Recent studies have shown that bacteria promote infection and stabilization of poliovirus particles, but the breadth of these effects on other members of the Picornaviridae family is unknown. Here, we compared the effects of bacteria on four distinct members of the Picornaviridae family. We found that bacteria reduced inactivation of all of the viruses during bleach treatment, but not all viral strains were stabilized by bacteria during heat treatment. Overall, our data provide insight into how bacteria play differential roles in picornavirus stability.
KEYWORDS: bacteria, picornaviruses, stability
ABSTRACT
Several viruses encounter various bacterial species within the host and in the environment. Despite these close encounters, the effects of bacteria on picornaviruses are not completely understood. Previous work determined that poliovirus (PV), an enteric virus, has enhanced virion stability when exposed to bacteria or bacterial surface polysaccharides such as lipopolysaccharide. Virion stabilization by bacteria may be important for interhost transmission, since a mutant PV with reduced bacterial binding had a fecal-oral transmission defect in mice. Therefore, we investigated whether bacteria broadly enhance stability of picornaviruses from three different genera: Enterovirus (PV and coxsackievirus B3 [CVB3]), Kobuvirus (Aichi virus), and Cardiovirus (mengovirus). Furthermore, to delineate strain-specific effects, we examined two strains of CVB3 and a PV mutant with enhanced thermal stability. We determined that specific bacterial strains enhance thermal stability of PV and CVB3, while mengovirus and Aichi virus are stable at high temperatures in the absence of bacteria. Additionally, we determined that bacteria or lipopolysaccharide can stabilize PV, CVB3, Aichi virus, and mengovirus during exposure to bleach. These effects are likely mediated through direct interactions with bacteria, since viruses bound to bacteria in a pulldown assay. Overall, this work reveals shared and distinct effects of bacteria on a panel of picornaviruses.
IMPORTANCE Recent studies have shown that bacteria promote infection and stabilization of poliovirus particles, but the breadth of these effects on other members of the Picornaviridae family is unknown. Here, we compared the effects of bacteria on four distinct members of the Picornaviridae family. We found that bacteria reduced inactivation of all of the viruses during bleach treatment, but not all viral strains were stabilized by bacteria during heat treatment. Overall, our data provide insight into how bacteria play differential roles in picornavirus stability.
INTRODUCTION
The Picornaviridae family includes important human pathogens that can cause a range of diseases such as the common cold, meningitis, hepatitis, and paralysis. The Picornaviridae family is diverse and currently includes 80 species in 35 genera. Members of this family are nonenveloped and contain a single-stranded, positive-sense viral genome approximately 7,500 nucleotides in length (1).
Recent studies have shown that bacteria, in particular the gut microbiota, play several important roles during viral infection. Enteric viruses encounter a milieu of microorganisms, including bacteria, both within and outside the host. It is estimated that these viruses encounter approximately 1011 bacteria in the host and are expected to encounter even more in the environment (2). Indeed, bacteria enhance infection of several unrelated viruses, including poliovirus, reovirus, rotavirus, mouse mammary tumor virus, and norovirus (3–9). These “proviral” effects are mediated by two known mechanisms: (i) direct interactions between bacteria and viruses that increase virion stability and attachment to host cells and (ii) indirect interactions between bacteria and the host immune system that modulate immune responses for productive viral infection (3–8, 10).
Intriguingly, bacteria and bacterial molecules can inhibit infection with certain viruses. For example, Ichinohe et al. demonstrated that certain bacteria promote host immune responses during influenza virus infection of mice (11). More recently, Bandoro and Runstadler determined that exposure to the bacterial surface molecule lipopolysaccharide (LPS) reduced stability of several strains of influenza virus by altering the morphology of the virion envelope (12).
Based on the importance of bacterial-viral interactions for viral infection, we sought to determine whether bacteria differentially affect different members of the same viral family, the Picornaviridae. We used a panel of four picornaviruses that are spread by the fecal-oral route and represent three separate genera: Enterovirus (coxsackievirus B3 [CVB3] and poliovirus [PV]), Kobuvirus (Aichi virus), and Cardiovirus (mengovirus). We found that a subset of the viral panel was stabilized by bacteria during heat treatment but that all of the picornaviruses tested were stabilized by bacteria during bleach treatment. We also determined that viruses bound to bacteria, indicating that direct interactions may be facilitating viral stabilization of these viruses. This work expands on bacterial enhancement effects previously observed with PV to other members of the Picornaviridae family. Ultimately, this work defines the unique interactions between specific viruses and bacteria which may provide insight into virion environmental stability and transmission.
RESULTS
Panel of viruses from the Picornaviridae family and bacterial strains.
