkins University, Control # IRB00067875; and Kales at University of Michigan, Control # HUM00066639). All study procedures are being followed similarly at both sites as depicted in Fig. 1. As shown, interested caregivers contact the research team at each respective site and are screened for eligibility by telephone, with those initially eligible and willing receiving a baseline interview at their home followed by randomization. Prior to conducting the in-home baseline interview, the research team member reviews study purpose/procedures and obtains written consents (using IRB-approved forms) from the caregiver and person with dementia for their participation in one part of the interview. If the person with dementia is unable to provide informed consent, then proxy consent from the family caregiver is obtained. The inability to provide informed consent is determined by asking the person with dementia specific questions during the consenting process to discover if he/she understands study purpose, and potential risks and benefits, an approach used in prior trials [24]. Also, the person with dementia may inform the research team member that he/she prefers a family member to review the consent and sign for them.
Fig. 1.
Flow chart of study design.
*Most screening questions for eligibility completed in Step 2 with final eligibility established in Step 3.
At the conclusion of the baseline home interview, the interviewer opens a randomization envelope determining group assignment. Those randomized to the delayed treatment group (1-month wait) are informed of their group assignment and an appointment in one month is scheduled. Those assigned to receive the WeCareAdvisor™ immediately (Treatment condition) receive: 1) an iPad and orientation; 2) optional email account setup for caregivers without prior email access; and 3) instruction in use of the tool (described below).
Two to three days after the initial home visit, caregivers in the immediate treatment condition receive a follow-up telephone call from the interviewer to “check-in” to see if they have any questions about using the tool and to trouble-shoot any difficulties. Beginning one week after the baseline interview, those in the initial treatment condition receive a weekly email reminder to use the online program to identify behaviors and strategies and evaluate their use. Also, caregivers in this group receive a weekly telephone call (up to 3) by a study research team member (nurse) who uses a guiding script to inquire about use of the tool and difficulties encountered. Caregivers expressing a medical or safety concern or that behaviors are significantly worsening, are referred immediately to their physician. In addition, the nurse caller has access to a “symptom dashboard” of the caregiver’s responses to their online self-reported information, enabling them to track changes in the dyad and tool use. This enables the nurse caller to evaluate whether a caregiver needs to be prompted to use the tool and each of its components or is using the tool independently, or if a referral to the physician of the person with dementia is needed. Although these weekly calls are not of a clinical nature (and the nurse is not introduced to the caregiver as a nurse, but instead as a study team member), having the nurse serve in this capacity facilitates rapid referrals if warranted. At one month from baseline, the interviewer completes a follow-up interview in the home for all study participants (treatment and delayed treatment groups). For the immediate treatment group, the interviewer collects the iPad and there is no further study participation or contact. For the delayed treatment group, following the one-month follow-up interview, the interviewer provides the caregiver with an iPad, instructs in its use and that of the tool. Identical procedures are then followed for this group and after one month of tool use, caregivers are re-interviewed at home and the iPad collected.
2.1. Aims and study hypotheses
Our primary study aims will be twofold: 1) to evaluate the extent to which the tool and each of its components are used; and 2) to evaluate its immediate effects on caregiver upset with and confidence managing activities. We expect that after one month of tool use, caregivers in the immediate treatment group will report less upset and more confidence managing behavioral symptoms compared to those in the delayed treatment group (between group comparison). We also expect that the delayed treatment group will experience a similar level of benefit following their one month tool use (within group comparison).
Secondarily, we will also evaluate other possible outcomes including change in level of caregiver overall distress, use of negative communications, and well-being of caregivers, as well as behavioral symptom frequency and severity in persons with dementia.
2.2. Recruitment and eligibility
A total of 57 families from a variety of clinical and non-clinical sites in Ann Arbor, Michigan and Baltimore, Maryland (30 from JHU; 27 from University of Michigan) have been recruited and are now enrolled in the trial using a variety of methods including: provider or staff referral; caregiver response to recruitment flyers placed in participating sites; advertising in the community, or mailings and having interested families contact research staff by phone. Recruitment began on August 10, 2015 and the first caregiver enrolled in the study was on August 20, 2015. Recruitment has now been completed.
Caregivers are eligible for study participation who fit the following criteria: self-identify as the primary caregiver, have been an active primary caregiver for at least 6 months, and planning to remain the primary caregiver for the next 2 months; are a family member 21 years of age or older; lives with a person diagnosed with dementia; reports managing one more behavioral symptoms; are English speaking; accessible by telephone to schedule interviews and weekly check-in calls; planning to live in area for 2 months (to reduce loss to follow-up); and have familiarity with use of technology (e.g., computers, tablets, or internet).
