Abstract
Transportation is an important social determinant of health. Transportation barriers disproportionately affect the most vulnerable groups of society who carry the highest burden of chronic diseases; therefore, it is critical to identify interventions that improve access to transportation. We synthesized evidence concerning the types and impact of interventions that address transportation to chronic care management. A systematic literature search of peer-reviewed studies that include an intervention with a transportation component was performed using three electronic databases —PubMed, EMBASE, and CINAHL—along with a hand-search. We screened 478 unique titles and abstracts. Two reviewers independently evaluated 41 full-text articles and 10 studies met eligibility criteria for inclusion. The transportation interventions included one or more of the following: providing bus passes (n=5), taxi/transport vouchers or reimbursement (n=3), arranging or connecting participants to transportation (n=2), and a free shuttle service (n=1). Transportation support was offered within multi-component interventions including counseling, care coordination, education, financial incentives, motivational interviewing, and navigation assistance. Community health/outreach workers (n=3), nurses (n=3), and research or clinic staff (n=3) were the most common interventionists. Studies reported improvements in cancer screening rates, chronic disease management, hospital utilization, linkage and follow up to care, and maternal empathy. Overall, transportation is a well-documented barrier to engaging in chronic care among vulnerable populations. We found evidence suggesting transportation services offered in combination with other tailored services improves patient health outcomes; however, future research is warranted to examine the separate impact of transportation interventions that are tested within multi-component studies.
Keywords: Chronic disease, Healthcare access, Systematic review, Transportation
Introduction
While overall life expectancy has increased since the 1940s, chronic conditions remain the top three causes of death, with heart disease and cancer accounting for 45% of all deaths in 2015 [1, 2]. Chronic diseases by nature require patients to have capacity and stamina to manage their treatment effectively. Efforts to meet goals and/or decrease burden of illness, though, can last a span of years or decades. To manage their illness, chronic care patients are tasked to consistently make outpatient clinic appointments and obtain medications. Access to transportation, therefore, is a necessity to ensure the completion of this care [3].
A 2005 report by the Transportation Research Board of the National Academies found that 3.6 million Americans delay or miss medical care due to a transportation barrier each year [4]. Transportation is an important social determinant of health, acting as a facilitator or barrier to health self-management [5, 6]. Known factors that influence access to transportation include socioeconomic status, ethnicity, geography (i.e., urban vs. rural), age, mode and type of travel, and distance or time burden [7]. Inaccessibility to health care due to lack of transportation affects the most vulnerable groups of society such as low-income inner-city residents who often belong to racial/ethnic minority communities [6, 8]. Multiple nationally-representative datasets have revealed that patients in ethnic minority groups were less likely to obtain medical care due to transportation barriers, controlling for socioeconomic status, and that patients who were White generally had increased access over those identifying as non-White [7], suggesting that transportation options are limited in minority communities.
Efforts have been made to mitigate the impact of transportation as a barrier to vulnerable communities affected by chronic illness. In recent literature, researchers have reported that when transportation services are offered to low-income patients through public health programs such as Medicaid, the highest users of such services are African Americans [6]. In fact, Medicaid beneficiaries who use non-emergency medical transportation services are significantly more likely to make the recommended number of annual visits for the management of chronic conditions than those who do not use the services [6].
Although a number of studies to date have aimed to improve access to chronic care by providing an intervention at the level of transportation, clear evidence on the effectiveness of these interventions is lacking, as they are often embedded within multicomponent studies [8–11]. There is a need to uncover the type and effect of transportation services in currently published research, where differences might exist in health outcomes for vulnerable populations with chronic conditions. Therefore, the objectives of this article are to: (1) review and synthesize the existing research regarding transportation as an intervention in chronic care management, and (2) discuss potential gaps and need for further research on this topic.
Methods
Search Strategy
A systematic search of peer-reviewed literature on interventions that included transportation assistance was undertaken. In consultation with a medical librarian, we searched PubMed, Embase, and CINAHL. Medical Subject Headings (MeSH) and non-MeSH search terms included variations of transportation, motor vehicle, automobile, taxi, hired transportation, Uber, Lyft, public transportation, bus, subway, travel voucher, health services research, participatory research, nursing research, clinical trials, and health services administration. We also included terms to limit our search to the top 10 chronic diseases, including: diabetes mellitus, neoplasms, cardiovascular disease, hypertension, dementia, depressive disorder, arthritis, osteoporosis, chronic obstructive pulmonary disease, plus HIV and chronic disease [12].
Study Eligibility
Peer-reviewed, original research articles written in English were included if they described an intervention with at least one component aimed at addressing transportation of the patient or participant in the context of chronic care (i.e., prevention or management of a chronic condition). All quantitative study designs were included. The search was conducted in January 2018 and comprised research published since 1992. Non-research articles or those that described no intervention were excluded.
Selection and Data Extraction
Two authors (L.S. and C.D.) independently screened the titles and abstracts of articles retrieved in the search. This screening was followed by a full text review by both authors. Conflicts were resolved through discussion. Data were then extracted by two or more reviewers (C.D., C.-A.S., and L.S.) from the eligible full text articles using a standardized extraction table developed for this review. The primary interest of this study was the transportation component of an intervention; therefore, data on multiple chronic care-related outcomes were examined.
