Abstract
Background and Purpose:
In the US, black Americans exhibit a greater risk of stroke and burden of stroke risk factors than whites; however, it is unclear whether these stroke risk factors influence stroke risk differently across racial groups.
Methods:
In total, 126,018 participants of the Women’s Health Initiative (11,389 black and 114,629 white women), free of stroke and coronary heart disease at baseline (1994–1998), were followed through 2010. Participants completed baseline clinical exams with standardized measurements of blood pressure and anthropometrics, medication inventory and self-reported questionnaires on socio-demographics, behaviors/lifestyle and medical history. Incident total, ischemic and hemorrhagic strokes were updated annually through questionnaires with medical record confirmation. Rate differences (RD/100,000 person-years) and hazard ratios (HR) based on multivariable Cox models and were estimated.
Results:
Over a median of 13 years, 4,344 stroke events were observed. Absolute incidence rates were higher in black than white women in each age group. In age-adjusted analyses, risk of stroke was significantly higher among black compared to white women (HR=1.47, 95%CI:1.33–1.63); adjustment for stroke risk factors, which may be on the causal pathway, attenuated the estimate. Racial disparities were greatest among women 50-<60 years (HR=3.48, 95%CI:2.31–5.26;RD=99) and diminished with increasing age (60-<70-HR=1.80, 95%CI:1.50–2.16, RD=107; ≥70 years: HR=1.26, 95%CI:1.10–1.43, RD=87; Pinteraction<0.001). Black women 50-<60 years remained at significantly higher risk than white women after adjustment for stroke risk factors (HR=1.76, 95%CI:1.09–2.83).
Conclusions:
There was a moderately greater risk of total stroke among black compared to white women; however, racial disparities were greatest among women aged 50-<60 years. Interventions targeted at younger black women may provide the greatest benefit in reducing disparities.
Keywords: race, women, stroke, Ischemic stroke, hemorrhagic stroke, stroke risk factors
Subject codes: risk factors for stroke, acute cerebral infarction, race
Introduction
The US Health and Human Services Healthy People 2020 goals aim to “achieve health equity, eliminate disparities and improve health of all groups.”1 However in 2014, stroke was the fifth leading cause of death across all Americans, but the third leading cause among black or African Americans.2 Data from the Reasons for Geographic and Racial Differences in Stroke study (REGARDS) demonstrated that racial disparities in stroke mortality persist despite a marginal absolute decrease of 12% over the past 30 years (1979–2010).3
The root causes of these disparities are not fully understood. Evidence suggests a younger age of stroke onset among blacks,4–6 potentially due to a heavier burden of stroke risk factors among blacks at younger ages, as early as adolescence.7 For example, elevated systolic blood pressure (SBP) may confer a greater risk of stroke among black adults compared to whites.8 Importantly, socioeconomic factors have demonstrated only a minimal role in explaining racial disparities in stroke compared to the contribution of traditional stroke risk factors.3, 6 However, few studies have examined the intersection of race and sex when examining disparities in stroke, nor has the role of potential confounders been examined specifically by race and sex, potentially minimizing residual confounding. To address these limitations, we examined racial disparities in stroke risk as well as interactions between race, stroke risk factors and total stroke specifically among women.
Materials & Methods
Women’s Health Initiative
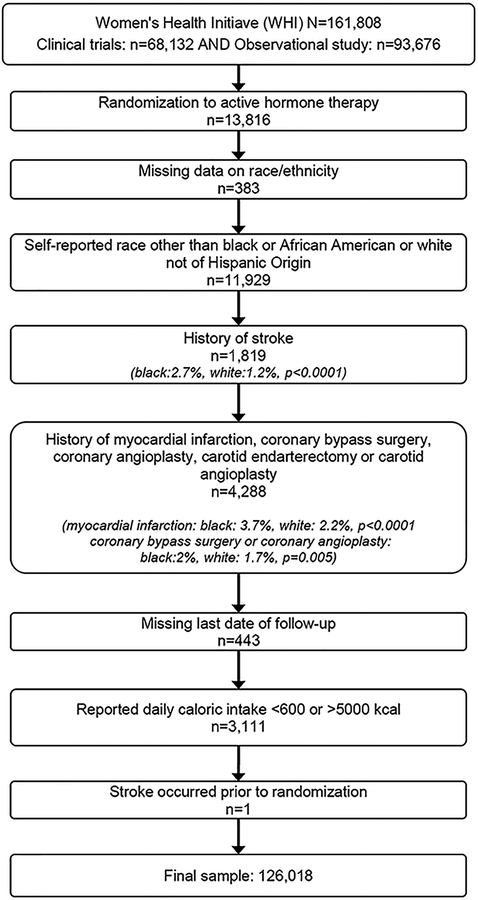
The Women’s Health Initiative (WHI) is an ongoing prospective study of 161,808 multi-ethnic postmenopausal women aged 50–79 years recruited at 40 clinical centers in the US, consisting of clinical trials (WHI-CT) and an observational study (WHI-OS), as previously described9 Of the 68,132 women free of cardiovascular disease (CVD) at baseline (1994–1998) in the WHI-CT, 10% were black or African American and 81.4% were white. Analyses among women enrolled in the WHI-CT were restricted to the dietary modification trial and the placebo arms of the hormone trials, including women who provided follow-up through 2005 as part of the main trial and those who participated in the extension study and provided follow-up through 2010 (Online supplement). A final sample of 126,018 women were available for analyses (Figure 1). Deidentified data and materials have been made publicly available at the NHLBI BioLINCC and can be accessed at (https://biolincc.nhlbi.nih.gov/search/).
