Abstract
Purpose
Burnout is a syndrome comprised of three major dimensions, namely, emotional exhaustion, depersonalization, and reduced personal accomplishment. Its etiology appears to be multifactorial, involving work-related and personal factors including personality traits. Personality has been associated with burnout among various physician groups; however, this has not been studied well amongst primary care physicians. This study therefore aimed to investigate the association between personality type and burnout in primary care physicians in Canada and Jamaica.
Methods
This cross-sectional study involved primary care physicians in Canada and Jamaica. Participants completed a questionnaire that included the Maslach Burnout Inventory Human Services Survey and The Big Five Inventory. Responses were analyzed to determine relationships between burnout, personality type, and various demographic factors.
Results
Seventy-seven physicians participated in the study. Approximately 38% of participants reported low levels of accomplishment, 34% reported high levels of emotional exhaustion, and 20% reported high levels of depersonalization, all equating to high levels of burnout. Neuroticism was negatively correlated with personal accomplishment (P<0.01) and positively correlated with emotional exhaustion (P≤0.001) and depersonalization (P<0.01). Agreeableness (P<0.05) and conscientiousness (P<0.05) were positively correlated with accomplishment and both were negatively correlated with depersonalization (P<0.01 and P<0.05, respectively).
Conclusion
In this multinational study, we found that burnout was a common problem among primary care physicians. Personality, particularly neuroticism, agreeableness, and conscientiousness, impacts physician burnout. Strategies that modulate the impact of personality on burnout may be beneficial for optimal health care delivery.
Keywords: personality types, occupational health, neuroticism, physician burnout
Introduction
The concept of staff burnout, first described by American psychologist Herbert Freudenberger in 1974,1 represents a syndrome with several associated symptoms, including exhaustion, frustration, and a feeling of failure, which compromises work performance.2 Three major dimensions or elements have subsequently been described, namely, emotional exhaustion, depersonalization, and reduced personal accomplishment,3 which can be measured by the Maslach Burnout Inventory (MBI).2
Burnout has been described in various occupational groups, including health professionals. Its reported prevalence is worrying with estimates of the three dimensions ranging, for example, from 11% to 62% among Japanese clinical oncologists and palliative care physicians4 and 32% to 43% among European family doctors in 12 countries.2 For American physicians, burnout was estimated to affect as many as 54.4% in 2014, an increase of ~9% compared with 2011 data.5 This syndrome transcends specialty, being well documented across physician groups, including family and other primary care physicians,2,6 emergency medical personnel,7 and various other specialists.4,8,9 In addition, burnout appears early in medical careers, even among residents10 and interns.11
The burnout syndrome has significant negative consequences for the affected practitioner. These include greater job dissatisfaction,12 increased reports of medical errors,13 and an enhanced risk of psychopathology.14,15 Equally important is the observation that physician burnout also affects patients, leading to lower empathy,16 poorer patient satisfaction,12 and decreased patient adherence.13 Ultimately, an impaired physician undermines safe and effective health care delivery.
The prevention and effective management of this syndrome is therefore an important health care objective. To achieve this, a comprehensive understanding of its various causes is crucial. Its etiology appears multifactorial, involving a demanding workload,14 diminished work-related control,13 difficulty balancing personal and professional responsibilities,14 and coping strategy.17 Lack of empathy,16 assertiveness,18 and emotional intelligence12 have also been associated with burnout. In addition, other psychological factors including personality19,20 may be important. Personality encompasses an individual’s unique way of interacting with the environment21 and has been categorized by the Five Factor Model into five dimensions: openness to experience, conscientiousness, extraversion, agreeableness, and neuroticism.22,23
Several associations have been reported between personality and physician burnout, including among family medicine residents,24 various physician groups,17,25 and consultants.26 However, the association between personality and burnout among primary care physicians is not well documented. This multisite study therefore sought to evaluate the association between personality type and physician burnout among primary care physicians in two distinct geographic locations: Canada and Jamaica.
Methods
This was a cross-sectional survey of primary care physicians in Canada and Jamaica. It was simultaneously approved by the research ethics boards of both the St. Michael’s Hospital (Ontario, Canada) and the University of the West Indies (Kingston, Jamaica). Informed consent was sought and obtained from all participants.
