Abstract
Zika virus (ZIKV) is spread among human populations primarily through the bite of Aedes mosquitoes. While most ZIKV infections are asymptomatic or cause self-limited symptoms, the major concerns are its association with Guillain-Barré Syndrome and fetal microcephaly together with other birth defects, known as congenital Zika syndrome (CZS). This article reviews the confirmed Zika cases in the continental United States (U.S.) and Hawai‘i thus far, as well as literature of Zika research relevant to Hawai‘i. The first case of CZS within the U.S. was reported in Hawai‘i, highlighting the unique position of Hawai‘i for emerging and re-emerging infectious diseases. Recent studies of the Zika outbreak in Florida demonstrate the key role of Ae. aegypti mosquito in transmission; continuous and proactive vector surveillance in Hawai‘i is warranted.
Additionally, an updated interim pregnancy guidance for pregnant women with possible ZIKV exposure was summarized. Due to recent decline of ZIKV transmission in the Americas, the risk of ZIKV importation to Hawai‘i has been greatly reduced. However, given the presence of Aedes mosquitoes, climate condition, and status of Hawai‘i as a travel destination and foreign import market, public health officials and healthcare providers should remain vigilant for a potential outbreak of mosquito-borne diseases in the future.
Keywords: Zika virus, microcephaly, congenital Zika syndrome, Hawai‘i
Introduction
Zika virus (ZIKV) belongs to the genus Flavivirus of the family Flaviviridae. It is spread among the human populations via the bite of Aedes mosquitoes.1 Following ZIKV infection most individuals are asymptomatic, however, approximately 20% of those infected with ZIKV exhibit symptoms such as fever, rash, joint pain or red eyes, typically lasting for 2–7 days.2 ZIKV can also be transmitted sexually and vertically from mother to fetus, resulting in microcephaly and other birth defects collectively known as congenital Zika syndrome (CZS).3,4 Microcephaly is a severe birth defect characterized by an abnormally small head and underdeveloped brain.3,4 CZS is also associated with seizures, developmental delay, intellectual disability, difficulties with movement and balance, along with other neurological issues such as dysphagia and hearing and vision problems. 3,4 In addition, ZIKV infection is associated with Guillain-Barré Syndrome (GBS), a demyelination of the peripheral nerves.4 Although several candidate Zika vaccines are undergoing clinical trials, none is currently available.5
ZIKV was first isolated from a rhesus monkey in 1947 and from Aedes mosquitoes in 1948 in Uganda.1,2 In 2007, the Island of Yap reported its first outbreak of Zika.1,2 During the 2013–2014 outbreak in French-Polynesia, ZIKV infection was found to be linked to GBS.1,2 According to the Centers for Disease Control and Prevention (CDC), Zika was endemic in over 100 areas including: Africa, Asia, the Caribbean, Central America, North America, the Pacific Islands, and South America during 2015–2017.6 Limited cases have been reported since August 2017.
ZIKV transmission to humans involves primarily the anthropophilic Ae. aegypti and to a lesser extent the peridomestic Ae. Albopictus.7 In Hawai‘i, Ae. aegypti arrived in ∼1890, followed by Ae. albopictus a few years later. Although previous surveys showed that the percentage of Ae. aegypti (out of Ae. aegypti and Ae. albopictus together) in Honolulu was once high (67% in 1913), it dropped to 0% in 2002.7 The decline of Ae. aegypti populations could be attributed to the regional Ae. aegypti eradication program in the 1960s. A survey in 2002 shows the dispersion of Ae. albopictus throughout the islands and the presence of Ae. aegypti in certain locations on Hawai‘i Island, mainly Hilo, Kona, Kealakekua, and the east and west coasts.7
Although all Zika cases reported in Hawai‘i thus far are travel-related, risk of an outbreak remains.8 In addition, Hawaii's large number of international and domestic travelers (∼8,900,000 visitors per year by air and cruise ships) together with its role as an import market, place it under continual threat of importation of mosquitoes, autochthonous infection, and potential outbreak.9–11 This article reviews the confirmed Zika cases in the continental United States (U.S.) and Hawai‘i, as well as scientific literature on Zika research relevant to Hawai‘i. The goal is to provide insights and recommendations to prevent and control a future Zika outbreak in Hawai‘i.
