Abstract
Ankle sprains are the most common lower extremity injuries associated with sports activity. Although ligament repair techniques are popular, reconstruction methods using free tendons are considered when the ligament remnant is insufficiently strong, when high-demand athletes sustain repeat ankle sprains, or in revision cases after repair. Recently, some arthroscopic reconstruction techniques have been reported. The distal fibular end is thin; therefore, surgeons must be careful while drilling the fibular tunnel. This report indicates the safe creation method of an anatomical fibular tunnel during anatomical arthroscopic reconstruction of the anterior talofibular ligament and calcaneofibular ligament. This also provides a stronger reconstruction using a 2-strand tendon graft for the anterior talofibular ligament substitute, which is thought to have less risk for postoperative graft failure.
Ankle sprains are the most common lower extremity injuries associated with sports activity.1 The Brostrom technique is the most popular procedure for repairing the ruptured anterior talofibular ligament (ATFL)2; however, postoperative results may be poor when a long time has passed after an ankle sprain, the ATFL remnant is insufficiently strong, and/or a high-demand athlete sustains a repeat ankle sprain. A ligament reconstruction method using a free tendon is believed to provide a better prognosis in such cases.3
There are a few technical reports4, 5, 6, 7, 8 and short-term clinical results9, 10, 11, 12 of the arthroscopic lateral ankle ligament reconstruction. The distal fibular end is thin; hence, surgeons should pay attention to avoid intraoperative fracture of the distal fibula during the tunnel drilling during the arthroscopic ATFL and calcaneofibular ligament (CFL) reconstruction. Moreover, previous technical reports of ATFL and CFL reconstruction use a tendon graft composed of 1-strand ATFL and CFL.4, 5, 6
Here, we describe the technique of an anatomical arthroscopic ATFL and CFL reconstruction using a hamstring tendon graft composed of a 2-strand ATFL and a 1-strand CFL using safe methods of creating a fibular tunnel. A summary of key steps is provided in Table 1; a summary of the technique is provided in Video 1.
Table 1.
Key Surgical Steps, Pearls, and Pitfalls
| Key Surgical Steps | Pearls | Pitfalls |
|---|---|---|
| Patient position | The foot is suspended from the distal edge of the bed. The contralateral leg is slightly lowered to provide a wide working space. | If the foot is not suspended from the distal edge of the bed, it will be difficult to dorsiflex the ankle using the surgeon's belly. |
| Harvest a hamstring tendon | The gracilis tendon is usually enough to create the graft. A semitendinosus tendon is harvested if the gracilis is too thin or too short. The harvested tendon usually needs to be longer than 160 mm. The length is determined by preoperative magnetic resonance imaging. | An extremely short tendon will be difficult to prepare the 2-strand ATFL graft. |
| Creation of the AM portal | The ankle is positioned neutrally. The AM portal is created medial to the anterior tibial tendon, which is slightly displaced laterally by pushing with the thumb. | If the AM portal is created too medially, visualization of the ATFL remnant will be difficult. |
| Creation of the AAL portal | The ankle is dorsiflexed to view the ATFL remnant. Before the AAL portal is created, a needle is inserted into the portal site to confirm accessibility to the ATFL talar footprint. | If the AAL portal is created without confirmation by the needle, the AAL portal position will not be suitable for the talar tunnel creation. |
| Creation of the talar tunnel | A microfracture awl is used to mark the center of the ATFL talar footprint, and a guidewire is inserted through the AAL portal to drill the talus towards the distal end of the medial malleolus. | A guidewire may slip at the ATFL talar footprint without marking. If a guidewire is directed too posteriorly, the neurovascular bundle is at risk for damage. If the tunnel is deeper than 20 mm, the risk for talar penetration may be higher. |
| Creation of the ST portal | The ST portal is created just below the distal end of fibula after confirming accessibility to the fibular footprint by a needle. | If the ST portal is created too anteriorly, the fibular tunnel is directed distally and the risk of tunnel fracture will be higher. |
| Creation of the fibular tunnel | Intraoperative fluoroscopy is used to confirm the guidewire position. | If the fibular tunnel is created without fluoroscopic assistance, the risk for tunnel fracture and tunnel malposition may be higher. |
| Dissection of the CFL remnant | The shaver opening can be safely directed toward the calcaneus during the CFL remnant dissection. | If the shaver opening is directed laterally or distally, the peroneal tendon might be damaged. |
| Creation of the calcaneal tunnel | A 25- to 30-mm-deep calcaneal tunnel is overdrilled through the ST portal. The drill should pass gently near the peroneal tendon. | If the tunnel is drilled through the AAL portal, the drill angle to the calcaneal surface will be too sharp and tunnel wall fracture might occur. |
| Passing pin to the fibular tunnel | A pin is inserted anteriorly from the anterior edge of the tunnel inlet to the posterior and proximal edge to penetrate the posterior cortical wall of the fibula and the skin. | If a pin is inserted parallel to the tunnel, it may not penetrate the skin on the posterior aspect, and a longer passing pin will be necessary. |
| Graft fixation | The ATFL graft should be fixed first. | If the CFL graft is fixed with extremely strong tension before the ATFL graft fixation, anterior drawer stress of the talus may occur and anterior stability will decrease. |
AAL, accessory anterolateral; AM, anteromedial; ATFL, anterior talofibular ligament; CFL, calcaneofibular ligament; ST, subtalar.
