Abstract
Purpose:
To characterize the reasons, extent, and impact of traditional medicine use among people with epilepsy (PWE) in the Republic of Guinea.
Methods:
Guinea is a low-income country in sub-Saharan Africa (SSA) with limited healthcare resources. PWE and their caregivers were seen at a public referral hospital in Conakry, the capital city, where they completed semi-structured interviews with physicians regarding their beliefs about epilepsy, medical care, and engagement with traditional healers.
Results:
Of 132 participants (49% children, 44% female, 55% with a university-educated head of household), 79% had seen a traditional healer, and 71% saw a traditional healer before seeing a medical provider for their epilepsy. Participants were treated by a traditional healer for a mean of 39 months before seeing a medical provider. By contrast, 58% of participants reported taking AEDs regularly, 46% reported having undergone a head CT, 58% reported having had an electroencephalogram, and 4% reported having had a brain MRI.
Conclusions:
Traditional healers in Guinea provide frontline care for PWE in Guinea with considerable delays in AED initiation, even among a cohort of PWE actively seeking medical care. Engaging with these healers is critical for both influencing community perceptions and appropriately managing epilepsy throughout the country.
Keywords: global health, epilepsy, traditional medicine, healthcare delivery, Africa
Background:
Approximately 10 million PWE live in SSA, where there exists a wide treatment gap of PWE who are not receiving necessary antiepileptic drugs (AEDs)[1–3]. Untreated epilepsy is a much more frequent cause of death in SSA than in wealthy countries, with status epilepticus, falls, drowning, bums, and sudden unexpected death contributing to epilepsy-related mortality[4].
PWE face multiple barriers that limit their access to the medical care offered by physicians, nurses, and other professional health workers. Throughout SSA, healthcare resources are often centralized in cities, requiring that PWE living in rural areas travel long distances to see medical providers[5]. Many countries lack sufficient numbers of medical providers to serve the population, and many providers are inexperienced with the best practices for epilepsy care[6,7]. A limited selection of AEDs is available, and pharmacies are often out of stock of common AEDs[8,9]. Finally, medical care is often disease-centered and may be unable to offer explanations of disease causality in keeping with patients’ own beliefs[10]. In the case of epilepsy, these often include supernatural and spiritual beliefs[11–15].
In this setting, PWE throughout SSA often seek care from traditional healers who are usually more geographically accessible than medical providers[16]. In regions with multiple local languages, traditional healers may be able to communicate more readily with patients and families than medical providers[17]. Unlike medical providers, traditional healers may also offer explanations of disease causality that are more familiar to patients and their families[11,18]. Traditional healers are embedded within communities and are instrumental in defining and disseminating beliefs and attitudes regarding illness[17–19]. Where there is limited access to biomedical services, these healers often also serve as the care provider of last resort. Even when PWE are able to access medical care, they may simultaneously or first seek care from traditional healers. These healers include herbalists, who utilize medicinal plants in their treatments; Islamic clerics who use Koranic verses and prayers in their healing; and Christian faith healers, who use holy water and prayer aids in their treatments[20].
Reliance on traditional healers has continued in spite of a very strong evidence base for biomedical care[5]. In response, the World Health Organization has established a Traditional Medicine Strategy to strengthen the role traditional medicine plays in keeping populations healthy, reporting that “traditional and complementary medicine is found in almost every country in the world and the demand for its services is increasing” [21].
The Republic of Guinea is a low-income country in SSA that is ranked 183th out of 187 countries in the United Nations Human Development Index with a critical shortage of health care workers [22][23]. Limited research has been published on epilepsy in Guinea; however, a prior study from our group found that 25% of PWE seen at a public hospital in Conakry had untreated epilepsy and 72% met operational criteria for poorly controlled epilepsy[24]. Here, we characterize the reasons, extent, and impact of traditional medicine use in a new cohort of PWE in Guinea. To our knowledge, no prior study has explored this critical aspect of epilepsy care in Guinea.
Methods:
Ethics:
The study protocol was approved by the Institutional Review Boards of Ignace Deen Teaching Hospital in Guinea and Massachusetts General Hospital. Written informed consent was provided by each participant. A parent or next of kin provided consent for any child <18 years old or for adult participants who were unable to provide consent. A thumbprint was used in place of a signature for low-literacy participants.
Setting:
The Republic of Guinea has an estimated population of 12.6 million people. Approximately 35% of the population lives below the international poverty line of 1.90 USD per day[22]. From 2014 to 2016, Guinea experienced an outbreak of Ebola Virus Disease, which further destabilized its already unstable health system[25]. There are four neurologists, all located in Conakry. Although the official language of Guinea is French, Guinea is a multilingual country, with more than 40 spoken languages. The national languages of Guinea are Fula or Pular, Malinké or Maninka, Susu, Kissi, Kpelle or Guerzé, and Toma. Guinea also hosts a number of migrants from neighboring African countries[24].
