Abstract
The objective of this review was to assess the evidence on relaxation training for management of paediatric headaches. Our methodology was a rapid review of English-language peer reviewed published literature focused on studies evaluating relaxation training as a primary or adjunct management option for headache in a paediatric population (0 to 18 years of age). Seven studies involving 571 children were included in the review. The quality of evidence was very low using GRADE criteria. Headache frequency, duration, and intensity were the primary outcomes in the included studies. Results for the effects of relaxation training for paediatric headache are inconsistent. Four of the seven studies reported decreased headache frequency, two of the five studies reported decreased headache duration, and two of the six studies reported decreased headache intensity following relaxation training. No adverse events were reported. The current state of the evidence for relaxation training for management of paediatric headache is both inconsistent and of very low quality. High-quality research evaluating the effects of relaxation training for paediatric headaches is required to advance the field.
Keywords: Headache, Migraine, Paediatric, Relaxation, Review
BACKGROUND
Paediatric headache is one of the most common presenting concerns of families accessing medical care (1). Mild, transient, and isolated paediatric headaches are typically managed without accessing medical care, whereas severe, long-lasting, and recurrent headaches cause significant suffering and often result in decreased quality of life through interference with school and social activities (2). Prevalence of paediatric headache lasting at least 3 months is approximately 60%, with girls more frequently affected (67%) than boys (58%) (3). Primary headaches do not have an underlying medical cause and include migraines, tension-type headache (TTH), and cluster headaches. Migraine and TTH are the most common primary headaches in children (1), and recommended management includes both pharmacological and nonpharmacological therapies (1,2).
Complementary therapies include a ‘group of diverse medical and health care interventions, practices, products, or disciplines that are not generally considered part of conventional medicine’ (4). Psychological therapies (e.g., biofeedback, cognitive behavioural therapy), some of which are considered complementary therapies (e.g., hypnosis, relaxation training), may be effective for managing primary headaches in children (5,6). In particular, depression and anxiety are often comorbid and may increase headache persistence (7). Relaxation is a therapy that has potential to decrease somatization of stress, depression, and anxiety thereby improving outcomes for children and adolescents experiencing primary headaches. Several systematic reviews have found benefit of psychological treatments for paediatric headache (5,6,8,9); however, the grouping of a wide variety of interventions (i.e., cognitive behavioural therapy, biofeedback, psychotherapy, etc.) creates ambiguity for translating these results in practice. Two more specific systematic reviews of cognitive behavioural therapy (10) and biofeedback (11) suggested both therapies were effective for management of paediatric migraine. Our searches did not locate any reviews focused solely on the effects of relaxation therapy for paediatric headache. Therefore, this review expands the clinical applicability of the field by specifically examining relaxation training and is intended to help clinicians support patients and families affected by paediatric headaches to make informed choices.
Psychological therapies for paediatric headache vary in training and equipment requirements. Biofeedback, for example, requires electronic equipment to measure and display physiological information to the patient (12). Cognitive behavioural therapy is a program-based treatment that requires support from a trained therapist, although it may also be delivered through electronic platforms (13). Relaxation, however, is a type of self-administered mind-body therapy that is considered easy to learn, and can be incorporated into a child or adolescent’s daily routine (14,15).
Relaxation therapy includes learning and practicing a variety of skills such as deep breathing, progressive muscle relaxation, cue-control relaxation (pairing exhalation in a relaxed state with a cue word to create a positive, reproducible association) (16), and differential relaxation (active relaxation of select muscle groups while others are purposely engaged) (17). In addition to being relatively easy to learn and administer, relaxation is considered a safe management option—an important consideration for clinicians and families when choosing between pharmacological and nonpharmacological options.
Relaxation training is typically taught by a mental health professional (e.g., registered social worker, psychologist, psychiatrist), although self-directed educational resources such as books, CDs, and Internet supports are also increasingly available. Coverage for professionally instructed relaxation training and the length and number of sessions required for patients to practice independently are all highly variable. There is currently no standardized guidance for the use of relaxation training for headache; however, establishing a daily relaxation practice with additional sessions in times of increased stress or with the onset of pain is a common pattern of use. There are significant limitations to cost and accessibility of therapist-guided relaxation therapy, whereas relaxation training allows patients to self-administer such therapies and may offer an effective alternative. Training can be therapist- or self-directed and done in groups or individually. Relaxation techniques are among the top 10 complementary therapies commonly used by children aged 4 to 17 years in the USA (12,18). Despite the popularity and relative ease of relaxation training, the evidence for its use as a management option for paediatric headache has not been comprehensively reviewed.
