Abstract
Background
Breast cancer is the cancer most frequently diagnosed in women worldwide. Even though survival rates are continually increasing, breast cancer is often associated with long‐term psychological distress, chronic pain, fatigue and impaired quality of life. Yoga comprises advice for an ethical lifestyle, spiritual practice, physical activity, breathing exercises and meditation. It is a complementary therapy that is commonly recommended for breast cancer‐related impairments and has been shown to improve physical and mental health in people with different cancer types.
Objectives
To assess effects of yoga on health‐related quality of life, mental health and cancer‐related symptoms among women with a diagnosis of breast cancer who are receiving active treatment or have completed treatment.
Search methods
We searched the Cochrane Breast Cancer Specialised Register, MEDLINE (via PubMed), Embase, the Cochrane Central Register of Controlled Trials (CENTRAL; 2016, Issue 1), Indexing of Indian Medical Journals (IndMED), the World Health Organization (WHO) International Clinical Trials Registry Platform (ICTRP) search portal and Clinicaltrials.gov on 29 January 2016. We also searched reference lists of identified relevant trials or reviews, as well as conference proceedings of the International Congress on Complementary Medicine Research (ICCMR), the European Congress for Integrative Medicine (ECIM) and the American Society of Clinical Oncology (ASCO). We applied no language restrictions.
Selection criteria
Randomised controlled trials were eligible when they (1) compared yoga interventions versus no therapy or versus any other active therapy in women with a diagnosis of non‐metastatic or metastatic breast cancer, and (2) assessed at least one of the primary outcomes on patient‐reported instruments, including health‐related quality of life, depression, anxiety, fatigue or sleep disturbances.
Data collection and analysis
Two review authors independently collected data on methods and results. We expressed outcomes as standardised mean differences (SMDs) with 95% confidence intervals (CIs) and conducted random‐effects model meta‐analyses. We assessed potential risk of publication bias through visual analysis of funnel plot symmetry and heterogeneity between studies by using the Chi2 test and the I2 statistic. We conducted subgroup analyses for current treatment status, time since diagnosis, stage of cancer and type of yoga intervention.
Main results
We included 24 studies with a total of 2166 participants, 23 of which provided data for meta‐analysis. Thirteen studies had low risk of selection bias, five studies reported adequate blinding of outcome assessment and 15 studies had low risk of attrition bias.
Seventeen studies that compared yoga versus no therapy provided moderate‐quality evidence showing that yoga improved health‐related quality of life (pooled SMD 0.22, 95% CI 0.04 to 0.40; 10 studies, 675 participants), reduced fatigue (pooled SMD ‐0.48, 95% CI ‐0.75 to ‐0.20; 11 studies, 883 participants) and reduced sleep disturbances in the short term (pooled SMD ‐0.25, 95% CI ‐0.40 to ‐0.09; six studies, 657 participants). The funnel plot for health‐related quality of life was asymmetrical, favouring no therapy, and the funnel plot for fatigue was roughly symmetrical. This hints at overall low risk of publication bias. Yoga did not appear to reduce depression (pooled SMD ‐0.13, 95% CI ‐0.31 to 0.05; seven studies, 496 participants; low‐quality evidence) or anxiety (pooled SMD ‐0.53, 95% CI ‐1.10 to 0.04; six studies, 346 participants; very low‐quality evidence) in the short term and had no medium‐term effects on health‐related quality of life (pooled SMD 0.10, 95% CI ‐0.23 to 0.42; two studies, 146 participants; low‐quality evidence) or fatigue (pooled SMD ‐0.04, 95% CI ‐0.36 to 0.29; two studies, 146 participants; low‐quality evidence). Investigators reported no serious adverse events.
Four studies that compared yoga versus psychosocial/educational interventions provided moderate‐quality evidence indicating that yoga can reduce depression (pooled SMD ‐2.29, 95% CI ‐3.97 to ‐0.61; four studies, 226 participants), anxiety (pooled SMD ‐2.21, 95% CI ‐3.90 to ‐0.52; three studies, 195 participants) and fatigue (pooled SMD ‐0.90, 95% CI ‐1.31 to ‐0.50; two studies, 106 participants) in the short term. Very low‐quality evidence showed no short‐term effects on health‐related quality of life (pooled SMD 0.81, 95% CI ‐0.50 to 2.12; two studies, 153 participants) or sleep disturbances (pooled SMD ‐0.21, 95% CI ‐0.76 to 0.34; two studies, 119 participants). No trial adequately reported safety‐related data.
Three studies that compared yoga versus exercise presented very low‐quality evidence showing no short‐term effects on health‐related quality of life (pooled SMD ‐0.04, 95% CI ‐0.30 to 0.23; three studies, 233 participants) or fatigue (pooled SMD ‐0.21, 95% CI ‐0.66 to 0.25; three studies, 233 participants); no trial provided safety‐related data.
Authors' conclusions
Moderate‐quality evidence supports the recommendation of yoga as a supportive intervention for improving health‐related quality of life and reducing fatigue and sleep disturbances when compared with no therapy, as well as for reducing depression, anxiety and fatigue, when compared with psychosocial/educational interventions. Very low‐quality evidence suggests that yoga might be as effective as other exercise interventions and might be used as an alternative to other exercise programmes.
Plain language summary
Yoga for women with a diagnosis of breast cancer
What is the issue?
Breast cancer is the most common cancer among women worldwide. Although the number of women who survive breast cancer is increasing, those women often suffer from psychological or physical problems. We wanted to find out whether yoga can improve quality of life, mental health and symptoms related to cancer in women with a diagnosis of breast cancer. We included all forms of yoga but excluded multi‐modal interventions such as mindfulness‐based stress reduction.
Why does it matter?
Many women with a diagnosis of breast cancer try yoga as a means of coping with their symptoms. Thus, it is important to find out whether yoga can really help these women. It is also important to find out whether any risks are associated with practising yoga.
What did we find?
We found 24 studies that involved 2166 women. Our evidence is current to January 2016. We found that women in 11 studies had completed surgery, chemotherapy and radiotherapy; women in three studies were currently undergoing chemotherapy; and women in five studies were currently undergoing radiotherapy. Women in the remaining five studies were either undergoing treatment or were not. Studies used a variety of questionnaires to assess quality of life, depression, fatigue and/or sleep disturbances.
We found that yoga was more effective than no therapy in improving quality of life and reducing fatigue and sleep disturbances. We also found that yoga was better for reducing depression, anxiety and fatigue in women when compared with psychosocial or educational interventions such as counselling. We are fairly certain that these observed results are probably true. Yoga might be as effective as exercise in improving quality of life and reducing fatigue; we do not have enough data to be sure. Studies have poorly reported risks of yoga. However, we found no evidence of serious risks of yoga among women with a diagnosis of breast cancer. No studies have assessed effects of yoga in women given a diagnosis of breast cancer more than five years ago.
What does this mean?
Our findings indicate that women with a diagnosis of breast cancer can use yoga as supportive therapy for improving their quality of life and mental health, in addition to standard cancer treatments.
Summary of findings
Summary of findings for the main comparison. Yoga versus no therapy for women with diagnosed breast cancer.
| Yoga versus no therapy for women with diagnosed breast cancer | ||||
| Patient or population: women with diagnosed breast cancer Settings: inpatient and outpatient facilities Intervention: yoga Comparison: no therapy | ||||
| Outcomes | Illustrative comparative risks* (95% CI) | Number of participants (studies) | Quality of the evidence (GRADE) | Comments |
| Corresponding risk | ||||
| Yoga vs no therapy | ||||
| Health‐related quality of life (short‐term) Self‐assessed questionnaires Follow‐up: 5‐12 weeks | Mean health‐related quality of life in intervention groups was 0.22 standard deviations higher (0.06 to 0.38 higher) | 675 (10 studies) | ⊕⊕⊕⊝ Moderatea | SMD 0.22 (95% CI 0.04 to 0.40) |
| Health‐related quality of life (medium‐term) Self‐assessed questionnaires Follow‐up: 30‐48 weeks | Mean health‐related quality of life in intervention groups was 0.10 standard deviations higher (0.23 lower to 0.42 higher) | 146 (2 studies) | ⊕⊕⊝⊝ Lowb,c | SMD 0.10 (95% CI ‐0.23 to 0.42) |
| Depression (short‐term) Self‐assessed questionnaires Follow‐up: 6‐12 weeks | Mean depression in intervention groups was 0.13 standard deviations lower (0.31 lower to 0.05 higher) | 496 (7 studies) | ⊕⊕⊝⊝ Lowb | SMD ‐0.13 (95% CI ‐0.31 to 0.05) |
| Anxiety (short‐term) Self‐assessed questionnaires Follow‐up: 2‐12 weeks | Mean anxiety in intervention groups was 0.53 standard deviations lower (1.1 lower to 0.04 higher) | 346 (6 studies) | ⊕⊝⊝⊝ Very lowb,d | SMD ‐0.53 (95% CI ‐1.10 to 0.04) |
| Fatigue (short‐term) Self‐assessed questionnaires Follow‐up: 6‐12 weeks | Mean fatigue in intervention groups was 0.49 standard deviations lower (0.75 to 0.23 lower) | 883 (11 studies) | ⊕⊕⊕⊝ Moderated | SMD ‐0.48 (95% CI ‐0.75 to ‐0.20) |
| Fatigue (medium‐term) Self‐assessed questionnaires Follow‐up: 30‐48 weeks | Mean fatigue in intervention groups was 0.04 standard deviations lower (0.36 lower to 0.29 higher) | 146 (2 studies) | ⊕⊕⊝⊝ Lowb,c | SMD ‐0.04 (95% CI ‐0.36 to 0.29) |
| Sleep disturbances (short‐term) Self‐assessed questionnaires Follow‐up: 4‐12 weeks | Mean sleep disturbances in intervention groups were 0.25 standard deviations lower (0.4 to 0.09 lower) | 657 (6 studies) | ⊕⊕⊕⊝ Moderatea | SMD ‐0.25 (95% CI ‐0.40 to ‐0.09) |
| *The basis for the assumed risk (e.g. median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; SMD: standardised mean difference. | ||||
| GRADE Working Group grades of evidence. High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||
aDowngraded one level because the 95% confidence interval includes negligible effects. bDowngraded two levels because the 95% confidence interval includes no effect. cDowngraded one level because fewer than 400 participants were included in the total. dDowngraded one level because of widely differing estimates of the treatment effect.
Summary of findings 2. Yoga versus psychosocial/educational interventions for women with diagnosed breast cancer.
| Yoga versus psychosocial/educational interventions for women with diagnosed breast cancer | ||||
| Patient or population: women with diagnosed breast cancer Settings: inpatient and outpatient facilities Intervention: yoga Comparison: psychosocial/educational interventions | ||||
| Outcomes | Illustrative comparative risks* (95% CI) | Number of participants (studies) | Quality of the evidence (GRADE) | Comments |
| Corresponding risk | ||||
| Yoga vs psychosocial/educationalinterventions | ||||
| Health‐related quality of life (short‐term) Self‐assessed questionnaires Follow‐up: 6 weeks | Mean health‐related quality of life in intervention groups was 0.81 standard deviations higher (0.5 lower to 2.12 higher) | 153 (2 studies) | ⊕⊝⊝⊝ Very lowa,b,c,d | SMD 0.81 (95% CI ‐0.50 to 2.12) |
| Depression (short‐term) Self‐assessed questionnaires Follow‐up: 6‐12 weeks | Mean depression in intervention groups was 2.29 standard deviations lower (3.97 to 0.61 lower) | 226 (4 studies) | ⊕⊕⊕⊝ Moderatec | SMD ‐2.29 (95% CI ‐3.97 to ‐0.61) |
| Anxiety (short‐term) Self‐assessed questionnaires Follow‐up: 6 weeks | Mean anxiety in intervention groups was 2.21 standard deviations lower (3.9 to 0.52 lower) | 195 (3 studies) | ⊕⊕⊝⊝ Lowa,c | SMD ‐2.21 (95% CI ‐3.90 to ‐0.52) |
| Fatigue (short‐term) Self‐assessed questionnaires Follow‐up: 6‐12 weeks | Mean fatigue in intervention groups was 0.90 standard deviations lower (1.31 to 0.5 lower) | 106 (2 studies) | ⊕⊕⊕⊝ Moderatec | SMD ‐0.90 (95% CI ‐1.31 to ‐0.50) |
| Sleep disturbances (short‐term) Self‐assessed questionnaires Follow‐up: 6‐12 weeks | Mean sleep disturbances in intervention groups were 0.21 standard deviations lower (0.76 lower to 0.34 higher) | 119 (2 studies) | ⊕⊝⊝⊝ Very lowb,c,d | SMD ‐0.21 (95% CI ‐0.76 to 0.34) |
| *The basis for the assumed risk (e.g. median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; SMD: standardised mean difference. | ||||
| GRADE Working Group grades of evidence. High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||
aDowngraded one level because of overall unclear risk of bias. bDowngraded one level because of widely differing estimates of the treatment effect. cDowngraded one level because fewer than 400 participants were included in the total. dDowngraded two levels because the 95% confidence interval includes no effect.
Summary of findings 3. Yoga versus exercise for women with diagnosed breast cancer.
| Yoga versus exercise for women with diagnosed breast cancer | ||||
| Patient or population: women with diagnosed breast cancer Settings: inpatient and outpatient facilities Intervention: yoga Comparison: exercise | ||||
| Outcomes | Illustrative comparative risks* (95% CI) | Number of participants (studies) | Quality of the evidence (GRADE) | Comments |
| Corresponding risk | ||||
| Yoga vs exercise | ||||
| Health‐related quality of life Self‐assessed questionnaires Follow‐up: 6‐12 weeks | Mean health‐related quality of life in intervention groups was 0.04 standard deviations lower (0.30 lower to 0.23 higher) | 233 (3 studies) | ⊕⊝⊝⊝ Very lowa,b,c,d | SMD ‐0.04 (95% CI ‐0.30 to 0.23) |
| Fatigue Self‐assessed questionnaires Follow‐up: 6‐12 weeks | Mean fatigue in intervention groups was 0.21 standard deviations lower (0.66 lower to 0.25 higher) | 233 (3 studies) | ⊕⊝⊝⊝ Very lowa,b,c,d | SMD ‐0.21 (95% CI ‐0.66 to 0.25) |
| *The basis for the assumed risk (e.g. median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; SMD: standardised mean difference. | ||||
| GRADE Working Group grades of evidence. High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||
aDowngraded one level because of overall unclear risk of bias. bDowngraded two levels because the 95% confidence interval includes no effect. cDowngraded one level because fewer than 400 participants were included in the total. dDowngraded two levels because the 95% confidence interval includes no effect.
Background
Description of the condition
With more than 1.67 million new cases each year, breast cancer is the most frequently diagnosed cancer among women worldwide (Ferlay 2013). Although more than 522,000 women die from breast cancer each year (Ferlay 2013), advances in cancer prevention, diagnosis and treatment have led to continually improved survival rates (Berry 2005). During breast cancer treatment, about one‐third of women experience substantial psychological distress, mainly depression and anxiety (Maass 2015;Rottmann 2016;Stafford 2013), which can persist over years after completion of treatment (Hopwood 2010; Maass 2015;Rottmann 2016). These psychological impairments can aggravate symptom burden and can seriously affect health‐related quality of life (Andrykowski 2008). Cancer‐related fatigue is another important symptom that interferes with usual functioning (Jones 2016;Patrick 2003). Up to 90% of women with breast cancer experience fatigue during chemotherapy (Hartvig 2006; Li 2016;Schmidt 2012) that may endure for several years (Abrahams 2016;Bower 2006; Garabeli Cavalli Kluthcovsky 2012;Jones 2016). Sleep disturbances are highly prevalent among women with breast cancer before surgery, during subsequent chemotherapy (Van Onselen 2012) and during antihormonal treatment (Desai 2013).
Description of the intervention
Yoga has its roots in Indian philosophy and has been a part of traditional Indian spiritual practice for about 4000 years (Feuerstein 1998). Yoga is a complex intervention that comprises advice for an ethical lifestyle, spiritual practice, physical activity, breathing exercises and meditation (De Michaelis 2005; Feuerstein 1998). Although yoga originally evolved as a spiritual practice, it has become a popular means of promoting physical and mental well‐being (De Michaelis 2005; Feuerstein 1998). In North America and Europe, yoga most often is associated with physical postures (asanas), breathing techniques (pranayama) and meditation (dyana) (De Michaelis 2005; Feuerstein 1998). Contrary to popular perceptions, meditation and breathing techniques are inherent parts of yoga practice. Different yoga forms have emerged that put varying focus on physical and mental practices (Feuerstein 1998). Although most forms of yoga practised in North America and Europe focus mainly on postures, many yoga traditions include only meditation (Shannahoff‐Khalsa 2005) or breathing techniques (Brown 2005) without specific physical components. An estimated 31 million American adults report that they have practised yoga at least once in their lifetime (Cramer 2016).
How the intervention might work
It is now widely accepted that therapeutic exercise programmes for women with a diagnosis of breast cancer who are receiving active treatment or have completed treatment can significantly improve physical functioning and quality of life, and can mitigate fatigue (McNeely 2006; Visovsky 2006). In addition, exercise decreases the percentage of body fat, improves cardiopulmonary function (Kim 2009; McNeely 2006) and decreases mortality among women who have completed treatment for breast cancer (Ibrahim 2011). Physical exercise reduces the blood level of the blood sugar‐lowering hormone insulin (Irwin 2009), strengthens the immune system and promotes the catabolism of stress hormones and oestrogens (Neilson 2009). Furthermore, exercising together in a group of similarly affected women should enhance the individual’s quality of life (Floyd 2009). Yoga involves physical activity, but it differs from purely gymnastic exercise in that the practitioner focusses her mind on specific postures with inner awareness and a meditative focus of mind (Büssing 2011; Cramer 2013). The mechanism proposed to explain how yoga can positively influence mental and physical health involves a decrease in dysregulation within the hypothalamic‐pituitary‐adrenal axis; this is known as the stress response (Carroll 2012; Streeter 2012). Yoga can decrease subjective stress in healthy adults (Chong 2011) and can reduce plasma levels of the stress hormone cortisol in individuals with cancer (Banasik 2011; Vadiraja 2009c) and in psychiatric patients (Devi 1986; Vedamurthachar 2006). Imaging studies have shown that yoga can increase endogenous release of the neurotransmitter, dopamine, within the ventral striatum (Kjaer 2002), as well as thalamic levels of the neurotransmitter, gamma‐aminobutyric acid (GABA) (Streeter 2010). Both dopamine (Syvälahti 1994) and GABA (Kalueff 2007) play a major role in the pathophysiology of psychological distress. It has been hypothesised that by increasing GABA activity, yoga can reduce allostatic load within stress response systems such that optimal homeostasis is restored (Streeter 2012).
Why it is important to do this review
Many women who currently are undergoing treatment or have completed treatment for breast cancer use complementary medicine (NIH 2012) to manage effects of the disease (Fouladbakhsh 2010), and yoga is among the most commonly used complementary therapies for breast cancer‐related impairment (Fouladbakhsh 2010). Systematic reviews and meta‐analyses have shown that yoga can improve health‐related quality of life among patients with cancer (Buffart 2012; Culos‐Reed 2012; Lin 2011; Smith 2009). However, as individuals with different types of cancer are heterogeneous in terms of sociodemographic factors, symptoms, treatments and side effects, meta‐analyses should focus on homogenous cancer groups. It is obvious from previous reviews that a vast majority of studies on yoga for cancer have involved women receiving active treatment or women who have completed treatment for breast cancer. Five systematic reviews so far have explicitly focussed on women undergoing treatment or those who have completed treatment for breast cancer (Cramer 2012b; Harder 2012; Levine 2012; Pan 2015; Zhang 2012), and only three of these included meta‐analyses (Cramer 2012b; Pan 2015; Zhang 2012). On the basis of six randomised trials that compared yoga versus no treatment, Zhang 2012 described statistically significant effects favouring yoga for health‐related quality of life but not for psychological outcomes. In contrast, Cramer 2012b found positive effects of yoga compared with no treatment or active control interventions on health‐related quality of life, depression and anxiety. Besides health‐related quality of life and mental health, only one prior review assessed physical cancer‐related symptoms, and this review did not include a meta‐analysis (Harder 2012). Evidence of effects on fatigue was inconclusive, with three of seven included trials reporting positive effects of yoga. Finally, Pan 2015 reported effects on health‐related quality of life, depression and anxiety.
Primarily on the basis of anecdotal evidence, the lay press has questioned the safety of yoga (Broad 2012). As this seems to have led to general uncertainty among yoga practitioners and those interested in starting practice, it seems important to systematically assess the safety of yoga. However, no prior review on yoga for women with breast cancer has quantitatively analysed safety data. Therefore, a comprehensive review of both efficacy (in terms of health‐related quality of life, physical and mental health) and safety of yoga for women undergoing active treatment or who have completed treatment for breast cancer seems warranted.
Objectives
To assess effects of yoga on health‐related quality of life, mental health and cancer‐related symptoms among women with a diagnosis of breast cancer who are receiving active treatment or have completed treatment.
Methods
Criteria for considering studies for this review
Types of studies
All randomised controlled trials (RCTs) assessing effects of yoga in women with breast cancer who are undergoing treatment or have completed treatment, or both. Both full‐text and abstract publications were eligible if sufficient information was available on study design, characteristics of participants, interventions and outcomes.
Types of participants
Women with a histologically confirmed diagnosis of non‐metastatic or metastatic breast carcinoma (stage I to IV), as defined by the American Joint Committee on Cancer (AJCC) tumour‐node‐metastasis (TNM) system (Compton 2012).
Women with a diagnosis of breast cancer who have completed treatment (i.e. have completed initial management of stage I to IV breast cancer) were also eligible.
We applied no limits regarding age groups or settings.
We excluded studies including participants with other cancer types unless outcomes for women with breast cancer were reported separately.
Types of interventions
Any form of yoga was eligible as the experimental intervention (i.e. Hatha yoga, Ashtanga yoga, Iyengar yoga, Integrated yoga therapy, Viniyoga, Bikram Yoga, Sivananda yoga, Kundalini yoga, Tibetan yoga, Yoga of Awareness or any other yoga form). Studies that did not mention a specific form of yoga but simply described the intervention as 'yoga' were also eligible. Interventions included at least one of the following: yoga postures, breath control, meditation and lifestyle advice (based on yoga theory or traditional yoga practices).
We excluded studies on multi‐modal interventions such as mindfulness‐based stress reduction, mindfulness‐based cognitive therapy or the Mind Body Program for Cancer by the Benson‐Henry Institute for Mind Body Medicine (which includes yoga among other therapies), as the relative effects of yogic practices could not be assessed separately in such programmes.
Attention control, wait‐list control, treatment as usual, no therapy and any other active therapy were eligible as comparators.
Breast cancer treatments such as chemotherapy, radiotherapy or antihormonal therapy and supportive care were allowed, as long as cointerventions were comparable between groups.
Types of outcome measures
Primary outcomes
Health‐related quality of life, assessed by any validated generic or disease‐specific self‐report scale
Depression, assessed by any validated self‐report or clinician‐rated scale
Anxiety, assessed by any validated self‐report or clinician‐rated scale
Fatigue, assessed by any validated self‐report scale
Sleep disturbances, assessed by any validated self‐report scale
When investigators assessed an outcome using more than one measure, we preferred standard instruments over novel instruments and multi‐item instruments over single‐item instruments.
Secondary outcomes
Safety of the intervention, assessed as the number of women with adverse events and the number of women with severe adverse events
Search methods for identification of studies
Electronic searches
We searched the following databases.
Cochrane Breast Cancer Specialised Register. Details of search strategies used by the Cochrane Breast Cancer Group (CBCG) for identification of studies and procedures used to code references are outlined in the CBCG module at www.mrw.interscience.wiley.com/cochrane/clabout/articles/BREASTCA/frame.html. We included trials with the following terms: "breast cancer", "early breast cancer", "locally advanced breast cancer", "advanced breast cancer", "high risk", "yoga", "alternative/complementary therapy", "yogic", "asana", "pranayama", "dhyana", "dharana" and "meditation".
MEDLINE (via PubMed) on 29 January 2016. See Appendix 1.
Embase (via Embase.com or OvidSP) on 29 January 2016. See Appendix 2.
Cochrane Central Register of Controlled Trials (CENTRAL; 2016, Issue 1). See Appendix 3.
World Health Organization (WHO) International Clinical Trials Registry Platform (ICTRP) search portal (http://apps.who.int/trialsearch/Default.aspx) for all prospectively registered and ongoing trials on 29 January 2016. See Appendix 4.
Clinicaltrials.gov (http://clinicaltrials.gov/) on 29 January 2016. See Appendix 5.
Indexing of Indian Medical Journals (IndMED) (http://indmed.nic.in/indmed.html) on 12 February 2016. See Appendix 6.
Searching other resources
Bibliographic search
We attempted to identify additional studies by searching reference lists of identified relevant trials or reviews. We obtained a copy of the full text of each reference reporting a potentially eligible trial. When this was not possible, we made attempts to contact study authors to ask them to provide additional information.
Grey literature search
We searched conference proceedings of the following congresses and annual meetings of societies for relevant abstracts.
International Congress on Complementary Medicine Research (ICCMR); searched up to 2015.
European Congress for Integrative Medicine (ECIM); searched up to 2015.
American Society of Clinical Oncology (ASCO); searched up to 2015.
Data collection and analysis
Selection of studies
Two review authors (HC and RL) screened independently the titles and abstracts of studies identified during the literature search and read potentially eligible articles in full to determine whether they met review eligibility criteria. We discussed disagreements with a third review author (PK) until we reached consensus. If necessary, we obtained additional information from study authors.
We recorded excluded studies in the Characteristics of excluded studies table.
We documented the study selection process in a PRISMA (Preferred Reporting Items for Systematic Reviews and Meta‐Analyses) flow chart (Moher 2009).
We applied no language restrictions and arranged for translation of studies published in languages other than English, German, French, Russian, Chinese, Norwegian, Swedish or Icelandic.
Data extraction and management
Two review authors (PK and SL) independently extracted and entered data from all included studies into the Characteristics of included studies table using Review Manager software (RevMan). We discussed disagreements with a third review author (HC, JL or GD) until we reached consensus. A third review author (HC, JL or GD) checked the extracted data.
Information collected included the following.
Methods: study design, methods of allocation, allocation concealment, blinding, dropout rates and reasons for dropping out.
Participants: country of origin, setting, sample size, diagnosis, age, ethnicity.
Intervention: type, programme length, frequency, duration (for experimental and comparator interventions).
Outcomes: types of outcomes, assessment instruments, assessment time point, follow‐up time point.
For studies with more than one publication, we considered the first publication as the primary reference, but we extracted data from all publications.
HC, RL and GD were not involved in data extraction or management for Cramer 2015.
Assessment of risk of bias in included studies
Two review authors (PK and SL) independently assessed risk of bias using the Cochrane 'Risk of bias assessment tool' (Higgins 2011). We assessed risk of bias for the following domains.
Random sequence generation.
Allocation concealment.
Blinding of participants and personnel.
Blinding of outcome assessment.
Incomplete outcome data.
Selective outcome reporting.
Other sources of bias.
We judged each domain as:
'low risk of bias' if requirements were adequately fulfilled, as described in Higgins 2011;
'high risk of bias' if requirements were not adequately fulfilled, as described in Higgins 2011; or
'unclear risk of bias' if data provided were insufficient for a judgement.
We incorporated risk of bias when we judged the quality of evidence for each outcome according to GRADE recommendations (Guyatt 2008).
HC, RL and GD were not involved in assessment of risk of bias for Cramer 2015.
Measures of treatment effect
We classified primary outcomes as continuous outcomes and expressed them as standardised mean differences (SMDs) with 95% confidence intervals (CIs) according to recommendations provided in the Cochrane Handbook for Systematic Reviews of Interventions (Chapter 7, Section 7.7.3) (Higgins 2011). The SMD expresses the size of the intervention effect in each study relative to the variability observed in that study. It can be used when all studies assess the same outcome but measure it in a variety of ways such as through different questionnaires. We used Hedges' correction to calculate SMD as the difference in means between groups divided by the pooled standard deviation (SD). When available, we preferred final values over change scores. We defined a positive SMD as indicating beneficial effects of the experimental intervention compared with the comparator intervention for quality of life, and a negative SMD as indicating beneficial effects for mental health and cancer‐related symptoms. If necessary, we inverted scores by subtracting the mean from zero (Higgins 2011).
We classified secondary outcomes as dichotomous outcomes and expressed them as risk ratios (RRs) with 95% CIs. Risk describes the probability that a health outcome will occur. Risk ratio is the ratio of risk of this health outcome in the two groups. We calculated the RR by dividing the risk of an event in the experimental group (i.e. the number of participants with the respective outcome divided by the total number of participants) by the risk of the event in the control group. We defined RRs less than 1.0 as favouring the experimental group (i.e. fewer adverse events than in the comparator group) and RRs greater than 1.0 as favouring the comparator group (Higgins 2011).
Unit of analysis issues
We handled special issues in the analysis of studies with non‐standard designs according to suggestions provided in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). For cross‐over trials, we planned to analyse paired data if available. Elsewise, we planned to use only data from the first active treatment. We included no cross‐over trials in the review.
For studies that contributed multiple, correlated comparisons, we planned to combine all relevant experimental intervention groups in the study (e.g. groups with yoga interventions of different intensities) into a single group and to combine all comparable relevant control intervention groups (e.g. groups with exercise interventions of different intensities) into a single control group. We included in the review no studies with multiple, correlated comparisons. We did not combine control groups with different types of interventions (e.g. wait‐list control and exercise) in a single meta‐analysis but analysed them separately. In this review, we included Chandwani 2014, a three‐arm study involving two control groups (i.e. yoga vs wait‐list/usual care (control); yoga vs exercise (control)). In analyses, we did not combine these two comparisons from one study but reported them separately.
If repeated outcome assessments were presented, we defined the time frames as short‐term (up to six months), medium‐term (six to 12 months) and long‐term follow‐up (longer than 12 months).
Dealing with missing data
When SDs were missing, we calculated them from standard errors, confidence intervals or t values, or we attempted by email to obtain the missing data from trial authors (Higgins 2011). If these data were not available, and SDs were missing, we planned to replace them with the mean of SDs of available studies that used the same outcome scale. This was not necessary for any of the studies. When means were missing, we attempted by email to obtain the missing data from trial authors.
We conducted sensitivity analyses by excluding studies for which missing data had to be substituted (see below).
We addressed in the Discussion section the potential impact of missing data on review findings.
Assessment of heterogeneity
We assessed statistical heterogeneity between studies by using the Chi2 test (Cochran 1954). We determined that a P value ≤ 0.10 indicates statistically significant heterogeneity. We also used the I2 statistic (Higgins 2003) to categorise the magnitude of heterogeneity as follows: I2 = 0% to 24%: low heterogeneity; I2 = 25% to 49%: moderate heterogeneity; I2 = 50% to 74%: substantial heterogeneity; and I2 = 75% to 100%: considerable heterogeneity.
Assessment of reporting biases
If we included at least 10 studies in a meta‐analysis, we generated funnel plots of effect estimates against their standard errors (on a reversed scale) by using Review Manager software (RevMan). We assessed potential risk of publication bias through visual analysis of funnel plots, with roughly symmetrical funnel plots indicating low risk and asymmetrical funnel plots hinting at high risk of publication bias (Higgins 2011). One should be aware that this is a rather subjective judgement, that funnel plot asymmetry might also arise from other sources and that publication bias need not lead to asymmetry in funnel plots. We further attempted to avoid publication bias by searching trials registries and conference proceedings for unpublished studies.
We addressed duplicate publication bias by including only once studies with more than one publication. If we had doubt about whether multiple publications referred to the same data, we attempted to contact trial authors by email.
We addressed location bias by searching multiple databases, including one Indian journal, and by including non‐English language journals.
We avoided language bias by including studies irrespective of the language of publication.
Data synthesis
For continuous outcomes, we pooled data by using a random‐effects model and the inverse variance method. For dichotomous outcomes, we used the random‐effects model of DerSimonian and Laird. We performed all analyses by using Review Manager 5 software (RevMan).
To grade the quality of evidence, we used the GRADE approach (Brozek 2009), along with GradePro software. We created a 'Summary of findings' table to present evidence for primary outcomes (health‐related quality, depression, anxiety, fatigue and sleep disturbances).
Subgroup analysis and investigation of heterogeneity
We conducted subgroup analyses for the following.
Current treatment status.
Women with breast cancer undergoing active cancer treatment (radiotherapy or chemotherapy).
Women who had completed active treatment.
Time since diagnosis.
Women with breast cancer diagnosed within five years before the time of study entry.
Women with breast cancer diagnosed more than five years before the time of study entry.
Stage of cancer.
Metastatic breast cancer at the time of study entry.
Non‐metastatic breast cancer at the time of study entry.
We conducted additional subgroup analyses for the type of yoga intervention.
Complex yoga interventions, including physical exercise and at least one of the following: breath control, meditation and lifestyle advice (based on yoga theory or traditional yoga practices).
Exercise‐based yoga interventions based on yoga theory or traditional yoga practices without breath control, meditation or lifestyle advice.
