Abstract
The Adolescent Brain Cognitive Development (ABCD) Study, a large, longitudinal study of brain development and child health, is uniquely positioned to explore relationships among stress, neurodevelopment, and psychiatric symptomatology, including substance use and addiction. There is much we do not know about how adverse experiences affect the developing brain and cognitive, social, emotional, and academic outcomes. The data collected by the ABCD Study will allow the examination of the relationships among these variables in adolescence, including the effects of stressors (e.g., abuse, neglect, household challenges, parental substance use) on psychological adjustment and other stress responses. A comprehensive protocol that includes physical and mental health, substance use, culture and environment, neurocognitive assessments, biospecimen analyses, and structural and functional neuroimaging will provide opportunities for learning about the impacts of stressors on health and other outcomes in the context of adolescent development. This knowledge could lead to the development of interventions that reduce or even reverse the impacts of stressors.
Keywords: Adolescent, Development, Stress
1. Introduction
Over the last decade, converging evidence has emerged regarding links between early life trauma and alterations in brain structure and function (reviewed in Teicher and Samson, 2016). Indeed, a growing body of literature has provided support for the enduring effects of childhood adversity and maltreatment on stress-susceptible brain circuitry (Marusak et al., 2016; Shonkoff and Garner, 2012). Nonetheless, the exact pathways through which early life trauma influences brain development and behavior have yet to be delineated. The Adolescent Brain Cognitive Development (ABCD) Study (Volkow et al., 2018), the largest long-term study of brain development and child health in the United States, is uniquely positioned to explore relationships among stress (familial and extrafamilial, as well as environmental stressors), neurodevelopment, and psychiatric symptomatology, including substance use and addiction. ABCD Study Investigators at 21 research sites across the country are tracking the development of 11,876 children starting at ages 9–10 at regular intervals for a decade. Participants will undergo multimodal structural and functional neuroimaging; assessments of neurocognition, physical, and mental health (e.g., psychiatric symptomatology), substance use, and culture and environment (e.g., parental monitoring and family conflict); as well as biospecimen collection for hormonal, genetic, environmental exposure, and substance use confirmation (visit the ABCD Study website to view the study's assessment protocols https://abcdstudy.org/). The goal of the study is to understand the many disparate factors, such as stressful experiences and substance use, that affect brain, cognitive, social, and emotional growth and, in turn, overall health and well-being. To that end, the ABCD Study is collecting information from youth participants and their parents/guardians about stressful life events over time. Importantly, these data can be correlated with other measures such as neurodevelopment, mental and physical health, sleep, and risky behaviors throughout adolescence, as well as variables that may moderate or mediate the stress response, to better understand the relationships among adverse life events and health outcomes.
1.1. Stressors and stress responses
“Stress” is a broad term that encompasses “stressors,” which refer to adverse life events (also known as environmental stressors, childhood adversity) as well as “stress responses” or behavioral and biological responses to stressors. Stressful events are not all experienced the same way, nor do they have universally negative impacts on health outcomes. Acute, short-term stressors lasting minutes or hours (e.g., being excluded from an activity during recess; anticipating the first day of school after summer break; cramming for a final exam), may be experienced differently from a prolonged stressor that persists for days or even years (e.g., chronic bullying; food insecurity), and may be associated with distinct physiological and behavioral responses (McEwen, 2007). Research has shown that there may be evolutionary advantages to some types of stress responses, but not others. For example, acute stress may activate “fight or flight” systems in the body associated with enhanced immune functioning. A recent study found that patients undergoing knee surgery recovered more quickly and completely if they mounted a robust short-term stress response where large numbers of immune cells mobilized to fight infection (Rosenberger et al., 2009). Subsequent research found that a temporary spike in cortisol levels following an induced mild stressor in rats (brief confinement to a small cage) led to a temporary boost in immune response (Dhabhar et al., 2012). Conversely, chronic stressors, such as witnessing ongoing violence in the family, can lead to chronic inflammation and increase the risk for autoimmune conditions and other diseases (e.g., Carlsson et al., 2014). Whereas short-term stress responses may have protective value since brief stimulation of the immune system prepares the body to fight infection and flee danger, responses to severe or chronic stressors may overtax the immune system and lead to negative health outcomes, including neurobiological alterations and early mortality (Chetty et al., 2016; Marmot et al., 1991; Mersky et al., 2013).
Here, we review classes of stressors (early life adversity, mass trauma) and their potential impact on health outcomes. We then describe elements of the ABCD Study protocol that assess exposures and outcomes (e.g., psychiatric symptomatology, neurodevelopment and onset of substance use), summarize preliminary baseline descriptive data from four domains that capture exposure to stressors (family conflict, food insecurity, history of parental substance use, history of parental depression), and describe two ABCD substudies that examine specific predictors of stress responses. We conclude with a brief look toward the future of the ABCD Study.
1.2. Early life adversity
Extensive research has demonstrated acute and chronic effects of persistent environmental stressors on health outcomes, including immune functioning, mental health, and neurodevelopment. A range of adverse childhood experiences (ACEs), including physical and sexual abuse, witnessing a crime, parental substance abuse, prolonged absence of parent, and frequent family conflict, are associated with increased risk for premature mortality and the presence of major non-communicable diseases (Mersky et al., 2013). Different forms of early life adversity are also suggested to uniquely impact the brain both structurally and functionally, contingent upon the characteristics of the stressor, e.g. age of onset, duration and frequency of exposure (Callaghan and Tottenham, 2016; Teicher and Samson, 2016). Moreover, Kisiel et al. (2014) suggest that cumulative stress is a risk factor for future psychopathology; however, impairment may result even when stress burden is not cumulative.
Stressors that may be more universally experienced in adolescence, such as perceived valuation from one's peers, can also impact stress burden and thus future health (McEwen, 2007). For example, in response to an experimental social stressor where participants gave a speech in front of a young adult viewer who evaluated their performance, female adolescents at risk for psychopathology exhibited increases in pro-inflammatory cytokines (i.e. IL-6 and IL1-b) that positively correlated with self-reported peer victimization exposure and perceived social status (Giletta et al., 2018). Long-term prospective work has shown that individuals exposed to peer victimization during childhood and adolescence display higher levels of low-grade systemic inflammation than their non-affected peers, even in adulthood, and that early peer victimization affects physical health and mental health outcomes, including internalizing (e.g., anxiety, depression) and externalizing disorders (e.g., aggression, delinquency), as well as academic achievement (reviewed in McDougall and Vaillancourt, 2015). In sum, the pressures of daily life, especially during adolescence, can lead to a “chronic stress burden” that is associated with poor health outcomes (McEwen, 2012).
