Abstract
Public transportation provides an opportunity to incorporate physical activity into journeys, but potential health impacts have not been systematically examined. We searched the literature for articles on public transportation and health published through December 2017 using Google (Google Inc., Mountain View, California), 5 medical databases, and 1 transportation-related database. We identified longitudinal studies which examined associations between public transportation and cardiometabolic health (including adiposity, type 2 diabetes mellitus, and cardiovascular disease). We assessed study quality using the Newcastle-Ottawa Scale for cohort studies and performed meta-analyses where possible. Ten studies were identified, 7 investigating use of public transportation and 3 examining proximity to public transportation. Seven studies used individual-level data on changes in body mass index (BMI; weight (kg)/height (m)2), with objective outcomes being measured in 6 studies. Study follow-up ranged from 1 year to 10 years, and 3 studies adjusted for nontransportation physical activity. We found a consistent association between use of public transportation and lower BMI. Meta-analysis of data from 5 comparable studies found that switching from automobile use to public transportation was associated with lower BMI (−0.30 units, 95% confidence interval: −0.47, −0.14). Few studies have investigated associations between public transportation use and nonadiposity outcomes. These findings suggest that sustainable urban design which promotes public transportation use may produce modest reductions in population BMI.
Keywords: active travel, adiposity, cardiometabolic health, physical activity, systematic reviews, transportation
Governments and city mayors worldwide increasingly recognize the importance of investing in local public transportation systems. For example, bus rapid transit systems have been introduced in cities in the United States, Europe, and Latin America, and many countries have recently made major investments in rail networks (1). Such actions directly deliver progress towards United Nations Sustainable Development Goal 11, which aims to “create safe, inclusive, resilient and sustainable cities, including through affordable, accessible and expanded public transportation systems” (2). Furthermore, investment in public transportation systems may also reduce carbon emissions, improve air quality, and increase economic activity through reduced congestion and improved connectivity, thus contributing to the achievement of several other Sustainable Development Goals (2–4).
Public transportation systems may substantially influence physical activity at the population level, as users commonly walk or cycle to transportation stops and interchanges. In a 2012 review, Rissel et al. (5) found that use of public transportation was associated with 8–33 minutes of physical activity per day, with one study finding that 29% of commuters achieved 30 minutes of daily physical activity as part of public transportation use (6). More recent studies using objective measures of physical activity found that public transportation use was associated with 10.2 minutes of moderate-to-vigorous physical activity per trip (7, 8). These findings are important given that public transportation use is typically more prevalent than walking or cycling for transportation; for example, in England and Wales, public transportation accounts for 16% of commutes, as compared with 11% for walking and 3% for cycling (9, 10). Encouraging public transportation use may be an especially effective approach to increasing physical activity among the least active members of society (11) and may be equity-enhancing, since minority ethnic and low-income groups with poorer cardiometabolic health profiles are, on average, more frequent users of public transportation (12, 13).
Most existing evidence is focused on the cardiometabolic benefits of walking and cycling for transportation (14, 15). This evidence shows that people who walk or cycle for transportation have lower adiposity, cardiovascular disease (CVD) risk, and CVD mortality (15–20). To our knowledge, the relationship between public transportation use and cardiometabolic outcomes has not previously been systematically assessed. We thus conducted a systematic review of studies examining associations between public transportation (including trains, buses, and subway systems) and cardiometabolic health outcomes.
METHODS
The protocol for this review was registered with the International Prospective Register of Systematic Reviews (identification number CRD42016048427).
Information sources
Studies were identified using published and gray literature databases, Internet searches (Google; Google Inc., Mountain View, California), and reference lists of included studies. The electronic databases searched were MEDLINE (National Library of Medicine, Bethesda, Maryland), Embase (Elsevier BV, Amsterdam, the Netherlands), the Transport Database (Organisation for Economic Cooperation and Development, Paris, France, and Transportation Research Board, Washington, DC), Scopus (Elsevier BV), the Cochrane Library (The Cochrane Collaboration, London, United Kingdom), and opengrey.eu (Institut de l’Information Scientifique et Technique, Vandoeuvre-lès-Nancy, France). No restrictions were placed on the dates of publication. Database searches took place in December 2017. The search strategy used in MEDLINE is given in Web Appendix 1 (available at https://academic.oup.com/aje), with adapted searches being used in the other databases and simplified searches used in opengrey.eu and Google. In general, keywords for identifying articles related to public transportation included “public transportation,” “bus,” “train,” “transit,” “subway,” and “commute,” and keywords for identifying cardiometabolic articles were “cardiovascular,” “diabetes,” “hypertension,” “mortality,” “obesity,” “adiposity,” “body fat,” and “body mass index.”
Initial study eligibility was assessed by reviewing titles and abstracts and was carried out independently by 2 of the authors (R.P./A.A.L.). These 2 authors then independently carried out full text screening, with any disagreement being resolved through discussion.
Inclusion criteria
In order to maximize the number of studies returned, all randomized controlled trials, quasiexperimental studies, and longitudinal observational studies were eligible for inclusion. We did not include cross-sectional studies, however, in order to increase causal inference and reduce potential bias from unobserved confounding (21). We included studies that assessed public transportation exposure, including public transportation use, change in public transportation use, or access to public transportation (e.g., proximity of bus stops). Eligible comparator groups included users of other modes of travel, such as automobile drivers, and persons at greater distance from bus stops. Studies without comparators were excluded. Eligible cardiometabolic outcomes included CVD mortality, diagnosis of CVD, type 2 diabetes mellitus, dysglycemia (e.g., elevated blood glucose level, insulin resistance, glucose intolerance), dyslipidemia (e.g., elevated triglyceride or low density lipoprotein level, depressed high density lipoprotein level, hypertension/blood pressure), and measures of adiposity (e.g., body mass index (BMI; calculated as weight (kg)/height (m)2), percentage of body fat, waist circumference, waist:hip ratio, and height:weight ratio). We included both self-reported and objectively measured outcomes. Any study population of adults and/or children aged ≥5 years was included. We only included studies published in English.
