Abstract
Background
Subspine impingement is a recognized source of extraarticular hip impingement. Although CT-based classification systems have been described, to our knowledge, no study has evaluated the morphology of the anteroinferior iliac spine (AIIS) with plain radiographs nor to our knowledge has any study compared its appearance between plain radiographs and CT scan and correlated AIIS morphology with physical findings. Previous work has suggested a correlation of AIIS morphology and hip ROM but this has not been clinically validated. Furthermore, if plain radiographs can be found to adequately screen for AIIS morphology, CT could be selectively used, limiting radiation exposure.
Questions/purposes
The purposes of this study were (1) to determine the prevalence of AIIS subtypes in a cohort of patients with symptomatic femoroacetabular impingement; (2) to compare AP pelvis and false profile radiographs with three-dimensional (3-D) CT classification; and (3) to correlate the preoperative hip physical examination with AIIS subtypes.
Methods
A retrospective study of patients undergoing primary hip arthroscopy for femoroacetabular impingement syndrome was performed. Between February 2013 and November 2016, 601 patients underwent hip arthroscopy. To be included here, each patient had to have undergone a primary hip arthroscopy for the diagnosis of femoroacetabular impingement syndrome. Each patient needed to have an interpretable set of plain radiographs consisting of weightbearing AP pelvis and false profile radiographs as well as full documentation of physical findings in the medical record. Patients who additionally had a CT scan with 3-D reconstructions were included as well. During the period in question, it was the preference of the treating surgeon whether a preoperative CT scan was obtained. A total of 145 of 601 (24%) patients were included in the analysis; of this cohort, 54% (78 of 145) had a CT scan and 63% (92 of 145) were women with a mean age of 31 ± 10 years. The AIIS was classified first on patients in whom the 3-D CT scan was available based on a previously published 3-D CT classification. The AIIS was then classified by two orthopaedic surgeons (TGM, MRK) on AP and false profile radiographs based on the position of its inferior margin to a line at the lateral aspect of the acetabular sourcil normal to vertical. Type I was above, Type II at the level, and Type III below this line. There was fair interrater agreement for AP pelvis (κ = 0.382; 95% confidence interval [CI], 0.239-0.525), false profile (κ = 0.372; 95% CI, 0.229-0.515), and 3-D CT (κ = 0.325; 95% CI, 0.156-0.494). There was moderate to almost perfect intraobserver repeatability for AP pelvis (κ = 0.516; 95% CI, 0.284-0.748), false profile (κ = 0.915; 95% CI, 0.766-1.000), and 3-D CT (κ = 0.915; 95% CI, 0.766-1.000). The plane radiographs were then compared with the 3-D CT scan classification and accuracy, defined as the proportion of correct classification out of total classifications. Preoperative hip flexion, internal rotation, external rotation, flexion adduction, internal rotation, subspine, and Stinchfield physical examination tests were compared with classification of the AIIS on 3-D CT. Finally, preoperative hip flexion, internal rotation, and external rotation were compared with preoperative lateral center-edge angle and alpha angle.
Results
The prevalence of AIIS was 56% (44 of 78) Type I, 39% (30 of 78) Type II, and 5% (four of 78) Type III determined from the 3-D CT classification. For the plain radiographic classification, the distribution of AIIS morphology was 64% (93 of 145) Type I, 32% (46 of 145) Type II, and 4% (six of 145) Type III on AP pelvis and 49% (71 of 145) Type I, 48% (70 of 145) Type II, and 3% (four of 145) Type III on false profile radiographs. False profile radiographs were more accurate than AP pelvis radiographs for classification when compared against the gold standard of 3-D CT at 98% (95% CI, 96-100) versus 80% (95% CI, 75-85). The false profile radiograph had better sensitivity for Type II (97% versus 47%, p < 0.001) and specificity for Types I and II AIIS (97% versus 53%, p < 0.001; 98% versus 90%, p = 0.046) morphology compared with AP pelvis radiographs. There was no correlation between AIIS type as determined by 3-D CT scan and hip flexion (rs = -0.115, p = 0.377), internal rotation (rs = 0.070, p = 0.548), flexion adduction internal rotation (U = 72.00, p = 0.270), Stinchfield (U = 290.50, p = 0.755), or subspine tests (U = 319.00, p = 0.519). External rotation was weakly correlated (rs = 0.253, p = 0.028) with AIIS subtype. Alpha angle was negatively correlated with hip flexion (r = -0.387, p = 0.002) and external rotation (r = -0.238, p = 0.043) and not correlated with internal rotation (r = -0.068, p = 0.568).
Conclusions
The findings in this study suggest the false profile radiograph is superior to an AP radiograph of the pelvis in evaluating AIIS morphology. Neither preoperative hip internal rotation nor impingement tests correlate with AIIS type as previously suggested questioning the utility of the AIIS classification system in identifying pathologic AIIS anatomy.
Level of Evidence
Level III, diagnostic study.
