Abstract
Background
Out‐of‐hospital cardiac arrest (OHCA) is a major cause of death worldwide. Cardiac arrest can be subdivided into asphyxial and non asphyxial etiologies. An asphyxia arrest is caused by lack of oxygen in the blood and occurs in drowning and choking victims and in other circumstances. A non asphyxial arrest is usually a loss of functioning cardiac electrical activity. Cardiopulmonary resuscitation (CPR) is a well‐established treatment for cardiac arrest. Conventional CPR includes both chest compressions and ‘rescue breathing’ such as mouth‐to‐mouth breathing. Rescue breathing is delivered between chest compressions using a fixed ratio, such as two breaths to 30 compressions or can be delivered asynchronously without interrupting chest compression. Studies show that applying continuous chest compressions is critical for survival and interrupting them for rescue breathing might increase risk of death. Continuous chest compression CPR may be performed with or without rescue breathing.
Objectives
To assess the effects of continuous chest compression CPR (with or without rescue breathing) versus conventional CPR plus rescue breathing (interrupted chest compression with pauses for breaths) of non‐asphyxial OHCA.
Search methods
We searched the Cochrane Central Register of Controlled Trials (CENTRAL; Issue 1 2017); MEDLINE (Ovid) (from 1985 to February 2017); Embase (1985 to February 2017); Web of Science (1985 to February 2017). We searched ongoing trials databases including controlledtrials.com and clinicaltrials.gov. We did not impose any language or publication restrictions.
Selection criteria
We included randomized and quasi‐randomized studies in adults and children suffering non‐asphyxial OHCA due to any cause. Studies compared the effects of continuous chest compression CPR (with or without rescue breathing) with interrupted CPR plus rescue breathing provided by rescuers (bystanders or professional CPR providers).
Data collection and analysis
Two authors extracted the data and summarized the effects as risk ratios (RRs), adjusted risk differences (ARDs) or mean differences (MDs). We assessed the quality of evidence using GRADE.
Main results
We included three randomized controlled trials (RCTs) and one cluster‐RCT (with a total of 26,742 participants analysed). We identified one ongoing study. While predominantly adult patients, one study included children.
Untrained bystander‐administered CPR
Three studies assessed CPR provided by untrained bystanders in urban areas of the USA, Sweden and the UK. Bystanders administered CPR under telephone instruction from emergency services. There was an unclear risk of selection bias in two trials and low risk of detection, attrition, and reporting bias in all three trials. Survival outcomes were unlikely to be affected by the unblinded design of the studies.
We found high‐quality evidence that continuous chest compression CPR without rescue breathing improved participants’ survival to hospital discharge compared with interrupted chest compression with pauses for rescue breathing (ratio 15:2) by 2.4% (14% versus 11.6%; RR 1.21, 95% confidence interval (CI) 1.01 to 1.46; 3 studies, 3031 participants).
One trial reported survival to hospital admission, but the number of participants was too low to be certain about the effects of the different treatment strategies on survival to admission(RR 1.18, 95% CI 0.94 to 1.48; 1 study, 520 participants; moderate‐quality evidence).
There were no data available for survival at one year, quality of life, return of spontaneous circulation or adverse effects.
There was insufficient evidence to determine the effect of the different strategies on neurological outcomes at hospital discharge (RR 1.25, 95% CI 0.94 to 1.66; 1 study, 1286 participants; moderate‐quality evidence). The proportion of participants categorized as having good or moderate cerebral performance was 11% following treatment with interrupted chest compression plus rescue breathing compared with 10% to 18% for those treated with continuous chest compression CPR without rescue breathing.
CPR administered by a trained professional
In one trial that assessed OHCA CPR administered by emergency medical service professionals (EMS) 23,711 participants received either continuous chest compression CPR (100/minute) with asynchronous rescue breathing (10/minute) or interrupted chest compression with pauses for rescue breathing (ratio 30:2). The study was at low risk of bias overall.
After OHCA, risk of survival to hospital discharge is probably slightly lower for continuous chest compression CPR with asynchronous rescue breathing compared with interrupted chest compression plus rescue breathing (9.0% versus 9.7%) with an adjusted risk difference (ARD) of ‐0.7%; 95% CI (‐1.5% to 0.1%); moderate‐quality evidence.
There is high‐quality evidence that survival to hospital admission is 1.3% lower with continuous chest compression CPR with asynchronous rescue breathing compared with interrupted chest compression plus rescue breathing (24.6% versus 25.9%; ARD ‐1.3% 95% CI (‐2.4% to ‐0.2%)).
Survival at one year and quality of life were not reported.
Return of spontaneous circulation is likely to be slightly lower in people treated with continuous chest compression CPR plus asynchronous rescue breathing (24.2% versus 25.3%; ‐1.1% (95% CI ‐2.4 to 0.1)), high‐quality evidence.
There is high‐quality evidence of little or no difference in neurological outcome at discharge between these two interventions (7.0% versus 7.7%; ARD ‐0.6% (95% CI ‐1.4 to 0.1).
Rates of adverse events were 54.4% in those treated with continuous chest compressions plus asynchronous rescue breathing versus 55.4% in people treated with interrupted chest compression plus rescue breathing compared with the ARD being ‐1% (‐2.3 to 0.4), moderate‐quality evidence).
Authors' conclusions
Following OHCA, we have found that bystander‐administered chest compression‐only CPR, supported by telephone instruction, increases the proportion of people who survive to hospital discharge compared with conventional interrupted chest compression CPR plus rescue breathing. Some uncertainty remains about how well neurological function is preserved in this population and there is no information available regarding adverse effects.
When CPR was performed by EMS providers, continuous chest compressions plus asynchronous rescue breathing did not result in higher rates for survival to hospital discharge compared to interrupted chest compression plus rescue breathing. The results indicate slightly lower rates of survival to admission or discharge, favourable neurological outcome and return of spontaneous circulation observed following continuous chest compression. Adverse effects are probably slightly lower with continuous chest compression.
Increased availability of automated external defibrillators (AEDs), and AED use in CPR need to be examined, and also whether continuous chest compression CPR is appropriate for paediatric cardiac arrest.
Plain language summary
Continuous chest compression versus interrupted chest compression for cardiopulmonary resuscitation (CPR) of non‐asphyxial out‐of‐hospital cardiac arrest (OHCA)
Background
A cardiac arrest is when the heart stops pumping blood around the body. It is a major cause of death worldwide. A large number of cardiac arrests occur outside of hospitals. Conventional CPR includes both chest compressions and rescue breathing such as mouth‐to‐mouth resuscitation. This is known as interrupted chest compression with pauses at a fixed ratio for rescue breathing (e.g. 2 breaths: 30 compressions) .
Rescue breathing can be given by mouth‐to‐mouth or by ventilation devices used by ambulance services. Some studies suggest that applying continuous chest compression is critical for an individual's survival and that interrupting the chest compressions for rescue breathing might increase the risk of death. Continuous chest compression CPR may be performed with, or without, rescue breathing. The theory is that chest compression mimics the heart's action of pumping blood around the body and maintains the supply of oxygen and nutrients to important organs such as the brain. Trying to give mouth‐to‐mouth ventilation means interrupting chest compressions which could weaken the action of pumping blood.
We compared the effects of the two treatments when they were given by bystanders at the scene of a non‐asphyxial OHCA and by ambulance crews who arrive later. (A non‐asphyxial arrest does not result from drowning or choking.)
Search date
The evidence is current to February 2017.
Study characteristics
We included four studies; three compared the two approaches to resuscitation when given by untrained bystanders under instruction by telephone. One study compared the two approaches when given by EMS personnel.
The three studies, comparing the approaches given by untrained bystanders, (3737 participants) were all undertaken in urban areas and some included both children and adult OHCA. The, bystanders were all untrained and given telephone instructions from the emergency services.
The fourth study compared approaches given by EMS professionals (23,711 participants); it was undertaken in urban areas and included only adult OHCA.
Key results
When CPR was performed by bystanders, we found that more people survived until discharge from hospital after chest compression alone than they did following interrupted chest compression with pauses at a fixed ratio for rescue breathing (15 compressions to 2 breaths) (14% versus 11.6%). For the outcomes of survival to hospital admission and neurological outcomes, we did not have sufficient data to be certain that either strategy was better. No data was available for adverse effects, quality of life or survival at one‐year.
When CPR was performed by EMS professionals, we found that survival to hospital discharge was slightly lower with continuous chest compressions (100/minute) plus asynchronous rescue breathing (10/minutes) CPR compared with interrupted chest compression plus rescue breathing. Around 9.7% of people lived when they received interrupted chest compression plus rescue breathing compared with 9% of people who received continuous chest compression plus asynchronous rescue breathing.
The number of people who survived to hospital admission was slightly higher in those treated with interrupted chest compression plus rescue breathing compared with continuous chest compression plus asynchronous rescue breathing (25.9% versus 24.6%). There was little or no difference in neurological outcomes. The proportion of people who experienced adverse events was probably similar with 55.4% people treated with interrupted chest compression plus rescue breathing experiencing an adverse event compared with 54.4% in those treated with continuous chest compression asynchronous rescue breathing.
Quality of evidence
For bystander‐provided CPR, the quality of the evidence was high for the outcome of survival to hospital discharge. For survival to hospital admission, one trial provided results and the evidence was of moderate‐quality because of low numbers of people for whom data were available. This was also the case for neurological outcomes.
In the one EMS professional‐provided CPR trial, the quality of the evidence was moderate for the outcome of survival to hospital discharge because the results do not exclude there being little or no difference between the two approaches, and this is also the case for adverse events. For survival to hospital admission there was high‐quality evidence.
The main limitation of the current evidence is that only a few trials have been undertaken, and for some outcomes, not enough data have been generated.
Summary of findings
Background
Description of the condition
Cardiac arrest is a condition in which the heart has stopped beating or is not beating efficiently enough to provide circulation to sustain life. It can be confirmed by the absence of a detectable pulse, the patient being unresponsive, or an individual stopping breathing, or breathing abnormally (apnoea, agonal or gasping respirations) (Cummins 1991). Cardiac arrest is a major cause of death in many countries around the world and an important public health problem. In 1998 in the USA, 456,076 deaths were recorded as resulting from sudden cardiac death (Zheng 2001). Approximately 350,000 people in the USA and Canada per year suffer from a cardiac arrest in which resuscitation is attempted (Jones‐Crawford 2007; Nadkarni 2006; Nichol 2008). In Europe, the incidence of emergency medical services (EMS) for treating out‐of‐hospital cardiac arrest is 38 per 100,000 persons per year (ERC 2010).
Cardiac arrest can be subdivided in asphyxial and non asphyxial etiologies. An asphyxia arrest is caused by lack of oxygen in the blood and occurs in drowning and choking victims and in other circumstances. A non asphyxial arrest is usually a loss of functioning cardiac electrical activity.
Description of the intervention
Cardiopulmonary resuscitation (CPR) has long been used to treat cardiac arrest. Conventional CPR includes both chest compressions and rescue breathing such as mouth‐to‐mouth breathing; this is denoted interrupted chest compression with pauses at a fixed ratio (either 2 breaths:15 compressions or 2 breaths: 30 compressions) for rescue breathing. Chest compression forces blood from the heart to the arterial system and increases the flow of blood to the coronary arteries, cardiac muscle and brain. In the release phase of the compression, the venous blood flows back to the heart under the force of the negative pressure of the thoracic cavity (Wolcke 2003). Thus, the external compressions lead to the heart 'working again' and so chest compressions provide partial circulatory support. The other important part of CPR is rescue breathing (artifical ventilation) . Rescue breathing can push air into the lungs and improve the blood oxygen saturation. The main form of artificial ventilation in out‐of‐hospital cardiac arrest (OHCA) is mouth‐to‐mouth resuscitation, but rescue breathing can also be provided by any kind of airway device, such as a bag‐valve mask.
CPR for out‐of‐hospital cardiac arrest can be performed using continuous chest compression‐only, or interrupted chest compression plus artificial ventilation (conventional CPR). The difference between continuous chest compression CPR and interrupted (conventional) chest compression CPR, is that in continuous chest compression CPR, rescuers do not interrupt compressions to perform artificial ventilation.
Conventional CPR emphasizes the equal importance of chest compressions and artificial ventilation, whereas compression‐only CPR considers continuous chest compression as being most critical for cardiac arrest victims.