1.3. Mass trauma
While traditionally studied within the immediate family and community, the impact of trauma on a large scale has been captured in response to natural disasters, acts of terrorism, and political stressors. Among nearly 400 low-income predominately African American single mothers who survived Hurricane Katrina, serious mental illness doubled, and more than half met diagnostic post-traumatic stress disorder (PTSD) criteria in response to the event (Rhodes et al., 2010). This symptomatology persisted over a year after the event, and physical illness and general health also worsened during this time (Rhodes et al., 2010). As this event was so widespread and catastrophic, pre-hurricane economic, social, and health resources were not significant in moderating the impact of Katrina on physical and mental health. Similar findings regarding prolonged PTSD were evident among a sample of 130 survivors of Hurricane Sandy in 2012 (Schwartz et al., 2017).
Studies also have looked at the impact of large disasters on brain structure and psychiatric symptomatology. In 2003, one hundred ninety-two individuals died, and hundreds were injured as a result of arson to two subway trains in South Korea. Over five years, Lyoo et al. (2011) examined structural brain morphometry among thirty survivors of the trauma and thirty-six matched controls. At the time of the trauma, all survivors met diagnostic criteria for PTSD, the prevalence of which diminished to 12% in three years. Survivors demonstrated greater cortical thickness in the dorsolateral prefrontal cortex (DLPFC), a brain region implicated in fear extinction learning, than controls one year after trauma exposure. DLPFC thickness early in the course of PTSD was positively correlated with PTSD symptom reduction several years later, even though DLPFC thickness gradually normalized to the level of controls. This finding suggests that greater neural recruitment of this region early on may have led to more pronounced symptom improvements. However, because brain imaging was not done on this cohort before trauma exposure, it is difficult to rule out the possibility that DLPFC thickness was a preexisting vulnerability factor for PTSD development (Lyoo et al., 2011).
1.4. Contributions of the ABCD Study to understanding impacts of adverse experiences
Adverse experiences are complex and multidimensional, and can occur within the family, among peers, and at the community-level. Over 20% of U.S. children will experience two or more adverse experiences in their childhood which makes them especially vulnerable to poor health outcomes (Child and Adolescent Health Measurement Initiative, 2013). The impact of these experiences may be felt beyond the developmental years, particularly when they occur early in life or during other sensitive periods, e.g., puberty (Blakemore et al., 2010; Tyborowska et al., 2018). There is much we do not know about how adversity affects the developing brain and cognitive, social, emotional, health and academic outcomes. The ABCD Study is uniquely positioned to examine the relationships among these variables as participants experience adolescence, and to address the question of whether some factors contribute to adjustment or maladjustment more than others. For example, the protocol includes assessments of family conflict, food insecurity, and history of parental substance use and mental illness (described in detail in Sections 2, 3) to gather a range of data about a child's exposure to adversity, both past (“have you ever experienced …“) and current. These data can then be correlated prospectively with indices of brain and cognitive development, as well as social, emotional, health, and academic outcomes. The study also will address possible indicators of vulnerability and plasticity of stress-susceptible brain circuitry, as well as potential moderating factors of chronic stress, such as social resiliency, involvement in sports and other recreational activities, and environmental factors such as neighborhood and school safety (see Section 3).
2. Assessing childhood stress in the ABCD protocol – exposures and outcomes
The ABCD protocol includes both categorical and dimensional assessment approaches (See Barch et al., 2018) to measure exposure to ACEs and their potential outcomes. Collectively, the exposure measures capture domains from the CDC - Kaiser ACE Study – abuse, household challenges, and neglect (Felitti et al., 1998) – and are summarized in Table 1.
Table 1.
Childhood stress exposure domains in the ABCD study.
| Adverse Childhood Experiences (ACEs) Domaina | ABCD Baseline Assessment (Parent, Youth) | Description |
|---|---|---|
| Abuse: | ||
| Emotional abuse | Not assessed | N/A |
| Physical abuse | Family Environment Scale (parent and youth); KSADS-5, PTSD module (parent) | Social-environmental characteristics of family function; youth exposure to and experience of trauma |
| Sexual abuse | KSADS-5, post-traumatic stress disorder module (parent) | Youth exposure to and experience of trauma |
| Household Challenges: | ||
| Mother treated violently | KSADS-5, PTSD module (parent) | Youth exposure to and experience of trauma |
| Household substance abuse | Family History Assessment; Adult Self-report (parent) | Family history of psychopathology and substance use; criminal behavior |
| Mental illness in household | Family History Assessment; Adult Self-report (parent) | Family history of psychopathology and substance use; criminal behavior |
| Parental separation or divorce | Demographics Survey (parent) | Family demographics, including race, gender, family structure, SES, education and occupation |
| Criminal household member | Family history Assessment (parent) | Family history of psychopathology and substance use; criminal behavior |
| Neglect: | ||
| Emotional neglect | CRPBI Acceptance Subscale (youth) | Youth perception of caregiver acceptance |
| Physical neglect | Parental Monitoring (youth); Demographics Survey (parent) | Youth perception of parental supervision; family demographics (economic hardship, e.g., food insecurity) |
All ACE questions refer to the respondent's first 18 years of life.
2.1. Exposure to adverse childhood experiences
The ABCD protocol (Barch et al., 2018; Zucker et al., 2018) captures information about adverse childhood experiences at the individual, family, peer, and community levels from both the youth and parents/guardians at various timepoints of the study. At baseline when the youth are 9–10 years old, individual traumatic experiences are assessed using parent-report in the post-traumatic stress disorder module of the Kiddie Schedule for Affective Disorders and Schizophrenia for DSM-5 (KSADS-5). At the one-year follow-up, youth and parents/caregivers complete a self-administered computerized version of the Life Events Scale, which describes stressful experiences, and youth complete the self-administered Delinquency Scale to assess criminal/violent behavior. At the family level, demographics and family history surveys collect information from parents/caregivers about a range of experiences, such as family history of depression, or problems due to substance use, such as school expulsion, divorce, arrests, being laid off from a job, etc., as well as whether families have experienced food insecurity. Youth also complete the Family Conflict Subscale from the Family Environment Scale, a 9-item categorical assessment of perceived conflict within the family. On the neighborhood/community level, parents and youth complete the Neighborhood Safety/Crime Survey, a dimensional assessment that consists of a single question, “my neighborhood is safe from crime.” Additionally, youth complete the School Risk and Protective Factors Survey, a 12-item dimensional assessment of feelings and perceptions associated with being in school, including exposure to substance use risk. See Zucker et al. (2018) for more detail on the culture and environment assessments that were selected for inclusion in the ABCD protocol.