OBJECTIVE
The objective of this analysis was to assess the effectiveness of relaxation training for paediatric headaches. Headache pain (e.g., frequency, duration, intensity) were considered primary outcomes of interest. Secondary or pain-related outcomes (e.g., pain catastrophizing, depression, quality of life, coping) and symptoms associated with headaches (e.g., nausea and vomiting, dizziness) were also relevant. Although quality of life and similar outcomes are a high priority for paediatric primary headaches, the findings pertaining to secondary outcomes were highly heterogenous and insufficient for synthesis.
METHODS
Search strategy and screening
The literature search was conducted using Medline, EMBASE, CINAHL, PsycINFO, Cochrane Central Register of Controlled Trials, and Google Scholar. The databases were searched from inception to September 2016 using the search terms listed in Appendix 1 (Medline search strategy) and the initial title and abstract screening were done by a health sciences librarian. Reference lists of review articles and included studies were also searched. Full-text assessments were performed by one author (APT) with additional reviewers available to generate consensus.
A priori inclusion criteria included:
1. English-language full-text peer reviewed publications
2. Paediatric population (0 to 18 years of age inclusive)
3. Relaxation training for management of primary headaches
4. One or more pain outcomes (duration, frequency, or intensity of pain)
5. Controlled trials
A priori exclusion criteria included:
1. Studies combining adult and paediatric populations unless they provided separate information for the paediatric groups
2. Studies investigating other psychological therapies (e.g., biofeedback, cognitive behavioural therapy, hypnosis, yoga) unless a relaxation training management group was explicitly specified
Synthesis and quality of evidence
After data extraction, synthesis was conducted using a narrative approach due to the heterogeneity of outcome measures. Articles were critically appraised to determine the quality of evidence using The Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach (19) and the Cochrane risk of bias tool (20). As suggested by GRADE recommendations, outcomes were reported individually (Table 1).
Table 1.
GRADE quality of evidence profile of included studies evaluating relaxation training for paediatric headache
| Outcome | Risk of biasa | Inconsistency | Indirectness | Imprecision | Publication bias | Quality determination |
|---|---|---|---|---|---|---|
| Headache frequency | Serious limitations | Serious limitationsb | No serious limitations | Serious limitationsc | Undetected | (+) very low |
| Headache intensity | Serious limitations | Serious limitationsb | No serious limitations | Serious limitationsc | Undetected | (+) very low |
| Headache duration | Serious limitations | Serious limitationsb | No serious limitations | Serious limitationsc | Undetected | (+) very low |
aRisk of bias detailed in Table 5.
bHigh heterogeneity related to variation of interventions and measurement of outcomes.
cWide confidence intervals, small sample sizes.
RESULTS
Summary of included studies
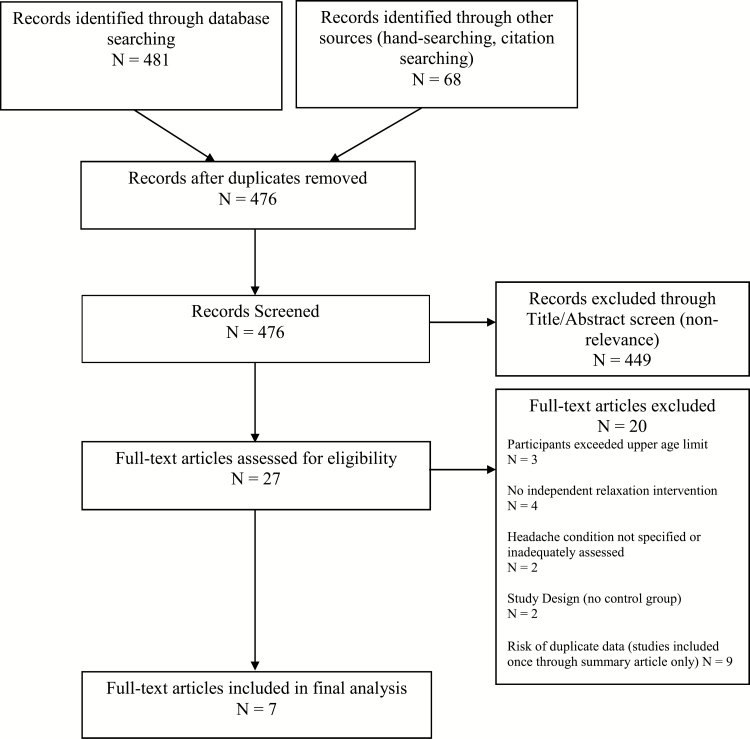
Our electronic and manual searches generated 476 titles for review. 449 articles were excluded through title and abstract screening, and 20 were excluded during full-text assessment and data extraction (Figure 1). Seven articles reporting on controlled trials published between 1986 and 2010 met the inclusion criteria and reported on a total n=571 children, aged 8 to 18 years (Table 2). Relaxation therapy was compared with other psychological therapies (such as cognitive behaviour therapy, biofeedback), waitlist control, or placebo. Headache frequency (n=7 studies), duration (n=5 studies), and intensity (n=6 studies) were the most common outcome measures (Tables 3 and 4). Outcomes in all studies were measured from subject headache diaries completed during a baseline period, treatment period, and at one or more post-treatment intervals.