Study population
All primary care physicians who had an available e-mail address affiliated with St. Michael’s Hospital Department of Family and Community Medicine (SMH DFCM), McMaster Department of Family Medicine and the Jamaica chapter of the Caribbean College of Family Physicians (CCFP), as well as family medicine residents (trainees) affiliated with SMH DFCM and the University of the West Indies (UWI) were eligible for inclusion. Informed consent was demonstrated by voluntary completion and submission of the survey, as outlined in the survey’s introduction.
Survey
An electronic anonymous survey was sent by e-mail to all potential participants. A reminder e-mail was sent 1 month later. The electronic survey was housed on the FluidSurveysTM website and removed 1 month after the reminder e-mail was sent out. Participants were able to complete the survey without the need to enter any personally identifiable information and received their results automatically from the electronic survey software.
The survey consisted of three sections: 1) demographics, 2) questions related to physician burnout, and 3) questions related to determining personality type. Demographics questions explored age, gender, practice setting, years in practice, and number of hours per week spent in patient care. Physician burnout was assessed by the MBI Human Services Survey (MBI-HSS), which consists of three subscales: accomplishment, emotional exhaustion, and depersonalization.2 Those with a low score on the accomplishment subscale and a high score on the exhaustion and depersonalization subscales were considered to be suffering from burnout. The cutoffs for low/moderate/high burnout were as follows: accomplishment, ≥40/34–39/≤33; emotional exhaustion, ≤18/19–26/≥27; and depersonalization, ≤5/6–9/≥10. The Big Five Inventory (BFI), which measures five components of personality (extraversion, agreeableness, conscientiousness, neuroticism, and openness), was used to determine personality type.22,23 The survey was estimated to take 20–25 minutes to complete. At the completion, participants received their results (ie, personality type and burnout scores), as well as resources related to burnout.
Statistical analyses
Descriptive analyses categorized respondents by age group, gender, role, location, years in practice, practice setting, and patient load. Respondents were further characterized by personality type and burnout dimensions, which were stratified by location. Bivariate analyses (correlation) were used to determine the relationship between burnout and personality type, as well as between these and other demographic variables. Statistical analyses were performed using SAS software, version 9.4 (SAS Institute Inc., Cary, NC, USA). A P-value <0.05 was considered statistically significant.
Ethics approval and informed consent
This study was approved by the research ethics boards of both the St. Michael’s Hospital (Ontario, Canada) and the University of the West Indies (Kingston, Jamaica). Informed consent was sought and obtained from all participants.
Results
Demographics
There were a total of 77 respondents (response rate of 19%). As shown in Table 1, among those who identified their location, 30 (54%) were from Canada and 26 (46%) from Jamaica. Females accounted for 46 (79%) of participants, and 50 (86%) were older than 30 years of age. Thirty-six (62%) identified themselves as family physicians or residents, with the remainder categorizing themselves as general practitioner or other.
Table 1.
Demographics
| Variable | (n) | (%) |
|---|---|---|
|
| ||
| Gender | ||
| Male | 12 | 21 |
| Female | 46 | 79 |
|
| ||
| Age (years) | ||
| ≤30 | 8 | 14 |
| 31–40 | 20 | 35 |
| 41–50 | 11 | 19 |
| >50 | 19 | 33 |
|
| ||
| Role | ||
| Certified family physician | 23 | 40 |
| Family medicine resident | 13 | 22 |
| General practitioner | 14 | 24 |
| Other | 8 | 14 |
|
| ||
| Location | ||
| Canada | 30 | 54 |
| Jamaica | 26 | 46 |
|
| ||
| Years of practice | ||
| ≤5 | 13 | 22 |
| 6–10 | 12 | 21 |
| 11–20 | 10 | 17 |
| >20 | 23 | 40 |
|
| ||
| Practice setting | ||
| Hospital | 15 | 20 |
| Academic health center | 31 | 40 |
| Health center | 7 | 9 |
| Solo private practice | 14 | 18 |
| Other | 9 | 12 |
|
| ||
| See patients daily? | ||
| Yes | 34 | 59 |
| No | 24 | 41 |
|
| ||
| Number of patients per week | ||
| ≤25 | 7 | 12 |
| 26–100 | 40 | 70 |
| >100 | 10 | 18 |
Participants exhibited a wide range of experience, with the largest category being those who practiced for >20 years (23 [40%]) and the smallest including those practicing between 11 and 20 years (10 [17%]). Thirteen (22%) reported practicing for up to 5 years. Thirty-one (40%) participants were affiliated with an academic health center, while ~20% were affiliated with either a hospital (n=15), solo private practice (n=14), or with either a health center or other setting (n=16). Thirty-four (59%) reported seeing patients daily and 40 (70%) saw between 26 and 100 patients per week.