Data extraction
Data extracted included information on the characteristics of study participants (including age, location, and proportion male), year of publication, study size, length of follow-up, sample selection, cohort/study names, exposure, outcome, covariates, analysis type, and effect estimates. Data were extracted by one author (R.P.) and checked by a second (A.A.L.). Where multiple studies used the same data source, we included the analysis using the most recent data.
Quality assessment
Studies were assessed for risk of bias using criteria derived from the Newcastle-Ottawa Scale for cohort studies. The Newcastle-Ottawa Scale is recommended by the Cochrane Collaboration for use with nonrandomized studies and was applicable to the study designs found (22, 23). Because of concerns about the validity of calculating overall risk-of-bias scores for heterogeneous studies, including concerns that the tool itself might introduce bias, we chose not to calculate an overall risk-of-bias score (24). Instead, we assessed the risk-of-bias domains separately to identify whether studies with greater risk of bias in a particular domain had systematically different conclusions than those with lower risk. Domains of the Newcastle-Ottawa Scale include the representativeness of the exposed group, ascertainment of exposure, the presence of adjustment for covariates (especially, in this case, adjustment for nontransportation physical activity), and assessment of the outcome (e.g., objective or self-reported).
Data analysis
We summarized associations between public transportation and each outcome studied. Where different types of exposure were available for the same outcome (e.g., public transportation use vs. proximity to public transportation), their findings were compared to evaluate consistency. Where there were sufficient studies presenting comparable exposure and outcome measures, a random-effects meta-analysis was carried out using the methods suggested by DerSimonian and Laird (25). This was possible for 5 studies that examined changes in mode of transportation and change in BMI. In order to allow comparison between studies, some harmonization was carried out as required; for example, in a study that measured distance to bus stops in miles, distance was converted to kilometers to allow comparison with other studies. I2 was calculated to assess heterogeneity in the data; this is interpreted as the proportion of total variation in estimates that is due to heterogeneity between the studies rather than due to chance (26). Funnel plots were used to assess reporting biases and heterogeneity in study findings attributable to study size (27).
RESULTS
Description of included studies
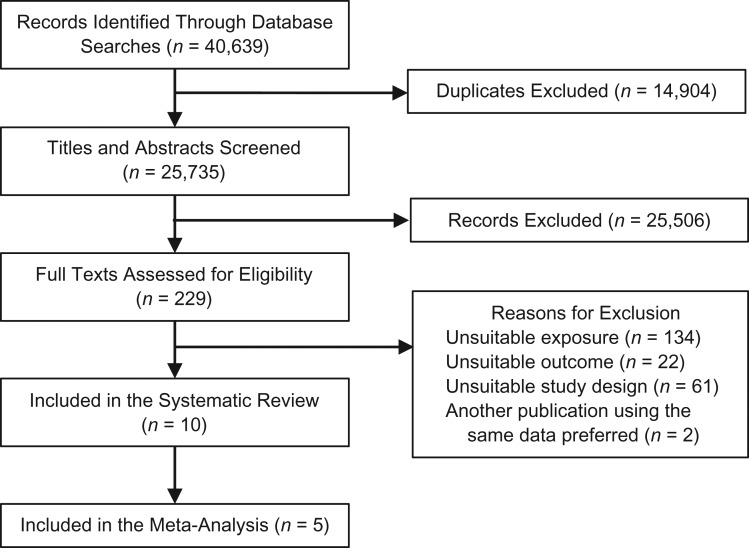
We identified 40,639 studies through literature searches, of which 14,904 were duplicates (Figure 1). Of the remaining articles, 229 studies were retained following title and abstract screening. After full text assessment, 10 studies were included in this review. Sixty-one studies were excluded because of an unsuitable study design, of which 29 were not longitudinal. We excluded 134 studies for unsuitable exposure (predominately not assessing public transportation use specifically) and 22 for ineligible outcomes (such as physical activity energy expenditure).
Figure 1.
Selection of studies for a systematic review of associations between public transportation use and cardiometabolic health outcomes, December 2017.
All included studies were of adults (range of mean ages at baseline, 41–62 years). Six were based in the United States (28–33), 3 were from the United Kingdom (34–36), and 1 was from China (37) (Table 1). No studies had been published before 2008, and 5 had been published since 2016 (28, 30, 33, 34, 37). Seven studies investigated the direct effects of public transportation use; that is, they compared users with nonusers (28–30, 32, 34–36). Public transportation use was assessed by means of survey questions about usual mode of commuting (30, 34, 35) or any use of public transportation (28, 29, 32, 36). The remaining 3 studies investigated proximity to public transportation, with 1 study examining the impact of a new light rail line (33) and the other 2 investigating the distance to the nearest bus stop or route (31, 37).
Table 1.