Eligibility criteria for persons living with dementia include a clinical diagnosis of dementia or a score of < 24 on the Mini Mental State Examination. Also, if the person with dementia is on any of four classes of psychotropic medications (antidepressant, benzodiazepines, antipsychotic, or anti-convulsant) or an anti-dementia medication (memantine or a cholinesterase inhibitor), he/she has to be on a stable dose for 60 days prior to enrollment (typical time frame in clinical trials) to minimize possible confounding effects of concomitant medications.
Caregivers are excluded if they are currently involved in another clinical trial of psychosocial or educational interventions for dementia, have a visual impairment that prohibits interaction with the tool, and/or have a hearing impairment sufficient to prohibit telephone communication. Caregivers are also excluded if the person they care for is 1) not responsive to his/her environment (e.g., unable to understand short commands or recognize a person coming in/out of the room); 2) an active suicide risk; or 3) likely to have an imminent placement in a long-term care facility (within 60 days). Also, caregivers are excluded if either they or the person they care for has a terminal illness with life expectancy < 6 months, is in active treatment for cancer, or has had > 3 acute medical hospitalizations in past year. These criteria are designed to exclude persons with dementia who are at the most severe disease stage and whose caregiver may not benefit from study participation. Although more than one family member may participate in the care of the person with dementia, we will ask families to identify the person most involved to serve as the primary caregiver and user of the WeCareAdivsor™ tool for purposes of this trial.
Table 5 summarizes the basic characteristics of the study sample.
Table 5.
Characteristics of study sample (N = 57).
| Characteristic | Mean (SD) | % (N) |
|---|---|---|
| Caregivers | ||
| Age | 65.49 (14.11) | |
| Sex | ||
| Male Female |
24.6% (14) 75.4% (43) |
|
| Education | ||
| < HS | 1.8% (1) | |
| HS/GED | 14% (8) | |
| > HS | 84.2% (48) | |
| Marital status | ||
| Single | 26.3% (15) | |
| Married | 73.7% (42) | |
| Relationship to person with dementia | ||
| Spouse | 47.37% (27) | |
| Non-spouse | 52.63% (30) | |
| Upset with behaviors | 2.10 (0.83) | |
| Depression | 12.66 (8.11)* | |
| CES-D score of ≥ 16 | 32.1% (18) | |
| Willingness to pay for WeCareAdvisor™ | ||
| One-time fee (US $) | 38.52 (68.34)** | |
| Monthly fee (US $) | 7.85 (12.08)*** | |
| Person with dementia | ||
| Age | 79.88 (20.15) | |
| Sex | ||
| Male | 36.8% (21) | |
| Female | 63.2% (36) | |
| MMSE | 16.49 (8.31)**** | |
| Number of behaviors | 7.26 (3.11) | |
| Functional dependence | 10.02 (4.20)* |
Notes: PwD = person with dementia; CES-D = Center for Epidemiological Studies; MMSE = Mini-Mental State Examination;
N = 56;
N = 40;
N = 42;
N = 49, missing data due to PwD being agitation, non-verbal, refusals.
2.3. Randomization
Eligible caregivers are randomized to the treatment group which receives the WeCareAdvisor™ immediately, or to the wait-list control group, which receives the tool one month later after the follow-up interview. A randomization table was created by the University of Michigan statistician and provided to a research team member at each site. The team member created a sealed envelope and placed a piece of paper with either WeCareAdvisor™ or Wait-list. The envelope was numbered based on the order given in the table (e.g., 1, 2, 3, etc.) and envelopes were placed in sequential order. Each consented caregiver received the envelope in the order of which they were enrolled (e.g., the first consented caregiver received the first envelope at the site and so forth). The team member had access to a spreadsheet that indicated the randomization order but the interviewers who consented caregivers were masked to randomization order and did not have access to this spreadsheet. The randomization table was derived in Stata using random blocks of sizes 4, 6 or 8.
2.4. Measures
Data are captured from two sources: telephone (nurse calls) or face-to-face interviews (baseline and follow-up) and the dashboard of the tool’s platform. Table 6 lists the key measures collected at the baseline and follow-up interviews. Measures include background information, behavioral symptoms, and caregiver-related factors including relationship closeness, communication style, depressive symptoms, burden, upset with behaviors, efficacy managing behaviors.
Table 6.
