Abstract
Background
Alcohol use and misuse in young people is a major risk behaviour for mortality and morbidity. Motivational interviewing (MI) is a popular technique for addressing excessive drinking in young adults.
Objectives
To assess the effects of motivational interviewing (MI) interventions for preventing alcohol misuse and alcohol‐related problems in young adults.
Search methods
We identified relevant evidence from the Cochrane Central Register of Controlled Trials (CENTRAL) (2015, Issue 12), MEDLINE (January 1966 to July 2015), EMBASE (January 1988 to July 2015), and PsycINFO (1985 to July 2015). We also searched clinical trial registers and handsearched references of topic‐related systematic reviews and the included studies.
Selection criteria
We included randomised controlled trials in young adults up to the age of 25 years comparing MIs for prevention of alcohol misuse and alcohol‐related problems with no intervention, assessment only or alternative interventions for preventing alcohol misuse and alcohol‐related problems.
Data collection and analysis
We used the standard methodological procedures expected by Cochrane.
Main results
We included a total of 84 trials (22,872 participants), with 70/84 studies reporting interventions in higher risk individuals or settings. Studies with follow‐up periods of at least four months were of more interest in assessing the sustainability of intervention effects and were also less susceptible to short‐term reporting or publication bias. Overall, the risk of bias assessment showed that these studies provided moderate or low quality evidence.
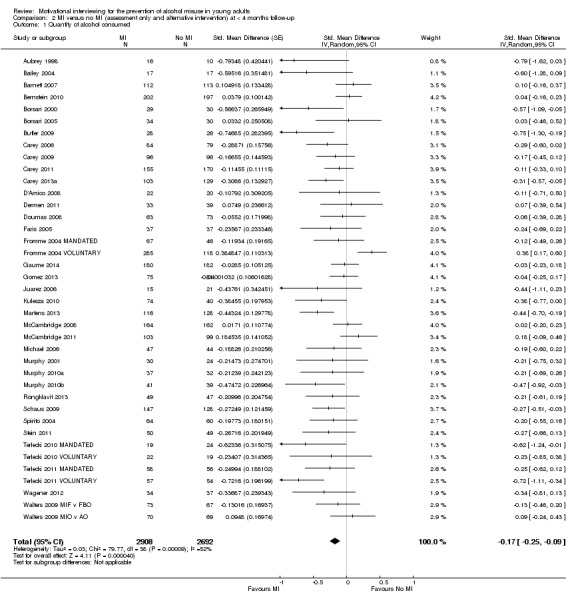
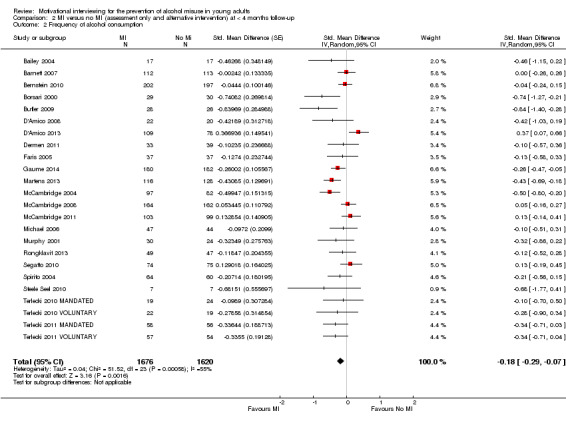
At four or more months follow‐up, we found effects in favour of MI for the quantity of alcohol consumed (standardised mean difference (SMD) −0.11, 95% confidence interval (CI) −0.15 to −0.06 or a reduction from 13.7 drinks/week to 12.5 drinks/week; moderate quality evidence); frequency of alcohol consumption (SMD −0.14, 95% CI −0.21 to −0.07 or a reduction in the number of days/week alcohol was consumed from 2.74 days to 2.52 days; moderate quality evidence); and peak blood alcohol concentration, or BAC (SMD −0.12, 95% CI −0.20 to 0.05, or a reduction from 0.144% to 0.131%; moderate quality evidence).
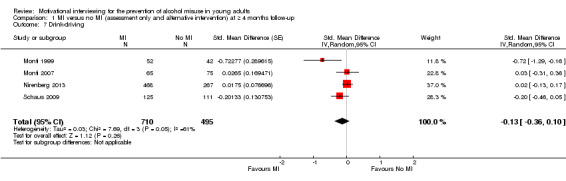
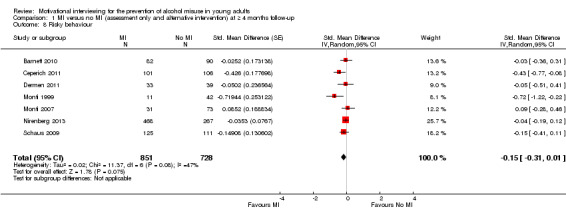
We found a marginal effect in favour of MI for alcohol problems (SMD −0.08, 95% CI −0.17 to 0.00 or a reduction in an alcohol problems scale score from 8.91 to 8.18; low quality evidence) and no effects for binge drinking (SMD −0.04, 95% CI −0.09 to 0.02, moderate quality evidence) or for average BAC (SMD −0.05, 95% CI −0.18 to 0.08; moderate quality evidence). We also considered other alcohol‐related behavioural outcomes, and at four or more months follow‐up, we found no effects on drink‐driving (SMD −0.13, 95% CI −0.36 to 0.10; moderate quality of evidence) or other alcohol‐related risky behaviour (SMD −0.15, 95% CI −0.31 to 0.01; moderate quality evidence).
Further analyses showed that there was no clear relationship between the duration of the MI intervention (in minutes) and effect size. Subgroup analyses revealed no clear subgroup effects for longer‐term outcomes (four or more months) for assessment only versus alternative intervention controls; for university/college vs other settings; or for higher risk vs all/low risk participants.
None of the studies reported harms related to MI.
Authors' conclusions
The results of this review indicate that there are no substantive, meaningful benefits of MI interventions for preventing alcohol use, misuse or alcohol‐related problems. Although we found some statistically significant effects, the effect sizes were too small, given the measurement scales used in the included studies, to be of relevance to policy or practice. Moreover, the statistically significant effects are not consistent for all misuse measures, and the quality of evidence is not strong, implying that any effects could be inflated by risk of bias.
Plain language summary
Motivational interviewing (MI) for preventing alcohol misuse in young adults is not effective enough
Review question
We reviewed the evidence about the effect of motivational interviewing (MI), a way of counselling to bring out and strengthen reasons for changing behaviour, for preventingalcohol misuse in young people.
Background
Alcohol misuse results in about 3.3 million deaths each year worldwide. Around 9% of deaths that occur in people aged 15 to 29 years are attributable to alcohol, mainly resulting from car accidents, homicides (murders), suicides and drownings.
We wanted to find out if MI had an effect on the prevention of alcohol misuse and problems in young adults aged up to 25 years. If those involved with tackling alcohol misuse in young people are to apply MI in practice, clear evidence needs to support it.
Search date: the evidence was current to December 2015.
Study characteristics
We found a total of 84 randomised controlled trials (studies where participants were randomly divided into one of two or more treatment or control groups) that compared MI with either no intervention or with a different approach. Seventy of these trials focused on higher risk individuals or settings. We were mainly interested in trials with a follow‐up period of 4 or more months, and the typical follow‐up period was 12 months. We also evaluated the quality of the studies' designs and their applicability to our research, finding that these studies provided moderate to low quality evidence.
In 66 trials, the MI consisted of a single, individual session. In 12 studies, young people attended multiple individual sessions or mixtures of both individual sessions and group sessions. Six trials used group MI sessions only. The length of MI sessions varied, but in 57 studies it was one hour or less. The shortest MI intervention was 10 to 15 minutes, and the longest had five dedicated MI sessions over a 19‐hour period.
Settings for the trials varied: 58 of the 84 studies took place in college (mainly university but also four vocational) settings. The remaining trials took place in healthcare locations, a youth centre, local companies, a job‐related training centre, an army recruitment setting, UK drug agencies and youth prisons.
The total number of young adults was 22,872, aged on average from 15 to 24 years old. The proportion of males in the trials with both males and females ranged from 22% to 90%. The ethnicity of the young adults was typically mixed, but 52 of the 67 studies that reported ethnicity involved mostly white people.
Key results
At four or more months follow‐up, we found only small or borderline effects showing that MI reduced the quantity of alcohol consumed, frequency of alcohol consumption, alcohol problems and peak blood alcohol concentration (BAC). We didn't find any effects for binge drinking, average BAC, drink‐driving or other alcohol‐related risky behaviour. We found no relationship between the length of MI and its effectiveness. Also, there were no clear subgroup differences in effects when we examined the type of comparison group (assessment only control or alternative intervention, the setting (college/university vs other settings), or risk status (higher risk students vs all/low‐risk students).
None of the studies reported harms related to MI.
Although we found some significant effects for MI, our reading of these results is that the strength of the effects was slight and therefore unlikely to confer any advantage in practice.
Quality of evidence
Overall, there is only low or moderate quality evidence for the effects found in this review. Many of the studies did not adequately describe how young people were allocated to the study groups or how they concealed the group allocation to participants and personnel. Study drop‐outs were also an issue in many studies. These problems with study quality could result in inflated estimates of MI effects, so we cannot rule out the possibility that any slight effects observed in this review are overstated.
The US National Institutes of Health provided funding for half (42/84) of the studies included in this review. Twenty‐nine studies provided no information about funding, and only eight papers had a clear conflict of interest statement.
Summary of findings
Summary of findings for the main comparison. Summary of findings ‐ 4 months or more of follow‐up.
| Motivational interviewing versus no motivational interviewing (assessment only or alternative intervention) for prevention of alcohol misuse | ||||||
|
Patient or population:young adults aged up to 25 years Settings: education, health, criminal justice or community settings Intervention: motivational interviewing Comparison: no intervention/placebo/treatment as usual Follow‐up: ≥ 4 months Measurement: self reported alcohol consumption (questionnaire scale) | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Quantity of alcohol consumed | The mean number of drinks per week was 13.74 in the control group, with a standard deviation of 10.77, from the DDQ measure in Martens 2013 | The SMD from the meta‐analysis (−0.11) corresponds to a decrease of 1.2 drinks consumed each week (95% CI 0.7 to 1.6), from an average of 13.7 drinks per week to 12.5 drinks per week, based on Martens 2013 | SMD −0.11 (−0.15 to −0.06) | 7971 (33) | ⊕⊕⊕⊝ Moderate | Downgraded 1 level due to risk of bias |
| Frequency of alcohol consumption | The mean drinking days per week was 2.74 in the control group, with a standard deviation of 1.54, from the DDQ measure in Martens 2013 | The SMD from the meta‐analysis (−0.14) corresponds to a decrease of 0.22 drinking days per week (95% CI 0.11 to 0.32), from an average of 2.74 drinking days per week to 2.52 drinking days per week, based on Martens 2013 | SMD −0.14 (−0.21 to −0.07) | 4377 (17) | ⊕⊕⊕⊝ Moderate | Downgraded 1 level due to risk of bias |
| Binge drinking | Binge drinking frequency in the previous month was 5.05 at baseline for the whole sample, with a standard deviation of 4.53, in the study by Carey 2011 | The SMD from the meta‐analysis (−0.04) corresponds to a decrease in binge drinking frequency in the previous month of −0.2 binge drinking occasions (95% CI −0.4 to 0.1), from an average of 5.1 occasions to 4.9 occasions per week, based on Carey 2011. | SMD −0.04 (−0.09 to 0.02) | 5479 (21) | ⊕⊕⊕⊝ Moderate | Downgraded 1 level due to risk of bias |
| Alcohol problems | The mean alcohol problems scale score was 8.91 in the control group, with a standard deviation of 9.17 (the 69‐point RAPI scale used by Martens 2013) | The SMD from the meta‐analysis (−0.08) corresponds to a decrease of 0.73 on the alcohol problems scale score (95% CI 0.00 to 1.56), from an average of 8.91 to 8.18, based on Martens 2013 | SMD −0.08 (−0.17 to 0.00) | 6868 (25) | ⊕⊕⊝⊝ Low | Downgraded 2 levels due to high heterogeneity (I2 = 58%) and risk of bias |
| Average BAC | The average BAC was 0.082% at baseline for the whole sample, with a standard deviation of 0.057, in the study by Carey 2011 | The SMD from the meta‐analysis (−0.05) corresponds to a decrease of −0.003 for average BAC (95% CI −0.010 to 0.005), from an average of 0.082% to 0.079%, based on Carey 2011 | SMD −0.05 (−0.18 to 0.08) | 901 (5) | ⊕⊕⊕⊝ Moderate | Downgraded 1 level due to risk of bias |
| Peak BAC | The mean peak BAC was 0.144% in the control group, with a standard deviation of 0.111, from the DDQ measure in Martens 2013 | The SMD from the meta‐analysis (−0.12) corresponds to a decrease of 0.013 for peak BAC (95% CI 0.006 to 0.025), from an average of 0.144% to 0.131%, based on Martens 2013 | SMD −0.12 (−0.20 to −0.05) | 2790 (13) | ⊕⊕⊕⊝ Moderate | Downgraded 1 level due to risk of bias |
| Drink‐driving | The number of drink‐driving occasions in the previous 12 months was 7.8 at baseline in the control group, with a standard deviation of 16.9, from the DrInC‐2L measure, in Schaus 2009 | The SMD from the meta‐analysis (−0.13) corresponds to a decrease of −2.2 drink‐driving occasions (95% CI −6.1 to 1.7), from an average of 7.8 to 5.6, based on Schaus 2009 | SMD −0.13 (−0.36 to 0.10) | 1205 (4) | ⊕⊕⊕⊝ Moderate | Downgraded 1 level due to high heterogeneity (I2 = 61%) |
| Risky behaviour | The number of times foolish risks were taken in the previous 12 months was 6.6 at baseline in the control group, with a standard deviation of 11.9, from the DrInC‐2L measure, in Schaus 2009 | The SMD from the meta‐analysis (−0.15) corresponds to a decrease of −1.8 risk taking occasions (95% CI −3.7 to 0.1), from an average of 6.6 to 4.8, based on Schaus 2009 | SMD −0.15 (−0.31 to 0.01) | 1579 (7) | ⊕⊕⊕⊝ Moderate | Downgraded 1 level due to risk of bias |
| *The basis for the assumed risk is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). BAC: blood alcohol concentration; CI: confidence interval; SMD: standardised mean difference; DDQ: Daily Drinking Questionnaire; RAPI: Rutgers Alcohol Problems Index. | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
In the columns illustrating comparative risks: for outcomes where the pooled analysis point estimate and confidence interval showed some effect, we have used results (mean scores and standard deviations) from Martens 2013 to illustrate the effect sizes in terms of the measures used in that study. We chose Martens 2013 because the outcome measures they use are well known, generally well regarded, and are typical of the measures used in this field of research: they used the Daily Drinking Questionnaire (DDQ) and the Rutgers Alcohol Problems Index (RAPI). For similar reasons, we used Carey 2011 as a basis for illustrating effect sizes for binge drinking, as they also based their measures on the DDQ, and Schaus 2009 as they used the Drinker Inventory of Consequences (DrInC‐2L; Miller 1995b). Furthermore, the sample sizes were typically larger than similar studies with potentially more reliable indication of variance (SD) for relevant outcomes.
Summary of findings 2. Summary of findings ‐ less than four months follow‐up.
| Motivational interviewing versus no motivational interviewing (assessment only or alternative intervention) for prevention of alcohol misuse | ||||||
|
Patient or population: young people aged up to 25 years Settings: education, health, criminal justice or community settings Intervention: motivational interviewing Comparison: no intervention/placebo/treatment as usual Follow‐up: < 4 months Measurement: self reported alcohol consumption (questionnaire scale) | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Quantity of alcohol consumed | The mean number of drinks per week was 13.74 in the control group, with a standard deviation of 10.77, from the DDQ measure in Martens 2013 | The SMD from the meta‐analysis (−0.18) corresponds to a decrease of 1.8 drinks consumed each week (95% CI 1.0 to 2.7), from an average of 13.7 drinks per week to 11.9 drinks per week, based on Martens 2013 | SMD −0.17 (−0.25 to −0.09) | 5600 (39) | ⊕⊕⊝⊝ Low | Downgraded 2 levels due to high heterogeneity (I2 = 52%) and risk of bias. |
| Frequency of alcohol consumption | The mean drinking days per week was 2.74 in the control group, with a standard deviation of 1.54, from the DDQ measure in Martens 2013 | The SMD from the meta‐analysis (−0.18) corresponds to a decrease of 0.28 drinking days per week (95% CI 0.11 to 0.45), from an average of 2.74 drinking days per week to 2.46 drinking days per week, based on Martens 2013 | SMD −0.18 (−0.29 to −0.07) | 3296 (24) | ⊕⊕⊝⊝ Low | Downgraded 2 levels due to high heterogeneity (I2 = 55%) and risk of bias. |
| Binge drinking | Binge drinking frequency in the previous month was 5.05 at baseline for the whole sample, with a standard deviation of 4.53, in the study by Carey 2011 | The SMD from the meta‐analysis (−0.13) corresponds to a decrease in binge drinking frequency in the previous month of 0.6 binge drinking occasions (95% CI 0.1 to 1.0), from an average of 5.1 occasions to 4.5 occasions per week, based on Carey 2011. | SMD −0.13; (−0.23 to 0.03) | 4090 (25) | ⊕⊕⊝⊝ Low | Downgraded 2 levels due to high heterogeneity (I2 = 54%) and risk of bias. |
| Alcohol problems | The mean alcohol problems scale score was 8.91 in the control group, with a standard deviation of 9.17 (the 69‐point RAPI scale was used by Martens 2013) | The SMD from the meta‐analysis (−0.10) corresponds to a decrease of 0.92 on the alcohol problems scale score (95% CI 0.09 to 1.65), from an average of 8.91 to 7.99, based on Martens 2013 | SMD −0.10; (−0.18 to −0.01) | 5109 (34) | ⊕⊕⊕⊝ Moderate | Downgraded 1 level due to risk of bias |
| Average BAC | The average BAC was 0.082% at baseline for the whole sample, with a standard deviation of 0.057, in the study by Carey 2011 | The SMD from the meta‐analysis (−0.14) corresponds to a decrease of −0.008 for average BAC (95% CI −0.017 to 0.001), from an average of 0.082% to 0.074%, based on Carey 2011 | SMD −0.14; (−0.30 to 0.01) | 1096 (6) | ⊕⊕⊕⊝ Moderate | Downgraded 1 level due to risk of bias |
| Peak BAC | The mean peak BAC was 0.144% in the control group, with a standard deviation of 0.111, from the DDQ measure in Martens 2013 | The SMD from the meta‐analysis (−0.23) corresponds to a decrease of 0.026 for peak BAC (95% CI 0.014 to 0.036), from an average of 0.144% to 0.118%, based on Martens 2013 | SMD −0.23 (−0.32 to −0.13) | 2408 (14) | ⊕⊕⊕⊝ Moderate | Downgraded 1 level due to risk of bias |
| Drink‐driving | The number of drink‐driving occasions in the previous 12 months was 7.8 at baseline in the control group, with a standard deviation of 16.9, from the DrInC‐2L measure, in Schaus 2009 | The SMD from the meta‐analysis (−0.22) corresponds to a decrease of −3.7 drink driving occasions (95% CI −6.4 to 1.0), from an average of 7.8 to 4.1, based on Schaus 2009 | SMD −0.22 (−0.38 to −0.06) | 895 (4) | ⊕⊕⊕⊝ Moderate | Downgraded 1 level due to risk of bias |
| Risky behaviour | The number of times foolish risks were taken in the previous 12 months was 6.6 at baseline in the control group, with a standard deviation of 11.9, from the DrInC‐2L measure, in Schaus 2009 | The SMD from the meta‐analysis (−0.05) corresponds to a decrease of −0.6 risk taking occasions (95% CI −3.9 to 2.6), from an average of 6.6 to 6.0, based on Schaus 2009 | SMD −0.05 (−0.33 to 0.22) | 745 (5) | ⊕⊕⊕⊝ Moderate | Downgraded 1 level due to high heterogeneity (I2 = 67%) |
| *The basis for the assumed risk is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). BAC: blood alcohol concentration; CI: confidence interval; SMD: standardised mean difference; DDQ: Daily Drinking Questionnaire; RAPI: Rutgers Alcohol Problems Index | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
In the columns illustrating comparative risks: for outcomes where the pooled analysis point estimate and confidence interval showed some effect, we have used results (mean scores and standard deviations) from Martens 2013 to illustrate the effect sizes in terms of the measures used in that study. We chose Martens 2013 because the outcome measures they use are well‐known, generally well regarded, and are typical of the measures used in this field of research: they used the Daily Drinking Questionnaire (DDQ) and the Rutgers Alcohol Problems Index (RAPI). For similar reasons, we used Carey 2011 as a basis for illustrating effect sizes for binge drinking, as they also based their measures on the DDQ, and Schaus 2009 as they used the Drinker Inventory of Consequences (DrinC‐2L; Miller 1995b) Furthermore, the sample sizes were typically larger than similar studies with potentially more reliable indication of variance (s.d.) for relevant outcomes.
Background
Description of the condition
Globally, harmful use of alcohol results in approximately 3.3 million deaths each year (WHO 2014). Around 9% of deaths between the ages of 15 and 29 years are attributable to alcohol, mainly resulting from car accidents, homicides, suicides and drownings (WHO 2011). Europe has the highest levels of mortality attributable to alcohol consumption amongst all age groups (WHO 2014).
Hazardous drinking levels for men (consuming over 40 g/day) doubles the risk of liver disease, raised blood pressure, some cancers and violent death (because some people who have this average alcohol consumption drink heavily on some days). For women, over 24 g/day average alcohol consumption increases the risk for developing liver disease and breast cancer (Corrao 1999; Edwards 1994; Greenfield 2001; Thakker 1998).
Description of the intervention
Motivational interviewing (MI) was developed as a way to help people work through ambivalence and commit to change (Miller 1983). Miller 1995a defined MI as "a directive, client‐centred counselling style for eliciting behaviour change by helping clients to explore and resolve ambivalence". As Miller 1996 and Miller 2002 have said, the term 'motivational interviewing' pertains both to a style of relating to others and a set of techniques to facilitate that process. Its five tenets include:
adopting an empathic, non‐judgemental stance;
listening reflectively;
developing discrepancy;
rolling with resistance and avoiding argument;
supporting efficacy to change.
Practitioners commonly combine MI with other intervention components, which have been called adaptations of MI (Burke 2003). The most widely used adaptation of MI is motivational enhancement therapy (MET), which combines MI components with personal feedback of assessment results (Miller 1993).
How the intervention might work
The theoretical basis of MI and motivational enhancement is grounded in client‐centred therapy and social cognitive theory. Firstly, studies have demonstrated that therapist behaviours such as genuineness, warmth and empathy promoted change in the client, while other behaviours such as non‐acceptance and negative confrontation were associated with failure to change or with other unhelpful outcomes (Miller 1993; Paterson 1985). Secondly, the emergence of social cognitive theories helped to promote the recognition that the external, social environment and the individual's interactions with it were important factors in motivation for changing drinking behaviours (Bandura 1977; Maisto 1999). Thirdly, the popularity of the transtheoretical model of behaviour change has increased awareness of change as occurring through a number of stages or steps (Prochaska 1992).
Why it is important to do this review
There have been several reviews of MI in the addiction field in recent years. Noonan 1997 reviewed 11 clinical trials of MIs that were available at the time and concluded that nine of the studies supported the efficacy of MIs for addictive behaviours. Following this study, Dunn 2001 performed a systematic review of 29 randomised trials of brief interventions that claimed to use the principles and techniques of MI and suggested that the strongest evidence for efficacy was found in the alcohol and drug abuse areas. A qualitative review of 26 studies of MIs by Burke 2002b concluded that the research supported the efficacy of MIs for alcohol problems, drug addiction, compliance in patients with hypertension and bulimia, as well as the efficacy of MIs for encouraging compliance in patients with diabetes. Burke 2003 and Burke 2002a performed a meta‐analysis of 30 controlled clinical trials investigating MIs. They concluded that MIs were equivalent to other active treatments and yielded moderate effects compared to no treatment or placebo for problems involving alcohol, drugs, diet and exercise. However, the effectiveness of MI across providers, populations, target problems, and settings was highly variable. Another qualitative review of the use of METs for substance use in adolescents reported that clinical trials of METs indicate that they decrease substance‐related negative consequences and problems, substance use and increase treatment engagement, with results particularly strong for those with heavier substance use patterns, less motivation to change, or both (O' Leary 2004). Hettema 2005 conducted a meta‐analysis of 72 clinical trials spanning a range of target problems including alcohol misuse. The average short‐term between‐group effect size of MI was 0.77, decreasing to 0.30 at one‐year follow‐up. Observed effect sizes of MI were larger with ethnic minority populations and when the practice of MI was not manual‐guided. Vasilaki 2006 conducted a meta‐analysis of 22 studies of the efficacy of MI in reducing alcohol consumption and concluded that brief MI is effective. Similarly, Rubak 2006 conducted a systematic review and meta‐analysis of 72 randomised controlled trials of MI to evaluate the effectiveness of the intervention in different areas of disease and showed a significant effect of MI for combined effect estimates for body mass index, total blood cholesterol, systolic blood pressure, blood alcohol concentration and standard ethanol content. Lundahl 2010 carried out a meta‐analysis of 119 studies targeting outcomes including substance use (tobacco, alcohol, drugs, marijuana), health‐related behaviours (diet, exercise, safe sex), gambling and engagement in treatment variables. Judged against weak comparison groups, MI produced statistically significant, durable results in the small effect range. Smedslund 2011 conducted a Cochrane systematic review of 59 randomised controlled trials to assess the effectiveness of MI for substance abuse on drug use, retention in treatment, readiness to change, and number of repeat convictions. They concluded that MI can reduce the extent of substance abuse compared to no intervention.
Tait 2003 evaluated the effectiveness of brief interventions (BI) with adolescents (mean age < 20 years) in reducing alcohol, tobacco or other drug use by means of a systematic review. They concluded that across a diverse range of settings, BI conferred benefits to adolescent substance users with a small effect on alcohol consumption and related measures. Grenard 2006 reviewed 17 clinical studies of MI interventions applied to adolescents and young adults using alcohol or other psychoactive substances. This review revealed mixed findings for the efficacy of brief MI among these populations. However, in 29% of the studies there was a clear advantage for the brief MI compared to standard care or other programming. Carey 2007 conducted a meta‐analysis of 62 studies and 98 intervention conditions with college drinkers. Over follow‐up intervals lasting up to six months, moderator analyses suggested that individual, face‐to‐face interventions using MI and personalised normative feedback predict greater reductions in alcohol‐related problems. Larimer 2007 conducted a review of the literature on individual‐focused prevention and treatment approaches for college drinking. Evidence was found in support of skills‐based interventions and motivational interventions that incorporated personalised feedback, with or without an in‐person intervention.
However, to our knowledge, the current review is the first examination of the MI literature as a Cochrane systematic review in relation to prevention of alcohol misuse and alcohol‐related problems in young people. If those involved with the prevention of alcohol misuse in young people are to implement MI in practice, clear evidence on its effectiveness is required.
Objectives
To assess the effects of motivational interviewing (MI) interventions for preventing alcohol misuse and alcohol‐related problems in young adults.
The specific objectives were:
to summarise current evidence about the effects of MI versus no intervention or a different intervention, for alcohol consumption and alcohol related problems in young adults;
to investigate whether the effects of MI are modified by the length of the intervention;
to investigate whether the effects of MI vary by type of control group, setting, and risk status.
We made the following comparison: MI versus no MI (assessment only or alternative intervention).
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials (RCTs) and cluster‐RCTs in young adults receiving MIs for prevention of alcohol misuse and alcohol‐related problems compared with no intervention, assessment only or alternative interventions without MI components.
Types of participants
Young adults aged up to 25 years old. We were interested in the effectiveness of MI delivered as a universal strategy (i.e. with individuals regardless of level of risk) and as a targeted strategy (i.e. with individuals identified as being at higher risk).
Types of interventions
Experimental intervention
MIs are defined as a one or more session approach including MI principles (adopting an empathic non‐judgemental stance, listening reflectively, developing discrepancy, rolling with resistance and avoiding argument, supporting efficacy to change) as the core of the intervention as well as a feedback element or other non‐MI techniques.
Comparator intervention(s)
No intervention, assessment only.
Alternative interventions without MI components. Alternative interventions are, for example, self control training, skills‐based training, normative feedback, confrontational feedback, skills‐based counselling, 12‐step facilitation, brief feedback, risk reduction, relapse prevention and cognitive behaviour therapy.
In the main analyses, we group all comparator interventions together, but we ran subgroup comparisons to explore the effects of MI versus alternative interventions, on the one hand, and assessment only controls, on the other.
Types of outcome measures
We reported outcome measures separately according to an a priori categorisation of study follow‐up periods (short‐ versus longer‐term). We defined a short‐term follow‐up period for data collected less than four months after the intervention and longer‐term follow‐up for data collected from four months or more following the intervention. This distinction is consistent with previous work by White 2007, who pointed out that short‐term results (up to four months) should be regarded with caution. We agree and consider shorter‐term results to be less interesting and less reliable, as they provide little information about sustained effects of an intervention, and they are also more susceptible to reporting or publication bias than long‐term outcomes.
Primary outcomes
Alcohol use, misuse and problems: self reported or objective.
Typical self reported measurement scales are, for example, the Daily Drinking Questionnaire (DDQ), Rutgers Alcohol Problem Index (RAPI), Alcohol Addiction Severity Index (AASI), Alcohol Use Disorders Identification Test (AUDIT), Short Michigan Alcoholism Screening Test (S‐MAST) and the Short Alcohol Dependence Data Questionnaire (SADD). Self reported measures include:
quantity of alcohol consumed;
frequency of alcohol consumption;
binge drinking;
alcohol problems (alcohol abuse or dependence).
Objective measures of alcohol misuse are assessed by breath or blood alcohol test and include:
average blood alcohol content (BAC);
peak BAC.
Secondary outcomes
Drink‐driving; driving under the influence (DUI)
Alcohol‐related risky behaviour, e.g. violence, criminal activity, unintended or unprotected sexual behaviour, other drug use, alcohol‐related injuries
Search methods for identification of studies
Electronic searches
We searched the following databases.
Cochrane Central Register of Controlled Trials (CENTRAL) (2015, Issue 12); see Appendix 1.
MEDLINE (January 1966 to July 2015); see Appendix 2.
EMBASE (January 1988 to July 2015); see Appendix 3.
PsycINFO (1985 to July 2015); see Appendix 4.
To identify the studies included in this review, we developed a detailed search strategy for MEDLINE and then adapted it to each of the other databases to take into account differences in controlled vocabulary and syntax rules. There were no language restrictions.
Searching other resources
We handsearched the references of topic‐related systematic reviews and included studies in order to identify potentially relevant citations. Unpublished reports, abstracts, dissertations, brief and preliminary reports were eligible for inclusion. These were identified via handsearching of references of topic‐related systematic reviews and included studies. Some study authors were contacted to collect additional information for meta‐analysis, or to clarify whether papers reported separate studies.
In April 2016, we also undertook a search of the ClinicalTrials.gov registry and the WHO International Clinical Trials Registry Platform (ICTRP).
Data collection and analysis
Selection of studies
Two authors read all titles and abstracts resulting from the search and eliminated any obviously irrelevant studies (screening level 1). We obtained full copies of those remaining, which two authors then independently classified according to the inclusion criteria. We resolved differences of opinion through discussion and where required through involvement of a third reviewer. We used all available information for each study by consulting all companion publications.
Data extraction and management
Two review authors extracted key information by using a standardised data extraction form, discussing and resolving any discrepancies and drawing in a third reviewer if required. We then entered information from data extraction into Review Manager (RevMan 2014). The data extraction form elicited information on study design, target population, reported outcomes, age, type of intervention and comparison, setting, inclusion and exclusion criteria, number eligible and recruited, risk of bias and relevant results.
Assessment of risk of bias in included studies
Two review authors independently assessed included studies.
We performed the 'Risk of bias' assessment for randomised controlled trials in this review using the criteria recommended by the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011a). The recommended approach for assessing risk of bias in studies included in a Cochrane Review is a two‐part tool addressing seven specific domains, namely sequence generation, allocation concealment (both related to selection bias), blinding of participants and providers (performance bias), blinding of outcome assessor (detection bias), incomplete outcome data (attrition bias), selective outcome reporting (reporting bias), and other risk of bias. For 'other risk of bias' we considered unit of analysis issues. The first part of the tool allows for a description of what was reported to have happened in the study. The second part of the tool involves assigning a judgement relating to the risk of bias for that entry in terms of low, high or unclear risk. To make these judgements, we adapted the criteria indicated by the Cochrane Handbook for Systematic Reviews of Interventions for the addiction field. Where information was missing from studies we categorised risk of bias as unclear. We did not contact study authors for further information about risk of bias. See Appendix 5 for details.
Measures of treatment effect
A standardised mean difference (SMD) was appropriate for this review, as trials typically reported outcomes as scale scores. Where they reported standard deviations or odds ratios, we converted these into SMDs, also including the corresponding 95% confidence intervals (CIs). We used Hedges'g as the SMD effect size measure in the meta‐analyses.
Unit of analysis issues
We included cluster‐randomised trials in the analyses along with individually randomised trials. We assessed specific bias related to unit of analysis in a number of aspects: recruitment bias, baseline imbalance, loss of clusters, incorrect analysis, and comparability with individually randomised trials. When trials did not account for clustering in their results, or when appropriately analysed cluster trials reported statistics that were not amenable to meta‐analysis and individual level descriptive results were available, we planned to adjust their sample sizes or standard errors using the methods described in Higgins 2011a, using an estimate of the intracluster correlation coefficient (ICC) derived from the trial. Where the ICC information was not available, we excluded cluster trials as part of a sensitivity analysis.
Dealing with missing data
Where data (study descriptive results and statistics) were missing or incomplete we contacted study authors for additional information. If authors did not respond we were not able to include the study or an outcome from the study in the meta‐analysis. We made no attempt to impute missing data from studies.
Assessment of heterogeneity
We assessed studies for clinical and methodological variability. We formally tested for statistical heterogeneity using the Chi2 test for statistical heterogeneity with a 10% level of significance as the cut‐off. We quantified the impact of any statistical heterogeneity using the I2 statistic.
Assessment of reporting biases
Publication bias is a significant threat to the validity of any systematic review. Such bias appears either when negative studies have lower likelihood of being published or if outcome data are selectively omitted from published reports because of their negative outcome. We constructed funnel plots for several of the primary outcomes where there was a reasonable number of trials.
Data synthesis
Where sufficient data were available across studies, we conducted meta‐analyses for overall effects using RevMan 5. As we expected intervention components, delivery, study samples and outcome measures to vary to a greater or lesser extent across studies, we used a random‐effects model, as is usual in studies of behavioural and preventive interventions. Where effect sizes or relevant results to allow calculation of effect sizes were not available for individual studies, we reported outcomes (for example significance levels) in a narrative way.
Subgroup analysis and investigation of heterogeneity
For both the outcomes reported at less than four months and those reported at four months or later, we analysed studies with assessment‐only controls separately from studies that had a control group that received an alternative intervention via subgroup analyses. We also undertook two further subgroup analyses for studies with longer‐term follow‐up, based on suggestions received from Mun 2015 on an earlier version of this review (). These were university or college settings versus other settings, and higher risk participants versus all or low‐risk participants. For all subgroup analyses, we report only the four self reported primary outcomes (quantity of alcohol consumed, frequency of alcohol consumption, binge drinking and alcohol problems).
We performed meta‐regression to examine the effect of intervention duration to assess the relationship between duration and effect size.
Sensitivity analysis
For studies where there was a high risk of selection bias, we carried out primary sensitivity analyses to examine the impact of inclusion or exclusion on the review findings. In secondary sensitivity analyses, we also removed studies that were at high risk for attrition and reporting bias from the meta‐analyses.
Summary of findings tables
We used the GRADE method to produce a 'Summary of findings' table for studies with longer‐term follow‐up (four months or more), as these are of more interest when considering the sustainability of intervention effects.
The Grading of Recommendation, Assessment, Development and Evaluation Working Group (GRADE) developed a system for grading the quality of evidence (GRADE 2004Guyatt 2008; Guyatt 2011) that takes into account issues not only related to internal validity but also to external validity, such as directness, consistency, imprecision of results and publication bias. The 'Summary of findings' tables present the main findings of a review in a transparent and simple tabular format. In particular, they provide key information concerning the quality of evidence, the magnitude of effect of the interventions examined, and the sum of available data on the main outcomes.
The GRADE system uses the following criteria for assigning grades of evidence.
High: We are very confident that the true effect lies close to that of the estimate of the effect.
Moderate: We are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different.
Low: Our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect.
Very low: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect.
We lowered the grade for the following reasons.
Serious (−1) or very serious (−2) limitation to study quality.
Important inconsistency (−1).
Some (−1) or major (−2) uncertainty about directness.
Imprecise or sparse data (−1).
High probability of reporting bias (−1)
Results
Description of studies
See: Characteristics of included studies and Characteristics of excluded studies.
Results of the search
The electronic search yielded 1751 bibliographic records (1430 through MEDLINE, EMBASE, PsycINFO; 311 through the CENTRAL). We identified a further 10 studies through handsearching systematic reviews and contacting authors. The process of de‐duplication resulted in 1314 unique bibliographic records. After screening titles and abstracts,we excluded 1210 records that were obviously irrelevant. We examined 104 full‐text reports, excluding 27. This left 77 published and unpublished study reports that met our criteria for inclusion.
Seven study reports described two comparisons, so we included 84 comparisons in this systematic review. Four study reports described two randomised subgroups (Fromme 2004 MANDATED; Fromme 2004 VOLUNTARY; Murphy 2010a; Murphy 2010b; Terlecki 2011 MANDATED; Terlecki 2011 VOLUNTARY; Terlecki 2010 MANDATED; Terlecki 2010 VOLUNTARY; Terlecki 2011 MANDATED; Terlecki 2011 VOLUNTARY), and three study reports only described analyses for two predefined subgroups (Daeppen 2011 HED; Daeppen 2011 non‐HED; Gaume 2011 HED; Gaume 2011 non‐HED; Walters 2009 MIF v FBO; Walters 2009 MIO v AO). Throughout this review we refer to each comparison as a 'trial', even if only one report reported two or more comparisons.
We present the study flow diagram of records identified from the search in Figure 1.
1.
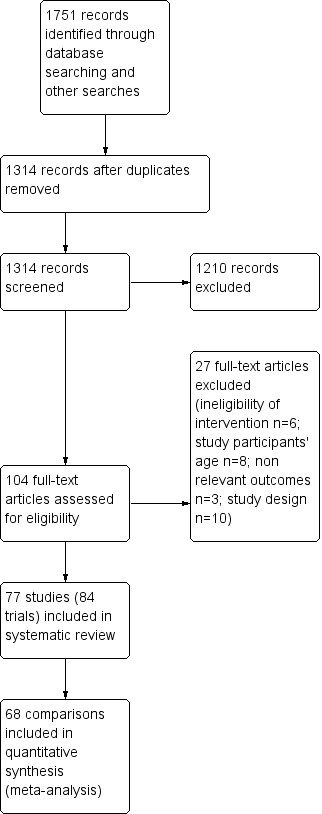
Study flow diagram.
We identified a further 12 trials for future classification and 1 ongoing study from the trial registry searches.
Included studies
See the Characteristics of included studies table. Total participants numbered 22,872. The unit of randomisation in 80 trials was the individual; four were cluster‐randomised (Larimer 2001; McCambridge 2004; McCambridge 2011; Wilke 2014). The total number of participants in cluster‐randomised trials was 1766, ranging from 159 in Larimer 2001 to 991 in Wilke 2014. McCambridge 2008 randomised by individual but adjusted for cluster effects associated with recruitment.
Country: Sixty‐six trials took place in the United States, four in the UK (Marsden 2006; McCambridge 2004; McCambridge 2008; McCambridge 2011), one in Australia (Bailey 2004), six in Switzerland (Daeppen 2011 HED; Daeppen 2011 non‐HED; Gaume 2011 HED; Gaume 2011 non‐HED; Gaume 2014; Gmel 2013), one in Spain (Goti 2010), one in France (Gomez 2013), two in Brazil (Christoff 2015; Segatto 2010), one in Thailand (Rongklavit 2013), one in Holland (Thush 2009), and one in Canada and the United States (Fleming 2010).
Participant characteristics: Study participants’ average age ranged from 15 in Bailey 2004 to 24 in Christoff 2015. Five studies did not report the age of participants (Cimini 2009; Marlatt 1998; Palmer 2004; White 2007; Wilke 2014). The proportion of males ranged from 22% in Feldstein 2007 to 90% in Stein 2006. Four trials enrolled only female students (Ceperich 2011; Clinton‐Sherrod 2011; LaBrie 2008; LaBrie 2009), and seven only recruited males (Daeppen 2011 HED; Daeppen 2011 non‐HED; Gaume 2011 HED; Gaume 2011 non‐HED; Gaume 2014; Gmel 2013; Larimer 2001).
Ethnicity of participants was mixed, with the majority (n = 52) of studies in largely (> 60%) white participants. In two studies participants were mainly (> 50%) Latino (D'Amico 2008; Aubrey 1998). In 13 other studies, fewer than 60% of participants were white (Bernstein 2010; Clair 2013; Juarez 2006; McCambridge 2004; McCambridge 2008; McCambridge 2011; Murphy 2012a; Naar‐King 2006; Schmiege 2009; Steele Seel 2010; Stein 2006; Stein 2011; Walton 2010), and in one of these, participants were 88% African American (Naar‐King 2006). Sixteen studies did not report ethnicity (Bailey 2004; Barnett 2010; Christoff 2015; D'Amico 2013; Daeppen 2011 HED; Daeppen 2011 non‐HED; Gaume 2011 HED; Gaume 2011 non‐HED; Gaume 2014; Gmel 2013; Gomez 2013; Goti 2010; Marlatt 1998; Rongklavit 2013; Thush 2009; Wilke 2014).
