Abstract
Objective:
The nonmedical use of stimulants (misuse) in the college setting remains of utmost public health and clinical concern. The objective of this study was to evaluate comprehensively the characteristics of college students who misused stimulants attending to rates of attention-deficit/hyperactivity disorder (ADHD), other psychopathology and substance use disorders (SUD).
Methods:
The data presented are from a cross-sectional study in college students who misused prescription stimulant medications (not including cocaine, methamphetamine) and controls (college students without stimulant misuse). College students were assessed blindly for psychopathology and SUD by way of structured psychiatric interview (SCID) and completion of self-report questionnaires.
Results:
The analysis included 200 controls (age 20.6 ± 2.6 years) and 100 stimulant misusers (age 20.7 ± 1.7 years). Misusers, when compared to controls, were more likely to endorse alcohol, drug, alcohol+drug, and any substance use disorder (all p values <0.01). Thirty-nine percent of stimulant misusers had a full or subthreshold use disorder of prescription stimulants. Misusers also had higher rates of conduct disorder (10% vs. 3%; p=0.02) and ADHD (including subthreshold cases; 27% vs. 16%; p=0.02) in addition to lower global assessment of functioning (GAF); (p< 0.05). Higher rates of misuse of immediate–relative to extended–release stimulants were reported.
Conclusion:
Our data suggest that compared to controls, college students who misuse stimulant medications are more likely to have ADHD, conduct disorder, stimulant and other SUD, and overall dysfunction.
Keywords: Stimulants, nonmedical use, misuse, substance use disorders
INTRODUCTION
Attention-deficit/hyperactivity disorder (ADHD) is estimated to affect up to 8% of college students in the United States.1 Stimulant medications are among the first-line agents for the treatment of ADHD in adolescents and young adults.2–4 Although stimulants are highly efficacious and have a well-documented safety profile2, the nonmedical use of stimulant medications (e.g. the use of stimulants without a prescription)5, particularly among college students, appears to be gaining weight as an important part of the drug use problem.
Several college-based studies have documented the prevalence of nonmedical use of stimulants.6–12 For example, Teter et al.9 surveyed a random sample of 4580 college students and found that the lifetime and past-year prevalence rates for illicit use of prescription stimulants were 8.3% and 5.9%, respectively. The College Alcohol Study (CAS) reported by McCabe et al.6 estimated that up to 25% of a nationally representative sample of US colleges endorsed nonmedical use of prescription stimulants in the past year. More recent data suggest that over a four-year period, almost two-thirds of college students were offered prescription stimulants for nonmedical use, and 31% had used stimulants for nonmedical purposes.11 Together, these studies show that rates of nonmedical use of prescription stimulants are a growing public health concern.
Studies have begun to shed light on the characteristics and context of stimulant misuse. Characteristics associated with stimulant misuse include Caucasian race, and reporting fraternity or sorority affiliation.6–9, 13 High rates of substance use disorders (SUD) have also been reported in association with stimulant misuse.12–14 Studies are inconsistent on findings between sexes including both rates and context of misuse.7, 8, 15–17.
Possible reasons for the high rates of stimulant misuse in college students are beginning to emerge.8, 18–22. In a survey conducted by Upadhyaya et al.,20 students with higher baseline ADHD symptoms were at elevated risk for misuse of stimulants. Teter and colleagues8 reported that 58% of college students reported misusing stimulants to concentrate, 43% to “get high”, 43% for alertness, and the remaining 14% for other motivation. Another survey found that students reported using stimulants to help study (57%), improve focus (20%), experiment (8%), get high (6%), and “self-medicate” (4%). 22 Also noteworthy is the growing assertion that the type of stimulant preparation may preclude more misuse. For instance, studies have suggested the higher abuse liability and likelihood of misuse with immediate−relative to extended−release stimulants 14, 23, 24.
Despite the clear evidence of stimulant misuse in college students, a dearth of information remains as to the reasons and context for use. For instance, to our knowledge, there is a scarcity of studies that have specifically evaluated ADHD and other psychopathological diagnoses using structured psychiatric interviews in college students misusing stimulants. To this end, we sought to examine the gaps in the literature by studying a heterogeneous sample of college students attending to ADHD, psychiatric and substance use disorders, types of stimulants misused, and context of misuse. Based on the literature12, 13, we hypothesized that stimulant misusers, compared to college students with no misuse of stimulants (controls), would have higher rates of ADHD symptoms or a full diagnosis of ADHD. We also hypothesized that rates of substance use disorders (SUD) would be higher in stimulant misusers than controls. Secondarily, we speculated that stimulant misusers would have higher rates of other psychopathology than controls, and that there would be a preponderance of misuse of immediate–relative to extended–release stimulants.