Methods
The authors searched and reviewed reports from government and state organizations, as well as published literature (in English) through the PubMed database. A search with the key words “Zika” and “Hawaii,” as of July 26, 2018, resulted in a total of 21 articles, of which 7 were excluded because they were non-Hawai‘i related or non-Zika. The remaining 14 articles (references 12–19, 21–22, 25–27 and 35) together with references cited in these articles were reviewed.
Results
Of the 14 peer-reviewed articles, eight are basic research on Zika trasmission,12–14 serodiagnosis,15,16 animal models,17,18 and vaccine studies19 conducted by local researchers, indicating several active Zika research programs in Hawai‘i. Six are related to clinical medicine and public health with implications to Hawai‘i. The major findings are summarized below:
1. The first case of CZS within the U.S. and a related study: The first case of microcephaly linked to ZIKV within the U.S. was reported on January 15, 2016 in a baby born in Hawai‘i.20 The Hawai‘i State Department of Health (HDOH) received a report from CDC confirming that the baby had been infected with ZIKV.21
The mother had resided in Brazil during the previous year, and was most likely infected by a mosquito during the first trimester of her pregnancy, potentially affecting embryonic brain development.21 Another retrospective study revealed higher prevalence of ZIKV antibodies in mothers from Hawai‘i (1 IgM positive and 3 IgG positive out of 6) who delivered babies with microcephaly compared with those (1 IgG positive out of 12) who delivered babies without microcephaly between 2009–2012, suggesting possible Zika cases and associated microcephaly before 2015.22
2. Travel-related Zika cases in Hawai‘i:
The first confirmed case of travel-related Zika in Hawai‘i was reported in October 2015 on Hawai‘i Island.23 This individual became infected outside of the state. By the time of discovery, local health officials determined that no mosquito had transmitted the disease, and that the ZIKV was not locally acquired. A state vector control team was sent to survey the patient's workplace and residence for mosquitoes. Hawaii's Civil Defense Administrator informed the public that County of Hawai‘i officials together with the HDOH were, at the time, assessing affected areas for mosquito activity, educating communities, and treating mosquito breeding sites.23 From 2015 to 2017, there were 21 laboratory-confirmed travel-related Zika cases in Hawai‘i (4 in 2015, 11 in 2016, and 6 in 2017).24
ZIKV infection is notifiable in Hawai‘i.8 Healthcare providers are required to report suspect ZIKV infections to the Disease Outbreak Control Division of HDOH as soon as a provisional diagnosis is established.8 The Disease Investigation Branch has investigation plans for ZIKV and other arboviruses including dengue virus (DENV) and chikungunya virus (CHIKV) in place.8–10 The State Laboratory Division performs different ZIKV tests including the reverse transcriptase polymerase chain reaction and IgM test for Hawai‘i and the Pacific Islands.8,25,26 Any positive or equivocal IgM result will be tested by plaque-reduction neutralization test at the CDC.8 A recent study comparing different surveillance strategies during the 2015–2017 ZIKV epidemic in the continental U.S. revealed that testing symptomatic patients at the emergency department is a more efficient strategy for detecting transmission compared with testing blood donors or pregnant women.27