Introduction
Femoroacetabular impingement (FAI) is now well established as a cause of hip pain in young, active adults and effective strategies have been developed to arthroscopically treat this intraarticular impingement syndrome with reliable outcomes [5-8, 10, 19, 22, 26]. Recently, a separate etiology of hip pain has been described, called extraarticular impingement syndrome. This includes iliopsoas, ischiofemoral, greater trochanteric, and subspine impingement [3, 4, 20, 28]. Subspine impingement as proposed occurs when a low-hanging anteroinferior iliac spine (AIIS) contacts the femoral neck in positions of extreme hip flexion and internal rotation [12, 25]. A CT-based classification of AIIS morphology has been described by Hetsroni et al. [12]; Type I AIIS has a clear shelf of ilium between the AIIS and the acetabular rim, Type II AIIS extends to the acetabular rim, and Type III extends distally beyond the level of the acetabular rim and has a downward “spur” appearance. Types II and III appeared to correlate with decreasing hip flexion and internal rotation in a computer simulation model and was viewed by the authors as evidence of a contribution to subspine impingement [12]. Consequently, Types II and III AIIS morphologies have subsequently been labeled as potential “pathologic” subtypes and are implicated in causing subspine impingement [2, 12]. Several studies have used two-dimensional (2-D) CT and plain radiographs to further characterize AIIS morphology [1, 17]; however, the only published classification system implements three-dimensional (3-D) CT imaging. A recent study found false profile radiography is comparable to CT in measuring novel angular measurements of AIIS anatomy [27]. No study has evaluated plain radiographs in classifying the AIIS based on the current 3-D classification system and if comparable may be a useful screening study in the evaluation AIIS anatomy.
Arthroscopic decompression has been proposed as treatment for extraarticular subspine impingement [11, 16, 23]. Most studies surrounding subspine impingement relate to a low-hanging AIIS exostosis related to previous direct head of rectus avulsion injury, so-called Type III AIIS as described by Hetsroni et al. [11, 13, 21, 23, 24, 30]. This entity likely represents a situation in which true subspinous bony impingement can occur. Many authors have also suggested that similar direct pathologic impingement may occur with Type II AIIS and patients with this morphologic variant sometimes undergo arthroscopic decompression. A recent study found no difference in the distribution of “abnormal” (Types II and III AIIS) morphology among asymptomatic and symptomatic patients [2]. The impetus to conclude Types II and III AIIS as pathologic was based on 3-D CT computer modeling, which demonstrated decreased hip motion; this decreased motion was felt to represent bony impingement in a cohort of patients with established symptomatic FAI [12]. Because FAI has been previously documented to coexist with decreased hip motion [14, 31], the conclusion reached may be confounded by a population with already limited hip motion and a known source of hip pain. Furthermore, to our knowledge, no study has corroborated these simulated hip motions with physical examination findings.
The purposes of this study were to (1) determine the prevalence of AIIS subtypes in a cohort of patients with symptomatic FAI; (2) compare AP pelvis and false profile radiographs with a 3-D CT AIIS classification system; and (3) correlate the preoperative hip physical examination with published “pathologic” AIIS subtypes.
Patients and Methods
A retrospective chart study of patients diagnosed with FAI from February 2013 to November 2016 was performed. Between February 2013 and November 2016, 601 patients underwent hip arthroscopy. Inclusion criteria for patients selected for this study were (1) persistent hip pain and mechanical symptoms consistent with FAI syndrome refractory to nonoperative management; (2) reproducible clinical examination findings suggestive of FAI syndrome; and (3) a joint space width of > 3 mm on all radiographic and 3-D CT views in addition to no full-thickness chondral defects on MRI. Nonoperative treatment included activity modification, nonsteroidal antiinflammatory drugs, physical therapy > 6 months, and intraarticular corticosteroid injections. To be included here, each patient had to have undergone primary hip arthroscopy for the diagnosis of FAI syndrome. Each patient needed to have an interpretable set of plain radiographs consisting of weightbearing AP pelvis and false profile radiographs as well as full documentation of physical findings in the medical record. Patients who additionally had a CT scan with 3-D reconstructions were included as well. During the period in question, it was the preference of the treating surgeon whether a preoperative CT scan was obtained. Surgeries were performed by two high-volume orthopaedic surgeons (SKA, TGM) experienced in hip arthroscopy. Exclusion criteria included revision surgery or any previous hip surgery (to avoid altered AIIS anatomy from previous acetabuloplasty), patients with Tönnis Grade ≥ 2, and any patients who did not have adequate AP pelvis and false profile preoperative radiographs. Demographic data were collected including age, sex, and laterality. This left 145 of 601 (24%) patients included in the analysis of whom 78 of 145 (54%) had a CT scan and 92 of 145 (63%) were women with a mean age of 31 ± 10 years (Table 1).
Table 1.
