Abstract
Objective:
Asthma is an increasing chronic respiratory disease affecting over 300 million people worldwide. Several studies have shown that herbal remedies may improve asthma control and reduce asthma symptoms. In this study, the effects of short-course administration of an herbal mixture (ASMATUSTM) in asthmatic children during viral respiratory tract infection, were evaluated.
Materials and Methods:
Forty-six children (7-12 years old) with intermittent asthma were enrolled in this double-blind randomized clinical trial. At the onset of common cold symptoms, the patients were randomly assigned to daily receive either the herbal mixture (comprised of Matricaria chamomilla, Althaea officinalis, Malva sylvestris, Hyssopus officinalis, Adiantum capillus-veneris, Glycyrrhiza glabra and Ziziphus jujube) or placebo for 5 days. Primary outcomes included day symptoms, night symptoms, and asthma attacks. Secondary outcomes included Peak Expiratory Flow Rate (PEFR), the need for β-agonist administration, oral prednisolone usage, necessity for re-visit due to uncontrolled or insupportable symptoms, as well as the number of hospital admissions and days absent from school.
Results:
the herbal mixture significantly decreased the severity of coughs (p=0.049) and nighttime awakenings (p=0.029) in comparison to placebo. There was no significant reduction in wheezing, tachypnea, respiratory distress, PEF rate, absence from school, outpatient visits, asthma exacerbation, oral prednisolone or β-agonist usage and hospitalization.
Conclusion:
Short-course of herbal mixture this traditional herbal mixture, starting at the onset of signs of a viral respiratory tract infection in children with intermittent asthma, reduced cough and nights awakening. Further studies should be done to determine the most effective herbal admixture, as well as dose and duration of treatment.
Key Words: Asthma, Viral respiratory tract infection, Child, Herbal remedies
Introduction
Asthma is a chronic inflammatory disease of the respiratory airways resulting in episodic airflow obstruction. Its global prevalence is increasing. The common cold, caused by rhinovirus and other viral respiratory infections, is the major cause (85%) of asthma exacerbations in children. Preschool-aged children get an average of 6-8 colds per year, whereas 10-15% of children get at least 12 infections per year. The incidence of the common cold decreases with age as it reduces to 2-3 episodes per year by adulthood (Kliegman et al., 2007 ▶; Niimi, 2011 ▶). This is a possible explanation for the frequency of asthma hospitalizations in young children that far exceeds that of older children and adults.
Complementary and alternative medicine (CAM) has become more popular worldwide over the past few decades, as CAM approaches are thought to be safe, effective, available and affordable. According to a recent study performed by the Centers for Disease Control and Prevention, ∼12% of children and 40% of adults in the United States use CAM, revealing higher rates among children with respiratory complaints (Barnes et al., 2008 ▶; Ottolini et al., 2001 ▶; Philp et al., 2012 ▶; Pitetti et al., 2001 ▶; Slader et al., 2006 ▶; Ziment and Tashkin, 2000 ▶). The use of CAM is even more common in eastern countries as they have a long history of herbal medicine consumption. The use of herbal drugs for the treatment of lung problems in Asia, goes back to thousands of years ago, and it was most commonly practiced in China, India and Iran. However, due to the lack of well-designed clinical trials, it is difficult to assess the efficacy and safety of these treatments (Clark et al., 2010 ▶; Clement et al., 2005 ▶; Houssen et al., 2010 ▶; Huntley and Ernst, 2000 ▶; Passalacqua et al., 2006 ▶; Saklani and Kutty, 2008 ▶; Shergis et al., 2016 ▶).
Herbal remedies have also been recommended by Islamic traditional physicians; for instance, several herbs including Hyssopus officinalis L. (from Lamiaceae), Althaea officinalis L. (from Malvaceae), Ficus carica L. (from Moraceae), Malva sylvestris L. (from Moraceae), Adiantum capillus-veneris L. (from Pteridaceae), Viola odorata L. (from Violaceae), Ziziphus jujuba Mill. (from Rhamnaceae), honey, Thymus vulgaris L. (from Lamiaceae) and Glycyrrhiza glabra L. (from Fabaceae) were used for treatment of asthma and bronchitis (Avecina, 1991 ▶; Jorjani, 1992 ▶). Herbal remedies can be used individually or in combination with other herbs (i.e. a mixture of several herbs). The physiological effects of herbal drugs vary depending on active compounds being present in a formulation. Empirical evidence propose significant beneficial effects for herbs (chamomile, Ziziphus jujube, Honey) on decreasing airway inflammation, bronchial constriction, mucus production and airway hyper-responsiveness (Ahmadi et al., 2013 ▶; Saller et al., 1990 ▶; Srivastava et al., 2010 ▶).