Characteristics of Studies Included in a Systematic Review of Associations Between Public Transportation Use and Cardiometabolic Health Outcomes, December 2017
| First Author, Year (Reference No.) | Study Name or Focus and Location | No. of Participants | Average Follow-up, years | Exposure | Outcome | Covariates Considered | Main Findings |
|---|---|---|---|---|---|---|---|
| Brown, 2008 (29) | Evaluation of TRAX light rail line, United States | 47 | 1 | Use of light rail | Proportion obese based on BMIa | Income and employment | 0.26 (95% CI: 0.01, 0.51) of those initiating public transportation use were obese as compared with 0.65 (95% CI: 0.41, 0.89) of non–public transportation users and 0.15 (95% CI: −0.05, 0.35) of continuing public transportation users. |
| Brown, 2017 (28) | Moving Across Places Study, United States | 536 | 1 | Use of public transportation | Change in BMI | Sex, age, education, time 1 accelerometer wear time, time 1 outcome values, changes in employment, temperature, self-reported health, participation interval, automotive time, and accelerometer wear time | BMI change was −0.56 units (95% CI: −0.97, −0.14) in persons initiating public transportation use, 0.66 units (95% CI: 0.21, 1.11) in those ceasing public transportation use, and 0.01 units (95% CI: −0.44, 0.42) in those continuing public transportation use. |
| Chen, 2017 (30) | Ecological study using government data, United States | —b | 10 | Proportion of the population commuting by public transportation | % of the population who were obese based on BMI | Per capita state income, state unemployment (% of labor force), % of state population that was white, log population density, % of state population with a bachelor’s degree or higher, % of state population that consumed fruit ≥2 times/day and vegetables ≥3 times/day, % of state population that engaged in daily physical exercise as recommended, per capita state health care expenditure (2010) | Higher levels of public transportation commuting were associated with lower prevalences of overweight (−0.32%, 95% CI: −0.05, −0.59) and obesity (−0.21%, 95% CI: −0.03, −0.39) 1 year later. A 1% increase in public transportation commuting was associated with a 0.21% reduction in obesity prevalence. |
| Flint, 2016 (34) | UK Biobank, United Kingdom | 5,861 | 4.4 | Commuting mode | Change in BMI | Baseline BMI, age, sex, ethnicity, baseline household income, household income change, educational attainment, self-rated general health transitions, manual occupation transitions, days/week of leisure moderate physical activity, change in days/week of leisure moderate physical activity, occupational physical activity, and change in occupational physical activity | Initiation of public transportation use was associated with a −0.30-unit (95% CI: −0.47, −0.13) change in BMI as compared with 0.32 units (95% CI: 0.13, 0.50) among persons ceasing public transportation use. |
| Hirsch, 2014 (31) | Multi-Ethnic Study of Atherosclerosis, United States | 5,506 | 9.1 | Distance from home to closest bus stop (objectively measured) | Change in BMI and waist circumference | Time-varying working status, current marital status, automobile ownership, cancer diagnosis, self-rated health compared with others, income, moving to a different house between waves, a measure of time, and interactions of time with selected covariates (baseline age and race/ethnicity), allowing time trends to vary by these characteristics. Model 2 also included potential mediators: time-varying transportation walking (minutes/week), time-varying smoking status, time-varying alcohol consumption status, and an interaction allowing time trends to vary by baseline calorie consumption. | A 1-km increase in distance to the closest bus stop was associated with no change in BMI (0.01 units, 95% CI: −0.01, 0.02) or waist circumference (0.02 cm, 95% CI: −0.03, 0.07). |
| MacDonald, 2010 (32) | Evaluation of a new light rail line, United States | 301 | ≥1 | Light rail use after completion of new rail line | Change in BMI | Sex, race, age, employed status (yes/no), distance (miles) to work, education, rent, social and physical environment, and planning to use light rail transit | Initiation of new light rail use was associated with a −1.18-unit (95% CI: −2.22, −1.13) change in BMI and reduced odds of becoming obese (odds ratio = 0.19, 95% CI: 0.04, 0.92). |
| Martin, 2015 (35) | British Household Panel Survey, United Kingdom | 4,056 | 2 | Commuting mode | Change in BMI | Age, sex, and BMI at t0, occupational status, working hours, household income, education, children, health status, automobile access at t0, home location, income, health, automobile access, and pregnancy | Initiation of public transportation use was associated with a change in BMI of −0.12 units (95% CI: −0.55, −0.30). Ceasing public transportation use was associated with a BMI change of 0.46 units (95% CI: 0.16, 0.86). |
| Park, 2017 (33) | Texas DSHS Center for Health Statistics data for 2002–2005, United States | —b | 2 | Distance from home to a new light rail line | % change in stroke mortality | Seasonal and long-term trends, day of the week (weekday vs. weekend), and weather effects | There were reductions in the daily total stroke mortality rate of 39.3% (95% CI: 6.8, 60.4) within 5 miles (8 km) of the light rail line and 33.3% (95% CI: 10.0, 50.6) within 10 miles (16 km) of the rail line but not in control areas (>10 miles (>16 km); −4.1%, 95% CI: −31.9, 35.1). |
| Sun, 2017 (37) | China Family Panel Study, China | 8,028 | 2 | Distance from home to the closest bus stop (self-reported) | Change in BMI | Facilities access (density of public service buildings), private motor transportation modec, age, age squared, male sex, married status, employed status, family income, family income squared, meat consumption, junk food consumption, eating out, sedentary time, exercise time, commuting time, sleep time, and eating time | A 1-km increase in distance to the closest bus stop was associated with a −0.10-unit change in BMI (95% CI: −0.20, −0.01). |
| Webb, 2012 (36) | English Longitudinal Study of Aging, United Kingdom | 4,686 | 4 | Use of public transportation | Change in BMI; odds of being obese, using BMI and waist circumference | Age, age squared, sex, use of public transportation in 2006, having difficulty with 1 or more Activities of Daily Living, automobile ownership, and financial circumstances | Initiation of public transportation use was not associated with a change in BMI (0.08 units, 95% CI: −0.10, 0.27), while cessation of public transportation use was associated with a BMI increase of 0.23 units (95% CI: 0.01, 0.46). An association was found between use of public transportation and BMI-measured obesity (AOR = 0.79, 95% CI: 0.63, 0.98). This was not seen with obesity measured by waist circumference(AOR = 0.96, 95% CI: 0.80, 1.16). |
Abbreviations: AOR, adjusted odds ratio; BMI, body mass index; CI, confidence interval; DSHS, Department of State Health Services; TRAX, Transit Express.
a BMI was calculated as weight (kg)/height (m)2.
b Ecological study.
c Binary variable coded as 1 for participants whose regular travel mode was automobile, taxicab, or motorcycle and coded as 0 for those using public transportation, walking, or cycling.
Seven studies investigated adiposity as a primary outcome and evaluated change in BMI using individual-level data (28, 31, 32, 34–37), while 2 studies investigated the percentage of obese participants in each exposure group (29, 30). One study also assessed the odds of being obese for public transportation users and nonusers (36). Waist circumference, in addition to BMI, was used as a measure of adiposity in 2 studies (31, 36). The only study with an outcome other than adiposity was an ecological study comparing stroke mortality among persons living proximate to new light rail infrastructure with that among persons living farther away (33). Eight of the studies used individual-level data (28, 29, 31, 32, 34–37), while the remaining 2 used ecological data, at the level of the US state (30) and the city neighborhood (33).