Meditation‐based yoga interventions, including at least one of the following: breath control, meditation and lifestyle advice (based on yoga theory or traditional yoga practices) without an exercise component.
We tested subgroup differences using the Chi2 test for heterogeneity across subgroups. We computed the I2 statistic for subgroup differences as the percentage of variance between different subgroups that is due to genuine subgroup differences rather than to chance (Higgins 2011).
If statistically significant heterogeneity was present in the respective meta‐analysis, we used subgroup and sensitivity analyses to explore possible reasons for the heterogeneity. However, given that the main purpose of subgroup analyses was to assess differences between subgroups, rather than to explore reasons for heterogeneity, we performed subgroup analyses regardless of the presence or absence of statically significant heterogeneity.
Sensitivity analysis
We performed sensitivity analyses by subsequently excluding studies with inadequate random sequence generation, studies with inadequate allocation concealment, studies without blinding of outcome assessors and studies with high risk of attrition bias.
We performed additional sensitivity analyses by excluding studies for which missing data had to be retrieved from study authors or imputed, and by excluding studies that were unpublished or were published only in abstract format.
Results
Description of studies
Results of the search
The literature search revealed a total of 428 records, and we obtained four records from other sources (Bernardi 2013; Blank 2005; Lötzke 2016; Ojha 2012). We screened the titles and abstracts of a total of 307 non‐duplicate records and excluded 245 because they did not meet eligibility criteria. We assessed a total of 62 full texts related to 32 studies. Of these, we excluded full texts on three studies for reasons provided in the Excluded studies section; in addition, seven full texts on five studies did not provide enough information to be classified and categorised as Characteristics of studies awaiting classification. Searching ICCMR, ECIM and ASCO conference proceedings did not yield additional relevant abstracts that had not already been identified through database searches; searching the WHO ICTRP search portal and Clinicaltrials.gov revealed no relevant ongoing studies.
Finally, we included in the qualitative synthesis 52 full texts on 24 studies with a total of 2166 women with a diagnosis of breast cancer. One of those studies did not provide measures of dispersion (Carson 2009). Because we could not obtain this information from the study authors, we excluded this study from quantitative analysis, leaving a total of 23 studies with 2129 participants included in the meta‐analysis. Figure 1 shows the flow of the literature search, included and excluded studies and those awaiting classification.
1.
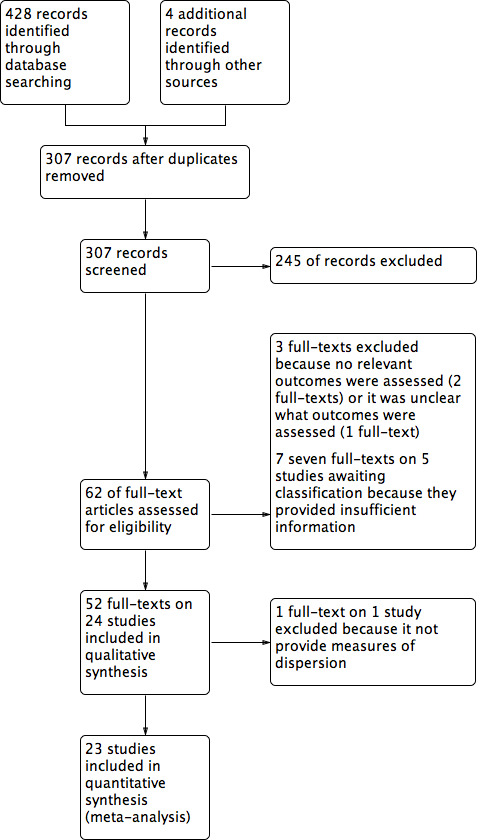
Study flow diagram.
Included studies
Study and participant characteristics
All studies were randomised controlled trials (RCTs) with parallel groups; two studies used minimisation (Chandwani 2010; Moadel 2007), and one study used adaptive randomisation (Chandwani 2014).
Of the 24 included studies, 11 originated from the USA (Banasik 2011;Bower 2012; Carson 2009; Chandwani 2010; Chandwani 2014; Danhauer 2009; Kiecolt‐Glaser 2014; Littman 2012; Moadel 2007; Mustian 2013; Pruthi 2012), one from Brazil (Bernardi 2013), three from Germany (Cramer 2015; Lötzke 2016; Siedentopf 2013), one from Slovenia (Kovacic 2013), one from Australia (Loudon 2014), four from India (Banerjee 2007; Chakrabarty 2015; Raghavendra 2007; Vadiraja 2009), one from Turkey (Vardar Yağlı 2015), one from China (Wang 2014) and one from Taiwan (Taso 2014).
Investigators recruited women from hospitals or clinical research centres (Banasik 2011; Banerjee 2007; Bernardi 2013; Carson 2009; Chakrabarty 2015; Chandwani 2010; Chandwani 2014; Cramer 2015; Danhauer 2009; Kiecolt‐Glaser 2014; Kovacic 2013; Lötzke 2016; Moadel 2007; Pruthi 2012; Raghavendra 2007; Siedentopf 2013; Taso 2014; Vadiraja 2009; Vardar Yağlı 2015; Wang 2014) and private clinics or health centres (Littman 2012; Loudon 2014; Moadel 2007; Mustian 2013) and through mailings or advertisements (Bower 2012; Littman 2012; Mustian 2013).
Studies included a total of 2166 women. Sample sizes ranged from 18 to 309, with a median of 74.5. Women’s mean age ranged from 44.0 to 62.9 years, with a median of 54.0 years. All studies included women with non‐metastatic breast cancer; one study additionally included women with metastatic breast cancer (Banasik 2011).
In 16 studies, women received a diagnosis of breast cancer within five years before the time of study entry (Banerjee 2007; Bernardi 2013; Chakrabarty 2015; Chandwani 2010; Chandwani 2014; Danhauer 2009; Kovacic 2013; Lötzke 2016; Moadel 2007; Mustian 2013; Pruthi 2012; Raghavendra 2007; Siedentopf 2013; Taso 2014; Vadiraja 2009; Wang 2014). Four studies included both women who received a diagnosis within five years and women who received a diagnosis more than five years before the time of study entry (Bower 2012; Carson 2009; Littman 2012; Vardar Yağlı 2015), two studies reported only mean time since diagnosis but no range (Cramer 2015; Kiecolt‐Glaser 2014) and two studies did not report time since diagnosis (Banasik 2011; Loudon 2014). None of the studies explicitly included only women who received a diagnosis of breast cancer more than five years before the time of study entry. Women in 11 studies had completed active cancer treatment (Banasik 2011; Bernardi 2013; Bower 2012; Carson 2009; Cramer 2015; Danhauer 2009; Kiecolt‐Glaser 2014; Littman 2012; Loudon 2014; Mustian 2013; Vardar Yağlı 2015), women in three studies were undergoing chemotherapy at the start of the study (Raghavendra 2007; Siedentopf 2013; Wang 2014), women in five studies were undergoing radiotherapy at the start of the study (Banerjee 2007; Chakrabarty 2015; Chandwani 2010; Chandwani 2014; Vadiraja 2009) and women in five studies were at various stages of cancer treatment (Kovacic 2013; Lötzke 2016; Moadel 2007; Pruthi 2012; Taso 2014).
Intervention characteristics
Two of the included studies used hatha yoga (an umbrella term for physically oriented yoga styles) without classifying the specific style (Kiecolt‐Glaser 2014; Moadel 2007), and five studies did not report the specific yoga style used (Bernardi 2013; Chakrabarty 2015; Pruthi 2012; Vardar Yağlı 2015; Wang 2014). Remaining studies used a variety of yoga styles: Anusara yoga (Taso 2014), Gitananda yoga (Siedentopf 2013), integrated yoga (Banerjee 2007; Chandwani 2014; Raghavendra 2007; Vadiraja 2009), Iyengar yoga (Banasik 2011; Bower 2012; Lötzke 2016), restorative yoga (Danhauer 2009), Satyananda yoga (Loudon 2014), Sivananda yoga (Cramer 2015), Viniyoga (Littman 2012; Siedentopf 2013), yoga based on Patanjali's yoga sutra (Chandwani 2010), the Yoga in Daily Life® system (Kovacic 2013), the Yoga for Cancer Survivors (YOCAS®) programme (Mustian 2013) and yoga of awareness (Carson 2009).
Of these, investigators classified 21 studies as using complex yoga interventions (Banerjee 2007; Bernardi 2013; Bower 2012; Carson 2009; Chandwani 2010; Chandwani 2014; Cramer 2015; Danhauer 2009; Kiecolt‐Glaser 2014; Kovacic 2013; Littman 2012; Lötzke 2016; Loudon 2014; Moadel 2007; Mustian 2013; Pruthi 2012; Raghavendra 2007; Siedentopf 2013; Taso 2014; Vadiraja 2009; Vardar Yağlı 2015), two as using exercise‐based yoga interventions (Banasik 2011; Wang 2014) and one as using a meditation‐based yoga intervention (Chakrabarty 2015).
The duration of yoga programmes ranged from two weeks to six months, with a median duration of eight weeks; the frequency of yoga interventions ranged from one to 10 (median: two) weekly yoga sessions of 20 to 120 (median: 67.5) minutes in length.
All but one study included one control group; Chandwani 2014 used two control groups (as defined in the protocol, the two groups were not combined in a single meta‐analysis but were analysed separately). Seventeen studies compared yoga versus no specific therapy (Banasik 2011; Bernardi 2013; Carson 2009; Chakrabarty 2015; Chandwani 2010; Chandwani 2014; Cramer 2015; Danhauer 2009; Kiecolt‐Glaser 2014; Littman 2012; Loudon 2014; Moadel 2007; Mustian 2013; Pruthi 2012; Siedentopf 2013; Taso 2014; Wang 2014); one study compared a combination of yoga and physiotherapy versus physiotherapy alone (Kovacic 2013); four studies compared yoga versus psychosocial or educational interventions, that is, active interventions not focussed on physical exercise, including supportive counselling or psychotherapy (Banerjee 2007; Raghavendra 2007; Vadiraja 2009) and health education (Bower 2012); and three studies compared yoga versus exercise, including stretching (Chandwani 2014), aerobic exercise (Vardar Yağlı 2015) and other not further defined physical exercise (Lötzke 2016).
Outcome measures
Fifteen studies assessed health‐related quality of life using the Medical Outcomes Study 36‐item short‐form health survey (Bower 2012; Chandwani 2010; Chandwani 2014; Kiecolt‐Glaser 2014), the Medical Outcomes Study 12‐item short‐form health survey (Danhauer 2009), the Functional Assessment of Cancer Therapy ‐ Breast (Cramer 2015; Danhauer 2009; Moadel 2007; Pruthi 2012), the Functional Assessment of Cancer Therapy ‐ General (Littman 2012), the Functional Assessment of Chronic Illness Therapy ‐ Spiritual Well‐Being (Danhauer 2009; Moadel 2007), the Lymphoedema Quality of Life Tool (Loudon 2014), the European Organisation of Research and Treatment of Cancer QLQ‐30 (Lötzke 2016; Siedentopf 2013; Vadiraja 2009; Vardar Yağlı 2015) or the Functional Living Index ‐ Cancer (Raghavendra 2007).
Eleven studies assessed depression using the Hospital Anxiety and Depression Scale (Banerjee 2007; Cramer 2015; Vadiraja 2009), the Beck Depression Inventory (Bower 2012; Raghavendra 2007), the Center for Epidemiologic Studies Depression Scale (Chandwani 2010; Chandwani 2014; Danhauer 2009; Kiecolt‐Glaser 2014) or the Profile of Mood States (Pruthi 2012; Taso 2014).
Ten studies measured anxiety using the Hospital Anxiety and Depression Scale (Banerjee 2007; Cramer 2015; Vadiraja 2009), the State‐Trait Anxiety Inventory (Bernardi 2013; Chandwani 2010; Kovacic 2013; Raghavendra 2007), the Distressed Mood Index (Moadel 2007) or the Profile of Mood States (Pruthi 2012; Taso 2014).
Seventeen studies assessed fatigue using the Fatigue Symptom Inventory (Bower 2012), the Multidimensional Fatigue Symptom Inventory (Bower 2012; Kiecolt‐Glaser 2014), the Brief Fatigue Inventory (Chandwani 2010; Chandwani 2014; Pruthi 2012; Taso 2014), the Functional Assessment of Chronic Illness Therapy ‐ Fatigue (Cramer 2015; Danhauer 2009; Littman 2012; Moadel 2007), the Cancer Fatigue Scale (Lötzke 2016; Wang 2014), the European Organisation of Research and Treatment of Cancer QLQ‐30 (Lötzke 2016; Vadiraja 2009), the Profile of Mood States ‐ Short Form (Pruthi 2012), the Fatigue Severity Scale (Vardar Yağlı 2015), a daily diary (Carson 2009), a visual analogue scale (Loudon 2014) or a self‐designed instrument (Chakrabarty 2015).
Eight studies measured sleep quality using the Pittsburgh Sleep Quality Index (Bower 2012; Chandwani 2010; Chandwani 2014; Danhauer 2009; Kiecolt‐Glaser 2014; Mustian 2013) or the European Organisation of Research and Treatment of Cancer QLQ‐30 (Vadiraja 2009; Vardar Yağlı 2015).
Five studies reported safety assessed as numbers of adverse events (Cramer 2015; Danhauer 2009; Kiecolt‐Glaser 2014; Mustian 2013) or intervention‐related adverse events (Bower 2012).
The time point of longest follow‐up ranged from four to 48 weeks, with a median of 12 weeks. We classified all but two studies as assessing short‐term effects; one study as assessing short‐term and medium‐term effects (Chandwani 2014); and one study as assessing only medium‐term effects (Littman 2012).
Excluded studies
We excluded three studies after full‐text review. Two studies assessed no outcomes relevant to this review (Blank 2005; Kumar 2013). A third study used a modified version of a standard outcome measure and provided an inconsistent description of what this instrument was intended to measure; thus, it remained unclear whether investigators assessed any relevant outcomes (Ojha 2012).
Studies awaiting classification
Five studies with a total of 565 participants are awaiting classification; these studies, which were published as conference abstracts only, provided insufficient information to be included in the review (Cohen 2015; Dominique 2010; Kumari 2015; Luu 2014; Stan 2013). We contacted the authors of the respective abstracts regarding publication status; two replied that the publishing process was ongoing (Cohen 2015; Dominique 2010), but three did not reply (Kumari 2015; Luu 2014; Stan 2013).
Risk of bias in included studies
We have provided a graphical representation of the risk of bias assessment in Figure 2. Refer to the Characteristics of included studies table for the full risk of bias assessment for each study.
2.
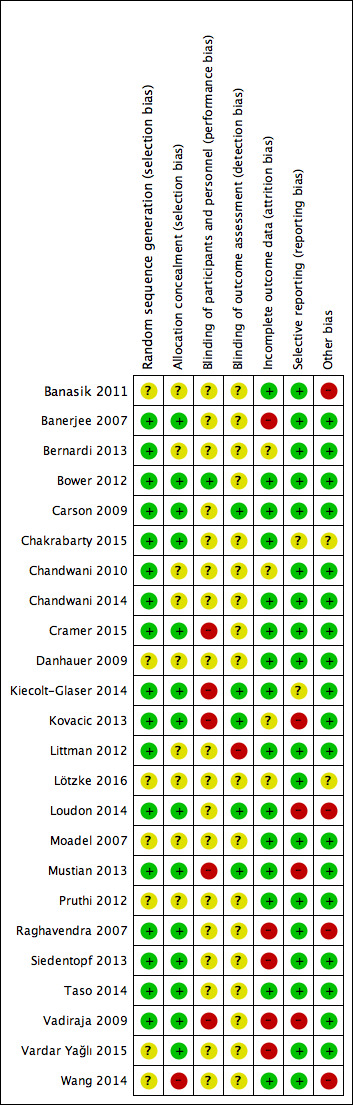
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
All included studies were described as randomised; however, seven studies did not report the method of random sequence generation (Banasik 2011; Danhauer 2009; Lötzke 2016; Moadel 2007; Pruthi 2012; Vardar Yağlı 2015; Wang 2014). Remaining studies used adequate methods for generating the random sequence. All studies adequately concealed allocation, except for nine studies that did not report methods used to do so (Banasik 2011; Bernardi 2013; Chandwani 2010; Chandwani 2014; Danhauer 2009; Littman 2012; Lötzke 2016; Moadel 2007; Pruthi 2012) and one study that did not conceal allocation (Wang 2014).
Blinding
Most studies provided no information on blinding. Five studies explicitly stated that participants and personnel were not blinded to group allocation (Cramer 2015; Kiecolt‐Glaser 2014; Kovacic 2013; Mustian 2013; Vadiraja 2009). One further study reported that participants and personnel were not blinded, although investigators presented both active interventions as effective at the start of the study and noted no group differences in perceived effectiveness; thus lack of blinding is not likely to introduce bias (Bower 2012). Only six studies provided information on blinding of outcome assessors; five studies reported adequate methods of blinding (Carson 2009; Kiecolt‐Glaser 2014; Kovacic 2013; Loudon 2014; Mustian 2013); and one study explicitly reported that researchers did not blind outcome assessors (Littman 2012).
Incomplete outcome data
Although 15 studies had low attrition rates and/or used an intention‐to‐treat analysis, four studies provided no or insufficient information on attrition (Bernardi 2013; Chandwani 2010; Kovacic 2013; Lötzke 2016); and five studies had inadequately high attrition rates (Raghavendra 2007; Siedentopf 2013; Vardar Yağlı 2015) and/or unbalanced attrition rates between groups (Banerjee 2007; Raghavendra 2007; Vadiraja 2009) without performing an adequate intention‐to‐treat analysis.
Selective reporting
Eighteen studies had low risk of selective reporting. For two studies, we judged the risk of reporting bias as unclear because the scale used in assessing outcomes was not validated, and its content and factor structure remained unclear (Chakrabarty 2015); or it was not clear from the study protocol which outcomes were to be assessed (Kiecolt‐Glaser 2014). For one study each, outcome measures clearly differed from those reported in the study protocol (Loudon 2014); or published subgroup analyses used outcomes that were not reported in the study protocol (Mustian 2013). Two additional studies produced duplicate publications that separately reported different outcomes of the same study without denoting assessment of those outcomes or the existence of other publications (Kovacic 2013; Vadiraja 2009). We judged the latter four studies as having high risk of reporting bias.
Other potential sources of bias
Although most studies were free of other suggested bias, risk of other bias was unclear in one study, for which the outcome measure was developed by study authors and validation data were not available (Chakrabarty 2015), and in another study, for which intervention length, period and compliance were unclear (Lötzke 2016). We judged four studies as having high risk of other bias because large baseline differences between groups were evident (Banasik 2011); the a priori calculated sample size was not reached (Loudon 2014); the number of participants randomised and the time frame of outcome assessment were not reported (Raghavendra 2007); or researchers used non‐validated outcome measures (Wang 2014).
Effects of interventions
See: Table 1; Table 2; Table 3
Comparison 1. Yoga versus no therapy
Health‐related quality of life
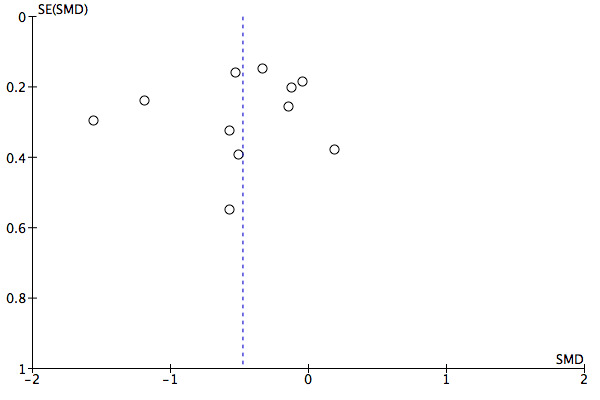
A total of 10 studies, involving 675 women, compared short‐term effects of yoga versus no therapy on health‐related quality of life. The pooled SMD was 0.22 (95% CI 0.04 to 0.40; Analysis 1.1; Figure 3), indicating statistically significant benefit from yoga with low heterogeneity (I2 = 19%). We downgraded the quality of evidence from high to moderate quality owing to serious imprecision (95% CI included negligible effects). Although the funnel plot was asymmetrical, hinting at potential risk of publication bias, this bias would have favoured no therapy rather than yoga (Figure 4). Two studies assessed medium‐term effects in 146 participants and found no overall effect from yoga (SMD 0.10, 95% CI ‐0.23 to 0.42; Analysis 1.2). Study results were homogeneous (I2 = 0%); we downgraded the quality of evidence from high to low quality because of very serious imprecision (95% CI included positive and negative effects, and sample size was very small).
1.1. Analysis.
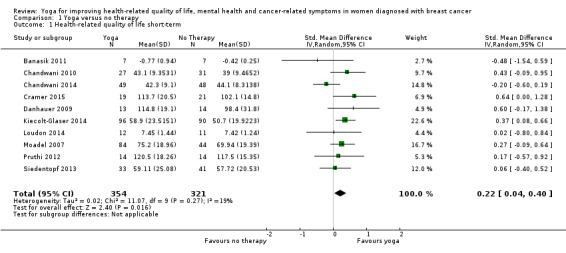
Comparison 1 Yoga versus no therapy, Outcome 1 Health‐related quality of life short‐term.
3.
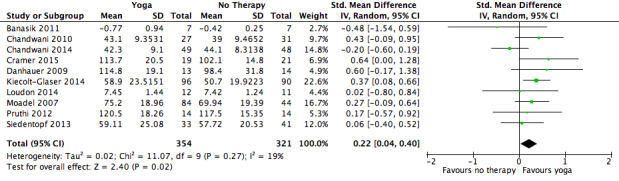
Forest plot of comparison: 1 Yoga versus no therapy, outcome: 1.1 Health‐related quality of life short‐term.
4.
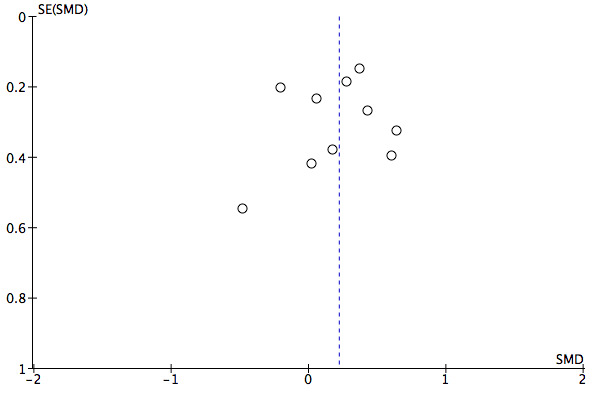
Funnel plot of comparison: 1 Yoga versus no therapy, outcome: 1.1 Health‐related quality of life short‐term.
1.2. Analysis.
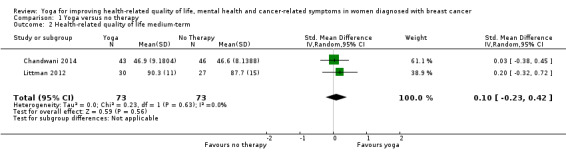
Comparison 1 Yoga versus no therapy, Outcome 2 Health‐related quality of life medium‐term.
Depression
Seven studies including 496 women assessed short‐term effects of yoga versus no therapy on depression. The pooled SMD was ‐0.13 (95% CI ‐0.31 to 0.05), indicating no statistically significant group differences (Analysis 1.3). Heterogeneity was low (I2 = 0%). We judged the quality of evidence to be low as the result of very serious imprecision (95% CI included positive and negative effects).
1.3. Analysis.
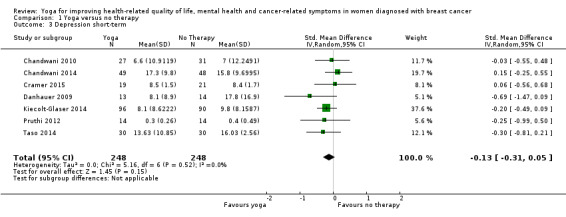
Comparison 1 Yoga versus no therapy, Outcome 3 Depression short‐term.
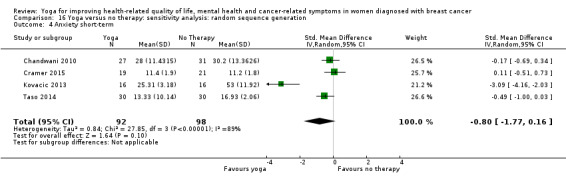
Anxiety
Regarding anxiety, six studies involving 346 women assessed short‐term effects of yoga versus no therapy. The pooled SMD was ‐0.53 (95% CI ‐1.10 to 0.04), indicating no statistically significant group differences (Analysis 1.4) with considerable heterogeneity (I2 = 83%), which was driven mainly by Kovacic 2013, which had by far the largest treatment effect. We downgraded the quality of evidence from high to very low owing to serious inconsistency (widely differing estimates of treatment effects) and very serious imprecision (95% CI included positive and negative effects).
1.4. Analysis.
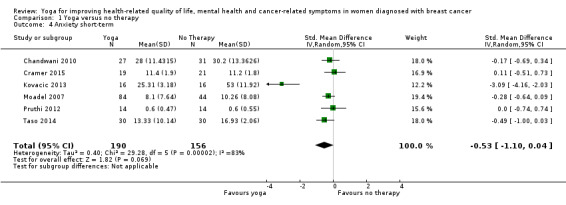
Comparison 1 Yoga versus no therapy, Outcome 4 Anxiety short‐term.
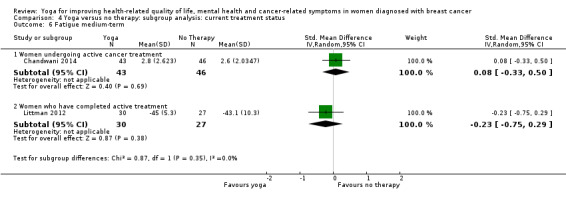
Fatigue
Eleven studies that enrolled 883 women assessed short‐term effects of yoga versus no therapy on fatigue. The pooled SMD was ‐0.48 (95% CI ‐0.75 to ‐0.20), indicating a statistically significant beneficial effect from yoga (Analysis 1.5; Figure 5) with substantial heterogeneity (I2 = 72%). We downgraded the quality of evidence from high to moderate owing to serious inconsistency (widely differing estimates of treatment effects). The funnel plot was roughly symmetrical, hinting at low risk of publication bias (Figure 6). Two studies with 146 participants assessed medium‐term effects and found no overall effect derived from yoga (SMD ‐0.04, 95% CI ‐0.36 to 0.29; Analysis 1.6). Study results were homogeneous (I2 = 0%). We downgraded the quality of evidence from high to low because of very serious imprecision (95% CI included positive and negative effects, and sample size was very small).
1.5. Analysis.
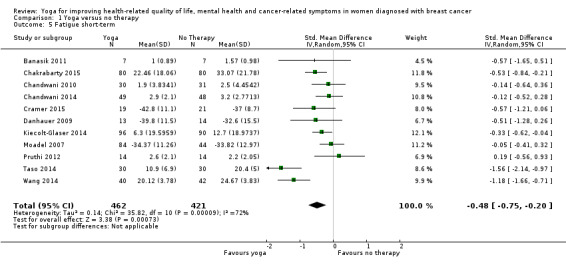
Comparison 1 Yoga versus no therapy, Outcome 5 Fatigue short‐term.
5.
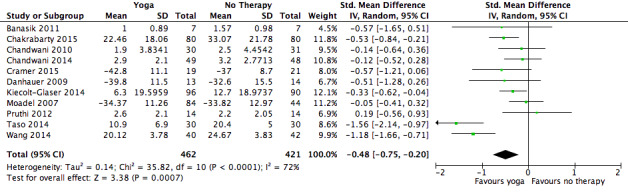
Forest plot of comparison: 1 Yoga versus no therapy, outcome: 1.5 Fatigue short‐term.
6.
Funnel plot of comparison: 1 Yoga versus no therapy, outcome: 1.5 Fatigue short‐term.
1.6. Analysis.
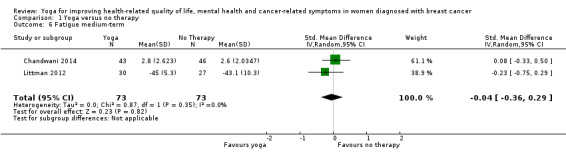
Comparison 1 Yoga versus no therapy, Outcome 6 Fatigue medium‐term.
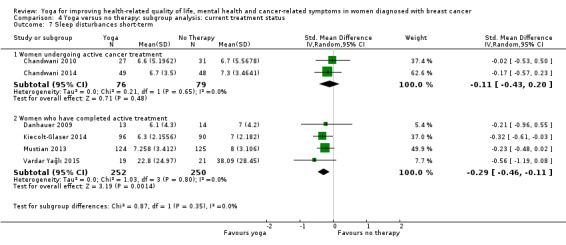
Sleep disturbances
A total of six studies (657 women) compared short‐term effects of yoga versus no therapy on sleep disturbances. The pooled SMD was ‐0.25 (95% CI ‐0.40 to ‐0.09), indicating a statistically significant effect (Analysis 1.7) with low heterogeneity (I2 = 0%). We downgraded the quality of evidence from high to moderate owing to serious imprecision (95% CI included negligible effects).
1.7. Analysis.
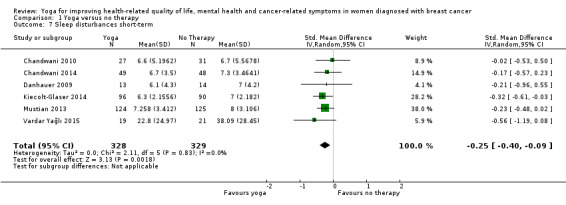
Comparison 1 Yoga versus no therapy, Outcome 7 Sleep disturbances short‐term.
Safety
Although four studies provided safety‐related data (Cramer 2015; Danhauer 2009; Kiecolt‐Glaser 2014; Mustian 2013), only two studies reported the numbers of women with adverse events and with severe adverse events (Cramer 2015; Danhauer 2009). The first study reported that no serious adverse events occurred in the short term; six of 19 women randomised to yoga and six of 21 randomised to no treatment experienced minor adverse events (Cramer 2015). The second study reported that no serious or minor adverse events occurred in either group (Danhauer 2009).
Comparison 2. Yoga versus psychosocial/educational interventions
Health‐related quality of life
A total of two studies (153 women) compared short‐term effects of yoga versus psychosocial/educational interventions on health‐related quality of life. The pooled SMD was 0.81 (95% CI ‐0.50 to 2.12), indicating no statistically significant group differences (Analysis 2.1) with considerable heterogeneity (I2 = 93%). We downgraded the quality of evidence from high to very low because of serious inconsistency (widely differing estimates of treatment effects) and very serious imprecision (95% CI included positive and negative effects, and sample size was very small).
2.1. Analysis.
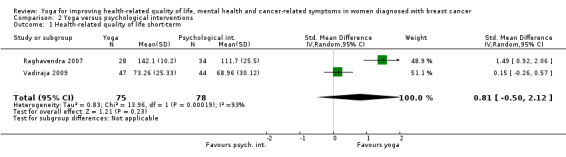
Comparison 2 Yoga versus psychological interventions, Outcome 1 Health‐related quality of life short‐term.
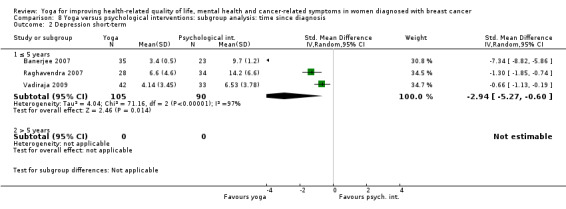
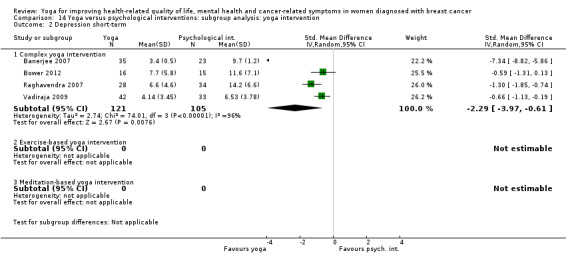
Depression
Four studies (226 women) assessed short‐term effects of yoga versus psychosocial/educational interventions on depression. The pooled SMD was ‐2.29 (95% CI ‐3.97 to ‐0.61), indicating a statistically significant effect (Analysis 2.2), and heterogeneity was considerably high (I2 = 96%). We judged the quality of evidence as moderate owing to the small sample size, indicating serious imprecision.
2.2. Analysis.
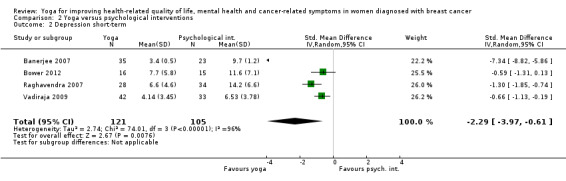
Comparison 2 Yoga versus psychological interventions, Outcome 2 Depression short‐term.
