Abstract
BACKGROUND
Laparoscopic sleeve gastrectomy (LSG) has been established as an effective means of weight loss. Multiple studies report LSG as a cost-effective procedure with few perioperative complications.
OBJECTIVES
Report long-term weight changes after LSG in a single center in Kuwait.
DESIGN
Retrospective analysis of data collected 5–8 years after surgery.
SETTING
A single medical center.
PATIENTS AND METHODS
All patients that had undergone LSG between December 2008 and December 2011.
MAIN OUTCOME MEASURES
Weight changes, short-term complications following surgery (within one month).
SAMPLE SIZE
187.
RESULTS
The mean age at the time of the surgery was 36.5 (10.3) years. Females composed 71.6% of this study population. Two patients (1.1%) presented with a leak within 30 days of the surgery. Twenty-one (11.2%) patients underwent revisional bariatric surgery after LSG. Mean (SD) BMI decreased from 47.1 (8.3) kg/m2 before surgery to 34.3 (7) kg/m2 5–8 years after surgery. Mean (SD) body weight decreased from 126.3 (25.3) kg to 91.6 (19.9) kg 5–8 years following LSG. The mean excess body weight loss was 58.8% (29.2%).
CONCLUSION
LSG is a bariatric procedure with low complications and mortality in relation to other forms of bariatric surgery. It is associated with a significant improvement in weight loss in the long term.
LIMITATIONS
Recall bias due to the nature of collecting the data, small sample size.
Obesity and its associated metabolic disorders are reaching pandemic proportions worldwide.1 It is considered a chronic disease that has a negative impact on the health of many individuals. Kuwait is considered one of the top 10 countries in the world in terms of obesity, with 42.8% of its population affected.2 Obesity is also a risk factor for the development of multiple comorbidities including type 2 diabetes mellitus, hypertension, dyslipidemia, and heart failure.3 Thus, discovery of effective weight loss methods is of global interest. Laparoscopic sleeve gastrectomy (LSG) has been established as an effective and safe method of weight loss for obese patients, as well as treatment for the metabolic disorders associated with obesity.4 Multiple studies report LSG as a cost-effective procedure with lower perioperative complications compared to bypass,5,6 but data on the use of surgery in Kuwait are lacking. We report long-term outcomes after several years as well as the immediate results 30 days after surgery.
PATIENTS AND METHODS
Beginning in June 2016, we collected patients who were morbidly obese and treated with LSG as a primary bariatric surgery between December 2008 and December 2011 at a single center (Al-Amiri), a governmental tertiary hospital in Kuwait. Patients had previously followed up once with their surgeon one month after surgery. We conducted another follow-up 5–8 years after LSG.
Inclusion criteria for the LSG were BMI ≥40 kg/m2 without associated comorbid conditions or BMI >35 kg/m2 with at least one comorbidity and unsuccessful attempts at medical treatment.7 Exclusion criteria were psychiatric illness or substance abuse.
All patients signed informed consent forms after a detailed explanation of the procedure, follow-up, advantages, and complications. Ethical approval was obtained from the medical research ethics committee. The data was collected from the hospital registry and patient files. Eligible patients were contacted by telephone. Patients who declined to participate or could not be reached by phone were excluded. Preoperative characteristics included age, gender, height, weight (WT), and body mass index (BMI). The mean excess body weight loss was calculated as (WT before – WT after) × 100/(WT before- ideal body WT). Ideal body WT= BMI of 25 kg/m2. The EBWL percentage was calculated using the formula: (WT before – WT after) Å~100/(WT before- ideal body WT). Ideal body WT=WT corresponding to a BMI of 25 kg/m2. The 5–8 year follow-up data were collected via telephone interview.
Laparoscopic sleeve gastrectomy technique
A standard split-leg French position was utilized for performing the LSG procedure using the placement of the standard five laparoscopic ports. Devascularization of the greater curvature of the stomach was started from 4–6 cm from the pylorus up to the angle of His. A 36-Fr calibrating bougie was then passed through the stomach to the duodenum and a linear laparoscopic stapler was used to perform the sleeve. Finally, an assessment for leakage was done by pulling the bougie proximally and injecting 100 mL of methylene blue. No intra-abdominal drains were placed. A semi-solid diet was permitted after 2 weeks and then the diet was gradually converted to normal diet over a 4-week period.
The policy at Amiri Hospital for bariatric patients with a BMI of less than 50 includes 40 mg enoxaparin twice daily for 2 weeks, which is then reduced to 40 mg once daily for another week. If the BMI is more than 50, 60 mg enoxaparin is started twice daily for two weeks, followed by 60 mg once daily for another week. Appropriate antibiotic therapy was given to patients preoperatively. Patients were followed up post-operatively at 2 weeks, 3 months, 6 months, 12 months, 18 months, and yearly afterward by bariatric surgeons. Nutritional status was assessed by routine laboratory tests and anthropometric measurements at each follow-up visit.