METHODS
Subjects
We ascertained 100 subjects who were not receiving prescription stimulants therapeutically (i.e., in relation to a diagnosis of ADHD) but endorsed stimulant misuse (misusers), and 200 subjects who used stimulants in the manner for which they were prescribed or had never misused (controls). Subjects from both groups were college students in the Boston metropolitan area recruited by way of Internet advertisements (e.g., craigslist.com, myspace.com, etc). We recruited both males and females between the ages of 18 and 28 who were currently enrolled in a local, undergraduate program. All subjects completed an informed consent to participate in the study. We obtained a federal release of confidentiality, and all aspects of the study were approved by the institutional review board.
We excluded those with any major sensorimotor handicaps that would impede the testing process such as paralysis, deafness, blindness, profound disorders of language such as autism, inadequate command of the English language, or an estimated Full Scale IQ less than 80. Subjects provided written informed consent to participate in the study. In order to have a more representative sample of both sexes, (40% of college students in the Boston area were male) we over recruited males.
A two-stage ascertainment procedure selected subjects. First, subjects answered a self-report Internet screen, which we designed using the online survey creation program DatStat Illume™. This is a platform for electronic data capture that streamlines data collection and management, and ensures data integrity. Second, following recruitment, subjects were asked to complete a brief Internet screening survey on “college lifestyle.” Embedded in the lifestyle survey was the 6-item WHO screen for ADHD, questions of stimulant misuse, and whether or not the potential subject had a diagnosis (by a doctor) and was currently being treated for ADHD with a stimulant. Potential subjects were able to respond by phone or email for further information before taking the survey. These screens were used to determine whether subjects were eligible for the stimulant misuse group or the control group. Eligible individuals were contacted to complete a direct interview and self-report questionnaires at Massachusetts General Hospital.
For the purpose of this research, stimulant misuse included those stimulants used for ADHD, namely amphetamine-AMPH (dextroamphetamine, lisdexamfetamine, immediate and extended release mixed amphetamine salts, and immediate and extended release methylphenidate-MPH) but did not include methamphetamine or other sympathomimetic amines (e.g. cocaine, MDMA).
Assessments
All diagnostic assessments were made using DSM-IV 25 -based structured interviews, by raters with bachelor’s or master’s degrees in psychology, with extensive training and supervision from the senior investigator. Raters and reviewers were blind to the ascertainment status of probands. Psychiatric assessments for subjects relied on the Structured Clinical Interview for DSM-IV (SCID). For every diagnosis, information was gathered regarding the ages at onset and offset of full syndromatic criteria, and treatment history. Global assessment of functioning (GAF) was rated lifetime and current for each study subject 25.
Self-report and clinician-rated measures were collected using DatStat Illume™. Subjects and/or research staff entered survey responses into electronic assessment forms, and the responses were then transmitted securely via encrypted connection and stored in a secure database.
All cases were presented to a committee composed of board certified child psychiatrists and/or licensed psychologists. Diagnoses presented for review were considered positive only if the diagnosis was considered clinically meaningful due to the nature of the symptoms, the associated impairment, and the coherence of the clinical picture. All cases of suspected drug or alcohol abuse or dependence were further reviewed with a child and adult psychiatrist with additional addiction credentials (moderate and/or severe SUD results are reported).
To assess the reliability of our diagnostic procedures, we previously computed kappa coefficients of agreement by having three experienced, board-certified child and adult psychiatrists diagnose subjects from audiotaped interviews made by the assessment staff. Based on 500 assessments from interviews of children and adults, the median kappa coefficient was 0.98. Kappa coefficients for individual diagnoses included: major depression (1.0), mania (0.95), ADHD (0.88), conduct disorder (CD; 1.0), oppositional defiant disorder (ODD; 0.90), antisocial personality disorder (ASPD; 0.80), and substance use disorder (1.0).
