Abstract
Background and Objectives
For nursing home residents, positive interactions with staff and engagement in daily life contribute meaningfully to quality of life. We sought to improve these aspects of person-centered care in an opportunistic snowball sample of six Veterans Health Administration nursing homes (e.g., Community Living Centers—CLCs) using an intervention that targeted staff behavior change, focusing on improving interactions between residents and staff and thereby ultimately aiming to improve resident engagement.
Research Design and Methods
We grounded this mixed-methods study in the Capability, Opportunity, Motivation, Behavior (COM-B) model of behavior change. We implemented the intervention by (a) using a set of evidence-based practices for implementing quality improvement and (b) combining primarily CLC-based staff facilitation with some researcher-led facilitation. Validated resident and staff surveys and structured observations collected pre and post intervention, as well as semi-structured staff interviews conducted post intervention, helped assess intervention success.
Results
Sixty-two CLC residents and 308 staff members responded to the surveys. Researchers conducted 1,490 discrete observations. Intervention implementation was associated with increased staff communication with residents during the provision of direct care and decreased negative staff interactions with residents. In the 66 interviews, staff consistently credited the intervention with helping them (a) develop awareness of the importance of identifying opportunities for engagement and (b) act to improve the quality of interactions between residents and staff.
Discussion and Implications
The intervention proved feasible and influenced staff to make simple enhancements to their behaviors that improved resident-staff interactions and staff-assessed resident engagement.
Keywords: Quality of care, Implementation science, Mixed-methods
Background and Objectives
Nursing home residents are at great risk of not being engaged in positive, individualized, stimulating activities (Harper Ice, 2002; Wood, Harris, Snider, & Patchel, 2005). Yet engagement in active, expressive, social activities is associated with higher quality of life (Beerens et al., 2016). Engagement of residents through positive interactions with staff and through behavioral interventions is, for example, specifically related to positive well-being, improved affect, and extended survival (Haugan, 2014; Meeks, Shah, & Ramsey, 2009; Schreiner, Yamamoto, & Shiotani, 2005). Improving resident involvement through individualized activities has numerous positive benefits, including reduced agitation and depression and improved mood, pleasure, and interest (Beerens et al., 2018; Travers et al., 2016). Ideally, staff facilitate resident engagement in meaningful activity by interacting with residents during work activities and socially, creating opportunities for residents to be occupied in ways and with the timing they like (Smit, de Lange, Willemse, Twisk, & Pot, 2016). While some staff may feel, for example, that juggling multiple responsibilities within a short time frame impedes their ability to interact with and engage residents, research shows staff are capable of improving their interactions (Carpiac-Claver & Levy-Storms, 2007; Smith, Mathews, & Gresham, 2010; Wilson & Davies, 2009).
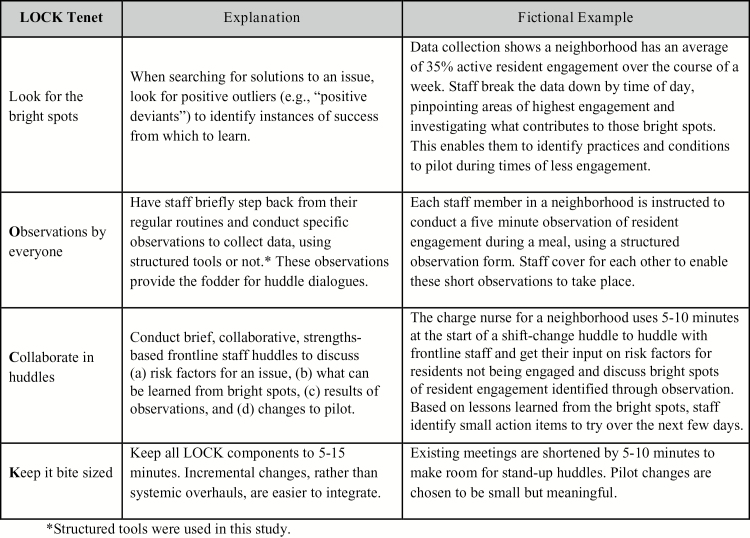
Quality improvement (QI) may offer feasible and sustainable opportunities for nursing home staff to work together to improve resident engagement by piloting, observing, and refining interventions. But to effect lasting and meaningful improvement, QI efforts must be grounded in a framework that fosters systemic change and long-term sustainability (Alexander & Hearld, 2011). In our previous work, we examined the QI, behavior change, and implementation science literatures to develop a theory-driven, user-friendly, integrated QI bundle for nursing home staff to improve resident-staff interactions to engage residents (Mills et al., 2017). We identified four critical practices to successful QI efforts: strengths-based learning, observation, relationship-based teams, and efficiency. We operationalized these for use in nursing homes, creating a bundle of four practices known by their acronym, LOCK: (a) Look for the bright spots, (b) Observe, (c) Collaborate in huddles, and (d) Keep it bite-sized (Mills et al., 2017)—see Figure 1. In this paper, we describe the outcomes of a LOCK-based intervention that targeted staff behavior change, focusing on improving staff interactions with residents and thereby ultimately aiming to improve resident engagement.
Figure 1.
LOCK model in the Community Living Center or nursing home setting.
Conceptual Model
The Capability, Opportunity, Motivation, Behavior (COM-B) model of behavior change (Michie, Atkins, & West, 2014; Michie, van Stralen, & West, 2011) guided implementation and evaluation of the LOCK model intervention. The COM-B model describes an ongoing cycle in which behaviors are generated by and also affect three components—capability, opportunity, and motivation. Specifically, capability is the psychological or physical ability to enact a behavior, opportunity is the physical and social environment that enables a behavior, and motivation is the automatic and reflective mechanisms that trigger or inhibit behavior. COM-B has been widely used to guide implementation work, including in long-term care (Fleming, Bradley, Cullinan, & Byrne, 2014; Peiris et al., 2015). In our study, we assumed that the LOCK-based intervention affected staff behavior by impacting their capability, opportunity, and motivation and that changed staff behavior would improve resident-staff interactions and resident engagement.