The literature search yielded a total of 486 potentially relevant references in our initial search, including 12 duplicates. After title and abstract review, 40 studies advanced to full text review. Twenty-six of those were excluded for the following reasons: the intervention did not include a transportation component (n=15), the study design did not include an intervention (n=8), the article did not describe a research study (n=2), and full text of the article could not be located (n=1). Further exclusion occurred of four studies: the study addressed recruitment/retention only and did not report on any outcome related to chronic care (n=3); and the study was not a research study but a quality improvement project (n=1). Thus, 10 studies met inclusion criteria and were relevant to the question addressed in this review (Figure 1).
Figure 1.
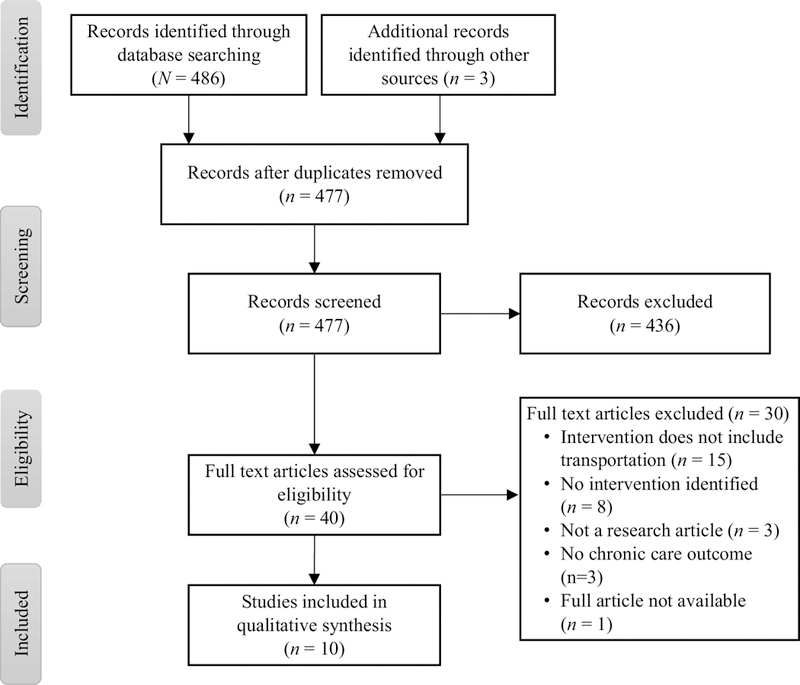
PRISMA flow diagram
Quality Assessment
Two reviewers (C.S. and H.H.) independently assessed the rigor of each included article using the Joanna Briggs Institute (JBI) quality appraisal tool [13]. Each research study’s methodological characteristics were evaluated using the corresponding tool according to study design (randomized controlled trial [RCT], quasi-experimental and cohort study). Studies were not excluded based on the quality appraisal; rather, the quality appraisal was used to evaluate and discuss the rigor of available evidence, including methodological gaps. Inter-rater agreement rates ranged from 69% to 100% with an average of 88%. Any discrepancies that occurred between raters were resolved via inter-rater discussion.
Results
Overview of studies included in the review
The systematic search revealed research studies from three different countries (Canada, Uganda, and United States) using RCT (n=5), quasi-experimental (n=4) or cohort (n=1) designs (Table 1). All studies included community-based adult participants and enrolled participants based on socioeconomic status or a chronic disease diagnosis or risk. Three studies comprised adults with hypertension [9, 14, 15] and one included adults with asthma, diabetes, depression, or obesity [14]. Other studies focused on patients overdue for cancer screenings, including colorectal cancer [10] cervical cancer [11, 16, 17], and mammography [18]. One study examined patients enrolled in Medicaid [19].
Table 1.
Studies reporting interventions to improve transportation to chronic care management
| Author & publication year | Sample & recruitment setting | Methods | Transportation intervention (Interventionist) | Additional intervention components | Main findings |
|---|---|---|---|---|---|
| Esperat et al., 2012 | N = 152 adults with diabetes, hypertension, asthma, co-morbidities of obesity, and depression Federally-qualified nurse-managed health center (Texas, USA) |
Quasi-experimental pre-post | Guidance on how to purchase bus passes (Community health worker [promotora]) |
Home visits, phone calls, motivational interviewing, self-care goal setting, social support assessments | Average HbA1c, blood pressure, HDL, and LDL decreased Triglycerides increased Chronic disease management and diabetes self-efficacy improved |
| Kaplan et al., 2000 | N = 4488 females with abnormal pap smear, 92% Hispanic Urban hospitals, public health centers, comprehensive health centers, (Los Angeles, CA, USA) |
Quasi-experimental Before-after nonequival ent control group |
Free mailed bus passes for 2 round-trip fares for follow-up care (Research staff including nurses) |
Tracking follow-up protocol including personal letter and informational brochures, phone calls, financial incentives to return for follow-up | Intervention group had 5.4% higher follow-up rate in year 2 (p<.05), 9.1% higher in year 4 (p<.05), and 4.5% higher years 2–4 (p<.0001) Control group had higher follow-up rate in year 3 at the CHC sites (p<.05) |
| Kotwani et al., 2014 | N = 214 hypertensive adults, 47% female, 32% no education Rural community health campaign (Southwest Uganda) |
Quasi-experimental | Transport voucher reimbursable for cost of a one-way journey to health center (Nurse) |
Individual education/counselin g session and referral appointment to nearest local health facility or regional hospital | 83% linked to care within 6 months; median time to link 22 days Age >60 years more likely to link than age 18–29 years Higher education more likely to link to care Men less likely than women to link to care Those referred to local health center more likely to go compared to referred to regional hospital |
| Krieger et al., 1999 | N = 421 adults with elevated blood pressure and income <200% federal poverty level, 72% male, 79% Black/African American, 40% uninsured, 24% less than high school education Public spaces in urban low-income neighborhoods (Seattle, WA, USA) |
Randomized controlled trial | Referral to community transportation (Community health worker) | Referral to medical care, assistance scheduling medical appointment, appointment reminder letter, post-appointment follow-up, referral to services to reduce barriers to care | Intervention group had 39% higher follow-up rate to medical care than control (p=0.001) |