Figure 1: Exclusion criteria from baseline sample to final analytic sample.
Covariate Ascertainment
All participants completed baseline clinical exams with questionnaires on socio-demographic, lifestyle/behaviors, diet, medical history and medication inventory as previously described (Online supplement).10 In this study, women who self-reported black or African American are referred to as black and white (not of Hispanic origin) women as white. Region of residence was assigned based on participant address at the baseline visit. Diet was categorized according to the Healthy Eating Index-2005 (HEI-2005)9, 10 based on the baseline food frequency questionnaire History of diabetes, atrial fibrillation, cancer were assessed by self-reported physician diagnosis and hypertension status was defined by self-reported physician diagnosis and treatment with anti-hypertensive medication. Use of antihypertensive medication was restricted to those with a history of hypertension; however, 1.2% reported conflicting responses to antihypertensive medication use (0.6% of stroke cases). All participants who reported current use were included in analyses for current use of antihypertensive medication. Updated values of systolic and diastolic blood pressure, body mass index (BMI) and hypertensive medication were available across all arms in the third year of follow-up.
Stroke Ascertainment
The primary endpoint for these analyses was total stroke (ischemic, hemorrhagic, unknown type) with ischemic and hemorrhagic strokes examined as secondary endpoints. Analyses include all incident nonfatal and fatal strokes diagnosed through 2010. WHI-CT participants attended mandatory clinic visits through the trial, and as of 2005 completed annual mailed questionnaires ascertaining data on medical outcomes including stroke. Women in the WHI-OS reported stroke events by annual self-reported questionnaires, direct reports or by third-party in between questionnaire cycles.9 Fatal events were ascertained by proxy or National Death Index. For all self-reported strokes, medical records and death certificates were requested. Stroke diagnosis requiring and/or occurring during hospitalization was defined as a rapid onset of a persistent neurologic deficit, not known to be secondary to brain trauma, tumor, infection or other cause and attributed to an obstruction or rupture of the brain arterial system, lasting more than 24 hours without evidence for other cause, unless superseded by death or evidence of an acute stroke was available on computed tomography or magnetic resonance imaging scan.11 Strokes were classified as ischemic stroke (thrombotic or embolic occlusion of a cerebral artery or lacunar infarction not procedure related), hemorrhagic stroke (subarachnoid, intracerebral or other unspecified intracranial hemorrhage not procedure related), or stroke of unknown type when a stroke was documented but the type could not be ascertained. Events were locally adjudicated with central adjudication by one of three neurologists available for uncertain events (95% confirmation).11
Statistical Analyses
Distributions of baseline characteristics were compared across race using Chi-square tests for categorical variables and Student’s t-test or Wilcoxon rank-sum tests, for continuous variables, as appropriate depending on the underlying distribution. The distributions of baseline characteristics were calculated across enrollment in extended follow-up and treatment arms (Online supplement). Additionally, race specific incidence rates (IR) of stroke were calculated. Multivariable Cox models stratified by treatment arm and adjusted for time-varying enrollment in extended follow-up (to meet assumptions of proportional hazards) were used to estimate hazard ratios (HR) and 95% confidence intervals (CI). Potential confounders and stroke risk factors were identified by subject matter knowledge and white women were used as the reference to maintain comparability with previous literature.