ADHD
We assessed ADHD using the SCID supplemented by childhood modules of ADHD from the Kiddie-schedule for affective disorders and schizophrenia (KSAD-S) 26 and included full and subthreshold cases in our results. We used the Adult ADHD Clinical Diagnostic Scale (ACDS) to additionally assess ADHD symptoms.27
Daily Functioning/Interaction with Peers
We used the self-reported, 16-item Quality of Life Enjoyment and Satisfaction Questionnaire (Q-LES-Q) to evaluate the degree of enjoyment and satisfaction experienced in eight areas of daily functioning. Socioeconomic status of each subject was determined by applying the Hollingshead-Redlich codes to the subject’s family of origin.
Drug Use
We evaluated the misuse of prescribed medications through the assessment of substance use, misuse, abuse, and dependence by structured interview, by self-report on the Drug Use Screening Inventory (DUSI)28, and by query for the appropriate use of prescribed medications on the MGH ADHD Medication Misuse and Diversion Assessment, a self-report tool which encompasses misuse or abuse of medication, euphoria on medication, and concurrent use of drugs or alcohol.29
Statistical Analysis
We used the Student’s t-test for continuous outcomes, the Wilcoxon rank-sum tests for SES, and Pearson’s χ2 for binary outcomes. Fisher’s exact test was used in the event of small numbers. We used Cox Proportional Hazard models and survival curves to examine the differences between substance use among controls and misusers. For the rating scales, we used logistic regression for the DUSI and the ACDS and ordered logistic regression for the Q-LES-Q. To determine whether sex affected the relationship between misusers and the endorsement of psychiatric disorders and SUD, we included the interaction term, misuse status-by-sex, in all models. If the interaction was not significant, we removed it from the analyses and collapsed the results, if it was significant we reported the results by sex. All statistical analyses were conducted using Stata 12.0. All tests were two-tailed with an alpha level set at 0.05 unless noted otherwise. Data are presented as mean ± standard deviation (SD) unless otherwise specified.
RESULTS
Clinical characteristics of the sample.
Our final sample included 100 misusers and 200 controls (N=300). There were no significant differences between misusers and controls in age, socioeconomic status (SES), or gender (see Table 1). We did find however, that misusers were more likely to be Caucasian than controls (p=0.004). As a result, we adjusted for race across all analyses.
Table 1.
Demographics of Sample (N=300)
| Controls (N=200) | Misusers (N=100) | Test Statistic | p-value | |
|---|---|---|---|---|
| Mean ± SD | Mean ± SD | |||
| Age | 20.64 ± 2.6 | 20.65 ± 1.7 | t=−0.05 | 0.96 |
| Socioeconomic status* | 1.9 ± 0.9 | 2.0 ± 1.0 | z=−0.58 | 0.57 |
| N (%) | N (%) | |||
| Gender (%male) | 82 (41) | 47 (47) | χ 2 ==0.98 | 0.32 |
| Race (% Caucasian) | 137 (69) | 84 (84) | χ 2 ==8.26 | 0.004 |
19 subjects were missing socioeconomic status data
Psychopathology.
As seen in Table 2, misusers compared to controls, were more likely to endorse ADHD (27 (27%) vs. 31 (16%); p=0.02) and conduct disorder (10 (10%) vs. 6 (3%); p=0.02) when adjusting for race and sex. The status-by sex interaction term was found to be significant for misuse status and multiple anxiety disorders (p=0.03); male misusers were more likely to endorse multiple anxiety disorders than male controls (Odds Ratio (OR): 16.8; 95% Confidence Interval (CI): 1.7, 170.4; p=0.02). There was no significant difference between female misusers and controls in the endorsement of multiple anxiety disorders (OR: 0.62, 95% CI: 0.19, 2.0; p=0.42). There were no significant differences between misusers and controls in the endorsement of any other disorder.
Table 2.