Surgical Technique
Step 1: Patient Positioning
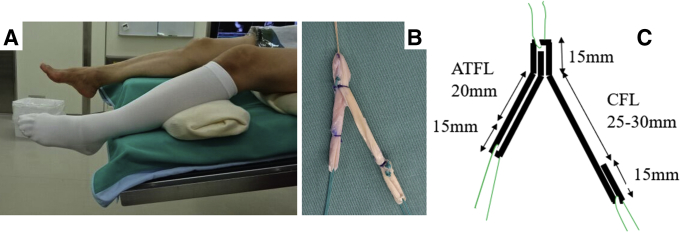
This surgery is performed under general anesthesia with the patient in the supine position. A tourniquet is placed on the proximal thigh. The foot is suspended from the distal edge of the bed. The contralateral leg is slightly lowered to provide a wide working space (Fig 1A).
Fig 1.
Patient position and graft preparation. (A) The right ankle is the operative side. Surgery is performed under general anesthesia with the patient in the supine position. A tourniquet is placed on the proximal thigh and the foot is suspended from the distal edge of the bed. The contralateral leg (left) is slightly lowered to provide a wide working space. (B, C) A gracilis tendon graft is harvested and a reversed Y-shaped graft is prepared. The semitendinosus tendon is used if the gracilis is too thin or too short. It contains 2 strands of an approximately 20-mm-long bundle for the ATFL and 1 strand of 25- to 30-mm-long bundle for the CFL. The length is determined by preoperative magnetic resonance imaging. The 3 ends form a 15-mm-long loop to facilitate attachment of a thread for graft delivery. Parts (A) and (B) are from patients different from the patient in the video case because of photo quality. (ATFL, anterior talofibular ligament; CFL, calcaneofibular ligament.)
Step 2: Graft Preparation
The gracilis tendon is harvested, and a reversed Y-shaped graft is prepared. The semitendinosus tendon is used if the gracilis is too thin or too short. The harvested tendon usually needs to be longer than 160 mm. It contains 2 strands of an approximately 20-mm-long bundle for ATFL and 1 strand of 25- to 30-mm-long bundle for CFL. The length is determined by a preoperative magnetic resonance imaging. The 3 ends form a 15-mm long loop to facilitate the attachment of the thread for graft delivery (Fig 1B and C). If the graft length is longer than 190 mm, the CFL graft can also be prepared as a 2-strand bundle. The recommended graft diameter is 4.5 to 6.0 mm.
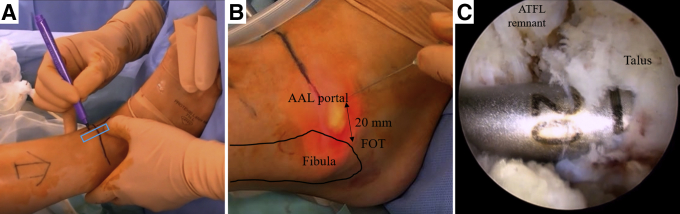
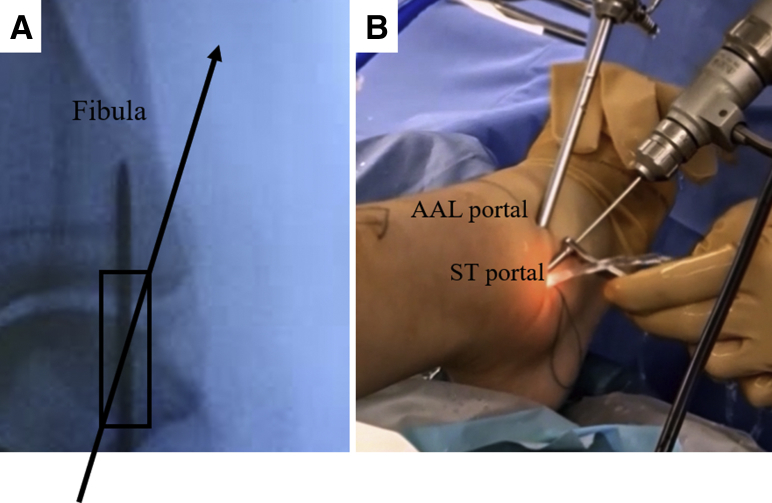
Step 3: Portal Placement of Ankle Arthroscopy
Three portals are created step by step: a conventional anteromedial (AM) portal, an accessory anterolateral (AAL) portal, and a subtalar (ST) portal. The ankle is positioned neutrally. The AM portal is created medial to the anterior tibial tendon, which is slightly displaced laterally by pushing with the thumb (Fig 2A). A 30° 2.7-mm- or 4.0-mm-diameter arthroscope is introduced through the AM portal. The ankle is dorsiflexed to view the ATFL remnant. Before the AAL portal is created, a needle is inserted into the portal site to confirm accessibility to the ATFL talar footprint. The portal is usually created at approximately 20 mm anterior to the anteroinferior tip of the distal fibula, which is called the fibular obscure tip (FOT) (Fig 2B).13 The intra-articular lesions are assessed through these 2 portals.
Fig 2.