3. A Zika outbreak in the continental U.S.: implications for Hawai‘i State
A study of the Zika outbreak in Florida in July 2016 showed that the primary mode of local transmission was the bite by Aedes mosquitos.28 Mosquito surveillance revealed that 99.8% of the 24,351 mosquitoes collected were Ae. aegypti, and 8 pools (≤ 50 mosquitoes each pool) tested positive for ZIKV. It was estimated that about 1 of 1600 Ae. aegypti mosquitoes were infected with ZIKV, similar to the infection rates reported during the DENV and CHIKV outbreaks.29,30 Additionally, the number of ZIKV cases strongly correlated with the abundance of Ae. aegypti in each transmission zone, suggesting the importance of vector abundance to human infection rates.28
Although Ae. Aegypti, the principal vector of DENV, ZIKV and CHIKV, is only present in certain locations on Hawai‘i island, its distribution correlates with the distribution of human cases during the 2015–2016 dengue outbreak, suggesting its potential contribution to future outbreaks of these three viruses.8–10 The public health response and control measures following the 2015–2016 outbreak have been described in the HDOH website and reviewed recently.8,31 Given the mutations of the East Central South African strain of CHIKV resulted in its adaptation to Ae. albopictus and contributed to the explosive spread in 2004–2006, the possibility that a new ZIKV strain better hosted by Ae. albopictus cannot be completely ruled out.32–34 These observations highlight the importance of proactive and continuous vector surveillance and control efforts in Hawai‘i, where the most recent state-wide surveillance was conducted in 2002.7
4. Recommendation for pregnant women
Although only 5%–6% of U.S. pregnant women with possible ZIKV infection during pregnancy gave birth to babies with CZS (9–11% if infection occurred during first trimester), it is an existing threat and must be monitored with close attention.35,36
Clinical features of CZS which includes microcephaly can be potentially identified by fetal ultrasonography but may need continued surveillance of the newborn through infancy to identify subtle abnormalities.3,4 According to the recent CDC recommendations, all pregnant women should be asked if they have possible ZIKV exposure including history of travel to or residence in areas with ZIKV transmission and possible sexual exposure to ZIKV before and during current pregnancy, or symptoms of Zika disease during current pregnancy.37,38 Before testing for ZIKV infection, the limitations and potential risks of misinterpretations of test results should be discussed. The updated interim pregnancy guidance for symptomatic and asymptomatic pregnant women with possible ZIKV exposure is summarized in Figure 1.37,38
Figure 1.
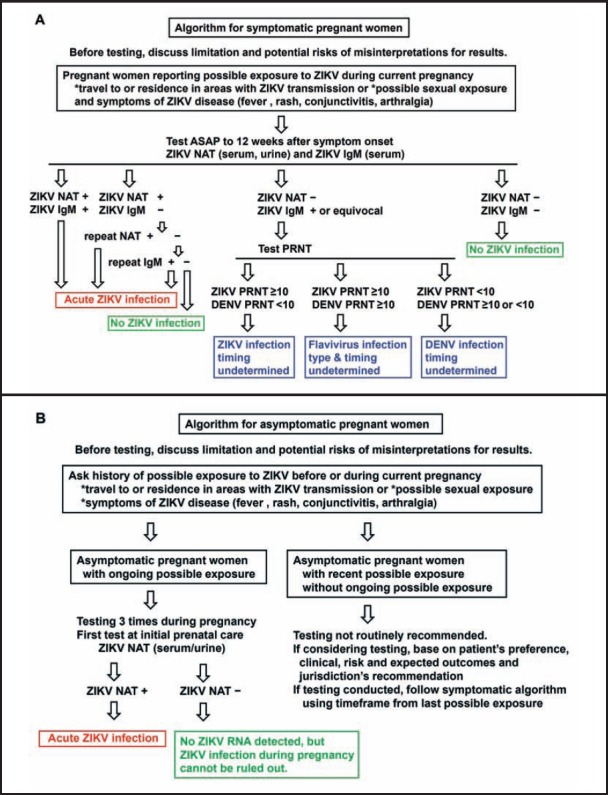
Summary of CDC's interim guidance for pregnant women with possible ZIKV exposure. Algorithm for symptomatic (A) and asymptomatic (B) pregnant women was presented as two concise flow-charts based on the text and figures in references 37 and 38. NAT: nucleic acid test; PRNT: plaque reduction neutralization test.37,38
Discussion
Since ZIKV transmission has dramatically declined recently in the Americas, the risk of importation of Zika to Hawai‘i has been greatly reduced. However, the specter of CZS and its potential re-emergence in the tropical and subtropical regions highlight the importance of continuous effort on research, vaccine development, surveillance and vector control.