Lifetime Rates of Psychopathology in College Students who Misuse Stimulants and Controls
| Controls (N=200) N (%) | Misusers (N=100) N (%) | Statistics | |
|---|---|---|---|
| Major Depression | 49 (25) | 32 (32) | Odds Ratio (OR): 1.5; 95% Confidence Interval (CI): 0.9, 2.5; p=0.15 |
| Bipolar Disorder | 4 (2) | 1 (1) | OR: 0.5; 95% CI: 0.05, 4.6; p=0.54 |
| Attention Deficit Hyperactivity Disorder (ADHD) | 31 (16) | 27 (27) | OR: 2; 95% CI: 1.11, 3.71; p=0.02 |
| Psychosis | 5 (3) | 4 (4) | OR: 1.5; 95% CI: 0.4, 6.0; p=0.53 |
| Conduct Disorder | 6 (3) | 10 (10) | OR: 3.8; 95% CI: 1.3, 11.3; p=0.02 |
| Anxiety Disorders | |||
| Separation Anxiety Disorder | 6 (3) | 3 (3) | OR: 0.9; 95% CI: 0.2, 3.8; p=0.90 |
| Post Traumatic Stress Disorder | 1 (0.5) | 0 (0) | Fisher’s exact test, p=0.10 |
| Agoraphobia | 7 (4) | 6 (6) | OR: 2.0; 95% CI: 0.6, 6.5; p=0.22 |
| Simple Phobia | 22 (11) | 7 (7) | OR: 0.6; 95% CI: 0.2, 1.5; p=0.27 |
| Social Phobia | 27 (14) | 10 (10) | OR: 0.7, 95% CI: 0.3, 1.6; p=0.42 |
| Panic Disorder | 6 (7) | 7 (7) | OR: 2.1; 95% CI: 0.7, 6.7; p=0.19 |
| Generalized Anxiety Disorder | 5 (3) | 3 (3) | OR: 1.0; 95% CI: 0.2, 4.5; p=0.97 |
We also found a significant effect of sex on misuse status and lifetime global assessment of functioning (GAF, p=0.045). Male misusers were more likely than male controls to have more impairment on the GAF (beta: −7.7; 95% CI: −10.8, −4.6; p<0.001). Female misusers were also more likely than female controls to have more impairment on the GAF (beta: −3.2; 95% CI: −6.0, −0.37; p=0.03).
We examined specific ratings on the ACDS. After adjusting for race and sex, misusers were more likely than controls to report moderate to severe difficulty sustaining attention (p=0.01) and being easily distracted during childhood (p=0.04). Similarly, misusers were more likely to report moderate to severe difficulty following instructions (p=0.03) and dislike for tasks that require attention during adulthood (p=0.02). Misusers were more likely to report an onset of ADHD prior to age 7 (p=0.048), the presence of significant and sufficient current ADHD symptoms (p=0.03), and report the symptoms as primarily due to ADHD and not another mental health disorder (p=0.03).
SUD.
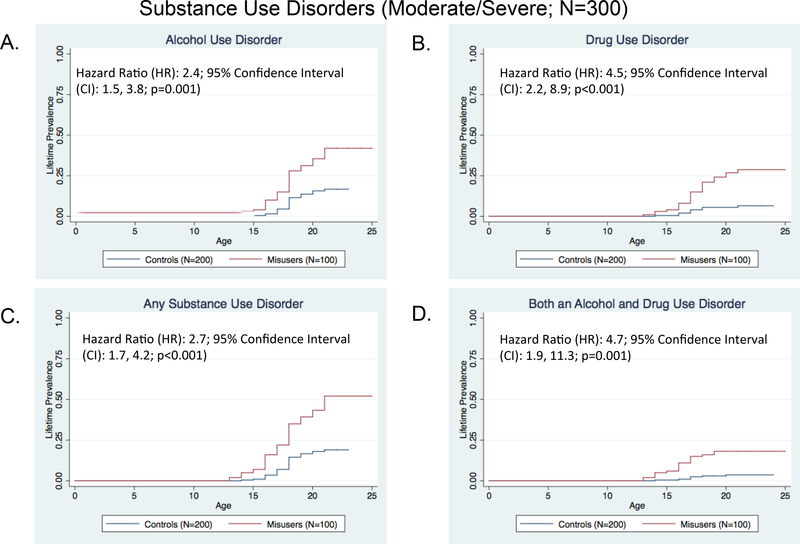
We found that stimulant misusers were more likely than controls to report having an alcohol, drug, alcohol+drug, or overall SUD (all p values <0.001, see Figure 1, parts a-c). Stimulant misusers were 2.7 times more likely to manifest a SUD compared to controls. Additionally, stimulant misusers were 4.7 times more likely than controls to report having a combined alcohol plus drug use disorder (p=0.001). We further examined our misuse group and found that 5% (N=5) met for a full (non-cocaine or methamphetamine) stimulant use disorder and 34% (N=34) met for a subthreshold diagnosis of a stimulant use disorder (e.g. abuse or dependence of prescription stimulants).
Figure 1.
(A--‐D) denotes rates of alcohol, drug, alcohol+drug, and overall substance use disorders in college students who misuse stimulants (N=100) and controls (N=200). There were significant differences between misusers and controls in all substance use disorder categories assessed, including alcohol (A), drug (B), overall SUD (C), and alcohol+drug use disorder.
