Key Points
Question
What is the association of long-term (≥1 year) exercise with the risk of falls, fractures, hospitalizations and death in older adults?
Findings
In this meta-analysis of 40 long-term randomized clinical trials (RCTs) of 21 868 participants, exercise significantly decreased the risk of being a faller and injurious faller but did not significantly reduce the risk of fractures. Exercise did not diminish the risk of multiple falls, hospitalization, and mortality.
Meaning
Long-term exercise, particularly moderate intensity, multicomponent training with balance exercises, performed 2 to 3 times per week, appears to be a safe and effective intervention for reducing the risk of being a faller/injurious faller in older populations.
This systematic review and meta-analysis investigates the association of long-term exercise interventions with the risk of falls, injurious falls, multiple falls, fractures, hospitalization, and mortality in older adults.
Abstract
Importance
Long-term exercise benefits on prevalent adverse events in older populations, such as falls, fractures, or hospitalizations, are not yet established or known.
Objective
To systematically review and investigate the association of long-term exercise interventions (≥1 year) with the risk of falls, injurious falls, multiple falls, fractures, hospitalization, and mortality in older adults.
Data Sources
PubMed, Cochrane Central Register of Controlled Trials, SportDiscus, PsychInfo, and Ageline were searched through March 2018.
Study Selection
Exercise randomized clinical trials (RCTs) with intervention length of 1 year or longer, performed among participants 60 years or older.
Data Extraction and Synthesis
Two raters independently screened articles, abstracted the data, and assessed the risk of bias. Data were combined with risk ratios (RRs) using DerSimonian and Laird’s random-effects model (Mantel-Haenszel method).
Main Outcomes and Measures
Six binary outcomes for the risk of falls, injurious falls, multiple falls (≥2 falls), fractures, hospitalization, and mortality.
Results
Forty-six studies (22 709 participants) were included in the review and 40 (21 868 participants) in the meta-analyses (mean [SD] age, 73.1 [7.1] years; 15 054 [66.3%] of participants were women). The most used exercise was a multicomponent training (eg, aerobic plus strength plus balance); mean frequency was 3 times per week, about 50 minutes per session, at a moderate intensity. Comparator groups were often active controls. Exercise significantly decreased the risk of falls (n = 20 RCTs; 4420 participants; RR, 0.88; 95% CI, 0.79-0.98) and injurious falls (9 RTCs; 4481 participants; RR, 0.74; 95% CI, 0.62-0.88), and tended to reduce the risk of fractures (19 RTCs; 8410 participants; RR, 0.84; 95% CI, 0.71-1.00; P = .05). Exercise did not significantly diminish the risk of multiple falls (13 RTCs; 3060 participants), hospitalization (12 RTCs; 5639 participants), and mortality (29 RTCs; 11 441 participants). Sensitivity analyses provided similar findings, except the fixed-effect meta-analysis for the risk of fracture, which showed a significant effect favoring exercisers (RR, 0.84; 95% CI, 0.70-1.00; P = .047). Meta-regressions on mortality and falls suggest that 2 to 3 times per week would be the optimal exercise frequency.
Conclusions and Relevance
Long-term exercise is associated with a reduction in falls, injurious falls, and probably fractures in older adults, including people with cardiometabolic and neurological diseases.
Introduction
Exercise training is an intervention of utmost importance for older adults’ health leading to benefits on multiple systems and functions, including muscle and bone health, the cardiometabolic system,1,2 as well as physical1,3,4 and potentially cognitive (results still mixed5,6) functions. Recent meta-analyses of randomized clinical trials (RCT) have shown that exercise reduces the number of incident falls in older adults,7,8,9 a major adverse event for this population.
Nevertheless, important gaps about the association of exercise with decreased risk of developing serious adverse outcomes still remain unclear. Most studies included in meta-analyses7,8,9 were short- to medium-term exercise interventions, evidencing a paucity of long-term (≥1 year) RCTs. Other important gaps are: a lack of evidence on exercise effects on death and hospitalization in diverse older adult populations, and the best exercise prescription (ie, type, intensity, frequency, session duration) for decreasing the risk of serious adverse events. The recent findings of the LIFE study,10 the largest and longest exercise trial performed to date among older people, showed, unexpectedly, increases in both hospitalization and mortality among exercisers compared with controls (differences statistically nonsignificant), raising doubts about safety issues of exercise for older individuals. Furthermore, meta-analyses have obtained mixed results for the effects of exercise in preventing fractures.2,11,12 Regarding falls, to the best of our knowledge, no meta-analyses have investigated the association of long-term exercise with falls-related outcomes, particularly multiple falls, which are common in older adults.13
The objectives of this systematic review of RCTs with preplanned meta-analysis were to investigate the association of long-term exercise interventions with the risk of mortality, hospitalization, becoming a faller, a faller with multiple falls, a faller with injurious falls, and sustaining a fracture.
Methods
This systematic review and meta-analysis was registered in PROSPERO (CRD42018090757) and follows the PRISMA guidelines.14 The protocol is available in the Supplement.
Search Strategy and Eligibility Criteria
One author (M.M.) performed the electronic searches between February 20 and March 5, 2018, using a search strategy approved by all authors, from inception until the date of search in the following databases: PubMed, Cochrane Central Register of Controlled Trials, SportDiscus, PsychInfo, and Ageline. Full search strategies are available in the Supplement. Language restrictions were not applied. Two authors performed title/abstract screening independently. After that, the full-text of potentially eligible studies was accessed by 2 authors (P.S.B. and M.M.) for finally determining eligibility and, then, proceeding to data extraction. The reference list of previous systematic reviews7,8,9,12,15,16 were scrutinized. Divergences between authors on articles’ eligibility were resolved in an in-person meeting (100% consensus on articles’ eligibility was reached).
To be included in this review, studies had to meet the following criteria: (1) RCT design with exercise length of 1 year or longer (or ≥12 months or ≥48 weeks); (2) the study compared the effects of at least 1 exercise intervention against a comparator group (ie, no intervention, attention or active controls). Studies operationalizing cointerventions were eligible if the sole difference between intervention and comparator was the exercise training. All kinds of intervention structure (eg, home-based or group-based) were eligible, with unsupervised exercises being included only when a personalized exercise plan had been used; (3) participants had to be 60 years or older at baseline or the mean population age should be 60 years or older.
Outcome Measures
Six binary outcomes including mortality; hospitalization: number of individuals admitted to the hospital (eg, inpatient hospitalization, ≥24-hour hospitalization); fallers: people who fell at least once; fallers with multiple falls: people who fell at least twice; injurious fallers: people who suffered an injurious fall (eg, fall with wound, head trauma, medical care, fracture, or hospitalization) according to original investigators; and fractures: number of people who sustained a fracture.
Data Extraction
Two raters (P.S.B. and M.M.) made the data abstraction independently using a standard data collection form specifically designed for this review. Divergences were solved in an in-person meeting (100% consensus reached). In case of doubts or insufficient data/information reported, original investigators were contacted by email.
When extracting data for the meta-analysis, we prioritized comparisons in which the sole difference between groups was the exercise intervention. In studies with multiple exercise groups vs a control group, we selected for the meta-analysis the group with higher amount of exercise sessions performed.
Risk of Bias
Two authors (P.S.B. and M.M.) independently coded the risk of bias in the 7 domains of the Cochrane Collaboration’s tool.17
Statistical Analysis
Data on death, people hospitalized, fallers, and people with fractures were obtained from baseline until the end of the intervention period; data from observational follow-up were not used. Estimates of the outcomes were combined using the risk ratio (RR). Regarding fractures, for 5 studies without data on the number of people with fractures, we assumed the number of people with fractures was the same as the number of fractures (multiple fractures representing a relatively uncommon outcome, which would not severely bias our estimations); a sensitivity analysis removing these studies was undertaken. As prespecified in the review protocol (Supplement), we employed DerSimonian and Laird’s random-effects model18 (with Mantel-Haenszel method). Heterogeneity was evaluated using the I2 statistics, with an I2 greater than 50% representing substantial heterogeneity.19 Potential bias was evaluated using the Egger’s test, with P < .10 indicating substantial asymmetry, and funnel plots. Randomized clinical trials with attrition rates of more than 40% and those with low compliance (<30%) to the exercise intervention did not enter into the primary analyses, but were added in sensitivity analyses. Trials with no data on a given outcome were removed from meta-analysis of the specific outcome. For cluster RCTs, we used appropriate intracluster correlation (ICC) values (from the study, from another similar study included in the review, or from external databases20,21,22) to estimate the effective sample size using the design effect. If no appropriate estimate was available, we presented unadjusted estimates and ran a sensitivity analysis by removing cluster RCTs.
Other sensitivity/subgroup analyses were undertaken as prespecified in the protocol: by using a fixed-effect model when I2 was less than 50%, by restricting the analysis to RCTs with a low risk of attrition bias, and by stratifying analysis according to study population (clinically specific or disease specific vs nonclinically specific). We further performed analysis restricted to trials that have randomized more than 203 participants (median of study population across included RCTs), and by removing the 2 trials23,24 in which the average baseline age of participants was around 59 to properly address this deviation to the protocol.
When the number of studies was 10 or more, exploratory metaregressions were undertaken in an attempt to find which aspects of the exercise regimen would be associated to the effect size (log-transformed) of the outcomes. The following variables were tested: exercise frequency (3 times per week or more than 3 times per week compared with twice per week or less) as well as effective exercise frequency (weekly frequency multiplied by exercise compliance: between 2-3 times per week or more than 3 times per week compared with less than twice per week), volume (product of intensity and session duration: between 120 minutes per week and 180 minutes per week or 180 or more minutes per week compared with less than 120 minutes per week), intensity (vigorous compared with moderate), and type (aerobic, strength, or other exercise type compared with multicomponent training); given the importance of balance for all outcomes of this review, we also compared multicomponent training comprising a balance component vs all other exercise types combined.
All analyses were performed using STATA statistical software (version 14, StataCorp).
Results
Forty-eight articles,10,13,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68 representing 46 studies, met eligibility criteria and were included in the review. The flowchart for study selection is provided in the Supplement. The Table provides the characteristics of the included RCTs. The 46 studies have randomized 22 709 (median of 203 participants; range from 20 to 6420) participants and have been conducted mainly in Europe (n = 15), North America (n = 13, with 11 studies in the United States), and Oceania (n = 10). Participants had a mean age of 73.1 years, 66.3% were women (2 RCTs included only men45,46 and 11 solely included women13,27,34,37,43,48,49,53,55,56,64); mean intervention length was 17 months (median, 12 months). Sixteen trials23,24,29,33,40,41,45,46,50,51,52,57,58,61,62,64 were conducted in clinically specific or disease specific populations (eg, mild cognitive impairment or dementia [n = 7] and cardiac diseases [n = 4]). Thirty-five studies were parallel-group RCTs, whereas 11 were cluster RCTs30,31,32,35,36,47,51,52,65,67,68; most of the trials involved community dwellers (n = 35). Two studies in which participants had a baseline age of 59 years23 and 59.324 were included because their follow-up length was among the largest (12023 and 30.124 months, respectively), meaning that the average age increased to above 60 still at the beginning of the study. Two cluster RCTs were removed from primary quantitative analysis because very few participants exercised (26%30) or a very small fraction of exercise sessions (24%31) were attended.
Table. Characteristics of the Included Studies.
| Source | Country | Study Design, Participants, Groups, and Sample Size | Setting | Intervention Length, mo |
|---|---|---|---|---|
| Belardinelli et al,23 2012 | Italy | Study population: 59 years; chronic heart failure; 22% women; 2 groups: exercise (n = 63), control (n = 60) | Community dwellersa | 120.0 |
| Barnett et al,42 2003 | Australia | Study population: 75 years; 67% women; 2 groups: exercise (n = 83), control (n = 80) | Community dwellers | 12.0 |
| Bunout et al,25 2005b | Chile | Study population: 75 years; 71% women; 2 groups | Community dwellers | 12.0 |
| O’Connor et al,24 2009 | United States/Canada/France | Study population: 59 years; chronic heart failure; 28% women; 2 groups: exercise (n = 1159), control (n = 1172) | Community dwellersa | 30.1 |
| Campbell et al,13 1997 | New Zealand | Study population: 84 years; 100% women; 2 groups: exercise (n = 116), control (n = 117) | Community dwellers | 12.0 |
| Dangour et al,31 2011 | Chile | Study population: 66 years, 68% women; 4 groups: nutrition supplement (n = 502), nutrition supplement + exercise (n = 516), exercise (n = 480),c control (n = 504)c | Health centers | 24.0 |
| El-Khoury et al,43 2015 | France | Study population: 80 years; 100% women; 2 groups: exercise (n = 352), control (n = 354) | Community dwellers | 24.0 |
| Galvão et al,45 2014 | Australia/New Zealand | Study population: 72 years; 0% women; prostate cancer; 2 groups: exercise (n = 50), control (n = 50) | Community dwellersa | 12.0 |
| Gianoudis et al,44 2014 | Australia | Study population: 68 years; 73% women; 2 groups: exercise (n = 81), control (n = 81) | Community dwellers | 12.0 |
| Hambrecht et al,46 2004 | Germany | Study population: 61 years; 0% women; coronary heart disease; 2 groups: exercise (n = 51), control (n = 50) | Community dwellers | 12.0 |
| Hewitt et al,47 2018 | Australia | Study population: 86 years; 65% women; 2 groups: exercise (n = 113), control (n = 108) | Institutionalized | 12.0 |
| Karinkanta et al,48 2007 | Finland | Study population: 73 years; 100% women; 4 groups: exercise (n = 37)d, control (n = 37) | Community dwellers | 12.0 |
| Kemmler et al,34 2010 | Germany | Study population: 69 years; 100% women; 2 groups: exercise (n = 123), control (n = 123) | Community dwellers | 18.0 |
| King et al,49 2002 | United States | Study population: 63 years; 100% women; 2 groups: exercise (n = 51), controls (n = 49) | Community dwellers | 12.0 |
| Kovács et al,50 2013 | Hungary | Study population:78 years; 81% women; MCI; 2 groups: exercise (n = 43), control (n = 43) | Institutionalized | 12.0 |
| Lam et al,51 2012 | Hong Kong | Study population: 78 years; 76% women; MCI; 2 groups: exercise (n = 171), controls (n = 218) | Community dwellers and institutionalized | 12.0 |
| Lam et al,52 2015 | Hong Kong | Study population: 76 years; 39% women; MCI; 4 groups: exercise (n = 147),c cognitive (n = 145), cognitive-physical (n = 132), control (n = 131)c | Community dwellers | 12.0 |
| Lord et al,53 1995 | Australia | Study population: 72 years; 100% women; 2 groups: exercise (n = 100), control (n = 97) | Community dwellers | 12.0 |
| Lord et al,35 2003 | Australia | Study population: 80 years; 86% women; 2 groups: exercise (n = 280), controls (n = 271) | Institutionalized | 12.0 |
| Liu-Ambrose et al,27 2010b | Canada | Study population: 70 years; 100% women; 3 groups: 2 weekly RT sessions (n = 52)c,e, 1 weekly RT session, balance training control (n = 49)c,e | Community dwellers | 12.0 |
| MacRae et al,68 1994 | United States | Study population: 71 years; 82% women; 2 groups: exercise (n = 49), control (n = 48) | Senior centers | 12.0 |
| Merom et al,36 2016 | Australia | Study population: 78 years; 85% women; 2 groups: exercise (n = 279), control (n = 251) | Institutionalized | 12.0 |
| Messier et al,40 2013 | United States | Study population: 66 years; 72% women; 3 groups: exercise only (n = 150), exercise + diet (n = 152)c, diet (n = 152)c | Community dwellers | 18.0 |
| Munro et al,30 2004 | United Kingdom | Study population: 75.4 years; 67% women; 2 groups: exercise (n = 2283), control (n = 4137) | Community dwellers | 24.0 |
| Muscari et al,28 2010b | Italy | Study population: 69 years; 52% women; 2 groups: exercise (n = 60), control (n = 60) | Community dwellers | 12.0 |
| Mustata et al,41 2011 | Canada | Study population: 68 years; 55% women; chronic kidney disease; 2 groups: exercise (n = 10), controls (n = 10) | Community dwellers | 12.0 |
| Nowalk et al,26 2001b | United States | Study population: 86 years; 85% women; 3 groups: exercise (n = 37),c tai-chi (n = 38), control (n = 35) | Institutionalized | 24.0 |
| Pahor et al,54 2006 | United States | Study population: 77 years; 69% women, 2 groups: exercise (n = 213), control (n = 211) | Community dwellers | 12.0 |
| Pahor et al,10 2014 | United States | Study population: 79 years; 67% women; 2 groups: exercise (n = 818), control (n = 817) | Community dwellers | 31.2 |
| Park et al,55 2008 | South Korea | Study population: 68 years; 100% women; 2 groups: exercise (n = 25), control (n = 25) | Community dwellers | 12.0 |
| Patil et al,56 2015f | Finland | Study population: 74 years, 100% women; 4 groups: exercise (n = 205), control (n = 204) | Community dwellers | 24.0 |
| Pitkälä et al,57 2013 | Finland | Study population: 78 years; 81% women; Alzheimer disease; 3 groups; home-based (n = 70)g, group-based exercise (n = 70), control (n = 70)g | Community dwellers | 12.0 |
| Prescott et al,58 2008 | Denmark | Study population: 68 years; 21% women; chronic heart failure; 2 groups: exercise (n = 36), control (n = 30) | Community dwellers | 14.0 |
| Reinsch et al,67 1992 | United States | Study population: 75 years, 80% women; 4 groups: exercisec (n = 57), cognitive (n = 51), exercise + cognitive (n = 72), controls (n = 50)c | Community dwellers | 12.0 |
| Rejeski et al,38 2017 | United States | Study population: 67 years, 71% women; overweight/obesity; 3 groups: WL+aerobic (n = 86), WL+RT (n = 81)d, controls (n = 82)d | Community dwellers | 18.0 |
| Rolland et al,33 2007 | France | Study population: 83 years; 75% women; Alzheimer disease; 2 groups: exercise (n = 67), controls (n = 67) | Institutionalized | 12.0 |
| Sherrington et al,39 2014 | Australia | Study population: 81 years; 74% women; 2 groups: exercise (n = 171), controls (n = 169) | Community dwellers | 12.0 |
| Suzuki et al,29 2012b | Japan | Study population: 76 years; 46% women; MCI; 2 groups: exercise (n = 25), controls (n = 25) | Community dwellers | 12.0 |
| Underwood et al,32 2013 | United Kingdom | Study population: 87 years; 76% women; 2 groups: exercise (n = 398), controls (n = 493) | Institutionalized | 12.0 |
| van Uffelen et al61 2008 | Netherlands | Study population: 75 years; 37% women; MCI; 2 groups: exercise (n = 86), controls (n = 93) | Community dwellers | 12.0 |
| Villareal et al,62 2011 | United States | Study population: 70 years; 63% women; Obese; 4 groups: diet (n = 26), exercise (n = 26)c, diet + exercise (n = 28), controls (n = 27)c | Community dwellers | 12.0 |
| Von Stengel et al,37 2011 | Germany | Study population: 69 years; 100% women; 3 groups: exercise + whole-body vibration (n = 50), exercise (n = 50)c, controls (n = 51)c | Community dwellers | 18.0 |
| Voukelatos et al,63 2015 | Australia | Study population: 73 years; 74% women; 2 groups: exercise (n = 192), controls (n = 194) | Community dwellers | 12.0 |
| Winters-Stone et al,64 2011b | United States | Study population: 62 years; 100% women; breast cancer survivors; 2 groups: exercise (n = 52), controls (n = 54) | Community dwellers | 12.0 |
| Wolf et al,65 2003 | United States | Study population 81 years; 86% women; 2 groups: exercise (n = 158), controls (n = 153) | Institutionalized | 12.0 |
| Woo et al,66 2007 | Hong Kong | Study population: 69 years; 50% women; 3 groups: exercise (n = 60),d controls (n = 60), Tai Chi (n = 60) | Community dwellers | 12.0 |
Abbreviations: MCI, mild cognitive impairment; RT, resistance training; WL, weight loss.
Study setting was not clearly mentioned in this study. We assume that these are community dwellers.
No data available for the quantitative analysis (not usable data or no event occurring in both exercisers and controls), but the articles were included in the qualitative analysis.
These study groups were selected for the meta-analyses.
We selected the exercise group with the highest attendance.
We selected the exercise group with highest frequency.
We used data from combined exercise groups (exercise alone and exercise plus vitamin D supplementation) vs combined nonexercise groups (vitamin D supplementation and placebo) because original investigators indicated no interaction was found between the use of vitamin D and exercise.
We selected the home-based exercise group instead of the group-base exercise group because the former had higher exercise adherence.
As for any behavioral intervention, most trials had a high risk of bias related to blinding participants. The risk of concealment allocation was mostly unclear (n = 24), whereas incomplete data (n = 15) and blinding of outcome assessors (n = 11) may have been an issue for several studies (Supplement).
The most used exercise was a multicomponent training (multiple exercises; eg, aerobic plus strength plus balance training; 29 RCTs), followed by aerobic (8 RTCs)23,24,28,41,46,49,61,63 and strength (5 RTCs)27,31,38,48,64 training (Supplement). Exercise regimen was: mean frequency of 3 times per/week, about 50 minutes per session, at a moderate intensity (n = 35 RCTs). Average compliance was about 65%. Group-based supervised (n = 29) and a mix of group-based supervised and home-based unsupervised exercises (n = 12) were the most common format of exercise delivery. Comparator groups were often active controls, ranging from attention controls to more intensive interventions (eg, stent angioplasty). Thirteen trials had more than two study arms,26,27,31,37,38,40,48,52,56,57,62,66,67 all of them with two exercise groups except two studies,27,48 which had three exercise groups. All exercise arms in these studies have been scrutinized qualitatively. ICC values32,60 for mortality (ICC = 0.001) and fractures (ICC = 0.03) applied for cluster-RCTs performed in long-term care facilities (LTCF). No other suitable ICC values were found.
Original investigators of 28 studies were contacted; 18 responded, and 9 provided new data and/or information.
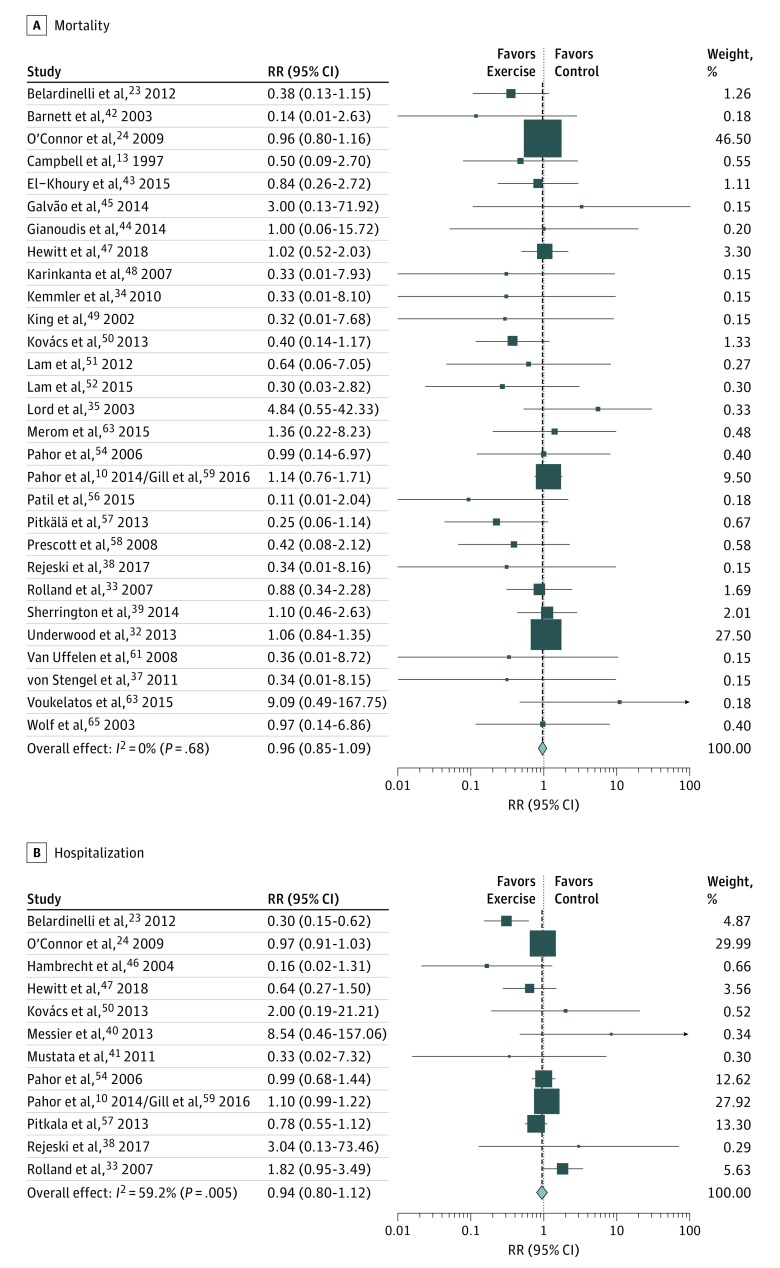
Mortality
Thirty-nine studies10,13,23,24,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,54,56,57,58,61,62,63,64,65 provided available information on death for 19 670 participants. Among them, 8 studies27,28,29,40,41,46,62,64 had no deaths during the trial. Twenty-nine RCTs10,13,23,24,32,33,34,35,36,37,38,39,42,43,44,45,47,48,49,50,51,52,54,56,57,58,61,63,65 were included in the primary analysis (2 excluded owing to low compliance),30,31 totaling 11 441 participants in the model; 406 of 5677 (7.1%) and 453 of 5764 (7.9%) people died in the exercise and control groups, respectively. Figure 1A10,13,23,24,32,33,34,35,37,38,39,42,43,44,45,47,48,49,50,51,52,54,56,57,58,61,63,65 displays the forest plot of the effects of exercise on mortality. Exercise had no effects on mortality (P = .51). Heterogeneity was low (I2 = 0%) and Egger’s test suggested no important asymmetry (P = .76). The funnel plot (Supplement) suggested the presence of some bias, with small studies presenting inflated RRs (exercisers at increased risk of death). All sensitivity analyses provided similar results (Supplement), except analysis restricted to clinically specific or disease-specific populations, which found that exercise tended to reduce the risk of mortality (10 RCTs; RR, 0.70; 95% CI, 0.49-1.00; P = .05; I2 = 15%). Meta-regressions found associations for exercise frequency of 3 times per week compared with 2 or fewer times per week (exp[b], 0.42; standard error [SE], 0.14; P = .01) and effective frequency of between 2 and 3 times per week compared with fewer than 2 times per week (exp[b], 0.35; SE, 0.15; P = .03) with a reduced mortality risk. All the other meta-regressions found nonsignificant associations.
Figure 1. Association of Exercise on the Risk of Mortality and Hospitalization.
Association of exercise with risk of mortality (A) and hospitalization (B). Weights are from random effects analysis.
Hospitalization
Fourteen studies10,23,24,30,32,33,38,40,41,46,47,50,54,57 had investigated hospitalization, but 1 RCT32 had no usable data on the number of people hospitalized; in this trial, exercisers and controls did not differ in terms of mean hospitalizations (0.87 vs 0.74, respectively). From the remaining thirteen studies (12 059 participants), 12 (5639 participants) entered into the primary analysis (1 exclusion owing to low compliance30): 1242 of 2822 (44%) and 1257 of 2817 (44.6%) people have been hospitalized in the exercise and control groups, respectively. Figure 1B23,24,33,38,40,41,46,47,50,54,57,59 shows that exercise has not reduced the risk of being hospitalized (P = .51), but heterogeneity was substantial (I2 = 59.2%). Even though the Egger’s test (P = .39) did not have evidence of small study effects, the funnel plot (Supplement) showed some asymmetry, with small studies having exaggerated large RR (increased risk of hospitalization among exercisers). Sensitivity and subgroup analyses (Supplement) provided unchanged nonsignificant findings. All meta-regressions provided nonsignificant associations of exercise variables with the risk of being hospitalized (Supplement).
Fallers and Fallers With Multiple Falls
Twenty-eight studies13,25,26,31,33,34,35,36,37,38,39,40,41,42,43,44,47,48,50,53,55,56,57,63,65,66,67,68 investigated falls; 7 had no usable information on the number of fallers,25,26,33,34,36,37,38 with 5 studies finding nonsignificant differences in number of falls across study groups, 134 showing significant effects favoring the exercise group, and 1 having no event across groups.38 Twenty-one studies contributed information on the number of fallers for 5220 participants. Of the 4420 people included in the primary analysis (20 RCTs13,35,39,40,41,42,43,44,47,48,50,53,55,56,57,63,65,66,67,68; 1 excluded31 owing to low compliance), 951 of 2207 (43.1%) and 1066 of 2213 (48.2%) became a faller in the exercise and control groups, respectively. As shown in Figure 2A,13,35,39,40,41,42,43,44,47,48,50,53,55,56,57,63,65,66,67,68 exercisers had a reduced risk of 12% to become a faller compared with controls (P = .02); heterogeneity was moderate (I2 = 50.7%). Although the Egger’s test did not evidence small study effects (P = .92), the funnel plot (Supplement) showed some asymmetry, with small studies having exaggeratedly large RRs (increased risk to be a faller in the exercise group). Sensitivity and subgroup analyses (Supplement) provided similar findings, with RRs for exercisers varying from 0.81 to 0.91, even if most of them did not reach statistical significance. All meta-regressions provided nonsignificant associations, except that exercise frequency (exp[b], 1.35; SE, 0.19; P = .05) as well as effective frequency (exp[b], 1.60; SE, 0.25; P = .01) more than 3 times per week were associated with increased risk of becoming a faller.
Figure 2. Association of Exercise on the Risk of Becoming a Faller and a Faller With Multiple Falls.
Association of exercise with risk of becoming a faller (A) and becoming a multiple faller (B). Weights are from random effects analysis.
For fallers of multiple falls, 13 studies (3060 participants)13,35,39,42,44,47,48,50,53,56,63,65,67 composed the primary analysis: 329 of 1526 (21.5%) and 374 of 1534 (24.4%) individuals have fallen at least twice in the exercise and control groups, respectively. Exercise had no significant effect (Figure 2B)13,35,39,42,44,47,48,50,53,56,63,65,67 in decreasing the risk of being a faller with multiple falls (P = .20); heterogeneity was moderate (I2 = 60.2%). Egger’s test did not find small study effects (P = .96), but the funnel plot (Supplement) showed that small studies had inflated RRs (increased risk to be a multiple faller in the exercise group). Sensitivity analysis provided similar results. Meta-regressions found no significant associations.
Injurious Fallers
Fourteen RCTs13,37,38,39,40,41,42,43,47,56,57,59,67,68 provided information on injurious falls, with 2 having no usable data for meta-analysis. These 2 studies found mixed results, with 1 showing more falls39 and the other37 reporting an average number of falls lower in exercisers compared with controls. Twelve RCTs gave data for 4972 participants, with 3 trials38,40,41 having no injurious fallers. Nine studies (n = 4481)13,42,43,47,56,57,59,67,68 composed the primary analysis, with 370 of 2192 (16.9%) and 471 of 2289 (20.6%) injurious fallers in the exercise and control groups, respectively. As displayed in Figure 3A,13,42,43,47,56,57,59,67,68 exercisers had a reduced risk of 26% to becoming injurious fallers compared with controls (P = .001); heterogeneity was moderate, but not substantial (I2 = 40%). Egger’s test (P = .22) and the funnel plot (Supplement) did not evidence any substantial asymmetry, even if there was a lack of small-to-medium scale studies collecting information on injurious falls (suggesting potential publication bias). All sensitivity and subgroup analyses (Supplement) provided unchanged results (except analysis restricted to disease-specific population; 1 RCT), with significant RRs favoring exercisers (range, 0.74-0.79). All 9 studies included in the primary analysis have operationalized a moderate-intensity, multicomponent training comprising balance exercises.
Figure 3. Association of Exercise on the Risk of Becoming an Injurious Faller and Sustaining a Fracture.
Association of exercise with risk of becoming an injurious faller (A) and sustaining a fracture (B). Weights are from random effects analysis.
Fractures
Twenty-three RCTs10,23,24,31,32,33,34,37,38,39,40,41,43,44,47,48,50,51,56,57,62,65,67 had information on fractures for 9701 individuals. Nineteen trials10,23,24,32,33,34,37,39,43,44,47,48,50,51,56,57,62,65,67 (no events occurred in 3 trials38,40,41 and 1 study was excluded owing to low compliance31) were entered into the primary analysis (8410 participants): 221 of 4138 (5.3%) and 270 of 4272 (6.3%) people in the exercise and control groups, respectively, have sustained a fracture. Figure 3B10,23,24,32,33,34,37,39,43,44,47,48,50,51,56,57,62,65,67 shows that exercise was not effective in reducing the number of fractures (P = .054). Heterogeneity was low (I2 = 0%), and the Egger’s test (P = .34) and funnel plot (Supplement) did not evidence any substantial asymmetry. Sensitivity analysis using a fixed-effect model found a significant effect of exercise for reducing the number of people with fractures by 16% (RR, 0.84; 95% CI, 0.70-1.00; P = .047). Excluding studies for which we assumed the number of fractures was equivalent to the number of people sustaining a fracture provided similar results (RR, 0.85; 95% CI, 0.71-1.03; P = .10). All the other analysis (Supplement) provided similar findings (favoring exercisers without reaching statistical significance). Meta-regressions found no significant association of exercise-related variables with this outcome.
Discussion
This systematic review and meta-analysis showed that long-term exercise had modest but significant association with reduced risk of becoming a faller and an injurious faller, but not a faller with multiple falls, in older adults. Moreover, exercise was associated with a nonsignificant reduction in the risk of sustaining a fracture. Exercise benefits occurred without increasing the risk of mortality and hospitalization.
This is the first meta-analysis focusing on the benefits of long-term exercise (≥1 year), which may potentially lead to longer-term positive effects, against major adverse events in older adult populations. Our findings corroborate the results of recent meta-analyses focusing on falls that showed exercise (any intervention length) benefited several fall-related outcomes.7,8,9,16,69 The magnitude of associations for the risk of becoming a faller in our study (RR, 0.88; 95% CI, 0.80-0.98) was small but consistent with those (RR, 0.89; 95% CI, 0.81-0.97 and RR, 0.83; 95% CI, 0.70-0.99) recently reported by Guirguis-Blake et al69 and Tricco et al,16 respectively; the similarities in the findings across these meta-analyses represents compelling evidence of the positive effects of exercise against fall-related outcomes because in the present work we have used different eligibility criteria (particularly regarding intervention length ≥1 year), leading, then, to the inclusion of different studies. Furthermore, our study further extends current knowledge by examining for the first time the association of exercise with the risk of being a faller with multiple falls: we did not evidence a positive association of exercise with this outcome. However, multiple falls were not reported in some of the largest, well-conducted original studies (because it was not an endpoint of those RCTs) that provided data on fallers and injurious fallers,43,59 resulting in a small number of participants in the analysis; this issue, alongside the asymmetry found in the funnel plot, suggest publication bias could have affected estimations. For injurious fallers, we provide herein the most comprehensive evidence on the topic, gathering information from more than 4000 people in 9 RCTs, going beyond previous meta-analyses16,43,69; we consistently (across sensitivity and subgroup analysis) found that exercise decreased the risk of injurious falls by about 26%. Regarding fractures, our study contributes to this still not well-established field by showing that exercise seems to protect against fractures; although the primary finding was not statistically significant, the absence of both heterogeneity across studies and asymmetry (small study effects and publication bias), alongside the positive results from the fixed effect, suggest that long-term exercise might lead to a reduction in the risk of fractures. Even though we overcame a major issue of previous meta-analyses,2,11,12,16,69 which have included only a small number of studies and participants, analysis incorporating data from future well-conducted long-term RCTs is still needed before solid conclusions can be drawn on the protective effects of exercise against fractures in older adults. To our knowledge, our study is the largest meta-analysis ever done on the association of long-term exercise with mortality and the first one reporting about the association of exercise with hospitalization in older populations. Exercise had no statistically significant association with mortality or hospitalizations, which corroborates the mortality findings of Guirguis-Blake et al69; this may mean that mortality and hospitalizations are difficult-to-change outcomes, probably because they are determined by multidimensional parameters that may be beyond the scope of exercise-induced benefits. Lack of power may also have affected our results for mortality. Importantly, exercise tended to decrease mortality risk in clinical populations (mostly people with cognitive decline or cardiac disease), which reinforces the role of exercise as a core therapeutic element for treating prevalent diseases in older people.
Meta-regressions found that vigorous-intensity is as safe as moderate-intensity exercise. Exercise frequency of between twice and thrice a week was associated with decreased mortality, whereas more than 3 times per week was associated with increased risk of being a faller; therefore, the best exercise frequency seems to be 2 to 3 times per week, lower frequencies probably resulting in less effective outcomes whereas higher frequencies would augment the risk of adverse events. The association between exercise frequency and risk of becoming faller might be dependent on the fall-related vulnerability of the population, with higher risks in more vulnerable participants70; indeed, among studies with exercise frequency of 4 or more times per week, whereas Sherrington et al39 showed a higher risk of being a faller in the exercise group in people at increased risk of falling (mean age about 81 years, about 70% had fallen in the past 12 months), Kemmler et al34 found that exercise reduced fall rates in a population at lower risk for falls (young women aged on average 69 years) and Von Stengel et al37 found a trend in fall rates favoring exercisers in a similar low-risk population. It is possible that the dose-response idea implying that “more exercise is always better” might not fully apply for the most vulnerable older adults. The potential mechanisms involved require further investigation, but it could be related to overtraining: excessive exercise leads to diminished immunity and energy metabolism according with animal models71 and is associated with reduced calorie intake, worse sleep, and negative psychological patterns in young and middle-aged adults.72 Our findings on the best exercise frequency, alongside the observation that all RCTs included in the injurious falls analysis had a similar exercise structure, suggests that the best exercise regimen for protecting older people against diverse adverse events would be moderate-intensity, multicomponent training comprising balance exercises, performed 2 to 3 times per week; a session duration of 30 to 60 minutes (average of 50 minutes, according to studies on injurious falls analysis) should be safe and effective.
Limitations
This review has limitations. First, several studies have not clearly reported exercise adherence, which impeded us to calculate the exact exercise volume performed by participants. Second, for examining the effects of long-term exercise, we arbitrarily established the 1-year length as the minimum intervention follow-up, which could lead to losing important studies that employed shorter follow-ups. A longer follow-up length would probably result in more precise data, particularly on less frequent events such as fractures, but it would have undermined the feasibility of the meta-analysis by reducing the number of eligible studies to 13. Third, owing to the several analyses performed, multiplicity may have elevated the chances of type I error. Finally, a high heterogeneity in terms of study population was found (from people with Alzheimer disease to overall healthy participants), but the small number of studies for most outcomes prevented us from performing stringent subgroup analysis. In an attempt to reduce such a bias, we performed subgroup analyses separately for populations with and without clinically and disease-specific profiles.
Conclusions
Exercise is associated with a modest decrease in the risk of becoming a faller, an injurious faller, and potentially sustaining a fracture in older adults. Exercise should be performed 2 to 3 times per week. Studies showing positive effects of exercise for reducing the risk of becoming an injurious faller operationalized moderate intensity, multicomponent training with balance exercises (eg, balance, strength training for the lower limbs, and aerobic exercise [eg, walking]), for about 50 minutes per session.
eAppendix 1. Study Protocol
eAppendix 2. Electronic Searches
eAppendix 3. Flow Chart of Study Selection
eAppendix 4. Risk of Bias
eAppendix 5. Description of Exercise Interventions
eAppendix 6. Meta-analyses and Meta-regressions for the Outcome “Mortality”
eAppendix 7. Meta-analyses and meta-regressions for the outcome “Number of people hospitalized
eAppendix 8. Meta-analyses and meta-regressions for the outcome “Fallers”
eAppendix 9. Meta-analyses and meta-regressions for the outcome “Fallers with multiple falls”
eAppendix 10. Meta-analyses for the outcome “Injurious fallers”
eAppendix 11. Meta-analyses and meta-regressions for the outcome “People with fractures”
eAppendix 12. Number of participants and events included in the main analysis per study and per outcome
References
- 1.Chodzko-Zajko WJ, Proctor DN, Fiatarone Singh MA, et al. ; American College of Sports Medicine . American College of Sports Medicine position stand: Exercise and physical activity for older adults. Med Sci Sports Exerc. 2009;41(7):1510-1530. doi: 10.1249/MSS.0b013e3181a0c95c [DOI] [PubMed] [Google Scholar]
- 2.Howe TE, Shea B, Dawson LJ, et al. Exercise for preventing and treating osteoporosis in postmenopausal women. Cochrane Database Syst Rev. 2011;(7):CD000333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Giné-Garriga M, Roqué-Fíguls M, Coll-Planas L, Sitjà-Rabert M, Salvà A. Physical exercise interventions for improving performance-based measures of physical function in community-dwelling, frail older adults: a systematic review and meta-analysis. Arch Phys Med Rehabil. 2014;95(4):753-769.e3. doi: 10.1016/j.apmr.2013.11.007 [DOI] [PubMed] [Google Scholar]
- 4.Jadczak AD, Makwana N, Luscombe-Marsh N, Visvanathan R, Schultz TJ. Effectiveness of exercise interventions on physical function in community-dwelling frail older people: an umbrella review of systematic reviews. JBI Database System Rev Implement Rep. 2018;16(3):752-775. doi: 10.11124/JBISRIR-2017-003551 [DOI] [PubMed] [Google Scholar]
- 5.Young J, Angevaren M, Rusted J, Tabet N. Aerobic exercise to improve cognitive function in older people without known cognitive impairment. Cochrane Database Syst Rev. 2015;(4):CD005381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kelly ME, Loughrey D, Lawlor BA, Robertson IH, Walsh C, Brennan S. The impact of exercise on the cognitive functioning of healthy older adults: a systematic review and meta-analysis. Ageing Res Rev. 2014;16:12-31. doi: 10.1016/j.arr.2014.05.002 [DOI] [PubMed] [Google Scholar]
- 7.El-Khoury F, Cassou B, Charles M-A, Dargent-Molina P. The effect of fall prevention exercise programmes on fall induced injuries in community dwelling older adults: systematic review and meta-analysis of randomised controlled trials. BMJ. 2013;347:f6234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gillespie LD, Robertson MC, Gillespie WJ, et al. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2012;(9):CD007146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sherrington C, Michaleff ZA, Fairhall N, et al. Exercise to prevent falls in older adults: an updated systematic review and meta-analysis. Br J Sports Med. 2017;51(24):1750-1758. doi: 10.1136/bjsports-2016-096547 [DOI] [PubMed] [Google Scholar]
- 10.Pahor M, Guralnik JM, Ambrosius WT, et al. ; LIFE study investigators . Effect of structured physical activity on prevention of major mobility disability in older adults: the LIFE study randomized clinical trial. JAMA. 2014;311(23):2387-2396. doi: 10.1001/jama.2014.5616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Silva RB, Eslick GD, Duque G. Exercise for falls and fracture prevention in long term care facilities: a systematic review and meta-analysis. J Am Med Dir Assoc. 2013;14(9):685-9.e2. doi: 10.1016/j.jamda.2013.05.015 [DOI] [PubMed] [Google Scholar]
- 12.Kemmler W, Häberle L, von Stengel S. Effects of exercise on fracture reduction in older adults: a systematic review and meta-analysis. Osteoporos Int. 2013;24(7):1937-1950. doi: 10.1007/s00198-012-2248-7 [DOI] [PubMed] [Google Scholar]
- 13.Campbell AJ, Robertson MC, Gardner MM, Norton RN, Tilyard MW, Buchner DM. Randomised controlled trial of a general practice programme of home based exercise to prevent falls in elderly women. BMJ. 1997;315(7115):1065-1069. doi: 10.1136/bmj.315.7115.1065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group . Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. doi: 10.1136/bmj.b2535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cameron ID, Gillespie LD, Robertson MC, et al. Interventions for preventing falls in older people in care facilities and hospitals. Cochrane Database Syst Rev. 2012;12:CD005465. [DOI] [PubMed] [Google Scholar]
- 16.Tricco AC, Thomas SM, Veroniki AA, Hamid JS, Cogo E, Strifler L, et al. Comparisons of interventions for preventing falls in older adults: a systematic review and meta-analysis. JAMA. 2017;318(17):1687-1699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Higgins JPT, Altman DG, Gøtzsche PC, et al. ; Cochrane Bias Methods Group; Cochrane Statistical Methods Group . The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. doi: 10.1136/bmj.d5928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177-188. doi: 10.1016/0197-2456(86)90046-2 [DOI] [PubMed] [Google Scholar]
- 19.Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557-560. doi: 10.1136/bmj.327.7414.557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Health Services Research Unit University of Aberdeen. Database of ICCs:Spreadsheet (Empirical estimates of ICCs from changing professional practice studies). Disponible sur: http://www.abdn.ac.uk/hsru/research/research-tools/study-design. Accessed October 29, 2013.
- 21.Elley CR, Kerse N, Chondros P, Robinson E. Intraclass correlation coefficients from three cluster randomised controlled trials in primary and residential health care. Aust N Z J Public Health. 2005;29(5):461-467. doi: 10.1111/j.1467-842X.2005.tb00227.x [DOI] [PubMed] [Google Scholar]
- 22.Ukoumunne OC, Gulliford MC, Chinn S, Sterne JA, Burney PG. Methods for evaluating area-wide and organisation-based interventions in health and health care: a systematic review. Health Technol Assess. 1999;3(5):iii-92. [PubMed] [Google Scholar]
- 23.Belardinelli R, Georgiou D, Cianci G, Purcaro A. 10-year exercise training in chronic heart failure: a randomized controlled trial. J Am Coll Cardiol. 2012;60(16):1521-1528. doi: 10.1016/j.jacc.2012.06.036 [DOI] [PubMed] [Google Scholar]
- 24.O’Connor CM, Whellan DJ, Lee KL, et al. ; HF-ACTION Investigators . Efficacy and safety of exercise training in patients with chronic heart failure: HF-ACTION randomized controlled trial. JAMA. 2009;301(14):1439-1450. doi: 10.1001/jama.2009.454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bunout D, Barrera G, Avendaño M, et al. Results of a community-based weight-bearing resistance training programme for healthy Chilean elderly subjects. Age Ageing. 2005;34(1):80-83. doi: 10.1093/ageing/afi005 [DOI] [PubMed] [Google Scholar]
- 26.Nowalk MP, Prendergast JM, Bayles CM, D’Amico FJ, Colvin GC. A randomized trial of exercise programs among older individuals living in two long-term care facilities: the FallsFREE program. J Am Geriatr Soc. 2001;49(7):859-865. doi: 10.1046/j.1532-5415.2001.49174.x [DOI] [PubMed] [Google Scholar]
- 27.Liu-Ambrose T, Nagamatsu LS, Graf P, Beattie BL, Ashe MC, Handy TC. Resistance training and executive functions: a 12-month randomized controlled trial. Arch Intern Med. 2010;170(2):170-178. doi: 10.1001/archinternmed.2009.494 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Muscari A, Giannoni C, Pierpaoli L, et al. Chronic endurance exercise training prevents aging-related cognitive decline in healthy older adults: a randomized controlled trial. Int J Geriatr Psychiatry. 2010;25(10):1055-1064. doi: 10.1002/gps.2462 [DOI] [PubMed] [Google Scholar]
- 29.Suzuki T, Shimada H, Makizako H, et al. Effects of multicomponent exercise on cognitive function in older adults with amnestic mild cognitive impairment: a randomized controlled trial. BMC Neurol. 2012;12:128. doi: 10.1186/1471-2377-12-128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Munro JF, Nicholl JP, Brazier JE, Davey R, Cochrane T. Cost effectiveness of a community based exercise programme in over 65 year olds: cluster randomised trial. J Epidemiol Community Health. 2004;58(12):1004-1010. doi: 10.1136/jech.2003.014225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dangour AD, Albala C, Allen E, et al. Effect of a nutrition supplement and physical activity program on pneumonia and walking capacity in Chilean older people: a factorial cluster randomized trial. PLoS Med. 2011;8(4):e1001023. doi: 10.1371/journal.pmed.1001023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Underwood M, Lamb SE, Eldridge S, et al. Exercise for depression in elderly residents of care homes: a cluster-randomised controlled trial. Lancet. 2013;382(9886):41-49. doi: 10.1016/S0140-6736(13)60649-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rolland Y, Pillard F, Klapouszczak A, et al. Exercise program for nursing home residents with Alzheimer’s disease: a 1-year randomized, controlled trial. J Am Geriatr Soc. 2007;55(2):158-165. doi: 10.1111/j.1532-5415.2007.01035.x [DOI] [PubMed] [Google Scholar]
- 34.Kemmler W, von Stengel S, Engelke K, Häberle L, Kalender WA. Exercise effects on bone mineral density, falls, coronary risk factors, and health care costs in older women: the randomized controlled senior fitness and prevention (SEFIP) study. Arch Intern Med. 2010;170(2):179-185. doi: 10.1001/archinternmed.2009.499 [DOI] [PubMed] [Google Scholar]
- 35.Lord SR, Castell S, Corcoran J, et al. The effect of group exercise on physical functioning and falls in frail older people living in retirement villages: a randomized, controlled trial. J Am Geriatr Soc. 2003;51(12):1685-1692. doi: 10.1046/j.1532-5415.2003.51551.x [DOI] [PubMed] [Google Scholar]
- 36.Merom D, Mathieu E, Cerin E, et al. Social dancing and incidence of falls in older adults: a cluster randomised controlled trial. PLoS Med. 2016;13(8):e1002112. doi: 10.1371/journal.pmed.1002112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.von Stengel S, Kemmler W, Engelke K, Kalender WA. Effects of whole body vibration on bone mineral density and falls: results of the randomized controlled ELVIS study with postmenopausal women. Osteoporos Int. 2011;22(1):317-325. doi: 10.1007/s00198-010-1215-4 [DOI] [PubMed] [Google Scholar]
- 38.Rejeski WJ, Ambrosius WT, Burdette JH, Walkup MP, Marsh AP. Community weight loss to combat obesity and disability in at-risk older adults. J Gerontol A Biol Sci Med Sci. 2017;72(11):1547-1553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sherrington C, Lord SR, Vogler CM, et al. A post-hospital home exercise program improved mobility but increased falls in older people: a randomised controlled trial. PLoS One. 2014;9(9):e104412. doi: 10.1371/journal.pone.0104412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Messier SP, Mihalko SL, Legault C, et al. Effects of intensive diet and exercise on knee joint loads, inflammation, and clinical outcomes among overweight and obese adults with knee osteoarthritis: the IDEA randomized clinical trial. JAMA. 2013;310(12):1263-1273. doi: 10.1001/jama.2013.277669 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mustata S, Groeneveld S, Davidson W, Ford G, Kiland K, Manns B. Effects of exercise training on physical impairment, arterial stiffness and health-related quality of life in patients with chronic kidney disease: a pilot study. Int Urol Nephrol. 2011;43(4):1133-1141. doi: 10.1007/s11255-010-9823-7 [DOI] [PubMed] [Google Scholar]
- 42.Barnett A, Smith B, Lord SR, Williams M, Baumand A. Community-based group exercise improves balance and reduces falls in at-risk older people: a randomised controlled trial. Age Ageing. 2003;32(4):407-414. doi: 10.1093/ageing/32.4.407 [DOI] [PubMed] [Google Scholar]
- 43.El-Khoury F, Cassou B, Latouche A, Aegerter P, Charles M-A, Dargent-Molina P. Effectiveness of two year balance training programme on prevention of fall induced injuries in at risk women aged 75-85 living in community: Ossébo randomised controlled trial. BMJ. 2015;351:h3830. doi: 10.1136/bmj.h3830 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gianoudis J, Bailey CA, Ebeling PR, et al. Effects of a targeted multimodal exercise program incorporating high-speed power training on falls and fracture risk factors in older adults: a community-based randomized controlled trial. J Bone Miner Res. 2014;29(1):182-191. doi: 10.1002/jbmr.2014 [DOI] [PubMed] [Google Scholar]
- 45.Galvão DA, Spry N, Denham J, et al. A multicentre year-long randomised controlled trial of exercise training targeting physical functioning in men with prostate cancer previously treated with androgen suppression and radiation from TROG 03.04 RADAR. Eur Urol. 2014;65(5):856-864. doi: 10.1016/j.eururo.2013.09.041 [DOI] [PubMed] [Google Scholar]
- 46.Hambrecht R, Walther C, Möbius-Winkler S, et al. Percutaneous coronary angioplasty compared with exercise training in patients with stable coronary artery disease: a randomized trial. Circulation. 2004;109(11):1371-1378. doi: 10.1161/01.CIR.0000121360.31954.1F [DOI] [PubMed] [Google Scholar]
- 47.Hewitt J, Goodall S, Clemson L, Henwood T, Refshauge K. Progressive resistance and balance training for falls prevention in long-term residential aged care: a cluster randomized trial of the sunbeam program. J Am Med Dir Assoc. 2018;19(4):361-369. doi: 10.1016/j.jamda.2017.12.014 [DOI] [PubMed] [Google Scholar]
- 48.Karinkanta S, Heinonen A, Sievänen H, et al. A multi-component exercise regimen to prevent functional decline and bone fragility in home-dwelling elderly women: randomized, controlled trial. Osteoporos Int. 2007;18(4):453-462. doi: 10.1007/s00198-006-0256-1 [DOI] [PubMed] [Google Scholar]
- 49.King AC, Baumann K, O’Sullivan P, Wilcox S, Castro C. Effects of moderate-intensity exercise on physiological, behavioral, and emotional responses to family caregiving: a randomized controlled trial. J Gerontol A Biol Sci Med Sci. 2002;57(1):M26-M36. doi: 10.1093/gerona/57.1.M26 [DOI] [PubMed] [Google Scholar]
- 50.Kovács E, Sztruhár Jónásné I, Karóczi CK, Korpos A, Gondos T. Effects of a multimodal exercise program on balance, functional mobility and fall risk in older adults with cognitive impairment: a randomized controlled single-blind study. Eur J Phys Rehabil Med. 2013;49(5):639-648. [PubMed] [Google Scholar]
- 51.Lam LCW, Chau RCM, Wong BML, et al. A 1-year randomized controlled trial comparing mind body exercise (Tai Chi) with stretching and toning exercise on cognitive function in older Chinese adults at risk of cognitive decline. J Am Med Dir Assoc. 2012;13(6):568.e15-568.e20. doi: 10.1016/j.jamda.2012.03.008 [DOI] [PubMed] [Google Scholar]
- 52.Lam LC-W, Chan WC, Leung T, Fung AW-T, Leung EM-F. Would older adults with mild cognitive impairment adhere to and benefit from a structured lifestyle activity intervention to enhance cognition?: a cluster randomized controlled trial. PLoS One. 2015;10(3):e0118173. doi: 10.1371/journal.pone.0118173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lord SR, Ward JA, Williams P, Strudwick M. The effect of a 12-month exercise trial on balance, strength, and falls in older women: a randomized controlled trial. J Am Geriatr Soc. 1995;43(11):1198-1206. doi: 10.1111/j.1532-5415.1995.tb07394.x [DOI] [PubMed] [Google Scholar]
- 54.Pahor M, Blair SN, Espeland M, et al. ; LIFE Study Investigators . Effects of a physical activity intervention on measures of physical performance: results of the lifestyle interventions and independence for Elders Pilot (LIFE-P) study. J Gerontol A Biol Sci Med Sci. 2006;61(11):1157-1165. doi: 10.1093/gerona/61.11.1157 [DOI] [PubMed] [Google Scholar]
- 55.Park H, Kim KJ, Komatsu T, Park SK, Mutoh Y. Effect of combined exercise training on bone, body balance, and gait ability: a randomized controlled study in community-dwelling elderly women. J Bone Miner Metab. 2008;26(3):254-259. doi: 10.1007/s00774-007-0819-z [DOI] [PubMed] [Google Scholar]
- 56.Patil R, Uusi-Rasi K, Tokola K, Karinkanta S, Kannus P, Sievänen H. Effects of a multimodal exercise program on physical function, falls, and injuries in older women: a 2-year community-based, randomized controlled trial. J Am Geriatr Soc. 2015;63(7):1306-1313. doi: 10.1111/jgs.13489 [DOI] [PubMed] [Google Scholar]
- 57.Pitkälä KH, Pöysti MM, Laakkonen M-L, et al. Effects of the Finnish Alzheimer disease exercise trial (FINALEX): a randomized controlled trial. JAMA Intern Med. 2013;173(10):894-901. doi: 10.1001/jamainternmed.2013.359 [DOI] [PubMed] [Google Scholar]
- 58.Prescott E, Hjardem-Hansen R, Dela F, Ørkild B, Teisner AS, Nielsen H. Effects of a 14-month low-cost maintenance training program in patients with chronic systolic heart failure: a randomized study. Eur J Cardiovasc Prev Rehabil. 2009;16(4):430-437. doi: 10.1097/HJR.0b013e32831e94f8 [DOI] [PubMed] [Google Scholar]
- 59.Gill TM, Pahor M, Guralnik JM, et al. Effect of structured physical activity on prevention of serious fall injuries in adults aged 70-89: randomized clinical trial (LIFE Study). BMJ. 2016;352:i254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Underwood M, Lamb SE, Eldridge S, et al. Exercise for depression in care home residents: a randomised controlled trial with cost-effectiveness analysis (OPERA). Health Technol Assess. 2013;17(18):1-281. doi: 10.3310/hta17180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.van Uffelen JGZ, Chinapaw MJM, van Mechelen W, Hopman-Rock M. Walking or vitamin B for cognition in older adults with mild cognitive impairment? a randomised controlled trial. Br J Sports Med. 2008;42(5):344-351. doi: 10.1136/bjsm.2007.044735 [DOI] [PubMed] [Google Scholar]
- 62.Villareal DT, Chode S, Parimi N, et al. Weight loss, exercise, or both and physical function in obese older adults. N Engl J Med. 2011;364(13):1218-1229. doi: 10.1056/NEJMoa1008234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Voukelatos A, Merom D, Sherrington C, Rissel C, Cumming RG, Lord SR. The impact of a home-based walking programme on falls in older people: the Easy Steps randomised controlled trial. Age Ageing. 2015;44(3):377-383. doi: 10.1093/ageing/afu186 [DOI] [PubMed] [Google Scholar]
- 64.Winters-Stone KM, Dobek J, Nail L, et al. Strength training stops bone loss and builds muscle in postmenopausal breast cancer survivors: a randomized, controlled trial. Breast Cancer Res Treat. 2011;127(2):447-456. doi: 10.1007/s10549-011-1444-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Wolf SL, Sattin RW, Kutner M, O’Grady M, Greenspan AI, Gregor RJ. Intense tai chi exercise training and fall occurrences in older, transitionally frail adults: a randomized, controlled trial. J Am Geriatr Soc. 2003;51(12):1693-1701. doi: 10.1046/j.1532-5415.2003.51552.x [DOI] [PubMed] [Google Scholar]
- 66.Woo J, Hong A, Lau E, Lynn H. A randomised controlled trial of Tai Chi and resistance exercise on bone health, muscle strength and balance in community-living elderly people. Age Ageing. 2007;36(3):262-268. doi: 10.1093/ageing/afm005 [DOI] [PubMed] [Google Scholar]
- 67.Reinsch S, MacRae P, Lachenbruch PA, Tobis JS. Attempts to prevent falls and injury: a prospective community study. Gerontologist. 1992;32(4):450-456. doi: 10.1093/geront/32.4.450 [DOI] [PubMed] [Google Scholar]
- 68.MacRae P, Feltner M, Reinsch S. A 1-year exercise program for older women: effects on falls, injuries, and physical performance. J Aging Phys Act. 2e éd. 1994;127-142. [Google Scholar]
- 69.Guirguis-Blake JM, Michael YL, Perdue LA, Coppola EL, Beil TL. Interventions to prevent falls in older adults: Updated evidence report and systematic review for the us preventive services task force. JAMA. 2018;319(16):1705-1716. [DOI] [PubMed] [Google Scholar]
- 70.Faber MJ, Bosscher RJ, Chin A Paw MJ, van Wieringen PC. Effects of exercise programs on falls and mobility in frail and pre-frail older adults: A multicenter randomized controlled trial. Arch Phys Med Rehabil. 2006;87(7):885-896. doi: 10.1016/j.apmr.2006.04.005 [DOI] [PubMed] [Google Scholar]
- 71.Yuan X, Xu S, Huang H, et al. Influence of excessive exercise on immunity, metabolism, and gut microbial diversity in an overtraining mice model. Scand J Med Sci Sports. 2018;28(5):1541-1551. doi: 10.1111/sms.13060 [DOI] [PubMed] [Google Scholar]
- 72.Cadegiani FA, Kater CE. Body composition, metabolism, sleep, psychological and eating patterns of overtraining syndrome: results of the EROS study (EROS-PROFILE). J Sports Sci. 2018;36(16):1902-1910. doi: 10.1080/02640414.2018.1424498 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eAppendix 1. Study Protocol
eAppendix 2. Electronic Searches
eAppendix 3. Flow Chart of Study Selection
eAppendix 4. Risk of Bias
eAppendix 5. Description of Exercise Interventions
eAppendix 6. Meta-analyses and Meta-regressions for the Outcome “Mortality”
eAppendix 7. Meta-analyses and meta-regressions for the outcome “Number of people hospitalized
eAppendix 8. Meta-analyses and meta-regressions for the outcome “Fallers”
eAppendix 9. Meta-analyses and meta-regressions for the outcome “Fallers with multiple falls”
eAppendix 10. Meta-analyses for the outcome “Injurious fallers”
eAppendix 11. Meta-analyses and meta-regressions for the outcome “People with fractures”
eAppendix 12. Number of participants and events included in the main analysis per study and per outcome