Patient demographics

Radiographic AIIS classifications were performed adapted from an established 3-D CT-based classification system [12]. These classifications were determined using a line perpendicular to the vertical axis placed at the lateral-most margin of the acetabular sourcil. The AIIS was classified based on the position of its inferior margin to this sourcil line (Fig. 1). A Type I AIIS was above, a Type II at the level, and a Type III below the level of the sourcil line. Classifications were determined on both standing AP and false profile radiographs for all hips. Two orthopaedic surgeons (TGM, MRK) independently determined the classification of the AIIS for all patients. One surgeon (TGM) is a fellowship-trained hip preservation specialist who had his patients included in the series, whereas the second surgeon was an orthopaedic sports medicine fellow specializing in hip preservation and was involved in the care of some of the patients in the series. There was fair interrater agreement for AP pelvis (κ = 0.382; 95% confidence interval [CI], 0.239-0.525), false profile (κ = 0.372; 95% CI, 0.229-0.515), and 3-D CT (κ = 0.325; 95% CI, 0.156-0.494). There was moderate to almost perfect intraobserver repeatability for AP pelvis (κ = 0.516; 95% CI, 0.284-0.748), false profile (κ = 0.915; 95% CI, 0.766-1.000, and 3-D CT (κ = 0.915; 95% CI, 0.766-1.000). To ensure pelvic tilt did not influence AIIS classification on the AP pelvis radiograph, the pubic symphysis-coccygeal distance was calculated [29]. This distance was calculated using a line that intersects the superior-most part of the pubic symphysis and a second line perpendicular to the pubic symphysis line. The distance from the pubic symphysis line to the inferior-most part of the coccyx was then measured. Lastly the preoperative lateral center-edge angle (LCEA) and alpha angle (AA) were measured on preoperative radiographs.
Fig. 1 A-B.
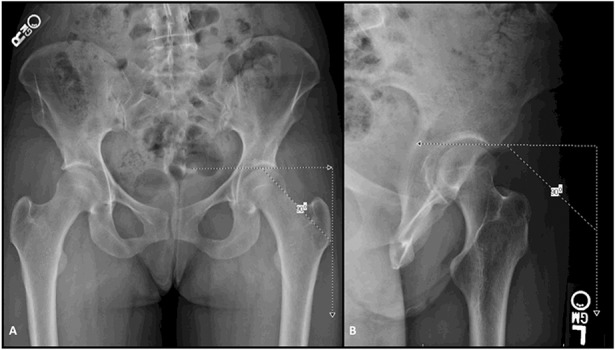
The AIIS was classified on 3-D CT scan based on a previous published classification system and then by the position of its inferior margin to the sourcil line on the AP pelvis (A) and false profile (B) radiographs. A Type I AIIS was above, a Type II at the level, and a Type III below the level of the sourcil line.
Of the 145 classified hips, 78 had CT with 3-D reconstructions available for review. The AIIS of these CT scans was classified using the Hetsroni classification: Type I = there is a smooth ilium wall without bony prominences between the caudad level of the AIIS and the acetabular rim; Type II = there are bony prominences on the ilium wall extending from the caudad area of the AIIS to the acetabular rim or, alternatively, the AIIS sits just at the level of the acetabular rim and appears as a “roof-like” prominence over the hip; and Type III = the AIIS extends distally to the anterosuperior acetabular rim [12].
Physical Examination Maneuvers
Preoperative physical examination data were collected including terminal hip flexion, internal rotation, external rotation, and results of the flexion adduction internal rotation (FADIR), subspine, and Stinchfield tests from a retrospective chart review. Hip ROM was measured and documented in the preoperative clinic visit by the treating senior surgeon (TGM, SKA). Terminal hip flexion and internal and external rotation were estimated in a supine position and were measured without the use of a goniometer. The examiner was not specifically blinded to imaging studies; however, ROM was calculated before any imaging review, and AIIS classifications were made retrospectively from the time of initial examination.
The flexion adduction internal rotation test is a physical examination test for FAI syndrome. The patient was positioned supine and with the hip and knee at 90° of flexion, the hip was brought through increasing hip flexion, internal rotation, and adduction in a smooth arc of motion. The examination was graded as positive if the patient reported pain in the groin reproducing their symptoms.
The subspine test was performed in the supine position by placing the hip into maximum hip flexion. A positive examination produced pain with maximal hip flexion. The Stinchfield examination is performed in the supine position while the patient is asked to perform a straight leg raise against resistance. A positive examination produces pain in a typical pattern related to the sensory innervation of the hip (groin, thigh, buttock, or knee).
Endpoints of Interest
The primary research question was to determine the prevalence of the various AIIS morphologies on what we consider to be the most definitive test for this assessment, the 3-D CT scan. Our second research question sought to determine the accuracy (defined as the proportion of correctly classified subjects out of the total number of subjects) and reproducibility of false profile and AP pelvis radiographs as compared with the gold standard of 3-D CT for classifying AIIS morphology; we also calculated the sensitivity and specificity of each modality (false profile and AP pelvis) as a diagnostic test. To answer our third question, we sought to correlate positive findings on physical examination maneuvers as described previously with the AIIS classification as determined by 3-D CT scan. This study was approved by the University of Utah institutional review board (#71733).
