Abstract
Background
Necrotising fasciitis is a rapidly progressing soft-tissue infection with a low incidence that carries a relevant risk of morbidity and mortality. Although necrotising fasciitis is often fatal in adults, its case fatality rate seems to be lower in children. A highly variable clinical presentation makes the diagnosis challenging, which often results in misdiagnosis and time-delay to therapy.
Methods
We conducted a protocol-based systematic review to identify specific features of necrotising fasciitis in children aged one month to 17 years. We searched ’PubMed’, ’Web of Science’ and ’SCOPUS’ for relevant literature. Primary outcomes were incidence and case fatality rates in population-based studies, and skin symptoms on presentation. We also assessed signs of systemic illness, causative organisms, predisposing factors, and reconstructive procedures as secondary outcomes.
Results
We included five studies reporting incidence and case fatality rates, two case-control studies, and 298 cases from 195 reports. Incidence rates varied between 0.022 and 0.843 per 100,000 children per year with a case-fatality rate ranging from 0% to 14.3%. The most frequent skin symptoms were erythema (58.7%; 175/298) and swelling (48%; 143/298), whereas all other symptoms occurred in less than 50% of cases. The majority of cases had fever (76.7%; 188/245), but other signs of systemic illness were present in less than half of the cohort. Group-A streptococci accounted for 44.8% (132/298) followed by Gram-negative rods in 29.8% (88/295), while polymicrobial infections occurred in 17.3% (51/295). Extremities were affected in 45.6% (136/298), of which 73.5% (100/136) occurred in the lower extremities. Skin grafts were necessary in 51.6% (84/162) of the pooled cases, while flaps were seldom used (10.5%; 17/162). The vast majority of included reports originate from developed countries.
Conclusions
Clinical suspicion remains the key to diagnose necrotising fasciitis. A combination of swelling, pain, erythema, and a systemic inflammatory response syndrome might indicate necrotising fasciitis. Incidence and case-fatality rates in children are much smaller than in adults, although there seems to be a relevant risk of morbidity indicated by the high percentage of skin grafts. Systematic multi-institutional research efforts are necessary to improve early diagnosis on necrotising fasciits.
Electronic supplementary material
The online version of this article (10.1186/s12879-019-3941-3) contains supplementary material, which is available to authorized users.
Keywords: Necrotising fasciitis, Children, Systematic review, Incidence rate, Case fatality rate, Predisposing factors, Symptoms
Background
Necrotising fasciitis is a rapidly progressing soft-tissue infection, which has historically been linked to penetrating trauma in war times [1]. Paediatric textbooks did not mention necrotising fasciitis before 1973 [2, 3] despite the first case of necrotising fasciitis in a child [4] being reported just six years after the initial description in adults [5]. Selective literature reviews dealing with necrotising fasciitis in childhood usually deduce their recommendations from small case series or reports on adults [6–9]. In them, considerable research effort has been made to analyze necrotising fasciitis on a population based level [10], for specific patient groups at risk for necrotising fasciitis [11], and to facilitate early diagnosis [12–14].
In contrast, the knowledge on paediatric necrotising fasciitis is scarce: One database article identified 334 children with necrotising soft-tissue infections, but focused on treatment, outcome, and a multivariate analysis of independent risk factors for fatal outcomes [15]. The two largest studies reporting on skin signs, risk factors and outcomes include 39 retrospectively assessed [16] and 32 prospectively included cases [17]. The 39 retrospective cases were collected within 30 years [16], whereas the prospective study was conducted within four years, but included 20 neonates [17]. The difference in research on necrotising fasciitis in adults and children may further be emphasised by studies on laboratory parameters that may aid in diagnosis of necrotising fasciitis: While 20 children were investigated in a case-control study [18], a meta-analysis of adult patients included 846 cases from 16 studies [14]. Recently, a systematic review of necrotising fasciitis in children has been published [19], which is hampered by several shortcomings: Limited to articles published in English language after 2010, lack of clearly defined inclusion and exclusion criteria, inclusion of neonates, and cases likely to be Fournier’s gangrene due to genital involvement. Therefore, we aimed to identify specific features of necrotising fasciitis in childhood that may aid in early diagnosis and treatment initiation of this devastating disease by means of a systematic review. Furthermore, we aimed to gather information on causative organisms and the necessity of reconstructive procedures following an episode of necrotising fasciitis in children.
Methods
Guidelines and protocol for the systematic review
We developed a Preferred Reporting Items for Systematic Reviews and Meta-Analyses - Protocols [20] compliant protocol (Additional file 1) for the systematic review, and closely followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines [21] during the systematic review.
Literature search strategy
The literature search strategy with its adaptations to the three databases ’PubMed’, ’Web of Science’ and ’SCOPUS’ is laid out in detail in the appendix of the protocol (Additional file 1). A sensitivity-oriented approach combining text elements and Medical Subject Headings was used in all three databases. Literature search was extended towards snowballing the reference lists of all included studies and relevant reviews. We conducted the literature search on the 9th of January 2016 and updated it at the 4th of December 2018.
Types of included studies
Preliminary searches failed to identify prospective studies on signs on presentation. We therefore opted to include retrospective case series and case reports to collect information on these aspects, because information from reports with higher quality were not available. Only population-based data were considered eligible to determine incidence and case-fatality rates.
Inclusion criteria
Inclusion criteria for our systematic review were: Patient age between one month and 17 years. Studies have reported symptoms on presentation separate for each patient or for the whole group if all cases were within the age limit. Studies should indicate whether risk factors were present. Studies have reported on case fatalities. Studies reporting on incidence and case fatality rates on a population-based level must include data within the same age limits as stated above, but do not have to report on signs at presentation or risk factors.
Exclusion criteria
Exclusion criteria for our systematic review were: Studies were narrative reviews. Studies include patient data outside the specified age group that cannot be removed from the reported results. Studies include data on neonates or Fournier’s grangrene that cannot be separated from the paediatric data. Studies were reported in languages that could not be adequately translated using Google translator into a language that one of the authors can speak fluently (English, German, French, Dutch/Afrikaans, and Spanish).
Primary and secondary outcomes
Our primary outcomes were: Determine incidence and case-fatality rates of necrotising fasciitis in children from population-based reports and assess skin symptoms on presentation. Our secondary outcomes were: Age-specific case fatality rates, risk factors for necrotising fasciitis, signs of systemic illness due to necrotising fasciitis, microbes causative for necrotising fasciitis and reconstructive procedures following necrotising fasciitis.
Literature selection and data extraction
Two researchers independently assessed the search results and extracted data from the included reports as described in the protocol (Additional file 1). Following de-duplication, titles were independently screened for eligibility followed by reading the abstracts as second and the full-text as a third step. Each step was checked for consistency by another researcher. Differences between the two independent researchers were settled by consensus. If consensus could not be reached, the assessment of a third researcher was decisive. We used a Data extraction sheet (Additional file 2) for the documentation of the results.
Definitions for data acquisition
We defined all skin symptoms which were not explicitly mentioned in a report as absent. This definition was also used for signs of systemic illness not reported. Signs of systemic illness and reconstructive procedures were only included if at least one item was reported in the study, otherwise the respective cells were not included in the analysis. Definitions for the systemic inflammatory response syndrome relied on the international paediatric sepsis consensus conference [22].
Risk factors in the pooled cases
We grouped the underlying conditions or preceding events of the included cases into five distinct risk groups: Varicella, surgery, immunocompromise, trauma, and minor trauma (e.g. an insect bite, a bruise from a fall etc.) and contrasted them with the cases in which necrotising fasciitis occurred without predisposing factors.
Protocol deviations
The study by Mulla reports cases of necrotising fasciitis in children caused by group-A streptococci in Florida between August 1996 and August 2000, but did not provide incidence data [23]. We extrapolated incidence data by using census data of Florida in 2000, which counted 3,646,340 persons below 18 years of age [24]. The population data used in the Finnish incidence study [25] had an age limit of 15 years. The neonatal case in the study by Eneli & Davies [26] has been excluded and the incidence data were recalculated using population data provided within the report. The report by Gjessing Jensen & Christensen [27] was not translated using Google translator as stated in the protocol, because the corresponding author supplied us with an author translation.
Results
Article selection
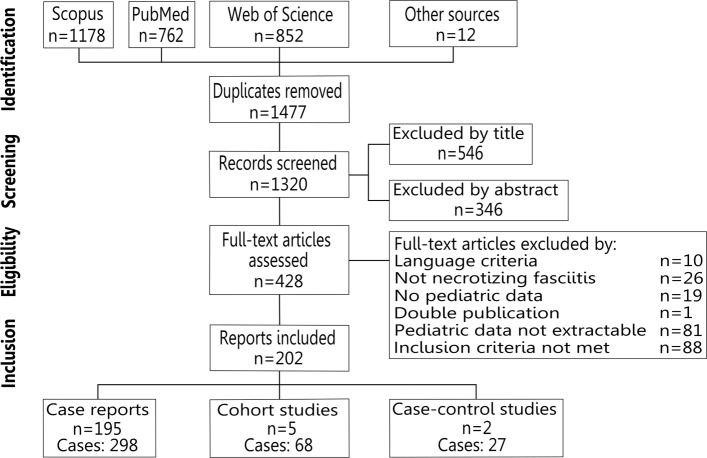
We identified five studies that reported population-based on incidence and case-fatality rates in 68 cases [23, 25, 26, 28, 29], two case-control studies with 27 cases [30, 31], and another 298 cases from 195 case series and case reports [2–4, 8, 27, 32–221] (Fig. 1).
Fig. 1.
Preferred reporting items for systematic reviews and meta-analyses flow diagram. Literature search and selection of studies for the systematic review
Incidence rate
Two studies from Canada were prospective: One monitored the whole country [26], whereas the other was limited to Ontario [28]. Another study collected retrospective data for Florida [23] and another relied on the database of a hospital chain in Utah, which claimed to cover 70-85% of all hospital admissions of children in this state [29]. The last report was based on the data of Finnish university hospitals and the childhood population living in their referral area [25]. Only one study [26] reports incidence data for cases of necrotising fasciitis for both group-A streptococci and non-group-A streptococci, whereas the remaining three studies were limited to necrotising fasciitis caused by group-A streptococci [23, 28, 29]. The incidence rate of necrotising fasciitis varied from 0.843 cases per 100,000 children per year due to group-A streptococci in the Finnish Oulu University Hospital area [25] to 0.022 cases per 100,000 children per year caused by group-A streptococci [23]. Incidence rates of 0.212 cases occurred due to group-A streptococci and 0.0729 cases were caused by all other organisms [26] 0.01 [29] and 0.08 per 100,000 children per year [28] were in between.
Case fatality rate
The case fatality rate differed between 14.3% (1/7) [29], 10% (1/10) [28], and 0% in two reports [(0/3) [23] and (0/13) [25]], but was 2.85% (1/35) in the only study that included cases caused by other germs than group-A streptococci [26].
Properties of the identified case-control studies
The first identified case-control study had a mixed design of retrospectively (5/19) and prospectively (14/19) included cases. It aimed to describe an association between necrotising fasciitis following primary varicella infection and a preceding treatment with ibuprofen [30]. Twenty-nine controls were prospectively identified and had non-necrotising skin infections following primary varicella infection [30]. Therefore, study parameters were collected with the intent to compare baseline variables between two groups [30]. The second case-control study aimed to identify specific features of necrotising fasciitis compared to non-necrotising soft tissue infections [31]. It included cases within 16 years [31], whereas the first study had a duration of 19 months [30].
Age, sex and geographic distribution
The included cases had a similar mean age compared to the case-control studies (Table 1). Distribution of age groups within the pooled cases was similar except for a slight over-representation of school children and a corresponding under-representation of adolescents and infants. Males were predominantly affected in the varicella and ibuprofen case-control study with 74% (14/19) [30], and within the pooled cases (57.4%, 171/298), but not in the second case-control study (3/8 males) [31]. North America accounted for 39.9% (119/298), Asia for 31.9% (95/298), and Europe for 21.1% (63/298) of the included cases. In contrast, South America contributed ten (3.3%), Africa nine (3%), and Oceania only two reports.
Table 1.