How the intervention might work
CPR provided by bystanders is crucial for cardiac arrest victims, and substantially improves their chances of survival prior to the arrival of EMS personnel. There has been a series of studies focusing on CPR instructions for bystanders; the conclusion is that early initiation of CPR by bystanders leads to better outcomes (AHA 2005; Sayre 2008). But the problem with conventional CPR is that the majority of bystanders (including health professionals) are reluctant to perform mouth‐to‐mouth ventilation, and therefore would not initiate CPR because of the perceived requirement for mouth‐to‐mouth ventilation (Brenner 1993; Brenner 1994; Locke 1995).
There are other reasons that individuals in the USA do not initiate bystander CPR besides the requirement of mouth‐to‐mouth ventilation (Coons 2009). It has been proved that continuity of chest compression is critical for the individual's survival, and interruption of circulation is negatively related to the prognosis of cardiac arrest victims (Bobrow 2008). The longer the compressions are interrupted, the lower the incidence of return of spontaneous circulation (Paradis 1990), and the less likely the defibrillation success (Yu 2002). The 2010 American Heart Association (AHA) guidelines advocate that chest compression is essential for providing blood flow, and all patients should receive it (AHA 2010).
Artificial ventilation as part of CPR, however, may also have adverse effects such as excessive ventilation and interruption of chest compression. Although cardiac arrest can result from hypoxaemia, in patients with circulatory standstill from primary cardiac causes, blood oxygenation is typically normal until the arrest. In the first four minutes of CPR without active ventilation, oxygen saturation was more than 90% in a canine model; even after 10 minutes, the oxygen saturation was above 70% (Chandra 1994). Noc et al, investigated a domestic pig model of cardiac arrest and found that the passive ventilation (precordial compression and spontaneous gasping) volume was more than 5 L in the fifth minute of ventricular fibrillation (Noc 1995). Moreover, about 55% of out‐of‐hospital cardiac arrests occur with spontaneous gasping, which can provide the patient with some ventilation (Clark 1992). So it appears to be more important to initially restore blood circulation than push air into the lungs. As a consequence, the key change of the 2010 AHA guideline is from a conventional airway‐breathing‐circulation (A‐B‐C) sequence to circulation‐airway‐breathing (C‐A‐B), and untrained lay rescuers in particular are encouraged to do compression‐only CPR (AHA 2010). These guidelines recommend initiating chest compressions as being most important (AHA 2010). Moreover, the effect of ventilation is related to the skill or training level of the provider. It is difficult and time consuming to provide a bystander with instructions to perform ventilation or rescue breaths during CPR. However, it is fairly simple to provide a bystander with instructions for chest compression. Some studies conclude that survival with compression‐only CPR initiated by bystanders is similar to, or even better than, that provided by compression and ventilation CPR. This has been demonstrated in several studies reporting improved survival or neurological function outcomes (Bobrow 2010; Hallstrom 2000; SOS‐KANTO Group 2007; Svensson 2010; Tang 1994).
The new CPR guidelines encourage bystanders to provide compression‐only CPR before the arrival of emergency medical service personnel. The American and European guidelines recommend continuous chest compression‐only CPR in telephone advice to bystanders, especially when the rescuer is either unable or unwilling to perform rescue breaths (AHA 2010; ERC 2010). Continuous chest compression CPR performed by emergency medical service providers reduce the interruption of compressions, which is associated with higher rates of survival than interrupted compressions (Bobrow 2008).
Why it is important to do this review
A flawed conclusion frequently encountered is that everybody should perform continuous chest compression‐only CPR, a fact that is not well supported by the evidence because solid evidence is available only for a specific situation. Specifically, the effect of continuous chest compression‐only CPR may be different if performed by lay bystanders who obtain telephone advice as compared to professional CPR providers who are well trained and equipped. For bystanders, the willingness to perform CPR is associated with fear of acquiring infectious diseases by performing mouth‐to‐mouth ventilation (Becker 1997). Less than 30% of all out‐of‐hospital cardiac arrests receive bystander CPR (Eckstein 2005), which could be related to an unwillingness to perform mouth‐to‐mouth ventilation. Effective instructions for bystanders by emergency dispatchers that omit instructions for mouth‐to‐mouth ventilation are a possible point of action to increase the rate of bystander CPR. Many studies on telephone instructions for bystander CPR have recently been published (Bobrow 2010; Svensson 2010; SOS‐KANTO Group 2007). Although there have been studies supporting the effects of continuous chest compression‐only CPR, others have shown that worse outcomes were obtained by the use of continuous chest compression‐only CPR compared to conventional interrupted chest compression with pauses for breathing CPR (Ogawa 2011; Travers 2010). Differences in study design and quality make the interpretation challenging.
For professional CPR providers, however, hyperventilation during CPR was identified as a relevant issue (Aufderheide 2004). Continuous chest compression‐only CPR may accordingly have a very different meaning here. Moreover, even if continuous chest compression‐only CPR proves effective, details on continuous chest compression‐only CPR performance, teaching and communication remain to be elucidated. And for professional CPR providers, if they could get an AED nearby, the time of the AED arrival would directly affect the outcome of the victim.
The first review on continuous chest compression‐only CPR was published in the Lancet (Hüpfl 2010). We consider that a Cochrane Review will help us to further examine the effectiveness of continuous chest compression‐only CPR versus conventional interrupted chest compression with pauses for breathing CPR.
Objectives
To assess the effects of continuous chest compression CPR (with or without rescue breathing), versus conventional CPR plus rescue breathing ( interrupted chest compression with pauses for breaths) of non‐asphyxial OHCA.
Methods
Criteria for considering studies for this review
Types of studies
We included all randomized, quasi‐randomized, and cluster‐randomized trials that compared the effects of continuous chest compression CPR (with or without rescue breathing)and conventional CPR plus rescue breathing (interrupted chest compression with pauses at a fixed ratio provided by rescuers (bystanders or professional CPR providers) for out‐of‐hospital cardiac arrest.
We excluded simulation studies on mannequins or other instruments related to this topic.
Types of participants
We included adults and children suffering from out‐of‐hospital cardiac arrest due to any cause.
Types of interventions
We considered continuous chest compression CPR (with or without rescue breathing) provided by rescuers to be the intervention group and conventional CPR plus rescue breathing ( interrupted chest compression with pauses at a fixed ratio (standard CPR recommended by the guidelines (AHA 2000; AHA 2005; AHA 2010; Handley 2005) as the control group.
The review question is addressed by two separate comparisons.
Bystander‐administered continuous chest compression CPR only versus interrupted chest compression plus artificial ventilation for an out‐of‐hospital cardiac arrest.
Emergency service personnel‐administered continuous chest compression with asynchronous ventilation versus interrupted chest compression plus artificial ventilation following dispatch to an out‐of‐hospital cardiac arrest.
Types of outcome measures
Primary outcomes
Survival to hospital discharge.
Survival to hospital admission, where a successful hospital admission was defined as a patient admitted to hospital with spontaneous circulation and measurable blood pressure, with or without vasopressors (Cummins 1991).
Secondary outcomes
Survival at one year, core data which Utstein Style recommend, and many studies routinely collect (Cummins 1991).
Neurological outcomes at hospital discharge and at one year, as neurological outcome was a measurement of brain function, the main vulnerable organ of cardiac arrest, measured by Cerebral Performance Category and overall performance category.
Return of spontaneous circulation (ROSC), where a detectable palpable pulse was an indication of ROSC, a useful outcome in intervention studies (Cummins 1991).
Quality of life (also health‐related quality of life), measured with the 136‐item self‐reporting Sickness Impact Profile, or the Health Utilities Index Mark 3, or other patient‐reported outcome scales.
Any adverse effects of an intervention.
Search methods for identification of studies
Electronic searches
We searched the following databases: the Cochrane Central Register of Controlled trials (CENTRAL; Issue 1 2017, see Appendix 1); MEDLINE (Ovid) (from 1985 to February 2017, see Appendix 2); Embase via Ovid (1985 to February 2017, see Appendix 3); and Web of Science (1985 to February 2017, see Appendix 4). We will base the search strategies for all other databases on the MEDLINE strategy.
We searched ongoing trials databases including controlledtrials.com and clinicaltrials.gov.
We will not impose any language or publication restrictions.
Searching other resources
We searched conference proceedings of important meetings and abstracts including the American Heart Association (AHA), European Resuscitation Council (ERC), American College of Cardiology, European Society of Cardiology, American Academy of Emergency Medicine, Society for Academic Emergency Medicine, Society of Critical Care Medicine, and European Society of Intensive Care Medicine. We searched the reference lists of International Liaison Committee on Resuscitation (ILCOR) evidence worksheets, and we contacted experts in order to identify unpublished research and trials. The search was completed in January 2016.
Data collection and analysis
Selection of studies
Two authors (YH and LZ) independently abstracted data from the results from the search methods above. We independently decided which articles would be included through assessing the titles and abstracts. An eligible study should have at least one of the outcomes defined above. We then read the articles thoroughly and extracted the necessary information. We recorded the information in the study selection form (Appendix 5). We resolved disagreements through discussion. If we did not reach a consensus, then we consulted a third review author (HQ). We also contacted the author of the relevant article to resolve the disagreement. If several articles were associated with one study, we chose one article which reported adequate data; if they contained mutual data, we combined the data sets together as one study.
Data extraction and management
We (LZ and YH) independently extracted and collected the data in a data extraction form (Appendix 6). We were not blinded to the author, institution, or the publication source of trials. We resolved disagreements by discussion. A third review author (QH) helped to resolve any discrepancies that the screening review authors did not deal with. We approached all corresponding authors of the included trials for additional information on the review's outcome measures and risk of bias components. For more specific information please see Contributions of authors.
Assessment of risk of bias in included studies
We (LZ and YH) judged the study quality from the risk of bias using Cochrane's tool for assessing risk of bias (Higgins 2011) (Appendix 7). We also assessed the methodological quality of included studies from four aspects, as described by Jüni 2001: selection bias, biased allocation to comparison groups; performance bias, unequal provision of care apart from treatment under evaluation; detection bias, biased assessment of outcome; and attrition bias, biased occurrence and handling of deviations from protocol and loss to follow‐up. We resolved any disagreements through discussion with a third author (QH). We displayed the results by creating a 'Risk of bias' graph and a 'Risk of bias' summary figure using Review Manager 5 software, if appropriate (RevMan 2014). We presented the risk of bias in the results section. We provided summary assessments of the risk of bias for each outcome, within and across studies.
We defined:
low risk of bias as plausible bias unlikely to seriously alter the results;
unclear risk of bias as plausible bias which raises some doubts about the results; and
high risk of bias as plausible bias that seriously weakens confidence in the results (Higgins 2011).
Measures of treatment effect
We used the risk ratio (RR) with 95% confidence interval (CI) to measure dichotomous outcome data. We used the adjusted risk difference and adjusted mean difference presented in the trial report for the cluster‐RCT (Nichol 2015).
Unit of analysis issues
We included a cluster‐RCT. We decided whether the method and analysis used in cluster‐randomized design was appropriate. We critically appraised whether the authors of the cluster‐RCT performed analysis on an individual level accounting for clustered randomization. As the data from the cluster‐RCT were not combined with any other study data, we used the adjusted risk difference presented in the trial report (Nichol 2015). In future updates we will consider methods for calculating effective sample sizes. None of the included studies had multiple treatment groups, although we planned to adopt the recommendations of the Cochrane Handbook for Systematic Review of Interventions (Higgins 2011) (either combine the groups to create a single pair‐wise comparison or select one pair of groups and exclude the other groups).
Dealing with missing data
We contacted the first authors and contacted persons of the trials with missing data in order to retrieve the relevant data. We inputted the missing data with replacement values and treated these as if they were observed. If the authors performed an intention‐to‐treat (ITT) analysis, we judged the detailed information provided by the study and decided whether the ITT was correct. If not, we created an ITT analysis (as far as possible) from information presented in the text or by obtaining extra information from the study author or by using imputation.
Assessment of heterogeneity
We addressed clinical heterogeneity through detailed depicting of the characteristics of the included studies (for example, participant age, sex, the training level of the rescuers, or the different emergency medical service systems. Provided that data were homogeneous enough to be combined, we performed a meta‐analysis for all the included studies. We assessed the risk of bias and this served to detect the methodological heterogeneity. We used the Chi2 test to evaluate whether heterogeneity exists; P < 0.1 would be considered as statistically significant. We used the I2 statistic to quantify the inconsistencies. If the I2 statistic was greater than 40%, we considered the heterogeneity to be important (Higgins 2011).