Stimulant preparation misused.
According to self-report on the MGH ADHD Medication Misuse and Diversion Assessment, stimulant misusers were more likely to use, purchase and/or trade immediate release (76%) compared to extended release (58%; not mutually exclusive) ADHD medication. Among those who met for a full or subthreshold diagnosis of a stimulant misuse disorder (N=39), we found 51% (N=20) were using mixed amphetamine salts–immediate release, 31% (N=12) could not recall the specific stimulant, 10% (N=4) reported immediate release methylphenidate, and 8% (N=3) used immediate release d−amphetamine. No subject with a stimulant use disorder endorsed misusing/abusing an extended-release stimulant.
Drug Use Screening Inventory (DUSI).
We had fully completed DUSI reports on 235 subjects. While adjusting for race and sex, misusers compared to controls, endorsed significantly higher rates of initiating use of their preferred drug to “get high” (73% vs. 40%, OR: 3.9; 95% CI: 2.2, 7.0; p<0.01) or to “sleep better” (19% vs. 7%, OR: 3.3; 95% CI: 1.4, 7.7; p<0.01). Misusers also reported continued use of their preferred drug to “get high” (73% vs. 38%, OR: 3.7; 95% CI: 2.0, 6.7; p<0.001) or to “sleep better” (23% vs. 13%, OR: 2.1; 95% CI: 1.02, 4.4; p=0.04). When adjusting for race and sex on the Quality of Life Enjoyment and Satisfaction Questionnaire (Q-LES-Q), misusers were more likely than controls to report a lower “overall sense of well being” (beta: −0.5; 95% CI: −0.9, −0.001; p=0.049).
DISCUSSION
The results of this study partially support our hypotheses that stimulant misusers, compared to controls, are at higher risk for ADHD and/or multiple drug and alcohol use disorders. In this study, stimulant misusers were also more likely to have a poorer quality of life relative to controls. These data add to the existing literature highlighting the elevated risk for ADHD and multiple SUDs in those with stimulant misuse. Accordingly, college students who misuse stimulants should be carefully screened for ADHD and SUD.
Our results are remarkably consistent with those of survey studies. For instance, the almost two-fold higher risk for ADHD among stimulant misusers is consistent with Upadhyaha et al.30 who showed increased risk for ADHD symptoms in college-aged stimulant misusers. Similarly, Rabiner et al.31 found that students who did not endorse frequent substance use, but endorsed severe attention problems, were five-times more likely to have an onset of nonmedical use of stimulants between freshman and sophomore year of college compared to those that did not endorse attention problems. Given that stimulants are used to treat ADHD and executive functioning deficits, and that “self medication” of executive dysfunctioning has been purported in stimulant misusers,32, 33 further analyses examining clinical and objective evidence of neuropsychological and executive functioning deficits in this population are necessary.
We found that nearly one-half of stimulant misusers manifest a SUD. Most commonly reported were alcohol, marijuana and then “prescription” stimulants. Moreover, a disproportionate rate of combined drug plus alcohol use disorders were found in stimulant misusers compared to controls. The high rates of SUD are consistent with other studies5, 12, 13, 34, 35. For instance, in a series of well conducted longitudinal analyses, Arria et al.35 also showed that the onset of SUD appears to precede stimulant misuse. The speculation can be made that SUD resulted in academic decline, which prompted ancillary stimulant misuse to improve academic performance.
It may be that stimulant misusers with SUD have a more pernicious use disorder; for instance, our data predominately show that stimulant misusers endorsed the use of alcohol and drugs for euphoria. In contrast, subjects in other samples of similarly aged individuals predominately endorsed continued drug and alcohol use for attenuation of mood, sleep, or other reasons, but not for euphoria as in the current study.36 These DUSI derived self-report data, coupled with the finding of a substantially higher risk for combined drug plus alcohol use disorders in stimulant misusers, suggest that stimulant misusers may manifest not only a higher risk, but a more severe form of SUD, relative to controls.
In previous studies of college students who use stimulants non-medically, the rates of actual stimulant use disorders remain largely uncharted. In the current study our data show that among stimulant misusers, a sizeable minority (39%) endorsed either a full or subthreshold stimulant use disorder−indicating that the nonmedical use of stimulants is not necessarily a single episode, and may be associated with a separate SUD that necessitates identification, referral, and treatment. Clearly, given the high rates of SUD in our groups, college students who misuse stimulants should be systematically screened for alcohol, stimulant, and other substance-related SUDs.