The LOCK-based intervention builds on team structures that already exist in nursing home environments and achieves behavior change through observation, feedback, and relationship-building that fits into existing staff workflow (Mills et al., 2017). Staff identify bright spots by looking for positive outliers, such as extremely high occurrences of resident engagement, and analyzing them for helpful information about how to facilitate behavior change. This conforms with the literature on the value of studying positive deviance (Bradley et al., 2009). In COM-B language, it can alter capability by affecting understanding and can affect motivation by providing evidence of existing success. Observation, in turn, provides staff with opportunities to study positive outliers and obtain critical information about the progress of an intervention, thus potentially affecting capability and motivation. Collaboration through huddles (i.e., brief, stand-up meetings at the point of care) potentially alters capability, opportunity, and motivation by promoting relationship-based team building and successful communication. Keeping all intervention activities confined to 5- to 15-min bursts enables easy integration into existing routines and can promote changes in capability, opportunity, and motivation by respecting staff members’ busy schedules and easing the activities’ incorporation into regular routines.
The study focused on Community Living Centers (CLCs, i.e., nursing homes) within the Veterans Health Administration, the largest integrated health system in the United States. Studying the implementation of the intervention in CLCs, we believe, provides valuable insights into how change can be facilitated at the local level within a large system.
Research Design and Methods
We nested implementation of the LOCK-based intervention within a research data collection framework. This enabled two separate sets of activities to run simultaneously—QI data collection and research data collection—and distinguished the QI portion of the study from the human subjects research arm. Each CLC implemented LOCK-based QI projects (the intervention). Researchers collected data to study the outcomes of these projects. Research data form the basis for this paper’s results and comprised (a) researcher-conducted structured observations of the CLC neighborhood (i.e., unit) pre and post intervention, (b) self-administered surveys of CLC staff pre and post intervention, (c) researcher-administered surveys of CLC residents pre and post intervention, and (d) researcher-led semi-structured interviews with CLC staff post intervention. Triangulating qualitative and quantitative data was designed to lead to deeper and potentially novel interpretations during and after analysis (Gibson, 2017).
Setting
We selected six CLCs through opportunistic and snowball sampling. Within each CLC, the intervention focused on two neighborhoods that provided skilled nursing/rehabilitation services and/or long-term care. Mean neighborhood size was 23 residents (range: 10–45). The VA’s central institutional review board approved all study procedures.
Intervention and Study Design
Ideal implementation of the intervention included the following components. Staff looked for bright spots in resident-staff interactions and resident engagement by conducting structured observations using data collection templates created in an early phase of the study (Hartmann et al., 2017). They discussed results of the observations in huddles that emphasized problem-solving, collaborative communication, and identifying and building on areas of strength. In the huddles, staff determined action steps to implement lessons learned from the observed bright spots and problem solved. They reviewed outcomes in subsequent huddles.
Researchers and CLC staff facilitated the intervention through a team-based approach known as blended facilitation, in which external and internal facilitators engage in interactive problem-solving and interpersonal support (Stetler et al., 2006). Researchers served as the external facilitators, as they had expertise in the intervention’s evidence base and implementation activities, as well as project and change management (Ritchie et al., 2017). CLC staff, particularly those designated as study points of contact or those who emerged to champion the project, served as internal facilitators, individuals who were familiar with the CLC’s organizational structures, procedures, culture, and clinical processes (Ritchie et al., 2017).
At all participating CLCs, leadership assigned designated staff to be the study points of contact. We advised leadership to choose individuals (a) with enough authority to function as credible project leaders and (b) who could benefit professionally from serving in this role. At each CLC, researchers held a series of 1-hr training pre-implementation phone calls with CLC leadership and study points of contact. They also visited each CLC at the beginning of the implementation period to collect baseline data and provide limited training and support for internal facilitators. Training focused primarily on nursing staff, with other staff invited. Timing and length of training was dictated by each CLC to fit into staff routines (i.e., up to two 1- or 2-hr training meetings and some on-the-floor training of approximately 30 min). Researchers also conducted weekly 30-min check-in calls over the course of the implementation period. The intervention lasted for an average of 30 weeks at a site (range: 23–39 weeks).
Quantitative Data Collection
Researchers visited each CLC at two time points (prior to and at the end of the intervention period) to collect quantitative study data. During these visits, researchers used the Resident-centered Assessment of Interactions with Staff and Engagement (RAISE) tool (see below) to conduct structured observations that captured data about staff and resident daily routines in the CLC. They used validated survey instruments to collect data from CLC residents. Concurrent with the visits, researchers also administered Internet-based and paper surveys using validated instruments to gather data from CLC staff.
RAISE Tool
We used the RAISE instrument (Snow et al., 2018) to measure the quality of interactions between staff and residents and the frequency and extent of CLC resident engagement in meaningful activity. The RAISE is a reliable and valid instrument comprising eight observation variables (Snow et al., 2018). Researchers used a time-sampling approach for specific physical locations. For a 20-min period, this involved standing in an unobtrusive public area and following a cycle of observing a target individual (staff or resident) for 5 s, noting observations, then switching observation to the next target in a structured, left-to-right pattern (Suen & Ary, 1989). All residents and staff in the researcher’s visual field were included in data collection. Raters achieved 90% accuracy on a series of training videos before collecting data. Measures derived from the RAISE instrument were the following: (a) percentage of actively engaged residents; (b) percentage of verbal or nonverbal interactions between staff and residents during provision of routine care (a variable we termed, “Realized Opportunities for building Relationship”); (c) quality of staff interactions when present with residents (i.e., positive, negative, or neutral); and (d) emotional tone of observed staff or residents (i.e., positive, negative, or neutral).
The Community-Oriented Programs Environment Scale
Resident experience and staff perception of resident experience were measured for residents and staff, respectively, using an adaptation of the Community-Oriented Programs Environment Scale (CPES, formerly COPES) (Moos & Otto, 1972). The CPES was developed to measure the social climate of community-based residential and semi-residential programs, to ascertain whether they operate according to intended values, and to monitor social climate over time. It includes three forms, of which we used Form R (“Real”), which is used to describe the setting. We excluded the anger and aggression and system maintenance subscales to maximize participation by keeping the number of items manageable for CLC residents and to align the content most closely with the study goal of measuring resident engagement. The final adapted instrument contained 60 true/false statements. A score of 0 or 1 was assigned to each answer based on a match with the CPES’s scoring key. Raw scores were calculated for each subscale and averaged separately for a CLC’s residents and staff members. Subscale scores varied between 0 and 10, and calculated averages were standardized against a normative U.S.-based sample (Moos, 2009).