Assessment of reporting biases
We planned to use a funnel plot analysis to examine publication bias if a minimum number of 10 studies were included in the review. However, this review only included four trials, and so we did not include a funnel plot. We planned to use the statistical methods proposed by Rucker 2008 to test funnel plot asymmetry.
Data synthesis
After assessment of heterogeneity and if appropriate, we used pooled RRs (dichotomous outcomes) and 95% CIs to perform a meta‐analysis, which was a method to summarize the effects across studies. We used the I2 statistic to estimate the heterogeneity and then decided which model we would use. If the I2 statistic was less than 40%, we considered that the heterogeneity might not be important and we would choose the fixed‐effect model meta‐analysis, which ignored the variability in different studies. The results of the fixed‐effect model represented the best estimate of the continuous chest compression‐only CPR compared to the conventional interrupted chest compression CPR effect, which did not actually exist in any population. If the I2 statistic was more than 40%, a random‐effects model meta‐analysis might be more appropriate. The pooled estimates in the random‐effects model presented the average effect of continuous chest compression‐only CPR compared to conventional interrupted chest compression CPR. We used Review Manager 5 to perform the analysis (RevMan 2014).
Subgroup analysis and investigation of heterogeneity
If there were sufficient studies, we planned to split the participants into adults and children in order to perform subgroups analysis. We planned to do subgroup analysis according to different basic aetiologies, different settings (rural and urban) and different providers' level of training (untrained layperson, trained layperson and healthcare provider).
Sensitivity analysis
To determine whether the findings of the systematic review were influenced by arbitrary or unclear decisions, we planned to perform sensitivity analyses as follows.
Exclude studies with large weight.
Exclude high risk of bias trials.
Use non‐ITT data and ITT data in the analyses.
Use fixed‐effect and random‐effects model analyses.
We decided not to exclude studies on the basis of bias since they were at low risk of bias for the domains of interest and we decided not to explore the effect of different analysis populations on the results for the outcomes of interest since this was available for only one study.
'Summary of findings' table and GRADE
We used the GRADE approach to assess the quality of the body of evidence (Guyatt 2008). We presented evidence for the following outcomes in two 'Summary of findings' tables.
Survival to hospital discharge.
Survival to hospital admission.
Survival at one year.
Neurological outcomes at hospital discharge and at one year (if available).
Return of spontaneous circulation.
Adverse effects
Quality of life
We prepared two 'Summary of findings' tables to present findings for the comparison of different CPR types for bystander‐continuous chest compression without rescue breathing versus interrupted compression with fixed ratio rescue breathing (15: 2) Table 1; and for professional‐provided CPR: continuous chest compression (100/min) with asynchronous rescue breathing (10/min) versus interrupted chest compression with fixed ratio rescue breathing (30: 2) Table 2
Summary of findings for the main comparison. Continuous chest compression alone compared to interrupted chest compression plus artificial ventilation for out‐of‐hospital cardiac arrest.
| Continuous chest compression alone compared to interrupted chest compression plus artificial ventilation for non asphyxial out‐of‐hospital cardiac arrest | ||||||
|
Patient or population: People with non‐trauma related out‐of‐hospital cardiac arrest
Settings: Urban settings in the USA, UK and Sweden (CPR performed by untrained bystanders)
Intervention: Continuous chest compression alone Comparison: Interrupted chest compression plus ventilation | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Interrupted chest compression plus ventilation | Continuous chest compression alone | |||||
| Survival to hospital discharge | 116 per 1000 | 141 per 1000 (117 to 170) | RR 1.21 (1.01 to 1.46) | 3031 (3 studies) | ⊕⊕⊕⊕ High1 | |
| Survival to hospital admission | 341 per 1000 | 402 per 1000 (320 to 504) |
RR 1.18 (0.94 to 1.48) |
520 (1 study) | ⊕⊕⊕⊝ Moderate2 | |
| Survival at one year | See comment | See comment | Not estimable | 0 (0) | See comment | No data available for this outcome |
|
Neurological outcomes at hospital discharge Measured as 'good' or 'moderate' with Cerebral Performance Category classification |
110 per 1000 | 138 per 1000 (103 to 183) |
RR 1.25 (0.94 to 1.66) |
1286 (1 study) | ⊕⊕⊕⊝ Moderate2 | 2/3 sites reported data for this outcome in Rea 2010 |
| Return of spontaneous circulation | See comment | See comment | Not estimable | 0 (0) | See comment | No data available for this outcome |
| Adverse effects | No adverse events were reported | Not estimable | 0 (0) | See comment | No data available for this outcome | |
| Quality of life | See comment | See comment | Not estimable | 0 (0) | See comment | No data available for this outcome |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; CPR: cardiopulmonary resuscitation; RR: risk ratio. | ||||||
| GRADE Working Group grades of evidence High‐quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate‐quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low‐quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low‐quality: We are very uncertain about the estimate. | ||||||
1 Not downgraded for risk of bias. Although the nature of the studies meant that study personnel, including dispatchers and bystanders would be aware of which mode of cardiopulmonary resuscitation (CPR) was administered, we do not believe that this would have affected survival outcomes. 2 We downgraded one level of the evidence due to imprecision because the total number of events was small.
Summary of findings 2. Continuous chest compression plus ventilation compared to interrupted chest compression plus ventilation for people with non asphyxial out‐of‐hospital cardiac arrest.
| Continuous chest compression plus ventilation compared to interrupted chest compression plus ventilation for patients with non asphyxial out‐of‐hospital cardiac arrest | ||||||
| Patient or population: Patients with non‐trauma related out‐of‐hospital cardiac arrest Settings: Urban settings in the USA and Canada (CPR performed by emergency medical staff) Intervention: Continuous chest compression with asynchronous rescue breathing Comparison: Interrupted chest compression plus ventilation | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) |
Risk Differences (95% CI) |
No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| interruptedchest compression plus ventilation | Continuous chest compression with asynchronous rescue breathing | |||||
| Survival to hospital discharge | 97 per 1000 | 90 per 1000 (82 to 98) |
ARD ‐0.7% (‐1.5% to 0.1%) |
23,648 (1 study) | ⊕⊕⊕⊝ Moderate1, 2 | |
| Survival to hospital admission | 259 per 1000 | 246 per 1000 (235 to 257) |
ARD ‐1.3% (‐2.4% to ‐0.2%) |
23,711 (1 study) | ⊕⊕⊕⊕ High1 | |
| Survival at one year | See comment | See comment | Not estimable | 0 (0) | See comment | No data available for this outcome |
| Neurological outcomes at hospital discharge (Rankin score ≤ 3) | 77 per 1000 |
70 per 1000 (56 to 78) |
ARD ‐0.6% (‐1.4% to 0.1%) |
23,555 (1 study) |
⊕⊕⊕⊕ High |
|
| Return of spontaneous circulation | 253 per 1000 | 242 per 1000 (230 to 255) |
ARD ‐1.1% (‐2.4% to 0.1%) |
23,697 (1 study) | ⊕⊕⊕⊕ High3 | |
|
Adverse effects Defined as any adverse event occurring post‐admission |
554 per 1000 |
544 per 1000 (540 to 567) |
ARD ‐1.0% (‐2.3% to 0.4%) |
23,711 (1 study) | ⊕⊕⊕⊝ Moderate2 | |
| Quality of life | See comment | See comment | Not estimable | 0 (0) | See comment | No data available for this outcome |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; CPR: cardiopulmonary resuscitation; ARD: adjusted risk difference. | ||||||
| GRADE Working Group grades of evidence High‐quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate‐quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low‐quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low‐quality: We are very uncertain about the estimate. | ||||||
1 Not downgraded for risk of bias. Although the nature of the studies meant that study personnel would be aware of which mode of CPR was administered, we do not believe that this would have affected survival outcomes.
2 Downgraded one level due to imprecision. The confidence interval of the absolute effect estimate includes little or no difference between the two interventions.
3 We did not downgrade return to spontaneous rhythm for imprecision because the confidence interval excluded a meaningful increase in the likelihood of this event with continuous chest compressions.
The GRADE approach appraises the quality of a body of evidence based on the extent to which one can be confident that an estimate of effect or association reflects the item being assessed. The quality of a body of evidence considers within study risk of bias, the directness of the evidence, heterogeneity of the data, precision of effect estimates, and risk of publication bias.
Results
Description of studies
See: Figure 1; Characteristics of included studies; Characteristics of excluded studies.
1.
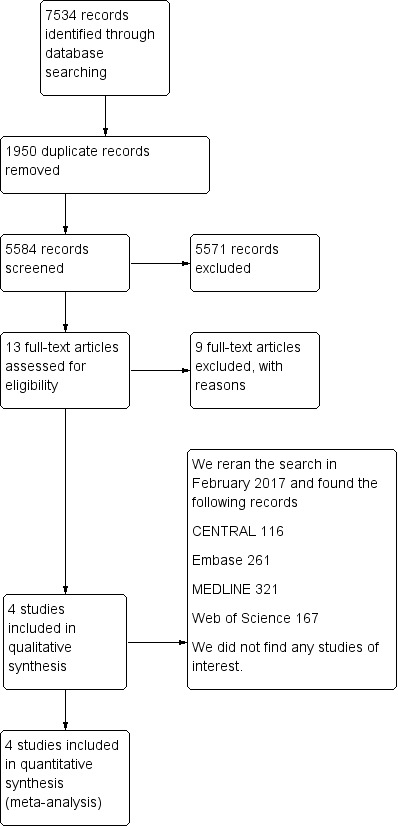
Study flow diagram.
Results of the search
We originally ran the searches in January 2016, we found 7534 records. From those 7534 records, we excluded 1950 duplicates. We excluded a further 5571 papers by judging the abstract or the title, as they did not fit our eligibility criteria (randomized, quasi‐randomized and cluster‐randomized trials that compared the effects of continuous chest compression and interrupted compression plus artificial ventilation in CPR provided by rescuers for out‐of hospital cardiac arrest). We found one ongoing study of interest (NCT02401633). Thirteen papers remained for closer inspection of the full‐text. From those 13 papers, we excluded five observational studies, three review articles, and one mannequin study. We included three RCTs in our review (Hallstrom 2000; Rea 2010; Svensson 2010), and one cross‐over cluster‐randomized trial (Nichol 2015). We reran the search in February 2017 and found the following records: CENTRAL 116; Embase 261; MEDLINE 321 and Web of Science 167; we did not find any studies of interest.
Included studies
We included three RCTs and one cluster‐RCT in our review. A total of 29,885 participants were included in the four trials, but only 26,742 participants were included for analysis in our review. One of the trials was undertaken in the USA (Hallstrom 2000), a second in Sweden (Svensson 2010),a third in both the USA and the UK (Rea 2010), and the fourth in both the USA and Canada (Nichol 2015).
All four trials included out‐of‐hospital cardiac arrest. In three trials CPR was delivered by bystanders (Hallstrom 2000; Rea 2010; Svensson 2010), and in one trial CPR was delivered by emergency medical service providers (Nichol 2015). We excluded participants who arrested due to non‐cardiac reasons, such as drug overdose, alcohol intoxication or trauma. One trial enrolled adult participants (Rea 2010), the second enrolled participants who were equal to, or older than eight years of age (Svensson 2010), and two trials provided no information regarding the age of the participants (Hallstrom 2000; Nichol 2015). The mean age (years) of the continuous chest compression group was 67.9 in Hallstrom 2000, 68 in Svensson 2010, 63.4 in Rea 2010, and 66.4 in Nichol 2015. The mean age (years) of the interrupted chest compression plus artificial ventilation group was 68.5 in Hallstrom 2000, 67 in Svensson 2010, 63.9 in Rea 2010, and 66.2 in Nichol 2015.
Interventions in the bystander‐provided CPR trials
In the three trials (Hallstrom 2000; Rea 2010; Svensson 2010), when the dispatchers received calls about suspected out‐of‐hospital cardiac arrest recognized by bystanders, they (the dispatchers) ascertained whether the patients met the inclusion criteria by communicating with the bystanders. In one trial (Rea 2010), a further postrandomization assessment of eligibility was performed by the emergency medical service personnel when they arrived. Participants with signs of irreversible arrest, or those considered not to be in arrest at this stage, were excluded from the study. This was because the emergency medical service personnel would not provide CPR for these participants (Rea 2010).
In all three trials (Hallstrom 2000; Rea 2010; Svensson 2010), when the dispatcher determined the participants' eligibility, and that the bystanders were willing to be instructed, the dispatcher then gave the bystanders instructions via the telephone on either continuous chest compression‐only CPR or conventional (interrupted chest compression with pauses at a fixed rate for rescue breathing) CPR.
