Abstract
Background
Venous thromboembolism (VTE) often complicates the clinical course of cancer. The risk is further increased by chemotherapy, but the trade‐off between safety and efficacy of primary thromboprophylaxis in cancer patients treated with chemotherapy is uncertain. This is the second update of a review first published in February 2012.
Objectives
To assess the efficacy and safety of primary thromboprophylaxis for VTE in ambulatory cancer patients receiving chemotherapy compared with placebo or no thromboprophylaxis.
Search methods
For this update the Cochrane Vascular Information Specialist searched the Cochrane Vascular Group Specialised Register (June 2016). In addition, the Information Specialist searched the Cochrane Central Register of Controlled Trials (CENTRAL) (2016, Issue 5). Clinical trials registries were searched up to June 2016.
Selection criteria
Randomised controlled trials comparing any oral or parenteral anticoagulant or mechanical intervention to no thromboprophylaxis or placebo, or comparing two different anticoagulants.
Data collection and analysis
We extracted data on methodological quality, participant characteristics, interventions, and outcomes including symptomatic VTE and major bleeding as the primary effectiveness and safety outcomes, respectively.
Main results
We identified five additional randomised controlled trials (2491 participants) in the updated search, considering in this update 26 trials with a total of 12,352 participants, all evaluating pharmacological interventions and performed mainly in people with locally advanced or metastatic cancer. The quality of the evidence ranged from high to very low across the different outcomes and comparisons. The main limiting factors were imprecision and risk of bias. One large trial of 3212 participants found a 64% (risk ratio (RR) 0.36, 95% confidence interval (CI) 0.22 to 0.60) reduction of symptomatic VTE with the ultra‐low molecular weight heparin (uLMWH) semuloparin relative to placebo, with no apparent difference in major bleeding (RR 1.05, 95% CI 0.55 to 2.00). When compared with no thromboprophylaxis, LMWH significantly reduced the incidence of symptomatic VTE (RR 0.54, 95% CI 0.38 to 0.75; no heterogeneity, Tau2 = 0.00%) with a non‐statistically significant 44% higher risk of major bleeding events (RR 1.44, 95% CI 0.98 to 2.11). In participants with multiple myeloma, LMWH was associated with a significant reduction in symptomatic VTE compared with the vitamin K antagonist warfarin (RR 0.33, 95% CI 0.14 to 0.83), while the difference between LMWH and aspirin was not statistically significant (RR 0.51, 95% CI 0.22 to 1.17). Major bleeding was observed in none of the participants treated with LMWH or warfarin and in less than 1% of those treated with aspirin. Only one study evaluated unfractionated heparin against no thromboprophylaxis but did not report on VTE or major bleeding. When compared with placebo, warfarin was associated with a non‐statistically significant reduction of symptomatic VTE (RR 0.15, 95% CI 0.02 to 1.20). Antithrombin, evaluated in one study involving paediatric patients, had no significant effect on VTE or on major bleeding when compared with no antithrombin. The direct oral factor Xa inhibitor apixaban was evaluated in a phase II dose‐finding study that suggested a low rate of major bleeding (2.1% versus 3.4%) and symptomatic VTE (1.1% versus 13.8%) in comparison with placebo.
Authors' conclusions
In this second update, we confirmed that primary thromboprophylaxis with LMWH significantly reduced the incidence of symptomatic VTE in ambulatory cancer patients treated with chemotherapy. In addition, the uLMWH semuloparin, which is not commercially available, significantly reduced the incidence of symptomatic VTE. The risk of major bleeding associated with LMWH, while not reaching statistical significance, suggest caution and mandate additional studies to determine the risk‐to‐benefit ratio of LMWH in this setting. Despite the encouraging results of this review, routine prophylaxis in ambulatory cancer patients cannot be recommended before safety issues are adequately addressed. We need additional studies investigating targeted primary prophylaxis in people with specific types or stages of cancer associated with a higher risk of VTE.
Plain language summary
Prevention of blood clots in non‐hospitalised cancer patients receiving chemotherapy
Background
Cancer patients are more likely than people without cancer to develop blood clots in their veins (known as venous thromboembolism). Chemotherapy further increases this risk. Yet a number of factors specific to the cancer, such as the bleeding tendency at the site of the cancer, or a relative decrease in the number of platelets in the blood (thrombocytopenia) caused by chemotherapy can increase the likelihood that cancer patients will have bleeding complications with medicines used to prevent and treat blood clots (anticoagulants). This systematic review looked at the effectiveness and safety of anticoagulants when used to prevent blood clots in cancer patients receiving chemotherapy.
Key results
We included 26 randomised controlled trials involving a total of 12,352 participants (current until June 2016). Low molecular weight heparin and the ultra‐low molecular weight heparin semuloparin were associated with a significant reduction in symptomatic blood clots. We found no evidence that the risk of major bleeding is increased with semuloparin or low molecular weight heparin, but based on the uncertainty around the estimates, we cannot exclude that the risk is doubled. There was no clear survival benefit for semuloparin or low molecular weight heparin. In people with multiple myeloma, low molecular weight heparin significantly reduced the incidence of blood clots when compared with the vitamin K antagonist warfarin, while the difference with aspirin was not significant. There were no major bleeds with low molecular weight heparin or warfarin, and in participants treated with aspirin the rate was below 1%. One study evaluated unfractionated heparin and did not report on venous thromboembolism or major bleeding. There was no mention of blood clots in the two study groups. Data for warfarin in comparison with placebo were too limited to support the use of warfarin in the prevention of blood clots in cancer patients. One study in children evaluated antithrombin, which had no significant effect on blood clots or major bleeding when compared with no antithrombin. A small pilot study evaluated the oral anticoagulant apixaban and found a low rate of bleeding and blood clots compared to placebo.
Quality of the evidence
The quality of the included studies ranged from low to high, such that future studies may change our confidence in the estimates and the size of the estimates, in particular with regard to the safety of anticoagulants. The quality of findings ranged from high to very low across the different outcomes and comparisons. The main limiting factors, which were the reason for a decrease in quality in some outcomes, were imprecision and risk of bias. The relatively low number of studies, participants, and clinical events prevented us from determining the potential influence of age and type or stage of cancer on treatment effects and providing more definitive conclusions about the risk of bleeding in association with anticoagulants. None of the studies tested intermittent pneumatic compression or graduated elastic stockings for the prevention of venous thromboembolism.
Summary of findings
Background
Cancer is often complicated by venous thromboembolism (VTE), which can present as deep vein thrombosis (DVT) or pulmonary embolism (PE), or both (Khorana 2009). Cancer patients with VTE have a two‐fold or greater increased mortality compared with cancer patients without thrombosis, which could be explained by the development of fatal PEs or by a worse prognosis for patients with those cancers complicated by VTE (Sorensen 2000). VTE in cancer patients may be hard to recognise due to aspecific symptoms, which may overlap and be confused with symptoms caused by the underlying cancer disease process or cancer treatments. VTE carries significant morbidity due to the need for hospitalisation and an increased risk of recurrent VTE or bleeding complications while on anticoagulation (Hutten 2000; Prandoni 2002). The occurrence of symptomatic or unsuspected VTE may delay the delivery of cancer treatments such as chemotherapy, with a further negative impact on morbidity and potentially mortality. In addition, the occurrence of venous thromboembolic events brings further emotional strain for patients and their families, which negatively impacts their quality of life. Finally, the costs related to the management of VTE may be considerable, resulting from the expenses related to the drugs and hospitalisation (Heit 2015).
Description of the condition
The incidence of VTE is higher in people with cancer compared with people without cancer (Heit 2015). Compared with an incidence of about 0.1% in the general population, the rate of VTE in people with cancer has been reported to vary between 0.6% and about 8% (Khorana 2009). Chemotherapy has been recognised as an independent predictor for symptomatic VTE, with reported rates of from 11%, in Otten 2004, up to 75%, in Heit 2015 and Khorana 2009, depending on the type of chemotherapeutic agent used. The risk of thrombosis in cancer patients receiving chemotherapy seems to vary based on the stage of the disease, ranging from 3% to 5% in patients with early‐stage cancer to 30% in those with metastatic or advanced malignancy (Khorana 2009). The benefit‐risk ratio of primary prophylaxis in ambulatory patients with cancer who are receiving chemotherapy is not well established, and current guidelines do not recommend routine thromboprophylaxis in such patients (Lyman 2013).
Description of the intervention
Currently available drugs for the prevention of VTE are the parenteral anticoagulants, which include unfractionated heparin (UFH), low molecular weight heparins (LMWH), and fondaparinux, vitamin K antagonists (VKAs), and the oral direct thrombin inhibitor dabigatran and the factor Xa inhibitors rivaroxaban, apixaban, and edoxaban. In fact, each one of these agents may present disadvantages for long‐term prophylaxis in the ambulatory patient with cancer. Heparins and fondaparinux, as well as the new ultra‐low molecular weight heparin (uLMWH) semuloparin, require daily subcutaneous injections, which represent a considerable burden for the patient. Of note is that marketing applications for the uLMWH semuloparin have been withdrawn worldwide, and it is therefore unlikely to ever be commercially available (EMEA 2012). Both the direct thrombin inhibitor dabigatran and the factor Xa inhibitors offer the potential advantages of an oral route of administration, and in comparison with VKAs do not require routine laboratory monitoring and have fewer pharmacological interactions. VKAs and direct thrombin or factor Xa inhibitors can be difficult to administer in cancer patients with nausea or vomiting.
The use of pharmacological prophylaxis may be more challenging in people with cancer. The efficacy of pharmacological thromboprophylaxis could be reduced by the intrinsic procoagulant state induced by the cancer itself, prothrombotic treatments for cancer (e.g. chemotherapy), as well as the decline in the patient's general condition leading to immobilisation. On the other hand, the risk of bleeding events could be high even with prophylactic doses because of a number of predisposing factors such as the bleeding tendency at the site of the cancer, the relative decrease in the number of platelets in the blood (thrombocytopenia) secondary to chemotherapy, and the concomitant use of drugs (e.g. bevacizumab) that affect the vessel wall integrity (Kamphuisen 2014).
Currently available mechanical interventions for the prevention of VTE include intermittent pneumatic compression and graduated elastic stockings. These non‐pharmacological interventions may be a valid option in cancer patients who are at risk of bleeding, however evidence supporting their benefit and assuring no harm is limited.
Why it is important to do this review
The overall burden of VTE in people with cancer is steadily increasing as a result of an aging population, greater awareness, frequent staging assessments using sensitive imaging techniques, prothrombotic anticancer treatments, as well as the growing cancer population that is due to the aforementioned aging (Heit 2015). Provision of widespread primary thromboprophylaxis for ambulatory cancer patients who receive chemotherapy may help in preventing this complication. However, the efficacy of thromboprophylaxis needs to be balanced against the risks, such as (major) bleeding events.
Objectives
Our main objective was to assess the efficacy and safety of primary thromboprophylaxis for VTE in ambulatory patients with cancer receiving chemotherapy compared with placebo or no thromboprophylaxis. The secondary objective was to compare the efficacy and safety of different types of primary thromboprophylaxis by stratifying the main results per type of drug or mechanical intervention, and by aggregating results from head‐to‐head comparisons.
Methods
Criteria for considering studies for this review
Types of studies
All randomised controlled trials (RCTs) and quasi‐randomised trials were eligible.
Types of participants
Ambulatory outpatients at the time of randomisation or study entry. Participants of any age (including paediatric patients) with either a solid or haematological cancer, at any stage, and receiving chemotherapy were eligible. We excluded studies of participants receiving anticoagulation for a previous VTE or an indication other than VTE if data could not be extracted separately for participants not on anticoagulants. We excluded studies evaluating prophylaxis for catheter‐related thrombosis, since this is already the subject of another Cochrane review (Akl 2011).
Types of interventions
Interventions included any oral or parenteral anticoagulant (for example UFH, LMWH, uLMWH, fondaparinux, direct thrombin or factor Xa inhibitors, VKAs) or mechanical intervention (intermittent pneumatic compression or graduated elastic stockings), or both, used to prevent VTE in ambulatory patients with cancer that were receiving chemotherapy. Comparison interventions included either no thromboprophylaxis in the form of an inactive control intervention (placebo, no treatment, standard care) or an active control intervention (a different scheme or regimen of the same intervention, a different pharmacological type of prophylaxis, a different type of non‐pharmacological prophylaxis). We considered any frequency or duration of administration, dosage or intensity, and timing of delivery of pharmacological prophylaxis.
Types of outcome measures
Primary outcomes
The main effectiveness outcome was symptomatic VTE, objectively verified by means of Doppler (compression) ultrasonography or venography for DVT, and spiral computed tomography, ventilation/perfusion lung scan, or pulmonary angiography for PE.
The main safety outcome was major bleeding, typically defined as overt bleeding associated with a fall in haemoglobin of 2 g/dL or more, or leading to a transfusion of two or more units of packed red blood cells or whole blood; bleeding that occurred at a critical site (intracranial, intraspinal, intraocular, pericardial, intra‐articular, intramuscular with compartment syndrome, retroperitoneal); or bleeding contributing to death (Schulman 2005).
Secondary outcomes
Secondary outcomes included symptomatic PE; symptomatic DVT; unsuspected (incidental) VTE; overall (symptomatic and unsuspected) VTE; clinically relevant bleeding (major and clinically relevant non‐major bleeding); minor bleeding; one‐year overall mortality; arterial thromboembolic events; superficial venous thrombosis; quality of life; and number of participants experiencing any serious adverse event. Clinically relevant non‐major bleeding is typically defined as overt bleeding that does not meet the criteria for major bleeding, but is associated with the need for medical intervention, contact with a physician, or interruption of the study drug or with discomfort or impairment of activities of daily life. Minor bleeding was defined as a bleeding event not matching the criteria for major bleeding or clinically relevant non‐major bleeding. Serious adverse events were defined as events resulting in patient hospitalisation, prolongation of hospitalisation, persistent or significant disability, congenital abnormality or birth defect of offspring, life‐threatening events or death. For trials using LMWH as the intervention or control, heparin‐induced thrombocytopenia (HIT) and the incidence of osteoporosis, as defined by the trial authors, were recorded. We considered all outcomes as binary outcomes except for quality of life, which we considered a continuous outcome.
For the 'Summary of findings' tables, we selected the following outcomes as the most patient‐relevant ones:
symptomatic VTE;
major bleeding;
symptomatic PE;
symptomatic DVT;
one‐year mortality;
clinically relevant bleeding.
Search methods for identification of studies
Electronic searches
For this update, the Cochrane Vascular Information Specialist (CIS) searched the following databases for relevant trials:
Cochrane Vascular Specialised Register (23 June 2016);
Cochrane Central Register of Controlled Trials (CENTRAL) (2016, Issue 5) via the Cochrane Register of Studies Online.
See Appendix 1 for details of the search strategy used to search CENTRAL.
The Cochrane Vascular Specialised Register is maintained by the CIS and is constructed from weekly electronic searches of MEDLINE Ovid, Embase Ovid, CINAHL, AMED, and through handsearching relevant journals. The full list of the databases, journals and conference proceedings which have been searched, as well as the search strategies used are described in the Specialised Register section of the Cochrane Vascular module in the Cochrane Library (www.cochranelibrary.com).
The CIS searched the following clinical trials registries (last searched 23 June 2016) by combining the search terms 'cancer' and 'thrombosis':
ClinicalTrials.gov (www.clinicaltrials.gov);
World Health Organization International Clinical Trials Registry Platform (www.who.int/trialsearch);
ISRCTN Register (www.isrctn.com/).
Searching other resources
The review authors searched the reference lists of identified studies and contacted content experts and trialists for relevant references. One review author screened the conference proceedings of the American Society of Clinical Oncology (from 2009 to 2015) and the International Society of Thrombosis and Haemostasis (from 2003 to 2016), combining the search terms of 'venous thrombosis', 'vein thrombosis', or 'pulmonary embolism' with 'cancer' or 'tumour'. We included studies if we could obtain adequate information from either the abstract or personal communication.
Data collection and analysis
Selection of studies
Two review authors (MDN, MC) independently reviewed the titles and abstracts identified from the database searches to determine whether they met the inclusion criteria. Any disagreements were resolved through discussion between the review authors. The review authors were not blinded to the journal, institution, or results of the study. We applied no language restrictions. We reassessed studies with insufficient information if we were able to obtain additional information from the trial authors. We documented reasons for excluding studies. In the event of multiple reports relating to the same trial, we considered all of the reports.
Data extraction and management
Two review authors (MDN, MC) independently extracted the data from the included studies onto standardised forms, resolving any disagreements by consensus or by involving a third review author (AR). We collected information on methodological quality, participant characteristics, characteristics of the intervention and control groups, and outcome characteristics of every group of participants. Whenever possible, we extracted the results from an intention‐to‐treat analysis. If we could not calculate effect sizes, we contacted the trial authors for additional data.
Assessment of risk of bias in included studies
Two review authors independently assessed randomisation, blinding, and adequacy of analyses (Higgins 2011; Rutjes 2009). Disagreements were resolved by consensus.
We assessed two components of randomisation: generation of allocation sequence and concealment of allocation. We considered generation of the allocation sequence to be adequate if it resulted in an unpredictable allocation schedule. Mechanisms considered to be adequate included random number tables, computer‐generated random numbers, minimisation, coin tossing, shuffling cards, and drawing lots. We considered trials using an unpredictable allocation sequence to be randomised. We considered trials using potentially predictable allocation mechanisms, such as alternation or allocation of participants according to date of birth, date of presentation, or case record number, to be quasi‐randomised.
We considered concealment of allocation to be adequate if participants and the investigators responsible for participant selection were unable to predict before allocation which treatment was next. Methods considered adequate included central randomisation; pharmacy‐controlled randomisation using identical, pre‐numbered containers; and sequentially numbered, sealed, opaque envelopes. We considered blinding of participants and therapists to be adequate if experimental and control preparations were explicitly described as indistinguishable, or if a double‐dummy technique was used. We considered assessors to be blinded if this was explicitly mentioned by the investigators.
We considered analyses to be at low risk of bias if all randomised participants were included in the analyses according to the intention‐to‐treat principle. We classified the item 'free of selective reporting' as at low risk of bias if we had both the protocol and the full report of a given study, where the full report presented results for all outcomes listed in the protocol. We classified a study as at high risk of bias if a report did not present data on all outcomes reported in either the protocol or the methods section. We did not consider the item 'free of other bias' in this review. We assessed the reporting of primary outcomes and sample size calculations. Finally, we used GRADE to describe the quality of the overall body of evidence (Guyatt 2008; Higgins 2011), defined as the extent of our confidence in the estimates of treatment benefits and harms.
Measures of treatment effect
We have presented results as summary risk ratios (RRs) for dichotomous variables, determining a 95% confidence interval (CI) for each estimate. We used inverse‐variance random‐effects model meta‐analysis to combine the trials (DerSimonian 1986). In the case of statistically significant overall estimates, we also calculated clinical effect summary statistics such as the number needed to treat for an additional beneficial outcome (NNTB) or the number needed to treat for an additional harmful outcome (NNTH) to express the final results of the review.
Assessment of heterogeneity
We measured heterogeneity of the treatment effect between trials using the variance estimate Tau2, as currently recommended by the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). A Tau2 of 0.04 is typically interpreted to indicate low heterogeneity, 0.09 moderate heterogeneity, and 0.16 high heterogeneity across trials (Rutjes 2012; Spiegelhalter 2004).
Assessment of reporting biases
We evaluated publication bias and other biases related to small study size using funnel plots, plotting the RRs on the vertical axis against their standard errors on the horizontal axis (Sterne 2001). Funnel plot symmetry would be expected in the absence of any bias related to small study size. We used the Harbord–Egger's test to assess symmetry (Harbord 2006). We further explored any anomaly in stratified analyses, in which we investigated the effects of differences in types of LMWH, age, type of cancer, and suboptimal design choices on the magnitude of the effects.
Data synthesis
In the main analyses, we analysed and presented data by stratifying for the type of thromboprophylaxis used.
We planned to explore the between‐trial heterogeneity by stratifying the main outcomes for the following trial characteristics: age (below or equal to 65 years versus above 65 years); type of cancer, stage of cancer (metastatic versus non‐metastatic); type of major bleeding (according to the definition provided by Schulman 2005 versus unclear or different definition); concealment of allocation (adequate versus inadequate or unclear); blinding (adequate versus inadequate or unclear); analysis in accordance with the intention‐to‐treat principle (yes versus no or unclear); trial size (large versus small); and differences in the use of co‐interventions in the trial groups. We planned to use univariate random‐effects model meta‐regression to determine whether treatment effects were affected by these factors and by three continuous variables at trial level: dosage of intervention, treatment duration, and length of follow‐up (Thompson 1999).
We defined large trials as those randomising 1360 participants or more. This threshold was informed by the following sample size calculation: according to the Khorana 2008 score, cancer patients at high risk of symptomatic VTE who could potentially receive thromboprophylaxis have an incidence of 7.1% over a period of about 3 months. Assuming that the risk of VTE can be halved by thromboprophylaxis, a total number of about 1360 participants would be needed to detect a statistically significant difference between groups.
We performed the data analysis in Review Manager 5 (RevMan 2014). We performed stratified analyses and funnel plot exploration in STATA release 14 (Stata 2015).
'Summary of findings' table
We presented the main findings of the review concerning the quality of the evidence, magnitude of effect of the interventions examined, and sum of available data in a 'Summary of findings' table, according to the GRADE principles described by Higgins 2011 and Guyatt 2008. For the critical outcome symptomatic VTE, we applied cutoffs to define high and intermediate risk groups. We used a cutoff of 7% to define high risk, which is in line with the cutoff proposed by Khorana 2008, which is between 6.7% and 7.1% over a period of about 3 months. We used event rates between 2% and 7% to define intermediate risk groups to experience symptomatic VTEs (Khorana 2008).
Results
Description of studies
See Characteristics of included studies; Characteristics of excluded studies.
Results of the search
See Figure 1.
1.
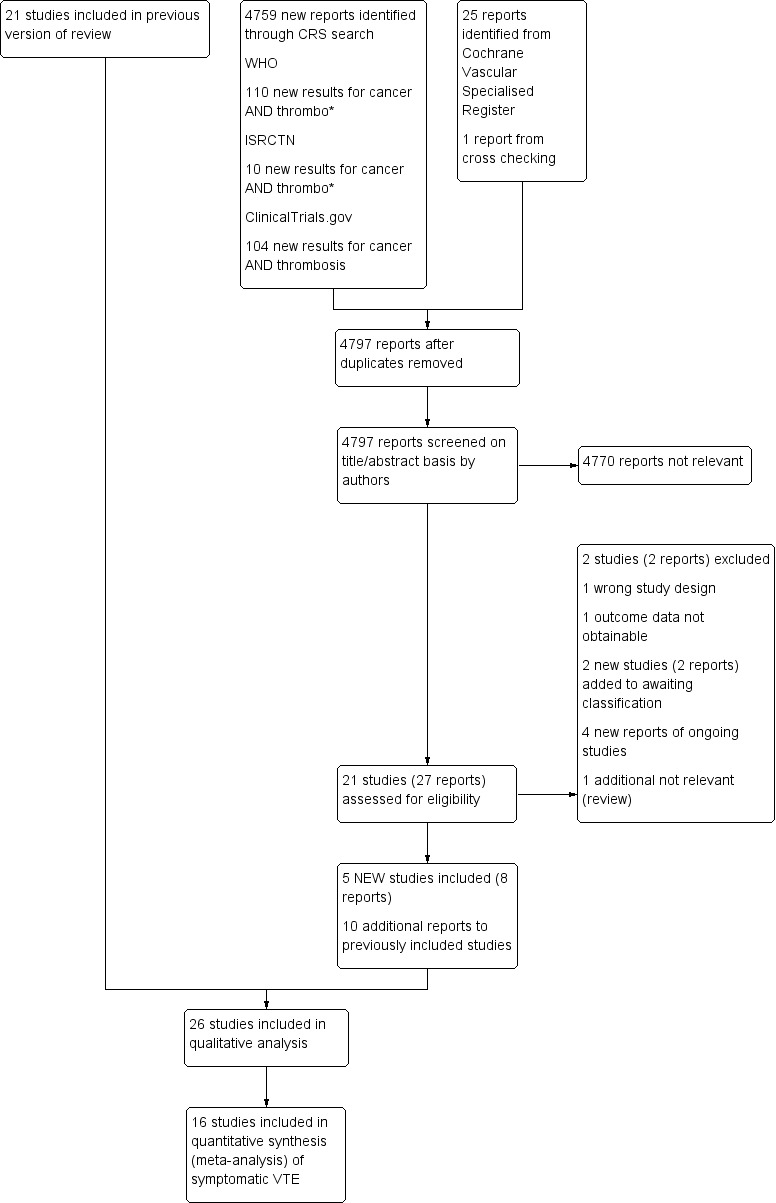
Study flow diagram.
Following title and abstract screening, we considered 27 reports (21 trials) to be potentially eligible for this update. We included eight reports related to five new trials (Elit 2012; Khorana 2015; Lecumberri 2013; Macbeth 2016; Vadhan‐Raj 2013), and 10 reports were related to previously included trials. We added four reports to the Characteristics of ongoing studies table (NCT00717938; NCT02048865; NCT02285738; NCT02555878), and two to the Characteristics of studies awaiting classification table (Ciftci 2012; NCT00771563). We added two reports to the excluded studies (Bocharov 2011; Gercor 2013). We assessed one report that was a review as not relevant.
Included studies
For this update we included five new studies (Elit 2012; Khorana 2015; Lecumberri 2013; Macbeth 2016; Vadhan‐Raj 2013). Four of these were reported as ongoing studies in the previous version of the review (Elit 2012; Khorana 2015; Macbeth 2016; Vadhan‐Raj 2013), and one was an excluded study (Lecumberri 2013). We added four additional ongoing studies (NCT00717938; NCT02048865; NCT02285738; NCT02555878), and added two additional studies to Studies awaiting classification (Ciftci 2012; NCT00771563).
In total, 26 RCTs randomising a total of 12,352 participants were eligible for inclusion in the review. The treatments evaluated consisted of the uLMWH semuloparin (Agnelli 2012), LMWH (Agnelli 2009; Altinbas 2004; Elit 2012; Haas 2012; Kakkar 2004; Khorana 2015; Klerk 2005; Larocca 2012; Lecumberri 2013; Macbeth 2016; Maraveyas 2012; Palumbo 2011; Pelzer 2015; Perry 2010; Sideras 2006; Vadhan‐Raj 2013; van Doormaal 2011; Zwicker 2013), UFH (Lebeau 1994), the VKA warfarin (Chahinian 1989; Levine 1994; Maurer 1997; Palumbo 2011; Zacharski 1981), antithrombin (Mitchell 2003), and the oral direct factor Xa inhibitor apixaban (Levine 2012). None of the included RCTs used non‐pharmacological prophylaxis, or pharmacological thromboprophylaxis with fondaparinux, the direct thrombin inhibitor dabigatran, or the direct factor Xa inhibitors rivaroxaban and edoxaban. In 15 (8056 participants, 65%) of the 26 studies, inclusion was restricted to people with locally advanced or metastatic cancer, in two studies limited cancer was included, in four studies both early and advanced disease were included, while in the remaining studies the stage was not clear (see Characteristics of included studies).
One study assessed the uLMWH semuloparin versus placebo.
Agnelli 2012 recruited participants (n = 3212) with metastatic or locally advanced solid cancer of the lung, pancreas, stomach, colon or rectum, bladder, or ovary and randomised them to the uLMWH semuloparin (20 mg once daily) versus placebo starting on the first day of a first or new regimen of chemotherapy. The intervention was continued for three months unless chemotherapy was stopped earlier.
Eigtheen studies assessed LMWH.
Sixteen studies assessed LMWH either versus placebo or no thromboprophylaxis (Agnelli 2009; Altinbas 2004; Haas 2012; Kakkar 2004; Khorana 2015; Klerk 2005; Lecumberri 2013; Macbeth 2016; Maraveyas 2012; Pelzer 2015; Perry 2010; Sideras 2006; Vadhan‐Raj 2013; van Doormaal 2011; Zwicker 2013), or compared different doses from prophylactic to full therapeutic of LMWH with each other (Elit 2012). These 16 trials varied in the duration and type of LMWH, including eight weeks to 48 months of subcutaneous (sc) dalteparin, enoxaparin, certoparin, nadroparin, bemiparin. The dose of LMWH was prophylactic in the majority of the studies and intermediate, in Pelzer 2015, or therapeutic, in Maraveyas 2012, in one study each. In two studies initial therapeutic LMWH was followed by intermediate doses (Klerk 2005; van Doormaal 2011). Fifteen of these 16 studies reported a mean age at study entry of 65 years or younger, whereas Zwicker 2013 included participants with a mean age above 65.
Agnelli 2009 recruited participants (n = 1150) with metastatic or locally advanced lung, gastrointestinal, pancreatic, breast, ovarian, or head and neck cancer and randomised them to nadroparin (3800 IU anti‐factor Xa sc, once daily) versus placebo. Study treatment started on the same day as chemotherapy and was given for the duration of the chemotherapy or up to a maximum of 120 days (± 10 days).
Altinbas 2004 recruited participants (n = 84) with histologically confirmed small cell lung carcinoma and randomised them to standard anticancer treatment with or without dalteparin (5000 IU sc, once daily). Dalteparin was stopped with disease progression or at the end of the 18 weeks of chemotherapy.
Elit 2012 recruited women (n = 77) with newly diagnosed epithelial ovarian cancer and randomised them to receive standard chemotherapy and one of three subcutaneous doses of dalteparin (50 IU/kg, 100 IU/kg, or 150 IU/kg), once daily during the first three of six cycles of three‐weekly chemotherapy.
Haas 2012 recruited participants with metastatic breast cancer (n = 353) or non‐small cell lung carcinoma (n = 547) and receiving first‐ or second‐line chemotherapy. Participants were randomised to six months of certoparin (3000 IU sc, once daily) versus placebo.
Kakkar 2004 recruited participants (n = 385) with histologically confirmed locally advanced or metastatic malignant disease of the breast, lung, gastrointestinal tract, pancreas, liver, genitourinary tract, ovary, or uterus and randomised them to dalteparin (5000 IU sc, once daily) versus placebo. Study treatment was given for one year or until the participant died, whichever occurred sooner.
Khorana 2015 recruited cancer patients (n = 98) at high risk for VTE (Khorana score ≥ 3) who initiated a new systemic chemotherapy regimen and randomised them to dalteparin (5000 IU sc, once daily) versus no thromboprophylaxis for 12 weeks.
Klerk 2005 recruited participants (n = 302) with metastasised or locally advanced solid tumours and randomised them to nadroparin versus placebo. Study treatment was given using pre‐filled syringes containing a fixed volume of nadroparin (anti‐factor Xa 9500 U/mL) or placebo according to the participant’s weight: 0.4 mL for those weighing less than 50 kg, 0.6 mL for those weighing between 50 kg and 70 kg, and 0.8 mL for those weighing more than 70 kg. Study treatment was to be administered sc twice daily during the initial 14 days of treatment and once daily thereafter for another four weeks.
Lecumberri 2013 recruited participants (n = 39) with newly diagnosed, limited‐stage small cell lung cancer and randomised them to standard chemoradiotherapy alone or combined with bemiparin 3500 IU daily for a maximum of 26 weeks.
Macbeth 2016 recruited participants (n = 2202) with histopathologic or cytologic diagnosis of primary bronchial carcinoma of any stage and histology (small cell or non‐small cell) and randomised them to standard anticancer treatment (including active supportive or palliative care) with or without dalteparin (5000 IU sc, once daily) for a maximum of 24 weeks.
Maraveyas 2012 recruited participants (n = 123) with advanced pancreatic cancer and randomised them to dalteparin (200 IU/kg sc, once daily for four weeks followed by 150 IU/kg for a further eight weeks) in combination with gemcitabine versus gemcitabine alone. Continuing dalteparin prophylaxis after 12 weeks was not recommended, but was left to the discretion of the investigator.
Pelzer 2015 recruited participants (n = 312) with histologically or cytologically confirmed advanced pancreatic cancer. Participants were randomised to standard anticancer treatment with or without enoxaparin (1 mg/kg once daily) for three months, started simultaneously with palliative systemic chemotherapy; after 12 weeks of initial chemotherapy, all participants who had not progressed received the standard therapy with or without enoxaparin (40 mg once daily) for an additional three months.
Perry 2010 recruited participants (n = 186) with newly diagnosed, pathologically confirmed World Health Organization (WHO) grade 3 or grade 4 glioma and randomised them to six months of dalteparin (5000 IU sc, once daily) versus placebo starting within the first month after surgery. Participants were allowed to continue the study medication for 12 months.
Sideras 2006 recruited participants (n = 138) with advanced breast cancer who did not respond to first‐line chemotherapy, advanced prostate cancer resistant to primary hormonal therapy, advanced lung cancer, or advanced colorectal cancer. In the first part of the study, participants were randomised to dalteparin (5000 IU sc, once daily) versus placebo, while in the second part participants were randomised to dalteparin (5000 IU sc, once daily) plus standard clinical care versus standard clinical care alone. Dalteparin (or placebo) was given for 18 weeks or until disease progression.
Vadhan‐Raj 2013 recruited participants (n = 75) with advanced stage (unresectable or metastatic) adenocarcinoma of the pancreas planning to initiate systemic chemotherapy and randomised them to chemotherapy with or without dalteparin (5000 IU sc, once daily) for 16 weeks.
van Doormaal 2011 recruited participants (n = 503) with non–small cell lung cancer (stage IIIB), hormone‐refractory prostate cancer, or locally advanced pancreatic cancer and randomised them to standard anticancer treatment with or without nadroparin. Subcutaneous nadroparin was administered for six weeks (two weeks at therapeutic dose and four weeks at half therapeutic dose). The participants were eligible to receive additional cycles of nadroparin (two weeks at therapeutic dose and four weeks washout period) for a maximum of six cycles.
Zwicker 2013 recruited participants (n = 34) with histologically confirmed advanced stage malignancy, which included adenocarcinoma of the pancreas (locally advanced or metastatic), colorectal (stage IV), non‐small cell lung cancer (stage III or IV), relapsed or stage IV ovarian, or surgically unresectable or metastatic gastric adenocarcinoma. Participants were randomised to enoxaparin (40 mg sc, once daily) for two months or observation.
In two additional studies, LMWH was compared against an active control:
Larocca 2012 recruited participants (n = 342) with newly diagnosed multiple myeloma treated with lenalidomide and low‐dose dexamethasone induction and melphalan‐prednisone‐lenalidomide consolidation. Participants were randomised to aspirin (100 mg per day) or LMWH (enoxaparin 40 mg per day). Prophylaxis was provided during the four (28‐day) cycles of induction and the six (28‐day) cycles of consolidation therapy.
Palumbo 2011 recruited participants (n = 667) with previously untreated myeloma who received thalidomide‐containing regimens and randomised them to aspirin (100 mg per day), low‐dose warfarin (1.25 mg per day) or LMWH (enoxaparin 40 mg per day). The prophylaxis was administered during the three cycles of induction therapy in participants ≤ 65 years of age and during the first six cycles of induction therapy in participants > 65 years.
Four studies compared the VKA warfarin against no thromboprophylaxis or placebo.
Chahinian 1989 recruited participants (n = 328) with extensive carcinoma of the lung and randomised them to warfarin (dose to maintain a prothrombin time 1.5 to twice the control values) versus no warfarin. Warfarin was continued throughout the course of chemotherapy.
Levine 1994 recruited participants (n = 311) with metastatic stage IV breast carcinoma who had been receiving first‐ or second‐line chemotherapy for four weeks or less and randomised them to warfarin (target of international normalised ratio (INR) 1.3 to 1.9) versus placebo. Study treatment began either at the start of chemotherapy or within the following four weeks and continued until one week after termination of chemotherapy.
Maurer 1997 recruited participants (n = 347) with limited‐stage small cell lung cancer who were to receive chemotherapy and radiotherapy and randomised them to warfarin or no warfarin. Warfarin (dose of 10 mg per day for the first three days and then at a dose to maintain the prothrombin time between 1.4 and 1.6 times the local institutional control standards) was continued through the complete course of chemotherapy and radiation therapy and was stopped three weeks after the last cycle of chemotherapy.
Zacharski 1981 recruited participants (n = 50) with small cell lung cancer and randomised them to warfarin (dose to prolong the prothrombin time to approximately two times the control value) versus no warfarin.
UFH, antithrombin, and the factor Xa inhibitor apixaban were evaluated against placebo or no thromboprophylaxis in one study each.
Lebeau 1994 recruited participants (n = 277) with limited and extensive small cell lung cancer who had not been previously treated with chemotherapy or radiotherapy. The dose of UFH was initially adapted to weight (500 IU/kg/day), then adjusted by clotting times (different techniques used, and results had to be between two and three times the control value). UFH was administered in two or three daily injections for five weeks and stopped one week after the second course of chemotherapy.
Levine 2012 recruited participants (n = 125) receiving either first‐ or second‐line chemotherapy for advanced or metastatic lung, breast, gastrointestinal, bladder, ovarian, or prostate cancer; cancer of unknown origin; myeloma; or selected lymphomas. Participants were randomised to apixaban 5 mg (n = 32), 10 mg (n = 30), 20 mg (n = 33), and placebo (n = 30). The study treatment was given for 12 weeks, beginning within four weeks of starting chemotherapy.
Mitchell 2003 recruited paediatric patients (n = 85) newly diagnosed with acute lymphoblastic leukaemia and randomised them to receive, or not, weekly infusions of antithrombin.