Burnout and personality type among primary care physicians
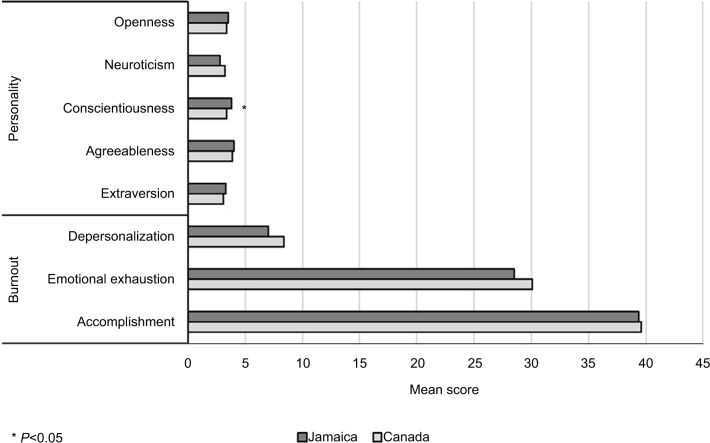
Burnout scores and personality types were assessed for all participants. Forty-nine (64%) completed the MBI-HSS in its entirety. Mean scale scores were 39.4±7.8 for accomplishment, 29.4±13.8 for emotional exhaustion, and 7.8±6.3 for depersonalization. Twenty-nine (38%) scored low on the accomplishment scale, while 26 (34%) and 15 (20%) scored high for emotional exhaustion and depersonalization, respectively (Table 2), translating to high levels of burnout. There were no statistical differences for any of the scale scores between Canada and Jamaica (Figure 1).
Table 2.
Degree of burnout, n (%)
| Subscale | Low burnout | Moderate burnout | High burnout |
|---|---|---|---|
| Accomplishment** | 35 (46) | 13 (17) | 29 (38) |
| Emotional exhaustion | 40 (52) | 11 (14) | 26 (34) |
| Depersonalization | 51 (66) | 11 (14) | 15 (20) |
Notes: Cutoffs for low/moderate/high burnout are: emotional exhaustion: ≤18, low; 19–26, moderate; ≥27, high. Accomplishment: ≤33, high; 34–39, moderate; ≥40, low. Depersonalization: ≤5, low; 6–9, moderate; ≥10, high.
The accomplishment subscale is interpreted in the opposite direction as the emotional exhaustion and depersonalization subscales.
Figure 1.
Differences in mean burnout and personality scores between Canada and Jamaica.
Other factors that may influence physician burnout were assessed (Table 3). Males were found to score significantly higher on the accomplishment scale than females (P<0.05). Staff physicians (non-trainees) reported higher accomplishment scores than residents though the difference was not statistically significant. Participants who saw >100 patients per week also scored higher on the depersonalization scale (P<0.05). Age and years of practice were not statistically associated with any of the burnout dimensions in this sample.
Table 3.