Key measures used in trial.
| Domain (purpose) | Measure (citation/source) | Description (alpha based on previous trials) | Respondent | Testing occasion |
|---|---|---|---|---|
| Demographics (descriptive, possible covariate) | CG and PwD Information (US census + other sources) | Basic background characteristics | Caregiver | T1 |
| Medications (descriptive, possible covariate) | PwD and CG medications (adapted from other trials) | Brown bag review of prescription and non-prescription meds | Brown bag review | T1 |
| PwD physical health (descriptive, possible covariate) | National Health Interview Survey – adult health questionnaire, medical conditions | CG Proxy report of health | Caregiver | T1 |
| PwD cognitive status (descriptive, possible covariate) | Mini-Mental State Examination [28] | Cognitive status | PwD/PwD & proxy | T1 |
| PwD physical health and comorbidities (descriptive, possible covariate) | Caregiver assessment of function (CAFU [29]) [2] | CG proxy report of PwD dependence level (a little to complete help) (alpha = 0.90) | Caregiver | T1 |
| NPS frequency, severity, and change (primary outcome) | NPI-Q (revised version to separate agitation and aggression and add frequency) [4] | Frequency scored on a 5-point Likert scale 0 = never to 4 = very frequently/once a more a day Severity scored on a 4-pint Likert scale 0 = none to 3 = marked: a major source of behavioral abnormality |
Caregiver | T1, T2/T3 |
| CG distress with behaviors (primary outcomes) | Upset/distress with behaviors (NPI-Q) | Scored on a 6-point Likert scale 0 = not distressing to 5 = extremely | Caregiver | T1, T2/T3 |
| CG Burden (secondary outcome) | Zarit burden scale [30] | 12 items scored on a 5-point Likert scale 1 = never to 5 = nearly always | Caregiver | T1, T2/T3 |
| CG Depressive symptoms (potential moderator) | CES-D [31] | 20 items scored on a 4 point Likert scale 1 = rarely or none of the time to 4 = all of the time |
Caregiver | T1, T2/T3 |
| Use of technology | Familiarity with technology from CREATE center scale [32] | 13 items. Ten ask about the use of technology and are scored Yes/No. The other 3 ask about time and purpose of use for computer and internet | Caregiver | T1 |
| Relationship closeness scale | Relationship closeness scale [33] | 6 items scored on 4-point Likert scale 1 = strongly disagree to 4 = strongly agree | Caregiver | T1, T2, T3 |
| Communication with person with dementia (secondary outcome) | Negative communication scale [16] | 6 item scale scored on a 5 point Likert scale 1 = never to 5 = always | Caregiver | T1, T2/T3 |
| Perceived change scale (secondary outcome) | Perceived Change Scale [34] is composed of 3 factors (mood, affect and somatic wellbeing in CG) | 5-point Likert scale 1 = gotten much worse to 5 = improved a lot | Caregiver | T1, T2/T3 |
| Readiness to change | Caregiver readiness to change scale [35] | 17 item scale scored on a 4-point Likert scale 1 = not at all true to 4 = very much true | Caregiver | T1,T2,T3 |
| Confidence managing activities (primary outcome) | 5-item scale (investigator developed) | 0 = not confident to 10 = very confident | Caregiver | T1,T2,T3 |
| Confidence managing behaviors (secondary outcome) | In reference to behaviors on NPI-Q | 5-point Likert scale 0 = no confidence to 4 = extremely confident | Caregiver | Dashboard |
| Stress level | NIH REACH stress thermometer [15] | 5-point Likert scale 1 = not stressed to 5 = extremely Stressed | Caregiver | T1, T2/T3 |
| Willingness to Pay | Investigator developed [36] | 1-item | Caregiver | T1, T2/T3 |
| Ease of Use/Usefulness/Acceptance | Technology Acceptance Model (TAM) [37] | 20 items scored on a 7-point Likert scale 1 = strongly disagree to 7 = strongly agree | Caregiver | T2/T3 |
| Overall Usability | Usability scale (SUS) [38] | 10 items scored on a 5-point Likert Scale 1 = strongly disagree to 5 = strongly agree. | Caregiver | T2/T3 |
| Time spent learning tool | Time measured by RA | RA | T1 | |
| Feasibility | Daily engagement rate Completion rate of DICE™ Number of behaviors tracked |
Note: PwD= person living with dementia; CG = Caregiver; RA =research assistant; T1, T2, T3 = testing occasion; DICE = Describe, Investigate, Create, Evaluation.
At baseline, we also ask caregivers questions that will inform dissemination of the tool if it is shown to be efficacious. Questions include caregiver familiarity with technology use and willingness to pay out-of-pocket for the tool. At baseline we also evaluate the cognitive status of the person with dementia using the Mini Mental State Examination and also ask caregivers about the level of physical dependence.