Hawaii's report of the first CZS case within the U.S. on January 15, 2016, 5 months before such reports in the continental U.S.,6 highlights the unique position of Hawai‘i for emerging and re-emerging pathogens.20 This is analogous to the report of the first H1N1 case in Hawai‘i during the 2009 pandemic, 21 days after the CDC reported the first cases in the continental U.S.26
Based on serological tests for ZIKV antibodies, the possibility that Zika cases and CZS might have occurred in Hawai‘i between 2009–2012 is an interesting observation but remains to be verified by further studies of archived samples collected in Hawai‘i using different serological tests.15,22
Studies of Zika outbreak in Florida indicate the critical role of Ae. aegypti in human transmission. Given the presence of Aedes mosquitoes (widespread Ae albopictus and Ae. aegypti in some sites on Hawai‘i Island), a climate compatible with a year-round mosquito season, and the geographic location of Hawai‘i as a travel destination and foreign import market, public health officials and healthcare providers should remain vigilant for a potential outbreak of mosquito-borne diseases such as ZIKV, DENV and CHIKV.
There are several limitations. First, since the literature search on PubMed database was up to July 2018, articles published subsequently or in non-PubMed database were not covered by this review. Second, this review focused on clinical and public health related research; basic research programs on ZIKV by scientists in Hawai‘i were beyond the scope of this review. Third, the summary of guidance for pregnant women with possible ZIKV exposure was based on the most recent CDC recommendations published in July 2017. Continuous update of any revision or new guidelines from the CDC is warranted.
Acknowledgements
The authors wish to acknowledge Pauline Mashima PhD, Shari Goo-Yoshino MS, and Melissa Kahili-Heede MS for their review and comments on this manuscript. This work was supported by the award R01AI110769-01 (Wang) from the National Institute of Allergy and Infectious Diseases, National Institutes of Health. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Abbreviations
- CDC
Centers for Disease Control and Prevention
- CHIKV
Chikungunya Virus
- CZS
Congenital Zika syndrome
- DENV
Dengue Virus
- GBS
Guillain-Barré Syndrome
- HDOH
Hawai‘i State Department of Health
- NAT
Nucleic Acid Test
- PRNT
Plaque Reduction Neutralization Test
- ZIKV
Zika Virus
Conflict of Interest
None of the authors identify any conflicts of interest.
References
- 1.Musso D, Gubler DJ. Zika Virus. Clinical Microbiology Reviews. 2016;29:487–524. doi: 10.1128/CMR.00072-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lessler J, Chaisson LH, Kucirka LM, Bi Q, Grantz K, Salje H, et al. Assessing the global threat from Zika virus. Science. 2016;353:aaf8160. doi: 10.1126/science.aaf8160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Melo AS, Aguiar RS, Amorim MM, et al. Congenital Zika Virus Infection: Beyond Neonatal Microcephaly. JAMA Neurology. 2016;73:1407–1416. doi: 10.1001/jamaneurol.2016.3720. [DOI] [PubMed] [Google Scholar]
- 4.Krauer F, Riesen M, Reveiz L, Oladapo OT, Martínez-Vega R, Porgo TV, et al. Zika Virus Infection as a Cause of Congenital Brain Abnormalities and Guillain-Barré Syndrome: Systematic Review. PLoS Med. 2017;14:e1002203. doi: 10.1371/journal.pmed.1002203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Barouch DH, Thomas SJ, Michael NL. Prospects for a Zika Virus Vaccine. Immunity. 2017;46:176–182. doi: 10.1016/j.immuni.2017.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.CDC, author. Zika Travel Information. 2017. Mar 10, [December 26, 2017]. https://wwwnc.cdc.gov/travel/page/world-map-areas-with-zika.