Statistical Analysis
Patient demographics were summarized with categorical variables reported as frequencies and percentages and continuous variables reported as means and SDs. The prevalence of each AIIS subtype was described by imaging modality. Sensitivity, specificity, and accuracy of each subtype on AP and false profile radiographs were compared with CT classification for patients with 3-D reconstructions. The sensitivity and specificity of each subtype on AP pelvis and false profile were compared using McNemar’s test or exact McNemar’s test where appropriate. Correlations among preoperative ROM, LCEA, AA, and AIIS subtype were analyzed using Spearman’s correlation. Preoperative physical examination tests (FADIR, subspine, and Stinchfield) were correlated to AIIS subtype using the Wilcoxon rank-sum test. Pearson’s correlation was used to compare preoperative ROM with preoperative LCEA and AA. Finally, interrater agreement and intraobserver repeatability were analyzed using Cohen’s κ statistic.
Results
The prevalence of AIIS was 56% (44 of 78) Type I, 39% (30 of 78) Type II, and 5% (four of 78) Type III determined from the 3-D CT classification. For the plain radiographic classification, the distributions of AIIS morphology were 64% (93 of 145) Type I, 32% (46 of 145) Type II, and 4% (six of 145) Type III on AP pelvis and 49% (71 of 145) Type I, 48% (70 of 145) Type II, and 3% (four of 145) Type III on false profile radiographs. The overall accuracy (the proportion of correctly classified subjects out of the total number of subjects) of the false profile radiographs was better than AP pelvis radiographs for AIIS classification when compared against the gold standard of 3-D CT (98% [95% CI, 96-100] versus 80% [95% CI, 75-85]). The sensitivity and specificity (Table 2) of AP pelvis versus the 3-D CT classification of Type 1 AIIS was 86% (95% CI, 73- 95) and 53% (95% CI, 35-70); 47% (95% CI, 28-66) and 90% (95% CI, 77-97) for Type II AIIS; and 75% (95% CI, 19-99) and 97% (95% CI, 91-100) for Type III, respectively. There was superior sensitivity and specificity of the false profile compared with 3-D CT scan with Type I AIIS at 98% (95% CI, 88-100; χ 2[1] = 5.0, p = 0.063) and 97% (95% CI, 85-100; χ2[1] = 15.0, p < 0.001); Type II at 97% (95% CI, 83-100; χ 2[1] = 15.0, p < 0.001) and 98% (95% CI, 89-100; χ 2[1] = 4.00, p = 0.046); and Type III at 100% (95% CI, 40-100; χ 2[1] = 1.00, p = 1.000) and 100% (95% CI, 95-100; χ 2[1] = 2.00, p = 0.500) sensitivity and specificity, respectively (Table 2).
Table 2 A-C.
(A) Total numbers for 3 x 3 matrix; (B) sensitivity, specificity, and accuracy of AP and false profile (FP) radiographs compared with CT imaging; and (C) sensitivity and specificity of AP and FP radiographs compared using McNemar’s test or exact McNemar’s test where appropriate
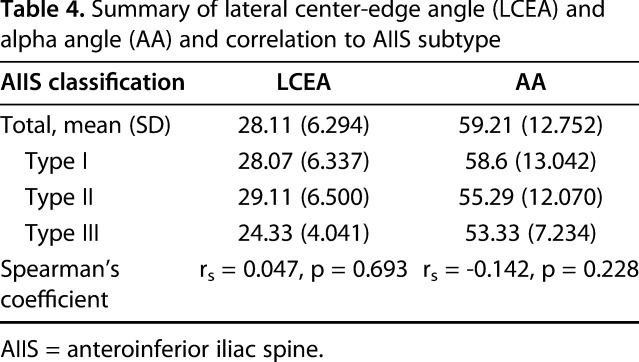
There was no correlation between AIIS type and hip flexion (rs = -0.115, p = 0.377) or internal rotation (rs = 0.070, p = 0.548) and a weak correlation between AIIS type and external rotation (rs = 0.253, p = 0.028) ROM; there were also no correlations to the specialized hip tests including the FADIR test (U = 72.00, p = 0.270), Stinchfield test (U = 290.50, p = 0.755), or subspine test (U = 319.00, p = 0.519) as compared with the 3-D CT AIIS classification (Table 3). There was no correlation between LCEA (rs = 0.047, p = 0.693) and AA (rs = -0.142, p = 0.228) to AIIS subtype (Table 4). Preoperative AA was negatively correlated with hip flexion (r = -0.387, p = 0.002) and external rotation (r = -0.238, p = 0.043) but was not correlated with internal rotation (r = -0.068, p = 0.568).
Table 3.
Correlation of physical examination to AIIS types

Table 4.