| Marcus et al., 1992 | N=2044 low-income women with abnormal pap smear, 69% minority non-white, 44% less than high school education, 69% no insurance Urban/suburban primary health care clinics (Los Angeles, CA, USA) |
Randomized controlled trial | Bus tickets mailed with letter that follow-up care is needed; passes for two one-way fares, two express bus supplemental fares, and five transfers ($2.00-$2.90 total); option of $2.00 parking permit (Clinic staff) |
Personalized follow-up letter and educational pamphlet, a slide-tape program on pap smears | Transportation incentives (OR = 1.48, p<.05) and the combined intervention with personalized follow-up and slide-tape program (OR 2.3, p<.01) both improved screening follow-up rate Transportation incentives alone improved return rates among county patients (OR: 1.51; p<.05), more severe pap smear results (OR 1.71; p<.05) and noninsured patients (OR: 1.77; p<.01). |
| Niccols et al., 2005 | N = 13 mothers age 21–36 with substance use disorder and their children (0–6 years), 85% low SES, 69% involved with child protection agency Central site (Hamilton, Ontario, Canada) |
Quasi-experimental Pilot pre-post |
Bus tickets provided (Staff members) |
Program 2 days/week with individual and group addictions counseling, nutrition counseling and grocery vouchers, skill development, parenting education and counseling, peer support, children’s programming Linkage to family medical services, home nurse visits, developmental services |
Maternal empathy improved at 3 months (p<0.05) Child’s social competence improved at 6 months (p<0.05) No significant change in substance use, use of health and childcare services, social support, or diet |
| Percac-Lima et al., 2009 | N = 1223 low-income, ethnically diverse adults 52–79 years old overdue for colorectal cancer screening, 59% female, 34% Spanish-speaking, 29% government insurance Urban primary clinics and community health centers (Boston, MA, USA) |
Randomized controlled trial | Free shuttle provided to hospital for colorectal cancer screening appointments, or taxi vouchers to get home (Patient navigators) |
Letter with educational material, phone or in-person patient education to overcome barriers to screening, procedure scheduling, translation, insurance support | Intervention more likely to undergo screening (15%) and colonoscopy (11%) than control (p<0.001). Effective in all patient subgroups regardless of gender, language, race/ethnicity, or insurance status. |
| Taylor et al., 1999 | N = 314 women age 50–74 due for mammography, 39% Black/African American, 66% Medicaid/Medicare Inner-city primary care clinic (Seattle, WA, USA) |
Randomized controlled trial | Bus passes provided to attend mammography appointments (Nurse) |
Nursing care coordination, video and printed patient education, appointment reminder phone calls and postcards, rescheduling assistance, provider education, provider computer prompts | Intervention improved mammograph y completion in 8 weeks by 27% (p<0.001). Only 4% of participants (n = 6) accepted bus passes |
| Taylor et al., 2002 | N = 482 Chinese women under-utilizing pap testing, 57% less than high school education, 3% English speaking, 54% lived in North America <25 years Urban (Seattle, WA, USA and Vancouver, BC, Canada) |
Randomized controlled trial | Taxi transportation to and from clinic appointments or two bus passes (Outreach worker) |
Education-entertainment video, motivational pamphlet, educational brochure, fact sheet, tailored counseling and logistic assistance | Intervention group more likely to report pap testing in 6 months than control (p<0.001) Few participants accepted transportation assistance |
| Tierney et al., 2000 | N = 23,707 (1994) compared to N = 23,015 (1993) Medicaid patients, 66% female, 60% Black/African American Urban inner-city public hospital (Indiana, USA) |
Cohort study Historical comparison |
Automatic reimbursement for <10 round trips to medical care per year, with prior authorization required for >9 trips (Medicaid policy change) |
None | Primary care visits declined 16% (p<0.001) Neighborhood health center visits increased 7% (p<0.001) Emergency and urgent visits decreased 8% (p<0.001) Medication refill visits decreased 18% (p<0.001) Blood pressure increased (systolic p=0.01; diastolic p=0.003) Visits for reactive airway disease decreased (p<0.001) |
Note: CHC = comprehensive health center; HbA1c = hemoglobin A1c; OR = odds ratio
The sample characteristics varied across studies. All studies focused on populations disproportionately affected by or at risk for a chronic illness with previously identified barriers to accessing primary care or follow-up care. Five of 10 studies (50%) enrolled women only [11, 16–18, 20], while one limited enrollment to older adults [18]. One study included children with their mothers [20]. In addition, one study focused solely on patients receiving Medicaid [19]. The one study from Uganda was conducted in a rural setting [9].