As few clinical trials have reported the benefits of herbal mixtures; the objective of this study was to determine the efficacy and safety of a short-course administration of an herbal mixture containing seven different anti-asthma herbs, in children with intermittent asthma during viral respiratory tract infection.
Materials and Methods
This study was a randomized, double-blind, placebo-controlled clinical trial carried out between September 2015 and November 2016 in the Allergy Research Center of Qaem University Hospital, Mashhad, Iran. The trial was approved by the Human Research Ethics Committee of Mashhad University of Medical Sciences (MUMS), Mashhad, Iran and a written informed consent was obtained from the patients and their parents/guardian prior to participation in the present trial. Also, the trial was registered at Iranian Registry of Clinical Trials (approval No. IRCT201608314976N5), which meets the World Health Organization (WHO) registry criteria.
Among the 251 visited patients, 46 subjects were recruited. Children aged between 7 to 12 years with mild intermittent asthma [based on global initiative for asthma (GINA) guideline] being on the first day of acute viral upper respiratory tract infection, were included in this study. All cases with bacterial infection (as confirmed by clinical evaluations), any symptom of asthma exacerbation, allergy to herbal drugs, congenital abnormalities, any underlying diseases, or poor compliance for drugs usage (missing 3 doses or more), and those missing follow-up visits, were excluded from the study.
The herbal mixture was supplied by a hospital pharmacist of MUMS. Raw materials were purchased from Ejaze-Sabz Company, Mashhad, Iran. Fifty grams of chamomile (Matricaria chamomilla), 100 grams of common marshmallow flower (Althaea officinalis), 100 grams of high mallow flowers (Malva sylvestris), 100 grams of floral branches of hyssop (Hyssopus officinalis), 50 grams of aerial parts of maidenhair fern (Adiantum capillus-veneris), 50 grams of licorice root (Glycyrrhiza glabra) powder and 50 grams of jujube fruit (Ziziphus jujuba) were blended together. Then, 2.5 mL of distilled water was added to the mixture and the mixture was heated in a Bain-Marie at 80°C for 4 hrs. and filtered. Next, 50 grams of “taranjebin” (Persian word for manna) and 400 g of honey were added to the mixture. The mixture was dried and the powder was poured in 250 mL bottles which were sealed and kept in a refrigerator.
The patients with intermittent asthma were visited at the early manifestation of viral respiratory infection and subsequently enrolled in the trial. Patients were randomly assigned to receive either the herbal mixture at a dose of 5 mL three times a day for 5 days, or placebo that was matched for volume, shape, and appearance and was produced by the same company. For minimizing treatment bias, the study investigators, pharmacist, patients and their parents were blinded to the type of intervention.
Patients were allowed to receive standard remedies for asthma such as inhaled β-agonist and oral prednisolone according to a customized asthma management plan. At the first visit, all information including demographic data, physical examinations and Peak Expiratory Flow Rate (PEFR) were recorded. All daily symptoms (including the number and severity of cough) and medications (salbutamol and prednisolone) were recorded by parents using a checklist. In severe cases, prednisolone was started after consultation with the physician. For each patient, a telephone follow-up was performed on the third and fourteenth day after treatment initiation. Visit by the physician and PEFR measurement were done on the seventh day of the treatment course.
Primary outcomes included clinical manifestations such as day symptoms, night symptoms, and the number of asthma attacks. Secondary outcomes were PEFR, need for β-agonists, oral prednisolone usage, necessity for re-visit due to uncontrolled or insupportable symptoms, as well as the number of hospital admission and days absent from school. Researchers recorded side effects or complications observed during the trial.
Statistical analysis
Statistical analysis was performed using SPSS ver. 24. Demographic and baseline characteristics of the study participants were analyzed by independent sample t-test, chi-square and Fisher's exact test. The efficacy of the new herbal mixture on asthma symptoms was assessed by generalized estimating equations (GEE). A P-value < 0.05 was considered statistically significant.