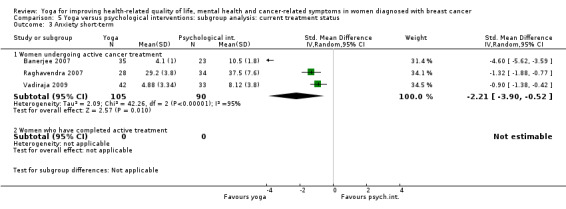
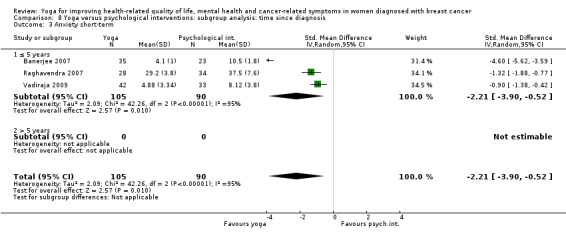
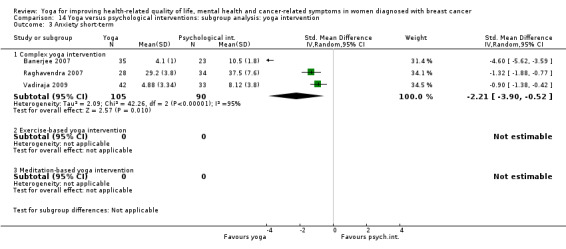
Anxiety
Regarding anxiety, three studies (195 women) assessed short‐term effects of yoga versus psychosocial/educational interventions. The pooled SMD was ‐2.21 (95% CI ‐3.90 to ‐0.52), indicating a favourable effect among women practising yoga (Analysis 2.3) with considerable heterogeneity (I2 = 95%). We downgraded the quality of evidence from high to moderate owing to serious imprecision (small sample size).
2.3. Analysis.
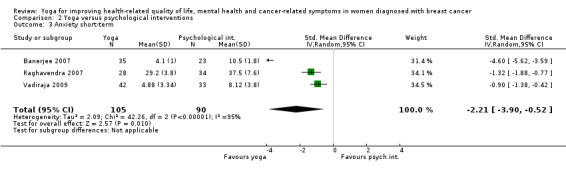
Comparison 2 Yoga versus psychological interventions, Outcome 3 Anxiety short‐term.
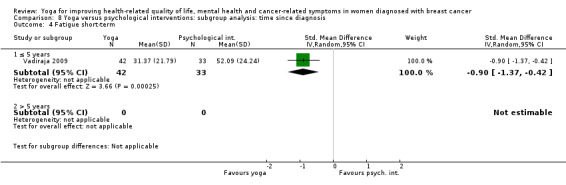
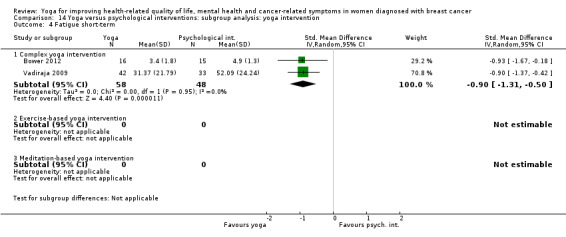
Fatigue
Two studies (106 women) compared short‐term effects of yoga versus psychosocial/educational interventions on fatigue. The pooled SMD was ‐0.90 (95% CI ‐1.31 to ‐0.50), indicating a statistically significant effect favouring yoga practice (Analysis 2.4) without heterogeneity (I2 = 0%). We downgraded the quality of evidence from high to moderate owing to serious imprecision associated with the small sample size.
2.4. Analysis.
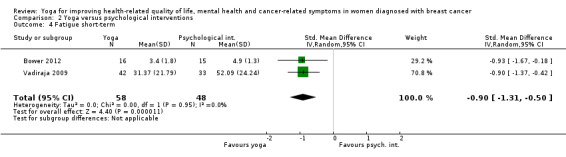
Comparison 2 Yoga versus psychological interventions, Outcome 4 Fatigue short‐term.
Sleep disturbances
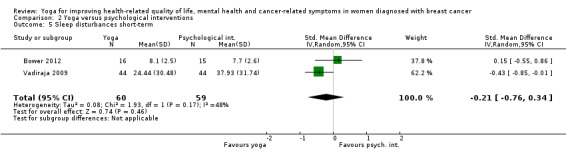
Two studies (119 women) compared short‐term effects of yoga versus psychosocial/educational interventions on sleep disturbances. The pooled SMD was ‐0.21 (95% CI ‐0.76 to 0.34), indicating no statistically significant group differences (Analysis 2.5) with moderate heterogeneity (I2 = 48%). We downgraded the quality of evidence from high to very low owing to serious inconsistency (widely differing estimates of treatment effects) and very serious imprecision (95% CI included positive and negative effects, and sample size was very small).
2.5. Analysis.
Comparison 2 Yoga versus psychological interventions, Outcome 5 Sleep disturbances short‐term.
Safety
One study provided safety‐related data but did not report the number of women with adverse events or severe adverse events (Bower 2012).
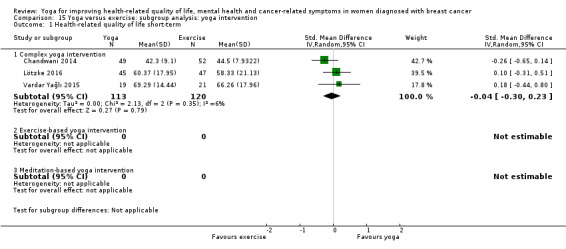
Comparison 3. Yoga versus exercise
Health‐related quality of life
Three studies (233 women) compared short‐term effects of yoga versus exercise on health‐related quality of life. The pooled SMD was ‐0.04 (95% CI ‐0.30 to 0.23), indicating no statistically significant group differences (Analysis 3.1) and low heterogeneity (I2 = 6%). We downgraded the quality of evidence from high to very low owing to serious risk of bias, serious inconsistency (widely differing estimates of treatment effects) and very serious imprecision (95% CI included positive and negative effects, and sample size was very small).
3.1. Analysis.
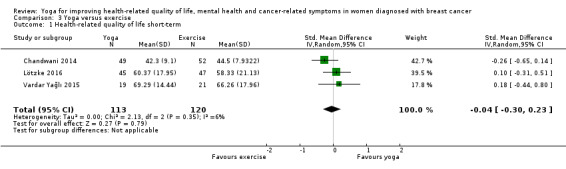
Comparison 3 Yoga versus exercise, Outcome 1 Health‐related quality of life short‐term.
Depression
None of the studies collected data related to depression.
Anxiety
None of the studies collected data related to anxiety.
Fatigue
Three studies (233 women) assessed short‐term effects of yoga versus exercise on fatigue. The pooled SMD was ‐0.21 (95% CI ‐0.66 to 0.25), indicating no statistically significant group differences (Analysis 3.2) with substantial heterogeneity (I2 = 64%). We downgraded the quality of evidence from high to very low owing to serious risk of bias, serious inconsistency (widely differing estimates of treatment effects) and very serious imprecision (95% CI included positive and negative effects, and sample size was very small).
3.2. Analysis.
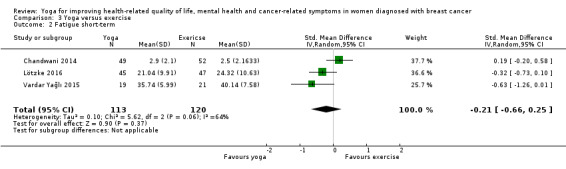
Comparison 3 Yoga versus exercise, Outcome 2 Fatigue short‐term.
Sleep disturbances
None of the studies collected data related to sleep disturbances.
Safety
The two studies comparing yoga versus exercise provided no safety‐related data.
Subgroup analyses
Current treatment status
Comparison 1. Yoga versus no therapy
For women undergoing active cancer treatment, we found statistically significant short‐term effects favouring yoga over no therapy for fatigue only (SMD ‐0.68, 95% CI ‐1.18 to ‐0.19; Analysis 4.5) with considerably high heterogeneity (I2 = 84%). We observed no differences between groups in health‐related quality of life (short‐term: Analysis 4.1; medium‐term: Analysis 4.2), depression (Analysis 4.3) or anxiety (Analysis 4.4); or in the medium term in fatigue (Analysis 4.6) or sleep patterns (Analysis 4.7).
4.5. Analysis.
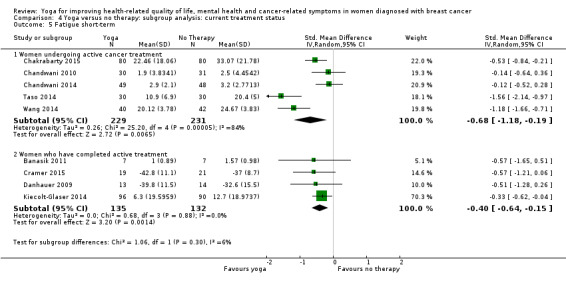
Comparison 4 Yoga versus no therapy: subgroup analysis: current treatment status, Outcome 5 Fatigue short‐term.
4.1. Analysis.
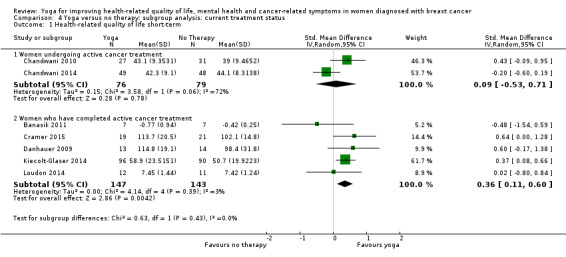
Comparison 4 Yoga versus no therapy: subgroup analysis: current treatment status, Outcome 1 Health‐related quality of life short‐term.
4.2. Analysis.
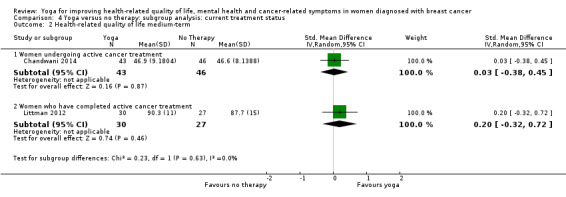
Comparison 4 Yoga versus no therapy: subgroup analysis: current treatment status, Outcome 2 Health‐related quality of life medium‐term.
4.3. Analysis.
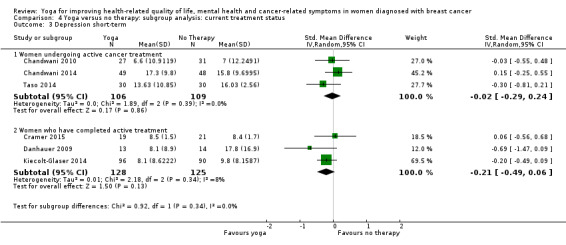
Comparison 4 Yoga versus no therapy: subgroup analysis: current treatment status, Outcome 3 Depression short‐term.
4.4. Analysis.
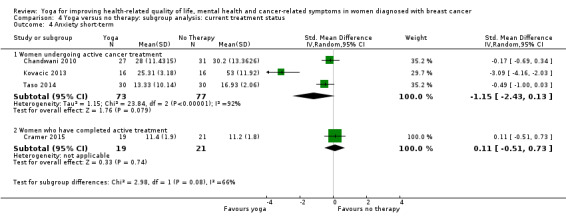
Comparison 4 Yoga versus no therapy: subgroup analysis: current treatment status, Outcome 4 Anxiety short‐term.
4.6. Analysis.
Comparison 4 Yoga versus no therapy: subgroup analysis: current treatment status, Outcome 6 Fatigue medium‐term.
4.7. Analysis.
Comparison 4 Yoga versus no therapy: subgroup analysis: current treatment status, Outcome 7 Sleep disturbances short‐term.
For women who had completed active cancer treatment, we found statistically significant short‐term effects favouring yoga over no therapy for health‐related quality of life (SMD 0.36; 95% CI 0.11 to 0.60; Analysis 4.1), fatigue (SMD ‐0.40; 95% CI ‐0.64 to ‐0.15; Analysis 4.5) and sleep disturbances (SMD ‐0.29; 95% CI ‐0.46 to ‐0.11; Analysis 4.6). Heterogeneity was low for all three outcomes (I2 = 3%, 0%, and 0%, respectively).
Comparison 2. Yoga versus psychosocial/educational interventions
For women undergoing active cancer treatment, we found statistically significant short‐term effects favouring yoga over psychosocial/educational interventions for depression (SMD ‐2.94, 95% CI ‐5.27 to ‐0.60; Analysis 5.2) and for anxiety (SMD ‐2.21, 95% CI ‐3.90 to ‐0.52; Analysis 5.3) with considerably high heterogeneity for both outcomes (I2 = 97% and 95%). Although we found additional statistically significant group differences for fatigue and sleep disturbances, these effects were based on single studies only. For women who had completed active cancer treatment, we found statistically significant short‐term effects favouring yoga over psychosocial/educational interventions for fatigue only; this effect was based on a single study.
5.2. Analysis.
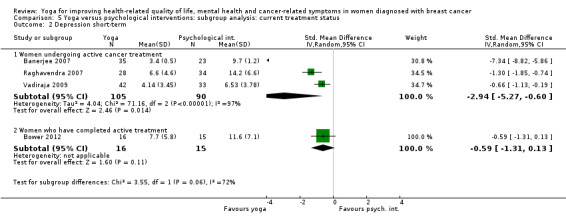
Comparison 5 Yoga versus psychological interventions: subgroup analysis: current treatment status, Outcome 2 Depression short‐term.
5.3. Analysis.
Comparison 5 Yoga versus psychological interventions: subgroup analysis: current treatment status, Outcome 3 Anxiety short‐term.
Comparison 3. Yoga versus exercise
We found no group differences for yoga compared with exercise, regardless of current treatment status.
Time since diagnosis
Comparison 1. Yoga versus no therapy
For women with breast cancer diagnosed within five years before the time of study entry, we found statistically significant short‐term effects favouring yoga over no therapy for anxiety (SMD ‐0.67, 95% CI ‐1.34 to ‐0.01; I2 = 85%; Analysis 7.4), fatigue (SMD ‐0.49, 95% CI ‐0.86 to ‐0.11; I2 = 80%; Analysis 7.5) and sleep disturbances (SMD ‐0.22, 95% CI ‐0.40 to ‐0.03; I2 = 0%; Analysis 7.7). No studies included only women with breast cancer diagnosed more than five years before the time of study entry.
7.4. Analysis.
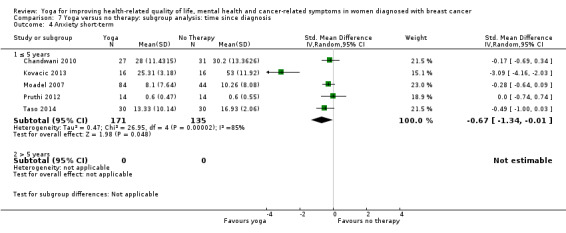
Comparison 7 Yoga versus no therapy: subgroup analysis: time since diagnosis, Outcome 4 Anxiety short‐term.
7.5. Analysis.
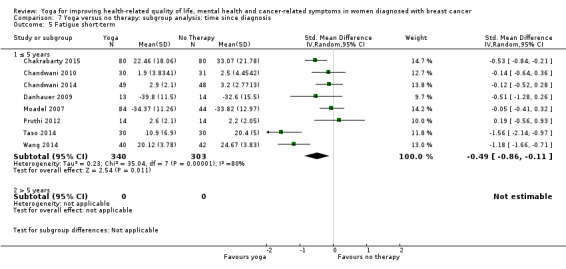
Comparison 7 Yoga versus no therapy: subgroup analysis: time since diagnosis, Outcome 5 Fatigue short‐term.
7.7. Analysis.
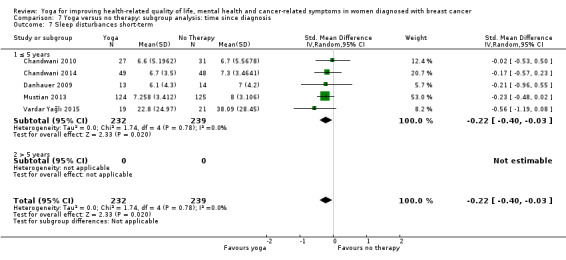
Comparison 7 Yoga versus no therapy: subgroup analysis: time since diagnosis, Outcome 7 Sleep disturbances short‐term.
Comparison 2. Yoga versus psychosocial/educational interventions
For women with breast cancer diagnosed within five years before the time of study entry, we found statistically significant short‐term effects favouring yoga over psychosocial/educational interventions for depression (SMD ‐2.94; 95% CI ‐5.27 to ‐0.60; I2 = 97%; Analysis 8.2), anxiety (SMD ‐2.21, 95% CI ‐3.90 to ‐0.52; I2 = 95%; Analysis 8.3) and fatigue (SMD ‐0.90, 95% CI ‐1.37 to ‐0.42; Analysis 8.4). However, the latter findings were based on a single study. No studies included only women with breast cancer diagnosed more than five years before the time of study entry.
8.2. Analysis.
Comparison 8 Yoga versus psychological interventions: subgroup analysis: time since diagnosis, Outcome 2 Depression short‐term.
8.3. Analysis.
Comparison 8 Yoga versus psychological interventions: subgroup analysis: time since diagnosis, Outcome 3 Anxiety short‐term.
8.4. Analysis.
Comparison 8 Yoga versus psychological interventions: subgroup analysis: time since diagnosis, Outcome 4 Fatigue short‐term.
Comparison 3. Yoga versus exercise
We found no group differences for yoga compared with exercise in women with breast cancer diagnosed within five years before the time of study entry. No studies included only women with breast cancer diagnosed more than five years before the time of study entry.
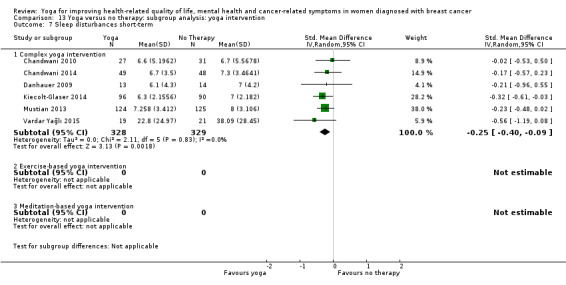
Stage of cancer
Comparison 1. Yoga versus no therapy
When we included only studies with women with a diagnosis of non‐metastatic breast cancer, we found statistically significant short‐term effects favouring yoga over no therapy for health‐related quality of life (SMD 0.24, 95% CI 0.04 to 0.45; I2 = 24%; Analysis 10.1), fatigue (SMD ‐0.38, 95% CI ‐0.67 to ‐0.09; I2 = 72%; Analysis 10.5) and sleep disturbances (SMD ‐0.25, 95% CI ‐0.40 to ‐0.09; I2 = 0%; Analysis 10.7). No studies included only women with a diagnosis of metastatic breast cancer.
10.1. Analysis.
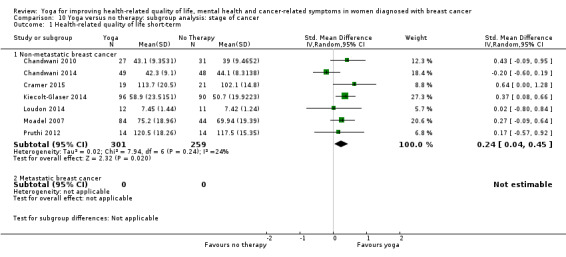
Comparison 10 Yoga versus no therapy: subgroup analysis: stage of cancer, Outcome 1 Health‐related quality of life short‐term.
10.5. Analysis.
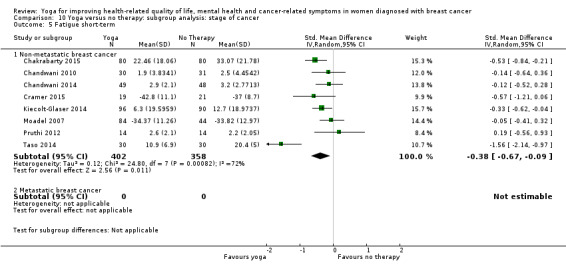
Comparison 10 Yoga versus no therapy: subgroup analysis: stage of cancer, Outcome 5 Fatigue short‐term.
10.7. Analysis.
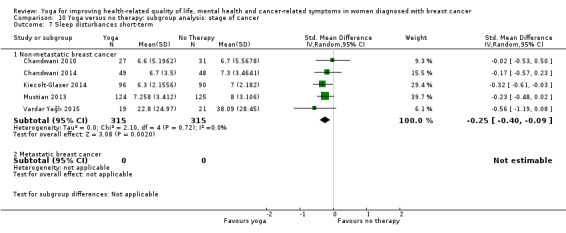
Comparison 10 Yoga versus no therapy: subgroup analysis: stage of cancer, Outcome 7 Sleep disturbances short‐term.
Comparison 2. Yoga versus psychosocial/educational interventions
When we included only studies with women with a diagnosis of non‐metastatic breast cancer, we found statistically significant short‐term effects favouring yoga over psychosocial/educational interventions for depression (SMD ‐2.29, 95% CI ‐3.97 to ‐0.61; I2 = 96%; Analysis 11.2), anxiety (SMD ‐2.21, 95% CI ‐3.90 to ‐0.52; I2 = 95%; Analysis 11.3) and fatigue (SMD ‐0.90, 95% CI ‐1.31 to ‐0.53; I2 = 0%; Analysis 11.4). No studies included only women with a diagnosis of metastatic breast cancer.
11.2. Analysis.
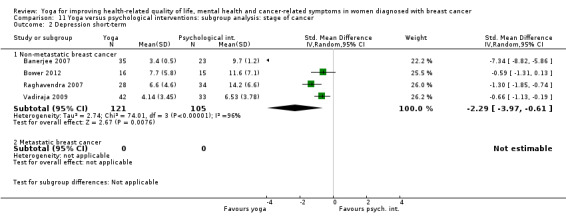
Comparison 11 Yoga versus psychological interventions: subgroup analysis: stage of cancer, Outcome 2 Depression short‐term.
11.3. Analysis.
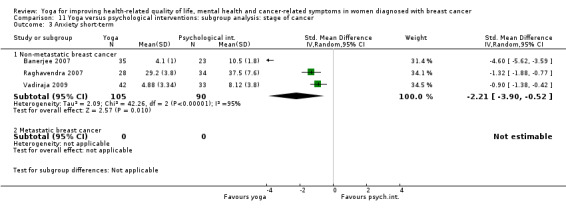
Comparison 11 Yoga versus psychological interventions: subgroup analysis: stage of cancer, Outcome 3 Anxiety short‐term.
11.4. Analysis.
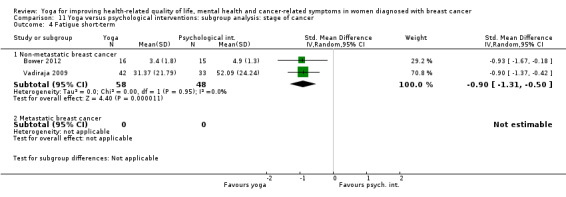
Comparison 11 Yoga versus psychological interventions: subgroup analysis: stage of cancer, Outcome 4 Fatigue short‐term.
Comparison 3. Yoga versus exercise
We found no group differences for studies with women with a diagnosis of non‐metastatic breast cancer; no studies included only women with a diagnosis of metastatic breast cancer.
Type of yoga intervention
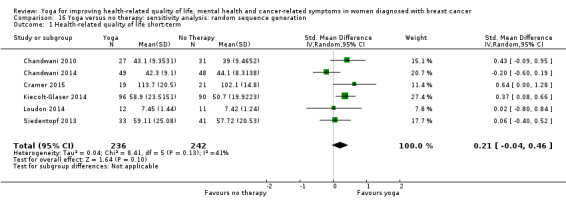
Comparison 1. Yoga versus no therapy
When we included only studies comparing complex yoga interventions versus no therapy, we found statistically significant short‐term effects for health‐related quality of life (SMD 0.24, 95% CI 0.06 to 0.41; I2 = 15%; Analysis 13.1), fatigue (SMD ‐0.37, 95% CI ‐0.69 to ‐0.05; I2 = 70%; Analysis 13.5) and sleep disturbances (SMD ‐0.25, 95% CI ‐0.40 to ‐0.09; I2 = 0%; Analysis 13.7). For studies comparing exercise‐based yoga interventions versus no therapy, we found statistically significant short‐term effects for fatigue (SMD ‐1.08, 95% CI ‐1.53 to ‐0.62; Analysis 13.5) with low heterogeneity (I2 = 5%). For studies comparing meditation‐based yoga interventions versus no therapy, we found statistically significant group differences for fatigue, but these effects were based on a single study.
13.1. Analysis.
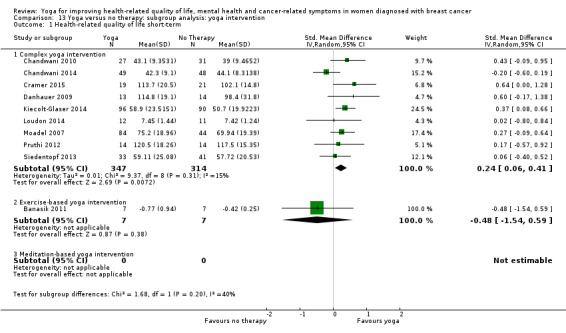
Comparison 13 Yoga versus no therapy: subgroup analysis: yoga intervention, Outcome 1 Health‐related quality of life short‐term.
13.5. Analysis.
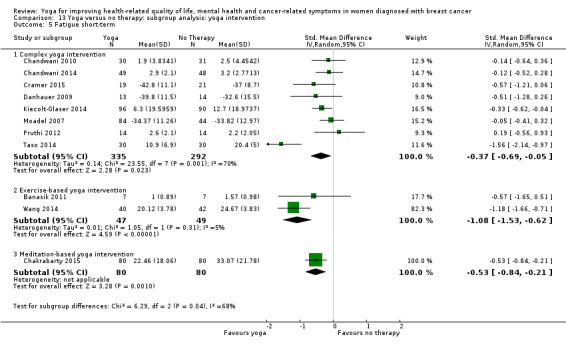
Comparison 13 Yoga versus no therapy: subgroup analysis: yoga intervention, Outcome 5 Fatigue short‐term.
13.7. Analysis.
Comparison 13 Yoga versus no therapy: subgroup analysis: yoga intervention, Outcome 7 Sleep disturbances short‐term.
Comparison 2. Yoga versus psychosocial/educational interventions
When we considered only studies using complex yoga interventions, we found statistically significant short‐term effects favouring yoga over psychosocial/educational interventions for depression (SMD ‐2.29, 95% CI ‐3.97 to ‐0.61; I2 = 96%; Analysis 14.2), anxiety (SMD ‐2.21, 95% CI ‐3.90 to ‐0.52; I2 = 95%; Analysis 14.3) and fatigue (SMD ‐0.90, 95% CI ‐1.31 to ‐0.50; I2 = 0%; Analysis 14.4). No studies compared exercise‐based or meditation‐based yoga interventions versus psychosocial/educational interventions.
14.2. Analysis.
Comparison 14 Yoga versus psychological interventions: subgroup analysis: yoga intervention, Outcome 2 Depression short‐term.
14.3. Analysis.
Comparison 14 Yoga versus psychological interventions: subgroup analysis: yoga intervention, Outcome 3 Anxiety short‐term.
14.4. Analysis.
Comparison 14 Yoga versus psychological interventions: subgroup analysis: yoga intervention, Outcome 4 Fatigue short‐term.
Comparison 3. Yoga versus exercise
We found no group differences for studies comparing complex yoga interventions versus exercise (Analysis 15.1; Analysis 15.2); no studies compared exercise‐based or meditation‐based yoga interventions versus exercise.
15.1. Analysis.
Comparison 15 Yoga versus exercise: subgroup analysis: yoga intervention, Outcome 1 Health‐related quality of life short‐term.
15.2. Analysis.
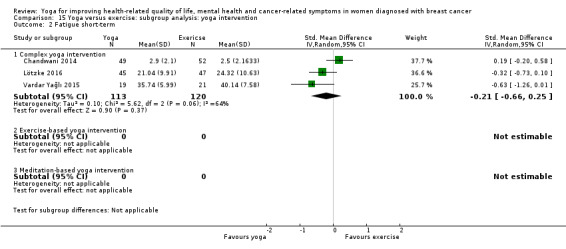
Comparison 15 Yoga versus exercise: subgroup analysis: yoga intervention, Outcome 2 Fatigue short‐term.
Sensitivity analyses
Random sequence generation
Comparison 1. Yoga versus no therapy
When we considered only studies with low risk of bias regarding random sequence generation comparing yoga versus no therapy, only short‐term effects on fatigue and sleep disturbances remained statistically significant (Analysis 16.1; Analysis 16.2; Analysis 16.3; Analysis 16.4; Analysis 16.5; Analysis 16.6; Analysis 16.7).
16.1. Analysis.
Comparison 16 Yoga versus no therapy: sensitivity analysis: random sequence generation, Outcome 1 Health‐related quality of life short‐term.
16.2. Analysis.
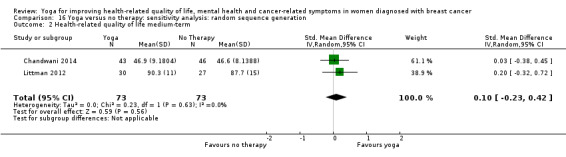
Comparison 16 Yoga versus no therapy: sensitivity analysis: random sequence generation, Outcome 2 Health‐related quality of life medium‐term.
16.3. Analysis.
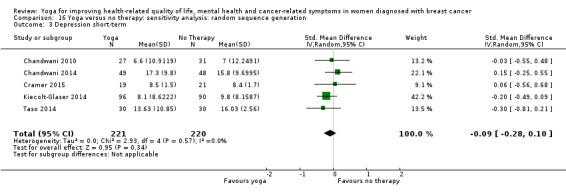
Comparison 16 Yoga versus no therapy: sensitivity analysis: random sequence generation, Outcome 3 Depression short‐term.
16.4. Analysis.
Comparison 16 Yoga versus no therapy: sensitivity analysis: random sequence generation, Outcome 4 Anxiety short‐term.
16.5. Analysis.
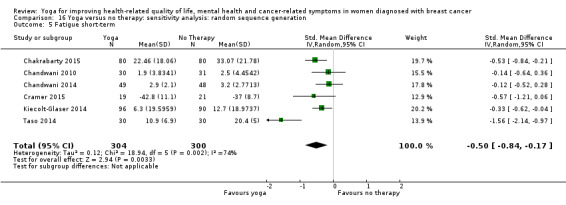
Comparison 16 Yoga versus no therapy: sensitivity analysis: random sequence generation, Outcome 5 Fatigue short‐term.
16.6. Analysis.
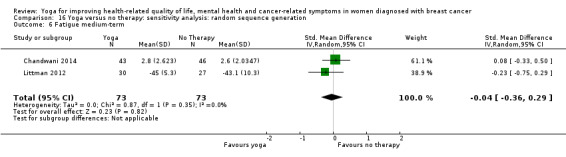
Comparison 16 Yoga versus no therapy: sensitivity analysis: random sequence generation, Outcome 6 Fatigue medium‐term.
16.7. Analysis.
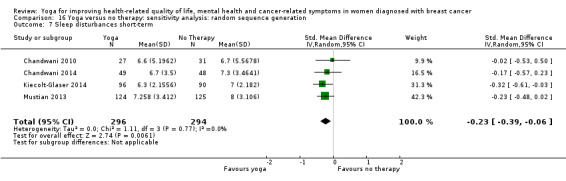
Comparison 16 Yoga versus no therapy: sensitivity analysis: random sequence generation, Outcome 7 Sleep disturbances short‐term.
Comparison 2. Yoga versus psychosocial/educational interventions
Results did not change when we considered only studies with low risk of bias regarding random sequence generation when comparing yoga versus psychosocial/educational interventions (Analysis 17.1; Analysis 17.2; Analysis 17.3; Analysis 17.4; Analysis 17.5).
17.1. Analysis.
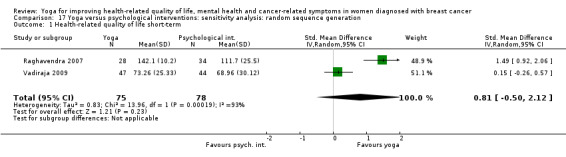
Comparison 17 Yoga versus psychological interventions: sensitivity analysis: random sequence generation, Outcome 1 Health‐related quality of life short‐term.
17.2. Analysis.
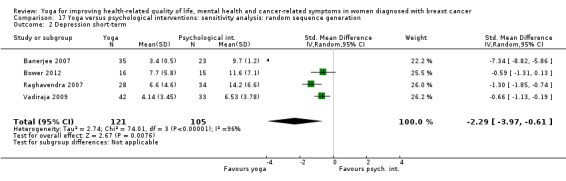
Comparison 17 Yoga versus psychological interventions: sensitivity analysis: random sequence generation, Outcome 2 Depression short‐term.
17.3. Analysis.
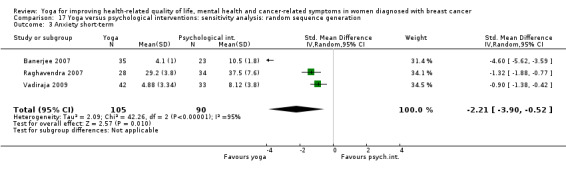
Comparison 17 Yoga versus psychological interventions: sensitivity analysis: random sequence generation, Outcome 3 Anxiety short‐term.