Figure 1.
Study selection flow diagram. Diagram adapted from ref. (29).
Table 2.
Condition and patient characteristics of included studies evaluating relaxation training for paediatric headache
| First Author | Condition Studied | N | Age Range (years) | Mean Age (years) | Gender (M:F) |
|---|---|---|---|---|---|
| Richter et al. | Migraine | 42 | 9–18 | 12.87 | 17:34a |
| Fentress et al. | Migraine | 18 | 8–12 | 10.1 | 7:11 |
| McGrath et al. | Migraine | 99 | 9–17 | 13.1 | 30:69 |
| Wisneiwski et al. | Migraine or TTH | 10 | 12–17 | 13.5 | 3:7 |
| Kroner-Herwig et al. | TTH or TTH/Migraine combined | 50 | 8–14 | 10.96 | 20:30 |
| Larsson et al. | Migraine or TTH | 288 | 10–18 | Not reported | 30:258 |
| Trautmann et al. | Migraine, TTH or both | 64 | 10–18b | 12.7 | 28:33 |
TTh Tension-type headache.
aGender was reported prior to attrition.
bThe upper age was discrepantly reported as 18 and 19. Follow-up was done at 12 months, so the variation is likely to represent the chronological progression during the study period.
Table 3.
Summary of included studies evaluating relaxation training for management of paediatric headache (descriptions as per primary study reporting)
| Author | Condition | Group description | Number of patients | Duration of intervention | Data collection intervals | Outcome | Measurement description | Reported Results |
|---|---|---|---|---|---|---|---|---|
| Richter et al., 1986 | Migraine | RelaxationTraining (subdivided into high and low headache severity after baseline) | 15 total7 low8 high | 6 weeks | Data collection × 4 weeks | Headache diary completed 4×/day | ||
| Baseline | ||||||||
| Post-treatment | ||||||||
| Cognitive Copinga (subdivided into high and low headache severity after baseline) | 15 total8 low7 high | Follow-up at 12–16 weeks post-treatment | Headache Frequency | Scoring not described | P<0.05 only for high severity group compared to placebo | |||
| NS compared to cognitive coping | ||||||||
| Headache Peak Intensity | Scored 0–5 | No significant effect | ||||||
| Headache Duration | Scoring not described | No significant effect | ||||||
| Placebo (subdivided into high and low headache severity after baseline) | 12 total7 low5 high | Medication Used | Scoring not described | Not reported | ||||
| Headache Index | Composite, not further described | P<0.05 only for high severity group | ||||||
| Headache Activity | Composite, not further described | Not reported | ||||||
| Fentress et al., 1986 | Migraine | Relaxation-response | 6 | 11 weeks | Data collection × 4 weeks | Weekly Headache Diary | ||
| Relaxation-response + biofeedback | 6 | Baseline | Headache Frequency | Scoring not described (headache-free days recorded in weekly diary) | Relaxation P<0.01 | |||
| Waitlist control | 6 | During intervention (11 weeks) | Hours of headache weekly | Total hours of headache/week | Relaxation P<0.01 | |||
| Relaxation + biofeedback P<0.05 | ||||||||
| 1 year after treatment | Headache Activity | Product of headache intensity (scored 0–4) and duration (weekly sum) | Relaxation P<0.05 | |||||
| Relaxation + biofeedback P<0.01 | ||||||||
| McGrath et al., 1988 | Migraine | Relaxation (subdivided into high and low headache severity after baseline) | 32 | 6 weeks | Data collection × 4 weeks | Headache diary completed 4×/day | All outcomes improved over time. No significant effect of treatment group on any outcome. | |
| Placebo (subdivided into high and low headache severity after baseline) | 30 | Baseline | Headache Index | Sum of all 28 ratings in 1 week | ||||
| Own best effortsb (subdivided into high and low headache severity after baseline) | 37 | Post-treatment | Headache Intensity | Scored 0–4 | ||||
| 3-month follow-up | Headache-free days | Not described further | ||||||
| 1-year follow-up | Highest weekly headache rating | Not described further | ||||||