Within the WeCareAdvisor™ tool itself, caregivers are asked to track the following: their stress level over the study period using a simple “stress thermometer,” caregiver confidence in managing identified behavioral symptoms, and the frequency, severity of behavioral occurrences and level of caregiver distress. Also tracked is frequency of use of each of the three components of the tool, length of time of each session, and completion rate of DICE™.
Finally, we also record the time spent learning the tool with the interviewer during the initial WeCareAdvisor™ visit in which the tool is introduced.
For interviews that follow the month after using the tool (one month post-baseline for immediate treatment group; two months post-baseline for delayed treatment group), we will examine the perceived ease of using the tool, overall usability of tool and overall satisfaction/perceived usefulness of WeCareAdvisor™.
2.5. Power considerations
Although this is a proof of concept trial evaluating feasibility, usability and preliminary outcomes, our initially proposed sample size of 30 dyads in each study group (N = 60) will afford 80% power, based on a two-group 0.05 significance level test, to detect a standardized effect size of 0.725, and the margin of error for the effect size estimate with 95% confidence will be ± 0.51 standard deviation.
2.6. Randomization scheme
A single enrollment and randomization application has been developed to assign identification codes to family caregivers during the pre-enrollment period, track eligibility status and subsequently randomize eligible caregivers.
2.7. Data management
Data management and all analyses are coordinated at the University of Michigan site for both sites. Data capture involves REDCap (Research Electronic Data Capture) that is available free of charge to both institutions. REDCap is a comprehensive, secure web application for building and managing online surveys and databases. Database design including code books of variable labels and coding decisions will be developed by the study statistician. A standard data entry system has been developed for each assessment instrument that performs immediate checks for valid ranges specified for each item.
2.8. Backups and security
Procedures are followed that protect the confidentiality of subject information. Access to the study databases is limited to appropriate study personnel using password protection. Study identification numbers are used on all research instruments and all completed assessments are kept in locked file cabinets. Daily backup of all study files is performed. A final study database that is housed at UM is being prepared and analyses will be conducted under the guidance of the project statistician and PIs.
2.9. Analytic approach
Primary outcomes will be the measures of caregiver upset (on a scale of 0 to 5) and caregiver confidence in managing behavioral symptoms (on a scale of 0 to 4) for the most problematic behavior targeted at baseline. We will also evaluate overall change in upset/distress across all behavioral occurrences reported by caregivers as well as the caregiver’s perceptions of whether everyday life for them is getting worse, staying the same or getting better in three areas: mood, affect and somatic wellbeing.
Summary descriptive statistics will be calculated at baseline and at 1 month, and also for change-scores in measures from baseline to 1 month. For the delayed treatment condition, we will evaluate change scores as well from baseline to 1 month to 2 month assessments. Summary statistics will be obtained by study group and by site. Tool-associated change will be tested using a regression model with the change-scores from baseline to 1 month as the dependent variable, and an indicator for the tool group as the primary independent variable. The model will also adjust for baseline values of the outcome variable (e.g. upset score, centered at the mean baseline value) and an indicator for sites. The parameter estimate of the tool group indicator will allow testing for the tool effect on upset (or confidence) and will estimate the expected changes in upset (or confidence) scores associated with the tool, adjusting for baseline values. Multiple regression models will also allow us to easily adjust for age and sex of the participating caregivers and persons with dementia. We note that because the delayed treatment group will receive the tool after a 1-month delay, their data at 1 to 2 months can also be added to estimate the tool effect based on a larger sample size; this estimate may reflect the impact of the tool in dyads already exposed to usual care for the 1-month period.
Other parameters of interest will include feasibility, satisfaction, tolerability, time required and ease of algorithm use. Feasibility will be assessed using daily engagement rate (% of days daily messages were open) and the DICE™ completion rate (completing the algorithm for a given behavior from start to finish) measured during the period from baseline to 1 month in the initial treatment group, and during the period between months 1 to 2 for the delayed treatment group.
We will also compare treatment to delayed group one-month post-baseline on changes in number, frequency and severity of behavioral symptoms and medication use of the person with dementia as well as caregiver well-being for purposes of generating effect size estimates for a future larger-scale trial of the tool vs. usual care.
3. Discussion
Behavioral symptoms represent one of the most challenging aspects of caring for persons with dementia for which few families are prepared to manage. The occurrence, frequency and severity of behavioral symptoms fluctuate, co-occur, present safety risks, signal the need for more vigilance and time caregiving, and diminish quality of life of families. Thus, finding ways to provide families with the knowledge and assistance they need and at the time they need it is paramount.