Results
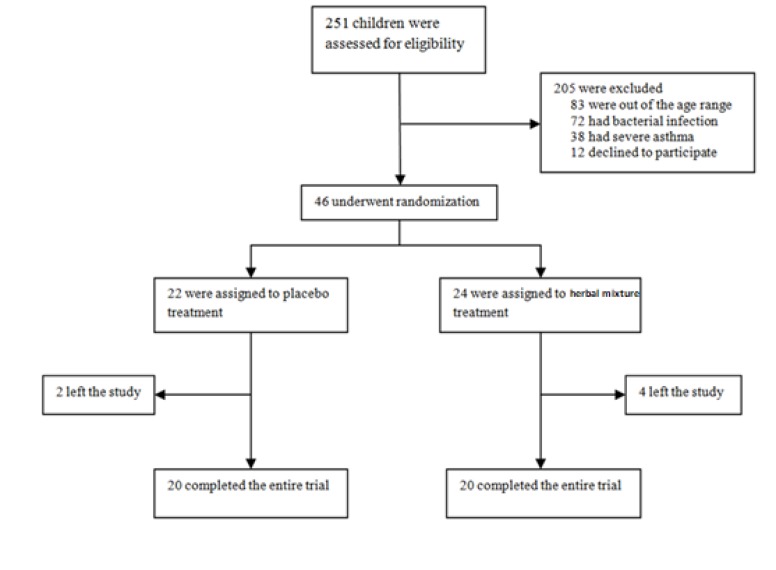
Forty-six asthmatic children (30 boys and 16 girls) were enrolled in this study (Figure 1). The baseline characteristics of the enrolled participants are demonstrated in Table 1. There was no significant difference in demographic nor clinical characteristics between the two groups at the beginning of the study.
Figure 1.
Flow diagram of the study participants recriuted and assigned to the studied groups
Table 1.
Demographics and baseline characteristics of the studied participants
| Characteristics | Herbal mixture | Placebo | P Value | ||
|---|---|---|---|---|---|
| Gender | Male | 14 | 16 | 0.306 | |
| Female | 10 | 6 | |||
| Age (Year)±SD | 7.33±1.45 | 7.91±2.54 | 0.357 | ||
| Family history | Asthma | Yes | 8 | 8 | 0.829 |
| No | 16 | 14 | |||
| Allergic rhinitis | Yes | 5 | 2 | 0.268 | |
| No | 19 | 20 | |||
| Urticaria | Yes | 2 | 2 | 0.927 | |
| No | 22 | 20 | |||
| Allergy | Yes | 12 | 13 | 0.536 | |
| No | 12 | 9 | |||
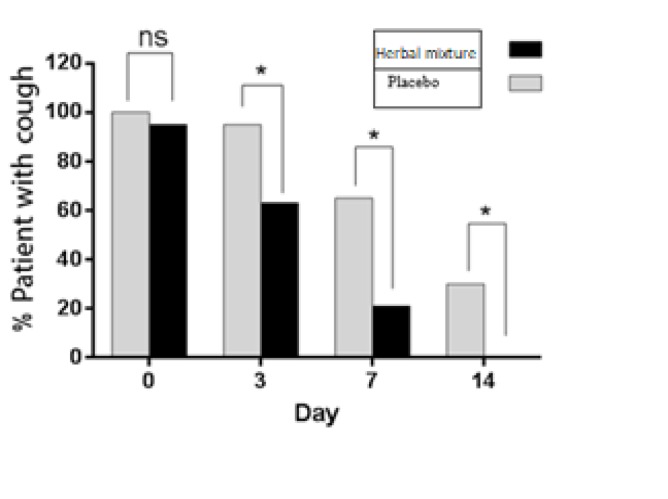
As illustrated in Figure 2, treatment of patients with Herbal mixture significantly reduced cough frequency 3, 7 and 14 days after treatment initiation in comparison to placebo (p<0.05).
Figure 2.
Effect of herbal mixture on the frequency of cough episodes during the study course
Moreover, GEE analysis showed that herbal mixture significantly decreased the severity of coughs (Table 2).
Table 2.