Recruitment and Participants:
PWE were recruited in summer 2018 by epilepsy providers at Ignace Deen Teaching Hospital, a public hospital. Self-referrals were also solicited through national radio and television programs. The participants in this study were recruited as part of a larger study on epilepsy in Guinea that included a medical visit with a neurologist and one or more electroencephalograms (EEGs). Prior engagement with traditional healers was not mentioned or selected for as part of the recruitment process. Participants enrolled in the broader study were offered participation in the traditional healing interview with no prior knowledge of their traditional healing engagement and completed a second, verbal consent for this sub-study. No study participants declined the traditional healing interview. Most participants were accompanied by at least one family member.
Study Instruments:
We developed a 13-question semi-structured interview survey instrument, grounded in the explanatory models of illness framework and adapted through discussions with Guinean epilepsy providers (Appendix 1). This framework explores beliefs about a condition, assessing perceptions regarding its cause, its course, its effects on the patient, and preferred treatment modalities[26]. Paired interviews were conducted with PWE and their caregivers whenever possible. Research staff also verbally administered a separate structured survey on demographic characteristics, level of education, seizure history, traditional medicine use, and previous exposure to biomedical care. Interviews were conducted by a U.S.-based neurologist with translation by a West African resident physician fluent in the participant’s preferred language.
Data Analysis:
Each participant interview was translated on-site by a West African resident physician fluent in the participant’s preferred language and was also transcribed on-site. Participant responses to semi-structured interview questions were subjected to formal thematic analysis. Quantitative data from structured questionnaires were summarized. The data were classified to understand the participant’s and community’s beliefs about the nature, causes, effects, and treatment of epilepsy.
Results
Participant characteristics:
132 PWE and their caregivers participated (Table 1). 92% of participants self-identified as Muslim, and 71% were from Conakry. The primary spoken language was divided roughly evenly between Susu, Fula, and Malinké, with several participants preferring other Guinean regional languages or regional languages of their country of origin. More than half of participants (55%) reported that the head of their household had a university-level education with a median household size of 8 individuals, including 4 adults.
Table 1.
Cohort characteristics
| Number | Percentage | |
|---|---|---|
| Total PWE included | 132 | 100 |
| Sex | ||
| Male | 74 | 56 |
| Female | 58 | 44 |
| Age (years) | ||
| ≤5 | 16 | 12 |
| 6-10 | 23 | 17 |
| 11-15 | 21 | 16 |
| 16-20 | 14 | 11 |
| 21-30 | 31 | 24 |
| 31-40 | 21 | 16 |
| > 40 | 6 | 5 |
| Age at first seizure (years) | ||
| <1 | 29 | 22 |
| 1-5 | 30 | 23 |
| 6-10 | 21 | 16 |
| 11-15 | 17 | 13 |
| 16-20 | 6 | 5 |
| 21-30 | 13 | 10 |
| 31-40 | 3 | 2 |
| >40 | 2 | 2 |
| Not recorded | 11 | 8 |
| Religion | ||
| Muslim | 122 | 92 |
| Christian | 9 | 7 |
| Other | 1 | 1 |
| Preferred language | ||
| Susu | 39 | 30 |
| Fula/Pular | 43 | 33 |
| Malinké/Maninka | 40 | 30 |
| Kpelle/Guerzé | 4 | 3 |
| Kissi | 2 | 2 |
| Toma | 2 | 2 |
| Sara (Chad) | 1 | 1 |
| Mina (Togo) | 1 | 1 |
| District of Residence | ||
| Conakry | 93 | 71 |
| Dubreka | 6 | 5 |
| Labe | 3 | 23 |
| Boke | 2 | 2 |
| Kindia | 2 | 2 |
| Other | 26 | 20 |
| Highest level of formal education of head of household | ||
| No education | 19 | 14 |
| Primary school | 3 | 2 |
| Began high school | 9 | 7 |
| Completed high school | 18 | 14 |
| University | 73 | 55 |
| Not answered | 10 | 8 |
Establishing terminology:
Common phrases used by PWE and their caretakers to describe epilepsy included maladie du diable in French, meaning “disease of the devil”; cri cri massa in Malinké, meaning “falling down suddenly”; djina-wake in Fula, meaning “bad spirit disease”; and om-ma-giri-giri in Susu, meaning “unsteadiness of the head” (Table 2). Traditional healers using Koranic scriptures in their practices were most often referred to as marabout, onstage, or karamoko. Less often, participants reported seeing a féticheur, a traditional healer who practices voodoo.
Table 2.