Most trials (70/84) reported that participants were assessed as being at higher risk for alcohol use or misuse because they were over a screening test threshold score, presented with evidence of alcohol misuse or had an associated risk factor (e.g. delinquency or other social or health conditions). We present details of risk characteristics, participants and setting for each study in the Characteristics of included studies. Fourteen studies did not restrict participants to those at higher risk (Carey 2006; D'Amico 2008; Daeppen 2011 non‐HED; Dermen 2011; Ewing 2009; Fromme 2004 VOLUNTARY; Gaume 2011 non‐HED; Gmel 2013; Larimer 2001; McCambridge 2011; Michael 2006; Naar‐King 2006; Wagener 2012; Wood 2010). A subgroup analysis assesses findings according to baseline risk status.
Setting: Settings for the trials varied; 51 of the 84 studies took place in higher education settings (university or colleges), mostly in the United States but also in one Brazilian and one Canadian study. Three UK trials and one Dutch trial took place at other post‐secondary educational institutions catering to pre‐university or vocational students (McCambridge 2004; McCambridge 2008; McCambridge 2011; Thush 2009). Fourteen trials took place in healthcare settings: hospital emergency departments (Barnett 2010; Bernstein 2010; Monti 1999; Monti 2007; Segatto 2010; Spirito 2004; Walton 2010), an outpatient substance abuse or psychiatry department (Goti 2010; Aubrey 1998), a community‐based healthcare clinic (D'Amico 2008; Nirenberg 2013), and an HIV centre (Murphy 2012a; Naar‐King 2006; Rongklavit 2013). Other settings were as follows: a youth centre in Australia (Bailey 2004); local companies (Doumas 2008), a vocational training centre (Steele Seel 2010), army recruitment setting (Daeppen 2011 HED; Daeppen 2011 non‐HED; Gaume 2011 HED; Gaume 2011 non‐HED; Gaume 2014; Gmel 2013), UK drug agencies (Marsden 2006), a youth court (D'Amico 2013), and juvenile detention centres (Clair 2013; Schmiege 2009; Stein 2006; Stein 2011). In the non‐college studies, the ethnicity balance was slightly different, with a lower proportion of whites.
Intervention: in 65 of the trials the intervention consisted only of an individual MI session. In one study participants attended both an individual session and a group session (Larimer 2001); in another study there were four group sessions and one individual session (Nirenberg 2013); in six studies there were two individual sessions (Clair 2013; Dermen 2011; Fleming 2010; Schaus 2009; White 2007; Wood 2010); and in four there were four sessions (Aubrey 1998; Murphy 2012a; Naar‐King 2006; Steele Seel 2010). Three studies used a single group session (LaBrie 2008; Michael 2006; Walters 2000), one used four group sessions (Bailey 2004), and another used six group sessions (D'Amico 2013). The duration of sessions varied: in 57 trials sessions took one hour or less; the shortest was a single 10 to 15 minute intervention (Wilke 2014), and the longest had five MI sessions over a 19‐hour period (Nirenberg 2013). One study reported a 'brief' intervention without specifying a duration (Barnett 2007), and six studies did not specify any information at all about session duration (Amaro 2009; Clinton‐Sherrod 2011; Marlatt 1998; Monti 1999; Steele Seel 2010; White 2007).
Comparisons: Forty‐nine trials compared MI versus an assessment‐only control group. Twenty‐five trials compared MI to alcohol counselling, education or information only (Amaro 2009; Barnett 2007; Bernstein 2010; Borsari 2005; Carey 2009; Carey 2013a; Ceperich 2011; Cimini 2009; D'Amico 2008; Ewing 2009; Faris 2005; Gomez 2013; LaBrie 2008; Marsden 2006; Martens 2013; McCambridge 2008; McCambridge 2011; Murphy 2010a; Rongklavit 2013; Schaus 2009; Schmiege 2009; Segatto 2010; Thush 2009; Walton 2010; Wilke 2014). Seven trials compared MI with feedback only (Barnett 2010; Christoff 2015; Doumas 2011; Monti 2007; Murphy 2004; Walters 2009 MIF v FBO; White 2007). Clair 2013, Stein 2006 and Stein 2011 compared MI with relaxation, while D'Amico 2013 compared MI with a six‐session Alcoholics Anonymous (AA) abstinence programme.
Outcomes: The alcohol‐related outcomes differed across the trials, as detailed in the Characteristics of included studies table. Many different outcome measures were used. The Rutgers Alcohol Problem Index (RAPI) was mostly used to measure alcohol‐related problems (White 1989); investigators measured quantity, frequency, BAC and binge drinking using various instruments, the most common of which were the Alcohol Use Disorders Test (AUDIT) (Saunders 1993), versions of the Daily Drinking Questionnaire (DDQ) (Collins1985), and the Timeline Followback (TLFB) technique (Sobell 1992).
The longest time points at which investigators measured the outcomes ranged from one month in Doumas 2008, Ewing 2009, Faris 2005, Goti 2010, Kulesza 2010, Martens 2013, Murphy 2010a, Murphy 2010b to four years postrandomisation in Marlatt 1998.
Excluded studies
We excluded many studies at screening because they clearly did not meet the inclusion criteria. A total of 27 studies required close scrutiny before we excluded them on the basis that they did not meet the inclusion criteria: ineligibility of intervention (N = 6, not MI), study participants’ age (N = 8, age > 25 years), outcomes (N = 3, no relevant outcomes), study design (N = 5, no control group; N = 6, reviews not trials; N = 6, non‐randomised study). We describe these excluded studies in the Characteristics of excluded studies table.
Risk of bias in included studies
We present the risk of bias assessment results for the included trials in Figure 2 and Figure 3.
2.
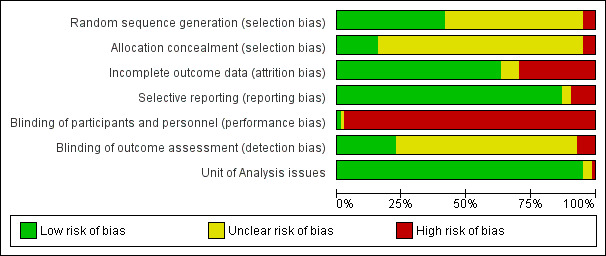
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
3.
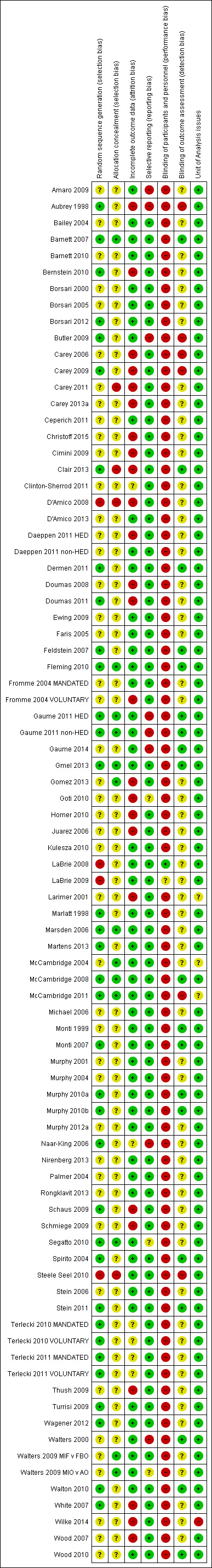
Risk of bias summary: review authors' judgements about risk of bias domains for each included study.
Allocation
Thirty‐five trials reported an adequate method of randomisation, and 13 described proper allocation concealment. In one study, we deemed that cluster randomisation had failed (McCambridge 2004).
Blinding
No study adequately blinded study participants and therapists. Fleming 2010 attempted to blind participants and therapists but only in the control condition, so this was a limited attempt with doubtful impact on performance bias. Investigators attempted blinding of outcome assessment in 21 studies (Barnett 2007; Clair 2013; Dermen 2011; Feldstein 2007; Fleming 2010; Daeppen 2011 HED; Daeppen 2011 non‐HED; Gaume 2011 HED; Gaume 2011 non‐HED; Gaume 2014; Gmel 2013; McCambridge 2008; Monti 1999; Monti 2007; Murphy 2010a; Murphy 2010b; Spirito 2004; Stein 2011; Walters 2000; Walton 2010; Wood 2010); in the other trials this was either not the case or not explicitly reported.
Incomplete outcome data
The attrition rate (at final follow‐up) in 54 trials was acceptable (20% or less), and for 25 trials it was not acceptable (> 20%). Five trials did not provide sufficiently clear information to adequately assess attrition (Naar‐King 2006; Terlecki 2010 MANDATED; Terlecki 2010 VOLUNTARY; Terlecki 2011 MANDATED; Terlecki 2011 VOLUNTARY). Five trials reported no losses to follow‐up (Bailey 2004; Clinton‐Sherrod 2011; Juarez 2006; Michael 2006; Steele Seel 2010).
Selective reporting
Most trials (73/84) were free of selective outcome reporting.
Other potential sources of bias
Three cluster‐randomised trials reported at least some efforts to adjust for the cluster level effect, but they provided insufficient details for inclusion of cluster‐adjusted estimates in the meta‐analysis (Larimer 2001; McCambridge 2004; McCambridge 2011). One cluster trial did not adjust for clustering and also did not report information about ICC (Wilke 2014). Therefore, we removed all four studies in the sensitivity analysis.
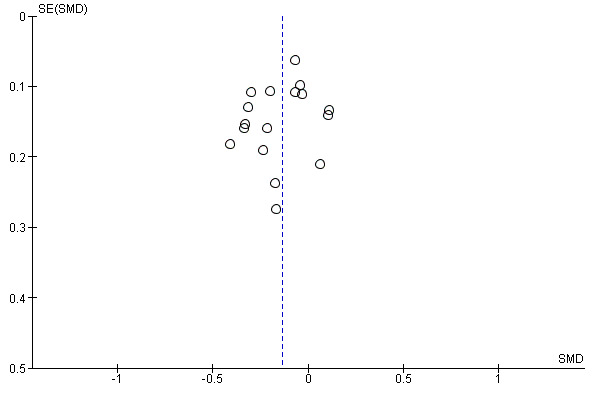
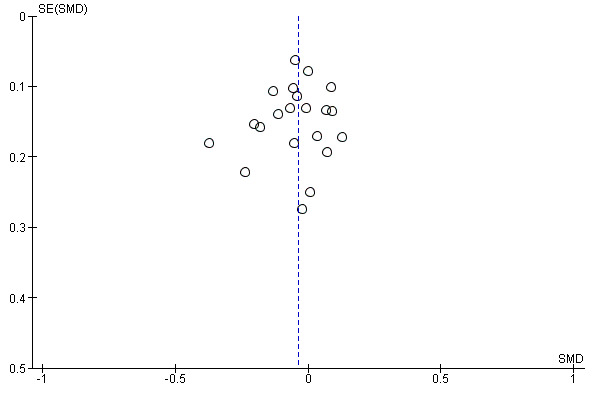
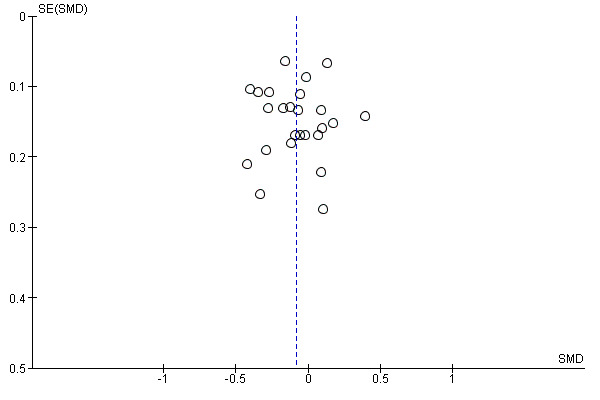
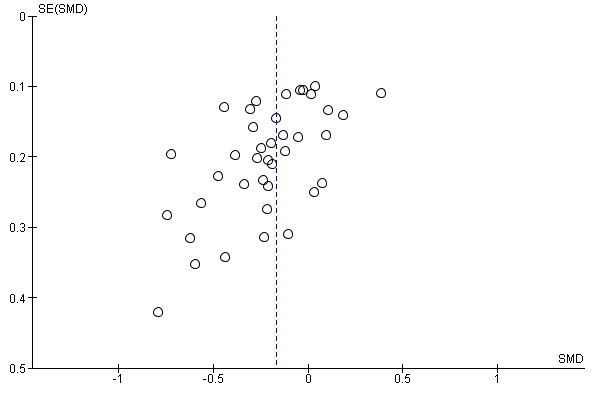
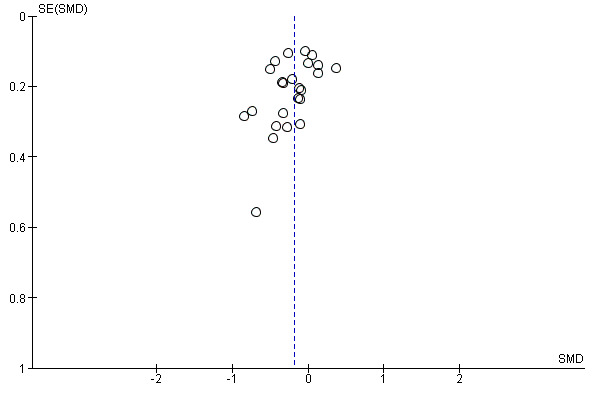
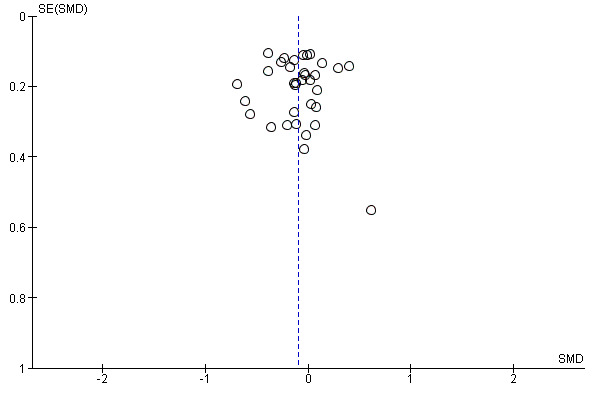
To assess possible publication bias, we constructed funnel plots for several of the primary outcomes where there were a reasonable number of trials, for both longer‐term and shorter‐term outcomes, and we visually inspected the plots. In all plots, a negative SMD indicates an effect in favour of the MI intervention. With longer‐term outcomes, there appeared to be reasonable symmetry and no notable outliers (Figure 4; Figure 5; Figure 6; Figure 7).
4.
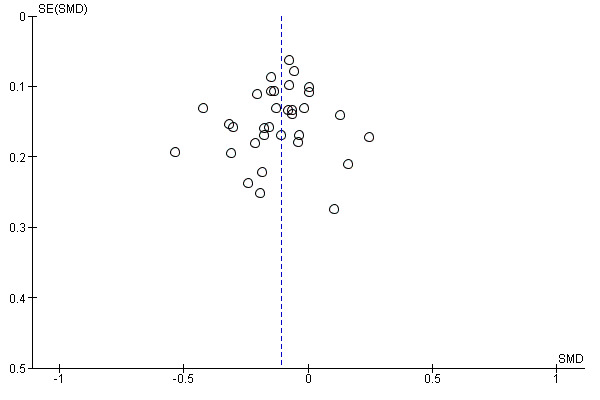
Funnel plot of comparison: 1 MI versus no MI (assessment only and alternative intervention) at ≥ 4 months follow‐up, outcome: 1.1 Quantity of alcohol consumed.
5.
Funnel plot of comparison: 1 MI versus no MI (assessment only and alternative intervention) at ≥ 4 months follow‐up, outcome: 1.2 Frequency of alcohol consumption.
6.
Funnel plot of comparison: 1 MI versus no MI (assessment only and alternative intervention) at ≥ 4 months follow‐up, outcome: 1.3 Binge drinking.
7.
Funnel plot of comparison: 1 MI versus no MI (assessment only and alternative intervention) at ≥ 4 months follow‐up, outcome: 1.4 Alcohol problems.
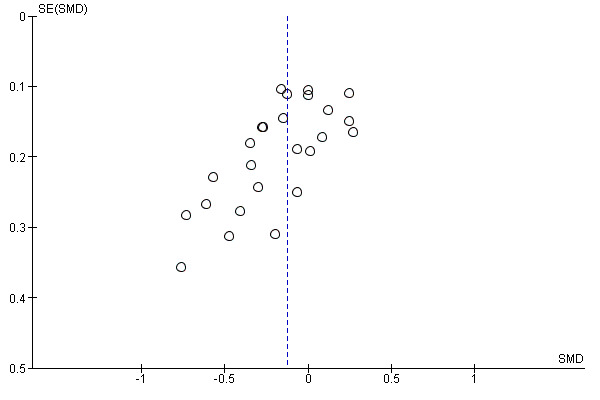
With shorter‐term outcomes (Figure 8; Figure 9; Figure 10; Figure 11), one plot had a notable outlier: Steele Seel 2010, a very small study (N = 14) with no significant effect (Figure 11). Two plots showed marked asymmetry (Figure 8; Figure 10). Several studies contributed notably to the asymmetry in Figure 8: Aubrey 1998, Bailey 2004, Butler 2009, D'Amico 2008, Juarez 2006, and Terlecki 2010 MANDATED, ; and Figure 10: Bailey 2004, Borsari 2000, Butler 2009, D'Amico 2008, Feldstein 2007, Murphy 2001, Murphy 2010a, and Murphy 2010b.
8.
Funnel plot of comparison: 2 MI versus no MI (assessment only and alternative intervention) at < 4 months follow‐up, outcome: 2.1 Quantity of alcohol consumed.
9.
Funnel plot of comparison: 2 MI versus no MI (assessment only and alternative intervention) at < 4 months follow‐up, outcome: 2.2 Frequency of alcohol consumption.
10.
Funnel plot of comparison: 2 MI versus no MI (assessment only and alternative intervention) at < 4 months follow‐up, outcome: 2.3 Binge drinking.
11.
Funnel plot of comparison: 2 MI versus no MI (assessment only and alternative intervention) at < 4 months follow‐up, outcome: 2.4 Alcohol problems.
This suggests that there may be a risk of publication bias in the shorter‐term outcome results, but it is also possible that other factors contributed, for example the poorer study quality in smaller studies, or the inclusion of studies with different sizes having participants with different risk profiles. It is interesting to note that asymmetry and the risk of publication bias was more of an issue for the shorter‐term follow‐up analyses.
Effects of interventions
We included 68 of the 84 included trials (81%) in the meta‐analysis. We contacted some authors who then provided additional information to enable their trials to be included in the meta‐analysis. The remaining 16 did not report results in a format that allowed inclusion in the meta‐analysis, and authors did not respond to requests for further information in time for inclusion in this review (Amaro 2009; Cimini 2009; Clair 2013; Clinton‐Sherrod 2011; Ewing 2009; Goti 2010; Horner 2010; LaBrie 2008; LaBrie 2009; Murphy 2004; Murphy 2012a; Naar‐King 2006; Palmer 2004; Thush 2009; Wood 2007; Wood 2010).
We summarise eight alcohol use and misuse outcomes below, categorised according to two follow‐up periods: four or more months (see Table 1), and less than four months (see Table 2). We summarise the quality of the evidence in both these tables according to GRADE criteria. Where trials reported several follow‐up points, we took the closest ones to 12‐month follow‐up (for longer‐term outcomes) or 3‐month follow‐up (for shorter‐term outcomes). For example, in a study with one‐year and two‐year outcomes, we used the one‐year results in the analysis on longer‐term outcomes.
The eight outcomes were as follows.
Quantity of alcohol consumed.
Frequency of alcohol consumed.
Binge drinking.
Alcohol problems.
Average blood alcohol concentration (BAC), calculated using a formula based on consumption, sex and weight.
Peak BAC, calculated using a formula based on consumption, sex and weight.
Drink‐driving.
Risky behaviour.
For the first four key outcome measures (drinking quantity, drinking frequency, binge drinking, and alcohol related problems) there were sufficient studies to conduct subgroup analyses.
During primary sensitivity analyses, we selectively removed all studies that were at high risk for selection bias (Carey 2011; D'Amico 2008; Steele Seel 2010). Carey 2013a presented results as change scores, and the author did not send means and standard deviations at follow‐up time points in time for inclusion in this review. Technically, direct comparison and pooling of final value and change scores is not straightforward when using standardised mean differences, since the difference in standard deviation reflects not differences in measurement scale, but differences in the reliability of the measurements. Therefore we also selectively removed Carey 2013a from the analysis as part of the sensitivity analysis. We also removed four cluster trialsduring the sensitivity analysis as there is a risk of inflated effects if clustering is not adequately accounted for in the analysis (Larimer 2001; McCambridge 2004; McCambridge 2011; Wilke 2014).
In secondary sensitivity analyses, we also removed studies that were high risk for attrition and reporting bias from the meta‐analyses (see Figure 3).
1. MI versus no MI (assessment only or alternative intervention) at four months or more of follow‐up
1.1 Quantity of alcohol consumed
See: Analysis 1.1.
1.1. Analysis.
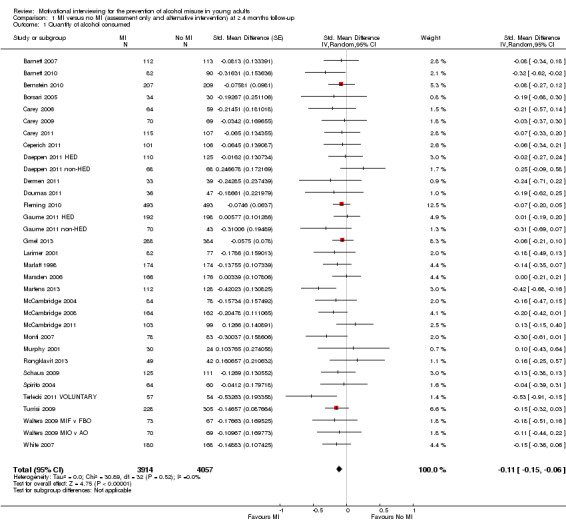
Comparison 1 MI versus no MI (assessment only and alternative intervention) at ≥ 4 months follow‐up, Outcome 1 Quantity of alcohol consumed.
Thirty‐three studies with 7971 participants reported measures of alcohol consumption at follow‐up periods of four months or more and were included in a random‐effects model meta‐analysis. There was an effect in favour of MI (SMD −0.11, 95% CI −0.15 to −0.06) representing a decrease of 1.2 drinks consumed each week (95% CI 0.7 to 1.6), from an average of 13.7 drinks per week to 12.5 drinks per week, based on a standard deviation (SD) of 10.8 (Martens 2013). Heterogeneity was not a problem (I2 = 0%, P = 0.52).
In the primary sensitivity analysis, the pooled effect estimate was unchanged. Similarly, there were no substantive changes to the pooled effect estimate in the more rigorous secondary sensitivity analysis.
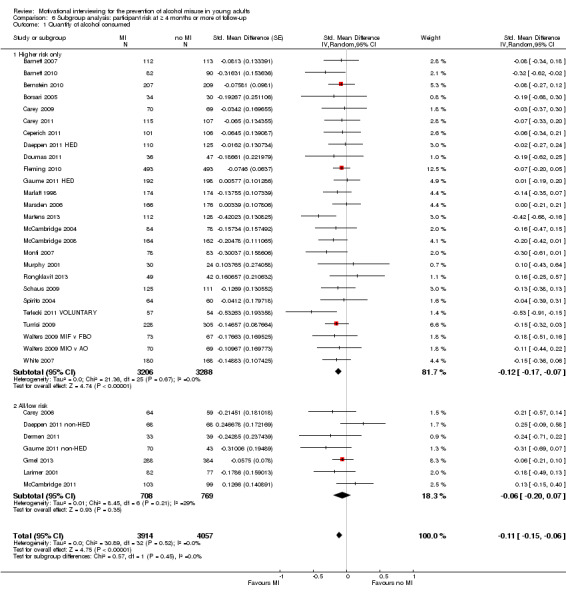
1.2 Frequency of alcohol consumption
See: Analysis 1.2.
1.2. Analysis.

Comparison 1 MI versus no MI (assessment only and alternative intervention) at ≥ 4 months follow‐up, Outcome 2 Frequency of alcohol consumption.
Seventeen studies with 4377 participants reported on frequency of alcohol consumption at follow‐up periods of four or more months and were included in a random‐effects model meta‐analysis. There was a difference in favour of MI (SMD −0.14, 95% CI −0.21 to −0.07) representing a decrease of 0.22 drinking days per week (95% CI 0.11 to 0.32), from an average of 2.74 drinking days per week to 2.52 drinking days per week, based on Martens 2013. Heterogeneity was not a problem (I2 = 24%, P = 0.18).
In the primary sensitivity analysis, there were no substantive changes to the pooled effect. There were no substantive changes to the pooled effect estimate in the more rigorous secondary sensitivity analysis, with one study removed.
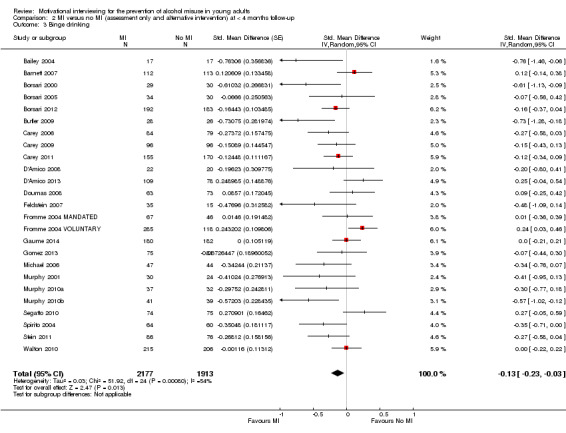
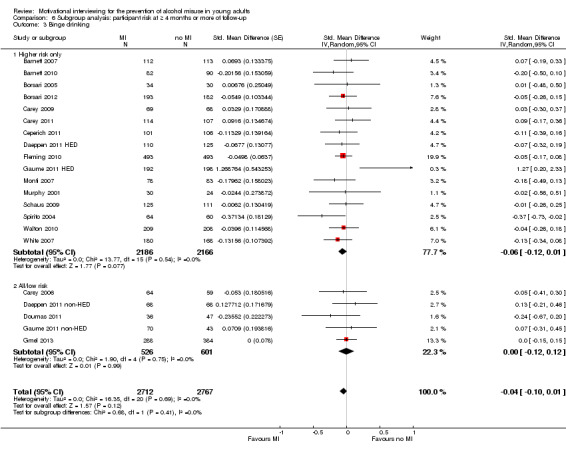
1.3 Binge drinking
See: Analysis 1.3.
1.3. Analysis.
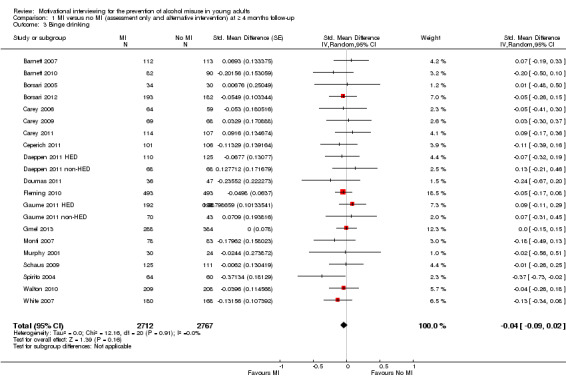
Comparison 1 MI versus no MI (assessment only and alternative intervention) at ≥ 4 months follow‐up, Outcome 3 Binge drinking.
Twenty‐one studies with 5479 participants reported on the frequency of alcohol consumption at follow‐up periods of four months and more and were included in a random‐effects model meta‐analysis. There was no clear effect of the MI intervention on binge drinking (SMD −0.04, 95% CI −0.09 to 0.02). A test for heterogeneity showed no significant variability between studies (I2 = 0%, P = 0.91).
In both the primary and secondary sensitivity analyses, there were no substantive changes to the pooled effect estimates.
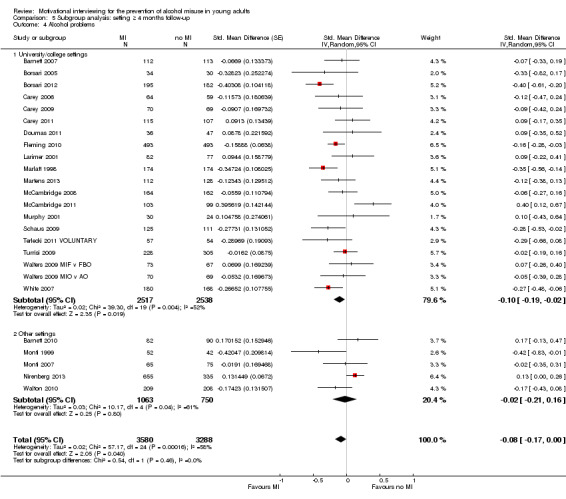
1.4 Alcohol problems
See: Analysis 1.4.
1.4. Analysis.
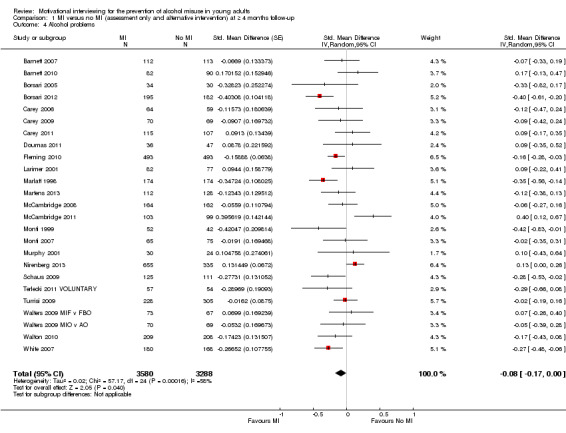
Comparison 1 MI versus no MI (assessment only and alternative intervention) at ≥ 4 months follow‐up, Outcome 4 Alcohol problems.
Twenty‐five studies with 6868 participants reported on alcohol problems at follow‐up periods of four or more months and were included in a random‐effects model meta‐analysis. There was a borderline effect (SMD −0.08, 95% CI −0.17 to 0.00), representing a decrease of 0.73 on the alcohol problems scale score (95% CI 0.00 to 1.56), from an average of 8.91 to 8.18, based on Martens 2013. A test for heterogeneity showed significant variability across studies (I2 = 58%, P = 0.0002).
In the primary sensitivity analysis, the strength of the effect increased (SMD −0.12, 95% CI −0.20 to −0.04), but we did not find any other change in the secondary sensitivity analysis.
1.5 Average BAC
See: Analysis 1.5.
1.5. Analysis.
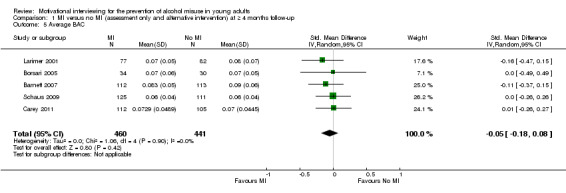
Comparison 1 MI versus no MI (assessment only and alternative intervention) at ≥ 4 months follow‐up, Outcome 5 Average BAC.
Five studies with 901 participants reported average BAC at four or more months follow‐up and were included in a random‐effects model meta‐analysis. There was no difference between groups (SMD −0.05, 95% CI −0.18 to 0.08). A test for heterogeneity showed no variability between studies (I2 = 0%, P = 0.90).
In both the primary and secondary sensitivity analyses there were no substantive changes to the pooled effect estimates.
1.6 Peak BAC
See: Analysis 1.6.
1.6. Analysis.
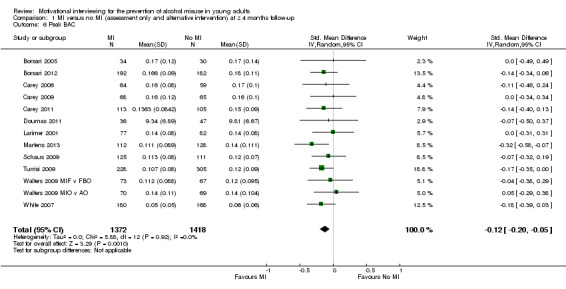
Comparison 1 MI versus no MI (assessment only and alternative intervention) at ≥ 4 months follow‐up, Outcome 6 Peak BAC.
Thirteen studies with 2790 participants reported peak BAC at four or more months follow‐up and were included in a random‐effects model meta‐analysis. There was a difference between groups (SMD −0.12, 95% CI −0.20 to −0.05), representing a decrease of 0.013% for peak BAC (95% CI 0.006 to 0.025), from an average of 0.144% to 0.131%, based on Martens 2013. A test for heterogeneity showed no significant variability across studies (I2 = 0%, P = 0.92).
In both the primary and secondary sensitivity analyses, there were no substantive changes to the pooled effect estimates.
1.7 Drink‐driving
See: Analysis 1.7
1.7. Analysis.
Comparison 1 MI versus no MI (assessment only and alternative intervention) at ≥ 4 months follow‐up, Outcome 7 Drink‐driving.
Four studies with 1205 participants reported on drink‐driving at four or more months follow‐up and were included in a random‐effects model meta‐analysis. There was no effect for MI (SMD −0.13, 95% CI −0.36 to 0.10). A test for heterogeneity showed significant variability across studies (I2 = 61%, P = 0.05).
No primary or secondary sensitivity analyses were undertaken, as no studies were eligible for removal.
1.8 Risky behaviour
This outcome combined various activities, from unspecified risky behaviour to alcohol‐related injury and unprotected sex. See: Analysis 1.8.
1.8. Analysis.
Comparison 1 MI versus no MI (assessment only and alternative intervention) at ≥ 4 months follow‐up, Outcome 8 Risky behaviour.
Seven studies with 1579 participants reported on risky behaviour at four or more months follow‐up. All studies were included in the meta‐analysis, which showed no effect for MI (SMD −0.15, 95% CI −0.31 to 0.01). A test for heterogeneity showed a significant effect (I2 = 47%, P = 0.08).
In both the primary and secondary sensitivity analyses, there were no substantive changes to the pooled effect estimates.
2. MI versus no MI (assessment only or alternative intervention) at less than four months of follow‐up
2.1 Quantity of alcohol consumed
See: Analysis 2.1.
2.1. Analysis.
Comparison 2 MI versus no MI (assessment only and alternative intervention) at < 4 months follow‐up, Outcome 1 Quantity of alcohol consumed.
Thirty‐nine studies (5600 participants) reported on quantity of drinking at less than four month follow‐up and were included in a random‐effects model meta‐analysis. There was an effect in favour of MI (SMD −0.17, 95% CI −0.25 to −0.09). Heterogeneity (I2 = 52%) was statistically significant at P<0.0001.
In both the primary and secondary sensitivity analyses, there were no substantive changes to the pooled effect estimates.
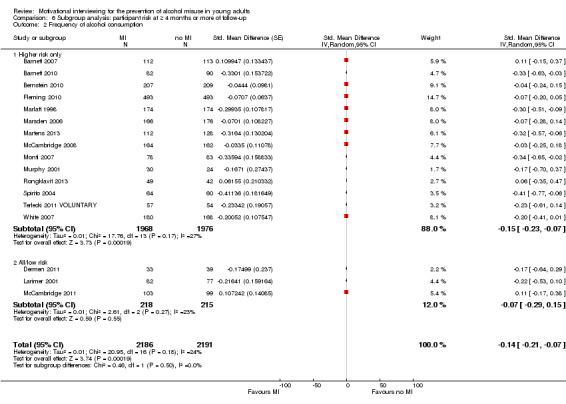
2.2 Frequency of alcohol consumption
See: Analysis 2.2.
2.2. Analysis.
Comparison 2 MI versus no MI (assessment only and alternative intervention) at < 4 months follow‐up, Outcome 2 Frequency of alcohol consumption.
Twenty‐four studies with 3296 participants reported on frequency of alcohol consumption at follow‐up periods of less than four months and were included in a random‐effects model meta‐analysis. There was a difference in favour of MI (SMD −0.18, 95% CI −0.29 to −0.07). Heterogeneity was problematic (I2 = 55%, P = 0.0006).
In both the primary and secondary sensitivity analyses, there were no substantive changes to the pooled effect estimates.
2.3 Binge drinking
See: Analysis 2.3.
2.3. Analysis.
Comparison 2 MI versus no MI (assessment only and alternative intervention) at < 4 months follow‐up, Outcome 3 Binge drinking.
Twenty‐five studies with 4090 participants reported a binge drinking measure at follow‐up periods of less than four months and were included in a random‐effects model meta‐analysis. There was a difference in favour of MI (SMD −0.13, 95% CI −0.23 to −0.03). A test for heterogeneity showed a significant variability between studies (I2 = 54%, P = 0.0008).
In both the primary and secondary sensitivity analyses, there were no substantive changes to the pooled effect estimates.
2.4 Alcohol problems
See: Analysis 2.4.
2.4. Analysis.
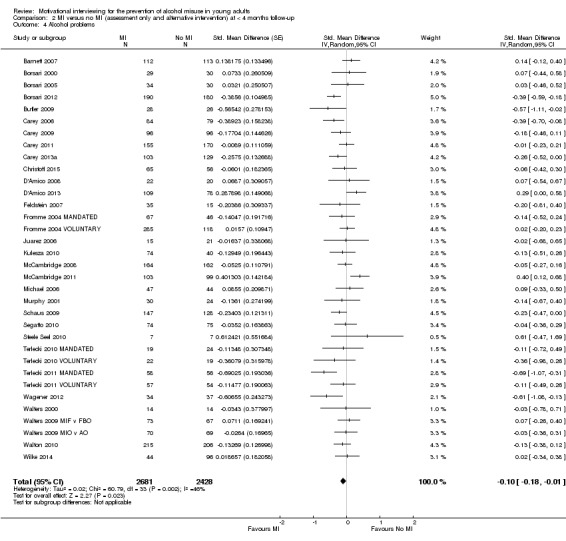
Comparison 2 MI versus no MI (assessment only and alternative intervention) at < 4 months follow‐up, Outcome 4 Alcohol problems.
Thirty‐four studies with 5109 participants reported a measure of alcohol problems at follow‐up periods of less than four months and were included in a random‐effects model meta‐analysis. There was a marginal effect of MI over comparison or controls (SMD −0.10, 95% CI −0.18 to −0.01). A test for heterogeneity showed significant variability across studies (I2 = 46%, P = 0.002).
In both the primary and secondary sensitivity analyses, there were no substantive changes to the pooled effect estimates.
2.5 Average BAC
See: Analysis 2.5.
2.5. Analysis.

Comparison 2 MI versus no MI (assessment only and alternative intervention) at < 4 months follow‐up, Outcome 5 Average BAC.
Six studies with 1096 participants were suitable for inclusion in a random‐effects model meta‐analysis. There was no effect of the intervention (SMD −0.14, 95% CI −0.30 to 0.01). Heterogeneity was not a problem (I2 = 34%, P = 0.18).
In both the primary and secondary sensitivity analyses, there were no substantive changes to the pooled effect estimates.
2.6 Peak BAC
See: Analysis 2.6.
2.6. Analysis.
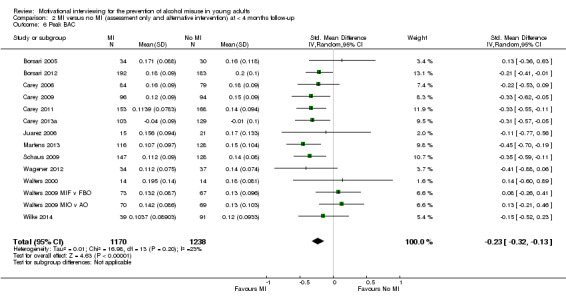
Comparison 2 MI versus no MI (assessment only and alternative intervention) at < 4 months follow‐up, Outcome 6 Peak BAC.
Fourteen studies with 2408 participants reported on peak BAC at follow‐up periods of up to three months and were included in a random‐effects model meta‐analysis. There was an effect in favour of the intervention (SMD −0.23, 95% CI −0.32 to −0.13). A test for heterogeneity found no variability across pooled studies (I2 = 23%, P = 0.20).
In both the primary and secondary sensitivity analyses, there were no substantive changes to the pooled effect estimates.
2.7 Drink‐driving
See: Analysis 2.7.
2.7. Analysis.
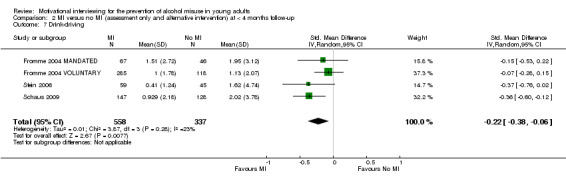
Comparison 2 MI versus no MI (assessment only and alternative intervention) at < 4 months follow‐up, Outcome 7 Drink‐driving.
Four studies with 895 participants were suitable for inclusion in a random‐effects model meta‐analysis. There was an effect of the intervention (SMD −0.22, 95% CI −0.38 to −0.06). Heterogeneity was not a problem (I2 = 23%, P = 0.28).
No primary sensitivity analysis was undertaken as there were no eligible studies. Removal of two studies in the secondary sensitivity analysis shifted the effect estimate (SMD −0.26, 95% CI −0.53 to 0.02).
2.8 Risky behaviour
See: Analysis 2.8.
2.8. Analysis.
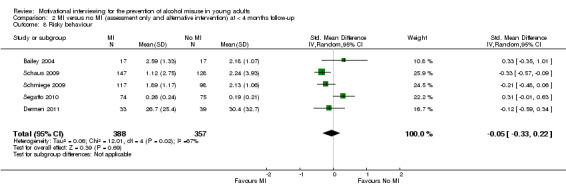
Comparison 2 MI versus no MI (assessment only and alternative intervention) at < 4 months follow‐up, Outcome 8 Risky behaviour.
Five studies with 745 participants reported on risky behaviour at less than four months follow‐up and were included in a random‐effects model meta‐analysis. There was no effect of MI (SMD −0.05, 95% CI −0.33 to 0.22). A test for heterogeneity showed significant heterogeneity (I2 = 67%, P = 0.02).
In both the primary and secondary sensitivity analyses, there were no substantive changes to the pooled effect estimates.
