Abstract
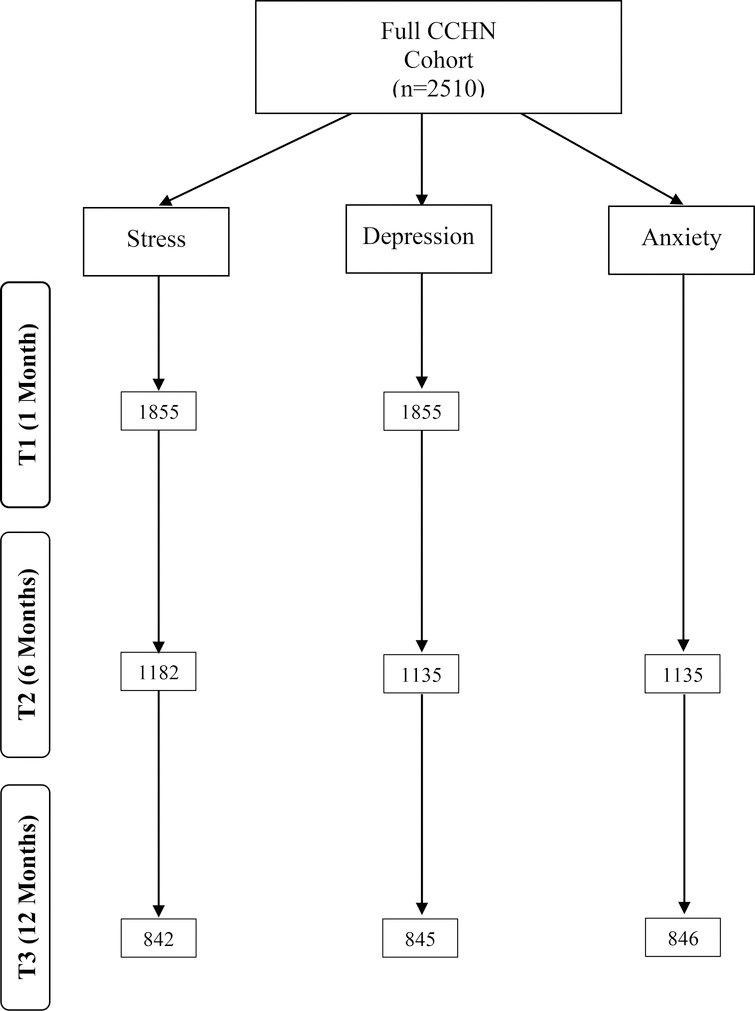
Up to 25% of postpartum women experience psychological distress including stress, depressive, or anxiety symptoms during the postpartum period. The purpose of this study was to explore the extent to which social determinants of health and allostatic load score, a 10-item index of biologic measures of chronic stress, predict psychological distress in low-income pregnant women over the first postpartum year. We conducted a secondary data analysis of the Child Community Health Research Network dataset. The psychological distress outcome variables were perceived stress (n = 842), depression (n = 845), and anxiety (n = 846) symptoms, all measured categorically over the first year postpartum (T1:1 month, T2: 24–29 weeks, T3: 50–65 weeks). Our predictors were social determinants of health (e.g., demographics, maternal hardship, percent poverty level, interpersonal violence, food security) and allostatic load score. Generalized linear mixed models were used to determine which predictors were significantly associated with psychological distress symptoms across the first postpartum year. Interpersonal violence was a statistically significant risk factor for stress, depression, and anxiety symptoms over the first year postpartum. Other significant risk factors included low-income level, nativity, and perceived food security. Receiving food stamps was a significant protective factor for stress symptoms. The significance of risk factors for psychological distress, both modifiable and non-modifiable, can be used as potential targets for further research, screening, and intervention. Future work should explore why and in what conditions these risk factors vary over time.
Keywords: psychological distress, low-income mothers, postpartum depression, anxiety, chronic stress, allostatic load, social determinants of health
During the postpartum period women often experience psychological distress, including elevated stress and depression symptoms (Holditch-Davis et al., 2009; Holditch-Davis et al., 2015). Psychological distress contributes to the development of functional impairments and negative mental health outcomes, including diagnosable psychopathology, such as postpartum depression (O’Hara & Wisner, 2014). In the United States, recent systematic reviews and meta analyses estimate the prevalence of experiencing a depressive episode during pregnancy and the first year postpartum as high as 12.9%, and the estimated prevalence of experiencing anxiety disorders is 8.5% (Gavin et al., 2005; Goodman, Watson, & Stubbs, 2016). More generally, maternal psychological distress, including stress, depression, or anxiety symptoms, occurs in an estimated 25% of postpartum women (Kingston, McDonald, Austin, & Tough, 2015). These psychological distress symptoms often co-occur in the 13.1% of postpartum women experiencing both depressive and anxiety symptomatology (Falah-Hassani, Shiri, & Dennis, 2016).