Association between burnout and other demographics (mean score, SD)
| Variable | Accomplishment | P-value | Emotional exhaustion | P-value | Depersonalization | P-value |
|---|---|---|---|---|---|---|
|
| ||||||
| Gender | ||||||
| Male | 43.9 (3.0) | <0.05 | 29.6 (15.6) | NS | 6.7 (6.1) | NS |
| Female | 38.3 (8.2) | 29.3 (13.5) | 8.1 (6.5) | |||
|
| ||||||
| Age (years) | ||||||
| ≤30 | 36.9 (7.2) | NS | 33.2 (9.1) | NS | 8.8 (4.1) | NS |
| 31–40 | 40.1 (4.7) | 31.2 (12.3) | 9.1 (7.7) | |||
| 41–50 | 37.3 (12.5) | 26.2 (16.4) | 8.4 (5.0) | |||
| >50 | 41.2 (7.2) | 27.7 (15.9) | 5.3 (5.7) | |||
|
| ||||||
| Years of practice | ||||||
| ≤5 | 37.8 (5.9) | NS | 33.6 (9.5) | NS | 9.8 (5.9) | NS |
| 6–10 | 40.7 (4.5) | 30.6 (12.2) | 8.4 (6.0) | |||
| 11–20 | 39.5 (6.2) | 26.7 (12.8) | 9.6 (7.7) | |||
| >20 | 39.6 (10.5) | 27.8 (17.2) | 5.5 (5.7) | |||
|
| ||||||
| Number of patients per week | ||||||
| ≤25 | 34.0 (14.3) | NS | 31.3 (10.8) | NS | 9.0 (6.1) | <0.05 |
| 26–100 | 40.2 (5.8) | 29.2 (13.4) | 6.5 (5.1) | |||
| >100 | 39.7 (9.3) | 29.4 (18.4) | 12.8 (9.4) | |||
|
| ||||||
| Role | ||||||
| Staff physician | 40.9 (6.4) | NS | 29.4 (2.6) | NS | 7.8 (7.0) | NS |
| Resident | 36.5 (6.3) | 28.6 (3.6) | 7.1 (4.5) | |||
Abbreviation: NS, not significant.
Forty-eight (62%) completed the BFI in its entirety. Mean scale scores, measured from 1 to 5, were 3.2±0.9 for extraversion, 4.0±0.6 for agreeableness, 3.6±0.7 for conscientiousness, 3.0±0.8 for neuroticism, and 3.5±0.6 for openness. Participants from Jamaica scored significantly higher on the conscientiousness scale (3.8±0.6 vs 3.4±0.7, P<0.05), while participants from Canada scored higher on the neuroticism scale (3.2±0.7 vs 2.8±0.8, P=not significant), though the difference did not reach statistical significance (Figure 1). Participant age was significantly associated with increased conscientiousness scores and decreased neuroticism scores (Table 4). Increased years of practice was also significantly associated with a decrease in neuroticism (P<0.05). Staff physicians scored higher on conscientiousness (P<0.05), and agreeableness appeared to peak among participants who saw between 26 and 100 patients per week (P<0.05).
Table 4.
Association between personality and other demographics (mean score, SD)
| Variable | Extraversion | P-value | Agreeableness | P-value | Conscientiousness | P-value | Neuroticism | P-value | Openness | P-value |
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Gender | ||||||||||
| Male | 3.2 (0.7) | NS | 4.0 (0.6) | NS | 3.7 (0.6) | NS | 2.9 (0.8) | NS | 3.8 (0.8) | NS |
| Female | 3.2 (0.9) | 3.9 (0.6) | 3.6 (0.7) | 3.1 (0.8) | 3.4 (0.6) | |||||
|
| ||||||||||
| Age (years) | ||||||||||
| ≤30 | 3.0 (1.0) | NS | 3.7 (0.4) | NS | 2.7 (0.6) | <0.05 | 4.1 (0.3) | <0.01 | 3.1 (0.8) | NS |
| 31–40 | 3.4 (0.8) | 3.9 (0.5) | 3.7 (0.5) | 3.1 (0.6) | 3.4 (0.5) | |||||
| 41–50 | 2.7 (0.8) | 4.0 (0.6) | 3.6 (0.5) | 2.8 (0.7) | 3.4 (0.5) | |||||
| >50 | 3.3 (0.9) | 4.1 (0.7) | 3.7 (0.5) | 2.7 (0.8) | 3.7 (0.8) | |||||
|
| ||||||||||
| Years of practice | ||||||||||
| ≤5 years | 2.9 (0.9) | NS | 3.7 (0.3) | NS | 3.2 (0.8) | NS | 3.8 (0.5) | <0.05 | 3.0 (0.6) | NS |
| 6–10 years | 3.3 (0.8) | 4.1 (0.4) | 3.5 (0.5) | 3.1 (0.5) | 3.6 (0.5) | |||||
| 11–20 years | 3.2 (1.1) | 3.8 (0.7) | 3.7 (0.7) | 2.9 (0.8) | 3.5 (0.4) | |||||
| >20 years | 3.2 (0.9) | 4.1 (0.6) | 3.7 (0.7) | 2.8 (0.8) | 3.6 (0.7) | |||||
|
| ||||||||||
| Number of patients per week | ||||||||||