Phrases used to describe seizure and epilepsy
| Phrase | Language | Meaning |
|---|---|---|
| cris | French | “to fall” |
| tombé | French | |
| maladie du diable | French | “disease of the devil” |
| djina-wake | Fula/Pular | “bad spirit disease” |
| fa-te-te | Fula/Pular | “he falls down” |
| fategol | Fula/Pular | |
| wo-wo | Kissi | “somebody who falls down suddenly’ |
| hweli-hweli | Kpelle/Guerzé | “falling down” |
| cri cri massa | Malinké/Maninka | “falling down suddenly” |
| djina-toye | Malinké/Maninka | “devil disease” |
| Ajibo | Mina (Togo) | “person who falls down” |
| djina-kill | Sara (Chad) | “spirit possession” |
| om-ma-giri-giri | Susu | “unsteadiness of the head” |
| bira-furi | Susu | “falling disease” |
| ina-furi | Susu | “devil disease” |
| foli-voli | Toma | “falling disease |
Explanatory models for epilepsy:
Participants were queried on beliefs held by members of their community in addition to their own beliefs regarding epilepsy. This technique has been previously described in the literature [27] and was used to characterize the spectrum of beliefs that PWE are exposed to, as well as to facilitate the discussion of beliefs that participants might otherwise have been reluctant to share.
Most participants reported multiple beliefs regarding the cause of epilepsy. 91% reported the belief that epilepsy is caused by a brain injury, 31% that epilepsy is hereditary, 24% that epilepsy is caused by malaria and other infections, and 16% that epilepsy is caused by problems during labor and delivery. 83% of participants reported the belief that epilepsy could be cured. 41% of participants reported the belief that epilepsy is contagious and can be transmitted from person to person through direct contact with PWE (Table 3). This belief was informed by the observation that PWE may produce saliva, bleed from tongue biting or skin wounds, and sweat during generalized seizures. Participants described the fear that epilepsy could be transmitted through saliva, sweat, or blood produced by someone having a seizure. Participants also described the fear that epilepsy could be transmitted by sharing food with PWE because of contamination of food or drinks by saliva, by kissing, and by sexual contact. According to one caregiver:
“When someone has a seizure and he falls, his saliva flows onto the ground. Even if he leaves that place, yon can easily get epilepsy by walking where he has fallen. If someone with a seizure has fallen somewhere, you have to clean that place with fire. If someone with a seizure has slept in a bed, it must be washed with soap and cleaned very well, because it can be contagious.”
Table 3.
Community1 beliefs regarding epilepsy
| Number | Percentage | |
|---|---|---|
| Epilepsy is contagious and can be transmitted through bodily fluids | 54 | 41 |
| Modes of transmission described: sexual contact, kissing, sharing food, and through contact with sweat, blood, or saliva produced during a seizure | ||
| Epilepsy is caused by brain injury | 120 | 91 |
| Epilepsy is caused by sorcellerie or witchcraft | 27 | 21 |
| Epilepsy is caused by djina or diable | 111 | 84 |
| Modes of transmission described: sexual contact, bathing or contact with water, walking in the forest during the new moon, meeting the devil in the road or on the beach | ||
| Epilepsy is caused by stress, anxiety, or strong emotions | 8 | 6 |
| Epilepsy is hereditary | 41 | 31 |
| Epilepsy is caused by ingestion | 10 | 8 |
| Vectors of transmission described: wine, peanuts, lamb or mutton, and salt | ||
| Epilepsy is caused by problems during delivery | 21 | 16 |
| Epilepsy is caused by contact with animals | 6 | 5 |
| Vectors of transmission described: bird droppings, saliva or blood from a dead goat, cats | ||
| Epilepsy is caused by malaria and other infections | 32 | 24 |
| Epilepsy in children is caused by exposures in utero | 13 | 10 |
| Risk factors described: too much salt consumed during pregnancy, contact between the foot of a pregnant woman with bird droppings, meeting a djina during pregnancy, experiencing anger or stress during pregnancy, seeing a particular animal during pregnancy, passing under a cursed tree during pregnancy | ||
| Epilepsy can be cured | 110 | 83 |
Participants were queried on beliefs held by members of their community in addition to their own beiiets regarding epilepsy. This technique has been previously described in the literature (27) and was used to characterize the spectrum of beliefs that PWE are exposed to, as well as to facilitate discussion of beliefs that participants might otherwise have been reluctant to share.
A majority of participants reported supernatural beliefs about the causes of epilepsy. 84% of participants described the belief that epilepsy is the result of possession by the devil or by jinn, or djina, invisible spirits described in the Koran. The djina are thought to reside in the ocean and other bodies of water and to possess those who bathe or swim at night or during the new moon. Other methods of possession described involved sexual contact with djina masquerading in human form and walking through the forest at night. Djina were also thought to target children who are particularly handsome or bright, out of jealousy. Many participants used the words djina and diable, devil, interchangeably, and reported that epilepsy can be contracted when a person meets djina or diable, most often in the road or at the beach.
“While I was pregnant, I went back and forth between my husband’s parents ‘ house and my parents ‘ house, and they say my baby has epilepsy because I met the devil in between.”
“Some say that by going in the ocean you can meet the devil. Others say that there are bad djina in the forest at night. If a pregnant woman passes through the forest, she may meet the djina under a tall tree, and her child will have epilepsy.”