In the intervention group, continuous chest compressions were performed without rescue breathing. In the control group, interrupted chest compressions plus rescue breathing were performed in a ratio of 2 to 15 (Hallstrom 2000; Rea 2010; Svensson 2010). In all three trials, CPR was performed by bystanders who had not been trained (Hallstrom 2000; Rea 2010; Svensson 2010). Other follow‐up treatments performed by emergency medical service personnel or emergency physicians were not detected in the three trials (Hallstrom 2000; Rea 2010; Svensson 2010).
All three trials reported survival to hospital discharge (Hallstrom 2000; Rea 2010; Svensson 2010).
Rea 2010 reported a favourable neurologic status at the time of hospital discharge, defined as a Cerebral Performance Category of 1 or 2. However, one study site (the author did not provide information on which site) was unable to assess the participants' neurologic status at discharge, so for this outcome, the author restricted presentation of the results to the two sites that were able to ascertain neurologic status.
Hallstrom 2000 reported admission to hospital. They also reported the neurological status in the survivors, however, they did not describe whether or not the neurologic status was measured by the Cerebral Performance Category.
Interventions in the professional‐provided CPR trial
In Nichol 2015, the author assessed whether outcomes after continuous chest compressions with positive‐pressure ventilation differed from interrupted compressions that were interrupted for ventilations at a ratio of 30 compressions to two ventilations. In the intervention group, participants received continuous chest compressions at a rate of 100 compressions per minute, with asynchronous positive‐pressure ventilations delivered at a rate of 10 ventilations per minute. In the control group, participants received compressions that were interrupted for ventilations at a ratio of 30 compressions to two ventilations; ventilations were to be given with positive pressure during a pause in compressions of less than 5 seconds in duration (Nichol 2015).
The primary outcome in Nichol 2015 was the rate of survival to hospital discharge. Secondary outcomes included survival to hospital admission, neurologic function at discharge (modified Rankin scale), return of spontaneous circulation at emergency department arrival, and adverse events.
Of 23,711 participants included in this study (Nichol 2015), the author found that in participants with out‐of‐hospital cardiac arrest, continuous chest compressions during CPR, with asynchronous rescue breathing, performed by emergency medical service providers did not result in significantly higher rates of survival or favourable neurologic function than did interrupted chest compressions and fixed ratio rescue breathing, and hospital‐free survival was significantly shorter in the continuous chest compressions group than in the interrupted chest compressions group.
See Table 3
1. The essential features of the intervention and comparator in the four included studies.
| Study | Caregiver | Intervention | Control |
| Hallstrom 2000 | Untrained (bystander) | Continuous compression without rescue breathing | Interrupted compression with Fixed ratio rescue breathing (15:2) |
| Nichol 2015 | Trained (EMT) | Continuous compression (100/min) with asynchronous rescue breathing (10/min) | Interrupted compression with fixed ratio rescue breathing (30:2) |
| Rea 2010 | Untrained (bystander) | Continuous compression without rescue breathing | Interrupted compression with fixed ratio rescue breathing (15:2) |
| Svensson 2010 | Untrained (bystander) | Continuous compression without rescue breathing | Interrupted compression with fixed ratio rescue breathing (15:2) |
Excluded studies
We excluded nine studies, five of which were observational studies (Bohm 2007; Bobrow 2010; Crane 2008; Kitamura 2010; Ong 2008); their characteristics are listed in the table Characteristics of excluded studies.
Studies awaiting classification
There are no studies awaiting classification.
Ongoing studies
There is one ongoing study (NCT02401633). Please see the Characteristics of ongoing studies table for more information.
Risk of bias in included studies
The assessment of risk of bias is shown in the Characteristics of included studies table and in Figure 2.
2.
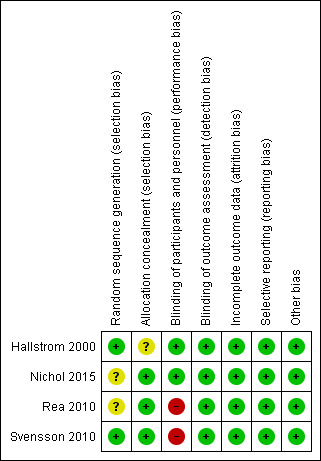
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
Two trials reported that the randomized number sequence was generated by a computer (Hallstrom 2000; Svensson 2010). The third trial did not describe how randomization was generated (Rea 2010). We considered two trials to have adequate allocation concealment (Rea 2010; Svensson 2010). In Rea 2010, a sealed envelope containing the CPR instructions was opened by the dispatcher after receiving the call and assessing the eligibility. In Svensson 2010, the type of CPR, with which the caller was instructed, was determined on the basis of the next available data collection sheet for each dispatcher, who removed a paper strip covering the treatment assignment on the sheet after determining that the inclusion criteria had been met. In Hallstrom 2000, it was reported that the allocation was determined by a microcomputer located at the dispatcher's console. We considered there to be an unclear risk of selection bias in Hallstrom 2000, as no further information was stated.
Nichol 2015, did not describe how randomization was generated, but allocation was concealed. Clusters of agencies in the trial were randomly assigned, in a 1:1 ratio to perform continuous chest compressions or interrupted chest compressions during all the out‐of‐hospital cardiac arrests to which they responded. Twice per year (Nichol 2015), each cluster was crossed over to the other intervention.
Blinding
In one trial (Hallstrom 2000), the emergency medical service personnel and the emergency physicians were blinded. The emergency medical service personnel and other physicians were not blinded in the other two trials examining bystander CPR (Rea 2010; Svensson 2010). In all three trials the bystanders were not blinded, but they did not know that they were recruited into the trial, so we considered that this would not have had an important effect on the outcomes. As the participants were unconscious and were not breathing normally, we considered that the blinding of the participants would not affect the outcomes. Thus, we considered there to be a low risk of performance bias for Hallstrom 2000 and a high risk of performance bias for the remaining two trials (Rea 2010; Svensson 2010).
Two trials reported blinded outcome assessment (Hallstrom 2000; Rea 2010). In one trial (Svensson 2010), data were collected from emergency medical service records, and information about survival status was collected from national registers. Although there was no description about blinding in the Svensson 2010 trial, 50% of the data collection forms were double‐checked and no relevant deviations were observed. In addition, the researchers evaluated 100 recorded calls and reviewed the corresponding data collection forms, finding no deviation of the information in each (Svensson 2010). Thus, we considered the three trials to be at a low risk of detection bias.
Nichol 2015 was an unblinded trial; the providers of CPR in each cluster knew that they were recruited in this study, so this might have performance bias. But in this trial, once a cluster was able to demonstrate proficiency with the given treatment by meeting prespecified performance and compliance benchmarks, as determined by the Study Monitoring Committee, they were progressed into the Active Enrolment Phase, if one cluster was unable to meet benchmarks after six months, it was subsequently dropped from the trial. Since the participants were unconscious and not breathing normally, we considered that the blinding of the participants would not affect the outcomes. So we considered performance bias as low, even though the providers of CPR in each cluster were unblinded.
In Nichol 2015, an interdisciplinary study monitoring committee periodically reviewed data masked to treatment outcome. This committee met at least monthly throughout the enrolment period of the trial, and had authority to require an emergency medical service agency to improve its study performance, or to place an agency on probation until performance improved, or to suspend an agency from ongoing enrolment in the trial. So we considered the detection bias in this trial as low.
Incomplete outcome data
In Hallstrom 2000, the data of two participants were missing. In Rea 2010, the missing data in both groups was 1.7%. In Svensson 2010, the percentage of missing data was 6.8%, furthermore the authors performed a subgroup analysis excluding districts where more than 18% of the participants were lost to follow‐up. No difference from the main results was found. In Nichol 2015, data regarding the primary outcome were available for 99.7% of the intervention group and 99.8% of the control group. Thus, we considered the four trials as being at a low risk of attrition bias.
Selective reporting
The core outcomes of out‐of‐hospital cardiac arrest patients recommended by the Utstein Style were reported in all four trials (Cummins 1991). So we considered the four trials to be at a low risk of reporting bias.
Other potential sources of bias
We did not find any other potential sources of bias (such as conflicts of interest) in the four included trials.
Effects of interventions
Primary outcomes
1. Survival to hospital discharge
Bystander‐provided CPR
(See: Analysis 1.1; Figure 3; Table 1).
1.1. Analysis.
Comparison 1 Bystander‐provided CPR, Outcome 1 Survival to hospital discharge.
3.
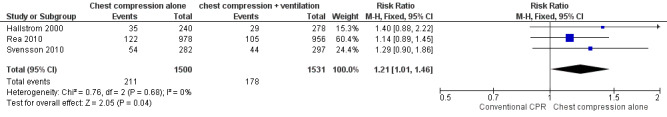
Forest plot of comparison: Bystander‐provided CPR , outcome: 1.1 Survival to hospital discharge.
All three trials in the bystander‐provided CPR comparison reported survival to hospital discharge (Hallstrom 2000; Rea 2010; Svensson 2010). There were 1500 participants recruited in the intervention group, and 1531 in the control group. There were no significant differences between the two groups in the trials. The pooled result showed better survival for the continuous chest compression alone group (risk ratio (RR) 1.21, 95% confidence interval (CI) 1.01 to 1.46; Chi² = 0.76, df = 2 (P = 0.68); I² statistic = 0%, 3 trials, 3031 participants, high‐quality evidence).
Professional‐provided CPR
(See: Table 4; Analysis 2.1; Table 2).
2. Professional provided CPR.
| Outcome | Continuous chest compression with asynchronous rescue breathing (raw data as provided in trial report) | Interrupted chest compression plus ventilation (raw data as provided in trial report) |
| Survival to hospital discharge (n/total n (%)) | 1129/12,613 (9.0) | 1072/11,035 (9.7) |
| Survival to hospital admission (n/total n (%)) | 3108/12,653 (24.6) | 2860/11,058 (25.9) |
| Neurological outcomes at hospital discharge (measured with modified Rankin scale ≤3) — (n/total n (%)) | 883/12,560 (7.0) | 844/10,995 (7.7) |
| Return of spontaneous circulation at ED arrival (n/total n (%)) | 3058/12,646 (24.2) | 2799/11,051 (25.3) |
| Adverse events (n/total n(%)) | 6889/12653 (54.4) | 6127/11058 (55.4) |
Data taken from Table 3 and from supplementary material provided in Nichol 2015.
Abbreviations and acronyms
ED: emergency department
n: number
Scores on the modified Rankin scale 3 or less indicates a favourable neurological function (0 indicates no symptoms and 6 indicates death).
2.1. Analysis.
Comparison 2 Professional‐provided CPR, Outcome 1 Survival to hospital discharge.
The one cluster‐RCT in the professional‐provided CPR (Nichol 2015) reported survival to hospital discharge on 12,613 participants recruited to the intervention group and 11,035 recruited in the control group. The difference in survival (9.0% versus 9.7%) did not achieve statistical, survival in the continuous compression group being lower with an ARD of ‐0.7% (95% CI ‐1.5% to 0.1%; P = 0.07, moderate‐quality evidence due to imprecision).
2. Survival to hospital admission
Bystander‐provided CPR
(See: Analysis 1.2; Table 1).
1.2. Analysis.
Comparison 1 Bystander‐provided CPR, Outcome 2 Survival to hospital admission.
Only one trial reported this outcome (Hallstrom 2000). The result showed no significant difference between the two groups (RR 1.18, 95% CI 0.94 to 1.48); 1 trial, 520 participants). We judged the evidence to be of moderate‐quality for this outcome due to imprecision.
Professional‐provided CPR
(See: Analysis 2.2; Table 2).
2.2. Analysis.
Comparison 2 Professional‐provided CPR, Outcome 2 Survival to hospital admission.
This outcome was reported for 12,653 participants to the intervention group and 11,058 to the control group (Nichol 2015). There was no significant difference (ARD ‐1.3% (95% CI ‐2.4% to ‐0.2%; P = 0.03, high‐quality evidence).
Secondary outcomes
1. Survival at one year
We found no data on this outcome.
2. Neurological outcomes at hospital discharge and at one year
Bystander‐provided CPR
(See: Analysis 1.3; Table 1).
1.3. Analysis.
Comparison 1 Bystander‐provided CPR, Outcome 3 Neurological outcomes at hospital discharge (measured with Cerebral Performance Category classification).