Excluded studies
We excluded two additional studies in this update (Bocharov 2011; Gercor 2013) making for a total of 24 excluded studies. The reasons for exclusion were: design other than an RCT (Baz 2005; Bocharov 2011; Kessler 2011; Meister 2008; Minnema 2004; Paydas 2008; Zangari 2003); studies on perioperative thromboprophylaxis (Bergqvist 1983; Heilmann 1995; Hills 1972; Macintyre 1974; Maxwell 2000; Sideras 2007; Welti 1981); inclusion of hospitalised cancer patients (Eichinger 2008; Haas 2011; Poniewierski 1987; Weber 2008); no relevant outcomes reported (Rajan 1995); no eligible intervention (Niesvizky 2007); prophylaxis was for catheter‐related thrombosis (Kwaan 2007). Three studies were terminated early: Levin 2008 because of a drug supply issue; Gercor 2013 due to the lack of eligible patients; Pandya 2002 with no reason for study termination reported.
We added four studies to ongoing studies (NCT00717938; NCT02048865; NCT02285738; NCT02555878).
Risk of bias in included studies
The 'Risk of bias' summary is shown in Figure 2.
2.
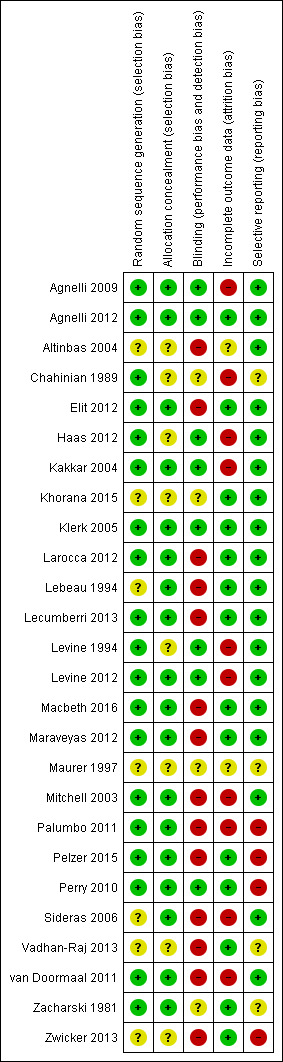
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
The random sequence was adequately generated in 19 studies (Agnelli 2009; Agnelli 2012; Chahinian 1989; Elit 2012; Haas 2012; Kakkar 2004; Klerk 2005; Larocca 2012; Lecumberri 2013; Levine 1994; Levine 2012; Macbeth 2016; Maraveyas 2012; Mitchell 2003; Palumbo 2011; Pelzer 2015; Perry 2010; van Doormaal 2011; Zacharski 1981), but was unclear in the remaining studies due to poor reporting.
Allocation was adequately concealed in 18 studies (Agnelli 2009; Agnelli 2012; Elit 2012; Kakkar 2004; Klerk 2005; Larocca 2012; Lebeau 1994; Lecumberri 2013; Levine 2012; Macbeth 2016; Maraveyas 2012; Mitchell 2003; Palumbo 2011; Pelzer 2015; Perry 2010; Sideras 2006; van Doormaal 2011; Zwicker 2013), and was unclear in the remaining studies due to poor reporting.
Blinding
Eight studies had a double‐blinded design (Agnelli 2009; Agnelli 2012; Haas 2012; Kakkar 2004; Klerk 2005; Levine 1994; Levine 2012; Perry 2010), and 14 were open studies (Altinbas 2004; Elit 2012; Larocca 2012; Lebeau 1994; Lecumberri 2013; Macbeth 2016; Maraveyas 2012; Mitchell 2003; Palumbo 2011; Pelzer 2015; Sideras 2006; Vadhan‐Raj 2013; van Doormaal 2011; Zwicker 2013). In four studies blinding was unclear due to poor reporting (Chahinian 1989; Khorana 2015; Maurer 1997; Zacharski 1981).
Incomplete outcome data
Fourteen studies performed the analysis according to the intention‐to‐treat principle (Agnelli 2012; Elit 2012; Khorana 2015; Klerk 2005; Larocca 2012; Lebeau 1994; Lecumberri 2013; Macbeth 2016; Maraveyas 2012; Pelzer 2015; Perry 2010; Vadhan‐Raj 2013; Zacharski 1981; Zwicker 2013), while in nine studies the percentages of participants randomised and subsequently excluded from the analyses ranged from 1.3% to 10% (Agnelli 2009; Chahinian 1989; Haas 2012; Kakkar 2004; Levine 1994; Levine 2012; Palumbo 2011; Sideras 2006; van Doormaal 2011); we considered these to be at high risk of bias. The study involving paediatric patients used a per‐protocol analysis and excluded 22% of the participants that were initially enrolled (Mitchell 2003); we considered this study to be at high risk of bias. Attrition bias was unclear in Altinbas 2004 and Maurer 1997.
Selective reporting
We judged 18 studies to be free of selective reporting (Agnelli 2009; Agnelli 2012; Altinbas 2004; Elit 2012; Haas 2012; Kakkar 2004; Khorana 2015; Klerk 2005; Larocca 2012; Lebeau 1994; Lecumberri 2013; Levine 1994; Levine 2012; Macbeth 2016; Maraveyas 2012; Mitchell 2003; Sideras 2006; van Doormaal 2011). In four studies one or more outcomes that were reported in the results were not anticipated in the methods sections of the publications (Chahinian 1989; Maurer 1997; Vadhan‐Raj 2013; Zacharski 1981). In four studies not all outcomes were reported in the results (Palumbo 2011; Pelzer 2015; Perry 2010; Zwicker 2013).
Effects of interventions
See: Table 1; Table 2; Table 3; Table 4; Table 5; Table 6; Table 7; Table 8; Table 9; Table 10
Summary of findings for the main comparison. Semuloparin versus placebo.
| Semuloparin compared with placebo for primary thromboprophylaxis in ambulatory cancer patients receiving chemotherapy | |||||||
|
Patient or population: ambulatory cancer patients receiving chemotherapy Settings: outpatient clinics Intervention: semuloparin Comparison: placebo | |||||||
| Outcomes | Relative effect (95% CI) | Illustrative comparative risks* (95% CI) | Difference2 (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | What it means | |
| Assumed risk1 | Corresponding risk | ||||||
| Without semuloparin | With semuloparin | ||||||
|
Symptomatic VTE: Follow‐up: median 3.5 months |
RR 0.36 (0.22 to 0.60) | Intermediate‐risk population3 | 22 per 1000 fewer events (14 to 27 fewer) | 3212 (1) | ⊕⊕⊕⊕ high |
Semuloparin decreases the incidence of symptomatic VTE across different cancer types. | |
| 34 per 1000 | 12 per 1000 (8 to 21) | ||||||
|
Major bleeding Follow‐up: median 3.5 months |
RR 1.05 (0.55 to 2.0) | Intermediate‐risk population3 | 1 per 1000 more events (5 fewer to 11 more) | 3172 (1) | ⊕⊕⊝⊝ low4 |
Semuloparin may increase major bleedings across different cancer types. | |
| 11 per 1000 | 12 per 1000 (6 to 23) | ||||||
|
Symptomatic PE Follow‐up: median 3.5 months |
RR 0.48 (0.22 to 1.01) | Intermediate‐risk population3 | 7 per 1000 fewer events (0 to 10 fewer) | 3212 (1) | ⊕⊕⊕⊝ moderate5 |
Semuloparin probably decreases the incidence of symptomatic PE across different cancer types. | |
| 13 per 1000 | 6 per 1000 (3 to 13) | ||||||
|
Symptomatic DVT Follow‐up: median 3.5 months |
RR 0.32 (0.16 to 0.63) | Intermediate‐risk population3 | 14 per 1000 fewer events (8 to 18 fewer) | 3212 (1) | ⊕⊕⊕⊕ high |
Semuloparin decreases the incidence of symptomatic DVT across different cancer types. | |
| 21 per 1000 | 7 per 1000 (3 to 13) | ||||||
|
1‐year mortality Follow‐up: 1 year |
RR 1.02 (0.96 to 1.08) | Intermediate‐risk population3 | 11 per 1000 more events (22 fewer to 44 more) | 3212 (1) | ⊕⊕⊕⊝ moderate5 |
Semuloparin probably has no effect on 1‐year mortality across different cancer types. | |
| 555 per 1000 | 566 per 1000 (533 to 599) | ||||||
|
Clinically relevant bleeding Follow‐up: median 3.5 months |
RR 1.40 (0.90 to 2.19) | Intermediate‐risk population3 | 8 per 1000 more events (2 fewer to 24 more) | 3172 (1) | ⊕⊕⊕⊝ moderate5 |
Semuloparin probably increases the incidence of clinically relevant bleeding across different cancer types. | |
| 20 per 1000 | 28 per 1000 (18 to 44) | ||||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; DVT: deep vein thrombosis; NA: not applicable; PE: pulmonary embolism; RR: risk ratio; VTE: venous thromboembolism | |||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | |||||||
1The assumed risk is calculated from the medium observed control group risk in the study. 2Difference calculated as the absolute risk difference between the assumed risk and corresponding risk, expressed per 1000. 3Intermediate risk population refers to the observed median risk to experience symptomatic VTE in the single trial contributing to the analyses (34 per 1000). Rates between 2% and 7% are considered intermediate risk (Khorana 2008). 4Downgraded (2 levels) because of imprecision. 5Downgraded (1 level) because of imprecision.
Summary of findings 2. Low molecular weight heparin versus no thromboprophylaxis.
| Low molecular weight heparin compared with no thromboprophylaxis for primary thromboprophylaxis in ambulatory cancer patients receiving chemotherapy | |||||||
|
Patient or population: ambulatory cancer patients receiving chemotherapy Settings: outpatient clinics Intervention: LMWH Comparison: no thromboprophylaxis (placebo or no LMWH) | |||||||
| Outcomes | Relative effect (95% CI) | Illustrative comparative risk (95% CI)* | Difference (95% CI)2 | No of participants (studies) | Quality of the evidence (GRADE) | What it means | |
| Assumed risk1 | Corresponding risk | ||||||
| No thromboprophylaxis | With LMWH | ||||||
|
Symptomatic VTE Follow‐up: median 10 months |
RR 0.54 (0.38 to 0.75) | High‐risk population3 | 33 per 1000 fewer events (18 to 44 fewer) | 3284 (9) | ⊕⊕⊕⊕ high4 | LMWH decreases the incidence of symptomatic VTE across different cancer types. | |
| 71 per 1000 | 39 per 1000 (27 to 54) |
||||||
|
Major bleeding Follow‐up: median 12 months |
RR 1.44 (0.98 to 2.11) | High‐risk population3 | 8 per 1000 more major bleeds (0 to 19 more) | 6356 (13) | ⊕⊕⊝⊝ low5 | LMWH may increase major bleedings across different cancer types. | |
| 17 per 1000 | 25 per 1000 (17 to 36) |
||||||
|
Symptomatic PE Follow‐up: median 10 months |
RR 0.59 (0.40 to 0.86) | High‐risk population3 | 6 per 1000 fewer events (2 to 8 fewer) | 5226 (7) | ⊕⊕⊝⊝ low6 | LMWH may decrease the incidence of symptomatic PE across different cancer types. | |
| 14 per 1000 | 8 per 1000 (6 to 12) |
||||||
|
Symptomatic DVT Follow‐up: median 10 months |
RR 0.49 (0.35 to 0.67) | High‐risk population3 | 15 per 1000 fewer events (10 to 19 fewer) | 5310 (8) | ⊕⊕⊕⊕ high7 |
LMWH decreases the incidence of symptomatic DVT across different cancer types. | |
| 29 per 1000 | 14 per 1000 | ||||||
|
1‐year mortality Follow‐up: median 12 months |
RR 0.93 (0.80 to 1.09) | High‐risk population3 | 41 per 1000 fewer deaths (117 fewer to 53 more) | 2304 (8) | ⊕⊕⊝⊝ low8 | LMWH may decrease the incidence of death across different cancer types. | |
| 587 per 1000 | 546 per 1000 (470 to 640) |
||||||
|
Clinically relevant bleeding Follow‐up: median 12 months |
RR 3.40 (1.20 to 9.63) | High‐risk population3 | 40 per 1000 more clinically relevant bleeds (3 to 145 more) | 3105 (4) | ⊕⊕⊕⊝ moderate9 |
LMWH probably increases the incidence of clinically relevant bleeding across different cancer types. | |
| 17 per 1000 | 57 per 1000 (20 to 162) |
||||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; DVT: deep vein thrombosis; LMWH: low molecular weight heparin; PE: pulmonary embolism; RR: risk ratio; VTE: venous thromboembolism | |||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | |||||||
1The assumed risk is calculated from the median control group risk across the studies. 2Difference calculated as the absolute risk difference between the assumed risk and corresponding risk, expressed per 1000. 3High‐risk population refers to the median observed risk to experience symptomatic VTE in the trials contributing to the analyses (71 per 1000). Rates from 7% and higher are considered high risk (Khorana 2008). 4Although 5 out of 9 trials were not double‐blinded trials, and 2 out of 9 trials used dosages exceeding typical prophylactic dosages, results were consistent across trials, so we did not downgrade. 5Downgraded (2 levels) because the 95% CI includes both negligible effect and appreciable benefit or appreciable harm; 7 out of 12 trials contributing to the analyses were not double‐blinded, and 3 out of 12 trials did not use standard definitions to ascertain major bleeding. One study reported zero events in both the experimental and control arm, and was not considered in the 'Summary of findings' table. 6Downgraded (2 levels) because the 95% CI includes both negligible effect and appreciable benefit or appreciable harm; risk of selective outcome reporting, with only 5 out of 7 trials reporting symptomatic PE. 7Although 4 out of 8 trials were not double‐blinded trials, and 2 out of 8 trials used dosages exceeding typical prophylactic dosages, results were consistent across trials, so we did not downgrade. 8Downgraded (2 levels) because the 95% CI includes both negligible effect and appreciable benefit or harm; with some variability in estimates across trials due to heterogeneity other than sampling error (chance). 9Downgraded (1 level) due to unexplained between‐trial variation.
Summary of findings 3. Prophylactic versus intermediate or therapeutic dose low molecular weight heparin.
| Low molecular weight heparin: prophylactic dose compared with intermediate or therapeutic dose for primary thromboprophylaxis in ambulatory cancer patients receiving chemotherapy | ||||||||
|
Patient or population: ambulatory cancer patients receiving chemotherapy Settings: outpatient clinics Intervention: prophylactic dose LMWH Comparison: intermediate or therapeutic dose LMWH | ||||||||
| Outcomes | Control type | Relative effect (95% CI) | Illustrative comparative risks* (95% CI) | Difference2 (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | What it means | |
| Assumed risk1 | Corresponding risk | |||||||
| Intermediate/ therapeutic dose | Prophylactic dose | |||||||
| Intermediate‐risk population3 | ||||||||
|
Symptomatic VTE: Follow‐up: median 3.5 months |
Intermediate | RR 2.89 (0.12 to 66.75) | 31 per 1000 | 90 per 1000 (4 to 2086) | 59 per 1000 more events (28 fewer to 2055 more) | 51 (1) | ⊕⊕⊝⊝ low4 |
Prophylactic‐dose LMWH may be associated with a higher risk of symptomatic VTE when compared to intermediate‐dose LMWH in ovarian cancer. |
| Therapeutic | RR 1.00 (0.07 to 15.15) | 53 per 1000 | 53 per 1000 (4 to 805) | 0 per 1000 fewer events (49 fewer events to 752 more) | 52 (1) | ⊕⊕⊝⊝ low4 |
We do not know if prophylactic‐dose LMWH is associated with a higher risk of symptomatic VTE when compared to therapeutic‐dose LMWH in ovarian cancer. | |
| Intermediate‐risk population3 | ||||||||
|
Major bleeding Follow‐up: median 3.5 months |
Intermediate | Not estimable5 | NA | NA | NA | NA | NA | As we have insufficient data to estimate the relative risk, we do not know how prophylactic‐dose LMWH affects major bleeding in ovarian cancer. |
| Therapeutic | Not estimable5 | NA | NA | NA | NA | NA | ||
| Intermediate‐risk population3 | ||||||||
|
Symptomatic PE Follow‐up: median 3.5 months |
Intermediate | RR 2.89 (0.12 to 66.75) | NA6 | NA | NA | NA | NA | As we have insufficient data to estimate the assumed risk, we do not know how prophylactic‐dose LMWH affects symptomatic PE. |
| Therapeutic | RR 3.00 (0.13 to 70.42) | NA6 | NA | NA | NA | NA | ||
| Intermediate‐risk population3 | ||||||||
|
Symptomatic DVT Follow‐up: median 3.5 months |
Intermediate | Not estimable5 | NA | NA | NA | NA | NA | We do not know how prophylactic‐dose LMWH affects symptomatic DVT. |
| Therapeutic | RR 0.33 (0.01 to 7.82) | 53 per 1000 | 18 per 1000 (1 to 415) | 36 per 1000 fewer DVT (53 fewer to 362 more) | 52 (1) | ⊕⊕⊝⊝ low4 |
Prophylactic‐dose LMWH may reduce the risk of symptomatic DVT when compared to therapeutic‐dose LMWH in ovarian cancer, although this seems an implausible finding. | |
| Intermediate‐risk population3 | ||||||||
|
1‐year mortality Follow‐up: NA |
Intermediate | NA7 | NA | NA | NA | NA | NA | We do not know how prophylactic‐dose LMWH affects all‐cause mortality when compared to intermediate or therapeutic‐dose LMWH. |
| Therapeutic | NA7 | NA | NA | NA | NA | NA | ||
| Intermediate‐risk population3 | ||||||||
|
Clinically relevant bleeding Follow‐up: median 3.5 months |
Intermediate | NA5 | NA | NA | NA | NA | NA | We do not know how prophylactic‐dose LMWH affects clinically relevant bleeding. |
| Therapeutic | RR 0.33 (0.01 to 7.82) | 38 per 10008 | 13 per 1000 (0 to 301) | 26 per 1000 fewer clinically relevant bleeding (38 fewer to 262 more) | 52 (1) | ⊕⊕⊝⊝ low4 |
Prophylactic‐dose LMWH may reduce clinically relevant bleeding when compared to therapeutic‐dose LMWH in ovarian cancer. | |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; DVT: deep vein thrombosis; LMWH: low molecular weight heparin; NA: not applicable; PE: pulmonary embolism; RR: risk ratio; VTE: venous thromboembolism | ||||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||||
1The assumed risk is calculated from the medium observed control group risk in Elit 2012 and Pelzer 2015 for the intermediate‐dose estimation, and from Elit 2012 and Maraveyas 2012 for therapeutic‐dose LMWH. 2Difference calculated as the absolute risk difference between the assumed risk and corresponding risk, expressed per 1000. 3Intermediate‐risk population refers to the median observed risk to experience symptomatic VTE in the trials contributing to the analyses (31 per 1000 and 53 per 1000). Rates between 2% and 7% are considered intermediate risk (Khorana 2008). 4Downgraded (2 levels) because of imprecision. 5Not estimable due to zero event count in both trial arms. 6We have insufficient data to estimate the assumed risk due to the zero event rate in both the intermediate‐dose and therapeutic‐dose LMWH. 7No trials contributed to this outcome. 8The assumed risk was based on the small trial by Elit 2012 only (the observed event rate in the control group was 1 out of 26).
Summary of findings 4. Low molecular weight heparin versus aspirin.
| Low molecular weight heparin compared with aspirin for primary thromboprophylaxis in ambulatory cancer patients receiving chemotherapy | |||||||
|
Patient or population: ambulatory cancer patients receiving chemotherapy Settings: outpatient clinics Intervention: LMWH Comparison: aspirin | |||||||
| Outcomes | Relative effect (95% CI) | Illustrative comparative risks* (95% CI) | Difference2 (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | What it means | |
| Assumed risk1 | Corresponding risk | ||||||
| Aspirin | With LMWH (any dosage) | ||||||
|
Symptomatic VTE: Follow‐up: median 18.5 months |
RR 0.51 (0.22 to 1.17) | Intermediate‐risk population3 | 19 per 1000 fewer events (30 fewer to 7 more) | 781 (2) | ⊕⊕⊕⊝ moderate4 | LMWH probably decreases the incidence of symptomatic VTE when compared with aspirin in multiple myeloma. | |
| 39 per 1000 | 20 per 1000 (9 to 45) | ||||||
|
Major bleeding Follow‐up: median 18.5 months |
RR 0.14 (0.01 to 2.76) | Intermediate‐risk population3 | 6 per 1000 fewer events (7 fewer to 12 more) | 781 (2) | ⊕⊕⊝⊝ low5 | LMWH may reduce the incidence of major bleeding when compared with aspirin in multiple myeloma. | |
| 7 per 1000 | 1 per 1000 (0 to 19) | ||||||
|
Symptomatic PE Follow‐up: median 18.5 months |
RR 0.13 (0.02 to 1.03) | Intermediate‐risk population3 | 15 per 1000 fewer events (17 fewer to 1 more) | 781 (2) | ⊕⊕⊕⊝ moderate4 | LMWH probably reduces the incidence of symptomatic PE when compared with aspirin in multiple myeloma. | |
| 18 per 1000 | 2 per 1000 (0 to 18) | ||||||
|
Symptomatic DVT Follow‐up: median 18.5 months |
RR 0.81 (0.32 to 2.04) | Intermediate‐risk population3 | 5 per 1000 fewer events (16 fewer to 25 more) | 781 (2) | ⊕⊕⊝⊝ low5 | LMWH may reduce the incidence of symptomatic DVT when compared with aspirin in multiple myeloma. | |
| 24 per 1000 | 19 per 1000 (8 to 49) | ||||||
|
1‐year mortality Follow‐up: NA |
NA6 | Intermediate‐risk population3 | NA | NA | NA | We do not know how LMWH affects 1‐year mortality when compared with aspirin in multiple myeloma. | |
| NA | NA | ||||||
|
Clinically relevant bleeding Follow‐up: NA |
NA6 | Intermediate‐risk population3 | NA | NA | NA | We do not know how LMWH affects clinically relevant bleeding when compared with aspirin in multiple myeloma. | |
| NA | NA | ||||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; DVT: deep vein thrombosis; LMWH: low molecular weight heparin; NA: not applicable; PE: pulmonary embolism; RR: risk ratio; VTE: venous thromboembolism | |||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | |||||||
1The assumed risk is calculated from the medium observed control group risk across the studies. 2Difference calculated as the absolute risk difference between the assumed risk and corresponding risk, expressed per 1000. 3Intermediate‐risk population refers to the median observed risk to experience symptomatic VTE in the trials contributing to the analyses (39 per 1000). Rates between 2% and 7% are considered intermediate risk (Khorana 2008). 4Downgraded (1 level) because of imprecision. 5Downgraded (2 levels) because of imprecision. 6No trials contributed to this outcome.
Summary of findings 5. Low molecular weight heparin versus vitamin K antagonists.
| Low molecular weight heparin compared with vitamin K antagonists for primary thromboprophylaxis in ambulatory cancer patients receiving chemotherapy | |||||||
|
Patient or population: ambulatory cancer patients receiving chemotherapy Settings: outpatient clinics Intervention: LMWH Comparison: VKA | |||||||
| Outcomes | Relative effect (95% CI) | Illustrative comparative risks* (95% CI) | Difference2 (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | What it means | |
| Assumed risk1 | Corresponding risk | ||||||
| With VKA | With LMWH (any dosage) | ||||||
|
Symptomatic VTE: Follow‐up: median 25 months |
RR 0.33 (0.14 to 0.83) | High‐risk population3 | 55 per 1000 fewer events (14 to 70 fewer) | 439 (1) | ⊕⊕⊕⊕ high4 | LMWH reduces the incidence of symptomatic VTE when compared to VKA in multiple myeloma. | |
| 82 per 1000 | 27 per 1000 (11 to 68) | ||||||
|
Major bleeding Follow‐up: median 25 months |
RR not estimable5 | High‐risk population3 | NA | NA | NA | We do not know how LMWH affects major bleeding when compared to VKA. | |
| NA | NA | ||||||
|
Symptomatic PE Follow‐up: median 25 months |
RR 0.11 (0.01 to 2.06) | High‐risk population3 | 16 per 1000 fewer events (18 fewer to 19 more) | 439 (1) | ⊕⊕⊝⊝ low6 | LMWH may reduce the incidence of symptomatic PE when compared to VKA in multiple myeloma. | |
| 18 per 1000 | 2 per 1000 (0 to 37) | ||||||
|
Symptomatic DVT Follow‐up: median 25 months |
RR 0.43 (0.17 to 1.10) | High‐risk population3 | 36 per 1000 fewer events (53 fewer to 6 more) | 439 (1) | ⊕⊕⊕⊝ moderate7 | LMWH probably reduces the incidence of symptomatic DVT when compared to VKA in multiple myeloma. | |
| 64 per 1000 | 27 per 1000 (11 to 70) | ||||||
|
1‐year mortality Follow‐up: NA |
NA8 | High‐risk population3 | NA | NA | NA | We do not know how LMWH affects 1‐year mortality when compared to VKA. | |
| NA | NA | ||||||
|
Clinically relevant bleeding Follow‐up: NA |
NA8 | High‐risk population3 | NA | NA | NA | We do not know how LMWH affects clinically relevant bleeding when compared to VKA. | |
| NA | NA | ||||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; DVT: deep vein thrombosis; LMWH: low molecular weight heparin; NA: not applicable; PE: pulmonary embolism; RR: risk ratio; VKA: vitamin K antagonists; VTE: venous thromboembolism | |||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | |||||||
1The assumed risk is calculated from the observed control group risk in Palumbo 2011. 2Difference calculated as the absolute risk difference between the assumed risk and corresponding risk, expressed per 1000. 3High‐risk population refers to the median observed risk to experience symptomatic VTE in the trials contributing to the analyses (82 per 1000). Rates from 7% and higher are considered high risk (Khorana 2008). 4Although there was some risk of attrition bias, imputation of the missing data in various ways showed that estimates would not change in a clinically relevant manner (data not shown). 5Not estimable due to zero event count in both trial arms. 6Downgraded (2 levels) because of imprecision. 7Downgraded (1 level) because of imprecision. 8No trials contributed to this outcome.
Summary of findings 6. Unfractionated heparin versus no thromboprophylaxis.
| Unfractionated heparin compared with no thromboprophylaxis for primary thromboprophylaxis in ambulatory cancer patients receiving chemotherapy | |||||||
|
Patient or population: ambulatory cancer patients receiving chemotherapy Settings: outpatient clinics Intervention: unfractionated heparin Comparison: no thromboprophylaxis | |||||||
| Outcomes | Relative effect (95% CI) | Illustrative comparative risks* (95% CI) | Difference2 (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | What it means | |
| Assumed risk1 | Corresponding risk | ||||||
| Without UFH | With UFH | ||||||
|
Symptomatic VTE: Follow‐up: NA |
NA3 | Population at unclear risk4 | NA | NA | NA | We do not know how UFH affects symptomatic VTE. | |
| NA | NA | ||||||
|
Major bleeding Follow‐up: NA |
NA3 | Population at unclear risk4 | NA | NA | NA | We do not know how UFH affects major bleeding. | |
| NA | NA | ||||||
|
Symptomatic PE Follow‐up: NA |
NA3 | Population at unclear risk4 | NA | NA | NA | We do not know how UFH affects symptomatic PE. | |
| NA | NA | ||||||
|
Symptomatic DVT Follow‐up: NA |
NA3 | Population at unclear risk4 | NA | NA | NA | We do not know how UFH affects symptomatic DVT. | |
| NA | NA | ||||||
|
1‐year mortality Follow‐up: 1 year |
RR 0.86 (0.72 to 1.03) | Population at unclear risk4 | 98 per 1000 fewer events (195 fewer to 21 more) | 277 (1) | ⊕⊕⊝⊝ moderate5 |
UFH probably decreases the incidence of 1‐year mortality in small cell lung cancer. | |
| 698 per 1000 | 600 per 1000 (502 to 719) | ||||||
|
Clinically relevant bleeding Follow‐up: median not reported, maximum of 4.9 years of follow‐up |
RR 2.01 (0.18 to 21.96) | Population at unclear risk4 | 7 per 1000 more events (6 fewer to 151 more) | 277 (1) | ⊕⊝⊝⊝ low6 |
UFH may increase the risk of clinically relevant bleeding in small cell lung cancer. | |
| 7 per 1000 | 14 per 1000 (1 to 158) | ||||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; DVT: deep vein thrombosis; NA: not applicable; PE: pulmonary embolism; RR: risk ratio; UFH: unfractionated heparin; VTE: venous thromboembolism | |||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | |||||||
1The assumed risk is calculated from the observed control group risk in Lebeau 1994. 2Difference calculated as the absolute risk difference between the assumed risk and corresponding risk, expressed per 1000. 3No trials contributed to this outcome. 4The risk profile refers to the median observed risk to experience symptomatic VTEs. As Lebeau 1994 did not report this outcome, the risk profile remains unclear. 5Downgraded (1 level) because of imprecision. 6Downgraded (2 levels) because of imprecision.
Summary of findings 7. Vitamin K antagonists versus placebo or no thromboprophylaxis.
| Vitamin K antagonists compared with placebo or no thromboprophylaxis for primary thromboprophylaxis in ambulatory cancer patients receiving chemotherapy | |||||||
|
Patient or population: ambulatory cancer patients receiving chemotherapy Settings: outpatient clinics Intervention: VKA Comparison: placebo or no thromboprophylaxis | |||||||
| Outcomes | Relative effect (95% CI) | Illustrative comparative risks* (95% CI) | Difference2 (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | What it means | |
| Assumed risk1 | Corresponding risk | ||||||
| Without VKA | With VKA | ||||||
|
Symptomatic VTE: Follow‐up: mean 6 months |
RR 0.15 (0.02 to 1.2) | Intermediate‐risk population3 | 37 per 1000 fewer events (43 fewer to 9 more) | 311 (1) | ⊕⊕⊝⊝ low4 | VKA may reduce the incidence of symptomatic VTE in breast cancer. | |
| 44 per 1000 | 7 per 1000 (1 to 53) | ||||||
|
Major bleeding Follow‐up: mean 6 months |
RR 3.82 (0.97 to 15.04) | Intermediate‐risk population3 | 18 per 1000 more events (0 fewer to 88 more) | 994 (4) | ⊕⊕⊝⊝ low5 | VKA may increase the incidence of major bleeding in breast cancer and small cell lung cancer. | |
| 6 per 1000 | 24 per 1000 (6 to 95) | ||||||
|
Symptomatic PE Follow‐up: mean 6 months |
RR 1.05 (0.07 to 16.58) | Intermediate‐risk population3 | 0 per 1000 fewer events (6 fewer to 101 more) | 311 (1) | ⊕⊝⊝⊝ very low6 | We have very little confidence in the estimated effect of VKA on symptomatic PE in breast cancer. | |
| 6 per 1000 | 7 per 1000 (0 to 108) | ||||||
|
Symptomatic DVT Follow‐up: mean 6 months |
RR 0.08 (0 to 1.42) | Intermediate‐risk population3 | 35 per 1000 fewer events (38 fewer to 16 more) | 311 (1) | ⊕⊕⊝⊝ low4 | VKA may reduce the incidence of symptomatic DVT in breast cancer. | |
| 38 per 1000 | 3 per 1000 (0 to 54) | ||||||
|
1‐year mortality Follow‐up: NA |
NA | Intermediate‐risk population3 | NA | NA | NA | We do not know how VKA affects 1‐year mortality. | |
| NA | NA | ||||||
|
Clinically relevant bleeding Follow‐up: NA |
NA | Intermediate‐risk population3 | NA | NA | NA | We do not know how VKA affects clinically relevant bleeding. | |
| NA | NA | ||||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; DVT: deep vein thrombosis; NA: not applicable; PE: pulmonary embolism; RR: risk ratio; VKA: vitamin K antagonists; VTE: venous thromboembolism | |||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | |||||||
1The assumed risk is calculated from the medium observed control group risk across the trials. 2Difference calculated as the absolute risk difference between the assumed risk and corresponding risk, expressed per 1000. 3Intermediate‐risk population refers to the median observed risk to experience symptomatic VTE in the trials contributing to the analyses (44 per 1000). Rates between 2% and 7% are considered intermediate risk (Khorana 2008). 4Downgraded (2 levels) because of imprecision, the risk for publication bias, as only 1 out of 4 trials reported on this outcome, and potential attrition bias, see Characteristics of included studies. 5Downgraded (2 levels) because of imprecision and potential attrition bias in 2 out of 4 trials. 6Downgraded (3 levels) because of imprecision (2 levels), the risk for publication bias, as only 1 out of 4 trials reported on this outcome, and potential attrition bias, see Characteristics of included studies.
Summary of findings 8. Vitamin K antagonists versus aspirin.
| Vitamin K antagonists compared with aspirin for primary thromboprophylaxis in ambulatory cancer patients receiving chemotherapy | |||||||
|
Patient or population: ambulatory cancer patients receiving chemotherapy Settings: outpatient clinics Intervention: VKA Comparison: aspirin | |||||||
| Outcomes | Relative effect (95% CI) | Illustrative comparative risks* (95% CI) | Difference2 (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | What it means | |
| Assumed risk1 | Corresponding risk | ||||||
| With aspirin | With VKA | ||||||
|
Symptomatic VTE: Follow‐up: median 2.1 years |
RR 1.50 (0.74 to 3.04) | Intermediate‐risk population3 | 27 per 1000 more events (14 fewer to 211 more) | 440 (1) | ⊕⊕⊕⊝ moderate4 | VKA probably increases the incidence of symptomatic VTE when compared to aspirin in multiple myeloma. | |
| 55 per 1000 | 82 per 1000 (40 to 166) | ||||||
|
Major bleeding Follow‐up: median 2.1 years |
RR 0.14 (0.01 to 2.75) | Intermediate‐risk population3 | 12 per 1000 fewer events (14 fewer to 24 more) | 440 (1) | ⊕⊕⊝⊝ low5 | VKA may reduce the incidence of major bleeding when compared to aspirin in multiple myeloma. | |
| 14 per 1000 | 2 per 1000 (0 to 38) | ||||||
|
Symptomatic PE Follow‐up: median 2.1 years |
RR 1.00 (0.25 to 3.95) | Intermediate‐risk population3 | 0 per 1000 fewer events (14 fewer to 54 more) | 440 (1) | ⊕⊕⊕⊝ moderate4 | VKA is probably as effective as aspirin in the prevention of symptomatic PE in multiple myeloma. | |
| 18 per 1000 | 18 per 1000 (5 to 72) | ||||||
|
Symptomatic DVT Follow‐up: median 2.1 years |
RR 1.75 (0.75 to 4.09) | Intermediate‐risk population3 | 27 per 1000 more events (9 fewer to 112 more) | 440 (1) | ⊕⊕⊕⊝ moderate4 | VKA probably increases the incidence of symptomatic DVT when compared to aspirin in multiple myeloma. | |
| 36 per 1000 | 64 per 1000 (27 to 149) | ||||||
|
1‐year mortality Follow‐up: NA |
NA6 | Intermediate‐risk population3 | NA | NA | NA | We do not know how VKA affects 1‐year mortality when compared to aspirin in multiple myeloma. | |
| NA | NA | ||||||
|
Clinically relevant bleeding Follow‐up: NA |
NA6 | Intermediate‐risk population3 | NA | NA | NA | We do not know how VKA affects clinically relevant bleeding when compared to aspirin in multiple myeloma. | |
| NA | NA | ||||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; DVT: deep vein thrombosis; NA: not applicable; PE: pulmonary embolism; RR: risk ratio; VKA: vitamin K antagonists; VTE: venous thromboembolism | |||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | |||||||
1The assumed risk is calculated from the observed control group risk in Palumbo 2011. 2Difference calculated as the absolute risk difference between the assumed risk and corresponding risk, expressed per 1000. 3Intermediate‐risk population refers to the median observed risk to experience symptomatic VTE in the trials contributing to the analyses (55 per 1000). Rates between 2% and 7% are considered intermediate risk (Khorana 2008). 4Downgraded (1 level) because of imprecision. Although attrition bias may have occurred, it is unlikely to have changed the results in a clinically relevant manner. 5Downgraded (2 levels) because of imprecision. Although attrition bias may have occurred, it is unlikely to have changed the results in a clinically relevant manner. 6No trials contributed to this outcome.
Summary of findings 9. Antithrombin versus placebo.
| Antithrombin compared with placebo for primary thromboprophylaxis in ambulatory cancer patients receiving chemotherapy | |||||||
|
Patient or population: ambulatory cancer patients receiving chemotherapy Settings: outpatient clinics Intervention: antithrombin Comparison: placebo | |||||||
| Outcomes | Relative effect (95% CI) | Illustrative comparative risks* (95% CI) | Difference2 (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | What it means | |
| Assumed risk1 | Corresponding risk | ||||||
| Without antithrombin | With antithrombin (any dosage) | ||||||
|
Symptomatic VTE: Follow‐up: NA |
NA3 | Population at unclear risk4 | NA | NA | NA | We do not know how antithrombin affects symptomatic VTE. | |
| NA | NA | ||||||
|
Major bleeding Follow‐up: median 4 months |
RR 0.78 (0.03 to 18.57) | Population at unclear risk4 | 4 per 1000 fewer events (16 fewer to 293 more) | 85 (1) | ⊕⊝⊝⊝ very low5 | We have very little confidence in the estimated effect of antithrombin on the incidence of major bleeding. | |
| 17 per 1000 | 13 per 1000 (1 to 310) | ||||||
|
Symptomatic PE Follow‐up: NA |
NA3 | Population at unclear risk4 | NA | NA | NA | We do not know how antithrombin affects symptomatic PE. | |
| NA | NA | ||||||
|
Symptomatic DVT Follow‐up: NA |
NA3 | Population at unclear risk4 | NA | NA | NA | We do not know how antithrombin affects symptomatic DVT. | |
| NA | NA | ||||||
|
1‐year mortality Follow‐up: NA |
NA3 | Population at unclear risk4 | NA | NA | NA | We do not know how antithrombin affects 1‐year mortality. | |
| NA | NA | ||||||
|
Clinically relevant bleeding Follow‐up: NA |
NA3 | Population at unclear risk4 | NA | NA | NA | We do not know how antithrombin affects clinically relevant bleeding. | |
| NA | NA | ||||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; DVT: deep vein thrombosis; NA: not applicable; PE: pulmonary embolism; RR: risk ratio; VTE: venous thromboembolism | |||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | |||||||
1The assumed risk is calculated from the observed control group risk in Mitchell 2003. 2Difference calculated as the absolute risk difference between the assumed risk and corresponding risk, expressed per 1000. 3No trials contributed to this outcome. 4The risk profile refers to the median observed risk to experience symptomatic VTEs. As Mitchell 2003 did not report this outcome, the risk profile remains unclear. 5Downgraded (3 levels) because of imprecision (2 levels) and attrition bias, see Characteristics of included studies.