Age, risk factors, skin symptoms, and signs of systemic illness in case-control studies and pooled cases
| Item | Zerr et al. [30] | Hsieh et al. [31] | Pooled cases [2–4, 8, 27, 32–221] |
|---|---|---|---|
| Age [years] (range) | 4.6 (0.5-9.6) | 5 (2-13) | 5.7 (0.1-17) |
| Varicella [%] (Number) | 100 (19/19) | 50 (4/8) | 25.9 (77/297) |
| No risk factor [%] (Number) | 0 | 12.5 (1/8) | 22.9 (68/297) |
| Minor trauma [%] (Number) | 0 | 0 | 12.5 (37/297) |
| Immunocompromise [%] (Number) | 0 | 0 | 11.8 (35/297) |
| Surgery [%] (Number) | 0 | 12.5 (1/8) | 9.4 (28/297) |
| Trauma [%] (Number) | 0 | 25 (2/8) | 8.1 (24/297) |
| Skin infection [%] (Number) | 0 | 0 | 6.1 (18/297) |
| Intramuscular injection [%] (Number) | 0 | 0 | 1.7 (5/297) |
| Neuropathy [%] (Number) | 0 | 0 | 1.4 (4/297) |
| Diabetes [%] (Number) | 0 | 0 | 0.4 (1/297) |
| Erythema [%] (Number) | 94.7 (18/19) | 87.5 (7/8) | 58.7 (175/298) |
| Swelling [%] (Number) | 100 (19/19) | 87.5 (7/8) | 48 (143/298) |
| Pain [%] (Number) | 100 (19/19) | 87.5 (7/8) | 33.6 (100/298) |
| Splinting [%] (Number) | 66.7 (12/18) | 37.5 (3/8) | 3 (9/298) |
| Tenderness [%] (Number) | 0 | 37.5 (3/8) | 25.2 (75/298) |
| Discolouration [%] (Number) | 0 | 0 | 32.6 (97/298) |
| Necrosis [%] (Number) | 0 | 0 | 32.2 (96/298) |
| Oedema [%] (Number) | 0 | 0 | 26.5 (79/298) |
| Induration [%] (Number) | 0 | 0 | 14.4 (43/298) |
| Warmth [%] (Number) | 0 | 0 | 10.7 (32/298) |
| Bullae [%] (Number) | 0 | 0 | 9.1 (27/298) |
| Discharge [%] (Number) | 0 | 0 | 8.4 (25/298) |
| Ecchymosis [%] (Number) | 0 | 0 | 8.4 (25/298) |
| Blister [%] (Number) | 0 | 0 | 6 (18/298) |
| Crepitus [%] (Number) | 0 | 0 | 3.7 (11/298) |
| Fever [%] (Number) | 100 (19/19) | Not reported | 76.7 (188/245) |
| Tachycardia [%] (Number) | 0 | Not reported | 40.7 (94/231) |
| Tachypnea [%] (Number) | 0 | Not reported | 27.7 (64/231) |
| Hypotension [%] (Number) | 26.3 (5/19) | Not reported | 29.9 (69/231) |
| Leukocytosis [%] (Number) | Not reported | Not reported | 49.5 (106/214) |
| Bandemia [%] (Number) | Not reported | Not reported | 22.9 (49/214) |
| Leukopenia [%] (Number) | Not reported | Not reported | 17.3 (29/214) |
| Hypothermia [%] (Number) | 0 | Not reported | 0.8 (2/245) |
| Bradycardia [%] (Number) | 0 | Not reported | 0.4 (1/231) |
| Systemic inflammatory response syndrome [%] (Number) | Not reported | Not reported | 65.1 (175/269) |
Items assessed in the systematic review
The results can be found in Tables 1 and 2. An itemisation for risk factors revealed that there were no obvious differences between them.
Table 2.
Isolated germs, involved body regions, fatalities, and reconstructive procedures in case-control studies and pooled cases
| Item | Zerr et al. [30] | Hsieh et al. [31] | Pooled cases[2–4, 8, 27, 32–221] |
|---|---|---|---|
| Group-A streptococci [%] (Number) | 84.2 (16/19) | 87.5 (7/8) | 44.8 (132/295) |
| Staphylococcus aureus [%] (Number) | 5.3 (1/19) | 12.5 (1/8) | 18.6 (55/295) |
| Gramnegative rods combined [%] (Number) | 0 | 0 | 29.8 (88/295) |
| Pseudomonas aeruginosa [%] (Number) | 0 | 0 | 10.2 (30/295) |
| Escherichia coli [%] (Number) | 0 | 0 | 7.8 (23/295) |
| Serratia marcescens [%] (Number) | 0 | 0 | 1.7 (5/295) |
| Klebsiella species [%] (Number) | 0 | 0 | 1.7 (5/295) |
| Other gramnegative rods [%] (Number) | 0 | 0 | 8.5 (25/295) |
| Anaerobe microbes [%] (Number) | 0 | 0 | 7.1 (21/295) |
| Other streptococci [%] (Number) | 0 | 0 | 6.8 (20/295) |
| Fungi [%] (Number) | 0 | 0 | 3.4 (10/295) |
| Other staphylococci [%] (Number) | 0 | 0 | 3.1 (9/295) |
| Enterococcus species [%] (Number) | 0 | 0 | 2.7 (8/295) |
| Polymicrobial infection [%] (Number) | 5.3 (1/19) | 0 | 17.3 (51/295) |
| Extremities [%] (Number) | 63.2 (12/19) | Not reported | 45.6 (136/298) |
| Lower extremity [%] (Number) | Not reported | Not reported | 33.9 (100/298) |
| Upper extremity [%] (Number) | Not reported | Not reported | 12.1 (36/298) |
| Trunk [%] (Number) | 21.1 (4/19) | Not reported | 32.9 (98/298) |
| Head [%] (Number) | 15.8 (3/19) | Not reported | 20.8 (62/298) |
| Retroperitoneum [%] (Number) | 0 | Not reported | 0.7 (2/298) |
| Second body region involved [%] (Number) | 0 | Not reported | 16.8 (50/298) |
| Lower extremity [%] (Number) | 0 | Not reported | 11.1 (33/298) |
| Trunk [%] (Number) | 0 | Not reported | 3.7 (11/298) |
| Upper extremity [%] (Number) | 0 | Not reported | 2 (6/298) |
| More than two body regions involved [%] (Number) | 0 | Not reported | 2.7 (8/298) |
| Fatalities [%] (Number) | 0 | 0 | 10.4 (31/295) |
| Primary closure [%] (Number) | Not reported | Not reported | 17.3 (28/162) |
| Secondary closure [%] (Number) | Not reported | Not reported | 20.4 (33/162) |
| Skin graft [%] (Number) | Not reported | Not reported | 51.6 (84/162) |
| Skin flap [%] (Number) | Not reported | Not reported | 10.5 (17/162) |
Discussion
We aimed to identify features specific to necrotising fasciitis in children by a systematic review. Whereas necrotising fasciitis had been subject to intensive research efforts in adults, knowledge on necrotising fasciitis in children is scarce. We identified four studies reporting population based incidences and case-fatality rates, of which two were prospectively conducted. Moreover, three of them were limited to cases of necrotising fasciitis caused by group-A streptococci and had a narrow geographic focus: Either a Canadian province [28], states within the United States of America [23, 29] or the referral area of Finnish university hospitals [25]. Only one report assessed necrotising fasciitis on a nationwide level [26] and included cases caused by other organisms than group-A streptococci. This might represent an accurate estimation of the burden of disease for an industrialised country. Necrotising fasciitis may be more common in developing countries as indicated by a monocentric Nigerian prospective observational study: It included 32 cases of necrotising fasciitis in childhood within 4 years [17]. Although 20 cases were neonates - leaving 12 children - the report [17] still hints at higher incidences in low-income countries. Moreover, all of these children presented with tissue necrosis [17] indicating an advanced disease [9, 222]. Similarly, ecchymosis and necrosis were found in 72% of cases in the other large case series [16]. In contrast to these late-appearing skin symptoms, pain, erythema, swelling, and - to a lesser extent - splinting were predominant skin symptoms in both case-control studies [30, 31]. The analysis of skin symptoms within the pooled cases did not identify highly frequent lesions: Only erythema had been noted in more than a half of the included cases and swelling in almost a half of the affected cases despite an advanced stage of disease - evidenced by either ecchymosis or necrosis - in 40.6% of the cases. This result may be explained by recall bias: The lack of clinical information that has been present in the patient, but was not documented in the patient’s file and thus not included in the published report [223]. Consequently, the more subtle skin symptoms might not be documented in light of the more dramatic changes such as necrosis or discolouration. Recall bias is also likely to have affected the signs of systemic illness within the pooled cases. Signs of systemic illness had similar frequencies among the pooled cases with the exception of fever in 76.6%. This percentage was smaller than the 100% reported in both case-control studies, and the 92% in the largest report on paediatric necrotising fasciitis [16]. Frank et al. [6] suggested that necrotising fasciitis would often go hand in hand with normal white cell counts combined with pronounced bandemia, whereas others associated necrotising fasciitis specifically with increased white cell counts [9]. In both case-control studies, white cell counts did not differ from those in patients diagnosed with cellulitis [30, 31]. Within the pooled cases, 49.5% had leukocytosis, 17.3% leukopenia, and 22.9% bandemia, of which the majority were found conjointly with leukocytosis. However, leukocyte counts are not part of the paediatric laboratory risk indicator for necrotising fasciitis, developed to differentiate cellulitis from necrotising fasciitis: Only C-reactive protein and sodium levels below 135mmol/L were found to be of relevance [18]. An abnormal leukocyte count or temperature are required to diagnose systemic inflammatory response syndrome, which occured in 65.1% of the pooled cases. A recent case-control study has shown that fever, tachycardia, and tachypnea might be used to differentiate necrotising fasciitis from abscesses or cellulitis [224]. Thus, a systemic inflammatory response syndrome conjointly with the combination of the most frequent skin symptoms from the case-control studies - swelling, pain, erythema, and probably splinting - might be predictive for necrotising fasciitis. Due to the limitations of the data included in the systematic review, this symptom combination needs to be evaluated for its predictive value before recommendations can be made. Predominant involvement of extremities followed by lesions on trunk and head was a common picture within all included studies. It also is in line with other reports [16] and adult data [11, 225, 226]. This is different concerning polymicrobial necrotising fasciitis: Previously, polymicrobial infection was commonly reported in paediatric necrotising fasciitis in developed [227] as well as developing countries [16, 17]. Among the pooled cases, in contrast, necrotising fasciitis was usually monomicrobial, which has previously been attributed to necrotising fasciitis following primary varicella infection [30, 31, 222]. Whether the pooled cases provide an accurate estimation of the distribution of mono- and polymicrobial infections needs to be assessed at a larger scale. In particular, Gram-negative rods isolated from wounds may depict a changing spectrum of necrotising fasciitis with a transition of risk factors from primary varicella towards immunocompromised or operated patients. Introduction of varicella vaccination resulted in reduction of the case load of necrotising fasciitis caused by group-A streptococci [228, 229]. Again, these results have to be validated by large scale studies. The necessary information seem to be available in certain databases as the negative association of both Streptococcus spp. and Staphylococcus spp. with case fatalities [15] could not have been calculated without knowledge of isolated germs. Case fatality rates have been [225] and still are high in adults [10, 226], but lower or absent in children [16–18, 222, 227, 230]. Higher case fatality rates of 14.3% [29] and 10% [28] have likely been influenced by small sample sizes as the case fatality rate was only 2.85% in the only cohort with more than ten patients [26]. Case fatality rate was 10.4% within the pooled cases and thus higher than in the aforementioned studies. Similarly, the number of cases that required a skin graft was 51.6%, which largely exceeds the previously reported values of skin grafting [17, 230]. There has been considerable variation within the literature: From skin grafts being exceptional [222] to institutions where skin grafting is the regular treatment modality for skin defects following necrotising fasciitis [227]. Probably, necessity for skin grafts was determined by extent of debridement and may thus have influenced the number of skin grafts. Different thresholds for using skin grafts could also play a role. Besides the already mentioned recall bias, several other limitations need to be taken into account for data from case series and case reports. Usually, case reports and series have an exorbitantly high success rate. Either due to preferential reporting of successful results [231] or an over-representation of specialised centres [232], whereas terrible results are scarce and those in between almost non-existent. The extent of this bias is however unclear as an assessment of case series included in Health Technology Assessments of the National Institute of Clinical Excellence of the United Kingdom found no differences in reported outcomes compared to randomised controlled clinical trials on the same subject [233]. Nevertheless, the results from the pooled cases have to be interpreted cautiously and thus require validation by studies of higher quality. Despite the relevance of necrotising fasciitis and its potential grave consequences for the future life of children, these studies are missing. Likely due to the rarity of necrotising fasciitis for the individual institutions, which could be overcome by multiinstitutional collaboration.
Conclusions
A high index of suspicion is necessary to diagnose necrotising fasciitis. A combination of swelling, pain, erythema, and a systemic inflammatory response syndrome might be indicative of early stages of necrotising fasciitis. Incidence and case-fatality rates of necrotising fasciitis in childhood are much smaller than in adults. Nevertheless, necrotising fasciitis seems to carry a relevant risk of morbidity exemplified skin grafting in more than a half of the pooled cases. A systematic multiinstitutional research effort is necessary to gain meaningful results from future studies to further elucidate necrotising fasciitis in childhood.
