Abstract
Introduction
Current residency didactic schedules that are built upon hour-long, lecture-based presentations are incongruous with adult learning theory and the needs of millennial generation residents. An alternative to the traditional lecture, the flipped classroom involves viewing a short video lecture at home, followed by an active discussion during class time. This module was developed for emergency medicine residents and rotating medical students without previous training on the subject.
Methods
The at-home portion of the module was designed to be delivered at home, while the in-class discussion was designed to be carried out over 30–45 minutes during a regularly scheduled didactic time. Small-group size may be determined by faculty availability, though groups of five are optimal. There is no requirement for faculty preparation prior to the in-class session. Associated materials include objectives, the at-home video, a discussion guide for faculty facilitators, a case-based handout for students and residents, and assessment questions. We assessed our module with a pretest, immediate posttest, and the posttest again after 90 days.
Results
The mean pretest score was 66%, mean posttest score 76%, and mean retention test score 66%. There was an immediate increase of 10%, which did not remain at 90 days.
Discussion
We developed a flipped classroom module that can be implemented in any emergency medicine residency or clerkship. It addresses the theoretical challenges posed to traditional conference didactics by increasing the focus on problem solving and self-directed learning.
Keywords: Editor's Choice, Video, Emergency Medicine, Low Back Pain, Flipped Classroom
Educational Objectives
At the end of this module, the learner will be able to:
-
1.
List the diagnoses critical to the emergency physician that may present with low back pain.
-
2.
Identify key historical and examination findings that help differentiate primary or low-risk, nonspecific (benign) from secondary (serious) causes of back pain.
-
3.
Discuss the indications for diagnostic imaging and other testing in patients with low back pain.
-
4.
Develop strategies to treat patients diagnosed with low-risk nonspecific back pain.
Introduction
Current didactic schedules are built upon hour-long, lecture-based presentations. However, adult learning theory suggests that adults learn differently than younger students, with an increased focus on problem solving and self-directed learning.1 Studies of millennial generation residents have shown an increasing desire to add interactive and social media components to the classroom.2,3 The emergency medicine education literature is beginning to trend towards alternate approaches to emergency medicine resident education.4
One alternative to the traditional lecture is the flipped classroom. In the flipped classroom model, students absorb an instructor's short lecture in a digital format in preparation for class time. Preparatory work is moved outside normal class time and into the students’ hands, allowing faculty to use class time in more creative ways: focusing on application, simulation, case-based, or problem-solving exercises. The flipped classroom has recently gained the support of prominent medical educators.5–7 It is currently being used in residency curricula in general surgery,8 anesthesia,9 orthopedics,10 internal medicine,11 emergency medicine,12 and critical care.13
A recent study of the flipped classroom in an emergency medicine residency found 95% of residents preferred the format to a traditional lecture.14 Though no outcome data exist in the graduate medical education context, the flipped classroom has shown significant performance improvement in undergraduate science courses, boosting grades by about 13% in one meta-analysis.15 The flipped classroom with active learning approach may be especially appropriate to emergency medicine residents, who are now mostly millennial learners.16
Based on this theoretical benefit and learner preference, we developed a flipped classroom module to teach acute low back pain to emergency medicine residents. This module was designed to make part of the traditional didactic requirement asynchronous, while still fulfilling some in-class time. This module is ideally implemented as part of the weekly didactic requirement specified by the Accreditation Council for Graduate Medical Education (ACGME).
To implement this didactic alternative, we selected a commonly encountered emergency department chief complaint that is a part of the American Board of Emergency Medicine's standard-setting Model of the Clinical Practice of Emergency Medicine: acute low back pain.17 The module consists of a short video to be viewed at home, then an in-class, case-based discussion.
Methods
The target audience for the module is beginning to advanced emergency medicine residents and rotating medical students with or without previous training on the subject. This module may also be useful in internal medicine, family medicine, orthopedic surgery, physical medicine and rehabilitation, physical therapy, chiropractic, and nursing. The in-class portion of the module can occur in the same room as previously scheduled didactics, though, if desired, separate rooms for small-group discussion may be optimal. We broke into groups of five to 10, though faculty availability will likely guide how small your groups can be.
The 10 pretest questions (Appendix E, answer key in Appendix G) should be given to the students 7 days prior to the conference day. Learners should be asked to complete the questions before watching the video. The questions can be reviewed at the start of the in-class session to allow students to explore their preconceptions or areas of difficulty while also permitting the facilitator to assess the learners’ needs and level of understanding. As the pretest is fairly challenging, faculty can consider encouraging the learners to complete this task in small groups. The National Board of Medical Examiners–style multiple-choice questions were developed based on each subject's consensus objectives. Twenty questions were developed by two of us with professional item-writing experience.