Effect of the herbal mixture and placebo on coughs' severity
| Time | Severity of cough | Herbal mixture | Placebo | P-Value |
|---|---|---|---|---|
| Day 0 | Very severe | 6 (25%) | 2 (9%) | 0.127 |
| Severe | 3 (12.5%) | 2 (9%) | ||
| Moderate | 12 (50%) | 10 (45.4%) | ||
| Mild | 2 (8.3%) | 8 (36.3%) | ||
| No cough | 1 (4.1%) | 0(0%) | ||
| Day 3 | Very severe | 4 (17.3%) | 2 (9.5%) | 0.011 |
| Severe | 1 (4.3%) | 1 (4.7%) | ||
| Moderate | 1 (4.3%) | 8 (38.1%) | ||
| Mild | 9 (39.1%) | 9 (42.8%) | ||
| No cough | 8 (34.7%) | 1 (4.7%) | ||
| Day 7 | Very severe | 1 (5.2%) | 2 (9.5%) | 0.007 |
| Severe | 1 (5.2%) | 0 (0%) | ||
| Moderate | 0 (0%) | 3 (14.2%) | ||
| Mild | 2 (10.5%) | 9 (42.8%) | ||
| No cough | 16 (80%) | 7 (33.3%) | ||
| Day 14 | Very severe | 0 (0%) | 1 (5%) | 0.020 |
| Severe | 0 (0%) | 0 (0%) | ||
| Moderate | 0 (0%) | 1 (5%) | ||
| Mild | 0 (0%) | 4 (20%) | ||
| No cough | 20 (100%) | 14 (70%) | ||
| GEE (Time) | <0.001 | |||
| GEE (Treatment) | 0.049 |
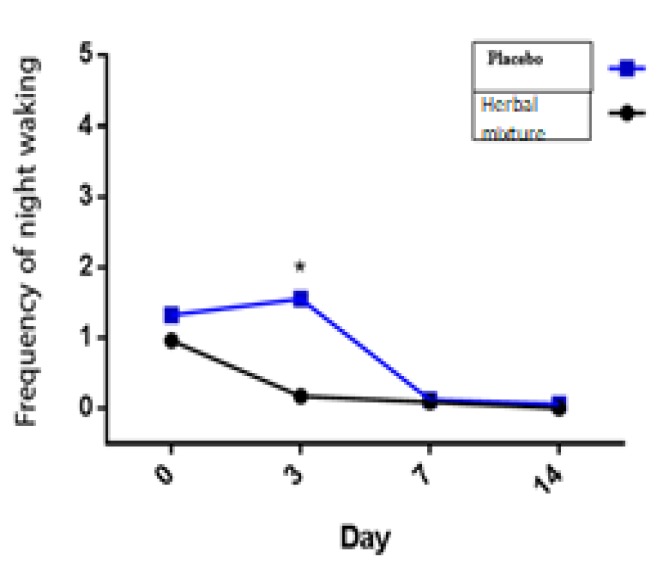
In the present study, the herbal mixture significantly improved night awakening in comparison to placebo (p=0.029; Figure 3).
Figure 3.
The effect of herbal mixture on night awakenings
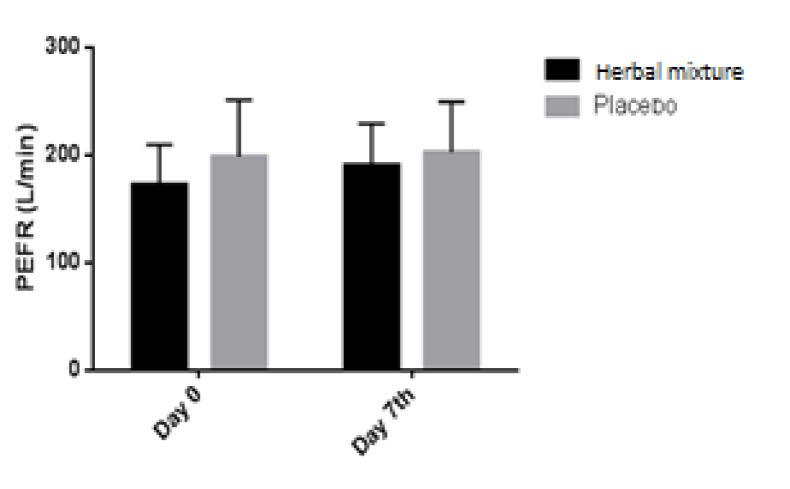
Statistical analysis using GEE demonstrated that the herbal mixture did not cause a significant effect on wheezing, intensity of respiratory distress, percentage of patients with tachypnea, days absent from school, frequency of physician's visits, frequency of inhaled salbutamol consumption, incidence of asthma attack, the need for oral steroids and PEFR (Figure 3.), when compared to placebo (Table 3 and 4). No adverse effects of the new herbal mixture were experienced in our patients.
Table 3.