| ≤25 | 3.1 (0.1) | NS | 3.1 (0.4) | <0.05 | 3.2 (0.7) | NS | 3.4 (0.5) | NS | 3.6 (0.2) | NS |
| 26–100 | 3.1 (0.9) | 4.1 (0.5) | 3.7 (0.7) | 3.0 (0.8) | 3.4 (0.6) | |||||
| >100 | 3.4 (0.9) | 3.8 (0.8) | 3.4 (0.5) | 3.1 (1.0) | 3.4 (0.7) | |||||
|
| ||||||||||
| Role | ||||||||||
| Staff physician | 3.2 (0.9) | NS | 4.0 (0.6) | NS | 3.7 (0.7) | <0.05 | 3.0 (0.7) | NS | 3.5 (0.6) | NS |
| Resident | 2.9 (1.0) | 3.7 (0.6) | 3.1 (0.7) | 3.5 (0.9) | 3.3 (0.7) | |||||
Abbreviation: NS, not significant.
Personality type correlated with burnout dimensions
Correlations between personality type and burnout were assessed among the 48 (62%) participants who completed both the MBI-HSS and BFI scales. As shown in Table 5, neuroticism was negatively associated with accomplishment (P<0.01), but positively correlated with both emotional exhaustion (P=<0.001) and depersonalization (P<0.01). Agreeableness (P<0.05) and conscientiousness (P<0.05) were positively correlated with accomplishment. Both were also negatively correlated with depersonalization (P<0.01 and P<0.05, respectively). Neither extraversion nor openness correlated with burnout in this sample.
Table 5.
Correlations between burnout and personality (correlation, P-value)
| Burnout
|
|||||||
|---|---|---|---|---|---|---|---|
| Accomplishment | Emotional exhaustion | Depersonalization | |||||
|
| |||||||
| Personality | Extraversion | 0.34 | NS | −0.13 | NS | 0.08 | NS |
| Agreeableness | 0.35 | <0.05 | −0.22 | NS | −0.40 | <0.01 | |
| Conscientiousness | 0.36 | <0.05 | −0.20 | NS | −0.32 | <0.05 | |
| Neuroticism | −0.39 | <0.01 | 0.59 | <0.001 | 0.42 | <0.01 | |
| Openness | 0.00 | NS | 0.13 | NS | 0.03 | NS | |
Abbreviation: NS, not significant.
Discussion
This study identified burnout as a common problem among primary care physicians and that the personality dimensions, neuroticism, agreeableness, and conscientiousness are correlated with primary care physician burnout.
Thirty-eight percent of participants scored low on the accomplishment scale, while 34% and 20%, respectively, scored high for emotional exhaustion and depersonalization, with no significant differences between Jamaican and Canadian participants. This high frequency of physician burnout among family physicians is consistent with previous surveys, for example, among US physicians5 and European family doctors.2 It also underscores the importance of better understanding this problem.
Among the potential causes of burnout is personality.19,20 The personality profile of the two physician groups was therefore explored. In this sample, mean scale scores for all personality types were between 3.0 and 4.0, with significantly higher scores on conscientiousness and a trend toward lower neuroticism among the Jamaican participants. This is in general agreement with Schmitt et al, who compared the big five personality traits across 56 nations.27 Unlike the trait extraversion, which demonstrated similar mean levels across most world regions including North America and Africa, the authors reported differences in mean neuroticism and conscientiousness scores between these regions. Specifically, the African region scored higher on conscientiousness and lower on neuroticism than all other world regions.27 Therefore, the differences reported here between Canada and Jamaica could simply reflect population-level variations based on cultural differences. The fact that this study did not also demonstrate differences in agreeableness and openness between the two populations may be due to the modest sample size.