Summary of lateral center-edge angle (LCEA) and alpha angle (AA) and correlation to AIIS subtype
Discussion
The current gold standard in evaluating AIIS morphology is a 3-D CT-based system proposed by Hetsroni et al. [12]. In this study, we found the overall distribution of AIIS morphology to be overwhelmingly Type I and Type II on 3-D CT images (95%). Additionally, we found the false profile radiograph to be accurate in classifying AIIS morphology with the Hetsroni 3-D CT AIIS classification adapted to plain 2-D radiographic projections. The false profile radiograph had better sensitivity for Type II and specificity for Types I and II AIIS morphology compared with AP pelvis radiographs. A previous study has implicated Type II and Type III AIIS morphology as pathologic based on the limitation of hip motion seen on a simulated model [12]. More recent studies have questioned the pathoanatomy of Types II and III AIIS variants, because no difference in symptoms was found in these subtypes [2]. This current study found no correlation among AIIS subtype, hip flexion, internal rotation, or hip impingement physical examination tests.
Limitations of this study include the potential for selection bias because approximately half of the patients had the gold standard test of the 3-D CT scan. We realize this could introduce bias toward certain clinical presentations or radiographic findings affecting the decision to obtain a CT scan, thus influencing the classification or the group of patients and subsequent correlation of physical examination findings. The practice of ordering a CT was at the discretion of the senior surgeons (TGM, SKA) in this study. The practice of one surgeon (TGM) was to obtain 3-D CT scans on all hips, whereas the other surgeon (SKA) did not routinely order CT scans. The majority of one of the author’s (SKA) patients obtained 3-D CT scans from referring physicians before evaluation. The potential for selection bias was thereby minimized because patient characteristics had no influence on either surgeon’s decision to obtain advanced imaging. Second, the potential for assessment bias exists in the accuracy of measuring hip ROM in the clinical setting. The authors acknowledge the difficulty in measuring hip ROM and the potential to induce error in measurements by the examiner. Hip motion was determined and recorded based on the estimate of motion obtained by the senior surgeons (TGM, SKA) experienced in the examination of the hip. We found no correlation between hip flexion and internal rotation and AIIS morphology. We acknowledge that variation in estimating hip ROM could lead to a Type II error. In the study of Hetsroni et al. [12], the mean difference in hip flexion and internal rotation between Type I and Type III AIIS was nearly 30° (120° versus 93°) and 15° (21° to 8°), respectively. If large differences of 15° to 30° exist between Types I and III AIIS as suggested by the previous study, these differences would have been able to be detected with clinical estimation of hip ROM by experienced clinicians. Similar to Hetsroni et al. [12], there is an overall low prevalence of Type III AIIS morphology in the current study as well (four of 53 in the Hetsroni et al. study versus four of 78 in this study). This reflects the overall rarity of this AIIS morphology in at least the FAI population and could underpower the conclusions of this and previous studies. Larger studies would be needed to see if these conclusions remain true. Third, the imaging in this study was performed in the supine or standing position and clinical ROM was documented with the patient in a supine position. A sitting or squatting position may lead to increased anterior pelvic tilt that could cause pathologic impingement that is underappreciated by clinical ROM evaluation. However, all ROM evaluations in this study were performed with the pelvis stabilized in a supine position, and end range of hip motion was documented immediately before initiating pelvic motion. Given this, it is reasonable to believe that the documented end range of hip motion serves as a surrogate evaluation for impingement initiation. Lastly, this series was similar to previous studies in that the current cohort was comprised of a heterogeneous group of patients with FAI with cam, pincer, mixed cam and pincer, and subspine impingement. Although no association was identified between AIIS subtype and hip physical examination data, this could be confounded by the multiple hip pathologies present in this patient cohort. However, the clinical scenario of isolated subspine decompression in practice rarely occurs and when present likely represents a large Type III AIIS avulsion. Given this, the current data may be applied to the majority of patients with impingement-related hip pain including both FAI and subspine impingement.
We found that most patients had Type I AIIS morphology on 3-D CT scan. In the series of Hetsroni et al., the overall distribution AIIS morphology was 17% Type I, 75% Type II, and 8% Type III with 83% being Type II or III. Similarly, Balazs et al. found 75% of asymptomatic and 80% of symptomatic patients to have Type II or III AIIS [2]. The distribution in our study demonstrated a much higher frequency of Type I morphology than what was observed in previous series [2, 12]. The interrater agreement between classification types in our study was only fair for all modalities with the highest disagreement occurring between AIIS Types I and II on 3-D CT. We believe that this interobserver variability occurred largely as a result of the definition of these types in the previously described classification system. The system proposed by Hetsroni et al. classifies Type II as a bony prominence of the ilium wall extending from the caudad area of the AIIS to the acetabular rim. However, in many patients, the AIIS can be seen as confluent with the ilium wall and acetabular rim without a distinct separation among these structures. In these situations, it can be difficult for the observer to differentiate between Type I and Type II AIIS. This difficulty was observed in the present study and accounted for the highest disagreement in classification of these two subtypes. The same situation was identified by Balazs et al. with only moderate interobserver agreement overall and substantial disagreement identified among observers between Types I and II subtypes. Moreover, these authors similarly commented on the difficult interpretation of the bony wall of the ilium between the AIIS and acetabular rim as a likely source of disagreement [2].