Summary of findings 10. Apixaban versus placebo.
| Apixaban compared with placebo for primary thromboprophylaxis in ambulatory cancer patients receiving chemotherapy | |||||||
|
Patient or population: ambulatory cancer patients receiving chemotherapy Settings: outpatient clinics Intervention: apixaban Comparison: placebo | |||||||
| Outcomes | Relative effect (95% CI) | Illustrative comparative risks* (95% CI) | Difference2 (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | What it means | |
| Assumed risk1 | Corresponding risk | ||||||
| Without apixaban | With apixaban (any dosage) | ||||||
|
Symptomatic VTE: Follow‐up: median 3 months |
RR 0.08 (0.01 to 0.67) | High‐risk population3 | 66 per 1000 fewer events (24 to 71 fewer) | 122 (1) | ⊕⊕⊕⊝ moderate4 | Apixaban probably decreases the incidence of symptomatic VTE across different cancer types. | |
| 71 per 1000 | 6 per 1000 (1 to 48) | ||||||
|
Major bleeding Follow‐up: median 3 months |
RR 0.62 (0.06 to 6.63) | High‐risk population3 | 6 per 1000 fewer events (16 fewer to 96 more) | 122 (1) | ⊕⊕⊕⊝ low5 | We are unsure whether apixaban increases the incidence of major bleeding across different cancer types. | |
| 17 per 1000 | 11 (1 to 113) | ||||||
|
Symptomatic PE Follow‐up: median 3 months |
RR 0.11 (0.00 to 2.54) | High‐risk population3 | 12 per 1000 fewer events (14 fewer to 22 more) | 122 (1) | ⊕⊕⊝⊝ low5 | We are unsure whether apixaban decreases the incidence of symptomatic PE across different cancer types. | |
| 14 per 1000 | 2 per 1000 (0 to 36) |
||||||
|
Symptomatic DVT Follow‐up: median 3 months |
RR 0.08 (0.01 to 0.67) | High‐risk population3 | 27 per 1000 fewer events (10 to 29 fewer) | 122 (1) | ⊕⊕⊕⊝ moderate4 | Apixaban probably decreases the incidence of symptomatic DVT across different cancer types. | |
| 29 per 1000 | 2 per 1000 (0 to 19) | ||||||
|
1‐year mortality Follow‐up: NA |
NA6 | High‐risk population3 | NA | 0 (0) | NA | We do not know how apixaban affects all‐cause mortality. | |
| NA | NA | ||||||
|
Clinically relevant bleeding Follow‐up: median 3 months |
RR 1.87 (0.23 to 14.91) | High‐risk population3 | 30 per 1000 more events (27 fewer to 480 more) | 122 (1) | ⊕⊕⊝⊝ low7 | We are unsure how much apixaban increases the incidence of clinically relevant bleeding across different cancer types. | |
| 34 per 1000 | 64 per 1000 (8 to 514) | ||||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; DVT: deep vein thrombosis; NA: not applicable; PE: pulmonary embolism; RR: risk ratio; VTE: venous thromboembolism | |||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | |||||||
1The assumed risk is calculated from the medium observed control group risk in the study, see Table 2. 2Difference calculated as the absolute risk difference between the assumed risk and corresponding risk, expressed per 1000. 3High‐risk population refers to the median observed risk to experience symptomatic VTE in the trials contributing to the analyses (71 per 1000). Rates from 7% and higher are considered high risk (Khorana 2008). 4Downgraded (1 level) because of attrition bias, see Characteristics of included studies. 5Downgraded (2 levels) because of attrition bias, see Characteristics of included studies, and imprecision. 6No trials contributed to this outcome. 7Downgraded (2 levels) because of indirectness, as we combined the different dosages to increase the statistical power we introduced indirectness, and the risk of attrition bias, see Characteristics of included studies.
Anticoagulants versus control
uLMWH versus placebo
Primary outcomes
In one large trial of 3212 participants (Agnelli 2012), semuloparin was associated with a significant reduction in symptomatic VTE (RR 0.36, 95% CI 0.22 to 0.60), corresponding to a NNTB of 46 (95% CI 31 to 87). There were 19/1589 major bleeding events in the semuloparin group versus 18/1583 in the placebo group (RR 1.05, 95% CI 0.55 to 2.00). The quality of the evidence was high for symptomatic VTE and low for major bleeding (see Table 1).
In participants with lung and pancreatic cancers, semuloparin reduced symptomatic VTE by 64% (9/591 versus 25/589; RR 0.36, 95% CI 0.17 to 0.76) and by 78% (3/126 versus 14/128; RR 0.22, 95% CI 0.06 to 0.74), respectively. Rates of major bleeding were not reported separately for these types of cancer.
Secondary outcomes
The risk of symptomatic PE was reduced by 52% (RR 0.48, 95% CI 0.22 to 1.01), and symptomatic DVT (RR 0.32, 95% CI 0.16 to 0.63) and overall VTE (RR 0.36, 95% CI 0.22 to 0.60) were reduced by about two‐thirds with semuloparin. We found moderate‐quality evidence for symptomatic PE and high‐quality evidence for DVT (see Table 1). Fatal PE occurred in 0.4% of participants on semuloparin and 0.6% of participants on placebo. Clinically relevant bleeding was reported in 2.8% and 2.0%, respectively (RR 1.40, 95% CI 0.90 to 2.19). We judged the quality of the evidence for clinically relevant bleeding as moderate. Semuloparin did not influence incidental VTE (RR 0.14, 95% CI 0.01 to 2.76) or one‐year mortality (RR 1.02, 95% CI 0.96 to 1.08; moderate‐quality evidence). The incidence of serious adverse events or thrombocytopenia was similar in the semuloparin and placebo groups (26% versus 25% and 7.1% versus 7.6%, respectively), with no cases of heparin‐induced thrombocytopenia (HIT).
LMWH versus placebo or no thromboprophylaxis
Primary outcomes
The clinical trials evaluating LMWH against placebo or no thromboprophylaxis varied in the duration and type of LMWH, including 8 weeks to 48 months of subcutaneous dalteparin, enoxaparin, certoparin, nadroparin, or bemiparin. The dose of LMWH was prophylactic in the majority of the studies, and intermediate, in Pelzer 2015, or therapeutic, in Maraveyas 2012, in one study each. In two studies initial therapeutic LMWH was followed by intermediate doses (Klerk 2005; van Doormaal 2011).
Based on pooled estimates from nine RCTs, LMWH, when compared with no thromboprophylaxis, was associated with a significant reduction in symptomatic VTE (RR 0.54, 95% CI 0.38 to 0.75; 3284 participants) (Figure 3) in the absence of heterogeneity (Tau2 = 0.00). This corresponded to a NNTB of 30 (95% CI 23 to 56), assuming a background risk of 71 symptomatic VTE events per 1000 patients (Table 2) (Khorana 2008). Funnel plot exploration did not show any evidence of biases associated with small studies (Figure 4). Stratified analyses did not show any effect of the type of LMWH, type of cancer, dosage, or design characteristics on the relative risk of symptomatic VTE (Table 23). Similarly, we found no evidence for a linear association between treatment duration and the risk of symptomatic VTE using meta‐regression analysis (P = 0.514).
3.
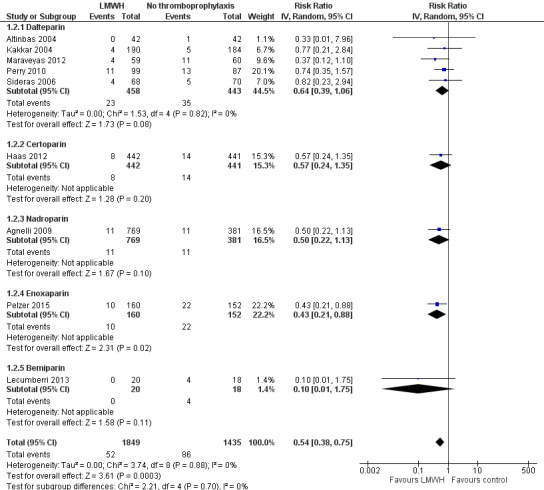
Forest plot of comparison: 1 Anticoagulants versus control: symptomatic VTE, outcome: 1.2 Symptomatic VTE: LMWH versus no thromboprophylaxis.
4.
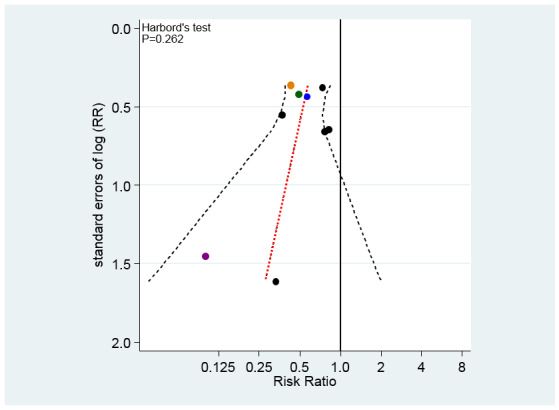
Funnel plot of comparison: 1 Anticoagulants versus control: symptomatic VTE, outcome: 1.2 Symptomatic VTE: LMWH versus no thromboprophylaxis.
1. Results of stratified analyses on symptomatic venous thromboembolism.
| Variable | N of trials | N of participants (LMWH) | N of participants (control) | RR (95% CI) |
Heterogeneity I2/Tau2 |
P for interaction |
| All trials | 9 | 1849 | 1435 | 0.54 (0.38 to 0.75) | 0.0/0.00 | |
| Type of LMWH | 0.710 | |||||
| Dalteparin | 5 | 458 | 443 | 0.64 (0.39 to 1.06) | 0.0/0.00 | |
| Certoparin | 1 | 442 | 441 | 0.57 (0.24 to 1.35) | NA | |
| Nadroparin | 1 | 769 | 381 | 0.50 (0.22 to 1.13) | NA | |
| Enoxaparin | 1 | 160 | 152 | 0.43 (0.21 to 0.88) | NA | |
| Bemiparin | 1 | 20 | 18 | 0.10 (0.01 to 1.75) | NA | |
| Type of dosage | 0.322 | |||||
| Prophylactic | 7 | 1630 | 1223 | 0.61 (0.41 to 0.92) | 0.0/0.00 | |
| Higher than prophylactic | 2 | 219 | 212 | 0.41 (0.23 to 0.75) | 0.0/0.00 | |
| Type of cancer | 0.610 | |||||
| Mixed | 3 | 828 | 555 | 0.70 (0.33 to 1.51) | 0.0/0.00 | |
| Lung | 4 | 529 | 404 | 0.40 (0.20 to 0.80) | 0.0/0.00 | |
| Pancreatic | 2 | 219 | 212 | 0.41 (0.23 to 0.75) | 0.0/0.00 | |
| Glioma | 1 | 99 | 87 | 0.74 (0.35 to 1.57) | NA | |
| Breast cancer | 1 | 174 | 177 | 0.76 (0.17 to 3.36) | NA | |
| Allocation concealment | 0.960 | |||||
| Adequate | 7 | 1365 | 952 | 0.54 (0.37 to 0.78) | 0.0/0.00 | |
| Inadequate or unclear | 2 | 484 | 483 | 0.55 (0.24 to 1.26) | 0.0/0.00 | |
| Blinding of participants | 0.353 | |||||
| Double‐blind | 4 | 1500 | 1093 | 0.62 (0.40 to 0.96) | 0.0/0.00 | |
| Inadequate or unclear blinding | 5 | 349 | 342 | 0.44 (0.26 to 0.74) | 0.0/0.00 | |
| Intention‐to‐treat analysis | 0.627 | |||||
| Yes | 4 | 338 | 317 | 0.50 (0.31 to 0.79) | 0.0/0.00 | |
| No or unclear | 5 | 1511 | 1118 | 0.59 (0.36 to 0.97) | 0.0/0.00 | |
| Selective outcome reporting | 0.857 | |||||
| Adequate | 7 | 1590 | 1196 | 0.52 (0.34 to 0.82) | 0.0/0.00 | |
| Incomplete or unclear | 2 | 259 | 239 | 0.56 (0.33 to 0.95) | 5.6/0.01 | |
CI: confidence interval LMWH: low molecular weight heparin NA: not applicable, only 1 trial contributing to this stratum RR: risk ratio
The difference in major bleeding was not statistically significant (RR 1.44, 95% CI 0.98 to 2.11; 6356 participants; 13 studies) (Figure 5), in the absence of heterogeneity (Tau2 = 0.00). Visual examination of the funnel plot and Harbord–Egger's test (P = 0.881) did not show asymmetry (Figure 6), so that we did not detect publication bias or other biases related to small study size. The results of the stratified analyses, which did not show any effect of the type of LMWH, dosage, type of cancer, definition of major bleeding, trial size, or design characteristics on the relative risk of major bleeding, are presented in Table 24. Again, we found no evidence for a linear association between treatment duration and the risk of major bleeding using meta‐regression analysis (P = 0.751).
5.
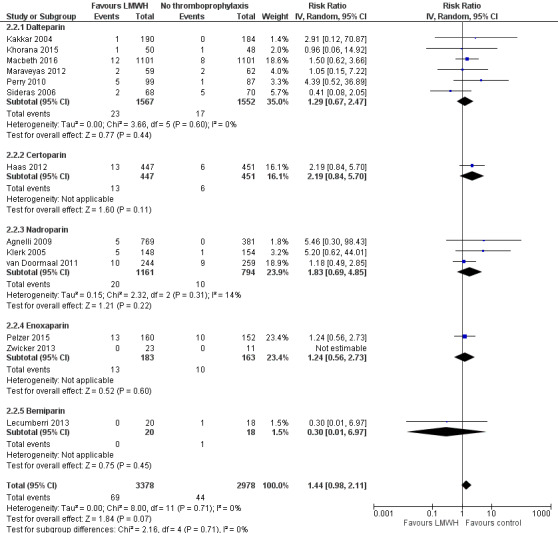
Forest plot of comparison: 2 Anticoagulants versus control: major bleeding, outcome: 2.2 Major bleeding: LMWH versus no thromboprophylaxis.
6.
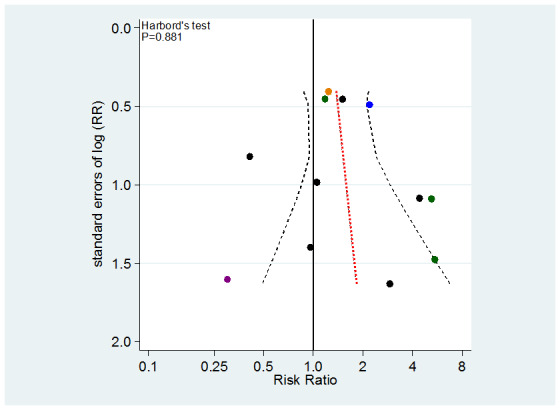
Funnel plot of comparison: 2 Anticoagulants versus control: major bleeding, outcome: 2.2 Major bleeding: LMWH versus no thromboprophylaxis.
2. Results of stratified analyses on major bleeding.
| Variable | N of trials | N of participants (LMWH) | N of participants (control) | RR (95% CI) |
Heterogeneity I2/Tau2 |
P for interaction |
| All trials | 12* | 3378 | 2978 | 1.44 (0.98 to 2.11) | 0.0/0.00 | |
| Type of LMWH | 0.736 | |||||
| Dalteparin | 6 | 1567 | 1552 | 1.29 (0.67 to 2.47) | 0.0/0.00 | |
| Certoparin | 1 | 447 | 451 | 2.19 (0.84 to 5.70) | NA | |
| Nadroparin | 3 | 1161 | 794 | 1.83 (0.69 to 4.85) | 13.8/0.15 | |
| Enoxaparin | 2 | 183 | 163 | 1.24 (0.56 to 2.73) | NA | |
| Bemiparin | 1 | 20 | 18 | 0.30 (0.01 to 6.97) | NA | |
| Type of dosage | 0.669 | |||||
| Prophylactic | 8 | 2744 | 2340 | 1.56 (0.91 to 2.69) | 0.0/0.00 | |
| Higher than prophylactic | 4 | 611 | 627 | 1.32 (0.76 to 2.27) | 0.0/0.00 | |
| Type of cancer | 0.641 | |||||
| Mixed | 6 | 1293 | 1027 | 1.24 (0.63 to 2.42) | 0.0/0.00 | |
| Lung | 4 | 1593 | 1472 | 1.49 (0.79 to 2.80) | 0.0/0.00 | |
| Pancreatic | 2 | 219 | 214 | 1.21 (0.58 to 2.51) | 0.0/0.00 | |
| Glioma | 1 | 99 | 87 | 4.39 (0.52 to 36.89) | NA | |
| Breast cancer | 1 | 174 | 178 | 7.16 (0.37 to 137.60) | NA | |
| Definition of major bleeding | 0.235 | |||||
| Standard** | 9 | 3077 | 2697 | 1.70 (1.07 to 2.70) | 0.0/0.00 | |
| Alternative or unclear | 3 | 278 | 270 | 0.99 (0.50 to 1.98) | 0.0/0.00 | |
| Trial size | 0.917 | |||||
| Large | 1 | 1101 | 1101 | 1.50 (0.62 to 3.66) | NA | |
| Small | 11 | 2254 | 1866 | 1.42 (0.93 to 2.18) | 0.0/0.00 | |
| Allocation concealment | 0.447 | |||||
| Adequate | 10 | 2858 | 2468 | 1.33 (0.87 to 2.04) | 0.0/0.00 | |
| Inadequate or unclear | 2 | 497 | 499 | 2.00 (0.81 to 4.94) | 0.0/0.00 | |
| Blinding of participants | 0.175 | |||||
| Double‐blind | 6 | 1897 | 1516 | 1.97 (1.11 to 3.51) | 0.0/0.00 | |
| Inadequate or unclear blinding | 6 | 1458 | 1451 | 1.11 (0.66 to 1.86) | 0.0/0.00 | |
| Intention‐to‐treat analysis | 0.941 | |||||
| Yes | 7 | 1637 | 1622 | 1.45 (0.87 to 2.43) | 0.0/0.00 | |
| No or unclear | 5 | 1718 | 1345 | 1.41 (0.76 to 2.61) | 6.0/0.03 | |
| Selective outcome reporting | 0.989 | |||||
| Adequate | 10 | 3096 | 2728 | 1.43 (0.91 to 2.25) | 0.0/0.00 | |
| Incomplete or unclear | 2 | 259 | 239 | 1.56 (0.59 to 4.11) | 16.7/0.13 | |
CI: confidence interval LMWH: low molecular weight heparin NA: not applicable, only 1 trial contributing to this stratum RR: risk ratio
*Zwicker 2013, who reported 0 events in both the LMWH and control group, was excluded from all analyses. **The definition of major bleeding was considered 'standard' when it matched the definition of the International Society of Thrombosis and Haemostasis (Schulman 2005).
The quality of the evidence was high for symptomatic VTE and low for major bleeding (see Table 2).
Secondary outcomes
There was a significant effect on symptomatic PE (RR 0.59, 95% CI 0.40 to 0.86; 5226 participants; 7 studies; Tau2 = 0.00). This corresponds to a NNTB of 174 (95% CI 119 to 510). Fatal PE was reported by Macbeth 2016 in 0.3% of participants receiving LMWH and 0.5% of those receiving no thromboprophylaxis, whereas Maraveyas 2012 reported 8% fatal VTEs in the group receiving no thromboprophylaxis versus none in the dalteparin group. In four studies no fatal VTEs were reported in any of the study groups (Agnelli 2009; Elit 2012; Lecumberri 2013; Pelzer 2015). We judged the quality of the evidence for symptomatic PE as low (see Table 2). The risk of symptomatic DVT was reduced by 51% (RR 0.49, 95% CI 0.35 to 0.67; 5310 participants; 8 studies; Tau2 = 0.00), corresponding to a NNTB of 68 (95% CI 53 to 105). We found high‐quality evidence for symptomatic DVT. Overall, VTE was reduced by 41% (RR 0.59, 95% CI 0.48 to 0.73; 5366 participants; 9 studies; Tau2 = 0.00), corresponding to a NNTB of 25 (95% CI 20 to 38). There was a significant increase in clinically relevant bleeding with LMWH (RR 3.40, 95% CI 1.20 to 9.63; 3105 participants; 4 studies; Tau2 = 0.73; moderate‐quality evidence). There was no statistically significant benefit or harm for incidental VTE, minor bleeding, one‐year mortality, symptomatic arterial thromboembolism, superficial venous thrombosis, or serious adverse events (Data and analyses). Only two studies evaluated quality of life through questionnaires (Macbeth 2016; Sideras 2006). Sideras 2006 found similar results in participants randomised to LMWH or no thromboprophylaxis, both at baseline and during the study period (Sideras 2006). Forty‐four per cent and 51% of the participants, respectively, reported decreased quality of life during the treatment period by a clinically meaningful amount of 10 points on a 100‐point scale. Macbeth 2016 found no difference between LMWH and no thromboprophylaxis with respect to quality‐adjusted life years gained in the first year and no difference in overall quality of life at 6 months (P = 0.94) or 12 months (P = 0.89). Three studies reported no cases of HIT with LMWH use (Haas 2012; Klerk 2005; Pelzer 2015). Haas 2012 reported objectively verified skeletal events (including all fractures, spinal cord compressions, and requirements for surgery to treat fractures or for bone irradiation) in 16/442 and 19/441 of participants in the LMWH and placebo groups, respectively.
Macbeth 2016 reported on compliance with LMWH. Of the 977 (89%) participants in whom compliance was evaluated, 180 (18.4%) were considered as fully compliant, whereas 431 (39%) received half of the planned syringes or less.
Five studies reported on symptomatic VTE and major bleeding in participants with non‐small cell lung cancer (Haas 2012), small cell lung cancer (Altinbas 2004; Lecumberri 2013), or both (Agnelli 2009; Macbeth 2016). Pooled analysis of these trials showed a significant 60% reduction in symptomatic VTE (RR 0.40, 95% CI 0.20 to 0.80), whereas there was no statistically significant higher risk of major bleeding with LMWH compared with the control treatment (RR 1.49, 95% CI 0.79 to 2.80) and no evidence of statistical heterogeneity (Tau2 = 0.00) (Table 23; Table 24).
Two studies reported on symptomatic VTE and major bleeding in participants with advanced pancreatic cancer (Maraveyas 2012; Pelzer 2015). Pooled analysis of these trials showed a significant 59% reduction in symptomatic VTE (RR 0.41, 95% CI 0.23 to 0.75) and no increase in major bleeding (RR 1.21, 95% CI 0.58 to 2.51) with LMWH and no evidence of statistical heterogeneity (Tau2 = 0.00) (Table 23; Table 24). Vadhan‐Raj 2013 also selectively included participants with advanced pancreatic cancer and reported 2 DVTs in the dalteparin arm and 8 VTEs (2 PE and 6 DVT) in 37 participants receiving no thromboprophylaxis. The abstract does not report whether these events were symptomatic, incidental, or both. There were no clinically significant bleeding events with dalteparin, although the definition of bleeding is not provided and it is not reported if any bleeding occurred in participants in the control group.
LMWH versus active control
Elit 2012 compared three doses of dalteparin against each other. There were no symptomatic VTEs or major bleeding events during dalteparin administration. Two participants developed symptomatic VTE, and one was diagnosed with incidental PE after dalteparin discontinuation. The quality of the evidence was low for symptomatic VTE and could not be evaluated for major bleeding as the RR was not estimable due to zero count in all trial arms (see Table 3). Three participants had minor bleeding in the highest‐dose group (150 IU/kg). There were no cases of HIT. Compliance with injections was more than 80% in all three dose groups.
In two studies of multiple myeloma patients receiving thalidomide‐ and lenalidomide‐based regimens, LMWH was compared against an active control, which in both studies was aspirin (Larocca 2012; Palumbo 2011), and in one of the studies was VKA (warfarin) (Palumbo 2011). When compared with aspirin, pooled analysis showed a not statistically significant 49% reduction in symptomatic VTE (RR 0.51, 95% CI 0.22 to 1.17; 781 participants; 2 studies). There were 3/396 major bleeding events with aspirin and none with LMWH (0/385). The quality of the evidence was moderate for symptomatic VTE and low for major bleeding (see Table 4). The incidence of symptomatic PE was reduced by 87% (RR 0.13, 95% CI 0.02 to 1.03; 781 participants; 2 studies; moderate‐quality evidence), but the CIs were wide and the estimate was not significant. Likewise, there were no significant differences between LMWH and aspirin regarding the incidence of symptomatic DVT (low‐quality evidence), minor bleeding, and symptomatic arterial thromboembolism.
In the study of Palumbo 2011, LMWH was associated with a 67% reduction in symptomatic VTE relative to warfarin (RR 0.33, 95% CI 0.14 to 0.83; 439 participants; high‐quality evidence), with no major bleeding events reported in either group. The pooled estimates did not conclusively rule out an increase or reduction in symptomatic PE (RR 0.11, 95% CI 0.01 to 2.06; low‐quality evidence) and symptomatic DVT (RR 0.43, 95% CI 0.17 to 1.10; moderate‐quality evidence). There were no differences between LMWH and warfarin regarding the incidence of minor bleeding and symptomatic arterial thromboembolism.
UFH versus no thromboprophylaxis
One study with 277 participants evaluated UFH against no thromboprophylaxis (Lebeau 1994), and did not report on symptomatic or incidental VTE or on major bleeding. Clinically relevant bleeding occurred in 2/138 versus 1/139 of participants, respectively (RR 2.01, 95% CI 0.18 to 21.96; P = 0.57; low‐quality evidence). The summary estimate did not conclusively rule out an increase or reduction in 1‐year mortality (RR 0.86, 95% CI 0.72 to 1.03; moderate‐quality evidence). There were no cases of HIT.
VKA versus placebo or no thromboprophylaxis
Levine 1994 (311 participants) reported an 85% reduction of symptomatic VTE (RR 0.15, 95% CI 0.02 to 1.20) with warfarin relative to placebo, albeit this finding was not statistically significant. There was no significant effect on major bleeding (RR 0.52, 95% CI 0.05 to 5.71), symptomatic PE (RR 1.05, 95% CI 0.07 to 16.58), symptomatic DVT (RR 0.08, 95% CI 0.00 to 1.42), or minor bleeding (RR 2.44, 95% CI 0.64 to 9.27). No symptomatic arterial thromboembolic events were observed in either group.
Three studies reported major bleeding events (Chahinian 1989; Maurer 1997; Zacharski 1981), but provided no data on the occurrence of symptomatic or incidental VTE. Pooled analysis of all studies evaluating VKA versus placebo or no thromboprophylaxis showed a non‐statistically significant four‐fold increase in major bleeding (RR 3.82, 95% CI 0.97 to 15.04) with evidence of a high degree of heterogeneity (Tau2 = 0.71).
The quality of the evidence was low for symptomatic VTE, major bleeding, and symptomatic DVT and very low for symptomatic PE (see Table 7).
VKA versus active control
Palumbo 2011 reported a non‐statistically significant difference between VKA (warfarin) and aspirin with regard to symptomatic VTE (RR 1.50, 95% CI 0.74 to 3.04; 440 participants; moderate‐quality evidence). There were 3 (3/220) major bleeding events in the aspirin group and none (0/220) in the warfarin group (RR 0.14, 95% CI 0.01 to 2.75; P = 0.20; 440 participants; low‐quality evidence). Evidence did not conclusively show that VKA increased or reduced the incidence of symptomatic PE or symptomatic DVT (moderate‐quality evidence) (Analysis 1.7; Analysis 2.7). There were no differences for the other secondary outcomes minor bleeding and symptomatic arterial thromboembolism (Palumbo 2011).
1.7. Analysis.
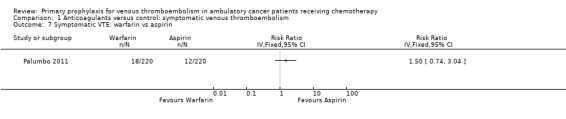
Comparison 1 Anticoagulants versus control: symptomatic venous thromboembolism, Outcome 7 Symptomatic VTE: warfarin vs aspirin.
2.7. Analysis.
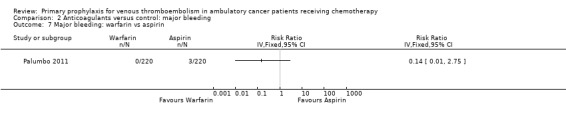
Comparison 2 Anticoagulants versus control: major bleeding, Outcome 7 Major bleeding: warfarin vs aspirin.
We refer to the previous section 'LMWH versus active control' for the description of the comparison of VKA versus LMWH.
Antithrombin versus no thromboprophylaxis
One study that recruited 85 paediatric patients assessed antithrombin (Mitchell 2003). The effects of antithrombin on major bleeding (RR 0.78, 95% CI 0.03 to 18.57; very low‐quality evidence) and overall VTE (RR 0.84, 95% CI 0.41 to 1.73) were not statistically significant. The remaining outcomes were not reported.
Factor Xa inhibitors versus placebo
In a phase II dose‐finding study, Levine 2012 observed 0/32, 0/29, 2/32, and 1/29 major bleeding events in the groups receiving apixaban 5 mg, 10 mg, 20 mg, and placebo, respectively, for an overall rate of major bleeding in the 93 apixaban participants of 2.1% versus 3.4% in the placebo group. There were 4 (13.8%) symptomatic VTEs in the placebo group, while one participant (1.1%) in the 20 mg apixaban group experienced a DVT of the arm. We judged the quality of the evidence as moderate for symptomatic VTE and low for major bleeding (see Table 10). Two participants in the 5 mg and one in the 20 mg apixaban groups (3.1%) experienced an adverse event, graded as 3 or higher, which was possibly or probably related to treatment, compared with none in the placebo group.
Evidence did not conclusively show that apixaban increased or reduced the incidence of symptomatic PE (RR 0.11, 95% CI 0.00 to 2.54; low‐quality evidence), but apixaban reduced the incidence of symptomatic DVT (RR 0.08, 95% CI 0.01 to 0.67; moderate‐quality evidence).
There were six cases of clinically relevant bleeding among the 93 participants on apixaban versus 1 in 29 placebo recipients (RR 1.87, 95% CI 0.23 to 14.91; low‐quality evidence).
Discussion
Summary of main results
When used as primary thromboprophylaxis in ambulatory cancer patients receiving chemotherapy, both the uLMWH semuloparin and LMWH reduce the incidence of symptomatic VTE by about half. Data on the risk of major bleeding were inconclusive; the confidence intervals around the risk estimate for LMWH were wide but close to statistical significance and the upper bound suggested that heparin treatment could be associated with as much as a doubling of the major bleeding risk. Both semuloparin and LMWH reduced the incidence of symptomatic PE but had no significant effects on one‐year mortality. LMWH was associated with a significantly three‐fold higher risk of clinically relevant bleeding compared to no thromboprophylaxis. Some types of cancer, such as pancreatic or lung cancer, obtained significant benefits from LMWH prophylaxis in terms of symptomatic VTE reduction with no apparent increases in major bleeding.
One study in myeloma patients receiving thalidomide‐ or lenalidomide‐based regimens showed that LMWH was associated with a 67% lower risk of symptomatic VTE compared with warfarin, but this study was underpowered to show differences for major bleeding. The lack of a control group receiving placebo or no thromboprophylaxis prevents firm judgements about the efficacy and safety of LMWH or warfarin in myeloma patients receiving thalidomide‐ or lenalidomide‐based regimens. The reduction of symptomatic VTE with warfarin in non‐myeloma patients was not statistically significant and was potentially associated with an increase in major bleeding. Apixaban was evaluated only in a dose‐finding study and antithrombin in a relatively small trial involving paediatric patients. No RCT evaluated fondaparinux, dabigatran, rivaroxaban, edoxaban, and mechanical interventions.
Quality of the evidence
The methodological quality of the individual studies ranged from low to high (Figure 2). Analytical exploration of the effects of design flaws was feasible for the comparison of LMWH versus no thromboprophylaxis only. We found no evidence of design‐related biases. An inspection of the funnel plot and formal analysis of asymmetry did not indicate asymmetry for the primary efficacy outcome (Figure 4), suggesting the absence of publication bias or other biases related to small study size (Figure 6).
Across comparisons, the quality of the evidence for symptomatic VTE ranged from low to high. Semuloparin was evaluated in a single study, although this study was relatively large and of high methodological quality (Agnelli 2012). While it is very unlikely that new evidence will change our confidence in the estimate of the effects of LMWH or semuloparin compared to placebo/no thromboprophylaxis or of LMWH compared to VKA, we are less certain about the estimates of the other comparisons. The quality of the evidence for major bleeding was at best low, indicating that further research is very likely to have an important effect on our confidence in the estimate of effect and is likely to change the estimate (Guyatt 2008). The largest concern overall was imprecision due to the small study size of the majority of the trials. We could not judge the quality of the evidence for several outcomes across comparisons due to incomplete reporting or the absence of events in both trial arms.
See Table 1; Table 2; Table 3; Table 4; Table 5; Table 6; Table 7; Table 8; Table 9; Table 10.
Potential biases in the review process
Our systematic approach to searching, study selection, and data extraction followed that described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). It is unlikely that we have missed relevant trials, but frequent updates of this review are warranted given that we identified several new trials since the previous version of this review, which covered published trials up to 2014 (Di Nisio 2012). We minimised data extraction errors by using two independent review authors (MDN, MC). Judgements on the grade of evidence were discussed with a third review author (AR). We acknowledge that quality assessment leaves room for different interpretations, especially where the quality of reporting is poor. We applied strict rules regarding the risk of attrition bias, requiring that all randomised participants were analysed according to the intention‐to‐treat principle. We chose this rather strict approach, as the incidence of symptomatic VTE varies considerably between trials and may be rather low, so that even a small proportion of participants not analysed may impact on the study estimates if the fraction not analysed is associated with the outcome. Other reviews have also applied this approach (Juni 2001; Rutjes 2009; Rutjes 2012). Following Cochrane guidance, we included quotes and the arguments on which we based our judgements, allowing the reader to reach different conclusions. Our systematic approach and the consistency of the results (lack of significant heterogeneity) increase confidence in the internal validity of our findings.
One limitation in the interpretation of this review is the 'no difference' findings. The lack of difference may be related to the small number of RCTs and small number of studied participants or events, or both, as well as the absence of a true effect. In this regard, the non‐significant association between semuloparin and LMWH and major bleeding events could indeed be the result of the relatively low number of events observed. For example, in the trial by Agnelli 2012, which evaluated semuloparin, there were only a total of 37 major bleeds; thus while the point estimate is 1.05 (seemingly reassuring), the upper value of the 95% confidence interval is 2.00, which means that there could have been at most a doubling of the major bleeding risk. With regard to LMWH, there were 5 new trials with 2491 additional participants, which resulted in a higher point estimate compared to the previous version of this review (1.44 versus 1.30), but the confidence interval remained wide.
Another limitation related to the small number of RCTs, poor reporting, or both, was our inability to conduct all subgroup analyses for the primary efficacy outcome. We had planned to explore the impact of the stage of cancer (metastatic versus non‐metastatic) and differences in the use of co‐interventions in the trial groups on the treatment effect. We performed subgroup analysis by type of cancer for the lung and pancreatic cancers, albeit the data for the pooled analysis were derived from only five and two studies, respectively. The lack of reporting, as well as the heterogeneity of the cancers treated, prevented us from assessing the importance of background chemotherapy on the response to thromboprophylaxis. Finally, the lack of evidence precluded any inference on the use of mechanical prophylaxis.