Nursing Home Certified Nurse Assistant Job Satisfaction Questionnaire
The Nursing Home Certified Nurse Assistant Job Satisfaction Questionnaire JSQ; (Castle, 2010) measured CLC staff members’ satisfaction with their work environment. This 21-item questionnaire has seven domains describing relationships with coworkers, work demands, work content, work load, training, rewards, and quality of resident care, as well as two global job satisfaction questions. The JSQ was previously administered in a study of 72 nursing homes in six states (Castle, 2007). Respondents use a 10-point visual analog scale to rate each item. Scores for each subscale were summed to create an overall score.
Survey Administration
For staff, the CPES and JSQ were administered together as one survey at two time points: prior to implementation of the intervention and at the conclusion of the study period. All CLC staff were invited to complete either an Internet-based or paper version. The survey was anonymous and collected minimal demographic and neighborhood information to maximize response rates and, for the same reason, did not attempt to link respondents between the two time points.
We administered the CPES to residents in-person. Residents were required to have lived in the CLC a minimum of 7 days. Staff members gave researchers a list of all cognitively intact residents. Researchers approached residents using a convenience sampling method, returning to each neighborhood multiple times. They screened potential participants to ensure adequate cognitive ability and comprehension, using a standardized question-and-answer format that assessed basic orientation, alertness, and comprehension of the key elements of the informed consent form.
Qualitative Data Collection
At the end of each CLC’s intervention period, researchers conducted in-person semi-structured qualitative interviews with CLC staff members. Participants were solicited via email and in-person contact. CLC leadership, clinicians, nurses, nursing assistants, social workers, physical/occupational therapists, psychologists, pharmacists, dietary staff, chaplains, and others whose jobs related to QI were eligible to participate. The study’s conceptual framework guided development and organization of interview guide. Questions elicited thoughts about experiences with the project, how the project or using the observation tools influenced how staff did their jobs, impressions of huddles, impressions of conducting observations, how the project influenced resident care, and how the environment of the CLC changed as a result of the project. Follow-up probes focused on understanding particular elements and COM-B components. Researchers recorded each interview.
Analysis
Quantitative
All quantitative data were analyzed at the CLC level because data, by design, could not be linked back to respondents. We used descriptive analyses to characterize resident experience, staff satisfaction, and RAISE measures before and after the intervention. For cross-sectional analyses, we combined all data (pre and post) and used generalized linear models to assess the association of RAISE-derived measures with resident experience and staff satisfaction, adjusting for CLC-level average length of staff work tenure in the CLC. For post- versus pre-intervention analyses, we used generalized linear models to assess the association of the intervention with the RAISE-derived measures, adjusting for site. Each of the RAISE instrument’s 5-s observation intervals was considered one unit of observation. A false discovery rate correction (Benjamini & Hochberg, 1995) was used to account for multiple hypothesis testing. Statistical significance was set at the p ≤ .05 level. All statistical analyses were performed using SAS 9.3 (SAS Institute, Cary, NC).
Qualitative
Six members of the research team with expertise in qualitative methodology listened to interview recordings and coded the content, entering each participant’s data into an analytic matrix that contained a priori analytic constructs based on the LOCK model (columns) and COM-B (rows). Data were entered as verbatim quotes or summarized content. We used thematic content analysis (Lincoln & Guba, 1985) to fit the data into the matrix and examine emerging themes across respondents within the a priori constructs. Data could have more than one code, and the matrix structure allowed for change during the coding process. Initial interviews were independently coded by two people and reviewed as a team until consistent agreement was reached (n = 6); subsequently, interviews were coded individually. The team met regularly to review the coding for each interview and discuss discrepancies, resolving them by reaching consensus. The team wrote detailed notes to serve as an audit trail (Bradley, Curry, & Devers, 2007). Analyses included all four COM-B concepts, but this paper presents only the Behavior outcomes.
Results
Quantitative
Staff surveys had overall response rates of 29.8% (range: 24.1%–37.5%) pre implementation and 30.7% (range: 9.1%–54.9%) post implementation. Because we employed convenience sampling, resident surveys had no response rates. Across both time points and all CLCs, 308 staff completed the CPES survey and 306 staff completed the JSQ instrument. Also across both time points and all six CLCs, 62 residents completed the CPES survey; only four residents completed it at both time points.
Of the 281 staff who provided information on gender, 80% were female. Among the 287 staff who provided information on job type, 39% (n = 113) were licensed nurses, 31% (n = 88) were nursing assistants, and 30% (n = 86) held other jobs. And of the 273 staff who provided data on length of time having worked in the CLC, the average was 7 years (range: 0.1–34). Resident surveys collected no demographic information.
Table 1 reports CPES and JSQ results. CLC-level mean scores for the CPES were 46.5 for staff (range: 40.0–50.3) and 44.0 for residents (range: 38.1–50.2). The CLC-level overall mean score for the JSQ, which was administered only to staff, was 7.7 (range: 6.4–8.3).
Table 1.
Facility-Level Measures of Resident Experience and Staff Satisfaction
| Reported by residents (Nsites = 6) | Reported by staff (Nsites = 6) | |
|---|---|---|
| Resident experience (i.e., CPES)a | ||
| Overall | 44.0 ± 4.3 | 46.5 ± 3.7 |
| Autonomy | 42.2 ± 5.9 | 44.1 ± 3.8 |
| Involvement | 45.7 ± 6.4 | 45.1 ± 5.5 |
| Practical orientation | 42.9 ± 6.5 | 46.5 ± 5.2 |
| Personal problem orientation | 39.0 ± 3.3 | 44.4 ± 2.4 |
| Support | 46.8 ± 6.2 | 46.1 ± 4.4 |
| Spontaneity | 47.2 ± 3.6 | 53.7 ± 3.3 |
| Staff satisfaction (i.e., JSQ)b | ||
| Overallc | 7.7 ± 0.7 | |
| Global | 7.4 ± 0.8 | |
| Relationships with coworkers | 7.6 ± 1.2 | |
| Work demands | 7.2 ± 0.9 | |
| Work content | 8.5 ± 0.3 | |
| Workload | 7.6 ± 0.5 | |
| Training | 8.6 ± 0.6 | |
| Rewards | 6.0 ± 1.0 | |
| Quality of resident care | 8.7 ± 0.6 | |
Note: Mean score (standardized for CPES, unadjusted raw mean for JSQ) ± SD shown. CPES = Community-Oriented Programs Environment Scale; JSQ = Nursing Home Certified Nurse Assistant Job Satisfaction Questionnaire.
aCPES (Nresidents = 62, Nstaff = 308). Higher score = better experience.
bMeasured by the JSQ (N = 306). Higher score = more job satisfaction.
cCalculated based on the mean of subscale scores.