2.2. Potential outcomes from adverse childhood experiences
In addition to assessing exposure to adverse experiences, the ABCD protocol includes measures that evaluate health outcomes throughout adolescence. Questionnaires from the Achenbach System of Empirically Based Assessment (ASEBA) measures are administered to obtain quantitative, multi-informant assessments of psychopathology that are normed by sex, age, and ethnicity. Specifically, parents/guardians complete the Child Behavior Checklist (CBCL) and teacher reports are collected using the Brief Problem Monitor (BPM-T) (Achenbach, 2009). Both measures assess dimensional psychopathology and adaptive functioning. In addition, youth complete a 20-item brief version of the UPPS Impulsive Behavior Scale (Cyders et al., 2014), as well as an abridged version of the Behavioral Inhibition System/Behavioral Activation System (BIS/BAS) scale (Carver and White, 1994; Pagliaccio et al., 2015). These latter two measures yield dimensional assessments of impulsivity-related behavior. Finally, parents/guardians and youth complete modules from the KSADS-5 to assess symptoms of mental illness (e.g., depression, anxiety) and substance use. See Barch et al. (2018) for more information about how and why these measures were selected.
The protocol combines comprehensive characterizations of physical and mental health with state-of-the-art multimodal neuroimaging techniques. The neuroimaging protocol includes high-resolution T1-and T2-weighted magnetic resonance imaging (MRI), advanced diffusion imaging, resting state functional MRI, and task-based functional MRI (see Casey et al., 2018). Functional neuroimaging tasks include the Stop Signal Task (SST), the Emotional N-Back (EmoN-back) Task, and the Monetary Incentive Delay (MID) Task. These tasks probe neural systems underpinning response inhibition and cognitive control, working memory, and reward processing—systems that are intricately tied to stress-susceptible prefrontal circuitry. As reviewed recently by Teicher and Samson (2016), several consistent findings coalesce from task-based functional neuroimaging studies of early life stress and maltreatment. First, numerous studies have reported heightened amygdala reactivity to emotional faces among maltreated individuals. Second, studies have reported decreased activation in striatal regions during the anticipation of reward among maltreated individuals. Resting state functional imaging and diffusion imaging provide opportunities to examine linkages between early life stress and alterations in functional and structural connectivity—particularly within fronto-limbic circuitry. Application of social network analysis and graph theoretical approaches to these data (see He and Evans, 2010) will make it possible to model the influence of early life stress and maltreatment on the developing brain's network architecture. Given the prospective longitudinal nature of the ABCD Study, these data will undoubtedly shed light on the causal pathways linking types of early life stress to changes in brain structure and function, and, ultimately, to the emergence of stress-related psychiatric symptomatology.
2.3. Potential moderators and mediators of outcome variables
The protocol also includes assessments of social support, exercise behavior, sleep quality, involvement in sports and the arts, parental monitoring and supervision, as well as electronic device usage and exposure to visual and social media—variables that may play a moderating role in the relationships among early life stress, brain structure and function, and behavior. Potential mediating variables also are assessed, including household education, income, family structure, family history of psychopathology and substance use, and environmental toxin exposure via deciduous (baby) teeth.
3. Preliminary baseline descriptive data
The diversity of the ABCD Study cohort makes it possible to answer a wide array of questions regarding exposure to stressors and to track potential outcomes as the participants move through adolescence into young adulthood. Summary baseline data from four domains that capture exposure to ACEs (family conflict, food insecurity, history of parental substance use, history of parental depression) reveal a range of experiences among approximately 4,500 participants at the time of their baseline visits when they were 9–10 years-old. The data come from the first (interim) annual curated data release and are available through the NIMH Data Archive website: https://data-archive.nimh.nih.gov/abcd. The ABCD Study is designed to include a diverse population that reflects the demographics of the U.S. (Garavan et al., 2018), however because enrollment was not complete at the time of the first data release, these data may not reflect the final cohort. The interim release includes baseline data on 4,524 participants, including 870 twins/multiples, less than half of the total enrollment of 11,876 (see Table 2, Table 3, Table 4 for participant demographics at time of interim data release).
Table 2.
Demographics of ABCD baseline data (n = 4,524): Participant sex.
| Sex | Total | Singletons | Twins/Multiples | ACSa |
|---|---|---|---|---|
| Male | 52.4% | 53.3% | 48.4% | 51.2% |
| Female | 47.5% | 46.5% | 51.6% | 48.8% |
ACS = American Community Survey: https://www.census.gov/programs-surveys/acs/.
Table 3.
Demographics of ABCD baseline data (n = 4,524): Household education.
| Education | Total | Singletons | Twins/Multiples | ACSa |
|---|---|---|---|---|
| <12th grade | 3.9% | 4.4% | 2.2% | 8.0% |
| HS or GED | 7.2% | 8.0% | 4.0% | 18.1% |
| Some College | 24.9% | 25.3% | 23.0% | 34.9% |
| Bachelor's Degree | 27.0% | 25.5% | 33.6% | 22.0% |
| Master's/Professional Degree | 30.1% | 30.5% | 32.6% | 15.1% |
| Doctoral Degree | 6.0% | 6.3% | 4.6% | 2.0% |
ACS = American Community Survey: https://www.census.gov/programs-surveys/acs/.
Table 4.
Demographics of ABCD baseline data (n = 4,524): Participant race/ethnicity.
| Race/Ethnicity | Total | Singletons | Twins/Multiples | ACSa |
|---|---|---|---|---|
| White | 58.6% | 55.4% | 72.1% | 52.4% |
| Black | 9.7% | 9.6% | 10.2% | 13.4% |
| Hispanic | 19.7% | 22.3% | 8.6% | 24.0% |
| Asian | 2.3% | 2.7% | 0.46% | 4.7% |
| Mixed | 8.6% | 8.7% | 8.0% | 4.2% |
| American Indian Alaska Native | 0.29% | 0.29% | 0.0% | 0.8% |
| Native Hawaiian Pacific Islander | 0.11% | 0.11% | 0.0% | 0.2% |
| Other | 0.53% | 0.57% | 0.3% | 0.3% |
ACS = American Community Survey: https://www.census.gov/programs-surveys/acs/.