Associations between personality and burnout have long been reported.24,25 In the present study, neuroticism was the only personality type associated with all three burnout dimensions; higher levels of neuroticism were associated with lower levels of accomplishment and higher levels of emotional exhaustion and depersonalization. This finding is consistent with recent studies of physicians17 and oncology nurses.28 Thirty years ago, McCranie and Brandsma also found correlations between burnout and several Minnesota Multiphasic Personality Inventory (MMPI) scales: obsessive worry, social anxiety, dysphoria, withdrawal from others, low self-esteem, passivity, and feelings of inadequacy.25 Neuroticism, as defined by the BFI, has been described to primarily comprise three facets, namely, anxiety, depression, and vulnerability,27 and it could be argued that the above-mentioned MMPI scales overlap conceptually with these BFI facets. In addition, it seems intuitive that these facets may impair one’s sense of accomplishment, particularly in a demanding and highly competitive profession. These occupational attributes could also negatively impact those who score high for neuroticism and increase the likelihood of emotional exhaustion and a sense of depersonalization.
On the contrary, both agreeableness and conscientiousness were positively correlated with accomplishment and negatively correlated with depersonalization. These findings are at odds with some studies. For example, conscientiousness was recently reported as a predictor of all three burnout dimensions among a group of health care employees, utilizing the inverse dimension “reduced personal accomplishment”.29 Others have reported negative correlations between all personality types (except neuroticism) and all three burnout dimensions, utilizing the Neuroticism-Extraversion-Openness Five-Factor Inventory questionnaire.28 Notwithstanding the different study populations and instruments used, these conflicting results suggest a need for larger studies to further evaluate this relationship.
To further assess potential contributory factors, other variables were examined. We found that males scored higher for accomplishment. The role of gender in physician burnout is not clear with studies reporting both males2 and females30 at increased risk. This together with the under-representation of males in this sample makes further interpretation challenging. Participants who saw >100 patients per week also scored higher for depersonalization, while this patient load was associated with lower agreeableness, compared with participants who saw 26–100 patients per week. This inverse relation above 100 patients is not surprising considering the negative correlation between agreeableness and depersonalization. Similarly, staff physicians not only scored higher on conscientiousness but also showed a non-significant trend toward higher accomplishment. Interestingly, increasing age was significantly associated with increased conscientiousness and reduced neuroticism. These findings are consistent with reported age-related changes in personality,31 although the present study did not find age-related changes in the other three dimensions. The reduced neuroticism with increased years of practice is possibly mediated by increasing age.
To the best of our knowledge, this is the first study to report an association between personality and burnout among primary care physicians in Canada and Jamaica; however, our findings correlated to those found among other health care providers. A recent study found that burnout was correlated with coping strategies that are emotion-focused, but negatively correlated with problem-focused strategies.17 These authors differentiated between emotion-focused approaches like helplessness, which attempt to reduce the distressing feelings, and problem-focused strategies that target the root cause of the stress, for example, by altering it. In addition to the predictive value of neuroticism, they reported that self-confidence and social support seeking approaches, both problem-focused strategies, were independent predictors of increased personal accomplishment. However, the self-confident approach protected against depersonalization, while the helpless approach, an emotion-focused strategy, was a predictor of increased emotional exhaustion. Given the apparent multifactorial etiology of burnout, possible interaction between personality and coping strategy in the development of burnout is plausible. Accordingly, promoting problem-focused strategies among physicians, for example, utilization of a support hotline or social support group, might mitigate the negative impact of certain personality traits on the risk of burnout.17
In fact, Deary et al reported emotion-oriented coping strategies as mediators of the relationship between neuroticism and job stress, while task-oriented strategies mediated the impact of conscientiousness on personal achievement.26 These findings suggest that the impact of personality traits that reduce burnout may be supported, and traits that promote burnout may be mitigated, by appropriate coping strategies. Such strategies that modulate the impact of personality on burnout may be beneficial for optimal health care delivery.
Limitations
This study had a few limitations. The low response rate and preponderance of females (79%) could limit the generalizability of our findings and should be considered in the interpretation of our results. In addition, the modest sample size limited the extent of analysis that was considered practical. Also, being a cross-sectional survey, causation cannot be inferred. It is therefore anticipated that a larger sample will be evaluated with a more robust study design, for example, a cohort study.