17.4. Analysis.
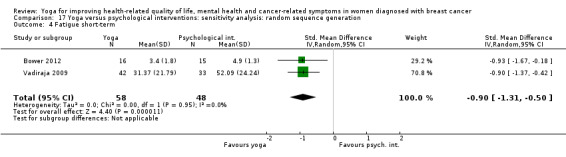
Comparison 17 Yoga versus psychological interventions: sensitivity analysis: random sequence generation, Outcome 4 Fatigue short‐term.
17.5. Analysis.
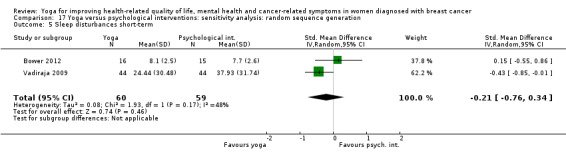
Comparison 17 Yoga versus psychological interventions: sensitivity analysis: random sequence generation, Outcome 5 Sleep disturbances short‐term.
Comparison 3. Yoga versus exercise
Results did not change substantially when we considered only the single study with low risk of bias regarding random sequence generation when comparing yoga versus exercise (Analysis 18.1; Analysis 18.2).
18.1. Analysis.
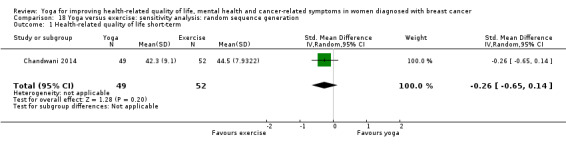
Comparison 18 Yoga versus exercise: sensitivity analysis: random sequence generation, Outcome 1 Health‐related quality of life short‐term.
18.2. Analysis.
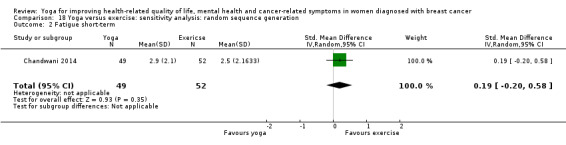
Comparison 18 Yoga versus exercise: sensitivity analysis: random sequence generation, Outcome 2 Fatigue short‐term.
Allocation concealment
Comparison 1. Yoga versus no therapy
Results did not change substantially when we considered only studies with low risk of bias regarding allocation concealment when comparing yoga versus no therapy (Analysis 19.1; Analysis 19.2; Analysis 19.3; Analysis 19.4; Analysis 19.5).
19.1. Analysis.
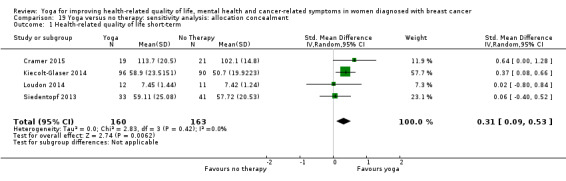
Comparison 19 Yoga versus no therapy: sensitivity analysis: allocation concealment, Outcome 1 Health‐related quality of life short‐term.
19.2. Analysis.
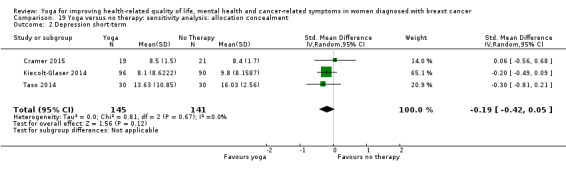
Comparison 19 Yoga versus no therapy: sensitivity analysis: allocation concealment, Outcome 2 Depression short‐term.
19.3. Analysis.
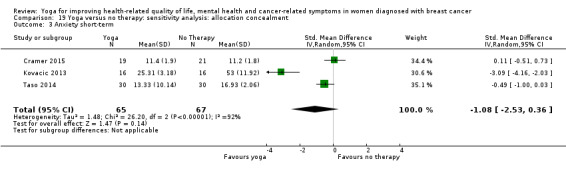
Comparison 19 Yoga versus no therapy: sensitivity analysis: allocation concealment, Outcome 3 Anxiety short‐term.
19.4. Analysis.
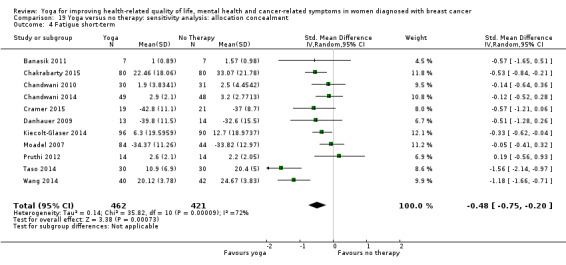
Comparison 19 Yoga versus no therapy: sensitivity analysis: allocation concealment, Outcome 4 Fatigue short‐term.
19.5. Analysis.
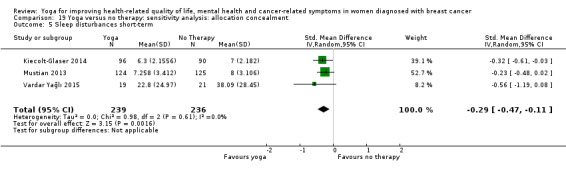
Comparison 19 Yoga versus no therapy: sensitivity analysis: allocation concealment, Outcome 5 Sleep disturbances short‐term.
Comparison 2. Yoga versus psychosocial/educational interventions
Results did not change when we considered only studies with low risk of bias regarding allocation concealment when comparing yoga versus psychosocial/educational interventions (Analysis 20.1; Analysis 20.2; Analysis 20.3; Analysis 20.4; Analysis 20.5).
20.1. Analysis.
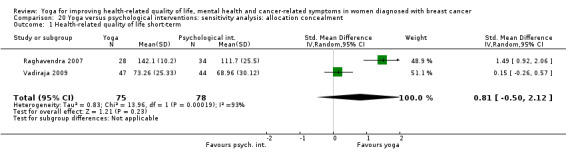
Comparison 20 Yoga versus psychological interventions: sensitivity analysis: allocation concealment, Outcome 1 Health‐related quality of life short‐term.
20.2. Analysis.
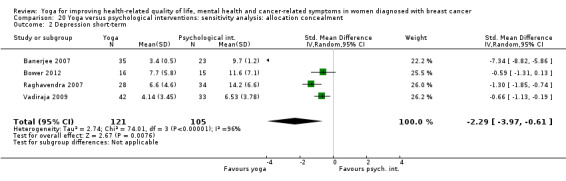
Comparison 20 Yoga versus psychological interventions: sensitivity analysis: allocation concealment, Outcome 2 Depression short‐term.
20.3. Analysis.
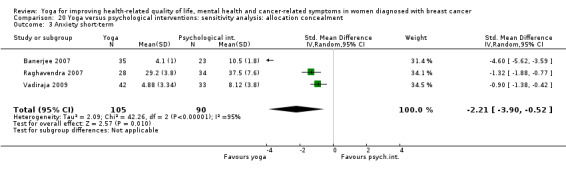
Comparison 20 Yoga versus psychological interventions: sensitivity analysis: allocation concealment, Outcome 3 Anxiety short‐term.
20.4. Analysis.
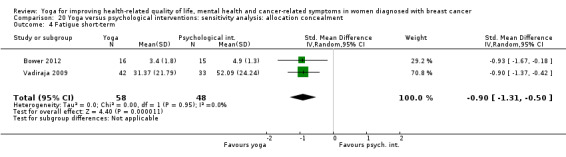
Comparison 20 Yoga versus psychological interventions: sensitivity analysis: allocation concealment, Outcome 4 Fatigue short‐term.
20.5. Analysis.
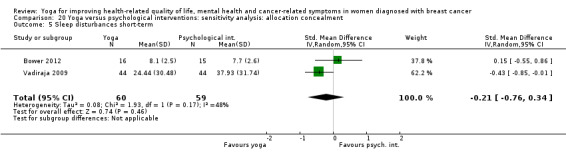
Comparison 20 Yoga versus psychological interventions: sensitivity analysis: allocation concealment, Outcome 5 Sleep disturbances short‐term.
Comparison 3. Yoga versus exercise
Results did not change substantially when we considered only the single study with low risk of bias regarding allocation concealment when comparing yoga versus exercise (Analysis 21.1; Analysis 21.2).
21.1. Analysis.
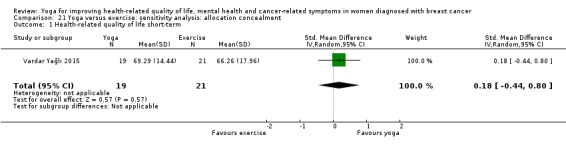
Comparison 21 Yoga versus exercise: sensitivity analysis: allocation concealment, Outcome 1 Health‐related quality of life short‐term.
21.2. Analysis.
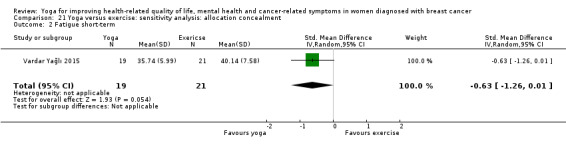
Comparison 21 Yoga versus exercise: sensitivity analysis: allocation concealment, Outcome 2 Fatigue short‐term.
Blinding of outcome assessors
Comparison 1. Yoga versus no therapy
Results did not change substantially when we considered only studies with low risk of detection bias when comparing yoga versus no therapy (Analysis 22.1; Analysis 22.2; Analysis 22.3; Analysis 22.5); however, we could include only one study in the analysis of effects on fatigue (Analysis 22.4).
22.1. Analysis.
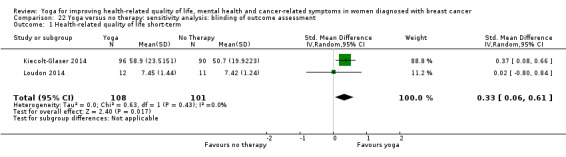
Comparison 22 Yoga versus no therapy: sensitivity analysis: blinding of outcome assessment, Outcome 1 Health‐related quality of life short‐term.
22.2. Analysis.
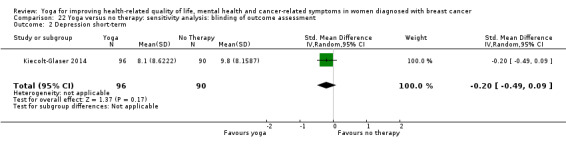
Comparison 22 Yoga versus no therapy: sensitivity analysis: blinding of outcome assessment, Outcome 2 Depression short‐term.
22.3. Analysis.
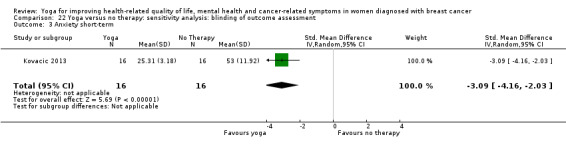
Comparison 22 Yoga versus no therapy: sensitivity analysis: blinding of outcome assessment, Outcome 3 Anxiety short‐term.
22.5. Analysis.
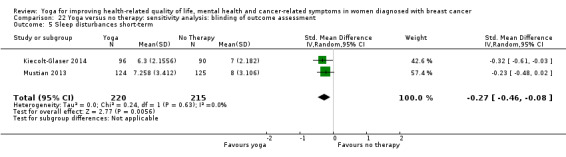
Comparison 22 Yoga versus no therapy: sensitivity analysis: blinding of outcome assessment, Outcome 5 Sleep disturbances short‐term.
22.4. Analysis.
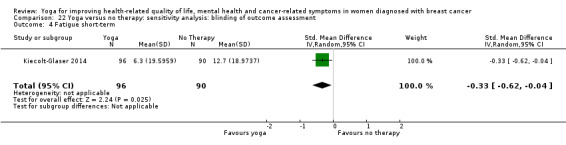
Comparison 22 Yoga versus no therapy: sensitivity analysis: blinding of outcome assessment, Outcome 4 Fatigue short‐term.
Comparison 2. Yoga versus psychosocial/educational interventions
We judged no studies comparing yoga versus psychosocial/educational interventions as having low risk of detection bias.
Comparison 3. Yoga versus exercise
We judged no studies comparing yoga versus exercise as having low risk of detection bias.
Incomplete outcome data
Comparison 1. Yoga versus no therapy
When we considered only studies with low risk of attrition bias when comparing yoga versus no therapy, only short‐term effects on fatigue and sleep remained statistically significant (Analysis 23.1; Analysis 23.2; Analysis 23.3; Analysis 23.4; Analysis 23.5; Analysis 23.6; Analysis 23.7).
23.1. Analysis.
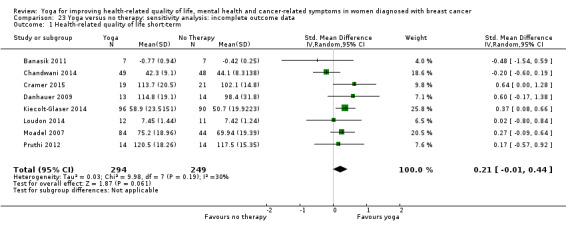
Comparison 23 Yoga versus no therapy: sensitivity analysis: incomplete outcome data, Outcome 1 Health‐related quality of life short‐term.
23.2. Analysis.
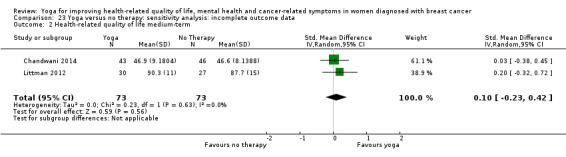
Comparison 23 Yoga versus no therapy: sensitivity analysis: incomplete outcome data, Outcome 2 Health‐related quality of life medium‐term.
23.3. Analysis.
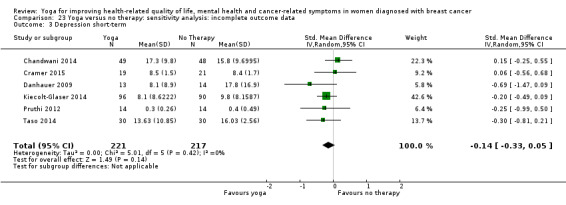
Comparison 23 Yoga versus no therapy: sensitivity analysis: incomplete outcome data, Outcome 3 Depression short‐term.
23.4. Analysis.
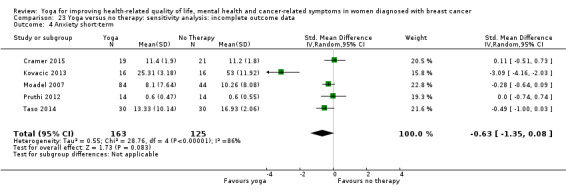
Comparison 23 Yoga versus no therapy: sensitivity analysis: incomplete outcome data, Outcome 4 Anxiety short‐term.
23.5. Analysis.
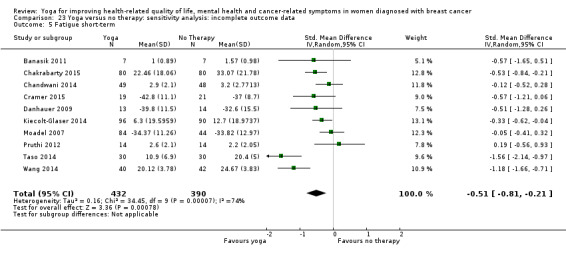
Comparison 23 Yoga versus no therapy: sensitivity analysis: incomplete outcome data, Outcome 5 Fatigue short‐term.
23.6. Analysis.
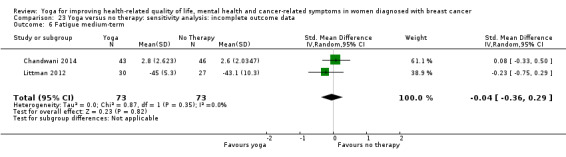
Comparison 23 Yoga versus no therapy: sensitivity analysis: incomplete outcome data, Outcome 6 Fatigue medium‐term.
23.7. Analysis.
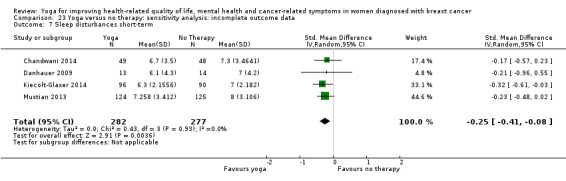
Comparison 23 Yoga versus no therapy: sensitivity analysis: incomplete outcome data, Outcome 7 Sleep disturbances short‐term.
Comparison 2. Yoga versus psychosocial/educational interventions
When we included only studies with low risk of attrition bias when comparing yoga versus psychosocial/educational interventions, only short‐term effects on fatigue remained statistically significant, and this comparison was based on a single study (Analysis 24.1; Analysis 24.2; Analysis 24.3).
24.1. Analysis.
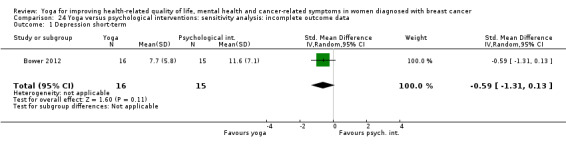
Comparison 24 Yoga versus psychological interventions: sensitivity analysis: incomplete outcome data, Outcome 1 Depression short‐term.
24.2. Analysis.

Comparison 24 Yoga versus psychological interventions: sensitivity analysis: incomplete outcome data, Outcome 2 Fatigue short‐term.
24.3. Analysis.
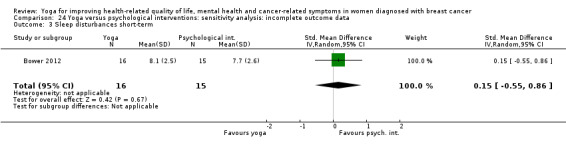
Comparison 24 Yoga versus psychological interventions: sensitivity analysis: incomplete outcome data, Outcome 3 Sleep disturbances short‐term.
Comparison 3. Yoga versus exercise
Results did not change when we considered only the single study with low risk of attrition bias when comparing yoga versus exercise (Analysis 25.1; Analysis 25.2).
25.1. Analysis.
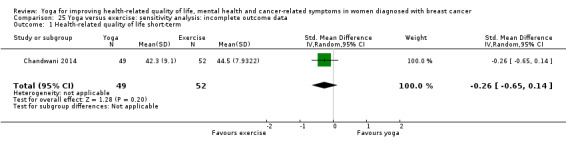
Comparison 25 Yoga versus exercise: sensitivity analysis: incomplete outcome data, Outcome 1 Health‐related quality of life short‐term.
25.2. Analysis.
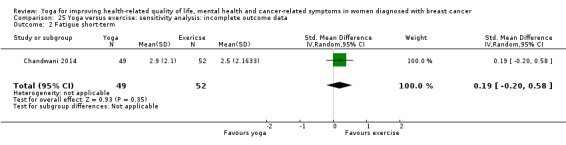
Comparison 25 Yoga versus exercise: sensitivity analysis: incomplete outcome data, Outcome 2 Fatigue short‐term.
Missing data retrieved from study authors or imputed
For four studies, we retrieved missing data from study authors by email (Chakrabarty 2015; Mustian 2013;Pruthi 2012;Taso 2014). Chakrabarty 2015 provided missing means and SDs for fatigue; Mustian 2013 provided means and SDs for the subgroup of women with breast cancer that was not reported separately in the original publication; Pruthi 2012 provided missing means and SDs for health‐related quality of life, depression, anxiety and fatigue; and Taso 2014 provided missing means and SDs for depression and anxiety. For two other studies, we sought but did not retrieve missing data from study authors (Bernardi 2013;Siedentopf 2013). We imputed no missing SDs from other studies.
Comparison 1. Yoga versus no therapy
We retrieved missing data from the authors of two studies for the short‐term outcomes of depression, anxiety and fatigue, and from the authors of one study for short‐term sleep disturbances. When we included only studies for which we retrieved no missing data from study authors, results of pooled analyses did not change substantially (Analysis 26.1; Analysis 26.2; Analysis 26.3; Analysis 26.4; Analysis 26.5; Analysis 26.6; Analysis 26.7).
26.1. Analysis.
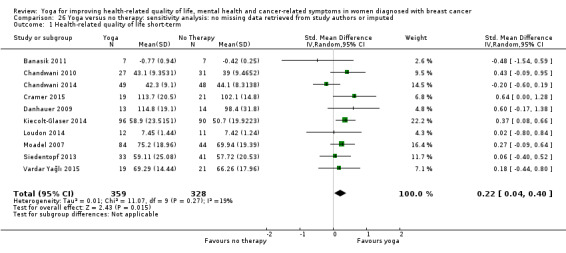
Comparison 26 Yoga versus no therapy: sensitivity analysis: no missing data retrieved from study authors or imputed, Outcome 1 Health‐related quality of life short‐term.
26.2. Analysis.
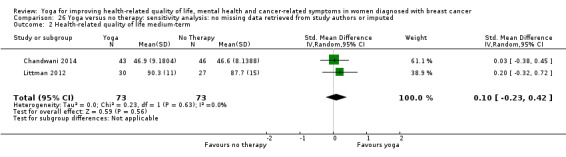
Comparison 26 Yoga versus no therapy: sensitivity analysis: no missing data retrieved from study authors or imputed, Outcome 2 Health‐related quality of life medium‐term.
26.3. Analysis.
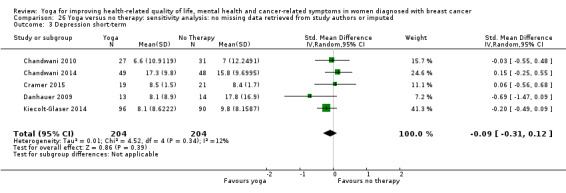
Comparison 26 Yoga versus no therapy: sensitivity analysis: no missing data retrieved from study authors or imputed, Outcome 3 Depression short‐term.
26.4. Analysis.
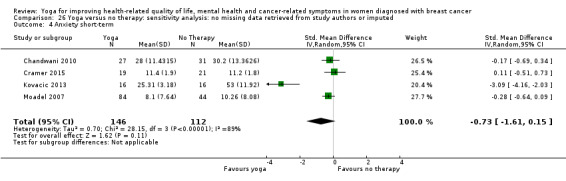
Comparison 26 Yoga versus no therapy: sensitivity analysis: no missing data retrieved from study authors or imputed, Outcome 4 Anxiety short‐term.
26.5. Analysis.
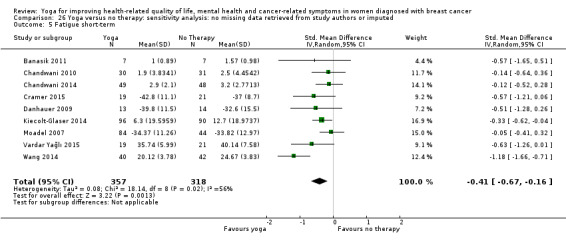
Comparison 26 Yoga versus no therapy: sensitivity analysis: no missing data retrieved from study authors or imputed, Outcome 5 Fatigue short‐term.
26.6. Analysis.
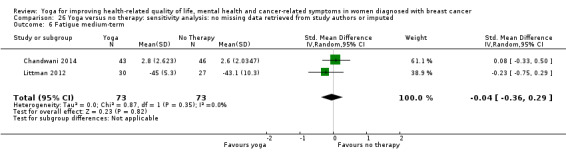
Comparison 26 Yoga versus no therapy: sensitivity analysis: no missing data retrieved from study authors or imputed, Outcome 6 Fatigue medium‐term.
26.7. Analysis.
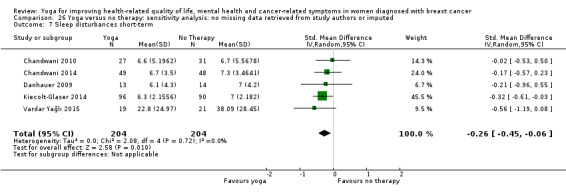
Comparison 26 Yoga versus no therapy: sensitivity analysis: no missing data retrieved from study authors or imputed, Outcome 7 Sleep disturbances short‐term.
Comparison 2. Yoga versus psychosocial/educational interventions
We did not impute or otherwise replace missing data; therefore, results did not change (Analysis 27.1; Analysis 27.2; Analysis 27.3; Analysis 27.4; Analysis 27.5).
27.1. Analysis.
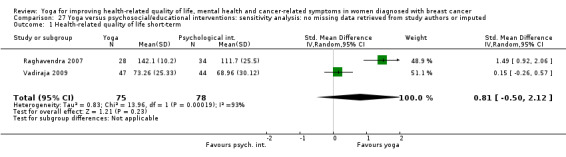
Comparison 27 Yoga versus psychosocial/educational interventions: sensitivity analysis: no missing data retrieved from study authors or imputed, Outcome 1 Health‐related quality of life short‐term.
27.2. Analysis.
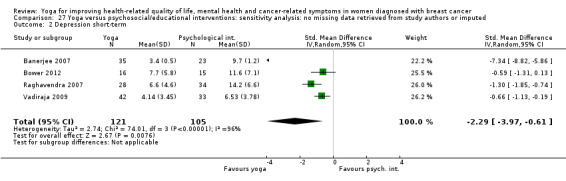
Comparison 27 Yoga versus psychosocial/educational interventions: sensitivity analysis: no missing data retrieved from study authors or imputed, Outcome 2 Depression short‐term.
27.3. Analysis.

Comparison 27 Yoga versus psychosocial/educational interventions: sensitivity analysis: no missing data retrieved from study authors or imputed, Outcome 3 Anxiety short‐term.
27.4. Analysis.
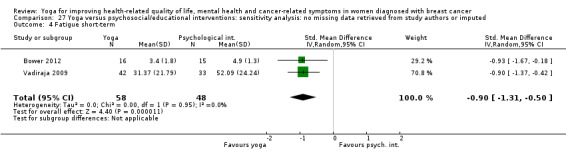
Comparison 27 Yoga versus psychosocial/educational interventions: sensitivity analysis: no missing data retrieved from study authors or imputed, Outcome 4 Fatigue short‐term.
27.5. Analysis.
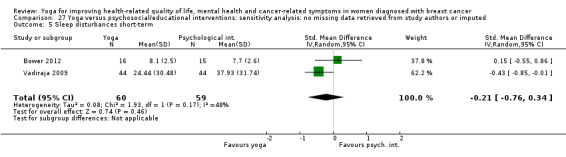
Comparison 27 Yoga versus psychosocial/educational interventions: sensitivity analysis: no missing data retrieved from study authors or imputed, Outcome 5 Sleep disturbances short‐term.
Comparison 3. Yoga versus exercise
We retrieved missing data from the authors of one study for the short‐term outcomes of health‐related quality of life and fatigue. When we included only studies for which we retrieved no missing data from study authors, results of pooled analyses did not change substantially (Analysis 28.1; Analysis 28.2).
28.1. Analysis.
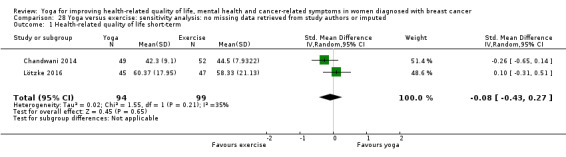
Comparison 28 Yoga versus exercise: sensitivity analysis: no missing data retrieved from study authors or imputed, Outcome 1 Health‐related quality of life short‐term.
28.2. Analysis.
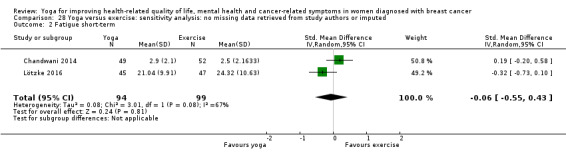
Comparison 28 Yoga versus exercise: sensitivity analysis: no missing data retrieved from study authors or imputed, Outcome 2 Fatigue short‐term.
Unpublished or published only in abstract format
Comparison 1. Yoga versus no therapy
All studies were published as full‐text articles; therefore, results did not change.
Comparison 2. Yoga versus psychosocial/educational interventions
All studies were published as full‐text articles; therefore, results did not change.
Comparison 3. Yoga versus exercise
All studies were published as full‐text articles; therefore, results did not change.
Discussion
Summary of main results
This review of 24 randomised controlled trials with a total of 2166 women with a diagnosis of breast cancer evaluated effects of yoga on patient‐reported outcomes. We found evidence of effects favouring yoga over no therapy for improving health‐related quality of life, fatigue and sleep disturbances. However, according to Cohen's categories (Cohen 1998), group differences were small or moderate in size. Thus, although statistically significant, these group differences might not be clinically relevant. Moreover, almost all studies assessed only short‐term effects; only two studies assessed medium‐term effects of yoga on health‐related quality of life and fatigue (Chandwani 2014; Littman 2012), which have not been sustained; and no study investigated long‐term effects. Evidence suggests short‐term effects of yoga compared with psychosocial/educational interventions on depression, anxiety and fatigue. Although effect sizes were large, all analyses had considerable heterogeneity that for the most part could not be reduced by subsequent subgroup analyses. Investigators have not assessed medium‐term and long‐term effects. Two studies compared yoga versus exercise interventions (Chandwani 2014; Lötzke 2016) and found comparable effects for the two interventions.
We found no evidence of publication bias favouring yoga and no evidence of serious adverse events. However, we did not formally test for publication bias, and only two studies adequately assessed and reported on serious adverse events (Cramer 2015; Danhauer 2009). Thus, conclusions regarding non‐publication of insignificant study results and judgements of safety remain preliminary.
Subgroup analyses revealed evidence of differential effects of yoga in relation to several factors. During active cancer treatment, yoga improved depression, anxiety and fatigue compared with no therapy or psychosocial/educational interventions; after completion of active cancer treatment, results showed effects on health‐related quality of life, fatigue and sleep disturbances. Regarding time since diagnosis, yoga improved depression, anxiety, fatigue and sleep disturbances during the first five years after diagnosis, and we could not evaluate effects of yoga after this time frame. Likewise, although yoga improved health‐related quality of life, depression, anxiety, fatigue and sleep disturbances in non‐metastatic breast cancer, we could not evaluate these effects in metastatic breast cancer. Most studies used complex yoga interventions incorporating physical exercise, breath control and/or meditation; these multi‐modal interventions improved women's health‐related quality of life, depression, anxiety, fatigue and sleep disturbances, but exercise‐based interventions influenced only fatigue, and we found no reliable evidence for meditation‐based interventions.
Overall completeness and applicability of evidence
A large number of studies assessed all predefined primary outcome measures. Most of the included studies (17 and 15 studies, respectively) assessed fatigue and health‐related quality of life while using a variety of outcome measures. On the other hand, although only eight studies assessed sleep disturbances, most of these studies used the Pittsburgh Sleep Quality Index. The main drawback regarding completeness of evidence was related to safety: Only five studies reported any safety‐related data, and only two reported adverse events consistent with our predefined criteria (Cramer 2015; Danhauer 2009). Thus, although meta‐analyses were possible for all efficacy outcomes, we could calculate no meta‐analysis for safety.
Very few studies have investigated medium‐term effects, and no studies have assessed long‐term effects; therefore, the evidence can be applied only to short‐term effects.
Most studies compared yoga versus no therapy; only five studies assessed the comparative efficacy of yoga and psychosocial/educational interventions, and meta‐analyses were adequately powered to detect group differences. Given that exercise is an effective intervention for improving health‐related quality of life and fatigue in women with a diagnosis of breast cancer (Mishra 2012a; Mishra 2012b), one can expect to see smaller group differences when yoga is compared with exercise. Thus, the three studies with a total of 233 participants (Chandwani 2014; Lötzke 2016; Vardar Yağlı 2015) might be underpowered to detect evidence of small effects favouring yoga over exercise, or vice versa.
Subgroup analyses suggest that findings are applicable to both women undergoing active cancer treatment and women who have completed active cancer treatment but pertain only to women whose non‐metastatic breast cancer had been diagnosed within the previous five years. Whether yoga can also benefit women with metastatic breast cancer or those whose breast cancer had been diagnosed longer ago cannot be concluded on the basis of available evidence. Moreover, the evidence is applicable only to complex yoga interventions; we found evidence for effects of exercise‐based interventions only for fatigue, and no reliable evidence shows effects of meditation‐based yoga in women with a diagnosis of breast cancer.
Quality of the evidence
Overall risk of bias in studies on yoga in patients with a diagnosis of breast cancer was unclear to low, presenting a somewhat better picture than other fields of yoga therapy research (Cramer 2015). However, seven and 10 of 24 included studies did not use and did not report adequate methods of random sequence generation and allocation concealment, respectively. We judged risk of detection bias as low in five studies (Carson 2009; Kiecolt‐Glaser 2014; Kovacic 2013; Loudon 2014; Mustian 2013) and risk of performance bias as low in only a single study (Bower 2012). In sensitivity analyses, all effects were robust against one or more domains of risk of bias; however, only effects on fatigue were consistently robust against all domains of risk of bias in almost all sensitivity analyses.
Although heterogeneity was low for most comparisons of yoga versus no therapy, we found moderately to considerably high heterogeneity in most meta‐analyses comparing yoga versus psychosocial/educational interventions, and subgroup analyses generally did not reduce detected heterogeneity.