Creation of the AM portal, ALL portal, and talar tunnel (right ankle). (A) The right ankle is positioned neutrally. The AM portal is created medial to the anterior tibial tendon (blue box), which is slightly displaced laterally by pushing with the thumb. An arthroscope is introduced through the AM portal. The ankle is dorsiflexed to view the ATFL remnant. (B) Before the AAL portal is created, a needle is inserted into the portal site to confirm accessibility to the ATFL talar footprint. It is usually created at a point approximately 20-mm anterior to the FOT. (C) The ATFL remnant is dissected. A microfracture awl is used to mark the center of the ATFL talar footprint, and a 2.4-mm guidewire is inserted through the AAL portal to drill the talus, from the ATFL footprint toward the distal end of the medial malleolus. The guidewire is then overdrilled, using a drill having the same diameter as the graft end, to create a 20-mm-deep talar tunnel. (AM, anteromedial; AAL, accessory anterolateral; ATFL, anterior talofibular ligament; CFL, calcaneofibular ligament; FOT, fibular obscure tip; ST, subtalar.)
Step 4: Tunnel Creation
The ATFL remnant is dissected. A microfracture awl is used to mark the center of the ATFL talar footprint and a 2.4-mm guidewire is inserted through the AAL portal to drill the talus from the ATFL footprint toward the distal end of the medial malleolus.14 The guidewire is then overdrilled, using a drill having the same diameter as the graft end, to create a 20-mm-deep talar tunnel (Fig 2C).
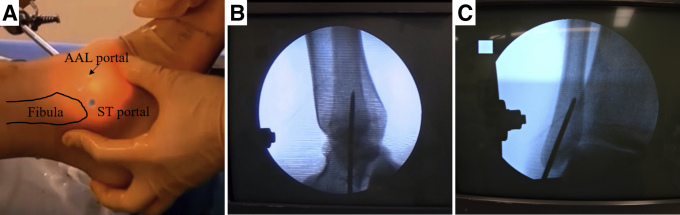
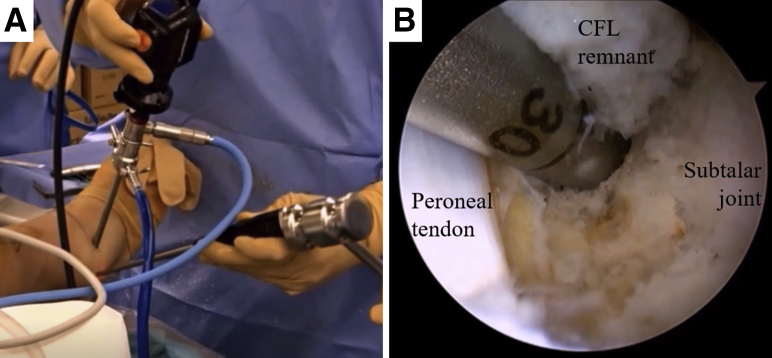
When the ATFL fibular footprint is not adequately viewed through the AM portal, surgeons can try to dorsiflex the ankle, change to the 70° arthroscope, or place the scope through the AAL portal. The ST portal is created just below the distal end of the fibula after confirming accessibility to the fibular footprint by a needle (Fig 3A). A guidewire is inserted through the ST portal. Intraoperative fluoroscopy is used to confirm the guidewire position. The insertion point should be below both of articular tip and the FOT.13 The guidewire is directed nearly along the long axis of the fibula on the lateral view (Fig 3B) and almost on the angle bisector of the fibular end on the anteroposterior view (Fig 3C). Viewed from the AAL portal, the guidewire is then overdrilled to create a 20-mm-deep fibular tunnel. The CFL remnant is debrided by a shaver through the ST portal. The surgeon must pay attention to the peroneal tendons because they run just superficial to the CFL. The shaver opening can be safely directed toward the calcaneus, with the debridement continuing to the lateral wall of the calcaneus. The CFL footprint can be observed. A 25- to 30-mm-deep calcaneal tunnel is overdrilled after the guidewire insertion through the ST portal (Fig 4A and B).
Fig 3.
Creation of the ST portal and the fibular tunnel (the right ankle). (A) The ST portal is created just below the distal end of the fibula after confirming accessibility to the fibular footprint by a needle. A guidewire is inserted through the ST portal. (B) Intraoperative fluoroscopy is used to confirm the guidewire position. Insertion point should be below the FOT. The guidewire is directed nearly along the long axis of the fibula on the lateral view. (C) The guidewire is directed almost on the angle bisector of the fibular end on the anteroposterior view. Viewed from the AAL portal, the guidewire is then overdrilled to create a 20-mm-deep fibular tunnel. (AAL, accessory anterolateral; FOT, fibular obscure tip; ST, subtalar.)
Fig 4.
Creation of the calcaneal tunnel (the right ankle). (A) Viewed from the AAL portal, the CFL remnant is debrided by the shaver through the ST portal. The surgeon must pay attention to the peroneal tendons because they run just superficial to the CFL. The shaver opening can be safely directed toward the calcaneus, with debridement continuing to the lateral wall of the calcaneus. The CFL footprint can be observed. A microfracture awl is used to mark the center of the CFL talar footprint. (B) A 25-to 30-mm-deep calcaneal tunnel for the CFL graft is overdrilled after the guidewire insertion through the ST portal. The ST joint is to the right side of the picture. Peroneal tendon is observed on the left side of the drill. (AAL, accessory anterolateral; CFL, calcaneofibular ligament; ST, subtalar.)
