Abstract
This study uses data from the 500 Cities Project to characterize inequities in cigarette smoking both between and within cities and their association with sociodemographic factors and chronic diseases.
Achieving universal health and well-being for all Americans is the ideal goal for US public health efforts, but inequities in chronic disease and life expectancy present a persistent challenge, particularly in large cities.1 In 2016, the Robert Wood Johnson Foundation and the US Centers for Disease Control and Prevention launched the 500 Cities Project, providing small-area estimates of modifiable risk factors for chronic disease in the 500 largest US cities.2 To guide prevention efforts, we used these data to characterize inequities in cigarette smoking both between and within cities and in relation to sociodemographic factors and chronic diseases.
Methods
The 500 Cities Project provides model-estimated health indicators at the census-tract level from the 2014 Behavioral Risk Factor Surveillance Survey.2 A census tract is generally smaller than a city, larger than a block group, and a fairly permanent subdivision of a county. Our analysis used the prevalence of adult (≥18 years) self-reported current smoking, asthma, chronic obstructive pulmonary disease (COPD), and coronary heart disease (CHD). Complete data from the 500 Cities Project were available for 27 204 tracts. We combined the 500 Cities Project estimates with tract-level sociodemographic data from the American Community Survey (2012-2016) and counts of likely tobacco retailers from 10 North American Industrial Classification System codes in the National Establishment Time Series Data for 2012 (120 470 tobacco retailers in the 27 204 tracts).3
We used linear mixed models to characterize smoking prevalence inequities within and between cities; assess tract-level smoking prevalence as a function of tract-level sociodemographic characteristics and tobacco retailer counts; and assess tract-level asthma, COPD, and CHD prevalence as a function of tract-level smoking prevalence. We also computed Gini coefficients to quantify the dispersion of smoking prevalence between census tracts within each of the 500 cities, where 0 = perfect equality and 1 = maximal inequality.4 Data sources and analytical methods are further detailed in the Supplement.
Results
Smoking prevalence inequities were greater between tracts within cities (56.1% of the total variation) than between cities (43.9% of the total variation) (Table). Tracts with higher smoking prevalence had more tobacco retailers (5-store increase, β = 0.11; 95% CI, 0.07-0.16; P < .001), lower median household income ($10 000 increase, β = −0.92; 95% CI, −0.94 to −0.90; P < .001), and a smaller percentage of non-Hispanic white residents (10% increase, β = −0.84; 95% CI, −0.86 to −0.82; P < .001).
Table. Fixed Effects and Random Effects Resulting From the Linear Mixed Models for Smoking Prevalence Among 27 204 Census Tracts in the 500 Cities Projecta.
| Fixed Effect | β (95% CI) | P Value |
|---|---|---|
| Intercept | 27.89 (27.54 to 28.24) | <.001 |
| No. of tobacco retailers (5-store increase) | 0.11 (0.07 to 0.16) | <.001 |
| Median household income ($10 000 increase) | −0.92 (−0.94 to −0.90) | <.001 |
| Percent non-Hispanic white population (10-percentage-point increase) | −0.84 (−0.86 to −0.82) | <.001 |
| Random effects (null model) | Variance (95% CI) |
|
| Between-city | 18.73 (16.46 to 21.33) | <.001 |
| Residual (within-city) | 23.97 (23.57 to 24.38) |
Listwise deletion was used for 125 tracts that were missing information on household income. All models with fixed effects simultaneously adjust for the listed fixed effects and also for total population size.
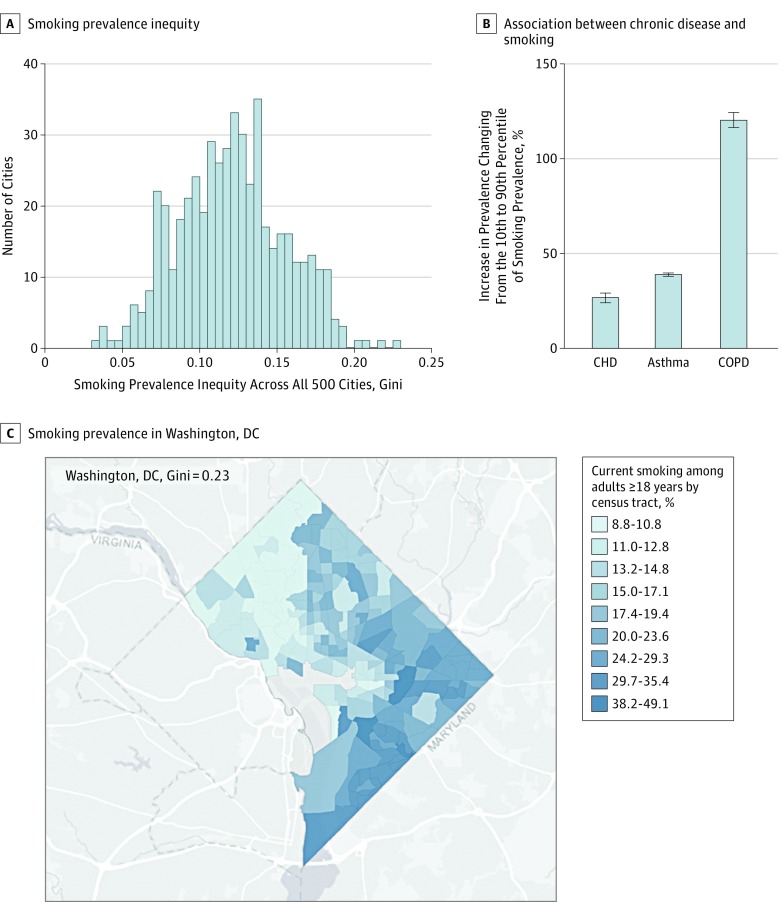
Although all cities had some smoking prevalence inequity (Figure, A) (Gini coefficients ≥0.03), inequity was greatest in Washington, DC (Gini = 0.23); Atlanta, Georgia (Gini = 0.22); Fort Lauderdale, Florida (Gini = 0.21); and Miami, Florida (Gini = 0.20). Figure, C illustrates smoking prevalence in the city with the greatest inequity, Washington, DC.