Overall, we judged statistically significant group differences between yoga and no therapy or psychosocial/educational interventions as having moderate quality; thus the true effect is likely to be close to the estimate of effect but may be substantially different, and further research may change the estimate (Balshem 2011; Guyatt 2008). Other comparisons, especially comparisons of yoga versus exercise, were of low to very low quality; therefore, any estimate of effect is very uncertain, and the true effect is likely to be substantially different from the estimate of effect (Balshem 2011; Guyatt 2008).
Potential biases in the review process
Given that we searched the most important medical databases, trial registries and conference proceedings with no language restrictions, it is unlikely that we introduced important bias during the literature search. We might have introduced potential bias by not including one study for which the outcome measure was unclear (Ojha 2012) and three conference abstracts that provided insufficient data (Cohen 2015; Dominique 2010; Stan 2013). In this way, we might have lost additional evidence. Further, upon request, study authors provided data that were missing from four studies (Chakrabarty 2015; Mustian 2013; Pruthi 2012; Taso 2014). Although exclusion of studies for which missing data were replaced in sensitivity analyses did not substantially change review findings, this inclusion of non‐peer‐reviewed data might have introduced bias. It is generally regarded as impossible to blind participants and especially personnel in yoga studies. This is why we performed no sensitivity analysis, but lack of blinding of participants and personnel might have introduced bias. As no adequate sham or placebo procedure for yoga interventions has yet been developed, specific and non‐specific effects of yoga interventions cannot be differentiated to date.
Agreements and disagreements with other studies or reviews
Although so far five systematic reviews have focussed explicitly on women with a diagnosis of breast cancer (Cramer 2012b; Harder 2012; Levine 2012; Pan 2015; Zhang 2012), none of them included all of the randomised trials that are included in the current review.
The meta‐analysis by Zhang 2012 included six randomised trials with a total of 382 women with a diagnosis of breast cancer that compared yoga versus no therapy and found small short‐term effects favouring yoga on health‐related quality of life. Although group differences in anxiety and depression favoured yoga, they were not statistically significant; likewise, researchers reported no statistically significant effects on fatigue. Although the current review found comparable effects, it includes almost three times as many trials and found statistically significant effects on depression, anxiety and fatigue.
A further meta‐analysis found positive effects of yoga versus no therapy or psychosocial/educational interventions on health‐related quality of life, depression, anxiety and fatigue (Cramer 2012a; Cramer 2012b). This meta‐analysis included 12 randomised controlled trials (RCTs) with a total of 742 participants that also were included in the current review. In contrast to current findings, subgroup analyses found effects only for women currently undergoing active treatment ‐ not for women who had completed active cancer treatment.
A systematic review not including a meta‐analysis found effects of yoga compared with various control interventions on health‐related quality of life, depression and anxiety (Harder 2012). Evidence showing effects on fatigue was inconclusive, with three of seven included trials reporting positive effects of yoga. Moreover, the review treated multiple publications on the same randomised trial (Raghavendra 2007; Vadiraja 2009) as unique studies.
Pan 2015 included 16 RCTs with a total of 930 participants; however, investigators included multiple publications by Raghavendra 2007 and Vadiraja 2009 as unique trials in their meta‐analysis, inadequately increasing the power of the analysis. Thus, one must interpret with care reported effects on health‐related quality of life, depression and anxiety.
Levine 2012 included both randomised and uncontrolled trials and concluded that yoga can improve health‐related quality of life; however, this review included only seven of the 24 trials included in the current review, did not provide a critical appraisal of available studies and did not conduct a meta‐analysis.
Although findings of the current review are more or less consistent with those of earlier reviews, differences between findings are due most likely to differences in time points of the literature search or inclusion criteria, and thus in the number of included studies and/or differences in analysis methods ‐ mainly use or non‐use of meta‐analytical methods.
Authors' conclusions
Implications for practice.
Yoga, specifically, complex yoga interventions incorporating breath control and/or meditation beyond physical yoga postures, can be considered a supportive intervention for improving short‐term health‐related quality of life, depression, anxiety, fatigue and sleep disturbances in women with recently diagnosed non‐metastatic breast cancer who are currently undergoing chemotherapy or radiotherapy or have completed curative cancer treatment. No conclusions can be reached regarding women with diagnosed metastatic breast cancer or long‐term cancer survivors. Given that evidence showing safety of the intervention is promising but preliminary, experienced yoga therapists should closely monitor this intervention.
Implications for research.
This review identified several gaps in available evidence for yoga as a supportive intervention in women with a diagnosis of breast cancer. More research is needed on the risks and benefits of yoga for women with diagnosed metastatic breast cancer, as well as for longer‐term breast cancer survivors. Moreover, future studies should investigate effects of different yoga interventions and should clarify which components of yoga (physical exercise, breath control, meditation) are essential for its effects in women with diagnosed breast cancer. Although no difference in effectiveness of different yoga styles is apparent (Cramer 2016), meta‐analyses have shown, for example, that inclusion of meditation in a yoga intervention seems to be essential for its efficacy in patients with depressive disorders (Cramer 2013). Given that chronic pain is an important problem for many women with diagnosed breast cancer, future RCTs and meta‐analyses should assess effects of yoga on chronic pain in this patient population.
Future trials should ensure rigorous methods and reporting, mainly adequate sample size, adequate randomisation, allocation concealment, intention‐to treat analysis and blinding of at least outcome assessors (Schulz 2010). Adequate control groups that control for therapist attention and other non‐specific effects associated with lack of blinding would be worthwhile to reduce risk of performance bias. Moreover, future trials should assess medium‐term and long‐term effects of the intervention.
Recently, the safety of yoga has been questioned (Broad 2012). Although a meta‐analysis of all available randomised trials on yoga across different participant groups found no evidence of increased risk of serious adverse events associated with yoga practice (Cramer 2015), most available trials examining yoga for women with diagnosed breast cancer have inadequately reported safety‐related data, rendering conclusions regarding safety of the interventions as preliminary. Thus, future studies should pay increased attention to adequately assessing and reporting safety data.
Acknowledgements
The review authors would like to thank the editorial team of the Cochrane Breast Cancer Review Group for help provided throughout the process of writing this protocol.
Appendices
Appendix 1. MEDLINE
#1 yoga [mh]
#2 yoga* [tiab]
#3 yogic [tiab]
#4 meditation [tiab]
#5 asana* [tiab]
#6 pranayama [tiab]
#7 dharana [tiab]
#8 dhyana [tiab]
#9 #1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8
#10 breast neoplasms [mh]
#11 breast neoplasm* [tiab]
#12 breast cancer [tiab]
#13 breast carcinoma* [tiab]
#14 breast tumor* [tiab]
#15 mamma carcinoma* [tiab]
#16 mammary neoplasm* [tiab]
#17 mammary carcinoma* [tiab]
#18 mammary gland carcinoma* [tiab]
#19 #10 OR #11 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18
#20 randomized controlled trial [pt]
#21 controlled clinical trial [pt]
#22 randomized [tiab]
#23 placebo [tiab]
#24 clinical trials as topic [mesh: noexp]
#25 randomly [tiab]
#26 trial [ti]
#27 #19 OR #20 OR #21 OR #22 OR #23 OR #24 OR #25 OR #26
#28 Search #7 AND #17 AND #25
#29 Search animals[mh] NOT humans[mh]
#30 Search #26 NOT #27
Appendix 2. Embase
#1
random* OR factorial* OR crossover* OR cross NEXT/1 over* OR placebo* OR (doubl* AND blind*) OR (singl* AND blind*) OR assign* OR allocat* OR volunteer*OR 'crossover procedure'/exp OR 'double blind procedure'/exp OR 'randomized controlled trial'/exp OR 'single blind procedure'/exp
#2
'breast neoplasm'
#3
'breast cancer'/exp OR 'breast cancer'
#4
'breast tumour'
#5
'breast tumor'/exp OR 'breast tumor'
#6
'breast carcinoma'/exp OR 'breast carcinoma'
#7
'mamma carcinoma'/exp OR 'mamma carcinoma'
#8
'mammary neoplasm'
#9
'mammary carcinoma'/exp OR 'mammary carcinoma'
#10
'mammary gland carcinoma'
#11
#2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10
#12
'breast cancer survivor'
#13
'breast cancer survivors'
#14
#12 OR #13
#15
#11 OR #14
#16
'yoga'/exp OR yoga
#17
yogic
#18
asana
#19
pranayama
#20
dhyana
#21
dharana
#22
'meditation'/exp OR meditation
#23
#16 OR #17 OR #18 OR #19 OR #20 OR #21 OR #22
#24
#1 AND #11 AND #23
#25
#24 NOT ([animals]/lim NOT [humans]/lim)
#26
#25 AND [embase]/lim
Embase (via OvidSP) search
| 1 | Randomized controlled trial/ |
| 2 | Controlled clinical study/ |
| 3 | Random$.ti,ab. |
| 4 | randomization/ |
| 5 | intermethod comparison/ |
| 6 | placebo.ti,ab. |
| 7 | (compare or compared or comparison).ti. |
| 8 | ((evaluated or evaluate or evaluating or assessed or assess) and (compare or compared or comparing or comparison)).ab. |
| 9 | (open adj label).ti,ab. |
| 10 | ((double or single or doubly or singly) adj (blind or blinded or blindly)).ti,ab. |
| 11 | double blind procedure/ |
| 12 | parallel group$1.ti,ab. |
| 13 | (crossover or cross over).ti,ab. |
| 14 | ((assign$ or match or matched or allocation) adj5 (alternate or group$1 or intervention$1 or patient$1 or subject$1 or participant$1)).ti,ab. |
| 15 | (assigned or allocated).ti,ab. |
| 16 | (controlled adj7 (study or design or trial)).ti,ab. |
| 17 | (volunteer or volunteers).ti,ab. |
| 18 | human experiment/ |
| 19 | trial.ti. |
| 20 | or/1‐19 |
| 21 | exp breast/ |
| 22 | exp breast disease/ |
| 23 | (21 or 22) and exp neoplasm/ |
| 24 | exp breast tumor/ |
| 25 | exp breast cancer/ |
| 26 | exp breast carcinoma/ |
| 27 | (breast$ adj5 (neoplas$ or cancer$ or carcin$ or tumo$ or metasta$ or malig$)).ti,ab. |
| 28 | or/21‐27 |
| 29 | exp yoga/ |
| 30 | (yora or yogic or asana or pranayama or dhyana or dharana or meditation).tw. |
| 31 | exp meditation/ |
| 32 | 29 or 30 or 31 |
| 33 | 20 and 28 and 32 |
| 34 | limit 33 to embase |
Appendix 3. CENTRAL
#1 MeSH descriptor: [Breast Neoplasms] explode all trees #2 breast near cancer* #3 breast near neoplasm* #4 breast near carcinoma* #5 breast near tumour* #6 breast near tumor* #7 #1 or #2 or #3 or #4 or #5 or #6 #8 MeSH descriptor: [Yoga] explode all trees #9 MeSH descriptor: [Meditation] explode all trees #10 yoga or yogic or meditation or asana or pranayama or dharana or dhyana #11 #8 or #9 or #10 #12 #7 and #11
Appendix 4. WHO ICTRP search portal
Basic searches:
1. Yoga for women with breast cancer and breast cancer survivors
2. Breast cancer AND yoga
3. Breast cancer survivors AND yoga
Advanced searches:
1. Title: Yoga for women with breast cancer and breast cancer survivors
Recruitment Status: ALL
2. Condition: breast cancer
Intervention: yoga OR yogic OR asana OR pranayama OR dhyana OR meditation OR dharana
Recruitment Status: ALL
3. Condition: breast cancer survivor*
Intervention: yoga OR yogic OR asana OR pranayama OR dhyana OR meditation OR dharana
Recruitment Status: ALL
4. Condition: breast cancer AND survivor
Intervention: yoga OR yogic OR asana OR pranayama OR dhyana OR meditation OR dharana
Recruitment Status: ALL
Appendix 5. Clinicaltrials.gov
Basic searches:
1. Yoga for women with breast cancer and breast cancer survivors
2. Breast cancer AND yoga
3. Breast cancer survivors AND yoga
Advanced searches:
1. Title: Yoga for women with breast cancer and breast cancer survivors
Recruitment: ALL
Study Results: ALL
Study Type: ALL
Gender: ALL
2. Condition: breast cancer
Intervention: yoga OR yogic OR yogic OR asana OR pranayama OR dhyana OR meditation OR dharana
Recruitment: ALL
Study Results: ALL
Study Type: ALL
Gender: ALL
3. Condition: breast cancer survivor
Intervention: yoga OR yogic OR yogic OR asana OR pranayama OR dhyana OR meditation OR dharana
Recruitment: ALL
Study Results: ALL
Study Type: ALL
Gender: ALL
4. Condition: breast cancer AND survivor
Intervention: yoga OR yogic OR yogic OR asana OR pranayama OR dhyana OR meditation OR dharana
Recruitment: ALL
Study Results: ALL
Study Type: ALL
Gender: ALL
Appendix 6. IndMed
(yoga OR yogic OR meditation OR asana OR asanas OR pranayama OR dharana OR dhyana) AND (breast neoplasm OR breast neoplasms OR breast cancer OR breast carcinoma OR breast carcinomas OR breast tumor OR breast tumors OR mamma carcinoma OR mamma carcinomas)
Data and analyses
Comparison 1. Yoga versus no therapy.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Health‐related quality of life short‐term | 10 | 675 | Std. Mean Difference (IV, Random, 95% CI) | 0.22 [0.04, 0.40] |
| 2 Health‐related quality of life medium‐term | 2 | 146 | Std. Mean Difference (IV, Random, 95% CI) | 0.10 [‐0.23, 0.42] |
| 3 Depression short‐term | 7 | 496 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.13 [‐0.31, 0.05] |
| 4 Anxiety short‐term | 6 | 346 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.53 [‐1.10, 0.04] |
| 5 Fatigue short‐term | 11 | 883 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.48 [‐0.75, ‐0.20] |
| 6 Fatigue medium‐term | 2 | 146 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.04 [‐0.36, 0.29] |
| 7 Sleep disturbances short‐term | 6 | 657 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.25 [‐0.40, ‐0.09] |
Comparison 2. Yoga versus psychological interventions.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Health‐related quality of life short‐term | 2 | 153 | Std. Mean Difference (IV, Random, 95% CI) | 0.81 [‐0.50, 2.12] |
| 2 Depression short‐term | 4 | 226 | Std. Mean Difference (IV, Random, 95% CI) | ‐2.29 [‐3.97, ‐0.61] |
| 3 Anxiety short‐term | 3 | 195 | Std. Mean Difference (IV, Random, 95% CI) | ‐2.21 [‐3.90, ‐0.52] |
| 4 Fatigue short‐term | 2 | 106 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.90 [‐1.31, ‐0.50] |
| 5 Sleep disturbances short‐term | 2 | 119 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.21 [‐0.76, 0.34] |
Comparison 3. Yoga versus exercise.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Health‐related quality of life short‐term | 3 | 233 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.04 [‐0.30, 0.23] |
| 2 Fatigue short‐term | 3 | 233 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.21 [‐0.66, 0.25] |
Comparison 4. Yoga versus no therapy: subgroup analysis: current treatment status.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Health‐related quality of life short‐term | 7 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 Women undergoing active cancer treatment | 2 | 155 | Std. Mean Difference (IV, Random, 95% CI) | 0.09 [‐0.53, 0.71] |
| 1.2 Women who have completed active cancer treatment | 5 | 290 | Std. Mean Difference (IV, Random, 95% CI) | 0.36 [0.11, 0.60] |
| 2 Health‐related quality of life medium‐term | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 Women undergoing active cancer treatment | 1 | 89 | Std. Mean Difference (IV, Random, 95% CI) | 0.03 [‐0.38, 0.45] |
| 2.2 Women who have completed active cancer treatment | 1 | 57 | Std. Mean Difference (IV, Random, 95% CI) | 0.20 [‐0.32, 0.72] |
| 3 Depression short‐term | 6 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.1 Women undergoing active cancer treatment | 3 | 215 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.02 [‐0.29, 0.24] |
| 3.2 Women who have completed active treatment | 3 | 253 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.21 [‐0.49, 0.06] |
| 4 Anxiety short‐term | 4 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 4.1 Women undergoing active cancer treatment | 3 | 150 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.15 [‐2.43, 0.13] |
| 4.2 Women who have completed active treatment | 1 | 40 | Std. Mean Difference (IV, Random, 95% CI) | 0.11 [‐0.51, 0.73] |
| 5 Fatigue short‐term | 9 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 5.1 Women undergoing active cancer treatment | 5 | 460 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.68 [‐1.18, ‐0.19] |
| 5.2 Women who have completed active treatment | 4 | 267 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.40 [‐0.64, ‐0.15] |
| 6 Fatigue medium‐term | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 6.1 Women undergoing active cancer treatment | 1 | 89 | Std. Mean Difference (IV, Random, 95% CI) | 0.08 [‐0.33, 0.50] |
| 6.2 Women who have completed active treatment | 1 | 57 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.23 [‐0.75, 0.29] |
| 7 Sleep disturbances short‐term | 6 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 7.1 Women undergoing active cancer treatment | 2 | 155 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.11 [‐0.43, 0.20] |
| 7.2 Women who have completed active treatment | 4 | 502 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.29 [‐0.46, ‐0.11] |
Comparison 5. Yoga versus psychological interventions: subgroup analysis: current treatment status.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Health‐related quality of life short‐term | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 Women undergoing active cancer treatment | 2 | 153 | Std. Mean Difference (IV, Random, 95% CI) | 0.81 [‐0.50, 2.12] |
| 1.2 Women who have completed active treatment | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2 Depression short‐term | 4 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 Women undergoing active cancer treatment | 3 | 195 | Std. Mean Difference (IV, Random, 95% CI) | ‐2.94 [‐5.27, ‐0.60] |
| 2.2 Women who have completed active treatment | 1 | 31 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.59 [‐1.31, 0.13] |
| 3 Anxiety short‐term | 3 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.1 Women undergoing active cancer treatment | 3 | 195 | Std. Mean Difference (IV, Random, 95% CI) | ‐2.21 [‐3.90, ‐0.52] |
| 3.2 Women who have completed active treatment | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Fatigue short‐term | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 4.1 Women undergoing active cancer treatment | 1 | 75 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.90 [‐1.37, ‐0.42] |
| 4.2 Women who have completed active treatment | 1 | 31 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.93 [‐1.67, ‐0.18] |
| 5 Sleep disturbances short‐term | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 5.1 Women undergoing active cancer treatment | 1 | 88 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.43 [‐0.85, ‐0.01] |
| 5.2 Women who have completed active treatment | 1 | 31 | Std. Mean Difference (IV, Random, 95% CI) | 0.15 [‐0.55, 0.86] |
5.1. Analysis.
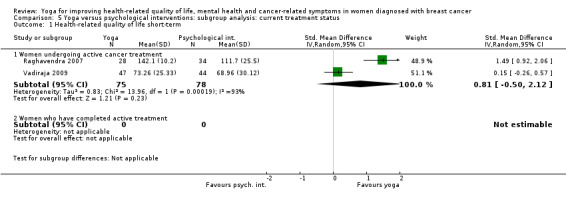
Comparison 5 Yoga versus psychological interventions: subgroup analysis: current treatment status, Outcome 1 Health‐related quality of life short‐term.
5.4. Analysis.
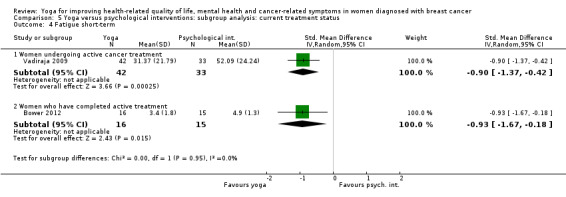
Comparison 5 Yoga versus psychological interventions: subgroup analysis: current treatment status, Outcome 4 Fatigue short‐term.
5.5. Analysis.
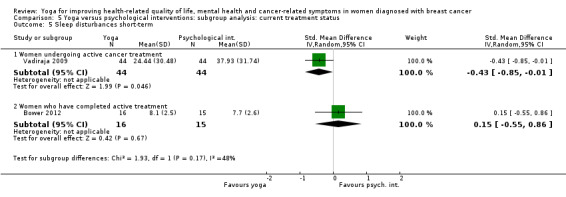
Comparison 5 Yoga versus psychological interventions: subgroup analysis: current treatment status, Outcome 5 Sleep disturbances short‐term.
Comparison 6. Yoga versus exercise: subgroup analysis: current treatment status.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Health‐related quality of life short‐term | 3 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 Women undergoing active cancer treatment | 2 | 193 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.08 [‐0.43, 0.27] |
| 1.2 Women who have completed active treatment | 1 | 40 | Std. Mean Difference (IV, Random, 95% CI) | 0.18 [‐0.44, 0.80] |
| 2 Fatigue short‐term | 3 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 Women undergoing active cancer treatment | 2 | 193 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.06 [‐0.55, 0.43] |
| 2.2 Women who have completed active treatment | 1 | 40 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.63 [‐1.26, 0.01] |
6.1. Analysis.
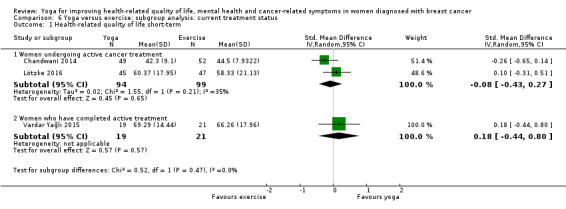
Comparison 6 Yoga versus exercise: subgroup analysis: current treatment status, Outcome 1 Health‐related quality of life short‐term.
6.2. Analysis.
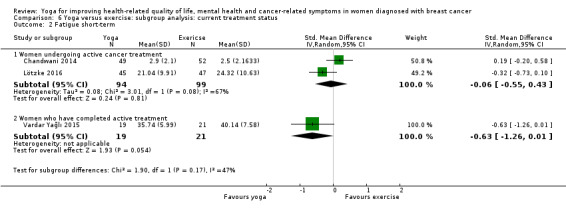
Comparison 6 Yoga versus exercise: subgroup analysis: current treatment status, Outcome 2 Fatigue short‐term.
Comparison 7. Yoga versus no therapy: subgroup analysis: time since diagnosis.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Health‐related quality of life short‐term | 6 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 ≤ 5 years | 6 | 412 | Std. Mean Difference (IV, Random, 95% CI) | 0.16 [‐0.06, 0.38] |
| 1.2 > 5 years | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2 Health‐related quality of life medium‐term | 1 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 ≤ 5 years | 1 | 89 | Std. Mean Difference (IV, Random, 95% CI) | 0.03 [‐0.38, 0.45] |
| 2.2 > 5 years | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 3 Depression short‐term | 5 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.1 ≤ 5 years | 5 | 270 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.12 [‐0.38, 0.14] |
| 3.2 > 5 years | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Anxiety short‐term | 5 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 4.1 ≤ 5 years | 5 | 306 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.67 [‐1.34, ‐0.01] |
| 4.2 > 5 years | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Fatigue short‐term | 8 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 5.1 ≤ 5 years | 8 | 643 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.49 [‐0.86, ‐0.11] |
| 5.2 > 5 years | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Fatigue medium‐term | 1 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 6.1 ≤ 5 years | 1 | 89 | Std. Mean Difference (IV, Random, 95% CI) | 0.08 [‐0.33, 0.50] |
| 6.2 > 5 years | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Sleep disturbances short‐term | 5 | 471 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.22 [‐0.40, ‐0.03] |
| 7.1 ≤ 5 years | 5 | 471 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.22 [‐0.40, ‐0.03] |
| 7.2 > 5 years | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
7.1. Analysis.
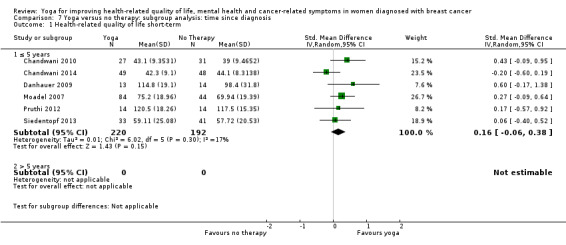
Comparison 7 Yoga versus no therapy: subgroup analysis: time since diagnosis, Outcome 1 Health‐related quality of life short‐term.
7.2. Analysis.
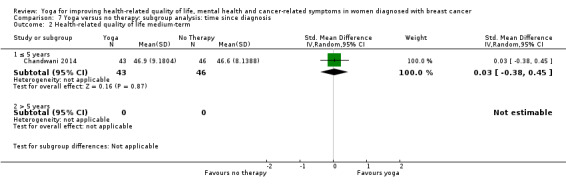
Comparison 7 Yoga versus no therapy: subgroup analysis: time since diagnosis, Outcome 2 Health‐related quality of life medium‐term.
7.3. Analysis.
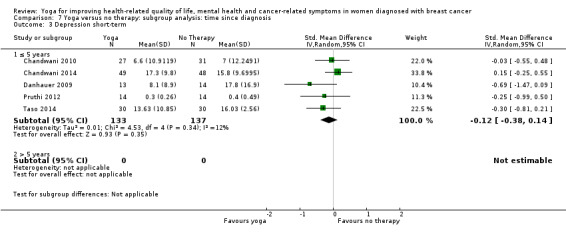
Comparison 7 Yoga versus no therapy: subgroup analysis: time since diagnosis, Outcome 3 Depression short‐term.
7.6. Analysis.
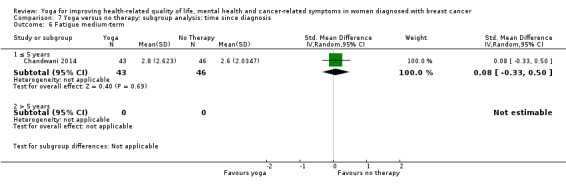
Comparison 7 Yoga versus no therapy: subgroup analysis: time since diagnosis, Outcome 6 Fatigue medium‐term.
Comparison 8. Yoga versus psychological interventions: subgroup analysis: time since diagnosis.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Health‐related quality of life short‐term | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 ≤ 5 years | 2 | 153 | Std. Mean Difference (IV, Random, 95% CI) | 0.81 [‐0.50, 2.12] |
| 1.2 > 5 years | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2 Depression short‐term | 3 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 ≤ 5 years | 3 | 195 | Std. Mean Difference (IV, Random, 95% CI) | ‐2.94 [‐5.27, ‐0.60] |
| 2.2 > 5 years | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 3 Anxiety short‐term | 3 | 195 | Std. Mean Difference (IV, Random, 95% CI) | ‐2.21 [‐3.90, ‐0.52] |
| 3.1 ≤ 5 years | 3 | 195 | Std. Mean Difference (IV, Random, 95% CI) | ‐2.21 [‐3.90, ‐0.52] |
| 3.2 > 5 years | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Fatigue short‐term | 1 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 4.1 ≤ 5 years | 1 | 75 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.90 [‐1.37, ‐0.42] |
| 4.2 > 5 years | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Sleep disturbances short‐term | 1 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 5.1 ≤ 5 years | 1 | 88 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.43 [‐0.85, ‐0.01] |
| 5.2 > 5 years | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
8.1. Analysis.
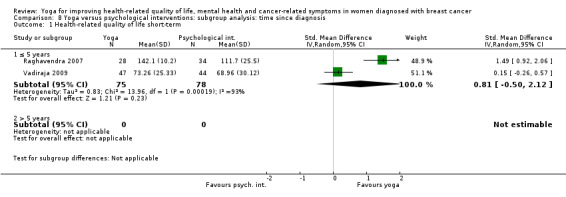
Comparison 8 Yoga versus psychological interventions: subgroup analysis: time since diagnosis, Outcome 1 Health‐related quality of life short‐term.
8.5. Analysis.
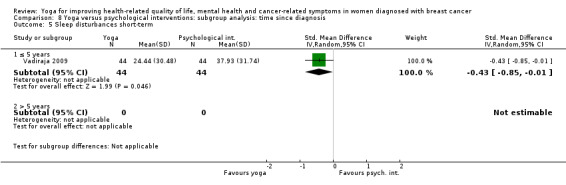
Comparison 8 Yoga versus psychological interventions: subgroup analysis: time since diagnosis, Outcome 5 Sleep disturbances short‐term.
Comparison 9. Yoga versus exercise: subgroup analysis: time since diagnosis.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Health‐related quality of life short‐term | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 ≤ 5 years | 2 | 193 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.08 [‐0.43, 0.27] |
| 1.2 > 5 years | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2 Fatigue short‐term | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 ≤ 5 years | 2 | 193 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.06 [‐0.55, 0.43] |
| 2.2 > 5 years | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
9.1. Analysis.
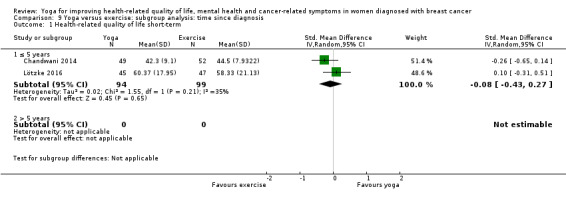
Comparison 9 Yoga versus exercise: subgroup analysis: time since diagnosis, Outcome 1 Health‐related quality of life short‐term.
9.2. Analysis.
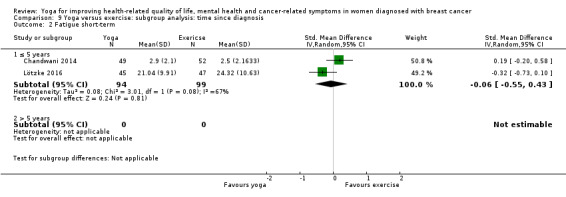
Comparison 9 Yoga versus exercise: subgroup analysis: time since diagnosis, Outcome 2 Fatigue short‐term.
Comparison 10. Yoga versus no therapy: subgroup analysis: stage of cancer.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Health‐related quality of life short‐term | 7 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 Non‐metastatic breast cancer | 7 | 560 | Std. Mean Difference (IV, Random, 95% CI) | 0.24 [0.04, 0.45] |
| 1.2 Metastatic breast cancer | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2 Health‐related quality of life medium‐term | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 Non‐metastatic breast cancer | 2 | 146 | Std. Mean Difference (IV, Random, 95% CI) | 0.10 [‐0.23, 0.42] |
| 2.2 Metastatic breast cancer | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 3 Depression short‐term | 6 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.1 Non‐metastatic breast cancer | 6 | 469 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.10 [‐0.28, 0.08] |
| 3.2 Metastatic breast cancer | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Anxiety short‐term | 6 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 4.1 Non‐metastatic breast cancer | 6 | 346 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.53 [‐1.10, 0.04] |
| 4.2 Metastatic breast cancer | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Fatigue short‐term | 8 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 5.1 Non‐metastatic breast cancer | 8 | 760 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.38 [‐0.67, ‐0.09] |
| 5.2 Metastatic breast cancer | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Fatigue medium‐term | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 6.1 Non‐metastatic breast cancer | 2 | 146 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.04 [‐0.36, 0.29] |
| 6.2 Metastatic breast cancer | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Sleep disturbances short‐term | 5 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 7.1 Non‐metastatic breast cancer | 5 | 630 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.25 [‐0.40, ‐0.09] |
| 7.2 Metastatic breast cancer | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
10.2. Analysis.
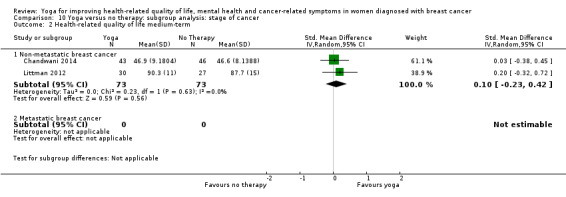
Comparison 10 Yoga versus no therapy: subgroup analysis: stage of cancer, Outcome 2 Health‐related quality of life medium‐term.
10.3. Analysis.
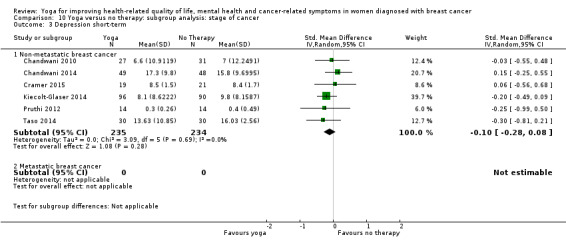
Comparison 10 Yoga versus no therapy: subgroup analysis: stage of cancer, Outcome 3 Depression short‐term.
10.4. Analysis.
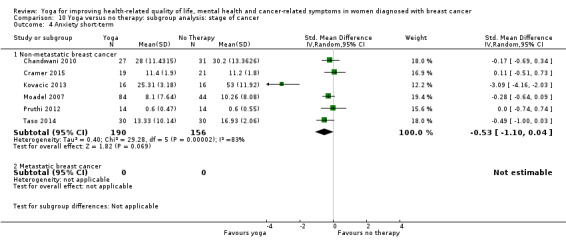
Comparison 10 Yoga versus no therapy: subgroup analysis: stage of cancer, Outcome 4 Anxiety short‐term.