21% of participants reported the belief that epilepsy could be the result of sorcellerie, or witchcraft. 10% reported the belief that epilepsy could be caused by exposures in utero, for instance if a pregnant woman experienced anger or stress during her pregnancy. 8% reported the belief that epilepsy could be caused by ingestion of alcohol or certain types of meat, salt, or peanuts. 6% reported that epilepsy could be caused by strong emotions, and 5% reported the belief that epilepsy could be caused by contact with animals.
“I think the seizures were caused by witchcraft. She had a dream that a cat bit her ear, and when she woke up, there was blood in her ear. I think this was a witch who came in her dream.”
“When my first seizure came, I was sleeping and a black shadow came and took my hand and I had the seizure. It was so tall. My parents said the neighbor might have been a sorcerer who came in my dream.”
AED use:
117 participants (89%) reported that they had tried AEDs in the past, and 89 (67%) reported currently taking AEDs. 76 (58%) reported taking AEDs regularly (Table 4). The reasons given for stopping AEDs included that the seizures had stopped, lack of access to AEDs, advice from a family member or traditional healer, side effects or fear of harm, inability to afford AEDs, the persistence of seizures on medication, taking medications only when having seizures, lack of understanding regarding how to take medications, and fear that medications were worsening seizures. Participants also cited the belief that epilepsy can be cured as a reason for stopping medications, reporting the hope that if seizures stopped on medications, the disease was cured and AEDs could be stopped. 46% of participants reported having undergone a head CT in the past, 58% reported having had an EEG, and 4% reported having had a brain MRI.
Table 4.
Treatment of epilepsy
| Number | Percentage | |
|---|---|---|
| Saw a traditional healer for epilepsy | 104 | 79 |
| Saw a traditional healer before seeing a physician in the hospital | 94 | 71 |
| Mean time elapsed: 39 months | ||
| Median time elapsed: 24 months | ||
| Saw a traditional healer and a physician simultaneously | 42 | 32 |
| Continuing to see a traditional healer | 12 | 9 |
| Traditional healing methods tried | ||
| Gris-gris or sebe tied around the waist or wrist | 22 | 17 |
| Drank or bathed in an herbal liquid | 55 | 42 |
| Read scriptures from the Koran | 8 | 6 |
| Koran verses applied to the body | 50 | 38 |
| Spoken into hands and rubbed on face or body | ||
| Spoken into water, consumed or bathed | ||
| Written on paper and rubbed on body | ||
| Concoction of leaves or twigs | 29 | 22 |
| Consumed animal sacrifice | 10 | 8 |
| Garlic, grains, alcohol, or orange in the nose or mouth during a seizure | 11 | 8 |
| Antiepileptic medications (AEDs) | ||
| Have taken AEDs in the past | 117 | 89 |
| Currently taking AEDs | 89 | 67 |
| Taking AEDs regularly | 76 | 58 |
| Taking medications only when having seizures |
Engagement with traditional healers:
104 participants (79%) reported seeing a traditional healer for their epilepsy, and 94 participants (71%) reported seeing a traditional healer before seeing a physician in the hospital. There was a mean duration of 39 months before seeing a physician. 42 participants (32%) had seen a physician and a traditional healer contemporaneously in the past, and 12 participants (9%) were continuing to see a traditional healer at the time of the study interview. No significant demographic differences were found between participants who were seen by a traditional healer before seeking medical care and those who were not (Table 5). Traditional healing use was not significantly different between households with and without a university-educated head (p>0.05). Of 73 participants with a university-educated head of household, 50 (69%) were seen by a traditional healer before seeking medical care.
Table 5.
Treatment costs
| Treatment | Costs in Guinean francs | Costs in US dollars1 |
|---|---|---|
| Visiting a traditional healer | 300,000 to 10,000,000, one or more cows, sheep, or goats | 33-1,100 |
| Imaging studies | ||
| Non-contrast brain MRI, 0.3 Tesla magnet | 3,800,000 | 418 |
| Gadolinium administration | 500,000 | 55 |
| Non-contrast head CT | 1,000,000 | 110 |
| Urinalysis | 20,000 | 2.20 |
| Medications | ||
| Valproic acid, 40 tablets, each 500 mg | 147,000 | 16.17 |
| Valproic acid, 147 mL, 200 mg/mL concentration syrup | 89,000 | 9.79 |
| Phenobarbital, 20 tablets; each 100 mg | 39,000 | 4.29 |
| Carbamazepine, 50 tablets; each 200 mg | 108,000 | 11.88 |
| Diazepam, 30 tablets; each 10 mg | 53,000 | 5.83 |
| Physicians | ||
| General practitioner, single visit | 3,000 | 0.33 |
| Specialist (e.g. neurologist), single visit | 50,000 | 5.50 |
| Hospital entry fee | 15,000 | 1.65 |
Costs were reported in September 2018 at an exchange rate ot 1 Guinean tranc to 0.00011 US dollars. Costs ot testing and hospital entry fee were obtained from Ignace Deen Teaching Hospital, a public hospital. Costs of medications were obtained from a private pharmacy in Conakry. Costs associated with traditional healers were self-reported by study participants. Guinea’s gross national income per capita was 670 USD in 2016[24].