The false profile view provided better accuracy than did the AP pelvis when compared with 3-D CT scans in terms of classifying AIIS morphology. Additionally, the false profile radiograph had better sensitivity for Type II and specificity for Types I and II AIIS morphology compared with AP pelvis radiographs. For Type III morphology, it is likely we were underpowered to detect a difference because there were only four Type III morphotypes in the series. Our results demonstrate the AIIS can be adequately evaluated using plain radiographs and is an accurate alternative to the current 3-D CT classification system. Moreover, the reduced cost and radiation exposure may make plain radiographic evaluation of the AIIS a better alternative to 3-D CT in most instances. The CT-based classification system of AIIS morphology proposed by Hetsroni et al. [12] is the only radiographic classification system regarding the morphologic characteristics of the AIIS. Lee et al. quantitatively evaluated the position of the AIIS relative to the teardrop line on the AP view and from the AIIS to the acetabular rim on the false profile view [17]. The authors did not describe morphologic classification of the AIIS. Additionally, Schindler et al. described quantitative distances from the AIIS to the 12 o’clock position of the acetabular rim and adapted the center-edge angle to the AIIS in both the AP and false profile views [27]. No study, to our knowledge, has compared the ability to classify the AIIS on plain radiographs based on the currently accepted 3-D CT system. Because the radiation exposure of CT evaluation is of concern [9], the ability to perform screening studies with plain imaging modalities is appealing from both patient safety and cost-saving perspectives. In this study, we have adapted the Hetsroni et al. 3-D CT classification system to plain radiographs. The false profile view as described by Lequesne and de Seze [18] provides a profile view of the AIIS, which has been shown to be more accurate than the AP view and as reliable as CT to demonstrate AIIS morphology [27]. Our data support these findings and suggest the false profile view is a superior method of characterizing AIIS morphology with an overall accuracy of 98% versus 80% with the AP view as compared with the current gold standard 3-D CT. This study suggests a false profile radiograph may be an adequate screening tool in the evaluation of the AIIS morphotype allowing selective 3-D CT scans in individuals in whom the clinical picture warrants further anatomic characterization. Future large-scale studies are needed to determine if the findings of this study remain true.
We found no correlation with the numbers available between AIIS morphology on 3-D CT scan and preoperative internal rotation and provocative examination tests in patients with FAI undergoing surgery. These findings bring into question the importance of the AIIS morphology and the role of this morphotype in causing bony impingement. With the relatively rare prevalence of Type III AIIS in this and previous investigations (1%-8%) [2, 12], it appears the most prevalent morphologic subtypes appear to be Types I and II, which may, in fact, represent normal AIIS morphology variants. Given this, the importance of distinguishing between Types I and II radiographically or clinically may be inconsequential if neither is pathologic as the aforementioned and current studies suggest. It could be, however, in individuals with prominent AIIS anatomy and supraphysiologic hip ROM that soft tissue impingement is possible despite no bony contact. A previous study by Kapron et al. utilizing high-speed dual fluoroscopy determined no bony contact actually occurs in the setting of FAI with a minimal bony distance of 3 mm in maximal hip flexion, adduction, and internal rotation implicating the femoral cam lesion in soft tissue but not bony impingement [14]. The possibility of a Type II AIIS clinically causing bony impingement has not been determined; however, this direct bony impingement seems unlikely given the findings of that study. We did not specifically study the influence of femoral version and hip motion, which has been recently suggested to be more influential to hip internal rotation over CAM deformity [15] and could account for the variation of internal rotation in this cohort. However, the present study found no effect of AA on internal rotation and demonstrated a negative correlation to hip flexion consistent with the findings of the previously mentioned study. These data further suggest that cam deformity likely influences hip flexion but may not have an effect on hip internal rotation as previously believed. Surgical treatment of subspine impingement has been described with favorable results [4]; however, the role of subspine decompression cannot be clearly delineated because all of these patients with Type II or III AIIS had other concomitant procedures including decompression for FAI morphology. Based on these confounding circumstances, it is difficult to conclude that subspine subtype in isolation is responsible for preoperative symptoms or that subspine decompression influences patient outcomes. Hetsroni et al. used simulated hip motion as a surrogate for impingement; we found in this study no correlation of clinical preoperative hip flexion or internal rotation among AIIS subtypes or FADIR, subspine, or Stinchfield tests. We did, however, find a weak correlation between preoperative external rotation and increasing AIIS morphotype, but the clinical importance of this finding is unclear. Balazs et al. also found no difference in the distribution of normal versus abnormal (Type II or III) AIIS morphology between symptomatic and asymptomatic patients questioning the implication of the AIIS in clinical extraarticular hip impingement [2]. Although large inferior extensions of the AIIS in Type III variants likely contribute to clinical impingement, these variants are rare both in our series and previous studies [2, 12] and in our opinion represent an AIIS avulsion or traction injury rather than an anatomic variant as previously described [13, 21, 23, 24, 30]. The implication of Type II AIIS morphology as pathologic based on the current study and previous studies appears to be unclear. Further studies need to be conducted to determine the clinical utility of subspine decompression of Type II AIIS.