Conclusion
In this multisite study, we found that burnout was a common problem among primary care physicians. Personality, particularly neuroticism, agreeableness, and conscientious ness, impacted physician burnout. Strategies that modulate the impact of personality on burnout may be beneficial for optimal health care delivery.
Acknowledgments
We are grateful to all the primary care physicians and residents who participated in this study. Thanks also to SMH DFCM, McMaster Department of Family Medicine, CCFP (Jamaica chapter), and the family medicine program at the UWI, for their assistance with this study. Drs Brown and Slater received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors. Dr Lofters was supported by a New Investigator Award from the Canadian Institutes of Health Research and as a Clinician Scientist by the University of Toronto Department of Family & Community Medicine.
Footnotes
Author contributions
All authors contributed to data analysis, drafting and revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Freudenberger HJ. Staff burn-out. J Soc Issues. 1974;30(1):159–165. [Google Scholar]
- 2.Soler JK, Yaman H, Esteva M, et al. Burnout in European family doctors: the EGPRN study. Fam Pract. 2008;25(4):245–265. doi: 10.1093/fampra/cmn038. [DOI] [PubMed] [Google Scholar]
- 3.Maslach C, Jackson SE. The measurement of experienced burnout. J Organ Behav. 1981;2(2):99–113. [Google Scholar]
- 4.Asai M, Morita T, Akechi T, et al. Burnout and psychiatric morbidity among physicians engaged in end-of-life care for cancer patients: a cross-sectional nationwide survey in Japan. Psychooncology. 2007;16(5):421–428. doi: 10.1002/pon.1066. [DOI] [PubMed] [Google Scholar]
- 5.Shanafelt TD, Hasan O, Dyrbye LN, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general us working population between 2011 and 2014. Mayo Clin Proc. 2015;90(12):1600–1613. doi: 10.1016/j.mayocp.2015.08.023. [DOI] [PubMed] [Google Scholar]
- 6.Houkes I, Winants Y, Twellaar M, Verdonk P. Development of burnout over time and the causal order of the three dimensions of burnout among male and female GPs. A three-wave panel study. BMC Public Health. 2011;11(1):240. doi: 10.1186/1471-2458-11-240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chng CL, Eaddy S. Sensation seeking as it relates to burnout among emergency medical personnel: a Texas study. Prehosp Disaster Med. 1999;14(04):36–40. [PubMed] [Google Scholar]
- 8.Roberts DL, Shanafelt TD, Dyrbye LN, West CP. A national comparison of burnout and work-life balance among internal medicine hospitalists and outpatient general internists. J Hosp Med. 2014;9(3):176–181. doi: 10.1002/jhm.2146. [DOI] [PubMed] [Google Scholar]
- 9.Lee RT, Seo B, Hladkyj S, Lovell BL, Schwartzmann L. Correlates of physician burnout across regions and specialties: a meta-analysis. Hum Resour Health. 2013;11(1):48. doi: 10.1186/1478-4491-11-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Galam E, Komly V, Tourneur AL, Jund J. Burnout among French GPs in training: a cross-sectional study. Br J Gen Pract. 2013;63(608):e217–e224. doi: 10.3399/bjgp13X664270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nason GJ, Liddy S, Murphy T, Doherty EM. A cross-sectional observation of burnout in a sample of Irish junior doctors. Ir J Med Sci. 2013;182(4):595–599. doi: 10.1007/s11845-013-0933-y. [DOI] [PubMed] [Google Scholar]
- 12.Weng HC, Hung CM, Liu YT, et al. Associations between emotional intelligence and doctor burnout, job satisfaction and patient satisfaction. Med Educ. 2011;45(8):835–842. doi: 10.1111/j.1365-2923.2011.03985.x. [DOI] [PubMed] [Google Scholar]
- 13.Dyrbye LN, Shanafelt TD. Physician burnout: a potential threat to successful health care reform. JAMA. 2011;305(19):2009–2010. doi: 10.1001/jama.2011.652. [DOI] [PubMed] [Google Scholar]