Reasons given for seeking care from a traditional healer before presenting to a physician included the belief that epilepsy is a djina disease rather than organic disease and the belief that traditional healers might be able to cure epilepsy entirely rather than treating it with lifelong medications.
“The marabout wrote scriptures from the Koran and had her read the scriptures. He said that epilepsy can be cured by this. If this can take away her epilepsy, I think it is better than the pills.”
PWE and caretakers who reported that they did not subscribe to supernatural beliefs regarding epilepsy reported being encouraged by family or community members to seek care from the traditional healer before presenting to a hospital. Factors discouraging PWE from seeking the care of a physician or hospital included expense, distance, and fear of harm from AEDs (Table 6).
“The epilepsy is different from other diseases. It happens so suddenly. That is why [others in my community] think it is a disease of the spirit.”
“Marabouts [traditional healers] were here before the hospital. They were always here, and so, the people will always go to them first.”
“My parents don’t believe in the hospital. They think that seizures are not a problem of hospitals, but a devil problem, so only a marabout can cure me.”
“He saw the marabout when he was a child. They cooked a vulture and he ate that bird. People said that if he ate it, the seizures would stop. When he ate the bird, he did not have seizures for six months. The marabout who treated him was from Ghana, and when he left to go back, the seizures returned.”
Traditional healing practices:
Traditional healing practices were classified into two different categories: treatments administered during a seizure and treatments administered with the goal of preventing seizures or curing epilepsy (Table 4). During seizures, practices included putting garlic, oranges, alcohol, or a paste made of grains into the nose or mouth of the seizing person. Family members reported reading Koranic scripture during a seizure. Many of these practices were believed to “send away the djina” and end a seizure. The practice of giving alcohol to a seizing person was thought to reduce fevers and thereby end seizures.
Preventative or curative treatments for epilepsy prescribed by traditional healers included application of a talisman (French), gris-gris (Malinké), or sebe (Susu), Koranic scripture blessed and then tightly wrapped and sewn in a piece of leather and worn on a specific part of the body, particularly the neck, the wrist, or the upper arm for protection against djina and other malevolent spirits (Figure 1A and B). Other practices included reciting Koranic scripture into bottles of water or rewriting scriptures onto a chalkboard that would then be rinsed with water and used as a bath, splashed in the eyes, or given as a drink to PWE. Related treatments included bathing with a concoction of leaves and oils (Figure 1C), rubbing Koranic scriptures over the body, reciting Koranic scriptures into the ear, recording Koranic scriptures onto a cellphone to be played back, and reading Koranic scriptures into one’s hands and then touching the head and body as a blessing. Some participants reported consuming soot from a burned animal, often a vulture, mixed with water and made into a soup. Almost all participants were asked to provide an animal sacrifice as part of their payment for provision of traditional medicine. These included a cow, goat, or sheep (Table 5), which were cited by participants as a significant expense.
“Three times, we gave a sheep to the marabout for sacrifice to treat my daughter’s epilepsy. The marabout wanted a very expensive sheep, a white sheep with a black line on the neck. I did all of this because I am a mother and I want my daughter to be well.”
Figure 1:
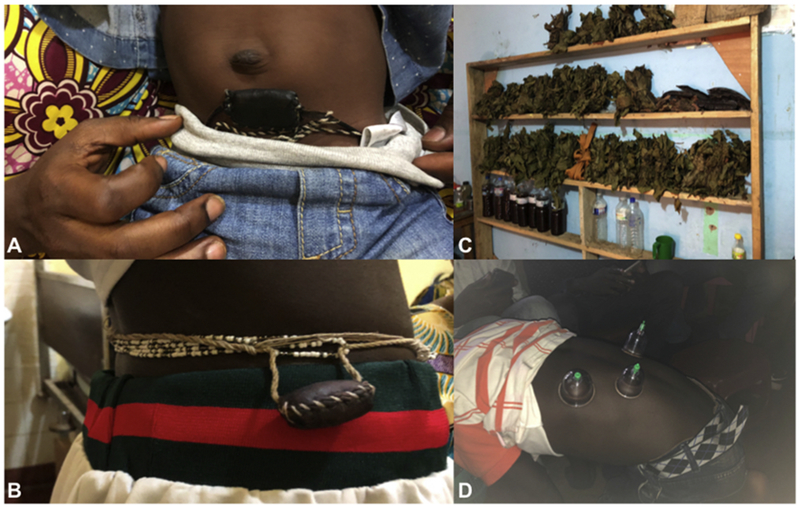
A) and B) Talisman (French), gris-gris (Malinké), or sebe (Susu) prescribed by traditional healers to PWE for protection against djina and other malevolent spirits. C) Herbs and extracts used by a traditional healer in Conakry. D) Application of suction cups to the skin by a traditional healer.