Researchers performed a total of 1,490 RAISE instrument observations (averaging 248.3 observations per site) across 55 observation periods prior to intervention implementation and 1,555 observations (averaging 259.2 per site) across 47 observation periods post intervention. Across all six CLCs prior to implementation, 86.9% of staff had Realized Opportunities for building Relationship with residents during provision of routine care and, among staff who were near residents (i.e., within 3 ft), 6.4% were observed interacting negatively with them (Table 2). After intervention implementation, more than 96% of staff had Realized Opportunities for building Relationship with residents and, among staff who were near residents, 2.3% interacted negatively with them.
Table 2.
RAISE Measures Before and After Implementation of the LOCK-Based Intervention
| Before LOCK intervention, % (95% CI) | After LOCK intervention, % (95% CI) | |
|---|---|---|
| Resident engagement, activea | 58.6 (54.6–62.7) | 62.5 (59.0–65.9) |
| Realized opportunities for relationshipb | 86.9 (82.7–91.0) | 96.2 (94.0–98.4) |
| Quality of staff interactions with residentsc | ||
| Positive | 72.0 (68.0–76.0) | 79.0 (75.0–82.3) |
| Neutral | 21.6 (17.9–25.3) | 19.0 (15.5–22.6) |
| Negative | 6.4 (4.2–8.6) | 2.3 (1.0–3.7) |
| Emotional toned | ||
| Positive | 33.8 (31.2–36.4) | 34.2 (31.6–36.9) |
| Neutral | 65.0 (62.4–67.6) | 64.8 (62.1–67.5) |
| Negative | 1.0 (0.05–1.6) | 0.7 (0.03–1.2) |
Note: Individual-level percentage (95% CI) shown. CI = confidence interval; RAISE = Resident-centered Assessment of Interactions with Staff and Engagement.
aBased on observations of residents (Npre-intervention = 337; Npost-intervention = 484).
bVerbal/nonverbal staff interactions with residents, based on observations of staff providing routine care to residents (Npre-intervention = 259; Npost-intervention = 289).
cBased on observations of staff who were verbally/nonverbally interacting with residents (Npre-intervention = 889; Npost-intervention = 1,254).
dBased on observations of staff and residents (Npre-intervention = 1,290; Npost-intervention = 1,206).
Cross-sectional Relationship Between RAISE Measures and CPES
Positive emotional tone as measured by the RAISE instrument was positively associated in generalized linear models with overall resident experience (resident-reported, β = 28.3, 95% CI: 1.1–55.4, p = .046; staff-reported, β = 33.1, 95% CI: 5.1–61.1, p = .033) and staff perceptions of residents’ involvement in CLC life (β = 49.4, 95% CI: 9.2–89.6, p = .030), autonomy (β = 34.9, 95% CI: 16.8–53.0, p = .009), and practical orientation (β = 45.8, 95% CI: 6.4–85.2, p = .034). Resident engagement as measured by the RAISE instrument was positively associated with residents’ involvement in CLC life (β = 0.33, 95% CI: 0.10–0.56, p = .019).
Cross-sectional Relationship Between RAISE Measures and JSQ
Staff satisfaction was high across all six CLCs, with a facility-level mean calculated overall score of 7.7 (range: 6.4–8.3). Scores were similarly high for the relationships with coworkers, work demands, work content, workload, training, rewards, and quality of resident care subscales, and global job satisfaction items. Positive emotional tone was positively associated with staff satisfaction with training (β = 5.1, 95% CI: 0.3–9.8, p = .042) and rewards (β = 8.0, 95% CI: 1.2–14.7, p = .033).
Post- versus Pre-intervention Association of the LOCK-Based Intervention With RAISE Measures
Across all six CLCs, implementation of the LOCK-based intervention was significantly associated with increased Realized Opportunities for Relationship between staff and residents (β = 0.083, 95% CI: 0.04–0.126, adjusted p = .0012; Table 3) and decreased negative staff interactions with residents (β = −0.035, 95% CI: −0.062 to −0.009, adjusted p = .0288).
Table 3.
Post- vs Pre-intervention Association of the LOCK-Based Intervention With RAISE Measures, Adjusting for Site
| βa | 95% CI | FDR adjusted p valuea | |
|---|---|---|---|
| Resident engagement, active | 0.017 | −0.034 to 0.069 | .585 |
| Realized opportunities for relationshipb | 0.083 | 0.040–0.126 | .0012 |
| Quality of staff interactions with residentsc | |||
| Positive | 0.055 | 0.000–0.111 | .1 |
| Negative | −0.035 | −0.062 to −0.009 | .0288 |
| Emotional toned | |||
| Positive | 0.011 | −0.027 to 0.048 | .585 |
| Negative | −0.003 | −0.011 to 0.004 | .5625 |
Note: CI = confidence interval; FDR = false discovery rate; RAISE = Resident-centered Assessment of Interactions with Staff and Engagement.
aFDR adjusted p values to account for multiple hypothesis testing.
bVerbal/nonverbal staff interactions with residents, based on observations of staff providing routine care to residents.
cBased on observations of staff who were verbally/nonverbally interacting with residents.
dBased on observations of staff and residents.
Qualitative Findings
Across all CLCs, we conducted 66 interviews (range: 5–23). Qualitative analysis focused on describing staff impressions of how the intervention affected their behaviors (as per the COM-B model). Behaviors grouped into two themes: “Identifying Opportunities for Engagement” and “Quality of Interactions Between Residents and Staff.”
Identifying Opportunities for Engagement
Conducting observations of life in the CLC as part of the intervention helped staff notice opportunities for engagement with residents. They became particularly aware of times when residents were waiting for events or when there were no formal recreational activities planned. A nurse practitioner described her initial experience of recognizing opportunities for engagement:
“You feel bad when you… actually see nothing is going on.”