Quality of included studies
Results of the JBI quality assessments are detailed in Table 2. The average rating of JBI quality scores for the five randomized controlled trials was 8.2 of a maximum possible score of 13 (range 7 to 10). Two studies were rated high-quality (9 or higher) [11, 15] and three studies fell under the medium-quality category (scores of 5 to 8) [10, 17, 18]. Three of the RCTs did not apply true randomization for assignment of participants to treatment groups [10, 17, 18] and only one study indicated that the allocation to treatment groups was concealed [15]. In addition, no RCTs discussed any type of blinding.
Table 2.
Quality ratings
| Randomized controlled trial | |||||
|---|---|---|---|---|---|
| Items | Krieger et al., 1999 | Marcus et al., 1992 | Percac-Lima et al., 2009 | Taylor et al., 1999 | Taylor et al., 2002 |
| 1. Was true randomization used for assignment of participants to treatment groups? | 0 | 0 | 0 | 0 | 1 |
| 2. Was allocation to treatment groups concealed? | 1 | 0 | 0 | 0 | 0 |
| 3. Were treatment groups similar at the baseline? | 1 | 0 | 1 | 0 | 1 |
| 4. Were participants blind to treatment assignment? | 0 | 0 | 0 | 0 | 0 |
| 5. Were those delivering treatment blind to treatment assignment? | 0 | 0 | 0 | 0 | 0 |
| 6. Were outcomes assessors blind to treatment assignment? | 0 | 0 | 0 | 0 | 0 |
| 7. Were treatment groups treated identically other than the intervention of interest? | 1 | 1 | 1 | 1 | 1 |
| 8. Was follow up complete and if not, were differences between groups in terms of their follow up adequately described and analyzed? | 1 | 1 | 1 | 1 | 1 |
| 9. Were participants analyzed in the groups to which they were randomized? | 1 | 1 | 1 | 1 | 1 |
| 10. Were outcomes measured in the same way for treatment groups? | 1 | 1 | 1 | 1 | 1 |
| 11. Were outcomes measured in a reliable way? | 1 | 1 | 1 | 1 | 1 |
| 12. Was appropriate statistical analysis used? | 1 | 1 | 1 | 1 | 1 |
| 13. Was the trial design appropriate, and any deviations from the standard RCT design (individual randomization, parallel groups) accounted for in the conduct and analysis of the trial? | 1 | 1 | 1 | 1 | 1 |
| Total Score | 10 | 7 | 8 | 7 | 9 |
| Quasi-Experimental Study | |||||
| Items | Esperat et al., 2012 | Kaplan et al., 2000 | Kotwani et al, 2014 | Niccols et al., 2005 | |
| 1. Is it clear in the study what is the ‘cause’ and what is the ‘effect’ (i.e. there is no confusion about which variable comes first)? | 1 | 1 | 1 | 1 | |
| 2. Were the participants included in any comparisons similar? | 1 | 0 | 1 | 1 | |
| 3. Were the participants included in any comparisons receiving similar treatment/care, other than the exposure or intervention of interest? | 1 | 1 | 1 | 1 | |
| 4. Was there a control group? | 0 | 1 | 0 | 0 | |
| 5. Were there multiple measurements of the outcome both pre and post the intervention/exposure? | 1 | 1 | 0 | 1 | |
| 6. Was follow up complete and if not, were differences between groups in terms of their follow up adequately described and analyzed? | 0 | 1 | 0 | 1 | |
| 7. Were the outcomes of participants included in any comparisons measured in the same way? | 1 | 1 | 1 | 1 | |
| 8. Were outcomes measured in a reliable way? | 0 | 1 | 0 | 1 | |
| 9. Was appropriate statistical analysis used? | 1 | 1 | 1 | 1 | |
| Total Score | 6 | 8 | 5 | 8 | |
| Cohort Study | |||||
| Items | Tierney et al., 2000 | ||||
| 1. Were the two groups similar and recruited from the same population? | 1 | ||||
| 2. Were the exposures measured similarly to assign people to both exposed and | 1 | ||||
| unexposed groups? | |||||
| 3. Were the exposure measured in a valid and reliable way? | 1 | ||||
| 4. Were confounding factors identified? | 1 | ||||
| 5. Were strategies to deal with confounding factors stated? | 1 | ||||
| 6. Were the groups/participants free of the outcome at the start of the study? | 1 | ||||
| 7. Were the outcomes measured in a valid and reliable way? | 1 | ||||
| 8. Was the follow up time reported and sufficient to be long enough for outcomes to occur? |
1 | ||||
| 9. Was follow up complete, and if not, were the reasons to loss to follow up described and explored? | 1 | ||||
| 10. Were strategies to address incomplete follow up utilized? | 1 | ||||
| 11. Was appropriate statistical analysis used? | 1 | ||||
| Total Score | 8 | ||||
Four quasi-experimental studies had an average JBI quality rating of 6.8 (range 5 to 8; maximum possible score=9). Two studies met the criterion of high-quality (7 or greater) [16, 20], while the other two were of medium-quality (scores of 4 to 6) [9, 14]. Only one quasi-experimental study had a control group [16].
One article included in this review described a cohort study [19]. The study had a quality rating of 8 out of 11, indicating an overall good quality of the study methods used [21].