Additional files
Preferred reporting items for systematic reviews and meta-analyses-protocol compliant systematic review protocol. Protocol for the systematic review. (PDF 259 kb)
Data extraction sheet. Sheet used for data extraction and documentation. (PDF 8 kb)
Dataset for the pooled cases. Complete database of all cases extracted from the literature and their coding for the respective items. (XLSX 91 kb)
Acknowledgements
We thank Dr. Karsten Gjessing Jensen for providing us with a translated version of his manuscript written in Danish. We acknowledge the capability of the German interlibrary loan service without whose support the retrieval of a dozen non-English reports would have been impossible. We also thank the corresponding authors who provided us with reprints of their articles. Moreover, we are indebted to our patient S. whose gruesome course [221] initiated the present study.
Funding
The systematic review was conducted without funding.
Availability of data and materials
The data used in the present study is appropriately cited. The information on the individual cases is available as Additional file 3.
Authors’ contributions
AS, AG, GBF, and CO conceptualised the systematic review and developed the protocol. AS and CO designed the search strategy, which was reviewed by AGr, AS, and CO performed the literature search. AS and CO independently extracted the data. GBF and KSH reviewed the protocol and settled disputes in the data extraction. AS and CO wrote the paper. AG, GBF, KSH, and AGr critically reviewed the manuscript. All authors approved the final version. CO is the guarantor of the work.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Arne Schroder̈, Email: ar.schroeder@gmail.com.
Aurelié Gerin, Email: aureliehe@gmail.com.
Gregory B. Firth, Email: greg.firth@gmail.com
Kelly S. Hoffmann, Email: storm_kelly@yahoo.co.uk
Andrew Grieve, Email: a.grieve@me.com.
Christina Oetzmann von Sochaczewski, Email: c.oetzmann@gmail.com.
References
- 1.Lamb Lucy E M, Sriskandan Shiranee, Tan Lionel K K. Bromine, bear-claw scratch fasciotomies, and the Eagle effect: management of group A streptococcal necrotising fasciitis and its association with trauma. The Lancet Infectious Diseases. 2015;15(1):109–121. doi: 10.1016/S1473-3099(14)70922-3. [DOI] [PubMed] [Google Scholar]
- 2.Wilson H. David. Acute Necrotizing Fasciitis in Childhood. American Journal of Diseases of Children. 1973;125(4):591. doi: 10.1001/archpedi.1973.04160040087018. [DOI] [PubMed] [Google Scholar]
- 3.Hardzog-Britt C, Riley Jr. HD. Acute necrotizing fasciitis in childhood. J Oklahoma State Med Assoc. 1995;88(9):392–7. [PubMed] [Google Scholar]
- 4.Meleney FL. Haemolytic streptococcus gangrene following the administration of scarlet fever antitoxin. Ann Surg. 1930;91(2):287–9. doi: 10.1097/00000658-193002000-00012. [DOI] [Google Scholar]
- 5.MELENEY FRANK L. HEMOLYTIC STREPTOCOCCUS GANGRENE. Archives of Surgery. 1924;9(2):317. doi: 10.1001/archsurg.1924.01120080083007. [DOI] [Google Scholar]
- 6.Frank Gary, Mahoney Henrietta M., Eppes Stephen C. Musculoskeletal Infections in Children. Pediatric Clinics of North America. 2005;52(4):1083–1106. doi: 10.1016/j.pcl.2005.04.003. [DOI] [PubMed] [Google Scholar]
- 7.Leung Alexander K.C., Eneli I., Davies H. Dele. Necrotizing Fasciitis in Children. Pediatric Annals. 2008;37(10):704–710. doi: 10.3928/00904481-20081001-03. [DOI] [PubMed] [Google Scholar]
- 8.Pandey A., Gangopadhyay A.N., Upadhyaya V.D. Necrotising fasciitis in children and neonates: current concepts. Journal of Wound Care. 2008;17(1):5–10. doi: 10.12968/jowc.2008.17.1.27914. [DOI] [PubMed] [Google Scholar]
- 9.Jamal Nazreen, Teach Stephen J. Necrotizing Fasciitis. Pediatric Emergency Care. 2011;27(12):1195–1199. doi: 10.1097/PEC.0b013e31823b583c. [DOI] [PubMed] [Google Scholar]
- 10.Audureau E., Hua C., de Prost N., Hemery F., Decousser J.W., Bosc R., Lepeule R., Chosidow O., Sbidian E. Mortality of necrotizing fasciitis: relative influence of individual and hospital-level factors, a nationwide multilevel study, France, 2007-12. British Journal of Dermatology. 2017;177(6):1575–1582. doi: 10.1111/bjd.15615. [DOI] [PubMed] [Google Scholar]
- 11.Tan J. H., Koh B. T. H., Hong C. C., Lim S. H., Liang S., Chan G. W. H., Wang W., Nather A. A comparison of necrotising fasciitis in diabetics and non-diabetics. The Bone & Joint Journal. 2016;98-B(11):1563–1568. doi: 10.1302/0301-620X.98B11.37526. [DOI] [PubMed] [Google Scholar]
- 12.Al Alayed K, Tan C, Daneman N. Red flags for necrotizing fasciitis: A case control study. Int J Infect Dis. 2015. 10.1016/j.ijid.2015.04.02. [DOI] [PubMed]
- 13.Borschitz Thomas, Schlicht Svenja, Siegel Ekkehard, Hanke Eric, von Stebut Esther. Improvement of a Clinical Score for Necrotizing Fasciitis: ‘Pain Out of Proportion’ and High CRP Levels Aid the Diagnosis. PLOS ONE. 2015;10(7):e0132775. doi: 10.1371/journal.pone.0132775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bechar J, Sepehripour S, Hardwicke J, Filobbos G. Laboratory risk indicator for necrotising fasciitis (LRINEC) score for the assessment of early necrotising fasciitis: a systematic review of the literature. The Annals of The Royal College of Surgeons of England. 2017;99(5):341–346. doi: 10.1308/rcsann.2017.0053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Endorf Frederick W., Garrison Michelle M., Klein Matthew B., Richardson Andrea, Rivara Frederick P. Characteristics, Therapies, and Outcome of Children With Necrotizing Soft Tissue Infections. The Pediatric Infectious Disease Journal. 2012;31(3):221–223. doi: 10.1097/INF.0b013e3182456f02. [DOI] [PubMed] [Google Scholar]
- 16.Fustes-Morales A, Gutierrez-Castrellon P, Duran-McKinster C, Orozco-Covarrubias L, Tamayo-Sanchez L, Ruiz-Maldonado R. Necrotizing fasciitis: Report of 39 pediatric cases. Arch Dermatol. 2002; 138(7):893–9. 10.1001/archderm.138.7.893. [DOI] [PubMed]
- 17.Legbo J. N., Shehu B. B. Necrotising fasciitis: experience with 32 children. Annals of Tropical Paediatrics. 2005;25(3):183–189. doi: 10.1179/146532805X58111. [DOI] [PubMed] [Google Scholar]
- 18.Putnam Luke R., Richards Morgan K., Sandvall Brinkley K., Hopper Richard A., Waldhausen John H.T., Harting Matthew T. Laboratory evaluation for pediatric patients with suspected necrotizing soft tissue infections: A case–control study. Journal of Pediatric Surgery. 2016;51(6):1022–1025. doi: 10.1016/j.jpedsurg.2016.02.076. [DOI] [PubMed] [Google Scholar]
- 19.Lemaréchal Angela, Kaiser Philipp, Szavay Philipp, Zundel Sabine. Diagnosis and Treatment of Pediatric Necrotizing Fasciitis: A Systematic Review of the Literature. European Journal of Pediatric Surgery. 2016;27(02):127–137. doi: 10.1055/s-0036-1584531. [DOI] [PubMed] [Google Scholar]
- 20.Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P, Stewart LA. Preferred reporting items for systematic review and meta-analysis protocols (prisma-p) 2015 statement. Syst Rev. 2015; 4(1):1. 10.1186/2046-4053-4-1. [DOI] [PMC free article] [PubMed]
- 21.Moher David, Liberati Alessandro, Tetzlaff Jennifer, Altman Douglas G. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Medicine. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Goldstein Brahm, Giroir Brett, Randolph Adrienne. International pediatric sepsis consensus conference: Definitions for sepsis and organ dysfunction in pediatrics*. Pediatric Critical Care Medicine. 2005;6(1):2–8. doi: 10.1097/01.PCC.0000149131.72248.E6. [DOI] [PubMed] [Google Scholar]
- 23.MULLA ZUBER D. Clinical and epidemiologic features of invasive group A streptococcal infections in children. Pediatrics International. 2007;49(3):355–358. doi: 10.1111/j.1442-200X.2007.02378.x. [DOI] [PubMed] [Google Scholar]
- 24.Demographic Estimating Conference Database. County population by age, race, gender and Hispanic origin, 2000 Census. 2006. Online last accessed: 16 June 2017. http://edr.state.fl.us/Content/population-demographics/data/web11.xls.
- 25.Tapiainen Terhi, Launonen Saana, Renko Marjo, Saxen Harri, Salo Eeva, Korppi Matti, Kainulainen Leena, Heiskanen-Kosma Tarja, Lindholm Laura, Vuopio Jaana, Huotari Tiina, Rusanen Jarmo, Uhari Matti. Invasive Group A Streptococcal Infections in Children. The Pediatric Infectious Disease Journal. 2016;35(2):123–128. doi: 10.1097/INF.0000000000000945. [DOI] [PubMed] [Google Scholar]
- 26.Eneli Ihuoma, Davies H. Dele. Epidemiology and Outcome of Necrotizing Fasciitis in Children: An Active Surveillance Study of the Canadian Paediatric Surveillance Program. The Journal of Pediatrics. 2007;151(1):79-84.e1. doi: 10.1016/j.jpeds.2007.02.019. [DOI] [PubMed] [Google Scholar]
- 27.Jensen KG, Kristensen K. Nekrotiserende fasciitis hos børn. Ugeskr Laeger. 2009;171(3):147. [PubMed] [Google Scholar]
- 28.Laupland K. B., Davies H. D., Low D. E., Schwartz B., Green K., McGeer A. Invasive Group A Streptococcal Disease in Children and Association With Varicella-Zoster Virus Infection. PEDIATRICS. 2000;105(5):e60–e60. doi: 10.1542/peds.105.5.e60. [DOI] [PubMed] [Google Scholar]
- 29.Stockmann Chris, Ampofo Krow, Hersh Adam L., Blaschke Anne J., Kendall Brian A., Korgenski Kent, Daly Judy, Hill Harry R., Byington Carrie L., Pavia Andrew T. Evolving Epidemiologic Characteristics of Invasive Group A Streptococcal Disease in Utah, 2002–2010. Clinical Infectious Diseases. 2012;55(4):479–487. doi: 10.1093/cid/cis422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zerr Danielle M., Alexander E. Russell, Duchin Jeffrey S., Koutsky Laura A., Rubens Craig E. A Case-Control Study of Necrotizing Fasciitis During Primary Varicella. Pediatrics. 1999;103(4):783–790. doi: 10.1542/peds.103.4.783. [DOI] [PubMed] [Google Scholar]
- 31.Hsieh T, Samson LM, Jabbour M, Osmond MH. Necrotizing fasciitis in children in eastern ontario: A case-control study. CMAJ. 2000;163(4):393–6. [PMC free article] [PubMed] [Google Scholar]
- 32.Tehrani M.A., Webster M.H.C., Robinson D.W., Ledingham I.McA. Necrotising fasciitis treated by radical excision of the overlying skin. British Journal of Plastic Surgery. 1976;29(1):74–77. doi: 10.1016/0007-1226(76)90097-7. [DOI] [PubMed] [Google Scholar]
- 33.Andiman Warren A., Soifer Scott. Severe Streptococcal Infection Complicating Chickenpox. Clinical Pediatrics. 1980;19(7):495–497. doi: 10.1177/000992288001900711. [DOI] [PubMed] [Google Scholar]
- 34.Bomar William E., Ferlauto Jerry J., Wells David H. An unusual presentation of a β hemolytic group B streptococcal infection. Journal of Pediatric Surgery. 1980;15(5):683–685. doi: 10.1016/S0022-3468(80)80528-8. [DOI] [PubMed] [Google Scholar]
- 35.Bush JK, Givner LB, Whitaker SH, Anderson DC, Percy AK. Necrotizing fasciitis of the parapharyngeal space with carotid-artery occlusion and acute hemiplegia. Pediatrics. 1984;73(3):343–7. [PubMed] [Google Scholar]