The findings in this study suggest the false profile radiograph is superior to an AP radiograph of the pelvis in evaluating AIIS morphology. Neither preoperative hip internal rotation nor impingement tests correlate with AIIS type as previously suggested questioning the utility of the AIIS classification system in identifying pathologic AIIS anatomy. Although the authors recommend that surgical decision-making for AIIS decompression is multifactorial, the current data suggest that AIIS Types I and II are difficult to subdivide and possibly may represent normal variants, whereas AIIS Type III subtypes are rare. Further clinical studies are warranted to determine if these findings remain true in larger series.
Acknowledgments
We thank Angela P. Presson PhD, for her assistance in the statistical analysis in this study.
Footnotes
This investigation was supported by the University of Utah Study Design and Biostatistics Center with funding in part from the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant 8UL1TR000105 (APP; formerly UL1RR025764). One of the authors certifies that he (SKA), or a member of his immediate family, has received or may receive payments or benefits, during the study period, an amount of USD 10,000 to USD 100,000 from Stryker (Kalamazoo, MI, USA). One of the authors certifies that he (TGM), or a member of his immediate family, has received or may receive payments or benefits, during the study period, an amount of less than USD 10,000 from Arthrex (Naples, FL, USA). One of the authors certifies that he (MJS), or a member of his immediate family, has received or may receive payments or benefits, during the study period, an amount of USD 10,000 to USD 100,000 from Smith & Nephew Endoscopy (London, UK). One of the authors certifies that he (MJS), or a member of his immediate family, has received or may receive payments or benefits, during the study period, an amount of USD 10,000 to USD 100,000 from Stryker.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at the University of Utah, Department of Orthopaedics, Salt Lake City, UT, USA.
References
- 1.Amar E, Druckmann I, Flusser G, Safran MR, Salai M, Rath E. The anterior inferior iliac spine: size, position, and location. An anthropometric and sex survey. Arthroscopy. 2013;29:874–881. [DOI] [PubMed] [Google Scholar]
- 2.Balazs GC, Williams BC, Knaus CM, Brooks DI, Dickens JF, McCabe MP, Anderson TD. Morphological distribution of the anterior inferior iliac spine in patients with and without hip impingement: reliability, validity, and relationship to the intraoperative assessment. Am J Sports Med. 2017;45:1117–1123. [DOI] [PubMed] [Google Scholar]
- 3.Cheatham SW. Extra-articular hip impingement: a narrative review of the literature. J Can Chiropr Assoc. 2016;60:47–56. [PMC free article] [PubMed] [Google Scholar]
- 4.de Sa D, Alradwan H, Cargnelli S, Thawer Z, Simunovic N, Cadet E, Bonin N, Larson C, Ayeni OR. Extra-articular hip impingement: a systematic review examining operative treatment of psoas, subspine, ischiofemoral, and greater trochanteric/pelvic impingement. Arthroscopy. 2014;30:1026–1041. [DOI] [PubMed] [Google Scholar]
- 5.Ejnisman L, Philippon MJ, Lertwanich P. Acetabular labral tears: diagnosis, repair, and a method for labral reconstruction. Clin Sports Med. 2011;30:317–329. [DOI] [PubMed] [Google Scholar]
- 6.Fabricant PD, Heyworth BE, Kelly BT. Hip arthroscopy improves symptoms associated with FAI in selected adolescent athletes. Clin Orthop Relat Res. 2012;470:261–269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ganz R, Leunig M, Leunig-Ganz K, Harris WH. The etiology of osteoarthritis of the hip: an integrated mechanical concept. Clin Orthop Relat Res. 2008;466:264–272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ganz R, Parvizi J, Beck M, Leunig M, Notzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:112–120. [DOI] [PubMed] [Google Scholar]
- 9.Giordano BD, Grauer JN, Miller CP, Morgan TL, Rechtine GR., 2nd Radiation exposure issues in orthopaedics. J Bone Joint Surg Am. 2011;93:e69(61–10). [DOI] [PubMed] [Google Scholar]
- 10.Gupta A, Redmond JM, Stake CE, Dunne KF, Domb BG. Does primary hip arthroscopy result in improved clinical outcomes? 2-Year clinical follow-up on a mixed group of 738 consecutive primary hip arthroscopies performed at a high-volume referral center. Am J Sports Med. 2016;44:74–82. [DOI] [PubMed] [Google Scholar]
- 11.Hetsroni I, Larson CM, Dela Torre K, Zbeda RM, Magennis E, Kelly BT. Anterior inferior iliac spine deformity as an extra-articular source for hip impingement: a series of 10 patients treated with arthroscopic decompression. Arthroscopy. 2012;28:1644–1653. [DOI] [PubMed] [Google Scholar]