10.6. Analysis.
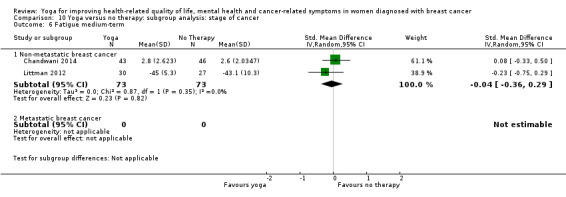
Comparison 10 Yoga versus no therapy: subgroup analysis: stage of cancer, Outcome 6 Fatigue medium‐term.
Comparison 11. Yoga versus psychological interventions: subgroup analysis: stage of cancer.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Health‐related quality of life short‐term | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 Non‐metastatic breast cancer | 2 | 153 | Std. Mean Difference (IV, Random, 95% CI) | 0.81 [‐0.50, 2.12] |
| 1.2 Metastatic breast cancer | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2 Depression short‐term | 4 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 Non‐metastatic breast cancer | 4 | 226 | Std. Mean Difference (IV, Random, 95% CI) | ‐2.29 [‐3.97, ‐0.61] |
| 2.2 Metastatic breast cancer | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 3 Anxiety short‐term | 3 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.1 Non‐metastatic breast cancer | 3 | 195 | Std. Mean Difference (IV, Random, 95% CI) | ‐2.21 [‐3.90, ‐0.52] |
| 3.2 Metastatic breast cancer | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Fatigue short‐term | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 4.1 Non‐metastatic breast cancer | 2 | 106 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.90 [‐1.31, ‐0.50] |
| 4.2 Metastatic breast cancer | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Sleep disturbances short‐term | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 5.1 Non‐metastatic breast cancer | 2 | 119 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.21 [‐0.76, 0.34] |
| 5.2 Metastatic breast cancer | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
11.1. Analysis.
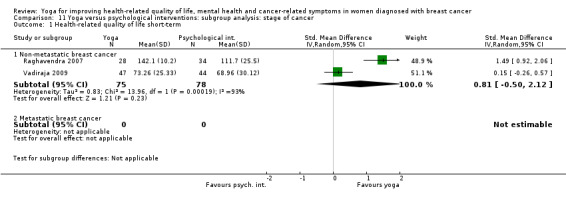
Comparison 11 Yoga versus psychological interventions: subgroup analysis: stage of cancer, Outcome 1 Health‐related quality of life short‐term.
11.5. Analysis.
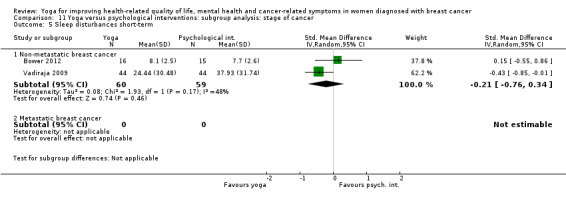
Comparison 11 Yoga versus psychological interventions: subgroup analysis: stage of cancer, Outcome 5 Sleep disturbances short‐term.
Comparison 12. Yoga versus exercise: subgroup analysis: stage of cancer.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Health‐related quality of life short‐term | 3 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 Non‐metastatic breast cancer | 3 | 233 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.04 [‐0.30, 0.23] |
| 1.2 Metastatic breast cancer | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2 Fatigue short‐term | 3 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 Non‐metastatic breast cancer | 3 | 233 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.21 [‐0.66, 0.25] |
| 2.2 Metastatic breast cancer | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
12.1. Analysis.
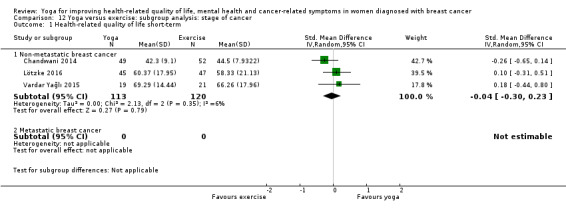
Comparison 12 Yoga versus exercise: subgroup analysis: stage of cancer, Outcome 1 Health‐related quality of life short‐term.
12.2. Analysis.
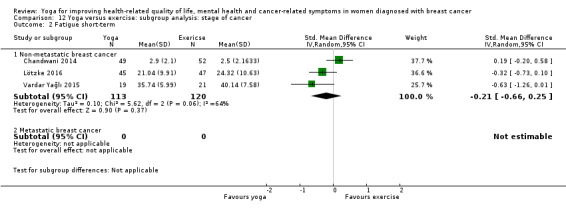
Comparison 12 Yoga versus exercise: subgroup analysis: stage of cancer, Outcome 2 Fatigue short‐term.
Comparison 13. Yoga versus no therapy: subgroup analysis: yoga intervention.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Health‐related quality of life short‐term | 10 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 Complex yoga intervention | 9 | 661 | Std. Mean Difference (IV, Random, 95% CI) | 0.24 [0.06, 0.41] |
| 1.2 Exercise‐based yoga intervention | 1 | 14 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.48 [‐1.54, 0.59] |
| 1.3 Meditation‐based yoga intervention | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2 Health‐related quality of life medium‐term | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 Complex yoga intervention | 2 | 146 | Std. Mean Difference (IV, Random, 95% CI) | 0.10 [‐0.23, 0.42] |
| 2.2 Exercise‐based yoga intervention | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2.3 Meditation‐based yoga intervention | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 3 Depression short‐term | 7 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.1 Complex yoga intervention | 7 | 496 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.13 [‐0.31, 0.05] |
| 3.2 Exercise‐based yoga intervention | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 3.3 Meditation‐based yoga intervention | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Anxiety short‐term | 6 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 4.1 Complex yoga intervention | 6 | 346 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.53 [‐1.10, 0.04] |
| 4.2 Exercise‐based yoga intervention | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 4.3 Meditation‐based yoga intervention | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Fatigue short‐term | 11 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 5.1 Complex yoga intervention | 8 | 627 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.37 [‐0.69, ‐0.05] |
| 5.2 Exercise‐based yoga intervention | 2 | 96 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.08 [‐1.53, ‐0.62] |
| 5.3 Meditation‐based yoga intervention | 1 | 160 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.53 [‐0.84, ‐0.21] |
| 6 Fatigue medium‐term | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 6.1 Complex yoga intervention | 2 | 146 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.04 [‐0.36, 0.29] |
| 6.2 Exercise‐based yoga intervention | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 6.3 Meditation‐based yoga intervention | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Sleep disturbances short‐term | 6 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 7.1 Complex yoga intervention | 6 | 657 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.25 [‐0.40, ‐0.09] |
| 7.2 Exercise‐based yoga intervention | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 7.3 Meditation‐based yoga intervention | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
13.2. Analysis.
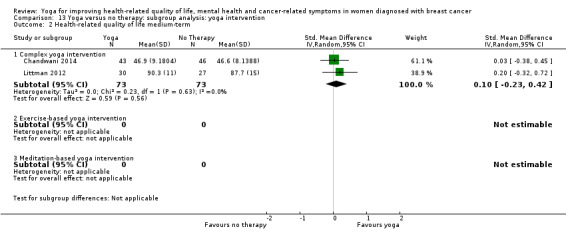
Comparison 13 Yoga versus no therapy: subgroup analysis: yoga intervention, Outcome 2 Health‐related quality of life medium‐term.
13.3. Analysis.
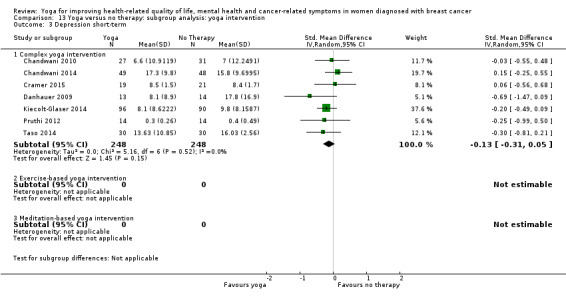
Comparison 13 Yoga versus no therapy: subgroup analysis: yoga intervention, Outcome 3 Depression short‐term.
13.4. Analysis.
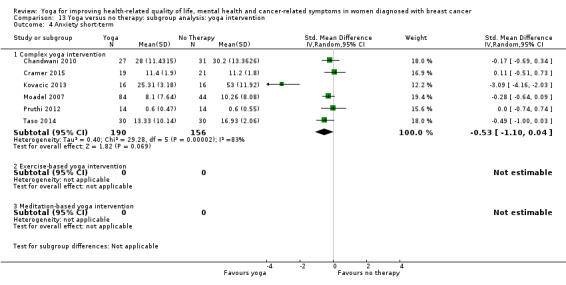
Comparison 13 Yoga versus no therapy: subgroup analysis: yoga intervention, Outcome 4 Anxiety short‐term.
13.6. Analysis.
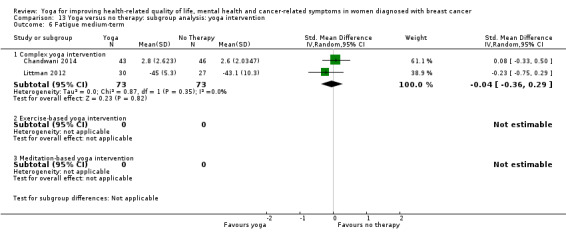
Comparison 13 Yoga versus no therapy: subgroup analysis: yoga intervention, Outcome 6 Fatigue medium‐term.
Comparison 14. Yoga versus psychological interventions: subgroup analysis: yoga intervention.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Health‐related quality of life short‐term | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 Complex yoga intervention | 2 | 153 | Std. Mean Difference (IV, Random, 95% CI) | 0.81 [‐0.50, 2.12] |
| 1.2 Exercise‐based yoga intervention | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 1.3 Meditation‐based yoga intervention | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2 Depression short‐term | 4 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 Complex yoga intervention | 4 | 226 | Std. Mean Difference (IV, Random, 95% CI) | ‐2.29 [‐3.97, ‐0.61] |
| 2.2 Exercise‐based yoga intervention | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2.3 Meditation‐based yoga intervention | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 3 Anxiety short‐term | 3 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.1 Complex yoga intervention | 3 | 195 | Std. Mean Difference (IV, Random, 95% CI) | ‐2.21 [‐3.90, ‐0.52] |
| 3.2 Exercise‐based yoga intervention | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 3.3 Meditation‐based yoga intervention | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Fatigue short‐term | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 4.1 Complex yoga intervention | 2 | 106 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.90 [‐1.31, ‐0.50] |
| 4.2 Exercise‐based yoga intervention | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 4.3 Meditation‐based yoga intervention | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Sleep disturbances short‐term | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 5.1 Complex yoga intervention | 2 | 119 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.21 [‐0.76, 0.34] |
| 5.2 Exercise‐based yoga intervention | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 5.3 Meditation‐based yoga intervention | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
14.1. Analysis.
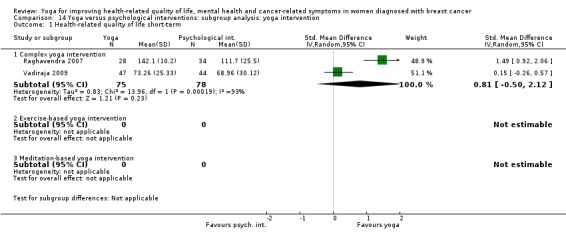
Comparison 14 Yoga versus psychological interventions: subgroup analysis: yoga intervention, Outcome 1 Health‐related quality of life short‐term.
14.5. Analysis.
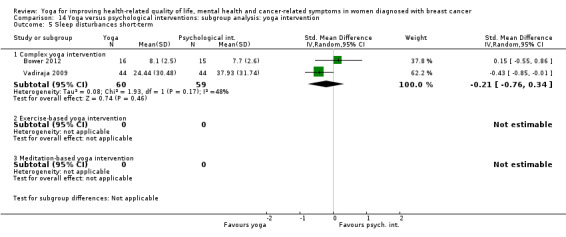
Comparison 14 Yoga versus psychological interventions: subgroup analysis: yoga intervention, Outcome 5 Sleep disturbances short‐term.
Comparison 15. Yoga versus exercise: subgroup analysis: yoga intervention.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Health‐related quality of life short‐term | 3 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 Complex yoga intervention | 3 | 233 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.04 [‐0.30, 0.23] |
| 1.2 Exercise‐based yoga intervention | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 1.3 Meditation‐based yoga intervention | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2 Fatigue short‐term | 3 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 Complex yoga intervention | 3 | 233 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.21 [‐0.66, 0.25] |
| 2.2 Exercise‐based yoga intervention | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2.3 Meditation‐based yoga intervention | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
Comparison 16. Yoga versus no therapy: sensitivity analysis: random sequence generation.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Health‐related quality of life short‐term | 6 | 478 | Std. Mean Difference (IV, Random, 95% CI) | 0.21 [‐0.04, 0.46] |
| 2 Health‐related quality of life medium‐term | 2 | 146 | Std. Mean Difference (IV, Random, 95% CI) | 0.10 [‐0.23, 0.42] |
| 3 Depression short‐term | 5 | 441 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.09 [‐0.28, 0.10] |
| 4 Anxiety short‐term | 4 | 190 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.80 [‐1.77, 0.16] |
| 5 Fatigue short‐term | 6 | 604 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.50 [‐0.84, ‐0.17] |
| 6 Fatigue medium‐term | 2 | 146 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.04 [‐0.36, 0.29] |
| 7 Sleep disturbances short‐term | 4 | 590 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.23 [‐0.39, ‐0.06] |
Comparison 17. Yoga versus psychological interventions: sensitivity analysis: random sequence generation.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Health‐related quality of life short‐term | 2 | 153 | Std. Mean Difference (IV, Random, 95% CI) | 0.81 [‐0.50, 2.12] |
| 2 Depression short‐term | 4 | 226 | Std. Mean Difference (IV, Random, 95% CI) | ‐2.29 [‐3.97, ‐0.61] |
| 3 Anxiety short‐term | 3 | 195 | Std. Mean Difference (IV, Random, 95% CI) | ‐2.21 [‐3.90, ‐0.52] |
| 4 Fatigue short‐term | 2 | 106 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.90 [‐1.31, ‐0.50] |
| 5 Sleep disturbances short‐term | 2 | 119 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.21 [‐0.76, 0.34] |
Comparison 18. Yoga versus exercise: sensitivity analysis: random sequence generation.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Health‐related quality of life short‐term | 1 | 101 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.26 [‐0.65, 0.14] |
| 2 Fatigue short‐term | 1 | 101 | Std. Mean Difference (IV, Random, 95% CI) | 0.19 [‐0.20, 0.58] |
Comparison 19. Yoga versus no therapy: sensitivity analysis: allocation concealment.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Health‐related quality of life short‐term | 4 | 323 | Std. Mean Difference (IV, Random, 95% CI) | 0.31 [0.09, 0.53] |
| 2 Depression short‐term | 3 | 286 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.19 [‐0.42, 0.05] |
| 3 Anxiety short‐term | 3 | 132 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.08 [‐2.53, 0.36] |
| 4 Fatigue short‐term | 11 | 883 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.48 [‐0.75, ‐0.20] |
| 5 Sleep disturbances short‐term | 3 | 475 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.29 [‐0.47, ‐0.11] |
Comparison 20. Yoga versus psychological interventions: sensitivity analysis: allocation concealment.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Health‐related quality of life short‐term | 2 | 153 | Std. Mean Difference (IV, Random, 95% CI) | 0.81 [‐0.50, 2.12] |
| 2 Depression short‐term | 4 | 226 | Std. Mean Difference (IV, Random, 95% CI) | ‐2.29 [‐3.97, ‐0.61] |
| 3 Anxiety short‐term | 3 | 195 | Std. Mean Difference (IV, Random, 95% CI) | ‐2.21 [‐3.90, ‐0.52] |
| 4 Fatigue short‐term | 2 | 106 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.90 [‐1.31, ‐0.50] |
| 5 Sleep disturbances short‐term | 2 | 119 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.21 [‐0.76, 0.34] |
Comparison 21. Yoga versus exercise: sensitivity analysis: allocation concealment.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Health‐related quality of life short‐term | 1 | 40 | Std. Mean Difference (IV, Random, 95% CI) | 0.18 [‐0.44, 0.80] |
| 2 Fatigue short‐term | 1 | 40 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.63 [‐1.26, 0.01] |
Comparison 22. Yoga versus no therapy: sensitivity analysis: blinding of outcome assessment.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Health‐related quality of life short‐term | 2 | 209 | Std. Mean Difference (IV, Random, 95% CI) | 0.33 [0.06, 0.61] |
| 2 Depression short‐term | 1 | 186 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.20 [‐0.49, 0.09] |
| 3 Anxiety short‐term | 1 | 32 | Std. Mean Difference (IV, Random, 95% CI) | ‐3.09 [‐4.16, ‐2.03] |
| 4 Fatigue short‐term | 1 | 186 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.33 [‐0.62, ‐0.04] |
| 5 Sleep disturbances short‐term | 2 | 435 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.27 [‐0.46, ‐0.08] |
Comparison 23. Yoga versus no therapy: sensitivity analysis: incomplete outcome data.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Health‐related quality of life short‐term | 8 | 543 | Std. Mean Difference (IV, Random, 95% CI) | 0.21 [‐0.01, 0.44] |
| 2 Health‐related quality of life medium‐term | 2 | 146 | Std. Mean Difference (IV, Random, 95% CI) | 0.10 [‐0.23, 0.42] |
| 3 Depression short‐term | 6 | 438 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.14 [‐0.33, 0.05] |
| 4 Anxiety short‐term | 5 | 288 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.63 [‐1.35, 0.08] |
| 5 Fatigue short‐term | 10 | 822 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.51 [‐0.81, ‐0.21] |
| 6 Fatigue medium‐term | 2 | 146 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.04 [‐0.36, 0.29] |
| 7 Sleep disturbances short‐term | 4 | 559 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.25 [‐0.41, ‐0.08] |
Comparison 24. Yoga versus psychological interventions: sensitivity analysis: incomplete outcome data.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Depression short‐term | 1 | 31 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.59 [‐1.31, 0.13] |
| 2 Fatigue short‐term | 1 | 31 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.93 [‐1.67, ‐0.18] |
| 3 Sleep disturbances short‐term | 1 | 31 | Std. Mean Difference (IV, Random, 95% CI) | 0.15 [‐0.55, 0.86] |
Comparison 25. Yoga versus exercise: sensitivity analysis: incomplete outcome data.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Health‐related quality of life short‐term | 1 | 101 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.26 [‐0.65, 0.14] |
| 2 Fatigue short‐term | 1 | 101 | Std. Mean Difference (IV, Random, 95% CI) | 0.19 [‐0.20, 0.58] |
Comparison 26. Yoga versus no therapy: sensitivity analysis: no missing data retrieved from study authors or imputed.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Health‐related quality of life short‐term | 10 | 687 | Std. Mean Difference (IV, Random, 95% CI) | 0.22 [0.04, 0.40] |
| 2 Health‐related quality of life medium‐term | 2 | 146 | Std. Mean Difference (IV, Random, 95% CI) | 0.10 [‐0.23, 0.42] |
| 3 Depression short‐term | 5 | 408 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.09 [‐0.31, 0.12] |
| 4 Anxiety short‐term | 4 | 258 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.73 [‐1.61, 0.15] |
| 5 Fatigue short‐term | 9 | 675 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.41 [‐0.67, ‐0.16] |
| 6 Fatigue medium‐term | 2 | 146 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.04 [‐0.36, 0.29] |
| 7 Sleep disturbances short‐term | 5 | 408 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.26 [‐0.45, ‐0.06] |
Comparison 27. Yoga versus psychosocial/educational interventions: sensitivity analysis: no missing data retrieved from study authors or imputed.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Health‐related quality of life short‐term | 2 | 153 | Std. Mean Difference (IV, Random, 95% CI) | 0.81 [‐0.50, 2.12] |
| 2 Depression short‐term | 4 | 226 | Std. Mean Difference (IV, Random, 95% CI) | ‐2.29 [‐3.97, ‐0.61] |
| 3 Anxiety short‐term | 3 | 195 | Std. Mean Difference (IV, Random, 95% CI) | ‐2.21 [‐3.90, ‐0.52] |
| 4 Fatigue short‐term | 2 | 106 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.90 [‐1.31, ‐0.50] |
| 5 Sleep disturbances short‐term | 2 | 119 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.21 [‐0.76, 0.34] |
Comparison 28. Yoga versus exercise: sensitivity analysis: no missing data retrieved from study authors or imputed.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Health‐related quality of life short‐term | 2 | 193 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.08 [‐0.43, 0.27] |
| 2 Fatigue short‐term | 2 | 193 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.06 [‐0.55, 0.43] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Banasik 2011.
| Methods | Randomised controlled trial | |
| Participants | Women with diagnosed stage II‐IV breast cancer at least 2 months post treatment Recruited through a local cancer centre's database Mean age 62.9 years N = 18 |
|
| Interventions | • Iyengar yoga (yoga postures), 8 weeks, twice weekly for 90 minutes • Wait‐list, no treatment for 8 weeks |
|
| Outcomes | Health‐related quality of life (Functional Assessment of Cancer Therapy ‐ Breast Cancer) at week 8 Fatigue (new non‐validated instrument) at week 8 |
|
| Notes | Small sample size without a priori sample size calculation Large baseline differences between groups |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information on random sequence generation ("[...] were randomly assigned [...]") |
| Allocation concealment (selection bias) | Unclear risk | No information on allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information on blinding |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information on blinding |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 22% dropout but well balanced across groups |
| Selective reporting (reporting bias) | Low risk | No protocol available but no hint of selective reporting |
| Other bias | High risk | Large baseline differences between groups |
Banerjee 2007.
| Methods | Randomised controlled trial | |
| Participants | Women with diagnosed stage II‐III breast cancer undergoing radiotherapy during the study period Recruited from 3 cancer hospitals in India Mean age 44.0 years N = 68 |
|
| Interventions | • Integrated yoga programme (yoga postures, deep relaxation, breathing techniques, meditation, guided imagery, group awareness), 6 weeks, frequency not reported, 90 minutes per session • Supportive counselling and advice to take light exercise, 6 weeks, frequency and duration not reported |
|
| Outcomes | Anxiety (Hospital Anxiety and Depression Scale) at week 6 Depression (Hospital Anxiety and Depression Scale) at week 6 |
|
| Notes | Intervention intensity not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Randomization was performed using a computer‐generated random number table [...]" |
| Allocation concealment (selection bias) | Low risk | "[...] random number table with group assignments that was sent to the clinics [...], which was used sequentially to order group assignments during recruitment. The order of randomization was verified with the hospital date of admission records for radiotherapy at intervals to make sure that field personnel had not altered the sequence of randomization to suit allocation of consenting participants into the 2 study arms." |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information on blinding |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information on blinding of patient‐reported outcomes |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 30% dropout in control group, no dropout in yoga group |
| Selective reporting (reporting bias) | Low risk | No protocol available but no hint of selective reporting |
| Other bias | Low risk | No hint of other bias |
Bernardi 2013.
| Methods | Randomised controlled trial | |
| Participants | Women with diagnosed non‐metastatic breast cancer post mastectomy Recruited from outpatient service of a clinical hospital Mean age 51.3 years N = 45 |
|
| Interventions | • Individually applied yoga (yoga postures, breathing techniques, meditation), 6 yoga sessions, 45 minutes per session • No treatment for 6 weeks |
|
| Outcomes | Anxiety (State‐Trait Anxiety Inventory) at week ? (2 weeks post intervention) | |
| Notes | Qualitative interview after each yoga session Study authors were contacted for unpublished data, but no such data were used |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Lottery randomization" |
| Allocation concealment (selection bias) | Unclear risk | No information on allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information on blinding |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information on blinding |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No information on attrition |
| Selective reporting (reporting bias) | Low risk | No protocol available but no hint of selective reporting |
| Other bias | Low risk | No hint of other bias |
Bower 2012.
| Methods | Randomised controlled trial | |
| Participants | Women with diagnosed stage 0‐II breast cancer with persistent post‐treatment fatigue who had completed local and/or adjuvant cancer therapy Recruited through tumour registry mailings, newspaper advertisements and flyers Mean age 53.9 years N = 31 |
|
| Interventions | • Iyengar yoga (postures, breathing techniques), 12 weeks, twice weekly for 90 minutes • Health education, 12 weeks, once weekly for 120 minutes |
|
| Outcomes | Health‐related quality of life (Medical Outcomes Study 36‐item short‐form health survey vitality scale) at weeks 12 to 14 and week 24 Depression (Beck Depression Inventory‐II) at weeks 12 to 14 and week 24 Fatigue (Fatigue Symptom Inventory; Multidimensional Fatigue Symptom Inventory vigour subscale) at weeks 12 to 14 and week 24 Subjective Sleep Quality (Pittsburgh Sleep Quality Index) at weeks 12 to 14 and week 24 Safety (intervention‐related adverse events) |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "The allocation sequence was generated independently by the study statistician (R.O.) and was concealed in opaque envelopes." |
| Allocation concealment (selection bias) | Low risk | "The allocation sequence was generated independently by the study statistician (R.O.) and was concealed in opaque envelopes." |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | "On a 7‐point Likert scale ranging from 0 (not at all effective) to 6 (very effective), the mean score was 3.86 for the yoga group and 3.2 for the health education group (P = .33)." "[...] participants unavoidably are aware of the treatment that they receive. We attempted to minimize the impact of pre‐existing beliefs and expectations on study outcomes by informing participants that we were testing 2 different treatments for cancer‐related fatigue, each of which presumably was effective. This presentation appeared to have been successful, because both groups had similar, positive expectations about the efficacy of the treatment to which they had been assigned." |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | "Outcomes assessors for the performance tasks were blinded to group assignment, and all were trained in standardized testing procedures." No information on blinding of patient‐reported outcomes |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 12.5% dropouts in the yoga group, none in the control group; intention‐to‐treat analysis |
| Selective reporting (reporting bias) | Low risk | No protocol available but no hint of selective reporting. Reported outcomes comparable with pilot trial |
| Other bias | Low risk | No hint of other bias |
Carson 2009.
| Methods | Randomised controlled trial | |
| Participants | Women with diagnosed stage IA‐IIB breast cancer at least 2 years before the start of the study, experiencing hot flashes and currently not receiving chemotherapy or taking hormone replacement therapy Recruited from Duke University Medical Cancer Center Breast Oncology Mean age 54.4 years N = 37 |
|
| Interventions | • Yoga of Awareness (yoga postures, breathing techniques, meditation, study of pertinent topics, group discussion), 8 weeks, once weekly for 120 minutes • Wait‐list, no treatment for 8 weeks |
|
| Outcomes | Fatigue (daily diary) weeks 7‐8 and week 20 | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Randomization assignments were generated by an individual not involved in the study using a random number table." |
| Allocation concealment (selection bias) | Low risk | "Assignments were concealed in envelopes that were not opened until patients had completed their baseline assessment." |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information on blinding of participants and personnel |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | "The research assistant collecting assessment data was kept blind with regard to patient condition assignments." "Diary data was collected via an interactive telephone voice system." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 24% dropout in the yoga group and 15% in the control group; intention‐to‐treat analysis |
| Selective reporting (reporting bias) | Low risk | No protocol available but no hint of selective reporting |
| Other bias | Low risk | No hint of other bias |
Chakrabarty 2015.
| Methods | Randomised controlled trial | |
| Participants | Women with diagnosed stage I‐III breast cancer undergoing daily adjuvant radiation therapy for 6 weeks after completing surgery and chemotherapy Recruited from a cancer hospital and research centre Mean age 43.6 years N = 160 |
|
| Interventions | • Pranayama (breathing techniques), 6 weeks, twice daily, 5 days a week for 20 minutes • Routine care for 6 weeks |
|
| Outcomes | Fatigue (Cancer Fatigue Scale), week 6 | |
| Notes | Cancer Fatigue Scale prepared by researchers; validation study not published Unpublished means and standard deviations for Cancer Fatigue Scale were provided by study authors upon request. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Block randomisation |
| Allocation concealment (selection bias) | Low risk | Concealed numbered envelopes |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information on blinding |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information on blinding |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No attrition |
| Selective reporting (reporting bias) | Unclear risk | Cancer Fatigue Scale prepared by researchers; validation study not published |
| Other bias | Unclear risk | Cancer Fatigue Scale prepared by researchers; validation study not published |
Chandwani 2010.
| Methods | Randomised controlled trial using minimisation | |
| Participants | Women with diagnosed stage 0‐III breast cancer undergoing radiotherapy during the study period Recruited from The University of Texas M.D. Anderson Cancer Center Mean age not reported N = 81 |
|
| Interventions | • Yoga based on Patanjali`s yoga sutras (yoga postures, deep relaxation, breath control, meditation), 6 weeks, twice weekly for 60 minutes • Wait‐list, no treatment |
|
| Outcomes | Health‐related quality of life (Medical Outcomes Study 36‐item short‐form health survey) at week 7 and week 18 Depression (Center for Epidemiologic Studies Depression Scale) at week 7 and week 18 Anxiety (Speilberger State/Trait Anxiety Inventory) at week 7 and week 18 Fatigue (Brief Fatigue Inventory) at week 7 and week 18 Sleep disturbances (Pittsburgh Sleep Quality Index) at week 7 and week 18 |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Participants were then randomly assigned to either the YG or the WL control group by use of minimization, a form of adaptive randomization described previously." |
| Allocation concealment (selection bias) | Unclear risk | No information on allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information on blinding |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information on blinding |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 10% dropout in the yoga group and 0% in the control group; intention‐to‐treat analysis |
| Selective reporting (reporting bias) | Low risk | No protocol available but no hint of selective reporting |
| Other bias | Low risk | No hint of other bias |
Chandwani 2014.
| Methods | Randomised controlled trial using adaptive randomisation | |
| Participants | Women with diagnosed stage 0‐III breast cancer undergoing daily radiotherapy for 6 weeks Recruited from The University of Texas M.D. Anderson Cancer Center Mean age 51.9 years N = 178 |
|
| Interventions | • Integrated yoga programme (yoga postures, breath control, meditation), 6 weeks, 3 times weekly for 60 minutes • Exercise (mainly stretching), 6 weeks, 3 times weekly for 60 minutes • Wait‐list, usual care |
|
| Outcomes | Health‐related quality of life (Medical Outcomes Study 36‐item short‐form health survey) at week 6, week 19, week 12 and week 30 Depression (Center for Epidemiologic Studies Depression Scale) at week 6, week 19, week 12 and week 30 Fatigue (Brief Fatigue Inventory) at week 6, week 19, week 12 and week 30 Sleep disturbances (Pittsburgh Sleep Quality Index) at week 6, week 19, week 12 and week 30 |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Adaptive randomisation, according to age, stage of disease, time since diagnosis, type of surgery and chemotherapy (adjuvant/neoadjuvant) |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information on allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information on blinding |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information on blinding |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Post‐treatment dropout rate 16.3%. Missing outcome data balanced in numbers across groups, no differences between patients with and without missing data on the basis of medical, demographic or baseline outcomes |
| Selective reporting (reporting bias) | Low risk | No protocol available but no hint of selective reporting |
| Other bias | Low risk | No hint of other bias |
Cramer 2015.
| Methods | Randomised controlled trial | |
| Participants | Women with diagnosed stage I‐III breast cancer with menopausal symptoms who had completed surgical, radiotherapeutic and/or chemotherapeutic treatment Recruited from a Department of Gynecology Certified Breast Center Mean age 49.2 years N = 40 |
|
| Interventions | • Traditional Hatha yoga based on the teachings of Sivananda Saraswati (yoga postures, breathing techniques, meditation), 12 weeks, once weekly for 90 minutes • Wait‐list, usual care |
|
| Outcomes | Health‐related quality of life (Functional Assessment of Cancer Therapy ‐ Breast) at week 12 and week 24 Depression (Hospital Anxiety and Depression Scale) at week 12 and week 24 Anxiety (Hospital Anxiety and Depression Scale) at week 12 and week 24 Fatigue (Functional Assessment of Chronic Illness Therapy ‐ Fatigue) at week 12 and week 24 Safety (adverse events) at week 12 and week 24 |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "block randomization with randomly varying block lengths, which were stratified by the intake of anti‐oestrogen medication during the study period (2 strata: no intake and intake). The randomization list was created by a biometrician who was not involved in patient recruitment or assessment using the Random Allocation Software." |
| Allocation concealment (selection bias) | Low risk | "The randomization list was password‐secured and no individual other than the biometrician was able to access it." "Sealed, sequentially numbered envelopes containing the treatment assignments. After obtaining written informed consent and baseline assessment, the study physician opened the lowest numbered envelope to reveal that patient’s assignment." |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | "Participants were not blinded to the allocated intervention." |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information on blinding of outcome assessment |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts |
| Selective reporting (reporting bias) | Low risk | Study protocol registered before patient recruitment. All of the study’s prespecified (primary and secondary) outcomes were reported in the prespecified way. |
| Other bias | Low risk | No hint of other bias |
Danhauer 2009.