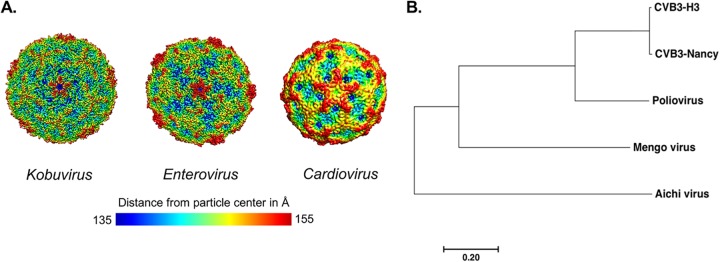
Previous studies have indicated that bacteria can reduce the inactivation of poliovirus particles after heat or bleach treatment (3, 7). In order to investigate whether bacteria stabilize other members of the Picornaviridae family from these inactivating conditions, we selected viruses from separate genera and viruses with differences in capsid sequence similarity (Fig. 1A and B and Table 1). These viruses differ in their capsid structure sequence and topology, which may confer different interactions with bacteria (Fig. 1A). The panel is composed of one virus from the Kobuvirus genus (Aichi virus), one virus from the Cardiovirus genus (mengovirus), and three viruses from the Enterovirus genus (PV, CVB3-H3 and CVB3-Nancy). CVB3-Nancy and CVB3-H3 have 98.4% capsid sequence similarity at the amino acid level and were compared to determine whether there are strain-specific differences in bacterial stabilization (Fig. 1B and Table 1). Additionally, our panel included a PV mutant with a single amino acid change in the VP1 capsid coding region (PV-M132V), which confers enhanced thermal stability in the absence of bacteria (13).
FIG 1.
Panel of picornaviruses used in this study. (A) Structural models of picornaviruses. Structural comparisons were performed using EMDB accession numbers for each viral genus and topological distances from the center of the virion calculated from 135 Å (blue) to 155 Å (red), as indicated by the scale bar (22). Representative viruses for each genus are Aichi virus (Kobuvirus), CVB3 (Enterovirus), and Saffold virus (Cardiovirus). The Aichi virus structure is at 3.7-Å resolution, the CVB3 structure is at 3.9-Å resolution, and the Saffold virus (A particle) is at 10.6-Å resolution. Models and distances were generated with UCSF Chimera software. (B) Phylogenetic tree of picornaviruses based on the amino acid sequence of the capsid coding region. The tree was generated using MEGA7 software. The evolutionary history was inferred using the neighbor-joining method. The scale bar represents the number of substitutions per site.
TABLE 1.
Percent sequence identity among panel of picornaviruses
| Picornaviridae genus | Virus | Capsid amino acid sequence similarity (%) |
||||
|---|---|---|---|---|---|---|
| Aichi virus | Mengovirus | CVB3-H3 | CVB3-Nancy | Poliovirus | ||
| Kobuvirus | Aichi virus | 100.0 | 28.6 | 23.3 | 23.3 | 24.3 |
| Cardiovirus | Mengovirus | 100.0 | 30.0 | 29.8 | 29.0 | |
| Enterovirus | CVB3-H3 | 100.0 | 98.6 | 54.4 | ||
| CVB3-Nancy | 100.0 | 54.2 | ||||
| Poliovirus | 100.0 | |||||
We also selected a representative panel of enteric bacteria and bacterial and nonbacterial molecules (Table 2). We included LPS, which is glycan found on the surface of Gram-negative bacteria. Additionally, we examined two representative Gram-negative bacterial strains (Escherichia coli 1470 and Prevotella ruminicola) and two representative Gram-positive bacterial strains (Bacillus badius and Lactobacillus johnsonii). We previously showed that E. coli 1470, P. ruminicola, B. badius, and L. johnsonii bind to PV (14), but whether these strains stabilize PV and other picornaviruses was unknown. We also previously showed that nonbacterial compounds, such as bovine albumin serum (BSA) and cellulose, had minimal effects on PV stability and were included in this study as controls (Table 2) (3, 7).
TABLE 2.
List of reagents and bacterial strains used in this study
| Name | Gram status | Phylum | Source |
|---|---|---|---|
| Bovine albumin serum (BSA) | Fisher Scientific | ||
| Cellulose | Sigma | ||
| Lipopolysaccharide | Sigma (0127:B8) | ||
| Escherichia coli 1470 | Negative | Proteobacteria | Mouse cecum |
| Prevotella ruminicola | Negative | Bacteroidetes | ATCC 19189 |
| Bacillus badius | Positive | Firmicutes | Mouse cecum |
| Lactobacillus johnsonii | Positive | Firmicutes | Mouse cecum |
Specific bacteria enhance stability of a subset of picornaviruses during heat treatment.