Staff also frequently noted recognizing previously missed opportunities to engage with residents during care activities, particularly around the process of handing out medications:
“I’ve noticed people really trying to connect with patients instead of just handing out meds. They can do their job and interact with people. [Observing] shows nurses or RNs that they can do more than just meds.” (Recreational Therapist)
Several participants described how staff, as they became aware of times of lower activity, initiated activities and spent more time interacting with residents to improve engagement. This nurse manager shared her surprise at the change she observed among her staff:
“Last week my CNA […] saw the residents just sitting there waiting for lunch. She […] brought out some games to get people engaged while they were waiting for their meal. That had never occurred before. She just got them all involved while they were waiting and took away the distraction of the residents’ trays being late…CNAs normally did not take initiative, and now I see them taking more initiative.”
Many participants shared that observing the outcomes of improved resident-staff engagement motivated staff to continue their efforts in the project. In some cases, the positive outcomes led to wider change that included staff not participating directly in the study. A registered nurse described how improved engagement with residents became a habit and improved the quality of care residents received:
“It becomes an instinct. When they see someone walking around on his own, they just go over and meet them in the middle and hold their hand and walk together instead of letting him wander around. You think it’s just a very small thing, but those are the ones that prevent bigger things from happening.”
Several participants, such as this ward clerk, described how non-nursing staff also became involved in the efforts to improve resident engagement:
“The biggest impact is to encourage everyone, from all walks of life, different staff, to pay close attention to the residents. […] You don’t have to be a nurse. As a housekeeper or secretary you can see things. It also encourages us to engage with the guys. Before we were like, ‘Fragile population, I don’t want to do anything to hurt them.’ Now you can go in there and interact with them and they like that. It’s really nice. Before I would wave to them, but now I can go in there and crack a joke or tell a silly story and open up.”
Quality of Interactions Between Residents and Staff
The act of doing observations also challenged many participants’ perceptions of how well they were engaging with residents. As a result of a new awareness, many staff members, including one registered nurse, reported adapting their interactions with residents to be more engaging:
“The tool is good to make people more cognizant of their behavior. It gets staff more engaged with the residents rather than hanging out and gossiping with each other.”
Participants reported a variety of ways they modified their behavior, including increased physical touch, brief acknowledgements, and conversation (e.g., during meal times, direct care activities, and medication distribution). Many participants felt they were able to learn more about resident preferences, particularly around food, activities, and verbal/nonverbal communication styles, through the increased engagement. As one registered nurse described, learning how to better engage residents was also personally rewarding:
“Observing the relationships allowed them to learn things about the residents or about the families […] It was educational just to see how they [residents] can communicate – not only verbally, but body language, and getting residents to smile and talk back and interact. It was really rewarding from that standpoint.”
Several CLC staff reported that the increased knowledge of resident preferences, derived from improved engagement, created the sense that their work day was easier. One licensed practical nurse described her experience:
“It eases the workload, because when you have an engaged person who’s not bored out of their mind, they’re calmer and you’re not running back and forth to the room.”
A neighborhood clerk described how even small gestures could improve resident engagement:
“Lately, when we got them up and stuff, and we got a free moment, and we see the patient just sitting there, somebody will go interact with them. And it brought life to them. They will offer them a snack or give them a little conversation and that seems to make them bright up more. And it really did.”
This was also true for residents with dementia. One assistant nurse manager reported that learning more about the preferences of a new resident with advanced dementia and aphasia led to the resident being more cooperative during direct care because he felt more comfortable with the staff. Another nurse manager said:
“I believe that even though they are not aware, they do have that sense of emotion. If you’re in a good mood, they’re in a good mood.”
Several participants felt that sharing information about residents in huddles improved interactions and the quality of care residents received. A nurse educator noticed that huddling helps the staff identify “who’s more in tune with certain residents” so they could provide care for that resident more regularly or be called in for challenging situations. The huddles also encouraged staff to be mindful of engagement on a regular basis, as described by a licensed practical nurse:
“It made everyone more aware [of engagement]. […] the huddles where they were able to talk about it, that really helped.”
Discussion
We built the LOCK-based intervention on the evidence-based premise that, for nursing home residents, positive interactions with staff and engagement in daily life contribute meaningfully to quality of life outcomes (Lawrence, Fossey, Ballard, Moniz-Cook, & Murray, 2012; Sullivan & Asselin, 2013). Although the positive effects of improving resident-staff interactions and increasing resident engagement are well established (Kolanowski, Litaker, Buettner, Moeller, & Costa, 2011; Schreiner et al., 2005), it has been challenging to move beyond researcher-delivered interventions to internally facilitated interventions that are feasible and sustainable beyond the life of the research endeavor. We aimed to achieve improvements in staff interactions with residents while relying primarily on internal facilitation for intervention delivery and sustainment. Our data suggest the intervention was successful in several respects.
Quantitative analyses indicated increased staff behaviors related to Realized Opportunities for building Relationship and decreased negative staff interactions with residents post-intervention. Our qualitative data supported these findings. Staff consistently reported a newly developed increased understanding of the impact of resident-staff interaction, an appreciation of the importance of resident engagement, sensitivity to instances of lack of resident engagement, and an increased awareness of times staff were and were not engaging with residents. The finding that negative staff interactions with residents decreased is noteworthy, given the evidence that negative staff interactions are linked with negative resident outcomes such as increased resistiveness to care (Lann-Wolcott, Medvene, & Williams, 2011; Williams & Herman, 2011). Our findings are also consistent with other studies demonstrating that staff respond positively to interventions to improve resident-staff interactions (Meeks, Van Haitsma, Schoenbachler, & Looney, 2015; Passalacqua & Harwood, 2012).
We developed the concept of Realizing Opportunities for building Relationship to highlight the possibility of staff using existing time to improve their relationships with residents through interactions in the course of daily routines. By interacting positively while working within a residents’ personal space, busy staff can increase resident engagement by using opportunities that are already present. In a major evaluation of the Green House model of person-centered care, aides were observed spending almost five times as long engaging with residents compared with traditional nursing home aides. Multitasking played an important role in this engagement success, with one-third of the total engagement time occurring while aides performed other activities, such as preparing a meal or folding laundry (Sharkey, Hudak, Horn, James, & Howes, 2011). The potential impact of such multitasking is highlighted by the large amount of time residents spend receiving personal care (18% in one time-sampling study [Harper Ice, 2002]) that could involve resident engagement and by the compelling evidence from time-sampling studies that nursing home residents do not receive enough interaction with staff and spend most of their time unengaged (Kolanowski & Litaker, 2006; Schreiner et al., 2005). One study reported that multitasking of resident interaction with hygiene and nutrition duties occurred in less than 20% of observed care encounters (Munyisia, Yu, & Hailey, 2011). Such non-communicative encounters are likely fraught with potential for negative outcomes such as resident distress, agitation, and aggression.