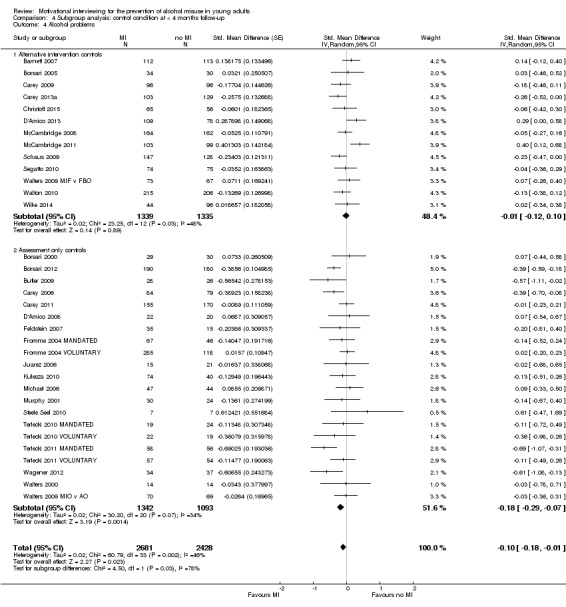
3. Subgroup analysis: control condition at four months or more of follow‐up
See Analysis 3.1; Analysis 3.2; Analysis 3.3; Analysis 3.4.
3.1. Analysis.
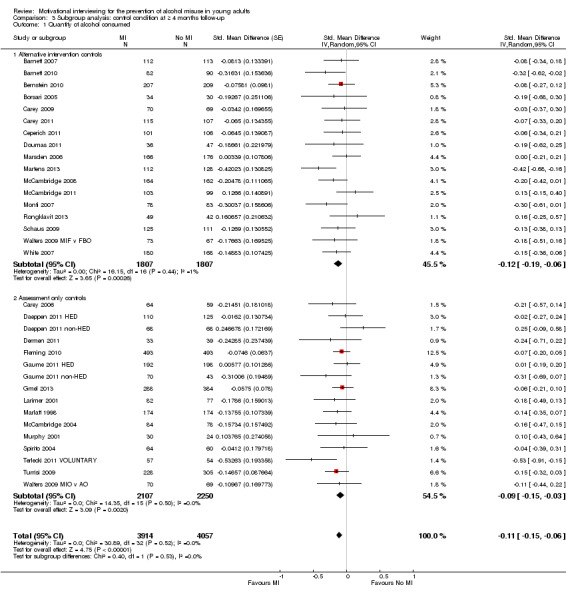
Comparison 3 Subgroup analysis: control condition at ≥ 4 months follow‐up, Outcome 1 Quantity of alcohol consumed.
3.2. Analysis.
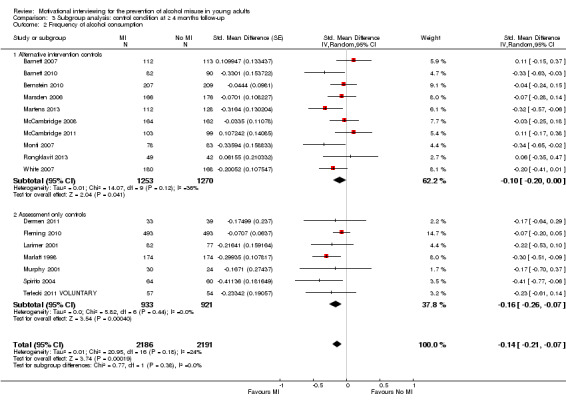
Comparison 3 Subgroup analysis: control condition at ≥ 4 months follow‐up, Outcome 2 Frequency of alcohol consumption.
3.3. Analysis.
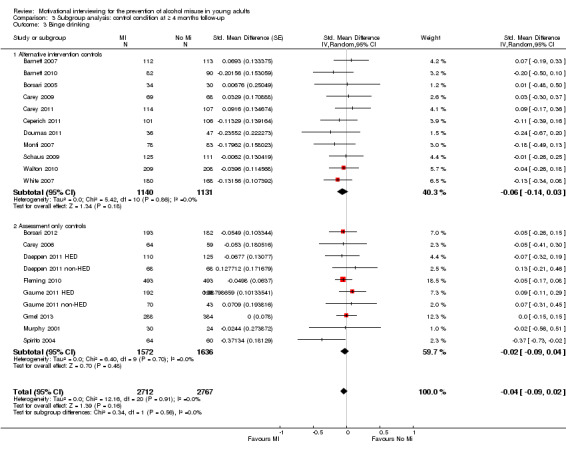
Comparison 3 Subgroup analysis: control condition at ≥ 4 months follow‐up, Outcome 3 Binge drinking.
3.4. Analysis.
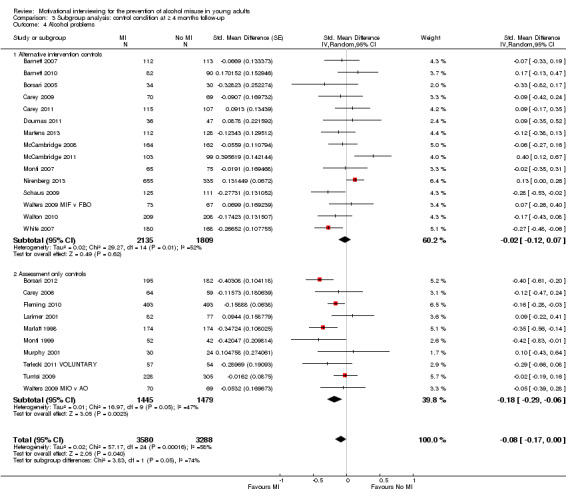
Comparison 3 Subgroup analysis: control condition at ≥ 4 months follow‐up, Outcome 4 Alcohol problems.
We analysed studies with assessment‐only controls separately from studies that had a control group that received an alternative intervention. There was no clearly discernible subgroup effect (using a P value of 0.05 to establish significance) for any of the outcomes considered (Table 3). Alcohol problems showed a borderline effect (P = 0.05), but given the number of tests and increased risk of chance findings, we have been cautious in interpretation.
1. Subgroup analysis, MI versus active control versus assessment only.
| Follow‐up | Outcome | SMD (95% CI), Active controls | SMD (95% CI), assessment only | Test for group differences |
| ≥ 4 months | Quantity of drinking | −0.12 (−0.19 to −0.06) | −0.11 (−0.15 to −0.03) | Chi2 = 0.40, df = 1 (P = 0.53) |
| Frequency of drinking | −0.10 (−0.20 to 0.00) | −0.14 (−0.21 to −0.07) | Chi2 = 0.77, df = 1 (P = 0.38) | |
| Binge drinking | −0.06 (−0.14 to 0.03) | −0.04 (−0.09 to 0.02) | Chi2 = 0.34, df = 1 (P = 0.56) | |
| Alcohol problems | −0.02 (−0.12 to 0.07) | −0.18 (−0.29 to −0.06) | Chi2 = 3.83, df = 1 (P = 0.05) | |
| < 4 months | Quantity of drinking | −0.11 (−0.21 to −0.02) | −0.23 (−0.36 to −0.10) | Chi2 = 1.62, df = 1 (P = 0.20) |
| Frequency of drinking | 0.00 (−0.15 to 0.14) | −0.33 (−0.44 to −0.23) | Chi2 = 12.73, df = 1 (P = 0.0004) | |
| Binge drinking | 0.00 (−0.13 to 0.13) | −0.21 (−0.35 to −0.08) | Chi2 = 4.62, df = 1 (P = 0.03) | |
| Alcohol problems | −0.01 (−0.12 to 0.10) | −0.18 (−0.29 to −0.07) | Chi2 = 4.50, df = 1 (P = 0.03) |
CI: confidence interval; df: degrees of freedom; SMD: standardised mean difference.
4. Subgroup analysis: control condition at less than four months of follow‐up
See Analysis 4.1; Analysis 4.2; Analysis 4.3; Analysis 4.4.
4.1. Analysis.
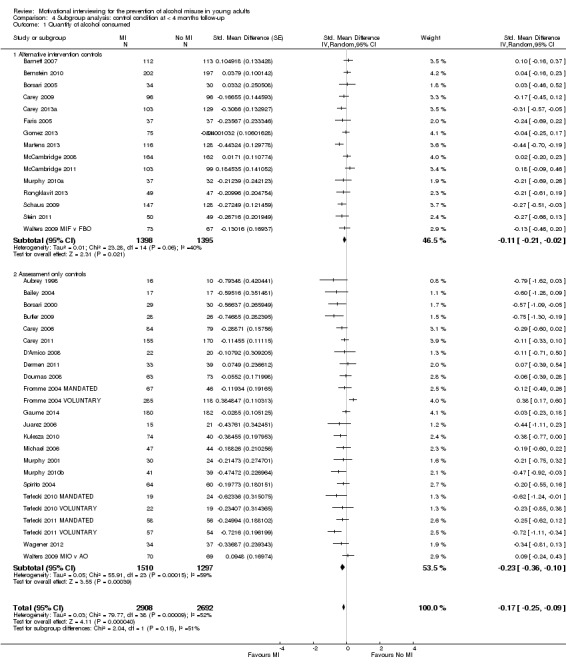
Comparison 4 Subgroup analysis: control condition at < 4 months follow‐up, Outcome 1 Quantity of alcohol consumed.
4.2. Analysis.
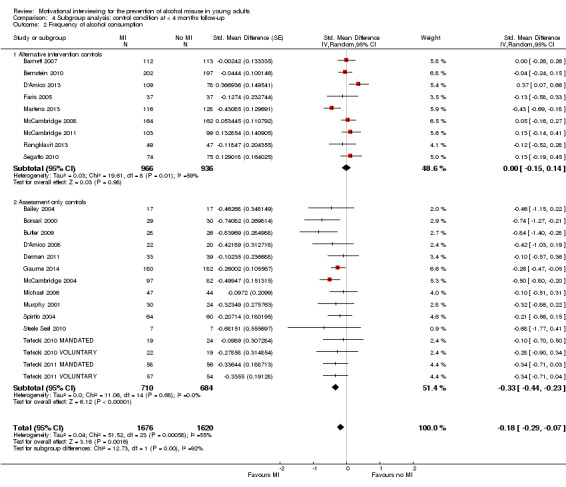
Comparison 4 Subgroup analysis: control condition at < 4 months follow‐up, Outcome 2 Frequency of alcohol consumption.
4.3. Analysis.
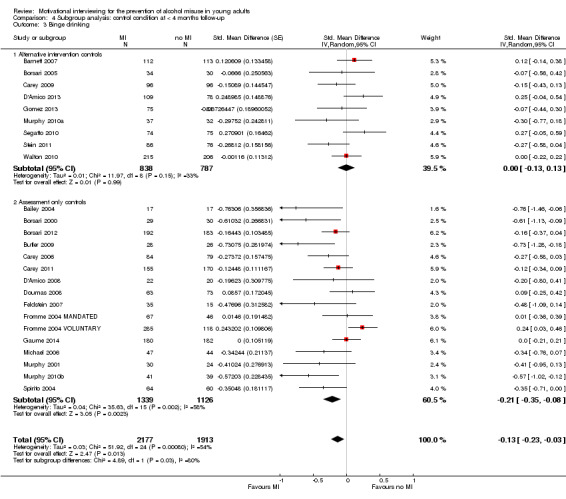
Comparison 4 Subgroup analysis: control condition at < 4 months follow‐up, Outcome 3 Binge drinking.
4.4. Analysis.
Comparison 4 Subgroup analysis: control condition at < 4 months follow‐up, Outcome 4 Alcohol problems.
In this subgroup analysis, there was a clear effect for three of the four outcomes. Pooled effects were clearly larger in the assessment only subgroup compared with the alternative intervention subgroup except for quantity of drinking (analysis 4.1 in Table 3).
5. Subgroup analysis: setting at four months or more of follow‐up
See Analysis 5.1; Analysis 5.2; Analysis 5.3; Analysis 5.4.
5.1. Analysis.
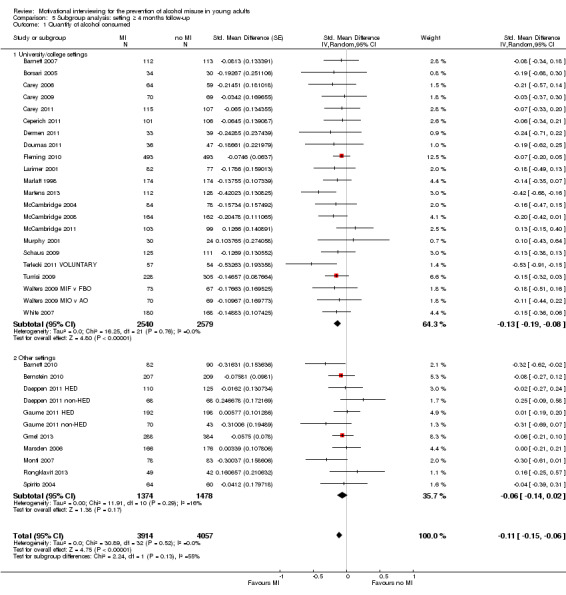
Comparison 5 Subgroup analysis: setting ≥ 4 months follow‐up, Outcome 1 Quantity of alcohol consumed.
5.2. Analysis.
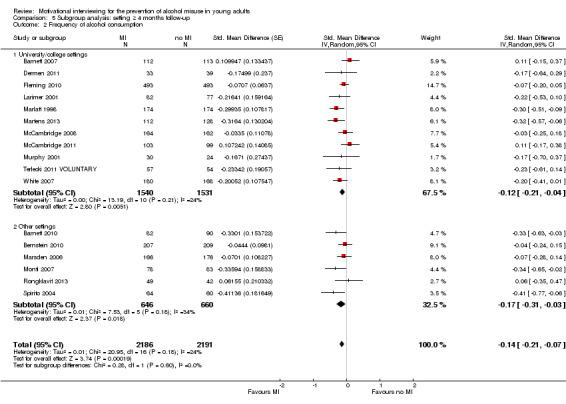
Comparison 5 Subgroup analysis: setting ≥ 4 months follow‐up, Outcome 2 Frequency of alcohol consumption.
5.3. Analysis.
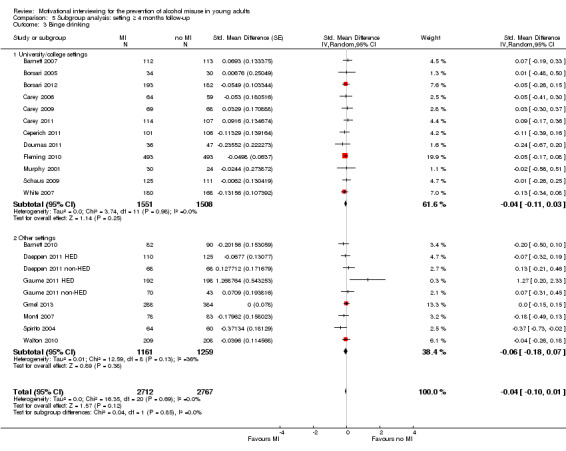
Comparison 5 Subgroup analysis: setting ≥ 4 months follow‐up, Outcome 3 Binge drinking.
5.4. Analysis.
Comparison 5 Subgroup analysis: setting ≥ 4 months follow‐up, Outcome 4 Alcohol problems.
We ran a separate subgroup analysis on studies with participants from university or college settings and studies that had participants from other settings. There was no discernible subgroup effect for any of the outcomes considered (Table 4).
2. Subgroup analysis, university/college settings versus other settings.
| Follow‐up | Outcome | SMD (95% CI), university/college | SMD (95% CI), other settings | Test for group differences |
| ≥ 4 months | Quantity of drinking | −0.13 (−0.19 to −0.08) | −0.06 (−0.14 to 0.02) | Chi2 = 2.24, df = 1 (P = 0.13) |
| Frequency of drinking | −0.12 (−0.21 to −0.04) | −0.17 (−0.31 to −0.03) | Chi2 = 0.28, df = 1 (P = 0.60) | |
| Binge drinking | −0.04 (−0.11 to 0.03) | −0.06 (−0.18 to 0.07) | Chi2 = 0.04, df = 1 (P = 0.85) | |
| Alcohol problems | −0.10 (−0.19 to −0.02) | −0.02 (−0.21 to 0.16) | Chi2 = 0.54, df = 1 (P = 0.46) |
CI: confidence interval; df: degrees of freedom; SMD: standardised mean difference.
6. Subgroup analysis: participant risk at four months or more of follow‐up
See Analysis 6.1; Analysis 6.2; Analysis 6.3; Analysis 6.4.
6.1. Analysis.
Comparison 6 Subgroup analysis: participant risk at ≥ 4 months or more of follow‐up, Outcome 1 Quantity of alcohol consumed.
6.2. Analysis.
Comparison 6 Subgroup analysis: participant risk at ≥ 4 months or more of follow‐up, Outcome 2 Frequency of alcohol consumption.
6.3. Analysis.
Comparison 6 Subgroup analysis: participant risk at ≥ 4 months or more of follow‐up, Outcome 3 Binge drinking.
6.4. Analysis.
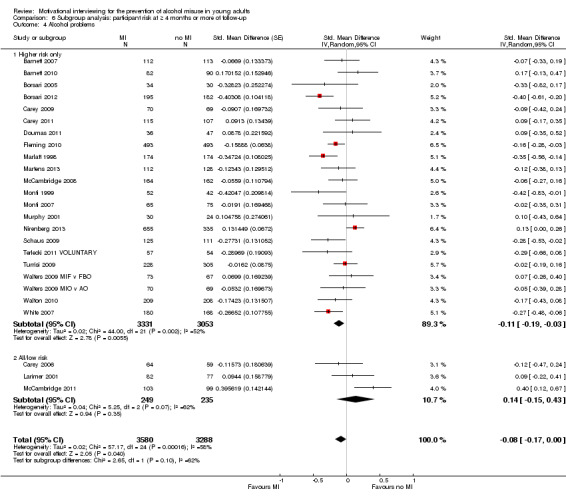
Comparison 6 Subgroup analysis: participant risk at ≥ 4 months or more of follow‐up, Outcome 4 Alcohol problems.
We ran a subgroup analysis on studies with participants at higher baseline risk of alcohol use or misuse versus studies that had participants who were not screened for risk or were assessed to be at lower risk. There was no discernible subgroup effect for any of the outcomes considered (Table 5).
3. Subgroup analysis, higher risk participants versus all or low risk participants.
| Follow‐up | Outcome | SMD (95% CI), high risk | SMD (95% CI), all/low risk | Test for group differences |
| ≥ 4 months | Quantity of drinking | −0.12 (−0.17 to −0.07) | −0.06 (−0.20 to 0.07) | Chi2 = 0.01, df = 1 (P = 0.94) |
| Frequency of drinking | −0.15 (−0.23 to −0.07) | −0.07 (−0.29 to 0.15) | Chi2 = 0.23, df = 1 (P = 0.63) | |
| Binge drinking | −0.06 (−0.12 to 0.01) | 0.00 (−0.12 to 0.12) | Chi2 = 0.68, df = 1 (P = 0.41) | |
| Alcohol problems | −0.11 (−0.19 to −0.03) | 0.14 (−0.15 to 0.43) | Chi2 = 0.86, df = 1 (P = 0.35) |
CI: confidence interval; df: degrees of freedom; SMD: standardised mean difference.
Meta‐regression
In mixed‐effects meta‐regression, we examined the relationship between MI duration (minutes) and SMD effect size (Table 6). For three of the outcomes we examined in the meta‐regression (quantity of drinking, frequency of drinking, binge drinking, all at 4 or more months) there was no significant relationship between MI duration and SMD (Hedges'g) effect size. Briefer MI interventions had, on average, similar effects as longer MI interventions. See Figure 12 for an illustrative plot showing the relationship between MI duration and SMD effect size, for quantity of alcohol consumed at four or more months follow‐up. The line represents the slope calculated in the meta‐regression, and the circles are individual studies.
4. Mixed effects meta‐regression of MI durations and study effect size.
| Follow‐up | Outcome | Point estimate | Standard error | Lower limit | Upper limit | Z value | P value |
| ≥ 4 months | Quantity of drinking | 0.00039 | 0.00079 | −0.00116 | 0.00194 | 0.49367 | 0.62154 |
| Frequency of drinking | 0.00107 | 0.00089 | −0.00068 | 0.00282 | 1.19916 | 0.23047 | |
| Binge drinking | −0.00084 | 0.00152 | −0.00382 | 0.00215 | −0.5494 | 0.58273 | |
| Alcohol problems | 0.00023 | 0.00007 | 0.0001 | 0.00036 | 3.51877 | 0.00043 | |
| < 4 months | Quantity of drinking | 0.00146 | 0.00071 | 0.00286 | 0.00313 | 2.04661 | 0.04070 |
| Frequency of drinking | 0.00169 | 0.00051 | 0.00069 | 0.0027 | 3.30565 | 0.00095 | |
| Binge drinking | 0.00132 | 0.00053 | 0.00027 | 0.00237 | 2.46732 | 0.01361 | |
| Alcohol problems | 0.00159 | 0.00054 | 0.00053 | 0.00265 | 2.93722 | 0.00331 |
12.
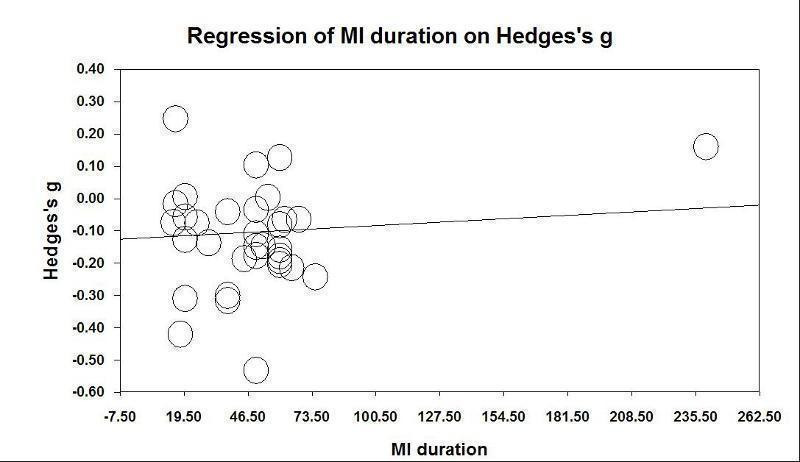
For alcohol problems at four months or more, there was a significant relationship, with the slope indicating a very small tendency for shorter duration MI to have a larger effect size. This slope direction was also apparent for all outcomes measured at less than four months, indicating a slight tendency for shorter duration MI to have a larger effect size (Table 6). To illustrate, a slope of 0.0017 indicates that for every 10 minute increase in MI duration, the standardised effect size (Hedges'g) would, on average, reduce by 0.017 units.
Studies not included in the meta‐analysis
Of the 16 studies that were not included in the meta‐analysis, 9 reported no statistically significant effects of the intervention, 4 reported mixed effects (some significant outcomes or some significant time points), and 3 reported overall positive effects. See Table 7. We think it is unlikely that these omitted studies would change the results of the meta‐analysis.
5. Studies not included in meta‐analysis.
| Amaro 2009 | Growth curve analyses showed that, relative to services as usual, the intervention was more efficacious in reducing past‐90‐day weekday alcohol consumption and the number of alcohol‐related consequences. No significant differences in growth trajectories were found between the 2 intervention conditions on past‐90‐day blood alcohol concentration, total alcohol consumption or weekend consumption. |
| Cimini 2009 | No significant effects of the intervention found |
| Clair 2013 | Hispanic adolescents who received MI significantly decreased total number of drinks on heavy drinking days (NDHD) and percentage of heavy drinking days (PHDD) compared to controls. No other alcohol outcomes reported |
| Clinton‐Sherrod 2011 | No significant effects of the intervention found |
| Ewing 2009 | No significant effects of the intervention found |
| Goti 2010 | No significant effects of the intervention found |
| Horner 2010 | No significant effects of the intervention found |
| LaBrie 2008 | Results indicated that, relative to the control group participants, intervention participants drank fewer drinks per week, drank fewer drinks at peak consumption events, and had fewer alcohol‐related consequences over a 10‐week follow‐up. Results for other measures were not reported: number of drinking days, average number of drinks, and number of binge drinking events (consuming 4 or more drinks in a row) |
| LaBrie 2009 | Intervention participants consumed significantly less than control participants on drinks per week, maximum drinks, and heavy episodic drinking events across 10 weeks of follow‐up. However, these effects did not persist at the 6‐month follow‐up. |
| Murphy 2004 | No significant effects of the intervention found |
| Murphy 2012a | At 15‐month follow‐up, past‐week alcohol use was significantly lower for intervention youth than control youth. |
| Naar‐King 2006 | No significant effects of the intervention found |
| Palmer 2004 | No significant effects of the intervention found |
| Thush 2009 | No significant effects of the intervention found |
| Wood 2007 | BMI produced significant decreases in Q/F, heavy drinking and problems |
| Wood 2010 | BMI participants were significantly less likely than non‐BMI participants to initiate heavy episodic drinking and to begin experiencing alcohol‐related consequences. |
BMI: brief motivational interviewing; MI: motivational interviewing; Q/F: quantity/frequency.
Discussion
Summary of main results
This systematic review assessed the effectiveness of motivational interviewing (MI) interventions for the prevention of alcohol use, misuse, problems and alcohol‐related risky behaviour in young people. Eighty‐four trials involving 22,872 participants were included, four of which were cluster‐randomised. Studies with longer‐term follow‐up (four months or more) were of more interest when considering the sustainability of intervention effects and were also less susceptible to short‐term reporting or publication bias.
Our primary outcome measures were quantity of alcohol consumed, frequency of alcohol consumption, binge drinking and alcohol problems. Some trials also reported average and peak BAC, but as these were calculated from consumption, sex and weight data, we did not regard them as objective measures of consumption; rather they were a variation of primary outcome measures relating to quantity and frequency. Secondary outcomes were alcohol‐impaired driving and other alcohol‐related risky behaviours.
At four or more months follow‐up, we found small effects in favour of MI for the quantity of alcohol consumed and frequency of alcohol consumption. We found no or only marginal effects for drinking problems and binge drinking. There was a very small effect for peak BAC in favour of MI, but not for average BAC, at four or more months follow‐up. We also considered other alcohol‐related behavioural outcomes, and at four or more months follow‐up we found no effects on drink‐driving or other alcohol‐related risky behaviour. The quality of the evidence for all outcomes was moderate, apart from drinking problems, which had low quality evidence.
At less than four months follow‐up, we found small effects in favour of MI for the quantity of alcohol consumed, the frequency of alcohol consumption, and alcohol problems. We found no effects for binge drinking. There was an effect in favour of MI for peak BAC, but not for average BAC, at less than four months follow‐up. For other alcohol‐related behavioural outcomes at less than four months follow‐up we found no effects on drink‐driving or other alcohol‐related risky behaviour. We consider these shorter‐term results to be less interesting and less reliable, as they provide little information about sustained effects of an intervention, and they are also more susceptible to reporting or publication bias influences than longer term outcomes. The quality of the evidence for all outcomes was moderate, apart from drinking problems, which had low quality evidence.
Further analyses showed that there was no clear relationship between the duration of the MI intervention (in minutes) and effect size. Subgroup analyses revealed no clear subgroup effects on longer‐term outcomes (four or more months) for assessment only versus alternative intervention controls; for university/college versus other settings; or for higher risk versus all/low risk students. At less than four months follow‐up, the subgroup analysis comparing no intervention versus alternative intervention controls showed a clear pattern of effect for the four primary outcomes analysed. Pooled effects were clearly larger in the assessment only subgroup compared with the alternative intervention subgroup. This suggests that, over the short‐term, MI may not confer any additional benefit over other, alternative interventions. One possible explanation is that participants' self reports are biased when they are exposed to an active intervention compared with no intervention, and this is more likely to manifest over the short term given the recentness of the intervention. An alternative explanation is that MI or other interventions do have a small effect on short term alcohol use and misuse, but these effects dissipate quickly, as they are not apparent in the longer term.
Our interpretation of these results is that, although we found some effects, the effect sizes are small and unlikely to be of any meaningful benefit in practice. For example, using mean and standard deviation figures from Martens 2013 to illustrate effect size characteristics, we estimate that for quantity of drinking at four or more months, the SMD from the meta‐analysis (−0.11) corresponds (approximately) to an average decrease in the number of drinks consumed each week from around 13.7 drinks/week to 12.5 drinks/week. Similarly, for frequency of drinking at four or more months, the SMD from the meta‐analysis (−0.14) corresponds (approximately) to an average decrease in the number of days/week alcohol was consumed from 2.74 days to 2.52 days. For alcohol problems, the SMD from the meta‐analysis (−0.08) corresponds to a decrease in the alcohol problems scale score (the 69‐point RAPI scale was used by Martens 2013) from 8.91 to 8.18). Similarly, For peak BAC, the SMD from the meta‐analysis (−0.12) corresponds to a decrease in peak BAC from around 0.144% to 0.131%, on average. We suggest that these achieved effect sizes would fall short, by some margin, of a minimally important clinical difference (MCID) if further research were to identify an MCID for alcohol misuse in young adults.
Overall completeness and applicability of evidence
This review has found a large number of studies and participants, with MIs implemented in a range of settings and of varying duration. It is possible that some studies that incorporated the core motivational interviewing components were not included in this review if these MI components were part of a more complex intervention and the MI aspects were not clearly identified enough in study articles to be found in our searches. For example, motivational techniques are sometimes described as being included in social normative feedback interventions, but the extent to which the core MI components are included is not clear. We have used our judgement to assess studies based on descriptions in articles retrieved during our searches, but it is possible that we have missed some studies that meet our eligibility criteria. However, we do not think the further inclusion of such studies would change the substantive results we have found in this review, for two reasons. First, in another, parallel, review that examined the effectiveness of social normative feedback, we found similarly weak effects unlikely to be of any meaningful benefit on their own (Foxcroft 2015). Any studies with poorly described MI components embedded in a social normative feedback intervention are likely to have been included in this other review. Second, the findings in the current review, based on a large number of studies and participants, are robust to new evidence being introduced: it would take a huge effect across numerous large studies to trouble the current findings, and we regard this as unlikely.
The results of the evidence in this review are applicable to all settings, including higher and vocational education and training, health system, social welfare and criminal justice settings. The results are also applicable to both universal and indication prevention: to young adults whether they are at higher risk, lower risk or where the risk of alcohol misuse is not known.
Quality of the evidence
Overall, there is only moderate or low quality evidence for these effects according to the GRADE method. The main reasons for downgrading the quality of the evidence in studies were either risk of bias, substantial heterogeneity, or both. Fewer than half the studies reported the method of randomisation, and less than a quarter of studies reported adequate allocation concealment. Only a minority of studies carried out blinding; this may have led to performance or detection bias. In non‐pharmaceutical studies, blinding of participants and therapists is not always feasible, and whilst the quality of studies can be high, the quality of the evidence is susceptible to risk of bias (Higgins 2011b).
When participants are not blinded to study condition and when outcomes are self reported behaviours, there is potential to overestimate intervention effects. In a systematic review of the effects of blinding participants in trials with self reported outcomes, Hrobjartsson 2014 found that non‐blinded participants exaggerated the standardised mean difference (SMD) effect size by an average of 0.56, though with considerable variation. It is therefore a strongly plausible hypothesis that the impact of non‐blinding of participants in motivational interviewing trials could fully account for any small effects found in our review.
Other forms of performance and detection bias are also important. For example, in a systematic review and meta‐analysis of 300 randomised trials, Petrosino 2005 looked at the impact of non‐independent researchers and found that in trials where programme developers were also the researchers the mean effect size was 0.47, compared with 0.00 when the evaluation team were external and independent. Petrosino 2005 concluded that "studies in which evaluators were greatly influential in the design and implementation of treatment report consistently and substantially larger effect sizes than other types of evaluators". The Cochrane 'Risk of bias' approach does not include an assessment of this particular risk of bias, and it is not always clear from studies the extent to which programme evaluators were involved in developing and delivering the intervention. Therefore we cannot rule out the possibility that the effect sizes obtained in the current review may be inflated by a conflict‐of‐interest bias.
Attrition rates were unacceptable in just under 30% of studies; this may limit the study power to detect pre‐specified between‐group differences or the extent of applicability of study results (Fewtrell 2008). We used a threshold of 20% attrition between low risk and high risk and, whilst this is consistent with other reviews, further research into the validity of this threshold is required: it may be that higher attrition rates are not problematic if there is no differential attrition. More importantly, in the case of differential attrition, study results may be seriously biased due to selection bias and confounding. Lack of adequate allocation concealment, blinding and attrition bias is associated with overestimation of intervention effects, and therefore we cannot rule out the possibility that the slight effects observed in this review may be exaggerated due to methodological limitations.
Potential biases in the review process
We found only one non‐English language study for inclusion. All other included studies were in English, making the review potentially vulnerable to English‐language bias as there may be other eligible studies in other languages. Although we searched for non‐English language literature, the bibliographic databases we searched are geared toward publications in English. We consider this to be a low risk as there would have to be a substantial number of large trials in other languages, which we did not find in our searches, to alter the conclusions of the review.
Agreements and disagreements with other studies or reviews
The findings of this review are consistent with other narrative syntheses of the literature, which have come to the conclusion that MIs show statistically significant effects in reducing alcohol misuse (Dunn 2001; Burke 2002a; Burke 2002b; Burke 2003; Hettema 2005; Lundahl 2010; O' Leary 2004; Rubak 2006; Smedslund 2011; Tanner‐Smith 2015; Vasilaki 2006).
However, our interpretation is different from these previous reviews because we conclude that the effect sizes are too small to have any meaningful impact on policy or practice. Moreover, the other reviews all differ somewhat from our review. Several of these reviews do not focus specifically on young people or alcohol‐related outcomes, or they do not solely evaluate MIs. Most of these reviews do not examine MIs from the perspective of prevention. Our literature search identified five relevant reviews with inclusion criteria similar to the current review, which reported that MIs produced statistically significant, durable results in the small to moderate effect range in relation to alcohol consumption, problems and other related measures (Carey 2007;Grenard 2006; Kohler 2015; Larimer 2007; Tait 2003).
In this review we have used very well established statistical methods for the meta‐analysis, as specified by Cochrane. Two other reviews have used a variety of more sophisticated but less well established multivariate statistical meta‐analytic techniques to include results from multiple time points and combine related outcomes. Tanner‐Smith 2015 reported that brief interventions led to significant reductions in alcohol consumption and alcohol‐related problems in young adults and that MI was associated with larger effects than some other types of interventions. Another review found no statistically significant effects of brief MIs for college student drinking over both the short and long term (Huh 2015).
One review examined which MI intervention characteristics might be predictive of intervention effects, and found that characteristics that were central concepts in a MI intervention were neither robust nor consistent predictors of effects (Bertholet 2014).
Authors' conclusions
Implications for practice.
The main results of this review indicate that there is no substantive, meaningful benefit of MI for alcohol misuse by young adults. Overall, there is only low or moderate quality evidence for the effects found in this review. Poorer quality evidence can overestimate intervention effects, so even the slight and unimportant effects found in some analyses may be overestimated.
Implications for research.
The evidence from this review, which alongside straightforward meta‐analyses also included further analyses as well as predictors or subgroups where effects could have been stronger, is fairly clear that effects across tested settings and subgroups are slight and likely to be unimportant. The quality of the evidence is not strong, but further higher quality research is likely only to strengthen the current findings as bias is reduced. However, if researchers wish to pursue this area in further studies, then questions include the optimal content of MI interventions and treatment exposure, whether they are likely to be more successful in young adults with certain characteristics, and whether MI in conjunction with other types of prevention interventions may be worthwhile (Foxcroft 2014). Studies should undertake more rigorous process evaluations alongside outcome evaluations. As small effects could provide important cost‐benefits for prevention programmes, it is important to undertake studies with sufficient statistical power to detect small effects and to undertake cost‐benefit analyses. Alongside this, further research should consider the minimal clinically important difference (MCID) to aid interpretation of small effects. Such small effects may vary in size and importance between subgroups, so further research should also be powered to detect other hypothesised subgroup effects. Reporting of programme content and context should be more detailed and systematic to enable comparison of these aspects across studies. Further improvement to study design, analysis and reporting, in line with accepted guidance, is required (CONSORT 2010).
Feedback
Critiques of the first published review
Summary
Two critiques of the first version of this review have been published: Grant 2015 and Mun 2015.
We respond to the main points raised in these critiques below.
Reply
Here we set out our overall response to the critiques. We have prepared this response with support from the Cochrane Drugs and Alcohol editorial group and statistical advisor.
First, we made a few data extraction and coding mistakes in our original review, so we asked the Cochrane group to withdraw the review whilst we fixed these mistakes and updated the search. Thanks to Mun 2015 for pointing out these mistakes. They also raised some other points.
The first is that they stated that potentially meaningful subgroups for MI were not explored in the presence of substantial statistical heterogeneity beyond chance. Post hoc subgroup analyses to explore heterogeneity are not advised by Cochrane (Higgins 2011a):
“Findings from multiple subgroup analyses may be misleading. Subgroup analyses are observational by nature and are not based on randomized comparisons. False negative and false positive significance tests increase in likelihood rapidly as more subgroup analyses are performed. If their findings are presented as definitive conclusions there is clearly a risk of patients being denied an effective intervention or treated with an ineffective (or even harmful) intervention. Subgroup analyses can also generate misleading recommendations about directions for future research that, if followed, would waste scarce resources”.
However, we did undertake some subgroup analyses in the revised review, as suggested by Mun 2015, but were circumspect about their value and interpretation. The subgroup analyses showed no important subgroup effects.
Second, it was suggested that our search strategy had not been comprehensive as some eligible studies were missed. They are partly right. Our search strategy was highly sensitive but not perfect. We did miss a small number of studies at initial screening stage that were not clearly identified in the title or abstract as motivational interviewing interventions. Where there was any doubt at initial screen we obtained the full paper for full checks, but obviously we missed a small number of studies. We have now included these in the revised review, with no substantive impact on the review findings. Mun 2015 also question the qualifications of reviewers, suggesting that these should have been published, but this is not in line with Cochrane policy or practice. The rules of the Cochrane Drugs and Alcohol Group are available at http://cda.cochrane.org/cdag‐editorial‐process, and state:
“During the registration process we request that a review team can support the review with respect to clinical expertise in addition to statistical and methodological experience. The team should include: at least two people; an experienced Cochrane review author; someone with topic expertise in the title you are registering; someone with statistical and methodological expertise; someone with English as a first language, or a very high standard of written English; a Contact author responsible for developing and co‐ordinating the review team, liaising with the editorial base and taking responsibility for the on‐going updates of the review. It is important that authors are aware of Conflicts of interest and Cochrane Reviews and Commercial Sponsorship Policy.”
Third, as mentioned above, Mun 2015 spotted a few data abstraction and coding mistakes. We apologise for these, and in the revised review have double checked all data entry and coding. Hopefully we have got this right now. Because of naming idiosyncrasies, we also made a mistake in the effect size measure used. RevMan uses the term standardised mean difference (SMD) to refer to Hedges'g . However, inComprehensive Meta Analysis, a software programme that we used for calculating pooled estimates, SMD refers to Cohen’s d rather than Hedges'g. We didn’t spot this issue until we went back to check the meta‐analysis. In the revised review all computed effect size estimates are Hedges'g . This correction has not made any substantive difference to the review results or conclusions.
Fourth, it was suggested that using subgroups from studies as separate comparisons in the meta‐analysis violates assumptions when combining estimates. But the approach we took, and which is maintained in the revised review, is consistent with Cochrane guidance for dealing with multiple comparisons (Higgins 2011a):
“Split the ‘shared’ group into two or more groups with smaller sample size, and include two or more (reasonably independent) comparisons” (Section 16.5.4).
Mun 2015 also pointed out that we counted multiple outcomes independently when they were likely correlated. This is correct, and it is usual in Cochrane meta‐analyses for related outcomes to be analysed in distinct meta‐analyses. Although there are some techniques available to combine related outcomes in meta‐analyses, these are not frequently used in Cochrane meta‐analyses.
Mun 2015 also suggested that we should always take account of baseline data in calculating effect sizes. When dealing with continuous data a common feature is that measurements used to assess outcomes of each participant are also measured at baseline, before interventions are administered. For this reason, differences in changes from baseline as the primary outcome can be used. The Cochrane Handbook for Systematic Reviews of Interventions says that review authors are advised not to focus on change from baseline unless this method of analysis was used in some of the study reports (Higgins 2011a). When addressing change from baseline, a single measurement is created for each participant, obtained either by subtracting the final measurement from the baseline measurement or by subtracting the baseline measurement from the final measurement. Analyses then proceed as for any other type of continuous outcome variable using the changes rather than the final measurements. Commonly, studies in a review will have used a mixture of changes from baseline and final values. Some studies will report both; others will report only change scores or only final values. As explained in Chapter 9 (Section 9.4.5.2) of Higgins 2011a, both final values and change scores can sometimes be combined in the same analysis so this is not necessarily a problem. Higgins 2011a also states that authors can extract data on both change from baseline and final value outcomes if the required means and standard deviations are available. In the review, where possible we used change from baseline scores. This was not always possible and in this case, we used final scores.
In another critique, Grant 2015 makes four points. The first three points raise questions about the general methodology of Cochrane reviews: risk of bias assessments, search strategies and assessing the quality of the body of evidence. Our response is that we followed the guidance in Higgins 2011a. Grant 2015 also suggests that performance bias should be dealt with more leniently. However, we believe that just because this bias is difficult to deal with in complex behavioural intervention trials, it does not mean we should downplay or ignore it. More research is needed to understand the problem and, in the meantime, it seems appropriate to be cautious. Of particular concern when participants are not blinded to study condition and when outcomes are self reported behaviours is the potential for overestimation of intervention effects. In a systematic review of the effects of blinding participants in trials with self reported outcomes, Hrobjartsson 2014 found that non‐blinded participants exaggerated the standardised mean difference (SMD) effect size by an average of 0.56, though with considerable variation. It is therefore a strongly plausible hypothesis that the impact of non‐blinded participants in motivational interviewing trials could fully account for any small effects found in our review.
Other forms of performance and detection bias are also important. For example, in a systematic review and meta‐analysis of 300 randomised trials, Petrosino 2005 looked at the impact of non‐independent researchers and found that in those trials where programme developers were also the researchers, the mean effect size was 0.47, compared with 0.00 when the evaluation team were external and independent. Petrosino 2005 concluded that "studies in which evaluators were greatly influential in the design and implementation of treatment report consistently and substantially larger effect sizes than other types of evaluators". The Cochrane risk of bias approach does not include an assessment of this particular risk of bias, and it is not always clear from studies the extent to which programme evaluators were involved in developing and delivering the intervention. Therefore we cannot rule out the possibility that the effect sizes obtained in the current review may be inflated by a conflict‐of‐interest bias.