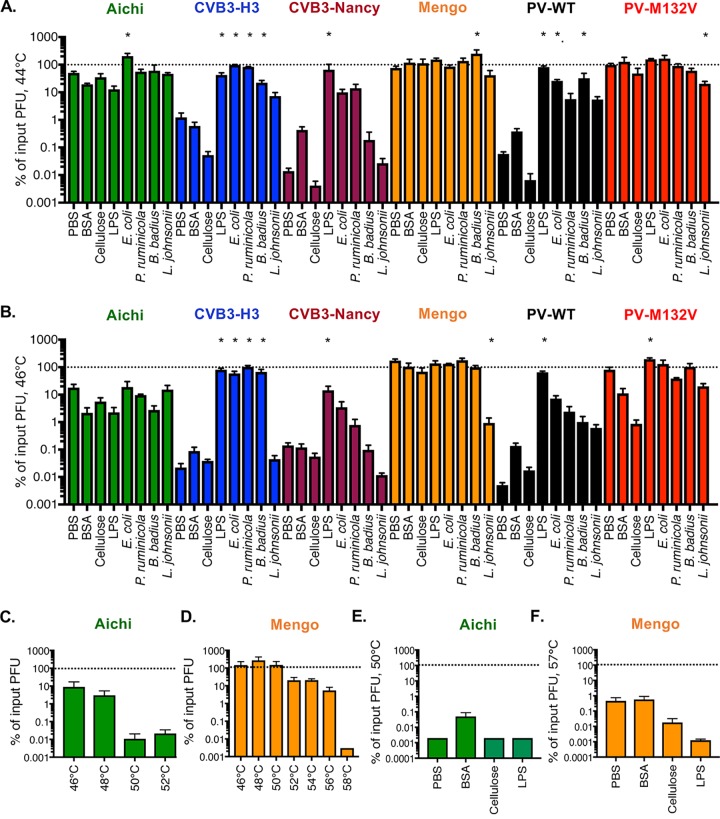
To determine whether bacteria enhance stability of picornaviruses, we first examined viral inactivation at elevated temperatures. Picornavirus particles can be inactivated by undergoing premature genome release at a range of temperatures, with faster inactivation at higher temperatures (7, 15, 16). To increase the tractability of our assays, we used relatively high temperatures for our thermal inactivation experiments because inactivation occurs relatively quickly. We first tested viral stability at 44°C for 4.5 h, a condition that we determined inactivates approximately 99% of PV infectivity during incubation in PBS (Fig. 2A). Viruses were mixed with PBS, compounds (BSA, cellulose, or LPS), or bacteria and incubated at 44°C for 4.5 h, and plaque assays were performed to quantify the amount of viable virus remaining. When we incubated PV with any of the bacterial strains or LPS, we observed an >50-fold increase in viral stability compared to PBS (Fig. 2A). A similar stabilization was observed for CVB3-H3 and CVB3-Nancy compared to PBS. Nonbacterial compounds (BSA and cellulose) did not stabilize PV or either CVB3 strain. Interestingly, Aichi virus and mengovirus were very stable in PBS under these conditions. We also tested a recently identified heat-resistant PV mutant, PV-M132V (13). Like Aichi virus and mengovirus, PV-M132V was resistant to heat treatment, and thus, incubation with any of the compounds or bacterial strains did not increase stability (Fig. 2A).
FIG 2.
Effects of bacteria and compounds on picornavirus stability at elevated temperatures. Thermal stability assays were performed by incubating 1 × 105 PFU of viruses in PBS, 1 mg/ml BSA, cellulose, LPS, or 1 × 1010 CFU of bacterial strains at various temperatures for 4.5 h. The amount of viable virus following each assay was determined by plaque assay and compared to PBS viral titer at 0 h to determine percentage of input PFU. (A) Assay at 44°C. Data are representative of 10 to 18 independent experiments (n = 4 to 47). (B) Assay at 46°C. Data are representative of 9 to 14 independent experiments (n = 4 to 25). (C) Incubation of Aichi virus in PBS at various temperatures. Data are representative of two or three independent experiments (n = 3 to 5). (D) Incubation of mengovirus in PBS at various temperatures. Data are representative of one to three independent experiments (n = 2 to 6). (E) Aichi virus 50°C assay. Data are representative of two independent experiments (n = 4). (F) Mengovirus 57°C assay. Data are representative of two experiments (n = 4). Bars are shown for SEM. Statistical significance was determined by one-way ANOVA (*, P < 0.05).
We next wanted to determine whether bacteria could increase stability of the heat-stable viruses at temperatures where they become heat labile. First, we increased the temperature in the thermal stability assay to 46°C and found that, similarly to the 44°C assay, PV, CVB3-H3, and CVB3-Nancy were stabilized by bacteria (Fig. 2B). Aichi virus, mengovirus, and PV-M132V were still stable in the 46°C assay, and incubation with any of the bacterial compounds or strains did not increase stability. To determine the temperature necessary to inactivate Aichi virus and mengovirus, we tested viability at temperatures from 46 to 58°C for 4.5 h. These additional experiments at different temperatures revealed that Aichi virus and mengovirus were ∼99% inactivated when incubated at 50°C or 57°C for 4.5 h, respectively (Fig. 2C to F). Despite viral inactivation under these conditions, none of the bacterial strains or bacterial polysaccharides could stabilize either of these viruses (Fig. 2D and F). Intriguingly, BSA stabilized Aichi virus during incubation at 50°C, indicating this virus may have different requirements for stabilization during heat treatment (Fig. 2E). Overall, these data indicate that bacteria do not stabilize Aichi virus and mengovirus during incubation at high temperatures but that bacterial stabilization of these viruses may be less important given their inherent high stability.
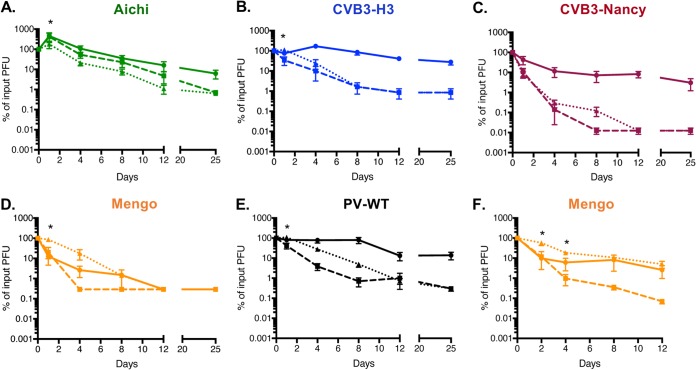
The effect of feces on picornaviruses.