- 36.Goldberg G. N., Hansen R. C., Lynch P. J. Necrotizing Fasciitis in Infancy: Report of Three Cases and Review of the Literature. Pediatric Dermatology. 1984;2(1):55–63. doi: 10.1111/j.1525-1470.1984.tb00444.x. [DOI] [PubMed] [Google Scholar]
- 37.Woo M L, Patrick W G, Simon M T, French G L. Necrotising fasciitis caused by Vibrio vulnificus. Journal of Clinical Pathology. 1984;37(11):1301–1304. doi: 10.1136/jcp.37.11.1301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kyong Catherine U., Smith C. D., Othersen H. Bieman. NECROTIZING FASCIITIS OF THE ABDOMINAL WALL AS A COMPLICATION OF CHICKENPOX. The Pediatric Infectious Disease Journal. 1985;4(4):420. doi: 10.1097/00006454-198507000-00025. [DOI] [PubMed] [Google Scholar]
- 39.Roos J, De Jong A, Bakker DJ. Een ernstige huid- of weke-deleninfectie is niet altijd gasgangreen. Ned Tijdschr Geneeskd. 1985;129(15):673–5. [PubMed] [Google Scholar]
- 40.Stalder JF, Leveque E, Pannier M, Dagorne M, Milpied B. Fasciité nécrosante périorbitaire chez l’entfant. Ann Dermatol Venerol. 1986;113(1):75. [Google Scholar]
- 41.Bailie FB, Linehan IP, Hadfield GJ, Gillett AP, Bailey BN. Infective cutaneous gangrene–urgency in diagnosis and treatment. Ann Plast Surg. 1987;19(3):238–46. doi: 10.1097/00000637-198709000-00010. [DOI] [PubMed] [Google Scholar]
- 42.Corrall C. James. Necrotizing Fasciitis Associated With Haemophilus influenzae Type b. Archives of Pediatrics & Adolescent Medicine. 1987;141(11):1146. doi: 10.1001/archpedi.1987.04460110016002. [DOI] [PubMed] [Google Scholar]
- 43.Cantaloube D, Combemale P, Larroque G, Vaisse D. Les gangrènes cutanées infectieuses du nourisson. Rev Stomatol Chir Maxillofac. 1988;89(3):162–8. [PubMed] [Google Scholar]
- 44.Cheng JCY, Leung PC. An unusual case of necrotizing fasciitis of the limb. J West Pac Orthop Assoc. 1988;25(2):15–18. [Google Scholar]
- 45.Falcone Philip A., Pricolo Victor E., Edstrom Lee E. Necrotizing Fasciitis as a Complication of Chickenpox. Clinical Pediatrics. 1988;27(7):339–343. doi: 10.1177/000992288802700706. [DOI] [PubMed] [Google Scholar]
- 46.Farrell LD, Karl SR, Davis PK, Bellinger MF, Ballantine TVN. Postoperative necrotizing fasciitis in children. Pediatrics. 1988;82(6):874–9. [PubMed] [Google Scholar]
- 47.Schwarz G, Sagy M, Barzilay Z. Multifocal necrotizing fasciitis in varicella. Pediatr Emerg Care. 1989;5(1):31–3. doi: 10.1097/00006565-198903000-00010. [DOI] [PubMed] [Google Scholar]
- 48.Goldwag David A., Purcell Thomas B. Necrotizing fasciitis in the pediatric age group: report of a case. The Journal of Emergency Medicine. 1990;8(3):299–304. doi: 10.1016/0736-4679(90)90010-S. [DOI] [PubMed] [Google Scholar]
- 49.Beiroa EN, James ET, Jenas CD, De Paz FB, De Frias EC. Fascitis necrotizante estreptococica. Ann Esp Pediatr. 1991;35(5):362–4. [PubMed] [Google Scholar]
- 50.Pannier M, Bouchot-Hermouet M, Lavergne-Hepner D, Hepner Y, David A, Stalder JF. Fasciité nécrosante péri-orbitaire à streptocoque bêta-hémolytique chez l’enfant. Ann Chir Plast Esthet. 1991; 36(1):75–8. [PubMed]
- 51.Rose Geoffrey E, Howard David J, Watts Mark R. Periorbital necrotising fasciitis. Eye. 1991;5(6):736–740. doi: 10.1038/eye.1991.135. [DOI] [PubMed] [Google Scholar]
- 52.Stone L, Codere F, Ma SA. Streptococcal lid necrosis in previously healthy-children. Can J Ophtalmol. 1991;26(7):386–90. [PubMed] [Google Scholar]
- 53.Boyle Michael F, Singer Jonathan. Necrotizing myositis and toxic strep syndrome in a pediatric patient. The Journal of Emergency Medicine. 1992;10(5):577–579. doi: 10.1016/0736-4679(92)90141-F. [DOI] [PubMed] [Google Scholar]
- 54.Duncan Brian W., Adzick N.Scott, deLorimier Alfred A., Longaker Michael T., Ferrell Linda D., Zoger Seymour, Harrison Michael R. Necrotizing fasciitis in two children with acute lymphoblastic leukemia. Journal of Pediatric Surgery. 1992;27(5):668–671. doi: 10.1016/0022-3468(92)90476-N. [DOI] [PubMed] [Google Scholar]
- 55.Zittergruen M, Grose C. Magnetic resonance imaging for early diagnosis of necrotizing fasciitis. Pediatr Emerg Care. 1993;9(1):26–8. doi: 10.1097/00006565-199302000-00009. [DOI] [PubMed] [Google Scholar]
- 56.Atiyeh Bishara C., Zaatari Ahmad M. Necrotizing fasciitis of the upper extremity. The Journal of Emergency Medicine. 1994;12(5):611–613. doi: 10.1016/0736-4679(94)90412-X. [DOI] [PubMed] [Google Scholar]
- 57.Molea G, Bocchini P, Adamo C, Tirone L, Simioli A. Necrotizing fasciitis as a complication of chickenpox - a case report and literature review. Eur J Plast Surg. 1994; 17(3):151–3. 10.1007/BF00178682.
- 58.Perez Moro A, Cebero Garcia M, Lopez-Herce Cid J, Rubia Fernandez Ldl, Martin Fernandez J, Garcia de Frias E. Fascitis necrotizante postoperatoria en la infancia. Acta Pediatr Esp. 1994;52(7):434–5. [Google Scholar]
- 59.Andze G, Pagbe JJ, Douala Mouteng V, Tchokoteu PF, Biwole Sida M, Sandjon JP, Ngonde Sende G, Eteme M, Ekane SN, Bankole R, Edzoa T. Fasciite necrosante post-operatoire chez le nourrisson. a propos d’un cas. J Chir (Paris) 1995;132(2):90–3. [PubMed] [Google Scholar]
- 60.Brogan TV, Nizet V, Waldhausen JHT, Rubens CE, Clarke WR. Group a streptococcal necrotizing fasciitis complicating primary varicella: A series of fourteen patients. Pediatr Infect Dis J. 1995;14(7):588–93. doi: 10.1097/00006454-199507000-00007. [DOI] [PubMed] [Google Scholar]
- 61.Misago Noriyuki, Tanaka Tatsurou, Takeuchi Minora, Oka Shohki. Necrotizing Fasciitis in Association with Hyperimmunoglobulin E Syndrome. The Journal of Dermatology. 1995;22(9):673–676. doi: 10.1111/j.1346-8138.1995.tb03896.x. [DOI] [PubMed] [Google Scholar]
- 62.Murphy James J., Granger Robert, Blair Geoffrey K., Miller Grant G., Fraser Graham C., Magee J.Fergall. Necrotizing fasciitis in childhood. Journal of Pediatric Surgery. 1995;30(8):1131–1134. doi: 10.1016/0022-3468(95)90004-7. [DOI] [PubMed] [Google Scholar]
- 63.Wilson G. J., Talkington D. F., Gruber W., Edwards K., Dermody T. S. Group A Streptococcal Necrotizing Fasciitis Following Varicella in Children: Case Reports and Review. Clinical Infectious Diseases. 1995;20(5):1333–1338. doi: 10.1093/clinids/20.5.1333. [DOI] [PubMed] [Google Scholar]
- 64.Barton Leslie L. Necrotizing Fasciitis in Children: Report of Two Cases and Review of the Literature. Archives of Pediatrics & Adolescent Medicine. 1996;150(1):105. doi: 10.1001/archpedi.1996.02170260109020. [DOI] [PubMed] [Google Scholar]
- 65.Estrada B, Stevens DL, Craver RD, Steele RW. A 5-year-old with leg pain. Infect Med. 1996;13(7):583–4594597. [Google Scholar]
- 66.Hernandez Gonzalez A, Quintero Otero S, Rubio Quinones F, Fernandez O’dogherty S, Ruiz Ruiz C, Marin P, Fregenal J, Pantoja Rosso S. Fascitis necrotizante: una grave complicacion tras cirugia banal en el nino. Rev Esp Pediatr. 1996;52(308):181–4. [Google Scholar]
- 67.Mills WJ, Mosca VS, Nizet V. Orthopaedic manifestations of invasive group a streptococcal infections complicating primary varicella. J Pediatr Orthop. 1996;16(4):522–8. doi: 10.1097/01241398-199607000-00021. [DOI] [PubMed] [Google Scholar]
- 68.Navarro Gomez ML, Sanchez Sanchez C, Gomez Campdera JA, Soleto Martin J, De Tomas Palacios E, Moral Torrero R, Hernandez-Sampelayo T. Fascitis necrotizante en la infancia. presentacion de dos casos. Rev Esp Pediatr. 1996;52(311):457–62. [Google Scholar]
- 69.Frias Perez MA, Munoz Bonet JI, Vazquez Martinez JL, de la Oliva Senovilla P, Ruza Tarrio F. Un niño con inflamación de tejidos blandos y signos de afectación sistémica. Ann Esp Pediatr. 1997;46(6):625–6. [PubMed] [Google Scholar]
- 70.Cordeiro Andréa Maria Gomes, Bousso A., Fernandes Iracema, Fernandes J. C., Elias F. M., Jorge W. A., Ejzenberg B., Okay Y. Cervical necrotizing fasciitis in an infant caused byHaemophilus non influenzae. Infection. 1997;25(6):383–384. doi: 10.1007/BF01740827. [DOI] [PubMed] [Google Scholar]
- 71.Mordehai J., Kurzbart E., Cohen Z., Mares A. J. Necrotizing fasciitis and myonecrosis in early childhood: a report of three patients. Pediatric Surgery International. 1997;12(7):538–540. doi: 10.1007/BF01258722. [DOI] [PubMed] [Google Scholar]
- 72.Poon Alice H., Terk Michael R., Colletti Patrick M. The association of primary varicella infection and streptococcal infection of the cutaneous and musculoskeletal system: A case report. Magnetic Resonance Imaging. 1997;15(1):131–133. doi: 10.1016/S0730-725X(96)00354-2. [DOI] [PubMed] [Google Scholar]
- 73.Sollazzo V, Bertolani G. Su di un raro caso di fascite necrosante. Ort Traum Oggi. 1997;17(1):29–31. [Google Scholar]
- 74.Sprotte Mira JG, Mocellin M, Pacheco Guedes C, Mercado M, Predebon Vanzo R, Guimaraes Pereira R. Fasceite necrotizante cervical em crianca: Relato de caso. Rev Bras Otorrinolaringol. 1997;63(1):87–90. [Google Scholar]
- 75.Viani Rolando M., Lewis Aimee, Bradley John S. POSTOPERATIVE GROUP B STREPTOCOCCAL NECROTIZING FASCIITIS IN A PREVIOUSLY HEALTHY CHILD. The Pediatric Infectious Disease Journal. 1997;16(6):630–631. doi: 10.1097/00006454-199706000-00019. [DOI] [PubMed] [Google Scholar]
- 76.Devin B, McCarthy A, Mehran R, Auger C. Necrotizing fasciitis of the retroperitoneum: an unusual presentation of group a streptococcus infection. Can J Surg. 1998;41(2):156–60. [PMC free article] [PubMed] [Google Scholar]
- 77.Donnelly L. F., Frush Donald P., O'Hara Sara M., Bisset III. George S. Necrotizing myofasciitis: an atypical cause of "acute abdomen" in an immunocompromised child. Pediatric Radiology. 1998;28(2):109–111. doi: 10.1007/s002470050306. [DOI] [PubMed] [Google Scholar]
- 78.Lin PC, Lee MJ, Yang W, Hwang CC. Group a streptococcal necrotizing fasciitis after varicella: Report of two cases. Acta Paed Sin. 1998;39(6):415–8. [PubMed] [Google Scholar]
- 79.Paya K, Hayek B.F, Rebhandl W, Pollak A, Horcher E. Retroperitoneal necrotizing fasciitis in a 4-year-old girl. Journal of Pediatric Surgery. 1998;33(5):778–780. doi: 10.1016/S0022-3468(98)90219-6. [DOI] [PubMed] [Google Scholar]
- 80.Nelson John D., McCracken George H. The Pediatric Infectious Disease Journal® Newsletter. The Pediatric Infectious Disease Journal. 1998;17(4):&NA. doi: 10.1097/00006454-199804000-00001. [DOI] [Google Scholar]
- 81.Barapouti F G, Kamel O R, Sampath R. Periorbital necrotising fasciitis in a child. Eye. 1999;13(5):676–678. doi: 10.1038/eye.1999.187. [DOI] [PubMed] [Google Scholar]
- 82.Chao H C, Kong M S, Lin T Y. Diagnosis of necrotizing fasciitis in children. Journal of Ultrasound in Medicine. 1999;18(4):277–281. doi: 10.7863/jum.1999.18.4.277. [DOI] [PubMed] [Google Scholar]
- 83.Feinerman Ilana L., Tan Henry K.K., Roberson David W., Malley Richard, Kenna Margaret A. Necrotizing fasciitis of the pharynx following adenotonsillectomy. International Journal of Pediatric Otorhinolaryngology. 1999;48(1):1–7. doi: 10.1016/S0165-5876(98)00148-7. [DOI] [PubMed] [Google Scholar]