The fourth point should be discussed more widely amongst researchers and policy makers: what sort of effect size is good enough? Our interpretation of the effect sizes we found across a series of meta‐analyses was that they were very small and unlikely to be of any meaningful benefit on their own, regardless of any possible but unknown reductions in effect sizes due to bias. For example, in the original review, we estimated that the obtained effect sizes would mean (approximately, on average): a decrease in the number of days per week alcohol was consumed from 2.7 days to 2.5 days; a decrease in the number of drinks consumed each week from 13 drinks per week to 11 drinks per week; and a decrease in the 69‐point Rutgers Alcohol Problems Index (RAPI) from a score of 8.9 to 8.7. We suggest that these achieved effect sizes may fall short of a minimally important clinical difference (MCID). In the revised review there are no substantive differences or changes in our conclusions. Grant 2015 disagree with our interpretation, a decision that we respect: users of research evidence should make up their own minds on the right interpretation of the evidence.
Overall, critical feedback supports scientific progress, and we are grateful to the authors who took time to carefully review our work and point out limitations. The review is now stronger and we believe that the results and conclusions, having not substantively changed from the initial review, should be regarded as scientifically robust.
Contributors
David R. Foxcroft, Laura Amato, Roberto D'Amico.
What's new
| Date | Event | Description |
|---|---|---|
| 5 January 2016 | New search has been performed | Revised to incorporate one study identified in more sensitive search of CCRCT to 2015 |
| 26 November 2015 | New citation required but conclusions have not changed | Revised review to correct several coding errors identified in previous version and communicated by study authors. Changed SMD effect size estimate from Cohen's d to Hedges' g. Search updated to July 2015 and additional studies incorporated from updated search and also from new information contributed by study authors. Two new subgroup analyses (setting and risk status) added based on suggestions made by study authors. No changes to overall findings or conclusions in the previous version of the review. |
History
Protocol first published: Issue 2, 2008 Review first published: Issue 8, 2014
| Date | Event | Description |
|---|---|---|
| 21 December 2007 | New citation required and major changes | Substantive amendment |
Acknowledgements
None.
Appendices
Appendix 1. CENTRAL search strategy
#1 MeSH descriptor: [Directive Counseling] explode all trees
#2 MeSH descriptor: [Motivation] explode all trees
#3 (motivat*) near/5 (interview* or counsel* or therap* or consult* or intervention* or enhance*):ti,ab,kw
#4 ((brief) near/3 (intervention* or interview*)):ti,ab
#5 #1 or #2 or #3 or #4
#6 MeSH descriptor: [Alcohol‐Related Disorders] explode all trees
#7 MeSH descriptor: [Alcohol Drinking] explode all trees
#8 (alcohol near/3 (drink* or use* or abus* or misus* or risk* or consum* or intoxicat* or detox* or treat* or therap* or excess* or reduc* or cessation or intervention)):ti,ab
#9 (drink* near/3 (excess or heavy or heavily or hazard* or binge or harmful or problem*)):ti,ab
#10 #6 or #7 or #8 or #9
#11 #5 and #10 in Trials
Appendix 2. MEDLINE search strategy
exp ALCOHOLS/ad, ae
exp Alcohol Drinking/
exp Alcohol Abuse/
exp Alcohol, Ethyl/ae
alcohol$.ti,ab.
drink$.ti,ab.
drunk$.ti,ab.
intoxicat$.ti,ab.
or/1‐8
(motivation* and interview*).ti,ab.
(motivation* and enhance*).ti,ab.
10 or 11
RANDOMIZED CONTROLLED TRIAL.pt.
CONTROLLED CLINICAL TRIAL.pt.
RANDOMIZED CONTROLLED TRIALS.sh.
RANDOM ALLOCATION.sh.
DOUBLE BLIND METHOD.sh.
SINGLE BLIND METHOD.sh.
or/13‐18
CLINICAL TRIAL.pt.
exp CLINICAL TRIALS/
(clin$ adj trial$).ti,ab.
((singl$ or doubl$ or trebl$ or tripl$) adj (blind$ or mask$)).ti,ab.
PLACEBOS.sh.
placebo$.ti,ab.
random$.ti,ab.
RESEARCH DESIGN.sh.
or/20‐27
19 or 28
(ANIMALS not HUMAN).sh.
30 not 31
9 and 12 and 31
Appendix 3. EMBASE search strategy
exp alcohol/
Drinking Behavior/
Alcoholism/
exp alcohol abuse/
exp Alcohol Drinking/
drink$.ti,ab.
drunk$.ti,ab.
intoxicat$.ti,ab.
alcohol$.ti,ab.
or/1‐9
motivation$ and interview$).ti,ab.
(motivation$ and enhance$).ti,ab.
11 or 12
random$.ab,ti.
placebo.ab,ti.
((singl$ or doubl$ or trebl$ or tripl$) and (blind$ or mask$)).mp. [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword]
(cross‐over$ or crossover$).tw.
randomized controlled trial/
phase‐2‐clinical‐trial/
phase‐3‐clinical‐trial/
double blind procedure/
single blind procedure/
crossover procedure/
Latin square design/
exp PLACEBOS/
multicenter study/
or/14‐26
limit 27 to humans
10 and 13 and 28
Appendix 4. PsycINFO search strategy
1. alcohol$.ti,ab. 2. drink$.ti,ab. 3. drunk$.ti,ab. 4. intoxicat$.ti,ab. 5. exp sobriety/ or exp alcohol withdrawal/ or exp alcohol intoxication/ or exp alcoholism/ or exp alcohols/ or exp blood alcohol concentration/ or exp binge drinking/ or exp driving under the influence/ or exp alcohol abuse/ or exp alcoholic psychosis/ or exp alcohol rehabilitation/ or exp alcohol drinking patterns/ 6. or/1‐5 7. (motivation$ and interview$).ti,ab. 8. (motivation$ and enhance$).ti,ab. 9. 7 or 8 10. clinical trials.sh. 11. placebo.sh. 12. (Single adj blind*).ab,ti. 13. (Single adj dumm*).ab,ti. 14. (Single adj mask*).ab,ti. 15. (Double adj blind*).ab,ti. 16. (Double adj dumm*).ab,ti. 17. (Double adj mask*).ab,ti. 18. (triple adj blind*).ab,ti. 19. (triple adj dumm*).ab,ti. 20. (triple adj mask*).ab,ti. 21. (treble adj blind*).ab,ti. 22. (treble adj dumm*).ab,ti. 23. (treble adj mask*).ab,ti. 24. (control* adj study).ab,ti. 25. (control* adj studies).ab,ti. 26. (control* adj trial*).ab,ti. 27. (Random* or sham or shams or placebo* or RCT*).ab,ti. 28. or/10‐27 29. 6 and 9 and 28
Appendix 5. criteria for risk of bias judgment
| Item | Judgment | Description |
| Random sequence generation (selection bias) | Low risk | The investigators describe a random component in the sequence generation process such as: random number table; computer random number generator; coin tossing; shuffling cards or envelopes; throwing dice; drawing of lots; minimisation |
| High risk | The investigators describe a non‐random component in the sequence generation process such as: odd or even date of birth; date (or day) of admission; hospital or clinic record number; alternation; judgement of the clinician; results of a laboratory test or a series of tests; availability of the intervention | |
| Unclear risk | Insufficient information about the sequence generation process to permit judgement of low or high risk | |
| Allocation concealment (selection bias) | Low risk | Investigators enrolling participants could not foresee assignment because one of the following, or an equivalent method, was used to conceal allocation: central allocation (including telephone, web‐based, and pharmacy‐controlled, randomisation); sequentially numbered drug containers of identical appearance; sequentially numbered, opaque, sealed envelopes |
| High risk | Investigators enrolling participants could possibly foresee assignments because one of the following methods was used: open random allocation schedule (e.g. a list of random numbers); assignment envelopes without appropriate safeguards (e.g. if envelopes were unsealed or non‐opaque or not sequentially numbered); alternation or rotation; date of birth; case record number; any other explicitly unconcealed procedure | |
| Unclear risk | Insufficient information to permit judgement of low or high risk; this is usually the case if the method of concealment is not described or not described in sufficient detail to allow a definite judgement | |
| Blinding of participants and providers (performance bias) | Low risk | No blinding or incomplete blinding, but the review authors judge that the outcome is not likely to be influenced by lack of blinding; blinding of participants and key study personnel ensured, and unlikely that the blinding could have been broken |
| High risk | No blinding or incomplete blinding, and the outcome is likely to be influenced by lack of blinding; blinding of key study participants and personnel attempted, but likely that the blinding could have been broken, and the outcome is likely to be influenced by lack of blinding | |
| Unclear risk | Insufficient information to permit judgement of low or high risk | |
| Blinding of outcome assessor (detection bias) | Low risk | No blinding of outcome assessment, but the review authors judge that the outcome measurement is not likely to be influenced by lack of blinding; blinding of outcome assessment ensured, and unlikely that the blinding could have been broken |
| High risk | No blinding of outcome assessment, and the outcome measurement is likely to be influenced by lack of blinding; blinding of outcome assessment, but likely that the blinding could have been broken, and the outcome measurement is likely to be influenced by lack of blinding | |
| Unclear risk | Insufficient information to permit judgement of low or high risk | |
| Incomplete outcome data (attrition bias) For all outcomes except retention in treatment or drop out |
Low risk | No missing outcome data; reasons for missing outcome data unlikely to be related to true outcome (for survival data, censoring unlikely to be introducing bias); missing outcome data balanced in numbers across intervention groups, with similar reasons for missing data across groups; for dichotomous outcome data, the proportion of missing outcomes compared with observed event risk not enough to have a clinically relevant impact on the intervention effect estimate; for continuous outcome data, plausible effect size (difference in means or standardized difference in means) among missing outcomes not enough to have a clinically relevant impact on observed effect size; missing data have been imputed using appropriate methods; all randomised patients are reported/analysed in the group they were allocated to by randomisation irrespective of non‐compliance and co‐interventions (intention‐to‐treat) |
| High risk | Reason for missing outcome data likely to be related to true outcome, with either imbalance in numbers or reasons for missing data across intervention groups; for dichotomous outcome data, the proportion of missing outcomes compared with observed event risk enough to induce clinically relevant bias in intervention effect estimate; for continuous outcome data, plausible effect size (difference in means or standardized difference in means) among missing outcomes enough to induce clinically relevant bias in observed effect size; Per protocol analysis done with substantial departure of the intervention received from that assigned at randomisation | |
| Unclear risk | Insufficient information to permit judgement of low or high risk (e.g. number randomised not stated, no reasons for missing data provided, number of drop out not reported for each group) | |
| Selective reporting (reporting bias) | Low risk | The study protocol is available and all of the study’s pre‐specified (primary and secondary) outcomes that are of interest in the review have been reported in the pre‐specified way; the study protocol is not available but it is clear that the published reports include all expected outcomes, including those that were pre‐specified (convincing text of this nature may be uncommon) |
| High risk | Not all of the study’s pre‐specified primary outcomes have been reported; one or more primary outcomes is reported using measurements, analysis methods or subsets of the data (e.g. subscales) that were not pre‐specified; one or more reported primary outcomes were not pre‐specified (unless clear justification for their reporting is provided, such as an unexpected adverse effect); one or more outcomes of interest in the review are reported incompletely so that they cannot be entered in a meta‐analysis; the study report fails to include results for a key outcome that would be expected to have been reported for such a study | |
| Unclear risk | Insufficient information to permit judgement of low or high risk | |
| Other sources of bias | Low risk | Not a cluster trial, or a cluster trial without any problems due to recruitment bias; baseline imbalance; loss of clusters; incorrect analysis |
| High risk | A cluster trial with weaknesses in one or more of the following aspects: recruitment bias; baseline imbalance; loss of clusters; incorrect analysis | |
| Unclear risk | Insufficient information to permit judgement of low or high risk |
Data and analyses
Comparison 1. MI versus no MI (assessment only and alternative intervention) at ≥ 4 months follow‐up.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Quantity of alcohol consumed | 33 | 7971 | Std. Mean Difference (Random, 95% CI) | ‐0.11 [‐0.15, ‐0.06] |
| 2 Frequency of alcohol consumption | 17 | 4377 | Std. Mean Difference (Random, 95% CI) | ‐0.14 [‐0.21, ‐0.07] |
| 3 Binge drinking | 21 | 5479 | Std. Mean Difference (Random, 95% CI) | ‐0.04 [‐0.09, 0.02] |
| 4 Alcohol problems | 25 | 6868 | Std. Mean Difference (Random, 95% CI) | ‐0.08 [‐0.17, ‐0.00] |
| 5 Average BAC | 5 | 901 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.05 [‐0.18, 0.08] |
| 6 Peak BAC | 13 | 2790 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.12 [‐0.20, ‐0.05] |
| 7 Drink‐driving | 4 | 1205 | Std. Mean Difference (Random, 95% CI) | ‐0.13 [‐0.36, 0.10] |
| 8 Risky behaviour | 7 | 1579 | Std. Mean Difference (Random, 95% CI) | ‐0.15 [‐0.31, 0.01] |
Comparison 2. MI versus no MI (assessment only and alternative intervention) at < 4 months follow‐up.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Quantity of alcohol consumed | 39 | 5600 | Std. Mean Difference (Random, 95% CI) | ‐0.17 [‐0.25, ‐0.09] |
| 2 Frequency of alcohol consumption | 24 | 3296 | Std. Mean Difference (Random, 95% CI) | ‐0.18 [‐0.29, ‐0.07] |
| 3 Binge drinking | 25 | 4090 | Std. Mean Difference (Random, 95% CI) | ‐0.13 [‐0.23, ‐0.03] |
| 4 Alcohol problems | 34 | 5109 | Std. Mean Difference (Random, 95% CI) | ‐0.10 [‐0.18, ‐0.01] |
| 5 Average BAC | 6 | 1096 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.14 [‐0.30, 0.01] |
| 6 Peak BAC | 14 | 2408 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.23 [‐0.32, ‐0.13] |
| 7 Drink‐driving | 4 | 895 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.22 [‐0.38, ‐0.06] |
| 8 Risky behaviour | 5 | 745 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.05 [‐0.33, 0.22] |
Comparison 3. Subgroup analysis: control condition at ≥ 4 months follow‐up.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Quantity of alcohol consumed | 33 | 7971 | Std. Mean Difference (Random, 95% CI) | ‐0.11 [‐0.15, ‐0.06] |
| 1.1 Alternative intervention controls | 17 | 3614 | Std. Mean Difference (Random, 95% CI) | ‐0.12 [‐0.19, ‐0.06] |
| 1.2 Assessment only controls | 16 | 4357 | Std. Mean Difference (Random, 95% CI) | ‐0.09 [‐0.15, ‐0.03] |
| 2 Frequency of alcohol consumption | 17 | 4377 | Std. Mean Difference (Random, 95% CI) | ‐0.14 [‐0.21, ‐0.07] |
| 2.1 Alternative intervention controls | 10 | 2523 | Std. Mean Difference (Random, 95% CI) | ‐0.10 [‐0.20, ‐0.00] |
| 2.2 Assessment only controls | 7 | 1854 | Std. Mean Difference (Random, 95% CI) | ‐0.16 [‐0.26, ‐0.07] |
| 3 Binge drinking | 21 | 5479 | Std. Mean Difference (Random, 95% CI) | ‐0.04 [‐0.09, 0.02] |
| 3.1 Alternative intervention controls | 11 | 2271 | Std. Mean Difference (Random, 95% CI) | ‐0.06 [‐0.14, 0.03] |
| 3.2 Assessment only controls | 10 | 3208 | Std. Mean Difference (Random, 95% CI) | ‐0.02 [‐0.09, 0.04] |
| 4 Alcohol problems | 25 | 6868 | Std. Mean Difference (Random, 95% CI) | ‐0.08 [‐0.17, ‐0.00] |
| 4.1 Alternative intervention controls | 15 | 3944 | Std. Mean Difference (Random, 95% CI) | ‐0.02 [‐0.12, 0.07] |
| 4.2 Assessment only controls | 10 | 2924 | Std. Mean Difference (Random, 95% CI) | ‐0.18 [‐0.29, ‐0.06] |
Comparison 4. Subgroup analysis: control condition at < 4 months follow‐up.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Quantity of alcohol consumed | 39 | 5600 | Std. Mean Difference (Random, 95% CI) | ‐0.17 [‐0.25, ‐0.09] |
| 1.1 Alternative intervention controls | 15 | 2793 | Std. Mean Difference (Random, 95% CI) | ‐0.11 [‐0.21, ‐0.02] |
| 1.2 Assessment only controls | 24 | 2807 | Std. Mean Difference (Random, 95% CI) | ‐0.23 [‐0.36, ‐0.10] |
| 2 Frequency of alcohol consumption | 24 | 3296 | Std. Mean Difference (Random, 95% CI) | ‐0.18 [‐0.29, ‐0.07] |
| 2.1 Alternative intervention controls | 9 | 1902 | Std. Mean Difference (Random, 95% CI) | ‐0.00 [‐0.15, 0.14] |
| 2.2 Assessment only controls | 15 | 1394 | Std. Mean Difference (Random, 95% CI) | ‐0.33 [‐0.44, ‐0.23] |
| 3 Binge drinking | 25 | 4090 | Std. Mean Difference (Random, 95% CI) | ‐0.13 [‐0.23, ‐0.03] |
| 3.1 Alternative intervention controls | 9 | 1625 | Std. Mean Difference (Random, 95% CI) | ‐0.00 [‐0.13, 0.13] |
| 3.2 Assessment only controls | 16 | 2465 | Std. Mean Difference (Random, 95% CI) | ‐0.21 [‐0.35, ‐0.08] |
| 4 Alcohol problems | 34 | 5109 | Std. Mean Difference (Random, 95% CI) | ‐0.10 [‐0.18, ‐0.01] |
| 4.1 Alternative intervention controls | 13 | 2674 | Std. Mean Difference (Random, 95% CI) | ‐0.01 [‐0.12, 0.10] |
| 4.2 Assessment only controls | 21 | 2435 | Std. Mean Difference (Random, 95% CI) | ‐0.18 [‐0.29, ‐0.07] |
Comparison 5. Subgroup analysis: setting ≥ 4 months follow‐up.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Quantity of alcohol consumed | 33 | 7971 | Std. Mean Difference (Random, 95% CI) | ‐0.11 [‐0.15, ‐0.06] |
| 1.1 University/college settings | 22 | 5119 | Std. Mean Difference (Random, 95% CI) | ‐0.13 [‐0.19, ‐0.08] |
| 1.2 Other settings | 11 | 2852 | Std. Mean Difference (Random, 95% CI) | ‐0.06 [‐0.14, 0.02] |
| 2 Frequency of alcohol consumption | 17 | 4377 | Std. Mean Difference (Random, 95% CI) | ‐0.14 [‐0.21, ‐0.07] |
| 2.1 University/college settings | 11 | 3071 | Std. Mean Difference (Random, 95% CI) | ‐0.12 [‐0.21, ‐0.04] |
| 2.2 Other settings | 6 | 1306 | Std. Mean Difference (Random, 95% CI) | ‐0.17 [‐0.31, ‐0.03] |
| 3 Binge drinking | 21 | 5479 | Std. Mean Difference (Random, 95% CI) | ‐0.04 [‐0.10, 0.01] |
| 3.1 University/college settings | 12 | 3059 | Std. Mean Difference (Random, 95% CI) | ‐0.04 [‐0.11, 0.03] |
| 3.2 Other settings | 9 | 2420 | Std. Mean Difference (Random, 95% CI) | ‐0.06 [‐0.18, 0.07] |
| 4 Alcohol problems | 25 | 6868 | Std. Mean Difference (Random, 95% CI) | ‐0.08 [‐0.17, ‐0.00] |
| 4.1 University/college settings | 20 | 5055 | Std. Mean Difference (Random, 95% CI) | ‐0.10 [‐0.19, ‐0.02] |
| 4.2 Other settings | 5 | 1813 | Std. Mean Difference (Random, 95% CI) | ‐0.02 [‐0.21, 0.16] |
Comparison 6. Subgroup analysis: participant risk at ≥ 4 months or more of follow‐up.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Quantity of alcohol consumed | 33 | 7971 | Std. Mean Difference (Random, 95% CI) | ‐0.11 [‐0.15, ‐0.06] |
| 1.1 Higher risk only | 26 | 6494 | Std. Mean Difference (Random, 95% CI) | ‐0.12 [‐0.17, ‐0.07] |
| 1.2 All/low risk | 7 | 1477 | Std. Mean Difference (Random, 95% CI) | ‐0.06 [‐0.20, 0.07] |
| 2 Frequency of alcohol consumption | 17 | 4377 | Std. Mean Difference (Random, 95% CI) | ‐0.14 [‐0.21, ‐0.07] |
| 2.1 Higher risk only | 14 | 3944 | Std. Mean Difference (Random, 95% CI) | ‐0.15 [‐0.23, ‐0.07] |
| 2.2 All/low risk | 3 | 433 | Std. Mean Difference (Random, 95% CI) | ‐0.07 [‐0.29, 0.15] |
| 3 Binge drinking | 21 | 5479 | Std. Mean Difference (Random, 95% CI) | ‐0.04 [‐0.10, 0.01] |
| 3.1 Higher risk only | 16 | 4352 | Std. Mean Difference (Random, 95% CI) | ‐0.06 [‐0.12, 0.01] |
| 3.2 All/low risk | 5 | 1127 | Std. Mean Difference (Random, 95% CI) | ‐0.00 [‐0.12, 0.12] |
| 4 Alcohol problems | 25 | 6868 | Std. Mean Difference (Random, 95% CI) | ‐0.08 [‐0.17, ‐0.00] |
| 4.1 Higher risk only | 22 | 6384 | Std. Mean Difference (Random, 95% CI) | ‐0.11 [‐0.19, ‐0.03] |
| 4.2 All/low risk | 3 | 484 | Std. Mean Difference (Random, 95% CI) | 0.14 [‐0.15, 0.43] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Amaro 2009.
| Methods |
Design: RCT Follow‐up: 3 and 6 months Attrition: 15.8% ‐ 3 months; 16.9% ‐ 6 months |
|
| Participants |
Mean age (years): 20.4 Sex: 71% male N participants: 265 Allocation: n = 133 intervention; n = 132 control Setting: university students mandated for alcohol or drug violation (higher risk) Country: USA |
|
| Interventions |
Programme type: motivational interviewing, University Assistance Programme (UAP) Set‐up: 2 individual sessions with UAP counsellor (3 sessions for serious offenders) Key components: feedback of assessment results: BMI incorporating motivational interviewing and skills training. For additional social, personal or adjustment issues: solution‐focused therapy, stress management, supportive counselling, coping skills‐based interventions Duration: not stated Control: standard care service offered by the university. First offenders (n = 66) completed a 2.5 h web‐based alcohol education programme, more serious offenders completed a series of 3 sessions plus 1.5 h educational group session focusing on the consequences of alcohol use. |
|
| Outcomes |
Outcomes: total weekly consumption; total weekend consumption; total weekday consumption, BAC; heavy episode drinking; consequences of alcohol; coping skills; use of protective behaviour Measures: Daily Drinking Questionnaire; Quantity and Frequency Index; Rutgers Alcohol Problem Index; Coping Skills Scale; Use of Protective Behaviors Scale |
|
| Funding and Declared Conflicts of Interest | Research funded by the NIAAA. No information about potential conflicts of interest | |
| Notes | Results not in suitable format for MA; author contacted for further information | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to make a judgement "Participants were randomized to one of two interventions conditions . . ." |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 16.9% attrition and ITT analysis |
| Selective reporting (reporting bias) | High risk | Not all alcohol outcomes reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to intervention. Insufficient information to make judgement about blinding of therapists |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to make a judgement |
| Unit of Analysis issues | Low risk | Not applicable |
Aubrey 1998.
| Methods |
Design: RCT Follow‐up: 3 months Attrition: 49% |
|
| Participants |
Mean age (years): 16.83 Sex: 78% male N participants: 77 Allocation: n = 39 intervention; n = 38 control Setting: outpatient substance abuse department (higher risk) Country: USA |
|
| Interventions |
Programme type: motivational interviewing Set‐up: individual single session Key components: feedback of assessment results: social norms, peak blood alcohol concentration, consequences, strategies, decisional balance Duration: 30 to 60 min Control: assessment only |
|
| Outcomes |
Outcomes: alcohol use; alcohol‐related consequences Measures: Form‐90; Alcohol Dependence Scale; Inventory of Drug Use Consequences (InDUC‐2R); Adolescent Consequences Inventory of Drinking and Drugs (ACID‐D) |
|
| Funding and Declared Conflicts of Interest | No information | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random assignment was assured by using a random numbers table to dictate the sequence of research packets |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a judgement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 49% attrition and no imputation of missing values |
| Selective reporting (reporting bias) | High risk | Not all alcohol outcomes reported (e.g. Alcohol Dependency Scale) |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to intervention. Insufficient information to make judgement about blinding of therapists |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Follow‐up was not carried out by an interviewer blind to the treatment condition |
| Unit of Analysis issues | Low risk | Not applicable |
Bailey 2004.
| Methods |
Design: RCT Follow‐up: 1 month, 2 months Attrition: 0% |
|
| Participants |
Mean age (years): 15.44 Sex: 50% male N participants: 34 Allocation: n = 17 intervention; n = 17 control Setting: youth service with higher risk clients due to low SES Country: Australia |
|
| Interventions |
Programme type: motivational interviewing and cognitive behaviour therapy Set‐up: 4 group sessions Key components: basic information about standard drinks, short‐term and long‐term effects of alcohol consumption, participant attitudes towards drinking, setting limits to drinking and alcohol refusal skills Duration: session 1: 40 min; sessions 2‐4: 30 min Control: assessment only |
|
| Outcomes |
Outcomes: readiness to reduce or quit drinking; alcohol consumption; harms associated with drinking; knowledge regarding recommended drinking levels, psychological and physical effects of alcohol consumption Measures: Readiness to Change Questionnaire; Alcohol Use Disorders Identification Test; Drug and Alcohol Problem (DAP) Quick Screen |
|
| Funding and Declared Conflicts of Interest | No information | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomisation was performed via a card selection task, which involved up to 10 participants at a time selecting a card from 10 shuffled cards (5 of which were red and 5 of which were black) |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No attrition |
| Selective reporting (reporting bias) | Low risk | All the outcome measures were reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to intervention. Treatment was delivered by one of the investigators (unblinded) |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to make a judgement |
| Unit of Analysis issues | Low risk | Not applicable |
Barnett 2007.
| Methods |
Design: RCT Follow‐up: 3 months, 12 months Attrition: 6% at 12 months |
|
| Participants |
Mean age (years): 18.8 Sex: 52% female N participants:225 Allocation: n = 112 intervention; n = 113 control Setting: university students mandated for intervention following alcohol incident Country: USA |
|
| Interventions |
Programme type: brief motivational interviewing Set‐up: individual single session Key components: introduction and review of alcohol incident, assessing motivation, enhancing motivation and establishing goals Duration: not stated Control: alternative intervention |
|
| Outcomes |
Outcomes number of drinking days; heavy drinking days; average number of drinks per day; average blood alcohol concentration; alcohol‐related problems Measures: Timeline Followback; Young Adult Alcohol Problems Screening Test |
|
| Funding and Declared Conflicts of Interest | Funded by NIAAA and Dept of Veterans Affairs. No information about potential conflicts of interest | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random numbers table used |
| Allocation concealment (selection bias) | Low risk | Sealed envelope prepared by project co‐ordinator |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition 6% |
| Selective reporting (reporting bias) | Low risk | All outcome measures are reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to intervention. Insufficient information to make a judgement about blinding of therapists |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | A research assistant who was blind to intervention condition conducted the 3‐ and 12‐month follow‐up assessments in person, or by phone and mail |
| Unit of Analysis issues | Low risk | Not applicable |
Barnett 2010.
| Methods |
Design: RCT Follow‐up: 6 and 12 months Attrition: 20% |
|
| Participants |
Mean age (years): 20.5 Sex: 65% male N participants: 215 Allocation: not reported Setting: hospital emergency department with recent or risky drinkers Country: USA |
|
| Interventions |
Programme type: motivational interviewing Set‐up: individual single session Key components: exploration, feedback, support for self efficacy, discussion re alcohol use and risky behaviour, establishing rapport, assessing and enhancing motivation for change, and establishing goals for change. Booster session 1 and 3 month Duration: 30‐45 min Control: alternative intervention |
|
| Outcomes |
Outcomes: 30‐day use; number of days drinking; number of heavy drinking days; average number of drinks per week Measures: Timeline Followback; Rutgers Alcohol Problem Index; Alcohol Use Disorders Identification Test |
|
| Funding and Declared Conflicts of Interest | Funded by NIAAA and Dept of Veterans Affairs. COI statement declares no conflicts | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to make a judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition 20% |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants or therapists to intervention. Insufficient information to make a judgement about blinding of therapists |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to make a judgement |
| Unit of Analysis issues | Low risk | Not applicable |
Bernstein 2010.
| Methods |
Design: RCT Follow‐up: 3 and 12 months Attrition: 28% |
|
| Participants |
Age range (years): 14‐21 Sex: 45% male N participants: 853 Allocation: n = 283 intervention; n = 570 control (286 minimally assessed control) Setting: hospital paediatric emergency department with risky drinkers Country: USA |
|
| Interventions |
Programme type: brief motivational interviewing Set‐up: single individual session Key components: obtaining engagement and permission to raise the subject; establishing context; offering brief feedback, information, and norms, specific to age and sex, exploring pros and cons of the consumption of mind‐altering substances while eliciting ‘change talk', and using the CRAFFT questions and a Readiness to Change ruler to reinforce movement toward behaviour change; generating a menu of options; calling up assets and instilling hope; discussing the challenges of change; and ending in a prescription for change generated by the subject and referrals to community drug treatment services Duration: 20‐30 min structured conversation; 5‐10 min booster phone call Control: alternative intervention |
|
| Outcomes |
Outcomes: number of drinks per day; drinking days per month; maximum drinks per drinking occasion; alcohol problems Measures: Timeline Followback; Adolescent Injury Checklist; Adolescent Health Behavior Questionnaire; Drinking and Driving Scale |
|
| Funding and Declared Conflicts of Interest | Funded by NIAAA. No information or declarations about potential conflicts of interest | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was based on computer‐generated lists, blocked to balance assignment after every 9 subjects and stratified by age group (14–17 and 18–21 years) |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Attrition 28%. Attrition was not related to intervention group or to any of the outcome, moderator or mediator variables |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to intervention. Insufficient information to permit judgement about blinding of therapist |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Unit of Analysis issues | Low risk | Not applicable |
Borsari 2000.
| Methods |
Design: RCT Follow‐up: 6 weeks Attrition: 1.7% |
|
| Participants |
Mean age (years): 18.58 Sex: 57% female N participants: 60 Allocation: n = 29 intervention; n = 31 control Setting: college campus setting with risky drinkers Country: USA |
|
| Interventions |
Programme type: motivational interviewing Set‐up: single individual session Key components: feedback with social norms, personal negative consequences; discussion of expectancies, risks and benefits for decisional balance; challenge to misconceptions about drinking Duration: 1 h Control: assessment only |
|
| Outcomes |
Outcomes: number of drinks consumed per week; number of times consuming alcohol in past week; drinking problems; frequency of binge drinking past month Measures: Drinking Norms Rating Form; Daily Drinking Questionnaire; Rutgers Alcohol Problems Inventory; Cognitive Appraisal of Risky Events |
|
| Funding and Declared Conflicts of Interest | No information | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The investigators describe a random component in the sequence generation |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition 1.7% |
| Selective reporting (reporting bias) | Low risk | All expected outcomes reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to intervention. Insufficient information to make a judgement about blinding of therapists |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to make a judgement |
| Unit of Analysis issues | Low risk | Not applicable |
Borsari 2005.
| Methods |
Design: RCT Follow‐up: 3 and 6 months Attrition: 11% |
|
| Participants |
Mean age (years): 19.1 Sex: 35% female N participants: 64 Allocation: n = 34 intervention; n = 30 control Setting: college campus seeting with students mandated for alcohol violation Country: USA |
|
| Interventions |
Programme type: motivational interviewing Set‐up: individual single session Key components: education and normative feedback Duration: 62 min on average Control: alternative intervention |
|
| Outcomes |
Outcomes: number of drinks consumed per week; frequency of binge drinking in the past 30 days; typical blood alcohol content; peak blood alcohol content; alcohol‐related problems Measures: Alcohol Use Disorders Identification Test; Alcohol and Drug Use Measure; Drinking Norms Rating Form; Inventory of Drinking Situations; binge‐drinking measure; Blood Alcohol Concentration; Rutgers Alcohol Problem Index |
|
| Funding and Declared Conflicts of Interest | Funded by NIAAA. No information or declarations about potential conflicts of interest | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to make a judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition 11% and attrition analyses revealed no baseline differences between participants who completed the study and those who did not or between participants who completed 1 versus 2 follow‐ups |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to intervention. Insufficient information to permit judgement about blinding of therapist |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to make a judgement |
| Unit of Analysis issues | Low risk | Not applicable |
Borsari 2012.
| Methods |
Design: RCT Follow‐up: 3, 6, and 9 months Attrition: 471 out of 505 (93%) eligible participants completed the 3‐month follow‐up; 468 out of 505 (89%) eligible participants completed the 6‐month assessment; and 473 out of 505 (94%) eligible participants completed their 9‐month assessment |
|
| Participants |
Mean age (years): 18.68 Sex: 33% female N participants: 405 Allocation: n = 211 intervention; n = 194 control Setting: college campus with students mandated for alcohol violation Country: USA |
|
| Interventions |
Programme type: brief motivational interviewing Set‐up: individual single session Key components: At the beginning of the BMI, the participant was given a personalised report that provided feedback from the participant’s responses to the baseline and 6‐week follow‐up. The participant then engaged in a discussion of topics such as normative quantity/frequency of drinking, BAC and tolerance, alcohol‐related onsequences (reported at baseline and also the recent 6‐week assessment), influence of setting on drinking, and alcohol expectancies. Throughout the BMI, interventionists followed the 4 principles of Motivational Interviewing (MI): express empathy, develop discrepancy, roll with resistance, and support self efficacy for change Duration: BMIs averaged 52.5 min (SD = 12.12). Control: alternative intervention |
|
| Outcomes |
Outcomes: Alcohol use: number of heavy drinking episodes; number of drinks prior to the citation event and the maximum number of drinks, amount of time spent drinking for each of those episodes; peak and event BAC; alcohol‐related problems Measures: Alcohol and Drug Use Measure (Borsari & Carey, 2000, 2005); Young Adult Alcohol Consequences Questionnaire (YAACQ; Read, Kahler, Strong, & Colder, 2006) |
|
| Funding and Declared Conflicts of Interest | Brian Borsari’s contribution to this manuscript was supported by National Institute on Alcohol Abuse and Alcoholism Grants R01‐AA015518 and R01‐AA017874. Nadine Mastroleo and John T.P. Hustad’s contribution to this manuscript was supported by the National Institute on Alcohol Abuse and Alcoholism grant T32 AA07459. Peter Monti’s contribution was sponsored by a Senior Research and Mentoring K05AA19681 | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Urn randomisation using sex and race as blocking variables, to assign these participants to the BMI or an assessment‐only control |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition < 20%. All participants, including those with missing data, were included in these analyses |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to intervention. Insufficient information to permit judgement about blinding of therapist |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to make a judgement |
| Unit of Analysis issues | Low risk | Not applicable |
Butler 2009.
| Methods |
Design: RCT Follow‐up: 4 weeks Attrition: 19.2% |
|
| Participants |
Mean age (years): 20.2 Sex: 65.3% female N participants: 84 (3 groups) Allocation: n = 28 intervention; n = 26 control Setting: undergraduate students at risk of alcohol problems Country: USA |
|
| Interventions |
Programme type: brief personalised feedback and motivational interviewing Set‐up: individual single session Key components: feedback of assessment results: corrective feedback regarding normative drinking on campus; sex‐specific percentile rank comparing participant’s alcohol consumption to campus norms; review of the participant’s binge drinking frequency and related consequences; didactic information on blood alcohol concentration (BAC), including the behavioural effects and potential legal consequences associated with specific BAC levels; personalised BAC curve for typical and heavy drinking occasions; review of the participant’s reported alcohol‐related problems with a sex‐specific percentile rank comparing severity of alcohol‐related problems to campus norms; review of participants' time allocation across alcohol‐related and alcohol‐free activities (e.g. studying, exercise); weekly and estimated yearly consumption of calories consumed from alcohol; weekly, monthly, and yearly money spent on alcohol; review of harm‐reduction strategies; review of on‐ and off‐campus mental health and alcohol treatment resources Duration: 41 min (average) Control: Did not receive any feedback during the duration of the study |
|
| Outcomes |
Outcomes: drinking occasions; binge episodes; drinkers per week; Rutgers Alcohol Problems Index (RAPI) score Measures: Daily drinking questionnaire; RAPI; questionnaire to measure the acceptability of the intervention |
|
| Funding and Declared Conflicts of Interest | No information | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random assignment was assured by randomised block design to separately randomise male and female participants |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 19.2% attrition rate |
| Selective reporting (reporting bias) | High risk | All alcohol outcomes not reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to intervention. Insufficient information to make judgement about blinding of therapists |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Follow‐up was not carried out by an interviewer blind to the treatment condition |
| Unit of Analysis issues | Low risk | Not applicable |
Carey 2006.
| Methods |
Design: RCT Follow‐up: 1 month, 6 months, 12 months Attrition: 22% |
|
| Participants |
Mean age (years): 19.2 Sex: 65% female N participants: 509 Allocation: n = 87 TLFB basic BMI; n = 86 enhanced BMI intervention; n = 89 TLFB control; n = 85 basic BMI; n = 81 enhanced BMI; n = 81 control Setting: college campus, all students Country: USA |
|
| Interventions |
Programme type: brief motivational interviewing Set‐up: individual single session Key components: drinking norms, consequences, strategies Duration: not stated Control: assessment only |
|
| Outcomes |
Outcomes: typical drinking; risky drinking; heavy drinking; blood alcohol concentration; drink‐related problems Measures: modified Daily Drinking Questionnaire; Rutgers Alcohol Problem Index |
|
| Funding and Declared Conflicts of Interest | Funded by NIAAA. No information or declarations about potential conflicts of interest | |
| Notes | Basic BMI and control conditions included in MA | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to make a judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a judgement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Attrition 22% |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to intervention. Insufficient information to make a judgement about blinding of therapists |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | RAs conducting assessments were always different from those conducting interventions, but were not blind to condition |
| Unit of Analysis issues | Low risk | Not applicable |
Carey 2009.
| Methods |
Design: RCT Follow‐up: 1, 6, and 12 months Attrition: 97% of the 198 students provided data at 1 month, 73% provided data at 6 months, and 70% provided data at 12 months |
|
| Participants |
Mean age (years): 19.17 Sex: 46% female N participants: 198 Allocation: n = 99 BMI; n = 99 Alcohol 101 Plus Setting: university campus with students mandated for alcohol violation Country: USA |
|
| Interventions |
Programme type: brief motivational interviewing Set‐up: individual single session Key components: personalised feedback and alcohol education to prompt exploration of options for reducing risks related to alcohol use Duration: average of 50 min (SD 13.11) Control: Alcohol 101 Plus |
|
| Outcomes |
Outcomes: alcohol use: drinking during a typical week and the heaviest drinking week in the month before the sanction event. maximum number of drinks consumed in a single day and the number of hours spent drinking on that day. peak BAC, frequency of heavy drinking in the month before the sanction event, number of standard drinks consumed on the day of the sanction; alcohol problems: harmful or hazardous alcohol Measures: Daily Drinking Questionnaire; Rutgers Alcohol Problem Index |
|
| Funding and Declared Conflicts of Interest | National Institute on Alcohol Abuse and Alcoholism Grant R01‐AA12518 to Kate B. Carey | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Used random numbers table |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a judgement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Attrition 30% at 12 months. A stepwise discriminant function analysis revealed no discrimination (prediction) between completers and drop‐outs for any of the pre‐sanction drinking variables measured at the baseline assessment |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to intervention. Insufficient information to make a judgement about blinding of therapists |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Assessment RAs were different staff from those conducting interventions but were not blind to condition |
| Unit of Analysis issues | Low risk | Not applicable |
Carey 2011.
| Methods |
Design: RCT Follow‐up: 1, 6, 12 months Attrition: 32% |
|
| Participants |
Mean age (years): 19 Sex: 64% male N participants: 677 Allocation: n = 164 BMI; n = 172 Alcohol 101; n = 167 AlcoholEdu; n = 174 control Setting: college with students mandated for alcohol violation Country: USA |
|
| Interventions |
Programme type: brief motivational interviewing Set‐up: individual single session Key components: social norms, consequences, goal setting Duration: 1 h Control: assessment only at 1 month; Alcohol 101 at 6 and 12 months |
|
| Outcomes |
Outcomes: quantity, binge drinking; alcohol problems; blood alcohol concentration Measures: Daily Drinking Questionnaire; Rutgers Alcohol Problems Index |
|
| Funding and Declared Conflicts of Interest | Funded by NIAAA. Authors declare no conflicts of interest | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Referred students were assigned randomly by sex to 1 of 4 conditions. Insufficient information to make a judgement |
| Allocation concealment (selection bias) | High risk | Insufficient information to make a judgement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Attrition 32% |
| Selective reporting (reporting bias) | Low risk | All outcomes communicated to reviewers |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to intervention |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to make a judgement |
| Unit of Analysis issues | Low risk | Not applicable |
Carey 2013a.