A 20-minute summary video lecture (Appendix B) can be posted to any video-hosting website (university-based, Vimeo, Google Drive, YouTube, etc.); then, an email with a link to the video needs to be sent to the participants. We suggest sending the email 5 days before conference, with a reminder email sent 2 days prior. The learners should be encouraged to review the normal components of a good back examination.
During the class session, the pretest should be reviewed before moving on to the case discussion. The learner handout (Appendix C) was used to guide the learners through in-class discussion. It consists of a series of cases written by experienced program faculty. It features questions on presentation, evaluation and diagnosis, management, and disposition that map to the objectives (Appendix A). The instructor handout (Appendix D) contains the same cases as the learner handout but is also comprehensive. It features detailed questions and answers to guide the discussion. Given the thoroughness of this handout, faculty leading discussions do not need extensive preparation prior to conference.
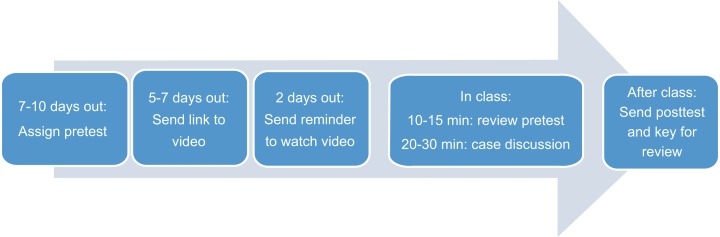
The 10 posttest questions (Appendix F, answer key in Appendix H) can be used at the end of the in-class session for assessment or, because explanations are provided, can be given to residents to review on their own after the session, capitalizing on spaced learning and the testing effect. (See the Figure for the module's time line.)
Figure. Flipped classroom module time line.
Results
The module has been given at three different ACGME-approved residency programs. Forty-two emergency medicine learners (fourth-year medical student, PGY-1, PGY-2, PGY-3, and PGY-4) experienced the module. More than six board-certified emergency medicine faculty have led the discussion groups. They had no special training for the discussion sessions.
Ten-item pre- and posttest assessments were given. The posttest was given again after 90 days. The mean pretest score was 66%, mean posttest score 76%, and mean retention test score 66%. There was an immediate increase of 10%, which did not remain at 90 days.
Discussion
We developed a flipped classroom module addressing the theoretical challenges posed to traditional conference didactics. We increased the focus on problem solving and self-directed learning. Our data show an immediate increase in knowledge from the flipped classroom module. We incorporated technology effectively and saw robust discussion amongst trainees during the in-class portion. The module was easily implementable into the existing didactic half-day schedule. We learned that it was helpful for the learners to have an explanation of the format prior to beginning so that they knew what to expect and had some comfort with the format.
The lack of knowledge retention at 90 days is a concern. To combat this knowledge leak, we recommend using the posttest and key as a tool for spaced repetition and retrieval practice. This spaced learning may help retention by having the learners revisit the material while forcing them to retrieve information from their memory.
Going forward, it is possible to implement the flipped classroom format with existing videos available free on the internet, which would greatly decrease the work required and eliminate a significant barrier to adoption. We also need to consider strategies to increase retention, a problem seen both in our data and with traditional lectures.
Disclosures
None to report.
Funding/Support
The development of this module was support by a grant from the Western Group on Education Affairs of the Association of American Medical Colleges.
Ethical Approval
This publication contains data obtained from human subjects and received ethical approval.
Appendices
A. Objectives.docx
B. Low Back Pain Video.mp4
C. Low Back Pain Learner Handout.docx
D. Low Back Pain Instructor Handout.docx
E. Low Back Pain Pretest.docx
F. Low Back Pain Posttest.docx
G. Low Back Pain Pretest Key.docx
H. Low Back Pain Posttest Key.docx
All appendices are peer reviewed as integral parts of the Original Publication.