Effect of herbal mixture on symptoms during the study course
| Sign and Symptoms | Day | Herbal mixture | Placebo | P-value |
|---|---|---|---|---|
| Respiratory distress | 0 | 5 (21.7 %) | 1 (4.5 %) | 0.45 |
| 3 | 1 (4.3 %) | 1 (5 %) | ||
| 7 | 0 (0%) | 1 (5 %) | ||
| 14 | 0 (0%) | 0 (0%) | ||
| Wheezing | 0 | 6 (24 %) | 8 (31 %) | 0.39 |
| 7 | 2 (8 %) | 1 (5 %) | ||
| Tachypnea | 0 | 0 (0%) | 0 (0%) | 0.99 |
| 7 | 0 (0%) | 1 (5 %) |
Table 4.
Effect of herbal mixture on secondary outcomes during the study course
| Outcomes | Day | Herbal mixture (%) | Placebo (%) | P-value |
|---|---|---|---|---|
| Absence from school | 0 | 6 (25 %) | 5 (22.7 %) | 0.64 |
| 3 | 0 (0 %) | 2 (10 %) | ||
| 7 | 1 (4.7 %) | 1 (5 %) | ||
| 14 | 0 (0%) | 0 (0 %) | ||
| Physician visit | 0 | 24 (100 %) | 21 (100 %) | 0.85 |
| 3 | 1 (4.3 %) | 3 (15 %) | ||
| 7 | 3 (15 %) | 1 (5 %) | ||
| 14 | 0 (0%) | |||
| Need for β2 agonist (Salbutamol) | 0 | 19 (25 %) | 0.91 | |
| 3 | 21 (87 %) | |||
| 7 | 14 (58 %) | 18 (85 %) | ||
| 14 | 11 (45 %) | 14 (66%) | ||
| Oral prednisolone usage | 0 | 17 (70 %) | 20 (95 %) | 0.91 |
| 3 | 17 (70 %) | 19 (90 %) | ||
| 7 | 18 (75 %) | 19 (90 %) | ||
| 0 (0%) | 17 (70 %) | 18 (85 %) | ||
| Hospital admission | 20 (22.7 %) | 0 (0%) | 0 (0%) | 0.97 |
| 19 (90 %) | 0 (0%) | 0 (0%) | ||
| 7 | 0 (0%) | 1 (5 %) | ||
| 14 | 0 (0%) | 0 (0%) |
Figure 4.
The effect of the herbal mixture on peak expiratory flow rate (PEFR). Data presented as mean±SD
Discussion
This study demonstrated that in children with intermittent asthma, a short-course administration of an herbal mixture at the onset of viral respiratory tract infection results in a significant reduction in day cough, night cough and night awakenings. As children with intermittent asthma commonly become symptomatic due to viral upper respiratory tract infections, the early use of short-course remedies may be regarded as a safe and cost-effective prophylactic alternative.
Some researchers have shown the benefits of single herbs in asthma; for example, Saller et al. (1990) ▶ showed the effectiveness of chamomile, and Ahmadi et al. (2013) ▶ reported that honey reduces the severity and frequency of day and night coughs versus diphenhydramine (p<0.02), (Salleret al., 1990 ▶; Ahmadi et al., 2013 ▶). Paul et al. (2007) ▶ also stated that honey has a significant effect on nocturnal cough and sleep quality in children and their parents (Paul et al., 2007 ▶). It is believed that co-administration of herbal medicines produces synergistic effects and reduces possible side effects of certain herbs. In another study, Broujeni et al. (2009) suggested that combination of the extracts of Zingiber officinale and Althaea officinalis reduces the severity of acute bronchitis-induced coughs (Broujeni et al., 2009).