| Methods |
Design: RCT Follow‐up: 1, 2 months Attrition: 95% provided data at 1 month and 79% provided at 2 months |
|
| Participants |
Mean age (years): 18.60 Sex: 60% male N participants: 141 Allocation: n = 74 alcohol 101; n = 67 BMI Setting: college with students mandated for alcohol violation Country: USA |
|
| Interventions |
Programme type: brief motivational interviewing Set‐up: individual single session Key components: interventionists provided a personalised feedback sheet that summarised drinking patterns (contrasted with sex‐specific national and local norms) and estimated typical and peak BAC, alcohol‐related negative consequences, and associated risk behaviours; interventionists also elicited personalised goal‐setting for risk reduction and provided tips for safer drinking. The BMI was administered with a collaborative, supportive, yet directive style, consistent with motivational interviewing Duration: approximately 1 h Control: alcohol 101 |
|
| Outcomes |
Outcomes: alcohol use: quantity and time spent drinking for their heaviest drinking night; peak BAC; alcohol problems: harmful or hazardous alcohol use in the last year; frequency of alcohol‐related problems in the last month Measures: Daily Drinking Questionnaire; Alcohol Use Disorders Identification Test; Brief Young Adult Alcohol Consequences Questionnaire |
|
| Funding and Declared Conflicts of Interest | Supported in part by NIAAA Grant R01‐AA012518 and K02‐AA015574 to Kate B. Carey | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to make a judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a judgement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 21% at 2 months follow‐up |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to intervention. Insufficient information to make a judgement about blinding of therapists |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Research Assistants who provided the instructions for the online assessments were different than those who conducted interventions |
| Unit of Analysis issues | Low risk | Not applicable |
Ceperich 2011.
| Methods |
Design: RCT Follow‐up: 1.4 months Attrition: 9% |
|
| Participants |
Mean age (years): 21 Sex: 100% female N participants: 228 Allocation: n = 114 intervention; n = 114 control Setting: university students at risk of pregnancy Country: USA |
|
| Interventions |
Programme type: motivational interviewing Set‐up: individual single session Key components: motivational interviewing plus feedback Duration: 60‐75 min Control: assessment only |
|
| Outcomes |
Outcomes: age first alcoholic drink; most standard drinks 1 day; binges past month/past 3 months; average drinks per day; average drinks per week; had blackouts; thought should cut down on drinking Measures: BALANCE Core Assessment |
|
| Funding and Declared Conflicts of Interest | Funded co‐operatively by AAMC, CDC and Virginia Commonwealth University. Also funded by NIH. Authors declare that funders had no influence. | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to make judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make judgement: "randomization envelope" mentioned but no details |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 9% attrition. Intention‐to‐treat analysis performed |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to intervention. Insufficient information to make a judgement about blinding of therapists |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to make judgement |
| Unit of Analysis issues | Low risk | Not applicable |
Christoff 2015.
| Methods |
Design: RCT Follow‐up: 3 months Attrition: 25% |
|
| Participants |
Mean age (years): 24 Sex: 43% male N participants: 333 Allocation: 234 to 2 BMI conditions; 99 control Setting: college campus with students identified as higher risk Country: Brazil |
|
| Interventions |
Programme type: motivational interviewing Set‐up: individual single session, either computer or counsellor delivered Key components: motivational interview Duration: 5‐20 min Control: alternative intervention: given feedback on ASSIST scores |
|
| Outcomes |
Outcomes: different substance use patterns detected by the ASSIST: low risk: occasional or non‐harmful use (scores 0–10 for alcohol or 0–3 for other substances); moderate risk: more regular use or harmful/hazardous use (scores 11–26 for alcohol or 4–26 for other substances); high risk: frequent high‐risk use or suggestive of dependence (scores ≥ 27 for all substances) Measures: ASSIST risky/problem drinking scale |
|
| Funding and Declared Conflicts of Interest | No external funding was provided for the study. Authors declared no conflicts of interest. | |
| Notes | Results pooled across 2 BMI conditions and sexes, for comparison with control in MA | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 25% attrition, though no evidence of differential attrition |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Students were not blind. The delivery was blind in 1 condition (computer‐based) |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information |
| Unit of Analysis issues | Low risk | Not applicable |
Cimini 2009.
| Methods |
Design: RCT Follow‐up: 6 months Attrition: 31% |
|
| Participants |
Mean age (years): not stated; college students Sex: 62.2% male N participants: 685 Allocation: not reported Setting: college campus with students mandated for alcohol violation Country: USA |
|
| Interventions |
Programme type: motivational interviewing Set‐up: group single session Key components: discussion focused on evaluation of alcohol consumption and associated problems Duration: 2 h Control: alternative intervention |
|
| Outcomes |
Outcomes: peak number of drinks on 1 occasion; average number of drinks per week; alcohol problems Protective behavioural strategies (possible mediator) Measures: Daily Drinking Questionnaire; Rutgers Alcohol Problem Index; Protective Behaviors Strategies Scale |
|
| Funding and Declared Conflicts of Interest | Funded by NIAAA. No information or declarations about potential conflicts of interest | |
| Notes | No significant effects of intervention found, but insufficient information to include in meta‐analysis. Authors contacted for further information on group size, means and standard deviations for all outcomes | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information about the sequence generation process to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a judgement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 31% attrition |
| Selective reporting (reporting bias) | Low risk | All expected outcomes were reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to intervention. Insufficient information to make a judgement about blinding of therapists |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to make a judgement |
| Unit of Analysis issues | Low risk | Not applicable |
Clair 2013.
| Methods |
Design: RCT Follow‐up: 3 months Attrition: 22% |
|
| Participants |
Mean age (years): 17.12 Sex: 86% male N participants: 147 Allocation: not reported Setting: state juvenile correctional facility; higher risk young adults Country: USA |
|
| Interventions |
Programme type: motivational interviewing Set‐up: individual single session + booster Key components: principles of MI were the basis of the intervention protocol. The protocol included developing rapport, exploration of motivation (pros and cons), personalised assessment feedback, imagining the future with and without change, and establishing goals at booster Duration: 90 min at baseline and about 60 min at booster Control: alternative intervention |
|
| Outcomes |
Outcomes: total number of drinks on heavy drinking days (NDHD) and percentage of heavy drinking days (PHDD) Measures: Timeline Followback |
|
| Funding and Declared Conflicts of Interest | Funded by NIAAA and NIDA. No information or declarations about potential conflicts of interest | |
| Notes | Not included in the MA: insufficient information in the published paper. Author contacted for more details | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was accomplished via random numbers table in advance |
| Allocation concealment (selection bias) | High risk | "[P]laced in an envelope by the project coordinator. Following baseline assessment, treatment providers opened the envelope to learn of intervention assignment" |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Attrition 22% |
| Selective reporting (reporting bias) | Low risk | All alcohol outcomes reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to intervention. Insufficient information to make a judgement about blinding of therapists |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Research staff blind to treatment assignment conducted a follow‐up assessment 3 months after release from the facility |
| Unit of Analysis issues | Low risk | Not applicable |
Clinton‐Sherrod 2011.
| Methods |
Design: RCT Follow‐up: 3 months Attrition: 0% attrition implied |
|
| Participants |
Age (years): First‐year female college students, most aged 18 Sex: 100% female N participants:229 Allocation: not reported Setting: university, all students Country: USA |
|
| Interventions |
Programme type: motivatonal interviewing Set‐up: individual single session Key components: empathic therapist style, helping participants perceive a discrepancy between their goals and their drinking, eliciting self motivational statements from participants, and discussing alternatives for aiding in changing drinking behaviour Duration: not stated Control: alternative intervention |
|
| Outcomes |
Outcomes: number of drinks on drinking occasions during past month; average number of drinks that participants had on drinking days during the past 30 days; number of days drinking; average number of drinks per drinking occasion; number of heavy episodic drinking days Measures: Young Adult Alcohol Problems Screening Test |
|
| Funding and Declared Conflicts of Interest | Funded by NIAAA. Authors declare no conflicts of interest | |
| Notes | Study results not in right format for MA; authors contacted | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to make a judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 0% implied, but not directly stated. Insufficient information to make a judgement |
| Selective reporting (reporting bias) | Low risk | All pre‐specified outcomes reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to intervention. Insufficient information to make a judgement about blinding of therapists |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to make a judgement |
| Unit of Analysis issues | Low risk | Not applicable |
D'Amico 2008.
| Methods |
Design: RCT Follow‐up: 3 months Attrition: 34% |
|
| Participants |
Mean age (years): 16 Sex: 47.6% male N participants: 64 Allocation: n = 38 intervention; n = 26 control Setting: community‐based health care clinic with higher risk youth Country: USA |
|
| Interventions |
Programme type: motivational interviewing Set‐up: individual single session Key components: not described in paper Duration: 15‐20 min; booster session phone call 5‐10 min Control: assessment only |
|
| Outcomes |
Outcomes: intention to use; perceived prevalence; number of friends who drink; how often with teens who drink; alcohol consequences; number of daysdrinking; how many drinks consumed; number of days consumed 3 + drinks Measures: Rutgers Alcohol Problem Index; CRAFFT screen for youth alcohol consumption; alcohol consequences from DSM IV |
|
| Funding and Declared Conflicts of Interest | No information | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Initially, youth were randomised on a 1‐to‐1 basis; that is, the probability of being assigned to either group was equal. However, as the trial progressed, investigators recognised that dropout rates were unequal between the groups, with youth from the intervention group less likely to be followed up. Thus, to maximise power, the allocation schedule was altered such that the probability of being allocated to the intervention group was higher |
| Allocation concealment (selection bias) | High risk | Inadequate ‐ higher rate of dropout from intervention so altered allocation schedule with higher probability of allocation to intervention group |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Attrition 34%. Sensitivity analysis showed that data were missing at random and not substantively different from complete case analysis so only reported complete case results |
| Selective reporting (reporting bias) | Low risk | All outcomes stated in Methods reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to intervention. Insufficient information to make a judgement about blinding of therapists |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to make a judgement |
| Unit of Analysis issues | Low risk | Not applicable |
D'Amico 2013.
| Methods |
Design: RCT Follow‐up: 3 months Attrition: 3% |
|
| Participants |
Mean age (years): 16.6 mean age at baseline Sex: 67% male N participants: 193 Allocation: n = 113 intervention; n = 80 control Setting: teen court referrals (for alcohol or marijuana offence); higher risk Country: USA |
|
| Interventions |
Programme type: motivational interviewing Set‐up: group based; 6 sessions Key components: group motivational interviewing; all sessions delivered using an MI approach Duration: each session 50‐55 min Control: usual care: 6 sessions of abstinence‐oriented AA approach |
|
| Outcomes |
Outcomes: frequency of drinking, binge drinking and alcohol‐related consequences Measures: from RAND adolescent panel study; consequences from questions based on DSM‐IV criteria |
|
| Funding and Declared Conflicts of Interest | Funded by NIDA. No information or declarations about potential conflicts of interest | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low attrition (3%) |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to intervention. Insufficient information to make a judgement about blinding of therapists |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information |
| Unit of Analysis issues | Low risk | Not applicable |
Daeppen 2011 HED.
| Methods |
Design: RCT Follow‐up: 6 months Attrition: 21.4% |
|
| Participants |
Mean age (years): 19.9 Sex: 100% male N participants: 271 Allocation: n = 125 intervention; n = 146 control Setting: army recruitment, binge drinkers Country: Switzerland |
|
| Interventions |
Programme type: brief motivational interviewing Set‐up: single individual sessions Key components: the strategies included were: opening strategy exploring lifestyle, general alcohol use, alcohol use within a typical day/session, then focusing on the hypothesis of a reduction in alcohol use among binge drinkers or on the status quo among non‐binge drinkers; focusing on the pros and cons of alcohol use; evoking hypothetical changes in drinking patterns; exploring importance, ability, and confidence to change; and eliciting commitment to change and identification of a hypothetical change Duration: 15.8 (± 5.5) min Control: assessment only |
|
| Outcomes |
Outcomes: the typical number of drinks per week (standard drink containing about 10 g of pure alcohol); and the typical number of binge drinking episodes per month (defined as an occasion with 6 drinks or more, where 6 drinks contain approximately 60 g of pure alcohol and equal to the most common measure of 5 or more drinks of 12 g per drink. Bingers were defined as subjects with typical binge drinking once a month or more. Measures: Alcohol Use Disorder Identification Test (AUDIT); the importance, readiness and confidence to change scales; Alcohol use was assessed using the 2 drinking outcome measures and a list of 12 alcohol‐related problems usually experienced by young heavy drinkers |
|
| Funding and Declared Conflicts of Interest | The study was funded by the “Dîme de l’alcool du Canton de Vaud” and declaration of conflicts of interest presented in the paper | |
| Notes | The paper reports results separately for binge and non‐binge drinkers. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | ". . . a priori randomization of conscripts to the intervention and the control groups" |
| Allocation concealment (selection bias) | Unclear risk | Insufficent information |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Attrition 21.4% |
| Selective reporting (reporting bias) | Low risk | All alcohol outcomes reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to intervention |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to make a judgement |
| Unit of Analysis issues | Low risk | Not applicable |
Daeppen 2011 non‐HED.
| Methods |
Design: RCT Follow‐up: 6 months Attrition: 7.5% |
|
| Participants |
Mean age (years): 19.9 Sex: 100% male N participants: 147 Allocation: n = 74 intervention; n = 73 control Setting: army recruitment, non‐binge drinkers (lower risk) Country: Switzerland |
|
| Interventions |
Programme type: brief motivational interviewing Set‐up: single individual sessions Key components: the strategies included were: opening strategy exploring lifestyle, general alcohol use, alcohol use within a typical day/session, then focusing on the hypothesis of a reduction in alcohol use among binge drinkers or on the status quo among non‐binge drinkers; focusing on the pros and cons of alcohol use; evoking hypothetical changes in drinking patterns; exploring importance, ability, and confidence to change; and eliciting commitment to change and identification of a hypothetical change Duration: 15.8 (±5.5) min Control: assessment only |
|
| Outcomes |
Outcomes: the typical number of drinks per week (standard drink containing about 10 g of pure alcohol); and the typical number of binge drinking episodes per month (defined as an occasion with 6 drinks or more, where 6 drinks contain approximately 60 g of pure alcohol and equal to the most common measure of 5 or more drinks of 12 g per drink (Gmel et al.,
2003)). Bingers were defined as subjects with typical binge drinking once a month or more. Measures: Alcohol Use Disorder Identification Test (AUDIT); the importance, readiness and confidence to change scales; Alcohol use was assessed using the 2 drinking outcome measures and a list of 12 alcohol‐related problems usually experienced by young heavy drinkers |
|
| Funding and Declared Conflicts of Interest | The study was funded by the “Dîme de l’alcool du Canton de Vaud” and declaration of conflicts of interest presented in the paper | |
| Notes | The paper reports results separately for binge and non‐binge drinkers. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | ."..a priori randomization of conscripts to the intervention and the control groups." |
| Allocation concealment (selection bias) | Unclear risk | Insufficent information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Atrrition 7.5% |
| Selective reporting (reporting bias) | Low risk | All alcohol outcomes reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to intervention |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to make a judgement |
| Unit of Analysis issues | Low risk | Not applicable |
Dermen 2011.
| Methods |
Design: RCT Follow‐up: 3, 6, 9, 12, and 15 months Attrition: 9% |
|
| Participants |
Mean age (years): 20.7 Sex: 59% female N participants: 154 Allocation: n = 39 alcohol risk intervention; n = 39 HIV risk intervention; n = 36 alcohol + HIV risk intervention; n = 40 control Setting: college students, all levels of risk Country: USA |
|
| Interventions |
Programme type: motivational interviewing Set‐up: 2 individual sessions Key components: create an awareness of the need for change, increase participants’ motivation to make a change, and discuss plans for change Duration: first session approximately 45 min; second session approximately 30 min Control: assessment only |
|
| Outcomes |
Outcomes: alcohol use and sexual behaviour during the prior 90 days; number of standard drinks per week; estimated blood alcohol concentration peaks in a typical week and on a heavier day of drinking; levels of risk associated with tolerance; other drug use, and family history; levels of lifetime and recent consequences of alcohol use; thoughts about cutting down Measures: modified Timeline Followback; Young Adult Alcohol Problems Screening Test; Readiness to Change Questionnaire |
|
| Funding and Declared Conflicts of Interest | Funded by NIAAA. No information or declarations about potential conflicts of interest | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Project director used a random number table |
| Allocation concealment (selection bias) | Unclear risk | Series of random assignment envelopes, but not stated whether opaque |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low attrition (9%) at 15‐month follow‐up. Participants who were missing outcome data from any follow‐up point were dropped from outcome analyses. Follow‐up completion rates for the 3‐, 6‐, 9‐, 12‐, and 15‐month windows were 95%, 94%, 92%, 91%, and 91%, respectively, and did not differ significantly by condition |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants. Counsellors were blind to condition assignment until after completion of the intake interview |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Follow‐up assessments were conducted by same‐sex interviewers blind to experimental condition |
| Unit of Analysis issues | Low risk | Not applicable |
Doumas 2008.
| Methods |
Design: RCT Follow‐up: 30 days Attrition: 37% |
|
| Participants |
Age (years): not stated: inclusion age 18‐24 Sex: 73% female N participants: 196 Allocation: n = 60 web‐based intervention; n = 63 web‐based intervention + MI intervention; n = 73 control Setting: local companies, all young people Country: USA |
|
| Interventions |
Programme type: web‐based intervention combined with motivational interviewing Set‐up: individual single session Key components: web feedback including normative and motivational interviewing Duration: 15 min + feedback Control: assessment only |
|
| Outcomes |
Outcomes: drinking quantity; peak consumption; frequency of drinking to excess; binge drinking Measures: Daily Drinking Questionnaire |
|
| Funding and Declared Conflicts of Interest | Funded by SAMHSA. No information or declarations about potential conflicts of interest | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to make a judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a judgement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Only 63% returned for the 30‐day follow‐up assessment. No differences found in drinking variables or other characteristics across those who completed the study versus those who did not complete the follow‐up assessment. Additionally, attrition rates were similar across the study groups, suggesting that attrition was not related to a specific study condition |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to intervention. Insufficient information to make a judgement about blinding of therapists |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to make a judgement |
| Unit of Analysis issues | Low risk | Not applicable |
Doumas 2011.
| Methods |
Design: RCT Follow‐up: 8 months Attrition: 38.5% |
|
| Participants |
Mean age (years): 19.07 Sex: 70% male N participants: 135 Allocation: not reported Setting: college students mandated for alcohol violation Country: USA |
|
| Interventions |
Programme type: web‐based programme (e‐CHUG) with review of their feedback in an MI Set‐up: individual single session Key components: web feedback including normative and motivational interviewing Duration: 30 min Control: web‐based assessment with self guided personalised normative feedback |
|
| Outcomes |
Outcomes: alcohol consumption: weekly drinking quantity, binge drinking frequency, and peak alcohol consumption. Typical quantity of weekly drinking; alcohol‐related consequences Measures: Daily Drinking Questionnaire; Rutgers Alcohol Problem Index |
|
| Funding and Declared Conflicts of Interest | No statement on funding or conflicts of interest | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random numbers table used |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a judgement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | High attrition (38.5%) There was no difference in the rate of attrition across the 2 intervention groups, Chi2 = 1.15, P = 0.19. In addition, a series of Chi2 and T tests revealed no differences in demographic variables or in any of the drinking variables between the participants who completed the study and those who did not, with the exception of binge drinking frequency. Participants who completed the study reported a higher frequency of binge drinking (M 1.45, SD 1.51) than those who did not complete the study (M = 0.89, SD 1.26) |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to intervention. Insufficient information to make a judgement about blinding of therapists |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to make a judgement |
| Unit of Analysis issues | Low risk | Not applicable |
Ewing 2009.
| Methods |
Design: RCT Follow‐up: 30 days Attrition: 10.6% |
|
| Participants |
Mean age (years): 21.72 Sex: 67.14% male N participants: 75 Allocation: not reported Setting: college campus, all students Country: USA |
|
| Interventions |
Programme type: motivational enhancement therapy Set‐up: single session individual Key components: focus on ambivalence, exploring strategies Duration: 45 min Control: assessment only |
|
| Outcomes |
Outcomes: motivation to change; number of drinks; number of drinking days; number of heavy drinking days; taking steps to reduce alcohol consumption Measures: Alcohol Use Disorders Identification Test; Rutgers Alcohol Problem Index; Timeline Followback; Stages of Change Readiness and Treatment Eagerness Scale |
|
| Funding and Declared Conflicts of Interest | Funded by NIAAA. No information or declarations about potential conflicts of interest | |
| Notes | Study results not in right format for MA; authors contacted | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to make a judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low attrition; 10.6% of participants did not complete the study |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to intervention. Insufficient information to make a judgement about blinding of therapists |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to make a judgement |
| Unit of Analysis issues | Low risk | Not applicable |
Faris 2005.
| Methods |
Design: RCT Follow‐up: 30 days Attrition: 2.6% |
|
| Participants |
Mean age (years): 19.61 Sex: 54% female N participants: 76 Allocation: n = 37 intervention; n = 37 control Setting: College, higher risk students Country: USA |
|
| Interventions |
Programme type: motivational interviewing Set‐up: individual single session Key components: discussion of alcohol use; consequences; strategies Duration: 45 min Control: alternative intervention |
|
| Outcomes |
Outcomes: alcohol use past 30 days; frequency; quantity; readiness to change Measures: Decisional Balance for Immoderate Drinking; Stages Of Change Readiness And Treatment Eagerness Scale; Process of Change Questionnaire; Self Efficacy Questionnaire |
|
| Funding and Declared Conflicts of Interest | No information. No information or declarations about potential conflicts of interest | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to make a judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low attrition (2.6%) |
| Selective reporting (reporting bias) | Low risk | All expected outcomes reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to intervention. Insufficient information to make a judgement about blinding of therapists |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to make a judgement |
| Unit of Analysis issues | Low risk | Not applicable |
Feldstein 2007.
| Methods |
Design: RCT Follow‐up: 2 months Attrition: 7% |
|
| Participants |
Mean age (years): 18.6 Sex: 78.2% female N participants: 55 Allocation: n = 40 intervention; n = 15 control Setting: college campus with higher risk students Country: USA |
|
| Interventions |
Programme type: motivational interviewing Set‐up: single individual session Key components: MI with option of general info on alcohol use Duration: 45 min Control: assessment only |
|
| Outcomes |
Outcomes: binge drinking; alcohol‐related problems Measures: Rutgers Alcohol Problem Index; modification of Monitoring the Future study; Working Alliance Inventory; Motivational Interview Treatment Integrity coding system |
|
| Funding and Declared Conflicts of Interest | Funded by University Graduate funding scheme. No information or declarations about potential conflicts of interest | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Using a Statistical Package for the Social Sciences random numbers list |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low attrition (7%) |
| Selective reporting (reporting bias) | Low risk | All expected outcomes reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to intervention. Insufficient information to make a judgement about blinding of therapists |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Undergraduate assistants blind to randomisation collected follow‐up data |
| Unit of Analysis issues | Low risk | Not applicable |
Fleming 2010.
| Methods |
Design: RCT Follow‐up: 6, 12 months Attrition: 12 % |
|
| Participants |
Mean age (years): 21 Sex: 49% male N participants: 986 Allocation: n = 493 intervention; n = 493 control Setting: college health clinics, higher risk students Country: USA and Canada |
|
| Interventions |
Programme type: brief motivational interviewing Set‐up: 2 individual sessions Key components: contracting and goal‐setting, diary cards and take‐home exercises Duration: 15 min each Control: assessment only |
|
| Outcomes |
Outcomes: number of drinks last 28 days; number of heavy drinking days; number of drinking days last 28 days; alcohol related problems; urgent health care utilisation; health status measures ‐ depression, smoking, injuries, violence Measures: Timeline Followback; Rutgers Alcohol Problem Index |
|
| Funding and Declared Conflicts of Interest | Funded by NIAAA. No information or declarations about potential conflicts of interest | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation achieved using a computer‐generated allocation method |
| Allocation concealment (selection bias) | Low risk | No identifiers available to recognise controls |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition 12%. Intention‐to‐treat analysis |
| Selective reporting (reporting bias) | Low risk | All expected outcomes reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding only occurred in the control condition: One of the goals of the trial was to blind subjects assigned to the control groups to minimise the intervention effect of the research procedures. The subjects randomised into the control group were told the trial focused on a number of health behaviours, including alcohol. The physicians and their staffs were not told which of their patients were randomised into the control group |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Assessors blinded to group status |
| Unit of Analysis issues | Low risk | Not applicable |
Fromme 2004 MANDATED.
| Methods |
Design: RCT Follow‐up: 1 month Attrition: 15% at 1 month |
|
| Participants |
Mean age (years): 19.26 Sex: 76% male N participants: 124 Allocation: n = 100 intervention; n = 24 control Setting: university, mandated for alcohol violation Country: USA |
|
| Interventions |
Programme type: Lifestyle Management Class (LMC) with brief motivational interviewing components Set‐up: 1 individual session Key components: change in drinking, negative consequences of intoxication, driving after drinking, and motivation for making behavioural changes Duration: 75 min Control: assessment only |
|
| Outcomes |
Outcomes:typical weekly drinking; monitored weekly drinking; heavy drinking composite, DUI composite; past month negative consequences Measures: University of Rhode Island Change Assessment; Daily Drinking Questionnaire; Positive and Negative Consequences Experienced Questionnaire; Drinking after Driving question, Past week monitorisation alcohol card; adherence and quality of the LMC co‐leaders |
|
| Funding and Declared Conflicts of Interest | Research Supported by the National Institute on Alcohol Abuse and Alcoholism. No information or declarations about potential conflicts of interest | |
| Notes | Results combined for professional and peer‐led intervention groups as there were no differences between these groups. Results reported separately for mandated and voluntary groups. Only 1 month outcomes reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to make a judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low attrition (15%); missing cases analyses used |
| Selective reporting (reporting bias) | Low risk | All expected outcomes reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to intervention |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to make a judgement |
| Unit of Analysis issues | Low risk | Not applicable |
Fromme 2004 VOLUNTARY.
| Methods |
Design: RCT Follow‐up: 1, 6 months Attrition: 27% at 1 month and 51% at 6 month |
|
| Participants |
Mean age (years): 19.26 Sex: 59% male N participants: 452 Allocation: not reported, though n = 285 intervention and n = 118 controls were included in the analysis Setting: university, all risk levels Country: USA |
|
| Interventions |
Programme type: Lifestyle Management Class (LMC) with brief motivational interviewing components Set‐up: 1 individual session Key components: change in drinking, negative consequences of intoxication, driving after drinking, and motivation for making behavioural changes Duration: 75 min Control: assessment only |
|
| Outcomes |
Outcomes: typical weekly drinking; monitored weekly drinking; heavy drinking composite, DUI composite; past month negative consequences Measures: University of Rhode Island Change Assessment; Daily Drinking Questionnaire; Positive and Negative Consequences Experienced Questionnaire; Drinking after Driving question, Past week monitorisation alcohol card; adherence and quality of the LMC co‐leaders |
|
| Funding and Declared Conflicts of Interest | Research Supported by the National Institute on Alcohol Abuse and Alcoholism. No information or declarations about potential conflicts of interest | |
| Notes | Results combined for professional and peer‐led intervention groups as there were no differences between these groups. Results reported separately for mandated and voluntary groups. Only 1 month outcomes reported and included in MA | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to make a judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a judgement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | High attrition (27%); missing cases analyses used |
| Selective reporting (reporting bias) | Low risk | All expected outcomes reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to intervention |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to make a judgement |
| Unit of Analysis issues | Low risk | Not applicable |
Gaume 2011 HED.
| Methods |
Design: RCT Follow‐up: 6 months Attrition: 13% |
|
| Participants |
Mean age (years): 19.9 Sex: 100% male N participants: 446 Allocation: n = 296 intervention; n = 276 control Setting: army recruitment, binge drinkers Country: Switzerland |
|
| Interventions |
Programme type: brief motivational interviewing Set‐up: single individual sessions Key components: the strategies included were: opening strategy: lifestyle and alcohol use, alcohol use within a typical day session; the good things and the less good things about drinking alcohol (decisional balance); evoking a hypothetical change; exploring importance, ability, and confidence to change; and eliciting commitment to change, identification of an eventual change, contracting and goal‐setting, diary cards and take‐home exercises Duration: mean length: 21.8 min Control: assessment only |
|
| Outcomes |
Outcomes: number of standard (about 10 g pure alcohol) drinks per week; number of heavy drinking episodes (6 drinks or more on 1 occasion) per month; number of alcohol‐related consequences Measures: Quick Drinking Screen; Alcohol Use Disorder Identification Test |
|
| Funding and Declared Conflicts of Interest | Funded by Swiss Foundation for Alcohol Research. No information provided about potential COI | |
| Notes | HED: baseline heavy episodic drinkers. The results were presented according to this baseline user subgroup | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Conscripts met in groups of 30, therefore 30 playing cards were placed face down on a table (15 linked to BMI and 15 to control conditions), and subjects were instructed to choose 1 of them |
| Allocation concealment (selection bias) | Low risk | Participants could not foresee assignment because 30 playing cards were placed face down on a table |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low attrition (13%). Missing values from cases lost to follow‐up were replaced with their baseline values to account for attrition |
| Selective reporting (reporting bias) | High risk | Not all pre‐specified outcomes are reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to intervention. Insufficient information to make a judgement about blinding of therapists |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | All follow‐up assessments were made by staff blinded to the treatment status |
| Unit of Analysis issues | Low risk | Not applicable |
Gaume 2011 non‐HED.
| Methods |
Design: RCT Follow‐up: 6 months Attrition: 9% |
|
| Participants |
Mean age (years): 19.9 Sex: 100% male N participants: 126 Allocation: n = 77 intervention; n = 49 control Setting: army recruitment, non‐binge drinkers Country: Switzerland |
|
| Interventions |
Programme type: brief motivational interviewing Set‐up: single individual sessions Key components: the strategies included were: opening strategy: lifestyle and alcohol use, alcohol use within a typical day session; the good things and the less good things about drinking alcohol (decisional balance); evoking a hypothetical change; exploring importance, ability, and confidence to change; and eliciting commitment to change, identification of an eventual change, contracting and goal‐setting, diary cards and take‐home exercises Duration: mean length: 21.8 min Control: assessment only |
|
| Outcomes |
Outcomes: number of standard (about 10 g of pure alcohol) drinks per week; number of heavy drinking episodes (6 drinks or more on 1 occasion) per month; number of alcohol‐related consequences Measures: Quick Drinking Screen; Alcohol Use Disorder Identification Test |
|
| Funding and Declared Conflicts of Interest | Funded by Swiss Foundation for Alcohol Research. No information provided about potential COI. | |
| Notes | Non‐HED: baseline non‐heavy episodic drinkers. The results were presented according to this baseline user subgroup | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Conscripts met in groups of 30, therefore 30 playing cards were placed face down on a table (15 linked to BMI and 15 to control conditions), and subjects were instructed to choose 1 of them |
| Allocation concealment (selection bias) | Low risk | Participants could not foresee assignment because 30 playing cards were placed face down on a table |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition 9%. Missing values from cases lost to follow‐up were replaced with their baseline values to account for attrition |
| Selective reporting (reporting bias) | High risk | Not all pre‐specified outcomes are reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to intervention. Insufficient information to make a judgement about blinding of therapists |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | All follow‐up assessments were made by staff blinded to the treatment status |
| Unit of Analysis issues | Low risk | Not applicable |
Gaume 2014.
| Methods |
Design: RCT Follow‐up: 3 months Attrition: 18% |
|
| Participants |
Mean age (years): 19.9 Sex: 100% male N participants: 441 Allocation: n = 217 intervention; n = 224 control Setting: army recruitment with higher risk recruits Country: Switzerland |
|
| Interventions |
Programme type: brief motivational interviewing Set‐up: single individual sessions Key components: BMI addressing alcohol use, its related consequences, and per client agreement, eventual change perspectives. Duration: 20‐30 min Control: assessment only |
|
| Outcomes | Outcomes: usual number of drinking days per week, usual number of drinks (defined as 10 g of alcohol) per drinking day, and frequency of binge drinking episodes (6 drinks or more) over the last year. Additional measures were as follows: a 9‐item questionnaire assessing the occurrence of a series of alcohol‐related consequences experienced over the last 12 months (e.g. argue with friends, miss a class, engage in unplanned sexual activity, get into trouble with police); the Alcohol Use Disorder Identification Test (AUDIT) with a cutoff of 12 for probable dependence; and the University of Rhode Island Change Assessment Scale – DELTA Project Reduced Drinking Version | |
| Funding and Declared Conflicts of Interest | Funded by Swiss National Science Foundation. No information provided about potential COI | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low attrition (18%) |
| Selective reporting (reporting bias) | High risk | Not all outcomes reported, only q‐f and binge results |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to intervention. Insufficient information to make a judgement about blinding of therapists |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Follow‐up assessment coders were blind to study condition |
| Unit of Analysis issues | Low risk | Not applicable |
Gmel 2013.
| Methods |
Design: RCT Follow‐up: 6 months Attrition: 20.4% |
|
| Participants |
Mean age (years): 20.1 Sex: 100% male N participants: 853 Allocation: n = 392 intervention; n = 461 control Setting: army recruitment, all risk levels Country: Switzerland |
|
| Interventions |
Programme type: brief motivational interviewing Set‐up: single individual sessions (booster telephone interview at 3 months) Key components: the strategies included were: establish a collaborative rapport to enable elicitation of multiple substance use; ensure confidentiality; ask permission to talk about behaviours; ask with open questions about substance use and focus on areas that the conscript considers problematic; explore pros and cons; reflect and affirm change talk and enhance values that might be incompatible with present substance use; explore the importance, confidence and readiness to change; evoke commitment to a change plan; and support the conscript's self efficacy Duration: 20 min (mean) Control: assessment only |
|
| Outcomes |
Outcomes: % drinkers past 6 months; % risk volume (> 21 drinks/week); % risk RSOD (>once a month); % at risk (either volume or RSOD); number of drinks per week; number of RSOD per month Measures: Quantity‐frequency instrument; Monthly frequency of risky single occasion drinking instrument (RSOD) |
|
| Funding and Declared Conflicts of Interest | No information or declarations about funding or potential conflicts of interest | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "[G]enerated via a computerized randomization algorithm by the research team." |
| Allocation concealment (selection bias) | Low risk | Participants could not foresee assignment |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Borderline low/high risk attrition ‐ rounded down to 20% |
| Selective reporting (reporting bias) | Low risk | All outcomes are reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to intervention |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Follow‐up assessments were made by staff blinded to the treatment status |
| Unit of Analysis issues | Low risk | Not applicable |
Gomez 2013.
| Methods |
Design: RCT Follow‐up: 3 months Attrition: 40.7% |
|
| Participants |
Mean age (years): 20 Sex: 71% male N participants: 263 Allocation: n = 132 intervention; n = 131 control Setting: hospital emergency department; patients aged 16‐24 who were positive for blood alcohol content (BAC) of 0.5g/L or above Country: France |
|
| Interventions |
Programme type: brief motivational interviewing Set‐up: single individual sessions (booster telephone interview at 1 and 3 months) Key components: motivational interviewing techniques Duration: 45‐90 min Control: practical guide on alcohol |
|
| Outcomes |
Outcomes: quantity of consumption; drunkenness; binge drinking Measures: glasses consumed; how many times drunk in previous period; drank 5 or more glasses in last month |
|
| Funding and Declared Conflicts of Interest | Funded by le Fonds d’Expérimentation pour la Jeunesse. No information on potential conflicts of interest | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information |
| Allocation concealment (selection bias) | Low risk | Envelope randomisation |
| Incomplete outcome data (attrition bias) All outcomes | High risk | > 40% attrition |
| Selective reporting (reporting bias) | Low risk | ALl outcomes reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to intervention |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information |
| Unit of Analysis issues | Low risk | Not applicable |
Goti 2010.
| Methods |
Design: RCT Follow‐up:1 month Attrition: 28% |
|
| Participants |
Mean age (years): 15.2 Sex: 15% male N participants: 143 Allocation: n = 78 intervention; n = 65 control Setting: Child and Adolescent Psychiatry and Psychology Department; higher risk patients Country: Spain |
|
| Interventions |
Programme type: brief motivational interviewing Set‐up: single individual session Key components: The intervention considered altogether 12 points to be discussed during the session: contact, feedback from the evaluation, analysis of an episode of substance use, pros and cons of substance use, personal goals, problems and risks of substance use, exploration of preoccupations, decision‐making, questions and answers, decisional balance, planning changes, self monitoring Duration: approximately 60 min Control: alternative intervention |
|
| Outcomes |
Outcomes: quantity and frequency measures; problems derived from use Measures: Spanish version of the Teen Addiction Severity Index (T‐ASI) |
|
| Funding and Declared Conflicts of Interest | Funded by Spanish Government National Plan on Drugs. No information or declarations about potential conflicts of interest | |
| Notes | No alcohol outcomes reported, only composite drug use measure; author contacted for more details | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to make a judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a judgement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | High attrition (28%). Intention‐to‐treat analysis |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information about alcohol use measures used in the study. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to intervention. Insufficient information to make a judgement about blinding of therapists |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to make judgement |
| Unit of Analysis issues | Low risk | Not applicable |
Horner 2010.
| Methods |
Design: RCT Follow‐up: 1 and 3 months Attrition: 43% |
|
| Participants |
Age (range): 18‐22 years Sex: 68.6% male N participants: 150 Allocation: n = 40 BMI intervention; n = 42 control ; n = 66 other intervention Setting: university; higher risk students Country: USA |
|
| Interventions |
Programme type: brief motivational interviewing Set‐up: 2 individual sessions (students randomised to BMI attended their initial treatment session immediately following completion of the pre‐assessment questionnaires. The second BMI intervention session was then scheduled within 7‐10 days from the initial meeting and was conducted by the same therapist. Key components: participants' current and past drinking experiences, including the circumstances that led to the violation of the University regulations, history of any other significant alcohol‐related consequences or prior treatment, and the individual’s family history of substance use and mental health. Participants were also asked to provide information about their academic major, career plans, non‐alcohol related activities they engage in regularly for relaxation and stress reduction, as well as spiritual or religious beliefs and practices Duration: session lasted 40‐60 min Control: no intervention or other intervention |
|
| Outcomes |
Outcomes: alcohol consumption variables, readiness to change, and problems experienced due to drinking, total number of drinking
days per week; total number of drinks per week; peak alcohol use; consequences experienced that indicate alcohol dependence; personal consequences; or social consequences. Measures: measures of alcohol use: Daily Drinking Questionnaire, Frequency‐Quantity Questionnaire; measures of perceived consequences related to alcohol use: Rutgers Alcohol Problem Index; measure of motivation to change: Readiness Ruler |
|
| Funding and Declared Conflicts of Interest | None stated | |
| Notes | Insufficient details contained in dissertation for study to be included in MA. Author contacted for more information. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to make a judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a judgement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Attrition: 43% |
| Selective reporting (reporting bias) | Low risk | All data reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to intervention or therapists |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to make a judgement |
| Unit of Analysis issues | Low risk | Not applicable |
Juarez 2006.
| Methods |
Design: RCT Follow‐up: 2 months Attrition: 27% |
|
| Participants |
Mean age (years): 19.4 Sex: 47% male N participants: 122 Allocation: not reported Setting: college; higher risk students Country: USA |
|
| Interventions |
Programme type: motivational interviewing Set‐up: motivational interviewing: single individual session; motivational interviewing plus feedback: 2 individual sessions Key components: decisional balance, readiness to change, drinking consequences. Feedback: student’s alcohol consumption, alcohol‐related consequences and risk, peak blood alcohol concentration, social norms Duration: motivational interiewing 40‐60 min; motivational interviewing with feedback 60‐80 min Control: alternative intervention |
|
| Outcomes |
Outcomes: number of drinks per day; peak blood alcohol concentration; alcohol‐related consequences; symptoms of alcohol dependence Measures: Daily Drinking Questionnaire; Rutgers Alcohol Problem Index; Short Alcohol Dependence Data |
|
| Funding and Declared Conflicts of Interest | Funded by NIAAA. No information or declarations about potential conflicts of interest | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to make judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make judgement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | High attrition (27%). 1 participant failed to complete but did follow‐up, included in analysis because her inclusion did not change results. Loss to follow‐up of 32 (73%) who did not differ in terms of demographics and alcohol or between groups |
| Selective reporting (reporting bias) | Low risk | All pre‐specified outcomes are reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to intervention. Insufficient information to make a judgement about blinding of therapists |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to make judgement |
| Unit of Analysis issues | Low risk | Not applicable |
Kulesza 2010.
| Methods |
Design: RCT Follow‐up: 4 weeks postintervention Attrition: 0% |
|
| Participants |
Mean age (years): 20 Sex: 72% female N participants: 114 Allocation: n = 35 50‐min; n = 39 10‐min; n = 40 control Setting: college; higher risk students Country: USA |
|
| Interventions |
Programme type: brief motivational interviewing Set‐up: single individual session Key components: the following topics were addressed in sessions: evaluation of typical drinking patterns from diary cards and baseline assessment; comparison of typical patterns of alcohol use and perceived norms to actual norms; review of the biphasic effects of alcohol; personalised review of drinking consequences; and placebo and tolerance effects of alcohol. Each participant received a handout with a list of strategies to encourage moderate drinking Duration: 10‐min or 50‐min Control: assessment only |
|
| Outcomes |
Outcomes: typical number of drinks consumed; hours spent drinking on each day of the week over the past month; whether and how often students had experienced consequences impacting personal, social, or academic functioning in the past 3 years Measures: Rutgers Alcohol Problem Index; Daily Drinking Questionnaire; Brief Drinker Profile |
|
| Funding and Declared Conflicts of Interest | No information on funding. Conflicts of interested stated as "none" | |
| Notes | 10 and 50 min brief MI feedback conditions pooled for MA | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No attrition |
| Selective reporting (reporting bias) | Low risk | All of the study's pre‐specified outcomes were reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to intervention. Insufficient information to make a judgement about blinding of therapists |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to make judgement |
| Unit of Analysis issues | Low risk | Not applicable |
LaBrie 2008.