There has been speculation about the differential abuse liabilities of immediate- and extended release stimulants.37 In our entire group of misusers, over three-quarters reported misusing the immediate release preparations. Moreover, among those with a stimulant use disorder, the vast majority reported misusing the immediate-release stimulant preparations, while one-quarter were unaware of the specific preparation, and no individual specifically endorsed using extended-release preparations. Our current data add to the human abuse liability stimulant literature23, 38 highlighting that immediate release stimulants appear to be misused at higher rates than extended release preparations in groups of college students. Accordingly, our study further supports the notion of utilizing extended–and not immediate–release stimulants in high risk groups such as college-aged individuals.37
The current study has a number of methodological limitations. Our students were derived from the metropolitan Boston area and may not generalize to other regions. While the overall sample size was modest (N=300), the cell sizes in specific groups were relatively small, thus limiting our Power. We utilized structured interviews for SUD instead of biological testing which may have underestimated the actual prevalence. Since we relied on self-report for some of our measures, our subjects may not have completed their questionnaires fully, and/or may have underreported their pathology. While we attempted to utilize descriptions, pictures, and brand/generic names of the various stimulants, our data were limited to our subjects’ recollection of the preparations they had misused. Our data are cross sectional, and as such, are associative in nature.
Despite these methodological shortcomings, the aggregate of high rates of ADHD, SUD including stimulant use disorders, and a lower quality of life indicate that college students who misuse prescription stimulants are clearly struggling. Our data suggest a preponderance of misuse of immediate–relative to extended–release stimulants. Added to previous calls for college health professionals to screen for stimulant misuse8, 12, 39, the current data, in conjunction with recent literature, emphasize the need to further screen those with nonmedical use of stimulants for ADHD, stimulant and other SUD, and overall dysfunction.
Funding Source:
This work was supported by a NIH K24 DA016264 grant to Dr. Timothy Wilens. The funding sources had no role in the design and conduct of the study; collection, management, analysis, or interpretation of the data; or preparation, review, or approval of the manuscript.
Previous Presentation: This study was accepted or presented at the American Society of Addiction Medicine on April 10–13, 2014 in Orlando Florida; the American Academy of Child and Adolescent Psychiatry, October 16–20th, 2014 in San Diego, California; and the American Academy of Addiction Psychiatry, December 4–7, 2014 in Orlando, Florida.
Financial Disclosures:
Timothy Wilens: Over the past three years Dr. Timothy Wilens receives/d research support from, or is/has been on the advisory board for the following: National Institute on Drug Abuse (NIDA), Euthymics, Shire, Theravance, and TRIS. Dr. Timothy Wilens is/or has been a consultant for: Bay Cove Human Services, Euthymics, Major and Minor League Baseball, the National Football League (ERM Associates) and TRIS. Dr. Timothy Wilens has a published book with Guilford Press. Straight Talk About Psychiatric Medications for Kids, co edited ADHD Across the Lifespan, and the MGH Comprehensive Textbook of Psychiatry.
Amy Yule: Dr. Amy Yule received grant support from the American Academy of Child and Adolescent Psychiatry Pilot Research Award for Junior Faculty supported by Lilly USA, LLC.
Footnotes
Courtney Zulauf, MaryKate Martelon, Nicholas Morrison and Rayce Anselmo: The authors have no conflict of interest relevant to this article to disclose.