Currently few treatment options for behavioral symptoms are available. Psychiatric medications, specifically, off-label anti-psychotics, remain a common clinical practice despite evidence of their limited efficacy and that risks may outweigh benefits [22,39]. In contrast, nonpharmacologic strategies that target modifiable factors listed above, have been recommended by medical organizations and expert groups as the preferred first-line treatment approach based on emerging evidence base and practical know-how [40–42].
WeCareAdvisor™ is designed to provide family caregivers with the requisite knowledge and skills to manage behavioral symptoms on demand. Its main features include: 1) daily tips designed to be helpful, supportive and motivating and address the daily challenges of dementia care; 2) an educational guide (Caregiver Survival Guide™) where caregivers can learn about dementia, behavioral symptoms, taking care of themselves, potential resources and tips, and 3) DICE™, an algorithm to systematically walk families through a clinical and evidence-informed approach to identifying a behavior, its underlying potential contributors, ways to prevent, reduce, or manage the behavioral symptom and evaluate effectiveness of strategies in addition to monitoring one’s own upset, confidence and stress levels.
WeCareAdvisor™ and its testing protocol are highly innovative in several ways. First, WeCareAdvisor™ has been developed with continuous input from end users (caregivers) and other stakeholders (clinicians) along with a research team of dementia experts. Our usability framework was designed to heighten the relevance and acceptability of the tool in terms of its look, feel and scope of content. Second, the tool operationalizes DICE™, an essentially clinical approach, for use by families who may have varying levels of understanding and knowledge of dementia and behavioral symptoms. Additionally, over 1000 strategies were identified and then “tagged” to specific contexts by the study team. Thus, families receive prescriptions that are tailored to their unique situation based on their responses to a series of questions concerning the context in which the targeted behavior occurs. Third, prescriptions provide recommendations that range from medical such as to consult with a specialist or physician regarding a potential medical or medication issue to nonpharmacological such as simplifying the physical environment or communicating more simply. Thus, a comprehensive and integrative approach is provided that spans consideration of medical to non-medical contributors to behaviors.
Unique to this trial is data capture from self-report as well as real-time usability through a dashboard to evaluate components most frequently used and immediate outcomes for families. Identifying effective approaches to manage behavioral symptoms is a national priority in dementia care to improve quality of life for persons with dementia and caregivers.
Although enrollment in the trial is now closed, trial procedures are in progress. If we show at this stage of its development that WeCareAdvisor™ is used by family caregivers and reduces their stress while improving their confidence managing behaviors, it will represent a highly promising new approach for behavioral management for family caregivers and their providers warranting replication and determination of its long term use and impact. Testimonies to date, a sample of which are shown in Table 7, suggest WeCareAdvisor™ is very promising.
Table 7.
Sample testimonies.
| Caregiver gender | Relationship to person with Dementia | Testimony |
|---|---|---|
| Female | Daughter | “I’m so excited to be part of this trail blazing moment in caregiver software” “It is a fantastic tool” |
| male | Spouse | “The survival guide is comprehensive with a lot of embedded links” |
| Female | Daughter | “I shared the app with my support group and everyone was impressed by the content and ease of use” |
| Female | Spouse | “The daily tips were very helpful, and also came during appropriate situations” “I learned a great deal more about dementia, and tools/skills to use in dealing with related behaviors” |
| male | Spouse | The daily tips gave …”good advice and one technique that I am now using more” |
| Female | Spouse | “This past week (PwD) had a UTI and the WeCareAdvisor™ helped to trigger in my mind that something was wrong and he should go see a doctor” |
| Female | Spouse | “We can go to the doctor, go to support groups but I see the value of having this daily. You only see the doctor once in a while. This (WeCareAdvisor™) is advice every day” |
Note: PwD = person with dementia.
In conclusion, this is one of the first tools developed within a usability framework to provide families with on demand assistance in managing one of the most challenging aspects of dementia care. The lessons learned from this trial will also help to inform future tool development for families and their providers.
Acknowledgements
This research is being supported by a grant from the National Institute of Nursing Research (NR014200–01). The funding organization had no role in any of the following: design and conduct of the study; collection, management, analysis and interpretation of the data; and preparation, review or approval of the manuscript. Funded by the National Institute of Nursing Research grants # R01 NR014200.
Sponsor’s role
The National Institute of Nursing Research who has funded the development and testing of WeCareAdvisor™ has had no role in the design, methods, study participant recruitment, data collections, analysis and preparation of this paper.