Three nested multivariable models were used to examine the association between race and stroke. Model 1 adjusted for age at baseline, model 2 additionally adjusted for baseline values of socioeconomic-related variables and model 3 additionally adjusted for baseline stroke risk factors (Online Supplement). Effect modification of the association between race and stroke by stroke risk factors was examined in two ways. First, race-specific relationships between stroke risk factors and total stroke were adjusted for covariates in model 3 to address race-specific confounding. This approach highlights how confounding may influence the association between stroke risk factors and total stroke differently among black and white women, while minimizing residual confounding and allowing for race-specific comparisons. Second, the association between race and total stroke was stratified by stroke risk factors and minimally adjusted for covariates in model 1because all other covariates may be intermediates on the causal pathway. This approach allows for the ascertainment of how racial disparities may differ across stroke risk factors. The associations between age and stroke, and race and stroke stratified by age, were modeled with time-varying age to assess the role of age-at-event, with updated values of SBP, DBP, BMI and use of hypertensive medications in model 3. Statistical significance of interactions for time-varying age were assessed by a Wald test, while all other interactions were assessed using a likelihood ratio test (model with the main effects of race and the stroke risk factor of interest compared to a model including an interaction term for the main effects). P-values from either method are referred to as Pinteraction.
Statement of Ethics
This study was approved by the institutional review board of Brigham and Women’s Hospital and all procedures were in accordance with institutional guidelines. Participants provided informed consent to participate.
Results
Overall, women in these analyses were generally healthy, demonstrated by a low prevalence of current smoking and hypertension, in addition to a high proportion of college or postgraduate education compared to women in the general US population.12 However, mean SBP and BMI values were above the optimal range. Although black women were younger than white women, they exhibited a higher BMI and mean SBP, had a lower dietary score and were more likely to report a history of cardiovascular risk factors (p<0.01;Table 1).
Table 1.
Baseline characteristics of participants by race
| Overall (N=126,018) | White women (n=114,629) | Black women (n=11,389) | p-value | |
|---|---|---|---|---|
| Age (years) | 63±7.2 | 63±7.2 | 61±7.1 | <0.0001 |
| Time to stroke (years) | 8 [4–11] | 8 [4–11] | 7 [4–10] | 0.07 |
| Follow-up among those without stroke (years) | 13 [10–14] | 13 [10–14] | 12 [8–14] | <0.0001 |
| Total Stroke events* | 4,344 | 3934 | 410 | |
| Total mortality, % | 15 | 15 | 13 | <0.0001 |
| Current Smoking, % | 7 | 6 | 11 | <0.0001 |
| Alcohol (g/day) | 0.4 [0–3.2] | 0.4 [0–3.2] | 0 [0–0.4] | <0.0001 |
| HEI-2005† | 67±11 | 68±11 | 63±12 | <0.0001 |
| Physical activity (mins/week) | 50 [0–165] | 60 [0–170] | 10 [0–100] | <0.0001 |
| Current hormone therapy Use, % | 47 | 49 | 30 | <0.0001 |
| History of hypertension, % | 36 | 34 | 56 | <0.0001 |
| Current antihypertensive medication, %‡ | 25 | 23 | 46 | <0.0001 |
| Systolic blood pressure | 127±18 | 126±17 | 132±18 | <0.0001 |
| Diastolic blood pressure | 75±9.2 | 75±9.1 | 78±9.4 | <0.0001 |
| Cholesterol lowering medication, % | 12 | 12 | 14 | <0.0001 |
| BMI (kg/m2) | 28±5.9 | 28±5.7 | 31±6.7 | <0.0001 |
| Diabetes, % | 5 | 4 | 13 | <0.0001 |
| Atrial fibrillation, % | 4 | 4 | 5 | 0.03 |
| Family history of stroke, % | 38 | 38 | 40 | <0.001 |
| Region of residence | <0.0001 | |||
| Northeast | 24 | 25 | 18 | |
| South | 26 | 23 | 47 | |
| Midwest | 23 | 23 | 24 | |
| West | 27 | 29 | 12 | |
| Educational attainment, % | ||||
| <HS diploma | 4 | 3 | 11 | <0.0001 |
| HS diploma | 17 | 17 | 13 | |
| Some college or vocational school | 37 | 37 | 39 | |
| College or Postgrad | 42 | 43 | 37 | |
| Household income, % | <0.0001 | |||
| <$20,000 | 14 | 13 | 27 | |