Only one trial reported neurological outcomes at hospital discharge (Rea 2010); the results showed no significant differences between the two groups in the number of patients with a Cerebral Performance Category classification of 1 (good cerebral performance) or 2 (moderate cerebral disability) (RR 1.25, 95% CI 0.94 to 1.66); 1 trial, 1286 participants, moderate‐quality evidence due to imprecision.
Professional‐provided CPR
(See: Analysis 2.3; Table 2).
2.3. Analysis.
Comparison 2 Professional‐provided CPR, Outcome 3 Neurological outcome at hospital discharge (Rankin score ≤ 3).
The Nichol 2015 cluster‐RCT measured this outcome using the modified Rankin scale (score 0 = no symptoms to 6 = death; score ≤ 3 indicates favourable neurological function). This outcome was reported for 12,560 participants recruited to the intervention group and 10,995 in the control group. The ARD (Rankin score ≤ 3) showed no significant difference (‐0.06% (95% CI 0.0% to 0.08%; P = 0.09, high‐quality evidence).
3. Return of spontaneous circulation
Bystander‐provided CPR
We found no data for this outcome.
Professional‐provided CPR
(See: Table 2).
The Nichol 2015 cluster‐RCT reported this outcome in 12,646 participants recruited to the intervention group and 11,051 in the control group. Those receiving continuous chest compression plus asynchronous rescue breathing were less likely to experience a return to spontaneous circulation (ARD ‐1.1% (95% CI ‐2.4% to 0.1%; P = 0.07, high‐quality evidence).
4. Quality of life
We found no data for this outcome.
5. Adverse effects
Bystander‐provided CPR
No adverse effects were reported.
Professional‐provided CPR
(See: Analysis 2.5; Table 2).
2.5. Analysis.
Comparison 2 Professional‐provided CPR, Outcome 5 Adverse events.
The Nichol 2015 cluster‐RCT reported that there was no significant difference between the two treatment groups in the rates of individual adverse events. Rates of adverse events were 54.4% in those treated with continuous chest compressions plus asynchronous rescue breathing versus 55.4% in people treated with interrupted chest compression plus rescue breathing, with the ARD being ‐1% (‐2.3 to 0.4, moderate‐quality evidence).
Subgroup analysis
We planned to perform a subgroup analysis according to the age of the victims, and so we contacted the authors of the trials by e‐mail in order to obtain the individual data. However no further data was forthcoming from the study authors. None of the three trials were performed in a rural setting, so we did not perform a subgroup analysis according to rural and urban settings. The bystanders in all three trials were untrained.
Sensitivity analysis
We conducted a sensitivity analysis by using different models; as would be expected with the low level of statistical heterogeneity the pooled results for survival to hospital discharge were identical with the random‐effects and the fixed‐effect models.
We performed a sensitivity analysis by excluding the trial with a large weight (Rea 2010). The pooled results were similar when this trial was excluded (RR 1.33, 95% CI 1.00 to 1.77).
Publication bias
There were too few trials to enable us to draw inferences from funnel plots (less than 10), so we did not present them in the current version of this review.
Discussion
Summary of main results
We identified four trials which evaluated the effect of continuous chest compression CPR versus conventional (interrupted chest compression) CPR for OHCA (Hallstrom 2000; Nichol 2015; Rea 2010; Svensson 2010). A total of 26,742 participants were enrolled for analysis in the four trials. Three trials were RCTs, in which CPR was delivered by bystanders (Hallstrom 2000; Rea 2010; Svensson 2010), and one trial was a cluster‐RCT, in which CPR was delivered by emergency medical service providers (Nichol 2015). All trials reported the primary outcomes of survival to hospital discharge and survival to hospital admission. Loss to follow‐up in all trials was within an acceptable range.
Pooled data from three trials of bystander‐initiated CPR showed an increase in the number of people surviving to hospital discharge from 11.6% to 14% when continuous chest compression‐only CPR was used compared with interrupted chest compression plus ventilation (Hallstrom 2000; Rea 2010; Svensson 2010). Only one trial reported the outcome of survival to hospital admission (Hallstrom 2000), and one trial reported neurological outcomes at hospital discharge (Rea 2010); we found no significant differences between the two treatment groups (see: Analysis 1.2; Analysis 1.3).
Only one trial involved CPR performed by emergency medical service providers (Nichol 2015). Nichol 2015 reported that continuous chest compressions plus asynchronous rescue breathing did not result in significantly higher rates of survival compared to interrupted chest compressions plus ventilation. The result showed a statistically significant difference between the two groups in survival to hospital admission (risk difference (RD) ‐1.3, 95% confidence interval (CI) ‐2.4% to ‐0.2%). There were no significant differences between the two treatment groups in neurological outcomes at hospital discharge (RD 0.04, 95% CI 0.00% to 0.08%) and the rate of return of spontaneous circulation (RD ‐1.1, 95% CI ‐2.4% to 0.2%). Nichol 2015 also showed that there was no significant difference between the two treatment groups in the rates of individual adverse events.
Overall completeness and applicability of evidence
All four trials included out‐of‐hospital cardiac arrest, but excluded asphyxial arrests (Hallstrom 2000; Rea 2010; Svensson 2010; Nichol 2015). Furthermore, the four trials included the common first cardiac rhythm of the participants who suffered cardiac arrest, such as ventricular fibrillation, asystole, pulseless electrical activity and ventricular tachycardia etc. We identified no data on return to spontaneous rhythm or long‐term outcomes following bystander‐initiated CPR (Table 1). Limited information was reported on adverse events.
Although the advanced life support methods were performed according to different guidelines respectively, we felt that such clinical heterogeneity was negligible because no evidence has been found to demonstrate that there was any effect of different guidelines on the clinical therapy. All four trials in our review were performed in urban settings. The mean intervals from call to emergency medical service arrival varied from 4.0 to 10.3 minutes in the four trials (Hallstrom 2000; Nichol 2015; Rea 2010; Svensson 2010). Unfortunately, we do not have enough data to perform a posthoc analysis to assess the association between the time interval of emergency medical service arrival and outcomes.
Quality of the evidence
We did not downgrade the quality of the evidence due to risk of bias for survival to hospital discharge because the objective nature of the outcome means that it is unlikely to be influenced by the unblinded nature of the interventions for bystander administered CPR. We downgraded the quality of the evidence due to imprecision for two outcomes following bystander administered CPR in Table 1 where there were a low number of events and small sample sizes. Although the lower limit of the confidence interval for risk ratio for the outcome of survival to hospital discharge following bystander CPR is close to 1, the high rate of mortality in this population overall means that our confidence in the result is high. For the comparison of different CPR approaches administered by emergency medical staff, we downgraded the quality of evidence for survival to discharge and adverse effects due to imprecision. The confidence intervals were wide enough to justify the decision to adopt either resuscitation strategy (Table 2). We did not consider the studies or outcomes to be indirect and there was no obvious evidence of publication bias in this review, so we did not downgrade the quality of the evidence for any outcomes due to these limitations.
Potential biases in the review process
Whilst our searches are comprehensive, there may be completed, unregistered studies that our searches have not been able to identify. Our attempts to examine the effect of age on survival outcomes were unsuccessful, and this remains an uncertainty that future research should investigate. For most outcomes from the Nichol 2015 trial, we have used data for the ITT population in preference to that available for the safety population. Whilst results obtained with these populations were similar for adverse event data, the effect on survival attenuated slightly from a difference in risk of 0.7% to 0.2%.
Agreements and disagreements with other studies or reviews
When CPR was performed by bystanders, three observational studies addressed similar objectives to our review (Bohm 2007; Crane 2008; Ong 2008). Theobservational studies showed that there were no significant differences in the outcomes between the two treatment groups. The lay bystanders made the decision as to whether to give mouth‐to‐mouth ventilation or not, and perform CPR, without the dispatchers' assistance.
However, in another prospective cohort study conducted in Arizona (Bobrow 2010), there was a CPR training programme called the Save Hearts in Arizona Registry and Education (SHARE) programme. The bystanders in that study, who called emergency medical service when an out‐of‐hospital cardiac arrest had taken place, were mostly trained in the continuous CPR technique. The results of this study show that layperson compression‐only CPR is associated with an increased survival rate compared with conventional CPR, which is consistent with our pooled results. The result of this study (Bobrow 2010),was different to our review when CPR was performed by emergency medical service providers. The quality of compression cannot be monitored when CPR was performed by bystanders, we presume that even the bystanders were trained in CPR training program, the quality of compression was poorer than that performed by professional providers. The technique of COCPR was easer than conventional CPR, so we presume that when CPR was performed by bystanders which were trained in CPR program, the quality of compression in COCPR would be better than that in conventional CPR. But when CPR was performed by professional providers, the quality of compress may be the same in most time whatever in COCPR or conventional CPR. This may be the reason that the result of Bobrow 2010 was different from our review when CPR was performed by professional providers, but the same when CPR was performed by bystanders.
In our review, there were two subgroups: bystander‐provided CPR; and professional‐provided CPR. The results of the two subgroups in our review were different. We suspect that a reason for the difference was because of differences in the quality of the compression.
The Hüpfl 2010 review performed a meta‐analysis of continuous chest compression‐only CPR versus standard CPR for out‐of‐hospital cardiac arrest, and included the same three RCTs as our Cochrane Review. As expected, the pooled data showed similar findings to our own.
Authors' conclusions
Implications for practice.
According to our pooled results, when CPR was performed by untrained bystanders who were assisted by receiving telephone instruction from emergency services, continuous chest compression‐only CPR led to more people surviving to hospital discharge compared with interrupted chest compression plus artificial ventilation CPR for non asphyxial OHCA. The difference in survival to hospital discharge is about 25 more people per 1000 following bystander administered continuous chest compression. When CPR was performed by professional providers, continuous chest compressions with asynchronous rescue breathing did not result in higher rates of survival compared with interrupted chest compressions plus rescue breathing CPR for non asphyxial OHCA. The results indicate slightly lower rates of survival to admission or discharge, favourable neurological outcome and return of spontaneous circulation observed following continuous chest compression. Adverse effects were slightly lower with continuous chest compression.
Implications for research.
Our review has identified moderate or high quality evidence for short‐term survival outcomes in bystander‐initiated resuscitation, and high quality evidence for short‐term survival outcomes in professionally provided resuscitation. Future studies should include evaluations of adverse effects, and of longer‐term neurological outcomes and quality of life. The influence of automated external defibrillator (AED) availability and AED use on the effect of continuous chest compression CPR needs to be examined. Likewise, it remains unclear whether the concept of continuous chest compression CPR is appropriate for paediatric cardiac arrest. One ongoing study is addressing the question of feasibility in a smaller sample size to the studies we have identified in this review (NCT02401633).
What's new
| Date | Event | Description |
|---|---|---|
| 17 December 2018 | Amended | Editorial team changed to Cochrane Emergency and Critical Care |
Acknowledgements
We would like to thank Harald Herkner (content and statistical editor), Nathan Pace (Co‐ordinating Editor), Jane Cracknell (Managing Editor), Janne Vendt (Information Specialist), Gordon A Ewy, Sandra M Marini (peer reviewers), Janet Wale (consumer editor), Liz Bickerdike (CEU editor), Toby Lasserson (Senior CEU editor), Clare Dooley and Elizabeth Royle (Copy Edit Support) for their help and editorial advice during the preparation of this Cochrane Review.
We would also like to thank the following people for their help and advice during the preparation of the protocol for the review (Yang 2012): Jane Cracknell, Karen Hovhannisyan, Yaxin Yu, Marialena Trivella, Sandra Marini, Gordon Ewy, Marc Afilalo, Ian Jacobs Clare Jeffrey and the Cochrane Prehospital and Emergency Health Field.