Elevated levels of psychological distress in postpartum mothers have been linked to adverse outcomes for mothers and children (Holditch-Davis et al., 2015). For example, postpartum depression has been associated with negative effects for child development across the lifespan, including behavioral problems, decreased academic performance, developmental delays, increased risk for developing depression, failure to thrive, insecure-avoidant attachment, and poorer social skills up to adolescence (Hübner-Liebermann, Hausner, & Wittmann, 2012; Marcus et al., 2011; Netsi et al., 2017; Pearson et al., 2013). Maternal anxiety is associated with poor birth outcomes as well as behavioral and emotional maladjustment in children (Sockol, Epperson, & Barber, 2014). The elevated perception of stress during the perinatal period is associated with increased likelihood of preterm birth (Shapiro, Fraser, Frasch, & Séguin, 2013). Furthermore, the lifetime economic consequences, meaning the total cost of health-related quality of life losses, of perinatal anxiety and depression have been estimated in the United Kingdom to be £8500 (approximately $11,844) per woman giving birth (Bauer, Knapp, & Parsonage, 2016).
Low-income women are at high risk to experience psychological distress (Chung, McCollum, Elo, Lee, & Culhane, 2004). The elevated risk of psychological distress has been hypothesized to be due, in part, to exposure to chronic or prolonged stress (Yim, Stapleton, Guardino, Hahn-Holbrook, & Schetter, 2015). Chronic stress, defined as long term exposure when demands exceed resources along with risk factors such as poverty, unsafe living environments, unstable social relationships, or exposure to racism or discrimination, can set a pathway of vulnerability to psychological distress (Lazarus & Folkman, 1984; Schetter & Tanner, 2012; Tanner Stapleton et al., 2016).
Allostatic load theory explores the cumulative effect of stressful environments and contexts on dynamic homeostatic physiologic adaptations associated with the wear and tear of chronic stress on the body (Juster, McEwen, & Lupien, 2010; McEwen & Seeman, 1999). This body of research exploring the negative effect of allostatic load has shown that increased allostatic load score is related to neurobiological and hormonal disruptions that are implicated in the development of psychopathology (Marin et al., 2011). McEwen & Stellar (1993) proposed an allostatic load composite score derived from 10 biological markers measuring neuroendocrine, immune, metabolic, and cardiovascular system health, which included systolic and diastolic blood pressure, waist-hip ratio, total and HDL cholesterol, hemoglobin A1C, urinary cortisol, norephinephrine, and ephineprhine, and dehydroepiandrosterone sulfate (Seeman, Singer, Rowe, Horwitz, & McEwen, 1997). Over time the original measure has been operationalized differently with alternative biological markers selected as indications of neuroendocrine, immune, metabolic and cardiovascular system functioning (Juster et al., 2010). For the current study we utilized a 15-measure allostatic load score including insulin, fibrinogen, albumin, creatinine and pancreatic amylase.
Few studies have applied measures of allostatic load in a racially and ethnically diverse population of postpartum women (Dunkel Schetter et al., 2013; O’Campo et al., 2016). Among low-income postpartum mothers, Latinas and African Americans have significantly higher allostatic load scores as compared to Caucasian mothers, suggesting racial and ethnic differences in biological regulation of chronic stress (O’Campo et al., 2016). In the O’Campo et al.(2016) study, which utilized the Child Community Health Research Network (CCHN) dataset, allostatic load was operationalized from 10 biologic markers including body mass index, high density lipoprotein cholesterol, total cholesterol/high density lipoprotein ratio, pulse, systolic and diastolic blood pressure, waist hip ratio, hemoglobin A1c, C-reactive protein, and salivary cortisol. In previous research allostatic load has been linked to social and environmental factors, which may contribute to its relationship with increased mortality as well as negative physical and mental health outcomes (Beckie, 2012; Marin et al., 2011). For example, cortisol levels contribute to the development of negative physical and mental health outcomes, including the development of depression and anxiety (Hammen, Kim, