Abstract
To examine the impact of moderate to vigorous intensity physical activity (MVPA) trajectories during midlife and older adulthood with subsequent fall risk in later life. Cross-temporal analyses were conducted in 15,792 participants (27% black, 55% women) aged 45 to 64 years enrolled in the Atherosclerosis Risk in Communities (ARIC) Study. MVPA was collected at Exams 1 (1987–89), 3 (1993–95) and 5 (2011–13) using the ARIC/Baecke questionnaire. Latent class growth analysis was used to identify the MVPA trajectory groups. Reported falls outcomes were collected in 2013–14, 2015–16, and 2016–17. Generalized Linear Models were used to estimate associations of baseline predictors with trajectory class membership, as well as associations of trajectory classes with any falling (adjusted incident relative risks, aIRR) and with number of falls (adjusted relative rates, aRR). Four primary trajectory classes emerged, reflecting longitudinal patterns of maintained high (48%), maintained low (22%), increasing (14%) and decreasing (15%) MVPA. After adjustment for covariates, the decreasing MVPA trajectory group had a 14% higher risk of reporting any falling compared to the maintained high MVPA group [aIRR=1.14 (1.01, 1.28)]. When compared to the maintained high MVPA group, the maintained low and decreasing group had a 28% [aRR=1.28 (1.14, 1.44)] and 27% [aRR=1.27 (1.17, 1.38)] higher rate in the reported number of falls, respectively. Findings support public health campaigns targeting habitual MVPA or exercise for fall prevention and suggest that interventions should be initiated in midlife; a time when individuals may be more able and willing to change behavior.
Keywords: exercise, falls, cohort study, midlife
INTRODUCTION
Substantial evidence has accumulated regarding the numerous health benefits of habitual moderate to vigorous intensity physical activity (MVPA) during leisure-time or exercise, including reducing risk of fall related outcomes in older adulthood.1,2 Yet, other studies have demonstrated a u-shaped relation between physical activity and fall risk, whereby more active individuals may be at an increased risk due simply to greater exposure time or opportunity to fall when active.3–6 Regardless, the 2018 Physical Activity Guidelines Advisory Committee concluded that exercise programs targeting fall prevention were effective among community dwelling older adults in reducing the risk of fall related injuries by 32–40% and bone fractures by 40–66%.1,7–9 As a result of these supportive findings, several organizations (e.g., American Geriatric Society10,11) and public health resources (e.g., Centers for Disease Control and Prevention (CDC) Compendium of Effective Fall Interventions: What Works For Community Dwelling Older Adults12 and the National Institute on Aging’s Go4Life public health campaign13) promote physical activity as a key fall prevention strategy. Yet, several questions regarding the complex association between physical activity and falls remain largely unexplored, including the influence of changes in midlife MVPA on subsequent risk of falls using a life-course framework.
Functional decline and the subsequent risk for disability begins in midlife.2 Similar to approaches used to reduce lifetime risk of cardiovascular disease and cancer14,15, strategies to promote MVPA during midlife could complement exercise programming that primarily targets an older adult population to reduce risk of falls. While the existing evidence base generally supports the beneficial effect of MVPA on risk of falls1,7–9, these studies have primarily utilized an older adult population16, with findings that may be influenced by reverse causality. Therefore, the importance of being physically active in midlife and the cumulative exposure of MVPA from midlife to older adulthood with subsequent risk of falls in later life is largely unknown. Further, midlife may correspond to a time during the life-course when individuals may be more willing and physically able to initiate a regular MVPA routine given changes in life circumstances (e.g., retirement)17 and the higher burden of disease and disability that is often more characteristic of older adulthood.
With longitudinal physical activity data that characterizes leisure-time MVPA across the midlife to older adulthood transition and the availability of falls data collected in later life, the Atherosclerosis Risk in Communities (ARIC) Study is uniquely positioned to provide novel information regarding the role of life-course changes in MVPA on subsequent risk of falls, rather than physical activity changes that result from an intervention that is being tested within the context of a randomized controlled trial. Therefore, the purpose of this study is to examine the impact of MVPA trajectories during midlife and older adulthood with subsequent fall outcomes in later life, including any falling and number of falls.
MATERIALS AND METHODS
Design Overview and Participants
The ARIC Study design and objectives have been described in detail.18 Briefly, ARIC included 15,792 adults aged 45 to 64 years at the Visit 1 examination (henceforth: Exam 1 or baseline; 1987–89). Male and female participants were recruited from defined populations in four field centers, including Forsyth County, NC, Jackson, MS (black participants, only), Minneapolis suburbs, MN, and Washington County, MD. Follow-up of the ARIC cohort is on-going and includes cohort exam visits and annual or semi-annual telephone calls. For this analysis, participants include those who completed Exam 1 (1987–89) and follow-up telephone surveys in 2013–14, 2015–16, and 2016–17 which included questions on falls. Information for MVPA trajectories was available from Exam 1 (1987–1989), Exam 3 (1993–95), and Exam 5 (2011–13). All ARIC participants provide informed consent and institutional review boards at each participating field center have approved the study.
Data Collection
Participant Characteristics and Anthropometric Measures
Standardized questionnaires were used at Exam 1 to assess participant characteristics including: age, socio-demographic factors (e.g., educational attainment), health behaviors (e.g., physical activity, sedentary behavior, smoking status, and television viewing), self-rated health, and prevalent chronic disease. In addition, height (stadiometer) and weight (balance-beam scale) were measured with the participant lightly clothed and without shoes.19 Body mass index (BMI) was calculated as weight (kg) divided by height squared (m2). Prevalent chronic disease included type 2 diabetes (fasting glucose ≥ 126 md/dL, non-fasting glucose ≥ 200, use of diabetes medication or self-report physician diagnosis), hypertension [mean of the second and third measurements (of three): systolic ≥140 mmHg and/or diastolic ≥ 90 mmHg or use of antihypertensive medications], and cardiovascular diseases (self-report physician diagnosis). Exam 1 measures were included in multivariable models as covariates given our study objective to predict subsequent risk of falls in later life; a strategy that reduces the biases associated with non-response and reverse causation that can be limitations of the prospective cohort study design.
Exposure: Moderate to Vigorous Intensity Physical Activity
A modified version of the Baecke Questionnaire was used to assess past year physical activity in ARIC.20,21 The ARIC version of the Baecke consists of the following three components: sports and exercise, leisure, and work. For these analyses, items from the sports and exercise index were used to derive the trajectory classes, which provides quantitative information related to higher intensity, structured physical activity during discretionary periods of the day (i.e., leisure-time domain). This type of physical activity is also reflective of behavioral targets included in fall prevention exercise programs or interventions.12 Briefly, participants were asked to report up to four sport or exercise activities performed most frequently. For each sport reported, additional information on the duration and frequency (hours per week and months per year) were recorded via response categories. While the sports and exercise component is traditionally reported as an index score, ranging from 1 (low active) to 5 (high active), for this analysis, data were re-scored by taking the product of the duration and frequency weighted by the metabolic equivalent of task (MET)22 that corresponds to each of the reported activity types. These activity specific estimates in MET min wk−1 were then summed across all reported activity types to derive the final MVPA summary score (also expressed as MET min wk−1).22 MVPA trajectory classes from midlife to older adulthood were estimated using the sports and exercise summary scores from Exams 1, 3, and 5.
Outcome: Falls
Information on falls was collected during three follow-up telephone calls (2013–14, 2015–16, and 2016–17) used for ongoing surveillance of the cohort. A fall was defined as unintentionally coming to rest on the ground, floor, or other level lower than one’s starting point.3,23,24 Participants were asked whether they experienced a fall (yes/no) in the previous six months (2013–14) or twelve months (2015–16 and 2016–17) and, if so, reported the total number of falls (up to six or more). The falls questions were included for the first time in the semi-annual follow-up call and utilized a six month recall time frame. This was revised to a twelve month recall time frame in subsequent administrations to be consistent with the question structure used in the Behavioral Risk Factor Surveillance System to facilitate comparability with a nationally representative sample of U.S. adults. A binary “any falling” outcome was assigned the value of 1 to participants who report falling in any of the three falls survey cycles, otherwise it was assigned 0. The “number of falls” outcome was calculated by taking the sum of the number of falls across all three survey cycles. Dates of falls were not available so averaged person-time accounting methods were used to incorporate differential fall times. Participants reporting no falls throughout the study period provided the full 6+12+12=30 person-months of observation. Participants who fell were assigned person-months based on the midpoint of the closest recall timeframe. As an example, a participant reporting their first fall on the 2016 (third) survey was assigned 6+12+(12/2) = 24 person-months of observation time. This approach averages out unknown differential fall times within the observation intervals.
Statistical Analysis
Descriptive statistics included frequency distributions, measures of central tendency (mean) and measures of variability [standard deviation (SD)]. Baseline characteristic comparisons over MVPA trajectory classes used analysis of variance (ANOVA) F-tests and Chi-square tests for continuous and categorical variables respectively. MVPA estimates (MET min wk−1) were skewed and log (base 2) transforms were used to derive the MVPA trajectory classes.
Latent class growth analysis was used to identify major trajectory classes of MVPA and model selection used Bayesian Information Criteria goodness of fit statististics and prior literature.25 Under a missing at random assumption, latent growth models are able to estimate MVPA trajectory classes for all participants regardless of whether data were missing, which generally decreases bias when compared to a complete-case analyses. After the MVPA trajectory classes were determined, participants were assigned to the trajectory class reflecting their highest posterior probability.26 Multinomial logistic models were used to examine adjusted relative risk ratio (aRRR) associations of predictors with the assigned trajectory classes. Generalized Linear Models using log-links, Poisson distributions and log(months) offset terms to account for differential recall assessment times were used to estimate adjusted incident relative risk (aIRR) associations of MVPA trajectory class with any falling, and adjusted rate ratio (aRR) associations with the number of falls. All models were adjusted for baseline values of age, sex, race-site, education, income, self-rated health, BMI, smoking, television viewing, diabetes, hypertension and prevalent cardiovascular disease. Television viewing was included as a covariate given it has been shown to be an acceptable proxy measure for sedentary behavior and is related to a variety of non-communicable disease outcomes.27 Further, under the 24-hour activity cycle framework28, physical activity and sedentary behaviors are inter-related behaviors that characterize waking time (i.e., time spent sedentary offsets active time). Sensitivity analyses to missing data were conducted by examining similar models using only the participant base who contributed physical activity data at all three exam visits. Additional sensitivity analyses to missing data were conducted using an inverse proportional weighting approach. All statistical analyses were conducted in STATA v. 15 (StataCorp, LLC., College Station, TX).
RESULTS
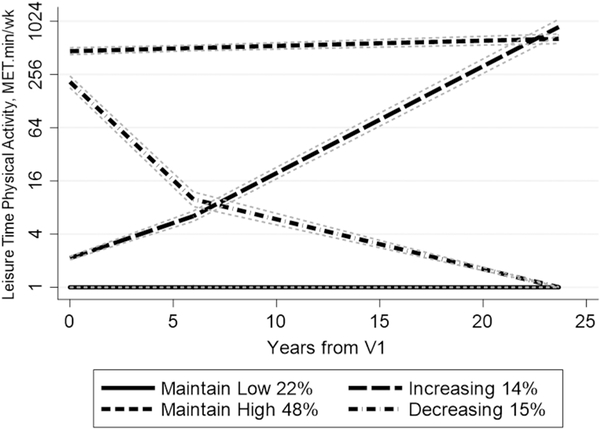
Four major MVPA trajectory classes were identified in ARIC participants with patterns reflecting: (1) maintained low (22%), (2) increasing (14%), (3) decreasing (15%), and (4) maintained high (48%) MVPA (Figure 1). Differences in baseline characteristics by MVPA trajectory group were all statistically significant (all comparisons p<0.001; Table 1). In general, men, whites, and those with a college education were more likely to be assigned to the maintained high MVPA trajectory group. Table 2 provides additional context on associations of socio-demographic, health status, and behavioral characteristics with MVPA trajectory groups. For example, men were approximately 40% less likely to be characterized as maintained low MVPA versus maintained high MVPA group compared to women [aRRR=0.60 (0.48, 0.73)]. Jackson participants were almost twice as likely to be in the maintained low MVPA group when compared with Washington County participants [aRRR=1.79 (1.36, 2.37)]. Similarly, participants were over three times as likely to be in the maintained low MVPA group versus the maintained high group if they had less than high school education versus college and above [aRRR=3.47 (2.54, 4.74)], or income less than $25,000 versus income ≥$50,000 [aRRR=1.45 (1.06, 2.00)], or fair/poor self-rated health versus excellent health [aRRR=1.82 (1.30, 2.55)], or obese versus underweight/normal [aRRR=2.16 (1.66, 2.81)], or a smoker versus non-smoker [aRRR=1.92 (1.52, 2.43)], or had prevalent versus no type 2 diabetes [aRRR=1.61 (1.11, 2.33)]. Table 3 shows the adjusted associations of MVPA trajectory groups with fall outcomes, including any falling (yes versus no) and number of falls. For the any falling outcome, the decreasing MVPA trajectory group had a 14% higher risk of any falling compared to the maintained high physical activity group [aIRR=1.14 (1.01, 1.28)]. For the number of falls outcome, when compared to the maintained high MVPA group (42 falls per 100 persons per year), the maintained low MVPA group had a 28% higher rate of falls [52 falls per 100 persons per year, aRR=1.28 (1.14, 1.44)] and the decreasing group had a 27% increased rate of falls [57 falls per 100 persons per year, aRR=1.27 (1.17, 1.38)]. Sensitivity analyses using both conditioning on the sample of ARIC participants with reported MVPA data at all three time-points (Supplemental Tables 1–3) and inverse-proportional weighting (Supplemental Table 4) showed similar associations as our main analyses and did not change overall interpretations.
Figure 1.
Latent class moderate to vigorous intensity physical activity trajectory classes identified in ARIC, using reported data from the ARIC/Baecke, a self-administered reliable and valid self-report recall questionnaire (n=15,792).20 A MET·min·wk−1 value of 450 is reflective of meeting aerobic physical activity guidelines (walking or lower threshold of moderate intensity physical activity = 3 METs * 150 min·wk−1).
Table 1.
Characteristics of Atherosclerosis Risk in Communities (ARIC) Study participants at Visit 1 by moderate to vigorous intensity physical activity (MVPA) trajectory class (n=15,792).
| VARIABLE | Overall | Maintain Low MVPA | Increasing MVPA | Decreasing MVPA | Maintain High MVPA | p-valuea | |
|---|---|---|---|---|---|---|---|
| n=15,792 | n=3,496 (22%) | n=2,243 (14%) | n=2,399 (15%) | n=7,654 (48%) | |||
| Age | Mean (SD) | 54.16 (5.76) | 54.43 (5.71) | 53.45 (5.66) | 54.11 (5.66) | 54.27 (5.83) | <0.001 |
| Sex | Female | 8710(55%) | 2061 (59%) | 1302 (58%) | 1463 (61%) | 3884 (51%) | <0.001 |
| Male | 7082 (45%) | 1435 (41%) | 941 (42%) | 936 (39%) | 3770 (49%) | ||
| Race | Black | 4266 (27%) | 1587 (45%) | 729 (33%) | 550 (23%) | 1400 (18%) | <0.001 |
| White | 11478 (73%) | 1904 (55%) | 1505 (67%) | 1846 (77%) | 6223 (82%) | ||
| Field Center | Forsyth County, NC | 4035 (26%) | 720 (21%) | 536 (24%) | 556 (23%) | 2223 (29%) | <0.001 |
| Jackson, MS | 3728 (24%) | 1459 (42%) | 664 (30%) | 475 (20%) | 1130 (15%) | ||
| Minneapolis Suburbs, MN | 4009 (25%) | 479 (14%) | 489 (22%) | 511 (21%) | 2530 (33%) | ||
| Washington County, MD | 4020 (25%) | 838 (24%) | 554 (25%) | 857 (36%) | 1771 (23%) | ||
| Education | < High School | 3767 (24%) | 1440 (41%) | 534 (24%) | 556 (23%) | 1237 (16%) | <0.001 |
| High School | 6412 (41%) | 1339 (38%) | 975 (44%) | 1086 (45%) | 3012 (39%) | ||
| College and above | 5586 (35%) | 712 (20%) | 728 (33%) | 754 (31%) | 3392 (44%) | ||
| Income | <$25,000 | 5683 (38%) | 1868 (58%) | 835 (40%) | 882 (39%) | 2098 (29%) | <0.001 |
| $25,000-$49,999 | 5524 (37%) | 983 (30%) | 829 (39%) | 918 (40%) | 2794 (39%) | ||
| >=$50,000 | 3658 (25%) | 397 (12%) | 439 (21%) | 468 (21%) | 2354 (32%) | ||
| Self-Rated Health | Excellent | 5246 (33%) | 668 (19%) | 689 (31%) | 787 (33%) | 3102 (41%) | <0.001 |
| Good | 7368 (47%) | 1584 (45%) | 1122 (50%) | 1166 (49%) | 3496 (46%) | ||
| Fair/Poor | 3170 (20%) | 1241 (36%) | 432 (19%) | 445 (19%) | 1052 (14%) | ||
| Body Mass Index (BMI) Category | Underweight/Normal | 5213 (33%) | 956 (27%) | 655 (29%) | 699 (29%) | 2903 (38%) | <0.001 |
| Overweight | 6206 (39%) | 1208 (35%) | 927 (41%) | 951 (40%) | 3120 (41%) | ||
| Obese | 4348 (28%) | 1323 (38%) | 661 (29%) | 745 (31%) | 1619 (21%) | ||
| Current Smoker | No | 11644 (74%) | 2173 (62%) | 1682 (75%) | 1829 (76%) | 5960 (78%) | <0.001 |
| Yes | 4132 (26%) | 1318 (38%) | 559 (25%) | 567 (24%) | 1688 (22%) | ||
| Television Viewing | Never | 140 (2%) | 10 (2%) | 21 (2%) | 41 (3%) | 68 (2%) | <0.001 |
| Seldom/Sometimes | 2889 (48%) | 235 (36%) | 544 (47%) | 541 (43%) | 1569 (53%) | ||
| Often/Very Often | 3003 (50%) | 399 (62%) | 594 (51%) | 679 (54%) | 1331 (45%) | ||
| Race-Site | Washington White | 3975 (25%) | 835 (24%) | 539 (24%) | 849 (36%) | 1752 (23%) | <0.001 |
| Minnesota White | 3972 (25%) | 474 (14%) | 485 (22%) | 508 (21%) | 2505 (33%) | ||
| Forsyth White | 3531 (23%) | 595 (17%) | 481 (22%) | 489 (20%) | 1966 (26%) | ||
| Forsyth Black | 483 (3%) | 123 (4%) | 52 (2%) | 67 (3%) | 241 (3%) | ||
| Jackson Black | 3728 (24%) | 1459 (42%) | 664 (30%) | 475 (20%) | 1130 (15%) | ||
| Prevalent Type 2 Diabetes | No | 13774 (88%) | 2803 (82%) | 1987 (89%) | 2137 (90%) | 6847 (90%) | <0.001 |
| Yes | 1870 (12%) | 632 (18%) | 234 (11%) | 247 (10%) | 757 (10%) | ||
| Prevalent Hypertension | No | 10208 (65%) | 1848 (53%) | 1479 (66%) | 1524 (64%) | 5357 (70%) | <0.001 |
| Yes | 5504 (35%) | 1627 (47%) | 750 (34%) | 864 (36%) | 2263 (30%) | ||
| Prevalent Cardiovascular Disease | No | 14682 (95%) | 3220 (94%) | 2136 (98%) | 2233 (95%) | 7093 (94%) | <0.001 |
| Yes | 766 (5%) | 191 (6%) | 52 (2%) | 106 (5%) | 417 (6%) |
P values representing differences in Visit 1 characteristics by moderate to vigorous intensity physical activity trajectory groups were obtained via analysis of variance (ANOVA) or Chi-Square Tests
CVD = cardiovascular disease.
Table 2:
Adjusted multinomial logistic regression models examining the adjusted relative risk ratios (aRRR)b of sociodemographic, health status, and behavioral characteristics with moderate to vigorous intensity physical activity (MVPA) trajectories, compared to the maintained high PA trajectory group.a
| Multivariable models (aRRR) b,c | |||||
|---|---|---|---|---|---|
| VARIABLE | Maintain Low MVPA | Increasing MVPA | Decreasing MVPA | Maintain High MVPA | |
| n=3,496 (22%) | n=2,243 (14%) | n=2,399 (15%) | n=7,654 (48%) | ||
| Age | Mean (SD) | 0.98 (0.96, 1.00) | 0.99 (0.97, 1.00) | 1.04 (1.02, 1.05) | -ref- |
| Sex | Female | -ref- | -ref- | -ref- | -ref- |
| Male | 0.60 (0.48, 0.73) | 0.80 (0.68, 0.94) | 0.59 (0.50, 0.69) | -ref- | |
| Race-Site | Washington White | -ref- | -ref- | -ref- | -ref- |
| Minnesota White | 0.42 (0.31, 0.56) | 0.91 (0.74, 1.13) | 0.39 (0.32, 0.47) | -ref- | |
| Forsyth White | 0.46 (0.33, 0.64) | 1.32 (1.05, 1.66) | 0.40 (0.32, 0.50) | -ref- | |
| Forsyth Black | 0.57 (0.26, 1.23) | 1.18 (0.67, 2.07) | 0.32 (0.17, 0.62) | -ref- | |
| Jackson Black | 1.79 (1.36, 2.37) | 2.05 (1.60, 2.62) | 0.63 (0.50, 0.80) | -ref- | |
| Education | College and above | -ref- | -ref- | -ref- | -ref- |
| High School | 1.97 (1.56, 2.50) | 1.38 (1.17, 1.63) | 1.35 (1.14, 1.59) | -ref- | |
| < High School | 3.47 (2.54, 4.74) | 1.84 (1.41, 2.40) | 1.65 (1.28, 2.13) | -ref- | |
| Income | >=$50,000 | -ref- | -ref- | -ref- | -ref- |
| $25,000-$49,999 | 1.26 (0.97, 1.64) | 1.50 (1.25, 1.80) | 1.30 (1.09, 1.56) | -ref- | |
| <$25,000 | 1.46 (1.06, 2.00) | 1.71 (1.35, 2.18) | 1.60 (1.27, 2.01) | -ref- | |
| Self-Rated | <$25,000 | 1.46 (1.06, 2.00) | 1.71 (1.35, 2.18) | 1.60 (1.27, 2.01) | -ref- |
| Excellent | -ref- | -ref- | -ref- | -ref- | |
| Health | Good | 1.40 (1.12, 1.75) | 1.51 (1.28, 1.78) | 1.29 (1.10, 1.51) | -ref- |
| Fair/Poor | 1.82 (1.30, 2.55) | 1.65 (1.23, 2.21) | 1.67 (1.26, 2.21) | -ref- | |
| BMI Category | Underweight /Normal | -ref- | -ref- | -ref- | -ref- |
| Overweight | 1.09 (0.86, 1.39) | 1.14 (0.95, 1.36) | 1.32 (1.11, 1.57) | -ref- | |
| Obese | 2.16 (1.66, 2.81) | 1.67 (1.35, 2.07) | 2.34 (1.90, 2.87) | -ref- | |
| Current Smoker | No | -ref- | -ref- | -ref- | -ref- |
| Yes | 1.92 (1.52, 2.43) | 1.36 (1.12, 1.65) | 1.48 (1.21, 1.80) | -ref- | |
| Television Viewing | Never | -ref- | -ref- | -ref- | -ref- |
| Seldom/ Sometimes | 1.22 (0.53, 2.77) | 1.01 (0.59, 1.72) | 0.58 (0.37, 0.90) | -ref- | |
| Often/Very Often | 1.91 (0.84, 4.34) | 1.11 (0.65, 1.89) | 0.76 (0.49, 1.18) | -ref- | |
| Prevalent Type 2 Diabetes | No | -ref- | -ref- | -ref- | -ref- |
| Yes | 1.61 (1.11, 2.33) | 0.72 (0.49, 1.05) | 1.20 (0.87, 1.65) | -ref- | |
| Prevalent Hypertension | No | -ref- | -ref- | -ref- | -ref- |
| Yes | 1.18 (0.94, 1.49) | 1.10 (0.91, 1.33) | 1.16 (0.97, 1.39) | -ref- | |
| Prevalent Cardiovascular Disease | No | -ref- | -ref- | -ref- | -ref- |
| Yes | 1.25 (0.63, 2.46) | 0.69 (0.37, 1.31) | 1.18 (0.70, 1.96) | -ref- | |
Moderate to vigorous intensity physical activity trajectory group assignment based on Visit 1 population (n=15,792)
adjusted for all other variables
p<0.05
p<0.01
p<0.001
Table 3:
Multivariable modelsa examining the adjusted incidence relative risk (aIRR) and rate ratio (aRR) of moderate to vigorous intensity physical activity (MVPA) trajectory group with any falling and number of falls outcomes, respectively.b
| Any Falling | Number of Falls | |||
|---|---|---|---|---|
| PA Trajectory Group | Obs %/yrc | aIRR (95% CI) | Obs #/100p/yrd | aRR (95% CI) |
| Maintain High MVPA | 20.00% | -ref- | 42 | -ref- |
| Maintain Low MVPA | 21.73% | 1.06 (0.89, 1.26) | 52 | 1.28 (1.14, 1.44) |
| Increasing MVPA | 18.81% | 0.98 (0.86, 1.12) | 37 | 0.94 (0.86, 1.04) |
| Decreasing MVPA | 24.65% | 1.14 (1.01, 1.28) | 57 | 1.27 (1.17, 1.38) |
Models adjusted for age, sex, race-site, education, income, self-rated health, body mass index (BMI) category, current smoking status, reported TV viewing, type 2 diabetes mellitus, hypertension, and prevalent coronary heart disease (CHD)
Moderate to vigorous intensity physical activity trajectory group assignment based on Visit 1 population (n=15,792)
Observed %/year (Obs %/yr) was calculated by dividing the total number of fallers by the total observed person years
Observed #/100 persons/year (Obs #/100p/yr) was calculated by dividing the total number of falls by the total observed person years, respectively.
DISCUSSION
In the current study, four distinct patterns of MVPA change emerged during midlife in a well-characterized and diverse sample of black and white men and women. Further, the majority of participants (70%) were assigned to a trajectory group that reflected patterns of MVPA maintenance across midlife, with the highest proportion of participants (48%) assigned to the maintained high group. When compared to the maintained high MVPA group, participant characteristics reflecting membership in the maintained low group largely mirrored factors shown in other studies to be related to inadequate MVPA levels.29,30 Finally, study findings suggest that when compared to a trajectory pattern supporting maintenance of high MVPA from midlife to older adulthood: 1) decreasing MVPA across midlife increases risk of any fall and 2) decreasing and maintaining low MVPA across midlife were susceptible to an increased rate in the number of falls during later life. Thus, we are unable to confirm findings from previous studies that demonstrated a u-shaped relation of physical activity and falls.3–6 Yet, study findings complement results of prior randomized controlled trials, but provide novel information on the influence of life-course changes in MVPA on subsequent fall risk within a naturalistic setting.
Falls are the leading cause of injury and death from injury in older adults.31 Based on 2014 CDC Behavioral Risk Factor Surveillance System data, 28.7% of U.S. older adults reported an estimated 29.0 million falls in the past 12 months.31 Using multiple data sources, Burns et al. reported that the direct costs for fatal and non-fatal falls in the U.S. were $616.5 million and $31.3 billion, respectively.32 With the aging Baby Boomer generation, it is expected that the U.S. older adult population will increase by 55% in 2030, which means that more individuals will be susceptible to falls than ever before. This Silver Tsumani is projected to result in an estimated 48.8 million falls and 11.9 million injurious falls.31 Therefore, it is of critical importance to continue to identify effective fall prevention strategies to minimize the impact of the Silver Tsunami.
Indeed, there is a strong body of literature that has identified a variety of intervention targets to reduce the risk of falls among older adults. For example, the CDC published the third edition of the CDC Compendium of Effective Fall Interventions: What Works For Community Dwelling Older Adults12 in 2015, which details specific interventions that have been shown to be effective for fall prevention, including those focused specifically on habitual physical activity. Yet, these evidence-based intervention strategies exclusively target older adults. Findings from the current study suggest that physical activity during midlife may also reduce the risk falls in older adulthood and supports the implementation of fall prevention strategies during midlife to optimize successful aging and reduce risk of falls.33 Regarding the outcome of any fall, participants demonstrating a pattern of decreasing MVPA overtime had a statistically significantly higher risk of falls in later life. This suggests that exercise participation closest in time to the outcome confers benefit in relation to any fall, which is a notion supported by the underlying biological plausibility including maintenance of optimal physical functioning34–36 and overall resilience (i.e., the ability to “bounce back” or recover from a fall).37
With no differences observed in any fall between the maintained low and maintained high MVPA groups, study findings also support the premise that fall risk can also decrease as a result of physical activity restriction due to mobility limitations and/or a fear of falling.38,39 However, regarding the number of falls outcome, the maintained low MVPA group had a 28% higher rate in the number of falls (an additional 10 reported falls per 100 person years) when compared to the maintained high MVPA group; an observed rate that was similar among the decreasing MVPA group. Yet, findings suggested no differences in either fall outcome in the increasing group compared to maintained high MVPA group, which supports the notion that it is never too late in life to become physically active or begin an exercise program. This important finding further supports the inclusion of midlife adults in health promotion efforts targeting physical activity initiation and maintenance for fall prevention.
Study strengths include use of the well-characterized ARIC cohort, including representation of black and white men and women. This provided the unique opportunity to examine the role of MVPA during the midlife to older adult transition as a possible fall prevention strategy in older adulthood, which has not been explored widely in the literature due to the limited number of studies with sufficient follow-up to characterize important adult life-course transitions. Despite these strengths, there are limitations to consider including the use of reported physical activity data, which may be prone to recall bias.40 Further, physical activity data from three time-points were used to construct the trajectories. Additional time-points may have resulted in greater refinement of the various trajectory classes. For example, in the Study of Women’s Health Across the Nation (SWAN) cohort, five physical activity trajectories (also utilizing reported participation in sports and exercise or MVPA) emerged including three patterns of maintenance [low (26.2%), middle (23.9%), and high (14.1%)] and increasing (13.4%) and decreasing (22.4%) physical activity based on data collected over ≥ 3 of 7 available time points.25 Also, the date of reported falls were not collected, which makes it challenging to report the average follow-up period with any precision. Therefore, the observed measures of association should be interpreted with caution given that averaged person-time accounting methods were used to incorporate differential fall times. However, physical activity data collection did precede the falls measures. Further, as previously mentioned, the recall time frame for falls ascertainment changed from six to twelve months after the first administration, which was done to optimize comparability with the Behavioral Risk Factor Surveillance System falls questions. Importantly, a six and twelve month recall time frame are relatively long periods and may have led to inaccuracies in the reporting of falls, and these biases may vary by recall time frame. Yet, a fall event, particularly if an injury was sustained, is likely more salient and easily recalled and reported than more habitual behaviors or events. Finally, several factors that have been shown to be associated with fall risk41, including depression, cognitive and physical functioning were not assessed in ARIC at Exam 1 and; therefore, not included in these analyses. However, given that these factors are also associated with low or declining MVPA levels1, their influence was likely characterized by MVPA trajectory exposure group assignment.
CONCLUSIONS
The principal findings from the current study suggest that promoting habitual MVPA during midlife, in addition to older adulthood, may be an effective intervention strategy to reduce subsequent risk of falls in older adulthood. Without additional fall prevention strategies, a Silver Tsunami is projected which will cause significant health and financial burden to the U.S. health care system. Future studies should examine the effectiveness of activity types across the intensity spectrum that are both effective in reducing late life falls and acceptable to a variety of populations across the lifespan, including the potential health benefits of light intensity physical activity.
Supplementary Material
HIGHLIGHTS.
Few studies have characterized physical activity from midlife to older adulthood.
Physical activity from midlife to older adulthood can reduce fall risk.
Findings support public health campaigns centered on physical activity promotion.
ACKNOWLEDGEMENTS
The Atherosclerosis Risk in Communities study has been funded in whole or in part with Federal funds from the National Heart, Lung, and Blood Institute, National Institutes of Health, Department of Health and Human Services, under Contract nos. (HHSN268201700001I, HHSN268201700002I, HHSN268201700003I, HHSN268201700005I, HHSN268201700004I). Additional support for this work was provided by the ARIC Physical Activity and Falls Study (R56 AG049886 to LAP & KPG). PP was supported by grant K99 AG 052830. The authors thank the staff and participants of the ARIC study for their important contributions.
Footnotes
Conflict of Interest: The authors have no conflicts of interest.
Conflict of Interest/Financial Disclosure: None
Disclosures: None
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.U.S. Department of Health and Human Services. 2018 Physical Activity Guidelines Advisory Committee Scientific Report. 2018; https://health.gov/paguidelines/second-edition/report/pdf/PAG_Advisory_Committee_Report.pdf. Accessed March 12, 2018.
- 2.U.S. Department of Health and Human Services. Physical Activity Guidelines Advisory Committee Report. 2008. http://www.health.gov/paguidelines/Report/pdf/CommitteeReport.pdf. Accessed March 19, 2011.
- 3.Campbell AJ, Borrie MJ, Spears GF. Risk factors for falls in a community-based prospective study of people 70 years and older. J Gerontol July 1989;44(4):M112–117. [DOI] [PubMed] [Google Scholar]
- 4.Chan BK, Marshall LM, Winters KM, Faulkner KA, Schwartz AV, Orwoll ES. Incident fall risk and physical activity and physical performance among older men: the Osteoporotic Fractures in Men Study. Am J Epidemiol. March 15 2007;165(6):696–703. [DOI] [PubMed] [Google Scholar]
- 5.Graafmans WC, Lips P, Wijlhuizen GJ, Pluijm SM, Bouter LM. Daily physical activity and the use of a walking aid in relation to falls in elderly people in a residential care setting. Zeitschrift fur Gerontologie und Geriatrie. February 2003;36(1):23–28. [DOI] [PubMed] [Google Scholar]
- 6.Heesch KC, Byles JE, Brown WJ. Prospective association between physical activity and falls in community-dwelling older women. Journal of epidemiology and community health. May 2008;62(5):421–426. [DOI] [PubMed] [Google Scholar]
- 7.El-Khoury F, Cassou B, Charles MA, Dargent-Molina P. The effect of fall prevention exercise programmes on fall induced injuries in community dwelling older adults: systematic review and meta-analysis of randomised controlled trials. Bmj October 29 2013;347:f6234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gillespie LD, Robertson MC, Gillespie WJ, et al. Interventions for preventing falls in older people living in the community. The Cochrane database of systematic reviews. September 12 2012(9):CD007146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhao R, Feng F, Wang X. Exercise interventions and prevention of fall-related fractures in older people: a meta-analysis of randomized controlled trials. Int J Epidemiol. February 1 2017;46(1):149–161. [DOI] [PubMed] [Google Scholar]
- 10.Summary of the Updated American Geriatrics Society/British Geriatrics Society clinical practice guideline for prevention of falls in older persons. J Am Geriatr Soc. January 2011;59(1):148–157. [DOI] [PubMed] [Google Scholar]
- 11.Guideline for the prevention of falls in older persons. American Geriatrics Society, British Geriatrics Society, and American Academy of Orthopaedic Surgeons Panel on Falls Prevention. J Am Geriatr Soc. May 2001;49(5):664–672. [PubMed] [Google Scholar]
- 12.U.S. Department of Health and Human Services. Centers for Disease Control and Prevention. Compendium of Effective Fall Interventions: What Works For Community Dwelling Older Adults 2015; https://www.cdc.gov/homeandrecreationalsafety/pdf/falls/cdc_falls_compendium-2015-a.pdf. Accessed October 17, 2017.
- 13.U.S. Department of Health and Human Services. National Institute on Aging. Go4Life: Preventing Falls. 2017; https://go4life.nia.nih.gov/sites/default/files/PreventingFalls_0.pdf. Accessed October 11, 2017.
- 14.Eckel RH, Jakicic JM, Ard JD, et al. 2013 AHA/ACC Guideline on Lifestyle Management to Reduce Cardiovascular Risk: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. November 12 2013. [Google Scholar]
- 15.Opportunities for Cancer Prevention During Midlife. American Journal of Preventive Medicine. 2014;46(3 (Supplement 1)). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Campbell AJ, Robertson MC. Rethinking individual and community fall prevention strategies: a meta-regression comparing single and multifactorial interventions. Age Ageing. November 2007;36(6):656–662. [DOI] [PubMed] [Google Scholar]
- 17.Evenson KR, Rosamond WD, Cai J, Diez-Roux AV, Brancati FL, Atherosclerosis Risk In Communities Study I. Influence of retirement on leisure-time physical activity: the atherosclerosis risk in communities study. Am J Epidemiol. April 15 2002;155(8):692–699. [DOI] [PubMed] [Google Scholar]
- 18.The Atherosclerosis Risk in Communities (ARIC) Study: design and objectives. The ARIC investigators. Am J Epidemiol. April 1989;129(4):687–702. [PubMed] [Google Scholar]
- 19.Cutter GR, Burke GL, Dyer AR, et al. Cardiovascular risk factors in young adults. The CARDIA baseline monograph. Control Clin Trials. February 1991;12(1 Suppl):1S–77S. [DOI] [PubMed] [Google Scholar]
- 20.Richardson MT, Ainsworth BE, Wu HC, Jacobs DR Jr., Leon AS. Ability of the Atherosclerosis Risk in Communities (ARIC)/Baecke Questionnaire to assess leisure-time physical activity. Int J Epidemiol. August 1995;24(4):685–693. [DOI] [PubMed] [Google Scholar]
- 21.Baecke JA, Burema J, Frijters JE. A short questionnaire for the measurement of habitual physical activity in epidemiological studies. Am J Clin Nutr. November 1982;36(5):936–942. [DOI] [PubMed] [Google Scholar]
- 22.Ainsworth BE, Haskell WL, Herrmann SD, et al. 2011 Compendium of Physical Activities: a second update of codes and MET values. Med Sci Sports Exerc. August 2011;43(8):1575–1581. [DOI] [PubMed] [Google Scholar]
- 23.Lamb SE, Jorstad-Stein EC, Hauer K, Becker C. Development of a common outcome data set for fall injury prevention trials: the Prevention of Falls Network Europe consensus. J Am Geriatr Soc September 2005;53(9):1618–1622. [DOI] [PubMed] [Google Scholar]
- 24.Tinetti ME, Williams CS. The effect of falls and fall injuries on functioning in community-dwelling older persons. J Gerontol A Biol Sci Med Sci March 1998;53(2):M112–119. [DOI] [PubMed] [Google Scholar]
- 25.Pettee Gabriel K, Sternfeld B, Colvin A, et al. Physical activity trajectories during midlife and subsequent risk of physical functioning decline in late midlife: The Study of Women’s Health Across the Nation (SWAN). Preventive Medicine. 2017;105:287–294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Andruff H, Carraro N, Thompson A, Gaudreau P, Louvet B. Latent class growth modelling: A tutorial. Tutorials in Quantitative Methods for Psychology. 2009;5(1):11–24. [Google Scholar]
- 27.Pettee KK, Ham SA, Macera CA, Ainsworth BE. The reliability of a survey question on television viewing and associations with health risk factors in US adults. Obesity (Silver Spring). March 2009;17(3):487–493. [DOI] [PubMed] [Google Scholar]
- 28.Rosenberger ME, Fulton JE, Buman MP, et al. The 24-Hour Activity Cycle: A New Paradigm for Physical Activity. Med Sci Sports Exerc. October 18 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bauman AE, Reis RS, Sallis JF, et al. Correlates of physical activity: why are some people physically active and others not? Lancet July 21 2012;380(9838):258–271. [DOI] [PubMed] [Google Scholar]
- 30.U.S. Department of Health and Human Services. Centers for Disease Control and Prevention. Adult participation in aerobic and muscle-strengthening physical activities--United States, 2011. MMWR Morb Mortal Wkly Rep. May 03 2013;62(17):326–330. [PMC free article] [PubMed] [Google Scholar]
- 31.Bergen G, Stevens MR, Burns ER. Falls and Fall Injuries Among Adults Aged >/=65 Years - United States, 2014. MMWR Morb Mortal Wkly Rep. September 23 2016;65(37):993–998. [DOI] [PubMed] [Google Scholar]
- 32.Burns ER, Stevens JA, Lee R. The direct costs of fatal and non-fatal falls among older adults - United States. J Safety Res. September 2016;58:99–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rowe JW, Kahn RL. Successful aging. Gerontologist. August 1997;37(4):433–440. [DOI] [PubMed] [Google Scholar]
- 34.Nelson ME, Rejeski WJ, Blair SN, et al. Physical activity and public health in older adults: recommendation from the American College of Sports Medicine and the American Heart Association. Med Sci Sports Exerc August 2007;39(8):1435–1445. [DOI] [PubMed] [Google Scholar]
- 35.Laurin D, Verreault R, Lindsay J, MacPherson K, Rockwood K. Physical activity and risk of cognitive impairment and dementia in elderly persons. Arch Neurol March 2001;58(3):498–504. [DOI] [PubMed] [Google Scholar]
- 36.Haskell WL, Lee IM, Pate RR, et al. Physical Activity and Public Health. Updated Recommendation for Adults From the American College of Sports Medicine and the American Heart Association. Circulation August 1 2007. [DOI] [PubMed] [Google Scholar]
- 37.MacLeod S, Musich S, Hawkins K, Alsgaard K, Wicker ER. The impact of resilience among older adults. Geriatr Nurs. Jul-Aug 2016;37(4):266–272. [DOI] [PubMed] [Google Scholar]
- 38.Jefferis BJ, Iliffe S, Kendrick D, et al. How are falls and fear of falling associated with objectively measured physical activity in a cohort of community-dwelling older men? BMC Geriatr. October 27 2014;14:114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jefferis BJ, Merom D, Sartini C, et al. Physical Activity and Falls in Older Men: The Critical Role of Mobility Limitations. Med Sci Sports Exerc. October 2015;47(10):2119–2128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Troiano RP, Pettee Gabriel KK, Welk GJ, Owen N, Sternfeld B. Reported physical activity and sedentary behavior: why do you ask? J Phys Act Health. Jan 2012;9 Suppl 1:S68–75. [DOI] [PubMed] [Google Scholar]
- 41.Rubenstein LZ. Falls in older people: epidemiology, risk factors and strategies for prevention. Age Ageing. September 2006;35 Suppl 2:ii37–ii41. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.