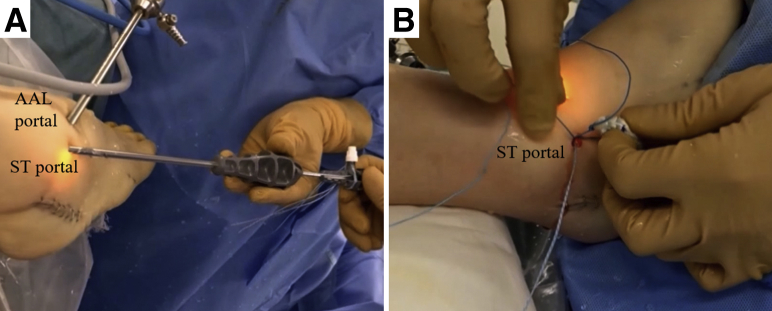
Step 5: Tendon Graft Introduction and Fixation
A 1.6-mm passing pin (Meira, Nagoya, Japan) is inserted into each tunnel. These pins penetrate the bone and skin on the opposite side. When piercing the fibular tunnel, a pin is inserted anteriorly from the anterior edge of the tunnel inlet to the posterior and proximal end to penetrate the posterior cortical wall of the fibula and the skin (Fig 5 A and B). A looped thread is passed through the eye of each passing pin. The passing pins are completely pulled. The looped thread penetrating the talar tunnel needs to be led from the AAL portal to the ST portal. All 3 looped threads are then connected with each graft end; then, the tendon graft is introduced from the ST portal to each tunnel by pulling the looped threads.
Fig 5.
Passing pin direction in the fibular tunnel (the right ankle). (A) A 1.6-mm passing pin is inserted into each tunnel. These pins penetrate the bone and the skin on the opposite side. When piercing the fibular tunnel, a pin is inserted anteriorly from the anterior edge of the tunnel inlet to the posterior and proximal edge to penetrate the posterior cortex wall of the fibula and the skin. A passing pin is passed along the diagonal line (arrow →) of the fibular bone tunnel (box) for graft delivery. (B) Viewed from the AAL portal, a passing pin is inserted to the fibular tunnel through the ST portal using a guide sleeve to protect the skin damage. Part (A) shows a different patient from that of the video case because of photo quality. (AAL, accessory anterolateral; ST, subtalar).
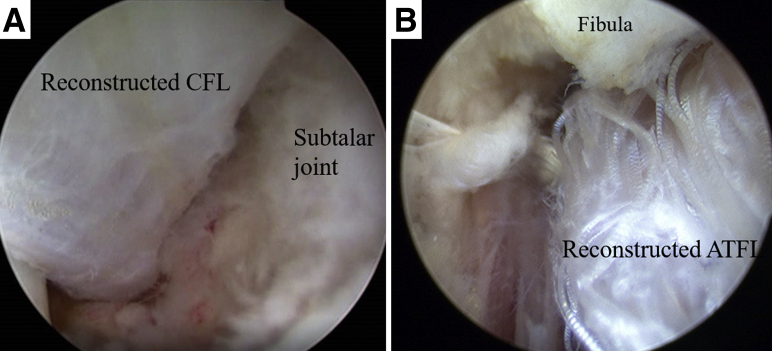
Manual tension is applied on the graft, and each tunneled end of the tendon graft is fixed with a 5- to 6-mm-diameter, 15-mm-long bioabsorbable interference screw, with the ankle in the neutral position (Fig 6). If the CFL graft is fixed with extremely strong tension before the ATFL graft fixation, anterior drawer stress of the talus may occur; therefore, the ATFL graft should be fixed first.
Fig 6.
Graft introduction and fixation (the right ankle). A looped thread is passed to the eye of each passing pin. Passing pins are completely pulled. The looped thread penetrating the talar tunnel needs to be led from the AAL portal to the ST portal. All 3 looped threads are then connected with each graft end; then, the tendon graft is introduced from the ST portal to each tunnel by pulling the looped threads. Each tunneled end of the tendon graft is fixed with a 5- to 6-mm-diameter 15-mm-long bioabsorbable interference screw, with the ankle in the neutral position. (A) Reconstructed CFL and ST joint. (B) Reconstructed ATFL and distal fibula. (AAL, accessory anterolateral; ATFL, anterior talofibular ligament; CFL, calcaneofibular ligament; ST, subtalar.)
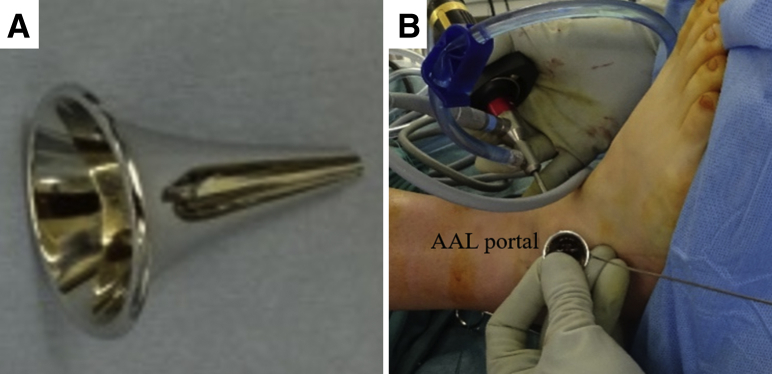
Optional Technique When the Screw Is Not Firmly Fixed
If the screw is not firmly fixed, the screw size is changed to a bigger size or the cancellous bone tips are grafted to the space between the tunnel and tendon graft, using a funnel-shaped device (Fig 7A) and a flat-ended 3-mm Kirschner wire for pushing the bone tips (Fig 7B). The cancellous bone can be harvested from the knee or be prepared from the allograft.