3.1. Exposure to ACEs
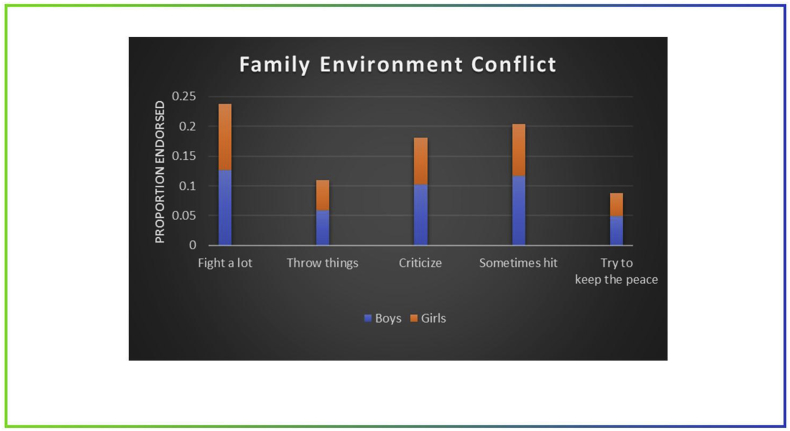
Preliminary data from the Family Conflict subscale of the Family Environment Scale and a food insecurity question provide a window into the family environment in which these first ∼4,500 participants live. The Family Conflict subscale (administered to youth) measures how family members communicate with one another during disagreements or conflict. Approximately 25% of the participants reported that their family fights a lot. About 10% said that family members sometimes throw things at each other out of anger. Over 15% said that family members often criticize each other, and 25% said that they sometimes hit each other. Ten percent said that the family makes efforts to “keep the peace” when there are disagreements (Fig. 1). For the food insecurity question of the Demographics Survey (administered to parent/guardian), 6% of parents/guardians reported at least one instance of food insecurity in the past 12 months where the immediate family needed food but could not afford to buy it.
Fig. 1.
Family environment scale. Family conflict subscale.
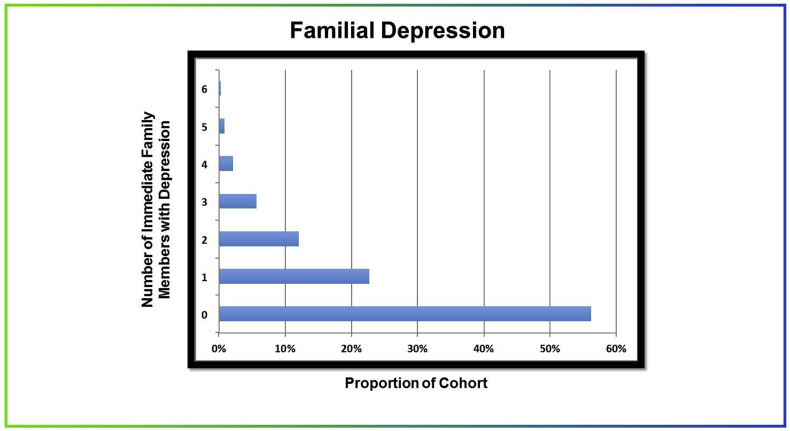
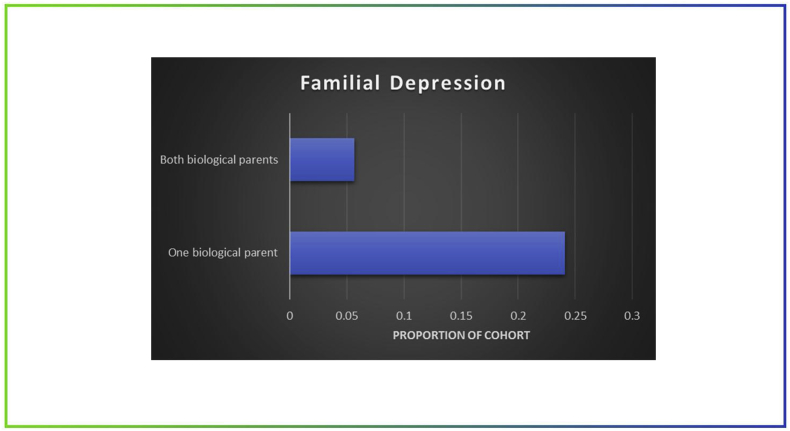
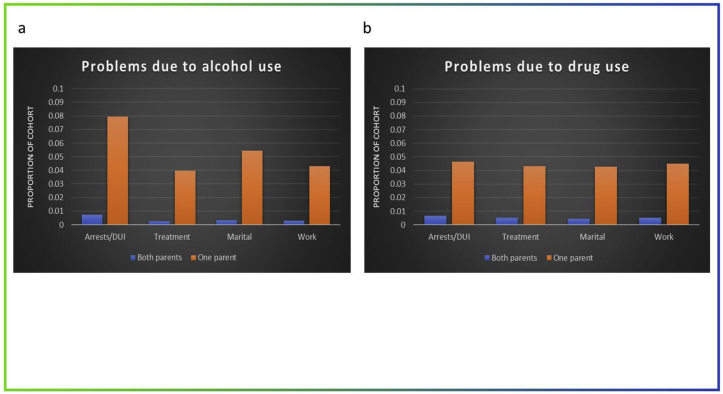
Additional assessments describe family history of depression and substance use that can impact the family environment. Fig. 2 shows the proportion of the cohort with up to 6 immediate family members with a history of depression. Approximately 24% said one biological parent has suffered from depression symptoms at some point. Five percent said that both parents have (Family History Assessment (parent); Fig. 3). Finally, the substance use questions in the Family History Assessment (administered to parent/guardian) ask about substance use in biological relatives and its impact: “Has any blood relative of child had any problems due to alcohol (drugs), such as marital separation or divorce; being laid off or fired from work; arrests or DUIs; alcohol (drugs) harmed their health; in an alcohol (drug) treatment program; suspended or expelled from school 2 or more times; isolated self from family, caused arguments or were drunk (high) a lot.” Fig. 4 shows the proportion of the cohort with a parent who experienced DUI, substance use treatment, separation or divorce, or work problems due to substance use. Approximately 8% said one biological parent ever had an arrest or DUI while drunk (Fig. 4a); about 5% said one biological parent ever had an arrest or DUI while high (Fig. 4b). Although we cannot speculate on the significance or the long-term impact of these experiences at this early stage, follow-up assessments will help determine what kinds of stressors confer enduring risk for negative social and health outcomes over time, as well as whether other factors moderate or mediate these outcomes.