Figure. Smoking Prevalence Inequities and Their Association With Inequities in Chronic Diseases.
A, All cities have at least some inequity (Gini coefficient ≥0.03) and 4 cities (Washington, DC; Atlanta, Georgia; Fort Lauderdale, Florida; and Miami, Florida) have particularly high inequity (Gini ≥0.20). B, The prevalence of current self-reported asthma, chronic obstructive pulmonary disease (COPD), and coronary heart disease (CHD) is higher in tracts with higher prevalence of current smoking. Estimates shown in Figure 1B result from multivariable linear mixed models that adjust for percent non-Hispanic white population, median household income, total population size, and a random effect for city. We calculated the expected percent increase in prevalence of each chronic disease of changing from the 10th to 90th percentile of smoking prevalence (from 10.7% to 27.6%) and the corresponding 95% confidence intervals using these multivariable linear mixed models and by using 1000 draws from the multivariate normal distribution with the mean equal to the maximum likelihood point estimate and the variance equal to the coefficient covariance matrix. C, Differences in tract-level smoking prevalence for the city with the greatest inequity in smoking prevalence: Washington, DC (Gini = 0.23). The color in the image uses Jenks natural breaks (9 classes) based on the data for the Washington, DC, census tracts. One Washington, DC, census tract had insufficient data to make a smoking prevalence estimate and is illustrated in gray. Data sources and analytical methods are further detailed in the supplementary appendix.
At the tract level, higher smoking prevalence was associated with higher prevalence of asthma, COPD, and CHD (Figure, B). For instance, a change from the 10th to the 90th percentile of smoking prevalence (from 10.7% to 27.6%) was associated with a 38.9% (95% CI, 38.1%-39.5%) increase in the prevalence of asthma, a 120.2% (95% CI, 116.6%-124.0%) increase in the prevalence of COPD, and a 26.6% (95% CI, 24.5%-29.0%) increase in the prevalence of CHD.
Discussion
Smoking prevalence was unevenly distributed both within and between America’s largest cities, and was associated with inequities in income, race, exposure to tobacco retailers, and smoking-related diseases. Strengthening existing tobacco control interventions, such as raising excise taxes and implementing cessation programs targeted to resource-poor communities, may aid in counteracting these inequities in smoking.5 In addition, novel policies that restrict the retail environment (eg, by limiting the quantity, location, and type of tobacco retailers) show promise for reducing the unequal distribution of tobacco retailers and warrant further investigation.6
Data Sources
eTable 1. Likely Tobacco Retailers Identified by North American Industry Classification System (NAICS) Codes: National Establishment Time Series Data (2012)
eTable 2. Top 50 Pharmacies in US
eMethods
eTable 3. The linear mixed models for asthma, COPD, and CHD prevalence among census-tracts in the 500 cities projects (n=27,704)
eReferences
References
- 1.Chetty R, Stepner M, Abraham S, et al. The Association Between Income and Life Expectancy in the United States, 2001-2014. JAMA. 2016;315(16):1750-1766. doi: 10.1001/jama.2016.4226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.500 Cities: Local Data for Better Health, 2017. release | Chronic Disease and Health Promotion Data & Indicators. https://chronicdata.cdc.gov/500-Cities/500-Cities-Local-Data-for-Better-Health-2017-relea/6vp6-wxuq. Accessed June 21, 2018.
- 3.Kaufman TK, Sheehan DM, Rundle A, et al. Measuring health-relevant businesses over 21 years: refining the National Establishment Time-Series (NETS), a dynamic longitudinal data set. BMC Res Notes. 2015;8:507. doi: 10.1186/s13104-015-1482-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cowell FA. Measurement of inequality In: Atkinson A, Bourguignon F, eds. Handbook of Income Distribution. Vol 1 Elsevier; 2000:87-166, doi: 10.1016/S1574-0056(00)80005-6. [DOI] [Google Scholar]
- 5.Brown T, Platt S, Amos A. Equity impact of population-level interventions and policies to reduce smoking in adults: a systematic review. Drug Alcohol Depend. 2014;138:7-16. doi: 10.1016/j.drugalcdep.2014.03.001 [DOI] [PubMed] [Google Scholar]
- 6.Luke DA, Hammond RA, Combs T, et al. Tobacco Town: Computational Modeling of Policy Options to Reduce Tobacco Retailer Density. Am J Public Health. 2017;107(5):740-746. doi: 10.2105/AJPH.2017.303685 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Sources
eTable 1. Likely Tobacco Retailers Identified by North American Industry Classification System (NAICS) Codes: National Establishment Time Series Data (2012)
eTable 2. Top 50 Pharmacies in US
eMethods
eTable 3. The linear mixed models for asthma, COPD, and CHD prevalence among census-tracts in the 500 cities projects (n=27,704)
eReferences