Fig 7.
Optional technique of cancellous bone tip transplantation (right ankle). (A) Funnel-shaped device. (B) If the screw is not firmly fixed, a bigger size screw or cancellous bone tips are grafted to the space between the tunnel and tendon graft using a funnel-shaped device and a flat-ended 3-mm Kirschner wire for pushing bone tips. The cancellous bone can be harvested from the knee or from the allograft. This indicates the transplantation of the bone tips into the talar tunnel through the AAL portal using a funnel-shaped device and a Kirshner wire. Parts (A) and (B) are from different patients than that of the video case because of the optional technique. (AAL, accessory anterolateral.)
Optional Technique for the Graft Fixation in the Fibular Tunnel
When the bone quality is weak, a JuggerKnot Soft Anchor-2.9 mm (Zimmer-Biomet, Warsaw, IN) is placed at the bottom of the fibular tunnel (Fig 8A). One strand is sutured to the fibular end of the graft and the other strand is pulled (Fig 8B); then, the strands are tied. If the patient is an athlete and wants to start rehabilitation as early as possible, both suture anchor and interference screw fixation are used for stronger initial fixation.
Fig 8.
Optional technique for the graft fixation in the fibular tunnel (right ankle). (A) When the bone quality is weak, the JuggerKnot Soft Anchor-2.9 mm is placed at the bottom of the fibular tunnel through the ST portal. (B) One strand is sutured to the fibular end of the tendon graft; the other strand is pulled; then, the strands are tied. If the patient is an athlete and wants to start rehabilitation as early as possible, both suture anchor and interference screw fixation are used for stronger initial fixation. There is another operative scar on the lateral skin of the calcaneus, and the tendon graft is a straight shape for ATFL reconstruction, because the patient in these figures underwent calcaneal osteotomy combined with arthroscopic ATFL reconstruction. (ATFL, anterior talofibular ligament; ST, subtalar.)
Discussion
About 20% to 40% of patients have persistent pain and experience recurrent sprains because of chronic lateral instability of the ankle,15 which eventually requires surgery. The Brostrom technique is the most popular procedure for repairing the ruptured ATFL,2 and recent reports have described arthroscopic repair methods.3, 16, 17, 18, 19 Arthroscopic ligament reconstruction techniques using a graft tendon have also been reported4, 5, 6; these are believed to be stronger than repair techniques but need tunnel creation at the distal fibular end. Surgeons should create a fibular tunnel carefully to avoid intraoperative fracture because the fibular end is thin. To date, however, no technical reports have focused on the safe creation method of the fibular tunnel during arthroscopic ATFL and CFL reconstruction. Because of the connection between the ATFL and CFL,20, 21 1 fibular tunnel is more reasonable and safer than the creation of 2 fibular tunnels.4 When the anatomical fibular tunnel is drilled through the AAL portal, the drill will pass anteroinferiorly to posterosuperiorly; therefore, the risk of the intraoperative fracture of the tunnel wall is greater. The drill should be introduced from the ST portal to direct it along the long axis of the fibula. To create a safer fibular tunnel, we strongly recommend using intraoperative fluoroscopy to confirm guidewire direction before overdrilling.
Intraoperative fluoroscopy is also necessary to confirm the guidewire insertion position for a correct fibular tunnel position because the intersection of the ATFL and CFL is located 2.4 mm (range, 0-6.3 mm) distal to the FOT, which is 1.3 mm (range, 0-5.3 mm) distal from the articular tip of the fibula, which can be observed by an arthroscope.13
In other techniques, the calcaneal tunnel is drilled through the sinus tarsi tunnel5 or the AAL portal;6 however, drilling through the ST portal is less risky for lateral wall fracture of the calcaneum because the ST portal is closer to the CFL footprint. In other words, the drilling direction becomes near perpendicular to the lateral wall of the calcaneus.
The present procedure is also easier for surgeons to get used to because there are only 2 looking portals: the AM portal and the ALL portal. One report needs 4 looking portals,5 which needs a longer learning curve. However, there are only 3 necessary portals in the present technique: the AM, AAL, and ST portals. The risk of superficial peroneal nerve damage near the AL portal can be diminished.
Some articles have described a similar Y-shaped tendon graft that contains single-strand ATFL and single-strand CFL.5, 6, 22 Grafts with larger diameters could cause fewer graft failures23; moreover, the tendon is folded into a 2-strand ATFL graft in the present technique.
We also provided an optional technique of the graft introduction and fixation in the fibular tunnel. Some older patients have weak bone quality and have a relatively high risk of intraoperative fibular fracture during interference screw fixation. Postoperative rehabilitation program should be slower when using only a suture anchor because of its weaker initial fixation strength than that of an interference screw fixation.24, 25 A summary of advantages and disadvantages is provided in Table 2.
Table 2.