- 14.Iliceto P, Pompili M, Spencer-Thomas S, et al. Occupational stress and psychopathology in health professionals: an explorative study with the multiple indicators multiple causes (mimic) model approach. Stress. 2013;16(2):143–152. doi: 10.3109/10253890.2012.689896. [DOI] [PubMed] [Google Scholar]
- 15.Rössler W. Depression und burnout. Praxis (Bern 1994) 2014;103(18):1067–1070. doi: 10.1024/1661-8157/a001776. [DOI] [PubMed] [Google Scholar]
- 16.Walocha E, Tomaszewski KA, Wilczek-Ruzyczka E, Walocha J. Empathy and burnout among physicians of different specialities. Folia Med Cracov. 2013;53(2):35–42. [PubMed] [Google Scholar]
- 17.Taycan O, Taycan SE, Çelik C. Relationship of burnout with personality, alexithymia, and coping behaviors among physicians in a semiurban and rural area in turkey. Arch Environ Occup Health. 2014;69(3):159–166. doi: 10.1080/19338244.2013.763758. [DOI] [PubMed] [Google Scholar]
- 18.Salazar IC, Roldan GM, Garrido L, Ramos-Navas Parejo JM. Assertiveness and its relationship to emotional problems and burnout in healthcare workers. Behav Psychology. 2014;22(3):523–549. [Google Scholar]
- 19.Alarcon G, Eschleman KJ, Bowling NA. Relationships between personality variables and burnout: a meta-analysis. Work Stress. 2009;23(3):244–263. [Google Scholar]
- 20.Armon G, Shirom A, Melamed S. The big five personality factors as predictors of changes across time in burnout and its facets. J Pers. 2012;80(2):403–427. doi: 10.1111/j.1467-6494.2011.00731.x. [DOI] [PubMed] [Google Scholar]
- 21.Coaley K. An Introduction to Psychological Assessment and Psychometrics. Los Angeles, CA: Sage; 2009. [Google Scholar]
- 22.John OP, Donahue EM, Kentle RL. The Big Five Inventory – Versions 4A and 54. Berkeley, CA: Institute of Personality and Social Research, University of California; 1991. [Google Scholar]
- 23.John OP, Robins RW, Pervin LA. Handbook of Personality: Theory and Research. New York, NY: Guilford Press; 2008. [Google Scholar]
- 24.Lemkau JP, Purdy RR, Rafferty JP, Rudisill JR. Correlates of burnout among family practice residents. J Med Educ. 1988;63(9):682–691. doi: 10.1097/00001888-198809000-00003. [DOI] [PubMed] [Google Scholar]
- 25.McCranie EW, Brandsma JM. Personality antecedents of burnout among middle-aged physicians. Behav Med. 1988;14(1):30–36. doi: 10.1080/08964289.1988.9935120. [DOI] [PubMed] [Google Scholar]
- 26.Deary IJ, Blenkin H, Agius RM, Endler NS, Zealley H, Wood R. Models of job-related stress and personal achievement among consultant doctors. Br J Psychol. 1996;87(Pt 1):3–29. doi: 10.1111/j.2044-8295.1996.tb02574.x. [DOI] [PubMed] [Google Scholar]
- 27.Schmitt DP, Allik J, McCrae RR, Benet-Martínez V. The geographic distribution of big five personality traits: patterns and profiles of human self-description across 56 nations. J Cross Cult Psychol. 2007;38(2):173–212. [Google Scholar]
- 28.De La Fuente-Solana EI, Gómez-Urquiza JL, Cañadas GR, Albendín-García L, Ortega-Campos E, Cañadas-de La Fuente GA. Burnout and its relationship with personality factors in oncology nurses. Eur J Oncol Nurs. 2017;30:91–96. doi: 10.1016/j.ejon.2017.08.004. [DOI] [PubMed] [Google Scholar]
- 29.Azeem SMDSM Conscientiousness, neuroticism and burnout among healthcare employees. IJARBSS. 2013;3(7):467–477. [Google Scholar]
- 30.Amoafo E, Hanbali N, Patel A, Singh P. What are the significant factors associated with burnout in doctors? OCCMED. 2015;65(2):117–121. doi: 10.1093/occmed/kqu144. [DOI] [PubMed] [Google Scholar]
- 31.McCrae RR, Costa PT, de Lima MP, et al. Age differences in personality across the adult life span: parallels in five cultures. Dev Psychol. 1999;35(2):466–477. doi: 10.1037//0012-1649.35.2.466. [DOI] [PubMed] [Google Scholar]