Furthermore, there are several famous herbal mixtures that have been used for treatment of asthma in different countries. Chang et al. (2006) ▶ investigated the Chinese herbal medicine formula, STA-1 (consisting of 10 herbs as follows: root of Rehmannia glutinosa, root bark of Paeonia suffruticosa, fruit of Cornus officinalis, rhizome of Alisma orientalis, root of Dioscorea opposita, root of Ophiopogon japonicus, root of Glycyrrhiza uralensis, root of Panax quinquefolius and tuber of Pinellia ternate) for treatment of allergic asthma and showed a statistically significant reduction in symptoms' scores, systemic steroid usage, total IgE and specific IgE in the STA-1 group. Furthermore, STA-1 also improved the pulmonary function (FEV1) in patients with mild-to-moderate chronic asthma demonstrating only minimal side effects (Chang et al., 2006 ▶). While Antiasthma Simplified Herbal Medicine Intervention (ASHMI) had no adverse effects on adrenal function, in contrast to prednisolone, it had beneficial effects on Th1/Th2 balance. ASHMI is a combination of three extracts namely, Ling Zhi from Ganoderma lucidum , Ku Shen from Sophora flavescens and Gan Cao from Glycyrhhiza uralensis, which has shown potential for treatment of asthma in both in vitro and in vivo models as well as in clinical settings (Zhang et al., 2010 ▶). In the study done by Wen et al. (2005) ▶, ASHMI was shown to improve lung function and clinical symptoms' score, reduce the need for β2-bronchodilators usage, serum IgE levels and Th2 cytokine levels. Serum IFN-gamma and cortisol levels were significantly increased in the ASHMI group, in contrast to the prednisolone group. Ziziphus jujuba has been used in several Chinese herbalformulations such as Saiboku-to, Sho-saiko-to and Bu Zhong Yi Qi Tang, and have shown efficacy in asthma treatment (Naik et al., 2013 ▶). Some investigations in mice have shown that Hyssopus officinalis plays an anti-inflammatory role through regulating the secretion of IL-4, IL-6, IL-17, and IFN-gamma and correcting the imbalance in Th1/Th2, therefore, relieving cough and asthma (Javadi et al., 2017 ▶; Ma et al., 2014 ▶). Several previous studies have reported that Adiantum capillus-veneris possesses antiasthmatic activity, justifying the traditional use of A. capillus-veneris in asthma (Dehdari and Hajimehdipoor, 2018 ▶; Swaroop et al., 2012 ▶).
It has been reported that night awaking is a common complication of asthma in both adults and children (Strunk et al., 2002 ▶; Sutherland, 2005 ▶). Clinical studies indicated that appropriate asthma control can result in better sleep quality in asthmatic patient (Cukic et al., 2011 ▶). Similarly, in our study, treatment of patient with herbal mixture improved sleep quality as well as other asthma complications. Since patients in placebo group received the standard treatment of asthma, they also reported less night awaking on days 7 and 14. Likewise, frequency of cough reduced in placebo group.
No side effect following the use of herbal mixture was experienced in this study. Nevertheless, physicians should consider balancing the risks and benefits of complementary and alternative medicine (CAM) utilization beforehand. These considerations are particularly important in with regard to allergy and immunology, as the most commonly reported CAM adverse events include urticaria, contact dermatitis and anaphylaxis (Benito et al., 1996 ▶; Fugh-Berman, 2000 ▶; Valli and Giardina, 2002 ▶). Wen et al. (2005) ▶ studied the efficacy and tolerability of anti-asthma herbal medicine intervention in adult patients with moderate-severe allergic asthma. They concluded that anti-asthma herbal medicine usage appears to be a safe and effective alternative approach for asthmatreatment. Despite the promising effects achieved in various researches, yet further detailed studies are required to better clarify the outcomes.
Taken together, in children with intermittent asthma, a short-course administration of an herbal mixture, introduced given at the earliest appearance of signs of a viral infection or common cold, could result in reduction of asthma symptoms in comparison to placebo. The herbal mixture was found a treatment with few side effects and low cost that can be used to improve asthma symptoms triggered by viral respiratory tract infections. Nevertheless, further studies are needed to evaluate the most effective herbal admixture, dose and duration of treatment.
Acknowledgment
We thank our colleagues from Pediatric group in Mashhad University of Medical Sciences who provided insight and expertise that greatly assisted the research.
Conflicts of interest
We have no conflict of interest to declare and the herbal mixture is a trade name that we chose for our herbal mixture.