References
- 1.Weyandt LL, DuPaul G. ADHD in college students. J Atten Disord 2006. August;10(1):9–19. [DOI] [PubMed] [Google Scholar]
- 2.Greenhill LL, Pliszka S, Dulcan MK, et al. Practice parameter for the use of stimulant medications in the treatment of children, adolescents, and adults. Journal of the American Academy of Child and Adolescent Psychiatry 2002. February;41(2 Suppl):26S–49S. [DOI] [PubMed] [Google Scholar]
- 3.Wilens TE, Spencer TJ. Understanding attention-deficit/hyperactivity disorder from childhood to adulthood. Postgrad Med 2010. September;122(5):97–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stevens JR, Wilens TE, Stern TA Using Stimulants for Attention-Deficit/Hyperactivity Disorder: Clinical Approaches and Challenges. Prim Care Companion for CNS Disord 2013;15(2):1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McCabe SE, West BT. Medical and nonmedical use of prescription stimulants: results from a national multicohort study. J Am Acad Child Adolesc Psychiatry 2013. December;52(12):1272–1280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McCabe SE, Knight JR, Teter CJ, Wechsler H. Non-medical use of prescription stimulants among US college students: prevalence and correlates from a national survey. Addiction 2005. January;99(1):96–106. [DOI] [PubMed] [Google Scholar]
- 7.McCabe SE, Teter CJ, Boyd CJ. Medical use, illicit use, and diversion of abusable prescription drugs. Journal of American college health : J of ACH 2006. Mar-Apr;54(5):269–278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Teter CJ, McCabe SE, Cranford JA, Boyd CJ, Guthrie SK. Prevalence and motives for illicit use of prescription stimulants in an undergraduate student sample. Journal of American college health : J of ACH 2005. May-Jun;53(6):253–262. [DOI] [PubMed] [Google Scholar]
- 9.Teter CJ, McCabe SE, LaGrange K, Cranford JA, Boyd CJ. Illicit use of specific prescription stimulants among college students: prevalence, motives, and routes of administration. Pharmacotherapy 2006. October;26(10):1501–1510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Teter CJ, Falone AE, Cranford JA, Boyd CJ, McCabe SE. Nonmedical use of prescription stimulants and depressed mood among college students: frequency and routes of administration. Journal of substance abuse treatment 2010;38(3):292–298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Garnier-Dykstra LM, Caldeira KM, Vincent KB, O’Grady KE, Arria AM. Nonmedical use of prescription stimulants during college: Four-year trends in exposure opportunity, use, motives, and sources. Journal of American college health 2012;60(3):226–234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Arria AM, Caldeira K, O’Grady KE, Vincent K, Johnson E, Wish ED. Nonmedical use of prescription stimulants among College Students: Associations with ADHD and Polydrug use. Pharmacotherapy 2008 February 2008;28(2):156–169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wilens TE, Adler LA, Adamson J, et al. Misuse and diversion of stimulants prescribed for ADHD: a systematic review of the literature. J Am Acad Child Adolesc Psychiatry 2008. January;47(1):21–31. [DOI] [PubMed] [Google Scholar]
- 14.Wilens T, Gignac M, Swezey A, Monuteaux M, Biederman J. Characteristics of Adolescents and Young Adults with ADHD Who Divert or Misuse their Prescribed Medications. J Am Acad Child Adolesc Psychiatry 2006;45(4):408–414. [DOI] [PubMed] [Google Scholar]
- 15.Poulin C Medical and nonmedical stimulant use among adolescents: from sanctioned to unsanctioned use. CMAJ : Canadian Medical Association journal = journal de l’Association medicale canadienne 2001;165(8):1039–1044. [PMC free article] [PubMed] [Google Scholar]
- 16.Wu LT, Schlenger WE. Psychostimulant dependence in a community sample. Subst Use Misuse 2003;38(2):221–248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hall KM, Irwin MM, Bowman KA, Frankenberger W, Jewett DC. Illicit use of prescribed stimulant medication among college students. Journal of American college health : J of ACH 2005. Jan-Feb;53(4):167–174. [DOI] [PubMed] [Google Scholar]
- 18.Barrett SP, Darredeau C, Bordy LE, Pihl RO. Characteristics of methylphenidate misuse in a university student sample. Can J Psychiatry 2005. July;50(8):457–461. [DOI] [PubMed] [Google Scholar]
- 19.Kollins SH, MacDonald EK, Cush CR. Assessing the abuse potential of methylphenidate in nonhuman and human subjects: A review. Pharmacology Biochemistry and Behavior 2001;68:611–627. [DOI] [PubMed] [Google Scholar]
- 20.Upadhyaya HP, Rose K, Wang W, et al. Attention deficit hyperactivity disorder, medication treatment, and substance use patterns among adolescents and young adults. J Child Adolesc Psychopharmacol 2005;15(5):799–809. [DOI] [PubMed] [Google Scholar]