Description of transportation interventions
We found substantial heterogeneity in the type of transportation interventions utilized and the way in which the transportation interventions were administered in the included studies. Half of the studies provided bus passes to participants [11, 16–18, 20], whereas three studies (30%) gave participants taxi/transport vouchers [9–11]. Participants received anywhere from one round trip bus fare including transfers [11, 17] to two round trip fares [16]. Two articles did not specify the type or amount of bus passes provided [18, 20]. For the studies using taxi/transport vouchers, the vouchers were reimbursable at the follow-up visit in an amount comparable to the cost of a one-way trip [9], or a voucher was given ahead of time for round trip to and from a clinic visit [11]. In Percac-Lima et al. [10], participants who requested it were provided with a free shuttle service from home to the medical appointment, with the option of a taxi voucher to return home.
Two studies aided connecting participants to transportation in the form of guidance on how to purchase bus passes [14] and providing a referral to community transportation [15]. Finally, one study examined the effect of Medicaid reimbursement policy changes for transportation in the state of Indiana [19]. Prior to the policy change, patients could be reimbursed for any number of round trips to and from medical care per year. The change included a new prior authorization requirement for any transportation reimbursement beyond nine round trips.
In addition to heterogeneity of the types of transportation interventions, we found that 8 of the 10 studies did not isolate the transportation assistance intervention within multifaceted interventions. With the exception of the study examining Medicaid’s transportation reimbursement policy [19], transportation support was offered within multi-component interventions in all studies. Patient navigation – including assistance with appointment scheduling, appointment reminders, and referrals to care – commonly accompanied a transportation service provided by community health workers, outreach workers, and nurses [9–11, 16–18, 20]. Chronic disease-specific education via mailed brochures and pamphlets from patient navigators and clinic staff, phone calls by research staff, or in-person visits with nurses and outreach workers also accompanied a transportation intervention in 70% of studies [9–11, 16–18, 20]. Community health workers and staff provided social service assistance such as a translation aid, insurance support, nutrition counseling, grocery vouchers, financial incentives, and social support assessments in conjunction with transportation assistance in four (40%) of the studies [10, 14, 16, 20].
Outcomes of transportation interventions
The studies included in this systematic review reported on multiple outcomes. Researchers reported results specific to the transportation component of their interventions in only two studies (20%) [17, 19]; the remaining eight studies primarily had interventions involving community health workers, nursing, outreach or navigator programs that included transportation but did not isolate it against the outcomes [9–11, 14–16, 18, 20].
Most transportation interventions sought to improve healthcare utilization. Healthcare utilization was measured as number of visits to the emergency department, outpatient care or hospital admissions [19], linkage to or receipt of care [9–11, 15, 18], and social service use [20]. Researchers reported that interventions including transportation had a greater effect on healthcare utilization outcomes among older adult participants [9, 10, 18]. Requiring a prior authorization for transportation reimbursement through Medicaid was associated with reduced visits to the emergency department; however, researchers also reported a decline in visits for medication refills and an increase in blood pressure among patients with hypertension [19]. Transport vouchers combined with education, individual counseling, and referral to care were associated with a high proportion of participants linking to care (83%) [9]. Furthermore, community health workers who coordinated care via appointment scheduling and referral to community transportation increased the rate of follow-up to hypertension care [15]. Follow-up for abnormal pap smears, mammography completion, and colorectal cancer screening improved when bus tickets, taxicab vouchers, or a free shuttle were offered within multi-component interventions that included education and social services [10, 11, 17, 18]. However, free bus passes had a mixed effect on follow-up rates when paired with an appointment tracking and reminder system [16].
Medical outcomes were also measured. Provision of bus tickets within a counseling and education program for substance use and parenting significantly improved maternal empathy and children’s social competence with trends toward decreased substance use and improved diet in a sample of mothers with substance use disorder and their children [20]. Esperat and colleagues reported that helping participants purchase bus passes in addition to home visits with motivational interviewing and self-care goal-setting significantly improved hemoglobin A1c, cholesterol, chronic care self-management, and diabetes self-efficacy among participants with chronic disease at a community health center [14].
Discussion
Although transportation is a well-documented barrier to engaging in the care of chronic diseases, evidence-based interventions to minimize this barrier are limited. Studies included in this review reported mixed effects, but indicated overall improvements in healthcare utilization and chronic care medical outcomes when multi-component interventions including transportation assistance were provided. Specifically, we found evidence suggesting bus passes, taxi vouchers, and free or reimbursed transportation costs offered in combination with other tailored services improves patient health outcomes, particularly among older patients and women.
The studies included in this review reported on diverse and socioeconomically disadvantaged samples such as minority [11, 16, 18], low education [9], and low-income communities [10, 14, 15, 17, 19, 20], representing the populations that are most affected by transportation barriers. Transportation barriers are especially prevalent among older adults, leading to risk of delays in care seeking, worsening health, and higher healthcare costs [7]. Because older adults are more likely to have more than one chronic condition [22, 23], they may also require more frequent clinic visits than the general population. Thus, incorporating transportation as part of chronic care seems an important avenue to consider for older adults in particular. When providing transportation services, transportation type in conjunction with population characteristics may be important to consider. For example, the findings of this review suggest that individualized transportation services using a free shuttle or taxi vouchers were effective in helping older adults engage in chronic care, including link to hypertension care and complete colorectal cancer screening [9, 10]. In contrast, in a study by Taylor and colleagues [18], only 4% of women participants ages 50–74 actually accepted the bus passes offered to return for mammography appointments. The authors note that the bus was likely not the preferred transportation mode in this group. This finding is consistent with prior data that older adults use public transportation at a lower rate than younger and middle-aged adults [24].