Agreements and disagreements with other studies or reviews
The evidence on the use of thromboprophylaxis in ambulatory cancer patients receiving chemotherapy was summarised by Rana 2009 and Lyman 2013, and more recently in the updated guidelines of the American Society of Clinical Oncology (Lyman 2015). The current systematic review adds substantial evidence to the narrative description provided by Rana 2009, as our systematic search identified 19 additional studies (Agnelli 2012; Altinbas 2004; Elit 2012; Kakkar 2004; Khorana 2015; Klerk 2005; Larocca 2012; Lebeau 1994; Lecumberri 2013; Levine 2012; Macbeth 2016; Maraveyas 2012; Mitchell 2003; Palumbo 2011; Pelzer 2015; Sideras 2006; Vadhan‐Raj 2013; van Doormaal 2011; Zwicker 2013). While most of the studies evaluated LMWH, additional data were available for other anticoagulants such as the uLMWH semuloparin, the direct orally administered factor Xa inhibitor apixaban, unfractionated heparin (UFH), and antithrombin. Eight of these studies evaluated the effects of prophylactic doses of LMWH on survival as the primary outcome, while reporting VTE events as secondary outcomes (Altinbas 2004; Elit 2012; Kakkar 2004; Klerk 2005; Lecumberri 2013; Macbeth 2016; Sideras 2006; van Doormaal 2011). Although the focus was not on VTE, and some cases may have been underdiagnosed, the overall incidence of symptomatic VTE was comparable with the other studies included in the review. In the recent update of Lyman 2013, nine RCTs and three systematic reviews, including the previous version of the current Cochrane review, were considered (Di Nisio 2012). In addition to performing a more comprehensive search of the literature, another advantage of the current review over the other reviews is that we provided pooled estimates with 95% confidence intervals for both efficacy and safety outcomes, allowing a better estimation of the risks and benefits of thromboprophylaxis in this setting. Lastly, the use of a larger dataset allowed us to stratify multiple outcomes by type of treatment. Despite these differences, our conclusions are in line with those of Rana 2009, Lyman 2013, and Lyman 2015 and do not support the widespread use of primary thromboprophylaxis in ambulatory cancer patients. Although both LMWH and semuloparin reduced the incidence of symptomatic VTE, we cannot exclude a significant increase in major bleeding. The confidence intervals around the risk of major bleeding with LMWH did not exclude a risk of major bleeding up to two‐fold higher compared to no thromboprophylaxis. In a previous meta‐analysis of six studies comparing LMWH versus no thromboprophylaxis, Kuderer 2009 obtained similar estimates of effects for symptomatic VTE and major bleeding. This work was published only as an abstract with limited data on the methods and type of analysis performed, which hampers any comparison with the current meta‐analysis. Other narrative reviews recently summarised the evidence on the use of thromboprophylaxis for VTE in ambulatory cancer patients (Aikens 2013; Maxwell 2012). These reviews lacked a systematic search of the literature and, as for Rana 2009 and Lyman 2013, no meta‐analysis or evaluation of study quality items and assessment of risk of bias were performed.
The conclusions of our review differ somewhat from the most recent guidelines of the American College of Chest Physicians (Kahn 2012), which suggest primary thromboprophylaxis with LMWH or UFH in ambulatory patients with solid tumours who have additional risk factors for VTE (that is previous venous thrombosis, immobilisation, angiogenesis inhibitors, thalidomide and lenalidomide) and a low risk of bleeding. Specific risk factors and their combination in risk scores may help to identify subgroups with a higher risk of VTE that may benefit substantially from prophylaxis (Ay 2010; Khorana 2008; Khorana 2009; Khorana 2009a).
In an earlier post hoc analysis of the SAVE‐ONCO study, rates of VTE in the placebo arm were 5.4% in the high‐risk population and down to 1.3% in the lower‐risk population (George 2011). The greatest reduction in VTE with thromboprophylaxis was observed among moderate‐ to high‐risk participants, with no apparent increased incidence of clinically relevant bleeding across the various levels of VTE risk. Similarly, in the post hoc analysis of the Prophylaxis of Thromboembolism During Chemotherapy (PROTECHT) study, rates of VTE were 11% in the high‐risk group down to 3% in the lower‐risk group, and the stratification of cancer patients reduced the NNTB from 50 in the full study population to 15 in the higher‐risk group (Verso 2012). Finally, preliminary findings from the pilot study of Zwicker 2013 suggest that microparticles may be a marker to stratify the risk and tailor the use of thromboprophylaxis, although it may be hard to implement these measurements for VTE risk stratification in routine practice.
Randomised controlled trials on subgroups of cancer patients considered at higher risk of VTE are under way (e.g. NCT02048865; NCT02555878), and this update included recent data from the Study of Dalteparin Prophylaxis in High‐Risk Ambulatory Cancer Patients (PHACS), which randomised participants at increased risk based on a Khorana score above 3 to LMWH prophylaxis or no thromboprophylaxis (Khorana 2015). Although findings from this study are encouraging, it should be noted that the study was terminated prematurely due to poor accrual, and was therefore underpowered.
Authors' conclusions
Implications for practice.
When deciding whether to use primary antithrombotic prophylaxis in ambulatory cancer patients receiving chemotherapy, clinicians need to determine the patient's baseline risk of venous thromboembolism (VTE) and weigh the magnitude of benefit with antithrombotic prophylaxis, especially on major clinical endpoints, against the risk of bleeding. Low molecular weight heparin (LMWH) was associated with a 46% lower incidence of symptomatic VTE and 41% reduced incidence of symptomatic pulmonary embolism, respectively, although the absolute differences were relatively small. Low molecular weight heparin did not increase major bleeding when compared with no thromboprophylaxis, but the confidence intervals were wide and the upper limit did not exclude a twice‐as‐high risk of bleeding with heparin. Comorbidities predisposing to bleeding, which often represent an exclusion criterion in randomised controlled trials on anticoagulants, might result in a greater number of major bleeding complications and limit the use of thromboprophylaxis in 'real life'. An additional concern may be the use of thromboprophylaxis in some types of cancers, such as those in the brain, which are considered to be at risk for major bleeding, although preliminary data in brain cancer seem reassuring and suggest a similar risk for LMWH and placebo (Perry 2010). Furthermore, in a recent retrospective analysis, LMWH at therapeutic doses did not increase the risk of intracranial bleeding in patients with brain metastases (Donato 2015). Thus, despite the encouraging results of this review, routine prophylaxis in ambulatory cancer patients cannot be recommended before safety issues are adequately addressed. Since this review mainly included patients with locally advanced or metastatic cancer, the results may not be generalisable to patients with earlier stages of cancer. Of note is that marketing applications for the ultra‐low molecular weight heparin semuloparin have been withdrawn worldwide, and it is therefore unlikely to ever be commercially available (EMEA 2012).
Data on the use of thromboprophylaxis with anticoagulants other than LMWH appear to be preliminary. Four studies compared the vitamin K antagonist warfarin with placebo or no warfarin, but only one reported on VTE. An almost four‐fold increase in major bleeding was observed with warfarin, which was close to, but did not reach, statistical significance. While additional studies are needed to clarify the efficacy and safety of warfarin, the bleeding concerns and the complexity of vitamin K antagonist management discourage the use of warfarin for primary prophylaxis in cancer patients. The lack of an adequate control group in the studies of myeloma patients hampers definitive recommendations for one specific thromboprophylaxis over another. In addition, the trials including myeloma patients focused on specific regimens (thalidomide‐ and lenalidomide‐based combinations). These findings and conclusions may not apply to all myeloma patients but only to those who are receiving such therapies. As renal insufficiency often complicates the course of multiple myeloma, caution should be taken in the administration and dosing of drugs such as LMWH or direct thrombin or factor Xa inhibitors with a predominant renal clearance. Patient subgroups that might benefit from prophylaxis cannot currently be specified, however ongoing studies may provide valuable information in this regard (e.g. NCT02048865; NCT02555878).
Implications for research.
Additional randomised studies are needed to clearly establish the risk‐to‐benefit ratio of anticoagulants in ambulatory cancer patients receiving chemotherapy and to identify subgroups that may benefit most from thromboprophylaxis, such as those with advanced lung or pancreatic cancer. The assessment of the net clinical benefit, for example the reduction of the combined symptomatic VTE and major bleeding, may prove to be more clinically relevant than the independent evaluation of safety and efficacy.
Evidence‐based thrombotic and bleeding risk assessment scores may help in selecting subgroups that are at higher risk of VTE and lower risk of bleeding complications. Several additional aspects related to thromboprophylaxis deserve further study, such as the optimal doses and duration, patient preferences, and quality of life. Future adequately sized studies should include the measurement of compliance and persistence with parenteral and oral treatment, and we would welcome explorations of compliance/persistence as potential effect modifiers on clinical outcomes. Finally, cost analysis data on the use of anticoagulation in people with cancer undergoing chemotherapy would be extremely valuable and supportive of a broader application of prophylaxis in the future. Although data from the six ongoing trials will be invaluable in addressing some of these issues (see Characteristics of ongoing studies), we still need more adequately powered randomised controlled trials evaluating the effects of the oral direct Xa inhibitors and direct thrombin inhibitors (Weitz 2012). Two ongoing studies are evaluating apixaban, in NCT02048865, and rivaroxaban, in NCT02555878, in high‐risk subgroups.
What's new
| Date | Event | Description |
|---|---|---|
| 9 July 2016 | New citation required but conclusions have not changed | Searches rerun. Five additional studies were added to the included studies. Two additional studies excluded on full‐text basis. New authors joined the review team. 'Summary of findings' tables added. Conclusions not changed. |
| 9 July 2016 | New search has been performed | Searches rerun. Five additional studies were added to the included studies. Two additional studies excluded on full‐text basis. |
History
Protocol first published: Issue 5, 2010 Review first published: Issue 2, 2012
| Date | Event | Description |
|---|---|---|
| 24 July 2013 | New citation required but conclusions have not changed | Searches rerun. Twelve additional studies were added to the included studies and nine additional studies to the excluded studies. Risk of bias was reassessed in all included trials. Conclusions not changed. Change in author team. |
| 24 July 2013 | New search has been performed | Searches rerun. Twelve additional studies were added to the included studies and nine additional studies to the excluded studies. |
Acknowledgements
The review authors would like to thank the personnel from Cochrane Vascular, especially Marlene Stewart and Karen Welch, for their invaluable assistance and advice. We are grateful to Professor Anthony Maraveyas, who provided additional unpublished data that proved useful for the current analysis (Maraveyas 2012).
We would like to thank Professor Hans‐Martin Otten for his contribution to the first version of this review.
Appendices
Appendix 1. CENTRAL search strategy
| Search run on Thu Jun 23 2016 | ||
| #1 | MESH DESCRIPTOR Thrombosis | 1211 |
| #2 | MESH DESCRIPTOR Thromboembolism | 880 |
| #3 | MESH DESCRIPTOR Venous Thromboembolism | 221 |
| #4 | MESH DESCRIPTOR Venous Thrombosis EXPLODE ALL TREES | 1979 |
| #5 | (thrombus* or thrombopro* or thrombotic* or thrombolic* or thromboemboli* or thrombos* or embol* or microembol*):TI,AB,KY | 16473 |
| #6 | MESH DESCRIPTOR Pulmonary Embolism EXPLODE ALL TREES | 719 |
| #7 | (PE or DVT or VTE):TI,AB,KY | 4294 |
| #8 | ((vein* or ven*) near thromb*):TI,AB,KY | 5939 |
| #9 | (blood near3 clot*):TI,AB,KY | 2358 |
| #10 | (pulmonary near3 clot*):TI,AB,KY | 5 |
| #11 | (lung near3 clot*):TI,AB,KY | 4 |
| #12 | MESH DESCRIPTOR Antineoplastic Protocols EXPLODE ALL TREES | 11008 |
| #13 | MESH DESCRIPTOR Survival EXPLODE ALL TREES | 123 |
| #14 | surviv*:TI,AB,KY | 51947 |
| #15 | chemotherap*:TI,AB,KY | 36001 |
| #16 | #1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14 OR #15 | 89289 |
| #17 | MESH DESCRIPTOR Anticoagulants EXPLODE ALL TREES | 7943 |
| #18 | (anticoagul* or anti‐coagu*):TI,AB,KY | 7083 |
| #19 | MESH DESCRIPTOR Heparin EXPLODE ALL TREES | 3794 |
| #20 | *parin*:TI,AB,KY | 51054 |
| #21 | UFH:TI,AB,KY | 431 |
| #22 | LMWH:TI,AB,KY | 775 |
| #23 | LMH:TI,AB,KY | 6 |
| #24 | (Ariven or Arteven or Calcilean or Hepalean or Hepathrom or Leparan or Lipo‐Hepin or Liquaemin or Liquemin or Pabyrin or Pularin or Thromboliquine or Vetren ):TI,AB,KY | 9 |
| #25 | (Clexane or klexane or lovenox ):TI,AB,KY | 41 |
| #26 | (Fragmin):TI,AB,KY | 178 |
| #27 | (Innohep):TI,AB,KY | 11 |
| #28 | clivarin* :TI,AB,KY | 20 |
| #29 | (danaproid or danaparoid):TI,AB,KY | 35 |
| #30 | (antixarin):TI,AB,KY | 2 |
| #31 | (Zibor or cy 222 or embolex or monoembolex):TI,AB,KY | 38 |
| #32 | (rd 11885 or RD1185):TI,AB,KY | 0 |
| #33 | (Kabi‐2165 or Kabi 2165):TI,AB,KY | 39 |
| #34 | (emt‐966 or emt966 or emt‐967 or emt977 or pk‐10169 or pk10169):TI,AB,KY | 8 |
| #35 | (fr‐860 or fr860 or cy‐216 or cy216):TI,AB,KY | 51 |
| #36 | (kb101 or lomoparan or orgaran ):TI,AB,KY | 28 |
| #37 | (fluxum or lohepa or lowhepa):TI,AB,KY | 11 |
| #38 | (op 2123 or op2123):TI,AB,KY | 1 |
| #39 | (ave 5026 or ave5026 ):TI,AB,KY | 2 |
| #40 | (M118 or RO‐1):TI,AB,KY | 9 |
| #41 | *coumar*:TI,AB,KY | 594 |
| #42 | (*warfarin or (vitamin near/3 antagonist*)):TI,AB,KY | 2604 |
| #43 | (VKA or phenindione or Sinthrome or nicoumalone or phenprocoumon or Marcoumar or Marcumar or Falithrom or AVK or phenprocoumon* or aldocumar or carfin or jantoven or kumatox or lawarin or marevan or prothromadin or sofarin or tedicumar or tintorane or waran or warfant or warfilone or warnerin):TI,AB,KY | 345 |
| #44 | MESH DESCRIPTOR Antithrombins EXPLODE ALL TREES | 1186 |
| #45 | MESH DESCRIPTOR Hirudin Therapy | 75 |
| #46 | (thrombin near3 inhib*):TI,AB,KY | 484 |
| #47 | hirudin*:TI,AB,KY | 359 |
| #48 | (dabigatran or Pradaxa or Rendix):TI,AB,KY | 305 |
| #49 | (BIBR‐953* or BIBR953* or BIBR‐1048 or BIBR1048):TI,AB,KY | 9 |
| #50 | (ximelagatran or Exanta or Exarta or melagatran):TI,AB,KY | 147 |
| #51 | (AZD0837 or AZD‐0837):TI,AB,KY | 13 |
| #52 | (S35972 or S‐35972):TI,AB,KY | 0 |
| #53 | MESH DESCRIPTOR Factor Xa Inhibitors | 269 |
| #54 | (Factor X* near4 (antag* or inhib* or block*)):TI,AB,KY | 521 |
| #55 | (FX* near4 (antag* or inhib* or block*)):TI,AB,KY | 43 |
| #56 | (10* near4 (antag* or inhib* or block*) ):TI,AB,KY | 1000 |
| #57 | (rivaroxaban or Xarelto):TI,AB,KY | 416 |
| #58 | (Bay‐597939 or Bay597939):TI,AB,KY | 0 |
| #59 | (betrixaban or PRT054021):TI,AB,KY | 14 |
| #60 | apixaban:TI,AB,KY | 222 |
| #61 | (BMS‐562247 or BMS‐562247 or ELIQUIS):TI,AB,KY | 0 |
| #62 | (DU‐176b or DU176b):TI,AB,KY | 11 |
| #63 | (PRT‐054021 or PRT054021):TI,AB,KY | 1 |
| #64 | (YM150 or YM‐150 or LY517717 or LY‐517717 or DU‐176b or DU176*):TI,AB,KY | 39 |
| #65 | (GW813893 or "Tak 442" or TAK442 or PD0348292 or GSK‐813893 or GSK813893):TI,AB,KY | 3 |
| #66 | edoxaban or lixiana:TI,AB,KY | 103 |
| #67 | *ixaban:TI,AB,KY | 243 |
| #68 | *axaban:TI,AB,KY | 6 |
| #69 | *exaban:TI,AB,KY | 11 |
| #70 | etexilate:TI,AB,KY | 108 |
| #71 | agatroban:TI,AB,KY | 1 |
| #72 | *parinux:TI,AB,KY | 281 |
| #73 | MESH DESCRIPTOR Bandages EXPLODE ALL TREES | 2109 |
| #74 | (stocking* or hosier* or tight* or sock* or bandag* ):TI,AB,KY | 4782 |
| #75 | (jobst or surepress or activa or kendall or elbeo or levante or lloveras or cette or sigvaris or solidea or medilast or VenoTrain* or Ulcertec or ComfortPro or Comfort‐Pro or "Ulcer Kit"):TI,AB,KY | 170 |
| #76 | MESH DESCRIPTOR Intermittent Pneumatic Compression Devices EXPLODE ALL TREES | 88 |
| #77 | (compres* or ICD):TI,AB,KY | 6671 |
| #78 | (foot near/3 impulse):TI,AB,KY | 0 |
| #79 | MESH DESCRIPTOR Platelet Aggregation Inhibitors EXPLODE ALL TREES | 8232 |
| #80 | MESH DESCRIPTOR Phosphodiesterase Inhibitors EXPLODE ALL TREES | 5420 |
| #81 | MESH DESCRIPTOR Tetrazoles | 1790 |
| #82 | (antiplatelet* or anti‐platelet* or antiaggreg* or anti‐aggreg*):TI,AB,KY | 2937 |
| #83 | (((platelet or thromboxane or thrombocyte or cyclooxygenase or cyclo‐oxygenase or phosphodiesterase or fibrinogen or PAR‐1) near3 (antagonist or inhibitor))):TI,AB,KY | 2199 |
| #84 | ((gp* or glycoprotein* or protease or P2Y12 or TXA2) near3 inhibit*):TI,AB,KY | 2986 |
| #85 | thienopyridine:TI,AB,KY | 237 |
| #86 | (ticlopidine or Ticlid):TI,AB,KY | 1675 |
| #87 | (clopidogrel or Plavix):TI,AB,KY | 2704 |
| #88 | (Prasugrel or Effient or Efient or Prasita):TI,AB,KY | 395 |
| #89 | (ticagrelor or AZD6140 or Brilinta):TI,AB,KY | 305 |
| #90 | (elinogrel or PRT060128 or PRT‐060128):TI,AB,KY | 8 |
| #91 | (cangrelor or AR‐C6993* or ARC6993*):TI,AB,KY | 43 |
| #92 | (SCH530348 or SCH‐530348):TI,AB,KY | 16 |
| #93 | E5555:TI,AB,KY | 5 |
| #94 | (terutroban or Triplion):TI,AB,KY | 14 |
| #95 | (aspirin* or nitroaspirin or ASA):TI,AB,KY | 16393 |
| #96 | (acetylsalicylic acid):TI,AB,KY | 4463 |
| #97 | (acetyl salicylic acid*):TI,AB,KY | 105 |
| #98 | (triflusal or disgren):TI,AB,KY | 96 |
| #99 | (Cilostazol or Pletal or Pletaal):TI,AB,KY | 440 |
| #100 | (dipyridamol* or Persantine):TI,AB,KY | 1109 |
| #101 | (OPC‐13013 or OPC13013):TI,AB,KY | 5 |
| #102 | (picotamide or picotinamide):TI,AB,KY | 41 |
| #103 | satigrel:TI,AB,KY | 3 |
| #104 | vorapaxar:TI,AB,KY | 65 |
| #105 | indobufen:TI,AB,KY | 82 |
| #106 | #17 OR #18 OR #19 OR #20 OR #21 OR #22 OR #23 OR #24 OR #25 OR #26 OR #27 OR #28 OR #29 OR #30 OR #31 OR #32 OR #33 OR #34 OR #35 OR #36 OR #37 OR #38 OR #39 OR #40 OR #41 OR #42 OR #43 OR #44 OR #45 OR #46 OR #47 OR #48 OR #49 OR #50 OR #51 OR #52 OR #53 OR #54 OR #55 OR #56 OR #57 OR #58 OR #59 OR #60 OR #61 OR #62 OR #63 OR #64 OR #65 OR #66 OR #67 OR #68 OR #69 OR #70 OR #71 OR #72 OR #73 OR #74 OR #75 OR #76 OR #77 OR #78 OR #79 OR #80 OR #81 OR #82 OR #83 OR #84 OR #85 OR #86 OR #87 OR #88 OR #89 OR #90 OR #91 OR #92 OR #93 OR #94 OR #95 OR #96 OR #97 OR #98 OR #99 OR #100 OR #101 OR #102 OR #103 OR #104 OR #105 | 96478 |
| #107 | MESH DESCRIPTOR Neoplasms EXPLODE ALL TREES | 46072 |
| #108 | (malignan* or *neoplas* or cancer*):TI,AB,KY | 86936 |
| #109 | (carcinoma* or adenocarcinoma*):TI,AB,KY | 22901 |
| #110 | (tumour* or tumor*):TI,AB,KY | 29725 |
| #111 | (glio* or leukemia):TI,AB,KY | 8101 |
| #112 | chemotherapy:TI,AB,KY | 35600 |
| #113 | chemoanticoagul*:TI,AB,KY | 0 |
| #114 | myeloma:TI,AB,KY | 2352 |
| #115 | oncolog*:TI,AB,KY | 13312 |
| #116 | metastas*:TI,AB,KY | 10714 |
| #117 | MESH DESCRIPTOR Antineoplastic Agents EXPLODE ALL TREES | 36522 |
| #118 | MESH DESCRIPTOR Neoplasm Metastasis EXPLODE ALL TREES | 3544 |
| #119 | #107 OR #108 OR #109 OR #110 OR #111 OR #112 OR #113 OR #114 OR #115 OR #116 OR #117 OR #118 | 126955 |
| #120 | #16 AND #106 AND #119 | 6302 |
Appendix 2. Abbreviations and scientific terms
| Abbreviation | Scientific description | Lay description |
| Anticoagulation therapy | Blood‐thinning therapy | |
| GES | Graduated elastic stockings | Special socks that improve blood flow in the leg veins and prevent blood from pooling in the legs |
| Incidence | Number of newly diagnosed diseases, in this review cases of VTE | |
| IPC | Intermittent pneumatic compression | A mechanical intervention using an air pump and inflatable leggings to provide pulsing pressure that pushes blood through the veins |
| Primary prophylaxis | Primary protective treatment aiming at the prevention of disease development | |
| Thromboprophylaxis | Treatment to prevent the development of blood clots | |
| VTE | Venous thromboembolism | Blood clots |
Data and analyses
Comparison 1. Anticoagulants versus control: symptomatic venous thromboembolism.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Symptomatic VTE: semuloparin vs placebo | 1 | Risk Ratio (IV, Fixed, 95% CI) | Totals not selected | |
| 2 Symptomatic VTE: LMWH vs no thromboprophylaxis | 9 | 3284 | Risk Ratio (IV, Random, 95% CI) | 0.54 [0.38, 0.75] |
| 2.1 Dalteparin | 5 | 901 | Risk Ratio (IV, Random, 95% CI) | 0.64 [0.39, 1.06] |
| 2.2 Certoparin | 1 | 883 | Risk Ratio (IV, Random, 95% CI) | 0.57 [0.24, 1.35] |
| 2.3 Nadroparin | 1 | 1150 | Risk Ratio (IV, Random, 95% CI) | 0.50 [0.22, 1.13] |
| 2.4 Enoxaparin | 1 | 312 | Risk Ratio (IV, Random, 95% CI) | 0.43 [0.21, 0.88] |
| 2.5 Bemiparin | 1 | 38 | Risk Ratio (IV, Random, 95% CI) | 0.10 [0.01, 1.75] |
| 3 Symptomatic VTE: LMWH vs aspirin | 2 | 781 | Risk Ratio (IV, Random, 95% CI) | 0.51 [0.22, 1.17] |
| 4 Symptomatic VTE: LMWH vs warfarin | 1 | Risk Ratio (IV, Fixed, 95% CI) | Totals not selected | |
| 5 Symptomatic VTE: prophylactic vs intermediate or therapeutic LMWH | 1 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 5.1 Prophylactic vs intermediate | 1 | 51 | Risk Ratio (IV, Fixed, 95% CI) | 2.89 [0.12, 67.75] |
| 5.2 Prophylactic vs therapeutic | 1 | 52 | Risk Ratio (IV, Fixed, 95% CI) | 1.0 [0.07, 15.15] |
| 6 Symptomatic VTE: vitamin K antagonists vs placebo | 1 | Risk Ratio (IV, Fixed, 95% CI) | Totals not selected | |
| 7 Symptomatic VTE: warfarin vs aspirin | 1 | Risk Ratio (IV, Fixed, 95% CI) | Totals not selected | |
| 8 Symptomatic VTE: apixaban vs placebo | 1 | Risk Ratio (IV, Fixed, 95% CI) | Totals not selected |
1.1. Analysis.
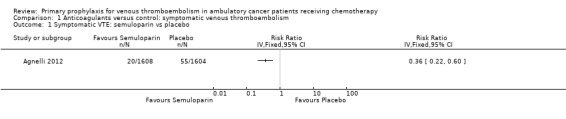
Comparison 1 Anticoagulants versus control: symptomatic venous thromboembolism, Outcome 1 Symptomatic VTE: semuloparin vs placebo.
1.2. Analysis.
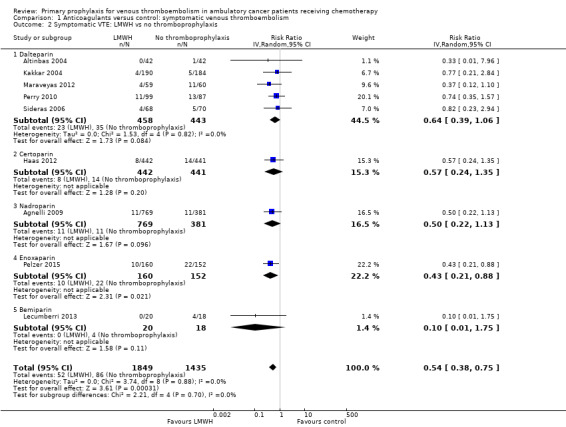
Comparison 1 Anticoagulants versus control: symptomatic venous thromboembolism, Outcome 2 Symptomatic VTE: LMWH vs no thromboprophylaxis.
1.3. Analysis.
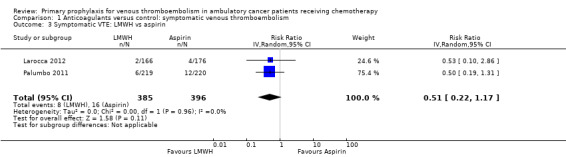
Comparison 1 Anticoagulants versus control: symptomatic venous thromboembolism, Outcome 3 Symptomatic VTE: LMWH vs aspirin.
1.4. Analysis.
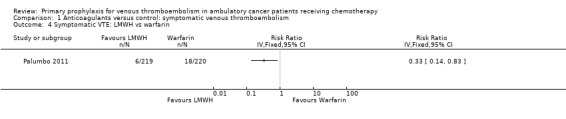
Comparison 1 Anticoagulants versus control: symptomatic venous thromboembolism, Outcome 4 Symptomatic VTE: LMWH vs warfarin.
1.5. Analysis.
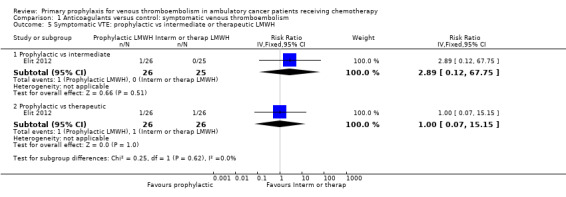
Comparison 1 Anticoagulants versus control: symptomatic venous thromboembolism, Outcome 5 Symptomatic VTE: prophylactic vs intermediate or therapeutic LMWH.
1.6. Analysis.
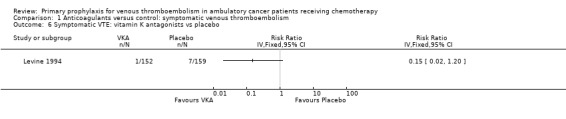
Comparison 1 Anticoagulants versus control: symptomatic venous thromboembolism, Outcome 6 Symptomatic VTE: vitamin K antagonists vs placebo.
1.8. Analysis.
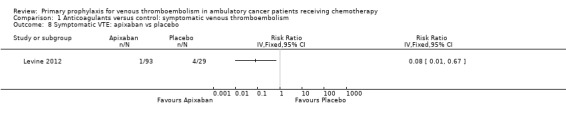
Comparison 1 Anticoagulants versus control: symptomatic venous thromboembolism, Outcome 8 Symptomatic VTE: apixaban vs placebo.
Comparison 2. Anticoagulants versus control: major bleeding.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Major bleeding: semuloparin vs placebo | 1 | Risk Ratio (IV, Fixed, 95% CI) | Totals not selected | |
| 2 Major bleeding: LMWH vs no thromboprophylaxis | 13 | 6356 | Risk Ratio (IV, Random, 95% CI) | 1.44 [0.98, 2.11] |
| 2.1 Dalteparin | 6 | 3119 | Risk Ratio (IV, Random, 95% CI) | 1.29 [0.67, 2.47] |
| 2.2 Certoparin | 1 | 898 | Risk Ratio (IV, Random, 95% CI) | 2.19 [0.84, 5.70] |
| 2.3 Nadroparin | 3 | 1955 | Risk Ratio (IV, Random, 95% CI) | 1.83 [0.69, 4.85] |
| 2.4 Enoxaparin | 2 | 346 | Risk Ratio (IV, Random, 95% CI) | 1.24 [0.56, 2.73] |
| 2.5 Bemiparin | 1 | 38 | Risk Ratio (IV, Random, 95% CI) | 0.30 [0.01, 6.97] |
| 3 Major bleeding: LMWH vs aspirin | 2 | 781 | Risk Ratio (IV, Random, 95% CI) | 0.14 [0.01, 2.76] |
| 4 Major bleeding: LMWH vs warfarin | 1 | 440 | Risk Ratio (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Major bleeding: prophylactic vs intermediate or therapeutic LMWH | 1 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 5.1 Prophylactic vs intermediate | 1 | 51 | Risk Ratio (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5.2 Prophylactic vs therapeutic | 1 | 52 | Risk Ratio (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Major bleeding: vitamin K antagonists vs no thromboprophylaxis | 4 | 994 | Risk Ratio (IV, Random, 95% CI) | 3.82 [0.97, 15.04] |
| 7 Major bleeding: warfarin vs aspirin | 1 | Risk Ratio (IV, Fixed, 95% CI) | Totals not selected | |
| 8 Major bleeding: antithrombin vs placebo | 1 | Risk Ratio (IV, Fixed, 95% CI) | Totals not selected | |
| 9 Major bleeding: apixaban vs placebo | 1 | Risk Ratio (IV, Fixed, 95% CI) | Totals not selected |
2.1. Analysis.
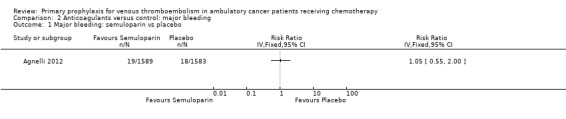
Comparison 2 Anticoagulants versus control: major bleeding, Outcome 1 Major bleeding: semuloparin vs placebo.
2.2. Analysis.
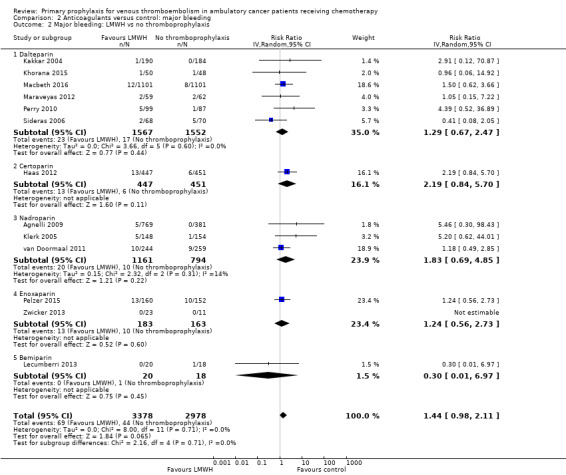
Comparison 2 Anticoagulants versus control: major bleeding, Outcome 2 Major bleeding: LMWH vs no thromboprophylaxis.
2.3. Analysis.
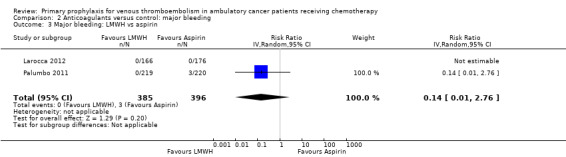
Comparison 2 Anticoagulants versus control: major bleeding, Outcome 3 Major bleeding: LMWH vs aspirin.
2.4. Analysis.
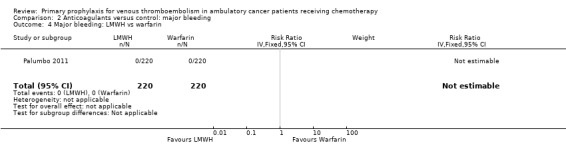
Comparison 2 Anticoagulants versus control: major bleeding, Outcome 4 Major bleeding: LMWH vs warfarin.
2.5. Analysis.
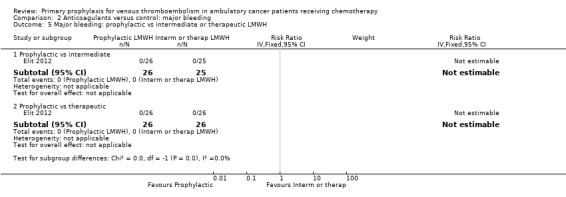
Comparison 2 Anticoagulants versus control: major bleeding, Outcome 5 Major bleeding: prophylactic vs intermediate or therapeutic LMWH.
2.6. Analysis.
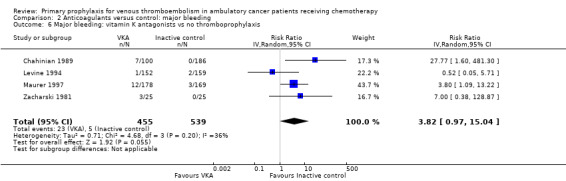
Comparison 2 Anticoagulants versus control: major bleeding, Outcome 6 Major bleeding: vitamin K antagonists vs no thromboprophylaxis.
2.8. Analysis.
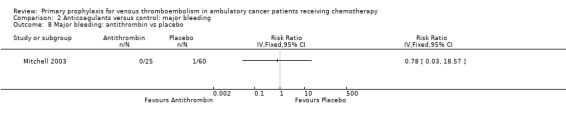
Comparison 2 Anticoagulants versus control: major bleeding, Outcome 8 Major bleeding: antithrombin vs placebo.
2.9. Analysis.
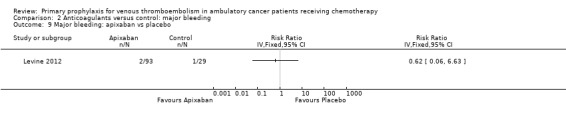
Comparison 2 Anticoagulants versus control: major bleeding, Outcome 9 Major bleeding: apixaban vs placebo.
Comparison 3. Anticoagulants versus control: symptomatic pulmonary embolism.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Symptomatic PE: semuloparin vs placebo | 1 | Risk Ratio (IV, Fixed, 95% CI) | Totals not selected | |
| 2 Symptomatic PE: LMWH vs no thromboprophylaxis | 7 | 5226 | Risk Ratio (IV, Random, 95% CI) | 0.59 [0.40, 0.86] |
| 2.1 Dalteparin | 4 | 2881 | Risk Ratio (IV, Random, 95% CI) | 0.61 [0.40, 0.92] |
| 2.2 Nadroparin | 1 | 1150 | Risk Ratio (IV, Random, 95% CI) | 0.50 [0.10, 2.44] |
| 2.3 Certoparin | 1 | 883 | Risk Ratio (IV, Random, 95% CI) | 0.60 [0.14, 2.49] |
| 2.4 Enoxaparin | 1 | 312 | Risk Ratio (IV, Random, 95% CI) | 0.14 [0.01, 2.61] |
| 3 Symptomatic PE: LMWH vs aspirin | 2 | 781 | Risk Ratio (IV, Random, 95% CI) | 0.13 [0.02, 1.03] |
| 4 Symptomatic PE: LMWH vs warfarin | 1 | Risk Ratio (IV, Fixed, 95% CI) | Totals not selected | |
| 5 Symptomatic PE: prophylactic vs intermediate or therapeutic LMWH | 1 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 5.1 Prophylactic vs intermediate | 1 | 51 | Risk Ratio (IV, Fixed, 95% CI) | 2.89 [0.12, 67.75] |
| 5.2 Prophylactic vs therapeutic | 1 | 52 | Risk Ratio (IV, Fixed, 95% CI) | 3.0 [0.13, 70.42] |
| 6 Symptomatic PE: vitamin K antagonists vs placebo | 1 | Risk Ratio (IV, Fixed, 95% CI) | Totals not selected | |
| 7 Symptomatic PE: warfarin vs aspirin | 1 | Risk Ratio (IV, Fixed, 95% CI) | Totals not selected | |
| 8 Symptomatic PE: apixaban vs placebo | 1 | Risk Ratio (IV, Fixed, 95% CI) | Totals not selected |
3.1. Analysis.
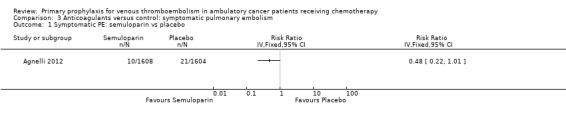
Comparison 3 Anticoagulants versus control: symptomatic pulmonary embolism, Outcome 1 Symptomatic PE: semuloparin vs placebo.
3.2. Analysis.
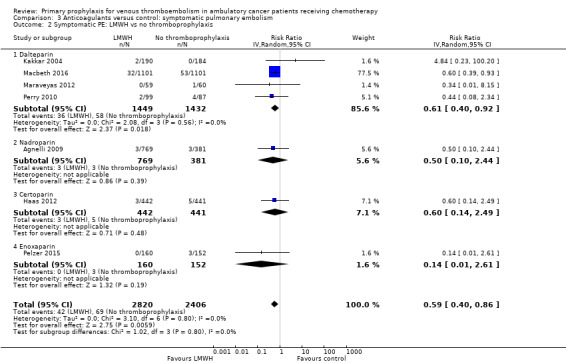
Comparison 3 Anticoagulants versus control: symptomatic pulmonary embolism, Outcome 2 Symptomatic PE: LMWH vs no thromboprophylaxis.