Appendices
Appendix 1. CENTRAL search strategy
#1 MeSH descriptor: [Cardiopulmonary Resuscitation] explode all trees #2 (chest near compression):ti,ab or chest compression* or cardiac massage or resuscitat*:ti,ab or artificial ventilation or rescue breathing #3 MeSH descriptor: [Heart Massage] explode all trees #4 MeSH descriptor: [Respiration, Artificial] explode all trees #5 #1 or #2 or #3 or #4 #6 MeSH descriptor: [Heart Arrest] explode all trees #7 MeSH descriptor: [Death, Sudden] explode all trees #8 ((arrest or attack or stoppage) near (cardiac or cardiopulmonary or heart or circulatory or cardiocirculatory or respiratory)):ti,ab #9 #6 or #7 or #8 #10 #5 and #9
Appendix 2. MEDLINE search strategy
1. exp Cardiopulmonary Resuscitation 2. chest adj5 compression.mp. 3. chest compression$.tw. 4. Cpr.tw 5. Exp Heart massage 6.Cardiac massage.tw. 7. resuscitat$.mp. 8. exp Respiration, Artificial 9. artificial ventilation.tw. 10. Rescue breathing.tw. 11. or/1‐10 12. exp Heart Arrest 13. cardiac arrest.tw. 14. cardiopulmonary arrest.tw. 15. heart attack.tw. 16. heart stoppage.tw. 17. exp Death, Sudden 18. Circulatory arrest.tw. 19. cardiocirculatory arrest.tw. 20. respiratory arrest.tw. 21. or/12‐20 22. 11 and 21 23. ((randomized controlled trial or controlled clinical trial).pt. or randomized.ab. or groups.ab. or clinical trials as topic.sh. or randomly.ab. or trial.ti.) not (animals not (humans and animals)).sh. 24. 22 and 23
Appendix 3. Embase (Ovid) search strategy
1. resuscitation/ or (chest adj3 compression).ti,ab. or chest compression$.ti,ab. or Cpr.tw. or heart massage/ or cardiac massage.mp. or resuscitat$.ti,ab. or artificial ventilation/ or artificial ventilation.ti,ab. or rescue breathing.mp. 2. heart arrest/ or ((arrest or attack or stoppage) adj3 (cardiac or cardiopulmonary or heart or circulatory or cardiocirculatory or respiratory)).ti,ab. or sudden death/ 3. 1 and 2 4. (controlled study.ab. or random*.ti,ab. or trial*.ti.) not (animals not (humans and animals)).sh. 5. 3 and 4
Appendix 4. Web of Science search strategy
#1 TS=(chest compression) or TI=((cardiac or heart) SAME massage) or TI=resuscitat* or TS=artificial ventilation or TS=rescue breathing #2 TS=((arrest or attack or stoppage) SAME (cardiac or cardiopulmonary or heart or circulatory or cardiocirculatory or respiratory)) #3 #2 AND #1 #4 TS=(random* or ((controlled or clinical) SAME trial*) or placebo* or multicenter or perspective) #5 #4 AND #3
Appendix 5. Study selection form
| First author | Journal/conference proceedings etc. | Year | |
| Study eligibility | |||
| RCT/quasi‐RCTs/ cluster‐RCTs | Relevant participants (out‐of‐hospital cardiac arrest) | Relevant interventions (compression‐only CPR compare with conventional CPR for cardiac arrest) | Relevant outcomes (Survival to hospital discharge, survival to hospital admission, survival at one year, neurological outcome at hospital discharge and at one year, ROSC, quality of life) |
| Yes/no/unclear | Yes/no/unclear | Yes/no/unclear | Yes/no/unclear |
| Do not proceed if any of the above answers are 'no'. If study to be included in 'Excluded studies' section of the review, record below the information to be inserted into 'Table of excluded studies' | |||
Appendix 6. Data extraction
| Code each paper | Author(s) | Journal/conference proceedings etc. | Year |
| Participant characteristics | |||
| Further details | |||
| Age (mean, median, range, etc.) | |||
| Sex of participants (numbers/%, etc.) | |||
| Disease status/type, etc. (if applicable) | |||
| Other | |||
| Trial characteristics | |||
| Further details | |||
| Single centre/multicentre | |||
| Country/countries | |||
| How was participant eligibility defined? | |||
| How many people were randomized? | |||
| Number of participants in each intervention group | |||
| Number of participants who received intended treatment | |||
| Number of participants who were analysed | |||
| Interventions used | |||
| Frequency of compressions and ratio of compression to ventilation | |||
| Duration of treatment | |||
| Median (range) length of follow‐up reported in this paper (state weeks, months or years or if not stated) | |||
| Time points when measurements were taken during the study | |||
| Time points reported in the study | |||
| Time points you are using in RevMan | |||
| Trial design (e.g. RCT/quasi‐randomized/cluster‐randomized trials) | |||
| Other | |||
| Outcomes relevant to our review | |||
| Reported in paper (circle) | Intervention group (n) n = number of participants, not number of events | Control group (n) n = number of participants, not number of events | |
| Outcome 1. Survival to hospital discharge | Yes/No | ||
| Outcome 2. Survival to hospital admission | Yes/No | ||
| Outcome 3. Survival at one year | Yes/No | ||
| Outcome 4. Neurological outcomes at hospital discharge | Yes/No | ||
| Outcome 5. Neurological outcomes at one year | Yes/No | ||
| Outcome 6. Return of spontaneous circulation | Yes/No | ||
| Outcome 7. Quality of life | Yes/No | ||
| Other information which you feel is relevant to the results. Indicate if: any data were obtained from the primary author; if results were estimated from graphs etc.; or calculated by you using a formula (this should be stated and the formula given). In general, if results not reported in paper(s) are obtained, this should be made clear here to be cited in review. | |||
| Freehand space for writing actions such as contact with study authors and changes. | |||
Appendix 7. Methodological quality
| Allocation of intervention | |
| State here method used to generate allocation and reasons for grading. | Grade (circle) |
| Adequate (Random) | |
| Inadequate (e.g. alternate) | |
| Unclear | |
| Concealment of allocation Process used to prevent foreknowledge of group assignment in a RCT, which should be seen as distinct from blinding. | |
| State here method used to conceal allocation and reasons for grading. | Grade (circle) |
| Adequate | |
| Inadequate | |
| Unclear | |
| Blinding | |
| Person responsible for participants' care | Yes/No |
| Participant | Yes/No |
| Outcome assessor | Yes/No |
| Other (please specify) | Yes/No |
| Intention‐to‐treat An intention‐to‐treat analysis is one in which all the participants in a trial are analysed according to the intervention to which they were allocated, whether they received it or not. | |
| All participants entering trial | |
| 15% or fewer excluded | |
| More than 15% excluded | |
| Not analysed as 'intention‐to‐treat' | |
| Unclear | |
Data and analyses
Comparison 1. Bystander‐provided CPR.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Survival to hospital discharge | 3 | 3031 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.21 [1.01, 1.46] |
| 2 Survival to hospital admission | 1 | 520 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.18 [0.94, 1.48] |
| 3 Neurological outcomes at hospital discharge (measured with Cerebral Performance Category classification) | 1 | 1286 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.25 [0.94, 1.66] |
Comparison 2. Professional‐provided CPR.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Survival to hospital discharge | 1 | Risk Difference (Fixed, 95% CI) | Totals not selected | |
| 2 Survival to hospital admission | 1 | Risk Difference (Fixed, 95% CI) | Totals not selected | |
| 3 Neurological outcome at hospital discharge (Rankin score ≤ 3) | 1 | Risk Difference (Fixed, 95% CI) | Totals not selected | |
| 4 Return of spontaneous circulation | 1 | Risk Difference (Fixed, 95% CI) | Totals not selected | |
| 5 Adverse events | 1 | Risk Difference (Fixed, 95% CI) | Totals not selected |
2.4. Analysis.
Comparison 2 Professional‐provided CPR, Outcome 4 Return of spontaneous circulation.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Hallstrom 2000.
| Methods | Randomized controlled trial | |
| Participants | Inclusion criteria: Participants who were recognized to be unconscious and not breathing normally by callers who willing to undertake CPR with the dispatcher's assistance Exclusion criteria: Cases in which there was no cardiac arrest; cases of drug overdose, alcohol intoxication, or carbon monoxide poisoning; cases in which advanced cardiac life support was not carried out; and cases due to trauma. And the caller was not at the scene, or cardiac arrest occurred after the call 520 participants were included |
|
| Interventions | Intervention group: the bystander was instructed to perform chest compressions alone Contral group: the bystander was instructed to perform chest compressions plus rescue breathing, with 2 initial rescue breaths followed by 15 chest compressions and subsequent cycles continuing the pattern in a ratio of 2 to 15 |
|
| Outcomes | The primary end point was survival to hospital discharge. Secondary end points included admission to the hospital and estimated neurologic status in the survivors | |
| Notes | The study started before the guidelines for CPR changed the recommendation from 2 ventilations alternating with 15 compressions to 30 compressions alternating with 2 ventilations.The instructions in this study of 2 ventilations alternating with 15 compressions were maintained | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomization was assigned by a microcomputer located at the dispatcher's console |
| Allocation concealment (selection bias) | Unclear risk | If the caller was willing to be instructed, the caller was given instructions for performing either continuous chest compression alone or interrupted chest compression plus mouth‐to‐mouth ventilation, as randomly assigned by a microcomputer located at the dispatcher's console |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | The bystanders were not blinded, but they did not know that they were recruited in this study, so we considered it having minimal effects on the rescue treatment. Performance bias is unlikely to affect the primary outcomes of interest in the review |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | In the study, emergency medical services personnel other than those in the dispatch office were generally unaware that an episode might be part of a trial. The paramedics who completed the field reports typically arrived after the first responding personnel and thus had limited knowledge of the type or quality of bystander CPR that may have been performed. Hospitalization data and functional status after discharge from the hospital were obtained through an existing follow‐up programme whose personnel were unaware of the treatment assignments |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data on discharge were not available for two participants who were admitted to the hospital, one in each treatment group |
| Selective reporting (reporting bias) | Low risk | Main outcomes of out‐of‐hospital cardiac arrest were reported in full |
| Other bias | Low risk | We did not identify other sources of bias |
Nichol 2015.
| Methods | Cluster‐randomized trial with cross‐over. Eight sites in the USA and Canada. Each cluster spent six months on the allocated arm before crossing over to the other arm of the study every six months | |
| Participants | Inclusion criteria: Adult participants with non‐trauma‐related out‐of‐hospital cardiac arrest who received chest compressions performed by providers from participating EMS agencies who were dispatched to the scene Exclusion criteria: Patients were excluded if they had an EMS‐witnessed arrest, a written advance directive to not resuscitate, a traumatic injury, an asphyxial cause of arrest, uncontrolled bleeding or exsanguination, known pregnancy, or preexisting tracheostomy; were known to be prisoners; had initial CPR performed by a nonparticipating EMS provider; were treated with a mechanical chest‐compression device before manual CPR by ROC EMS personnel; had advanced airway management before ROC EMS agency arrival; or had, a priori, opted not to participate in resuscitation research |
|
| Interventions | Intervention group: Continuous chest compressions at a rate of 100 compressions/min with asynchronous positive‐pressure ventilations (10/min) Control group: Interrupted chest compressions plus ventilations at a ratio of 30 compressions to two positive‐pressure ventilations (given during < 5 second pause in compressions. |
|
| Outcomes | The primary outcome was the rate of survival to hospital discharge Secondary outcomes included survival to hospital admission, neurologic function at discharge (modified Rankin scale), ROSC at emergency department arrival, adverse events |
|
| Notes | In this trial, participants with out‐of‐hospital cardiac arrest received chest compressions performed by providers from participating EMS agencies who were dispatched to the scene, not bystanders which was different from the other three trials in this review. Bystander‐initiated CPR was reported in 46.9% of the intervention group and 47.1% of the control group | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Intervention (i.e. interrupted chest compression or continuous chest compression) allocated using randomized cluster‐cross‐over design. Each site subdivided into multiple clusters by EMS agency, station, or other unit as appropriate to the site's EMS structure. Insufficient detail available to determine method for generating randomisation sequence |
| Allocation concealment (selection bias) | Low risk | Randomization of clusters was stratified by site and by blocks of concealed size within sites. Information from study protocol suggests that allocation was concealed: 'Random assignment of treatment sequence will be performed at the coordinating center prior to the start of the study. Clusters will not be informed of their group assignments until necessary to make preparations to start the trial or cross over to another intervention' |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | This trial is an unblinded trial, the providers of CPR in each cluster knew that they are recruited in this study, so this may have performance bias. But in this trial, once a cluster was able to demonstrate proficiency with the given treatment by meeting prespecified performance and compliance benchmarks as determined by the Study Monitoring Committee, they were progressed into the Active Enrolment Phase, if one cluster was unable to meet benchmarks after 6 months, it was subsequently dropped from the trial. So we considered performance bias to be low even though the providers of CPR in each cluster were unblinded. Since the participants were unconscious and not breathing normally, we considered that the blinding of the participants would not affect the outcomes |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | An interdisciplinary study monitoring committee periodically reviewed data masked to treatment outcome. This committee met at least monthly throughout the enrolment period of the trial, and had authority to require an EMS agency to improve its study performance, or to place an agency on probation until performance improved, or to suspend an agency from ongoing enrolment in the trial. So we considered detection bias to be low |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data regarding the primary outcome were available for 99.7% of the intervention group and 99.8% of the control group |
| Selective reporting (reporting bias) | Low risk | All outcomes specified in the protocol were reported in full |
| Other bias | Low risk | We did not identify other sources of bias |
Rea 2010.