Study quality
Information on study quality is presented in Table 1, with additional information on quality assessments presented in Web Tables 1 and 2 and Web Appendix 2. There was a combined total of 29,021 participants in the included studies, with each study contributing between 47 and 8,028 participants, plus an additional 2 ecological studies. Three studies provided nationally representative samples using large-scale population surveys, reducing the risk of selection bias (30, 35, 36), while 5 studies selected participants on the basis of proximity to public transportation infrastructure (28, 29, 32, 33, 37). Control groups were drawn from the same population as the exposed groups in all but 1 case (33). Eight studies examined self-reported public transportation use ascertained by structured interview, which is potentially subject to recall bias (28–30, 32, 34–37). The exceptions were those which used proximity to new infrastructure and compared proximate persons with those less proximate (33) and those in which exposure was distance to the nearest bus stop, measured using geographic information systems (31).
Adiposity was measured objectively in 5 studies (28, 29, 31, 34, 36), with 4 using self-reported data (30, 32, 35, 37), which are known to be susceptible to misclassification bias (38). Stroke mortality data were obtained from a death registry, with cause of death assessed using International Classification of Diseases, Tenth Revision, codes I60–I69 (33, 39). One individual-level study pooled obesity data from both time points, which increased the risk of reverse causality or selection bias (e.g., generally healthier people choosing to live in an area in order to take advantage of proximity to public transportation) (29).
Adjustment for important potential confounders such as nontransportation physical activity and general health was inconsistent. Three studies adjusted for nontransportation physical activity (30, 34, 37), with 1 additional study adjusting for transportation walking (which included walking to get to destinations such as work or stores) (31). Five studies adjusted for a measure of general health (28, 30, 31, 34, 35), with an additional study adjusting for difficulties with Activities of Daily Living, a measure of a participant’s ability to conduct basic daily self-care activities, such as getting up from a chair (36). One ecological study adjusted for health expenditure at the state level (30), and 2 studies adjusted for diet quality (31, 37).
Public transportation and adiposity
Studies of public transportation use
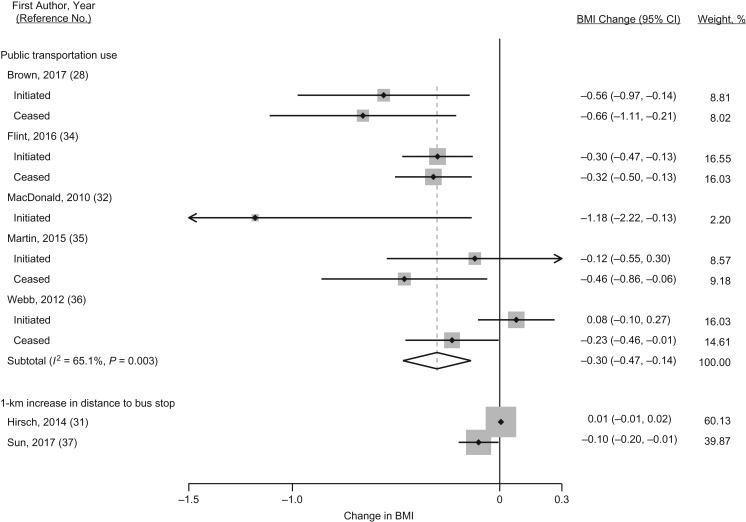
Seven of the 10 studies investigated public transportation use and adiposity, with 6 using individual-level data and 1 using ecological data. Exposure was self-reported usual mode of commuting (e.g., bus, train) in 3 studies and whether any public transportation was used in 4 studies. In comparison with persons who never used public transportation, there was a consistent association between public transportation use and lower adiposity. Five of these 7 studies measured changes in BMI and were included in the meta-analysis of initiation of public transportation use (Figure 2) (28, 32, 34–36). Four of these studies measured the impact of both initiating and ceasing public transportation use and therefore contributed 2 outcome data points to our meta-analysis (28, 34–36). Results from the meta-analysis showed that initiating public transportation use was associated with a BMI reduction of 0.30 units (95% confidence interval (CI): 0.14, 0.47). The I2 value for heterogeneity in the meta-analysis was 65.1% (Figure 2), indicating a moderate level of between-study heterogeneity (40). The largest change in BMI was seen in the study by MacDonald et al. (32), the smallest of the 5 studies and the only study not to account for the baseline health status of participants, which may have increased the risk of bias. Excluding this study resulted in an estimated BMI reduction of 0.28 units (95% CI: 0.12, 0.44) and a slightly increased I2 value of 64.6% (Web Figure 1) (32).
Figure 2.
Change in body mass index (BMI; weight (kg)/height (m)2) associated with initiation of public transportation use or distance to the nearest bus stop in a systematic review, December 2017. The direction of BMI change was reversed in persons who ceased public transportation use in order to allow comparison with those initiating use. The gray squares surrounding the point estimates represent the weighting given within each analysis. Weights were from random-effects analysis. CI, confidence interval.
We combined a range of studies in this review, which may partly explain some heterogeneity in findings. Both US-based studies evaluated the impacts of new light rail infrastructure in proximate populations and had relatively smaller sample sizes (n = 536 and n = 301) (28, 32) than comparable United Kingdom studies, which used survey data from the general population (n = 5,861, n = 4,056, and n = 4,686) (34–36). A funnel plot of the studies in this meta-analysis was inconclusive, with insufficient studies available for formal statistical tests (Web Figure 2). Differences in findings may therefore have been due to national contexts, length of follow-up, or differences in study design—specifically the fact that the 2 US studies were evaluations of new infrastructure rather than studies based on the general population. The 4 studies providing 2 data points all had a smaller magnitude of change in BMI associated with initiating public transportation use than with ceasing use, although 95% confidence intervals overlapped in each case (28, 34–36). The only studies to adjust for nontransportation physical activity provided estimates comparable with those from the other studies and similar estimates with and without adjustment: BMI change was −0.30 units (95% CI: −0.47, −0.13) with physical activity adjustment and −0.32 units (95% CI: −0.49, −0.15) without such adjustment (34).