We next wanted to determine whether the viruses in our panel are stabilized in feces. As enteric viruses are transmitted by the fecal-oral route, the potential effects of fecal components on their stability and infection are highly relevant. We previously showed that PV is stabilized in feces from conventional mice (7). Feces contain many other factors in addition to bacteria; thus, examining virion stability in feces provides a broader view of factors that influence viral infectivity. Here, we compared viral stability when viruses were incubated in PBS or feces from conventional mice over the course of several days at 37°C followed by quantification of remaining viable virus by plaque assay. We found that Aichi virus was not stabilized by feces compared to PBS at 37°C after day 1 (Fig. 3A). Feces only moderately stabilized CVB3-H3 at early time points (Fig. 3B). However, CVB3-Nancy and PV were stabilized by feces at later time points (see day 8) (Fig. 3C and E). We also demonstrated that PV-M132V was stable during 8 days of incubation at 37°C in both PBS and feces (13). Interestingly, mengovirus exhibited significant inactivation after 4 days at 37°C, but incubation in feces limited this inactivation (Fig. 3D). This result was surprising given the stability of mengovirus at 46°C for 4.5 h and the lack of bacterial stabilization of mengovirus at 57°C (Fig. 2B and F). However, mengovirus may have enhanced thermal sensitivity over longer time courses and bacterial effects may be apparent only under these conditions and/or nonbacterial components of feces could affect mengovirus. When we incubated mengovirus with mixtures of E. coli, P. ruminicola, and L. johnsonii at 37°C for several days, mengovirus was stabilized compared to PBS at 37°C (see dashed line compared to dotted line) (Fig. 3F). These findings indicate that bacteria stabilize mengovirus during longer exposures to body temperature (37°C) (Fig. 3F). Overall, these data indicate that several picornaviruses, but not all, are stabilized in feces, which could facilitate transmission.
FIG 3.
Picornavirus stability in feces. (A to E) A 1 × 105-PFU amount of Aichi virus (A), CVB3-H3 (B), CVB3-Nancy (C), mengovirus (D), or PV (E) was incubated with PBS or a slurry of feces from mice and incubated at 37°C (PBS, dashed lines; feces, dotted lines) or 4°C (PBS, solid lines). Data are representative of two or three experiments (n = 4 to 5). (F) A 1 × 105-PFU amount of mengovirus was incubated with PBS or a mixture of E. coli, P. ruminicola, and L. johnsonii and incubated at 37°C (PBS, dashed lines; bacteria, dotted lines) or 4°C (PBS, solid lines). Data are representative of two independent experiments (n = 4). Samples were taken at designated time points and processed prior to plaque assay for quantification of viable virus. Bars are shown for SEM. Statistical significance between PBS and feces or bacteria at 37°C was determined by two-way ANOVA (*, P < 0.05).
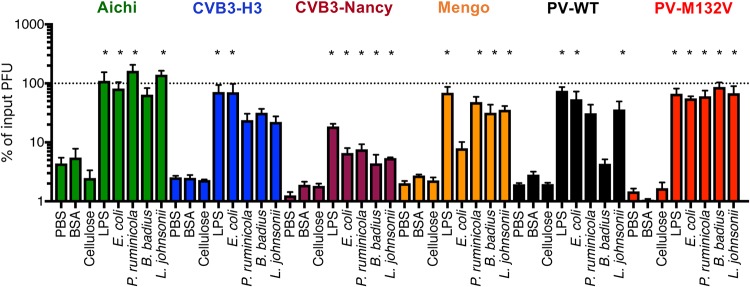
Bacteria enhance stability of picornaviruses during bleach exposure.
In addition to heat, virions can be inactivated by chlorine bleach via capsid penetration and damage and/or genome release (17–21). To determine whether bacteria affect bleach inactivation of viruses, we preincubated viruses in PBS, compounds, or bacterial strains for 1 h followed by exposure to dilute bleach (0.0001%) for 1 min, neutralization, and plaque assay to determine the amount of viable virus present. We determined that when preincubated in PBS, all viruses lost ∼90% of their infectivity (Fig. 4). However, when preincubated with LPS or bacterial strains, all viruses were stabilized by at least some of the treatments (Fig. 4). Importantly, preincubation of the viruses with BSA or cellulose did not prevent viral inactivation by bleach treatment, indicating that the effects were specific to bacteria and LPS and not just due to the presence of additional molecules (Fig. 4). Interestingly, the heat-stable PV-M132V mutant virus was inactivated by bleach to the same extent as PV-WT, and bacteria limited bleach inactivation of PV-M132V. These results suggest that thermal inactivation and bleach inactivation occur through separable mechanisms and that bacteria stabilize virions for both. Overall, these results indicate that bacteria enhance viral stability of fecal-orally transmitted picornaviruses during bleach treatment.
FIG 4.
Effects of bacteria on picornavirus stability during bleach treatment. A 1 × 105-PFU amount of virus was incubated individually in PBS, 1 mg/ml BSA, cellulose, LPS, or 1 × 108 CFU of bacterial strains at 37°C for 1 h. After incubation, samples were treated with 0.0001% bleach for 1 min and neutralized with sodium thiol sulfate. The amount of viable virus was determined by plaque assay and compared to PBS viral titer at 0 h to determine % of input PFU. Data are representative of 7 to 20 independent experiments (n = 4 to 40). Bars are shown for SEM. Statistical significance was determined by one-way ANOVA (*, P < 0.05).
Bacteria bind to a select panel of picornaviruses.