| Methods | Randomized controlled trial. | |
| Participants | Eligibility assessing when dispatcher's received call: Inclusion criteria: Participants who were recognized to be unconscious and not breathing normally by bystander willing to undertake CPR with the dispatcher's assistance Exclusion criteria: Participants with arrest due to trauma, drowning, or asphyxiation (from choking, strangulation, or suffocation), as well as participants who were under 18 years of age; and those who had 'do‐not‐resuscitate' status or were already receiving CPR Final eligibility determination after randomization: Participants who were unconscious and not breathing normally but were deemed not to be in arrest and persons who had a confirmed arrest but were found to have signs of irreversible death, in which case EMS personnel did not attempt resuscitation 1941 participants were included |
|
| Interventions | Intervention group: the bystander was instructed to perform chest compressions alone, providing 50 consecutive compressions in one cycle. Control group: the bystander was instructed to perform chest compressions plus rescue breathing, with 2 initial rescue breaths followed by 15 chest compressions and subsequent cycles continuing the pattern in a ratio of 2 to 15 In both groups, with the dispatcher still on the telephone, the bystander then performed one cycle of CPR during which the dispatcher asked the bystander to count the chest compressions out loud. After the first cycle, the dispatcher could inquire about signs of life and, if warranted, encourage the bystander to continue CPR |
|
| Outcomes | Survival to hospital discharge, ROSC at the end of EMS care, neurologic status at the time of hospital discharge (a favourable neurologic status was defined as a cerebral performance category of 1 or 2. (There are five Cerebral Performance Categories: category 1 represents good cerebral performance, 2 moderate cerebral disability, 3 severe cerebral disability, 4 coma or vegetative state, and 5 death) | |
| Notes | The study started before the guidelines for CPR changed the recommendation from 2 ventilations alternating with 15 compressions to 30 compressions alternating with 2 ventilations. The instructions in this study of 2 ventilations alternating with 15 compressions were maintained | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | This was not described in detail in the article |
| Allocation concealment (selection bias) | Low risk | If the caller was willing to undertake CPR with the dispatcher's assistance, a randomization envelope containing CPR instructions was opened |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Bystanders did not know that they were recruited in this study, so this would not have affected survival outcomes The EMS personnel and other physicians who gave advance therapy for the participants were not blinded and so care received following the arrival of EMS and other medical teams could have been affected by knowledge prior to treatment received |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | The review of EMS and hospital information was done without knowledge of participants' randomization status |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | In both groups, the missing data were 1.7 percent |
| Selective reporting (reporting bias) | Low risk | Main outcomes of out‐of‐hospital cardiac arrest were reported in full |
| Other bias | Low risk | We did not identify other sources of bias |
Svensson 2010.
| Methods | Randomized controlled trial | |
| Participants | Inclusion criteria: The collapse had been witnessed (seen or heard), and the participant was unconscious and was not breathing or not breathing normally Exclusion criteria: Cardiac arrest caused by trauma, airway obstruction, drowning, or intoxication; participants's age under 8 years; and difficulty of the dispatcher in communicating with the caller. Some at the scene had started CPR already before the caller, or the caller already knew how to perform CPR 1276 participants were included |
|
| Interventions | Intervention group: the caller was instructed to perform compression‐only CPR Contral group: the caller was instructed to perform standard CPR (mouth‐to‐mouth ventilation plus chest compression, consisting of 2 ventilations alternating with 15 compressions) |
|
| Outcomes | The primary end point was 30‐day survival. The secondary end points were 1‐day survival, defined as survival until midnight of the day of admission to the hospital, as well as the first detected cardiac rhythm and survival to discharge from the hospital | |
| Notes | The study started before the guidelines for CPR changed the recommendation from 2 ventilations alternating with 15 compressions to 30 compressions alternating with 2 ventilations. The instructions in this study of 2 ventilations alternating with 15 compressions were maintained, since the new guidelines did not address dispatcher‐assisted CPR | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The random sequence generation was based on the random number generator in SPSS software |
| Allocation concealment (selection bias) | Low risk | If the inclusion criteria had been met, the type of CPR on which the caller was instructed was determined on the data collection sheet. Data collection sheets were distributed in blocks of 100 sheets, 50 for each treatment assignment. The order of sheets within each block was unique and was based on the random number generator in SPSS software |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Bystanders did not know that they were recruited in this study, so this would not have affected survival outcomes. EMS personnel and other physicians who gave advance therapy for the participants were not blinded and so care received following the arrival of EMS and other medical teams could have been affected by knowledge prior to treatment received |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | The data were collected from EMS records, and information about survival status was collected from national registers. Although there was no description about blinding in this study, 50% of the data collection forms were double‐checked and no relevant deviations were observed. In addition, the researchers evaluated 100 recorded calls and reviewed the corresponding data‐collection forms, finding no deviation of the information in each |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Information on follow‐up was unavailable for 132 of 1952 participants (6.8%) in this study. The main reason being loss of the corresponding EMS field reports, occurring primarily in a small number of EMS districts. The authors, therefore, performed a subgroup analysis excluding districts where more than 18% of participants were lost to follow‐up. No difference from the main results was found |
| Selective reporting (reporting bias) | Low risk | Main outcomes of out‐of‐hospital cardiac arrest were reported in full |
| Other bias | Low risk | We did not identify other sources of bias |
CPR: cardiopulmonary resuscitation; EMS: emergency medical service; ROC: resuscitation outcomes consortium; ROSC: return of spontaneous circulation.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Bobrow 2010 | Prospective observational cohort study |
| Bohm 2007 | Retrospective investigation study |
| Cabrini 2010 | Review |
| Crane 2008 | Prospective observational study |
| Hüpfl 2010 | Review |
| Kitamura 2010 | Prospective observational cohort study |
| Ong 2008 | Prospective cohort study |
| Sayre 2008 | Review |
| Swor 2003 | Mannequin study |
Characteristics of ongoing studies [ordered by study ID]
NCT02401633.
| Trial name or title | A randomized trial comparing the effect of a simplified form of cardiopulmonary resuscitation (CPR) consisting of only chest compressions compared to CPR with compressions and rescue breaths ‐ the run‐in phase |
| Methods | Randomized controlled trial |
| Participants | Inclusion criteria: Unconsciousness with no abnormal or agonal breathing (suspected OHCA) The suspected OHCA is witnessed (seen or heard), bystander has previous training in CPR Exclusion Criteria: Age 18 or younger Collapse is not witnessed Bystander has never been trained in CPR (these bystanders should be instructed to administer CO‐CPR in accordance with guidelines) Obvious asphyxia, i.e. drowning, strangulation, hanging Obvious intoxication or drug overdose Obvious pregnancy Trauma Bystander is unwilling to participate or to perform CPR |
| Interventions | Intervention group: CPR provided by bystander with chest compressions only Control group: Instructions by dispatcher to bystander to provide CPR with chest compressions and rescue breaths in a 30:2 ratio |
| Outcomes | Unknown |
| Starting date | February 2015 |
| Contact information | Contact: Jacob Hollenberg, MD, PhD, +46704133442, jacob.hollenberg@ki.se Contact: Gabriel Riva, MD, +46705452086, gabriel.riva@ki.se |
| Notes |
CO‐CPR: Chest compression‐only cardiopulmonary resuscitation; CPR: cardiopulmonary resuscitation; OHCA: out‐of‐hospital cardiac arrest.
Differences between protocol and review
We made the following changes to the published protocol (Yang 2012).
The title was changed. The title of the published protocol was: 'Chest compression alone versus chest compression plus artificial ventilation for out‐of‐hospital cardiac arrest' (Yang 2012). The title of the review is: 'Continuous chest compression versus interrupted chest compression for cardiopulmonary resuscitation of non asphyxial out‐of‐hospital cardiac arrest'. The changes to the title have been reflected in other parts of the review, for example the objectives, types of studies and types of interventions sections.
The harms of an intervention are as important as the benefits, so we added the outcome 'adverse effects' to this review.
A recently published large trial involving professional‐provider CPR (Nichol 2015), compared continuous chest compression plus ventilation CPR with conventional CPR. This trial was a cluster‐RCT trial with cross‐over design, so we revised our review and included the cross‐over design study. As the data from the cluster‐RCT were not combined with any other study data we used the adjusted risk difference presented in the trial report.
Contributions of authors
Li J Yang (LJY), Yu Huang (YH), Qing He (QH), Guan J Liu (GJL), Lei Zhan (LZ)
Conceiving the review: LJY Designing the review: LJY Co‐ordinating the review: LJY Undertaking manual searches: LJY Screening search results: LZ and YH Organizing retrieval of papers: LZ Screening retrieved papers against inclusion criteria: LZ and YH Appraising quality of papers: LZ, YH Abstracting data from papers: LZ, YH Writing to authors of papers for additional information: HY Providing additional data about papers: LZ Obtaining and screening data on unpublished studies: LZ, YH Data management for the review: LJY, GJL Entering data into Review Manager (RevMan 2014): LZ, YH RevMan statistical data: GJL, LZ Other statistical analysis not using RevMan: GJL, LZ Double entry of data: (data entered by person one: LZ; data entered by person two: YH) Interpretation of data: LZ, QH, GJL Statistical inferences: GJL, LZ Writing the review: LZ Providing guidance on the review: QH Guarantor for the review (one author): LZ Person responsible for reading and checking review before submission: LZ
Declarations of interest
Lei Zhan: No conflict of interest.
Li J Yang: No conflict of interest.
Yu Huang: No conflict of interest.
Qing He: No conflict of interest.
Guan J Liu: No conflict of interest.
Edited (no change to conclusions)
References
References to studies included in this review
Hallstrom 2000 {published data only}
- Hallstrom A, Cobb L, Johnson E, Copass M. Cardiopulmonary resuscitation by chest compression alone or with mouth‐to‐mouth ventilation. New England Journal of Medicine 2000;25:1546‐53. [PUBMED: 10824072] [DOI] [PubMed] [Google Scholar]
Nichol 2015 {published data only}
- Nichol G, Leroux B, Wang H, Callaway CW, Sopko G, Weisfeldt M, et al. Trial of continuous or interrupted chest compressions during CPR. New England Journal of Medicine 2015;373(23):2203‐14. [PUBMED: 26550795] [DOI] [PubMed] [Google Scholar]
Rea 2010 {published data only}
- Rea TD, Fahrenbruch C, Culley L, Donohoe RT, Hambly C, Innes J, et al. CPR with chest compression alone or with rescue breathing. New England Journal of Medicine 2010;363:423‐33. [PUBMED: 20818863] [DOI] [PubMed] [Google Scholar]
Svensson 2010 {published data only}
- Svensson L, Bohm K, Castrèn M, Pettersson H, Engerström L, Herlitz J, et al. Compression‐only CPR or standard CPR in out‐of‐hospital cardiac arrest. New England Journal of Medicine 2010;363:434‐42. [PUBMED: 20818864] [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Bobrow 2010 {published data only}
- Bobrow BJ, Spaite DW, Berg RA, Stolz U, Sanders AB, Kern KB, et al. Chest compression‐only CPR by lay rescuers and survival from out‐of‐hospital cardiac arrest. JAMA 2010;304:1447‐54. [PubMe: 20924010 ] [DOI] [PubMed] [Google Scholar]
Bohm 2007 {published data only}
- Bohm K, Rosenqvist M, Herlitz J, Hollenberg J, Svensson L. Survival is similar after standard treatment and chest compression only in out‐of‐hospital bystander cardiopulmonary resuscitation. Circulation 2007;116(25):2908‐12. [PUBMED: 18071077] [DOI] [PubMed] [Google Scholar]
Cabrini 2010 {published data only}
- Cabrini L, Biondi‐Zoccai G, Landoni G, Greco M, Vinciguerra F, Greco T, et al. Bystander‐initiated chest compression‐only CPR is better than standard CPR in out‐of‐hospital cardiac arrest. HSR Proceedings in Intensive Care and Cardiovascular Anesthesia 2010;2:279‐85. [PUBMED: 23439400] [PMC free article] [PubMed] [Google Scholar]
Crane 2008 {published data only}
- Crane SA, Callaway CW, Milbrandt EB, Huang DT. Rethinking bystander CPR for out‐of‐hospital cardiac arrest. Critical Care 2008;12:302. [PUBMED: 18341712] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hüpfl 2010 {published data only}
- Hüpfl M, Selig HF, Nagele P. Chest‐compression‐only versus standard cardiopulmonary resuscitation: a meta‐analysis. Lancet 2010;376:1552‐7. [PUBMED: 20951422] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kitamura 2010 {published data only}
- Kitamura T, Iwami T, Kawamura T, Nagao K, Tanaka H, Nadkarni VM, et al. Conventional and chest‐compression‐only cardiopulmonary resuscitation by bystanders for children who have out‐of‐hospital cardiac arrests: a prospective, nationwide, population‐based cohort study. Lancet 2010;375:1347‐54. [PUBMED: 20202679] [DOI] [PubMed] [Google Scholar]
Ong 2008 {published data only}
- Ong ME, Ng FS, Anushia P, Tham LP, Leong BS, Ong VY, et al. Comparison of chest compression only and standard cardiopulmonary resuscitation for out‐of‐hospital cardiac arrest in Singapore. Resuscitation 2008;78:119‐26. [PUBMED: 18502559] [DOI] [PubMed] [Google Scholar]
Sayre 2008 {published data only}
- Sayre MR, Berg RA, Cave DM, Page RL, Potts J, White RD. Hands‐only (compression‐only) cardiopulmonary resuscitation: a call to action for bystander response to adults who experience out‐of‐hospital sudden cardiac arrest: a science advisory for the public from the American Heart Association Emergency Cardiovascular Care Committee. Circulation 2008;117:2162‐7. [PUBMED: 18378619] [DOI] [PubMed] [Google Scholar]
Swor 2003 {published data only}
- Swor R, Compton S, Vining F, Ososky Farr L, Kokko S, Pascual R, et al. A randomized controlled trial of chest compression only CPR for older adults ‐ a pilot study. Resuscitation 2003;58:177‐85. [PUBMED: 12909380] [DOI] [PubMed] [Google Scholar]
References to ongoing studies
NCT02401633 {unpublished data only}
- NCT02401633. Compression‐only CPR versus standard‐CPR ‐ the run‐in phase [A randomized trial comparing the effect of a simplified form of cardiopulmonary resuscitation (CPR) consisting of only chest compressions compared to CPR with compressions and rescue breaths ‐ the run‐in phase]. clinicaltrials.gov/ct2/show/NCT02401633 (first received 7 March 2015).