Abbreviations:
- PwD
person with dementia
- CG
caregiver
- RA
research assistant
- T1, T2, T3
baseline (T1), one month (T2), 2 month (T3) testing occasions
- DICE
Describe, Investigate, Create, Evaluation
Footnotes
Ethics and consent statement
The protocol received ethical approval from each sites Institutional Review Boards (Gitlin and Lyketsos at Johns Hopkins University, Control # IRB00067875; and Kales at University of Michigan, Control # HUM00066639). Prior to conducting the in-home baseline interview, the research team member reviews study purpose/procedures and obtains written consents (using IRB-approved forms) from the caregiver and person with dementia for their participation in one part of the interview. If the person with dementia is unable to provide informed consent, then proxy consent from the family caregiver is obtained. The inability to provide informed consent is determined by asking the person with dementia specific questions during the consenting process to discover if he/she understands study purpose, and potential risks and benefits, an approach used in prior trials. Also, the person with dementia may inform the research team member that he/she prefers a family member to review the consent and sign for them.
We are not reporting individual patient data or any identifiable data of enrolled participants. Images shown and examples are hypothetical cases.
Competing interests and financial statement
The authors declare that they have no competing interests related to this study.
Availability of data and materials
Data for the study involve two sources: the dashboard for the online platform and self-report questionnaires entered in REDCap at the University of Michigan. Data will not be shared as it is designed to advance the tool itself. The WeCareAdvisor™ is also not available to the general public as it is under development and testing.
References
- [1].Association Alzheimer, 2016 Alzheimer’s disease facts and figures, Alzheimer’s Dement 12 (2016) (2016) 1–80, 10.1016/j.jalz.2016.03.001. [DOI] [PubMed] [Google Scholar]
- [2].Lyketsos CG, Carrillo MC, Ryan JM, Khachaturian AS, Trzepacz P, Amatniek J, Cedarbaum J, Brashear R, Miller DS, Neuropsychiatric symptoms in Alzheimer’s disease, Alzheimers Dement 7 (2011) 532–539, 10.1016/j.jalz.2011.05.2410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Rockwood K, Mitnitski A, Richard M, Kurth M, Kesslak P, Abushakra S, Neuropsychiatric symptom clusters targeted for treatment at earlier versus later stages of dementia, Int. J. Geriatr. Psychiatry 30 (2015) 357–367, 10.1002/gps.4136. [DOI] [PubMed] [Google Scholar]
- [4].Kaufer DI, Cummings JL, Ketchel P, Smith Vanessa, MacMillan Audrey, Shelley C. Timothy, Lopez M.L. Oscar, DeKosky ST, Validation of the NPI-Q, a Brief Clinical Form of the Neuropsychiatric Inventory, J. Neuropsychiatry Clin. Neurosci 12 (2000) 233–239, 10.1176/appi.neuropsych.12.2.233. [DOI] [PubMed] [Google Scholar]
- [5].Rabins P, Schwartz S, Tschanz J, Corcoran C, Black B, Fauth E, Mielke M, Lyketsos C, Risk factors for severe dementia from a population-based sample of incident Alzheimer’s Disease: the Cache County Dementia Progression Study, Alzheimer’s Dement 7 (2011) S356, 10.1016/j.jalz.2011.05.1031. [DOI] [Google Scholar]
- [6].Forrester SN, Gallo JJ, Smith GS, Leoutsakos J-MS, Patterns of neuropsychiatric symptoms in mild cognitive impairment and risk of dementia, Am. J. Geriatr. Psychiatry (2015) 1–9, 10.1016/j.jagp.2015.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Sacuiu S, Insel PS, Mueller S, Tosun D, Mattsson N, Jack CR, DeCarli C, Petersen R, Aisen PS, Weiner MW, Scott MacKin R, Chronic depressive symptomatology in mild cognitive impairment is associated with frontal atrophy rate which hastens conversion to Alzheimer dementia, Am. J. Geriatr. Psychiatry 24 (2016) 126–135, 10.1016/j.jagp.2015.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Wancata J, Windhaber J, Krautgartner M, Alexandrowicz R, The consequences of non-cognitive symptoms of dementia in medical hospital departments, Int. J. Psychiatry Med 33 (2003) 257–271, 10.2190/ABXK-FMWG-98YP-D1CU. [DOI] [PubMed] [Google Scholar]