- 21.White BP, Becker-Blease KA, Grace-Bishop K. Stimulant medication use, misuse, and abuse in an undergraduate and graduate student sample. Journal of American college health : J of ACH 2006. Mar-Apr;54(5):261–268. [DOI] [PubMed] [Google Scholar]
- 22.Stone AM, Merlo LJ. Attitudes of college students toward mental illness stigma and the misuse of psychiatric medications. J Clin Psychiatry 2011. February;72(2):134–139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Parasrampuria DA, Schoedel KA, Schuller R, et al. Do formulation differences alter abuse liability of methylphenidate? A placebo-controlled, randomized, double-blind, crossover study in recreational drug users. Journal of Clinical Psychopharmacology 2007. October;27(5):459–467. [DOI] [PubMed] [Google Scholar]
- 24.Spencer TJ, Biederman J, Ciccone PE, et al. PET study examining pharmacokinetics, detection and likeability, and dopamine transporter receptor occupancy of short- and long-acting oral methylphenidate. Am J Psychiatry 2006. March;163(3):387–395. [DOI] [PubMed] [Google Scholar]
- 25.APA. Diagnostic and Statistical Manual of Mental Disorders IV. 4th ed. Washington, D.C.: American Psychiatric Association Press; 1994. [Google Scholar]
- 26.Ambrosini PJ. Historical development and present status of the schedule for affective disorders and schizophrenia for school-age children (K-SADS). J Am Acad Child Adolesc Psychiatry 2000;39(1):49–58. [DOI] [PubMed] [Google Scholar]
- 27.Kessler RC, Green JG, Adler LA, et al. Structure and diagnosis of adult attention-deficit/hyperactivity disorder: analysis of expanded symptom criteria from the Adult ADHD Clinical Diagnostic Scale. Arch Gen Psychiatry 2010. November;67(11):1168–1178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tarter RE, Kirisci L. The Drug Use Screening Inventory for adults: psychometric structure and discriminative sensitivity. Am J Drug Alcohol Abuse 1997. May;23(2):207–219. [DOI] [PubMed] [Google Scholar]
- 29.Winhusen TM, Lewis DF, Riggs PD, et al. Subjective effects, misuse, and adverse effects of osmotic-release methylphenidate treatment in adolescent substance abusers with attention-deficit/hyperactivity disorder. J Child Adolesc Psychopharmacol 2011. October;21(5):455–463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Upadhyaya HP, Kroutil LA, Deas D, Durell TM, Van Brunt DL, Novak SP. Stimulant formulation and motivation for nonmedical use of prescription attention-deficit/hyperactivity disorder medications in a college-aged population. Am J Addict 2010. November;19(6):569–577. [DOI] [PubMed] [Google Scholar]
- 31.Rabiner DL, Anastopoulos AD, Costello EJ, Hoyle RH, Swartzwelder HS. Predictors of nonmedical ADHD medication use by college students. J Atten Disord 2010. May;13(6):640–648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Boyd CJ, McCabe SE, Cranford JA, Young A. Adolescents’ motivations to abuse prescription medications. Pediatrics 2006. December;118(6):2472–2480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rabiner DL, Anastopoulos AD, Costello EJ, Hoyle RH, McCabe SE, Swartzwelder HS. Motives and perceived consequences of nonmedical ADHD medication use by college students: are students treating themselves for attention problems? J Atten Disord 2009. November;13(3):259–270. [DOI] [PubMed] [Google Scholar]
- 34.McCabe SE, West BT, Teter CJ, Ross-Durow P, Young A, Boyd CJ. Characteristics associated with the diversion of controlled medications among adolescents. Drug Alcohol Depend 2011. November 1;118(2–3):452–458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Arria AM, Caldeira KM, O’Grady KE, et al. Drug exposure opportunities and use patterns among college students: results of a longitudinal prospective cohort study. Subst Abus 2008;29(4):19–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wilens TE, Gignac M, Swezey A, Monuteaux MC, Biederman J. Characteristics of adolescents and young adults with ADHD who divert or misuse their prescribed medications. J Am Acad Child Adolesc Psychiatry 2006. April;45(4):408–414. [DOI] [PubMed] [Google Scholar]
- 37.Wilens TE, Morrison NR. The intersection of attention-deficit/hyperactivity disorder and substance abuse. Curr Opin Psychiatry 2011. April 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Spencer T, Abikoff H, Connor DF, et al. Efficacy and safety of mixed amphetamine salts extended release (adderall XR) in the management of oppositional defiant disorder with or without comorbid attention-deficit/hyperactivity disorder in school-aged children and adolescents: A 4-week, multicenter, randomized, double-blind, parallel-group, placebo-controlled, forced-dose-escalation study. Clinical Therapeutics 2006;28(3):402–418. [DOI] [PubMed] [Google Scholar]
- 39.Arria AM, DuPont RL. Nonmedical prescription stimulant use among college students: why we need to do something and what we need to do. J Addict Dis 2010. October;29(4):417–426. [DOI] [PMC free article] [PubMed] [Google Scholar]