- 84.Lee Bonita E., Robinson Joan L. The Use of Technetium‐99m‐Labeled White Blood Cell Scan in the Management of a Case of Group A Streptococcus Necrotizing Fasciitis with Polymyositis. Clinical Infectious Diseases. 1999;28(1):153–154. doi: 10.1086/517187. [DOI] [PubMed] [Google Scholar]
- 85.SZTAJNBOK Jaques, LOVGREN Marguerite, BRANDILEONE Maria Cristina C., MAROTTO Paulo C.F., TALBOT James A., SEGURO Antonio C. FATAL GROUP A STREPTOCOCCAL TOXIC SHOCK-LIKE SYNDROME IN A CHILD WITH VARICELLA: REPORT OF THE FIRST WELL DOCUMENTED CASE WITH DETECTION OF THE GENETIC SEQUENCES THAT CODE FOR EXOTOXINS SPE A AND B, IN SÃO PAULO, BRAZIL. Revista do Instituto de Medicina Tropical de São Paulo. 1999;41(1):63–65. doi: 10.1590/S0036-46651999000100011. [DOI] [PubMed] [Google Scholar]
- 86.Meza A, Gil H. Severe streptococcal infections and toxic shock in children. Int Pediatr. 2000;15(4):232–5. [Google Scholar]
- 87.Wang Shih-Min, Liu Ching-Chuan, Chiou Yuan-Yow, Yang Hsiao-Bai, Chen Chun-Ta. Vibrio vulnificus infection complicated by acute respiratory distress syndrome in a child with nephrotic syndrome. Pediatric Pulmonology. 2000;29(5):400–403. doi: 10.1002/(SICI)1099-0496(200005)29:5<400::AID-PPUL10>3.0.CO;2-J. [DOI] [PubMed] [Google Scholar]
- 88.Goncalves E, Furtado F, Estrada J, Vale MC, Pinto M, Santos M, Moura G, Vasconcelos C. Fasceíte necrosante pós varicela. Acta Med Port. 2001;14(3):367–70. [PubMed] [Google Scholar]
- 89.Johnston Donna L., Waldhausen John H. T., Park Julie R. Deep Soft Tissue Infections in the Neutropenic Pediatric Oncology Patient. Journal of Pediatric Hematology/Oncology. 2001;23(7):443–447. doi: 10.1097/00043426-200110000-00010. [DOI] [PubMed] [Google Scholar]
- 90.Marie–Cardine A, Mallet E, Billiemaz K, Boulesteix J, Bourrillon A, Dechamps C, Duhamel J.F, Garnier J.M, Gaudelus J, Gendrel D, Jeannot E, Küpfer I, Labbé A, Lagardère B, Meunier M, Olivier C, Reinert P. Infections cutanées sévères à Streptococcus pyogenes chez l’enfant : résultats d’une enquête multicentrique. Archives de Pédiatrie. 2001;8(12):1325–1332. doi: 10.1016/S0929-693X(01)00653-4. [DOI] [PubMed] [Google Scholar]
- 91.Pijnenburg MWH, Cotton MF. Necrotising fasciitis in an hiv-1-infected infant. South Afr Med J. 2001;91(6):500–1. [PubMed] [Google Scholar]
- 92.YANAY OFER, VAUGHAN DAVID J., DIAB MOHAMMAD, BROWNSTEIN DENA, BROGAN THOMAS V. Retained wooden foreign body in a child’s thigh complicated by severe necrotizing fasciitis: A case report and discussion of imaging modalities for early diagnosis. Pediatric Emergency Care. 2001;17(5):354–355. doi: 10.1097/00006565-200110000-00009. [DOI] [PubMed] [Google Scholar]
- 93.Billiemaz K, Lavocat M.P, Teyssier G, Chavrier Y, Allard D, Varlet F. Varicelle compliquée d’une fasciite nécrosante à streptocoque hémolytique du groupe A. Archives de Pédiatrie. 2002;9(3):262–265. doi: 10.1016/S0929-693X(01)00762-X. [DOI] [PubMed] [Google Scholar]
- 94.Billington M, Goulden N, Tyrrell J, Shield J. Streptococcal fasciitis causing phlegmasia cerulea dolens. Pediatr Infect Dis J. 2002;21(2):179. doi: 10.1097/00006454-200202000-00025. [DOI] [PubMed] [Google Scholar]
- 95.Chakrabarti C, Nehama J, Sood SK. Staphylococcal necrotizing fasciitis and toxic shock syndrome in an adolescent. Infect Dis Clin Pract. 2002;11(7):399–402. doi: 10.1097/00019048-200209000-00006. [DOI] [Google Scholar]
- 96.Chiu Shun, Chiu Cheng-Hsun, Jaing Tang-Her, Chang Kao-Jung, Lin Tzou-Yien. Necrotising fasciitis caused by Vibrio vulnificus in a child without known risk factors. European Journal of Pediatrics. 2002;161(8):464–465. doi: 10.1007/s00431-002-0975-z. [DOI] [PubMed] [Google Scholar]
- 97.Costet-Fighiera C, Lagier J, Bastiani-Griffet F, Bernard E, Gastaud P. Fasciite nécrosante orbito-palpébrale: Une urgence ophtalmologique à pronostic vital. J Fr Ophtalmol. 2002;25(4):375–8. [PubMed] [Google Scholar]
- 98.Kobayashi Shogo, Kato Tomoaki, Nishida Seigo, Buttrago Efren, Mittal Naveen, Thompson John, Tzakis Andreas G. Necrotizing fasciitis following liver and small intestine transplantation. Pediatric Transplantation. 2002;6(4):344–347. doi: 10.1034/j.1399-3046.2002.00210.x. [DOI] [PubMed] [Google Scholar]
- 99.Newton CL, deLEMOS D, Abramo TJ, Murrey A, Noell C. Cervical necrotizing fasciitis caused by serratia marcescens in a 2 year old. Pediatr Emerg Care. 2002;18(6):433–5. doi: 10.1097/00006565-200212000-00007. [DOI] [PubMed] [Google Scholar]
- 100.Shaaban Hassan, Bayat Ardeshir, Davenport Peter, Shah Mamta. Necrotising fasciitis in an infant with congenital insensitivity to pain syndrome. British Journal of Plastic Surgery. 2002;55(2):160–163. doi: 10.1054/bjps.2001.3771. [DOI] [PubMed] [Google Scholar]
- 101.Yuen JC, Puri SK, Feng Z. Scalp necrotizing fasciitis with osteomyelitis of the skull from aspergillus. J Craniofac Surg. 2002; 13(6):762–4. 10.1097/01.SCS.0000026372.14357.D9. [DOI] [PubMed]
- 102.Clark P, Davidson D, Letts M, Lawton L, Jawadi A. Necrotizing fasciitis secondary to chickenpox infection in children. Can J Surg. 2003;46(1):9–14. [PMC free article] [PubMed] [Google Scholar]
- 103.Maheboob SN, Louon AM, Ahmed AH. Necrotizing fasciitis complicated by multiple pneumoceles. Saudi Med J. 2003;24(12):1394–6. [PubMed] [Google Scholar]
- 104.Miron Dan, Lev Ami, Colodner Raul, Merzel Yoseph. Pediatric Infectious Disease Journal. 2003;22(7):666–668. [PubMed] [Google Scholar]
- 105.Rao Vijaykumar P. Sadashiva, Bhat Narayana, Chattopadhyay A., Nagendhar M. Yoga. Necrotizing fasciitis with chickenpox. The Indian Journal of Pediatrics. 2003;70(12):961–963. doi: 10.1007/BF02723820. [DOI] [PubMed] [Google Scholar]
- 106.Ãzyazgan I, DaÇdelen F, Baykan H. Development of necrotizing fasciitis following varicella in two sisters. Erciyes Tip Dergisi. 2004;26(1):39–43. [Google Scholar]
- 107.Goldschmidt WFM, De Vries HJC, Fijn Van Draat CJ, Van Der Horst CMAM, Sillevis Smitt JH. Necrotiserende fasciitis bij een kind met varicella. Ned Tijdschr Dermatol Venerol. 2004;14(5):187–9. [Google Scholar]
- 108.Gröger A., Ulrich D, Unglaub F, Pallua N. Varizellenassoziierte nekrotisierende fasziitis beim kind. Unfallchirurg. 2004; 107(4):325–7. 10.1007/s00113-004-0759-1. [DOI] [PubMed]
- 109.Kordy Faisal N., Al-Mohsen Ibrahim Z., Hashem Fuad, Almodovar Edna, Al Hajjar Sami, Walsh Thomas J. Successful Treatment of a Child with Posttraumatic Necrotizing Fasciitis Caused by Apophysomyces elegans: Case Report and Review of Literature. The Pediatric Infectious Disease Journal. 2004;23(9):877–879. doi: 10.1097/01.inf.0000136870.17071.fd. [DOI] [PubMed] [Google Scholar]
- 110.Ricalde P, Engroff S.L, Jansisyanont P, Ord R.A. Paediatric necrotizing fasciitis complicating third molar extraction: report of a case. International Journal of Oral and Maxillofacial Surgery. 2004;33(4):411–414. doi: 10.1016/j.ijom.2003.08.008. [DOI] [PubMed] [Google Scholar]
- 111.Ruiz Carmen Elena, Arango Myrtha, Correa Ana Lucía, López Luz Saider, Restrepo Angela. Fascitis necrosante por Apophysomyces elegans, moho de la familia Mucoraceae, en paciente inmunocompetente. Biomédica. 2004;24(3):239. doi: 10.7705/biomedica.v24i3.1270. [DOI] [PubMed] [Google Scholar]
- 112.Sachdev A, Seth S. Necrotizing fascitis. Indian Pediatr. 2004;41(6):623. [PubMed] [Google Scholar]
- 113.Sakran Waheeb, Mazzawi Salim, Merzel Yosef, Colodner Raul. Streptococcal necrotizing fasciitis with toxic shock syndrome following cervical adenitis. International Journal of Pediatric Otorhinolaryngology. 2004;68(9):1209–1213. doi: 10.1016/j.ijporl.2004.04.019. [DOI] [PubMed] [Google Scholar]
- 114.Darbar A, Harris IA, Gosbell IB. Necrotizing infection due to bacillus cereus mimicking gas gangrene following penetrating trauma. J Orthop Trauma. 2005; 19(5):353–5. https://doi.org/01.bot.0000140314.00508.c1. [PubMed]
- 115.Delibaş Ali, Bek Kenan, Bülbül Mehmet, Demircin Gülay, Baysun Şahika, Öner Ayşe. Necrotizing fasciitis in a child: a rare complication of idiopathic nephrotic syndrome. Pediatric Nephrology. 2004;20(1):99–101. doi: 10.1007/s00467-004-1669-8. [DOI] [PubMed] [Google Scholar]
- 116.Kurekci A. Emin, Aydin H. Ibrahim, Atay A. Avni, Akar Nejat, Cetan Turker, Ozcan Okan, Gokcay Erdal. FAMILIAL HIGH FACTOR VIII LEVEL IN A CHILD WITH NECROTIZING FASCIITIS COMPLICATING PRIMARY VARICELLA INFECTION. Pediatric Hematology and Oncology. 2005;22(3):219–222. doi: 10.1080/08880010590921540. [DOI] [PubMed] [Google Scholar]
- 117.Lo Wen-Tsung, Cheng Shin-Nan, Wang Chih-Chien, Chu Mong-Ling. Extensive necrotising fasciitis caused by Pseudomonas aeruginosa in a child with acute myeloid leukaemia: case report and literature review. European Journal of Pediatrics. 2004;164(2):113–114. doi: 10.1007/s00431-004-1554-2. [DOI] [PubMed] [Google Scholar]
- 118.Luo Chih-Cheng, Chin Chao Hsun, Hsun Chiu Cheng. Necrotizing fasciitis: a rare complication of hypospadias surgery in a child. Journal of Pediatric Surgery. 2005;40(4):E29–E31. doi: 10.1016/j.jpedsurg.2005.01.024. [DOI] [PubMed] [Google Scholar]
- 119.Neo Eu Nice, Haritharan Thamutaram, Thambidorai Conjeevaram Rajendrarao, Suresh Venugobal. Pseudomonas Necrotizing Fasciitis in an Immunocompetent Infant. The Pediatric Infectious Disease Journal. 2005;24(10):942–943. doi: 10.1097/01.inf.0000179548.30554.19. [DOI] [PubMed] [Google Scholar]
- 120.Abuhammour Walid, Hasan Rashed A., Rogers Donza. Necrotizing Fasciitis Caused by Aeromonas hydrophilia in an Immunocompetent Child. Pediatric Emergency Care. 2006;22(1):48–51. doi: 10.1097/01.pec.0000195755.66705.f8. [DOI] [PubMed] [Google Scholar]
- 121.Cidoncha Escobar E., Urbano Villaescusa J., Marañón Pardillo R., Rodríguez Fernández R., Aritmendi Moreno C., Parente Hernández A., Riquelme García O. Fascitis necrosante por Streptococcus pyogenes. Anales de Pediatría. 2006;64(2):167–169. doi: 10.1157/13084178. [DOI] [PubMed] [Google Scholar]
- 122.De Decker Koen, Van Poucke Sven, Wojciechowski Marek, Ieven Margareta, Colpaert Cecile, Vogelaers Dirk, Jorens Philippe G. Successful use of posaconazole in a pediatric case of fungal necrotizing fasciitis. Pediatric Critical Care Medicine. 2006;7(5):482–485. doi: 10.1097/01.PCC.0000235255.68759.05. [DOI] [PubMed] [Google Scholar]
- 123.Sethi Ashwani, Sabherwal Anup. Cervicofacial necrotizing fasciitis: an unusual complication of chronic suppurative otitis media. The Journal of Laryngology & Otology. 2006;120(3):1–3. doi: 10.1017/S002221510600154X. [DOI] [PubMed] [Google Scholar]
- 124.Toledo Juan, Luis López-Prats Jose, Ibiza Emilio, Modesto Vicente, Sanchis Ramon, Vento Maximo. Case 2: An 18-month-old child with necrotic lesions on the limbs. Acta Paediatrica. 2006;95(11):1506–1508. doi: 10.1080/08035250600732005. [DOI] [PubMed] [Google Scholar]