The bite-size nature of Realized Opportunities for building Relationship is also consistent with the science of habit, which underscores that behavior changes are most likely to be sustained when they can be repeated regularly (Lally & Gardner, 2013). The brief nature of interactions during direct care may have contributed to staff success with incorporating Realized Opportunities for building Relationship behavior change. Changes focused on Realized Opportunities for building Relationship may also have a positive economic impact because they require no changes in staffing ratios—a potentially fruitful area for future research.
Internal facilitators proved key to the success of our intervention. Research staff provided some external support, but it was largely up to the CLC-based internal facilitators to deliver the intervention to their staff. Staff themselves collected engagement and interaction data using short observational QI tools. It was expected that the observation experiences along with the feedback provided by the data would be among the active behavior change ingredients of the intervention. Although the published literature includes examples of many engagement and interaction interventions that yielded positive results when the investigator team themselves delivered the intervention (e.g., Barbosa, Marques, Sousa, Nolan, & Figueiredo, 2016; Coleman, Medvene, & Van Haitsma, 2013), studies using internal facilitators are rarer and typically include intensive, multi-day trainings provided by external facilitators (Roberts, Morley, Walters, Malta, & Doyle, 2015; Stein-Parbury et al., 2012; van Weert et al., 2006). To the best of our knowledge, the intensity of our external facilitation was less than that described in any other published nursing home interaction or engagement intervention. We posit that the sustainability of interventions such as ours, with more limited external facilitation, will be greater than that experienced by prior studies and hope to investigate this in the future.
Limitations
Several limitations are worthy of note. Our study used a staff-focused intervention that was designed, through changes in staff behavior, to affect resident engagement. But primary data collection from residents was only through a survey, and our main measure of resident engagement was from structured observations. Future work of this type would ideally assess resident engagement through longitudinal qualitative data collection from residents, such as through interviews, PhotoVoice, etc. In addition, the researchers’ structured observations may have produced a Hawthorne effect, although the observation interval per target individual was only 5 s, and our extensive work with the RAISE instrument suggests that the short actual observation interval for each target, combined with the 20-min data collection timeframe—which allows the observer to blend more into the landscape—reduces this possibility. In addition, any effect would likely have been the same for both pre- and post-implementation observations. Our opportunistic and snowball sampling methodology meant that the CLCs participating in this study, while coming from different areas of the country, may not be representative of CLCs in general. Our results, however, were indicative of the potential for success of the intervention across different CLC types and, in consequence, the entire program described here and elsewhere (Hartmann et al., 2017; Mills et al., 2017) was rolled out nationally to all CLCs in the Veterans Health Administration system.
The staff survey had a somewhat low response rate but one that is comparable to or better than other surveys performed in VA (Linsky, Meterko, Stolzmann, & Simon, 2017; Sullivan et al., 2013). In addition, to ameliorate some effects of potential biases, we triangulated data sources, having both residents and staff respond to the same survey instrument. However, due to limited sample sizes, our quantitative analyses were at the CLC level rather than neighborhood level and did not control for CLC characteristics such as size or resident case-mix. Future studies with larger sample sizes would be useful to investigate differential effects of such variables.
In the interview portion of the study, CLC staff may have felt uncomfortable responding negatively about the program because the research staff who conducted the training and support activities were also those who conducted the interviews. We also did not include residents with cognitive impairments as respondents for the resident survey due to concerns about adequate informed consent and used a convenience sample of residents due to the time constraints imposed by a short site visit comprising many components. This may have resulted in a response bias. Although multiple attempts were made to contact all residents on the lists we received, residents who were continually out of the CLC were less likely to be interviewed, and these may have included some of the highest functioning residents. Finally, because of the mixed-methods nature of the study, findings presented from each set of analyses are missing some richness and detail.
Implications
This study provides preliminary support for a new approach to improving resident–staff interaction and resident engagement that relies on the LOCK model. We found that nursing home staff were favorably impacted by experiences in which they positively engaged with residents and by the opportunity to witness, as a consequence of their actions, what they perceived as meaningful and pleasant engagement on the part of the residents they cared for. Using the combination of observations, huddles, and a focus on the positive to support staff in discovering the causal relationship between resident engagement and resident well-being proved effective. Larger tests of this LOCK-based intervention or similar relational team-based approaches for other outcomes or combinations of outcomes would be a logical extension of this work.
Funding
This work was supported by the Department of Veterans Affairs, Veterans Health Administration, Office of Research and Development, Health Services Research and Development (I01HX000797) and Department of Veterans Affairs, Veterans Health Administration, Office of Research and Development, Rehabilitation Research and Development (IK2RX001241 to W. L. Mills).
Acknowledgement
The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs.
Conflict of Interest
None reported.