| Methods | Randomised controlled trial | |
| Participants | Women with diagnosed breast cancer (any stage) 2‐24 months post surgery or recurrence of breast cancer within past 24 months Recruited from Breast Care Center in the Comprehensive Cancer Center of Wake Forest University Mean age 55.8 years N = 44 |
|
| Interventions | • Restorative yoga (yoga postures, breathing techniques, deep relaxation, meditation), 10 weeks, once weekly for 75 minutes • Wait‐list, no treatment |
|
| Outcomes | Health‐related quality of life (Functional Assessment of Cancer Therapy ‐ Breast Cancer; Functional Assessment of Chronic Illness Therapy ‐ Spiritual Well‐Being; Medical Outcomes Study 12‐item short‐form health survey) at week 10 Depression (Center for Epidemiologic Studies Depression Scale) at week 10 Fatigue (Functional Assessment of Cancer Therapy ‐ Fatigue) at week 10 Sleep disturbances (Pittsburgh Sleep Quality Index) at week 10 Safety (adverse events) |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Women were randomized to the RY group or a waitlist control group." |
| Allocation concealment (selection bias) | Unclear risk | "Women were randomized to the RY group or a waitlist control group." |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information on blinding |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information on blinding |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 40% dropout in yoga group and 36% dropout in control group; intention‐to‐treat analysis |
| Selective reporting (reporting bias) | Low risk | No protocol available but no hint of selective reporting |
| Other bias | Low risk | No hint of other bias |
Kiecolt‐Glaser 2014.
| Methods | Randomised controlled trial | |
| Participants | Women with diagnosed stage 0‐III breast cancer at least 2 months after completion of surgery and adjuvant treatment (except for aromatase inhibitors or tamoxifen) Recruited from clinical research centre Mean age 51.6 years N = 200 |
|
| Interventions | • Hatha yoga (yoga postures, breathing techniques), 12 weeks, twice a week for 90 minutes • Wait‐list, no treatment |
|
| Outcomes | Health‐related quality of life (Medical Outcomes Study 36‐item‐short‐form health survey) at week 12 Depression (Center for Epidemiological Studies Depression Scale) at week 12 Fatigue (Multidimensional Fatigue Symptom Inventory‐Short Form) at week 12 Sleep quality (Pittsburgh Sleep Quality Index) at week 12 Safety (adverse events) at week 12 |
|
| Notes | Duplicate publications separately reported different outcomes of the same trial. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "The data manager stratified participants by cancer stage (0 v I v II and IIIA) as well as radiation therapy received or not, and then used an online randomization program to obtain the block randomization sequence (six per block) for assignment to yoga or control within strata." |
| Allocation concealment (selection bias) | Low risk | "The data manager had no participant contact." |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants were told to not mention their group assignment to study personnel. Personnel were blinded but participants were not. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | "The data manager had no participant contact." Participants were told to not mention their group assignment to study personnel during their post‐treatment assessments; questionnaires were administered via computer. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 4% attrition in yoga group, 10% in control group |
| Selective reporting (reporting bias) | Unclear risk | Study protocol registered. Several reported outcome parameters not listed in study protocol. Duplicate publications separately reported different outcomes of the same trial. |
| Other bias | Low risk | No hint of other bias |
Kovacic 2013.
| Methods | Randomised controlled trial using Latin Square randomisations | |
| Participants | Women with diagnosed stage I‐II breast cancer receiving multi‐modal therapy (surgery, radiotherapy, chemotherapy) Recruited from the Institute for Oncology Ljubljana Mean age not reported N = 32 |
|
| Interventions | • Yoga in Daily Life® System (yoga postures, breathing techniques, deep relaxation, progressive muscle relaxation, meditation), 1 week, once daily for 45 minutes combined with standard physiotherapy • Standard physiotherapy |
|
| Outcomes | Anxiety (Spielberger's State‐Trait Anxiety Inventory) at week 2 and week 5 | |
| Notes | Duplicate publications separately reported different outcomes of the same trial. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "The Latin Square randomization method was used in the study. Stratifying factors were type of surgery, severity and stage of breast cancer, and socio‐demographic
characteristics (age, marital status, employment status, education). Baseline values between experimental and control group regarding stratifying factors were successfully equalized." "A randomization list was prepared by the independent statistician using the random permuted blocks. This technique has ensured that equal numbers of patients within each stratum were randomized to each intervention (restricted stratified randomization)." |
| Allocation concealment (selection bias) | Low risk | No information on allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | "[...] patient blinding was impossible [...]" |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | "Outcome measures were obtained by blinded assessors [...]." |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No information on attrition |
| Selective reporting (reporting bias) | High risk | Duplicate publications separately reported different outcomes of the same trial. |
| Other bias | Low risk | No hint of other bias |
Littman 2012.
| Methods | Randomised controlled trial | |
| Participants | Overweight or obese women with diagnosed stage 0‐III breast cancer at least 3 months post treatment (with the exception of antihormonal treatment) Recruited via oncologist referrals, advertising, announcements, a website and direct mailings to interested women Mean age 60.6 years N = 63 |
|
| Interventions | • Viniyoga (yoga postures, breathing techniques, deep relaxation, meditation), 6 months, 1 to 3 times a week for 75 minutes • Wait‐list, no treatment for 6 months |
|
| Outcomes | Health‐related quality of life (Functional Assessment of Cancer Therapy ‐ General) at week 48 Fatigue (Functional Assessment of Chronic Illness Therapy ‐ Fatigue) at week 48 |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Eligible women were block randomized to the intervention or a waitlist control group on age (three strata: 21–49, 50–69, and 70–75 years), stage (two strata: 0/I and II/III), and BMI (two strata: 24–29.9 and ≥30 kg/m2) to assure comparability in the two groups." |
| Allocation concealment (selection bias) | Unclear risk | No information on allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information on blinding of participants and personnel |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | "[...] due to the pilot nature of the study and limited funding, we were unable to blind assessors to group assignment." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 16% dropout in yoga group and 13% dropout in control group within 12 months; intention‐to‐treat analysis |
| Selective reporting (reporting bias) | Low risk | No protocol available but no hint of selective reporting |
| Other bias | Low risk | No hint of other bias |
Loudon 2014.
| Methods | Randomised controlled trial | |
| Participants | Women with diagnosed breast cancer and stage I unilateral secondary lymphoedema of the arm Recruited from community health centres Mean age 57.7 years N = 23 |
|
| Interventions | • Satyananda yoga (yoga postures, breathing techniques, relaxation techniques, meditation), 8 weeks, once weekly for 90 minutes • Wait‐list, usual care for 8 weeks |
|
| Outcomes | Health‐related quality of life (Lymphoedema Quality of Life Tool) at week 8 and week 12 Fatigue (Visual Analogue Scale) at week 8 and week 12 |
|
| Notes | Other outcome measures related to lymphoedema | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was conducted by a person not associated with the trial by a computer‐generated random number system. |
| Allocation concealment (selection bias) | Low risk | Participants received notification of their group allocation in sealed envelopes after baseline testing. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information on blinding of participants and personnel |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Researchers blinded to group allocation and previous results |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 20% dropout in yoga group, 15% dropout in control group at week 8 |
| Selective reporting (reporting bias) | High risk | Results differ compared with study protocol. Quality of life changed from primary to secondary outcome. 4‐week measurements no longer mentioned, not all outcomes reported |
| Other bias | High risk | Small sample size; original sample size calculation: 19 participants per group necessary. From Mixed‐Methods Study (Protocol) to Pilot Study |
Lötzke 2016.
| Methods | Randomised controlled trial | |
| Participants | Women with diagnosed stage I‐III breast cancer undergoing cytotoxic (neo)adjuvant or endocrine adjuvant treatment Recruited from a University Hospital's Interdisciplinary Breast Center Mean age 51.2 years N = 119 |
|
| Interventions | • Iyengar yoga (yoga postures, breathing techniques), 12 weeks, once weekly for 20 minutes • Physical exercise, 12 weeks, once weekly for 20 minutes |
|
| Outcomes | Health‐related quality of life (European Organisation of Research and Treatment of Cancer QLQ‐30) at week 12 and week 24 Fatigue (EORTC QLQ‐C30 Fatigue Symptom Scale; 15‐item Cancer Fatigue Scale (CFS‐D)) at week 12 and week 24 |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Participants were randomized to one of the two intervention groups." No information on procedure of randomisation |
| Allocation concealment (selection bias) | Unclear risk | No information on allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information on blinding |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information on blinding |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | "Three patients dropped out at t1 and finally 54 patients at t2 (59%). Reasons could not be documented clearly." Sample size was not large enough to compensate for dropouts. |
| Selective reporting (reporting bias) | Low risk | No protocol available but no hint of selective reporting |
| Other bias | Unclear risk | "The number of lessons varied from 5 to 12, and the lapse of time, in between the patients performed, varied from 6 weeks to 25 weeks. This variation was not considered in the analysis." Intervention period and compliance unclear |
Moadel 2007.
| Methods | Randomised controlled trial using minimisation | |
| Participants | Women with diagnosed stage I‐III breast cancer within the previous 5 years Recruited from a university medical centre and from private clinics Mean age 54.8 years N = 164 |
|
| Interventions | • Hatha yoga (yoga postures, breathing techniques, meditation), 12 weeks, once weekly for 90 minutes • Wait‐list, no treatment |
|
| Outcomes | Health‐related quality of life (Functional Assessment of Cancer Therapy ‐ Breast Cancer; Functional Assessment of Chronic Illness Therapy ‐ Spiritual Well‐Being) at week 4, week 12 and week 24 Anxiety (Distressed Mood Index) at week 4, week 12 and week 24 Fatigue (Functional Assessment of Chronic Illness Therapy ‐ Fatigue) at week 4, week 12 and week 24 |
|
| Notes | Outcomes at week 24 not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Random assignment was in a 2:1 ratio to intervention or control after stratification by treatment (chemotherapy or antiestrogen therapy)." "After acquisition of written informed consent and the baseline assessment, patients were randomly assigned to start classes either immediately or in 3 months." |
| Allocation concealment (selection bias) | Unclear risk | No information on allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information on blinding |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information on blinding |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 22% dropout in yoga group and 21% dropout in control group; intention‐to‐treat analysis |
| Selective reporting (reporting bias) | Low risk | No protocol available but no hint of selective reporting |
| Other bias | Low risk | No hint of other bias |
Mustian 2013.
| Methods | Randomised controlled trial | |
| Participants | Women with diagnosed non‐metastatic breast cancer between 2 and 24 months after surgery, chemotherapy and/or radiation with sleep disturbances Recruited from Community Clinical Oncology Program (CCOP) clinics and through the use of flyers in communities Mean age 54.1 years N = 309 |
|
| Interventions | • Yoga for Cancer Survivors (YOCAS) programme (yoga postures, breathing techniques, meditation), 4 weeks, twice weekly for 75 minutes • Wait‐list, no treatment |
|
| Outcomes | Sleep disturbances (Pittsburgh Sleep Quality Index) at week 4 Safety (adverse events) at week 4 |
|
| Notes | Subgroup analysis for women with diagnosed breast cancer was derived from a study on patients with mixed cancer sites; unpublished sample size, means and standard deviations for Pittsburgh Sleep Quality Index were provided by study authors upon request. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Survivors were recruited in cohorts (n = 20 to 30), stratified by sex and baseline sleep disturbance (two levels…) and randomly assigned to both groups at each CCOP. Group assignment was determined by a computer‐generated random numbers table in blocks of two and an allocation ratio of 1:1." |
| Allocation concealment (selection bias) | Low risk | "Allocation was concealed from coordinators until after they registered the participants by using a computerized Web site that generated an e‐mail to the research base and CCOP site." |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | "Participants received their allocation assignment after completing baseline assessments." |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | "The study primary investigator and biostatistician were blinded to allocation." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 22% of enrolled participants were lost to follow‐up and/or did not provide fully evaluable data; intention‐to‐treat analysis |
| Selective reporting (reporting bias) | High risk | Published substudy with additional questionnaires that were not mentioned in the original study protocol |
| Other bias | Low risk | No hint of other bias |
Pruthi 2012.
| Methods | Randomised controlled trial | |
| Participants | Women with diagnosed non‐metastatic breast cancer without metastasis Recruited from an academic medical centre breast clinic Mean age 56.5 years N = 30 |
|
| Interventions | • Individual yoga sessions (yoga postures, breathing techniques), 3 weeks, once weekly for 60 minutes, followed by group yoga sessions (yoga postures, breathing techniques), 8 weeks, once weekly for 60 minutes (total of 11 weeks) • Wait‐list, usual care for 11 weeks |
|
| Outcomes | Health‐related quality of life (Functional Assessment of Cancer Treatment ‐ Breast Cancer) at week 12 Depression (Profile of Mood States ‐ Short Form) at week 12 Anxiety (Profile of Mood States ‐ Short Form) at week 12 Fatigue (Brief Fatigue Inventory, Profile of Mood States ‐ Short Form) at week 12 |
|
| Notes | Unpublished means and standard deviations for the Functional Assessment of Cancer Treatment ‐ Breast Cancer and the Profile of Mood States ‐ Short Form were provided by study authors upon request. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information on methods of random sequence generation |
| Allocation concealment (selection bias) | Unclear risk | No information on allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information on blinding |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information on blinding |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Balanced numbers of dropouts in both groups |
| Selective reporting (reporting bias) | Low risk | No protocol available but no hint of selective reporting |
| Other bias | Low risk | No hint of other bias |
Raghavendra 2007.
| Methods | Randomised controlled trial | |
| Participants | Women with diagnosed stage II‐III operable breast cancer undergoing adjuvant chemotherapy during the study period Recruited from the Bangalore Institute of Oncology Mean age not reported N = 98 |
|
| Interventions | • Integrated yoga programme (yoga postures, breathing techniques, relaxation with imagery, chanting), programme length not reported, 30 minutes 4 times, 60 minutes every 10 days • Brief supportive therapy, programme length not reported, 60 minutes once, 30 minutes every 10 days |
|
| Outcomes | Health‐related quality of life (Functional Living Index ‐ Cancer) Depression (Beck Depression Inventory) Anxiety (Speilberger State/Trait Anxiety Inventory) |
|
| Notes | Subgroup analyses were published separately. Time frame of outcome assessment was not reported. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Subjects [...] were randomly allocated to receive either one of these interventions prior to their primary treatment or surgery, using random numbers generated by a random number table." |
| Allocation concealment (selection bias) | Low risk | "Randomization was performed using opaque envelopes with group assignments. The envelopes were opened sequentially in the order of assignment during recruitment, with the names and registration numbers of the participants written on the covers. The order of randomization was verified with the hospital date of admission records for surgery at study intervals to make sure that field personnel had not altered the sequence of randomization to suit the allocation of consenting participants into two study arms." |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information on blinding |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information on blinding |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 43% dropout in the yoga group and 30% dropout in the control group |
| Selective reporting (reporting bias) | Low risk | No protocol available but no hint of selective reporting |
| Other bias | High risk | Time frame of outcome assessment was not reported. Participants were excluded if they did not receive their prescribed chemotherapy cycles. The number of randomised participants in each group was not reported. |
Siedentopf 2013.
| Methods | Randomised controlled trial | |
| Participants | Women with diagnosed breast cancer in the immediate postoperative phase Recruited from a hospital breast centre Mean age 57.0 years N = 93 |
|
| Interventions | • Gitananda yoga and viniyoga (yoga postures, breathing techniques, relaxation techniques), 5 weeks, twice weekly for 75 minutes • Wait‐list, usual care for 5 weeks |
|
| Outcomes | Health‐related quality of life (European Organisation of Research and Treatment of Cancer QLQ‐30 and QLQ‐BR23) at week 5 and week 17 | |
| Notes | Study authors were contacted for unpublished data, but no such data were used. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Lottery randomisation process |
| Allocation concealment (selection bias) | Low risk | "sealed envelopes" |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information on blinding |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information on blinding |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Missing outcome data balanced in numbers across groups with high dropout (16 in IG, 16 in WG, total of 32.3%); no intention‐to‐treat analysis |
| Selective reporting (reporting bias) | Low risk | No protocol available but no hint of selective reporting |
| Other bias | Low risk | No hint of other bias |
Taso 2014.
| Methods | Randomised controlled trial | |
| Participants | Women with diagnosed stage I‐III breast cancer undergoing adjuvant chemotherapy Recruited from a medical centre Mean age 57.0 years N = 93 |
|
| Interventions | • Anusara yoga (yoga postures, breathing techniques, meditation), 8 weeks, twice weekly for 60 minutes • Wait‐list, usual care for 8 weeks |
|
| Outcomes | Depression (Profile of Mood States) at week 4, week 8 and week 12 Anxiety (Profile of Mood States) at week 4, week 8 and week 12 Fatigue (Brief Fatigue Inventory) at week 4, week 8 and week 12 |
|
| Notes | Unpublished means and standard deviations for the Profile of Mood States were provided by study authors upon request. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Computer‐generated numbers were used to randomly assign…" |
| Allocation concealment (selection bias) | Low risk | "Randomization used opaque envelopes with group assignments, and personnel who had no involvement in the trial performed randomization. The envelopes were opened sequentially in the order of assignment during recruitment, with the names and registration numbers of the participants written on the covers." |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | "this study did not apply an ideal double‐blind approach" |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | "this study did not apply an ideal double‐blind approach" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No attrition |
| Selective reporting (reporting bias) | Low risk | No protocol available but no hint of selective reporting |
| Other bias | Low risk | No hint of other bias |
Vadiraja 2009.
| Methods | Randomised controlled trial | |
| Participants | Women with diagnosed stage II‐III breast cancer undergoing radiotherapy during the study period Recruited from 2 comprehensive cancer care centres Mean age 47.2 years N = 88 |
|
| Interventions | • Integrated yoga programme (yoga postures, breathing techniques, relaxation with imagery, meditation), 6 weeks, 60 minutes at least 3 times a week (18–24 sessions in total) • Brief supportive therapy, 6 weeks, 15 minutes every 10 days (3–4 sessions in total) |
|
| Outcomes | Health‐related quality of life (European Organisation for Research in the Treatment of Cancer ‐ Quality of Life) at week 6
Anxiety (Hospital Anxiety and Depression Scale) at week 6
Depression (Hospital Anxiety and Depression Scale) at week 6 Fatigue (European Organisation for Research in the Treatment of Cancer ‐ Quality of Life) at week 6 Insomnia (European Organisation for Research in the Treatment of Cancer ‐ Quality of Life) at week 6 |
|
| Notes | Duplicate publications separately reported different outcomes of the same trial. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "[...] participants [...] were randomized, via computer‐generated random numbers, to receive yoga (n = 44) or supportive therapy (n = 44) before intervention (prior to radiotherapy)." |
| Allocation concealment (selection bias) | Low risk | "Randomization was performed using opaque envelopes with group assignments. Personnel who had no part in the trial performed randomization. The envelopes were opened sequentially in the order of assignment during recruitment, with the names and registration numbers of the participants written on the covers. The order of randomization was verified with the hospital date of admission records for radiotherapy at study intervals to make sure that field personnel had not altered the sequence of randomization to suit the allocation of consenting participants into 2 study arms." |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | "[...] it was not possible to mask the yoga intervention from the study participants." |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information on blinding of outcome assessment |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 5% dropout in yoga group and 25% dropout in control group |
| Selective reporting (reporting bias) | High risk | No protocol available. Duplicate publications separately reported different outcomes of the same trial. Complete outcome measures were not disclosed. |
| Other bias | Low risk | No hint of other bias |
Vardar Yağlı 2015.
| Methods | Randomised controlled trial | |
| Participants | Women with diagnosed unilateral non‐metastatic breast cancer who had completed treatment at least 3 years before Recruited from a rehabilitation unit Mean age 48.6 years N = 52 |
|
| Interventions | • Yoga (yoga postures, breathing techniques, meditation), 6 weeks, 3 times a week for 60 minutes plus aerobic exercise, 6 weeks, 3 times a week for 60 minutes • Aerobic exercise, 6 weeks, 3 times a week for 60 minutes |
|
| Outcomes | Health‐related quality of life (European Organisation of Research and Treatment of Cancer QLQ‐30) at week 6 Fatigue (Fatigue Severity Scale) at week 6 Insomnia (European Organisation of Research and Treatment of Cancer QLQ‐30) at week 6 |
|
| Notes | Power analysis was performed post hoc according to the primary outcome (6MWT) but revealed that the study had sufficient power (85%) to support our conclusions. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information on random sequence generation |
| Allocation concealment (selection bias) | Low risk | "The randomization procedures were performed by an independent person who selected a random envelope from a box with sealed envelopes." |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information on blinding |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information on blinding |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 25% attrition in yoga group; 21% attrition in control group at end of week 6 |
| Selective reporting (reporting bias) | Low risk | No protocol available but no hint of selective reporting |
| Other bias | Low risk | No hint of other bias |
Wang 2014.
| Methods | Randomised controlled trial | |
| Participants | Women with diagnosed breast cancer after first round of chemotherapy Recruited from a university hospital Mean age not reported N = 100 |
|
| Interventions | • Yoga (yoga postures, relaxation), 4 months, 4 times a week for 50 minutes • Usual care for 4 months |
|
| Outcomes | Fatigue (Cancer Fatigue Scale) at week ? (second, fourth and sixth rounds of chemotherapy) | |
| Notes | Only Abstract in English (Chinese text read by PK) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information on random sequence generation |
| Allocation concealment (selection bias) | High risk | Use of a randomisation table; yoga group and control group were separated into 2 different parts of the hospital |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information on blinding |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information on blinding |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 20% attrition in yoga group, 16% in control group |
| Selective reporting (reporting bias) | Low risk | No protocol available but no hint of selective reporting |
| Other bias | High risk | Cancer Fatigue Scale validated only in Japanese |
6MWD: six‐minute walking distance test. EORTC QLQ‐BR23: European Organisation for Research and Treatment of Cancer core quality of life questionnaire ‐ breast cancer specific. CCOP: Community Clinical Oncology Program. CFS: Cancer Fatigue Scale. EORTC QLQ: European Organisation for Research and Treatment of Cancer core quality of life questionnaire IG: Intervention Group. RY: Restorative Yoga. WG: Waiting Group. WL: Wait List. YG: Yoga Group. YOCAS: Yoga for Cancer Survivors.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Blank 2005 | No primary outcomes assessed |
| Kumar 2013 | No primary outcomes assessed |
| Ojha 2012 | Unclear whether any primary outcomes were assessed |
Characteristics of studies awaiting assessment [ordered by study ID]
Cohen 2015.
| Methods | Randomised controlled trial |
| Participants | Women with diagnosed stage I‐III breast cancer undergoing chemotherapy Mean age 49.5 years N = 249 |
| Interventions | • Tibetan yoga (yoga postures, breathing techniques, meditation), 4‐12 weeks, once weekly or once every 3 weeks for 90 minutes (total of 4 classes) • Stretching, 4‐12 weeks, once weekly or once every 3 weeks for 90 minutes (total of 4 classes) • Usual care |
| Outcomes | Health‐related quality of life (Functional Assessment of Cancer Therapy ‐ Breast Cancer) at week 1, week 12 and week 24 Fatigue (Brief Fatigue Inventory) at week 1, week 12 and week 24 Sleep (Pittsburgh Sleep Quality Index) at week 1, week 12 and week 24 |
| Notes | Published as conference abstract only |
Dominique 2010.
| Methods | Randomised controlled trial |
| Participants | Women with diagnosed stage I‐III breast cancer undergoing chemotherapy Mean age not reported N = 101 |
| Interventions | • Yoga Bali method (yoga postures, breathing techniques, meditation, relaxation), 8 weeks, once weekly for 90 minutes • Wait‐list, 8 weeks |
| Outcomes | Health‐related quality of life (Quality of Life Systemic Inventory) at week ? Depression (Beck Depression Inventory) at week ? |
| Notes | Published as conference abstract only |
Kumari 2015.
| Methods | Randomised controlled trial |
| Participants | Women with diagnosed stage I‐III breast cancer undergoing chemotherapy Mean age not reported N = 207 |
| Interventions | • Yoga (yoga postures, breathing techniques, meditation, relaxation), 6 weeks, 4 times a week • No adjunctive therapy, 6 weeks |
| Outcomes | Health‐related quality of life (European Organisation of Research and Treatment of Cancer QLQ‐30) at weeks 6, 10, 18 and 30 |
| Notes | Published as conference abstract only |
Luu 2014.
| Methods | Randomised controlled trial |
| Participants | Women with diagnosed breast cancer Mean age 51.3 years N = 38 |
| Interventions | • Yoga, 60‐minute classes for 12 weeks • ?, 12 weeks |
| Outcomes | Health‐related quality of life (Functional Assessment of Cancer Therapy ‐ Breast Cancer, Functional Assessment of Chronic Illness Therapy ‐ Spiritual Well‐Being) at week 12 |
| Notes | Published as conference abstract only |
Stan 2013.
| Methods | Randomised controlled trial |
| Participants | Women with diagnosed stage 0‐II breast cancer 4 to 12 months post surgery who experienced fatigue Mean age not reported N = 70 |
| Interventions | • Home‐based DVD‐based yoga • Home‐based strengthening exercises |
| Outcomes | Health‐related quality of life (Functional Assessment of Cancer Therapy ‐ Breast Cancer) at week ? and week 24 Fatigue (Multidimensional Fatigue Symptom Inventory ‐ Short Form) at week ? and week 24 |
| Notes | Published as conference abstracts only |
Differences between protocol and review
In the review, we revised the 'Randomised controlled trial' and 'Human' limit in the Embase search strategy.
For the review, we added the CENTRAL search strategy and used the Embase (via OvidSP) search instead of the previous one, as the group no longer has access to the EMBASE.com platform.
Contributions of authors
Drafting the protocol: HC.
Selecting studies: HC, RL, PK.
Extracting data from studies: SL, PK, HC.
Entering data into RevMan: HC.
Carrying out the analysis: HC.
Interpreting the analysis: HC, RL.
Drafting the final review: HC.
Resolving disagreements: HC, PK, JL, GD.
Updating the review: HC, RL.
Sources of support
Internal sources
Department of Internal and Integrative Medicine, Kliniken Essen‐Mitte, Faculty of Medicine, University of Duisburg‐Essen, Germany.
External sources
Rut‐ and Klaus‐Bahlsen‐Foundation, Germany.
Declarations of interest
HC: none known.
RL: none known.
PK: none known.
SL: none known.
JL: none known.
GD: none known.
New
References
References to studies included in this review
Banasik 2011 {published data only}
- Banasik J, Williams H, Haberman M, Blank SE, Bendel R. Effect of Iyengar yoga practice on fatigue and diurnal salivary cortisol concentration in breast cancer survivors. Journal of the American Academy of Nurse Practitioners 2011;23(3):135‐42. [DOI] [PubMed] [Google Scholar]
Banerjee 2007 {published data only}
- Banerjee B, Vadiraj HS, Ram A, Rao R, Jayapal M, Gopinath KS, et al. Effects of an integrated yoga program in modulating psychological stress and radiation‐induced genotoxic stress in breast cancer patients undergoing radiotherapy. Integrative Cancer Therapies 2007;6(3):242‐50. [DOI] [PubMed] [Google Scholar]
Bernardi 2013 {published data only (unpublished sought but not used)}
- Bernardi MLD, Costa Amorim MH, Zandonade E, Forghieri Santaella D, Assis Novais Barbosa J. The effects of hatha yoga exercises on stress and anxiety levels in mastectomized women. Ciência & Saúde Coletiva 2013;18(12):3621‐32. [DOI] [PubMed] [Google Scholar]
Bower 2012 {published data only}
- Bower JE, Garet D, Ganz PA, Sternlieb B, Irwin M, Olmstead R, et al. Randomized controlled trial of Iyengar yoga for cancer‐related fatigue: results of a targeted intervention for fatigued breast cancer survivors. Psychosomatic Medicine 2011;73(3):A14. [Google Scholar]
- Bower JE, Garet D, Sternlieb B, Ganz PA, Irwin M, Olmstead R, et al. Yoga for persistent fatigue in breast cancer survivors: a randomized controlled trial. Cancer 2012;118(15):3766‐75. [DOI] [PMC free article] [PubMed] [Google Scholar]
Carson 2009 {published data only}
- Carson JW, Carson KM, Porter LS, Keefe FJ, Seewaldt VL. Yoga of Awareness program for menopausal symptoms in breast cancer survivors: results from a randomized trial. Supportive Care in Cancer 2009;17(10):1301‐9. [DOI] [PubMed] [Google Scholar]
Chakrabarty 2015 {published and unpublished data}
- Chakrabarty J, Vidyasagar M, Fernandes D, Joisa G, Varghese P, Mayya S. Effectiveness of pranayama on cancer‐related fatigue in breast cancer patients undergoing radiation therapy: a randomized controlled trial. International Journal of Yoga 2015;8(1):47‐53. [DOI] [PMC free article] [PubMed] [Google Scholar]
Chandwani 2010 {published data only}
- Chandwani KD, Thornton B, Perkins GH, Arun B, Raghuram NV, Nagendra HR, et al. Yoga improves quality of life and benefit finding in women undergoing radiotherapy for breast cancer. Journal of the Society for Integrative Oncology 2010;8(2):43‐55. [PubMed] [Google Scholar]
- Cohen L, Chandwani K, Thornton B, Perkins G. Randomized trial of yoga in women with breast cancer undergoing radiation treatment. Journal of Clinical Oncology 2006;24(18 Suppl):469s. [Google Scholar]
- Cohen L, Chandwani KD, Perkins G, Thornton B, Arun B, Raghuram NV, et al. Randomized trial of yoga in women with breast cancer undergoing radiation treatment: long‐term effects. Journal of Clinical Oncology 2008;26(15 Suppl):9639. [Google Scholar]
Chandwani 2014 {published data only}
- Chandwani KD, Perkins G, Nagendra HR, Raghuram NV, Spelman A, Nagarathna R, et al. Randomized, controlled trial of yoga in women with breast cancer undergoing radiotherapy. Journal of Clinical Oncology 2014;32(10):1058‐65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen L, Chandwani K, Raghuram N, Haddad R, Perkins G, Spelman A, et al. Yoga for women with breast cancer undergoing radiotherapy (XRT): a randomized clinical trial with an active stretching control group. BMC Complementary and Alternative Medicine 2012;12:O38. [Google Scholar]
- Cohen L, Chandwani K, Raghuram NV, Haddad R, Perkins GH, Spelman A, et al. Effect of yoga on QOL, cortisol rhythm, and HRV for women with breast cancer undergoing radiotherapy. Journal of Clinical Oncology 2011;29(15):9009. [Google Scholar]
- Haddad R, Chandwani K, Perkins G, Spelman A, Johnson K, Fortier A, et al. Randomized, controlled trial of yoga for women with breast cancer undergoing radiotherapy. Psychosomatic Medicine 2011;73(3):A119‐20. [Google Scholar]
Cramer 2015 {published data only}
- Cramer H, Rabsilber S, Lauche R, Kummel S, Dobos G. Yoga and meditation for menopausal symptoms in breast cancer survivors ‐ A randomized controlled trial. Cancer 2015;121(13):2175‐84. [DOI] [PubMed] [Google Scholar]
Danhauer 2009 {published data only}
- Danhauer SC, Mihalko SL, Russel GB, Campbell CR, Felder L, Daley K, et al. Restorative yoga for women with breast cancer: finding from a randomized pilot study. 2009 Psycho‐Oncology;18(4):360‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kiecolt‐Glaser 2014 {published data only}
- Kiecolt‐Glaser JK, Bennett JM, Andrigde R, Peng J, Shapiro CL, Malarkey WB, et al. Yoga's impact on inflammation, mood, and fatigue in breast cancer survivors: a randomized controlled trial. Journal of Clinical Oncology 2014;32(10):1040‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kovacic 2013 {published data only}
- Kovacic T, Zagoricnik M, Kovacic M. Impact of relaxation training according to the Yoga In Daily Life system on anxiety after breast cancer surgery. Journal of Complementary & Integrative Medicine 2013;10(1):153‐64. [DOI] [PubMed] [Google Scholar]
Littman 2012 {published data only}
- Littman AJ, Bertram LC, Ceballos R, Ulrich CM, Ramaprasad J, McGregor B, et al. Randomized controlled pilot trial of yoga in overweight and obese breast cancer survivors: effects on quality of life and anthropometric measures. Supportive Care in Cancer 2012;20(2):267‐77. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lötzke 2016 {published data only}
- Lötzke D, Wiedemann F, Rodrigues Recchia D, Ostermann T, Sattler D, Ettl J, et al. Iyengar‐yoga compared to exercise as a therapeutic intervention during (neo)adjuvant therapy in women with stage I‐III breast cancer: health‐related quality of life, mindfulness, spirituality and cancer‐related fatigue. Evidence‐Based Complementary and Alternative Medicine 2016;2016:5931816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiedemann F, Buessing A, Halle M, Kiechle M, Kohls N, Ostermann T, et al. Iyengar yoga compared to exercise in women with stage I‐III breast cancer: feasibility of therapeutic interventions during adjuvant cytotoxic or endocrine therapy. Journal of Clinical Oncology 2013;31(15):e20623. [Google Scholar]
- Wiedemann F, Buessing A, Halle M, Kiechle M, Kohls N, Ostermann T, et al. Yoga compared to exercise as a therapeutic intervention during (neo)adjuvant chemotherapy in women with stage I‐III breast cancer. Cancer Research 2011;71(24 Suppl):OT3‐02‐02. [Google Scholar]
Loudon 2014 {published data only}
- Loudon A, Barnett T, Piller N, Immink MA, Williams AD. Yoga management of breast cancer‐related lymphoedema: a randomised controlled pilot‐trial. BMC Complementary and Alternative Medicine 2014;14:214. [DOI] [PMC free article] [PubMed] [Google Scholar]
Moadel 2007 {published data only}
- Moadel AB, Shah C, Patel S, Wylie‐Rosett J, Siedlecki H, Porcelli T, et al. Randomized controlled trial of yoga for symptom management during breast cancer treatment. Proceedings of the American Society of Clinical Oncology. 2003:726.