- 125.Shenoy Rathika, Kamath Nutan, Bhat Kamalakshi. Necrotizing fasciitis in children: Experience in a teaching hospital. Journal of Pediatric Infectious Diseases. 2015;02(04):225–229. doi: 10.1055/s-0035-1557055. [DOI] [Google Scholar]
- 126.Bingöl-Koloğlu Meltem, Yıldız Rahşan Vargün, Alper Bilal, Yağmurlu Aydın, Çiftçi Ergin, Gökçora İsmail Haluk, İnce Erdal, Emiroğlu Murat, Dindar Hüseyin. Necrotizing fasciitis in children: diagnostic and therapeutic aspects. Journal of Pediatric Surgery. 2007;42(11):1892–1897. doi: 10.1016/j.jpedsurg.2007.07.018. [DOI] [PubMed] [Google Scholar]
- 127.Brady KeriAnne B., Levin Terry L. Necrotizing Fasciitis in a Young Girl With Atopic Eczema. Clinical Pediatrics. 2007;46(2):181–183. doi: 10.1177/0009922806293865. [DOI] [PubMed] [Google Scholar]
- 128.Farrier J. N., Kittur M. A., Sugar A. W. Necrotising fasciitis of the submandibular region; a complication of odontogenic origin. British Dental Journal. 2007;202(10):607–609. doi: 10.1038/bdj.2007.425. [DOI] [PubMed] [Google Scholar]
- 129.Hon Kam-Iun Ellis, Leung Erica, Burd David Andrew, Leung Alexander K. C. Necrotizing fasciitis and gangrene associated with topical herbs in an infant. Advances in Therapy. 2007;24(4):921–925. doi: 10.1007/BF02849985. [DOI] [PubMed] [Google Scholar]
- 130.López-Gil Á, Peraza Marín S, Gabrielli G, Burdeinick I, Gabrielli I, Urdaneta C. Zigomicosis cutanea en un paciente de 10 años: Primer caso pediatrico en venezuela. revision de la literatura. Arch Venez Puer Ped. 2007;70(1):22–7. [Google Scholar]
- 131.Visser Douwe H., van den Berg Yvette L. F., van Furth A Marceline, Oomen Matthijs W., Schouten-van Meeteren Antoinette Y. N., Pajkrt Dasja, van den Bos Cor, van Well Gijs Th. J. DIAGNOSIS AND TREATMENT OF CUTANEOUS ZYGOMYCOSIS. The Pediatric Infectious Disease Journal. 2007;26(12):1165–1166. doi: 10.1097/INF.0b013e3181462a4b. [DOI] [PubMed] [Google Scholar]
- 132.Abass Kotb, Saad Hekma, Abd-Elsayed Alaa A. Necrotizing fasciitis with toxic shock syndrome in a child: a case report and review of literature. Cases Journal. 2008;1(1):228. doi: 10.1186/1757-1626-1-228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.de Benedictis F M, Osimani P. Necrotising fasciitis complicating varicella. Archives of Disease in Childhood. 2008;93(7):619–619. doi: 10.1136/adc.2008.141994. [DOI] [PubMed] [Google Scholar]
- 134.Demirel Nihal, Bas Ahmet Yagmur, Zenciroglu Aysegul. Can necrotizing fasciitis be the first symptom of Hyperimmunoglobulin E syndrome. The Indian Journal of Pediatrics. 2008;75(10):1090–1090. doi: 10.1007/s12098-008-0171-x. [DOI] [PubMed] [Google Scholar]
- 135.Schiavetto RR, Cancian LRL, Haber DM, Maniglia MP, Maniglia CP, Fernandes AM. Fasceíte necrotizante cervical em lactente: Relato de caso. Arq Int Otorrinolaringol. 2008;74(4):596–9. [Google Scholar]
- 136.Kamran Mohammad, Wachs Jane, Putterman Chaim. Necrotizing Fasciitis in Systemic Lupus Erythematosus. Seminars in Arthritis and Rheumatism. 2008;37(4):236–242. doi: 10.1016/j.semarthrit.2007.04.005. [DOI] [PubMed] [Google Scholar]
- 137.Minodier Philippe, Chaumoitre Kathia, Vialet Renaud, Imbert Guenièvre, Bidet Philippe. Fatal streptococcal toxic shock syndrome in a child with varicella and necrotizing fasciitis of the face. European Journal of Emergency Medicine. 2008;15(4):231–233. doi: 10.1097/MEJ.0b013e3282f08d3d. [DOI] [PubMed] [Google Scholar]
- 138.Samsel Chase Baldwin, Bassali Reda W., Steele John CH, Hultén Kristina G., Murray Dennis Lynn. Community-Acquired Methicillin-Resistant Staphylococcus aureus Necrotizing Fasciitis in an Infant. Clinical Microbiology Newsletter. 2008;30(22):171–173. doi: 10.1016/j.clinmicnews.2008.10.003. [DOI] [Google Scholar]
- 139.Tsai Hsin-Lin, Liu Chin-Su, Chang Jei-Wen, Wei Chou-Fu, Lin Jin-Teh, Chin Tai-Wai. Severe Necrotizing Fasciitis of the Abdominal Wall Secondary to Colon Perforation in a Child. Journal of the Chinese Medical Association. 2008;71(5):259–261. doi: 10.1016/S1726-4901(08)70117-5. [DOI] [PubMed] [Google Scholar]
- 140.Bustos B R, Soto G G, Hickmann O L, Torres B C. Fascitis necrosante palpebral y shock tóxico por streptoccus pyogenes. Rev Chilena Infectol. 2009; 26(2):152–5. 10.4067/S0716-10182009000200007. [PubMed]
- 141.Chang Yu-Che, Lee Ching-Hsing, Tseng Chiu-Liang, Chen Jih-Chang. Children with lethal streptococcal fasciitis after a minor contusion injury. The American Journal of Emergency Medicine. 2009;27(8):1017.e3-1017.e5. doi: 10.1016/j.ajem.2008.12.007. [DOI] [PubMed] [Google Scholar]
- 142.Eggert J, Bird N, Leitze Z, Peterson M, Van Gils C. Diagnosis and treatment of type ii necrotizing fasciitis in a child presenting with a minor abrasion, edema, and apparent bruising. Wounds. 2009;21(3):74–8. [PubMed] [Google Scholar]
- 143.Gerard Delphine, Mariani-Kurkdjian Patricia, Sachs Philippe, Berrebi Dominique, Van-Den-Abbeele Thierry, Dauger Stéphane. Facial necrotizing fasciitis in an infant caused by a five toxin-secreting methicillin-susceptible Staphylococcus aureus. Intensive Care Medicine. 2009;35(6):1145–1146. doi: 10.1007/s00134-009-1401-z. [DOI] [PubMed] [Google Scholar]
- 144.Lee Chun-Yi, Lee Hsiu-Fen, Huang Fang-Liang, Chen Po-Yen. Haemorrhagic bullae associated with a chicken scratch. Annals of Tropical Paediatrics. 2009;29(4):309–311. doi: 10.1179/027249309X12547917869168. [DOI] [PubMed] [Google Scholar]
- 145.O’Regan Kevin, O’Mahony Edward, MacEneaney Peter, Fitzgerald Edward, Maher Michael M. Fulminant limb and retroperitoneal necrotizing fasciitis in a 15-year-old girl with Fanconi anaemia. Pediatric Radiology. 2009;39(10):1095–1097. doi: 10.1007/s00247-009-1324-4. [DOI] [PubMed] [Google Scholar]
- 146.Statham Melissa M., Vohra Amit, Mehta Deepak K., Baker Troy, Sarlay Robert, Rutter Michael J. Serratia marcescens causing cervical necrotizing oropharyngitis. International Journal of Pediatric Otorhinolaryngology. 2009;73(3):467–473. doi: 10.1016/j.ijporl.2008.10.019. [DOI] [PubMed] [Google Scholar]
- 147.Tobeña Rué M., Coll Usandizaga F., García Fontecha C., Bartolomé Comas R., Moraga Llop F.A. Fascitis necrosante por Staphylococcus aureus resistente a la meticilina adquirido en la comunidad productor de leucocidina de Panton-Valentine. Anales de Pediatría. 2009;70(4):374–378. doi: 10.1016/j.anpedi.2008.11.027. [DOI] [PubMed] [Google Scholar]
- 148.Uzel A.-P., Steinmann G., Bertino R., Korsaga A. Dermohypodermite bactérienne et phlegmon du membre supérieur par morsure de scolopendre : à propos de deux cas. Chirurgie de la Main. 2009;28(5):322–325. doi: 10.1016/j.main.2009.05.001. [DOI] [PubMed] [Google Scholar]
- 149.Al-Shubi FS, Zuker RM, Cole WG. Vacuum-assisted closure as a surgical assistant in life-threatening necrotizing fasciitis in children. Can J Plast Surg. 2010;18(4):139–42. doi: 10.1177/229255031001800412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Lehman Deborah, Tseng Ching Wen, Eells Samantha, Miller Loren G., Fan Xuemo, Beenhouwer David O., Liu George Y. Staphylococcus aureusPanton‐Valentine Leukocidin Targets Muscle Tissues in a Child with Myositis and Necrotizing Fasciitis. Clinical Infectious Diseases. 2010;50(1):69–72. doi: 10.1086/649217. [DOI] [PubMed] [Google Scholar]
- 151.Perbet S., Soummer A., Vinsonneau C., Vandebrouck A., Rackelboom T., Etienne J., Cariou A., Chiche J.-D., Mira J.-P., Charpentier J. Multifocal community-acquired necrotizing fasciitis caused by a Panton-Valentine leukocidin-producing methicillin-sensitive Staphylococcus aureus. Infection. 2010;38(3):223–225. doi: 10.1007/s15010-010-0002-7. [DOI] [PubMed] [Google Scholar]
- 152.Ploier R. Starke Schmerzen bei anfangs diskretem Lokalbefund. Monatsschrift Kinderheilkunde. 2010;158(3):210–213. doi: 10.1007/s00112-009-2082-y. [DOI] [Google Scholar]
- 153.Samanta Tryambak, Basu Biswanath, Ganguly Sutapa, Purkait Radheshyam. Unusual associations of necrotizing fascitis: A case series report from a tertiary care hospital. Indian Journal of Dermatology. 2010;55(4):399. doi: 10.4103/0019-5154.74571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Robinson Angela Byun, DeWitt Esi Morgan, Schanberg Laura Eve, Moody M Anthony. Necrotizing Fasciitis Caused by Haemophilus influenzae Type E in a 17-Year-Old Girl With Systemic Lupus Erythematosus. JCR: Journal of Clinical Rheumatology. 2010;16(1):49–50. doi: 10.1097/RHU.0b013e3181c7e095. [DOI] [PubMed] [Google Scholar]
- 155.Roy Mahua, Ahmed S. Moied, Pal Jyotishka, Biswas Siddhartha. Community Acquired Methicillin Resistant Staphylococcus Aureus: A Rare Presentation. The Indian Journal of Pediatrics. 2010;77(11):1332–1334. doi: 10.1007/s12098-010-0171-5. [DOI] [PubMed] [Google Scholar]
- 156.Sablier Frédérique, Slaouti Tayeb, Drèze Pierre-Alexandre, El Fouly Pierre Emmanuel, Allemeersch Daniel, Van Melderen Laurence, Smeesters Pierre R. Nosocomial transmission of necrotising fasciitis. The Lancet. 2010;375(9719):1052. doi: 10.1016/S0140-6736(10)60052-9. [DOI] [PubMed] [Google Scholar]
- 157.Scheepers Marius Anton, Keel Sandra, Michaelides Michel. Bilateral Necrotising Fasciitis of the Ocular Adnexa Secondary toPseudomonas aeruginosaSepticaemia in a HIV-Positive Child. Orbit. 2010;29(1):63–64. doi: 10.3109/01676830903258847. [DOI] [PubMed] [Google Scholar]
- 158.SENARAN Hakan, KARALEZLİ Nazim, ÖĞÜN Tunç Cevat. A Very Uncommon Complication Following Vaccination: Necrotizing Fasciitis and Myonecrosis: Case Report. Turkiye Klinikleri Journal of Medical Sciences. 2010;30(1):384–386. doi: 10.5336/medsci.2008-8341. [DOI] [Google Scholar]
- 159.Benatiya Andaloussi I, Abdellaoui M, Bhallil S, Tahri H. Fasciite nécrosante orbito-palpébrale, compliquant une pansinusite chez un patiente diabétique. Pan Afr Med J. 2011; 10:10. 10.11604/pamj.2011.10.10.1096. [PMC free article] [PubMed]
- 160.Delasobera B. Elizabeth, Place Rick, Howell John, Davis Jonathan E. Serious Infectious Complications Related to Extremity Cast/Splint Placement in Children. The Journal of Emergency Medicine. 2011;41(1):47–50. doi: 10.1016/j.jemermed.2010.05.031. [DOI] [PubMed] [Google Scholar]
- 161.Fernandes C, Dâmaso C, Duarte R, Cardoso DS, Casella P. Fasceíte necrotizante pós-apendicite aguda. Acta Med Port. 2011;24(SUPPL.3):621–6. [PubMed] [Google Scholar]
- 162.Gupta Anil K., Bonajmah Abdullah A. Varicella-related musculoskeletal complications in children. Journal of Pediatric Orthopaedics B. 2011;20(4):264–269. doi: 10.1097/BPB.0b013e328345348f. [DOI] [PubMed] [Google Scholar]
- 163.Kuzdan C, Soysal A, Altinkanat G, Aksu B, Soyletir G, Bakir M. Recurrent fatal necrotizing fasciitis due to streptococcus pyogenes in a child with hereditary sensory and automic neuropathy type iv. Jpn J Infect Dis. 2011;64(2):147–9. [PubMed] [Google Scholar]
- 164.Manzani Baldi JR, Rodríguez G. Fascitis necrosante bilateral de diseminación hematógena por staphylococcus aureus: Caso pediátrico. Cir Plast Iberolatinoam. 2011; 37(2):171–5. 10.4321/s0376-78922011000200011.