References
- Alexander J. A., & Hearld L. R (2011). The science of quality improvement implementation: Developing capacity to make a difference. Medical Care, 49(Suppl), S6–20. doi:10.1097/MLR.0b013e3181e1709c [DOI] [PubMed] [Google Scholar]
- Barbosa A., Marques A., Sousa L., Nolan M., & Figueiredo D (2016). Effects of a psycho-educational intervention on direct care workers’ communicative behaviors with residents with dementia. Health Communication, 31, 453–459. doi:10.1080/10410236.2014.965382 [DOI] [PubMed] [Google Scholar]
- Beerens H. C., de Boer B., Zwakhalen S. M., Tan F. E., Ruwaard D., Hamers J. P., & Verbeek H (2016). The association between aspects of daily life and quality of life of people with dementia living in long-term care facilities: A momentary assessment study. International Psychogeriatrics, 28, 1323–1331. doi:10.1017/S1041610216000466 [DOI] [PubMed] [Google Scholar]
- Beerens H. C., Zwakhalen S. M. G., Verbeek H., E. S. Tan F., Jolani S., Downs M., … Hamers J. P. H (2018). The relation between mood, activity, and interaction in long-term dementia care. Aging & Mental Health, 22, 26–32. doi:10.1080/13607863.2016.1227766 [DOI] [PubMed] [Google Scholar]
- Benjamini Y., & Hochberg Y (1995). Controlling the false discovery rate: A practical and powerful approach to multiple testing. Journal of the Royal Statistical Society, Series B (Methodological), 57, 289–300. [Google Scholar]
- Bradley E. H., Curry L. A., & Devers K. J (2007). Qualitative data analysis for health services research: Developing taxonomy, themes, and theory. Health Services Research, 42, 1758–1772. doi:10.1111/j.1475-6773.2006.00684.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradley E. H., Curry L. A., Ramanadhan S., Rowe L., Nembhard I. M., & Krumholz H. M (2009). Research in action: Using positive deviance to improve quality of health care. Implementation Science, 4, 25. doi:10.1186/1748-5908-4-25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carpiac-Claver M. L., & Levy-Storms L (2007). In a manner of speaking: Communication between nurse aides and older adults in long-term care settings. Health Communication, 22, 59–67. doi:10.1080/10410230701310307 [DOI] [PubMed] [Google Scholar]
- Castle N. G. (2007). Assessing job satisfaction of nurse aides in nursing homes: The nursing home nurse aide job satisfaction questionnaire. Journal of Gerontological Nursing, 33, 41–47. [DOI] [PubMed] [Google Scholar]
- Castle N. G. (2010). An instrument to measure job satisfaction of certified nurse assistants. Applied Nursing Research, 23, 214–220. doi:10.1016/j.apnr.2008.09.005 [DOI] [PubMed] [Google Scholar]
- Coleman C. K., Medvene L. J., & Van Haitsma K (2013). A person-centered care intervention for geriatric certified nursing assistants. The Gerontologist, 53, 687–698. doi:10.1093/geront/gns135 [DOI] [PubMed] [Google Scholar]
- Fleming A., Bradley C., Cullinan S., & Byrne S (2014). Antibiotic prescribing in long-term care facilities: A qualitative, multidisciplinary investigation. BMJ Open, 4, e006442. doi:10.1136/bmjopen-2014-006442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibson C. B. (2017). Elaboration, generalization, triangulation, and interpretation: On enhancing the value of mixed method research. Organizational Research Methods, 20, 193–223. doi:10.1177/1094428116639133 [Google Scholar]
- Harper Ice G. (2002). Daily life in a nursing home. Journal of Aging Studies, 16, 345–359. doi:10.1016/s0890-4065(02)00069-5 [Google Scholar]
- Hartmann C. W., Palmer J. A., Mills W. L., Pimentel C. B., Allen R. S., Wewiorski N. J., … Snow A. L (2017). Adaptation of a nursing home culture change research instrument for frontline staff quality improvement use. Psychological Services, 14, 337–346. doi:10.1037/ser0000137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haugan G. (2014). The relationship between nurse-patient interaction and meaning-in-life in cognitively intact nursing home patients. Journal of Advanced Nursing, 70, 107–120. doi:10.1111/jan.12173 [DOI] [PubMed] [Google Scholar]
- Kolanowski A., & Litaker M (2006). Social interaction, premorbid personality, and agitation in nursing home residents with dementia. Archives of Psychiatric Nursing, 20, 12–20. doi:10.1016/j.apnu.2005.08.006 [DOI] [PubMed] [Google Scholar]
- Kolanowski A., Litaker M., Buettner L., Moeller J., & Costa P. T. Jr (2011). A randomized clinical trial of theory-based activities for the behavioral symptoms of dementia in nursing home residents. Journal of the American Geriatrics Society, 59, 1032–1041. doi:10.1111/j.1532-5415.2011.03449.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lally P., & Gardner B (2013). Promoting habit formation. Health Psychology Review, 7(suppl. 1), S137–S158. doi:10.1080/17437199.2011.603640 [Google Scholar]
- Lann-Wolcott H., Medvene L. J., & Williams K (2011). Measuring the person-centeredness of caregivers working with nursing home residents with dementia. Behavior Therapy, 42, 89–99. doi:10.1016/j.beth.2010.02.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawrence V., Fossey J., Ballard C., Moniz-Cook E., & Murray J (2012). Improving quality of life for people with dementia in care homes: Making psychosocial interventions work. British Journal of Psychiatry, 201, 344–351. doi:10.1192/bjp.bp.111.101402 [DOI] [PubMed] [Google Scholar]
- Lincoln Y. S., & Guba E. G (1985). Naturalistic inquiry. Newbury Park, CA: Sage Publications. [Google Scholar]
- Linsky A., Meterko M., Stolzmann K., & Simon S. R (2017). Supporting medication discontinuation: Provider preferences for interventions to facilitate deprescribing. BMC Health Services Research, 17, 447. doi:10.1186/s12913-017-2391-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meeks S., Shah S. N., & Ramsey S. K (2009). The pleasant events schedule - nursing home version: A useful tool for behavioral interventions in long-term care. Aging & Mental Health, 13, 445–455. doi:10.1080/13607860802534617 [DOI] [PubMed] [Google Scholar]
- Meeks S., Van Haitsma K., Schoenbachler B., & Looney S. W (2015). BE-ACTIV for depression in nursing homes: Primary outcomes of a randomized clinical trial. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 70, 13–23. doi:10.1093/geronb/gbu026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michie S., Atkins L., & West R (2014). The behaviour change wheel: A guide to designing interventions. London, Great Britain: Silverback Publishing. [Google Scholar]