| Methods |
Design: RCT Follow‐up: weekly for 10 weeks following intervention Attrition: 1% |
|
| Participants |
Mean age (years): 18.10 Sex: 100% female N participants: 220 Allocation: n = 126 intervention n = 94 control Setting: college; higher risk students Country: USA |
|
| Interventions |
Programme type: motivational enhancement Set‐up: single individual session Key components: individual TLFB assessment and self confrontation with personal drinking over the previous 3 months, an introductory discussion of alcohol expectancies and the 'good things' and 'not‐so‐good things' about drinking, normative feedback, information on blood alcohol concentration and alcohol effects specific to women, a discussion of reasons for drinking, a decisional balance exercise weighing the pros and cons of drinking, and the setting of personal behavioural goals Duration: 2 h Control: assessment only |
|
| Outcomes |
Outcomes: alcohol attitudes: motivations for drinking alcohol; alcohol‐related negative consequences: problems encountered during the prior month while drinking or as a result of alcohol use; alcohol use: during group sessions, participants reported alcohol use over the past 3 months. Using the TLFB, variables for number of drinks per
week, number of drinking days, average number of drinks, maximum number of drinks consumed at one time, and number of binge drinking events (consuming 4 or more drinks in a row) Measures: Drinking Motives Questionnaire; Rutgers Alcohol Problem Index; Timeline Followback |
|
| Funding and Declared Conflicts of Interest | Funded by NIAAA. No information or declarations about potential conflicts of interest | |
| Notes | Study results not in right format for MA; authors contacted | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | A true random sample cannot be assumed, because the first‐come, first‐served basis may have catered to highly motivated individuals |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition < 1% |
| Selective reporting (reporting bias) | Low risk | All of the study's pre‐specified outcomes were reported |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Participants blindly self selected into randomised intervention or control groups |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Unit of Analysis issues | Low risk | Not applicable |
LaBrie 2009.
| Methods |
Design: RCT Follow‐up: 10 weeks of online follow‐up assessment, and a 6‐month online follow‐up Attrition: 8.8% at 10 weeks postintervention; 12.7% at 6‐month follow‐up |
|
| Participants |
Mean age (years): 17.93 Sex: 100% female N participants: 285 Allocation: n = 159 intervention; n = 126 control Setting: college students mandated for alcohol violation Country: USA |
|
| Interventions |
Programme type: motivational enhancement group intervention Set‐up: single individual session Key components: the intervention contained several elements of MI, including a decisional balance (weighing the pros and cons) and the use of normative feedback, as well as BAC information and information about the unique ways alcohol impacts women. Further, the intervention included an open‐ended discussion of female‐specific reasons for drinking focusing on relational and interpersonal reasons Duration: 2 h Control: assessment only |
|
| Outcomes |
Outcomes: number of drinks they had consumed on each day; drinks per month (total number of drinks in the past month); maximum drinks per occasion (greatest number of drinks on any occasion in the past month); heavy episodic drinking events (number of occasions in the past month in which 4 or more drinks were consumed) Measures: Timeline Followback |
|
| Funding and Declared Conflicts of Interest | No information about funding or declarations about potential conflicts of interest | |
| Notes | Study results not in right format for MA; authors contacted | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Participants self selected into randomised intervention or control groups, a true random sample cannot be assumed, because the first‐come, first‐served basis may have catered to highly motivated individuals |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a judgement about blinding of therapists |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low attrition (12.7%). Based on tests of independent proportions, participant retention was not significantly disparate between the control and intervention groups, nor were there any significant demographic differences (age, race, college, and location of residence) between participants with and without data completed from all time points. |
| Selective reporting (reporting bias) | Low risk | All of the study's pre‐specified outcomes were reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Participants selected a group session blind to condition status. Insufficient information to make a judgement about blinding of therapists |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to make a judgement about blinding of therapists |
| Unit of Analysis issues | Low risk | Not applicable |
Larimer 2001.
| Methods |
Design: cluster‐RCT Follow‐up: 1 year Attrition: 24% |
|
| Participants |
Mean age (years): 18.8 Sex: 100% male N participants: 12 fraternity houses, 159 students Allocation: n = 6 fraternity houses (n = 77 participants) intervention; n = 6 fraternity houses (n = 82 participants) control Setting: college students in fraternity houses; no distinction by level of individual risk Country: USA |
|
| Interventions |
Programme type: motivational enhancement therapy Set‐up: individual single session and group feedback session Key components: drinking norms, consequences, strategies Duration: individual session 60 min Control: alternative intervention |
|
| Outcomes |
Outcomes: drinking quantity; frequency; average use; blood alcohol concentration; alcohol‐related problems; perceived norms Measures: Daily Drinking Questionnaire; Rutgers Alcohol Problem Index; Alcohol Dependence Scale; Drinking Norms Rating Form; Short Michigan Alcoholism Screening Test for mother and father; University of Rhode Island Change Assessment; Alcohol Perceived Risk Assessment |
|
| Funding and Declared Conflicts of Interest | Funded by NIAAA. No information or declarations about potential conflicts of interest | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Moderate attrition (24%). No analysis of differential attrition |
| Selective reporting (reporting bias) | Low risk | All expected outcomes reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to intervention. Insufficient information to make a judgement about blinding of therapists |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Unit of Analysis issues | Unclear risk | Unusual method of adjustment for cluster effects; unclear if this adequately accounted for ICC. Study results removed from MA in a sensitivity analysis |
Marlatt 1998.
| Methods |
Design: RCT Follow‐up: 6 months, 1, 2, 3, 4 years Attrition: 17% |
|
| Participants |
Age: not stated: college freshmen > 19 Sex: 54% female N participants: 348 Allocation: not reported Setting: college campus; higher risk students Country: USA |
|
| Interventions |
Programme type: brief motivational interviewing Set‐up: individual single session Key components: feedback sheet, interview (manualised); college drinking norms compared; perceived risks identified and discussed; risk reduction suggestions Duration: not mentioned Control: assessment only |
|
| Outcomes |
Outcomes: alcohol quantity; frequency; peak consumption; frequency of drinking per week; average quantity of alcohol; alcohol‐related consequences; alcohol dependence Measures: Daily Drinking Questionnaire; Rutgers Alcohol Problem Index; Alcohol Dependence Scale; Family Tree Questionnaire |
|
| Funding and Declared Conflicts of Interest | Funded by NIAAA. No information or declarations about potential conflicts of interest | |
| Notes | 12 month follow‐up results included in MA | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Students were randomly assigned by computer‐generated random numbers |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition 17% |
| Selective reporting (reporting bias) | Low risk | All expected outcomes reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to intervention. Insufficient information to make a judgement about blinding of therapists |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Unit of Analysis issues | Low risk | Not applicable |
Marsden 2006.
| Methods |
Design: RCT Follow‐up: 6 months Attrition: 13% |
|
| Participants |
Mean age (years): 18.4 Sex: 66.4% male N participants: 342 Allocation: n = 166 intervention n = 176 control Setting: drug agencies; stimulant users (higher risk) Country: UK |
|
| Interventions |
Programme type: brief motivational interviewing Set‐up: individual single session Key components: self assessment with feedback + standard printed information about drugs and alcohol Duration: 45‐60 min Control: assessment only |
|
| Outcomes |
Outcomes: frequency of alcohol use; amount of alcohol consumed weekday and weekend past 90 days; problematic stimulant use; hazardous drinking past 90 days; behaviour change Measures: Maudsley Addiction Profile; Severity of Dependence Scale; Alcohol Use Disorder Identification Test |
|
| Funding and Declared Conflicts of Interest | Funded by Department of Health with support from Altrix Healthcare Limited. No information or declarations about potential conflicts of interest | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Allocation of participants to the experimental and control condition was controlled and balanced by random permuted blocks |
| Allocation concealment (selection bias) | Low risk | Worker received allocation by phone after questionnaire completion |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition 13%. Intention‐to‐treat analysis performed |
| Selective reporting (reporting bias) | Low risk | All expected outcomes reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | It was not possible to blind participants and workers to the allocated trial condition beyond completion of the self assessment questionnaire at baseline |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Unit of Analysis issues | Low risk | Not applicable |
Martens 2013.
| Methods |
Design: RCT Follow‐up: 1, 6 months Attrition: 4%, 6% |
|
| Participants |
Mean age (years): 20.09 Sex: 65.2% female N participants: 365 Allocation: n = 111 PBSF; n = 121 PNF; n = 133 control Setting: university; higher risk students Country: USA |
|
| Interventions |
Programme type: motivational interviewing Set‐up: individual single session Key components: The format of the PNF interventions is modelled on the BASICS intervention, and involved the delivery of personalised feedback in an MI‐based framework Duration: 15‐20 min Control: alternative intervention |
|
| Outcomes |
Outcomes: alcohol consumption were average drinks per week, average number of drinking days per week, and peak blood alcohol concentration (BAC); alcohol‐related problems Measures: modified Daily Drinking Questionnaire; Rutgers Alcohol Problems Index |
|
| Funding and Declared Conflicts of Interest | Funded by US NIH. No information or declarations about potential conflicts of interest | |
| Notes | A third trial arm that also comprised an MI‐based intervention has not been included in this review and meta‐analysis; we selected the PNF‐based intervention as this is a more common MI‐oriented intervention | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were randomised, stratified by sex, via a random number table |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low attrition (6%). |
| Selective reporting (reporting bias) | Low risk | All alcohol outcomes reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to intervention. Insufficient information to make a judgement about blinding of therapists |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to make judgement |
| Unit of Analysis issues | Low risk | Not applicable |
McCambridge 2004.
| Methods |
Design: cluster‐RCT Follow‐up: 3 and 12 months Attrition: 19% at 12 months |
|
| Participants |
Median age (years): 17 Sex: 45% female N participants: 200 Allocation: n = 105 intervention; n = 95 control (10 clusters; cluster allocation not reported) Setting: further education colleges; illegal drug users: higher risk Country: UK |
|
| Interventions |
Programme type: motivational interviewing Set‐up: individual single session Key components: discussion on individuals drug use, problems, consequences, goals Duration: 1 h Control: assessment only |
|
| Outcomes |
Outcomes: units per week of alcohol, cigarettes, cannabis, other drugs Measures: Severity of Dependence Scale; adolescent alcohol problems measure; Drug Attitudes Scale; General Health Questionnaire |
|
| Funding and Declared Conflicts of Interest | Funded by NHS. No information or declarations about potential conflicts of interest | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomisation was non‐computerised and consisted of colleague (not involved in study) allocating clusters randomly with complete concealment. Randomisation for ethnicity was deemed to have failed in 4 variables |
| Allocation concealment (selection bias) | Low risk | Researchers say that complete concealment was employed |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low attrition: 19% at 12 months |
| Selective reporting (reporting bias) | Low risk | All expected outcomes reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants not blinded. Unclear information about personnel |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | A second independent interviewer who was blind to study condition was employed to interview a sample of participants, though not all participants |
| Unit of Analysis issues | Unclear risk | Substantial baseline imbalances indicated poor achieved cluster randomisation. Authors report that reported regression coefficients were not adjusted for clustering as this was found not to be important. But details not provided. No ICC estimate provided. Study results removed from MA in a sensitivity analysis |
McCambridge 2008.
| Methods |
Design: RCT Follow‐up: 3, 6 months Attrition: 19% |
|
| Participants |
Mean age (years): 18.0 Sex: 69% male N participants: 326 students Allocation: n = 164 intervention n = 162 control Setting: inner city further education colleges; cannabis users: higher risk Country: UK |
|
| Interventions |
Programme type: motivational interviewing Set‐up: individual single session Key components: costs and the benefits of drug use was followed by discussion of values and goals, risks, problems and concerns, decision‐making and either self monitoring or change as appropriate Duration: 1 h Control: alternative intervention |
|
| Outcomes |
Outcomes: frequency; quantity; alcohol problems Measures: Alcohol Use Disorder Identification Test |
|
| Funding and Declared Conflicts of Interest | Funded by Wellcome Trust. Declarations of interest stated as "none" | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐randomised by clinical trials unit |
| Allocation concealment (selection bias) | Low risk | Central allocation (telephone/email) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low attrition (19%). Intention‐to‐treat analysis performed |
| Selective reporting (reporting bias) | Low risk | All expected outcomes reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to intervention. Insufficient information to make a judgement about blinding of therapists |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Participants self completed questionnaires were distributed by a researcher who was blind to study allocation |
| Unit of Analysis issues | Low risk | Stratified allocation by college, so that equivalent numbers of groups recruited from any one college were allocated to each study condition. No evidence of baseline differences. Clustering accounted for in statistical analysis. |
McCambridge 2011.
| Methods |
Design: Cluster‐randomised trial Follow‐up: 3 and 12 months Attrition: 18% |
|
| Participants |
Mean age (years): 17.5 Sex: 53% male N participants: n = 416 Allocation: n = 206 intervention n = 210 control (12 colleges; allocation not reported) Setting: further education colleges; all students Country: UK |
|
| Interventions |
Programme type: motivational interviewing Set‐up: delivery during a lesson to group of students Key components: participants were encouraged to think through and discuss a series of hypothetical situations in which they might find it difficult to refuse offers of drugs they had not previously used. Reasons for not using specific substances, and how initiation of use might affect future plans were explored Duration: 1 h Control: alternative intervention |
|
| Outcomes | Outcomes: measures of use assessed over the past month; measures of risk and harm for hazardous drinking; Alcohol Use Disorder Identification Test | |
| Funding and Declared Conflicts of Interest | Funded by Big Lottery. Authors declare no conflicts of interest | |
| Notes | Results included in MA only for baseline drinkers (n = 103 intervention and n = 99 control) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computerised randomisation stratified allocation by college, so that equivalent numbers of groups recruited from any one college would be allocated to each study condition |
| Allocation concealment (selection bias) | Low risk | Randomisation was undertaken by the local Clinical Trials Unit and decisions were communicated by telephone to researchers after recruitment and baseline data collection on an individual college basis to preserve allocation concealment |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low attrition (18%). Intention‐to‐treat analysis performed |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes were reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to intervention. Insufficient information to make a judgement about blinding of therapists |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | The researcher involved in the administration of the follow‐up data collection at any college had not been involved in the delivery of interventions in that college, though was not always blind to study allocation |
| Unit of Analysis issues | Unclear risk | Stratified allocation by college, so that equivalent numbers of groups recruited from any one college were allocated to each study condition. No evidence of baseline differences. Clustering accounted for in statistical analysis reported in paper. but individual level data only available for inclusion in MA. ICC not reported. Study removed as part of sensitivity analysis |
Michael 2006.
| Methods |
Design: RCT Follow‐up: 30‐45 days after the MI intervention Attrition: 0% |
|
| Participants |
Mean age (years): 18.35 Sex: 37% male N participants: 91 Allocation: n = 47 intervention n = 44 control Setting: college; all students Country: USA |
|
| Interventions |
Programme type: motivational interviewing Set‐up: 2 group sessions Key components: exploration, feedback, support for self efficacy, discussion re alcohol use and risky behaviour. establishing rapport, assessing and enhancing motivation for change, and establishing goals for change. Booster session at 1 and 3 months Duration: Each session 50 min in duration (100 min total; approximately 2 weeks apart) Control: assessment only |
|
| Outcomes |
Outcomes: drinking (self reported number of drinking days during the past 30 days, number of intoxicating events during the past 30 days); alcohol‐related problems during the past 30 days; psychopathology; Big Five personality traits Measures: 2‐week Alcohol Timeline Followback; Rutgers Alcohol Problem Index; Symptom Checklist 90–Revised; International Personality Item Pool |
|
| Funding and Declared Conflicts of Interest | No information. No information or declarations about potential conflicts of interest | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No attrition |
| Selective reporting (reporting bias) | Low risk | All pre‐specified outcomes were reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to intervention. Insufficient information to make a judgement about blinding of therapists |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Unit of Analysis issues | Low risk | Not applicable |
Monti 1999.
| Methods |
Design: RCT Follow‐up: 3 months, 6 months Attrition: 11% |
|
| Participants |
Mean age (years): 18.4 Sex: 64% male N participants: 94 Allocation: n = 52 intervention; n = 42 control Setting: hospital emergency department; higher risk patients Country: USA |
|
| Interventions |
Programme type: motivational interviewing Set‐up: individual single session Key components: pros and cons, imagining future, establishing goals Duration: not clear Control: alternative intervention |
|
| Outcomes |
Outcomes: harm reduction effects; drinking and driving; moving violations; alcohol‐related injuries; alcohol‐related problems Measures: Adolescent Drinking Index; Young Adult Drinking and Driving Questionnaire; Adolescent Injury Checklist; Health Behaviour Questionnaire; Adolescent Drinking Questionnaire; Stage‐Change Algorithm |
|
| Funding and Declared Conflicts of Interest | No information. No information or declarations about potential conflicts of interest | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low attrition (11%). Intention‐to‐treat analysis performed |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes were reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to intervention. Insufficient information to make a judgement about blinding of therapists |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Follow‐up interviews were conducted at 3 months by telephone and at 6 months in person by research assistants who were unaware of treatment condition |
| Unit of Analysis issues | Low risk | Not applicable |
Monti 2007.
| Methods |
Design: RCT Follow‐up: 6, 12 months Attrition: 16.7 % |
|
| Participants |
Mean age (years): 20.5 Sex: 67.7% male N participants: 198 Allocation: n = 87 intervention; n = 91 control Setting: emergency department; higher risk patients Country: USA |
|
| Interventions |
Programme type: motivational interviewing Set‐up: individual single session Key components: exploration, feedback, support for self efficacy, discussion re alcohol use and risky behaviour. establishing rapport, assessing and enhancing motivation for change, and establishing goals for change. Booster session at 1 and 3 monthd Duration: 30‐45 min Control: alternative intervention |
|
| Outcomes |
Outcomes: number of days drinking; number of heavy drinking days; average drinks per week; alcohol related problems; adolescent Injury; frequency of drink driving Measures: Timeline Followback; Rutgers Alcohol Problem Index; Adolescent Injury Checklist |
|
| Funding and Declared Conflicts of Interest | Funded by NIAAA and Dept of Veterans Affairs. No information or declarations about potential conflicts of interest | |
| Notes | Gwaltney 2011 reported 3‐month outcome data for number of heavy drinking days | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Patients were assigned randomly to a treatment condition (by the project co‐ordinator using a random numbers table) |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low attrition (17%) |
| Selective reporting (reporting bias) | Low risk | All measures reported at least for baseline and 12 months |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to intervention. Insufficient information to make a judgement about blinding of therapists |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Research assistants blind to intervention condition |
| Unit of Analysis issues | Low risk | Not applicable |
Murphy 2001.
| Methods |
Design: RCT Follow‐up: 3 months, 9 months Attrition: 20% |
|
| Participants |
Mean age (years): 19.60 Sex: 54% female N participants: 99 Allocation: n = 25 education; n = 30 BASICS; n = 24 control Setting: university; higher risk students Country: USA |
|
| Interventions |
Programme type: motivational interviewing Set‐up: individual single session Key components: personalised feedback sheet created from initial assessment data: information regarding the student's drinking patterns relative to normative college student drinking, blood alcohol concentrations, alcohol‐related problems, and risk factors. Clinicians adopted an empathic and non‐confrontational approach while highlighting risks associated with the student's alcohol consumption and inquiring about the impact of heavy drinking on the student's other life goals Duration: 50 min Control: alternative intervention |
|
| Outcomes |
Outcomes: drinks per week; drinking days per week; binge drinking per week; alcohol‐related problems Measures: Daily Drinking Questionnaire; Rutgers Alcohol Problem Index |
|
| Funding and Declared Conflicts of Interest | No information. No information or declarations about potential conflicts of interest | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition 20%. Missing data have been imputed using appropriate methods: using the baseline value for that measure as the predictor for missing data at 3 months and the 3‐month value as the predictor for missing data at 9 months |
| Selective reporting (reporting bias) | Low risk | All expected outcomes including those pre‐specified were reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to intervention. Insufficient information to make a judgement about blinding of therapists |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Unit of Analysis issues | Low risk | Not applicable |
Murphy 2004.
| Methods |
Design: RCT Follow‐up: 6 months Attrition: 6% |
|
| Participants |
Mean age (years): 19.94 Sex: 69% female N participants: 54 Allocation: n = 28; n = 24 control Setting: college; higher risk students Country: USA |
|
| Interventions |
Programme type: motivational interviewing Set‐up: individual single session Key components: drinking norms, consequences, planning Duration: 30‐50 min Control: alternative intervention |
|
| Outcomes |
Outcomes: drinks per week; frequency of drinking; frequency of heavy drinking; alcohol‐related problems Measures: Daily Drinking Questionnaire; Rutgers Alcohol Problem Index |
|
| Funding and Declared Conflicts of Interest | Funded by US Department of Education. No information or declarations about potential conflicts of interest | |
| Notes | No significant effects reported, but insufficient information for inclusion in meta‐analysis; author contacted for more details | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit a judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit a judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low attrition (6%) |
| Selective reporting (reporting bias) | Low risk | All outcomes are reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to intervention. Insufficient information to make a judgement about blinding of therapists |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit a judgement |
| Unit of Analysis issues | Low risk | Not applicable |
Murphy 2010a.
| Methods |
Design: RCT Follow‐up: 1 month Attrition: 6% |
|
| Participants |
Mean age (years): 18.6 Sex: 60% female N participants: 73 Allocation: n = 38 intervention; n = 35 control Setting: public university; higher risk students Country: USA |
|
| Interventions |
Programme type: motivational interviewing Set‐up: individual single session Key components: an introductory discussion that emphasised confidentiality, harm reduction, and the student’s autonomy/responsibility to make decisions about the information provided in the session; a discussion of the student’s college and career goals, and how they might relate to decisions about substance use; a decisional balance exercise; personalised feedback; and summary, goal setting, and, if the student was interested, reviewing protective behavioural strategies Duration: 50‐60 min Control: alternative intervention |
|
| Outcomes |
Outcomes: total drinks per week; frequency of heavy drinking Measures: Daily Drinking Questionnaire |
|
| Funding and Declared Conflicts of Interest | Funded by Alcohol Research Foundation and US NIH. No information about potential conflicts | |
| Notes | Study 1: Feedback delivered by MI; control: Alcohol 101 alcohol education CD‐ROM | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomly assigned to a condition using a random number table that was stratified by sex and ethnicity |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low attrition (6%). To examine the potential impact of missing follow‐up data on primary drinking outcomes, additional analyses using the last observation carried forward method were performed to replace data for the 5 participants who did not complete a follow‐up |
| Selective reporting (reporting bias) | Low risk | All pre‐specified outcomes were reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to intervention. The clinician who performed the intervention also completed the baseline assessment but was not aware of the condition assignment until the completion of the assessment |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | A research assistant who was blind to the intervention condition conducted the 1‐month follow‐up assessments. |
| Unit of Analysis issues | Low risk | Not applicable |
Murphy 2010b.
| Methods |
Design: RCT Follow‐up: 1 month Attrition: 11% |
|
| Participants |
Mean age (years): 18.6 Sex: 49% female N participants: 133 Allocation: n = 46 intervention; n = 42 control Setting: public university Country: USA |
|
| Interventions |
Programme type: motivational interviewing Set‐up: individual single session Key components: an introductory discussion that emphasised confidentiality, harm reduction, and the student’s autonomy/responsibility to make decisions about the information provided in the session; a discussion of the student’s college and career goals, and how they might relate to decisions about substance use; a decisional balance exercise; personalised feedback; and summary, goal setting, and, if the student was interested, reviewing protective behavioural strategies Duration: 50‐60 min Control: assessment only |
|
| Outcomes |
Outcomes: total drinks per week; frequency of heavy drinking Measures: Daily Drinking Questionnaire |
|
| Funding and Declared Conflicts of Interest | Funded by Alcohol Research Foundation and US NIH. No information about potential conflicts | |
| Notes | Feedback delivered by MI; control: assessment only | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomly assigned to a condition using a random number table that was stratified by sex and ethnicity |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low attrition (11%). To examine the potential impact of missing follow‐up data on primary drinking outcomes, additional analyses using the last‐observation carried forward method were performed to replace data for the 5 participants who did not complete a follow‐up |
| Selective reporting (reporting bias) | Low risk | All pre‐specified outcomes were reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to intervention. The clinician who performed the intervention also completed the baseline assessment but was not aware of the condition assignment until the completion of the assessment |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | A research assistant who was blind to the intervention condition conducted the 1‐month follow‐up assessments |
| Unit of Analysis issues | Low risk | Not applicable |
Murphy 2012a.
| Methods |
Design: RCT Follow‐up: 3, 6, 9, 12, and 15‐month follow‐ups Attrition: 20%, 15%, 20%, 19%, 20% |
|
| Participants |
Mean age (years): 20.7 Sex: 52% male N participants: 143 Allocation: n = 68 intervention n = 75 control Setting: HIV primary care; higher risk sub‐group Country: USA |
|
| Interventions |
Programme type: motivational enhancement therapy Set‐up: 4 individual sessions Key components: sessions were focused on 2 of the 3 possible problem behaviours based on entry screening. The study focused on young people who received the intervention for substance use. The intervention was derived from motivational enhancement therapy, in which principles of MI are manualised and combined with structured personalised feedback in order to facilitate behaviour change Duration: 60 min Control: alternative treatment |
|
| Outcomes |
Outcomes: youth reported alcohol use (including used/not and the maximum times of use) Measures: Timeline Followback Procedure |
|
| Funding and Declared Conflicts of Interest | No information about funding. Authors declare no competing financial interests | |
| Notes | Insufficient information in the published paper for inclusion in the MA. Author contacted for more details | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low attrition, max 20%. Missing data were imputed using the MCMC method for those who were lost follow‐up |
| Selective reporting (reporting bias) | Low risk | All alcohol outcomes reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to intervention. Insufficient information to make a judgement about blinding of therapists |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Unit of Analysis issues | Low risk | Not applicable |
Naar‐King 2006.
| Methods |
Design: RCT Follow‐up: 3 months, 9 months Attrition: unclear |
|
| Participants |
Mean age (years): 21.09 Sex: 52% male N participants: 65 Allocation: n = 32 intervention n = 33 control Setting: adolescent HIV clinic; all patients Country: USA |
|
| Interventions |
Programme type: motivational enhancement therapy Set‐up: 4 individual sessions Key components: session 1: focus on the 2 most difficult behaviours based on their baseline assessment; personalised feedback of risk behaviours based on the baseline assessment; behavioural change plan. Choice of which behaviour to focus on first; session 2: followed the same format for the second target behaviour. In the subsequent 2 sessions the therapist reviewed the personalised behaviour change plan, continued to monitor and encourage progress, problem‐solved barriers, and elicited strategies to maintain health behaviours and to prevent relapse Duration: 60 min Control: assessment only |
|
| Outcomes |
Outcomes: Frequency of (drug and) alcohol use; sexual risk behaviour; viral load Measures: Timeline Followback |
|
| Funding and Declared Conflicts of Interest | Funded by NIDA. Authors declare no conflicts | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random numbers were generated by the project manager using an Internet‐based random number generator |
| Allocation concealment (selection bias) | Unclear risk | Sealed envelopes used but unclear whether opaque or sequentially numbered |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Attrition not stated. Intention‐to‐treat analysis completed |
| Selective reporting (reporting bias) | High risk | Not all alcohol outcomes reported (e.g. Alcohol dependency scale) |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to intervention. Insufficient information to make a judgement about blinding of therapists |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Unit of Analysis issues | Low risk | Not applicable |
Nirenberg 2013.
| Methods |
Design: RCT Follow‐up: 6 months Attrition: 7% |
|
| Participants |
Mean age (years): 17.9 Sex: 69% male N participants:990 Allocation: n = 323 MI plus a hospital trauma centre visit/exposure (MI‐H); n = 332 MI; n = 335 control Setting: Court referred 16‐21 year olds as part of their community service sanctions for high‐risk driving and/or alcohol/other drug charges Country: USA |
|
| Interventions |
Programme type: MI Set‐up: 4 group sessions, 1 individual session, and a community service experience. 2 MI groups: 1 (MI) received MI as described above; the other received MI‐H. The 2 MI groups were combined for analysis and compared with counselling service only (CS) Key components: stressed the pivotal role of the participant in the decision to change behaviour, the locus of control for change resting with the youth, and the non‐judgmental role of the counsellor Duration: 19 h Control: alternative intervention |
|
| Outcomes |
Outcomes: drinking in a hazardous manner Measures: modified AUDIT |
|
| Funding and Declared Conflicts of Interest | Funded by NIAAA. No information or declarations about potential conflicts of interest | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition 7% |
| Selective reporting (reporting bias) | Low risk | All alcohol outcomes reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to intervention. Insufficient information to make a judgement about blinding of therapists |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Unit of Analysis issues | Low risk | Not applicable |
Palmer 2004.
| Methods |
Design: RCT Follow‐up: 3 months Attrition:20 % |
|
| Participants |
Mean age (years): not stated Sex: 53% female N participants: 214 Allocation: n = 119 voluntary; n = 85 control Setting: university heavy drinkers Country: USA |
|
| Interventions |
Programme type: the Alcohol Skills Training Programme Interventiom (ASTP) Set‐up: 2 workshops with 8‐12 participants Key components: used reflective listening and motivational interviewing techniques to built rapport, minimise resistance, and present the non‐judgmental philosophy of the workshop Duration: 2 90 min sessions Control: no intervention |
|
| Outcomes |
Outcomes: drinking days/week; drinks on peak occasion; average drinks per occasion; total drinks per week; RAPI total; defensiveness; readiness to change Measures: Rutgers Alcohol Problems Index; Brief Drinker Profile; Single item Q/F/P index; Modified Daily Drinking Questionnaire; Readiness to Change Questionnaire; defensiveness Scale; Therapeutic Reactance Scale; Drinking Norms Rating form; revised version of the General Causality Orientation scale; Campus Alcohol Policies Scale; Comprehensive Effects of Alcohol Scale; Participants Satisfaction Scale; Adherence and Competence Measure |
|
| Funding and Declared Conflicts of Interest | Not stated | |
| Notes | Insufficient details in dissertation for inclusion in MA. Further information requested | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 20% attrition rate |
| Selective reporting (reporting bias) | Low risk | all data reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to intervention. No information about MI counsellor blinding |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Unit of Analysis issues | Low risk | Not applicable |
Rongklavit 2013.
| Methods |
Design: RCT Follow‐up: 1, 6 months Attrition: 10‐20% |
|
| Participants |
Age: 16‐25 years, mean age 21 Sex: 48% male N participants: 110 Allocation: n = 55 intervention; n = 55 control Setting: Thai stigmatised youth living with HIV attending a Red Cross centre; regarded as higher risk Country: Thailand |
|
| Interventions |
Programme type: Healthy Choices ‐ 4 session motivational interviewing counselling session Set‐up: 4 individual sessions Key components: MI strategies of reflective listening, asking open‐ended questions, affirmation, summarising, and elicitation of self motivational statements were used throughout all sessions Duration: each session lasted 60 min Control: 4 individual sessions of general health education |
|
| Outcomes |
Outcomes: frequency and quantity Measures: TLFB |
|
| Funding and Declared Conflicts of Interest | Funded by NIMH, NIDA and Public Health Solutions, NY. No information or declarations about potential conflicts of interest | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low attrition (10‐20%) |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to intervention. Insufficient information to make a judgement about blinding of therapists |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to say whether outcome assessors were blind |
| Unit of Analysis issues | Low risk | Not applicable |
Schaus 2009.
| Methods |
Design: RCT Follow‐up: 3, 6, 9, 12 months Attrition: 35% |
|
| Participants |
Mean age (years): 20.55 Sex: 48% male N participants: 363 Allocation: n = 181 intervention; n = 182 control Setting: college campus; higher risk students Country: USA |
|
| Interventions |
Programme type: brief motivational interviewing Set‐up: 2 individual sessions Key components: intervention combined patient‐centred motivational interviewing techniques and cognitive behavioural skills training Duration: 20 min Control: assessment only |
|
| Outcomes |
Outcomes: alcohol consumption: quantity, frequency, number of days, peak number of drinks; blood alcohol concentration; readiness to change; expectations; harm behaviours Measures: TLFB; Healthy Lifestyle Questionnaire, including Rutgers Alcohol Problem Index and Readiness to Change Questionnaire |
|
| Funding and Declared Conflicts of Interest | Funded by NIAAA. No information or declarations about potential conflicts of interest | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Investigators describe a random component in the sequence generation i.e. using a computer random number generator |
| Allocation concealment (selection bias) | Unclear risk | Group assignment was placed into a sealed envelope by the data manager and was not available to those recruiting subjects until after informed consent was obtained |
| Incomplete outcome data (attrition bias) All outcomes | High risk | High attrition (35%). Missing outcome data have been imputed using appropriate methods, and balanced in number across intervention groups |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to intervention. Insufficient information to make a judgement about blinding of therapists |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to say whether outcome assessors were blind |
| Unit of Analysis issues | Low risk | Not applicable |
Schmiege 2009.
| Methods |
Design: RCT Follow‐up: 3, 6, 9, 12 months Attrition: 35% |
|
| Participants |
Mean age (years): 15.8 Sex: 83% male N participants: 484 Allocation: n = 157 GPI n = 165 GPI+GMET; n = 162 control Setting: detention facility; higher risk participants Country: USA |
|
| Interventions |
Programme type: group motivational enhancement therapy Type: single group session Key components: MET style to facilitate a group discussion that was designed to be empathic, open, and non‐confrontational to encourage motivation to change alcohol use behaviour in the context of sexual activity. Participants were then given printed feedback regarding their alcohol use behaviour on the basis of their pre‐test responses to questions Duration: 2‐4 h Control: assessment only |
|
| Outcomes |
Outcomes: Risky Sexual Behaviour Index and a measure addressing the co‐occurrence of alcohol use with sexual behaviour Measures: risky sexual behaviour index; Alcohol Use Disorders Identification Test; Rutgers Alcohol Problems Inventory |
|
| Funding and Declared Conflicts of Interest | Funded by NIAAA. No information or declarations about potential conflicts of interest | |
| Notes | Bryan et al (2009) report longer‐term outcomes but insufficient information to include in MA; author contacted for more details | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | High attrition (35%). Mplus to test models using a full information (direct) maximum likelihood estimator, which addresses data that display levels of missingness |
| Selective reporting (reporting bias) | Low risk | All expected outcomes reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Adolescents were instructed that they would be randomly assigned to 1 of 3 possible educational sessions, although they were kept blind to the precise nature of each condition and to the study hypotheses. Not possible to blind personnel |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Unit of Analysis issues | Low risk | Not applicable |
Segatto 2010.
| Methods |
Design: RCT Follow‐up: 3 months Attrition: 15% |
|
| Participants |
Mean age (years): 21.8 Sex: 90.3% male N participants: 175 Allocation: n = 87 intervention n = 88 control Setting: emergency room; higher risk patients Country: Brazil |
|
| Interventions |
Programme type: brief motivational interviewing Set‐up: single individual session Key components: roll with resistance, express empathy, avoid argumentation, develop discrepancy and support self efficacy Duration: 45 min Control: assessment only |
|
| Outcomes |
Outcomes: pattern of alcohol consumption over the previous 3 months, considering the number of abstinent days, and amount of alcohol consumed; alcohol‐related problems; traffic violations, police involvement, physical health and sexuality; perception of future risks associated with excessive alcohol ingestion considering that the pattern of alcohol abuse does not change within 3 months; motivational stage to change behaviour Measures: Alcohol Consumption Questionnaire; Rutgers Alcohol Problem Index; Alcohol Consumption Risk Questionnaire; Alcohol Perception of Risk Assessment; Readiness to Change Questionnaire |
|
| Funding and Declared Conflicts of Interest | No information | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A lottery system was employed |
| Allocation concealment (selection bias) | Low risk | Lottery system performed by ER personnel not linked to the clinical trial in order to avoid selection bias |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition 15% |
| Selective reporting (reporting bias) | Unclear risk | All outcomes reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | "Patients were blinded to the intervention applied" (Procedures section). Personnel not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Instruments were applied by an independent researcher |
| Unit of Analysis issues | Low risk | Not applicable |
Spirito 2004.
| Methods |
Design: RCT Follow‐up: 3, 6, 12 months Attrition: 10.5% |
|
| Participants |
Mean age (years): 15.6 Sex: 36% female N participants: 152 Allocation: n = 78 intervention n = 74 control Setting: emergency department of hospital; higher risk patients Country: USA |
|
| Interventions |
Programme type: motivational interviewing Set‐up: single individual session Key components: exploration of motivation; feedback, establishing goals Duration: 35‐45 min Control: alternative intervention |
|
| Outcomes |
Outcomes: alcohol‐related injuries; drink‐driving; drinking days per month; drinking quantity; binge drinking frequency; frequency of intoxication past 3 months; alcohol‐related problems Measures: Adolescent Injury Checklist; Young Adult Drinking and Driving Questionnaire; Adolescent Drinking Questionnaire; Adolescent Health Behavior Questionnaire |
|
| Funding and Declared Conflicts of Interest | Funded by NIAAA. No information or declarations about potential conflicts of interest | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Patients were randomly assigned to the MI or SC plus assessment condition using a random numbers table |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low attrition (10.5%) |
| Selective reporting (reporting bias) | Low risk | All expected outcomes reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to intervention. Insufficient information to make a judgement about blinding of therapists |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | All follow‐up interviews were conducted by research assistants who were blind to treatment group assignment |
| Unit of Analysis issues | Low risk | Not applicable |
Steele Seel 2010.
| Methods |
Design: RCT Follow‐up: 1, 3 months Attrition: 0% |
|
| Participants |
Mean age (years): 19.3 Sex: 71.4% male N participants: 14 Allocation: n = 7 intervention n = 7 control Setting: vocational training centre; higher risk (low income) young people Country: USA |
|
| Interventions |
Programme type: motivational enhancement therapy Set‐up: 4 individual sessions Key components: The first session was focused primarily on building rapport, listening to their description of their drug use, providing information and feedback regarding the effects of substances on their lives and bodies and discussing their motivation to change their substance use behaviours (per SOCRATES responses). The second and third sessions were focused on an in‐depth look into their values using either a values card sort or by having a discussion regarding their values, and identifying the discrepancies between their values and drug‐using behaviours. The 4th session reviewed the change plan, assessed high‐risk situations that had occurred during the past week, and elicited strategies for coping with these situations, cravings and slips Duration: not stated Control: alternative intervention |
|
| Outcomes |
Outcomes: percentage days absent; standard drinks per using day Measures: Form 90; Addiction Severity Index; Stages of Change Readiness and Treatment Eagerness Scale SOCRATES |
|
| Funding and Declared Conflicts of Interest | No information | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Due to unexpected complications relating to study therapists, randomisation to therapist had to be compromised. At the beginning of the study, participants were randomly assigned via urn randomisation to balance on: sex, ethnicity, total months of addiction(s) and therapist. However, due to unexpectedly having to replace 1 therapist with another who was under time constraints, the first 7 participants were randomised to either treatment or control group by sex, ethnicity and total months of addiction and more heavily weighted to the new therapist if assigned to the treatment group. Also, 3 months into the study there were unexpected time limitations imposed on the duration of the study by the Job Corps due to supervisory issues, and participants were then alternatively assigned to either the control group or treatment group based on entry into Job Corps to ensure equal representation for both groups. In addition, the participants unexpectedly reported their drug screen results to the TEAP counsellor, and were often granted extensions for their final retest, thereby compromising the study’s measure of retention in Job Corps |
| Allocation concealment (selection bias) | High risk | See above |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No attrition |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to intervention. Personnel were not blind to participants' condition |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | The researcher who conducted the 3‐month follow‐ups was not blind to study conditions, introducing potential bias |
| Unit of Analysis issues | Low risk | Not applicable |
Stein 2006.
| Methods |
Design: RCT Follow‐up: 3 months Attrition: 17% |
|
| Participants |
Mean age (years): 17.06 Sex: 89.5% male N participants: 105 Allocation: n = 59 intervention; n = 46 control Setting: state juvenile correctional facility; higher risk substance using youth Country: USA |
|
| Interventions |
Programme type: motivational interviewing Set‐up: individual single session Key components: developing rapport, exploration of motivation (pros and cons), personalised assessment feedback, imagining the future with and without change, and establishing goals Duration: 90 min with 60 min booster session Control: alternative intervention |
|
| Outcomes |
Outcomes: risky behaviours including driving under the influence of alcohol Measures: adaptation of Young Adult Drinking and Driving Questionnaire |
|
| Funding and Declared Conflicts of Interest | Funded by NIDA. No information or declarations about potential conflicts of interest. | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low attrition (17%) |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to intervention. Insufficient information to make a judgement about blinding of therapists |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Unit of Analysis issues | Low risk | Not applicable |
Stein 2011.
| Methods |
Design: RCT Follow‐up: 3 months Attrition: 14% |
|
| Participants |
Mean age (years): 17.10 Sex: 84% male N participants: 162 Allocation: not reported Setting: state juvenile correctional facility; higher risk substance using youth Country: USA |
|
| Interventions |
Programme type: motivational interviewing Set‐up: individual session + booster Key components: sections of the MI included developing rapport, exploration of motivation (pros and cons), personalised assessment feedback, imagining the future with and without change, and establishing goals. Handouts were provided (e.g. goals chosen) Duration: 90 min with 60 min booster session Control: alternative intervention |
|
| Outcomes |
Outcomes: drinks per drinking day and number of heavy drinking days Measures: Structured Clinical Interview for DSM‐IV; Timeline Followback |
|
| Funding and Declared Conflicts of Interest | Funded by NIDA. No information or declarations about potential conflicts of interest | |
| Notes | Attrition/missing data is higher in analysis of drinks per drinking day | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was accomplished via random numbers table |
| Allocation concealment (selection bias) | Unclear risk | Placed in an envelope by the project coordinator, but not clear whether envelope was sealed, opaque, not sequentially numbered. Following baseline assessment, research staff opened the envelope to learn of intervention assignment |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition 14% |
| Selective reporting (reporting bias) | Low risk | All pre‐specified outcomes reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to intervention. Insufficient information to make a judgement about blinding of therapists |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Investigators report research staff conducting assessments were blind to treatment assignment |
| Unit of Analysis issues | Low risk | Not applicable |
Terlecki 2010 MANDATED.