Fig. 2.
Family history assessment. History of depression symptomatology.
Fig. 3.
Family history assessment. History of depression symptomatology.
Fig. 4.
Family history assessment. History of parental problems due to substance use*.
* such as material separation or divorce; being laid off or fired from work: arrests or DUIs; alcohol (drugs) harmed their health; in an alcohol (drug) treatment program; suspended or expelled from school 2 or more times; isolated self from family, caused arguments or were drunk (high) a lot.
3.2. Potential outcomes from ACEs
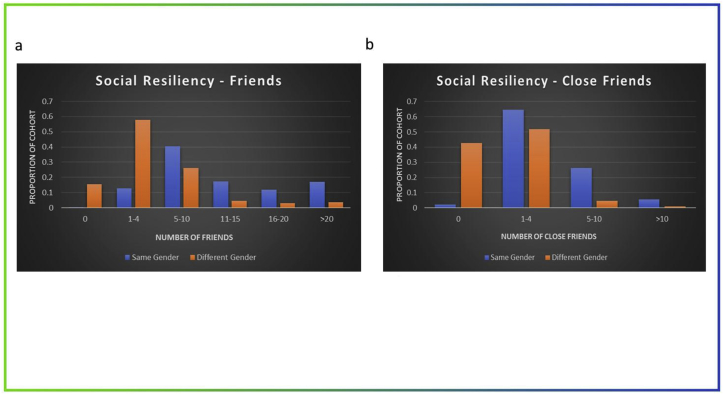
A range of experiences define the ABCD cohort at this age. The benefit of a longitudinal design is that we can examine various outcome variables (e.g., psychiatric symptomatology, neurodevelopment, onset of substance use) as participants develop, as well as potential moderators and mediators of these outcome variables (e.g., participation in sports or the arts; social support; socioeconomic status; cognitive vulnerability). One question that could be asked, for example, is whether social support moderates the relationship between family conflict and onset of substance use. At baseline assessment, most participants reported having at least one same-gender friend (Youth Resilience Scale, Fig. 5). However, a small proportion (2%; n = 95) reported having zero same-gender close friends (Fig. 5b). Without the protective value of social support from their peers, these individuals could be more susceptible to long-term negative health outcomes (Ozbay et al., 2008). Many other questions about the relationship between ACEs and development can be addressed by this study, such as 1) Does parental substance use predict delinquency or victimization in adolescence? Is that relationship moderated by positive environmental factors, like peer friendships, involvement in after-school activities, etc.? 2) How does early life stress lead to changes in brain structure and function, and, ultimately, to the emergence of stress-related psychiatric symptomatology? 3) What is the relationship between early life stress and neural systems underpinning response inhibition and cognitive control, working memory, and reward processing—systems that are intricately tied to stress-susceptible prefrontal circuitry? 4) Do neighborhood characteristics (e.g., crime and safety; local drug laws and policies) mediate the relationship between early life adversity and substance use?
Fig. 5.
Youth Resilience Scale. Number of Friends (a) and Number of close Friends (b).
4. ABCD substudies – examining predictors of stress response
ABCD Study investigators interested in extending the scope of ABCD Study objectives may conduct substudies of the cohort if they do not increase participant burden or otherwise interfere with the original ABCD Study design. Described below are two substudies that are conducting more in-depth assessments of exposure to specific adverse events and potential social and health outcomes over time.
4.1. Natural disaster exposure
The impact of mass trauma on exposed individuals can be severe and persistent and may lead to poor health outcomes later in life (see Section 1.3 for review). In September 2017, the Southeastern United States experienced the effects of Hurricane Irma, the largest Atlantic hurricane on record. This massive storm led to the largest human evacuation in American history (∼7 million people) and made landfall in the Florida Keys as a Category 4 Hurricane. The storm caused 92 deaths in the contiguous U.S., as well as extensive damage from significant flooding, storm surge, and high winds. Three of the 21 ABCD Study sites were directly affected - Florida International University (Miami, Florida), the University of Florida (Gainesville, Florida), and the Medical University of South Carolina (Charleston, South Carolina).
Before Hurricane Irma hit Florida, 545 9- and 10-year-old children and their families at the three affected sites had completed the full baseline protocol, including neuroimaging, for the ABCD Study. A substudy for ABCD was funded by the National Science Foundation RAPID grant (#1805645) to understand how Hurricane Irma affected these youth, as well as a demographically-matched site that was not directly affected by the hurricane (University of California at San Diego; n = 335). Three-hundred eighty-seven youth and 439 of their parents at the four sites completed online surveys of their experiences during the Hurricane to assess hurricane-related traumatic exposure and evacuation stress, as well as brief screeners to assess posttraumatic stress symptoms, hurricane-related media exposure, and mood/behavior problems. Data from these participants will provide information about how variations in disaster exposure can affect structural and functional brain development, and cognitive and affective development, as well as how pre-disaster neural and cognitive factors may predict and/or moderate the effects of disasters on youth psychological responses. Preliminary results suggest that Hurricane Irma exposure predicts post-Irma PTSD symptoms among South Florida youth (r = 0.23, p < 0.01) and that Irma-related media exposure predicts post-Irma PTSD symptoms among youth near (r = 0.31, p < 0.001) and far (r = 0.36, p < 0.001) (Dick and Comer, 2018). As part of the longitudinal design of the ABCD Study, these same children have either completed their first annual follow-up assessments or will complete them in the coming months and will undergo repeat neuroimaging at their two-year follow-up to allow for prospective analyses. The substudy also will identify factors that promote resilience in children who experience trauma from natural disasters.
4.2. Social development, delinquency and victimization
The age-crime curve peaks during the critical adolescent period (Loeber et al., 2017). Deficits in brain functions that provide foundations for executive functioning and reward processing have been hypothesized to contribute to adolescent delinquency as well as accelerated substance use involvement (Clark et al., 2013; Hyde et al., 2013). Conversely, adolescent substance use may exacerbate neurobiological vulnerabilities by disrupting the development of maturing executive control and reward processing systems (Koob and Volkow, 2010). While observational studies have inherent limitation in clarifying causal relationships, initiating assessments prior to the onset of significant substance use facilitates the examination of chronological sequences involving victimization, substance use, and subsequent mental and physical health consequences (Clark and Winters, 2002; Clark et al., 2003, 2010).