Traditional healing practices.
Discussion:
The majority of PWE in Guinea see traditional healers, on average receiving traditional treatments for more than 3 years prior to seeking medical care and initiating AEDs. Although it is recognized that medically untreated epilepsy is a significant problem throughout SSA, the role of traditional healing in health systems has been under-reported compared to its impact.
Previous studies of traditional healing practices for epilepsy in SSA have described frequent use of herbal remedies and have documented the beliefs that epilepsy is contagious and that it may be caused by witchcraft[11,18]. However, our cohort appears to be unique among previously described populations in SSA because of the predominance of Islamic spiritual beliefs regarding the provenance and treatment of epilepsy. The belief that epilepsy is caused by possession by djina shares similarities with prior studies of predominantly Muslim populations in Morocco, Saudi Arabia, and South Asia, where this belief has been described as a cause of both epilepsy and psychiatric illness[13,28,29]. Many of the healing practices described by participants here involve the use of Koranic scriptures, either spoken or applied to the body, also distinct from prior studies in SSA.
Use of traditional healers was nearly ubiquitous, independent of age, gender, and broadly, household level of education. Notably, more than half of our cohort reported a head of household with university-level of education, yet continued to seek care from traditional healers. Traditional healers are common throughout Guinea and throughout much of SSA, with at least one traditional healer in each village throughout the country compared with just four neurologists centralized in Conakry. Participants reported significant costs associated with both traditional healers and medical care, however, this geographic availability allows PWE to see traditional healers more easily than medical providers.
Participants also reported making the choice to see a traditional healer first because of supernatural beliefs regarding the etiology of epilepsy and because of the belief that traditional healers are able to provide a cure for the spiritual cause of epilepsy rather than medication to control seizures. Given the possibility that an individual will not have a second seizure or will have a second seizure only after a prolonged latency period, traditional healing practices may be erroneously perceived to represent a “cure” for epilepsy and perpetuated. Even those participants and families who denied subscribing to supernatural beliefs regarding the causes of epilepsy reported that community members or relatives had encouraged them to see a traditional healer.
Our data also underscore that traditional healers may be important in influencing community beliefs regarding epilepsy and in changing perceptions. PWE reported referral to medical care by traditional healers if the healers felt that herbal or spiritual interventions were unlikely to improve symptoms. Healers are thus an essential target population for potential interventions and represent a potentially important group for collaborative and multidisciplinary approaches to epilepsy care. Previous studies and public health endeavors in Guinea during the Ebola epidemic found that beliefs and traditional practices represented a key component of disease transmission and that traditional healers were critical in curbing the spread of the disease[30–32]. Our study suggests that this approach is also applicable to a more common, non-communicable disease like epilepsy.
PWE in our cohort were evaluated by a team of West African and U.S.A.-based physicians to make a diagnosis of epilepsy, a strength of the study. However, the study relied on participants’ self-reports of traditional healing use, and interviews were conducted in a clinic setting by medical personnel. A second strength of the study is that participants were recruited as part of a larger study on epilepsy in Guinea and were not specifically recruited for their engagement with traditional healers. However, as a result, our study was also limited to participants who sought medical care at a hospital. It does not describe the beliefs and practices of PWE who are not seeking and who have never sought care from a physician. In this way, we are likely underestimating the impact of traditional healing, since our study sample almost certainly reflects a referral bias of patients who have at least some expectations that medical care can help seizures and may reflect a reporting bias on the part of participants.
We also found that the head of household for the majority of our participants was far more educated than other Guineans. For instance, the United Nations Educational, Scientific and Cultural Organization reports that the literacy rate for Guineans between the ages of 15-24 is 38% for men and 22% for women[33]. The over-representation of highly educated households our cohort is likely related to our study location in a capital city hospital and the self-referred nature of many of our participants. In our view, these findings underscore that even more-educated Guineans retain traditional beliefs about epilepsy. A similar study to ours has not yet been conducted in more rural or remote locations in Guinea to our knowledge.
Interviews revealed shared goals of seizure freedom and improved quality of life for PWE; however, these goals remain out-of-reach for many in Guinea because of misinformation and lack of access to AEDs. As a result, epilepsy causes stigmatization, missed days of school and work, and other financial and social opportunity costs for PWE[34]. Empowering traditional healers to better inform their communities and connect PWE with medical care will be essential in mitigating the public health and personal burden of epilepsy in Guinea.
Highlights:
-
-
The majority of PWE in Guinea seek care from traditional healers before medical care.
-
-
Traditional medicine use is independent of household level of education.
-
-
PWE see traditional healers for >3 years on average before presenting to medical care.
-
-
Epilepsy is believed to be contagious, curable, and caused by spiritual possession.