| Methods |
Design: RCT Follow‐up: 4 weeks after intervention, (6 weeks from baseline for control) Attrition: 18% (estimate) |
|
| Participants |
Age: 18–24 years Sex: 62% male (across voluntary and mandated students) N participants:43 mandated students Allocation: n = 19 intervention; n = 24 control Setting: college; students mandated for alcohol violation Country: USA |
|
| Interventions |
Programme type: brief motivational interviewing Set‐up: single individual session Key components: The intervention covered the following topics in each session: evaluation of typical drinking patterns as recorded on the alcohol monitoring and baseline assessments of drinking behaviour; comparison of typical patterns of alcohol use and perceived norms to actual campus norms of same‐age peers; review of the biphasic effects of alcohol; personalised review of drinking consequences; and placebo and tolerance effects of alcohol Duration: 50 min Control: assessment only |
|
| Outcomes |
Outcomes: harmful and hazardous drinking; physical dependence on alcohol (family history of alcohol problems, history of conduct disorder, and personal drinking history); alcohol‐related negative consequences; average weekly drinking frequency and quantity over the last month; drinking behaviour in terms of quantity and frequency of their alcohol consumption on a typical occasion and peak drinking occasion within the past month Measures: Alcohol Use Disorder Identification Test; Alcohol Dependence Scale; the Brief Drinker Profile; Rutgers Alcohol Problem Inventory; Daily Drinking Questionnaire; Quantity/Frequency Index |
|
| Funding and Declared Conflicts of Interest | Funded by NIAAA. No information about potential conflicts | |
| Notes | Baseline analysis revealed significant demographic differences between study groups where mandated students were significantly more likely to be males relative to their voluntary high‐risk peers. Interaction between treatment condition and referral status was significant for measures of typical consumption. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were assigned to treatment conditions using a computer‐based urn randomisation to ensure matching on sex and current Greek membership status |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Attrition not directly indicated but possibly around 18%; missing data at the 12‐month follow‐up assessment did not significantly exceed the projected 30% (32% was missing) and as a result, missing outcome data were not imputed for any follow‐up assessment period to protect the integrity of the analyses |
| Selective reporting (reporting bias) | Low risk | All pre‐specified outcomes are reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to intervention. Study interventionist was not blind to treatment assignment or study hypotheses |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Unit of Analysis issues | Low risk | Not applicable |
Terlecki 2010 VOLUNTARY.
| Methods |
Design: RCT Follow‐up: 4 weeks after intervention, (6 weeks from baseline for control) Attrition: 18% (estimate) |
|
| Participants |
Age (years): 18–24 Sex: 62% male N participants: 41 voluntary students Allocation: n = 22 intervention n = 19 control Setting: college; heavier drinkers Country: USA |
|
| Interventions |
Programme type: brief motivational interviewing Set‐up: single individual session Key components: The intervention covered the following topics in each session: evaluation of typical drinking patterns as recorded on the alcohol monitoring and baseline assessments of drinking behaviour; comparison of typical patterns of alcohol use and perceived norms to actual campus norms of same‐age peers; review of the biphasic effects of alcohol; personalised review of drinking consequences; and placebo and tolerance effects of alcohol Duration: 50 min Control: assessment only |
|
| Outcomes |
Outcomes: harmful and hazardous drinking; physical dependence on alcohol (family history of alcohol problems, history of conduct disorder, and personal drinking history); alcohol‐related negative consequences; average weekly drinking frequency and quantity over the last month; drinking behaviour in terms of quantity and frequency of their alcohol consumption on a typical occasion and peak drinking occasion within the past month Measures: Alcohol Use Disorder Identification Test; Alcohol Dependence Scale; the Brief Drinker Profile; Rutgers Alcohol Problem Inventory; Daily Drinking Questionnaire; Quantity/Frequency Index |
|
| Funding and Declared Conflicts of Interest | Funded by NIAAA. No information about potential conflicts | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were assigned to treatment conditions using computer‐based urn randomisation to ensure matching on sex and current Greek membership status |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Attrition not directly indicated but possibly around 18%; missing data at the 12‐month follow‐up assessment did not significantly exceed the projected 30% (32% was missing) and as a result, missing outcome data were not imputed for any follow‐up assessment period to protect the integrity of the analyses |
| Selective reporting (reporting bias) | Low risk | All pre‐specified outcomes are reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to intervention. Study interventionist was not blind to treatment assignment or study hypotheses |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Unit of Analysis issues | Low risk | Not applicable |
Terlecki 2011 MANDATED.
| Methods |
Design: RCT Follow‐up: 4 weeks, 3 months, 6 months, 12 months Attrition: 16% |
|
| Participants | Age: 20.12 Sex: 61% male N participants: 123 Allocation: n = 64 intervention; n = 59 control Setting: college; mandated for alcohol violation Country: USA |
|
| Interventions |
Programme type: brief motivational interviewing Set‐up: single individual session Key components: The intervention covered the following topics in each session: evaluation of typical drinking patterns as recorded on the alcohol monitoring and baseline assessments of drinking behaviour; comparison of typical patterns of alcohol use and perceived norms to actual campus norms of same‐age peers; review of the biphasic effects of alcohol; personalised review of drinking consequences; and placebo and tolerance effects of alcohol Duration: 50 min Control: assessment only |
|
| Outcomes |
Outcomes: harmful and hazardous drinking; physical dependence on alcohol (family history of alcohol problems, history of conduct disorder, and personal drinking history); alcohol‐related negative consequences; average weekly drinking frequency and quantity over the last month; drinking behaviour in terms of quantity and frequency of their alcohol consumption on a typical occasion and peak drinking occasion within the past month Measures: Alcohol Use Disorder Identification Test; Alcohol Dependence Scale; the Brief Drinker Profile; Rutgers Alcohol Problem Inventory; Daily Drinking Questionnaire; Quantity/Frequency Index |
|
| Funding and Declared Conflicts of Interest | Funded by NIAAA. No information about potential conflicts | |
| Notes | Marked baseline differences between intervention and controls for alcohol problems | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were assigned to treatment conditions using computer‐based urn randomisation to ensure matching on sex and current Greek membership status |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Attrition not directly indicated but possibly around 16%; missing data at the 12‐month follow‐up assessment did not significantly exceed the projected 30% (32% was missing) and as a result, missing outcome data were not imputed for any follow‐up assessment period to protect the integrity of the analyses |
| Selective reporting (reporting bias) | Low risk | All pre‐specified outcomes are reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to intervention. Study interventionist was not blind to treatment assignment or study hypotheses |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Unit of Analysis issues | Low risk | Not applicable |
Terlecki 2011 VOLUNTARY.
| Methods |
Design: RCT Follow‐up: 4 weeks, 3 months, 6 months, 12 months Attrition: 16% |
|
| Participants |
Mean age (years): 20.12 Sex: 61% male N participants: 132 voluntary students Allocation: n = 67 intervention; n = 65 control Setting: college; heavier drinkers Country: USA |
|
| Interventions |
Programme type: brief motivational interviewing Set‐up: single individual session Key components: The intervention covered the following topics in each session: evaluation of typical drinking patterns as recorded on the alcohol monitoring and baseline assessments of drinking behaviour; comparison of typical patterns of alcohol use and perceived norms to actual campus norms of same‐age peers; review of the biphasic effects of alcohol; personalised review of drinking consequences; and placebo and tolerance effects of alcohol Duration: 50 min Control: assessment only |
|
| Outcomes |
Outcomes: harmful and hazardous drinking; physical dependence on alcohol (family history of alcohol problems, history of conduct disorder, and personal drinking history); alcohol‐related negative consequences; average weekly drinking frequency and quantity over the last month; drinking behaviour in terms of quantity and frequency of their alcohol consumption on a typical occasion and peak drinking occasion within the past month Measures: Alcohol Use Disorder Identification Test; Alcohol Dependence Scale; the Brief Drinker Profile; Rutgers Alcohol Problem Inventory; Daily Drinking Questionnaire; Quantity/Frequency Index |
|
| Funding and Declared Conflicts of Interest | Funded by NIAAA. No information about potential conflicts | |
| Notes | Marked baseline differences between intervention and controls for alcohol problems | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were assigned to treatment conditions using a computer‐based urn randomisation to ensure matching on sex and current Greek membership status |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Attrition not directly indicated but possibly around 16%; missing data at the 12‐month follow‐up assessment did not significantly exceed the projected 30% (32% was missing) and as a result, missing outcome data were not imputed for any follow‐up assessment period to protect the integrity of the analyses |
| Selective reporting (reporting bias) | Low risk | All pre‐specified outcomes are reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to intervention. Study interventionist was not blind to treatment assignment or study hypotheses |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Unit of Analysis issues | Low risk | Not applicable |
Thush 2009.
| Methods |
Design: RCT Follow‐up: 1, 6 months Attrition: 28.2% |
|
| Participants |
Mean age (years): 17.07 Sex: 59.2% female N participants: 125 Allocation: n = 61 intervention; n = 64 control Setting: low‐level vocational school; adolescents specified as at risk Country: Holland |
|
| Interventions |
Programme type: motivational interviewing Set‐up: individual single session Key components: Duration: 30 min with information flyers Control: information flyers only |
|
| Outcomes |
Outcomes: alcohol outcome expectancies; readiness to change; alcohol Use Measures: Alcohol Use Questionnaire; Implicit Association Test; Expectancy Questionnaire; Readiness to Change Questionnaire |
|
| Funding and Declared Conflicts of Interest | No information for funding or declarations about potential conflicts of interest | |
| Notes | Insufficient details for inclusion in MA. Authors contacted for more information | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | High attrition 28.5% |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to intervention. No information about blinding of MI counsellors |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Unit of Analysis issues | Low risk | Not applicable |
Turrisi 2009.
| Methods |
Design: RCT Follow‐up: 10 months Attrition: 14% |
|
| Participants |
Mean age (years): 17.92 Sex: 44.4% male N participants:1275 Allocation: n = 277 intervention; n = 340 control Setting: university; student athletes identified as higher risk Country: USA |
|
| Interventions |
Programme type: brief motivational interviewing Set‐up: single individual session Key components: provision of personalised feedback and discussion of alcohol norms, alcohol expectancies, negative consequences, and protective behavioural strategies and skills, delivered in a motivational‐enhancement style Duration: 45‐60 min Control: assessment only |
|
| Outcomes |
Outcomes: peak blood alcohol content; maximum drinks consumed on an occasion within the past 30 days; number of hours they spent drinking on that occasion; number of drinks they consumed on each day of a typical week; total number of drinks during a typical week.; alcohol‐related consequences; consumption, weekly and peak blood alcohol concentration Measures: Daily Drinking Questionnaire; Rutgers Alcohol Problem Index |
|
| Funding and Declared Conflicts of Interest | Funded by NIAAA. No information or declarations about potential conflicts of interest | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were randomised using a computerised algorithm. The computerised algorithm used simple randomisation, drawing 1 of 4 numbers corresponding to the 4 conditions on a random basis as the participants’ data were submitted |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The amount of missing data as a result of attrition was low (14%) |
| Selective reporting (reporting bias) | Low risk | All pre‐specified outcomes reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to intervention. Insufficient information to make a judgement about blinding of therapists |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to make a judgement |
| Unit of Analysis issues | Low risk | Not applicable |
Wagener 2012.
| Methods |
Design: RCT Follow‐up: 10 weeks Attrition: 7% |
|
| Participants |
Mean age (years): 20.9 Sex: 55% male N participants: 76 Allocation: n = 37 intervention; n = 39 control Setting: Midwestern university; all students Country: USA |
|
| Interventions |
Programme type: MI Set‐up: individual single session Key components: students interacted with an all‐inclusive, interactive programme called the Drinking Assessment and Feedback Tool for College Students (DrAFT‐CS). The DrAFT‐CS covered alcohol use behaviours, consequences, and perceived norms followed immediately by on‐screen personalised feedback. The personalised feedback included quantity and frequency of use; typical and peak blood alcohol levels achieved on drinking occasions; perceptions of social norms; dependence criteria; alcohol‐related problems experienced; financial and caloric costs of alcohol use; familial risk for alcohol problems; perceptions of risk; alcohol expectancies; psychological problems, such as depression and anxiety, that may exacerbate or contribute to alcohol abuse; and motivation for changing current alcohol use. The face‐to‐face group received feedback regarding their assessment from an advanced graduate student who had completed 30 h of training in MI and 6 h of training in using the style with this specific feedback intervention Duration: 60‐90 min Control: assessment only |
|
| Outcomes |
Outcomes: alcohol consumption; alcohol‐related problems Measures: modified version of the Daily Drinking Questionnaire; the Brief Young Adult Alcohol Consequences Questionnaire (B‐YAACQ) |
|
| Funding and Declared Conflicts of Interest | Funded by Oklahoma Department of Mental Health and Substance Abuse Services. No information or declarations about potential conflicts of interest | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Students were randomly assigned, using a computerised random number generator |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low attrition (7%) |
| Selective reporting (reporting bias) | Low risk | All pre‐specified outcomes were reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to intervention. Insufficient information to make judgement about blinding of therapists |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Unit of Analysis issues | Low risk | Not applicable |
Walters 2000.
| Methods |
Design: RCT Follow‐up: 6 weeks Attrition: 14% |
|
| Participants |
Mean age (years): 19.7 Sex: 40% female N participants: 37 Allocation: not reported Setting: psychology department mass testing session; higher risk students Country: USA |
|
| Interventions |
Programme type: motivational interviewing Set‐up: group single session Key components: values clarification; suggestions to promote responsible drinking; information about campus resources Duration: 2 h Control: assessment only |
|
| Outcomes |
Outcomes: consumption; weekly and peak blood alcohol concentration Measures: Short Index of Problems; Alcohol Use Disorders Identification Test; Check Up to Go (CHUG; Q/F index) |
|
| Funding and Declared Conflicts of Interest | No information | |
| Notes | AUDIT outcomes not reported; final group numbers not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low attrition (14%) |
| Selective reporting (reporting bias) | High risk | Not all outcomes were reported (e.g. AUDIT results) |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to intervention. Insufficient information to make a judgement about blinding of therapists |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | "In order to increase valid responding, all responses were anonymous and participants were identified only by numbers. All measures were scored by trained raters who were unaware of treatment condition" |
| Unit of Analysis issues | Low risk | Not applicable |
Walters 2009 MIF v FBO.
| Methods |
Design: RCT Follow‐up: 3, 6 months Attrition: 14% |
|
| Participants |
Mean age (years): 19.8 Sex: 64% female N participants: 279 Allocation: n = 67 feedback only; n = 70 MI only; n = 73 MI + feedback; n = 69 control Setting: college campus; higher risk students Country: USA |
|
| Interventions |
Programme type: motivational interviewing with web feedback Set‐up: individual single session Key components: orienting the participant to the session and the limits of confidentiality; exploring the participant’s drinking, including peak episodes and related problems; discussing ambivalence around drinking; using readiness rulers to elicit importance and confidence language; discussing change in the hypothetical or concrete; and, if appropriate, developing a plan for change. The counsellor also provided the participant with a list of campus and community resources related to alcohol Duration: not stated Control: assessment only |
|
| Outcomes |
Outcomes: alcohol consumption; peak blood alcohol concentration; alcohol related problems; normative drinking perceptions; readiness to change Measures: Daily Drinking Questionnaire; Rutgers Alcohol Problem Index; Protective Behaviours Strategies Survey; Readiness to Change Questionnaire; Alcohol Use Disorders Test |
|
| Funding and Declared Conflicts of Interest | Funded by NIAAA. No information about potential conflicts | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Low risk | Participants and investigators enrolling participants could not foresee assignment because of central allocation by computer |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low attrition (14%). Intention‐to‐treat analysis performed |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and counsellors were not blind to the group assignment |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Unit of Analysis issues | Low risk | Not applicable |
Walters 2009 MIO v AO.
| Methods |
Design: RCT Follow‐up: 3, 6 months Attrition: 14 % |
|
| Participants |
Mean age (years): 19.8 Sex: 64% female N participants: n = 139 Allocation: n = 70 intervention; n = 69 control Setting: college campus; higher risk students Country: USA |
|
| Interventions |
Programme type: motivational interviewing with web feedback Set‐up: individual single session Key components: orienting the participant to the session and the limits of confidentiality; exploring the participant’s drinking, including peak episodes and related problems; discussing ambivalence around drinking; using readiness rulers to elicit importance and confidence language; discussing change in the hypothetical or concrete; and, if appropriate, developing a plan for change. The counsellor also provided the participant with a list of campus and community resources related to alcohol Duration: not stated Control: assessment only |
|
| Outcomes |
Outcomes: alcohol consumption; peak blood alcohol concentration; alcohol related problems; normative drinking perceptions; readiness to change Measures: Daily Drinking Questionnaire; Rutgers Alcohol Problem Index; Protective Behaviours Strategies Survey; Readiness to Change Questionnaire; Alcohol Use Disorders Test |
|
| Funding and Declared Conflicts of Interest | Funded by NIAAA. No information about potential conflicts | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Low risk | Participants and investigators enrolling participants could not foresee assignment because of central allocation by computer |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low attrition (14%). Intention‐to‐treat analysis performed |
| Selective reporting (reporting bias) | Unclear risk | All outcomes reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and counsellors were not blind to the group assignment |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Unit of Analysis issues | Low risk | Not applicable |
Walton 2010.
| Methods |
Design: RCT Follow‐up: 3, 6, 12 months Attrition: 15% at 12 months |
|
| Participants |
Mean age (years): 16.8 Sex: 44% male N participants: 726 Allocation: n = 237 computerised BMI; n = 254 therapist BMI; n = 235 control Setting: hospital emergency department; higher risk patients Country: USA |
|
| Interventions |
Programme type: brief motivational interviewing Set‐up: individual single session Key components: included goals, personalised feedback for alcohol, violence, and weapon carriage, decisional balance exercise for the potential benefit of staying away from drinking and fighting, tailored roleplays (e.g. anger management, conflict resolution, alcohol refusals, not drinking and driving), and referral Duration: not stated Control: pamphlet with community resources |
|
| Outcomes |
Outcomes: alcohol use frequency; quantity (on a typical occasion); binge drinking (≥ 5 drinks); alcohol consequences Measures: Problem Oriented Screening Instrument for Teenagers; Alcohol Use Disorders Identification Test–Consumption |
|
| Funding and Declared Conflicts of Interest | Funded by NIAAA. Authors declare no financial or competing interests | |
| Notes | Only therapist BMI and control group used in MA. 12 month results included in MA | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was stratified by sex and age (14‐15 or 16‐18 years) and assigned based on computer‐generated algorithm. Randomisation occurred in blocks of 21 (7 per group) |
| Allocation concealment (selection bias) | Unclear risk | Assigned based on computer‐generated algorithm |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low attrition (15%). A single imputation procedure was used to complete missing alcohol misuse scores for 5 participants |
| Selective reporting (reporting bias) | Low risk | All pre‐specified outcomes were reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to intervention. Insufficient information to make judgement about blinding of therapists |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Follow‐up staff were blinded to baseline condition assignment |
| Unit of Analysis issues | Low risk | Not applicable |
White 2007.
| Methods |
Design: RCT Follow‐up: 4 months, 15 months Attrition: 37% |
|
| Participants |
Mean age (years): not reported Sex: 40% female N participants: 348 Allocation: n = 180 intervention; n = 168 control Setting: college campus; students mandated for alcohol violation Country: USA |
|
| Interventions |
Programme type: brief motivational interviewing Set up: individual single session Key components: discussion of feedback using MI principles Duration: not mentioned Control: alternative intervention |
|
| Outcomes |
Outcomes: number of drinks; peak blood alcohol concentration; alcohol problems Measures: Daily Drinking Questionnaire; Rutgers Alcohol Problem Index |
|
| Funding and Declared Conflicts of Interest | Funded by NIDA. No information or declarations about potential conflicts of interest. | |
| Notes | 15 month results included in MA | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | All students were randomly assigned by the flip of a coin after the first assessment |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | High attrition (37%) |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to intervention. Insufficient information to make judgement about blinding of therapists |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Unit of Analysis issues | Low risk | Not applicable |
Wilke 2014.
| Methods |
Design: cluster‐RCT, by fraternity/sorority house Follow‐up: 3 months Attrition: 80% (data cleaning led to removal of substantial number of respondents reporting high levels of consumption, with more removed from the intervention group) |
|
| Participants |
Mean age (years): 20 Sex: 39% male (sample from fraternity houses) N participants: 4 houses, 991 individuals Allocation: n = 442 intervention; n = 549 control (unclear re: group allocation) Setting: college campus; higher risk students from fraternity and sorority houses Country: USA |
|
| Interventions |
Programme type: brief motivational interviewing Set‐up: individual single session Key components: brief motivational interview and normative feedback Duration: 10‐15 min Control: existing alcohol awareness programming on campus, which includes a social norms marketing campaign and required risk management educational programs on high‐risk drinking and related consequences |
|
| Outcomes |
Outcomes: estimated BAC and alcohol problems Measures: Modified Daily Drinking Questionnaire; Rutgers Alcohol Problem Index |
|
| Funding and Declared Conflicts of Interest | Funded by Social Sciences Program Enhancement Grant from the Florida State University (FSU) Council on Research and Creativity. No information or declarations about potential conflicts of interest | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | High risk | High attrition (80%) |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants unblinded. No information about blinding of MI counsellors |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information |
| Unit of Analysis issues | High risk | 1 intervention cluster removed from analysis because of untimely data. No adjustment for cluster effects, and ICC not reported. Study results removed from MA in a sensitivity analysis |
Wood 2007.
| Methods |
Design: RCT Follow‐up: 1, 3, 6 months Attrition: cumulative participant attrition was 17.6%, 24.5%, and 27.5% at 1‐, 3‐, and 6‐month follow‐ups, respectively |
|
| Participants |
Mean age (years): 20.5 Sex: 47.5% male N participants: 335 Allocation: not reported Setting: college campus; higher risk students Country: USA |
|
| Interventions |
Programme type: brief motivational interviewing Set up: individual single session Key components: a personalised feedback report, generated from the student's responses on the baseline assessment, was presented in order to guide the discussion, which focused on normative information, alcohol‐related consequences, and risk factors such as family history of alcoholism. Duration: 45‐60 min Control: assessment only |
|
| Outcomes |
Outcomes: alcohol use: total drinks in the past 30 days, past 30 days heavy episodic drinking; alcohol problems Measures: Timeline Followback; Young Adult Alcohol Problems Screening Test |
|
| Funding and Declared Conflicts of Interest | Supported by grant R29 AA12241 from the National Institute on Alcohol Abuse and Alcoholism to Mark Wood | |
| Notes | Study results not in right format for MA; authors contacted | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | High attrition at final follow‐up (27.5%) |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to intervention. Insufficient information to make judgement about blinding of therapists |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to permit judgement |
| Unit of Analysis issues | Low risk | Not applicable |
Wood 2010.
| Methods |
Design: RCT Follow‐up: 10, 22 months Attrition: 16% |
|
| Participants |
Mean age (years): 18.4 Sex: 57% female N participants: 1014 Allocation: n = 253 BMI; n = 256 PBI; n = 249 PBI + BMI; n = 256 control Setting: university; all students Country: USA |
|
| Interventions |
Programme type: brief motivational interviewing Set up: 2 individual sessions plus booster session Key components: questions on alcohol use, consequences, and socioenvironmental influences on college drinking Duration: initial BMI lasted approximately 45–60 min; booster session lasted 20–30 min Control: assessment only |
|
| Outcomes |
Outcomes: the number of times in the last month that students had consumed 5 or more drinks (4 or more for women) in a row; alcohol consequences Measures: Young Adult Alcohol Problems Screening Test |
|
| Funding and Declared Conflicts of Interest | Funded by NIDA. No information or declarations about potential conflicts of interest | |
| Notes | Study results not in right format for MA; authors contacted | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to make a judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low attrition (16%). Full‐information maximum likelihood estimation with robust standard error estimation, which assumes data are missing at random, was used in both Parts 1 and 2 |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes were reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to intervention. Insufficient information to make a judgement about blinding of therapists |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Interviewers were not members of the research team, were blind to experimental condition |
| Unit of Analysis issues | Low risk | Not applicable |
AAMC: Association of American Medical Colleges; BAC: blood alcohol concentration; BMI: brief motivational interviewing; CDC: Centers for Disease Control and Prevention; COI: conflict of interest; CS: counselling service; DSM IV: Diagnostic and Statistical Manual of Mental Disorders, 4th edition; DUI: driving under the influence; ER: emergency room; HED: heavy episodic drinkers; ICC: inter‐cluster correlation; ITT: intention‐to‐treat; LMC: lifestyle management class; MA: meta‐analysis; MCMC: Markov chain Monte Carlo; MET: motivational enhancement therapy; MI: motivational interviewing; NDHD: number of drinks on heavy drinking; NIAAA: National Institute on Alcohol Abuse and Alcoholism; NIDA: National Institute on Drug Abuse; NIH: National Institutes of Health: NIMH: National Institute of Mental Health; NHS: National Health System; PBI: performance based interviewing; PBSF: protective behavioral strategies feedback; PHDD: percentage of heavy drinking days; PNF: personalized normative feedback: Q/F/P: Quantity/Frequency/Peak; RAPI: Rutgers Alcohol Problems Index; RCT: randomised controlled trial; RSOD: risky single occasion drinking; SES: socioeconomic status; T‐ASI: Teen Addiction Severity Index; TEAP: Trainee Employee Assistance Program; TLFB: Timeline Followback; UAP: university assistance programme.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Baer 1992 | No control group |
| Battjes 2004 | Not RCT |
| Carey 2013b | 2 arms of this trial were non‐randomised (choice condition) |
| Collins 2002 | Mailed intervention |
| Cowell 2012 | Not RCT |
| Dauer 2005 | Participants over 25 years |
| Gregory 2001 | Not MI |
| Hayes 2007 | No control group |
| Hustad 2014 | Although this study followed a randomised controlled design with 2 intervention groups, it did not have a non‐MI control or comparison |
| Kypri 2008 | Not MI |
| Kypri 2009 | Not MI |
| LaBrie 2002 | No control group |
| LaBrie 2011 | No control group |
| Longabaugh 2001 | Participants over 25 years |
| Magill 2009 | No relevant outcomes |
| Maisto 2001 | Participants over 25 years |
| Morgenstern 2007 | Participants over 25 years |
| Morgenstern 2012 | Participants over 25 years |
| Murphy 2012b | No non‐MI control |
| Nirenberg 2013b | Follow‐up data collection referred to baseline time frame (methodological study) |
| Ondersma 2007 | Participants over 25 years |
| Peterson 2006 | Alcohol outcomes not reported separately |
| Potts 2001 | Not RCT |
| Smith 2003 | Participants over 25 years |
| Spirito 2011 | No non‐MI comparison group |
| Wei Sun 2006 | Not MI |
| Woodhall 2007 | Participants over 25 years |
MI: motivational interviewing; RCT: randomised controlled trial.
Characteristics of studies awaiting assessment [ordered by study ID]
Cunningham 2015.
| Methods | Parallel assignment randomised controlled trial |
| Participants | Patients aged 14‐20 in Emergency Department who screen positive for problematic alcohol use in past 3 months |
| Interventions | Adapted motivational enhancement therapy |
| Outcomes | Alcohol use; alcohol related consequences |
| Study identifier | NCT01051141 |
| Notes | Final data collection listed as March 2014. No results listed. |
ISRCTN31234060.
| Methods | Parallel assignment randomised controlled trial |
| Participants | Adolescents treated for intoxication in hospital emergency department |
| Interventions | Manualised brief motivational intervention |
| Outcomes | Binge‐drinking frequency |
| Study identifier | ISRCTN31234060 |
| Notes | Marked as completed |
NCT00229983.
| Methods | Parallel assignment, randomised controlled trial |
| Participants | 12−18 year‐old medical patients who use drugs |
| Interventions | Motivational enhancement therapy |
| Outcomes | Drug and alcohol use |
| Study identifier | NCT00229983 |
| Notes | Study has been listed as completed on the registry web site. No results are currently available. |
NCT00907309.
| Methods | Parallel assignment randomised controlled trial |
| Participants | 12‐21 year‐old medical patients attending for routine care |
| Interventions | Motivational enhancement therapy |
| Outcomes | Frequency of tobacco, alcohol, marijuana and other drug use |
| Study identifier | NCT00907309 |
| Notes | Study has been listed as completed on the registry web site. No results are currently available. |
NCT01128140.
| Methods | Single blind, parallel assignment, randomised controlled trial |
| Participants | Military personnel |
| Interventions | Motivational enhancement therapy |
| Outcomes | Timeline Follow back for alcohol (90 days) |
| Study identifier | NCT01128140 |
| Notes | Study has been listed as completed on the registry web site. No results are currently available. |
NCT01204229.
| Methods | Parallel assignment randomised controlled trial |
| Participants | College drinkers |
| Interventions | Motivational and cognitive intervention for drinkers |
| Outcomes | Alcohol consumption |
| Study identifier | NCT01204229 |
| Notes | Final data collection listed as May 2012. No results listed. |
NCT01546025.
| Methods | Single blind, parallel assignment, randomised controlled trial |
| Participants | Heavy drinkers aged 17‐20 |
| Interventions | Brief motivational counselling |
| Outcomes | Number of drinks per week, frequency of drinking, frequency of binge drinking, average BAC and peak BAC |
| Study identifier | NCT01546025 |
| Notes | Study has been listed as completed on the registry web site. No results are currently available. |
NCT01616212.
| Methods | Parallel assignment randomised controlled trial |
| Participants | Adolescent referred for alcohol or marijuana offence |
| Interventions | Motivational Enhancement Therapy for Adolescents |
| Outcomes | Adolescent Substance Use and Related Problems |
| Study identifier | NCT01616212 |
| Notes | Final data collection 2014. No results listed |
NCT02056535.
| Methods | Single blind, parallel assignment, randomised controlled trial |
| Participants | Young adults (aged 18‐30) admitted to Texas Tech Health Sciences Center ER in El Paso |
| Interventions | Brief motivational intervention |
| Outcomes | Change in the number of drinks per week and the number of drinks per drinking day |
| Study identifier | NCT02056535 |
| Notes | Study has been listed as completed on the registry web site. No results are currently available. |
NCT02252471.
| Methods | Parallel assignment randomised controlled trial |
| Participants | Female adolescents |
| Interventions | Motivational‐interviewing‐based counselling sessions |
| Outcomes | Risk of alcohol‐exposed pregnancy |
| Study identifier | NCT02252471 |
| Notes | Study listed as completed. No results posted |
Newbury‐Birch 2014.
| Methods | Cluster‐randomised controlled trial with parallel assignment |
| Participants | Students aged 14−15 from schools in the North East of England |
| Interventions | FRAMES approach for behaviour change plus 1 h of behaviour change counselling |
| Outcomes | Abstinence, daily quantity and total alcohol consumption |
| Study identifier | ISRCTN07073105 |
| Notes | Trial recorded as completed |
Walton 2012.
| Methods | Parallel assignment randomised controlled trial |
| Participants | Adolescents in urban primary care clinics |
| Interventions | Therapist delivered brief motivational intervention |
| Outcomes | alcohol use |
| Study identifier | NCT01329315 |
| Notes | Study completion date 2012 |
Characteristics of ongoing studies [ordered by study ID]
ACTRN12613000108718.
| Trial name or title | Brief telephone interventions for reducing future alcohol use and related harm in young people accessing emergency departments |
| Methods | Blinded parallel assignment randomised controlled trial |
| Participants | Aged 16‐25 years, and either consumed more than 6 standard drinks on 1 occasion in the previous 2 weeks or scored equal to or greater than 8 on the 10‐item Alcohol Use Disorders Identification Test (AUDIT) |
| Interventions | Telphone‐based motivational interviewing |
| Outcomes | Alcohol use (quantity/frequency of days alcohol use/days abstinent assessed on the Timeline Followback (TLFB) and related problems (e.g. social, medical, legal, family, vocational assessed on the Rutgers Alcohol Problem Index (RAPI) |
| Starting date | 4 March 2013 |
| Contact information | Dr Leanne Hides; leanne.hides@qut.edu.au |
| Study identifier | ACTRN12613000108718 |
| Notes | Due to be completed 2016 |
Differences between protocol and review
The protocol stated that the review would analyse data with a fixed‐effect model but then switch to a random‐effects model in the presence of heterogeneity based on the statistical test for heterogeneity. However, in the review the approach adopted was to use a random‐effects model throughout given the difference in study samples, interventions and measures.
Meta‐regression was not outlined in the protocol (although the intention was clearly stated in the objectives to consider duration as an effect modifier by comparing very brief MI versus longer MI). We adopted this particular statistical method after publication of the protocol.
We included additional subgroup analyses based on suggestions from other authors.
Contributions of authors
LC wrote the protocol. DF conducted the searches; DF, LC, NS, TM and SW undertook screening. LC, DA, NS, SW, TM and DF extracted data. SW and DF performed data analysis. SW drafted the initial version of the review. DF and LC edited the review.
Sources of support
Internal sources
Oxford Brookes University, UK.
External sources
None, Other.
Declarations of interest
Oxford Brookes University has received funding from the alcohol industry for prevention programme development and training. There is no perceived conflict of interest between that funding and this Cochrane review.
DF: none known.
LC: none known.
SW: none known.
DA: none known.
NS: none known.
TM: none known.
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Amaro 2009 {published data only}
- Amaro H, Ahl M, Matsumoto A, Prado G, Mule C, Kemmemer A, et al. Trial of the university assistance program for alcohol use among mandated students. Journal of Studies on Alcohol 2009;Suppl 16:45‐56. [DOI] [PMC free article] [PubMed] [Google Scholar]
Aubrey 1998 {unpublished data only}
- Aubrey LL. MI with adolescents presenting for outpatient substance abuse treatment. Dissertation Abstracts International: Section B: The Sciences and Engineering. 1998, pp. 1357.
Bailey 2004 {published data only}
- Bailey KA, Baker AL, Webster RA, Lewin TJ. Pilot randomized controlled trial of a brief alcohol intervention group for adolescents. Drug and Alcohol Review 2004;23(2):157–66. [DOI] [PubMed] [Google Scholar]
Barnett 2007 {published data only}
- Barnett N, Murphy JG, Colby SM, Monti PM. Efficacy of counselor vs. computer delivered intervention with mandated college students. Addictive Behavior 2007;32(11):2529‐48. [DOI] [PMC free article] [PubMed] [Google Scholar]
Barnett 2010 {published data only}
- Barnett NP, Apodaca TR, Magill M, Colby SM, Gwaltney C, Rohsenow D, et al. Moderators and mediators of two brief interventions for alcohol in the emergency department. Addiction 2010;105(3):452‐65. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bernstein 2010 {published data only}
- Bernstein J, Heeren T, Edward E, Dorfman D, Bliss C, Winter M, et al. A brief motivational interview in a pediatric emergency department, plus 10‐day telephone follow‐up, increases attempts to quit drinking among youth and young adults who screen positive for problematic drinking. Academic Emergency Medicine 2010;17(8):890‐902. [DOI] [PMC free article] [PubMed] [Google Scholar]
Borsari 2000 {published data only}
- Borsari B, Carey KB. Effects of brief motivational interviewing with college student drinkers. Journal of Consulting and Clinical Psychology 2000;68(4):728‐33. [PubMed] [Google Scholar]
Borsari 2005 {published data only}
- Borsari B, Carey KB. Two brief alcohol interventions for mandated college students. Psychology of Addictive Behaviors 2005;19(3):296‐302. [DOI] [PMC free article] [PubMed] [Google Scholar]
Borsari 2012 {published and unpublished data}
- Borsari B, Hustad JTP, Mastroleo NR, Tevyaw TOL, Barnett NP, Kahler CW, et al. Addressing alcohol use and problems in mandated college students: A randomized clinical trial using stepped care. Journal of Consulting and Clinical Psychology 2012;80(6):1062–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
Butler 2009 {published data only}
- Butler LH, Correia CJ. Brief alcohol intervention with college student drinkers: face‐to‐face versus computerized feedback. Psychology of Addictive Behaviors 2009;23(1):163‐7. [DOI] [PubMed] [Google Scholar]
Carey 2006 {published data only}
- Carey KB, Carey MP, Maisto SA, Henson JM. Brief motivational interventions for heavy college drinkers: a randomized controlled trial. Journal of Consulting and Clinical Psychology 2006;74(5):943‐54. [DOI] [PMC free article] [PubMed] [Google Scholar]
Carey 2009 {published and unpublished data}
- Carey KB, Henson JM, Carey MP, Maisto SA. Computer versus in‐person intervention for students violating campus alcohol policy. Journal of Consulting and Clinical Psycholology 2009;77(1):74–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
Carey 2011 {published and unpublished data}
- Carey KB, Carey MP, Henson JM, Maisto SA, DeMartini KS. Brief alcohol interventions for mandated college students: comparison of face‐to‐face counseling and computer‐delivered interventions. Addiction 2011;106(3):528‐37. [DOI] [PMC free article] [PubMed] [Google Scholar]
Carey 2013a {published data only}
- Carey KB, DeMartini KS, Prince MA, Luteran C, Carey MP. Effects of choice on intervention outcomes for college students sanctioned for campus alcohol policy violations. Psychology of Addictive Behaviors 2013;27(3):596–603. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ceperich 2011 {published data only}
- Ceperich SD, Ingersoll KS. Motivational interviewing + feedback intervention to reduce alcohol‐exposed pregnancy risk among college binge drinkers: determinants and patterns of response. Journal of Behavioural Medicine 2011;34(5):381‐95. [DOI] [PMC free article] [PubMed] [Google Scholar]
Christoff 2015 {published data only}
- Adriana de Oliveira Christoff, Roseli Boerngen‐Lacerda. Reducing substance involvement in college students:A three‐arm parallel‐group randomized controlled trial of a computer‐based intervention. Addictive Behaviors 2015;45:164‐71. [DOI] [PubMed] [Google Scholar]
Cimini 2009 {published data only}
- Cimini MD, Martens MP, Larimer ME, Kilmer JR, Neighbors C, Monserrat JM. Assessing the effectiveness of peer‐facilitated interventions addressing high‐risk drinking among judicially mandated college students. Journal of Studies on Alcohol and Drugs 2009;Suppl 16:57‐66. [DOI] [PMC free article] [PubMed] [Google Scholar]
Clair 2013 {published data only}
- Clair M, Stein LAR, Soenksen S, Martin RA, Lebeau R, Golembeske C. Ethnicity as a moderator of motivational interviewing for incarcerated adolescents after release. Journal of Substance Abuse Treatment 2013;45:370–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Clinton‐Sherrod 2011 {published data only}
- Clinton‐Sherrod M, Morgan‐Lopez A, Brown JM, McMillen BA, Cowell A. Incapacitated sexual violence involving alcohol among college women: the impact of a brief drinking intervention. Violence Against Women 2011;17(1):135‐54. [DOI] [PubMed] [Google Scholar]
D'Amico 2008 {published data only}
- D'Amico EJ, Miles JNV, Stern SA, Meredith LS. Brief motivational interviewing for teens at risk of substance use consequences: a randomized pilot study in a primary care clinic. Journal of Substance Abuse Treatment 2008;35(1):53–61. [DOI] [PubMed] [Google Scholar]
D'Amico 2013 {published data only}
- D’Amico EJ, Hunter SB, Miles JN, Ewing BA, Osilla KC. A randomized controlled trial of a group motivational interviewing intervention for adolescents with a first time alcohol or drug offense. Journal of Substance Abuse Treatment 2013;45(5):400‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Daeppen 2011 HED {published and unpublished data}
- Daeppen JB, Bertholet N, Gaume J, Fortini C, Faouzi M, Gmel G. Efficacy of brief motivational intervention in reducing binge drinking in young men: a randomized controlled trial. Drug and Alcohol Dependence 2011;113(1):69‐75. [DOI] [PubMed] [Google Scholar]
Daeppen 2011 non‐HED {published and unpublished data}
- Daeppen JB, Bertholet N, Gaume J, Fortini C, Faouzi M, Gmel G. Efficacy of brief motivational intervention in reducing binge drinking in young men: a randomized controlled trial. Drug and Alcohol Dependence 2011;113(1):69‐75. [DOI] [PubMed] [Google Scholar]
Dermen 2011 {published data only}
- Dermen KH, Thomas SN. Randomized controlled trial of brief interventions to reduce college students’ drinking and risky sex. Psychology of Addictive Behaviors 2011;25(4):583–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
Doumas 2008 {published data only}
- Doumas DM, Hannah E. Preventing high‐risk drinking in youth in the workplace: a web‐based normative feedback program. Journal of Substance Abuse Treatment 2008;34(3):263–71. [DOI] [PubMed] [Google Scholar]
Doumas 2011 {published data only}
- Doumas DM, Workman C, Smith D, Navarro A. Reducing high‐risk drinking in mandated college students: evaluation of two personalized normative feedback interventions. Journal of Substance Abuse Treatment 2011;40(4):376–85. [DOI] [PubMed] [Google Scholar]
Ewing 2009 {published data only}
- Ewing SW, LaChance HA, Bryan A, Hutchison KE. Do genetic and individual risk factors moderate the efficacy of motivational enhancement therapy? Drinking outcomes with an emerging adult sample. Addiction Biology 2009;14(3):356‐65. [DOI] [PMC free article] [PubMed] [Google Scholar]
Faris 2005 {unpublished data only}
- Faris AS. Examining process variables in a motivational intervention for college student drinkers. Dissertation Abstracts International: Section B: The Sciences and Engineering 2005;67(7‐B):4102. [Google Scholar]
Feldstein 2007 {published data only}
- Feldstein SW, Forcehimes AA. Motivational Interviewing with underage college drinkers: a preliminary look at the role of empathy and alliance. The American Journal of Drug and Alcohol Abuse 2007;33(5):737‐46. [DOI] [PubMed] [Google Scholar]
Fleming 2010 {published data only}
- Fleming MF, Balousek SL, Grossberg PM, Mundt MP, Brown D, Wiegel JR, et al. Brief physician advice for heavy drinking college students: a randomized controlled trial in college health clinics. Journal of Studies on Alcohol and Drugs 2010;71(1):23‐31. [DOI] [PMC free article] [PubMed] [Google Scholar]
Fromme 2004 MANDATED {published data only}
- Fromme K, Corbin W. Prevention of heavy drinking and associated negative consequences among mandated and voluntary college students. Journal of Consulting and Clinical Psychology 2004;72(6):1038‐49. [DOI] [PubMed] [Google Scholar]
Fromme 2004 VOLUNTARY {published data only}
- Fromme K, Corbin W. Prevention of heavy drinking and associated negative consequences among mandated and voluntary college students. Journal of Consulting and Clinical Psychology 2004;72(6):1038‐49. [DOI] [PubMed] [Google Scholar]
Gaume 2011 HED {published and unpublished data}
- Gaume J, Gmel G, Faouzi M, Bertholet N, Daeppen JB. Is brief motivational intervention effective in reducing alcohol use among young men voluntarily receiving it? A randomized controlled trial. Alcoholism: Clinical and Experimental Research 2011;35(10):1‐9. [DOI] [PubMed] [Google Scholar]
Gaume 2011 non‐HED {published and unpublished data}
- Gaume J, Gmel G, Faouzi M, Bertholet N, Daeppen JB. Is brief motivational intervention effective in reducing alcohol use among young men voluntarily receiving it? A randomized controlled trial. Alcoholism: Clinical and Experimental Research 2011;35(10):1‐9. [DOI] [PubMed] [Google Scholar]
Gaume 2014 {published data only}
- Jacques Gaume, Molly Magill, Richard Longabaugh, Nicolas Bertholet, Gerhard Gmel, andJean‐Bernard Daeppen. Influence of counselor characteristics and behaviors on the efficacy of a brief motivational intervention for heavy drinking in young men — a randomized controlled trial. Alcoholism, Clinical and Experimental Research 2014;38(7):2138‐47. [DOI] [PubMed] [Google Scholar]
Gmel 2013 {published and unpublished data}
- Gmel G, Gaume J, Bertholet N, Flückiger J, Daeppen JB. Effectiveness of a brief integrative multiple substance use intervention among young men with and without booster sessions. Journal of Substance Abuse Treatment 2013;44(2):231‐40. [DOI] [PubMed] [Google Scholar]
Gomez 2013 {unpublished data only}
- Gomez CD, Ngantcha M. [Admission aux urgences de Rennes des adolescents enivresse aiguë: Evaluation de l’impact à trois mois d’une intervention motivationnelle auprès des jeunes de 16 à 24 ans admis pour alcoolisation aiguë dans le service d’accueil des urgences de l’Hôpitalde Pontchaillou. Observatoire Français de Drogues et des Toxicomanies, 2013]. www.ofdt.fr/BDD/publications/docs/epfxcdtc.pdf (accessed 15 January 2016); Vol. ].