- 165.Shirley Rebecca, Mackey Simon, Meagher Peter. Necrotising fasciitis: A sequelae of varicella zoster infection. Journal of Plastic, Reconstructive & Aesthetic Surgery. 2011;64(1):123–127. doi: 10.1016/j.bjps.2010.03.031. [DOI] [PubMed] [Google Scholar]
- 166.Singh D. V., Thomas S., Nair P. P., Cyriac S., Tripathi G. M. Necrotizing fasciitis of face - our experience in its management. Case Reports. 2011;2011(aug31 1):bcr0720114453–bcr0720114453. doi: 10.1136/bcr.07.2011.4453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Ahmed Shakeel, Ali Syed Rehan, Samani Zahra Aziz. Pseudomonas Necrotizing Fasciitis in an Otherwise Healthy Infant. Case Reports in Infectious Diseases. 2012;2012:1–3. doi: 10.1155/2012/517135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Chung Victor, Scott Andrew. Cervical necrotizing fasciitis in children under two years of age. International Journal of Pediatric Otorhinolaryngology. 2012;76(12):1857–1860. doi: 10.1016/j.ijporl.2012.09.012. [DOI] [PubMed] [Google Scholar]
- 169.de Carvalho Ferreira Dennis, Cisne Frota Ana Cristina, Cavalcante Fernanda Sampaio, Abad Eliane Dios, Netto dos Santos Kátia Regina. Necrotizing Fasciitis Secondary to Community Pneumonia by Panton-Valentine Leukocidin–Positive Methicillin-ResistantStaphylococcus aureus. American Journal of Respiratory and Critical Care Medicine. 2012;186(2):202–203. doi: 10.1164/ajrccm.186.2.202. [DOI] [PubMed] [Google Scholar]
- 170.King E, Chun R, Sulman C. Pediatric cervicofacial necrotizing fasciitis: A case report and review of a 10-year national pediatric database. Arch Otolaryngol Head Neck Surg. 2012; 138(4):372–5. 10.1001/archoto.2012.119. [DOI] [PMC free article] [PubMed]
- 171.Li F, Xia J. Necrotizing fasciitis following varicella in a child. Chin Med J. 2012; 125(5):951–3. 10.3760/cma.j.issn.0366-6999.2012.05.040. [PubMed]
- 172.Muggeo Paola, Arcamone Giampaolo, Rizzo Antonino, Santoro Nicola. Necrotizing Fasciitis of the lower limbs. Pediatric Reports. 2012;4(1):4. doi: 10.4081/pr.2012.e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Prelog Tomaž, Jereb Matjaž, Čuček Igor, Jazbec Janez. Necrotizing Fasciitis Caused by Serratia marcescens After Venous Access Port Implantation in a Child With Acute Lymphoblastic Leukemia. Journal of Pediatric Hematology / Oncology. 2012;34(6):e246–e248. doi: 10.1097/MPH.0b013e318253f047. [DOI] [PubMed] [Google Scholar]
- 174.Seigel JK, Stadler ME, Lombrano JL, Almony JS, Couch ME, Belhorn TH. Chromobacterium violaceum necrotizing fasciitis: A case report and review of the literature. ENT J. 2012;91(11):479–83. doi: 10.1177/014556131209101108. [DOI] [PubMed] [Google Scholar]
- 175.Yeilding Ruth H., O'Day Denis M., Li Chun, Alexander Pauline T., Mawn Louise A. Periorbital infections after Dermabond closure of traumatic lacerations in three children. Journal of American Association for Pediatric Ophthalmology and Strabismus. 2012;16(2):168–172. doi: 10.1016/j.jaapos.2011.11.014. [DOI] [PubMed] [Google Scholar]
- 176.Bagri N, Saha A, Dubey NK, Rai A, Bhattacharya S. Skin grafting for necrotizing fasciitis in a child with nephrotic syndrome. Iran J Kidney Dis. 2013;7(6):496–8. [PubMed] [Google Scholar]
- 177.Belmir R., Fejjal N., Khales A., Achbouk H., El Omari M., El Mazouz S., Gharib N., Abassi A., Belmahi A. Fasciite nécrosante compliquant un bandage de Dujarier : à propos d’une observation. Annales de Chirurgie Plastique Esthétique. 2013;58(4):362–366. doi: 10.1016/j.anplas.2010.12.002. [DOI] [PubMed] [Google Scholar]
- 178.Ho C., Israni M., Johnson J. Visual Diagnosis: 10-Year-Old Girl With Fever and Altered Mental Status. Pediatrics in Review. 2013;34(10):474–477. doi: 10.1542/pir.34-10-474. [DOI] [PubMed] [Google Scholar]
- 179.Jing-Chun Z, Chun-Jing X, Shi K, Jia-Ao Y. Severe multiple necrotizing fasciitis complicated by abdominal compartment syndrome in an infant. Iran J Pediatr. 2013;23(5):601–3. [PMC free article] [PubMed] [Google Scholar]
- 180.Ocaña Yohel, Ulloa-Gutierrez Rolando, Yock-Corrales Adriana. Fatal Necrotizing Fasciitis in a Child following a Blunt Chest Trauma. Case Reports in Pediatrics. 2013;2013:1–3. doi: 10.1155/2013/373712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Rosenbaum A, Papaliodis D, Alley M, Lisella J, Flaherty M. Bacillus cereus fasciitis: a unique pathogen and clinically challenging sequela of inoculation. Am J Orthop (Belle Mead NJ) 2013;42(1):37–9. [PubMed] [Google Scholar]
- 182.Tancevski Aleksandar, Bono Kenneth, Willis Leisel, Klingele Kevin. Necrotizing Fasciitis in a Pediatric Orthopedic Population. Orthopedics. 2013;36(6):e741–e745. doi: 10.3928/01477447-20130523-18. [DOI] [PubMed] [Google Scholar]
- 183.Van Crombrugge L., Van Hoecke H., Roche N., Dhooge I. A rare case of necrotizing fasciitis of the external ear. International Journal of Pediatric Otorhinolaryngology Extra. 2013;8(2):44–46. doi: 10.1016/j.pedex.2013.01.004. [DOI] [Google Scholar]
- 184.Bhasin Aarti, Tolan Robert W. Resurgence of Methicillin-Sensitive Staphylococcus aureus in the Community-Associated, Methicillin-Resistant Staphylococcus aureus Era. Infectious Diseases in Clinical Practice. 2014;22(1):1–7. doi: 10.1097/IPC.0b013e31828f4ff8. [DOI] [Google Scholar]
- 185.Hernandez CRI, Herrera CB, Medina PL, Soto BOG. La fascitis necrosante en niños: Ana complicación indeseable. Rev Mex Pediatr. 2014;81(1):15–7. [Google Scholar]
- 186.Karakus Süleyman, Koku Naim, Parmaksiz Mehmet, Kilincaslan Huseyin. Necrotizing Fasciitis following Soave Procedure in Hirschsprung Disease. European Journal of Pediatric Surgery. 2012;24(02):190–192. doi: 10.1055/s-0032-1330849. [DOI] [PubMed] [Google Scholar]
- 187.Kwak Byung Ok, Lee Min Jung, Park Hye Won, Song Min Kyung, Chung Sochung, Kim Kyo Sun. Necrotizing fasciitis and streptococcal toxic shock syndrome secondary to varicella in a healthy child. Korean Journal of Pediatrics. 2014;57(12):538. doi: 10.3345/kjp.2014.57.12.538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Lithgow Anna, Duke Trevor, Steer Andrew, Smeesters Pierre Robert. Severe group A streptococcal infections in a paediatric intensive care unit. Journal of Paediatrics and Child Health. 2014;50(9):687–692. doi: 10.1111/jpc.12601. [DOI] [PubMed] [Google Scholar]
- 189.Alsaif Manal A., Robinson Joan L. Escherichia coli necrotizing fasciitis in Hirschsprung's disease. Journal of Pediatric Surgery Case Reports. 2015;3(4):174–175. doi: 10.1016/j.epsc.2015.03.002. [DOI] [Google Scholar]
- 190.Boo YJ, Nam MH, Lee EH, Lee KC. Cyclic neutropenia with a novel gene mutation presenting with a necrotizing soft tissue infection and severe sepsis: case report. BMC Pediatr. 2015; 15:34. 10.1186/s12887-015-0352-5. [DOI] [PMC free article] [PubMed]
- 191.Cutillas-Ruiz R., Mateos-Segura C., Montoliu-Peco C., Covaci-Covaci O., Pérez de la Fuente T. Fascitis necrosante en un niño. Evolución y tratamiento. Rehabilitación. 2015;49(4):256–259. doi: 10.1016/j.rh.2015.05.002. [DOI] [Google Scholar]
- 192.Goldberg BE, Sulman CG, Chusid MJ. Group a beta streptococcal infections in children after oral or dental trauma: A case series of 5 patients. ENT J. 2015;94(1):e1. [PubMed] [Google Scholar]
- 193.Haseeb Ahmed A., Okasha Shadi, Elbarawi Atef. Multifocal necrotizing fasciitis following Hirshsprung’s disease surgery away from the surgical wound site. Annals of Pediatric Surgery. 2015;11(2):159–161. doi: 10.1097/01.XPS.0000462930.03634.9f. [DOI] [Google Scholar]
- 194.Hearn Pasco, Miliya Thyl, Hor Songly, Sar Vuthy, Turner Paul. Necrotizing fasciitis complicating snakebite in Cambodia. IDCases. 2015;2(3):86–87. doi: 10.1016/j.idcr.2015.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Jain Jagriti, Thatte Shreya, Singhai Prakhar. Periorbital varicella gangrenosa: A rare complication of chicken pox. Oman Journal of Ophthalmology. 2015;8(1):64. doi: 10.4103/0974-620X.149874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Jauregui J. J., Bor N., Thakral R., Standard S. C., Paley D., Herzenberg J. E. Life- and limb-threatening infections following the use of an external fixator. The Bone & Joint Journal. 2015;97-B(9):1296–1300. doi: 10.1302/0301-620X.97B9.35626. [DOI] [PubMed] [Google Scholar]
- 197.Khurana Saurbhi, Pushker Neelam, Naik Sreedhara S, Changole Milind Devidas, Ghonsikar Vishnukant, Bajaj Mandeep. Periorbital necrotising fasciitis in infants: Presentation and management of six cases. Tropical Doctor. 2015;45(3):188–193. doi: 10.1177/0049475515575671. [DOI] [PubMed] [Google Scholar]
- 198.Kumar Monica, Meeks Andrew, Kearl Liza. Necrotizing Fasciitis of the Chest Wall. Pediatric Emergency Care. 2015;31(9):656–660. doi: 10.1097/PEC.0000000000000316. [DOI] [PubMed] [Google Scholar]
- 199.Mugambi Machoki S., Theron Andre, Cox Sharon, Pillay Komala, Millar Alastair J.W., Numanoglu Alp. Disseminated mucormycosis and necrotizing fasciitis in immune-compromised patients. Annals of Pediatric Surgery. 2015;11(1):35–39. doi: 10.1097/01.XPS.0000459980.60002.27. [DOI] [Google Scholar]
- 200.Song Christopher Tam, Hamilton Róisín, Song Colin, Kong Tze Yean, Lo Steven. Enabling the diagnosis of necrotising fasciitis without associated skin changes in a paediatric patient with acute lymphoblastic leukaemia: The LRINEC score. Journal of Plastic, Reconstructive & Aesthetic Surgery. 2015;68(1):e23–e24. doi: 10.1016/j.bjps.2014.08.044. [DOI] [PubMed] [Google Scholar]