| $20,000-<$50,000 | 45 | 45 | 43 | |
| $50,000-<$75,000 | 21 | 21 | 18 | |
| $>75,000 | 20 | 21 | 12 | |
| Partnership status, % | ||||
| Never married | 4 | 4 | 6 | <0.0001 |
| Divorced or separated | 15 | 14 | 30 | |
| Widowed | 17 | 16 | 21 | |
| Married/Partnered | 64 | 66 | 42 | |
| Last usual medical care provider visit within last year, % | 80 | 81 | 79 | <0.0001 |
| Treatment arm, % | ||||
| Observational study only | 63 | 63 | 54 | <0.0001 |
| Dietary modification trial only-Active | 12 | 11 | 15 | |
| Dietary modification trial only-Controls | 17 | 17 | 20 | |
| Hormone therapy controls only | 6 | 6 | 6 | |
| E-alone control | 2 | 2 | 4 | |
| E± P control | 4 | 4 | 3 | |
| Hormone therapy controls and dietary modification trial | 3 | 3 | 4 | |
Values are relative frequencies and sample, mean ± std, median [25th-75th percentiles]
t-test, Wilcoxon rank-sum test or Chi-square test used as appropriate on non-missing values
Frequency of stroke type by race provided in Table 2;
Healthy Eating Index-2005;
Among those with self-reported hypertension
Association between race and stroke
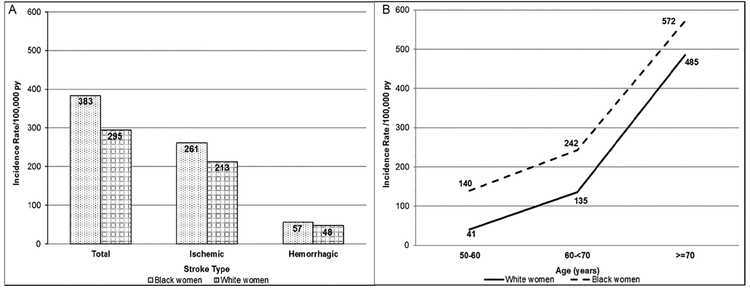
Over 17 years of follow-up (1,496,314 person-years), we observed 4,344 stroke events of which 3,136 were ischemic, 708 hemorrhagic and 500 of unknown origin. There were 410 stroke events among black women and 3,934 among white women. The age-adjusted IR of stroke was higher among black women compared to whites across total and ischemic stroke (Figure 2A). In multivariable analyses, adjusted for age, black women exhibited a 47% greater risk of total stroke compared to white women (95%CI:1.33–1.63; Table 2). The association was modestly attenuated but remained statistically significant after adjusting for socioeconomic variables (model 2) and was attenuated towards the null and no longer statistically significant after adjustment for stroke risk factors (model 3). Estimates for ischemic and hemorrhagic stroke were similar to those for total stroke.
Figure 2: Incidence rates and rate difference (RD) per 100,000 person-years (py) for racial disparities among women of the Women’s Health Initiative.
A) Age standardized incidence rate of stroke (total, ischemic, hemorrhagic) by race, B) Incidence rates and RD for total stroke between black and white women by age. Panel A: P-values for differences between black and white women by stroke type (total stroke: p<0.001; ischemic stroke: p=0.03; hemorrhagic stroke: p=0.38); Panel B, incidence rates for black women (dotted line) and white women (solid line). Rate difference (RD) and P-values between black and white women by age (50–60 years: RD=99/100,000 py, p<0.0001; 60-<70 years: RD=107/100,000 py, p<0.0001; ≥70 years: RD=87/100,000 py, p=0.004).
Table 2.
Multivariable association between race and risk of stroke (total, ischemic, and hemorrhagic)*, HR (95% CI)
| N=126,018 | White Women | Black Women |
|---|---|---|
| HR (95% CI) | ||
| Total Stroke | ||
| Events (n=4,344) | 3934 | 410 |
| Model 1 | 1.00 | 1.47 (1.33–1.63) |
| Model 2 | 1.00 | 1.35 (1.21–1.50) |
| Model 3 | 1.00 | 1.05 (0.94–1.17) |
| Ischemic Stroke | ||
| Events (n=3,136) | 2852 | 284 |
| Model 1 | 1.00 | 1.41 (1.24–1.59) |
| Model 2 | 1.00 | 1.29 (1.14–1.47) |
| Model 3 | 1.00 | 0.99 (0.87–1.13) |
| Hemorrhagic Stroke | ||
| Events (n=708) | 643 | 65 |
| Model 1 | 1.00 | 1.38 (1.07–1.78) |
| Model 2 | 1.00 | 1.24 (0.95–1.62) |
| Model 3 | 1.00 | 1.10 (0.84–1.45) |
Unknown strokes: n=500 (black women n=439, white women n=61)
p<0.05 indicated in bold
Model 1: Adjusted for age and time-varying effects for enrollment in extended follow-up and stratified by treatment arm.
Model 2: Model 1 and socioeconomic factors (marital/partnership status, highest level of attained education, household income, region of residence, last usual medical care provider visit within last year).
Model 3: Model 2 and stroke risk factors (smoking status, systolic blood pressure, diastolic blood pressure, hypertension status, anti-hypertensive medication, hyperlipidemia medication, diabetes, atrial fibrillation, history of cancer, BMI, hormone therapy use, alcohol consumption, weekly minutes of physical activity, Healthy Eating Index-2005 score and family history of stroke).