| Headaches greater than scale 2 | Not described further | |||||||
| Wisneiwski et al., 1988 | Migraine or TTH | Relaxation | 5 | 8-session training – duration not reported. | Data collection × 2–3 weeks | Headache diary completed 4×/day | ||
| Waitlist control | 5 | Baseline (3 weeks) | Headache index | Average daily headache score (sum of 28 ratings divided by 4) | Treatment vs. control, P=0.004 | |||
| Post-treatment (2 weeks) | Headache-free days | Number of days in a week for which the patient has no headache | No significant effect | |||||
| 1-month Follow-up (2 weeks) | Peak headache rating | Single highest headache rating among the 28 ratings from the week | No significant effect | |||||
| Percent improvement | Average headache index during baseline minus average headache index for the last 2 weeks of treatment divided by the average headache index during baseline and multiplied by 100 | Treatment Participants: 3 Improved (score of 50% or higher) 1 Slightly Improved (score between 20%-49%) 1 unimproved (score less than 20%) Control Participants: 5 Unimproved (score less than 20%) |
||||||
| Medication index | Sum of the product of the number of doses of a drug multiplied by its potency scale (adopted from a cited external source). | Not significant | ||||||
| Kroner-Herwig et al., 1998 | TTH or TTH/Migraine combined | Relaxation (subdivided into with or without parental involvement) | 20 total 10 with 10 without parental involvement |
6 weeks | Data collection × 4 weeks | Frequency of diary completion not reported | ||
| Baseline | Headache frequency | Yes / no | Improvement over time | |||||
| Post-treatment | Headache duration | Graphic presentation on a clock, not further described | Improvement over time | |||||
| Biofeedback (subdivided into with or without parental involvement) | 20 total 10 with 10 without parental involvement |
6-month follow-up | Headache intensity | Scored 0–10 | Pooled effect of treatment vs. control, P=0.024 | |||
| Waitlist control | 10 | Medication use | # medication intakes/day | No significant effect | ||||
| Disruptive effects of headache | Selections from 6 possible categories, not described further | Not reported | ||||||
| Larsson et al., 2005 | Migraine or TTH | Therapist-assisted relaxation (TAR) | 47 | Not reported | Data collection × 3–4 weeks | Headache diary completed 4×/day | ||
| School nurse-assisted relaxation (SNAR) | 44 | Baseline | Headache sum | Sum of all headache intensity scores weekly (range 0–140) | P<0. 001 for TTH | |||
| Self-help relaxation (SHR) | 59 | Post-treatment | Headache-free days | Number of days when no headache was recorded (range 0–7) Scored yes/no |
P<0.05 by treatment group | |||
| Attention-control (ATCO) | 57 | 6–10-month follow-up | Peak headache intensity | Highest intensity rating recorded per week (range 0–5) Visual analogue scale (range 0–10) |
P< 0.001 | |||
| Self-monitoring (SM) | 81 | Headache duration | Reported in hours. Mean length of all weekly headache episodes (range 0–4) |
No significant effect | ||||
| Medication Usage | Number of analgesic pills each week | P< 0.05 TAR for TTH | ||||||
| Trautmann et al., 2010 | Migraine, TTH or both | Cognitive Behavioural Therapy | 24 | 6 weeks | Data collection × 4 weeks | Headache diary completed daily | All groups showed reduction in headache frequency and duration between pre–post. Clinical improvement = > 50% reduction in headache frequency. 63% of CBT group, 32% of AR group, and 19% of EDU group met clinical improvement criteria. |
|
| Applied Relaxationc | 22 | Baseline | Headache frequency | Scored yes/no | ||||
| Educational Intervention | 18 | Post-treatment | Headache duration | Reported in hours | ||||
| 6-month follow-up | Headache intensity | Visual analogue scale (range 0–10) | ||||||
TTH Tension-type headache.