RESULTS
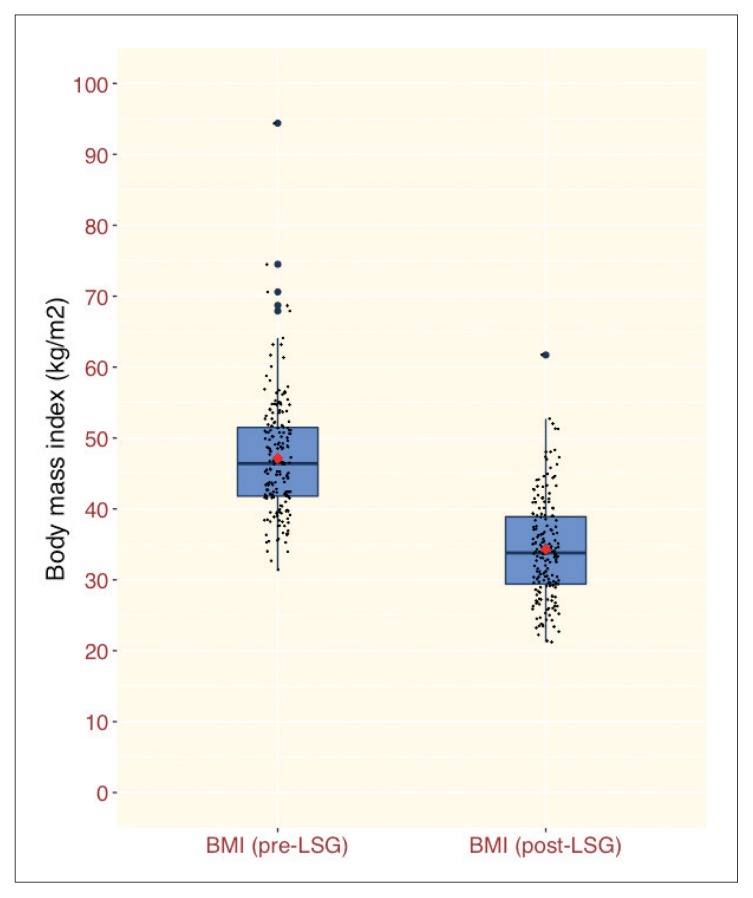
The 187 patients who underwent LSG included 134 females (71.6%) and 53 males (28.4%). The time of follow up for this study ranged from 5 years for 66 patients to 8 years for 4 patients. The mean age of the patients at the time of the surgery was 36.5 (10.3) years, ranging from 13 to 62 years. Mean (SD) BMI decreased from 47.1 (8.3) kg/m2 before surgery to 34.3(7) kg/m2 5–8 years after surgery (Figure 1). Mean (SD) body weight decreased from 126.3 (25.3) kg to 91.6 (19.9) kg 5–8 years following LSG. The mean excess body weight loss was 58.8% (29.2%). The mean excess body weight loss (EBWL) was 58.8% (29.2%). There were neither intraoperative complications nor postoperative mortalities. The only acute complication within 30 days of surgery was leakage (1.1%) in 2 patients. No bleeding or obstruction was reported during these 30 days. Long-term complications included gastroesophageal reflux disease (n=78), gallstones (n=36), musculoskeletal pain (n=32), depression (n=4), and deep vein thrombosis (n=3).
Figure 1.
Body mass index before and 5–8 years after laparoscopic sleeve gastrectomy (median, 25th and 75th percentile, red dot=mean) (P<.001).
DISCUSSION
Bariatric surgery has become a popular procedure for those with morbid obesity. There are several bariatric surgical procedures. LSG is a restrictive technique in which the size of the stomach is reduced by removing up to 3/4 of it. This effectively restricts the stomach capacity without affecting its function, so that the amount of food that can be consumed in one sitting is restricted.8–10
As LSG and other types of bariatric surgery are more widely practiced, the surgical techniques for performing them are improving significantly, leading to lower rates of complications. Previous studies have reported leak rates ranging from 1.5% to 5.4%.11–13 Eng-Hong et al reported 14 leaks in 667 patients (2.1%).14 In comparison, our study showed a 1.1% leak rate, consistent with rates lower than those previously reported in the long term. In addition, there was no bleeding, obstruction or mortality within the 30-day post-op period.
In our study, 21 patients (11.2%) underwent revisional bariatric surgery post LSG. In Seki et al.’s study, revisional surgeries were required in 6 patients (3.4 %).15 Eng-Hong et al reported a revision rate for LSG in 18 patients (2.2%).14 The rate of revisional bariatric surgery was higher in our study compared to other studies. This could be due to multiple factors.
A higher commitment with patients to follow-up and stressing the importance of concurrent diet and exercise in preventing weight regain and increasing weight loss might be useful to achieve the most out of LSG. After following up our patients for 5–8 years, their mean BMI was decreased to 34.3 kg. In Eng-Hong et al.’s study, the mean BMI at the 5-year postoperative follow-up was 26.2 kg.14 Seki et al reported a decline in the mean BMI to 32.7 at 5 years or more.15 The mean excess body weight loss in our study was 58.8%. Aridi et al, in comparison, reported a mean total weight loss of 69.8% at 5 years.16 Our results and other data available illustrate the role of LSG in sustained, long-term weight loss.