Race specific associations between stroke risk factors and total stroke
In fully adjusted analysis stratified by race, significant associations were observed between current smoking, diabetes, atrial fibrillation, time-varying age and total stroke (Table 3). Moreover, significant effect modification of the association between stroke risk factors and total stroke by race was observed for family history of stroke (Table 3) and time-varying age. In fully adjusted models, family history of stroke was associated with a modest increase in stroke among white (HR=1.16, 95%CI:1.09–1.24) but not black women (HR=0.90, 95%CI:0.74–1.11; Pinteraction=0.01). Additionally, the association between time-varying age and stroke was stronger among white women than among black women after adjustment for socioeconomic variables and stroke risk factors (Pinteraction<0.0001). White women aged 60-<70 years and ≥70 years exhibited a 2.56 (95%CI:2.01–3.26) and 7.07 (95%CI:5.56–8.99) times greater risk of stroke compare to those 50-<60 years; whereas, among black women, the risk was 1.38 (95%CI:0.94–2.04) and 2.74 (95%CI:2.26–4.12), respectively. Although the relative associations between age and stroke were higher in white women, the age-specific IR remained higher for black women in each age group (Figure 2B).
Table 3.
Race specific multivariable associations between stroke risk factors and total stroke, HR (95% CI)
| Stroke Risk Factors | White Women | Black Women | |||
|---|---|---|---|---|---|
| Events | HR (95% CI) | Events | HR (95% CI) | Pinteraction | |
| Smoker | 0.90 | ||||
| Never | 1961 | 1.00 | 199 | 1.00 | |
| Former | 1634 | 1.06 (0.99–1.13) | 148 | 0.98 (0.79–1.22) | |
| Current | 286 | 1.83 (1.61–2.09) | 57 | 1.68 (1.24–2.29) | |
| Hypertension | 0.14 | ||||
| No hypertension | 1957 | 1.00 | 125 | 1.00 | |
| Hypertensive non-treated | 368 | 1.38 (0.69–2.76) | 45 | 0.98 (0.14–7.08) | |
| Hypertensive treated | 1343 | 1.51 (0.68–3.38) | 209 | 1.18 (0.13–10.77) | |
| Antihypertensive medication* | 1367 | 1.02 (0.67–1.55) | 213 | 0.68 (0.24–1.90) | 0.06 |
| Use of cholesterol lowering medication | 521 | 0.93 (0.84–1.02) | 61 | 0.98 (0.74–1.30) | 0.88 |
| Diabetes | 302 | 1.59 (1.41–1.80) | 84 | 1.66 (1.29–2.14) | 0.92 |
| Atrial fibrillation | 318 | 1.64 (1.46–1.84) | 37 | 1.92 (1.36–2.71) | 0.59 |
| Family history of stroke | 1665 | 1.16 (1.09–1.24) | 157 | 0.90 (0.74–1.11) | 0.01 |
| Physical activity ≥150 min/week | 935 | 0.86 (0.80–0.93) | 66 | 1.01 (0.77–1.32) | 0.30 |
| BMI ≥30 kg/m2 | 1122 | 1.01 (0.94–1.09) | 213 | 1.02 (0.83–1.25) | 0.61 |
p<0.05 indicated in bold.
Among hypertensive women.
Adjusted for covariates in Model 3 of Table 2, except for stratification factor.
Reference groups are the complement of the indicated category unless otherwise indicated.
Association between race and stroke stratified by stroke risk factors
Racial disparities in total stroke were greatest among those aged 50-<60 years compared to older women after adjustment for covariates in model 1 (<60: HR=3.48, 95%CI:2.31–5.26; 60-<70: HR=1.80, 95%CI:1.50–2.16; ≥70: HR=1.26, 95%CI:1.10–1.43). Further adjustment for covariates in model 3, including time-varying SBP, DBP, BMI and hypertension medication use, resulted in attenuation towards the null, primarily due to hypertension status, but remained statistically significant among younger women (<60: HR=1.76, 95%CI:1.09–2.83; 60-<70: HR=1.09, 95%CI:0.89–1.33; ≥70: HR=0.98, 95%CI:0.85–1.12). Additionally, there was a greater racial disparity in stroke among women without a family history of stroke (HR=1.69, 95%CI:1.47–1.94, Pinteraction=0.02) which remained statistically significant in fully adjusted models (HR=1.21, 95%CI:1.04–1.40, Pinteraction=0.01; Table 4). Among women with hypertension, there was a suggestion that racial differences in the incidence of total stroke were only observed among those not taking antihypertensive medication; however, the interaction was not statistically significant (HR=1.42, 95%CI:1.00–2.02, Pinteraction=0.08; Table 4).
Table 4.