References
- Ahmadi M, Moosavi S, Zakeri S. Comparison of the effect of honey and diphenhydramine on cough alleviation in 2-5-year-old children with viral upper respiratory tract infection. J Gorgan Univ Med Sci. 2013;15:8–13. [Google Scholar]
- Avecina A. Ghanoon in Medicine. Vol. 2. Tehran, Iran: Soroush Co; 1991. pp. 196–197. [Google Scholar]
- Barnes PM, Bloom B, Nahin RL. Complementary and alternative medicine use among adults and children; United States, 2007. Natl Health Stat Report. 2008;10:1–23. [PubMed] [Google Scholar]
- Benito M, Jorro G, Morales C, Peláez A, Fernández A. Labiatae allergy: systemic reactions due to ingestion of oregano and thyme. Ann Allergy Asthma Immunol. 1996;76:416–418. doi: 10.1016/S1081-1206(10)63456-4. [DOI] [PubMed] [Google Scholar]
- Chang TT, Huang CC, Hsu CH. Clinical evaluation of the Chinese herbal medicine formula STA‐1 in the treatment of allergic asthma. Phytother Res. 2006;20:342–347. doi: 10.1002/ptr.1843. [DOI] [PubMed] [Google Scholar]
- Clark CE, Arnold E, Lasserson TJ, Wu T. Herbal interventions for chronic asthma in adults and children: a systematic review and meta-analysis. Prim Care Respir J. 2010;19:307–314. doi: 10.4104/pcrj.2010.00041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clement YN, Williams AF, Aranda D, Chase R, Watson N, Mohammed R, Stubbs O, Williamson D. Medicinal herb use among asthmatic patients attending a specialty care facility in Trinidad. BMC Complement Altern Med. 2005;5:3. doi: 10.1186/1472-6882-5-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cukic V, Lovre V, Dragisic D. Sleep Disorders in Patients with Bronchial Asthma. Materia Socio-Medica. 2011;23:235–237. doi: 10.5455/msm.2011.23.235-237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dehdari S, Hajimehdipoor H. Medicinal Properties of Adiantum capillus-veneris Linn In Traditional Medicine and Modern Phytotherapy: A Review Article. Iran J Public Health. 2018;47:188–197. [PMC free article] [PubMed] [Google Scholar]
- Fugh-Berman A. Herb-drug interactions. The Lancet. 2000;355:134–138. doi: 10.1016/S0140-6736(99)06457-0. [DOI] [PubMed] [Google Scholar]
- Houssen ME, Ragab A, Mesbah A, El-Samanoudy , AZ , Othman G, Moustafa AF, Badria FA. Natural anti-inflammatory products and leukotriene inhibitors as complementary therapy for bronchial asthma. Clin Biochem. 2010;43:887–890. doi: 10.1016/j.clinbiochem.2010.04.061. [DOI] [PubMed] [Google Scholar]
- Huntley A, Ernst E. Herbal medicines for asthma: a systematic review. Thorax. 2000;55:925–929. doi: 10.1136/thorax.55.11.925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Javadi B, Sahebkar A, Emami SA. Medicinal Plants for the Treatment of Asthma: A Traditional Persian Medicine Perspective. Curr Pharm Des. 2017;23:1623–1632. doi: 10.2174/1381612822666161021143332. [DOI] [PubMed] [Google Scholar]
- Jorjani L. Zakhireh kharazmshahi. Bonyade Farhang Iran. 1992;Tehran:101–174. [Google Scholar]
- Kliegman RM, Behrman RE, Jenson HB, Stanton BM. Nelson textbook of pediatrics e-book. Elsevier Health Sciences; 2007. [Google Scholar]
- Ma X, Ma X, Ma Z, Wang J, Sun Z, Yu W, Li F, Ding J. Effect of Hyssopus officinalis L on inhibiting airway inflammation and immune regulation in a chronic asthmatic mouse model. Exp Ther Med. 2014;8:1371–1374. doi: 10.3892/etm.2014.1978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naik SR, Bhagat S, Shah PD, Tare AA, Ingawale D, Wadekar RR. Evaluation of anti-allergic and anti-anaphylactic activity of ethanolic extract of Zizyphus jujuba fruits in rodents. Rev bras farmacogn. 2013;23:811–818. [Google Scholar]
- Niimi A. Cough and asthma. Curr Respir Med Rev. 2011;7:47–54. doi: 10.2174/157339811794109327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ottolini MC, Hamburger EK, Loprieato JO, Coleman RH, Sachs HC, Madden R, Brasseux C. Complementary and alternative medicine use among children in the Washington, DC area. Ambul Pediatr. 2001;1:122–125. doi: 10.1367/1539-4409(2001)001<0122:caamua>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- Passalacqua G, Bousquet PJ, Carlsen KH, Kemp J, Lockey RF, Niggemann B, Pawankar R, Price D, Bousquet J. ARIA update: I—Systematic review of complementary and alternative medicine for rhinitis and asthma. J Allergy Clin Immunol. 2006;117:1054–1062. doi: 10.1016/j.jaci.2005.12.1308. [DOI] [PubMed] [Google Scholar]