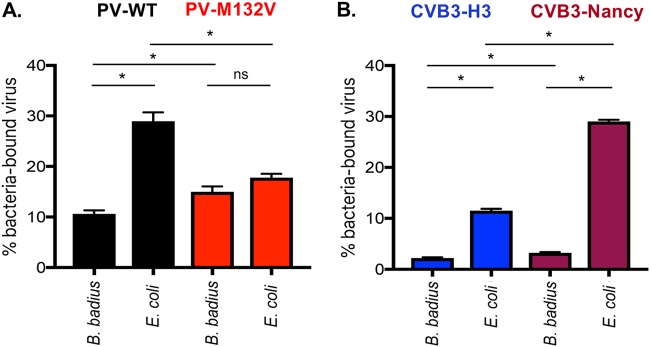
Since bacteria enhanced stability of specific picornaviruses during heat or bleach inactivation, we wanted to determine whether viruses directly interact with bacteria. In particular, we were curious whether bacterial binding efficiencies vary among closely related viruses, such as CVB3-Nancy and CVB3-H3, or between the PV-M132V heat-stable mutant and PV-WT. Previously, we showed that PV can bind directly to the surface of bacteria (3, 7, 14). 35S-labeled CVB3-Nancy, CVB3-H3, PV-WT, or PV-M132V was incubated with beads, B. badius, or E. coli for 1 h followed by centrifugation, washing, and scintillation counting of the bacterial pellets to quantify viral binding. We determined that PV-WT and PV-M132V bound to the two bacterial strains to approximately the same extent (Fig. 5A). This indicates that while the PV-M132V mutant does not require the presence of bacteria for stability during heat treatment, it still binds to bacteria, which could explain why bacteria limit bleach inactivation of PV-M132V (Fig. 4). Additionally, we determined that both CVB3 strains bind to the two bacterial strains tested (Fig. 5B). Interestingly, binding of CVB3-Nancy to E. coli was nearly 3-fold higher than that of CVB3-H3 (Fig. 5B). Overall, these results indicate that multiple picornaviruses bind to bacteria but with different efficiencies.
FIG 5.
Picornaviruses bind to bacteria. 35S-labeled viruses (3,000 cpm/approximately 1 × 106 PFU) were incubated with 1 × 108 CFU of bacteria for 1 h at 37°C. After incubation, samples were spun down and washed to remove unbound virus. Bound virus was quantified by scintillation counting. Data are representative of two independent experiments (n = 3 to 4). Bars are shown for SEM. *, P < 0.05, based on Student’s t test. ns, not significant.
DISCUSSION
The Picornaviridae family is diverse and includes a large number of medically relevant human pathogens. While it has been shown that bacteria promote infection, coinfection, and transmission of poliovirus, the impact of bacteria on other picornaviruses is unclear (3, 7, 14). Here, we show that bacteria increase stability of several viruses from the Picornaviridae family, likely through direct interactions.
Our data show that bacteria can vary in their capacity to enhance thermal stability of viruses within a single viral family. We determined that certain picornaviruses (Enterovirus genus members: CVB3-H3, CVB3-Nancy, and PV) are sensitive to heat treatment and that bacteria increase stability of these viruses (Fig. 2 and 3). We also determined that another picornavirus (Cardiovirus genus: mengovirus) has mixed phenotypes depending on the condition tested. While mengovirus was very stable at high temperatures during relatively short incubation times (4.5 h) and was not impacted by bacteria under these conditions, it was inactivated after 4 days at 37°C and exposure to feces reduced this inactivation (Fig. 3D). This suggests that mengovirus may be stabilized by bacteria at physiological temperatures in the host. Finally, we determined that a distantly related picornavirus (Kobuvirus genus: Aichi virus) is relatively resistant to high temperature but is not stabilized by bacteria or bacterial products (Fig. 2 and 3A). In fact, exposure to feces slightly reduced Aichi virus infectivity (Fig. 3A). Although Aichi virus is transmitted by the fecal-oral route, there are large sequence and structural differences between Aichi virus and other picornaviruses that may contribute to the different phenotype (Fig. 1A and B) (22, 23). Although a member of the Caliciviridae, human norovirus can bind to and is stabilized by bacteria that express certain histo-blood group antigens (24, 25). Similarly, reovirus (Reoviridae family) can be stabilized by exposure to certain bacteria or bacterial surface molecules, but stabilization efficiency and specificity vary among different reovirus strains (8). Taken together, these results indicate that viruses from separate viral families can be stabilized by bacteria but that not all viruses within a given family share phenotypes.
While picornaviruses vary in bacterial thermal stabilization, we found that bacteria enhanced viability of all picornaviruses tested during bleach treatment (Fig. 4). Although the PV-M132V mutant was not inactivated at high temperatures, it was inactivated by bleach treatment and bacteria limited this inactivation. Indeed, the PV-M132V virus was determined to bind to bacteria, which could explain stabilization during bleach treatment (Fig. 4). Thus, heat inactivation and bleach inactivation are independent and could have separate requirements for stabilization.
Bacterial strains, feces, and compounds varied in their ability to stabilize the panel of viruses. Generally, Gram-negative bacteria stabilized viruses more efficiently than Gram-positive bacteria. In several scenarios, LPS, rather than whole bacteria, had the most potent stabilizing activity. For example, LPS had the highest thermal stabilization for CVB3-Nancy and poliovirus (Fig. 2A and B), and LPS had the highest bleach stabilization of CVB3-H3, CVB3-Nancy, poliovirus, and mengovirus (Fig. 4). It is possible that purified LPS has more efficient binding to virions than glycans in the context of whole bacteria.