The National Institute of Justice [NIJ: 2017-MU-CX-0044], with additional support from the Centers for Disease Control and Prevention, is supporting a substudy, ABCD Social Development (ABCD-SD), within ABCD to advance understanding of the relationships among adolescent risk characteristics, substance use, delinquency and victimization, and brain development. Specifically, ABCD-SD will examine the extent to which premorbid brain deficits, expressed through neurocognitive and psychological dysfunction, predict delinquency and early substance use. The participating ABCD Study sites are the University of Pittsburgh [Coordinating Center], University of Michigan, Yale University, University of Florida, and University of Maryland-Baltimore. ABCD-SD will involve a projected total of 2,700 participants, who will be 11-12 years-old at their first substudy assessment visit.
Particularly relevant to the focus of this paper, ABCD-SD will contribute to the understanding of responses to victimization by providing a detailed evaluation covering a range of severity, and by examining effects in the context of adolescent cognitive and brain development. Childhood and adolescent victimization experiences have been found to be associated with increased substance use, with more severe traumas showing greater adverse effects (Clark et al., 2010; Scheidell et al., 2017). To understand multiple types of victimization and their potential outcomes, several subscales from the Juvenile Victimization Questionnaire (JVQ) (Finkelhor et al., 2005) are included in the ABCD-SD protocol: Conventional crime, Peer and sibling victimization, Peer aggression (including social aggression), Witnessing (exposure) and indirect victimization, Gun violence (including exposure), School violence and threat, and Internet victimization. The JVQ includes detailed follow-up questions to determine the circumstances and context where any victimization occurred. All the assessments are administered to both youth and parent/guardian. Youth also will complete the Peer Delinquent Behavior survey from the Rochester Youth Study (Thornberry et al., 1994) to examine the influence of variations in peer characteristics on the development of delinquency and victimization in adolescence. The supplemental measures on delinquency, victimization and related risks will be collected at annual assessments.
Other issues related to delinquency and victimization may be addressed through analyses with data from the main ABCD Study. For example, information about some types of victimization, including physical and sexual abuse, are collected across all ABCD sites (see Table 1). Since parental substance use may contribute to both early victimization and substance use through multiple mechanisms (Sher et al., 1997), consideration of environmental and genetic influences would clarify their relationship. Environmental influences on substance use initiation, such as substance use availability (Lisdahl et al., 2018) and neighborhood characteristics (Zucker et al., 2018), are also assessed across sites. The inclusion of monozygotic and dizygotic twin pairs will inform the examination of genetic and environmental contributions to developmental associations (Iacono et al., 2018), such as relationships among delinquency, victimization and substance use. However, the assessment of delinquency and victimization in the core ABCD assessment is limited. Expansion of data collection on these constructs strengthens the capabilities of the ABCD Study to contribute to the understanding of the development of delinquency and the factors that influence the occurrence and responses to victimization.
By providing a thorough account of delinquency and victimization over time in the context of the ABCD Study protocol, ABCD-SD will advance understanding of the interactions among substance use, delinquency, victimization, and brain development in adolescence.
5. Summary and future directions
The ABCD Study provides opportunities for learning about the impact of stress exposures on health and other outcomes in the context of adolescent development. Understanding the relationships among these variables could lead to the development of interventions that reduce or even reverse the impacts of stressors. For example, previous studies suggest that stress-reducing interventions can alter brain morphometry. A recent study found that while poverty and unenriched environments have been associated with volume reductions in the hippocampus and amygdala, supportive parenting (in terms of emotions and behaviors) during adolescence has been shown to attenuate these disparities (Brody et al., 2017).
Although most of the assessments in the ABCD protocol will be repeated at each annual visit, we expect that there will be modifications in response to maturation of the participant cohort, as well as advances in scientific knowledge and data collection tools. The 2-year follow-up protocol, which is administered to participants when they are 11–12 years-old, has additional measures that delve more deeply into peer relationships (including victimization), gender identity, and mobile technology (including screen time, social media use, and cyberbullying), as well as blood pressure measurements to assess hypertension.
Investigators interested in these topics can access and analyze data via the NIMH Data Archive website: https://data-archive.nimh.nih.gov/abcd. Fast-track data containing unprocessed neuroimaging data from study participants to date (high-resolution structural MRI, advanced diffusion MRI, resting state fMRI, and task fMRI), as well as basic participant demographics (age, sex), will continue to be released on an ongoing basis. The second annual curated data release in spring of 2019 includes baseline data from the full participant cohort, including data related to physical & mental health, substance use, culture and environment, neurocognition, and biospecimen analyses, as well as minimally processed brain image volumes and tabulated magnetic resonance imaging data.
Acknowledgements