3.3. Analysis.
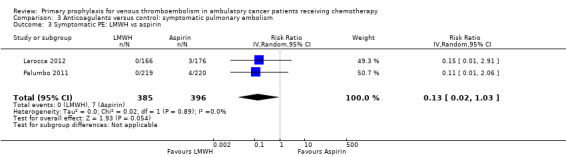
Comparison 3 Anticoagulants versus control: symptomatic pulmonary embolism, Outcome 3 Symptomatic PE: LMWH vs aspirin.
3.4. Analysis.
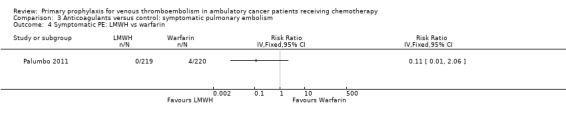
Comparison 3 Anticoagulants versus control: symptomatic pulmonary embolism, Outcome 4 Symptomatic PE: LMWH vs warfarin.
3.5. Analysis.
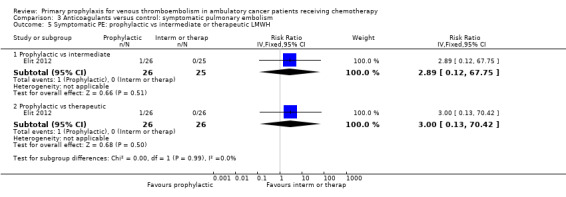
Comparison 3 Anticoagulants versus control: symptomatic pulmonary embolism, Outcome 5 Symptomatic PE: prophylactic vs intermediate or therapeutic LMWH.
3.6. Analysis.
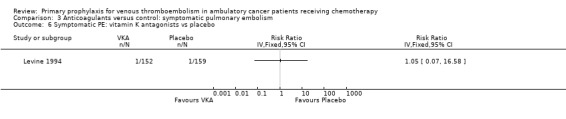
Comparison 3 Anticoagulants versus control: symptomatic pulmonary embolism, Outcome 6 Symptomatic PE: vitamin K antagonists vs placebo.
3.7. Analysis.
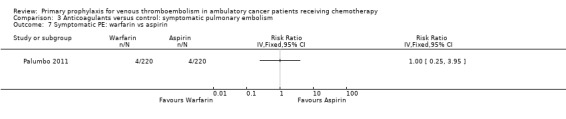
Comparison 3 Anticoagulants versus control: symptomatic pulmonary embolism, Outcome 7 Symptomatic PE: warfarin vs aspirin.
3.8. Analysis.
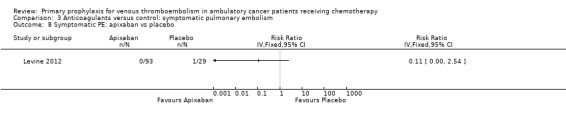
Comparison 3 Anticoagulants versus control: symptomatic pulmonary embolism, Outcome 8 Symptomatic PE: apixaban vs placebo.
Comparison 4. Anticoagulants versus control: symptomatic deep vein thrombosis.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Symptomatic DVT: semuloparin vs placebo | 1 | Risk Ratio (IV, Fixed, 95% CI) | Totals not selected | |
| 2 Symptomatic DVT: LMWH vs no thromboprophylaxis | 8 | 5310 | Risk Ratio (IV, Random, 95% CI) | 0.49 [0.35, 0.67] |
| 2.1 Dalteparin | 5 | 2965 | Risk Ratio (IV, Random, 95% CI) | 0.50 [0.32, 0.78] |
| 2.2 Nadroparin | 1 | 1150 | Risk Ratio (IV, Random, 95% CI) | 0.50 [0.19, 1.31] |
| 2.3 Certoparin | 1 | 883 | Risk Ratio (IV, Random, 95% CI) | 0.46 [0.18, 1.20] |
| 2.4 Enoxaparin | 1 | 312 | Risk Ratio (IV, Random, 95% CI) | 0.45 [0.22, 0.93] |
| 3 Symptomatic DVT: LMWH vs aspirin | 2 | 781 | Risk Ratio (IV, Random, 95% CI) | 0.81 [0.32, 2.04] |
| 4 Symptomatic DVT: LMWH vs warfarin | 1 | Risk Ratio (IV, Fixed, 95% CI) | Totals not selected | |
| 5 Symptomatic DVT: prophylactic vs intermediate or therapeutic LMWH | 1 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 5.1 Prophylactic vs intermediate | 1 | 51 | Risk Ratio (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5.2 Prophylactic vs therapeutic | 1 | 52 | Risk Ratio (IV, Fixed, 95% CI) | 0.33 [0.01, 7.82] |
| 6 Symptomatic DVT: vitamin K antagonists vs placebo | 1 | Risk Ratio (IV, Fixed, 95% CI) | Totals not selected | |
| 7 Symptomatic DVT: warfarin vs aspirin | 1 | Risk Ratio (IV, Fixed, 95% CI) | Totals not selected | |
| 8 Symptomatic DVT: apixaban vs placebo | 1 | Risk Ratio (IV, Fixed, 95% CI) | Totals not selected |
4.1. Analysis.
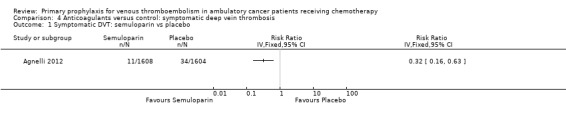
Comparison 4 Anticoagulants versus control: symptomatic deep vein thrombosis, Outcome 1 Symptomatic DVT: semuloparin vs placebo.
4.2. Analysis.
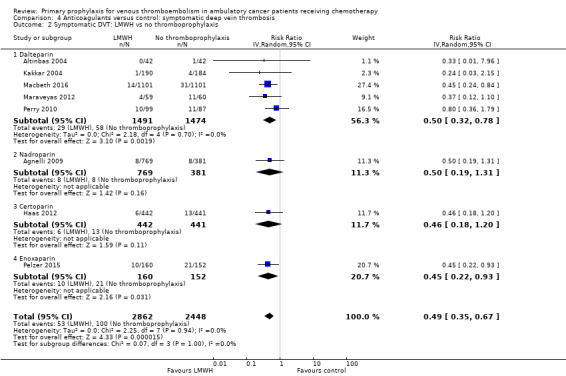
Comparison 4 Anticoagulants versus control: symptomatic deep vein thrombosis, Outcome 2 Symptomatic DVT: LMWH vs no thromboprophylaxis.
4.3. Analysis.
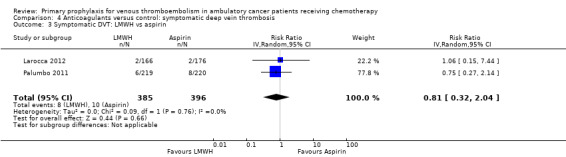
Comparison 4 Anticoagulants versus control: symptomatic deep vein thrombosis, Outcome 3 Symptomatic DVT: LMWH vs aspirin.
4.4. Analysis.
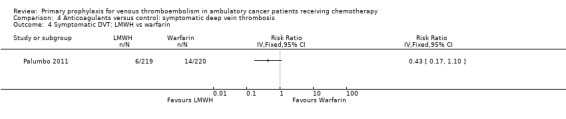
Comparison 4 Anticoagulants versus control: symptomatic deep vein thrombosis, Outcome 4 Symptomatic DVT: LMWH vs warfarin.
4.5. Analysis.
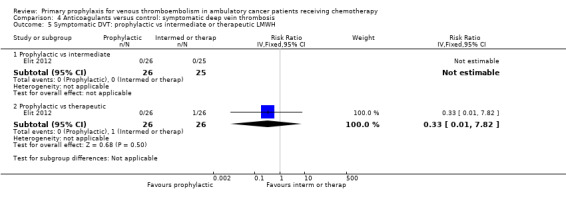
Comparison 4 Anticoagulants versus control: symptomatic deep vein thrombosis, Outcome 5 Symptomatic DVT: prophylactic vs intermediate or therapeutic LMWH.
4.6. Analysis.
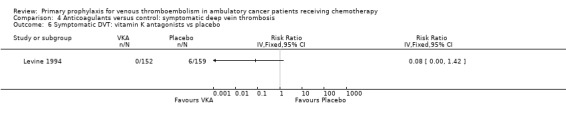
Comparison 4 Anticoagulants versus control: symptomatic deep vein thrombosis, Outcome 6 Symptomatic DVT: vitamin K antagonists vs placebo.
4.7. Analysis.
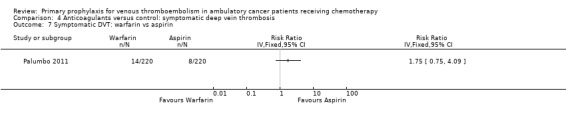
Comparison 4 Anticoagulants versus control: symptomatic deep vein thrombosis, Outcome 7 Symptomatic DVT: warfarin vs aspirin.
4.8. Analysis.
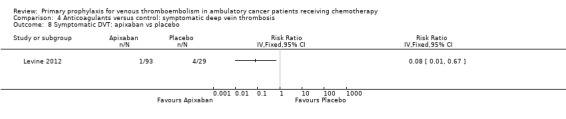
Comparison 4 Anticoagulants versus control: symptomatic deep vein thrombosis, Outcome 8 Symptomatic DVT: apixaban vs placebo.
Comparison 5. Anticoagulants versus control: incidental venous thromboembolism.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Incidental VTE: semuloparin vs placebo | 1 | Risk Ratio (IV, Fixed, 95% CI) | Totals not selected | |
| 2 Incidental VTE: LMWH vs no thromboprophylaxis | 4 | 4354 | Risk Ratio (IV, Random, 95% CI) | 0.66 [0.41, 1.08] |
| 2.1 Dalteparin | 2 | 2321 | Risk Ratio (IV, Random, 95% CI) | 0.62 [0.33, 1.14] |
| 2.2 Nadroparin | 1 | 1150 | Risk Ratio (IV, Random, 95% CI) | 0.74 [0.21, 2.62] |
| 2.3 Certoparin | 1 | 883 | Risk Ratio (IV, Random, 95% CI) | 0.75 [0.26, 2.14] |
| 3 Incidental VTE: prophylactic vs intermediate or therapeutic LMWH | 1 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 3.1 Prophylactic vs intermediate | 1 | 51 | Risk Ratio (IV, Fixed, 95% CI) | 2.89 [0.12, 67.75] |
| 3.2 Prophylactic vs therapeutic | 1 | 52 | Risk Ratio (IV, Fixed, 95% CI) | 3.0 [0.13, 70.42] |
5.1. Analysis.
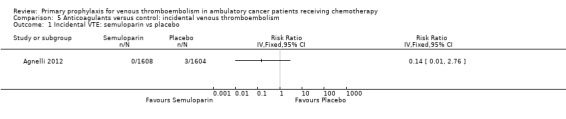
Comparison 5 Anticoagulants versus control: incidental venous thromboembolism, Outcome 1 Incidental VTE: semuloparin vs placebo.
5.2. Analysis.
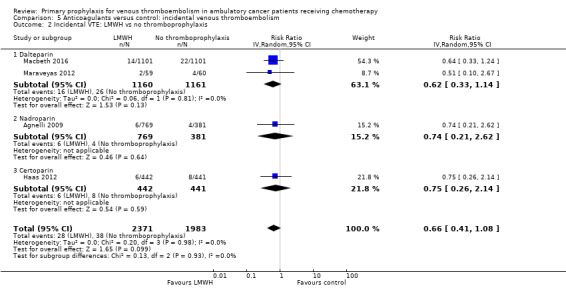
Comparison 5 Anticoagulants versus control: incidental venous thromboembolism, Outcome 2 Incidental VTE: LMWH vs no thromboprophylaxis.
5.3. Analysis.
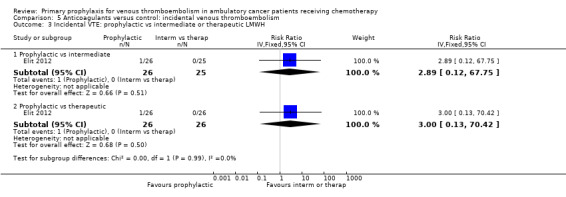
Comparison 5 Anticoagulants versus control: incidental venous thromboembolism, Outcome 3 Incidental VTE: prophylactic vs intermediate or therapeutic LMWH.
Comparison 6. Anticoagulants versus control: overall venous thromboembolism.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Overall VTE: semuloparin vs placebo | 1 | Risk Ratio (IV, Fixed, 95% CI) | Totals not selected | |
| 2 Overall VTE: LMWH vs no thromboprophylaxis | 9 | 5366 | Risk Ratio (IV, Random, 95% CI) | 0.59 [0.48, 0.73] |
| 2.1 Dalteparin | 4 | 2494 | Risk Ratio (IV, Random, 95% CI) | 0.54 [0.41, 0.70] |
| 2.2 Nadroparin | 3 | 1955 | Risk Ratio (IV, Random, 95% CI) | 0.78 [0.48, 1.27] |
| 2.3 Certoparin | 1 | 883 | Risk Ratio (IV, Random, 95% CI) | 0.65 [0.37, 1.15] |
| 2.4 Enoxaparin | 1 | 34 | Risk Ratio (IV, Random, 95% CI) | 0.16 [0.02, 1.36] |
| 3 Overall VTE: prophylactic vs intermediate vs therapeutic LMWH | 1 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 3.1 Prophylactic vs intermediate | 1 | 51 | Risk Ratio (IV, Fixed, 95% CI) | 4.81 [0.24, 95.58] |
| 3.2 Prophylactic vs therapeutic | 1 | 52 | Risk Ratio (IV, Fixed, 95% CI) | 5.0 [0.25, 99.34] |
| 4 Overall VTE: antithrombin vs placebo | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected |
6.1. Analysis.
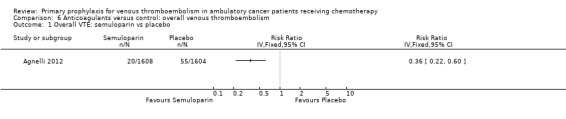
Comparison 6 Anticoagulants versus control: overall venous thromboembolism, Outcome 1 Overall VTE: semuloparin vs placebo.
6.2. Analysis.
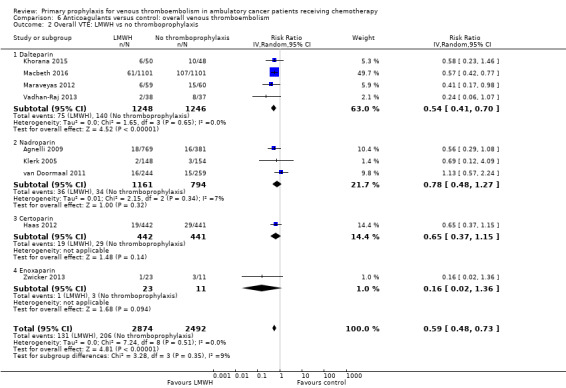
Comparison 6 Anticoagulants versus control: overall venous thromboembolism, Outcome 2 Overall VTE: LMWH vs no thromboprophylaxis.
6.3. Analysis.
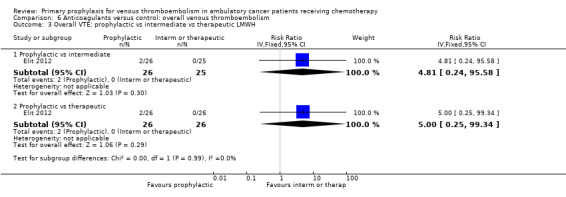
Comparison 6 Anticoagulants versus control: overall venous thromboembolism, Outcome 3 Overall VTE: prophylactic vs intermediate vs therapeutic LMWH.
6.4. Analysis.
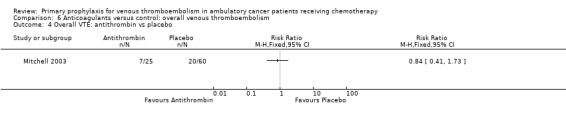
Comparison 6 Anticoagulants versus control: overall venous thromboembolism, Outcome 4 Overall VTE: antithrombin vs placebo.
Comparison 7. Anticoagulants versus control: clinically relevant bleeding.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Clinically relevant bleeding: semuloparin vs placebo | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2 Clinically relevant bleeding: LMWH vs no thromboprophylaxis | 4 | 3105 | Risk Ratio (IV, Random, 95% CI) | 3.40 [1.20, 9.63] |
| 3 Clinically relevant bleeding: prophylactic vs intermediate vs therapeutic LMWH | 1 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 3.1 Prophylactic vs intermediate | 1 | 51 | Risk Ratio (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3.2 Prophylactic vs therapeutic | 1 | 52 | Risk Ratio (IV, Fixed, 95% CI) | 0.33 [0.01, 7.82] |
| 4 Clinically relevant bleeding: apixaban vs placebo | 1 | Risk Ratio (IV, Fixed, 95% CI) | Totals not selected | |
| 5 Clinically relevant bleeding: UFH vs no thromboprophylaxis | 1 | Risk Ratio (IV, Fixed, 95% CI) | Totals not selected |
7.1. Analysis.
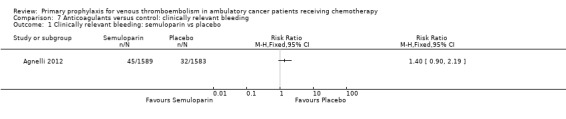
Comparison 7 Anticoagulants versus control: clinically relevant bleeding, Outcome 1 Clinically relevant bleeding: semuloparin vs placebo.
7.2. Analysis.
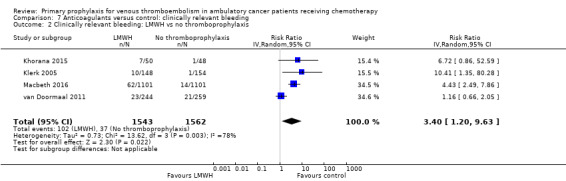
Comparison 7 Anticoagulants versus control: clinically relevant bleeding, Outcome 2 Clinically relevant bleeding: LMWH vs no thromboprophylaxis.
7.3. Analysis.
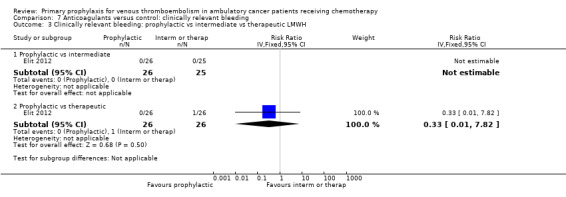
Comparison 7 Anticoagulants versus control: clinically relevant bleeding, Outcome 3 Clinically relevant bleeding: prophylactic vs intermediate vs therapeutic LMWH.
7.4. Analysis.
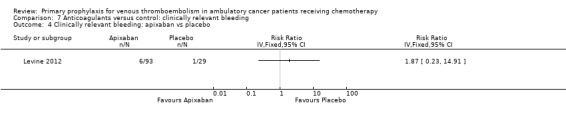
Comparison 7 Anticoagulants versus control: clinically relevant bleeding, Outcome 4 Clinically relevant bleeding: apixaban vs placebo.
7.5. Analysis.
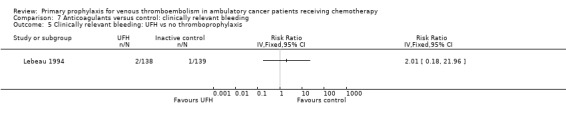
Comparison 7 Anticoagulants versus control: clinically relevant bleeding, Outcome 5 Clinically relevant bleeding: UFH vs no thromboprophylaxis.
Comparison 8. Anticoagulants versus control: minor bleeding.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Minor bleeding: LMWH vs no thromboprophylaxis | 7 | 2803 | Risk Ratio (IV, Random, 95% CI) | 1.23 [0.89, 1.70] |
| 1.1 Dalteparin | 4 | 717 | Risk Ratio (IV, Random, 95% CI) | 1.25 [0.72, 2.17] |
| 1.2 Nadroparin | 1 | 1150 | Risk Ratio (IV, Random, 95% CI) | 1.00 [0.69, 1.45] |
| 1.3 Certoparin | 1 | 898 | Risk Ratio (IV, Random, 95% CI) | 1.96 [1.11, 3.46] |
| 1.4 Bemiparin | 1 | 38 | Risk Ratio (IV, Random, 95% CI) | 0.45 [0.09, 2.17] |
| 2 Minor bleeding: LMWH vs aspirin | 2 | 781 | Risk Ratio (IV, Random, 95% CI) | 0.70 [0.17, 2.84] |
| 3 Minor bleeding: LMWH vs warfarin | 1 | Risk Ratio (IV, Fixed, 95% CI) | Totals not selected | |
| 4 Minor bleeding: prophylactic vs intermediate or therapeutic LMWH | 1 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 4.1 Prophylactic vs intermediate | 1 | 51 | Risk Ratio (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4.2 Prophylactic vs therapeutic | 1 | 52 | Risk Ratio (IV, Fixed, 95% CI) | 0.2 [0.01, 3.97] |
| 5 Minor bleeding: UFH vs no thromboprophylaxis | 1 | Risk Ratio (IV, Fixed, 95% CI) | Totals not selected | |
| 6 Minor bleeding: vitamin K antagonists vs placebo | 1 | Risk Ratio (IV, Fixed, 95% CI) | Totals not selected | |
| 7 Minor bleeding: warfarin vs aspirin | 1 | Risk Ratio (IV, Fixed, 95% CI) | Totals not selected | |
| 8 Minor bleeding: antithrombin vs placebo | 1 | Risk Ratio (IV, Fixed, 95% CI) | Totals not selected |
8.1. Analysis.
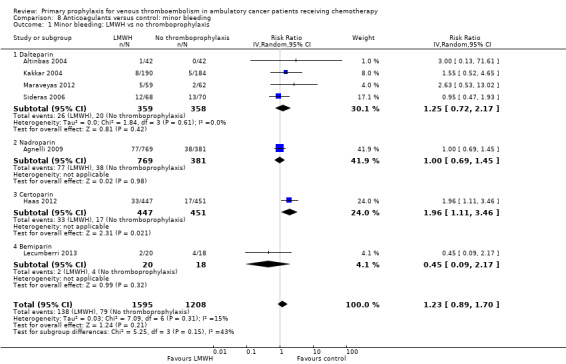
Comparison 8 Anticoagulants versus control: minor bleeding, Outcome 1 Minor bleeding: LMWH vs no thromboprophylaxis.
8.2. Analysis.
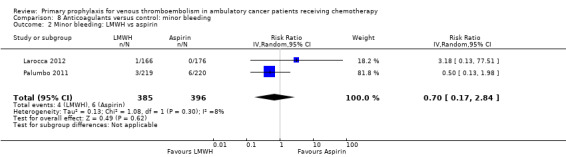
Comparison 8 Anticoagulants versus control: minor bleeding, Outcome 2 Minor bleeding: LMWH vs aspirin.
8.3. Analysis.
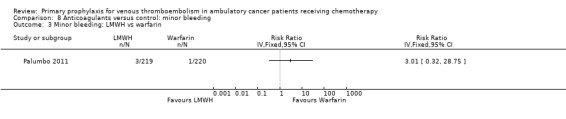
Comparison 8 Anticoagulants versus control: minor bleeding, Outcome 3 Minor bleeding: LMWH vs warfarin.
8.4. Analysis.
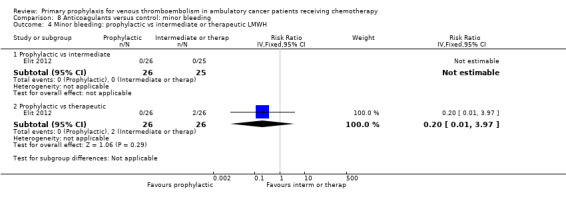
Comparison 8 Anticoagulants versus control: minor bleeding, Outcome 4 Minor bleeding: prophylactic vs intermediate or therapeutic LMWH.
8.5. Analysis.
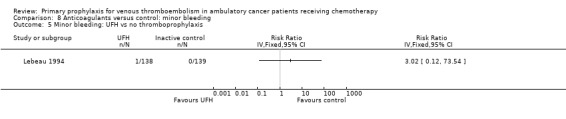
Comparison 8 Anticoagulants versus control: minor bleeding, Outcome 5 Minor bleeding: UFH vs no thromboprophylaxis.
8.6. Analysis.
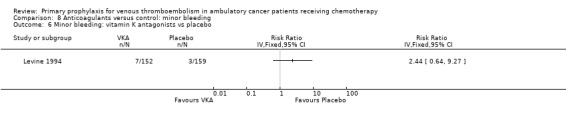
Comparison 8 Anticoagulants versus control: minor bleeding, Outcome 6 Minor bleeding: vitamin K antagonists vs placebo.
8.7. Analysis.
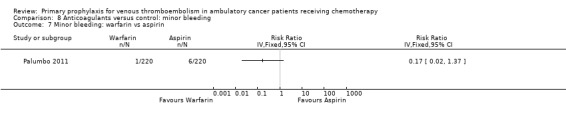
Comparison 8 Anticoagulants versus control: minor bleeding, Outcome 7 Minor bleeding: warfarin vs aspirin.
8.8. Analysis.
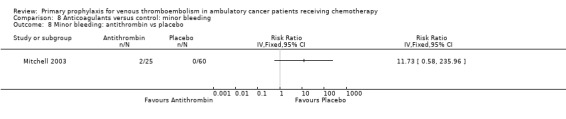
Comparison 8 Anticoagulants versus control: minor bleeding, Outcome 8 Minor bleeding: antithrombin vs placebo.
Comparison 9. Anticoagulants versus control: 1‐year mortality.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 1‐year mortality: semuloparin vs placebo | 1 | Risk Ratio (IV, Fixed, 95% CI) | Totals not selected | |
| 2 1‐year mortality: LMWH vs no thromboprophylaxis | 8 | 2304 | Risk Ratio (IV, Random, 95% CI) | 0.93 [0.80, 1.09] |
| 2.1 Dalteparin | 4 | 782 | Risk Ratio (IV, Random, 95% CI) | 0.97 [0.77, 1.21] |
| 2.2 Nadroparin | 2 | 1452 | Risk Ratio (IV, Random, 95% CI) | 0.95 [0.77, 1.18] |
| 2.3 Enoxaparin | 1 | 34 | Risk Ratio (IV, Random, 95% CI) | 0.72 [0.34, 1.51] |
| 2.4 Bemiparin | 1 | 36 | Risk Ratio (IV, Random, 95% CI) | 0.18 [0.05, 0.70] |
| 3 1‐year mortality: UFH vs no thromboprophylaxis | 1 | Risk Ratio (IV, Fixed, 95% CI) | Totals not selected |
9.1. Analysis.
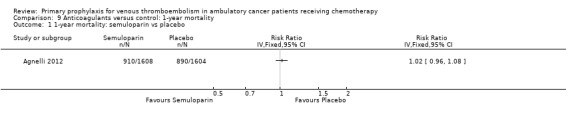
Comparison 9 Anticoagulants versus control: 1‐year mortality, Outcome 1 1‐year mortality: semuloparin vs placebo.
9.2. Analysis.
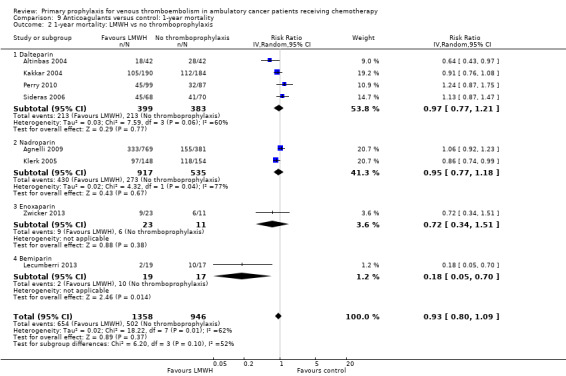
Comparison 9 Anticoagulants versus control: 1‐year mortality, Outcome 2 1‐year mortality: LMWH vs no thromboprophylaxis.
9.3. Analysis.
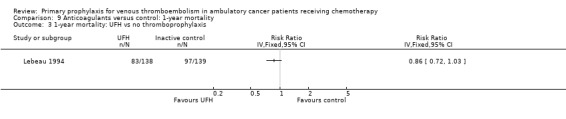
Comparison 9 Anticoagulants versus control: 1‐year mortality, Outcome 3 1‐year mortality: UFH vs no thromboprophylaxis.
Comparison 10. Anticoagulants versus control: symptomatic arterial thromboembolism.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Symptomatic arterial thromboembolism: LMWH vs no thromboprophylaxis | 4 | 3974 | Risk Ratio (IV, Random, 95% CI) | 0.74 [0.46, 1.18] |
| 1.1 Dalteparin | 2 | 2321 | Risk Ratio (IV, Random, 95% CI) | 0.90 [0.52, 1.53] |
| 1.2 Nadroparin | 2 | 1653 | Risk Ratio (IV, Random, 95% CI) | 0.38 [0.14, 1.03] |
| 2 Symptomatic arterial thromboembolism: LMWH vs aspirin | 2 | 781 | Risk Ratio (IV, Random, 95% CI) | 2.01 [0.37, 10.86] |
| 3 Symptomatic arterial thromboembolism: LMWH vs warfarin | 1 | Risk Ratio (IV, Fixed, 95% CI) | Totals not selected | |
| 4 Symptomatic arterial thromboembolism: vitamin K antagonists vs placebo | 1 | Risk Ratio (IV, Fixed, 95% CI) | Totals not selected | |
| 5 Symptomatic arterial thromboembolism: warfarin vs aspirin | 1 | Risk Ratio (IV, Fixed, 95% CI) | Totals not selected |
10.1. Analysis.
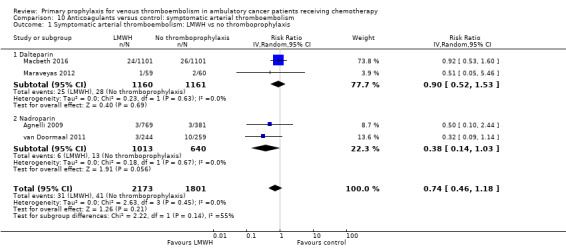
Comparison 10 Anticoagulants versus control: symptomatic arterial thromboembolism, Outcome 1 Symptomatic arterial thromboembolism: LMWH vs no thromboprophylaxis.
10.2. Analysis.
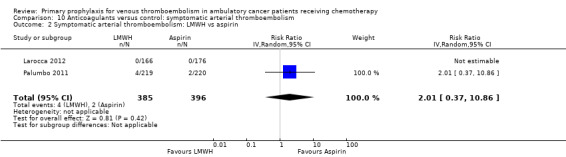
Comparison 10 Anticoagulants versus control: symptomatic arterial thromboembolism, Outcome 2 Symptomatic arterial thromboembolism: LMWH vs aspirin.
10.3. Analysis.
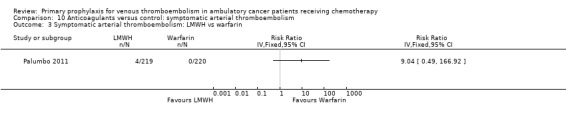
Comparison 10 Anticoagulants versus control: symptomatic arterial thromboembolism, Outcome 3 Symptomatic arterial thromboembolism: LMWH vs warfarin.
10.4. Analysis.
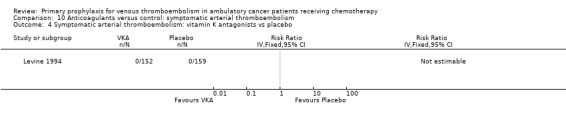
Comparison 10 Anticoagulants versus control: symptomatic arterial thromboembolism, Outcome 4 Symptomatic arterial thromboembolism: vitamin K antagonists vs placebo.
10.5. Analysis.
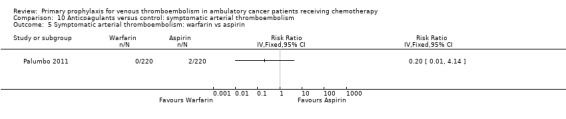
Comparison 10 Anticoagulants versus control: symptomatic arterial thromboembolism, Outcome 5 Symptomatic arterial thromboembolism: warfarin vs aspirin.
Comparison 11. Anticoagulants versus control: superficial venous thrombosis.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Superficial venous thrombosis: LMWH vs no thromboprophylaxis | 2 | 2033 | Risk Ratio (IV, Random, 95% CI) | 0.83 [0.30, 2.26] |
| 1.1 Certoparin | 1 | 883 | Risk Ratio (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 1.2 Nadroparin | 1 | 1150 | Risk Ratio (IV, Random, 95% CI) | 0.83 [0.30, 2.26] |
| 2 Superficial venous thrombosis: LMWH vs aspirin | 1 | Risk Ratio (IV, Fixed, 95% CI) | Totals not selected |
11.1. Analysis.
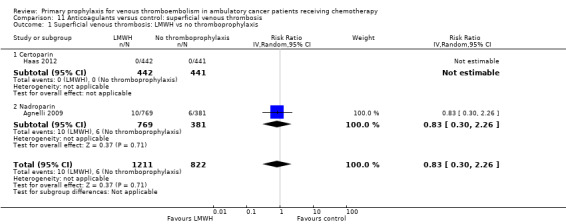
Comparison 11 Anticoagulants versus control: superficial venous thrombosis, Outcome 1 Superficial venous thrombosis: LMWH vs no thromboprophylaxis.
11.2. Analysis.
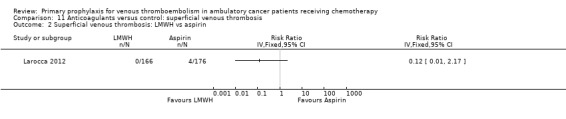
Comparison 11 Anticoagulants versus control: superficial venous thrombosis, Outcome 2 Superficial venous thrombosis: LMWH vs aspirin.
Comparison 12. Anticoagulants versus control: serious adverse events.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Serious adverse events: semuloparin vs placebo | 1 | Risk Ratio (IV, Fixed, 95% CI) | Totals not selected | |
| 2 Serious adverse events: LMWH vs no thromboprophylaxis | 5 | 1531 | Risk Ratio (IV, Random, 95% CI) | 0.86 [0.70, 1.07] |
| 2.1 Dalteparin | 3 | 343 | Risk Ratio (IV, Random, 95% CI) | 1.22 [0.45, 3.34] |
| 2.2 Nadroparin | 1 | 1150 | Risk Ratio (IV, Random, 95% CI) | 0.89 [0.68, 1.17] |
| 2.3 Bemiparin | 1 | 38 | Risk Ratio (IV, Random, 95% CI) | 0.75 [0.43, 1.30] |
| 3 Serious adverse events: apixaban vs placebo | 1 | Risk Ratio (IV, Fixed, 95% CI) | Totals not selected |
12.1. Analysis.
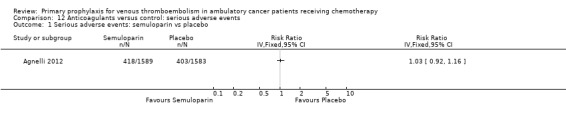
Comparison 12 Anticoagulants versus control: serious adverse events, Outcome 1 Serious adverse events: semuloparin vs placebo.
12.2. Analysis.
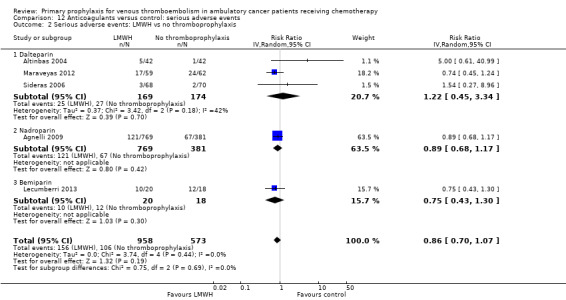
Comparison 12 Anticoagulants versus control: serious adverse events, Outcome 2 Serious adverse events: LMWH vs no thromboprophylaxis.