Multivariable association between race and total stroke stratified by stroke risk factors, HR (95% CI)
| Stratification Factor | Events white women | Events black women | Model 1* | Pinteraction | Model 3† |
|---|---|---|---|---|---|
| Smoking | |||||
| Never | 1961 | 199 | 1.48 (1.27–1.71) | 0.69 | 1.06 (0.91–1.25) |
| Former smoker | 1634 | 148 | 1.40 (1.18–1.66) | 1.02 (0.85–1.22) | |
| Current smoker | 286 | 57 | 1.45 (1.09–1.93) | 1.11 (0.81–1.52) | |
| Hypertension | 0.16 | ||||
| No hypertension | 1957 | 125 | 1.42 (1.19–1.71) | 1.09 (0.90–1.32) | |
| Hypertensive non-treated | 368 | 45 | 1.46 (1.07–2.00) | 1.35 (0.97–1.88) | |
| Hypertensive treated | 1343 | 209 | 1.11 (0.96–1.29) | 0.95 (0.81–1.12) | |
| Antihypertensive Medication‡ | 0.08 | ||||
| No | 336 | 40 | 1.55 (1.11–2.16) | 1.42 (1.00–2.02) | |
| Yes | 1367 | 213 | 1.11 (0.96–1.29) | 0.96 (0.82–1.12) | |
| Cholesterol Lowering Medication | 0.69 | ||||
| No | 3144 | 316 | 1.48 (1.32–1.66) | 1.04 (0.91–1.17) | |
| Yes | 521 | 61 | 1.33 (1.02–1.74) | 1.00 (0.75–1.34) | |
| Diabetes | 0.69 | ||||
| Non-diabetic | 3628 | 324 | 1.39 (1.24–1.56) | 1.06 (0.94–1.20) | |
| Diabetic | 302 | 84 | 1.15 (0.90–1.47) | 0.91 (0.69–1.19) | |
| Atrial Fibrillation | 0.55 | ||||
| No | 3520 | 360 | 1.46 (1.31–1.62) | 1.03 (0.92–1.16) | |
| Yes | 318 | 37 | 1.64 (1.16–2.31) | 1.30 (0.89–1.90) | |
| Family History of stroke | 0.02§ | ||||
| No | 2048 | 229 | 1.69 (1.47–1.94) | 1.21 (1.04–1.40) | |
| Yes | 1665 | 157 | 1.29 (1.09–1.52) | 0.92 (0.77–1.10) | |
| Physical Activity | 0.40 | ||||
| <150 mins/week | 2999 | 344 | 1.40 (1.25–1.57) | 1.01 (0.90–1.14) | |
| ≥150 mins/week | 935 | 66 | 1.62 (1.26–2.09) | 1.25 (0.96–1.63) | |
| BMI (kg/m2) | 0.90 | ||||
| <30 | 2812 | 197 | 1.43 (1.23–1.65) | 1.03 (0.89–1.20) | |
| ≥30 | 1122 | 213 | 1.36 (1.17–1.57) | 1.05 (0.89–1.23) | |
Discussion
Among more than 100,000 women free of CVD at baseline with up to 17 years of follow-up, we observed a moderate, significantly increased risk of stroke among black compared to white women. However, this association was no longer statistically significant after adjustment for traditional stroke risk factors. We observed significant variation by race of the association between time-varying age and total stoke, such that the age-related risk of stroke among older white women was higher than that observed among black women due to the higher baseline risk of stroke among younger black women; however, in all age groups black women had a higher incidence rate of stroke than white women. Additionally, racial disparities were greater among women without a family history of stroke.
In the US, black adults have consistently exhibited a higher incidence of stroke than their white counterparts;13 however, few studies have examined these racial disparities separately by sex or across stroke risk factors.5, 6 Our findings suggest a moderately greater risk of total stroke among black women, albeit weaker than those previously reported. Several studies, including the Northern Manhattan Stroke Study (NOMAS)5 and the Atherosclerosis Risk in Communities (ARIC) Study have reported a nearly three-fold greater risk of stroke among black compared to white women (NOMAS: RR=2.8, 95%CI:2.0–3.8; ARIC: IR black=3.96, 95%CI:3.10–5.06, IR white=1.49, 95%CI:1.16–1.92).6 The older baseline age distribution (50–79 years) of the WHI compared to NOMAS and ARIC, may partially explain the attenuated racial disparities we observed and highlights the role of age in understanding racial disparities in stroke.