- 7.Winchester JC, Kapan DD. History of Aedes mosquitoes in Hawaii. J Am Mosq Control Assoc. 2013;29:154–163. doi: 10.2987/12-6292R.1. [DOI] [PubMed] [Google Scholar]
- 8.Hawaii State Department of Health, author. Zika Virus. [July 26, 2018]. http://health.hawaii.gov/docd/disease_listing/zika-virus/
- 9.Hawaii State Department of Health, author. Dengue outbreak 2015–16. [July 26, 2018]. http://health.hawaii.gov/docd/dengue-outbreak-2015/
- 10.Hawaii State Department of Health, author. Chikungunya. [July 26, 2018]. http://health.hawaii.gov/docd/disease_listing/chikungunya/
- 11.Hawaii Tourism Authority, author. [January 2, 2018]. http://files.hawaii.gov/dbedt/visitor/visitor-research/2016-annual-visitor.pdf.
- 12.Siemann DN, Strange DP, Maharaj PN, Shi PY, Verma S. Zika Virus Infects Human Sertoli Cells and Modulates the Integrity of the In Vitro Blood-Testis Barrier Model. J Virol. 2017;91:e00623–e00717. doi: 10.1128/JVI.00623-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Strange DP, Green R, Siemann DN, Gale M, Jr, Verma S. Immunoprofiles of human Sertoli cells infected with Zika virus reveals unique insights into host-pathogen crosstalk. Sci Rep. 2018 Jun 7;8(1):8702. doi: 10.1038/s41598-018-27027-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Strange DP, Zarandi NP, Trivedi G, Atala A, Bishop CE, Sadri-Ardekani H, et al. Human testicular organoid system as a novel tool to study Zika virus pathogenesis. Emerg Microbes Infect. 2018;7:82. doi: 10.1038/s41426-018-0080-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tsai WY, Youn HH, Brites C, Tsai JJ, Tyson JJ, Pedroso C, et al. Distinguishing Secondary Dengue Virus Infection From Zika Virus Infection With Previous Dengue by a Combination of 3 Simple Serological Tests. Clin Infect Dis. 2017;65:1829–1836. doi: 10.1093/cid/cix672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Herrera BB, Tsai WY, Chang CA, Hamel DJ, Wang WK, Lu Y, et al. Sustained Specific and Cross-Reactive T Cell Responses to Zika and Dengue Virus NS3 in West Africa. J Virol. 2018;92:e01992–e02017. doi: 10.1128/JVI.01992-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kumar M, Krause KK, Azouz F, Nakano E, Nerurkar VR. A guinea pig model of Zika virus infection. Virol J. 2017;14:75. doi: 10.1186/s12985-017-0750-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Krause KK, Azouz F, Shin OS, Kumar M. Understanding the Pathogenesis of Zika Virus Infection Using Animal Models. Immune Netw. 2017;17:287–297. doi: 10.4110/in.2017.17.5.287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.To A, Medina LO, Mfuh KO, Lieberman MM, Wong TAS, Namekar M, et al. Recombinant Zika Virus Subunits Are Immunogenic and Efficacious in Mice. mSphere. 2018;3:e00576–e00617. doi: 10.1128/mSphere.00576-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McNeil DG., Jr Hawaii Baby With Brain Damage Is First U.S. Case Tied to Zika Virus. NY Times. 2016 Jan 16; [Google Scholar]
- 21.Culjat M, Darling SE, Nerurkar VR, et al. Clinical and Imaging Findings in an Infant With Zika Embryopathy. Clin Infect Dis. 2016;63:805–811. doi: 10.1093/cid/ciw324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kumar M, Ching L, Astern J, Lim E, Stoles AJ, Melish M, et al. Prevalence of Antibodies to Zika Virus in Mothers from Hawaii Who Delivered Babies with and without Microcephaly between 2009–2012. PLoS Negl Trop Dis. 2016;10:e0005262. doi: 10.1371/journal.pntd.0005262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.First case of travel-related Zika reported on Hawaii island. Honolulu Star Advertiser. 2016 Oct 11;
- 24.CDC, author. Zika cases in the United States. 2017. [December 26, 2017]. https://www.cdc.gov/zika/reporting/case-counts.html.