Data used in the preparation of this article were obtained from the Adolescent Brain Cognitive Development (ABCD) Study (https://abcdstudy.org), held in the NIMH Data Archive (NDA). This is a multisite, longitudinal study designed to recruit more than 10,000 children age 9–10 and follow them over 10 years into early adulthood. The ABCD Study is supported by the National Institutes of Health and additional federal partners under award numbers U01DA041022, U01DA041028, U01DA041048, U01DA041089, U01DA041106, U01DA041117, U01DA041120, U01DA041134, U01DA041148, U01DA041156, U01DA041174, U24DA041123, and U24DA041147. A full list of supporters is available at https://abcdstudy.org/federal-partners.html. A listing of participating sites and a complete listing of the study investigators can be found at https://abcdstudy.org/Consortium_Members.pdf. ABCD consortium investigators designed and implemented the study and/or provided data but did not necessarily participate in analysis or writing of this report. Representatives from NIDA contributed to the interpretation of the data and participated in the preparation, review and approval of the manuscript. Dr. Elizabeth Hoffman was substantially involved in all of the cited grants consistent with her role as a Scientific Officer. This manuscript reflects the views of the authors and may not reflect the opinions or views of the NIH, its affiliated Institutes, Centers or offices, or ABCD consortium investigators. The ABCD data repository grows and changes over time. The ABCD data used in this report came from NIMH Data doi:https://doi.org/10.15154/1412097.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ynstr.2019.100157.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Achenbach T.M. University of Vermont Research Center for Children, Youth & Families; Burlington, VT: 2009. The Achenbach System of Empirically Based Assessment (ASEBA). Development, Findings, Theory, and Applications. [Google Scholar]
- Barch D. Demographic, physical and mental health assessments in the adolescent brain and cognitive development study: rationale and description. Develop. Cogn. Neurosci. 2018;32:55–66. doi: 10.1016/j.dcn.2017.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blakemore S.J., Burnett S., Dahl R.E. The role of puberty in the developing adolescent brain. Hum. Brain Mapp. 2010;31(6):926–933. doi: 10.1002/hbm.21052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brody G.H. Protective prevention effects on the association of poverty with brain development. JAMA Pediatr. 2017;4527(1):46–52. doi: 10.1001/jamapediatrics.2016.2988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Callaghan B.L., Tottenham N. The Stress Acceleration Hypothesis: effects of early-life adversity on emotion circuits and behavior. Curr. Opin. Behav. Sci. 2016;7:76–81. doi: 10.1016/j.cobeha.2015.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlsson E., Frostell A., Ludvigsson J., Faresjo M. Psychological stress in children may alter the immune response. J. Immunol. 2014 doi: 10.4049/jimmunol.1301713. [DOI] [PubMed] [Google Scholar]
- Carver C.S., White T.L. Behavioral inhibition, behavioral activation, and affective responses to impending reward and punishment: the BIS/BAS scales. J. Personal. Soc. Psychol. 1994;67:319–333. [Google Scholar]
- Casey B.J. The adolescent brain cognitive development (ABCD) study: imaging acquisition across 21 sites. Develop. Cogn. Neurosci. 2018;32:43–54. doi: 10.1016/j.dcn.2018.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chetty R., Stepner M., Abraham S., Lin S., Scuderi B., Turner N., Bergeron A., Cutler D. The association between income and life expectancy in the United States, 2001-2014. J. Am. Med. Assoc. 2016;315(16):1750–1766. doi: 10.1001/jama.2016.4226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Child and Adolescent Health Measurement Initiative . Data Resource Center, U.S. Department of Health and Human Services, Health Resources and Services Administration, Maternal and Child Health Bureau; 2013. Overview of Adverse Child and Family Experiences Among US Children. [Google Scholar]
- Clark D.B., Winters K.C. Measuring risks and outcomes in substance use disorders prevention research. J. Consult. Clin. Psychol. 2002;70(6):1207–1223. doi: 10.1037//0022-006x.70.6.1207. [DOI] [PubMed] [Google Scholar]
- Clark D.B., De Bellis M.D., Lynch K.G., Cornelius J., Martin C. Physical and sexual abuse, depression and alcohol use disorders in adolescents. Drug Alcohol Depend. 2003;69:51–60. doi: 10.1016/s0376-8716(02)00254-5. [DOI] [PubMed] [Google Scholar]
- Clark D.B., Thatcher D.L., Martin C.S. Child abuse and other traumatic experiences, alcohol use disorders, and health problems in adolescence and young adulthood. J. Pediatr. Psychol. 2010;35(5):499–510. doi: 10.1093/jpepsy/jsp117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark D.B., Chung T., Pajtek S., Zhai Z., Long E., Hasler B. Neuroimaging methods for adolescent substance use disorder prevention science. Prev. Sci. 2013;14:300–309. doi: 10.1007/s11121-012-0323-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cyders M., Littlefield A., Coffey S., Karyadi K. Examination of a short English version of the UPPS-P impulsive behavior scale. Addict. Behav. 2014;39(9):1372–1376. doi: 10.1016/j.addbeh.2014.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dhabhar F.S., Malarkey W.B., Neri E., McEwen B.S. Stress-induced redistribution of immune cells – from barracks to boulevards to battlefields: a tale of three hormones. Psychoneuroendocrinology. 2012;37(9):1345–1368. doi: 10.1016/j.psyneuen.2012.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dick A.S., Comer J.S. Presented at the Coalition for National Science Funding Exhibition on Capitol Hill. Washington, DC. 2018. Leveraging the ABCD study to examine the effects of hurricane Irma exposure: the disaster and youth, neural and affective maturation in context (dynamic) study. [Google Scholar]
- Felitti V.J., Anda R.F., Nordenberg D., Williamson D.F., Spitz A.M., Edwards V., Koss M.P., Marks J.S. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am. J. Prev. Med. 1998;14(4):245–258. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- Finkelhor D., Ormrod R., Turner H., Hamby S. The victimization of children and youth: a comprehensive, national survey. Child. Maltreat. 2005;10(1):5–25. doi: 10.1177/1077559504271287. [DOI] [PubMed] [Google Scholar]
- Garavan H., Bartsch H., Conway K., Decastro A., Goldstein R.Z., Heeringa S., Jernigan T., Potter A., Thompson W., Zahs D. Recruiting the ABCD sample: design considerations and procedures. Develop. Cogn. Neurosci. 2018;32:16–22. doi: 10.1016/j.dcn.2018.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giletta M., Slavich G.M., Rudolph K.D., Hastings P.D., Nock M.K., Prinstein M.J. Peer victimization predicts heightened inflammatory reactivity to social stress in cognitively vulnerable adolescents. JCPP (J. Child Psychol. Psychiatry) 2018;59(2):129–139. doi: 10.1111/jcpp.12804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He Y., Evans A. Graph theoretical modeling of brain connectivity. Curr. Opin. Neurol. 2010;23(4):341–350. doi: 10.1097/WCO.0b013e32833aa567. [DOI] [PubMed] [Google Scholar]