A possible limitation of this study is that recent patient data was collected via telephone and therefore may contain some form of recall bias in addition to the small sample size. Possible future approaches might be to conduct studies that include a larger sample size over a longer period of time, and to follow up patients in the outpatient department with proper investigations to evaluate the after-effects of LSG. In conclusion, this study shows that LSG is an effective type of bariatric procedure with a low complication rate and mortality relative to other forms of bariatric surgery that achieves sustained weight loss.
Acknowledgments
The authors wish to thank all patients who agreed to participate in this research for their time and effort in completing the questionnaires.
Footnotes
Funding: None.
CONFLICT OF INTEREST: None.
Availability of data and materials: The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
REFERENCES
- 1.Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Gakidou E. Global, regional and national prevalence of overweight and obesity in children and adults 1980–2013: A systematic analysis. Lancet. 2014;384(9945):766–781. doi: 10.1016/S0140-6736(14)60460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Alnohair S. Obesity in Gulf Countries. International Journal of Health Sciences. 2014;8(1):79–83. doi: 10.12816/0006074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pi-Sunyer X. The Medical Risks of Obesity. Postgraduate Medicine. 2009;121(6):21–33. doi: 10.3810/pgm.2009.11.2074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Silecchia G, Boru C, Pecchia A, Rizzello M, Casella G, Leonetti F, et al. Effectiveness of laparoscopic sleeve gastrectomy (first stage of biliopancreatic diversion with duodenal switch) on co-morbidities in super-obese high-risk patients. Obesity Surgery. 2006 Sep 1;16(9):1138–44. doi: 10.1381/096089206778392275. [DOI] [PubMed] [Google Scholar]
- 5.Aridi HD, Khazen G, Safadi BY. Comparison of Outcomes Between Laparoscopic Roux-en-Y Gastric Bypass and Sleeve Gastrectomy in a Lebanese Bariatric Surgical Practice. Obesity Surgery. 2017;28(2):396–404. doi: 10.1007/s11695-017-2849-5. [DOI] [PubMed] [Google Scholar]
- 6.Gadiot RP, Biter LU, van Mil S, Zengerink HF, Apers J, Mannaerts GH. Long-term results of laparoscopic sleeve gastrectomy for morbid obesity: 5 to 8-year results. Obesity surgery. 2017 Jan 1;27(1):59–63. doi: 10.1007/s11695-016-2235-8. [DOI] [PubMed] [Google Scholar]
- 7.Consensus Development Conference Panel. NIH conference. Gastrointestinal surgery for severe obesity. Ann Intern Med. 1991;115:956–61. [PubMed] [Google Scholar]
- 8.Your Practice On ine - IFSO. n.d. Retrieved from http://www.ifso.com/wp-content/themes/ypo-theme/pdfs/tube-gastrectomy.pdf.
- 9.http://care.zulekhahospitals.com/medical-tourism-bariatrics/?utm_source=acs&utm_medium=ppc&keyword=sleeve%20gastrectomy
- 10.Arterburn DE, Courcoulas AP. Bariatric surgery for obesity and metabolic conditions in adults. BMJ. 2014 Aug; doi: 10.1136/bmj.g3961. 27349g3961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Casella G, Soricelli E, Giannotti D, Collalti M, Maselli R, Genco A, et al. Long-term results after laparoscopic sleeve gastrectomy in a large monocentric series. Surgery for Obesity and Related Diseases. 2016 May 1;12(4):757–62. doi: 10.1016/j.soard.2015.09.028. [DOI] [PubMed] [Google Scholar]
- 12.Sieber P, Gass M, Kern B, Peters T, Slawik M, Peterli R. Five-year results of laparoscopic sleeve gastrectomy. Surgery for Obesity and Related Diseases. 2014 Mar 1;10(2):243–9. doi: 10.1016/j.soard.2013.06.024. [DOI] [PubMed] [Google Scholar]
- 13.El-Anwar A, Shaker H. Laparoscopic sleeve gastrectomy for morbid obesity: Does the size of the bougie matter? The Egyptian Journal of Surgery. 2016;35(1):35. doi: 10.4103/1110-1121.176801. [DOI] [Google Scholar]
- 14.Pok E, Lee W, Ser K, Chen J, Chen S, Tsou J, Chin K. Laparoscopic sleeve gastrectomy in Asia: Long term outcome and revisional surgery. Asian Journal of Surgery. 2016;39(1):21–28. doi: 10.1016/j.asjsur.2015.03.006. [DOI] [PubMed] [Google Scholar]
- 15.Seki Y, Kasama K, Hashimoto K. Long-Term Outcome of Laparoscopic Sleeve Gastrectomy in Morbidly Obese Japanese Patients. Obesity Surgery. 2015;26(1):138–145. doi: 10.1007/s11695-015-1728-1. [DOI] [PubMed] [Google Scholar]
- 16.Aridi HD, Alami R, Tamim H, Shamseddine G, Fouani T, Safadi B. Long-term outcomes of laparoscopic sleeve gastrectomy: A Lebanese center experience. Surgery for Obesity and Related Diseases. 2016;12(9):1689–1696. doi: 10.1016/j.soard.2015.11.025. [DOI] [PubMed] [Google Scholar]