The type of transportation interventions offered must be congruent with the needs of the population. Clearly, for some demographics, options beyond public transportation to chronic health care need to be considered. With the expansion of supplemental healthcare benefits announced by the Centers for Medicare & Medicaid Services in April of 2018, additional reimbursement for transportation for the most vulnerable citizens may be on the horizon [25]. Similarly, in 2017, Blue Cross Blue Shield partnered with Lyft, an on-demand ride-sharing mobile application, to provide transportation to medical care for its insured [26]. Given that our review did not find any articles that included car services such as Lyft as a transportation intervention, future research will be needed in this area; we are likely on the precipice of a new era of transportation options for people living with chronic diseases.
We observed a number of methodological challenges in the studies included in the review. High attrition rates ranging from 26% to 31% were found in several studies [9, 15, 17]. True randomization did not apply in several RCTs [10, 17, 18], leading to dissimilar group characteristics [17, 18]. Secondly, the study designs precluded blinding of intervention status for all included RCTs [10, 11, 15, 17, 18]. Finally, ascertainment of the intervention effect might be unclear because self-report was used often to measure outcomes such as whether a participant received care, which could not be confirmed by the researchers [10, 11, 15, 18]. Among quasi-experimental studies, a small sample size was notable [20] and often with no comparison group [9, 14, 20].
Based on the findings from this systematic review, future research is warranted to examine the isolated impact of transportation interventions that are tested within multi-component studies. Only two studies looked at the effect of the transportation intervention alone [17, 19] and one compared this effect to the combined effect of the multi-component intervention [17]. Hence, we do not have sufficient evidence to support whether the transportation components are responsible for improving outcomes in chronic care management. In addition, descriptions of transportation interventions were not specific enough to be reproduced. Some papers in this review included only a single sentence noting that a type of transportation was provided, without further explanation [14, 15, 20]. The depth of reporting of transportation interventions needs to be improved to fully assess their effect on healthcare utilization and chronic disease health outcomes.
This systematic review has some limitations. We included only articles written in English; therefore, the findings cannot be generalized to studies published in non-English languages and relevant articles may have been excluded. Another limitation is the heterogeneity in the quality and quantity of data reported in the ten studies, limiting our ability to conduct a more rigorous analysis such as meta-analysis. To expand our results, we included outcomes related to the top ten chronic diseases in the United States; however, this led to numerous outcomes measured by the included studies that are not easily comparable. As more research is published that intervenes at the level of transportation, a review of these interventions’ effect on specific health outcomes will be needed. While it is possible our search terms missed relevant research, the fact that we only identified ten studies that met our inclusion criteria is noteworthy. Our small sample indicates that transportation interventions are not well identified or described in the published literature; greater standardization in reporting of transportation interventions, desired outcomes, and measurement of their effect has previously been called for [7] and is still a need in this field.
Conclusions
This systematic review found evidence to support the provision of bus passes, taxi vouchers, and reimbursement for transportation to improve healthcare utilization and chronic disease health outcomes among diverse socioeconomically disadvantaged populations, particularly older adults. However, current transportation interventions are reported within heterogeneous multi-component interventions, limiting our ability to independently assess their effect on reported outcomes. Future research must thoroughly describe and isolate transportation interventions to determine the type, cost, and effect of different transportation strategies to improve chronic care management in vulnerable populations.
Acknowledgments
Funding: This study was supported by a grant from the Brancati Center for the Advancement of Community Care. Additional resources were provided by Center for Cardiovascular and Chronic Care and Center for Community Innovation and Scholarship at the Johns Hopkins University.
Appendix 1. Complete Search Strategy
| PubMed | |||
| January 5, 2018 | |||
| 146 results | |||