- Hyde L.W., Shaw D.S., Hariri A.R. Understanding youth antisocial behavior using neuroscience through a developmental psychopathology lens: review, integration, and directions for research. Dev. Rev. 2013;33(3):168–223. doi: 10.1016/j.dr.2013.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iacono W.G., Heath A.C., Hewitt J.K., Neale M.C., Banich M.T., Luciana M.M., Madden P.A., Barch D.M., Bjork J.M. The utility of twins in developmental cognitive neuroscience research: how twins strengthen the ABCD research design. Develop. Cogn. Neurosci. 2018;32:30–42. doi: 10.1016/j.dcn.2017.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kisiel C.L., Fehrenbach T., Torgersen E., Stolbach B., Mcclelland G., Griffin G., Burkman K. Constellations of interpersonal trauma and symptoms in child welfare: implications for a developmental trauma framework. J. Fam. Violence. 2014;29:1–14. doi: 10.1007/s10896-013-9559-0. [DOI] [Google Scholar]
- Koob G.F., Volkow N.D. Neurocircuitry of addiction. Neuropsychopharmacology. 2010;35:217–238. doi: 10.1038/npp.2009.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lisdahl K.M., Sher K.J., Conway K.P., Gonzalez R., Feldstein Ewing S.W., Nixon S.J., Tapert S., Bartsch H., Goldstein R.Z., Heitzeg M. Adolescent brain cognitive development (ABCD) study: overview of substance use assessment methods. Develop. Cogn. Neurosci. 2018;32:80–96. doi: 10.1016/j.dcn.2018.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loeber R., Jennings W.G., Ahonen L., Piquero A.R., Farrington D.P. Springer; New York: 2017. Female Delinquency from Childhood to Young Adulthood: Recent Results from the Pittsburgh Girls Study. [Google Scholar]
- Lyoo I.K., Kim J.E., Yoon S.J., Hwang J., Bae S., Kim D.J. The neurobiological role of the dorsolateral prefrontal cortex in recovery from trauma. Arch. Gen. Psychiatr. 2011;68(7):701–713. doi: 10.1001/archgenpsychiatry.2011.70. [DOI] [PubMed] [Google Scholar]
- Marmot M.G., Smith G., Stansfeld S., Patel C., North F., Head J., White I., Brunner E., Feeney A. Health inequalities among British civil servants: the Whitehall II study. Lancet. 1991;337:1387–1393. doi: 10.1016/0140-6736(91)93068-k. [DOI] [PubMed] [Google Scholar]
- Marusak H.A., Thomason M.E., Peters C., Zundel C., Elrahal F., Rabinak C.A. You say ‘prefrontal cortex’ and I say ‘anterior cingulate’: meta-analysis of spatial overlap in amygdala-to-prefrontal connectivity and internalizing symptomology. Transl. Psychiatry. 2016;6:1–10. doi: 10.1038/tp.2016.218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDougall P., Vaillancourt T. Long-term adult outcomes of peer victimization in childhood and adolescence. Am. Psychol. 2015;70:300–310. doi: 10.1037/a0039174. [DOI] [PubMed] [Google Scholar]
- McEwen B. Physiology and neurobiology of stress and adaptation: central role of the brain. Physiol. Rev. 2007;87:873–904. doi: 10.1152/physrev.00041.2006. [DOI] [PubMed] [Google Scholar]
- McEwen B. Brain on stress: how the social environment gets under the skin. Proc. Natl. Acad. Sci. Unit. States Am. 2012;109:17180–17185. doi: 10.1073/pnas.1121254109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mersky J.P., Topitzes J., Reynolds A.J. Impacts of adverse childhood experiences on health, mental health, and substance use in early adulthood: a cohort study of an urban, minority sample in the U.S. Child Abuse Negl. 2013;37(11):917–925. doi: 10.1016/j.chiabu.2013.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ozbay F., Fitterling H., Charney D., Southwick S. Social support and resilience to stress across the life span: a neurobiologic framework. Curr. Psychiatr. Rep. 2008;10:301–310. doi: 10.1007/s11920-008-0049-7. [DOI] [PubMed] [Google Scholar]
- Pagliaccio D., Luking K., Anokhin A., Gotlib I., Hayden E., Olino T., Peng C., Hajcak G., Barch D. Revising the BIS/BAS Scale to study development: Measurement invariance and normative effects of age and sex from childhood through adulthood. Psychol. Assess. 2015;28(4) doi: 10.1037/pas0000186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhodes J., Chan C., Paxson C., Rouse C.E., Waters M., Fussell E. The impact of hurricane Katrina on the mental and physical health of low-income parents in New Orleans. Am. J. Orthopsychiatry. 2010;80(2):237–247. doi: 10.1111/j.1939-0025.2010.01027.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenberger P., Ickovics J., Epel E., Nadler E., Jokl P., Fulkerson J., Tillie J., Dhabhar F. Surgical stress-induced immune cell redistribution profiles predict short-term and long-term postsurgical recovery: a prospective study. J. Bone Jt. Surg. 2009;91(12):2783–2794. doi: 10.2106/JBJS.H.00989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scheidell J.D., Quinn K., McGorry S.P., Frueh B.C., Beharie N.N., Cottler L.B., Khan M.R. Childhood traumatic experiences and the association with marijuana and cocaine use in adolescence through adulthood. Addiction. 2017;113:44–56. doi: 10.1111/add.13921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz R.M., Gillezeau C.N., Liu B., Lieberman-Cribbin W., Taioli E. Longitudinal impact of hurricane Sandy exposure on mental health symptoms. Int. J. Environ. Res. Public Health. 2017;14(9):957–969. doi: 10.3390/ijerph14090957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sher K.J., Gershuny B.S., Peterson L., Raskin G. The role of childhood stressors in the intergenerational transmission of alcohol use disorders. J. Stud. Alcohol. 1997;58(4):414–427. doi: 10.15288/jsa.1997.58.414. [DOI] [PubMed] [Google Scholar]
- Shonkoff J., Garner A. The lifelong effects of early childhood adversity and toxic stress. Pediatrics. 2012;129(1):232–246. doi: 10.1542/peds.2011-2663. [DOI] [PubMed] [Google Scholar]
- Teicher M.H., Samson J.A. Annual Research Review: enduring neurobiological effects of childhood abuse and neglect. J. Child Psychol. Psychiatry Allied Discip. 2016;57(3):241–266. doi: 10.1111/jcpp.12507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thornberry T., Lizotte A., Krohn M., Farnworth M., Jang S. Delinquent peers, beliefs, and delinquent behavior: a longitudinal test of interactional theory. Criminology. 1994;32:47–83. [Google Scholar]
- Tyborowska A., Volman I., Niermann H., Pouwels J., Smeekens S., Cillessen A., Toni I., Roelofs K. Early-life and pubertal stress differentially modulate grey matter development in human adolescents. Sci. Rep. 2018;8:1–11. doi: 10.1038/s41598-018-27439-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volkow N.D., Koob G.F., Croyle R.T., Bianchi D.W., Gordon J.A., Koroshetz W.J., Perez-Stable E.J., Riley W.W.T., Bloch M.H., Conway K., Deeds B.G., Dowling G.J., Grant S., Howlett K.D., Matochik J.A., Morgan G.D., Murray M.M., Noronha A., Spong C.Y., Wargo E.M., Warren K.R., Weiss S.R.B. The conception of the ABCD study: from substance use to a broad NIH collaboration. Develop. Cogn. Neurosci. 2018;32:4–7. doi: 10.1016/j.dcn.2017.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zucker R., Gonzalez R., Feldstein-Ewing S., Paulus M., Arroyo J., Fuligni A., Sheffield-Morris A., Sanchez M., Wills T. Assessment of culture and environment in the adolescent brain and cognitive development study: rationale, description of measures, and early data. Develop. Cogn. Neurosci. 2018;32:107–120. doi: 10.1016/j.dcn.2018.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.