aCognitive coping – a program developed by the authors which included used elements of cognitive restructuring, the cognitive control of pain, fantasy simple problem solving, and stress-inoculation training.
bOwn best efforts – a single session to discuss the use of a headache diary to determine triggers. The baseline headache diary was reviewed with the therapist in one session to elicit and supply suggestions to reduce triggers.
cApplied relaxation – self-help modules provided by CD with instructions for progressive relaxation, differential relaxation, and cue-controlled relaxation.
Table 4.
Summary of findings of relaxation training for paediatric headache
| Outcome | Measure used | Number and design of studies | Number of patients | Quality of evidence (GRADE)a | Comments |
|---|---|---|---|---|---|
| Headache Duration | Duration in hours Some studies used total duration and others a mean score. |
5 RCTs | N=462 | (+) very low | Unable to calculate estimate of effect due to measurement heterogeneity and incomplete reporting. Two of the five studies found benefit of relaxation training. |
| Headache Frequency | Headache yes/no Data collection ranged from weekly to 4×/day. Some studies analyzed frequency and others used headache-free days. |
7 RCTs | N=571 | (+) very low | Unable to calculate estimate of effect due to measurement heterogeneity and incomplete reporting. Four of the seven studies found benefit of relaxation training. |
| Headache Intensity | Pain scale, range 0–5 and 0–10 Some studies used peak intensity (highest reported score) and others a mean score. |
6 RCTs | N=553 | (+) very low | Unable to calculate estimate of effect due to measurement heterogeneity and incomplete reporting. Two of the six studies found benefit of relaxation training. |
Quality of evidence
The quality of evidence on the effectiveness of relaxation training for paediatric headaches across all outcomes was very low. Areas of concern regarding risk of bias (Table 5), threats to statistical conclusion validity (i.e., low statistical power, unreliability of treatment implementation, unreliability of measures), heterogeneity of headache type, width of confidence intervals, and unclear reporting required downgrading of the quality of evidence determination. The methods used for obtaining and calculating data from the headache diary were generally underreported, limiting the transparency and reproducibility of study findings. Effect estimates were not calculated due to heterogeneity of outcome measurements.
Table 5.
Risk of bias* of included studies evaluating relaxation training for paediatric headache
| First author, year | Selection bias | Performance bias | Detection bias | Attrition bias | Reporting bias | |
|---|---|---|---|---|---|---|
| Random sequence generation | Allocation concealment | Blinding of participants and personnel | Blinding of outcome assessment | Incomplete outcome data | Selective reporting | |
| Richter et al., 1986 | ? | ? | ✗ | ✗ | ✓ | ✓ |
| Fentress et al., 1986 | ? | ? | ✗ | ✗ | ✗ | ✓ |
| McGrath et al., 1988 | ? | ? | ✗ | ✗ | ✗ | ✗ |
| Wisneiwski et al., 1988 | ✗ | ? | ✗ | ✗ | ✗ | ✗ |
| Kroner-Herwig et al., 1998 | ? | ? | ✗ | ✗ | ✗ | ✓ |
| Larsson et al., 2005 | ? | ? | ✗ | ✗ | ✗ | ✓ |
| Trautmann et al., 2010 | ? | ? | ✗ | ✗ | ✓ | ✓ |
*Risk of bias for each study was determined using the criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions (20).
✓ low risk of bias for the selected domain.
✗ high risk of bias for the selected domain.
? unclear due to reporting.
Headache frequency
All seven included studies assessed headache frequency. Four of the seven studies reported a beneficial effect of relaxation training (21–24), although Larsson and colleagues (23) only noted the significant main effect for children with TTH. Results also suggested possible enduring effects of relaxation training, with subjects reporting maintained or improved scores of headache frequency between post-treatment and follow-up assessments 1-month to 1-year post-treatment across the studies.