Three studies provided noncomparable data which could not be included in the meta-analysis (29, 30, 36). A United Kingdom–based study found reduced odds of BMI-measured obesity among public transportation users (adjusted odds ratio = 0.79, 95% CI: 0.63, 0.98), although this association was not seen with obesity measured by waist circumference (36). A further study found that the proportion of obese participants among non–public transportation users was 0.65 (95% CI: 0.41, 0.89), but among initiating users and continuing users the proportions were 0.26 (95% CI: 0.01, 0.51) and 0.15 (95% CI: −0.05, 0.35), respectively (29). However, that study pooled obesity measures taken before and after public transportation use (29), increasing the potential for both selection bias and reverse causality. The final study was an ecological comparison of 50 US states over a period of 10 years which found that higher levels of public transportation commuting in 1 year were associated with lower levels of overweight (change in prevalence: −0.32%, 95% CI: −0.05, −0.59) and obesity (−0.21%, 95% CI: −0.03, −0.39) a year later (30). Results of this study mean that a 1% increase in public transportation commuting at the state level was associated with a 0.21% reduction in obesity prevalence.
Studies of proximity to public transportation
Two studies investigated associations between distance from the participant’s home to the nearest bus route and adiposity, harmonized here for comparison to express change in adiposity per 1-km change in the distance to bus routes (Figure 2) (31, 37). The 2 studies had divergent findings, with one study from China finding a negative association with BMI (−0.10 units, 95% CI: −0.20, −0.01) (37) and the other study, a US study, finding no association with BMI (0.01 units, 95% CI: −0.01, 0.02) or waist circumference (31). There were several differences between these 2 studies, including the use of objectively measured exposure in the US study and self-reported distance to bus stops in the Chinese study, which is susceptible to reporting bias; participants with higher BMIs may be more likely to overestimate the distance to the nearest bus stop. The study of Chinese participants adjusted for physical exercise, while the US study adjusted for transportation walking but no other physical activity.
Public transportation and stroke mortality
One study examined the impact of a new light rail line on stroke mortality for 2 years before and after the line opened (33). This study compared daily incidence of stroke mortality among persons of all ages living within 3, 5, and 10 miles (4.8, 8, and 16 km) of the new railway line with that among persons living more than 10 miles (>16 km) away. It employed an interrupted time series design, taking account of seasonal and long-term trends, day of the week (weekday vs. weekend), and the effects of traffic pollution (as measured by acetylene concentration). Both exposure and mortality rates were measured at an area level. There were reductions in the daily total stroke mortality rate of 39.3% (95% CI: 6.8, 60.4) within 5 miles of the light rail line and 33.3% (95% CI: 10.0, 50.6) within 10 miles of the light rail line but not in control areas (>10 miles from the light rail line; −4.1%, 95% CI: −31.9, 35.1). Using the same interrupted time series model, the study also identified reductions in average atmospheric acetylene concentrations over time, which may be a potential causal mechanism for the reduction in stroke mortality found.
DISCUSSION
This systematic review of studies examining associations between public transportation use and cardiometabolic outcomes identified 10 studies. These studies present consistent evidence that initiation of public transportation use is associated with reduced adiposity. Distance from the residential address to the nearest bus route had mixed associations with adiposity. Few studies have investigated associations between public transportation use and nonadiposity outcomes.
Comparison with previous research
The association between public transportation use and adiposity identified here is perhaps unsurprising given that public transportation use is associated with increased physical activity, that is, through walking to transportation stops and interchanges. While dietary factors may be a more important determinant of adiposity, there is a large body of literature indicating that physical activity may also confer protective benefits against adiposity. The majority of previous research on the cardiometabolic benefits of transportation has focused on walking and cycling, which have been found to have greater benefits than those identified here for public transportation (14, 15). For example, the magnitude of association we identified between public transportation use and BMI (−0.30 units, 95% CI: −0.47, −0.14) was smaller than that identified in a recent systematic review of walking interventions, which found a BMI change of −0.53 units (95% CI: −0.72, −0.35) (41). These results may be consistent with there being higher levels of physical activity among people who walk whole journeys, although this is not always the case, as many walking journeys may take place over short distances (42, 43).
We found only 1 study on the association between public transportation use and a nonadiposity outcome (stroke), so a lack of data precluded us from making any firm conclusions regarding cardiometabolic health more generally. In contrast, walking or cycling for transportation has been found to be associated with an 11% reduction in global CVD risk (15), and both pedestrian and cycle commuting have been associated with lower risks of CVD mortality (14). Further research on public transportation and cardiometabolic health is needed, including studies which better quantify associated physical activity, examine dose-response relationships, and adequately control for potential confounders, including dietary intake.
Strengths and limitations
To our knowledge, this is the first systematic review that has examined associations between public transportation use and cardiometabolic health. Strengths included the use of strict inclusion criteria which excluded cross-sectional studies and identified studies with repeated measures to capture intraindividual changes in outcomes, thus minimizing the impacts of unobserved confounding (21). While only 1 individual-level study adjusted for nontransportation physical activity, that study found an effect size comparable to that of the other studies included in this review in fully adjusted models (34). Our search strategy was broad and covered both health and transportation databases, reducing the risk of missing potential studies. The comprehensiveness of our search strategy was enhanced by the inclusion of gray literature searches through the Transport Database, Opengrey.eu, and Google. We were able to perform meta-analysis using data from 5 of the studies. Findings from this meta-analysis were broadly consistent with those from studies that we were unable to incorporate in the meta-analysis.
This review had some limitations, however. The majority of studies assessed public transportation use by self-report, which may encourage people to overstate the amount of walking and cycling they engage in as part of transportation use (7, 8). Nonetheless, 3 of the included studies used usual mode of commuting as the exposure, which is less likely to be subject to recall bias, although it may fail to capture the use of multiple modes within the same day or on different days of the week. Depending on the alternative travel modes used, this might lead to over- or underestimation of any associations between public transportation use and cardiometabolic health. Additionally, assessment of exposure across the studies was heterogeneous, making comparison difficult. For example, the Flint et al. study (34) combined walking, cycling, and public transportation commuters when investigating switching to and from automobile use. This may have produced a slightly higher estimate of adiposity changes, since walking and cycling commuters may experience greater benefits than public transportation commuters. BMI was used as the outcome in all studies assessing adiposity, although 2 also investigated waist circumference (31, 36). While questions have been raised over the validity of BMI as a measure of adiposity, particularly about its accuracy across ages and ethnic groups, it remains a common metric for assessing adiposity at the population level (44, 45).