12.3. Analysis.
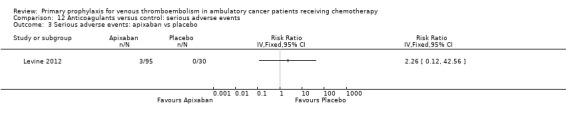
Comparison 12 Anticoagulants versus control: serious adverse events, Outcome 3 Serious adverse events: apixaban vs placebo.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Agnelli 2009.
| Methods | PROTECHT study: multicentre, double‐blind, placebo‐controlled trial; modified intention‐to‐treat analysis, including participants who received at least 1 dose of study treatment | |
| Participants | Ambulatory patients older than 18 years of age who were receiving chemotherapy for metastatic or locally advanced lung, gastrointestinal, pancreatic, breast, ovarian, or head and neck cancer. Mean age (SD): 62.1 (10.3) years in the nadroparin group; 63.7 (9.2) years in the placebo group; male sex, n (%): 372 (48.4) in nadroparin and 183 (48) in placebo; metastatic disease, n (%): not reported; previous VTE: 12 (1.6%) in nadroparin and 6 (1.6) in placebo. The median duration of follow‐up was 111 and 113 days in the nadroparin and placebo groups, respectively. | |
| Interventions | Intervention: LMWH, nadroparin (3800 IU sc, once daily) Control: placebo Study treatment started on the same day as chemotherapy (the first cycle or a new course), and was given for the duration of chemotherapy or up to a maximum of 120 days (± 10 days). |
|
| Outcomes | Primary outcomes: composite of symptomatic venous or arterial thromboembolic events occurring during the study treatment plus 10 days; major bleeding that occurred between randomisation and 48 hours after the last injection of the study drug Secondary efficacy outcomes: incidental thromboembolic events incidentally diagnosed; survival at the end of study treatment and at 12 months; superficial venous thrombosis of the lower limbs; response to chemotherapy; central venous catheter‐related complications of possible thrombotic origin Secondary safety outcome: minor bleeding |
|
| Notes | Antiplatelet agents, oral anticoagulants, fibrinolytic agents, unfractionated heparin, or low molecular weight heparin other than nadroparin not allowed during the study period. Funding: Italfarmaco SpA, Milan, Italy Disclosure of potential conflicts of interest: The scientific director of Italfarmaco was involved as an author. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The randomisation list was generated by an independent statistician who used a standard permuted block of six without stratification. The list was generated with SAS version 8.2." Comment: adequate method of sequence generation |
| Allocation concealment (selection bias) | Low risk | Quote: "The allocation sequence was available online to the investigators using the Hypernet web‐based system. At the time the investigator accessed the web‐based system with personal codes (user ID and password) and requested the treatment allocation for a new patient who fulfilled the eligibility criteria, the system assigned the next free number in accordance with the randomisation sequence" Comment: adequate method of allocation concealment |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Quote: "Patients and investigators did not know whether study drug or placebo was being given, since pre‐filled syringes were used which were identical in appearance. Treatment assignments were masked from all study personnel and participants for the duration of the study." "All study outcomes were assessed by a central independent adjudication committee whose members were unaware of patients’ study‐group allocation" Comment: double‐blinded RCT and adequate methods of blinding |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Quote: "All randomised patients who received at least one dose
of the study treatment were included in the efficacy and
safety analyses" Comment: 769 out of 779 (98.7%) participants randomised were analysed in the LMWH group, 381 out of 387 (98.4%) randomised were analysed in the placebo group. |
| Selective reporting (reporting bias) | Low risk | All outcomes reported in the methods section were addressed in the results or discussion section. |
Agnelli 2012.
| Methods | SAVE‐ONCO study: multicentre, double‐blinded RCT, intention‐to‐treat for effectiveness and modified intention‐to‐treat analysis for safety outcomes, including participants who received at least 1 study dose | |
| Participants | Patients with metastatic or locally advanced solid cancer of the lung, pancreas, stomach, colon or rectum, bladder, or ovary who were beginning a course of chemotherapy. Mean age: 59.8 years in the semuloparin group and 59.4 years in the placebo group. Male, n (%): 974 (60.6) in semuloparin and 956 (59.6) in placebo; metastatic disease: not reported; previous VTE: 2% in semuloparin and 2.3% in placebo. Mean duration of follow‐up: not reported | |
| Interventions | Intervention: uLMWH semuloparin (20 mg sc, once daily)
Control: placebo The first dose of the study drug was administered on the first day of a course of chemotherapy (first regimen or a new regimen), continuing for the duration of chemotherapy (intended to be a minimum of 3 months). Median treatment duration was 3.5 months. |
|
| Outcomes | Primary efficacy outcome: composite of any symptomatic DVT, any non‐fatal PE, and death related to VTE Primary safety outcome: clinically relevant bleeding (major and non‐major) Secondary efficacy outcome: 1‐year overall survival or at the study end date |
|
| Notes | Funding, quote: "Supported by Sanofi". "The study was designed by the steering committee members and sponsored by Sanofi. Data were collected through a clinical research organization and analyzed by Sanofi. No Sanofi employees were members of the steering committee or the data and safety monitoring board" Disclosure of potential conflicts of interest: In the section "The Work Under Consideration for Publication", some of the authors declared they were employed by Sanofi or had received consulting fee or honorarium and support for travel to meetings by Sanofi‐Aventis. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomization was performed centrally by means of an interactive voice‐response system." Comment: adequate method of sequence generation |
| Allocation concealment (selection bias) | Low risk | Quote: "Randomization was performed centrally by means of an interactive voice‐response system." Comment: adequate method of allocation concealment |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Quote: "Efficacy and bleeding outcomes were assessed by a central independent adjudication committee, whose members were unaware of the study treatment" Comment: double‐blinded RCT and blinding of outcome assessors |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "All patients who underwent randomization were included in the primary efficacy population (intention‐to‐treat population), and those who underwent randomization and received at least one dose of the study treatment were included in the safety population" Comment: For safety, 1589 out of 1608 participants (98.8%) randomised are analysed in the uLMWH group, 1583 out of 1604 participants (98.7%) randomised are analysed in the placebo group. |
| Selective reporting (reporting bias) | Low risk | All outcomes reported in the protocol and in the methods section of the full report were addressed in the results or discussion section, except for 1 outcome mentioned in the protocol only: "Secondary efficacy variables include the initiation of curative treatment by the investigator after VTE". We did not consider this outcome to be relevant for the current review. |
Altinbas 2004.
| Methods | RCT; intention‐to‐treat analysis for survival outcomes | |
| Participants | Patients between ages 18 and 75 years with histologically confirmed small cell lung carcinoma with an ECOG performance status of less than 3 and normal haematological, renal, and hepatic function tests. Median age: 58 years (range 34 to 75); gender, n: 33 males and 9 females in dalteparin, 35 males and 7 females in control; metastatic disease, n: 19 in dalteparin and 17 in control; previous VTE: 0/84. Median duration of follow‐up: 10 months (range 2 to 33 months) | |
| Interventions | Intervention: LMWH, dalteparin (5000 IU sc, once daily) Control: no dalteparin Dalteparin was stopped with disease progression or at the end of the 18 weeks of chemotherapy. Median duration of treatment was 18 weeks. |
|
| Outcomes | Primary outcome: overall survival Secondary outcomes: progression‐free survival, side effects |
|
| Notes | Funding: not reported Disclosure of potential conflicts of interest: not disclosed, no COI forms available |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Patients were randomized to receive either CT or CT plus LMWH" Comment: method of random sequence generation not reported |
| Allocation concealment (selection bias) | Unclear risk | Quote: "Patients were randomized to receive either CT or CT plus LMWH" Comment: method of allocation concealment not reported |
| Blinding (performance bias and detection bias) All outcomes | High risk | Comment: The trial is reported as a "Chemotherapy‐only" versus Chemotherapy + LMWH" trial, without mentioning the use of placebo LMWH, or any attempt to blind. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Comment: For effectiveness is not reported. For safety, survival is analysed according to the intention‐to‐treat principle. |
| Selective reporting (reporting bias) | Low risk | Comment: All outcomes reported in the methods section were addressed in the results or discussion section. |
Chahinian 1989.
| Methods | Multicentre, 3‐arm RCT, type of analyses not reported | |
| Participants | Patients with extensive carcinoma of the lung. Patients aged 60 years or older: 55% warfarin and 60% control group; males: 68% and 67%, respectively. Metastatic or extensive disease: 100%; previous VTE: not reported | |
| Interventions | Intervention: warfarin to maintain a prothrombin 1.5 to twice the control values Control: no warfarin Warfarin was continued throughout the course of chemotherapy, and it was withheld in participants with brain metastases during cranial irradiation and whenever platelet counts fell below 75,000/μL. |
|
| Outcomes | Main outcomes: overall survival, failure‐free survival, and cancer response (complete response, partial response, and objective response rate) to therapy Secondary outcomes: toxicity |
|
| Notes | Funding: grants from the National Cancer Institute, Department of Health and Human Services, and the T.J. Martell Foundation for Leukemia and Cancer Research Disclosure of potential conflicts of interest: not disclosed, no COI forms available 2 out of 3 available trial arms were considered in this review, as the chemotherapy provided was the same in both arms. The excluded trial arm provided a different chemotherapy regimen. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "allocation was determined by a Latin square arrangement balancing the sequence within and across institutions" Comment: adequate method of sequence generation; stratified randomisation, use of Latin square design |
| Allocation concealment (selection bias) | Unclear risk | Comment: method of allocation concealment not reported |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Comment: blinding not reported, use of placebo warfarin not reported |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Comment: 34 out of 328 participants (10%) enrolled in the study were not considered for the analysis. Exclusions per trial arm were not reported. |
| Selective reporting (reporting bias) | Unclear risk | Comment: All outcomes reported in the methods section were addressed in the results or discussion section. Toxicity was addressed in the results, but not explicitly reported as an outcome in the methods section. |
Elit 2012.
| Methods | Multicentre, open‐label, phase II randomised trial with 3 active treatment arms | |
| Participants | Women with newly diagnosed epithelial ovarian cancer stage IIB to IV. Age, median (min‐max): 61 years (34, 74); female: 100%; metastatic disease: not reported; previous VTE, n (%): 4 (5) | |
| Interventions | Intervention 1: standard adjuvant chemotherapy (taxane and platinum‐based) and dalteparin 50 IU/kg subcutaneously once daily during the first 3 of 6 cycles of 3‐weekly CT Intervention 2: standard adjuvant chemotherapy (taxane and platinum‐based) and dalteparin 100 IU/kg subcutaneously once daily during the first 3 of 6 cycles of 3‐weekly CT Intervention 3: standard adjuvant chemotherapy (taxane and platinum‐based) and dalteparin 150 IU/kg subcutaneously once daily during the first 3 of 6 cycles of 3‐weekly CT Study medication was started within 7 days prior to the first 21‐day cycle of chemotherapy and continued until day 21 of cycle 3. |
|
| Outcomes | Primary outcome: tumour response defined by ≥ 50% reduction in serum CA125 from baseline sustained for at least 28 days Secondary outcomes: major bleeding up to 24 hours after the last dose of dalteparin; any bleeding up to 24 hours after the last dose of dalteparin; symptomatic VTE up to 7 days after the last dose of dalteparin; death up to the last day of follow‐up; and compliance with dalteparin administration Participants were followed until the end of CT. |
|
| Notes | Funding, quote: "The Steering Committee wishes to acknowledge the financial support from both the Juravinski Cancer Centre Foundation and Pfizer Canada Inc" Disclosure of potential conflicts of interest, quote: "There are no financial disclosures from any of the authors related to this work except for Dr. Lee who has provided educational lectures and received financial reimbursement from Pfizer Canada Inc." Quote: "The study was terminated early due to poor recruitment." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Concealed randomization was performed centrally ... using a computer‐generated, permuted‐block randomization schedule." Comment: adequate method of sequence generation |
| Allocation concealment (selection bias) | Low risk | Quote: "Concealed randomization was performed centrally ... using a computer‐generated, permuted‐block randomization schedule." Comment: adequate method of allocation concealment |
| Blinding (performance bias and detection bias) All outcomes | High risk | Quote: "Study outcomes were adjudicated by members of a Central Adjudication Committee masked to treatment assignment." Comment: open‐label study with blinded adjudication of outcomes |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "The primary analysis included all patients as randomized" Comment: All participants who were randomised were included in the analysis. |
| Selective reporting (reporting bias) | Low risk | Comment: All outcomes indicated in the methods are presented in the results. |
Haas 2012.
| Methods | TOPIC‐1 and TOPIC‐2 studies: multicentre RCTs, intention‐to‐treat analysis for effectiveness and modified intention‐to‐treat analysis for safety outcomes | |
| Participants | Patients with metastatic breast cancer (n = 353) or non‐small cell lung carcinoma (n = 547) receiving first‐ or second‐line chemotherapy. In the TOPIC‐1 study (breast cancer patients), the mean age (SD) was 54.6 (10.3) years in the certoparin group and 56.6 (11.0) years in the placebo group. In the TOPIC‐2 study (lung cancer patients), the mean age (SD) was 60.8 (9.5) years in the certoparin group and 60.3 (10.0) years in the placebo group. Males, n (%): TOPIC‐1: none, TOPIC‐2: 227 (83.2) in both certoparin and placebo; metastatic disease: not reported; previous VTE: 0/900 | |
| Interventions | Intervention: LMWH, certoparin (3000 IU sc, once daily) Control: placebo Study treatment was given for 6 months. |
|
| Outcomes | Primary outcomes: symptomatic or incidental VTE, major bleeding Secondary outcomes: symptomatic VTE, overall thrombosis rate (to include arterial thrombotic events, superficial venous thrombosis, and central‐line thrombosis), minor bleeding, thrombocytopenia, heparin‐induced thrombocytopenia, osteoporotic fractures, survival Post hoc: mortality, symptomatic or incidental VTE according to tumour stage |
|
| Notes | Funding: grant from Novartis Pharma, Nuremberg, Germany. Quote: "The TOPIC studies were supported by an unrestricted grant from Novartis Pharma GmbH, Germany." Disclosure of potential conflicts of interest, quote: "The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article." The study on breast cancer was prematurely halted after an interim analysis. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Using a computer‐generated randomisation list" and "Randomization was block‐stratified according to treatment with hormone‐based chemotherapy" Comment: adequate method of sequence generation |
| Allocation concealment (selection bias) | Unclear risk | Quote: "Randomization numbers were allocated sequentially as patients were enrolled at each center." Comment: Concealment of allocation was poorly reported. It was not reported if sealed, opaque, and consecutively numbered envelopes, coded syringes, or other methods were used. In addition, it remains unclear what is meant by randomisation number in "Patients were allocated to the lowest available randomisation number available for each study center." |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Quote: "Efficacy outcomes were validated by a blinded, independent Central Thrombosis Evaluation Team; safety end points were validated by a Data Safety Monitoring Committee consisting of 2 clinicians (blinded to treatment) and an independent statistician with access to the treatment assignments." and "Only the external statistician from the Safety Committee had access to the randomization codes." Comment: double‐blinded, placebo‐controlled RCT with blinding of participants, physicians, and outcome assessors |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Comment: For effectiveness, 442 out of 447 (98.9%) in the LMWH group and 441 out of 453 (97.4%) in the placebo group were analysed. For safety, 447 out of 447 (100%) in the LMWH group and 451 out of 453 (99.6%) in the placebo group were analysed. |
| Selective reporting (reporting bias) | Low risk | Comment: All outcomes reported in the methods section were addressed in the results or discussion section. However, the outcome osteoporotic fracture was incompletely reported; it remained unclear in which of the TOPIC‐2 trial arms the single event occurred. Post hoc analyses were reported transparently. |
Kakkar 2004.
| Methods | FAMOUS study: double‐blind, placebo‐controlled, multicentre RCT; modified intention‐to‐treat analysis for both effectiveness and safety analyses, including participants with at least 1 study dose and 1 follow‐up visit | |
| Participants | Patients of 18 and 80 years with histologically confirmed advanced stage III or IV (locally advanced or metastatic) malignant disease of the breast, lung, gastrointestinal tract, pancreas, liver, genitourinary tract, ovary, or uterus. Age: 62 years in the dalteparin group and 60.9 years in the placebo group; female, n (%): 113 (59.5) in dalteparin and 100 (54.3) in placebo; metastatic disease, n: 161 in both dalteparin and placebo; previous VTE: 0/385. Median duration of follow‐up: 10 months in the dalteparin group and 9 months in the placebo group | |
| Interventions | Intervention: LMWH, dalteparin (5000 IU sc, once daily) Control: placebo (0.9% normal saline) Study treatment given for 1 year or until the participant died, whichever occurred sooner |
|
| Outcomes | Primary outcomes: mortality after 1 year of therapy Secondary outcomes: symptomatic, objectively confirmed VTE disease and bleeding complications |
|
| Notes | Funding: Pharmacia Corp, New York, NY Disclosure of potential conflicts of interest: The lead author declared having acted as a consultant for Pfizer. Quote: "The following authors or their immediate family members have indicated a financial interest. No conflict exists for drugs or devices used in a study if they are not being evaluated as part of the investigation. Acted as a consultant within the last 2 years: Ajay K. Kakkar, Pfizer. Received more than $2,000 a year from a company for either of the last 2 years: Ajay K. Kakkar, Pfizer" |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomization was performed centrally by computer‐generated code" Comment: adequate method of sequence generation |
| Allocation concealment (selection bias) | Low risk | Quote: "Randomization was performed centrally by computer‐generated code" Comment: adequate method of allocation concealment |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Quote: "placebo (0.9% normal saline), each supplied in 0.2‐mL prefilled
syringes" Comment: trial reported as double‐blind, with active substance or placebo provided in prefilled syringes. It is not reported whether syringes were identical in appearance. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Comment: Both for effectiveness and safety, 190 out of 196 (96.9%) were analysed in the LMWH group and 184 out of 189 (97.4%) were analysed in the placebo group. |
| Selective reporting (reporting bias) | Low risk | Comment: All outcomes reported in the methods section were addressed in the results or discussion section. |
Khorana 2015.
| Methods | PHACS trial: a multicentre RCT | |
| Participants | Cancer patients at high risk for VTE (Khorana score ≥ 3) and initiating a new systemic chemotherapy regimen. Mean age (SD): dalteparin 60 (10) and observation 58 (12); gender, female/male: 21/29 dalteparin and 24/24 observation; metastatic disease: not reported; previous history of VTE, n (%): dalteparin 4 (8) and observation 2 (4) | |
| Interventions | Intervention: LMWH, dalteparin 5000 IU daily subcutaneously for 12 weeks Control: no dalteparin |
|
| Outcomes | Primary outcome: any VTE over 12 weeks Participants in both arms were screened with lower extremity ultrasounds every 4 weeks of study. Primary safety endpoint was clinically relevant bleeding events over 13 weeks. |
|
| Notes |
NCT00876915 Funding: not reported Disclosure of potential conflicts of interest: All authors report conflicts of interest. The study was terminated due to poor accrual. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "randomized to either dalteparin 5000 units daily subcutaneously or no prophylactic anticoagulation" Comment: method of sequence generation not reported |
| Allocation concealment (selection bias) | Unclear risk | Quote: "randomized to either dalteparin 5000 units daily subcutaneously or no prophylactic anticoagulation" Comment: method of allocation concealment not reported |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Comment: It is not reported whether participants, personnel, and outcome assessors were blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "Of 117 enrolled patients, 19 were not randomized due to the presence of VTE on initial screening (N =10, 8.5%) or for other reasons (N = 9)." Comment: All randomised participants were included in the analysis. |
| Selective reporting (reporting bias) | Low risk | Comment: All outcomes indicated in the methods of the abstract are reported in the results. |
Klerk 2005.
| Methods | MALT study: multicentre, double‐blinded, randomised, placebo‐controlled study with intention‐to‐treat analyses for both effectiveness and safety, including participants who received at least 1 study dose | |
| Participants | Patients with metastasised or locally advanced solid tumours. Median age (range): 63 years (36 to 86) in the nadroparin group and 64 years (28 to 83) in the placebo group; male, n (%): 77 (52) in nadroparin and 81 (53) in placebo; metastatic disease, n (%): 137 (93) in nadroparin and 139 (90) in placebo; previous VTE: 0/302. Mean duration of follow‐up: 12 months | |
| Interventions | Intervention: LMWH, nadroparin Control: placebo Prefilled syringes containing a fixed volume of nadroparin (9500 anti‐factor Xa U/mL) or placebo were provided according to participant’s weight: 0.4 mL for those weighing less than 50 kg, 0.6 mL for those weighing between 50 kg and 70 kg, and 0.8 mL for those weighing more than 70 kg. Study treatment was to be administered sc twice daily during the initial 14 days of treatment and once daily thereafter for another 4 weeks. |
|
| Outcomes | Primary efficacy outcome: death from any cause
Primary safety outcome: major bleeding Secondary safety outcome: clinically relevant non‐major bleeding |
|
| Notes | Funding: The study treatment was provided by Sanofi‐Synthelabo (Paris, France). The authors state that "protocol design, data collection, and analysis were solely the responsibility of the authors". Disclosure of potential conflicts of interest: The senior author and statistician declared consultancy activities for various pharmaceutical companies, including Sanofi‐Synthelabo. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Sequentially numbered boxes of syringes with nadroparin or placebo were prepared using a central computer‐generated randomization schedule, stratified for body weight with blocks of four" Comment: adequate method of sequence generation |
| Allocation concealment (selection bias) | Low risk | Quote: "Sequentially numbered boxes of syringes with nadroparin or placebo were prepared using a central computer‐generated randomization schedule, stratified for body weight with blocks of four" Comment: adequate method of allocation concealment |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Quote: "Prefilled syringes containing a fixed volume of nadroparin (9,500 antifactor Xa U/mL) or placebo were provided according to patient’s weight" Comment: trial reported as double‐blind, with active substance or placebo provided in prefilled syringes. It is not reported whether syringes were identical in appearance. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: All enrolled participants were included in the analysis. |
| Selective reporting (reporting bias) | Low risk | Comment: All outcomes reported in the methods section were addressed in the results or discussion section. The authors reported reasons for the discontinuation of the study drug in the results section only, but this was for descriptive purposes, so unlikely to introduce bias. |
Larocca 2012.
| Methods | Prospective, multicentre, open‐label, randomised substudy of a phase III trial with modified intention‐to‐treat analyses of both effectiveness and safety outcomes, including participants who received at least 1 study dose | |
| Participants | Patients with newly diagnosed multiple myeloma treated with lenalidomide and low‐dose dexamethasone induction and melphalan‐prednisone‐lenalidomide consolidation. Median age: 57 years in the aspirin group, 58 years in the enoxaparin group; male, n (%): 87 (49) in aspirin and 99 (60) in LMWH; metastatic disease: not reported; previous VTE: 0/342 | |
| Interventions | Intervention 1: LMWH, enoxaparin (40 mg/day sc) Intervention 2: aspirin (100 mg/day) Prophylaxis was provided during the 4 (28‐day) cycles of lenalidomide and low‐dose dexamethasone and the 6 (28‐day) cycles of melphalan‐prednisone‐lenalidomide consolidation. Median treatment duration was 3.6 months for aspirin and 3.5 months for LMWH. |
|
| Outcomes | Primary endpoint: composite of symptomatic DVT, PE, arterial thrombosis, any acute cardiovascular event, or sudden otherwise‐unexplained death in the first 6 months after randomisation Secondary outcomes: major and minor bleeding, any complications related to thromboprophylaxis |
|
| Notes | Funding: The main study (RV‐MM‐PI209) was supported by Fondazione Neoplasie Sangue Onlus, and Celgene supplied free lenalidomide. The authors declared that Celgene had no role in the study design, data analysis, data interpretation, or writing of the report. Disclosure of potential conflicts of interest: Several authors declared having received honoraria or consultancy fees from various pharmaceutical companies, including Celgene. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "simple randomization sequence run by a central computer, which generated an automated assignment procedure that was concealed from the investigators in each study center" Comment: adequate method of sequence generation |
| Allocation concealment (selection bias) | Low risk | Quote: "simple randomization sequence run by a central computer, which generated an automated assignment procedure that was concealed from the investigators in each study center" Comment: adequate method of allocation concealment |
| Blinding (performance bias and detection bias) All outcomes | High risk | Quote: "Open‐label" study Comment: open study with no blinding of participants, physicians, and outcome assessors |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: All randomised participants were included in the analysis. |
| Selective reporting (reporting bias) | Low risk | Comment: All outcomes reported in the methods section were addressed in the results or discussion section. |
Lebeau 1994.
| Methods | Multicentre, open‐label, randomised substudy, with intention‐to‐treat analyses | |
| Participants | Patients with limited and extensive small cell lung cancer who had not been previously treated with chemotherapy or radiotherapy. Male, n (%): 120 (87) in heparin and 132 (95) in control; extensive disease: 74 (54) in heparin and 82 (59) in control; previous VTE: not reported | |
| Interventions | Intervention: chemotherapy with sc UFH. The dose of UFH was initially adapted to weight (500 IU/kg/day) then adjusted by clotting times. UFH was administered in 2 or 3 daily injections for 5 weeks and stopped 1 week after the second course of chemotherapy. Control: chemotherapy without UFH |
|
| Outcomes | Primary outcome: overall survival, response to chemotherapy Secondary outcomes: bleeding, UFH‐related thrombocytopenia |
|
| Notes | Funding: none reported Disclosure of potential conflicts of interest: not disclosed, no COI forms available |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "randomized through a centralized blind telephone assignment procedure" Comment: method of sequence generation not clearly reported |
| Allocation concealment (selection bias) | Low risk | Quote: "randomized through a centralized blind telephone assignment procedure" Comment: adequate method of allocation concealment |
| Blinding (performance bias and detection bias) All outcomes | High risk | Quote: "No bIinding procedure for patients and physicians was used" Comment: open label study with no blinding of participants or physicians. Not reported if there was blinding of outcome assessors |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "No patient was lost to follow up" Comment: All participants enrolled in the randomised substudy were analysed. |
| Selective reporting (reporting bias) | Low risk | Comment: All outcomes reported in the methods section were addressed in the results section. |
Lecumberri 2013.
| Methods | Adjuvant Bemiparin in Small Cell Lung Cancer (ABEL) study: a multicentre, investigator‐initiated, open‐label, randomised study | |
| Participants | Patients with newly diagnosed, limited‐stage small cell lung cancer. Mean age 62.7 ± 8.9 years; 33 males and 5 females; previous VTE: none; metastatic disease: none | |
| Interventions | Intervention: standard chemoradiotherapy plus bemiparin 3500 IU daily for a maximum of 26 weeks Bemiparin was started on the first day of the first cycle of chemotherapy and stopped at disease progression or at the end of the 26 weeks of treatment. Control: standard first‐line platinum‐based chemotherapy and radiotherapy |
|
| Outcomes | Primary efficacy outcome: progression‐free survival Primary safety outcome: major bleeding Secondary outcomes were overall survival, tumour response rate to chemoradiotherapy, incidence of objectively confirmed symptomatic VTE, minor bleeding, thrombocytopenia, death from any cause, and incidence of any other adverse event. |
|
| Notes | Funding, quote: "Bemiparin 3,500 IU syringes were provided without charge by Laboratorios Farmacéuticos ROVI. S.A. The company also gave economic support for the expenses of the CRO, but was not directly involved in the design of the study, collection or analysis of the data or in the preparation of the manuscript." Quote: "The study was terminated early due to slow recruitment" |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomization was performed through an automatic central randomization system" Comment: adequate method of sequence generation |
| Allocation concealment (selection bias) | Low risk | Quote: "Randomization was performed through an automatic central randomization system" Comment: adequate method of allocation concealment |
| Blinding (performance bias and detection bias) All outcomes | High risk | Quote: "there was no central adjudication committee." Comment: open study with unblinded adjudication of outcomes |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: 1 of 39 (2.56%) included participants was excluded from the analysis. |
| Selective reporting (reporting bias) | Low risk | Comment: All outcomes indicated in the methods are reported in the results. |
Levine 1994.
| Methods | Multicentre, double‐blind, randomised, placebo‐controlled trial; intention‐to‐treat analysis | |
| Participants | Patients with metastatic stage IV breast carcinoma who had been receiving first‐ or second‐line chemotherapy for 4 weeks or less. Mean age: 57 years in the warfarin group and 56 years in the placebo group; metastatic disease: not reported; previous VTE: none in warfarin and 2/159 in placebo. Mean duration of follow‐up: 199 days (SD 126) for warfarin and 188 days (SD 137) for placebo | |
| Interventions | Intervention: warfarin (1 mg daily for 6 weeks and then adjusted to maintain the INR between 1.3 to 1.9) Control: placebo Study treatment began either at the start of chemotherapy or within the next 4 weeks and continued until 1 week after termination of chemotherapy. Median treatment duration: 181 days (SD 123) for warfarin and 166 (SD 139) for placebo |
|
| Outcomes | Primary outcomes: VTE and arterial thrombosis; major and minor bleeding Secondary outcome: survival |
|
| Notes | Funding: study supported by a grant‐in‐aid from the National Cancer Institute of Canada Disclosure of potential conflicts of interest: none disclosed, no COI forms available |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "according to a computer‐generated random arrangement." Comment: adequate method of sequence generation |
| Allocation concealment (selection bias) | Unclear risk | Comment: method of allocation concealment not reported |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Quote: "neither patients nor doctors were aware of treatment allocation" and "All outcome events were reviewed by a central adjudicating committee, unaware of treatment allocation" and "placebo patients took an identical inert tablet" Comment: adequate blinding of participants, physicians, and outcome assessors |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Comment: For effectiveness and safety, 152 out of 154 (98.7%) in the warfarin and 159 out of 161 (98.8%) in the placebo group were analysed. |
| Selective reporting (reporting bias) | Low risk | Comment: All outcomes reported in the methods section were addressed in the results. |
Levine 2012.
| Methods | Randomised, double‐blind, phase II trial; intention‐to‐treat analyses not reported | |
| Participants | Patients receiving either first‐ or second‐line chemotherapy for advanced or metastatic lung, breast, gastrointestinal, bladder, ovarian, or prostate cancer; cancer of unknown origin; myeloma; or selected lymphomas. Median age (years, range): 57 (41 to 67) in apixaban 5 mg, 60 (39 to 76) in 10 mg, 64 (25 to 86) in 20 mg, and 59 (20 to 82) in the placebo group; male, n (%): 15 (46.9), 13 (43.3), 20 (60.6), and 15 (50), respectively; advanced or metastatic: 100%; previous VTE: 0/125 | |
| Interventions | Intervention: factor Xa inhibitor, apixaban (5 mg, 10 mg, or 20 mg once daily oral)
Control: placebo Study treatment was given for 12 weeks beginning within 4 weeks of starting chemotherapy. Median treatment duration for apixaban 5 mg, 10 mg, and 20 mg and placebo: 79.2 (29 to 90) days, 76.0 (16 to 90) days, 73.6 (14 to 92) days, and 69.6 (7 to 91) days, respectively |
|
| Outcomes | Primary outcome: major bleeding or clinically relevant non‐major bleeding Secondary outcomes: VTE, grade III or higher adverse events related to study drug |
|
| Notes | Trials closed prematurely due to slow accrual rate. Funding, quote: "The study was sponsored by Bristol‐Myers Squibb and Pfizer Inc." Disclosure of potential conflicts of interest: No other COI reported, no COI forms available, but 2 of the authors were employees of the sponsor. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomisation was performed centrally by contacting a computerised telephone voice response system provided by Bristol Myers Squibb" Comment: adequate method of sequence generation |
| Allocation concealment (selection bias) | Low risk | Quote: "Randomisation was performed centrally by contacting a computerised telephone voice response system provided by Bristol Myers Squibb" and "BMS generated and kept the randomization schedules." Comment: adequate method of allocation concealment |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Quote: "Double‐blind" study, "treatment groups or all placebo tablets for the placebo treatment group such that the study supplies for subjects in all treatment groups were identical in appearance", and "All bleeding and VTE events were adjudicated by a committee unaware of treatment allocation." Comment: participants, physicians, and outcome assessors blinded |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Comment: for effectiveness and safety, 32 out of 32 (100%) analysed in the 5 mg group; 29 out of 30 (96.7%) analysed in the 10 mg group; 32 out of 33 (97%) analysed in the 20 mg group; and 29 out of 30 (96.7%) analysed in the placebo group. None of these excluded participants received study treatment, and we cannot rule out that their exclusion was associated with the outcome. In addition to these 3 excluded participants, it also remains unclear why the 5 participants (4%) enrolled after the protocol amendment were not considered in the analyses. |
| Selective reporting (reporting bias) | Low risk | Comment: All outcomes reported in the methods section were addressed in the results section. |
Macbeth 2016.
| Methods | The FRAGMATIC trial: an open‐label, multicentre, parallel‐group, superiority, randomised phase III trial. Median follow‐up of 23.1 months (IQR 3.6 to 31.2 months) | |
| Participants | Patients with histopathologic or cytologic diagnosis of primary bronchial carcinoma of any stage and histology (small cell or non‐small cell) within 6 weeks. Median age, years (IQR): LMWH 65 (59 to 71) and control 64 (58 to 71); female, n (%): LMWH 440 (40.0) and control 444 (40.4); metastatic disease, n(%): LMWH 670 (60.9) and control 666 (60.5); previous VTE: not reported | |
| Interventions | Intervention: standard anticancer treatment (including active supportive or palliative care) plus dalteparin (5000 IU subcutaneously once daily) for a maximum of 24 weeks Dalteparin was started as soon as possible and before first definitive anticancer treatment. Control: standard anticancer treatment (including active supportive or palliative care) Use of prophylactic anticoagulant outside of trial (short‐term use, e.g. inpatient thromboprophylaxis, and therapeutic anticoagulation were allowed if clinically indicated according to local guidelines), n (%): LMWH 106 (9.7) Control 88 (8.0) |
|
| Outcomes | Primary outcome: overall survival
Secondary outcomes: VTE‐free survival, bleeding (major and clinically relevant non‐major), metastasis‐free survival, toxic effects, quality of life, dyspnoea, cost‐effectiveness, and cost utility Compliance with dalteparin was assessed by counting empty syringes at follow‐up visits and from the local pharmacy logs. |
|
| Notes | Funding, quote: "Supported by Cancer Research UK Grant No. CR UK/06/007, an educational grant from Pfizer, and the National Institute for Health Research Cancer Network; sponsored by Velindre National Health Service Trust, Cardiff; and coordinated by the Cancer Research UK core‐funded Wales Cancer Trials Unit at Cardiff University" Disclosure of potential conflicts of interest: Some of the authors report conflict of interest. Quote: "The trial did not reach its intended number of events for the primary analysis" |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Eligible patients were randomly assigned by the Wales Cancer Trials Unit in a 1:1 ratio to receive either LMWH or no LMWH, by use of a computer algorithm using the method of minimization and a random element" Comment: adequate method of sequence generation |
| Allocation concealment (selection bias) | Low risk | Quote: "Allocation concealment was by research nurses (who recruited patients) telephoning the Wales Cancer Trials Unit, where randomization and treatment allocation was done by a trial/data manager using a computerized system." Comment: adequate method of allocation concealment |
| Blinding (performance bias and detection bias) All outcomes | High risk | Quote: "The study had an open‐label design" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "All analyses were performed using intention to treat." Comment: For the analysis of the primary outcomes and most of the secondary outcomes, all randomised participants were apparently included in the analysis. For the evaluation of compliance with LMWH, 977 of 1101 participants were assessed. |
| Selective reporting (reporting bias) | Low risk | Comment: All outcomes indicated in the methods are reported in the results of the main or related papers. |
Maraveyas 2012.
| Methods | FRAGEM study: phase IIb RCT; intention‐to‐treat analyses not reported | |
| Participants | Patients with non‐resectable, recurrent, or metastatic pancreatic adenocarcinoma. Median age: 63 years (range 40 to 82); males: 59%; patients with metastatic disease: 54%; previous VTE: 0/123. Median follow‐up time: 19.3 months | |
| Interventions | Intervention: LMWH, dalteparin (200 IU/kg once daily, sc for 4 weeks followed by a stepdown to 150 IU/kg for a further 8 weeks) and gemcitabine Continuing dalteparin prophylaxis beyond 12 weeks was not recommended, but was left to the discretion of the investigator. Control: gemcitabine with no dalteparin |
|
| Outcomes | Primary outcome: reduction of all‐type vascular thromboembolism during the study period. All‐type vascular thromboembolism included DVT, PE, all arterial events (e.g. cerebrovascular accident/myocardial infarction), and all visceral thromboembolic events diagnosed on the basis of clinical symptomatology, post‐mortem, or incidentally. Outcome data kindly provided by the authors: VTE |
|
| Notes | Central venous access devices and inferior vena cava filters were not allowed. Funding: the Hull and East Yorkshire Hospitals National Health Service Trust; Pfizer provided a grant covering the cost of dalteparin; Lilly provided a grant covering the cost of biostatistics. Disclosure of potential conflicts of interest: The lead author has received honoraria and participated on advisory boards for Pfizer. Another author received travel expenses from Pfizer. None of the other authors has any conflicting interests. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Patients were randomised in the facilities of the Postgraduate Medical Institute in Hull with software developed by York University" Allocation and stratification were done through remote telephone "block" randomisation (personal communication). Comment: adequate method of sequence generation |
| Allocation concealment (selection bias) | Low risk | Comment: performed centrally at the Medical Institute in Hull for all of the 7 recruiting sites. Allocation and stratification were done through remote telephone "block" randomisation (personal communication). |
| Blinding (performance bias and detection bias) All outcomes | High risk | Comment: open study (personal communication) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: For effectiveness and safety, 59 out of 60 (98.3%) were analysed in the LMWH group, and 62 out of 63 (98.4%) were analysed in the control group. |
| Selective reporting (reporting bias) | Low risk | Comment: All outcomes reported in the methods section were addressed in the results section. |
Maurer 1997.
| Methods | Multicentre RCT; intention‐to‐treat analyses not reported | |
| Participants | Patients with limited‐stage small cell lung cancer receiving chemotherapy and radiotherapy. Patients 60 years of age or older: 57.6%; males: 64.8%; metastatic disease: none; previous VTE: not reported | |
| Interventions | Intervention: warfarin 10 mg/day for the first 3 days and then at a dose to maintain the prothrombin time between 1.4 and 1.6 times the local institutional control standards Control: no warfarin Warfarin was continued through the complete course of chemotherapy and radiation therapy and stopped 3 weeks after the last cycle of chemotherapy. Warfarin was administered for a median of 112.5 days. |
|
| Outcomes | Primary: overall survival and cancer response to therapy Secondary: failure‐free survival, disease‐free survival, patterns of relapse, toxicity |
|
| Notes | Funding: grants from the National Cancer Institute, Bethesda, MD Disclosure of potential conflicts of interest: not reported, no COI forms available |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Patients were randomized to receive warfarin or no warfarin" Comment: method of sequence generation not reported |
| Allocation concealment (selection bias) | Unclear risk | Quote: "Patients were randomized to receive warfarin or no warfarin" Comment: method of allocation concealment not reported |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Comment: It is not reported whether participants, physicians, and outcome assessors were blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Comment: Table 6 of the study full‐text indicates that not all randomised participants were analysed, but the exact numbers were not reported. |
| Selective reporting (reporting bias) | Unclear risk | Comment: Only the outcomes overall survival and complete tumour response were specified in the methods section. All other outcomes were addressed in the results section only, including the survival analyses at 8 months, 2, 3, and 4 years. Only the 8 months' analyses were reported to be exploratory. |
Mitchell 2003.