References
- 1.Knowles M. The Adult Learner: A Neglected Species. Houston, TX: Gulf Publishing; 1973. [Google Scholar]
- 2.Tan E, Brainard A, Larkin GL. Acceptability of the flipped classroom approach for in-house teaching in emergency medicine. Emerg Med Australas. 2015;27(5):453–459. http://dx.doi.org/10.1111/1742-6723.12454 [DOI] [PubMed] [Google Scholar]
- 3.Purdy E, Thoma B, Bednarczyk J, Migneault D, Sherbino J. The use of free online educational resources by Canadian emergency medicine residents and program directors. CJEM. 2015;17(2):101–106. http://dx.doi.org/10.1017/cem.2014.73 [DOI] [PubMed] [Google Scholar]
- 4.Deiorio NM, Fitch MT, Jung J, et al. Evaluating educational interventions in emergency medicine. Acad Emerg Med. 2012;19(12):1442–1453. http://dx.doi.org/10.1111/acem.12022 [DOI] [PubMed] [Google Scholar]
- 5.Prober CG, Heath C. Lecture halls without lectures—a proposal for medical education. N Engl J Med. 2012;366(18):1657–1659. http://dx.doi.org/10.1056/NEJMp1202451 [DOI] [PubMed] [Google Scholar]
- 6.Prober CG, Khan S. Medical education reimagined: a call to action. Acad Med. 2013;88(10):1407–1410. http://dx.doi.org/10.1097/ACM.0b013e3182a368bd [DOI] [PubMed] [Google Scholar]
- 7.Mehta NB, Hull AL, Young JB, Stoller JK. Just imagine: new paradigms for medical education. Acad Med. 2013;88(10):1418–1423. http://dx.doi.org/10.1097/ACM.0b013e3182a36a07 [DOI] [PubMed] [Google Scholar]
- 8.DaRosa D. What's missing from the flipped classroom model? AM Rounds: Beyond the Pages of Academic Medicine Web site. http://academicmedicineblog.org/whats-missing-from-the-flipped-classroom-model Published October 15, 2013. Accessed January 15, 2014.
- 9.Udani A, Clemenson A, Harrison T, Garbin M, Chu L. ImPRINT: a flipped classroom curriculum to increase medical knowledge during the CB-1 year. Presented at: American Society of Anesthesiologists (ASA) Annual Meeting; October 14, 2013; San Francisco, CA.
- 10.Leung JY, Kumta SM, Jin Y, Yung AL. Short review of the flipped classroom approach. Med Educ. 2014;48(11):1127 http://dx.doi.org/10.1111/medu.12576 [DOI] [PubMed] [Google Scholar]
- 11.Vincent DS. Out of the wilderness: flipping the classroom to advance scholarship in an internal medicine residency program. Hawaii J Med Public Health. 2014;73(11)(suppl 2):2–3. [PMC free article] [PubMed] [Google Scholar]
- 12.Cooney R. How we are flipping EM education. The Teaching Course Web site. http://www.thetcblog.com/?p=1919 Published January 15, 2014. Accessed January 15, 2014.
- 13.Ramar K, Hale CW, Dankbar EC. Innovative model of delivering quality improvement education for trainees—a pilot project. Med Educ Online. 2015;20:28764 http://dx.doi.org/10.3402/meo.v20.28764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Young TP, Bailey CJ, Guptill M, Thorp AW, Thomas TL. The flipped classroom: a modality for mixed asynchronous and synchronous learning in a residency program. West J Emerg Med. 2014;15(7):938–944. http://dx.doi.org/10.5811/westjem.2014.10.23515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bernard RM, Borokhovski E, Schmid RF, Tamim RM, Abrami PC. A meta-analysis of blended learning and technology use in higher education: from the general to the applied. J Comput High Educ. 2014;26(1):87–122. http://dx.doi.org/10.1007/s12528-013-9077-3 [Google Scholar]
- 16.Roberts DH, Newman LR, Schwartzstein RM. Twelve tips for facilitating millennials’ learning. Med Teach. 2012;34(4):274–278. http://dx.doi.org/10.3109/0142159X.2011.613498 [DOI] [PubMed] [Google Scholar]
- 17.Counselman FL, Borenstein MA, Chisholm CD, et al; for the American Board of Emergency Medicine. The 2013 Model of the Clinical Practice of Emergency Medicine. Acad Emerg Med. 2014;21(5):574–598. http://dx.doi.org/10.1111/acem.12373 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
A. Objectives.docx
B. Low Back Pain Video.mp4
C. Low Back Pain Learner Handout.docx
D. Low Back Pain Instructor Handout.docx
E. Low Back Pain Pretest.docx
F. Low Back Pain Posttest.docx
G. Low Back Pain Pretest Key.docx
H. Low Back Pain Posttest Key.docx
All appendices are peer reviewed as integral parts of the Original Publication.