Given the broad range of eligible outcomes, the number of included studies was low, with 9 studies investigating adiposity and 1 examining stroke mortality. There was substantial variation in the methodological quality and approach of the included studies; for example, some studies investigated intraindividual changes in outcome and some did not. In their 2008 study, Brown et al. (29) investigated change in transportation mode and BMI using measurements pooled from 2 time points, increasing the risk of reverse causality and self-selection. Statistical adjustment for potential confounders was limited in many of the included studies, with only 3 providing adjustment for nontransportation physical activity (30, 34, 37), only 2 adjusting for diet quality (31, 37), and only 1 adjusting for activity-limiting illnesses (36). The included studies may have been subject to selection bias, since such studies often focus on commuter populations—persons who are employed, more affluent, healthier, and more likely to live near transportation infrastructure. Publication bias and other small-study effects are a potential concern, but insufficient data precluded formal statistical tests of this. All studies except 1 were from the United States and the United Kingdom, which differ substantially in terms of population density, intersection density, public transportation density, and level of automobile dependence (10, 46, 47). More studies in a range of settings are required to better understand how these contextual factors may influence the relationship between transportation use and cardiometabolic health, and the generalizability of our findings to other countries is uncertain (48–50).
Policy implications
It is expected that by 2050, 66% of the global population will be living in urban areas (51, 52); therefore, it is essential in future urban planning and design to create sustainable cities which facilitate healthy lives and meet Sustainable Development Goals (2). In densely populated urban areas, particularly, well-planned efficient public transportation systems can facilitate residents’ travel while helping to maintain health. Concomitant benefits of switching from automobile use to public transportation include reduced traffic congestion, safe, walkable neighborhoods, and reduced emissions of carbon dioxide, nitrogen dioxide, particulate matter, and other pollutants (53, 54). This systematic review highlights some adiposity benefits derived from public transportation use in addition to these benefits. In the English population, a BMI reduction of 0.30 units among persons initiating public transportation use is equivalent to a mean difference of 0.9 kg in men and 0.8 kg in women (55)—sufficient to be clinically relevant and greater than changes seen with many individually focused interventions (56). Transportation planning could usefully be aimed towards encouraging increased use of public transportation by improving its availability, accessibility, and affordability in order to increase physical activity and potentially reduce adiposity (57, 58). Additionally, any increases in physical activity from such efforts would be particularly beneficial for the most sedentary people in society (11, 59), such as the elderly and members of some ethnic minority groups, who are less likely to reach recommended levels of physical activity from leisure-based activities but have high levels of public transportation use (60–64).
This review also highlights a lack of research into public transportation use and nonadiposity cardiometabolic health outcomes. Elevated adiposity in and of itself is only a marker of poor health, albeit one strongly linked with clinical health outcomes such as diabetes, CVD, and mortality (65–67). We found no individual-level prospective studies examining the association between public transportation use and nonadiposity cardiometabolic health outcomes, and we found very few studies investigating this association at all, even at an ecological level (33, 68). Further research on the health impacts of public transportation use, including the use of methods which account for selection bias and unobserved confounding and investigation of the potential effects of public transportation on incident CVD and type 2 diabetes, would be beneficial to inform policy.
CONCLUSION
This systematic review found that initiating public transportation use was associated with modestly lower adiposity. Little evidence was available for other outcomes. Incorporating public transportation into sustainable urban design should be considered a potential mechanism for reducing overweight and obesity in the general population.
Supplementary Material
ACKNOWLEDGMENTS
Author affiliations: Public Health Policy Evaluation Unit, Department of Primary Care and Public Health, School of Public Health, Imperial College London, London, United Kingdom (Richard Patterson, Thomas Hone, Christopher Millett, Anthony A. Laverty); and Economic and Social Research Council International Centre for Lifecourse Studies, Department of Epidemiology and Public Health, University College London, London, United Kingdom (Elizabeth Webb).
This report reflects independent research supported by the National Institute for Health Research (NIHR) (Research Professorship RP 2014-04-032 awarded to C.M.). The Public Health Policy Evaluation Unit at Imperial College London received financial support from the NIHR School of Public Health Research. E.W. was supported by the Economic and Social Research Council’s International Centre for Lifecourse Studies in Society and Health (grant ES/J019119/1).
The views expressed in this publication are those of the author(s) and not necessarily those of the United Kingdom National Health Service, the NIHR, or the Department of Health and Social Care.
Conflict of interest: none declared.
Abbreviations
- BMI
body mass index
- CI
confidence interval
- CVD
cardiovascular disease
REFERENCES
- 1. Deng T, Nelson JD. Recent developments in bus rapid transit: a review of the literature. Transp Rev. 2011;31(1):69–96. [Google Scholar]
- 2. United Nations Sustainable Development Goals. 2015. http://www.un.org/sustainabledevelopment/sustainable-development-goals/. Accessed March 8, 2018.
- 3. United Kingdom Department for Transport The Bus Services Bill: An Overview London, United Kingdom: Department for Transport; 2016. https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/558349/the-bus-services-bill-an-overview.pdf. Accessed October 27, 2016.
- 4. Chapman L. Transport and climate change: a review. J Transp Geogr. 2007;15(5):354–367. [Google Scholar]
- 5. Rissel C, Curac N, Greenaway M, et al. Physical activity associated with public transport use—a review and modelling of potential benefits. Int J Environ Res Public Health. 2012;9(7):2454–2478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Besser LM, Dannenberg AL. Walking to public transit: steps to help meet physical activity recommendations. Am J Prev Med. 2005;29(4):273–280. [DOI] [PubMed] [Google Scholar]
- 7. Chaix B, Kestens Y, Duncan S, et al. Active transportation and public transportation use to achieve physical activity recommendations? A combined GPS, accelerometer, and mobility survey study. Int J Behav Nutr Phys Act. 2014;11:Article 124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Saelens BE, Vernez Moudon A, Kang B, et al. Relation between higher physical activity and public transit use. Am J Public Health. 2014;104(5):854–859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. McKenzie B. Modes Less Traveled—Bicycling and Walking to Work in the United States: 2008–2012 (Report no. ACS-25). Washington, DC: Bureau of the Census, US Department of Commerce; 2014. https://www.census.gov/library/publications/2014/acs/acs-25.html. Accessed January 8, 2017.