Our findings of significant variation of racial disparities in stroke by age were similar, albeit attenuated, to previous reports. In age-stratified analyses, the greatest racial disparities in total stroke were among younger women even after adjustment for socioeconomic and stroke risk factors, while minimal disparities were observed among women aged ≥70 years and were no longer significant in fully adjusted models. In analyses stratified by race and additionally adjusted for stroke risk factors, the age-related risk of total stroke was greater among white than among black women on the relative scale, due to the higher baseline risk of stroke among younger black women. The lack of diminishing absolute rates by age was likely due to the sharp increase in the incidence of stroke among older compared to younger white women (Figure 2B). Similar to our findings, among participants of REGARDS in unadjusted analyses, blacks aged 45–54 years exhibited a significant four-fold greater risk of total stroke (95%CI:1.23–13.11) compared to whites, with no significant association observed for those aged ≥75 years.4 Older black women may represent a survivor cohort or the role of race on health may be diminished by chronic disease in older age. Additionally, due to historical differences in the distribution of cardiovascular factors, older women in our cohort may have been exposed to cardiovascular risk factors at older ages, attenuating their influence on stroke risk. Moreover, racial variation in stroke risk by family history of stroke has not been previously reported. These findings suggest that genetic predisposition to stroke is unlikely to explain racial disparities, further supporting the role of social and environmental factors in shaping these disparities.
These findings have several key implications and highlight the importance of examining disparities across multiple dimensions of the lived experience, for example, across race, sex and age. Younger black women have been shown to carry a disproportionate burden of stroke risk factors beginning at earlier ages than their white counterparts. The attenuated magnitude of racial disparities among black women in our cohort compared to previous findings4–6, 14 suggests a key role of socioeconomic factors underlying racial inequities in stroke. Overall, both black and white women in this WHI sample had somewhat better health status and higher educational status than women in REGARDS. They were less likely to be current smokers (WHI v. REGARDS: black women [11% v. 15%], white women [6% v. 13%])15 or diabetic (WHI v. REGARDS: black women [13% v. 28%], white women [4% v. 12%])15 and black women were more likely to have achieved college or post-graduate education in WHI (36%) than in REGARDS (22%).16 These differences may also explain the lack of variation in racial disparities across other risk factors, in contrast to previous findings for SBP and diabetes.8, 17 Although higher socioeconomic status may attenuate racial disparities in stroke, the elevated stroke incidence among younger black women and those without a family history of stroke, may reflect persistent racial differences in the distribution of deleterious exposures at the individual, neighborhood and institutional levels across the life course. It is uncertain whether stroke risk factors may influence risk differently not just across various life stages but whether the layering of risk life across particular life stages may confer or alter stroke risk. Unequal access to material and social resources and psychologic stress among black women may result in “accelerated cardiovascular aging,” due to a longer duration and heavier burden of stroke risk factors potentially beginning in childhood, inequities in stroke incidence and ultimately greater years of life and productivity lost than similarly aged white women.18 Additionally, research is needed to understand the role of positive social constructs within US black communities that can support resiliency and mitigate such inequities in health attainment.
Important strengths and limitations of this study warrant consideration. The long follow-up and large sample size allowed for the accrual of ample events to conduct within-race comparisons across stroke risk factors which provided improved interpretability by using relevant reference groups (i.e. within race comparisons). In contrast, comparisons across racial groups may suffer from residual confounding due to unmeasured confounders and inequities in the comparability of socioeconomic measures, quality or access to care or compliance to medication. The minimal confounding by socioeconomic factors observed in our multivariable analyses may reflect limitations of education and income to capture nuances of access to social and material resources or childhood socioeconomic factors. Additionally, analyses exploring generational differences may elucidate potential cohort effects. Moreover, the higher prevalence of atrial fibrillation among black women and differences in anticoagulant use may also inform racial disparities in stroke. While generalizability may be limited, any potential bias would be expected to be towards the null. Moreover, potential misclassification due to self-report was minimized by standardized clinical measurements of blood pressure and anthropometrics and medication inventories. Despite ample total stroke events, power to examine stroke types was limited due to few hemorrhagic strokes among black women. Lastly, this study was not originally powered to examine interaction analyses; therefore, chance findings associated with evaluation of multiple subgroups may potentially explain the observed heterogeneity.
In conclusion, in this cohort of middle-to-older aged women, free of CVD at baseline, we found a moderately greater risk of total stroke among black compared to white women. However, the association varied significantly by age and family history of stroke. These findings highlight the greater impact of stroke among young black women and suggest racial disparities in stroke risk may be reduced by environmental, clinical and behavioral interventions targeted at younger black women to address inequities in the burden of stroke risk factors.
Supplementary Material
Acknowledgments:
We acknowledge all WHI centers, principle investigators and participants for their commitment to this research (Online supplement).
Sources of Funding: The WHI program is funded by the National Heart, Lung, and Blood Institute (NHLBI), NIH, U.S. Department of Health and Human Services through contracts HHSN268201100046C, HHSN268201100001C, HHSN268201100002C, HHSN268201100003C, HHSN268201100004C, and HHSN271201100004C. Dr. Jiménez is supported by K01HL124391 from the NHLBI and the Brigham and Women’s Minority Faculty Career Development Award.