There was heterogeneity across the studies relating to the definition and measurement of headache frequency. For example, headache frequency was measured and reported as weekly frequency (22), however, we noted variability in outcome measurement between studies that used a single daily diary entry (24) and those that gathered data up to four times daily (25,26). Variability was also noted wherein headache frequency was reported as a sum over the duration of data collection compared to a mean score. In addition, four of the included studies (21,22,24,27) reported headache frequency as a positive value assigned if a headache occurred on a given day, whereas the remaining studies measured and reported headache-free days (23,25,26).
Headache duration
Five of the seven included articles reported on headache duration. Results for the effect of relaxation training on headache duration were mixed: Two reported benefit (22,24) and three reported no significant effect (21,23,27). Headache duration was operationalized differently across the included articles. For example, one study created a mean duration score (no units provided) from the reported length of headache episode which was recorded in a diary four times daily (23). Another study used total hours of headache reported weekly, although it is unclear if the weekly scores were summed or averaged for the final included measurement (22).
Headache intensity
Severity of headache pain was reported as a headache intensity variable and was assessed in six (21,23–27) of the seven included articles. Headache intensity was measured differently across the studies. In one article, the highest intensity score (range 0 to 5) per week was used (23), whereas another study used the average daily intensity ratings of a visual analogue scale (range 0 to 10) that included headache-free days which lowered the mean ratings (24). Results did not clearly support relaxation training to significantly decrease headache intensity, with only two of the six articles reporting a positive effect (23,27). The effects for headache intensity were additionally ambiguous because one of the positive studies divided the relaxation group into subgroups: with and without parental involvement. The relaxation group with parental involvement was associated with decreased headache intensity, whereas the relaxation group without parental involvement was not significantly more effective than the control group (27). The remaining four studies found no significant effect of relaxation training on headache intensity (21,24–26).
Additional headache outcomes
Among included articles, secondary outcomes such as medication usage (21,23,26,27) and psychological states such as depression and pain catastrophizing (24) were measured but were either not reported in enough detail or not captured in multiple studies to allow for synthesis. Composite headache outcomes were also included in some analyses; however, these were generally not clearly defined or reported. For example, one combined headache outcome was identified as total headache activity (23), but authors did not report how this score was calculated. Other studies (21,25,26) used a headache index which was also poorly operationalized. One study reported headache index as the sum of 28 ratings from one week, but did not specify how the score was attained from the headache diary. The headache diary contained ratings of headache frequency, intensity, and duration that were recorded four times daily over a 4-week period (21).
Adverse events
Specific adverse event data collection was not evident in any of the included studies. No adverse events were reported in any of the included studies. While relaxation therapy is generally considered very safe, there have been reports of anxiety, intrusive thoughts, and fear of losing control (28).
LIMITATIONS
Limitations are related to the quality of individual studies and diversity across the evidence which hindered the ability generates clear recommendations for practice. Specifically, the small number of studies, threats to statistical conclusion validity within included studies, incomplete or unclear reporting, and lack of adverse event monitoring denote the preliminary state of the evidence. For example, authors included common headache outcomes such as frequency, duration, and intensity, but measurement approaches differed across studies (e.g., sums, mean scores, and peak scores). In addition, variables and measurement were often poorly reported (e.g., vague or missing variable definitions, not describing methods to calculate scores from raw data) which limited our ability to aggregate the data and generate clear evidence of outcomes. Additional limitations of the literature relate to heterogeneity of the relaxation intervention, specifically ambiguity about the use of relaxation as a sole compared to adjunct therapy, and the impact of varying dose and frequency regimens.
IMPLICATIONS
The results concerning the effects of relaxation training to decrease pain associated with headaches in children were mixed and the quality of evidence was very low by GRADE assessment. Across all outcomes, there were no clear effect estimates and results were highly inconsistent. Findings from the included studies suggest the potential for relaxation training to decrease paediatric headache frequency, with four out of seven studies reporting significant positive effects. Results for headache intensity and duration did not clearly support a benefit of relaxation training. Given the inconsistency of the findings and low quality of the studies, generating strong conclusions about the effectiveness of relaxation training for children with headaches is limited. Future research will benefit from the use of reliable and validated measures, addition of secondary outcomes such as quality of life, and better study design to mitigate threats such as low statistical power. Despite low-quality evidence, the safety of relaxation therapy can be a positive starting point for clinicians to engage in discussions with families and children expressing interest in nonpharmacological approaches for headaches.
PRACTICE POINTS
• Very-low-quality evidence (per GRADE criteria) suggests a possible benefit of relaxation training to reduce frequency but not duration or intensity of paediatric primary headache.