- 201.Srinivas SahanaM, Patil AlkaraniT, Shankar Gowri, Lakshmikantha KeshavmurthyM, Govindraj Munirathnam. Necrotizing fasciitis associated with systemic lupus erythematosus in a child. Indian Dermatology Online Journal. 2015;6(6):441. doi: 10.4103/2229-5178.169737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Stone Lindsay A., Harshbarger Raymond J. Orbital Necrotizing Fasciitis and Osteomyelitis Caused by Arcanobacterium Haemolyticum. Ophthalmic Plastic and Reconstructive Surgery. 2015;31(2):e31–e33. doi: 10.1097/IOP.0000000000000057. [DOI] [PubMed] [Google Scholar]
- 203.Sturgeon Jonathan P., Segal Laura, Verma Anita. Going Out on a Limb. Pediatric Emergency Care. 2015;31(7):503–507. doi: 10.1097/PEC.0000000000000255. [DOI] [PubMed] [Google Scholar]
- 204.Szabó Levente, Szegedi István, Kiss Csongor, Szikszay Edit, Remenyik Éva, Csízy István, Juhász István. Excessive pediatric fasciitis necrotisans due toPseudomonas aeruginosainfection successfully treated with negative pressure wound therapy. Dermatologic Therapy. 2015;28(5):300–302. doi: 10.1111/dth.12252. [DOI] [PubMed] [Google Scholar]
- 205.Rudramurthy ShivaprakashM, Singh Meenu, Parashar Atul, Chakrabarti Arunaloke, Zaman Kamran, Kaur Harsimran. Cutaneous mucormycosis of scalp and eyelids in a child with type I diabetes mellitus. Indian Journal of Dermatology, Venereology, and Leprology. 2015;81(3):275. doi: 10.4103/0378-6323.152740. [DOI] [PubMed] [Google Scholar]
- 206.Lin Yu-San, Hung Min-Hsiang, Chen Chi-Chung, Huang Kuo-Feng, Ko Wen-Chien, Tang Hung-Jen. Tigecycline salvage therapy for necrotizing fasciitis caused by Vibrio vulnificus: Case report in a child. Journal of Microbiology, Immunology and Infection. 2016;49(1):138–141. doi: 10.1016/j.jmii.2013.04.008. [DOI] [PubMed] [Google Scholar]
- 207.Waldeck Kate, Daniels Rodney, Watson Michael, Shahbaz Leena. 1768. Critical Care Medicine. 2016;44:517. doi: 10.1097/01.ccm.0000510441.27310.11. [DOI] [Google Scholar]
- 208.Zundel Sabine, Szavay Philipp, Lemaréchal Angela. Pediatric Necrotizing Fasciitis: Restitutio Ad Integrum after Early Diagnosis and Aggressive Surgical Treatment. European Journal of Pediatric Surgery Reports. 2016;04(01):034–036. doi: 10.1055/s-0036-1594307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Tyler K, Patterson A, Hebra A. Necrotizing fasciitis in a healthy pediatric patient caused by enterobacter cloacae and serratia marcescens: A discussion of diagnosis and management. Am Surg. 2016;82:e292–3. [PubMed] [Google Scholar]
- 210.Al-Hashmi Sheikhan Nasser, Sethu Arun, Al-Busaidi Said Saud, Nelofer Maimuna. Immediate nasal reconstruction with a forehead flap in a 2.5-year-old girl following Pseudomonas aeruginosa- induced necrotising fasciitis – A case report and literature review. JPRAS Open. 2017;14:16–22. doi: 10.1016/j.jpra.2017.08.002. [DOI] [Google Scholar]
- 211.Pfeifle Viktoria A., Gros Stephanie J., Holland-Cunz Stefan, Kämpfen Alexandre. Necrotizing fasciitis in children due to minor lesions. Journal of Pediatric Surgery Case Reports. 2017;25:52–55. doi: 10.1016/j.epsc.2017.08.005. [DOI] [Google Scholar]
- 212.Emami SM, Mirmohamadi P, Jafarzadeh Esfehani R. Skin and soft tissue infection as a complication of varicella infection ended up in using intravenous immunoglobulin instead of surgical debridement: A case report and short review of literature. Arch Clin Infect Dis. 2017;12(4). 10.5812/archcid.66108.
- 213.Ballesteros-Betancourt J.R., García-Tarriño R., Ríos-Guillermo J., Rodriguez-Roiz J.M., Camacho P., Zumbado-Dijeres A., Domingo-Trepat A., Llusá-Pérez M., Combalia-Aleu A., García-Ramiro S., Soriano-Viladomiu A. Infecciones necrosantes de partes blandas atendidas en un servicio de urgencias de tercer nivel: evolución y correlación con la escala laboratory risk indicator for necrotizing fasciitis (LRINEC) Revista Española de Cirugía Ortopédica y Traumatología. 2017;61(4):265–272. doi: 10.1016/j.recot.2017.04.003. [DOI] [PubMed] [Google Scholar]
- 214.Kauffman Jeremy D., O'Brien Megan, Snyder Christopher W., Rottgers S. Alex, Rideout Drew A., Chandler Nicole M. Acute appendicitis complicated by necrotizing fasciitis in a teenager. Journal of Pediatric Surgery Case Reports. 2018;37:77–82. doi: 10.1016/j.epsc.2018.07.018. [DOI] [Google Scholar]
- 215.Fernández-Ibieta María. Necrotic Lesions Following Elective Urological Surgery in an Infant. The Surgery Journal. 2018;04(03):e133–e135. doi: 10.1055/s-0038-1668112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Olsson Lewis, Vuity Drazsen, McAllister Peter, Ansell Mark. Periorbital necrotising soft tissue infection in a 12-year-old patient. Scottish Medical Journal. 2018;63(3):87–90. doi: 10.1177/0036933018776830. [DOI] [PubMed] [Google Scholar]
- 217.Proia Alan D. Periocular necrotizing fasciitis in an infant. Survey of Ophthalmology. 2018;63(2):251–256. doi: 10.1016/j.survophthal.2017.03.002. [DOI] [PubMed] [Google Scholar]
- 218.Bloch Deborah, Gonzalez Mark D., Haight Ann, Abramowsky Carlos, Yildirim Inci. Necrotizing fasciitis caused by Mucor indicus in a pediatric bone marrow transplant recipient. Pediatric Transplantation. 2018;22(8):e13294. doi: 10.1111/petr.13294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Darmasseelane K, Banks T, Rjabova T. Necrotising fasciitis as a complication of primary varicella infection in an immunocompetent child. BMJ Case Reports. 2018. 10.1136/bcr-2018-225018. [DOI] [PMC free article] [PubMed]
- 220.Setiawati W, Satari HHI, Irawati Y, Susiyanti M. Successful management of bilateral periorbital necrotising fasciitis with ocular involvement. BMJ Case Reports. 2018. 10.1136/bcr-2017-223457. [DOI] [PMC free article] [PubMed]
- 221.Firth GB, Oetzmann von Sochaczewski C, Ramguthy Y, Khalfallah A. Necrotising fasciitis following a supracondylar and an open radius fracture in a child. SA Orthop J. 2018; 17(2):49–53. 10.17159/2309-8309/2018/v17n2a9.
- 222.Waldhausen John H.T., Holterman Mark J., Sawin Robert S. Surgical implications of necrotizing fasciitis in children with chickenpox. Journal of Pediatric Surgery. 1996;31(8):1138–1141. doi: 10.1016/S0022-3468(96)90103-7. [DOI] [PubMed] [Google Scholar]
- 223.Nissen T, Wynn R. The clinical case report: a review of its merits and limitations. BMC Research Notes. 2014; 7(1):264. 10.1186/1756-0500-7-264. [DOI] [PMC free article] [PubMed]
- 224.Sullivan Thomas B., Bastrom Tracey P., Marino Nikolas, Edmonds Eric W. Presenting features of extremity necrotizing fasciitis in the pediatric patient. Journal of Pediatric Orthopaedics B. 2018;27(5):461–466. doi: 10.1097/BPB.0000000000000493. [DOI] [PubMed] [Google Scholar]
- 225.Rea WJ, Wyrick WJr. Necrotizing fasciitis. Ann Surg. 1970;172(6):957–64. doi: 10.1097/00000658-197012000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Hansen MB, Rasmussen LS, Svensson M, Chakrakodi B, Bruun T, Madsen MB, Perner A, Garred P, Hyldegaard O, Norrby-Teglund A. INFECT study group Association between cytokine response, the lrinec score and outcome in patients with necrotising soft tissue infection: a multicentre, prospective study. Sci Rep. 2017; 7:42179. 10.1038/srep42179. [DOI] [PMC free article] [PubMed]
- 227.Moss R. Lawrence, Musemeche Catherine A., Kosloske Ann M. Necrotizing fasciitis in children: Prompt recognition and aggressive therapy improve survival. Journal of Pediatric Surgery. 1996;31(8):1142–1146. doi: 10.1016/S0022-3468(96)90104-9. [DOI] [PubMed] [Google Scholar]
- 228.Patel Roopal A., Binns Helen J., Shulman Stanford T. Reduction in pediatric hospitalizations for varicella-related invasive group a streptococcal infections in the varicella vaccine era. The Journal of Pediatrics. 2004;144(1):68–74. doi: 10.1016/j.jpeds.2003.10.025. [DOI] [PubMed] [Google Scholar]
- 229.Frère Julie, Bidet Philippe, Tapiéro Bruce, Rallu Fabien, Minodier Philippe, Bonacorsi Stephane, Bingen Edouard, Ovetchkine Philippe. Clinical and Microbiological Characteristics of Invasive Group A Streptococcal Infections Before and After Implementation of a Universal Varicella Vaccine Program: Table 1. Clinical Infectious Diseases. 2015;62(1):75–77. doi: 10.1093/cid/civ793. [DOI] [PubMed] [Google Scholar]
- 230.VanderMeulen Heather, Pernica Jeffrey M., Roy Madan, Kam April J. A 10-Year Review of Necrotizing Fasciitis in the Pediatric Population: Delays to Diagnosis and Management. Clinical Pediatrics. 2016;56(7):627–633. doi: 10.1177/0009922816667314. [DOI] [PubMed] [Google Scholar]
- 231.ALBRECHT J, MEVES A, BIGBY M. Case reports and case series from had significant impact on medical literature. Journal of Clinical Epidemiology. 2005;58(12):1227–1232. doi: 10.1016/j.jclinepi.2005.04.003. [DOI] [PubMed] [Google Scholar]
- 232.Chambers Duncan, Rodgers Mark, Woolacott Nerys. Not only randomized controlled trials, but also case series should be considered in systematic reviews of rapidly developing technologies. Journal of Clinical Epidemiology. 2009;62(12):1253-1260.e4. doi: 10.1016/j.jclinepi.2008.12.010. [DOI] [PubMed] [Google Scholar]
- 233.Dalziel K, Round A, Stein K, Garside R, Castelnuovo E, Payne L. Do the findings of case series studies vary significantly according to methological characteristics?Health Technol Assess. 2005;9(2). https://doi.org/10.3310/hta9020. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Preferred reporting items for systematic reviews and meta-analyses-protocol compliant systematic review protocol. Protocol for the systematic review. (PDF 259 kb)
Data extraction sheet. Sheet used for data extraction and documentation. (PDF 8 kb)
Dataset for the pooled cases. Complete database of all cases extracted from the literature and their coding for the respective items. (XLSX 91 kb)
Data Availability Statement
The data used in the present study is appropriately cited. The information on the individual cases is available as Additional file 3.