- [9].Gitlin LN, Kales HC, Lyketsos CG, Nonpharmacologic management of behavioral symptoms in dementia, J. Am. Med. Assoc 308 (2012) 2020–2029, 10.1001/jama.2012.36918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Jutkowitz E, Kuntz KM, Dowd B, Gaugler JE, MacLehose RF, Kane RL, Effects of cognition, function, and behavioral and psychological symptoms on out-of-pocket medical and nursing home expenditures and time spent caregiving for persons with dementia, Alzheimer’s Dement (2017), 10.1016/j.jalz.2016.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Beeri MS, Werner P, Davidson M, Noy S, The cost of behavioral and psychological symptoms of dementia (BPSD) in community dwelling Alzheimer’s disease patients, Int. J. Geriatr. Psychiatry 17 (2002) 403–408, 10.1002/gps.490. [DOI] [PubMed] [Google Scholar]
- [12].Murman DL, Chen Q, Powell MC, Kuo SB, Bradley CJ, Colenda CC, The incremental direct costs associated with behavioral symptoms in AD, Neurology 59 (2002) 1721–1729, 10.1212/01.WNL.0000036904.73393.E4. [DOI] [PubMed] [Google Scholar]
- [13].Marx KA, Stanley IH, Van Haitsma K, Moody J, Alonzi D, Hansen BR, Gitlin LN, Knowing versus doing: education and training needs of staff in a chronic care hospital unit for individuals with dementia, J. Gerontol. Nurs 40 (2014), 10.3928/00989134-20140905-01 (26–35–7). [DOI] [PubMed] [Google Scholar]
- [14].Werner N, Stanislawski B, Marx K, Watkins D, Kobayashi M, Kales H, Gitlin L, Getting what they need when they need it: Sociotechnical system barriers to informal caregivers’ information needs, Appl. Clin. Inform. (n.d.) (submitted). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Belle SH, Burgio L, Burns R, Coon D, Czaja SJ, Gallagher-Thompson D, Gitlin LN, Klinger J, Koepke KM, Lee CC, Martindale-Adams J, Nichols L, Schulz R, Stahl S, Stevens A, Winter L, Zhang S, Enhancing the quality of life of dementia caregivers from different ethnic or racial groups: a randomized, controlled trial, Ann. Intern. Med 145 (2006) 727–738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Gitlin LN, Winter L, Dennis MP, Hodgson N, Hauck WW, Targeting and managing behavioral symptoms in individuals with dementia: A randomized trial of a nonpharmacological intervention, J. Am. Geriatr. Soc 58 (2010) 1465–1474, 10.1111/j.1532-5415.2010.02971.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Brodaty H, Arasaratnam C, Meta-analysis of nonpharmacological interventions for neuropsychiatric symptoms of dementia, Am. J. Psychiatry 169 (2012) 946–953, 10.1176/appi.ajp.2012.11101529. [DOI] [PubMed] [Google Scholar]
- [18].Gitlin LN, Marx K, Stanley IH, Hodgson N, Translating evidence-based dementia caregiving interventions into practice: State-of-the-science and next steps, Gerontologist 55 (2015) 210–226, 10.1093/geront/gnu123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Northouse LL, Mood DW, Schafenacker A, Kalemkerian G, Zalupski M, Lorusso P, Hayes DF, Hussain M, Ruckdeschel J, Fendrick AM, Trask PC, Ronis DL, Kershaw T, Randomized clinical trial of a brief and extensive dyadic intervention for advanced cancer patients and their family caregivers, Psychooncology 22 (2013) 555–563, 10.1002/pon.3036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Strecher VJ, McClure J, Alexander G, Chakraborty B, Nair V, Konkel J, Greene S, Couper M, Carlier C, Wiese C, Little R, Pomerleau C, Pomerleau O, The role of engagement in a tailored web-based smoking cessation program: randomized controlled trial, J. Med. Internet Res 10 (2008), 10.2196/jmir.1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Joseph CLM, Havstad SL, Johnson D, Saltzgaber J, Peterson EL, Resnicow K, Ownby DR, Baptist AP, Johnson CC, Strecher VJ, Factors associated with nonresponse to a computer-tailored asthma management program for urban adolescents with asthma, J. Asthma 47 (2010) 667–673, 10.3109/02770900903518827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Kales HC, Gitlin LN, Lyketsos CG, Management of neuropsychiatric symptoms of dementia in clinical settings: recommendations from a multidisciplinary expert panel, J. Am. Geriatr. Soc 62 (2014) 762–769, 10.1111/jgs.12730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Kales HC, Gitlin LN, Lyketsos CG, Assessment and management of behavioral and psychological symptoms of dementia, BMJ 350 (2015) h369, 10.1136/bmj.h369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Gitlin LN, Piersol CV, Hodgson N, Marx K, Roth DL, Johnston D, Samus Q, Pizzi L, Jutkowitz E, Lyketsos CG, Reducing neuropsychiatric symptoms in persons with dementia and associated burden in family caregivers using tailored activities: design and methods of a randomized clinical trial, Contemp. Clin. Trials 49 (2016) 92–102, 10.1016/j.cct.2016.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Kales H, Gitlin L, Stanislawski B, Marx K, Turnwald M, Watkins D, Lyketsos C, WeCareAdvisor™: the development of a caregiver-focused, web-based online program to assess and manage behavioral and psychological symptoms of dementia, (n. d.) (submitted). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Gitlin LN, Piersol CV, A Caregiver’s Guide to Dementia: Using Activities and Other Strategies to Prevent, Reduce and Manage Behavioral Symptoms, 1st ed., Camino Books, Inc, 2014. [Google Scholar]