- 25.Hancock WT, Soeters HM, Hills SL, et al. Establishing a Timeline to Discontinue Routine Testing of Asymptomatic Pregnant Women for Zika Virus Infection - American Samoa, 2016–2017. MMWR. 2017;66:299–301. doi: 10.15585/mmwr.mm6611a5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Whelen AC, Becker SJ, Uluiviti VR, Maddox N. Insights in Public Health: Leveraging Pacific Laboratories to Boost Global Health Security. Hawaii J Med Public Health. 2016;75:389–392. [PMC free article] [PubMed] [Google Scholar]
- 27.Russell S, Ryff K, Gould C, Martin S, Johansson M. Detecting local Zika virus transmission in the continental United States: a comparison of surveillance strategies. PLoS Curr. 2017 Nov 22;:9. doi: 10.1371/currents.outbreaks.cd76717676629d47704170ecbdb5f820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Grubaugh ND, Ladner JT, Kraemer MUG, Dudas G, Tan AL, Gangavarapu K, et al. Genomic epidemiology reveals multiple introductions of Zika virus into the United States. Nature. 2017;546:401–405. doi: 10.1038/nature22400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dzul-Manzanilla F, Martínez NE, Cruz-Nolasco M, Gutiérrez-Castro C, López-Damián L, Ibarra-López J, et al. Evidence of vertical transmission and co-circulation of chikungunya and dengue viruses in field populations of Aedes aegypti (L.) from Guerrero, Mexico. Trans R Soc Trop Med Hyg. 2016;110:141–144. doi: 10.1093/trstmh/trv106. [DOI] [PubMed] [Google Scholar]
- 30.Yoon IK, Getis A, Aldstadt J, Rothman AL, Tannitisupawong D, Koenraadt CJ, et al. Fine scale spatiotemporal clustering of dengue virus transmission in children and Aedes aegypti in rural Thai villages. PLoS Negl Trop Dis. 2012;6:e1730. doi: 10.1371/journal.pntd.0001730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lew RJ, Tsai WY, Wang WK. Dengue outbreaks in Hawaii after WWII- a review of public health response and scientific literatures. Hawaii J Med Public Health. 2018;77(12):315–318. [PMC free article] [PubMed] [Google Scholar]
- 32.Tsetsarkin KA, Vanlandingham DL, McGee CE, Higgs S. A single mutation in chikungunya virus affects vector specificity and epidemic potential. PLoS Pathog. 2007;3:e201. doi: 10.1371/journal.ppat.0030201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Petersen LR, Powers AM. Chikungunya: epidemiology. F1000Res. 2016:5. doi: 10.12688/f1000research.7171.1. F1000 Faculty Rev-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Aliota MT, Bassit L, Bradrick SS, Cox B, Garcia-Blanco MA, Gavegnano C, et al. Zika in the Americas, year 2: What have we learned? What gaps remain? A report from the Global Virus Network. Antiviral Res. 2017;144:223–246. doi: 10.1016/j.antiviral.2017.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Honein MA, Dawson AL, Petersen EE, et al. Birth Defects Among Fetuses and Infants of US Women With Evidence of Possible Zika Virus Infection During Pregnancy. JAMA. 2017;317:59–68. doi: 10.1001/jama.2016.19006. [DOI] [PubMed] [Google Scholar]
- 36.Reynolds MR, Jones AM, Petersen EE, Lee EH, Rice ME, Bingham A, et al. Vital Signs: Update on Zika Virus-Associated Birth Defects and Evaluation of All U.S. Infants with Congenital Zika Virus Exposure - U.S. Zika Pregnancy Registry, 2016. MMWR. 2017;66:366–373. doi: 10.15585/mmwr.mm6613e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Oduyebo T, Polen KD, Walke HT, et al. Update: Interim Guidance for Health Care Providers Caring for Pregnant Women with Possible Zika Virus Exposure - United States (Including U.S. Territories), July 2017. MMWR. 2017;66:781–793. doi: 10.15585/mmwr.mm6629e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.CDC, author. Testing & Diagnosis. 2017. [January 2, 2018]. https://www.cdc.gov/pregnancy/zika/testing-follow-up/testing-and-diagnosis.html.