| ((((((“Transportation of Patients”[Mesh:NoExp] OR “Transportation”[Mesh:NoExp] OR “Motor Vehicles”[Mesh:NoExp] OR “Automobiles”[Mesh] OR automobile* [tiab] OR autos [tiab] OR taxi [tiab] OR taxis [tiab] OR uber [tiab] OR lyft [tiab] OR “hired transportation” OR “public transportation” OR bus [tiab] OR busses [tiab] OR subway [tiab] OR “travel voucher” [tiab])))) AND (“Health Services Research”[Mesh] OR “Community-Based Participatory Research”[Mesh] OR “Nursing Research”[Mesh] OR “Clinical Trials as Topic”[Mesh] OR “Clinical Trial” [Publication Type] OR interven* [tiab] OR random* [tiab]) AND (“Health Services Administration”[Mesh] OR “Health Services”[Mesh] NOT “Emergency Medical Services”[Mesh]) AND ((((((((((“Diabetes Mellitus”[Mesh]) OR “HIV”[Mesh]) OR “Neoplasms”[Mesh]) OR “Cardiovascular Diseases”[Mesh]) OR “Hypertension”[Mesh]) OR “Dementia”[Mesh]) OR “Depressive Disorder”[Mesh]) OR “Arthritis”[Mesh]) OR “Osteoporosis, Postmenopausal”[Mesh]) OR “Pulmonary Disease, Chronic Obstructive”[Mesh] OR “Chronic Disease”[Mesh]) | |||
| CINAHL Plus | |||
| January 5, 2018 | |||
| 175 results | |||
| Search ID# | Search Terms | Search Options | Number of Items |
| S4 | S1 AND S2 AND S3 | Search modes – Boolean/Phrase | 175 |
| S3 | MH diabetes mellitus OR MH osteoporosis OR MH chronic disease OR MH hiv OR MH hiv/aids OR MH neoplasm OR MH cardiovascular disease OR MH hypertension OR MH dementia OR MH depression OR MH arthritis OR MH chronic obstructive pulmonary disease | Search modes – Boolean/Phrase | 259,866 |
| S2 | MH health services research OR MH community based participatory research OR MH nursing research OR MH clinical trials as topic OR MH clinical trials OR AB interven* OR AB random* | Search modes – Boolean/Phrase | 515,457 |
| S1 | MH transportation OR MH patient transportation OR MH motor vehicle OR MH automobile OR TX taxi OR TX taxicab OR TX uber OR TX lyft OR TX travel voucher OR TX public transportation OR TX bus OR TX subway train | Search modes – Boolean/Phrase | 23,433 |
| Embase | |||
| January 5, 2018 | |||
| 161 results | |||
| #5: #1 AND #2 AND #3 AND #4 | |||
| 161 | |||
| #4: ‘diabetes mellitus’/exp OR ‘human immunodeficiency virus infection’/exp OR ‘osteoporosis’/exp OR ‘chronic disease’/exp OR ‘neoplasm’/exp OR ‘cardiovascular disease’/exp OR ‘hypertension’/exp OR ‘dementia’/exp OR ‘depression’/exp OR ‘arthritis’/exp OR ‘chronic obstructive lung disease’/exp | |||
| 9,877,679 | |||
| #3: ‘health service’ OR ‘health care utilization’ | |||
| 553,521 | |||
| #2: ‘health services research’ OR ‘participatory research’ OR ‘nursing research’ OR ‘clinical trial (topic)’ OR ‘clinical trial’ OR ‘intervention study’ OR ‘randomized controlled trial’ | |||
| 1,720,531 | |||
| #1: ‘traffic’/exp AND ‘transport’/exp OR ‘patient transport’/exp OR ‘motor vehicle’/exp OR ‘car’/exp OR taxicab OR ‘subway’:ti,ab,kw OR (hired AND transportation) OR (travel AND voucher) | |||
Footnotes
Conflict of Interest: The authors declare that they have no conflicts of interest.
Contributor Information
Laura E. Starbird, Postdoctoral Research Fellow. Center for Health Policy, Columbia University School of Nursing 560 W. 168th Street, New York, NY 10032 les2163@cumc.columbia.edu tel. (978) 758-7909, fax (646) 962-0105.
Caitlin DiMaina, Graduate Student, Johns Hopkins University School of Nursing.
Chun-An Sun, Doctoral Student, Johns Hopkins University School of Nursing.
Hae-Ra Han, Isabel Hampton Robb Professor, Center for Cardiovascular and Chronic Care, Center for Community Innovation and Scholarship, Johns Hopkins University School of Nursing.
References
- 1.Jones DS, Podolsky SH, & Greene JA (2012). The burden of disease and the changing task of medicine. The New England Journal of Medicine, 366(25), 2333–2338. doi: 10.1056/NEJMp1113569 [DOI] [PubMed] [Google Scholar]
- 2.National Center for Health Statistics (US). (2017). Health, United States, 2016: With Chartbook on Long-term Trends in Health Hyattsville (MD): National Center for Health Statistics (US) Retrieved from http://www.ncbi.nlm.nih.gov/books/NBK453378/ [PubMed] [Google Scholar]
- 3.Locatelli SM, Sharp LK, Syed ST, Bhansari S, & Gerber BS (2017). Measuring Health-related Transportation Barriers in Urban Settings. Journal of Applied Measurement, 18(2), 178–193. [PMC free article] [PubMed] [Google Scholar]
- 4.Wallace R, Hughes-Cromwick P, Mull H, & Khasnabis S (2005). Access to Health Care and Nonemergency Medical Transportation (No. 1924) (pp. 76–84). Washington, DC: Trasnportation Research Board of the National Academies. [Google Scholar]
- 5.Ruggiano N, Shtompel N, Whiteman K, & Sias K (2017). Influences of Transportation on Health Decision-Making and Self-Management Behaviors among Older Adults with Chronic Conditions. Behavioral Medicine (Washington, D.C.), 43(1), 61–70. doi: 10.1080/08964289.2015.1065788 [DOI] [PubMed] [Google Scholar]
- 6.Thomas LV, & Wedel KR (2014). Nonemergency medical transportation and health care visits among chronically ill urban and rural Medicaid beneficiaries. Social Work in Public Health, 29(6), 629–639. doi: 10.1080/19371918.2013.865292 [DOI] [PubMed] [Google Scholar]