- Moadel AB, Shah C, Wylie‐Rosett J, Harris MS, Patel SR, Hall CB, et al. Randomized controlled trial of yoga among a multiethnic sample of breast cancer patients: effects on quality of life. Journal of Clinical Oncology 2007;25(28):4387‐95. [DOI] [PubMed] [Google Scholar]
Mustian 2013 {published and unpublished data}
- Janelsins M, Peppone L, Heckler C, Sprod L, Mohile S, Morrow G, et al. YOCAS® Yoga: improved memory and memory‐mediated improvements in fatigue and quality of life (QOL) in a nationwide phase III RCT. Supportive Care in Cancer 2013;21:S280‐1. [Google Scholar]
- Janelsins MC, Peppone LJ, Heckler CE, Sprod L, Mohile SG, Chandwani KD, et al. YOCAS yoga, fatigue, memory difficulty, and quality of life: results from a URCC CCOP randomized, controlled clinical trial among 358 cancer survivors. Journal of Clinical Oncology 2012;30(15):9142. [Google Scholar]
- Mustian K, Palesh O, Sprod L, Peppone L, Mohile S, Morrow G. YOCAS(registered trademark) yoga significantly improves multidimensional domains of cancer‐related‐fatigue: a URCC CCOP randomized, controlled, clinical trial among 410 cancer survivors. Supportive Care in Cancer 2010b;18:S97‐8. [Google Scholar]
- Mustian KM, Janelsins M, Sprod L, Peppone L, Mohile S, Frizzell B, et al. YOCAS yoga significantly improves circadian rhythm, anxiety, mood and sleep: a randomized, controlled clinical trial among 410 cancer survivors. Supportive Care in Cancer 2011b;1:S317‐8. [Google Scholar]
- Mustian KM, Palesh O, Sprod L, Peppone LJ, Heckler CE, Yates JS, et al. Effect of YOCAS yoga on sleep, fatigue, and quality of life: a URCC CCOP randomized, controlled clinical trial among 410 cancer survivors. Journal of Clinical Oncology 2010a;28(15):9013. [Google Scholar]
- Mustian KM, Sprod L, Peppone LJ, Mohile SG, Janelsins MC, Palesh O, et al. Effect of YOCAS yoga on circadian rhythm, anxiety, and mood: a URCC CCOP randomized, controlled clinical trial among 410 cancer survivors. Journal of Clinical Oncology 2011a;29(15):9034. [Google Scholar]
- Mustian KM, Sprod LK, Janelsins M, Peppone LJ, Palesh OG, Chandwani K, et al. Multicenter, randomized controlled trial of yoga for sleep quality among cancer survivors. Journal of Clinical Oncology 2013;31(26):3233‐41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peppone L, Janelsins MC, Kamen C, Peoples AR, Heckler C, Kirshner JJ, et al. Effect of YOCAS® yoga on fatigue and circadian activity rhythms among breast cancer patients receiving hormone therapy: a URCC CCOP randomized, controlled clinical trial. Supportive Care in Cancer 2013a;21:S291. [Google Scholar]
- Peppone LJ, Janelsins MC, Kamen C, Mohile SG, Sprod LK, Gewandter JS, et al. The effect of YOCAS(R) yoga for musculoskeletal symptoms among breast cancer survivors on hormonal therapy. Breast Cancer Research and Treatment 2015;150(3):597‐604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peppone LJ, Janelsins MC, Peoples AR, Kamen CS, Kirshner JJ, Gaur R, et al. Effect of YOCAS yoga on insomnia and sleep medication usage among breast cancer patients receiving hormone therapy: a URCC CCOP randomized, controlled clinical trial. Journal of Clinical Oncology 2013b;31(15 Suppl):9531. [Google Scholar]
- Peppone LJ, Mohile SG, Janelsins MC, Sprod L, Gewandter JS, Heckler CE, et al. YOCAS yoga for musculoskeletal symptoms in breast cancer patients receiving aromatase inhibitors: a URCC CCOP randomized, controlled clinical trial. Journal of Clinical Oncology 2012b;30(15). [Google Scholar]
- Peppone LJ, Mohile SG, Janelsins MC, Sprod LK, Gewandter JS, Heckler CE, et al. The effect of YOCAS® yoga on aromatase inhibitor‐induced musculoskeletal symptoms in breast cancer patients: a URCC CCOP randomized, controlled clinical trial. Supportive Care in Cancer 2012a;20:S139. [Google Scholar]
Pruthi 2012 {published and unpublished data}
- Pruthi S, Solberg Nes L, Boughey J, Huebner M, Borg B, Jenkins S, et al. A randomized controlled pilot study assessing quality of life, stress and feasibility of yoga practice in women newly diagnosed with breast cancer. BMC Complementary and Alternative Medicine 2012b;12:P231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pruthi S, Stan DL, Jenkins SM, Huebner M, Borg BA, Thomley BS, et al. A randomized controlled pilot study assessing feasibility and impact of yoga practice on quality of life, mood, and perceived stress in women with newly diagnosed breast cancer. Global Advances In Health and Medicine 2012a;1(5):30‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Raghavendra 2007 {published data only}
- Ajaikumar BS, Raghavendra RM, Patil S, Ravi DB, Srinath SB, Gopinath KS, et al. Antidepressant effects of a yoga program in breast cancer patients undergoing conventional treatment: a randomized controlled trial. Journal of Clinical Oncology. 2008; Vol. 26 (Suppl 15):9556.
- Gopinath KS, Rao R, Raghuram N, Rama Rao N, Shirley T, Vinay C, et al. Evaluation of yoga therapy as a psychotherapeutic intervention in breast cancer patients on conventional combined modality of treatment. Prodeedings of American Society of Clinical Oncology. 2003; Vol. 22:26.
- Gopinath SK, Rao RM, Sanjeevarao VH, Diwakar RB, Basavalingaiah AS, Patil S, et al. Effects of an integrated yoga program on mood states, distress, quality of life, diurnal cortisol rhythms and natural killer cell counts in metastatic breast cancer survivors. Cancer Research 2011;71(24 Suppl):P3‐08‐01. [Google Scholar]
- Raghavendra RM, Ajaikumar BS, Vadiraja HS, Patil S, Diwakar RB, Sashidhara P, et al. Role of yoga in modulating fatigue, sleep disturbances, salivary cortisol, and immune measures in breast cancer survivors: a randomized controlled trial. Journal of Clinical Oncology 2010;28(15):9099. [Google Scholar]
- Raghavendra RM, Nagarathna R, Nagendra HR, Gopinath KS, Srinath BS, Ravi BD, et al. Effects of an integrated yoga programme on chemotherapy‐induced nausea and emesis in breast cancer patients. European Journal of Cancer Care 2007;16(6):462‐74. [DOI] [PubMed] [Google Scholar]
- Rao MR, Raghuram N, Nagendra HR, Gopinath KS, Srinath BS, Diwakar RB, et al. Anxiolytic effects of a yoga program in early breast cancer patients undergoing conventional treatment: a randomized controlled trial. Complementary Therapies in Medicine 2009;17(1):1‐8. [DOI] [PubMed] [Google Scholar]
- Rao RM, Nagendra HR, Raghuram N, Vinay C, Chandrashekara S, Gopinath KS, et al. Influence of yoga on mood states, distress, quality of life and immune outcomes in early stage breast cancer patients undergoing surgery. International Journal of Yoga 2008;1(1):11‐20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rao RM, Raghuram HR, Nagendra HR, Usharani MR, Gopinath KS, Diwakar RB, et al. Effects of an integrated yoga program on self‐reported depression scores in breast cancer patients undergoing conventional treatment: a randomized controlled trial. Indian Journal of Palliative Care 2015;21(2):174‐81. [DOI] [PMC free article] [PubMed] [Google Scholar]
Siedentopf 2013 {published data only (unpublished sought but not used)}
- Isabell UB, Maja R. Yoga supports physical and mental well‐being after breast cancer surgery. Abstracts of XVI International Congress of ISPOG ‐ Journal of Psychosomatic Obstetrics and Gynecology. 2010; Vol. 31 (Suppl 1):P63.
- Siedentopf F, Utz‐Billing I, Gairing S, Schoenegg W, Kentenich H, Kollak I. Yoga for patients with early breast cancer and its impact on quality of life ‐ a randomized controlled trial. Geburtshilfe und Frauenheilkunde 2013;73(4):311‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Taso 2014 {published and unpublished data}
- Taso CJ, Lin HS, Lin WL, Chen SM, Huang WT, Chen SW. The effect of yoga exercise on improving depression, anxiety, and fatigue in women with breast cancer: a randomized controlled trial. The Journal of Nursing Research 2014;22(3):155‐64. [DOI] [PubMed] [Google Scholar]
Vadiraja 2009 {published data only}
- Vadiraja HS, Raghavendra RM, Nagarathna R, Nagendra HR, Rekha M, Vanitha N, et al. Effects of a yoga program on cortisol rhythm and mood states in early breast cancer patients undergoing adjuvant radiotherapy: a randomized controlled trial. Integrative Cancer Therapies 2009;8(1):37‐46. [DOI] [PubMed] [Google Scholar]
- Vadiraja HS, Rao MR, Nagarathna R, Nagendra HR, Rekha M, Vanitha N, et al. Effects of yoga program on quality of life and affect in early breast cancer patients undergoing adjuvant radiotherapy: a randomized controlled trial. Complementary Therapies in Medicine 2009;17(5‐6):274‐80. [DOI] [PubMed] [Google Scholar]
- Vadiraja SH, Rao MR, Nagendra RH, Nagarathna R, Rekha M, Vanitha N, et al. Effects of yoga on symptom management in breast cancer patients: a randomized controlled trial. International Journal of Yoga 2009;2(2):73‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Vardar Yağlı 2015 {published data only}
- Vardar Yagli N, Sener G, Afrikan H, Saglam M, Inal Ince D, Savci S, et al. Do yoga and aerobic exercise training have impact on functional capacity, fatigue, peripheral muscle strength, and quality of life in breast cancer survivors?. Integrative Cancer Therpies 2015;14(2):125‐32. [DOI] [PubMed] [Google Scholar]
- Vardar‐Yagli N, Sener G, Afrikan H, Saglam M, Inal‐Ince D, Savci S, et al. Effects of yoga and aerobic exercise training on functional capacity, respiratory muscle strength, and quality of life in breast cancer survivors. European Respiratory Journal. 2013; Vol. 42 (Suppl 57):P1316.
Wang 2014 {published data only}
- Wang G, Wang S, Jiang P, Zeng C. Effect of Yoga on cancer related fatigue in breast cancer patients with chemotherapy. Zhong Nan da Xue Xue Bao 2014;39(10):1077‐82. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Blank 2005 {published data only}
- Blank S, Kittel J, Haberman M. Active practice of Iyengar yoga as an intervention for breast cancer survivors. International Journal of Yoga Therapy 2005;15(1):51‐9. [Google Scholar]
Kumar 2013 {published data only}
- Kumar N, Bhatnagar S, Velpandian T, Patnaik S, Menon G, Mehta M, et al. Randomized controlled trial in advance stage breast cancer patients for the effectiveness on stress marker and pain through Sudarshan Kriya and Pranayam. Indian Journal of Palliative Care 2013;19(3):180‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ojha 2012 {published data only}
- Ohja K, Goyal RK, Sharma S, Sharma S, Yadav N. A case study: investigation of yoga's potential to treat breast cancer survivors facing cancer related fatigue. Journal of Yoga and Physical Therapy 2012;2(5). [Google Scholar]
References to studies awaiting assessment
Cohen 2015 {published data only (unpublished sought but not used)}
- Cohen L, Spelman A, Engle R, Arun B, Harrison C, Perkins G, et al. Three‐arm randomized trial of Tibetan yoga in breast cancer patients. Psychosomatic Medicine 2015;77(3):A70. [Google Scholar]
- Cohen L, Spelman A, Engle R, Arun B, Wei Q, Harrison C, et al. Randomized trial of Tibetan yoga in breast cancer patients undergoing chemotherapy. Journal of Clinical Oncology 2014;32(15 Suppl):9539. [Google Scholar]
Dominique 2010 {published data only (unpublished sought but not used)}
- Dominique L, Gilles D, Annelie A, Madan B, Pierre D, Ginette M. Impact of the Yoga Bali method on quality of life and depressive symptoms among women diagnosed with breast cancer undergoing chemotherapy. Psycho‐Oncology 2010;19:S139‐40. [Google Scholar]
Kumari 2015 {published data only (unpublished sought but not used)}
- Kumari P, Kumari S, Kapoor A, Narayan S, Maharia S, Nirban RK, et al. A phase III open label randomized controlled trial of yoga in women with breast cancer undergoing radiotherapy. Supportive Care in Cancer 2015;1:S356. [Google Scholar]
Luu 2014 {published data only}
- Luu X, Rifkind K, Dhage S, Castaneda M, Zeng X, Joseph KAP. The effects of yoga on urban underserved breast cancer patients. Journal of Clinical Oncology 2014;32(15 Suppl). [Google Scholar]
Stan 2013 {published data only (unpublished sought but not used)}
- Stan D, Croghan K, Croghan I, Jenkins S, Pruthi S. Randomized trial of yoga versus strengthening exercises in breast cancer survivors with persistent fatigue. Supportive Care in Cancer 2015;1:S81‐2. [DOI] [PubMed] [Google Scholar]
- Stan D, Loprinzi CL, Ruddy KJ. Breast cancer survivorship issues. Hematology/Oncology Clinics of North America 2013;27(4):805‐27. [DOI] [PMC free article] [PubMed] [Google Scholar]
Additional references
Abrahams 2016
- Abrahams HJ, Gielissen MF, Schmits IC, Verhagen CA, Rovers MM, Knoop H. Risk factors, prevalence, and course of severe fatigue after breast cancer treatment: a meta‐analysis involving 12 327 breast cancer survivors. Annals of Oncology 2016;27(6):965‐74. [DOI] [PubMed] [Google Scholar]
Andrykowski 2008
- Andrykowski MA, Lykins E, Floyd A. Psychological health in cancer survivors. Seminars in Oncology Nursing 2008;24(3):193‐201. [PUBMED: 18687265] [DOI] [PMC free article] [PubMed] [Google Scholar]
Balshem 2011
- Balshem H, Helfand M, Schünemann HJ, Oxman AD, Kunz R, Brozek J, et al. GRADE guidelines: 3. Rating the quality of evidence. Journal of Clinical Epidemiology 2011;64(4):401‐6. [DOI] [PubMed] [Google Scholar]
Berry 2005
- Berry DA, Cronin KA, Plevritis SK, Fryback DG, Clarke L, Zelen M, et al. Effect of screening and adjuvant therapy on mortality from breast cancer. New England Journal of Medicine 2005;353(17):1784‐92. [PUBMED: 16251534] [DOI] [PubMed] [Google Scholar]
Bower 2006
- Bower JE, Ganz PA, Desmond KA, Bernaards C, Rowland JH, Meyerowitz BE, et al. Fatigue in long‐term breast carcinoma survivors: a longitudinal investigation. Cancer 2006;106(4):751‐8. [PUBMED: 16400678] [DOI] [PubMed] [Google Scholar]
Broad 2012
- Borad WJ. How yoga can wreck your body. The New York Times 5 January 2012.
Brown 2005
- Brown RP, Gerbarg PL. Sudarshan Kriya Yogic breathing in the treatment of stress, anxiety, and depression. Part II ‐ clinical applications and guidelines. Journal of Alternative and Complementary Medicine 2005;11(4):711‐7. [DOI] [PubMed] [Google Scholar]
Brozek 2009
- Brozek JL, Akl EA, Alonso‐Coello P, Lang D, Jaeschke R, Williams JW, et al. Grading quality of evidence and strength of recommendations in clinical practice guidelines. Part 1 of 3. An overview of the GRADE approach and grading quality of evidence about interventions. Allergy 2009;64(5):669‐77. [DOI] [PubMed] [Google Scholar]
Buffart 2012
- Buffart LM, Uffelen JG, Riphagen II, Brug J, Mechelen W, Brown WJ, et al. Physical and psychosocial benefits of yoga in cancer patients and survivors, a systematic review and meta‐analysis of randomized controlled trials. BMC Cancer 2012;12:559. [PUBMED: 23181734] [DOI] [PMC free article] [PubMed] [Google Scholar]
Büssing 2011
- Büssing A, Edelhauser F, Weisskircher A, Fouladbakhsh JM, Heusser P. Inner correspondence and peacefulness with practices among participants in eurythmy therapy and yoga: a validation study. Evidence‐Based Complementary and Alternative Medicine 2011;Article ID 329023. [PUBMED: 20953427] [DOI] [PMC free article] [PubMed] [Google Scholar]
Carroll 2012
- Carroll BJ, Iranmanesh A, Keenan DM, Cassidy F, Wilson WH, Veldhuis JD. Pathophysiology of hypercortisolism in depression: pituitary and adrenal responses to low glucocorticoid feedback. Acta Psychiatrica Scandinavica 2012;125(6):478‐91. [PUBMED: 22211368] [DOI] [PMC free article] [PubMed] [Google Scholar]
Chong 2011
- Chong CS, Tsunaka M, Tsang HW, Chan EP, Cheung WM. Effects of yoga on stress management in healthy adults: a systematic review. Alternative Therapies in Health and Medicine 2011;17(1):32‐8. [PUBMED: 21614942] [PubMed] [Google Scholar]
Cochran 1954
- Cochran WG. The combination of estimates from different experiments. Biometrics 1954;10(1):101‐29. [Google Scholar]
Cohen 1998
- Cohen J. Statistical power analysis for the behavioral sciences. Statistical Power Analysis for the Behavioral Sciences. Hillsdale, NJ: Lawrence Erlbaum Associates, 1998. [Google Scholar]
Compton 2012
- Compton CC, Byrd DR, Garcia‐Aguilar J, Kurtzman SH, Olawaiye A, Washington MK. AJCC Cancer Staging Atlas. A Companion to the Seventh Edition of the AJCC Cancer Staging Manual and Handbook. 2nd Edition. New York: Springer, 2012. [Google Scholar]
Cramer 2012a
- Cramer H, Lange S, Klose P, Paul A, Dobos G. Can yoga improve fatigue in breast cancer patients? A systematic review. Acta Oncologia 2012;51(4):559‐60. [DOI] [PubMed] [Google Scholar]
Cramer 2012b
- Cramer H, Lange S, Klose P, Paul A, Dobos G. Yoga for breast cancer patients and survivors: a systematic review and meta‐analysis. BMC Cancer 2012;12:412. [PUBMED: 22988934] [DOI] [PMC free article] [PubMed] [Google Scholar]
Cramer 2013
- Cramer H, Lauche R, Haller H, Langhorst J, Dobos G, Berger B. "I'm more in balance": a qualitative study of yoga for patients with chronic neck pain. Journal of Alternative and Complementary Medicine 2013;19(6):536‐42. [PUBMED: 23336342] [DOI] [PubMed] [Google Scholar]
Cramer 2016
- Cramer H, Lauche R, Langhorst J, Dobos G. Is one yoga style better than another? A systematic review of associations of yoga style and conclusions in randomized yoga trials. Complementary Therapies in Medicine 2016;25:178‐87. [DOI] [PubMed] [Google Scholar]
Culos‐Reed 2012
- Culos‐Reed SN, Mackenzie MJ, Sohl SJ, Jesse MT, Zahavich AN, Danhauer SC. Yoga & cancer interventions: a review of the clinical significance of patient reported outcomes for cancer survivors. Evidence‐Based Complementary and Alternative Medicine 2012;Article ID 642576. [PUBMED: 23125870] [DOI] [PMC free article] [PubMed] [Google Scholar]
De Michaelis 2005
- Michaelis E. A History of Modern Yoga: Patanjali and Western Esotericism. London, UK: Continuum International Publishing Group, 2005. [Google Scholar]
Desai 2013
- Desai K, Mao JJ, Su I, Demichele A, Li Q, Xie SX, et al. Prevalence and risk factors for insomnia among breast cancer patients on aromatase inhibitors. Supportive Care in Cancer 2013;21(1):43‐51. [DOI] [PMC free article] [PubMed] [Google Scholar]
Devi 1986
- Devi SK, Chansauria JP, Udupa KN. Mental depression and kundalini yoga. Ancient Science of Life 1986;6(2):112‐8. [PUBMED: 22557558] [PMC free article] [PubMed] [Google Scholar]
Ferlay 2013
- Ferlay J, Soerjomataram I, Ervik M, Dikshit R, Eser S, Mathers C, et al. GLOBOCAN 2012 v1.0. Cancer Incidence and Mortality Worldwide: IARC CancerBase No. 11. Lyon, France: International Agency for Research on Cancer, 2013. http://globocan.iarc.fr.
Feuerstein 1998
- Feuerstein G. The Yoga Tradition. Prescott: Hohm Press, 1998. [Google Scholar]
Floyd 2009
- Floyd A, Moyer A. Group vs. individual exercise interventions for women with breast cancer: a meta‐analysis. Health Psychology Review 2009;4(1):22‐41. [PUBMED: 20607139] [DOI] [PMC free article] [PubMed] [Google Scholar]
Fouladbakhsh 2010
- Fouladbakhsh JM, Stommel M. Gender, symptom experience, and use of complementary and alternative medicine practices among cancer survivors in the U.S. cancer population. Oncology Nursing Forum 2010;37(1):E7‐15. [PUBMED: 20044334] [DOI] [PubMed] [Google Scholar]
Garabeli Cavalli Kluthcovsky 2012
- Garabeli Cavalli Kluthcovsky AC, Urbanetz AA, Carvalho DS, Pereira Maluf EM, Schlickmann Sylvestre GC, Bonatto Hatschbach SB. Fatigue after treatment in breast cancer survivors: prevalence, determinants and impact on health‐related quality of life. Supportive Care in Cancer 2012;20(8):1901‐9. [DOI] [PubMed] [Google Scholar]
Guyatt 2008
- Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck‐Ytter Y, Alonso‐Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008;336(7650):924‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Harder 2012
- Harder H, Parlour L, Jenkins V. Randomised controlled trials of yoga interventions for women with breast cancer: a systematic literature review. Supportive Care in Cancer 2012;20(12):3055‐64. [PUBMED: 23052917] [DOI] [PubMed] [Google Scholar]
Hartvig 2006
- Hartvig P, Aulin J, Hugerth M, Wallenberg S, Wagenius G. Fatigue in cancer patients treated with cytotoxic drugs. Journal of Oncology Pharmacy Practice 2006;12(3):155‐64. [PUBMED: 17022870] [DOI] [PubMed] [Google Scholar]
Higgins 2003
- Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analyses. BMJ 2003;327:557‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.1 [updated March 2011]. The Cochrane Collaboration, 2011. www.cochrane‐handbook.org.
Hopwood 2010
- Hopwood P, Sumo G, Mills J, Haviland J, Bliss JM. The course of anxiety and depression over 5 years of follow‐up and risk factors in women with early breast cancer: results from the UK Standardisation of Radiotherapy Trials (START). Breast 2010;19(2):84‐91. [PUBMED: 20042336] [DOI] [PubMed] [Google Scholar]
Ibrahim 2011
- Ibrahim EM, Al‐Homaidh A. Physical activity and survival after breast cancer diagnosis: meta‐analysis of published studies. Medical Oncology 2011;28(3):753‐65. [PUBMED: 20411366] [DOI] [PubMed] [Google Scholar]
Irwin 2009
- Irwin ML, Varma K, Alvarez‐Reeves M, Cadmus L, Wiley A, Chung GG, et al. Randomized controlled trial of aerobic exercise on insulin and insulin‐like growth factors in breast cancer survivors: the Yale exercise and survivorship study. Cancer Epidemiology, Biomarkers & Prevention 2009;18(1):306‐13. [PUBMED: 19124513] [DOI] [PMC free article] [PubMed] [Google Scholar]
Jones 2016
- Jones JM, Olson K, Catton P, Catton CN, Fleshner NE, Krzyzanowska MK, et al. Cancer‐related fatigue and associated disability in post‐treatment cancer survivors. Journal of Cancer Survivorship 2016;10(1):51‐61. [DOI] [PubMed] [Google Scholar]
Kalueff 2007
- Kalueff AV, Nutt DJ. Role of GABA in anxiety and depression. Depression and Anxiety 2007;24(7):495‐517. [PUBMED: 17117412] [DOI] [PubMed] [Google Scholar]
Kim 2009
- Kim CJ, Kang DH, Park JW. A meta‐analysis of aerobic exercise interventions for women with breast cancer. Western Journal of Nursing Research 2009;31(4):437‐61. [PUBMED: 19176403] [DOI] [PubMed] [Google Scholar]
Kjaer 2002
- Kjaer TW, Bertelsen C, Piccini P, Brooks D, Alving J, Lou HC. Increased dopamine tone during meditation‐induced change of consciousness. Brain Research. Cognitive Brain Research 2002;13(2):255‐9. [PUBMED: 11958969] [DOI] [PubMed] [Google Scholar]
Levine 2012
- Levine AS, Balk JL. Yoga and quality‐of‐life improvement in patients with breast cancer: a literature review. International Journal of Yoga Therapy 2012;22:95‐9. [PUBMED: 23070679] [PubMed] [Google Scholar]
Li 2016
- Li J, Humphreys K, Eriksson M, Dar H, Brandberg Y, Hall P, et al. Worse quality of life in young and recently diagnosed breast cancer survivors compared with female survivors of other cancers: a cross‐sectional study. International Journal of Cancer 2016;139(11):2415‐25. [DOI] [PubMed] [Google Scholar]
Lin 2011
- Lin KY, Hu YT, Chang KJ, Lin HF, Tsauo JY. Effects of yoga on psychological health, quality of life, and physical health of patients with cancer: a meta‐analysis. Evidence‐Based Complementary and Alternative Medicine 2011;Article 659876. [PUBMED: 21437197] [DOI] [PMC free article] [PubMed] [Google Scholar]
Maass 2015
- Maass SW, Roorda C, Berendsen AJ, Verhaak PF, Bock GH. The prevalence of long‐term symptoms of depression and anxiety after breast cancer treatment: a systematic review. Maturitas 2015;82(1):100‐8. [DOI] [PubMed] [Google Scholar]
McNeely 2006
- McNeely ML, Campbell KL, Rowe BH, Klassen TP, Mackey JR, Courneya KS. Effects of exercise on breast cancer patients and survivors: a systematic review and meta‐analysis. CMAJ: Canadian Medical Association Journal 2006;175(1):34‐41. [PUBMED: 16818906] [DOI] [PMC free article] [PubMed] [Google Scholar]
Mishra 2012a
- Mishra SI, Scherer RW, Geigle PM, Berlanstein DR, Topaloglu O, Gotay CC, et al. Exercise interventions on health‐related quality of life for cancer survivors. The Cochrane Database of Systematic Reviews 2012, Issue 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mishra 2012b
- Mishra SI, Scherer RW, Snyder C, Geigle PM, Berlanstein DR, Topaloglu O. Exercise interventions on health‐related quality of life for people with cancer during active treatment. The Cochrane Database of Systematic Reviews 2012, Issue 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Moher 2009
- Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta‐Analyses: the PRISMA statement. Annals of Internal Medicine 2009;151(4):1‐7. [DOI] [PubMed] [Google Scholar]
Neilson 2009
- Neilson HK, Friedenreich CM, Brockton NT, Millikan RC. Physical activity and postmenopausal breast cancer: proposed biologic mechanisms and areas for future research. Cancer Epidemiology, Biomarkers & Prevention 2009;18(1):11‐27. [PUBMED: 19124476] [DOI] [PubMed] [Google Scholar]
NIH 2012
- National Institutes of Health. What is complementary and alternative medicine?. http://nccam.nih.gov/health/whatiscam (accessed 1 December 2016) 2012.
Pan 2015
- Pan Y, Yang K, Wang Y, Zhang L, Liang H. Could yoga practice improve treatment‐related side effects and quality of life for women with breast cancer? A systematic review and meta‐analysis. Asia‐Pacific Journal of Clinical Oncology 2015 Jan 6 [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
Patrick 2003
- Patrick DL, Ferketich SL, Frame PS, Harris JJ, Hendricks CB, Levin B, et al. National Institutes of Health state‐of‐the‐science conference statement: symptom management in cancer: pain, depression, and fatigue. Journal of the National Cancer Institute 2003;95(15):1110‐7. [PUBMED: 12902440] [DOI] [PubMed] [Google Scholar]
RevMan [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.1. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2011.
Rottmann 2016
- Rottmann N, Hansen DG, Hagedoorn M, Larsen PV, Nicolaisen A, Bidstrup PE, et al. Depressive symptom trajectories in women affected by breast cancer and their male partners: a nationwide prospective cohort study. Journal of Cancer Survivorship 2016;10(5):915‐26. [DOI] [PubMed] [Google Scholar]
Schmidt 2012
- Schmidt ME, Chang‐Claude J, Vrieling A, Heinz J, Flesch‐Janys D, Steindorf K. Fatigue and quality of life in breast cancer survivors: temporal courses and long‐term pattern. Journal of Cancer Survivorship 2012;6(1):11‐9. [DOI] [PubMed] [Google Scholar]
Schulz 2010
- Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. BMJ (Clinical research ed.) 2010;340:c332. [DOI] [PMC free article] [PubMed] [Google Scholar]
Shannahoff‐Khalsa 2005
- Shannahoff‐Khalsa DS. Patient perspectives: Kundalini yoga meditation techniques for psycho‐oncology and as potential therapies for cancer. Integrative Cancer Therapies 2005;4(1):87‐100. [DOI] [PubMed] [Google Scholar]
Smith 2009
- Smith KB, Pukall CF. An evidence‐based review of yoga as a complementary intervention for patients with cancer. Psycho‐Oncology 2009;18(5):465‐75. [PUBMED: 18821529] [DOI] [PubMed] [Google Scholar]
Stafford 2013
- Stafford L, Judd F, Gibson P, Komiti A, Mann GB, Quinn M. Screening for depression and anxiety in women with breast and gynaecologic cancer: course and prevalence of morbidity over 12 months. Psycho‐Oncology 2013;22(9):2071‐8. [DOI] [PubMed] [Google Scholar]
Streeter 2010
- Streeter CC, Whitfield TH, Owen L, Rein T, Karri SK, Yakhkind A, et al. Effects of yoga versus walking on mood, anxiety, and brain GABA levels: a randomized controlled MRS study. Journal of Alternative and Complementary Medicine 2010;16(11):1145‐52. [PUBMED: 20722471] [DOI] [PMC free article] [PubMed] [Google Scholar]
Streeter 2012
- Streeter CC, Gerbarg PL, Saper RB, Ciraulo DA, Brown RP. Effects of yoga on the autonomic nervous system, gamma‐aminobutyric‐acid, and allostasis in epilepsy, depression, and post‐traumatic stress disorder. Medical Hypotheses 2012;78(5):571‐9. [PUBMED: 22365651] [DOI] [PubMed] [Google Scholar]
Syvälahti 1994
- Syvälahti EK. Biological aspects of depression. Acta Psychiatrica Scandinavica Supplementum 1994;377:11‐5. [PUBMED: 7914394] [DOI] [PubMed] [Google Scholar]
Vadiraja 2009
- Vadiraja SH, Rao MR, Nagendra RH, Nagarathna R, Rekha M, Vanitha N, et al. Effects of yoga on symptom management in breast cancer patients: a randomized controlled trial. International Journal of Yoga 2009;2(2):73‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Van Onselen 2012
- Onselen C, Cooper BA, Lee K, Dunn L, Aouizerat BE, West C, et al. Identification of distinct subgroups of breast cancer patients based on self‐reported changes in sleep disturbance. Supportive Care in Cancer 2012;20(10):2611‐9. [DOI] [PubMed] [Google Scholar]
Vedamurthachar 2006
- Vedamurthachar A, Janakiramaiah N, Hegde JM, Shetty TK, Subbakrishna DK, Sureshbabu SV, et al. Antidepressant efficacy and hormonal effects of Sudarshana Kriya Yoga (SKY) in alcohol dependent individuals. Journal of Affective Disorders 2006;94(1‐3):249‐53. [PUBMED: 16740317] [DOI] [PubMed] [Google Scholar]
Visovsky 2006
- Visovsky C. Muscle strength, body composition, and physical activity in women receiving chemotherapy for breast cancer. Integrative Cancer Therapies 2006;5(3):183‐91. [PUBMED: 16880422] [DOI] [PubMed] [Google Scholar]
Zhang 2012
- Zhang J, Yang KH, Tian JH, Wang CM. Effects of yoga on psychologic function and quality of life in women with breast cancer: a meta‐analysis of randomized controlled trials. Journal of Alternative and Complementary Medicine 2012;18(11):994‐1002. [PUBMED: 22909345] [DOI] [PubMed] [Google Scholar]