- 12.Hetsroni I, Poultsides L, Bedi A, Larson CM, Kelly BT. Anterior inferior iliac spine morphology correlates with hip range of motion: a classification system and dynamic model. Clin Orthop Relat Res. 2013;471:2497–2503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Irving MH. Exostosis formation after traumatic avulsion of the anterior inferior iliac spine. Report of two cases. J Bone Joint Surg Br. 1964;46:720–722. [PubMed] [Google Scholar]
- 14.Kapron AL, Aoki SK, Peters CL, Anderson AE. Subject-specific patterns of femur-labrum contact are complex and vary in asymptomatic hips and hips with femoroacetabular impingement. Clin Orthop Relat Res. 2014;472:3912–3922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kraeutler MJ, Chadayammuri V, Garabekyan T, Mei-Dan O. Femoral version abnormalities significantly outweigh effect of cam impingement on hip internal rotation. J Bone Joint Surg Am. 2018;100:205–210. [DOI] [PubMed] [Google Scholar]
- 16.Larson CM, Kelly BT, Stone RM. Making a case for anterior inferior iliac spine/subspine hip impingement: three representative case reports and proposed concept. Arthroscopy. 2011;27:1732–1737. [DOI] [PubMed] [Google Scholar]
- 17.Lee WA, Saroki AJ, Loken S, Trindade CA, Cram TR, Schindler BR, LaPrade RF, Philippon MJ. Radiographic identification of arthroscopically relevant acetabular structures. Am J Sports Med. 2016;44:67–73. [DOI] [PubMed] [Google Scholar]
- 18.de Seze Lequesne M. [False profile of the pelvis. A new radiographic incidence for the study of the hip. Its use in dysplasias and different coxopathies] [in French]. Rev Rhum Mal Osteoartic. 1961;28:643–652. [PubMed] [Google Scholar]
- 19.Levy DM, Kuhns BD, Chahal J, Philippon MJ, Kelly BT, Nho SJ. Hip arthroscopy outcomes with respect to patient acceptable symptomatic state and minimal clinically important difference. Arthroscopy. 2016;32:1877–1886. [DOI] [PubMed] [Google Scholar]
- 20.Marin-Pena O, Sierra-Madrid P, Lax-Perez R, Ferrero-Manzanal F. Extrarticular hip impingement. Hip Int. 2016;26(Suppl 1):14–16. [DOI] [PubMed] [Google Scholar]
- 21.Matsuda DK, Calipusan CP. Adolescent femoroacetabular impingement from malunion of the anteroinferior iliac spine apophysis treated with arthroscopic spinoplasty. Orthopedics. 2012;35:e460–463. [DOI] [PubMed] [Google Scholar]
- 22.Nho SJ, Magennis EM, Singh CK, Kelly BT. Outcomes after the arthroscopic treatment of femoroacetabular impingement in a mixed group of high-level athletes. Am J Sports Med. 2011;39(Suppl):14S–19S. [DOI] [PubMed] [Google Scholar]
- 23.Pan H, Kawanabe K, Akiyama H, Goto K, Onishi E, Nakamura T. Operative treatment of hip impingement caused by hypertrophy of the anterior inferior iliac spine. J Bone Joint Surg Br. 2008;90:677–679. [DOI] [PubMed] [Google Scholar]
- 24.Rajasekhar C, Kumar KS, Bhamra MS. Avulsion fractures of the anterior inferior iliac spine: the case for surgical intervention. Int Orthop. 2001;24:364–365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rossi F, Dragoni S. Acute avulsion fractures of the pelvis in adolescent competitive athletes: prevalence, location and sports distribution of 203 cases collected. Skeletal Radiol. 2001;30:127–131. [DOI] [PubMed] [Google Scholar]
- 26.Sansone M, Ahlden M, Jonasson P, Thomee C, Sward L, Ohlin A, Baranto A, Karlsson J, Thomee R. Outcome after hip arthroscopy for femoroacetabular impingement in 289 patients with minimum 2-year follow-up. Scand J Med Sci Sports. 2017;27:230–235. [DOI] [PubMed] [Google Scholar]
- 27.Schindler BR, Venderley MB, Mikula JD, Chahla J, Dornan GJ, Turnbull TL, LaPrade RF, Philippon MJ. Comparison of radiographs and computed tomography for the screening of anterior inferior iliac spine impingement. Arthroscopy. 2017;33:766–772. [DOI] [PubMed] [Google Scholar]
- 28.Sutter R, Pfirrmann CW. Atypical hip impingement. AJR Am J Roentgenol. 2013;201:W437–442. [DOI] [PubMed] [Google Scholar]
- 29.Tannast M, Zheng G, Anderegg C, Burckhardt K, Langlotz F, Ganz R, Siebenrock KA. Tilt and rotation correction of acetabular version on pelvic radiographs. Clin Orthop Relat Res. 2005;438:182–190. [DOI] [PubMed] [Google Scholar]
- 30.Yildiz C, Yildiz Y, Ozdemir MT, Green D, Aydin T. Sequential avulsion of the anterior inferior iliac spine in an adolescent long jumper. Br J Sports Med. 2005;39:e31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yuan BJ BR, Levy BA, Bond JR, Trousdale RT, Sierra RJ. Decreased range of motion is associated with structural hip deformity in asymptomatic adolescent athletes. Am J Sports Med. 2013;41:1519–1525. [DOI] [PubMed] [Google Scholar]