Additional references
AHA 2000
- American Heart Association. Part 1: Introduction to the International Guidelines 2000 for CPR and ECC: a consensus on science. Circulation 2000;102((8 Suppl)):1‐11. [PUBMED: 10964901] [DOI] [PubMed] [Google Scholar]
AHA 2005
- ECC Committee, Subcommittees and Task Forces of the American Heart Association. 2005 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 2005;112 Suppl((24 Suppl)):IV1‐203. [PUBMED: 16314375] [DOI] [PubMed] [Google Scholar]
AHA 2010
- Travers AH, Rea TD, Bobrow BJ, Edelson DP, Berg RA, Sayre MR, et al. Part 4: CPR overview: 2010 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 2010;122((18 Suppl 3)):S676‐84. [PUBMED: 20956220] [DOI] [PubMed] [Google Scholar]
Aufderheide 2004
- Aufderheide TP, Sigurdsson G, Pirrallo RG, Yannopoulos D, McKnite S, Briesen C. Hyperventilation‐induced hypotension during cardiopulmonary resuscitation. Circulation 2004;109:1960‐5. [PUBMED: 15066941] [DOI] [PubMed] [Google Scholar]
Becker 1997
- Becker LB, Berg RA, Pepe PE, Idris AH, AufderheideTP, Barnes TA. A reappraisal of mouth‐to‐mouth ventilation during bystander‐initiated cardiopulmonary resuscitation. A statement for healthcare professionals from the Ventilation Working Group of the Basic Life Support and Pediatric Life Support Subcommittees, American Heart Association. Circulation 1997;96:2102‐12. [PUBMED: 9323122] [DOI] [PubMed] [Google Scholar]
Bobrow 2008
- Bobrow BJ, Clark LL, Ewy GA, Chikani V, Sanders AB, Berg RA. Minimally interrupted cardiac resuscitation by emergency medical services for out‐of‐hospital cardiac arrest. JAMA 2008;299:1158‐65. [PUBMED: 18334691] [DOI] [PubMed] [Google Scholar]
Brenner 1993
- Brenner BE, Kauffman J. Reluctance of internists and medical nurses to perform mouth‐to‐mouth resuscitation. Archives of Internal Medicine 1993;153:1763‐9. [PUBMED: 8333813] [PubMed] [Google Scholar]
Brenner 1994
- Brenner B, Stark B, Kauffman J. The reluctance of house staff to perform mouth‐to‐mouth resuscitation in the inpatient setting: what are the considerations?. Resuscitation 1994;28:185‐93. [PUBMED: 7740188] [DOI] [PubMed] [Google Scholar]
Chandra 1994
- Chandra NC, Gruben KG, Tsitlik JE, Brower R, Guerci AD, Halperin HH. Observations of ventilation during resuscitation in a canine model. Circulation 1994;304:1447‐54. [PUBMED: 7994856] [DOI] [PubMed] [Google Scholar]
Clark 1992
- Clark JJ, Larsen MP, Culley LL, Graves JR, Eisenberg, MS. Incidence of agonal respirations in sudden cardiac arrest. Annals of Emergency Medicine 1992;21:1464‐7. [PUBMED: 1443844] [DOI] [PubMed] [Google Scholar]
Coons 2009
- Coons SJ, Guy MC. Performing bystander CPR for sudden cardiac arrest: behavioral intentions among the general adult population in Arizona. Resuscitation 2009;80:334‐40. [PUBMED: 19157675] [DOI] [PubMed] [Google Scholar]
Cummins 1991
- Cummins RO, Chamberlain DA, Abramson NS, Allen M, Baskett PJ, Becker L. Recommended guidelines for uniform reporting of data from out‐of‐hospital cardiac arrest: the Utstein Style. Circulation 1991;84:960‐75. [PUBMED: 1860248] [DOI] [PubMed] [Google Scholar]
Eckstein 2005
- Eckstein M, Stratton SJ, Chan LS. Cardiac Arrest Resuscitation Evaluation in Los Angeles: CARE‐LA. Annals of Emergency Medicine 2005;45:504‐9. [PUBMED: 15855947] [DOI] [PubMed] [Google Scholar]
ERC 2010
- European Resuscitation Council. European Resuscitation Council guidelines for resuscitation 2010 section 1. Executive summary. Resuscitation 2010;81:1219‐76. [PUBMED: 20956052] [DOI] [PubMed] [Google Scholar]
Guyatt 2008
- Guyatt GH, Oxman AD, Vist GE, Kunz, R, Falck‐Ytter Y, Alonso‐Coello P. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008;336:924‐6. [PUBMED: 2335261] [DOI] [PMC free article] [PubMed] [Google Scholar]
Handley 2005
- Handley AJ, Koster R, Monsieurs K, Perkins GD, Davies S, Bossaert L, European Resuscitation Council. European Resuscitation Council guidelines for resuscitation 2005. Section 2. Adult basic life support and use of automated external defibrillators. Resuscitation 2005;67 Suppl 1:S7‐23. [PUBMED: 16321717] [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Jones‐Crawford 2007
- Jones‐Crawford JL, Parish DC, Smith BE, Dane FC. Resuscitation in the hospital: circadian variation of cardiopulmonary arrest. American Journal of Medcine 2007;120:158–64. [PUBMED: 17275457] [DOI] [PubMed] [Google Scholar]
Jüni 2001
- Jüni P, Altman D, Egger M. Systematic reviews in healthcare: assessing the quality of controlled clinical trials. BMJ 2001;323:42‐6. [PUBMED: 11440947] [DOI] [PMC free article] [PubMed] [Google Scholar]
Locke 1995
- Locke CJ, Berg RA, Sanders AB, Davis MF, Milander MM, Kern KB, et al. Bystander cardiopulmonary resuscitation. Concerns about mouth‐to‐mouth contact. Archives of Internal Medicine 1995;155:938‐43. [PUBMED: 7726702] [DOI] [PubMed] [Google Scholar]
Nadkarni 2006
- Nadkarni VM, Larkin GL, Peberdy MA, Carey SM, Kaye W, Mancini ME, et al. First documented rhythm and clinical outcome from in‐hospital cardiac arrest among children and adults. JAMA 2006;295:50‐7. [PUBMED: 16391216] [DOI] [PubMed] [Google Scholar]
Nichol 2008
- Nichol G, Thomas E, Callaway CW, Hedges J, Powell JL, Aufderheide TP, et al. Regional variation in out‐of‐hospital cardiac arrest incidence and outcome. JAMA 2008;300:1423‐32. [PUBMED: 18812533] [DOI] [PMC free article] [PubMed] [Google Scholar]
Noc 1995
- Noc M, Weil MH, Tang W, Turner T, Fukui M. Mechanical ventilation may not be essential for initial cardiopulmonary resuscitation. Chest 1995;108:821‐7. [PUBMED: 7656640] [DOI] [PubMed] [Google Scholar]
Ogawa 2011
- Ogawa T, Akahane M, Koike S, Tanabe S, Mizoguchi T, Imamura T. Outcomes of chest compression only CPR versus conventional CPR conducted by lay people in patients with out of hospital cardiopulmonary arrest witnessed by bystanders: nationwide population based observational study. BMJ 2011;342:c7106. [PUBMED: 21273279] [DOI] [PubMed] [Google Scholar]
Paradis 1990
- Paradis NA, Martin GB, Rivers EP, Goetting MG, Appleton TJ, Feingold M. Coronary perfusion pressure and the return of spontaneous circulation in human cardiopulmonary resuscitation. JAMA 1990;263:1106‐13. [PUBMED: 2386557] [PubMed] [Google Scholar]
RevMan 2014 [Computer program]
- Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager 5 (RevMan 5). Version 5.3. Copenhagen: Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Rucker 2008
- Rucker G, Schwarzer G, Carpenter J. Arcsine test for publication bias in meta‐analyses with binary outcomes. Statistics in Medicine 2008;27:746‐63. [PUBMED: 17592831] [DOI] [PubMed] [Google Scholar]
SOS‐KANTO Group 2007
- SOS‐KANTO Group. Cardiopulmonary resuscitation by bystanders with chest compression only (SOS‐KANTO): an observational study. Lancet 2007;369:920‐6. [PUBMED: 17368153] [DOI] [PubMed] [Google Scholar]
Tang 1994
- Tang W, Weil MH, Sun S, Kette D, Kette F, Gazmuri RJ. Cardiopulmonary resuscitation by precordial compression but without mechanical ventilation. American Journal of Respiratory and Critical Care Medicine 1994;150:1709‐13. [PUBMED: 7952638] [DOI] [PubMed] [Google Scholar]
Travers 2010
- Travers S, Dubourg O, Bon O, Banville IL, Jost D, VerretC. Chest compressions only or full CPR for out‐of‐hospital cardiac arrest? Unexpected outcomes from the DEFI2005 trial. Resuscitation 2010;81:S9. [DOI: 10.1016/j.resuscitation.2010.09.048] [DOI] [Google Scholar]
Wolcke 2003
- Wolcke BB, Mauer DK, Schoefmann MF, TeichmannH, Provo TA, Lindner KH. Comparison of standard cardiopulmonary resuscitation versus the combination of active compression‐decompression cardiopulmonary resuscitation and an inspiratory impedance threshold device for out‐of‐hospital cardiac arrest. Circulation 2003;108:2201‐1. [PUBMED: 14568898] [DOI] [PubMed] [Google Scholar]
Yu 2002
- Yu T, Weil MH, Tang W, Sun S, Klouche K, Povoas H. Adverse outcomes of interrupted precordial compression during automated defibrillation. Circulation 2002;106:368‐72. [PUBMED: 12119255] [DOI] [PubMed] [Google Scholar]
Zheng 2001
- Zheng ZJ, Janet BC, Wayne HG, George AM. Sudden cardiac death in the United States, 1989 to 1998. Circulation 2001;104:2158‐63. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Yang 2012
- Yang LJ, He Q, Huang Y, Liu GJ. Chest compression alone versus chest compression plus artificial ventilation for out‐of‐hospital cardiac arrest. Cochrane Database of Systematic Reviews 2012, Issue 10. [DOI: 10.1002/14651858.CD010134] [DOI] [Google Scholar]