- Paul IM, Beiler J, McMonagle A, Shaffer ML, Duda L, Berlin CM. Effect of honey, dextromethorphan, and no treatment on nocturnal cough and sleep quality for coughing children and their parents. Arch Pediatr Adolesc Med. 2007;161:1140–1146. doi: 10.1001/archpedi.161.12.1140. [DOI] [PubMed] [Google Scholar]
- Philp JC, Maselli J, Pachter LM, Cabana MD. Complementary and alternative medicine use and adherence with pediatric asthma treatment. Pediatrics. 2012;129:e1148–e1154. doi: 10.1542/peds.2011-2467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pitetti R, Singh S, Hornyak D, Garcia SE, Herr S. Complementary and alternative medicine use in children. Pediatr Emerg Care. 2001;17:165–169. doi: 10.1097/00006565-200106000-00004. [DOI] [PubMed] [Google Scholar]
- Roohi Broujeni H, Ganji F, Roohi Broujeni P. The effect of combination of Zingeber and Althea officinalis extracts in acute bronchitis-induced cough. J Shahrekord Univ Med Sci. 2009;10:38–43. [Google Scholar]
- Saklani A, Kutty SK. Plant-derived compounds in clinical trials. Drug Discov Today. 2008;13:161–171. doi: 10.1016/j.drudis.2007.10.010. [DOI] [PubMed] [Google Scholar]
- Saller R, Beschorner M, Hellenbrecht D, Bühring M. Dose-dependancy of symptomatic relief of complaints by chamomile steam inhalation in patients with common cold. Eur J Pharmacol. 1990;183:728–729. [Google Scholar]
- Shergis JL, Wu L, Zhang AL, Guo X, Lu C, Xue CC. Herbal medicine for adults with asthma: a systematic review. J Asthma. 2016;53:650–659. doi: 10.3109/02770903.2015.1101473. [DOI] [PubMed] [Google Scholar]
- Slader CA, Reddel HK, Jenkins CR, Armour CL. Complementary and alternative medicine use in asthma: who is using what? Respirology. 2006;11:373–387. doi: 10.1111/j.1440-1843.2006.00861.x. [DOI] [PubMed] [Google Scholar]
- Srivastava JK, Shankar E, Gupta S. Chamomile: a herbal medicine of the past with a bright future. Mol Med Report. 2010;3:895–901. doi: 10.3892/mmr.2010.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strunk RC, Sternberg AL, Bacharier LB, Szefler SJ. Nocturnal awakening caused by asthma in children with mild-to-moderate asthma in the childhood asthma management program. J Allergy Clin Immunol. 2002;110:395–403. doi: 10.1067/mai.2002.127433. [DOI] [PubMed] [Google Scholar]
- Sutherland ER. Nocturnal asthma: underlying mechanisms and treatment. Curr Allergy Asthma Rep. 2005;5:161–167. doi: 10.1007/s11882-005-0091-z. [DOI] [PubMed] [Google Scholar]
- Swaroop K, Anbu J, Ashwini A, Sumithra M, Sathish R. Influence of ethanolic leaf extract of Sargassum wightii and Adiantum capillus on histamine induced asthma in animal model. Int J Pharm Pharm Sci. 2012;4:121–123. [Google Scholar]
- Valli G, Giardina E-GV. Benefits, adverse effects and drug interactionsof herbal therapies with cardiovascular effects. J Am Coll Cardiol. 2002;39:1083–1095. doi: 10.1016/s0735-1097(02)01749-7. [DOI] [PubMed] [Google Scholar]
- Wen MC, Wei CH, Hu ZQ, Srivastava K, Ko J, Xi ST, Mu DZ, Du JB, Li GH, Wallenstein S, Sampson H, Kattan M, Li XM. Efficacy and tolerability of antiasthma herbal medicine intervention in adult patients with moderate-severe allergic asthma. J Allergy Clin Immunol. 2005;116:517–524. doi: 10.1016/j.jaci.2005.05.029. [DOI] [PubMed] [Google Scholar]
- Zhang T, Srivastava K, Wen MC, Yang N, Cao J, Busse P, Birmingham N, Goldfarb J, Li XM. Pharmacology and immunological actions of a herbal medicine ASHMITM on allergic asthma. Phytother Res. 2010;24:1047–1055. doi: 10.1002/ptr.3077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ziment I, Tashkin DP. Alternative medicine for allergy and asthma. J Allergy Clin Immunol. 2000;106:603–614. doi: 10.1067/mai.2000.109432. [DOI] [PubMed] [Google Scholar]