- Michie S., van Stralen M. M., & West R (2011). The behaviour change wheel: A new method for characterising and designing behaviour change interventions. Implementation Science, 6, 42. doi:10.1186/1748-5908-6-42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mills W. L., Pimentel C. B., Palmer J. A., Snow A. L., Wewiorski N. J., Allen R. S., & Hartmann C. W (2017). Applying a theory-driven framework to guide quality improvement efforts in nursing homes: The LOCK model. The Gerontologist. 2017 June 23. [Epub ahead of print] doi:10.1093/geront/gnx023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moos R., & Otto J (1972). The Community-Oriented Programs Environment Scale: A methodology for the facilitation and evaluation of social change. Community Mental Health Journal, 8, 28–37. [DOI] [PubMed] [Google Scholar]
- Moos R. H. (2009). Community Oriented Programs Environment Scale sampler set: Manual, instrument, and scoring guide. 4th ed Palo Alto, CA: Mind Garden, Inc. [Google Scholar]
- Munyisia E. N., Yu P., & Hailey D (2011). How nursing staff spend their time on activities in a nursing home: An observational study. Journal of Advanced Nursing, 67, 1908–1917. doi:10.1111/j.1365-2648.2011.05633.x [DOI] [PubMed] [Google Scholar]
- Passalacqua S. A., & Harwood J (2012). VIPS communication skills training for paraprofessional dementia caregivers: An intervention to increase person-centered dementia care. Clinical Gerontologist, 35, 425–445. doi:10.1080/07317115.2012.702655 [Google Scholar]
- Peiris D., Thompson S. R., Beratarrechea A., Cardenas M. K., Diez-Canseco F., Goudge J., … Yusoff K (2015). Behaviour change strategies for reducing blood pressure-related disease burden: Findings from a global implementation research programme. Implementation Science, 10, 158. doi:10.1186/s13012-015-0331-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ritchie M. J., Dollar K. M., Miller C. J., Oliver K. A., Smith J. L., Lindsay J. A., & Kirchner J. E (2017). Using implementation facilitation to improve care in the Veterans Health Administration (version 2) Retrieved from https://www.queri.research.va.gov/tools/implementation/Facilitation-Manual.pdf
- Roberts G., Morley C., Walters W., Malta S., & Doyle C (2015). Caring for people with dementia in residential aged care: Successes with a composite person-centered care model featuring Montessori-based activities. Geriatric Nursing (New York, N.Y.), 36, 106–110. doi:10.1016/j.gerinurse.2014.11.003 [DOI] [PubMed] [Google Scholar]
- Schreiner A. S., Yamamoto E., & Shiotani H (2005). Positive affect among nursing home residents with Alzheimer’s dementia: The effect of recreational activity. Aging & Mental Health, 9, 129–134. doi:10.1080/13607860412331336841 [DOI] [PubMed] [Google Scholar]
- Sharkey S. S., Hudak S., Horn S. D., James B., & Howes J (2011). Frontline caregiver daily practices: A comparison study of traditional nursing homes and the Green House project sites. Journal of the American Geriatrics Society, 59, 126–131. doi:10.1111/j.1532-5415.2010.03209.x [DOI] [PubMed] [Google Scholar]
- Smit D., de Lange J., Willemse B., Twisk J., & Pot A. M (2016). Activity involvement and quality of life of people at different stages of dementia in long term care facilities. Aging & Mental Health, 20, 100–109. doi:10.1080/13607863.2015.1049116 [DOI] [PubMed] [Google Scholar]
- Smith R., Mathews R. M., & Gresham M (2010). Pre- and postoccupancy evaluation of new dementia care cottages. American Journal of Alzheimer’s Disease and Other Dementias, 25, 265–275. doi:10.1177/1533317509357735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snow A. L., Jacobs M. L., Palmer J. A., Parmelee P. A., Allen R. S., Wewiorski N. J., … Hartmann C. W (2018). Development of a new tool for systematic observation of nursing home resident and staff engagement and relationship. The Gerontologist, 58, e15–e24. doi:10.1093/geront/gnw255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein-Parbury J., Chenoweth L., Jeon Y. H., Brodaty H., Haas M., & Norman R (2012). Implementing person-centered care in residential dementia care. Clinical Gerontologist, 35, 404–424. doi:10.1080/07317115.2012.702654 [Google Scholar]
- Stetler C. B., Legro M. W., Rycroft-Malone J., Bowman C., Curran G., Guihan M., … Wallace C. M (2006). Role of “external facilitation” in implementation of research findings: A qualitative evaluation of facilitation experiences in the Veterans Health Administration. Implementation Science, 1, 23. doi:10.1186/1748-5908-1-23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suen H., & Ary D (1989). Analyzing quantitative behavioral observation data. Hillsdale, NJ: Erlbaum. [Google Scholar]
- Sullivan J. L., Meterko M., Baker E., Stolzmann K., Adjognon O., Ballah K., & Parker V. A (2013). Reliability and validity of a person-centered care staff survey in Veterans Health Administration Community Living Centers. The Gerontologist, 53, 596–607. doi:10.1093/geront/gns140 [DOI] [PubMed] [Google Scholar]
- Sullivan L. J., & Asselin M. E (2013). Revisiting quality of life for elders in long-term care: An integrative review. Nursing Forum, 48, 191–204. doi:10.1111/nuf.12030 [DOI] [PubMed] [Google Scholar]
- Travers C., Brooks D., Hines S., O’Reilly M., McMaster M., He W., … Beattie E (2016). Effectiveness of meaningful occupation interventions for people living with dementia in residential aged care: A systematic review. JBI Database of Systematic Reviews and Implementation Reports, 14, 163–225. doi:10.11124/JBISRIR-2016-003230 [DOI] [PubMed] [Google Scholar]
- van Weert J. C., Janssen B. M., van Dulmen A. M., Spreeuwenberg P. M., Bensing J. M., & Ribbe M. W (2006). Nursing assistants’ behaviour during morning care: Effects of the implementation of Snoezelen, integrated in 24-hour dementia care. Journal of Advanced Nursing, 53, 656–668. doi:10.1111/j.1365-2648.2006.03772.x [DOI] [PubMed] [Google Scholar]
- Williams K. N., & Herman R. E (2011). Linking resident behavior to dementia care communication: Effects of emotional tone. Behavior Therapy, 42, 42–46. doi:10.1016/j.beth.2010.03.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson C. B., & Davies S (2009). Developing relationships in long term care environments: The contribution of staff. Journal of Clinical Nursing, 18, 1746–1755. doi:10.1111/j.1365-2702.2008.02748.x [DOI] [PubMed] [Google Scholar]
- Wood W., Harris S., Snider M., & Patchel S. A (2005). Activity situations on an Alzheimer’s disease special care unit and resident environmental interactions, time use, and affect. American Journal of Alzheimer’s Disease and Other Dementias, 20, 105–118. doi:10.1177/153331750502000210 [DOI] [PMC free article] [PubMed] [Google Scholar]