• There is insufficient evidence to generate conclusions relating to relaxation training for a particular headache type (TTH, migraine, or mixed-type), population subgroup, or use as single therapy compared with adjunctive therapy.
• Further research is necessary to improve the quality of evidence and to clarify the role of relaxation training in the management of paediatric headaches.
Funding
APT is funded by the generous support of the Stollery Children’s Hospital Foundation through the Women and Children’s Health Research Institute. The funding body supported the authors’ time commitment for this research without input into the design of the study, collection, analysis and interpretation of data, or writing of the manuscript.
Potential Conflicts of Interest
All authors: No reported conflicts of interest. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
Ethics Approval and Consent to Participate
Not applicable.
ACKNOWLEDGEMENTS
The authors thank Dr. Susanne King-Jones for her expertise developing and conducting the search strategy for this review.
APPENDIX 1
Medline Search - September 27, 2016
1. exp Pain/
2. exp Headache/
3. exp Acute Pain/
4. exp Pain, Postoperative/
5. pediatric pain.mp.
6. Pain Management/
7. neonatal pain.mp.
8. facial pain/ or neck pain/ or pain, intractable/
9. exp Meditation/
10. exp Relaxation Therapy/
11. exp Mindfulness/
12. MBSR.mp.
13. mindfulness-based stress reduction.mp.
14. relaxation training.mp.
15. 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8
16. 9 or 10 or 11 or 12 or 13 or 14
17. 15 and 16
18. limit 17 to “all child (0 to 18 years)”
19. limit 18 to english language
References
- 1. Gofshteyn JS, Stephenson DJ. Diagnosis and management of childhood headache. Curr Probl Pediatr Adolesc Health Care 2016;46(2):36–51. [DOI] [PubMed] [Google Scholar]
- 2. Hershey AD. Pediatric headache. Continuum (Minneap Minn) 2015;21(4 Headache):1132–45. [DOI] [PubMed] [Google Scholar]
- 3. Abu-Arafeh I, Razak S, Sivaraman B, Graham C. Prevalence of headache and migraine in children and adolescents: A systematic review of population-based studies. Dev Med Child Neurol 2010;52(12):1088–97. [DOI] [PubMed] [Google Scholar]
- 4. U.S. Department of Health and Human Services, National Institutes of Health, National Center for Complementary and Alternative Medicine. Exploring the science of complementary and alternative medicine: third strategic plan 2011–2015 [Internet]. Washington, DC: National Center for Complementary and Alternative Medicine; 2011; 2015 (cited March 30, 2017). Report No.: NIH Publication Number 11–7643, D45. Available from: https://nccih.nih.gov/sites/nccam.nih.gov/files/about/plans/2011/NCCAM_SP_508.pdf (Accessed March 30, 2017). [Google Scholar]
- 5. Trautmann E, Lackschewitz H, Kröner-Herwig B. Psychological treatment of recurrent headache in children and adolescents–a meta-analysis. Cephalalgia 2006;26(12):1411–26. [DOI] [PubMed] [Google Scholar]
- 6. Eccleston C, Palermo TM, Williams A, et al. Psychological therapies for the management of chronic and recurrent pain in children and adolescents. Cochrane Database Syst Rev [Internet] 2014 (cited January 2, 2017). Available from: http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD003968.pub4/pdf (Accessed January 2, 2017).