| Methods | PARKAA study: multicentre, open, phase II RCT; per‐protocol analysis | |
| Participants | Paediatric patients newly diagnosed with acute lymphoblastic leukaemia treated with L‐asparaginase and a functioning central venous line placed within 2 weeks of initiating induction chemotherapy. Mean age: 3.8 years in antithrombin and 5.9 years in control; female, n (%): 10 (40) in antithrombin and 23 (38.3) in control; previous VTE: not reported | |
| Interventions | Intervention: Thrombate III, a sterile, lyophilised preparation of purified human antithrombin manufactured and supplied by Bayer Corporation, USA. Antithrombin was infused once weekly for 4 weeks to increase plasma concentrations of antithrombin to approximately 3.0 U/mL but no more than 4.0 units/mL. Control: standard care |
|
| Outcomes | Primary outcomes: clinically symptomatic or incidental thrombotic event in any location; major and minor bleeding Secondary outcomes: surrogate outcome for thrombotic events by measuring markers of thrombin generation |
|
| Notes | Participants did receive small amounts of UFH for prophylaxis of central venous line blockage either by continuous infusion (1 to 3 U/mL) or intermittent flushes (50 to 100 U/mL up to 4 times per day) according to local standard of care. Funding: The study was supported by a grant from the Canadian Institutes of Health Research and Bayer Inc. Disclosure of potential conflicts of interest: not reported, no COI forms available |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomisation was performed by the pharmacist‐on‐call using a computer generated random number list." Comment: adequate method of sequence generation |
| Allocation concealment (selection bias) | Low risk | Quote: "Investigators at participating centres were blinded to the randomisation code and unaware of patient treatment allocation until after patients had been randomised." Comment: adequate method of allocation concealment |
| Blinding (performance bias and detection bias) All outcomes | High risk | Quote: "The PARKAA study was an open, randomised, multi‐centre extended phase II clinical study" and "The thrombotic events outcomes were adjudicated centrally by committees consisting of physicians with appropriate expertise, who were not involved with study patients’ care and were blinded to treatment groups" Comment: Participants and physicians were not blinded, whereas outcome assessors were. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Comment: For effectiveness and safety, 25 out of 37 (67.6%) were analysed in the antithrombin group, and 60 out of 72 (83.3%) were analysed in the control group. |
| Selective reporting (reporting bias) | Low risk | Comment: All outcomes reported in the methods section were addressed in the results section. |
Palumbo 2011.
| Methods | Randomised, open‐label, multicentre study; modified intention‐to‐treat analysis, including participant receiving at least 1 study dose | |
| Participants | Patients with previously untreated myeloma who received thalidomide‐containing regimens and had no clinical indication or contraindication for a specific antiplatelet or anticoagulant therapy. Median age: aspirin 61 years (55 to 66), warfarin 60 years (54 to 66), heparin 62 years (55 to 66); male, n (%): 117 (53), 115 (52), and 130 (59), respectively; previous VTE: none. Median follow‐up time: 24.9 months | |
| Interventions | Intevention 1: aspirin (100 mg/d) Intervention 2: low‐dose warfarin (1.25 mg/d) Intervention 3: LMWH (enoxaparin 40 mg/d) Prophylaxis was administered during the 3 cycles of induction therapy in participants ≤ 65 years and during the first 6 cycles of induction therapy in participants > 65 years. Median treatment duration: 2.6 months for aspirin, 2.4 months for low‐dose warfarin, and 2.6 months for LMWH |
|
| Outcomes | Primary outcomes: a composite measure of a first episode of objectively confirmed symptomatic DVT, PE, arterial thrombosis, acute myocardial infarction or stroke, or sudden, otherwise‐unexplained death during the first 6 months from random assignment Secondary outcomes: each component of the composite primary endpoint; long‐term cumulative incidence of the primary endpoint; major and minor bleeding events; any toxicity that required interruption of study prophylaxis |
|
| Notes | The trial sampled participants from 2 distinct RCTs, of which participants who received thalidomide‐based regimens were eligible to the substudy randomising antithrombotic prophylaxis treatments. Karnofsky performance status < 70%: aspirin 25%, warfarin 29%, heparin 30% Funding: none reported Disclosure of potential conflicts of interest: Several authors reported paid consultant or advisory roles, honoraria, and research funds that were relevant to the subject matter under consideration in their trial report. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "A simple random assignment sequence was generated by a centralized computer" Comment: adequate method of sequence generation |
| Allocation concealment (selection bias) | Low risk | Quote: "After registration in a centralized database through the Internet and validation of eligibility, patients were randomly allocated to treatments using an automated assignment procedure concealed to the investigators" Comment: adequate method of allocation concealment |
| Blinding (performance bias and detection bias) All outcomes | High risk | Quote: "open‐label" Comment: This was an open‐label study. It is not reported whether outcomes were assessed blindly. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Comment: For effectiveness and safety, 220 out of 224 (98.2%) in the aspirin group, 220 out of 222 (99.1%) in the warfarin group, and 219 out of 221 (99.1%) in the LMWH group were analysed. In addition, 1 participant was not randomised by "clinician mistake". |
| Selective reporting (reporting bias) | High risk | Comment: The outcome "any toxicity that required interruption of study prophylaxis" was not reported in the final report. |
Pelzer 2015.
| Methods | CONKO 004 trial: open‐label, multicentre RCT; intention‐to‐treat and per‐protocol analyses | |
| Participants | Outpatients with histologically confirmed advanced pancreatic cancer treated with first‐line chemotherapy. Age, median (range): enoxaparin 62 (32 to 81) and control 63 (27 to 83); female, n (%): enoxaparin 69 (43) and control 58 (38); metastatic disease, n (%): enoxaparin 119 (74) and control 118 (78); previous VTE: not reported. Median follow‐up: 30.4 weeks | |
| Interventions | Intervention: LMWH, enoxaparin (1 mg/kg once daily) for 3 months started simultaneously to palliative systemic chemotherapy Control: no enoxaparin Quote: "After 3 months of initial enoxaparin use at half the therapeutic dosage (time point of primary end point), treatment was continued with a fixed dose of 40 mg daily until disease progression" |
|
| Outcomes | Primary outcome: symptomatic VTEs within 3 months after random assignment Secondary outcomes: progression‐free survival; overall survival; overall symptomatic VTE after 6, 9, and 12 months; major bleeding Additional outcomes reported in related references: incidental DVT during months 6, 9, and 12; toxicity of the therapeutic regimen; time to cancer progression; remission at 3, 6, 9, and 12 months; quality of life |
|
| Notes | Funding, quote: "Supported by Charité–Forschungsförderung, Arbeitsgemeinschaft Internistische Onkologie, Deutsche Krebsgesellschaft, Amgen, Eli Lilly, and sanofi‐aventis, which provided enoxaparin free of charge." Disclosure of potential conflicts of interest: Quote: "Employment or Leadership Position: None Consultant or Advisory Role: Helmut Oettle, Celgene (C), Eli Lilly (C), Fresenius (C); Hanno Riess, sanofi‐aventis (C) Stock Ownership: None Honoraria: Helmut Oettle, Celgene; Hanno Riess, sanofi‐aventis, Roche, Amgen, Bayer, Novartis, Eli Lilly Research Funding: Helmut Oettle, Celgene, Eli Lilly Expert Testimony: None Patents, Royalties, and Licenses: None Other Remuneration: Uwe Pelzer, sanofi‐aventis, Roche, Eli Lilly, Amgen; Jens M. Stieler, sanofi‐aventis, Roche, Eli Lilly, Amgen" |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "computer‐generated random numbers generated at the study coordination center at the Charité–Universitätsmedizin Berlin" Comment: adequate method of random sequence generation |
| Allocation concealment (selection bias) | Low risk | Quote: "computer‐generated random numbers generated at the study coordination center at the Charité–Universitätsmedizin Berlin" Comment: adequate method of allocation concealment |
| Blinding (performance bias and detection bias) All outcomes | High risk | Quote: "All symptomatic VTEs and major hemorrhages were documented using the serious adverse event form, centrally reviewed and evaluated by an independent, blinded event review board" Comment: open‐label study, with blinded outcome assessment |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: All randomised participants were included in the analysis. |
| Selective reporting (reporting bias) | High risk | Comment: Some of the outcomes indicated in the related reports or in the main article (quality of life) are not reported. |
Perry 2010.
| Methods | PRODIGE study: phase III, randomised, placebo‐controlled trial; intention‐to‐treat analysis | |
| Participants | Patients over 18 years of age with newly diagnosed, pathologically confirmed WHO grade 3 or grade 4 glioma. Mean age: 57 years (30 to 81) in the dalteparin group and 55 years (26 to 77) in the placebo group; male, n (%): 61 (62) and 50 (57), respectively; previous VTE: none | |
| Interventions | Intervention: LMWH, dalteparin (5000 IU sc, once daily) Control: placebo Study treatment was given for 6 months starting within the first month after surgery. Participants were allowed to continue study medication for 12 months. Median treatment duration: 183 days for LMWH and 157 days for placebo |
|
| Outcomes | Primary outcomes: objectively documented symptomatic DVT or PE occurring during the 6 months postrandomisation Secondary outcomes: major and all bleeding, quality of life, cognition assessments, and death |
|
| Notes | Funding: Pfizer Inc, Ontario Clinical Oncology Group, Crolla Chair in Brain Tumour Research Disclosure of potential conflicts of interest: The lead author disclosed research support (and funding) by Pfizer. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "using a computer‐generated randomization list" Comment: adequate method of sequence generation |
| Allocation concealment (selection bias) | Low risk | Quote: "Consenting patients were randomized by contacting the Ontario Clinical Oncology Group (OCOG) Coordinating and Methods Centre at the Henderson Research Centre" Comment: adequate method of allocation concealment |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Quote: "In our study, investigators, patients and outcome assessors were blinded to treatment allocation. In addition, VTE and bleeding outcomes were adjudicated by a central committee unaware of treatment assignment." Comment: Participants, physicians, and outcome assessors were blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: All randomised participants were included in the analysis. |
| Selective reporting (reporting bias) | High risk | Comment: The outcomes quality of life and cognition assessment were mentioned in the methods but not reported in the results. |
Sideras 2006.
| Methods | Multicentre, placebo‐controlled randomised study; type of analyses not reported | |
| Participants | Patients with advanced breast cancer who had failed first‐line chemotherapy; advanced prostate cancer who had failed primary hormonal therapy; advanced lung cancer; or advanced colorectal cancer. Median age for blinded LMWH: 64.5 years; placebo: 63.5 years; unblinded LMWH: 68.5 years; standard care: 70.5 years | |
| Interventions |
First part of the study, double‐blinded (52 participants): LMWH, dalteparin (5000 IU sc, once daily) plus standard clinical care Control: placebo (saline injections) plus standard clinical care Second part of the study, open (86 participants): LMWH, dalteparin (5000 IU sc, once daily) plus standard clinical care Control: standard clinical care alone Duration: 18 weeks or until disease progression |
|
| Outcomes | Primary outcome: overall survival Secondary outcomes: toxic effects, incidence of thromboembolic events, changes in quality of life |
|
| Notes | Funding: Public Health Services grants from the National Cancer Institute, Department of Health and Human Services Disclosure of potential conflicts of interest: not reported and no COI forms available |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: method of random sequence generation not reported |
| Allocation concealment (selection bias) | Low risk | Quote: "The randomization processes applied were handled through the North Central Cancer Treatment Group (NCCTG) Randomization Office." Comment: adequate method of allocation concealment |
| Blinding (performance bias and detection bias) All outcomes | High risk | Comment: The study used a double‐blinded design in the first part of the trial, and an open‐label design in the second part. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Comment: For effectiveness and safety, 68 out of 69 participants (98.6%) were analysed in the LMWH group, and 70 out of 72 (97.2%) were analysed in the placebo group. |
| Selective reporting (reporting bias) | Low risk | Comment: All outcomes reported in the methods section were addressed in the results or discussion sections. |
Vadhan‐Raj 2013.
| Methods | Randomised, open‐label, parallel‐group trial | |
| Participants | Patients 18 years or older with a diagnosis of advanced stage (unresectable or metastatic) adenocarcinoma of the pancreas planning to initiate systemic chemotherapy within 2 weeks, ECOG performance status 0 to 2, adequate renal function (creatinine clearance of > 50 mL/min). Median age 52 years (range 36 to 77 years); gender: 41 males and 34 females; previous VTE and metastatic disease: not reported | |
| Interventions | Intervention: LMWH, dalteparin (5000 IU sc, once daily) for 16 weeks during chemotherapy Control: chemotherapy alone |
|
| Outcomes | Primary outcome: venous thromboembolic events during 16 weeks of treatment Other outcomes mentioned in the abstract: adverse events, clinically significant bleeding, overall survival |
|
| Notes | Funding: not reported Disclosure of potential conflicts of interest: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "were randomized 1:1 to dalteparin vs control arms" Comment: method of sequence generation not reported |
| Allocation concealment (selection bias) | Unclear risk | Quote: "were randomized 1:1 to dalteparin vs control arms" Comment: method of allocation concealment not reported |
| Blinding (performance bias and detection bias) All outcomes | High risk | Comment: open‐label study. It is not reported in the abstract if outcome assessors were blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "All 75 patients were evaluable for response in an intent‐to‐treat analysis" Comment: All randomised participants were included in the analysis. |
| Selective reporting (reporting bias) | Unclear risk | Comment: It is not clear from the abstract if all outcomes are reported. |
van Doormaal 2011.
| Methods | INPACT study: multicentre, open‐label RCT; intention‐to‐treat analyses for mortality | |
| Participants | Patients with non–small cell lung cancer (stage IIIB), hormone‐refractory prostate cancer, or locally advanced pancreatic cancer. Age, mean (SD): 65 (10) years in the nadroparin group and 65 (9.8) years in the no‐nadroparin group; male, n (%): 197 (81) in nadroparin and 206 (80) in no‐nadroparin; metastatic disease in prostate cancer, n (%): 73 (73.7) in nadroparin and 85 (87.6) in no‐nadroparin; previous VTE: none. Median duration of follow‐up: 10.4 months | |
| Interventions | Intervention: LMWH, nadroparin in addition to standard anticancer treatment Subcutaneous nadroparin was administered for 6 weeks (2 weeks at therapeutic dose and 4 weeks at half therapeutic dose). Participants were eligible to receive additional cycles of nadroparin (2 weeks at therapeutic dose and 4 weeks of washout period) for a maximum of 6 cycles. Mean duration of treatment: 12.6 weeks Control: standard anticancer treatment |
|
| Outcomes | Primary efficacy outcome: all‐cause mortality Primary safety outcome: major bleeding Secondary efficacy outcomes: time to disease progression, clinically relevant non‐major bleeding, VTE, arterial thromboembolic events |
|
| Notes | Funding: The study was supported by a grant from GlaxoSmithKline (Paris, France). Disclosure of potential conflicts of interest: 2 authors reported consultant or advisory roles, honoraria, and research funds that were relevant to the subject matter under consideration in their trial report. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Allocation of treatment proceeded centrally by using an interactive‐voice response system" Comment: adequate method of sequence generation |
| Allocation concealment (selection bias) | Low risk | Quote: "Allocation of treatment proceeded centrally by using an interactive‐voice response system" Comment: adequate method of allocation concealment |
| Blinding (performance bias and detection bias) All outcomes | High risk | Quote: "all study outcomes were adjudicated by an independent, blinded committee" Comment: open study with blinded outcome assessors |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Comment: For effectiveness and safety, the overall percentage of participants enrolled and subsequently excluded from the analysis was 2.2% (11/503). |
| Selective reporting (reporting bias) | Low risk | Comment: All outcomes reported in the methods section were addressed in the results or discussion section. |
Zacharski 1981.
| Methods | Veterans Administration Study No. 75: multicentre RCT, type of analyses not reported | |
| Participants | Patients with small cell lung carcinoma treated with chemotherapy and radiation therapy. Males: 100%. Extensive cancer: 52% warfarin and 48% control group; previous VTE: not reported | |
| Interventions | Intervention: warfarin at doses to prolong the prothrombin time to approximately 2 times the control value Control: no warfarin The median duration of warfarin administration was 27 weeks. |
|
| Outcomes | Primary efficacy outcomes: survival and cancer response to treatment | |
| Notes | Funding: VA Cooperative Studies Program Disclosure of potential conflicts of interest: not reported, no COI forms available |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "subjected to computer randomization" Comment: adequate method of sequence generation |
| Allocation concealment (selection bias) | Low risk | Quote: "subjected to computer randomization" Comment: adequate method of allocation concealment |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Comment: It is not reported whether participants, physicians, and outcome assessors were blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "No patient has been lost to follow‐up." Comment: All enrolled participants were included in the analysis. |
| Selective reporting (reporting bias) | Unclear risk | Comment: Bleeding was addressed in the results section, but not mentioned in the methods section. |
Zwicker 2013.
| Methods | MicroTEC study: randomised, multicentre phase II study; use of intention‐to‐treat analyses reported | |
| Participants | Patients with histologically confirmed advanced‐stage malignancy for which standard curative therapies did not exist. Eligible malignancies included: adenocarcinoma of the pancreas (locally advanced or metastatic), colorectal (stage IV), non‐small cell lung cancer (stage III or IV), relapsed or stage IV ovarian, or surgically unresectable or metastatic gastric adenocarcinoma. Median age was 68.1 years (46.6 to 80.1) in the LMWH group and 67.5 years (28.8 to 78.7) in the observation group. Male sex: 61% and 46%, respectively. Overall, 78.8% of the participants had metastatic disease; previous VTE: none | |
| Interventions | Intervention: LMWH, enoxaparin (40 mg sc, once daily) Control: observation Treatment was given for 2 months. |
|
| Outcomes | Primary efficacy outcome: cumulative incidence of VTE (i.e. any symptomatic proximal or distal lower extremity DVT, incidental proximal DVT, symptomatic PE, or fatal PE) at 2 months Primary safety outcome: major bleeding Secondary: toxicity and survival |
|
| Notes | Funding, quote: "the study was supported by grants from the National Institutes of Health, K23 HL84052 (JIZ) and R01 HL095084 (BF), as well as a research grant from Sanofi" Disclosure of potential conflicts of interest: 1 author has served on steering committees for Sanofi, and another has received research funds and served on advisory boards for Sanofi and Eisai. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "were randomized (2:1) to enoxaparin 40 mg subcutaneously once daily or observation." Comment: method of sequence generation not reported |
| Allocation concealment (selection bias) | Unclear risk | Quote: "Study coordination, randomization, and monitoring were performed by the Quality Assurance Office for Clinical Trials (QACT) at Dana Farber/Harvard Cancer Center." Comment: method of allocation concealment not clearly specified |
| Blinding (performance bias and detection bias) All outcomes | High risk | Comment: Both the treating physicians and participants in the observation arms were blinded to microparticle status. However, participants in the control group were only observed; the use of placebo, blinding method, or an independent and blinded adjudication committee was not reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: All randomised participants were included in the analysis. 4 of the 70 participants initially enrolled were excluded prior to randomisation. |
| Selective reporting (reporting bias) | High risk | Comment: The outcome toxicity was not reported in the results section. |
COI: conflict of interest CT: chemotherapy DVT: deep vein thrombosis ECOG: Eastern Cooperative Oncology Group INR: international normalised ratio IQR: interquartile range LMWH: low molecular weight heparin PE: pulmonary embolism RCT: randomised controlled trial sc: subcutaneous SD: standard deviation UFH: unfractionated heparin uLMWH: ultra‐low molecular weight heparin VTE: venous thromboembolism WHO: World Health Organization
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Baz 2005 | Not an RCT |
| Bergqvist 1983 | Perioperative thromboprophylaxis |
| Bocharov 2011 | Not an RCT and study includes surgical patients |
| Eichinger 2008 | Inadequate population: hospitalised cancer patients |
| Gercor 2013 | Study terminated. No published data available and results not reported in ClinicalTrials.gov |
| Haas 2011 | Inadequate population: hospitalised cancer patients |
| Heilmann 1995 | Perioperative thromboprophylaxis |
| Hills 1972 | Perioperative thromboprophylaxis |
| Kessler 2011 | Not an RCT |
| Kwaan 2007 | Prophylaxis for catheter‐related thrombosis |
| Levin 2008 | Study was terminated early because of a drug supply issue. Results of a single participant are posted (accessed at clinicaltrials.gov/ct2/show/results/NCT00790452 on 11 December 2012). |
| Macintyre 1974 | Perioperative thromboprophylaxis |
| Maxwell 2000 | Perioperative thromboprophylaxis |
| Meister 2008 | Not an RCT |
| Minnema 2004 | Not an RCT |
| Niesvizky 2007 | Inadequate type of intervention: antiplatelet agent versus placebo |
| Pandya 2002 | Study was terminated early, and no results were posted on ClinicalTrials.gov (accessed at clinicaltrials.gov/ct2/show/NCT00031837 on 13 June 2013). |
| Paydas 2008 | Not an RCT |
| Poniewierski 1987 | Inadequate population: hospitalised cancer patients |
| Rajan 1995 | Inadequate outcomes |
| Sideras 2007 | Perioperative thromboprophylaxis |
| Weber 2008 | Inadequate population: hospitalised cancer patients |
| Welti 1981 | Perioperative thromboprophylaxis |
| Zangari 2003 | Not an RCT |
RCT: randomised controlled trial
Characteristics of studies awaiting assessment [ordered by study ID]
Ciftci 2012.
| Methods | Single‐centre, randomised study |
| Participants | Patients with lung cancer |
| Interventions | Intervention: warfarin in addition to standard anticancer treatment. Warfarin was given orally for 6 months starting on day 1 of chemotherapy at a dose of 5 mg/d to achieve a target international normalised ratio of 1.5 to 2.5. Control: standard anticancer treatment |
| Outcomes | No clear distinction between primary and secondary outcomes. Outcomes reported in the abstract: overall median survival, response rates (complete + partial), bleeding |
| Notes |
NCT00771563.
| Methods | Open‐label RCT |
| Participants | Patients with locally advanced or metastatic non‐small cell lung cancer (stage IIIB or IV) who were not candidates for radical combined‐modality treatments or high‐dose radiation therapy |
| Interventions | Intervention: chemotherapy (cisplatin + docetaxel) and enoxaparin 1 mg/kg/day sc Control: chemotherapy (cisplatin + docetaxel) |
| Outcomes | Primary outcome: progression‐free survival Secondary outcomes: symptom control evaluated with the Lung Cancer Symptoms Scale, overall survival, best overall response, incidence of total documented thromboembolic and haemorrhagic events, overall safety and tolerability |
| Notes | ClinicalTrials.gov identifier: NCT00771563 |
Salat 1990.
| Methods | Prospective RCT |
| Participants | Patients (n = 80) with malignant diseases |
| Interventions | Intervention: unfractionated heparin (2 x 7500 IU/mL) Control: low molecular weight heparin, dalteparin (5000 IU sc, once daily) |
| Outcomes | Thrombosis and haemorrhagic complications |
| Notes |
RCT: randomised controlled trial sc: subcutaneous
Characteristics of ongoing studies [ordered by study ID]
NCT00662688.
| Trial name or title | Chemotherapy with or without preventive anticoagulation for metastatic cancer of the pancreas |
| Methods | Randomised, multicentre study. Methods of randomisation and allocation concealment unclear |
| Participants | Patients with histologically confirmed adenocarcinoma of the pancreas (metastatic disease, not amenable to treatment, no localised or locally advanced disease) receiving treatment with different combinations of gemcitabine and capecitabine |
| Interventions | Arm 1A: gemcitabine hydrochloride IV over 150 minutes on days 1 and 15 Arm 1B: gemcitabine hydrochloride as in arm 1A and LMWH, dalteparin sc on day 1 Arm 2A: gemcitabine hydrochloride IV over 30 minutes on days 1, 8, and 15 and oral capecitabine every 12 hours on days 1 to 21 Arm 2B: gemcitabine hydrochloride and capecitabine as in arm 2A and LMWH, dalteparin sc as in arm 1B Treatment is repeated every 28 days in the absence of disease progression or unacceptable toxicity. |
| Outcomes | Primary outcome measures: thromboembolic events Secondary outcome measures: thromboembolic‐related survival, progression‐free survival, overall survival, time to response of tumour, tolerance of regimens |
| Starting date | October 2007 |
| Contact information | Chibauldel B |
| Notes |
NCT00662688 Note: The study status in ClinicalTrials.gov is "terminated". |
NCT00717938.
| Trial name or title | A randomized phase III study of standard treatment +/‐ enoxaparin in small cell lung cancer |
| Methods | Open‐label RCT |
| Participants | Patients with histologically or cytologically verified small cell lung cancer, all stages |
| Interventions | Intervention: cisplatinum or carboplatin and e.g. etoposide + enoxaparin Control: cisplatinum or carboplatin and e.g. etoposide |
| Outcomes | Primary outcome: overall survival Secondary outcome: toxicity |
| Starting date | June 2008 |
| Contact information | Lars Ek, lars.ek@skane.se |
| Notes | ClinicalTrials.gov identifier: NCT00717938 |
NCT00718354.
| Trial name or title | Randomized, phase III‐b, multi‐centre, open‐label, parallel study of enoxaparin (low molecular weight heparin) given concomitantly with chemotherapy vs chemotherapy alone in patients with inoperable gastric and gastro‐oesophageal cancer |
| Methods | Randomised, open‐label, multicentre study. Methods of randomisation and allocation concealment unclear |
| Participants | Patients with inoperable (locally advanced) or metastatic newly diagnosed gastric or gastro‐oesophageal cancer |
| Interventions | Intervention: LMWH, enoxaparin (1 mg/kg sc once daily) in addition to standard chemotherapy up to 6 months Control: standard chemotherapy (up to 6 cycles) |
| Outcomes | Primary outcome measures: event‐free survival (composite endpoint of overall survival plus free of symptomatic VTE) Secondary outcome measures: incidence of symptomatic VTE, overall survival, major and minor bleeding during chemotherapy and/or up to 30 days after last dose is provided, serious adverse events, all reported adverse events, HIT |
| Starting date | July 2008 |
| Contact information | Maganji JM, mmaganji@tri‐london.ac.uk |
| Notes |
NCT00718354 Note: Study status in ClinicalTrials.gov is "complete". |
NCT02048865.
| Trial name or title | Apixaban for the prevention of venous thromboembolism in high‐risk ambulatory cancer patients: a randomized placebo‐controlled, double‐blind clinical trial |
| Methods | Double‐blind (participant, caregiver, investigator, outcomes assessor), parallel‐assignment RCT |
| Participants | Patients with a newly diagnosed cancer site or progression of the malignant disease after complete or partial remission who are initiating a new course of chemotherapy with a minimum intent of 3 months' therapy and who have a VTE risk stratification score of ≥ 2, according to the scoring method |
| Interventions | Intevention: apixaban 2.5 mg twice daily for 6 months Control: placebo drug |
| Outcomes | Primary outcome: symptomatic or incidental VTE (DVT or PE, or both) Secondary outcomes: rate of adverse events, clinical overt bleeding (major and minor bleeding), and death within the study period |
| Starting date | January 2014 |
| Contact information | Marc Carrier, mcarrier@toh.on.ca |
| Notes | ClinicalTrials.gov identifier: NCT02048865 |
NCT02285738.
| Trial name or title | Anti‐platelet and statin therapy to prevent cancer‐associated thrombosis: a pilot study |
| Methods | Open‐label, parallel‐assignment RCT |
| Participants | Patients with a histologic diagnosis of malignancy of a solid organ or lymphoma who have a VTE risk score of 1 or higher and will be initiating a new systemic chemotherapy regimen |
| Interventions | Intervention 1: aspirin Intervention 2: simvastatin Control: observation |
| Outcomes | Primary outcome: change in average sP‐selectin levels Secondary outcomes: major bleeding complications or clinically significant non‐bleeding complications, change in circulating biomarkers, thrombotic events including venus thrombosis, pulmonary embolism, visceral vein thrombosis as well as arterial thromboembolic events including stroke, myocardial infarction, or arterial embolism |
| Starting date | December 2014 |
| Contact information | |
| Notes | ClinicalTrials.gov identifier: NCT02285738 |
NCT02555878.
| Trial name or title | Efficacy and safety of rivaroxaban prophylaxis compared with placebo in ambulatory cancer patients initiating systemic cancer therapy and at high risk for venous thromboembolism |
| Methods | Multicentre, randomised, double‐blind (participant, caregiver, investigator), placebo‐controlled, parallel‐group superiority study |
| Participants | Patients with histologically confirmed solid malignancy including but not limited to: pancreas, lung, stomach, colon, rectum, bladder, breast, ovary, renal, or lymphoma (haematologic), with locally advanced or metastatic disease who have a Khorana thromboembolic risk score ≥ 2 |
| Interventions | Intervention: rivaroxaban 10 mg tablet orally once daily for 180 days Control: placebo |
| Outcomes | Primary efficacy outcome: symptomatic and incidental lower extremity proximal DVT, symptomatic upper extremity DVT, symptomatic non‐fatal PE, incidental PE, VTE‐related death Primary safety outcome: major bleeding Secondary outcomes: symptomatic VTE and VTE‐related deaths, all‐cause mortality, clinically relevant non‐major bleeding, minor bleeding, any bleeding adverse events, and serious adverse events |
| Starting date | September 2015 |
| Contact information | Janssen Research & Development, LLC Clinical Trial |
| Notes | ClinicalTrials.gov identifier: NCT02555878 |
DVT: deep vein thrombosis HIT: heparin‐induced thrombocytopenia IV: intravenous LMWH: low molecular weight heparin PE: pulmonary embolism RCT: randomised controlled trial sc: subcutaneous VTE: venous thromboembolism
Differences between protocol and review
In this update, we added clinically relevant bleeding to the safety outcomes. Clinically relevant bleeding, which is the composite of major and clinically relevant non‐major bleeding, has a significant impact on cancer patients' morbidity and has been reported more consistently in recent studies.
The protocol specified that we would evaluate heterogeneity in results between trials with the I2 statistic (Higgins 2003; Rücker 2008). However, we added the variance estimate Tau2 to indicate and interpret heterogeneity, as currently advised by the Cochrane Handbook for Systematic reviews of Interventions (Higgins 2011).
For the comparison of LMWH versus no thromboprophylaxis, we could not perform stratified analyses of the main outcomes by age, stage of cancer (metastatic versus non‐metastatic), and differences in the use of co‐interventions in the trial groups due to poor reporting or lack of contrast (age). Reported mean age at study entry was 65 years or younger in all studies on LMWH except for Zwicker 2013, which included participants with a mean age above 65. Although we were unable to analyse dosage as a continuous variable, we could stratify the analyses according to trials using prophylactic dosage versus those using other (higher than prophylactic) dosages. In addition, we could not stratify by trial size for the outcome symptomatic VTE, as none of the trials reporting this outcome was considered large. In the previous versions of this review, we defined large trials as those randomising at least 1450 participants. This number was informed by a sample size calculation, assuming a symptomatic VTE rate of 2.7% in the LMWH group and 5.8% in the non‐active control group, a power of 80%, and a two‐sided alpha of 0.05. In this version of the review, we used a slightly lower threshold of 1360 to define large trials, using the event rate of 7.1% as suggested by Khorana 2008 for the control event rate (see Methods). The change in threshold did not affect the classification in large versus small trials. We could not use the uni‐variable random‐effects meta‐regression model by dosage of intervention.
We planned to perform meta‐regression on both treatment duration and follow‐up duration. The treatment duration equaled the follow‐up duration in all studies except the one by Pelzer and colleagues (Pelzer 2015), which added one month of follow‐up after the end of treatment. We therefore only analysed the effect of treatment duration on major bleeding and symptomatic VTE. In all other comparisons, no exploration of the effects of participant or trial characteristics on symptomatic VTE or major bleeding could be done due to the low number of studies identified.
Contributions of authors
Study conception: Di Nisio Acquisition of data: Di Nisio, Rutjes Analysis and interpretation of data: Di Nisio, Porreca, Candeloro, De Tursi, Russi, Rutjes Drafting of the manuscript: Di Nisio, Rutjes Critical revision of the manuscript for important intellectual content: Di Nisio, Porreca, Candeloro, De Tursi, Russi, Rutjes Statistical analysis: Di Nisio, Rutjes Grading of the evidence: Di Nisio, Rutjes
Sources of support
Internal sources
-
None, Italy.
No funding source available
-
None, Netherlands.
No funding source available
External sources
-
None, Italy.
No funding source available
-
None, Netherlands.
No funding source available
-
Chief Scientist Office, Scottish Government Health Directorates, The Scottish Government, UK.
The Cochrane Vascular editorial base is supported by the Chief Scientist Office.
Declarations of interest
MDN: I have received consultancy fees from Bayer, Grifols, and Daiichi Sankyo not related to the present review. EP: none known MC: none known MDT: none known IR: none known AWSR: none known
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Agnelli 2009 {published data only}
- Agnelli G, Gussoni G, Bianchini C, Verso M, Mandala M, Cavanna L, et al. Nadroparin for the prevention of thromboembolic events in ambulatory patients with metastatic or locally advanced solid cancer receiving chemotherapy: a randomised, placebo‐controlled, double‐blind study. Lancet Oncology 2009;10(10):943‐9. [DOI] [PubMed] [Google Scholar]
- Barni S, Bonizzoni E, Verso M, Gussoni G, Petrelli F, Perrone T, et al. The effect of low‐molecular‐weight heparin in cancer patients: the mirror image of survival?. Blood 2014;124:155‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barni S, Labianca R, Agnelli G, Bonizzoni E, Mandalà M, Verso M, et al. Thromboembolic risk related to type of chemotherapy and efficacy of nadroparin in cancer outpatients with metastatic or locally advanced cancer. Supportive Care in Cancer 2011;19 (Suppl 2):S206. [Google Scholar]
- Barni S, Labianca R, Agnelli G, Bonizzoni E, Verso M, Mandala M, et al. Chemotherapy‐associated thromboembolic risk in cancer outpatients and effect of nadroparin thromboprophylaxis: results of a retrospective analysis of the PROTECHT study. Journal of Translational Medicine 2011;9:179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barni S, Petrelli F, Bonizzoni E, Verso M, Gussoni G, Perrone T, et al. Survival benefit with low‐molecular‐weight heparin in patients with advanced solid tumors: a post hoc analysis of PROTECHT Trial. Journal of Clinical Oncology 2014;32 (Suppl):abstract 9640. [Google Scholar]
Agnelli 2012 {published data only}
- Agnelli G, George D, Fisher WD, Kakkar AK, Lassen MR, Mismetti P, et al. Ultra‐low‐molecular‐weight heparin (ULMWH) semuloparin for prevention of venous thromboembolism (VTE) in cancer patients receiving chemotherapy: consistent beneficial effect across cancer stage and location subgroups. European Journal of Cancer 2011;47:S222. [Google Scholar]
- Agnelli G, George DJ, Kakkar AK, Fisher W, Lassen MR, Mismetti P, et al. for the SAVE‐ONCO Investigators. Semuloparin for thromboprophylaxis in patients receiving chemotherapy for cancer. New England Journal of Medicine 2012;366(7):601‐9. [DOI] [PubMed] [Google Scholar]
- Hull RD. Semuloparin reduced venous thromboembolism in patients receiving chemotherapy for cancer. Annals of Internal Medicine 2012;156:JC6‐5. [DOI] [PubMed] [Google Scholar]
- NCT00694382. A multinational, randomized, double blind, placebo‐controlled study to evaluate the efficacy and safety of AVE5026 in the prevention of venous thromboembolism (VTE) in cancer patients at high risk for VTE and who are undergoing chemotherapy. clinicaltrials.gov/show/NCT00694382 (first received 7 May 2008).
Altinbas 2004 {published data only}
- Altinbas M, Coskun HS, Er O, Ozkan M, Eser B, Unal A, et al. A randomized clinical trial of combination chemotherapy with and without low‐molecular‐weight heparin in small cell lung cancer. Journal of Thrombosis and Haemostasis 2004;2(8):1266‐71. [DOI] [PubMed] [Google Scholar]
Chahinian 1989 {published data only}
- Chahinian AP, Propert KJ, Ware JH, Zimmer B, Perry MC, Hirsh V, et al. A randomized trial of anticoagulation with warfarin and of alternating chemotherapy in extensive small‐cell lung cancer by the Cancer and Leukemia Group B. Journal of Clinical Oncology 1989;7(8):993‐1002. [DOI] [PubMed] [Google Scholar]
Elit 2012 {published data only}
- Elit LM, Lee AY, Parpia S, Swystun LL, Liaw PC, Hoskins P, et al. Dalteparin low molecular weight heparin (LMWH) in ovarian cancer: a phase II randomized study. Thrombosis Research 2012;130:894‐900. [DOI] [PubMed] [Google Scholar]
- NCT00239980. A phase II randomized study of Fragmin in ovarian cancer: utility on survival (FOCUS). clinicaltrials.gov/show/NCT00239980 (first received 13 October 2005).
Haas 2012 {published data only}
- Freund M, Kakkar AK, Haas S, Heilmann L, von‐Tempelhoff GF, Brom J, et al. A randomized trial of the low molecular weight of heparin certoparin against placebo in the long‐term prevention of venous thromboembolism in patients with metastatic breast cancer. Blood 2003;102(11 (Pt1)):210a. [Google Scholar]
- Haas SK, Freund M, Heigener D, Heilmann L, Kemkes‐Matthes B, Tempelhoff GF, TOPIC Investigators. Low‐molecular‐weight heparin versus placebo for the prevention of venous thromboembolism in metastatic breast cancer or stage III/IV lung cancer. Clinical and Applied Thrombosis Hemostasis 2012;18(2):159‐65. [DOI] [PubMed] [Google Scholar]
- Haas SK, Kakkar AK, Kemkes‐Matthes B, Freund M, Gatzemeier U, Heilmann L, et al. Prevention of venous thromboembolism with low‐molecular‐weight heparin in patients with metastatic breast or lung cancer ‐ Results of the TOPIC studies. Journal of Thrombosis and Haemostasis 2005; Vol. 3, issue 1:Abstract OR059.