Overall, this study provides insight into the effects of bacteria on a panel of viruses from the same family, the Picornaviridae. Understanding the role of bacteria during stabilization of and infection by viruses could provide insight into efficient infection within specific hosts (i.e., harboring specific microbiota) as well as between hosts (i.e., environmental bacteria).
MATERIALS AND METHODS
Cells and viruses.
HeLa cells were propagated in Dulbecco’s modified Eagle’s medium (DMEM) supplemented with 10% calf serum and 1% penicillin-streptomycin. HeLa cells were used for CVB3, mengovirus, and PV propagation and quantification of viral titer by plaque assay (26–28). Vero cells were propagated in DMEM supplemented with 10% fetal bovine serum (FBS) and 1% penicillin-streptomycin. Vero cells were used for Aichi virus propagation and quantification of viral titer by plaque assay. All infections were performed using viruses derived from infectious cDNA clones (the mengovirus clone was a kind gift from Marco Vignuzzi) (29, 30). All viruses were confirmed by Sanger sequencing.
To quantify virus, plaque assay was performed as previously described (26, 27, 30) Briefly, virus was diluted in phosphate-buffered saline supplemented with 100 μg/ml CaCl2 and 100 μg/ml MgCl2 (PBS+) and added to cells for 30 min at 37°C in the presence of 5% CO2 to allow for attachment. Agar overlay containing DMEM, supplemented with 20% calf serum, and 2% agar was used for CVB3 and PV samples and removed after 48 h. Agar overlay containing DMEM, supplemented with 20% FBS, and 2% agar was used for Aichi virus samples and removed after 48 h. Agar overlay containing P5 buffer and 2% agar was used for mengovirus samples and removed after 48 h (27).
Radiolabeling of picornaviruses was performed as previously described (3, 7, 28). Briefly, viruses were propagated in the presence of [35S]cysteine-methionine and were purified using cesium chloride gradients. Purity of viruses was confirmed by phosphorimaging of radiolabeled capsid proteins on SDS-PAGE gels and scintillation count to determine cpm and viable fractions (3).
Bacterial strains.
Strains of bacteria were from ATCC or from the cecum of mice, as previously described (14). Cultures were inoculated from glycerol stocks in strain-specific nutrient medium as previously described (14). Briefly, cultures were grown overnight, and bacterial cell pellets were collected and washed in PBS+. After resuspension in 1 ml PBS+, OD600 values were obtained by spectrophotometer (Eppendorf BioPhotometer D30) to determine CFU needed specifically for each assay. Bacteria were UV inactivated prior to use in assays. The amount of bacteria was confirmed by plating on nutrient-specific agar and conditions prior to UV inactivation (14).
Quantifying picornavirus binding to bacterial cells.
The bacterial binding assay was performed as previously described for poliovirus (14). Briefly, approximately 3,000 cpm (approximately 1 × 106 PFU) of 35S-radiolabeled virus was mixed with PBS+ or 1 × 108 CFU of bacteria and incubated at 37°C in the presence of CO2 for 1 h. After incubation, bacteria were pelleted and washed with PBS+ to remove unbound virus. The amount of cpm (virus bound to bacterial cells) was determined by scintillation counting.
Quantifying effects of bacteria on virion stability.
To determine the effect of bacteria on thermal stability of picornaviruses, 1 × 105 PFU of each virus was mixed with PBS+, 1 mg/ml of bacterial surface polysaccharides, or 1 × 1010 CFU of bacteria and incubated at 44°C for 4.5 h. The same procedure was followed for elevated temperature assays. After incubation, plaque assays were performed using virus-specific conditions to determine the amount of viable virus before and after heat treatment.
The bleach inactivation assay was performed as previously described for PV, except that a lower concentration of bleach was used here (7). Briefly, 1 × 105 PFU of each virus was mixed with PBS+, 1 mg/ml of bacterial surface polysaccharides, or 1 × 108 CFU of bacteria. Samples were incubated at 37°C for 1 h and then added to 0.0001% fresh bleach for 1 min. Bleach neutralization was done by adding 0.01% sodium thiosulfate (Sigma). Plaque assays using virus-specific conditions were performed to determine the amount of viable virus before and after bleach treatment.
To examine effects of feces on viral stability, feces from 4- to 10-week-old male C57BL/6 PVR-IFNAR−/− mice were collected and resuspended in PBS+ to a final concentration of 0.0642 mg/μl. Briefly, 1 × 105 PFU of virus was mixed with 300 μl of PBS+ or resuspended fecal samples and incubated at 37°C in the presence of 5% CO2. Additional samples in PBS+ were placed at 4°C as a control. Samples were taken at designated time points and processed by chloroform extraction as previously described (3, 7). Plaque assay was performed to determine amount of viable virus before and at designated time points, as described earlier. In Fig. 3F, 1 × 105 PFU of mengovirus was mixed with approximately 1 × 105 CFU each of E. coli, P. ruminicola, and L. johnsonii in a total volume of 300 μl and samples were incubated at 37°C. Samples were collected and titers were determined as described above.
Mouse experiments.
Animals were handled according to the Guide for the Care and Use of Laboratory Animals (31). C57BL/6 PVR-IFNAR−/− mice were obtained from S. Koike (Tokyo, Japan) (32). Feces collection was performed at UT Southwestern Medical Center.
Data analysis.