- 7. Huguet A, Tougas ME, Hayden J, et al. Systematic review of childhood and adolescent risk and prognostic factors for recurrent headaches. J Pain 2016;17(8):855–73.e8. [DOI] [PubMed] [Google Scholar]
- 8. Bonvanie IJ, Kallesøe KH, Janssens KAM, Schröder A, Rosmalen JGM, Rask CU. Psychological interventions for children with functional somatic symptoms: A systematic review and meta-analysis. J Pediatr 2017;187:272–81.e17. [DOI] [PubMed] [Google Scholar]
- 9. Fisher E, Heathcote L, Palermo TM, de C Williams AC, Lau J, Eccleston C. Systematic review and meta-analysis of psychological therapies for children with chronic pain. J Pediatr Psychol 2014;39(8):763–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ng QX, Venkatanarayanan N, Kumar L. A systematic review and meta-analysis of the efficacy of cognitive behavioral therapy for the management of pediatric migraine. Headache 2017;57(3):349–62. [DOI] [PubMed] [Google Scholar]
- 11. Stubberud A, Varkey E, McCrory DC, Pedersen SA, Linde M. Biofeedback as prophylaxis for pediatric migraine: A meta-analysis. Pediatrics. 2016;138(2):e20160675. [DOI] [PubMed] [Google Scholar]
- 12. Section on Integrative Medicine. Mind-body therapies in children and youth. Pediatrics. 2016;138(3):e20161896. [DOI] [PubMed] [Google Scholar]
- 13. Noel M, Petter M, Parker J, Chambers C. Cognitive behavioral therapy for pediatric chronic pain: The problem, research, and practice. J Cogn Pyschotherapy. 2012;26(2):143–56. [Google Scholar]
- 14. Sun-Edelstein C, Mauskop A. Complementary and alternative approaches to the treatment of tension-type headache. Curr Pain Headache Rep 2012;16(6):539–44. [DOI] [PubMed] [Google Scholar]
- 15. Verhagen AP, Damen L, Berger MY, Passchier J, Koes BW. Behavioral treatments of chronic tension-type headache in adults: Are they beneficial?CNS Neurosci Ther 2009;15(2):183–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Hayes-Skelton SA, Roemer L, Orsillo SM, Borkovec TD. A contemporary view of applied relaxation for generalized anxiety disorder. Cogn Behav Ther 2013;42(4):292–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Conrad A, Roth WT. Muscle relaxation therapy for anxiety disorders: It works but how?J Anxiety Disord 2007;21(3):243–64. [DOI] [PubMed] [Google Scholar]
- 18. Black LI, Clarke TC, Barnes PM, Stussman BJ, Nahin RL. Use of complementary health approaches among children aged 4–17 years in the United States: National health interview survey, 2007–2012. Natl Health Stat Rep. 2015;10(78):1–19. [PMC free article] [PubMed] [Google Scholar]
- 19. Guyatt GH, Oxman AD, Vist GE, et al. ; GRADE Working Group GRADE: An emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008;336(7650):924–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Higgins JP, Altman DG, Gøtzsche PC, et al. ; Cochrane Bias Methods Group; Cochrane Statistical Methods Group The Cochrane collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011;343:d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Richter IL, McGrath PJ, Humphreys PJ, Goodman JT, Firestone P, Keene D. Cognitive and relaxation treatment of paediatric migraine. Pain 1986;25(2):195–203. [DOI] [PubMed] [Google Scholar]
- 22. Fentress DW, Masek BJ, Mehegan JE, Benson H. Biofeedback and relaxation-response training in the treatment of pediatric migraine. Dev Med Child Neurol 1986;28(2):139–46. [DOI] [PubMed] [Google Scholar]
- 23. Larsson B, Carlsson J, Fichtel A, Melin L. Relaxation treatment of adolescent headache sufferers: Results from a school-based replication series. Headache 2005;45(6):692–704. [DOI] [PubMed] [Google Scholar]
- 24. Trautmann E, Kröner-Herwig B. A randomized controlled trial of internet-based self-help training for recurrent headache in childhood and adolescence. Behav Res Ther 2010;48(1):28–37. [DOI] [PubMed] [Google Scholar]
- 25. McGrath PJ, Humphreys P, Goodman JT, et al. Relaxation prophylaxis for childhood migraine: A randomized placebo-controlled trial. Dev Med Child Neurol 1988;30(5):626–31. [DOI] [PubMed] [Google Scholar]
- 26. Wisniewski JJ, Genshaft JL, Mulick JA, Coury DL, Hammer D. Relaxation therapy and compliance in the treatment of adolescent headache. Headache 1988;28(9):612–7. [DOI] [PubMed] [Google Scholar]
- 27. Kröner-Herwig B, Mohn U, Pothmann R. Comparison of biofeedback and relaxation in the treatment of pediatric headache and the influence of parent involvement on outcome. Appl Psychophysiol Biofeedback 1998;23(3):143–57. [DOI] [PubMed] [Google Scholar]
- 28. National Center for Complementary and Integrative Health. Relaxation Techniques for Health [Internet]. National Center for Complementary and Integrative Health. 2011 [cited 2018 Mar 23] Available from: https://nccih.nih.gov/health/stress/relaxation.htm (Accessed March 23, 2017).
- 29. Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ 2009;339:b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]