Goti 2010 {published data only}
- Goti J, Diaz R, Serrano L, Gonzalez L, Calvo R, Gual A, Castro J. Brief intervention in substance use among adolescent psychiatric patients: a randomized controlled trial. European Child and Adolescent Psychiatry 2010;19(6):503–11. [DOI] [PubMed] [Google Scholar]
Horner 2010 {unpublished data only}
- Horner KJ. Brief Motivational Interviewing: An Intervention for Alcohol Abusing College Students [unpublished PhD thesis]. State University of New York, 2010. [Google Scholar]
Juarez 2006 {published data only}
- Juarez P, Walters ST, Daugherty M, Radi CA. A randomized trial of motivational interviewing and feedback with heavy drinking college students. Journal of Drug Education 2006;36(3):233‐46. [DOI] [PubMed] [Google Scholar]
Kulesza 2010 {published data only}
- Kulesza M, Apperson M, Larimer M, Copeland A. Brief alcohol intervention for college drinkers: How brief is?. Addictive Behaviors 2010;35(7):730–3. [DOI] [PubMed] [Google Scholar]
LaBrie 2008 {published data only}
- LaBrie J, Huchtin K, Tawalbeh S, Pedersen ER, Thompson AD, Shelesky K, et al. A randomized motivational enhancement prevention group reduces drinking and alcohol consequences. Psychology of Addictive Behaviors 2008;22(1):149‐55. [DOI] [PMC free article] [PubMed] [Google Scholar]
LaBrie 2009 {published data only}
- LaBrie JW, Huchting KK, Lac A, Tawalbeh S, Thompson AD, Larimer MA. Preventing risky drinking in first‐year college women: further validation of a female‐specific motivational‐enhancement group intervention. Journal of Studies on Alcohol and Drugs 2009;Suppl 16:77‐85. [DOI] [PMC free article] [PubMed] [Google Scholar]
Larimer 2001 {published data only}
- Larimer ME, Turner AP, Anderson BK, Foder JS, Kilmer JR, Palmer RS, et al. Evaluating a brief alcohol intervention with fraternities. Journal of Studies on Alcohol 2001;62(3):370‐80. [DOI] [PubMed] [Google Scholar]
Marlatt 1998 {published data only}
- Baer JS, Kivlahan DR, Blume AW, McKnight P, Marlatt GA. Brief intervention for heavy‐drinking college students: 4‐year follow‐up and natural history. American Journal of Public Health 2001;91(8):1310‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marlatt GA, Baer JS, Kivlahan DR, Dimeff LA, Larimer ME, Quigley LA, et al. Screening and brief intervention for high‐risk college student drinkers results from a 2‐year follow‐up assessment. Journal of Consulting and Clinical Psychology 1998;66(4):604‐7. [DOI] [PubMed] [Google Scholar]
Marsden 2006 {published data only}
- Marsden J, Stillwell G, Barlow H, Boys A, Taylor C, Hunt N, et al. An evaluation of a brief motivational intervention among young ecstasy and cocaine users: no effect on substance and alcohol use outcomes. Addiction 2006;101(7):1014‐26. [DOI] [PubMed] [Google Scholar]
Martens 2013 {published data only}
- Martens MP, Smith AE, Murphy JG. The efficacy of single‐component brief motivational interventions among at‐risk college drinkers. Journal of Consulting and Clinical Psychology 2013;81(4):691–701. [DOI] [PMC free article] [PubMed] [Google Scholar]
McCambridge 2004 {published data only}
- McCambridge J, Strang J. Deterioration over time in effect of Motivational Interviewing in reducing drug consumption and related risk among young people. Addiction 2004;100(4):470‐8. [DOI] [PubMed] [Google Scholar]
- McCambridge J, Strang J. Efficacy of single session MI in reducing drug consumption and perceptions of drug‐related risk and harm among young people: results from a multi‐site cluster randomized trial. Addiction 22004;99(1):39‐52. [DOI] [PubMed] [Google Scholar]
McCambridge 2008 {published data only}
- McCambridge J, Slym R, Strang J. Randomized controlled trial of motivational interviewing compared with drug information and advice for early intervention among young cannabis users. Addiction 2008;103(11):1809–18. [DOI] [PubMed] [Google Scholar]
McCambridge 2011 {published data only}
- McCambridge J, Hunt C, Jenkins R, Strang J. Cluster randomised trial of the effectiveness of motivational interviewing for universal prevention. Drug and Alcohol Dependence 2011;114(2):177–84. [DOI] [PubMed] [Google Scholar]
Michael 2006 {published data only}
- Michael KD, Curtin L, Kirkley DE, Jones DL Harris R Jr. Group‐based motivational interviewing for alcohol use among college students: an exploratory study. Professional Psychology: Research and Practice 2006;37(6):629‐34. [Google Scholar]
Monti 1999 {published data only}
- Monti PM, Colby S, Barnett NP, Spirito A, Rohsenow DJ, Myers M, et al. Brief intervention for harm reduction with alcohol‐positive older adolescents in a hospital emergency department. Journal of Consulting and Clinical Psychology 1999;67(6):989‐94. [DOI] [PubMed] [Google Scholar]
Monti 2007 {published data only}
- Gwaltney CJ, Magill M, Barnett NP, Apodaca TR, Colby SM, Monti PM. Using daily drinking data to characterize the effects of a brief alcohol intervention in an emergency room. Addictive Behaviors 2011;36(3):248‐50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monti P, Barnett NP, Colby SM, Gwaltney CJ, Spirito A, Rohsenow DJ, et al. Motivational interviewing versus feedback only in emergency care for young adult problem drinking. Addiction 2007;102(8):1234–43. [DOI] [PubMed] [Google Scholar]
Murphy 2001 {published data only}
- Murphy JG, Duchnick JJ, Vuchinich RE, Davison JW, Karg R, Olson AM, et al. Relative efficacy of a brief motivational intervention for college student drinkers. Psychology of Addictive Behaviors 2001;15:373‐9. [DOI] [PubMed] [Google Scholar]
Murphy 2004 {published data only}
- Murphy JG, Benson TA, Vuchinich RE, Deskins MM, Eakin D, Flood AM, et al. A comparison of personalized feedback for college student drinkers delivered with and without a motivational interview. Journal of Studies on Alcohol 2004;65(2):200‐3. [DOI] [PubMed] [Google Scholar]
Murphy 2010a {published data only}
- Murphy J, Dennhardt A, Skidmore J, Martens M, McDevitt‐Murphy M. Computerized versus motivational interviewing alcohol interventions: impact on discrepancy, motivation, and drinking. Psychology of Addictive Behaviors 2010;24(4):628–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
Murphy 2010b {published data only}
- Murphy J, Dennhardt A, Skidmore J, Martens M, McDevitt‐Murphy M. Computerized versus motivational interviewing alcohol interventions: impact on discrepancy, motivation, and drinking. Psychology of Addictive Behaviors 2010;24(4):628–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
Murphy 2012a {published data only}
- Murphy D, Chen X, Naar‐King S, Parsons JT. Alcohol and marijuana use outcomes in the healthy choices motivational interviewing intervention for HIV‐positive youth. Aids Patient Care and STDS 2012;26(2):95‐100. [DOI] [PMC free article] [PubMed] [Google Scholar]
Naar‐King 2006 {published data only}
- Naar‐King S, Lam P, Wang B, Wright K, Parsons JT, Frey MA. Brief report: maintenance of effects of motivational enhancement therapy to improve risk behaviors and HIV‐related health in a randomized controlled trial of youth living with HIV. Journal of Pediatric Psychology 2008;33(4):441‐5. [DOI] [PubMed] [Google Scholar]
- Naar‐King S, Wright K, Parsons JT, Frey M, Templin T, Lam P, et al. Healthy choices: motivational enhancement therapy for health risk behaviors in HIV‐positive youth. AIDS Education and Prevention 2006;18(1):1‐11. [DOI] [PubMed] [Google Scholar]
Nirenberg 2013 {published data only}
- Nirenberg T, Longabaugh R, Baird J, Mello MJ. Treatment may influence self‐report and jeopardize our understanding of outcome. Journal of Studies on Alcohol and Drugs 2013;74(5):770‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Palmer 2004 {unpublished data only}
- Palmer RS. Efficacy of the Alcohol Skills Training Program in Mandated and Non‐mandated Heavy Drinking College Students [unpublished PhD thesis]. University of Washington, 2004. [Google Scholar]
Rongklavit 2013 {published data only}
- Rongkavilit C, Naar‐King S, Wang B, Panthong A, Bunupuradah T, Parsons JT, et al. Motivational interviewing targeting risk behaviors for youth living with HIV in Thailand. AIDS an Behavior 2013;17(6):2063–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
Schaus 2009 {published data only}
- Schaus JF, Sole ML, McCoy TP, Mullett N, O'Brien MC. Alcohol screening and brief intervention in a college student health centre: a randomized trial. Journal of Studies on Alcohol and Drugs 2009;16:131‐41. [DOI] [PMC free article] [PubMed] [Google Scholar]
Schmiege 2009 {published data only}
- Bryan AD, Schmiege SJ, Broaddus MR. HIV risk reduction among detained adolescents: a randomized, controlled trial. Pediatrics 2009;124(6):e1180‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmiege SJ, Broaddus MR, Levin M, Bryan AD. Randomized trial of group interventions to reduce HIV/STD risk and change theoretical mediators among detained adolescents. Journal of Consulting and Clinical Psychology 2009;77(1):38‐50. [DOI] [PMC free article] [PubMed] [Google Scholar]
Segatto 2010 {published data only}
- Segatto ML, Andreoni S, Souza e Silva R, Diehl A, Pinsky I. Intervenção motivacional breve e brochura educacional em pronto‐socorro para adolescentes e adultos jovens com problemas relacionados ao álcool: um ensaio clínico simples cego randomizado. [Brief motivational interview and educational brochure in emergency room settings for adolescents and young adults with alcohol related problems: a randomized single blind clinical trial]. Revista Brasileira de Psiquiatria 2010;33(3):225‐33. [DOI] [PubMed] [Google Scholar]
Spirito 2004 {published data only}
- Spirito A, Monti PM, Barnett NP, Colby SM, Sindelar H, Rohsenow DJ, et al. A randomized clinical trial of a brief motivational intervention for alcohol‐positive adolescents treated in an emergency department. Journal of Pediatrics 2004;145(3):396‐402. [DOI] [PubMed] [Google Scholar]
Steele Seel 2010 {published data only}
- Steele Seel JM. Eliciting Abstinence and Improving Retention in a Vocational and Educational Training Program for Young People: A Pilot Study. Albuquerque, NM: University of New Mexico, 2010. [Google Scholar]
Stein 2006 {published data only}
- Stein LAR, Colby SM, Barnett NP, Monti PM, Golembeske C, Lebeau‐Craven R. Effects of motivational interviewing for incarcerated adolescents on driving under the influence after release. American Journal on Addictions 2006;15(1):50‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Stein 2011 {published data only}
- Stein L, Lebau R, Colby S, Barnett N, Golombeske C, Monti P. Motivational interviewing for incarcerated adolescents: effects of depressive symptoms on reducing alcohol and marijuana use after release. Journal of Studies on Alcohol and Drugs 2011;72:497–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
Terlecki 2010 MANDATED {published data only}
- Terlecki MA, Larimer ME, Copeland AL. Clinical outcomes of a brief motivational intervention for heavy drinking mandated college students: a pilot study. Journal of Studies on Alcohol and Drugs 2010;71(1):54‐60. [DOI] [PubMed] [Google Scholar]
Terlecki 2010 VOLUNTARY {published data only}
- Terlecki MA, Larimer ME, Copeland AL. Clinical outcomes of a brief motivational intervention for heavy drinking mandated college students: a pilot study. Journal of Studies on Alcohol and Drugs 2010;71(1):54‐60. [DOI] [PubMed] [Google Scholar]
Terlecki 2011 MANDATED {unpublished data only}
- Terlecki M. The Long‐term Effect of a Brief Motivational Alcohol Intervention for Heavy Drinking Mandated College Students [PhD thesis]. Baton Rouge, LA: Louisiana State University and Agricultural and Mechanical College, 2010. [Google Scholar]
Terlecki 2011 VOLUNTARY {published data only}
- Terlecki M. The Long‐term Effect of a Brief Motivational Alcohol Intervention for Heavy Drinking Mandated College Students [PhD thesis]. Baton Rouge, LA: Louisiana State University and Agricultural and Mechanical College, 2011. [Google Scholar]
Thush 2009 {published data only}
- Thrush C, Wiers RW, Moerbeek M, Ames SL, Grenard JL, Sussman S, Stacy AW. Influence of motivational interviewing on explicit and implicit alcohol‐related cognition and alcohol use in at‐risk adolescents. Psychology of Addictive Behaviors 2009;23(1):146‐51. [DOI] [PMC free article] [PubMed] [Google Scholar]
Turrisi 2009 {published data only}
- Turrisi R, Larimer ME, Mallett KA, Kilmer JR, Ray AE, Mastroleo NR, et al. A randomized clinical trial evaluating a combined alcohol intervention for high‐risk college students. Journal of Studies on Alcohol and Drugs 2009;70(4):555‐67. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wagener 2012 {published data only}
- Wagener TL, Leffingwell TR, Mignogna J, Mignogna MR, Weaver CC, Cooney NJ, et al. Randomized trial comparing computer‐delivered and face‐to‐face personalized feedback interventions for high‐risk drinking among college students. Journal of Substance Abuse Treatment 2012;43:260–7. [DOI] [PubMed] [Google Scholar]
Walters 2000 {published data only}
- Walters ST, Bennett ME, Miller JE. Reducing alcohol use in college students: a controlled trial of two brief interventions. Journal of Drug Education 2000;30(3):361‐72. [DOI] [PubMed] [Google Scholar]
Walters 2009 MIF v FBO {published data only}
- Walters ST, Vader AM, Harris TR. Dismantling motivational interviewing and feedback for college drinkers: a randomized clinical trial. Journal of Consulting and Clinical Psychology 2009;77(1):64‐73. [DOI] [PMC free article] [PubMed] [Google Scholar]
Walters 2009 MIO v AO {published data only}
- Walters ST, Vader AM, Harris TR. Dismantling motivational interviewing and feedback for college drinkers: a randomized clinical trial. Journal of Consulting and Clinical Psychology 2009;77(1):64‐73. [DOI] [PMC free article] [PubMed] [Google Scholar]
Walton 2010 {published data only}
- Cunningham RM, Chermack ST, Zimmerman MA, Shope JT, Bingham R, Blow FC, et al. Brief motivational interviewing intervention for peer violence and alcohol use in teens: one‐year follow‐up. Pediatrics 2012;129(6):1083‐90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walton M, Chermack S, Shope J, Bingham R, Zimmerman M, Blow F, et al. Effects of a brief intervention for reducing violence and alcohol misuse among adolescents: a randomized controlled trial. JAMA 2010;304(5):527‐35. [DOI] [PMC free article] [PubMed] [Google Scholar]
White 2007 {published data only}
- White HR, Morgan TJ, Pugh LA, Celinska K, Labouvie EW, Pandina RJ. Evaluating two brief substance‐use interventions for mandated college students. Journal of Studies on Alcohol 2006;67(2):309‐17. [DOI] [PubMed] [Google Scholar]
- White HR, Mun EY, Pugh L, Morgan TJ. Long‐term effects of brief substance use interventions for mandated college students: sleeper effects of an in‐person personal feedback intervention. Alcoholism Clinical and Experimental Research 2007;31(8):1380‐91. [DOI] [PubMed] [Google Scholar]
Wilke 2014 {published and unpublished data}
- Wilke DJ, Mennicke A, Howell RL, Magnuson AB. A peer‐facilitated intervention to reduce risky drinking among fraternity and sorority members. Journal of Social Work Practice in the Addictions 2014;14(1):42‐63. [Google Scholar]
Wood 2007 {published data only}
- Wood MD, Capone C, Laforge R, Erickson DJ, Brand NH. Brief motivational intervention and alcohol expectancy challenge with heavy drinking college students: a randomized factorial study. Addictive Behaviors 2007;32(11):2509–28. [DOI] [PubMed] [Google Scholar]
Wood 2010 {published data only}
- Wood M, Fairlie A, Borsari B, Capone C, Fernandez A, Laforge R, et al. Brief motivational and parent interventions for college students: a randomized factorial study. Journal of Consulting and Clinical Psychology 2010;78(3):349–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies excluded from this review
Baer 1992 {published data only}
- Baer JS, Marlatt GA, Kivlahan DR, Fromme K, Larimer ME, Williams E. An experimental test of three methods of alcohol risk reduction with adults. Journal of Consulting and Clinical Psychology 1992;60(6):974‐9. [DOI] [PubMed] [Google Scholar]
Battjes 2004 {published data only}
- Battjes RJ, Gordon MS, O'Grady KE, Kinlock TW, Katz EC, Sears EA. Evaluation of a group‐based substance abuse treatment program for adolescents. Journal of Substance Abuse Treatment 2004;27(2):123‐34. [DOI] [PubMed] [Google Scholar]
Carey 2013b {published data only}
- Carey KB, DeMartini KS, Prince MA, Luteran C, Carey MP. Effects of choice on intervention outcomes for college students sanctioned for campus alcohol policy violations. Psychology of Addictive Behaviors 2013;27(3):596‐603. [DOI] [PMC free article] [PubMed] [Google Scholar]
Collins 2002 {published data only}
- Collins SE, Carey KB, Sliwinski MJ. Mailed personalized normative feedback as a brief intervention for at‐risk college drinkers. Journal of Studies on Alcohol 2002;63(5):559‐67. [DOI] [PubMed] [Google Scholar]
Cowell 2012 {published data only}
- Cowell AJ, Brown JM, Mills MJ, Bender RH, Wedehase BJ. Cost‐effectiveness analysis of motivational interviewing with feedback to reduce drinking among a sample of college students. Journal of Studies on Alcohol and Drugs 2012;73(2):226‐37. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dauer 2005 {published data only}
- Dauer ARM, Rubio ES, Coris ME, Valls JM. Brief Intervention in alcohol‐positive traffic casualties: is it worth the effort?. Alcohol and Alcoholism 2006;41(1):76‐83. [DOI] [PubMed] [Google Scholar]
Gregory 2001 {unpublished data only}
- Gregory BM. College Alcohol and Life Skills Study with Student‐Athletes [unpublished PhD thesis abstract: 2001‐95013‐033] 2001.
Hayes 2007 {unpublished data only}
- Hayes, BB. Comparing the effectiveness of cognitive‐behavioral group therapy with and without motivational interviewing at reducing the social anxiety, alcohol consumption, and negative consequences of socially anxious college students. Dissertation Abstracts International: Section B: The Sciences and Engineering 67(9‐B):5405. [Google Scholar]
Hustad 2014 {published data only}
- Hustad JT, Mastroleo NR, Kong L, Urwin R, Zeman S, Lasalle L, Borsari B. The comparative effectiveness of individual and group brief motivational interventions for mandated collegestudents. Psychology of Addictive Behaviors 2014;28(1):74–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kypri 2008 {published data only}
- Kypri K, Langley JD, Saunders JB, Cashell‐Smith ML, Herbison P. Randomized controlled trial of web‐based alcohol screening and brief intervention in primary care. Archives of Internal Medicine 2008;168(5):530‐6. [DOI] [PubMed] [Google Scholar]
Kypri 2009 {published data only}
- Kypri K, Hallett J, Howat P, McManus A, Maycock B, Bowe S, et al. Randomized controlled trial of proactive web‐based alcohol screening and brief intervention for university students. Archives of Internal Medicine 2009;169(16):1508‐14. [DOI] [PubMed] [Google Scholar]
LaBrie 2002 {published data only}
- LaBrie JW. Weighing the pros and cons: A brief motivational intervention reduces risk associated with drinking and unsafe sex. Dissertation Abstracts International 2002.
LaBrie 2011 {published data only}
- LaBrie J, Cail J, Pedersen E, Migliuri S. Reducing alcohol risk in adjudicated male college students: further validation of a group motivational enhancement intervention. Journal of Child & Adolescent Substance Abuse 2011;20(1):82–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
Longabaugh 2001 {published data only}
- Longabaugh R, Woolard RE, Nirenberg TD, Minugh AP, Becker B, Clifford PR, et al. Evaluating the effects of a brief motivational intervention for injured drinkers in the emergency department. Journal of Studies on Alcohol 2001;62(6):806‐16. [DOI] [PubMed] [Google Scholar]
Magill 2009 {published data only}
- Magill M, Barnett NP, Apodaca TR, Rohsenow DJ, Monti PM. The role of marijuana use in brief motivational intervention with young adult drinkers treated in an emergency department. Journal of Studies on Alcohol and Drugs 2009;70(3):409‐13. [DOI] [PMC free article] [PubMed] [Google Scholar]
Maisto 2001 {published data only}
- Maisto SA, Conigliaro J, McNeil M, Kraemer K, Conigliaro RL, Kelley ME. Effects of two types of brief intervention and readiness to change on alcohol use in hazardous drinkers. Journal of Studies on Alcohol 2001;62(5):605‐14. [DOI] [PubMed] [Google Scholar]
Morgenstern 2007 {published data only}
- Morgenstern J, Irwin TW, Wainberg ML, Parsons JT, Muench F, Bux DA Jr, et al. A randomized controlled trial of goal choice interventions for alcohol use disorders among men who have sex with men. Journal of Consulting and Clinical Psychology 2007;75(1):72‐84. [DOI] [PubMed] [Google Scholar]
Morgenstern 2012 {published data only}
- Morgenstern J, Kuerbis A, Amrhein P, Hail L, Lynch K, McKay JR. Motivational interviewing: a pilot test of active ingredients and mechanisms of change. Psychology of Addictive Behaviors 2012;26(4):859–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
Murphy 2012b {published data only}
- Murphy JG, Dennhardt AA, Skidmore JR, Borsari B, Barnett NP, Colby SM, et al. A randomized controlled trial of a behavioral economic supplement to brief motivational interventions for college drinking. Journal of Consulting and Clinical Psychology 2012;80(5):876–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
Nirenberg 2013b {published data only}
- Nirenberg T, Baird J, Longabaugh R, Mello MJ. Motivational counseling reduces future police charges in court referred youth. Accident Analysis and Prevention 2013;53:89–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ondersma 2007 {published data only}
- Ondersma SJ, Svikis DS, Schuster CR. Computer‐based brief intervention: a randomized trial with postpartum women. American Journal of Preventive Medicine 2007;32(3):232‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Peterson 2006 {published data only}
- Peterson PL, Baer JS, Wells EA, Ginzler JA, Garrett SB. Short‐term effects of a brief motivational intervention to reduce alcohol and drug risk among homeless adolescents. Psychology of Addictive Behaviors 2006;20(3):254‐64. [DOI] [PubMed] [Google Scholar]
Potts 2001 {unpublished data only}
- Potts KAF. Efficacy of the Alcohol Skills Training Program, a Brief Group Intervention for High Risk College Student Drinkers [unpublished PhD thesis]. Lincoln, NE: University of Nebraska, 2001. [Google Scholar]
Smith 2003 {published data only}
- Smith AJ, Hodgson RJ, Bidgeman K, Sheherd JP. A randomized controlled trial of a brief intervention after alcohol‐related facial injury. Addiction 2003;98(1):43‐52. [DOI] [PubMed] [Google Scholar]
Spirito 2011 {published data only}
- Spirito A, Sindelar‐Manning H, Colby SM, Barnett NP, Lewander W, Rosenhow DJ, et al. Individual and family motivational interventions for alcohol‐positive adolescents treated in an emergency department: results of a randomized clinical trial. Archives of Pediatrics and Adolescent Medicine 2011;165(3):269‐74. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wei Sun 2006 {published data only}
- Sun W, Skara S, Sun P, Dent CW, Sussman S. Project towards no drug abuse: long‐term substance use outcomes evaluation. Preventive Medicine 2006;42(3):188‐92. [DOI] [PubMed] [Google Scholar]
Woodhall 2007 {published data only}
- Woodhall WG, Delaney HD, Kunitz SJ, Westerberg VS, Zhao H. A randomized trial of a DWI Intervention program for first offenders: intervention outcomes and interactions with antisocial personality disorder among a primarily American‐Indian sample. Alcoholism: Clinical and Experimental Research 2007;31(6):974‐87. [DOI] [PubMed] [Google Scholar]
References to studies awaiting assessment
Cunningham 2015 {published data only}
- Cunningham RM, Chermack ST, Ehrlich PF, Carter PM, Booth BM, Blow FC, et al. Alcohol interventions among underage drinkers in the ED: a randomized controlled trial. Pediatrics 2015;136(4):e783‐93. [DOI: 10.1542/peds.2015-1260] [DOI] [PMC free article] [PubMed] [Google Scholar]
ISRCTN31234060 {published data only}
- ISRCTN31234060. Brief motivational intervention in adolescents treated in emergency departments for acute alcohol intoxication: a randomized controlled trial. http://www.isrctn.com/ISRCTN31234060 (accessed 1 April 2016). [DOI] [PMC free article] [PubMed]
NCT00229983 {published data only}
- NCT00229983. Medical office intervention for adolescent drug use. https://clinicaltrials.gov/show/NCT00229983 (accessed 1 April 2016).
NCT00907309 {published data only}
- NCT00907309. Dental and medical office iMET to reduce teen tobacco, alcohol, and drug use. https://clinicaltrials.gov/show/NCT00907309 (accessed 1 April 2016).
NCT01128140 {published data only}
- NCT01128140. Efficacy trial of warrior check‐up. https://clinicaltrials.gov/show/NCT01128140 (accessed 1 April 2016).
NCT01204229 {published data only}
- NCT01204229. Motivational and cognitive intervention for college drinkers (MCID). https://clinicaltrials.gov/show/NCT01204229 (accessed 1 April 2016).
NCT01546025 {published data only}
- NCT01546025. Brief alcohol intervention for school‐to‐work transitions. https://clinicaltrials.gov/show/NCT01546025 (accessed 1 April 2016).
NCT01616212 {published data only}
- NCT01616212. Early intervention for minors in possession of alcohol/drugs: a feasibility study (MAST1). https://clinicaltrials.gov/show/NCT01616212 (accessed 1 April 2016).
NCT02056535 {published data only}
- NCT02056535. Screening and brief intervention in the ED among Mexican‐origin young adults. https://clinicaltrials.gov/show/NCT02056535 (accessed 1 April 2016).
NCT02252471 {published data only}
- NCT02252471. Choices‐teen: a bundled risk reduction intervention for juvenile justice females. https://clinicaltrials.gov/show/NCT02252471 (accessed 1 April 2016).
Newbury‐Birch 2014 {published data only}
- Newbury‐Birch D, Scott S, O’Donnell A, Coulton S, Howel D, McColl E, et al. A pilot feasibility cluster randomised controlled trial of screening and brief alcohol intervention to prevent hazardous drinking in young people aged 14–15 years in a high school setting (SIPS JR‐HIGH). Public Health Research. NIHR Journals Library 2014;No. 2.6:Available from: http://www.ncbi.nlm.nih.gov/books/NBK263999/. [DOI: 10.3310/phr02060] [DOI] [PubMed] [Google Scholar]
Walton 2012 {published data only}
- Walton MA, Bohnert K, Resko S, Barry KL, Chermack ST, Zucker RA, et al. Computer and therapist based brief interventions among cannabis‐using adolescents presenting to primary care: one year outcomes. Drug and Alcohol Dependence 2013;132(3):646‐53. [DOI: 10.1016/j.drugalcdep.2013.04.020] [DOI] [PMC free article] [PubMed] [Google Scholar]
References to ongoing studies
ACTRN12613000108718 {published data only}
- ACTRN12613000108718. Brief telephone delivered personality‐targeted versus standard motivational interviewing for for reducing future alcohol use and related harm in young people accessing emergency departments. https://www.anzctr.org.au/Trial/Registration/TrialReview.aspx?ACTRN=12613000108718 (accessed 1 April 2016).
Additional references
Bandura 1977
- Bandura A. Social Learning Theory. Englewood Cliffs, NJ: Prentice Hall, 1977. [Google Scholar]
Bertholet 2014
- Bertholet N, Palfai T, Gaume J, Daeppen JB, Saitz R. Do brief alcohol motivational interventions work like we think they do?. Alcoholism: Clinical and Experimental Research 2014;38(3):853‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Burke 2002a
- Burke BL, Vassilev G, Kantchelov A, Zweben A. Motivational interviewing with couples. Motivational Interviewing: Preparing People for Change. 2nd Edition. New York: Guilford Press, 2002:347‐61. [Google Scholar]
Burke 2002b
- Burke B, Arkowitz H, Dunn C. The efficacy of motivational interviewing. In: W.R. Miller, S. Rollnick editor(s). Motivational interviewing: Preparing People for Change. 2nd Edition. New York: Guilford Press, 2002:217‐50. [Google Scholar]
Burke 2003
- Burke BL, Arkowitz H, Menchola M. The efficacy of motivational interviewing: a meta‐analysis of controlled clinical trials. Journal of Consulting and Clinical Psychology 2003;71(5):843‐61. [DOI] [PubMed] [Google Scholar]
Carey 2007
- Carey KB, Henson JM, Carey MP, Maisto SA. Which heavy drinking college students benefit from a brief motivational intervention?. Journal of Consulting and Clinical Psychology 2007;75(4):663‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Collins1985
- Collins RL, Parks GA, Marlatt GA. Social determinants of alcohol consumption: The effects of social interaction and model status on the self‐administration of alcohol. Journal of Consulting and Clinical Psychology 1985;53(2):189‐200. [DOI] [PubMed] [Google Scholar]
CONSORT 2010
- CONSORT. Consolidated Standards of Reporting Trials. Library for health research reporting. http://www.equator‐network.org/resource‐centre/library‐of‐health‐research‐reporting/ (accessed 16 July 2010).
Corrao 1999
- Corrao G, Bagnardi V, Zambon A, Arico S. Exploring the dose‐response relationship between alcohol consumption and the risk of several alcohol‐related conditions: a meta‐analysis. Addiction 1999;94(10):1551‐73. [DOI] [PubMed] [Google Scholar]
Dunn 2001
- Dunn C, Deroo L, Rivara FP. The use of brief interventions adapted from motivational interviewing across behavioral domains: a systematic review. Addiction 2001;96(12):1725‐42. [DOI] [PubMed] [Google Scholar]
Edwards 1994
- Edwards AP, Babor G, Casswell TF, Ferrence S. The individual's drinking and degree of risk. Alcohol Policy and the Public Good. Oxford: Oxford University Press, 1994. [Google Scholar]
Fewtrell 2008
- Fewtrell MS, Kennedy K, Singhal A, Martin RM, Ness A, Hadders‐Algra M, et al. How much loss to follow‐up is acceptable in long‐term randomised trials and prospective studies?. Archives of Disease in Childhood 2008;93(6):458‐61. [DOI] [PubMed] [Google Scholar]
Foxcroft 2014
- Foxcroft DR. Can prevention classification be improved by considering the function of prevention?. Prevention Science 2014;15(6):818‐22. [DOI] [PubMed] [Google Scholar]
Foxcroft 2015
- Foxcroft DR, Moreira M, Almeida Santimano NML, Smith LA. Social norms information for alcohol misuse in university and college students. Cochrane Database of Systematic Reviews 2015, Issue 12. [DOI: 10.1002/14651858.CD006748.pub4] [DOI] [PMC free article] [PubMed] [Google Scholar]
GRADE 2004
- The GRADE working group. Grading quality of evidence and strength of recommendations.. BMJ 2004;328(7454):1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
Grant 2015
- Grant S, Pedersen ER, Osilla KC, Kulesza M, D'Amico E J. Reviewing and interpreting the effects of brief alcohol interventions: comment on a Cochrane review about motivational interviewing for young adults. Addiction 2015 [Epub ahead of print]. [DOI: 10.1111/add.13136] [DOI] [PMC free article] [PubMed] [Google Scholar]
Greenfield 2001
- Greenfield TK. Individual risk of alcohol related disease and problems. In: Heather N, Stockwell T editor(s). International Handbook of Alcohol Dependence and Problems. Chichester, UK: John Wiley & Sons, 2001:413‐438. [Google Scholar]
Grenard 2006
- Grenard JL, Ames SL, Pentz MA, Sussman S. Motivational interviewing with adolescents and young adults for drug‐related problems. Int J Adolesc Med Health 2006;18(1):53‐67. [DOI] [PubMed] [Google Scholar]
Guyatt 2008
- Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck‐Ytter Y, Alonso‐Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008;336(7560):924‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Guyatt 2011
- Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, et al. GRADE guidelines 1. Introduction‐GRADE evidence profiles and summary of findings tables. Journal of Clinical Epidemiology 2011;64(4):383‐94. [DOI] [PubMed] [Google Scholar]
Hettema 2005
- Hettema J, Steele J, Miller WR. Motivational Interviewing. Annual Review of Clinical Psychology 2005;1:91‐111. [DOI] [PubMed] [Google Scholar]
Higgins 2011a
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Higgins 2011b
- Higgins JPT, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011;343:d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hrobjartsson 2014
- Hrobjartsson A, Emanuelsson F, Skou Thomsen AS, Hilden J, Brorson S. Bias due to lack of patient blinding in clinical trials. A systematic review of trials randomizing patients to blind and nonblind sub‐studies. International Journal of Epidemiology 2014;43(4):1272‐83. [DOI] [PMC free article] [PubMed] [Google Scholar]
Huh 2015
- Huh D, Mun EY, Larimer ME, White HR, Ray AE, Rhew IC, et al. Brief motivational interventions for college student drinking may not be as powerful as we think: an individual participant‐level data meta‐analysis. Alcoholism: Clinical and Experimental Research 2015;39(5):919‐31. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kohler 2015
- Kohler S, Hofmann A. Can motivational interviewing in emergency care reduce alcohol consumption in young people? A systematic review and meta‐analysis. Alcohol and Alcoholism 2015;50(2):107‐17. [DOI] [PubMed] [Google Scholar]
Larimer 2007
- Larimer ME, Cronce JM. Identification, prevention, and treatment revisited: individual‐focused college drinking prevention strategies 1999–2006. Addictive Behaviors 2007;32(11):2439–68. [DOI] [PubMed] [Google Scholar]
Lundahl 2010
- Lundahl BW, Kunz C, Brownell C, Tollefson D, Burke BL. A meta‐analysis of motivational interviewing: twenty‐five years of empirical studies. Database of Abstracts of Reviews of Effects (DARE): Quality‐assessed Reviews. 2010;20(2):137‐60. [Google Scholar]
Maisto 1999
- Maisto SA, Carey KB, Bradizza CM. Social learning theory. In: Blane HT, Leonard KE editor(s). Psychological Theories of Drinking and Alcoholism. 2nd Edition. New York: Guilford Press, 1999:106‐163. [Google Scholar]
Miller 1983
- Miller WR. Motivational interviewing with problem drinkers. Behavioral Psychotherapy 1983;11(2):147‐72. [Google Scholar]
Miller 1993
- Miller WR, Benefield RG, Tonigan JS. Enhancing motivation for change in problem drinking; a controlled comparison of two therapist styles. Journal of Consulting and Clinical Psychology 1993;61:455‐61. [DOI] [PubMed] [Google Scholar]
Miller 1995a
- Miller WR, Rollnick S. What is motivational interviewing?. Behavioral and Cognitive Psychotherapy 1995;23(4):325–34. [DOI] [PubMed] [Google Scholar]
Miller 1995b
- Miller WR, Tonigan JS, Longabaugh R. The Drinker Inventoryof Consequences (DrInC): An Instrument for Accessing Adverse Consequences of Alcohol Abuse (Test Manual). NIAAA Project MATCH Monograph Series, NIH Publication No. 95‐3911. Vol. 4, Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism, 1995. [Google Scholar]
Miller 1996
- Miller WR. Motivational interviewing: research, practice, and puzzles. Addictive Behaviors 1996;21:835‐42. [DOI] [PubMed] [Google Scholar]
Miller 2002
- Miller WR, Rollnick S. Motivational Interviewing: Preparing People to Change Addictive Behavior. New York: Guilford Press, 2002. [Google Scholar]
Mun 2015
- Mun EY, Atkins DC, Walters ST. Is motivational interviewing effective at reducing alcohol misuse in young adults: a critical review of Foxcroft et al. (2014). Psychology of Addictive Behaviours 2015;29(4):836‐46. [PUBMED: 26237287] [DOI] [PMC free article] [PubMed] [Google Scholar]
Noonan 1997
- Noonan WC, Myers TB. Motivational interviewing: a review. Journal of Substance Misuse 1997;2:8‐16. [Google Scholar]
O' Leary 2004
- O' Leary TT, Monti PM. Motivational enhancement and other brief interventions for adolescent substance abuse: foundations, applications and evaluations. Addiction 2004;99(Suppl 2):63‐75. [DOI] [PubMed] [Google Scholar]
Paterson 1985
- Paterson GA, Forgatch MS. Therapist behavior as a determinant for client non compliance: a paradox for the behavior modifier. Journal of Consulting and Clinical Psychology 1985;53:846‐51. [DOI] [PubMed] [Google Scholar]
Petrosino 2005
- Petrosino A, Soydan H. The impact of program developers as evaluators on criminal recidivism: results from meta‐analyses of experimental and quasi‐experimental research. Journal of Experimental Criminology 2005;1(4):435‐50. [Google Scholar]
Prochaska 1992
- Prochaska JO, DiClemente CC, Norcross JC. In search of how people change: applications to addictive behaviors. American Psychologist 1992;47:1102‐14. [DOI] [PubMed] [Google Scholar]
RevMan 2014 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Rubak 2006
- Rubak S, Sandbaek A, Lauritzen T, Christensen B. Motivational interviewing: a systematic review and meta‐analysis. British Journal of General Practice 2006;55(513):305‐12. [PMC free article] [PubMed] [Google Scholar]
Saunders 1993
- Saunders JB, Aasland OG, Babor TF, Delafuente JR, Grant M. Development of the Alcohol‐Use Disorders IdentificationTest (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption. Addiction 1993;88(6):791–804. [DOI] [PubMed] [Google Scholar]
Smedslund 2011
- Smedslund G, Berg RC, Hammerstrøm KT, Steiro A, Leiknes KA, Dahl HM, et al. Motivational interviewing for substance abuse. Cochrane Database of Systematic Reviews 2011, Issue 5. [DOI: 10.1002/14651858.CD008063.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Sobell 1992
- Sobell LC, Sobell MB. Timeline follow‐back: technique for assessing self‐reported alcohol consumption. In: Litten RZ, Allen JP editor(s). Measuring Alcohol Consumption: Psychosocial and Biological Methods. Totowa, NJ: Humana Press, 1992:41‐72. [Google Scholar]
Tait 2003
- Tait RJ, Hulse GK. A systematic review of the effectiveness of brief interventions with substance using adolescents by type of drug. Drug and Alcohol Review 2003;22(3):337–46. [DOI] [PubMed] [Google Scholar]
Tanner‐Smith 2015
- Tanner‐Smith EE, Lipsey MW. Brief alcohol interventions for adolescents and young adults: a systematic review and meta‐analysis. Journal of Substance Abuse Treatment 2015;51:1‐18. [DOI] [PMC free article] [PubMed] [Google Scholar]
Thakker 1998
- Thakker KD. An overview of health risks and benefits of alcohol consumption. Alcoholism: Clinical and Experimental Research 1998;22(7 Suppl):285‐98. [DOI] [PubMed] [Google Scholar]
Vasilaki 2006
- Vasilaki EI, Hosier SG, Cox WM. The efficacy of motivational interviewing as a brief intervention for excessive drinking: a meta‐analytic review. Alcohol Alcohol 2006;41(3):328‐35. [DOI] [PubMed] [Google Scholar]
White 1989
- White HR, Labouvie EW. Towards the assessment of adolescent problem drinking. Journal of Studies on Alcohol 1989;50(1):30‐7. [DOI] [PubMed] [Google Scholar]
WHO 2011
- World Health Organization. Global Status Report on Alcohol and Health. Geneva: WHO, 2011. [Google Scholar]
WHO 2014
- World Health Organization. Global Status Report on Alcohol and Health 2014. Geneva: WHO, 2014. [Google Scholar]
References to other published versions of this review
Foxcroft 2014a
- Foxcroft DR, Coombes L, Wood S, Allen D, Almeida Santimano NM. Motivational interviewing for alcohol misuse in young adults. Cochrane Database of Systematic Reviews 2014, Issue 8. [DOI: 10.1002/14651858.CD007025.pub2] [DOI] [PubMed] [Google Scholar]