- 7.Syed ST, Gerber BS, & Sharp LK (2013). Traveling towards disease: Transportation barriers to health care access. Journal of Community Health, 38(5), 976–993. doi: 10.1007/s10900-013-9681-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Balaban RB, Zhang F, Vialle-Valentin CE, Galbraith AA, Burns ME, Larochelle MR, & Ross-Degnan D (2017). Impact of a Patient Navigator Program on Hospital-Based and Outpatient Utilization Over 180 Days in a Safety-Net Health System. Journal of General Internal Medicine, 32(9), 981–989. doi: 10.1007/s11606-017-4074-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kotwani P, Balzer L, Kwarisiima D, Clark TD, Kabami J, Byonanebye D, … SEARCH Collaboration. (2014). Evaluating linkage to care for hypertension after community-based screening in rural Uganda. Tropical Medicine & International Health: TM & IH, 19(4), 459–468. doi: 10.1111/tmi.12273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Percac-Lima S, Grant RW, Green AR, Ashburner JM, Gamba G, Oo S, … Atlas SJ (2009). A culturally tailored navigator program for colorectal cancer screening in a community health center: A randomized, controlled trial. Journal of General Internal Medicine, 24(2), 211–217. doi: 10.1007/s11606-008-0864-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Taylor VM, Hislop TG, Jackson JC, Tu S-P, Yasui Y, Schwartz SM, … Thompson B (2002). A randomized controlled trial of interventions to promote cervical cancer screening among Chinese women in North America. Journal of the National Cancer Institute, 94(9), 670–677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Centers for Disease Control and Prevention. (2018). National Center for Chronic Disease Prevention and Health Promotion Retrieved August 2, 2018, from https://www.cdc.gov/chronicdisease/about/index.htm
- 13.Tufanaru C, Munn Z, Aromataris E, Campbell J, & Hopp L (2017). Chapter 3: Systematic reviews of effectiveness. In Joanna Briggs Institute Reviewer’s Manual The Joanna Briggs Institute; Retrieved from https://wiki.joannabriggs.org/display/MANUAL/Chapter+3%3A+Systematic+reviews+of+effectiveness [Google Scholar]
- 14.Esperat MC, Flores D, McMurry L, Feng D, Song H, Billings L, & Masten Y (2012). Transformacion Para Salud: A patient navigation model for chronic disease self-management. Online Journal of Issues in Nursing, 17(2), 2. [PubMed] [Google Scholar]
- 15.Krieger J, Collier C, Song L, & Martin D (1999). Linking community-based blood pressure measurement to clinical care: A randomized controlled trial of outreach and tracking by community health workers. American Journal of Public Health, 89(6), 856–861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kaplan CP, Bastani R, Belin TR, Marcus A, Nasseri K, & Hu MY (2000). Improving follow-up after an abnormal pap smear: Results from a quasi-experimental intervention study. Journal of Women’s Health & Gender-Based Medicine, 9(7), 779–790. doi: 10.1089/15246090050147754 [DOI] [PubMed] [Google Scholar]
- 17.Marcus AC, Crane LA, Kaplan CP, Reading AE, Savage E, Gunning J, … Berek JS (1992). Improving adherence to screening follow-up among women with abnormal Pap smears: Results from a large clinic-based trial of three intervention strategies. Medical Care, 30(3), 216–230. [DOI] [PubMed] [Google Scholar]
- 18.Taylor V, Thompson B, Lessler D, Yasui Y, Montano D, Johnson KM, … Goldberg HI (1999). A clinic-based mammography intervention targeting innercity women. Journal of General Internal Medicine, 14(2), 104–111. [DOI] [PubMed] [Google Scholar]
- 19.Tierney WM, Harris LE, Gaskins DL, Zhou XH, Eckert GJ, Bates AS, & Wolinsky FD (2000). Restricting Medicaid payments for transportation: effects on inner-city patients’ health care. The American Journal of the Medical Sciences, 319(5), 326–333. [DOI] [PubMed] [Google Scholar]
- 20.Niccols A, & Sword W (2005). “New Choices” for substance‐ using mothers and their children: Preliminary evaluation. Journal of Substance Use, 10(4), 239–251. doi: 10.1080/146598904123313416 [DOI] [Google Scholar]
- 21.Moola S, Munn Z, Tufanaru C, Aromataris E, Sears K, Sfetcu R, … Mu P-F (2017). Chapter 7: Systematic review of etiology and risk: Critical appraisal checklist for cohort studies. In Joanna Briggs Institute Reviewer’s Manual (p. 7). Retrieved from https://reviewersmanual.joannabriggs.org/ [Google Scholar]
- 22.Chamberlain AM, St Sauver JL, Gerber Y, Manemann SM, Boyd CM, Dunlay SM, … Roger VL (2015). Multimorbidity in heart failure: a community perspective. The American Journal of Medicine, 128(1), 38–45. doi: 10.1016/j.amjmed.2014.08.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Weiss CO, Boyd CM, Yu Q, Wolff JL, & Leff B (2007). Patterns of prevalent major chronic disease among older adults in the United States. JAMA, 298(10), 1160–1162. doi: 10.1001/jama.298.10.1160-b [DOI] [PubMed] [Google Scholar]
- 24.Clark HM (2017). Who Rides Public Transportation: Passenger Demographics and Travel (p. 86). Washington, DC: American Public Transportation Association. [Google Scholar]
- 25.The Centers for Medicare & Medicaid Services. (2018, April). 2019 Medicare Advantage and Part D Rate Announcement and Call Letter Retrieved August 9, 2018, from https://www.cms.gov/newsroom/fact-sheets/2019-medicare-advantage-and-part-d-rate-announcement-and-call-letter
- 26.Blue Cross Blue Shield Association. (2017). Blue Cross and Blue Shield and Lyft Join Forces to Increase Access to Health Care in Communities with Transportation Deserts Retrieved August 13, 2018, from https://www.bcbs.com/news/press-releases/blue-cross-and-blue-shield-and-lyft-join-forces-increase-access-health-care