Advantages and Disadvantages
| Advantages |
| Safe and reproducible tunnel creation |
| Stronger graft and less risk of ligament rupture recurrence |
| Anatomical reconstruction and less postoperative risk of range of motion restriction |
| Only 2 looking portals and shorter learning curve |
| Smaller operative scar formation |
| Less risk of superficial peroneal nerve damage |
| Optional technique for the graft fixation in the fibular tunnel in patient with lower bone quality |
| Optional technique when the screw is not firmly fixed |
| Disadvantages |
| Possible longer operative time than open technique |
| Possible risk of tunnel fracture |
| Necessary for the basic arthroscopy skill |
| Usage of intraoperative fluoroscopy |
Precise anatomical ligament reconstruction with a stronger tendon graft and safe tunnel creation method should be preferred to restore the normal kinematics of the ankle joint and ST joint, and long-term results will be promising.
Acknowledgment
We would like to thank Editage (www.editage.jp) for English language editing.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Surgical technique for anatomical arthroscopic ATFL and CFL reconstruction using an autogenic hamstring tendon for a safe creation of an anatomical fibular tunnel. This surgery is performed under general anesthesia with the patient in the supine position. A tourniquet is placed on the proximal thigh and the foot is suspended from the distal edge of the bed. The contralateral leg is lowered. The gracilis tendon is harvested and a reversed Y-shaped graft is prepared. The harvested tendon usually needs to be longer than 160 mm. It contains 2 strands of an approximately 20-mm-long bundle for ATFL and 1 strand of 25- to 30-mm-long bundle for CFL. The length is determined by preoperative magnetic resonance imaging. The 3 ends form a 15-mm-long loop to facilitate the attachment of the thread for graft delivery. Three portals are created step by step: a conventional AM, AAL, and ST portals. The ankle is positioned neutrally. The AM portal is created medial to the anterior tibial tendon, which is slightly displaced laterally by pushing with the thumb. A 30° 2.7- or 4.0-mm-diameter arthroscope is introduced through the AM portal. The ankle is dorsiflexed to view the ATFL remnant. Before the AAL portal is created, a needle is inserted into the portal site to confirm accessibility to the ATFL talar footprint. The portal is usually created at approximately 20 mm anterior to the anteroinferior tip of the distal fibula, which is called the FOT. The ATFL remnant is dissected. A microfracture awl is used to mark the center of the ATFL talar footprint, and a 2.4-mm guidewire is inserted through the AAL portal to drill the talus from the ATFL footprint toward the distal end of the medial malleolus. The guidewire is then overdrilled, using a drill having the same diameter as the graft end, to create a 20-mm-deep talar tunnel. The ST portal is created just below the distal end of the fibula after confirming accessibility to the fibular footprint by a needle. A guidewire is inserted through the ST portal. Intraoperative fluoroscopy is used to confirm the guidewire position. Insertion point should be below both of the articular tip and the FOT. The guidewire is directed nearly along the long axis of the fibula on the lateral view and almost on the angle bisector of the fibular end on the anteroposterior view. Viewed from the AAL portal, the guidewire is then overdrilled to create a 20-mm-deep fibular tunnel. The CFL remnant is debrided by a shaver through the ST portal. The surgeon must pay attention to the peroneal tendons. The CFL footprint can be observed in which a 25- to 30-mm-deep calcaneal tunnel is overdrilled after the guidewire insertion through the ST portal. A 1.6-mm passing pin (Meira, Nagoya, Japan) is inserted into each tunnel. These pins penetrate the bone and the skin on the opposite side. When piercing the fibular tunnel, a pin is inserted anteriorly from the anterior edge of the tunnel inlet to the posterior and proximal end to penetrate the posterior cortical wall of the fibula and skin. A looped thread is passed through the eye of each passing pin. The passing pins are completely pulled. The looped thread penetrating the talar tunnel needs to be led from the AAL portal to the ST portal. All 3 looped threads are then connected with each graft end and then the tendon graft is introduced from the ST portal to each tunnel by pulling the looped threads. Manual tension is applied on the graft, and each tunneled end of the tendon graft is fixed with a 5- to 6-mm-diameter 15-mm-long bioabsorbable interference screw, with the ankle in the neutral position. The ATFL graft is fixed first, and the CFL graft is then fixed. If the screw is not firmly fixed, the cancellous bone tips are grafted to the space between the tunnel and tendon graft, using a funnel-shaped device. The cancellous bone can be harvested from the knee or be prepared from the allograft. When the bone quality is weak, a JuggerKnot Soft Anchor-2.9 mm is placed at the bottom of the fibular tunnel. One strand is sutured to the fibular end of the graft and the other strand is pulled; the strands are then tied. (AAL, accessory anterolateral; AM, anteromedial; ATFL, anterior talofibular ligament; CFL, calcaneofibular ligament; FOT, fibular obscure tip; ST, subtalar.)