Footnotes
Clinical Trial Registration: This trial was not registered because enrollment began prior to July 1, 2005
Disclosures/Conflict of Interest: None
References
- 1.The Secretary’s Advisory Committee on National Health Promotion and Disease Prevention Objectives for 2020 Recommendations for the framework and format of healthy people 2020. Washington, D.C.: Department of Health and Human Services; 2008. [Google Scholar]
- 2.National Center for Health Statistics (US). Health, united states, 2015: With special feature on racial and ethnic health disparities,. Hyattsville, MD: U.S. Department of Health and Human Services; 2016. [PubMed] [Google Scholar]
- 3.Howard G, Cushman M, Kissela BM, Kleindorfer DO, McClure LA, Safford MM, et al. Traditional risk factors as the underlying cause of racial disparities in stroke: Lessons from the half-full (empty?) glass. Stroke. 2011;42:3369–3375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Howard VJ, Kleindorfer DO, Judd SE, McClure LA, Safford MM, Rhodes JD, et al. Disparities in stroke incidence contributing to disparities in stroke mortality. Ann Neurol. 2011;69:619–627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sacco RL, Boden-Albala B, Gan R, Chen X, Kargman DE, Shea S, et al. Stroke incidence among white, black, and hispanic residents of an urban community: The northern manhattan stroke study. Am J Epidemiol. 1998;147:259–268. [DOI] [PubMed] [Google Scholar]
- 6.Rosamond WD, Folsom AR, Chambless LE, Wang CH, McGovern PG, Howard G, et al. Stroke incidence and survival among middle-aged adults: 9-year follow-up of the atherosclerosis risk in communities (aric) cohort. Stroke. 1999;30:736–743. [DOI] [PubMed] [Google Scholar]
- 7.Shay CM, Ning H, Daniels SR, Rooks CR, Gidding SS, Lloyd-Jones DM. Status of cardiovascular health in us adolescents: Prevalence estimates from the national health and nutrition examination surveys (nhanes) 2005–2010. Circulation. 2013;127:1369–1376. [DOI] [PubMed] [Google Scholar]
- 8.Howard G, Lackland DT, Kleindorfer DO, Kissela BM, Moy CS, Judd SE, et al. Racial differences in the impact of elevated systolic blood pressure on stroke risk. JAMA internal medicine. 2013;173:46–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Design of the women’s health initiative clinical trial and observational study. The women’s health initiative study group. Control Clin Trials. 1998;19:61–109. [DOI] [PubMed] [Google Scholar]
- 10.Anderson GL, Manson J, Wallace R, Lund B, Hall D, Davis S, et al. Implementation of the women’s health initiative study design. Ann Epidemiol. 2003;13:S5–17. [DOI] [PubMed] [Google Scholar]
- 11.Wassertheil-Smoller S, Hendrix SL, Limacher M, Heiss G, Kooperberg C, Baird A, et al. Effect of estrogen plus progestin on stroke in postmenopausal women: The women’s health initiative: A randomized trial. JAMA. 2003;289:2673–2684. [DOI] [PubMed] [Google Scholar]
- 12.Ryan CL, Bauman K. Educational attainment in the united states: 2015. Washington, D.C.: 2016. [Google Scholar]
- 13.Benjamin EJ, Virani SS, Callaway CW, Chamberlain AM, Chang AR, Cheng S, et al. Heart disease and stroke statistics-2018 update: A report from the american heart association. Circulation. 2018;137:e67–e492. [DOI] [PubMed] [Google Scholar]
- 14.Kleindorfer DO, Khoury J, Moomaw CJ, Alwell K, Woo D, Flaherty ML, et al. Stroke incidence is decreasing in whites but not in blacks: A population-based estimate of temporal trends in stroke incidence from the greater cincinnati/northern kentucky stroke study. Stroke. 2010;41:1326–1331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cushman M, Cantrell RA, McClure LA, Howard G, Prineas RJ, Moy CS, et al. Estimated 10-year stroke risk by region and race in the united states: Geographic and racial differences in stroke risk. Ann Neurol. 2008;64:507–513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Roth DL, Haley WE, Wadley VG, Clay OJ, Howard G. Race and gender differences in perceived caregiver availability for community-dwelling middle-aged and older adults. Gerontologist. 2007;47:721–729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sacco RL, Boden-Albala B, Abel G, Lin IF, Elkind M, Hauser WA, et al. Race-ethnic disparities in the impact of stroke risk factors: The northern manhattan stroke study. Stroke. 2001;32:1725–1731. [DOI] [PubMed] [Google Scholar]
- 18.Freid V, Prager K, MacKay A, Xia H. Chartbook on trends in the health of americans Health united states, 2003. National Center for Health Statistics; 2003. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.