Figures of viral structures were generated using the UCSF Chimera software (http://www.rbvi.ucsf.edu/chimera). The Electron Microscopy Data Bank (EMDB) IDs used for each virus are as follows: Aichi virus (EM-9517), CVB3 (EM-6637), and Saffold virus (EM-3097), to represent their respective genera. The phylogenetic tree was generated using the MEGA7 software and following the neighbor-joining method (33, 34). The optimal tree with the sum of branch length = 2.65090397 is shown. The tree is drawn to scale, with branch lengths in the same units as those of the evolutionary distances used to infer the phylogenetic tree. The evolutionary distances were computed using the Poisson correction method and are in the units of the number of amino acid substitutions per site (33). The analysis involved 5 amino acid sequences. All positions containing gaps and missing data were eliminated. There were a total of 766 positions in the final phylogeny tree data set.
All statistical analyses were performed using GraphPad Prism software. Outliers were identified and removed by the ROUT method, Q = 1%. All one-way ANOVAs were performed with Dunnett’s multiple-comparison post hoc test. All two-way ANOVAs were performed with Tukey’s post hoc test.
ACKNOWLEDGMENTS
We thank Andrea Erickson, Broc McCune, and Arielle Woznica for critical review of the manuscript. We thank Marco Vignuzzi for the mengovirus infectious clone. We thank Mikal Woods-Acevedo for providing 35S-labeled CVB3-H3 and CVB3-Nancy viruses. We also thank Nam Nguyen for assistance with structural modeling.
Molecular graphics and analyses were performed with the UCSF Chimera package. Chimera is developed by the Resource for Biocomputing, Visualization, and Informatics at the University of California, San Francisco (supported by NIGMS P41-GM103311).
Work in J.K.P.’s lab is funded through NIH NIAID grant R01 AI74668, a Burroughs Wellcome Fund Investigators in the Pathogenesis of Infectious Diseases Award, and a Faculty Scholar grant from the Howard Hughes Medical Institute. E.R.A. was supported in part by the National Science Foundation Graduate Research Fellowship grant 2014176649.
REFERENCES
- 1.Knipe DM, Howley PM, Cohen JI, Griffin DE, Lamb RA, Martin MA, Racaniello VR, Roizman B (ed). 2013. Fields virology, 6th ed. Lippincott Williams & Wilkins, Philadelphia, PA. [Google Scholar]
- 2.Sender R, Fuchs S, Milo R. 2016. Revised estimates for the number of human and bacteria cells in the body. PLoS Biol 14:e1002533. doi: 10.1371/journal.pbio.1002533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kuss SK, Best GT, Etheredge CA, Pruijssers AJ, Frierson JM, Hooper LV, Dermody TS, Pfeiffer JK. 2011. Intestinal microbiota promote enteric virus replication and systemic pathogenesis. Science 334:249–252. doi: 10.1126/science.1211057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kane M, Case LK, Kopaskie K, Kozlova A, MacDearmid C, Chervonsky AV, Golovkina TV. 2011. Successful transmission of a retrovirus depends on the commensal microbiota. Science 334:245–249. doi: 10.1126/science.1210718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Baldridge MT, Nice TJ, McCune BT, Yokoyama CC, Kambal A, Wheadon M, Diamond MS, Ivanova Y, Artyomov M, Virgin HW. 2015. Commensal microbes and interferon-lambda determine persistence of enteric murine norovirus infection. Science 347:266–269. doi: 10.1126/science.1258025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jones MK, Watanabe M, Zhu S, Graves CL, Keyes LR, Grau KR, Gonzalez-Hernandez MB, Iovine NM, Wobus CE, Vinje J, Tibbetts SA, Wallet SM, Karst SM. 2014. Enteric bacteria promote human and mouse norovirus infection of B cells. Science 346:755–759. doi: 10.1126/science.1257147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Robinson CM, Jesudhasan PR, Pfeiffer JK. 2014. Bacterial lipopolysaccharide binding enhances virion stability and promotes environmental fitness of an enteric virus. Cell Host Microbe 15:36–46. doi: 10.1016/j.chom.2013.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Berger AK, Yi H, Kearns DB, Mainou BA. 2017. Bacteria and bacterial envelope components enhance mammalian reovirus thermostability. PLoS Pathog 13:e1006768. doi: 10.1371/journal.ppat.1006768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Uchiyama R, Chassaing B, Zhang B, Gewirtz AT. 2014. Antibiotic treatment suppresses rotavirus infection and enhances specific humoral immunity. J Infect Dis 210:171–182. doi: 10.1093/infdis/jiu037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pfeiffer JK, Virgin HW. 2016. Viral immunity. Transkingdom control of viral infection and immunity in the mammalian intestine. Science 351:aad5872. doi: 10.1126/science.aad5872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ichinohe T, Pang IK, Kumamoto Y, Peaper DR, Ho JH, Murray TS, Iwasaki A. 2011. Microbiota regulates immune defense against respiratory tract influenza A virus infection. Proc Natl Acad Sci U S A 108:5354–5359. doi: 10.1073/pnas.1019378108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bandoro C, Runstadler JA. 2017. Bacterial lipopolysaccharide destabilizes influenza viruses. mSphere 2:e00267-17. doi: 10.1128/mSphere.00267-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nguyen Y, Jesudhasan PR, Aguilera ER, Pfeiffer JK. 2019. Identification and characterization of a poliovirus capsid mutant with enhanced thermal stability. J Virol 93:e01510-18. doi: 10.1128/JVI.01510-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Erickson AK, Jesudhasan PR, Mayer MJ, Narbad A, Winter SE, Pfeiffer JK. 2018. Bacteria facilitate enteric virus co-infection of mammalian cells and promote genetic recombination. Cell Host Microbe 23:77–88.e5. doi: 10.1016/j.chom.2017.