References
- 1.Miklovic T.M., Donovan L., Protzuk O.A. Acute lateral ankle sprain to chronic ankle instability: A pathway of dysfunction. Phys Sportsmed. 2018;46:116–122. doi: 10.1080/00913847.2018.1409604. [DOI] [PubMed] [Google Scholar]
- 2.Brostrom L. Sprained ankles. VI. Surgical treatment of "chronic" ligament ruptures. Acta Chir Scand. 1966;132:551–565. [PubMed] [Google Scholar]
- 3.Acevedo J.I., Mangone P. Ankle instability and arthroscopic lateral ligament repair. Foot Ankle Clin. 2015;20:59–69. doi: 10.1016/j.fcl.2014.10.002. [DOI] [PubMed] [Google Scholar]
- 4.Lui T.H. Arthroscopic-assisted lateral ligamentous reconstruction in combined ankle and subtalar instability. Arthroscopy. 2007;23:554–555. doi: 10.1016/j.arthro.2006.07.038. [DOI] [PubMed] [Google Scholar]
- 5.Guillo S., Archbold P., Perera A., Bauer T., Sonnery-Cottet B. Arthroscopic anatomic reconstruction of the lateral ligaments of the ankle with gracilis autograft. Arthrosc Tech. 2014;3:e593–e598. doi: 10.1016/j.eats.2014.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Takao M., Glazebrook M., Stone J., Guillo S. Ankle arthroscopic reconstruction of lateral ligaments (Ankle Anti-ROLL) Arthrosc Tech. 2015;4:e595–e600. doi: 10.1016/j.eats.2015.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Higashiyama R. Ankle arthroscopic ligament reconstruction. Jpn J Orthop Surg Tech. 2017;7:77–83. [Google Scholar]
- 8.Higashiyama R. Arthroscopic reconstruction of the posterior talofibular, anterior talofibular, and calcaneofibular ligaments: Scopic PAC. In: Lui T.H., editor. Arthroscopy and Endoscopy of the foot and ankle: Principle & Practice. Springer Singapore; Singapore: 2019. pp. 159–169. [Google Scholar]
- 9.Song B., Li C., Chen N. All-arthroscopic anatomical reconstruction of anterior talofibular ligament using semitendinosus autografts. Inter Orthop. 2017;41:975–982. doi: 10.1007/s00264-017-3410-9. [DOI] [PubMed] [Google Scholar]
- 10.Higashiyama R., Aikawa J., Iwase D. Arthroscopic anterior talofibular ligament reconstruction using a gracilis tendon. Knee Surg Sports Traumatol Arthrosc. 2014;22(suppl):S324–S325. [Google Scholar]
- 11.Higashiyama R., Aikawa J., Iwase D. A case report of arthroscopic ATFL reconstruction using a gracilis tendon. J Jpn Soc Surg Foot. 2014;35:313–316. [Google Scholar]
- 12.Higashiyama R., Aikawa J., Iwase D. Creation of a safe fibular bone tunnel in the anatomical arthroscopic ATFL and CFL reconstruction. J Jpn Orthop Soc Knee Arthrosc Sports Med. 2016;41:1047–1052. [Google Scholar]
- 13.Matsui K., Oliva X.M., Takao M. Bony landmarks available for minimally invasive lateral ankle stabilization surgery: A cadaveric anatomical study. Knee Surg Sports Traumatol Arthrosc. 2017;25:1916–1924. doi: 10.1007/s00167-016-4218-7. [DOI] [PubMed] [Google Scholar]
- 14.Michels F., Guillo S., Vanrietvelde F., Brugman E., Stockmans F. How to drill the talar tunnel in ATFL reconstruction? Knee Surg Sports Traumatol Arthrosc. 2016;24:991–997. doi: 10.1007/s00167-016-4018-0. [DOI] [PubMed] [Google Scholar]
- 15.Gribble P.A., Bleakley C.M., Caulfield B.M. Evidence review for the 2016 International Ankle Consortium consensus statement on the prevalence, impact and long-term consequences of lateral ankle sprains. Br J Sports Med. 2016;50:1496–1505. doi: 10.1136/bjsports-2016-096189. [DOI] [PubMed] [Google Scholar]
- 16.Corte-Real N.M., Moreira R.M. Arthroscopic repair of chronic lateral ankle instability. Foot Ankle Inter. 2009;30:213–217. doi: 10.3113/FAI.2009.0213. [DOI] [PubMed] [Google Scholar]
- 17.Nery C., Raduan F., Del Buono A., Asaumi I.D., Cohen M., Maffulli N. Arthroscopic-assisted Brostrom-Gould for chronic ankle instability: A long-term follow-up. Am J Sports Med. 2011;39:2381–2388. doi: 10.1177/0363546511416069. [DOI] [PubMed] [Google Scholar]
- 18.Matsui K., Burgesson B., Takao M., Stone J., Guillo S., Glazebrook M. Minimally invasive surgical treatment for chronic ankle instability: A systematic review. Knee Surg Sports Traumatol Arthrosc. 2016;24:1040–1048. doi: 10.1007/s00167-016-4041-1. [DOI] [PubMed] [Google Scholar]
- 19.Lui T.H. Modified arthroscopic Brostrom procedure with bone tunnels. Arthrosc Tech. 2016;5:e775–e780. doi: 10.1016/j.eats.2016.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Edama M., Kageyama I., Kikumoto T. Morphological features of the anterior talofibular ligament by the number of fiber bundles. Annals Anat. 2018;216:69–74. doi: 10.1016/j.aanat.2017.11.001. [DOI] [PubMed] [Google Scholar]
- 21.Matsui K., Takao M., Tochigi Y., Ozeki S., Glazebrook M. Anatomy of anterior talofibular ligament and calcaneofibular ligament for minimally invasive surgery: A systematic review. Knee Surg Sports Traumatol Arthrosc. 2017;25:1892–1902. doi: 10.1007/s00167-016-4194-y. [DOI] [PubMed] [Google Scholar]
- 22.Takao M., Oae K., Uchio Y., Ochi M., Yamamoto H. Anatomical reconstruction of the lateral ligaments of the ankle with a gracilis autograft: A new technique using an interference fit anchoring system. Am J Sports Med. 2005;33:814–823. doi: 10.1177/0363546504272688. [DOI] [PubMed] [Google Scholar]