- 10. Gower TL. 2011 Census Analysis—Method of Travel to Work in England and Wales Report London, United Kingdom: United Kingdom Office for National Statistics; 2013. http://webarchive.nationalarchives.gov.uk/20160105160709/http://www.ons.gov.uk/ons/dcp171766_299766.pdf. Accessed March 27, 2017.
- 11. Woodcock J, Franco OH, Orsini N, et al. Non-vigorous physical activity and all-cause mortality: systematic review and meta-analysis of cohort studies. Int J Epidemiol. 2011;40(1):121–138. [DOI] [PubMed] [Google Scholar]
- 12. Laverty AA, Mindell JS, Webb EA, et al. Active travel to work and cardiovascular risk factors in the United kingdom. Am J Prev Med. 2013;45(3):282–288. [DOI] [PubMed] [Google Scholar]
- 13. Dalton AR, Bottle A, Soljak M, et al. Ethnic group differences in cardiovascular risk assessment scores: national cross-sectional study. Ethn Health. 2014;19(4):367–384. [DOI] [PubMed] [Google Scholar]
- 14. Celis-Morales CA, Lyall DM, Welsh P, et al. Association between active commuting and incident cardiovascular disease, cancer, and mortality: prospective cohort study. BMJ. 2017;357:j1456. [DOI] [PubMed] [Google Scholar]
- 15. Hamer M, Chida Y. Active commuting and cardiovascular risk: a meta-analytic review. Prev Med. 2008;46(1):9–13. [DOI] [PubMed] [Google Scholar]
- 16. Hamer M, Chida Y. Walking and primary prevention: a meta-analysis of prospective cohort studies. Br J Sports Med. 2008;42(4):238–243. [DOI] [PubMed] [Google Scholar]
- 17. Kelly P, Kahlmeier S, Götschi T, et al. Systematic review and meta-analysis of reduction in all-cause mortality from walking and cycling and shape of dose response relationship. Int J Behav Nutr Phys Act. 2014;11:Article 132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Murphy MH, Nevill AM, Murtagh EM, et al. The effect of walking on fitness, fatness and resting blood pressure: a meta-analysis of randomised, controlled trials. Prev Med. 2007;44(5):377–385. [DOI] [PubMed] [Google Scholar]
- 19. Oja P, Titze S, Bauman A, et al. Health benefits of cycling: a systematic review. Scand J Med Sci Sports. 2011;21(4):496–509. [DOI] [PubMed] [Google Scholar]
- 20. Mytton OT, Ogilvie D, Griffin S, et al. Associations of active commuting with body fat and visceral adipose tissue: a cross-sectional population based study in the UK. Prev Med. 2018;106:86–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Sedgwick P. Cross sectional studies: advantages and disadvantages. BMJ. 2014;348:g2276. [DOI] [PubMed] [Google Scholar]
- 22. Higgins JPT, Green S, eds. Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1.0 (Updated March 2011) London, United Kingdom: The Cochrane Collaboration; 2011. www.handbook.cochrane.org. Accessed February 15, 2018.
- 23. Wells GA, Shea B, O’Connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Published 2000. Accessed August 21, 2015.
- 24. Juni P, Witschi A, Bloch R, et al. The hazards of scoring the quality of clinical trials for meta-analysis. JAMA. 1999;282(11):1054–1060. [DOI] [PubMed] [Google Scholar]
- 25. DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–188. [DOI] [PubMed] [Google Scholar]
- 26. Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–1558. [DOI] [PubMed] [Google Scholar]
- 27. Sterne JA, Sutton AJ, Ioannidis JP, et al. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ. 2011;343:d4002. [DOI] [PubMed] [Google Scholar]
- 28. Brown BB, Tharp D, Smith KR, et al. Objectively measured active travel and uses of activity-friendly neighborhood resources: does change in use relate to change in physical activity and BMI? Prev Med Rep. 2017;8:60–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Brown BB, Werner CM. Before and after a new light rail stop: resident attitudes, travel behavior, and obesity. J Am Plann Assoc. 2008;75(1):5–12. [Google Scholar]
- 30. Chen C, Menifield CE. An ecological study on means of transportation to work and obesity: evidence from US states. Transp Policy. 2017;59:174–180. [Google Scholar]
- 31. Hirsch JA, Moore KA, Barrientos-Gutierrez T, et al. Built environment change and change in BMI and waist circumference: Multi-Ethnic Study of Atherosclerosis. Obesity (Silver Spring). 2014;22(11):2450–2457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. MacDonald JM, Stokes RJ, Cohen DA, et al. The effect of light rail transit on body mass index and physical activity. Am J Prev Med. 2010;39(2):105–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Park ES, Sener IN. Impact of light rail transit on traffic-related pollution and stroke mortality. Int J Public Health. 2017;62(7):721–728. [DOI] [PubMed] [Google Scholar]
- 34. Flint E, Webb E, Cummins S. Change in commute mode and body-mass index: prospective, longitudinal evidence from UK Biobank. Lancet Public Health. 2016;1(2):e46–e55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Martin A, Panter J, Suhrcke M, et al. Impact of changes in mode of travel to work on changes in body mass index: evidence from the British Household Panel Survey. J Epidemiol Community Health. 2015;69(8):753–761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Webb E, Netuveli G, Millett C. Free bus passes, use of public transport and obesity among older people in England. J Epidemiol Community Health. 2012;66(2):176–180. [DOI] [PubMed] [Google Scholar]
- 37. Sun B, Yan H, Zhang T. Built environmental impacts on individual mode choice and BMI: evidence from China. J Transp Geogr. 2017;63:11–21. [Google Scholar]
- 38. Gosse MA. How accurate is self-reported BMI? Nutr Bull. 2014;39(1):105–114. [Google Scholar]
- 39. World Health Organization The ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines Geneva, Switzerland: World Health Organization; 1992. https://www.who.int/classifications/icd/en/bluebook.pdf. Accessed October 10, 2018.