Acknowledgments
Funding Sources: The Guinea Epilepsy Project is funded by R21 NS098886. Airfare to Dr. Anand was provided by a Massachusetts General Hospital Center for Global Health travel grant.
Appendix 1: Semi-Structured Interview Questions
We would like to talk with you about your experiences with epilepsy as part of our study on epilepsy in Guinea. We are interested in your understanding of your epilepsy. We are also interested in treatments you have tried for your epilepsy and what types of providers you have seen to treat your epilepsy. We hope that your answers to these questions will help us to better take care of people with epilepsy in the future.
What is your primary language?
What are words or phrases that are used for your condition by members of your family or community? What do members of your community think is the cause of your epilepsy?
What do you think caused your epilepsy? Why do you think it started when it did?
Do you think your epilepsy is permanent? Can your epilepsy be cured?
What are the main problems your epilepsy has caused for you? What do you fear most about your epilepsy?
What happens when you have a seizure? What is a seizure? Can you tell when you are going to have a seizure?
What is your religion? What does your religion believe is the cause of your epilepsy?
What providers have you seen regarding treatment for your epilepsy (traditional healer, physician, etc)? Which of these providers is best able to treat your epilepsy?
What are types of treatment for epilepsy? Which treatments are most effective for epilepsy?
What is your desired outcome from treatment (symptom relief, cure, etc)?
What types of biomedical treatments have you received for your epilepsy? Where did you get these medications? Did these treatments work? Did these treatments harm you in any way, and if so, how?
What types of traditional treatments have you received for your epilepsy? Where did you get these treatments? Did these treatments work? Did these treatments harm you in any way, and if so, how?
Are there reasons you would not see a physician for your epilepsy?
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures:
All authors report no conflicts of interest in association with this work.
References
- [1].Preux PM, Druet-Cabanac M. Epidemiology and aetiology of epilepsy in sub-Saharan Africa. Lancet Neurol 2005. doi: 10.1016/S1474-4422(04)00963-9. [DOI] [PubMed] [Google Scholar]
- [2].WHO. EPILEPSY IN THE WHO AFRICAN REGION: Bridging the Gap. World Heal Organ; 2004. doi: 10.1111/j.1528-1167.2009.02184.x. [DOI] [Google Scholar]
- [3].Prevett M Epilepsy in sub-Saharan Africa. Pract Neurol 2013. doi: 10.1136/practneurol-2012-000388. [DOI] [PubMed] [Google Scholar]
- [4].Levira F, Thurman DJ, Sander JW, Hauser WA, Hesdorffer DC, Masanja H, et al. Premature mortality of epilepsy in low- and middle-income countries: A systematic review from the Mortality Task Force of the International League Against Epilepsy. Epilepsia 2017;58:6–16. doi: 10.1111/epi.13603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Birbeck G, Chomba E, Atadzhanov M, Mbewe E, Haworth A. The social and economic impact of epilepsy in Zambia: a cross-sectional study. Lancet Neurol 2007. doi: 10.1016/S1474-4422(06)70629-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Hjortsberg CA. Cost of access to health services in Zambia. Health Policy Plan 2002. doi: 10.1093/heapol/17.1.71. [DOI] [PubMed] [Google Scholar]
- [7].Bias E, Limbambala M. The challenge of hospitals in health sector reform: the case of Zambia. Health Policy Plan 2001. doi: 10.1093/heapol/16.suppl_2.29. [DOI] [PubMed] [Google Scholar]
- [8].lost J, Ratsimbazafy V, Nguyen TT, Nguyen TL, Dufat H, Dugay A, et al. Quality of anti epileptic drugs in sub-Saharan Africa: A study in Gabon, Kenya, and Madagascar. Epilepsia 2018. doi: 10.1111/epi.14445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].lost J, Raharivelo A, Ratsimbazafy V, Nizard M, Auditeau E, Newton CR, et al. Availability and cost of major and first-line antiepileptic drugs: a comprehensive evaluation in the capital of Madagascar. Springerplus; 2016. doi: 10.1186/s40064-016-3409-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Cassell EJ. The Nature of Suffering and the Goals of Medicine. 2004. doi: 10.1093/acprof:oso/9780195156164.001.0001. [DOI] [Google Scholar]
- [11].Kpobi L, Swartz L, Keikelame MJ. Ghanaian traditional and faith healers’ explanatory models for epilepsy. Epilepsy Behav 2018;84:88–92. doi: 10.1016/j.yebeh.2018.04.016. [DOI] [PubMed] [Google Scholar]