- 23.Spragg L., Chen J., Mirzayan R., Love R., Maletis G. The effect of autologous hamstring graft diameter on the likelihood for revision of anterior cruciate ligament reconstruction. Am J Sports Med. 2016;44:1475–1481. doi: 10.1177/0363546516634011. [DOI] [PubMed] [Google Scholar]
- 24.Waldrop N.E., III, Wijdicks C.A., Jansson K.S., LaPrade R.F., Clanton T.O. Anatomic suture anchor versus the Brostrom technique for anterior talofibular ligament repair: A biomechanical comparison. Am J Sports Med. 2012;40:2590–2596. doi: 10.1177/0363546512458420. [DOI] [PubMed] [Google Scholar]
- 25.Clanton T.O., Viens N.A., Campbell K.J., Laprade R.F., Wijdicks C.A. Anterior talofibular ligament ruptures, part 2: Biomechanical comparison of anterior talofibular ligament reconstruction using semitendinosus allografts with the intact ligament. Am J Sports Med. 2014;42:412–416. doi: 10.1177/0363546513509963. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Surgical technique for anatomical arthroscopic ATFL and CFL reconstruction using an autogenic hamstring tendon for a safe creation of an anatomical fibular tunnel. This surgery is performed under general anesthesia with the patient in the supine position. A tourniquet is placed on the proximal thigh and the foot is suspended from the distal edge of the bed. The contralateral leg is lowered. The gracilis tendon is harvested and a reversed Y-shaped graft is prepared. The harvested tendon usually needs to be longer than 160 mm. It contains 2 strands of an approximately 20-mm-long bundle for ATFL and 1 strand of 25- to 30-mm-long bundle for CFL. The length is determined by preoperative magnetic resonance imaging. The 3 ends form a 15-mm-long loop to facilitate the attachment of the thread for graft delivery. Three portals are created step by step: a conventional AM, AAL, and ST portals. The ankle is positioned neutrally. The AM portal is created medial to the anterior tibial tendon, which is slightly displaced laterally by pushing with the thumb. A 30° 2.7- or 4.0-mm-diameter arthroscope is introduced through the AM portal. The ankle is dorsiflexed to view the ATFL remnant. Before the AAL portal is created, a needle is inserted into the portal site to confirm accessibility to the ATFL talar footprint. The portal is usually created at approximately 20 mm anterior to the anteroinferior tip of the distal fibula, which is called the FOT. The ATFL remnant is dissected. A microfracture awl is used to mark the center of the ATFL talar footprint, and a 2.4-mm guidewire is inserted through the AAL portal to drill the talus from the ATFL footprint toward the distal end of the medial malleolus. The guidewire is then overdrilled, using a drill having the same diameter as the graft end, to create a 20-mm-deep talar tunnel. The ST portal is created just below the distal end of the fibula after confirming accessibility to the fibular footprint by a needle. A guidewire is inserted through the ST portal. Intraoperative fluoroscopy is used to confirm the guidewire position. Insertion point should be below both of the articular tip and the FOT. The guidewire is directed nearly along the long axis of the fibula on the lateral view and almost on the angle bisector of the fibular end on the anteroposterior view. Viewed from the AAL portal, the guidewire is then overdrilled to create a 20-mm-deep fibular tunnel. The CFL remnant is debrided by a shaver through the ST portal. The surgeon must pay attention to the peroneal tendons. The CFL footprint can be observed in which a 25- to 30-mm-deep calcaneal tunnel is overdrilled after the guidewire insertion through the ST portal. A 1.6-mm passing pin (Meira, Nagoya, Japan) is inserted into each tunnel. These pins penetrate the bone and the skin on the opposite side. When piercing the fibular tunnel, a pin is inserted anteriorly from the anterior edge of the tunnel inlet to the posterior and proximal end to penetrate the posterior cortical wall of the fibula and skin. A looped thread is passed through the eye of each passing pin. The passing pins are completely pulled. The looped thread penetrating the talar tunnel needs to be led from the AAL portal to the ST portal. All 3 looped threads are then connected with each graft end and then the tendon graft is introduced from the ST portal to each tunnel by pulling the looped threads. Manual tension is applied on the graft, and each tunneled end of the tendon graft is fixed with a 5- to 6-mm-diameter 15-mm-long bioabsorbable interference screw, with the ankle in the neutral position. The ATFL graft is fixed first, and the CFL graft is then fixed. If the screw is not firmly fixed, the cancellous bone tips are grafted to the space between the tunnel and tendon graft, using a funnel-shaped device. The cancellous bone can be harvested from the knee or be prepared from the allograft. When the bone quality is weak, a JuggerKnot Soft Anchor-2.9 mm is placed at the bottom of the fibular tunnel. One strand is sutured to the fibular end of the graft and the other strand is pulled; the strands are then tied. (AAL, accessory anterolateral; AM, anteromedial; ATFL, anterior talofibular ligament; CFL, calcaneofibular ligament; FOT, fibular obscure tip; ST, subtalar.)