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Plevka P, Perera R, Yap ML, Cardosa J, Kuhn RJ, Rossmann MG. 2013. Structure of human enterovirus 71 in complex with a capsid-binding inhibitor. Proc Natl Acad Sci U S A 110:5463–5467. doi: 10.1073/pnas.1222379110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Walter TS, Ren J, Tuthill TJ, Rowlands DJ, Stuart DI, Fry EE. 2012. A plate-based high-throughput assay for virus stability and vaccine formulation. J Virol Methods 185:166–170. doi: 10.1016/j.jviromet.2012.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Alvarez ME, O’Brien RT. 1982. Effects of chlorine concentration on the structure of poliovirus. Appl Environ Microbiol 43:237–239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.O’Brien RT, Newman J. 1979. Structural and compositional changes associated with chlorine inactivation of polioviruses. Appl Environ Microbiol 38:1034–1039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sharp DG, Floyd R, Johnson JD. 1975. Nature of the surviving plaque-forming unit of reovirus in water containing bromine. Appl Microbiol 29:94–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Goda H, Ikeda K, Nishide M, Nagao T, Koyama AH. 2018. Characterization of virucidal activities of chlorous acid. Jpn J Infect Dis 71:333–337. doi: 10.7883/yoken.JJID.2018.089. [DOI] [PubMed] [Google Scholar]
- 21.Wigginton KR, Pecson BM, Sigstam T, Bosshard F, Kohn T. 2012. Virus inactivation mechanisms: impact of disinfectants on virus function and structural integrity. Environ Sci Technol 46:12069–12078. doi: 10.1021/es3029473. [DOI] [PubMed] [Google Scholar]
- 22.Sabin C, Fuzik T, Skubnik K, Palkova L, Lindberg AM, Plevka P. 2016. Structure of Aichi virus 1 and its empty particle: clues to kobuvirus genome release mechanism. J Virol 90:10800–10810. doi: 10.1128/JVI.01601-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zhu L, Wang X, Ren J, Kotecha A, Walter TS, Yuan S, Yamashita T, Tuthill TJ, Fry EE, Rao Z, Stuart DI. 2016. Structure of human Aichi virus and implications for receptor binding. Nat Microbiol 1:16150. doi: 10.1038/nmicrobiol.2016.150. [DOI] [PubMed] [Google Scholar]
- 24.Li D, Breiman A, le Pendu J, Uyttendaele M. 2015. Binding to histo-blood group antigen-expressing bacteria protects human norovirus from acute heat stress. Front Microbiol 6:659. doi: 10.3389/fmicb.2015.00659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Miura T, Sano D, Suenaga A, Yoshimura T, Fuzawa M, Nakagomi T, Nakagomi O, Okabe S. 2013. Histo-blood group antigen-like substances of human enteric bacteria as specific adsorbents for human noroviruses. J Virol 87:9441–9451. doi: 10.1128/JVI.01060-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pfeiffer JK, Kirkegaard K. 2003. A single mutation in poliovirus RNA-dependent RNA polymerase confers resistance to mutagenic nucleotide analogs via increased fidelity. Proc Natl Acad Sci U S A 100:7289–7294. doi: 10.1073/pnas.1232294100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rueckert RR, Pallansch MA. 1981. Preparation and characterization of encephalomyocarditis (EMC) virus. Methods Enzymol 78:315–325. doi: 10.1016/0076-6879(81)78136-9. [DOI] [PubMed] [Google Scholar]
- 28.Wang Y, Pfeiffer JK. 2016. Emergence of a large-plaque variant in mice infected with coxsackievirus B3. mBio 7:e00119-16. doi: 10.1128/mBio.00119-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Racaniello VR, Baltimore D. 1981. Molecular cloning of poliovirus cDNA and determination of the complete nucleotide sequence of the viral genome. Proc Natl Acad Sci U S A 78:4887–4891. doi: 10.1073/pnas.78.8.4887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sasaki J, Kusuhara Y, Maeno Y, Kobayashi N, Yamashita T, Sakae K, Takeda N, Taniguchi K. 2001. Construction of an infectious cDNA clone of Aichi virus (a new member of the family Picornaviridae) and mutational analysis of a stem-loop structure at the 5′ end of the genome. J Virol 75:8021–8030. doi: 10.1128/JVI.75.17.8021-8030.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.National Research Council. 2011. Guide for the care and use of laboratory animals, 8th ed National Academies Press, Washington, DC. [Google Scholar]
- 32.Ida-Hosonuma M, Iwasaki T, Yoshikawa T, Nagata N, Sato Y, Sata T, Yoneyama M, Fujita T, Taya C, Yonekawa H, Koike S. 2005. The alpha/beta interferon response controls tissue tropism and pathogenicity of poliovirus. J Virol 79:4460–4469. doi: 10.1128/JVI.79.7.4460-4469.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kumar S, Stecher G, Tamura K. 2016. MEGA7: Molecular Evolutionary Genetics Analysis version 7.0 for bigger datasets. Mol Biol Evol 33:1870–1874. doi: 10.1093/molbev/msw054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tamura K, Nei M, Kumar S. 2004. Prospects for inferring very large phylogenies by using the neighbor-joining method. Proc Natl Acad Sci U S A 101:11030–11035. doi: 10.1073/pnas.0404206101. [DOI] [PMC free article] [PubMed] [Google Scholar]