- Verso M, Gussoni G, Agnelli G. Prevention of venous thromboembolism in patients with advanced lung cancer receiving chemotherapy: a combined analysis of the PROTECHT and TOPIC‐2 studies. Journal of Thrombosis and Haemostasis 2010;8(7):1649‐51. [DOI] [PubMed] [Google Scholar]
Kakkar 2004 {published data only}
- Kakkar AK, Levine MN, Kadziola Z, Lemoine NR, Low V, Patel HK, et al. Low molecular weight heparin, therapy with dalteparin, and survival in advanced cancer: the fragmin advanced malignancy outcome study (FAMOUS). Journal of Clinical Oncology 2004;22(10):1944‐8. [DOI] [PubMed] [Google Scholar]
Khorana 2015 {published data only}
- Khorana AA, Francis CW, Kuderer N, Carrier M, Ortel TL, Wun T, et al. Dalteparin thromboprophylaxis in cancer patients at high risk for venous thromboembolism: a randomized trial. Blood 2015;126:427. [DOI] [PubMed] [Google Scholar]
- NCT00876915. A prospective randomized multicenter study of dalteparin prophylaxis in high‐risk ambulatory cancer patients. clinicaltrials.gov/show/NCT00876915 (first received 31 March 2009).
Klerk 2005 {published data only}
- Klerk CP, Smorenburg SM, Otten HM, Lensing AW, Prins MH, Piovella F, et al. The effect of low molecular weight heparin on survival in patients with advanced malignancy. Journal of Clinical Oncology 2005;23(10):2130‐5. [DOI] [PubMed] [Google Scholar]
Larocca 2012 {published data only}
- Cavallo F, Caravita T, Raimondo F, Ciccone G, Lupo B, Marcatti M, et al. A phase III study of enoxaparin vs aspirin as thromboprophylaxis for patients with newly diagnosed of multiple myeloma treated with lenalidomide‐based regimens. Haematologica 2011;96:S30. [Google Scholar]
- Cavallo F, Raimondo F, Harda I, Lupo B, Romano A, Catalano L, et al. A phase III study of enoxaparin vs aspirin as thromboprophylaxis for newly diagnosed myeloma patients treated with lenalidomide‐based regimen. Blood 2010; Vol. 116:Abstract 1092.
- Larocca A, Caravita TT, Raimondo F, Cavallo F, Cascavilla N, Galli M, et al. Thromboprophylaxis for newly diagnosed myeloma patients treated with lenalidomide‐based regimens: an interim analysis of a prospective, randomized study of enoxaparin vs aspirin. Haematologica 2013;95:S40. [Google Scholar]
- Larocca A, Cavallo F, Bringhen S, Raimondo F, Falanga A, Evangelista A, et al. Aspirin or enoxaparin thromboprophylaxis for patients with newly diagnosed multiple myeloma treated with lenalidomide. Blood 2012;119(4):933‐9. [DOI] [PubMed] [Google Scholar]
Lebeau 1994 {published data only}
- Lebeau B, Chastang C, Brechot J‐M, Capron F, Dautzenberg B, Delaisements C, et al. Subcutaneous heparin treatment increases survival in small cell lung cancer. "Petites Cellules" Group. Cancer 1994;74(1):38‐45. [DOI] [PubMed] [Google Scholar]
Lecumberri 2013 {published data only}
- Lecumberri R, Lopez VG, Font A, Gonzalez BE, Gurpide A, Gomez CJ, et al. Adjuvant therapy with bemiparin in patients with limited‐stage small cell lung cancer: Results from the ABEL study. Thrombosis Research 2013;132:666‐70. [DOI] [PubMed] [Google Scholar]
- NCT00324558. Multicenter, randomized, open and sequential study to evaluate the efficacy and safety of bemiparin administration on the response to treatment in patients diagnosed with limited small cell lung cancer. clinicaltrials.gov/show/NCT00324558 (first received 9 May 2006).
Levine 1994 {published data only}
- Dickson L, Levine M, Gent M. Efficacy of double‐blinding in a randomized controlled trial (RCT) of low dose warfarin to prevent thromboembolic disease in patients with metastatic breast cancer. Controlled Clinical Trials 1993;14(5):462. [Google Scholar]
- Levine M, Hirsh J, Gent M, Arnold A, Warr D, Falanga A, et al. Double‐blind randomised trial of very‐low‐dose warfarin for prevention of thromboembolism in stage IV breast cancer. Lancet 1994;343(8902):886‐9. [DOI] [PubMed] [Google Scholar]
Levine 2012 {published data only}
- Levine MN, Gu C, Liebman HA, Escalante CP, Solymoss S, Deitchman D, et al. A randomized phase II trial of Apixaban for the prevention of thromboembolism in patients with metastatic cancer. Journal of Thrombosis and Haemostasis 2012;10(5):807‐14. [DOI] [PubMed] [Google Scholar]
- Levine MN, Liebman HA, Esclanate CP, Julian JA, Deitchman D, O'Brien MC, et al. Randomized phase II trial of an oral factor Xa inhibitor in patients with metastatic cancer on chemotherapy. Thrombosis Research 2010;125 (Suppl 2):S161‐2. [Google Scholar]
- Liebman H, Levine MN, Deitchman D, Julian J, Escalante CP, O'Brien MC, et al. Apixaban in patients with metastatic cancer: a randomized phase II feasibility study. Journal of Thrombosis and Haemostasis 2009;7 Suppl 2:Abstract PP‐WE‐489. [DOI] [PubMed] [Google Scholar]
- NCT00320255. A randomized, double‐blind, placebo‐controlled study of apixaban for the prevention of thromboembolic events in patients undergoing treatment for advanced cancer: a phase 2 pilot study. clinicaltrials.gov/show/NCT00320255 (first received 28 April 2006).
Macbeth 2016 {published data only}
- Griffiths GO, Burns S, Noble SI, Macbeth FR, Cohen D, Maughan TS. FRAGMATIC: a randomised phase III clinical trial investigating the effect of fragmin added to standard therapy in patients with lung cancer. BMC Cancer 2009;9:355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macbeth F, Noble S, Evans J, Ahmed S, Cohen D, Hood K, et al. Randomized phase III trial of standard therapy plus low molecular weight heparin in patients with lung cancer: FRAGMATIC trial. Journal of Clinical Oncology 2016;34:488‐94. [DOI] [PubMed] [Google Scholar]
- Macbeth F, Noble S, Griffiths G, Chowdhury R, Rolfe C, Hood K, et al. Preliminary results from the fragmatic trial: A randomised phase iii clinical trial investigating the effect of fragmin added to standard therapy in patients with lung cancer. Journal of Thoracic Oncology 2013;8(Suppl 2):O27.02. [Google Scholar]
- Noble S, Harrop E, Edwards M, Sivell S, Hood K, Griffiths G, et al. Applying the results of the Fragmatic trial to real life: longitudinal qualitative study exploring the experiences of patients partcipating in a randomised phase III clinical trial investigating the effect of Fragmin added to standard therapy in lung cancer. Journal of Thoracic Oncology 2013;8 (Suppl 2):S1011‐2. [Google Scholar]
Maraveyas 2012 {published data only}
- Maraveyas A, Ettelaie C, Echrish H, Li C, Gardiner E, Greenman J, et al. Weight‐adjusted dalteparin for prevention of vascular thromboembolism in advanced pancreatic cancer patients decreases serum tissue factor and serum‐mediated induction of cancer cell invasion. Blood Coagulation and Fibrinolysis 2010;21(5):452‐8. [DOI] [PubMed] [Google Scholar]
- Maraveyas A, Waters J, Roy R, Fyfe D, Propper D, Lofts F, et al. Gemcitabine versus gemcitabine plus dalteparin thromboprophylaxis in pancreatic cancer. European Journal of Cancer 2012;48(9):1283‐92. [DOI] [PubMed] [Google Scholar]
- NCT00462852. A phase II randomised study of chemo‐anticoagulation (gemcitabine‐dalteparin) vs chemotherapy alone (Gemcitabine) for locally advanced and metastatic pancreatic adenocarcinoma. clinicaltrials.gov/show/NCT00462852 (first received 18 April 2007).
Maurer 1997 {published data only}
- Maurer LH, Herndon JE II, Hollis DR, Aisner J, Carey RW, Skarin AT, et al. Randomized trial of chemotherapy and radiation therapy with or without warfarin for limited‐stage small‐cell lung cancer: a Cancer and Leukemia Group B study. Journal of Clinical Oncology 1997;15(11):3378‐87. [DOI] [PubMed] [Google Scholar]
Mitchell 2003 {published data only}
- Mitchell L, Andrew M, Hanna K, Abshire T, Halton J, Wu J, et al. Trend to efficacy and safety using antithrombin concentrate in prevention of thrombosis in children receiving l‐asparaginase for acute lymphoblastic leukemia. Results of the PAARKA study. Thrombosis and Haemostasis 2003;90(2):235‐44. [DOI] [PubMed] [Google Scholar]
Palumbo 2011 {published data only}
- Cavo M, Palumbo A, Bringhen S, Di RF, Patriarca F, Rossi D, et al. Phase III study of enoxaparin versus aspirin versus low dose warfarin as thromboprophylaxis for patients with newly diagnosed multiple myeloma treated up front with thalidomide‐containing regimens. Haematologica 2010;95 Suppl 2:391, Abstract 0941. [Google Scholar]
- Palumbo A, Cavo M, Bringhen S, Patriarca F, Rossi D, Petrucci MT, et al. A phase III study of enoxaparin versus aspirin versus low‐dose warfarin as thromboprophylaxis for patients with newly diagnosed multiple myeloma treated up‐front with thalidomide based‐regimens. Haematologica 2009; Vol. 94 Suppl 2:213.
- Palumbo A, Cavo M, Bringhen S, Zamagni E, Romano A, Patriarca F, et al. Aspirin, warfarin, or enoxaparin thromboprophylaxis in patients with multiple myeloma treated with thalidomide: a phase III, open‐label, randomized trial. Journal of Clinical Oncology 2011;29:986‐93. [DOI] [PubMed] [Google Scholar]
- Palumbo A, Rus C, Cavallo F, Bertola A, Petrucci MT, Liberati AM, et al. Enoxaparin or aspirin for the prevention of recurrent thromboembolism in newly diagnosed myeloma patients treated with melphalan and prednisone plus thalidomide or lenalidomide. Haematologica 2006; Vol. 91 Suppl 1. [DOI] [PubMed]
Pelzer 2015 {published data only}
- Pelzer U, Deutschinoff G, Opitz B, Stauch M, Reitzig P, Hahnfeld S, et al. A prospective, randomized trial of simultaneous pancreatic cancer treatment with enoxaparin and chemotherapy. First results of the CONKO‐004 trial. Onkologie‐DGHO meeting; 2009 Oct 2‐6; Mannheim. 2009:Abstract 580.
- Pelzer U, Deutschinoff G, Opitz B, Stauch M, Reitzig P, Hahnfeld S, et al. The impact of low molecular weight heparin in first‐line pancreatic cancer treatment ‐ final results of the CONKO‐004 trial. Onkologie 2010;33(6):200. [Google Scholar]
- Pelzer U, Hilbig A, Stieler J, Roll L, Riess H, Dörken B, et al. A prospective, randomized trial of simultaneous pancreatic cancer treatment with enoxaparin and chemotherapy (PROSPECT – CONKO 004). Onkologie 2005; Vol. 28 Suppl 3:Abstract 151.
- Pelzer U, Oettle H, Stauch M, Opitz B, Stieler J, Scholten T, et al. Prospective, randomized open trial of enoxaparin in patients with advanced pancreatic cancer undergoing first‐line chemotherapy. XXIst Congress of the International Society on Thrombosis and Haemostasis; 2007 Jul 6‐12; Geneva. 2007:Abstract P‐T‐488.
- Pelzer U, Opitz B, Deutschinoff G, Stauch M, Reitzig PC, Hahnfeld S, et al. Efficacy of prophylactic low‐molecular weight heparin for ambulatory patients with advanced pancreatic cancer: outcomes from the CONKO‐004 Trial. Journal of Clinical Oncology 2015;33:2028‐34. [DOI] [PubMed] [Google Scholar]
- Pelzer U, Sinn M, Stieler J, Reiss H. Primary pharmacological prevention of thromboembolic events in ambulatory patients with advanced pancreatic cancer treated with chemotherapy?. Deutsche Medizinische Wochenschrift 2013;138:2084‐8. [DOI] [PubMed] [Google Scholar]
- Riess H, Pelzer U, Hilbig A, Stieler J, Opitz B, Scholten T, et al. Rationale and design of PROSPECT‐CONKO 004: a prospective, randomized trial of simultaneous pancreatic cancer treatment with enoxaparin and chemotherapy. BMC Cancer 2008;8:361. [DOI] [PMC free article] [PubMed] [Google Scholar]
Perry 2010 {published data only}
- Perry JR, Julian JA, Laperriere NJ, Geerts W, Agnelli G, Rogers LR, et al. PRODIGE: a randomized placebo‐controlled trial of dalteparin low‐molecular‐weight heparin thromboprophylaxis in patients with newly diagnosed malignant glioma. Journal of Thrombosis and Haemostasis 2010;8(9):1959‐65. [DOI] [PubMed] [Google Scholar]
- Perry JR, Rogers L, Laperriere N, Julian J, Geerts W, Agnelli G, et al. PRODIGE: A phase III randomized placebo‐controlled trial of thromboprophylaxis using dalteparin low molecular weight heparin (LMWH) in patients with newly diagnosed malignant glioma. Journal of Clinical Oncology 2007;25(18 Suppl):2011. [Google Scholar]
Sideras 2006 {published data only}
- Sideras K, Schaefer PL, Okuno SH, Sloan JA, Kutteh L, Fitch TR, et al. Low‐molecular‐weight heparin in patients with advanced cancer: a phase 3 clinical trial. Mayo Clinic Proceedings 2006;81(6):758‐67. [DOI] [PubMed] [Google Scholar]
Vadhan‐Raj 2013 {published data only}
- NCT00966277. Randomized clinical trial of dalteparin for primary venous thromboembolism (VTE) prophylaxis in pancreatic cancer patients undergoing chemotherapy treatment. clinicaltrials.gov/show/NCT00966277 (first received 25 August 2009).
- Vadhan‐Raj S, Zhou X, Varadhachary GR, Milind J, Fogelman D, Shroff R, et al. Randomized controlled trial of dalteparin for primary thromboprophylaxis for venous thromboembolism (VTE) in patients with advanced pancreatic cancer (APC): risk factors predictive of VTE. 55th Annual Meeting of the American Society of Hematology. 21 2013.
- Zhou X, Varadhachary GR, Milind J, Fogelman D, Shroff R, Bueso‐Ramos CE, et al. Randomized controlled trial of dalteparin for primary thromboprophylaxis for venous thromboembolism (VTE) in patients with advanced pancreatic cancer (APC): risk factors predictive of VTE. Blood 2013;122(21):580. [Google Scholar]
van Doormaal 2011 {published data only}
- Doormaal FF, Nisio M, Otten H‐M, Richel DJ, Prins M, Buller HR. Randomized trial of the effect of the low molecular weight heparin nadroparin on survival in patients with cancer. Journal of Clinical Oncology 2011;29(15):2071‐6. [DOI] [PubMed] [Google Scholar]
Zacharski 1981 {published data only}
- Zacharski LR, Henderson WG, Rickles FR, Forman WB, Cornell CJ Jr, Forcier RJ, et al. Effect of warfarin anticoagulation on survival in carcinoma of the lung, colon, head and neck, and prostate. Final report of VA Cooperative Study #75. Cancer 1984;53(10):2046‐52. [DOI] [PubMed] [Google Scholar]
- Zacharski LR, Henderson WG, Rickles FR, Forman WB, Cornell CJ Jr, Forcier RJ, et al. Effect of warfarin on survival in small cell carcinoma of the lung. Veterans Administration Study No. 75. JAMA 1981;245(8):831‐5. [PubMed] [Google Scholar]
Zwicker 2013 {published data only}
- Zwicker J, Liebman HA, Bauer KA, Caughey T, Rosovsky R, Mantha S, et al. A randomized‐controlled phase II trial of primary thromboprophylaxis with enoxaparin in cancer patients with elevated tissue factor bearing microparticles (The Microtec Study). Journal of Thrombosis and Haemostasis 2013;11 (Suppl s3):6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zwicker JI, Liebman HA, Bauer KA, Caughey T, Campigotto F, Rosovsky R, et al. Prediction and prevention of thromboembolic events with enoxaparin in cancer patients with elevated tissue factor‐bearing microparticles: a randomized‐controlled phase II trial (the Microtec study). British Journal of Haematology 2013;160(4):530–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies excluded from this review
Baz 2005 {published data only}
- Baz R, Li L, Kottke‐Marchant K, Srkalovic G, McGowan B, Yiannaki E, et al. The role of aspirin in the prevention of thrombotic complications of thalidomide and anthracycline‐based chemotherapy for multiple myeloma. Mayo Clinic Proceedings 2005;80(12):1568‐74. [DOI] [PubMed] [Google Scholar]
Bergqvist 1983 {published data only}
- Bergqvist D, Lindblad B. Is it possible to potentiate the thromboprophylactic effect of dextran with elastic compression stockings?. Thrombosis and Haemostasis 1983; Vol. 50, issue 1:247 Abstract 0777.
Bocharov 2011 {published data only}
- Bocharov AV, Cherenkov VG, Ukhanov AP, Chentsov VI. Potential endovascular prophylaxis for pulmonary thromboembolism in the combined treatment of cancer patients. Voprosy Onkologii 2011;57:513‐6. [PubMed] [Google Scholar]
Eichinger 2008 {published data only}
- Eichinger S, Traby L, Kaider A, Quehenberger P, Kyrle PA. Prevention of venous thrombosis in cancer patients: a randomized, double‐blind study comparing two different dosages of low‐molecular weight heparin. Blood 2008;112(11):690 Abstract 1977. [Google Scholar]
Gercor 2013 {unpublished data only}
- Groupe Cooperateur Multidisciplinaire en Oncologie. Chemotherapy with or without dalteparin in treating patients with metastatic pancreatic cancer (PAM07). clinicaltrials.gov/show/NCT00662688 (first received 18 April 2008).
Haas 2011 {published data only}
- Haas S, Schellong SM, Tebbe U, Gerlach H‐E, Bauersachs R, Melzer N, et al. Heparin based prophylaxis to prevent venous thromboembolic events and death in patients with cancer ‐ a subgroup analysis of CERTIFY. BMC Cancer 2011;11:316. [DOI] [PMC free article] [PubMed] [Google Scholar]
Heilmann 1995 {published data only}
- Heilmann L, Schneider D, Herrle B, Tempelhoff G‐F, Manstein J, Wolf H. A prospective randomized trial of low molecular weight heparin (LMWH) versus unfractionated heparin (UFH) in patients with gynecologic cancer. Thrombosis and Haemostasis 1995; Vol. 73, issue 6:974 Abstract No 286.
Hills 1972 {published data only}
- Hills NH, Pflug JJ, Jeyasingh K, Boardman L, Calnan JS. Prevention of deep vein thrombosis by intermittent pneumatic compression of calf. British Medical Journal 1972;1(5793):131‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kessler 2011 {published data only}
- Kessler P. Prophylaxis and treatment of venous thromboembolism in patients with multiple myeloma. Onkologie 2011;5(3):160‐2. [Google Scholar]
- Kessler P, Pour L, Gregora E, Zemanova M, Penka M, Brejcha M, et al. Czech Myeloma Group. Low molecular weight heparins for thromboprophylaxis during induction chemotherapy in patients with multiple myeloma. Klinicka Onkologie 2011;24(4):281‐6. [PubMed] [Google Scholar]
Kwaan 2007 {unpublished data only}
- NCT00004875. Heparin or enoxaparin in patients with cancer. clinicaltrials.gov/show/NCT00004875 (first received 7 March 2000).
Levin 2008 {unpublished data only}
- NCT00790452. A randomized phase II trial of aspirin for primary prophylaxis of venous thromboembolism in glioblastoma. clinicaltrials.gov/show/NCT00790452 (first received 7 November 2008).
Macintyre 1974 {published data only}
- Macintyre MC, Vasilescu C, Jones DRB. Heparin versus dextran in the prevention of deep‐vein thrombosis. A multi‐unit controlled trial. Lancet 1974;2(7873):118‐20. [PubMed] [Google Scholar]
Maxwell 2000 {published data only}
- Maxwell GL. A prospective randomized trial comparing external pneumatic compression stockings (EPC) to the low molecular weight heparin (LMWH) dalteparin in the prevention of thromboembolic events (TE) among gynecologic oncology patients. Proceedings of the American Society of Clinical Oncology 2000; Vol. 19:388a, Abstract 1535.
Meister 2008 {published data only}
- Meister B, Kropshofer G, Klein Franke A, Strasak AM, Hager J, Streif W. Comparison of low‐molecular‐weight heparin and antithrombin versus antithrombin alone for the prevention of symptomatic venous thromboembolism in children with acute lymphoblastic leukemia. Pediatric Blood and Cancer 2008;50(2):298‐303. [DOI] [PubMed] [Google Scholar]
Minnema 2004 {published data only}
- Minnema MC, Breitkreutz I, Auwerda JJ, van‐der Holt B, Cremer FW, van‐Marion AM, et al. Prevention of venous thromboembolism with low molecular‐weight heparin in patients with multiple myeloma treated with thalidomide and chemotherapy. Leukemia 2004;18(12):2044‐6. [DOI] [PubMed] [Google Scholar]
Niesvizky 2007 {published data only}
- Niesvizky R, Martinez‐Banos D, Jalbrzikowski J, Christos P, Furst J, Sancho M, et al. Prophylactic low‐dose aspirin is effective antithrombotic therapy for combination treatments of thalidomide or lenalidomide in myeloma. Leukemia and Lymphoma 2007;48(12):2330–7. [DOI] [PubMed] [Google Scholar]
Pandya 2002 {unpublished data only}
- NCT00031837. A prospective randomized controlled multicenter study of the effect of dalteparin on quality of life in unresectable pancreatic cancer. clinicaltrials.gov/show/NCT00031837 (first received 8 March 2002).
Paydas 2008 {published data only}
- Paydas S. Tailored thromboprophylaxis for patients with multiple myeloma treated by IMIDs. Leukemia and Lymphoma 2008;49(8):1644‐5. [DOI] [PubMed] [Google Scholar]
Poniewierski 1987 {published data only}
- Poniewierski M, Barthels M, Kuhn M, Poliwoda H. Efficacy of low molecular weight heparin (Fragmin) for thromboprophylaxis in medical patients: a randomized double blind trial. Medizinische Klinik 1988;83(7):241‐5. [PubMed] [Google Scholar]
- Poniewierski M, Barthels M, Poliwoda H. The safety and efficacy of a low molecular weight heparin (fragmin) in the prevention of deep vein thrombosis in medical patients: a randomized double‐blind trial. Thrombosis and Haemostasis 1987; Vol. 58, issue 1:119 Abstract 425.
Rajan 1995 {published data only}
- Rajan R, Gafni A, Levine M, Hirsh J, Gent M. Very low‐dose warfarin prophylaxis to prevent thromboembolism in women with metastatic breast cancer receiving chemotherapy: an economic evaluation. Journal of Clinical Oncology 1995;13(1):42‐6. [DOI] [PubMed] [Google Scholar]
Sideras 2007 {published data only}
Weber 2008 {published data only}
- Weber C, Merminod T, Herrmann FR, Zulian GB. Prophylactic anti‐coagulation in cancer palliative care: a prospective randomised study. Support Care in Cancer 2008;16(7):847‐52. [DOI] [PubMed] [Google Scholar]
Welti 1981 {published data only}
- Welti H. Thrombo‐embolytic prophylaxis using physiotherapy with and without low doses of heparin in gynecology and obstetrics. Results of a controlled and randomized multi‐cancer study. Revue Medicale de la Suisse Romande 1981;101(11):925‐34. [PubMed] [Google Scholar]
Zangari 2003 {published data only}
- Zangari M, Barlogie B, Saghafifar F, Eddlemon P, Jacobson J, Lee CK, et al. Effect of anticoagulation on development and recurrence of deep vein thrombosis (DVT) in multiple myeloma patients treated with chemotherapy and thalidomide (total therapy II). Hematology Journal 2003;4 Suppl 1:S248. [Google Scholar]
References to studies awaiting assessment
Ciftci 2012 {published data only}
- Ciftci A, Altiay G. The effect of warfarin on survival in patients with lung cancer. Journal of Thoracic Oncology 2012;7:S122. [Google Scholar]
NCT00771563 {published data only}
- Enoxaparin low molecular weight heparin (LMWH) in advanced non small cell lung cancer: effect on survival and symptom control in patients undergoing first line chemotherapy (SYRINGES). clinicaltrials.gov/ct2/show/NCT00771563 (first received 10 October 2008).
Salat 1990 {published data only}
- Salat C, Breitruck H, Reinhardt B, Hiller E. Thromboprophylaxis with low molecular weight heparin (LMWH) and conventional low dose heparin in patients with malignant diseases. Blut 1990;61(2‐3):142. [Google Scholar]
References to ongoing studies
NCT00662688 {unpublished data only}
- NCT00662688. Chemotherapy with or without preventive anticoagulation for metastatic cancer of the pancreas. clinicaltrials.gov/ct2/show/NCT00662688?term=NCT00662688&rank=1 (first received 18 April 2008).
NCT00717938 {unpublished data only}
- NCT00717938. A study of standard treatment +/‐ enoxaparin in small cell lung cancer (RASTEN). clinicaltrials.gov/ct2/show/NCT00717938 (first received 16 July 2008).
NCT00718354 {unpublished data only}
- NCT00718354. Randomized, phase III‐b, multi‐centre, open‐label, parallel study of Enoxaparin (low molecular weight heparin) given concomitantly with chemotherapy vs chemotherapy alone in patients with inoperable gastric and gastro‐oesophageal cancer. clinicaltrials.gov/ct2/show/NCT00718354?term=NCT00718354&rank=1 (first received 16 July 2008).
NCT02048865 {published data only}
- NCT02048865. Apixaban for the prevention of venous thromboembolism in cancer patients (AVERT). clinicaltrials.gov/ct2/show/NCT02048865 (first received 27 January 2014).
NCT02285738 {published data only}
- NCT02285738. Anti‐platelet and statin therapy to prevent cancer‐associated thrombosis. clinicaltrials.gov/ct2/show/NCT02285738 (first received 5 November 2014).
NCT02555878 {published data only}
- NCT02555878. Efficacy and safety of rivaroxaban prophylaxis compared with placebo in ambulatory cancer patients initiating systemic cancer therapy and at high risk for venous thromboembolism. clinicaltrials.gov/ct2/show/NCT02555878 (first received 18 September 2015).
Additional references
Aikens 2013
- Aikens GB, Rivey MP, Hansen CJ. Primary venous thromboembolism prophylaxis in ambulatory cancer patients. The Annals of Pharmacotherapy 2013;47(2):198‐209. [DOI] [PubMed] [Google Scholar]
Akl 2011
- Akl EA, Vasireddi SR, Gunukula S, Yosuico VED, Barba M, Sperati F, et al. Anticoagulation for patients with cancer and central venous catheters. Cochrane Database of Systematic Reviews 2011, Issue 4. [DOI: 10.1002/14651858.CD006468.pub4] [DOI] [Google Scholar]
Ay 2010
- Ay C, Dunkler D, Marosi C, Chiriac AL, Vormittag R, Simanek R, et al. Prediction of venous thromboembolism in cancer patients. Blood 2010;116(24):5377‐82. [DOI] [PubMed] [Google Scholar]
DerSimonian 1986
- DerSimonian R, Laird N. Meta‐analysis in clinical trials. Controlled Clinical Trials 1986;7:177‐88. [DOI] [PubMed] [Google Scholar]
Donato 2015
- Donato J, Campigotto F, Uhlmann EJ, Coletti E, Neuberg D, Weber GM, et al. Intracranial hemorrhage in patients with brain metastases treated with therapeutic enoxaparin: a matched cohort study. Blood 2015;126:494‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
EMEA 2012
- European Medicines Agency (EMEA). Withdrawal of the marketing authorisation application for Mulsevo (semuloparin sodium). www.emea.europa.eu/docs/en_GB/document_library/Medicine_QA/2012/07/WC500130168.pdf (accessed 11 December 2012).
George 2011
- George D, Agnelli G, Fisher W, Kakkar A, Lassen MR, Mismetti P, et al. Venous thromboembolism (VTE) prevention with semuloparin in cancer patients initiating chemotherapy: benefit‐risk assessment by VTE risk in SAVE‐ONCO. Blood 2011;118:Abstract 206. [Google Scholar]
Guyatt 2008
- Guyatt G, Oxman AD, Vist GE, Kunz R, Falck‐Ytter Y, Alonso‐Coello P, et al. GRADE Working Group. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008;336(7656):924‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Harbord 2006
- Harbord RM, Egger M, Sterne JA. A modified test for small‐study effects in meta‐analyses of controlled trials with binary endpoints. Statistics in Medicine 2006;25(20):3443‐57. [DOI] [PubMed] [Google Scholar]
Heit 2015
- Heit JA. Epidemiology of venous thromboembolism. Nature Reviews. Cardiology 2015;12:464‐74. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2003
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analyses. BMJ 2003;327(7414):557‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Hutten 2000
- Hutten B, Prins M, Gent M, Ginsberg J, Tijsen JG, Büller HR. Incidence of recurrent thromboembolic and bleeding complications among patients with venous thromboembolism in relation to both malignancy and achieved international normalized ratio: a retrospective analysis. Journal of Clinical Oncology 2000;18(17):3078‐83. [DOI] [PubMed] [Google Scholar]
Juni 2001
- Juni P, Altman DG, Egger M. Systematic reviews in health care: Assessing the quality of controlled clinical trials. BMJ 2001;323(7303):42‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kahn 2012
- Kahn SR, Lim W, Dunn AS, Cushman M, Dentali F, Akl EA, et al. Prevention of VTE in nonsurgical patients: antithrombotic therapy and prevention of thrombosis, 9th edition: American College of Chest Physicians evidence‐based clinical practice guidelines. Chest 2012;141(2 Suppl):e195S‐226S. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kamphuisen 2014
- Kamphuisen PW, Beyer‐Westendorf J. Bleeding complications during anticoagulant treatment in patients with cancer. Thrombosis Research 2014;133(S2):S49–55. [DOI] [PubMed] [Google Scholar]
Khorana 2008
- Khorana AA, Kuderer NM, Culakova E, Lyman GH, Francis CW. Development and validation of a predictive model for chemotherapy‐associated thrombosis. Blood 2008;111(10):4902‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Khorana 2009
- Khorana AA, Connolly GC. Assessing risk of venous thromboembolism in the patient with cancer. Journal of Clinical Oncology 2009;27(29):4839‐47. [DOI] [PMC free article] [PubMed] [Google Scholar]
Khorana 2009a
- Khorana AA, Streiff MB, Farge D, Mandala M, Debourdeau P, Cajfinger F, et al. Venous thromboembolism prophylaxis and treatment in cancer: a consensus statement of major guidelines panels and call to action. Journal of Clinical Oncology 2009;27(29):4919‐26. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kuderer 2009
- Kuderer NM, Khorana AA, Francis CW, Lyman GH, Falanga A, Ortel TL. Low‐molecular‐weight heparin for venous thromboprophylaxis in ambulatory cancer patients: a meta‐analysis. Journal of Clinical Oncology. ASCO Annual Meeting Proceedings (Post‐Meeting Edition) 2009;27(15S):9537. [Google Scholar]
Lyman 2013
- Lyman GH, Khorana AA, Kuderer NM, Lee AY, Arcelus JI, Balaban EP, et al. Venous thromboembolism prophylaxis and treatment in patients with cancer: American Society of Clinical Oncology clinical practice guideline update. Journal of Clinical Oncology 2013;31(24):2189‐204. [DOI] [PubMed] [Google Scholar]
Lyman 2015
- Lyman GH, Bohlke K, Khorana AA, Kuderer NM, Lee AY, Arcelus JI, et al. Venous thromboembolism prophylaxis and treatment in patients with cancer: American Society of Clinical Oncology clinical practice guideline update 2014. Journal of Clinical Oncology 2015;33:654‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Maxwell 2012
- Maxwell WD, Bennett CL. Thromboprophylaxis guidelines in cancer with a primary focus on ambulatory patients receiving chemotherapy: a review from the southern network on adverse reactions (SONAR). Seminars in Thrombosis and Hemostasis 2012;38(8):759–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
Otten 2004
- Otten H‐M, Mathijssen J, Cate H, Soesan M, Inghels M, Richel DJ, et al. Symptomatic venous thromboembolism in cancer patients treated with chemotherapy. An underestimated phenomenon. Archives of Internal Medicine 2004;164(2):190‐4. [DOI] [PubMed] [Google Scholar]
Prandoni 2002
- Prandoni P, Lensing AW, Piccioli A, Bernardi E, Simioni P, Girolami B, et al. Recurrent venous thromboembolism and bleeding complications during anticoagulant treatment in patients with cancer and venous thrombosis. Blood 2002;100(10):3484‐8. [DOI] [PubMed] [Google Scholar]
Rana 2009
- Rana P, Levine MN. Prevention of thrombosis in ambulatory patients with cancer. Journal of Clinical Oncology 2009;27(29):4885‐8. [DOI] [PubMed] [Google Scholar]
RevMan 2014 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Rutjes 2009
- Rutjes AW, Nüesch E, Sterchi R, Kalichman L, Hendriks E, Osiri M, et al. Transcutaneous electrostimulation for osteoarthritis of the knee. Cochrane Database of Systematic Reviews 2009, Issue 4. [DOI: 10.1002/14651858.CD002823.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Rutjes 2012
- Rutjes AW, Juni P, Costa BR, Trelle S, Nuesch E, Reichenbach S. Viscosupplementation for osteoarthritis of the knee: a systematic review and meta‐analysis. Annals of Internal Medicine 2012;157(3):180‐91. [DOI] [PubMed] [Google Scholar]
Rücker 2008
- Rücker G, Schwarzer G, Carpenter JR, Schumacher M. Undue reliance on I2 in assessing heterogeneity may mislead. BMC Medical Research Methodology 2008;8(1):79. [DOI] [PMC free article] [PubMed] [Google Scholar]
Schulman 2005
- Schulman S, Kearon C on behalf of the subcommittee on control of anticoagulation of the Scientific and Standardization committee of the International Society on Thrombosis and Haemostasis. Definition of major bleeding in clinical investigations of antihemostatic medicinal products in non‐surgical patients. Scientific and Standardization Committee Communication. Journal of Thrombosis and Haemostasis 2005;3:692–4. [DOI] [PubMed] [Google Scholar]
Sorensen 2000
- Sorensen HT, Mellemkjaer L, Olsen JH, Baron JA. Prognosis of cancers associated with venous thromboembolism. New England Journal of Medicine 2000;343(25):1846‐50. [DOI] [PubMed] [Google Scholar]
Spiegelhalter 2004
- Spiegelhalter DJ, Abrams KR, Myles JP. Bayesian Approaches to Clinical Trials and Health‐Care Evaluation. Chichester, UK: John Wiley & Sons, 2004. [Google Scholar]
Stata 2015 [Computer program]
- StataCorp LP. Stata Statistical Software: Release 14. College Station, TX: StataCorp LP, 2015.
Sterne 2001
- Sterne JA, Egger M. Funnel plots for detecting bias in meta‐analysis: guidelines on choice of axis. Journal of Clinical Epidemiology 2001;54(10):1046‐55. [DOI] [PubMed] [Google Scholar]
Thompson 1999
- Thompson SG, Sharp SJ. Explaining heterogeneity in meta‐analysis: a comparison of methods. Statistics in Medicine 1999;18(20):2693‐708. [DOI] [PubMed] [Google Scholar]
Verso 2012
- Verso M, Agnelli G, Barni S, Gasparini G, LaBianca R. A modified Khorana risk assessment score for venous thromboembolism in cancer patients receiving chemotherapy: the Protecht score. Internal and Emergency Medicine 2012;7(3):291–2. [DOI] [PubMed] [Google Scholar]
Weitz 2012
- Weitz JI, Eikelboom JW, Samama MM, American College of Chest Physicians. New antithrombotic drugs: antithrombotic therapy and prevention of thrombosis, 9th edition: American College of Chest Physicians evidence‐based clinical practice guidelines. Chest 2012;141(2 Suppl):e120S‐51S. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to other published versions of this review
Di Nisio 2010
- Nisio M, Rutjes AWS, Ferrante N, Otten HM, Porreca E, Cuccurullo F. Primary prophylaxis for venous thromboembolism in ambulatory cancer patients receiving chemotherapy. Cochrane Database of Systematic Reviews 2010, Issue 5. [DOI: 10.1002/14651858.CD008500] [DOI] [PubMed] [Google Scholar]
Di Nisio 2012
- Nisio M, Porreca E, Ferrante N, Otten HM, Cuccurullo F, Rutjes AWS. Primary prophylaxis for venous thromboembolism in ambulatory cancer patients receiving chemotherapy. Cochrane Database of Systematic Reviews 2012, Issue 2. [DOI: 10.1002/14651858.CD008500.pub2] [DOI] [PubMed] [Google Scholar]
Di Nisio 2014
- Nisio M, Porreca E, Otten HM, Rutjes AWS. Primary prophylaxis for venous thromboembolism in ambulatory cancer patients receiving chemotherapy. Cochrane Database of Systematic Reviews 2014, Issue 8. [DOI: 10.1002/14651858.CD008500.pub3] [DOI] [PubMed] [Google Scholar]