- 40. Higgins JP, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Murtagh EM, Nichols L, Mohammed MA, et al. The effect of walking on risk factors for cardiovascular disease: an updated systematic review and meta-analysis of randomised control trials. Prev Med. 2015;72:34–43. [DOI] [PubMed] [Google Scholar]
- 42. Foley L, Panter J, Heinen E, et al. Changes in active commuting and changes in physical activity in adults: a cohort study. Int J Behav Nutr Phys Act. 2015;12:Article 161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Saunders LE, Green JM, Petticrew MP, et al. What are the health benefits of active travel? A systematic review of trials and cohort studies. PLoS One. 2013;8(8):e69912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Scholes S, Mindell J. Physical activity in adults In: Craig R, Mindell J, eds. Health Survey for England 2012. Volume 1: Health, Social Care and Lifestyles. Leeds, United Kingdom: Health and Social Care Information Centre; 2013:12–18. [Google Scholar]
- 45. Ogden CL, Carroll MD, Kit BK, et al. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014;311(8):806–814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Adams MA, Frank LD, Schipperijn J, et al. International variation in neighborhood walkability, transit, and recreation environments using geographic information systems: the IPEN adult study. Int J Health Geogr. 2014;13:Article 43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. McKenzie B, Rapine M. Commuting in the United States: 2009 (American Community Survey Reports, ACS-15). Washington, DC: Bureau of the Census, US Department of Commerce; 2011. https://www2.census.gov/library/publications/2011/acs/acs-15.pdf. Accessed June 15, 2018.
- 48. Barr A, Bentley R, Simpson JA, et al. Associations of public transport accessibility with walking, obesity, metabolic syndrome and diabetes. J Transp Health. 2016;3(2):141–153. [Google Scholar]
- 49. Hess DB, Russell JK. Influence of built environment and transportation access on body mass index of older adults: survey results from Erie County, New York. Transp Policy. 2012;20:128–137. [Google Scholar]
- 50. Rundle A, Diez Roux AV, Free LM, et al. The urban built environment and obesity in New York City: a multilevel analysis. Am J Health Promot. 2007;21(4 suppl):326–334. [DOI] [PubMed] [Google Scholar]
- 51. Carmichael L, Racioppi F, Calvert T, et al. Environment and Health for European Cities in the 21st Century: Making a Difference Copenhagen, Denmark: World Health Organization Regional Office for Europe; 2017. http://www.euro.who.int/__data/assets/pdf_file/0020/341615/bookletdef.pdf?ua=1. Accessed December 11, 2017.
- 52. World Health Organization Regional Office for Europe Towards More Physical Activity in Cities Copenhagen, Denmark: World Health Organization Regional Office for Europe; 2017. http://www.euro.who.int/__data/assets/pdf_file/0018/353043/2017_WHO_Report_FINAL_WEB.pdf?ua=1. Accessed December 11, 2017.
- 53. Xia T, Zhang Y, Crabb S, et al. Cobenefits of replacing car trips with alternative transportation: a review of evidence and methodological issues. J Environ Public Health. 2013;2013:797312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Sallis JF, Floyd MF, Rodriguez DA, et al. Role of built environments in physical activity, obesity, and cardiovascular disease. Circulation. 2012;125(5):729–737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Moody A. Adult anthropometric measures, overweight and obesity In: Craig R, Mindell J, eds. Health Survey for England 2012. Volume 1: Health, Social Care and Lifestyles. Leeds, United Kingdom: Health and Social Care Information Centre; 2012:12–15. [Google Scholar]
- 56. Stephens SK, Cobiac LJ, Veerman JL. Improving diet and physical activity to reduce population prevalence of overweight and obesity: an overview of current evidence. Prev Med. 2014;62:167–178. [DOI] [PubMed] [Google Scholar]
- 57. Martin A, Suhrcke M, Ogilvie D. Financial incentives to promote active travel: an evidence review and economic framework. Am J Prev Med. 2012;43(6):e45–e57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. National Institute for Health and Care Excellence Physical Activity and the Environment (NICE Guideline 90). London, United Kingdom: National Institute for Health and Care Excellence; 2018. https://www.nice.org.uk/guidance/ng90/chapter/Recommendations. Accessed March 23, 2018.
- 59. Smith AD, Crippa A, Woodcock J, et al. Physical activity and incident type 2 diabetes mellitus: a systematic review and dose-response meta-analysis of prospective cohort studies. Diabetologia. 2016;59(12):2527–2545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. United Kingdom Department for Transport National Travel Survey: 2016. https://www.gov.uk/government/statistics/national-travel-survey-2016. Published July 27, 2017. Updated January 18, 2018. Accessed June 5, 2018.
- 61. United Kingdom Department for Transport Travel by distance, trips, type of transport and purpose. https://www.ethnicity-facts-figures.service.gov.uk/culture-and-community/transport/travel-by-distance-trips-type-of-transport-and-purpose/latest. Published October 1, 2018. Accessed June 5, 2018.
- 62. Higgins V, Dale A. Ethnic differences in physical activity and obesity In: Stillwell J, van Ham M, eds. Ethnicity and Integration: Understanding Population Trends and Processes. Vol. 3 London, United Kingdom: Springer-Verlag London Ltd.; 2010:203–206. [Google Scholar]
- 63. Paterson DH, Warburton DE. Physical activity and functional limitations in older adults: a systematic review related to Canada’s Physical Activity Guidelines. Int J Behav Nutr Phys Act. 2010;7:Article 38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Physical Activity Guidelines Advisory Committee 2008 Physical Activity Guidelines for Americans Washington, DC: Office of Disease Prevention and Health Promotion, US Department of Health and Human Services; 2008. http://health.gov/paguidelines/guidelines/. Accessed February 26, 2016.
- 65. Masters RK, Reither EN, Powers DA, et al. The impact of obesity on US mortality levels: the importance of age and cohort factors in population estimates. Am J Public Health. 2013;103(10):1895–1901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Bastien M, Poirier P, Lemieux I, et al. Overview of epidemiology and contribution of obesity to cardiovascular disease. Prog Cardiovasc Dis. 2014;56(4):369–381. [DOI] [PubMed] [Google Scholar]
- 67. Abdullah A, Peeters A, de Courten M, et al. The magnitude of association between overweight and obesity and the risk of diabetes: a meta-analysis of prospective cohort studies. Diabetes Res Clin Pract. 2010;89(3):309–319. [DOI] [PubMed] [Google Scholar]
- 68. Langerudi MF, Abolfazl M, Sriraj PS. Health and transportation: small scale area association. J Transp Health. 2015;2(2):127–134. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.