- [12].Chomba EN, Haworth A, Atadzhanov M, Mbewe E, Birbeck GL. Zambian health care workers’ knowledge, attitudes, beliefs, and practices regarding epilepsy. Epilepsy Behav 2007;10:111–9. doi: 10.1016/j.yebeh.2006.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Ismail H, Wright J, Rhodes P, Small N. Religious beliefs about causes and treatment of epilepsy. Br J Gen Pract 2005;55:26–31. [PMC free article] [PubMed] [Google Scholar]
- [14].Kaddumukasa M, Kaddumukasa MN, Buwembo W, Munabi IG, Blixen C, Lhatoo S, et al. Epilepsy misconceptions and stigma reduction interventions in sub-Saharan Africa, a systematic review. Epilepsy Behav 2018;85:21–7. doi: 10.1016/j.yebeh.2018.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Millogo A, Ratsimbazafy V, Nubukpo P, Barro S, Zongo I, Preux PM. Epilepsy and traditional medicine in Bobo-Dioulasso (Burkina Faso). Acta Neurol Scand 2004;109:250–4. doi: 10.1111/j.1600-0404.2004.00248.X. [DOI] [PubMed] [Google Scholar]
- [16].Hewson MG. Traditional healers in southern Africa. Ann Intern Med 1998. doi: 10.1074/jbc.M311964200. [DOI] [PubMed] [Google Scholar]
- [17].Puckree T, Mkhize M, Mgobhozi Z, Lin J. African traditional healers: What health care professionals need to know. Int J Rehabil Res 2002. doi: 10.1097/00004356-200212000-00001. [DOI] [PubMed] [Google Scholar]
- [18].Baskind R, Birbeck G. Epilepsy care in Zambia: A study of traditional healers. Epilepsia 2005. doi: 10.1111/j.1528-1167.2005.03505.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Campaign TA, Richter M. Traditional Medicines and Traditional Healers in South Africa. Mercury 2003. [Google Scholar]
- [20].Bradshaw D, Timaeus I. Disease and Mortality in Sub-Saharan Africa: Levels and Trends of Adult Mortality. 2006. doi: 10.1596/978-0-8213-6397-3. [DOI] [Google Scholar]
- [21].World Health Organization (WHO). WHO Traditional Medicine Strategy 2002-2005. 2002. doi:WHO/EDM/TRM/2002.1. [Google Scholar]
- [22].Sen A Human development index. Elgar Companion to Dev. Stud, 2006. doi: 10.1016/S0950-1401(07)80028-0. [DOI] [Google Scholar]
- [23].MSHP. Estimation des Besoins en Ressources Humaines. World Heal Organ; 2012. [Google Scholar]
- [24].Jang M, Sakadi F, Tassiou NR, Abass CF, Grundy SJ, Woga A, et al. Impact of poorly controlled epilepsy in the Republic of Guinea. Seizure 2018;61:71–7. doi: 10.1016/j.seizure.2018.07.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Mclane HC, Berkowitz AL, Patenaude BN, Mckenzie ED, Wolper E, Wahlster S, et al. Availability, accessibility, and affordability of neurodiagnostic tests in 37 countries. Neurology 2015. doi: 10.1212/WNL.0000000000002090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Kleinman A Patients and healers in the context of culture: An Exploration of the Borderland between Anthropology, Medicine, and Psychiatry. Berkeley, CA: University of California Press; 1981. [Google Scholar]
- [27].Hinton DE, Pich V, Chhean D, Pollack MH. ‘The Ghost Pushes You Down’: SleeP Paralysis-Type Panic Attacks in a Khmer Refugee Population. Transcult Psychiatry 2005. doi: 10.1177/1363461505050710. [DOI] [PubMed] [Google Scholar]
- [28].Obeid T, Abulaban A, Al-Ghatani F, Al-Malki AR, Al-Ghamdi A. Possession by “Jinn” as a cause of epilepsy (Saraa): A study from Saudi Arabia. Seizure 2012;21:245–9. doi: 10.1016/j.seizure.2012.01.001. [DOI] [PubMed] [Google Scholar]
- [29].Lim A, Hoek HW, Blom JD. The attribution of psychotic symptoms to jinn in Islamic patients. Transcult Psychiatry 2015;52:18–32. doi: 10.1177/1363461514543146. [DOI] [PubMed] [Google Scholar]
- [30].Bausch DG, Schwarz L. Outbreak of Ebola Virus Disease in Guinea: Where Ecology Meets Economy. PLoS Negl Trop Dis 2014;8:1–5. doi: 10.1371/journal.pntd.0003056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Manguvo A, Mafuvadze B. The impact of traditional and religious practices on the spread of Ebola in West Africa: time for a strategic shift. Pan Afr Med J 2015;22. doi: 10.11694/pamj.supp.2015.22.1.6190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Aminu K, Jegede AS. Traditional Healers ‘ Knowledge of Ebola Virus Disease. SciMedCentral 2017;4:1–6. [Google Scholar]
- [33].UNESCO-UIS. Adult and youth literacy. 2015. doi: 10.1542/peds.107.2.344. [DOI] [Google Scholar]
- [34].Baskind R, Birbeck GL. Epilepsy-associated stigma in sub-Saharan Africa: The social landscape of a disease. Epilepsy Behav 2005;7:68–73. doi: 10.1016/j.yebeh.2005.04.009. [DOI] [PubMed] [Google Scholar]