- [27].Rabins PV, Lyketsos CG, Steele CD, Practical Dementia Care, Oxford University Press, 2006, 10.1093/med/9780195169782.001.0001. [DOI] [Google Scholar]
- [28].Folstein MF, Folstein SE, McHugh PR, “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician, J. Psychiatr. Res 12 (1975) 189–198, 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- [29].Gitlin LN, Roth DL, Burgio LD, Loewenstein DA, Nichols L, Corcoran M, Burns R, Martindale J, Caregiver appraisals of functional dependence in individuals with dementia and associated caregiver upset: psychometric properties of a new scale and response patterns by caregiver and care recipient characteristics, J. Aging Heal 17 (2005) 148–171, 10.1177/0898264304274184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Bédard M, Molloy DW, Squire L, Dubois S, Lever JA, O’Donnell M, The Zarit Burden Interview: a new short version and screening version, Gerontologist 41 (2001) 652–657, 10.1093/geront/41.5.652. [DOI] [PubMed] [Google Scholar]
- [31].Santor DA, Coyne JC, Shortening the CES-D to improve its ability to detect cases of depression, Psychol. Assess 9 (1997) 233–243, 10.1037/1040-3590.9.3.233. [DOI] [Google Scholar]
- [32].Czaja SJ, Charness N, Fisk AD, Hertzog C, Nair SN, Rogers WA, Sharit J, Factors predicting the use of technology: findings from the Center for Research and Education on Aging and Technology Enhancement (CREATE), Psychol. Aging 21 (2006) 333–352, 10.1037/0882-7974.21.2.333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Whitlatch CJ, Schur D, Noelker LS, Ejaz FK, Looman WJ, The stress process of family caregiving in institutional settings, Gerontologist 41 (2001) 462–473, 10.1093/geront/41.4.462. [DOI] [PubMed] [Google Scholar]
- [34].Gitlin LN, Winter L, Dennis MP, Hauck WW, Assessing perceived change in the well-being of family caregivers: psychometric properties of the perceived change index and response patterns, Am. J. Alzheimers Dis. Other Demen 21 (2006) 304–311, 10.1177/1533317506292283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Gitlin LN, Rose K, Impact of caregiver readiness on outcomes of a nonpharmacological intervention to address behavioral symptoms in persons with dementia, Int. J. Geriatr. Psychiatry 31 (2016) 1056–1063, 10.1002/gps.4422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Jutkowitz E, Gitlin LN, Pizzi LT, Evaluating willingness-to-pay thresholds for dementia caregiving interventions: application to the tailored activity program, Value Health 13 (2010) 720–725, 10.1111/j.1524-4733.2010.00739.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Davis FD, Perceived usefulness, perceived ease of use, and user acceptance of information technology, MIS Q 13 (1989) 319–340, 10.2307/249008. [DOI] [Google Scholar]
- [38].Brooke J, SUS - a quick and dirty usability scale, Usability Eval. Ind 189 (1996) 4–7, 10.1002/hbm.20701. [DOI] [Google Scholar]
- [39].Maust DT, Kim HM, Seyfried LS, Chiang C, Kavanagh J, Schneider LS, Kales HC, Antipsychotics, other psychotropics, and the risk of death in patients with dementia: number needed to harm, JAMA Psychiatry 48109 (2015) 1–8, 10.1001/jamapsychiatry.2014.3018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].American Geriatrics Society, Choosing Wisely: Five Things Physicians and Patients Should Question, (2012). [Google Scholar]
- [41].Dementia: A NICE-SCIE Guideline on Supporting People With Dementia and Their Carers in Health and Social Care. http://www.ncbi.nlm.nih.gov/pubmed/21834193, (2016). [PubMed]
- [42].American Geriatrics Society, American Association for Geriatric Psychiatry, Consensus statement on improving the quality of mental health care in U.S. nursing homes: management of depression and behavioral symptoms associated with dementia, J. Am. Geriatr. Soc 51 (2003) 1287–1298 http://www.ncbi.nlm.nih.gov/pubmed/12919243. [DOI] [PubMed] [Google Scholar]



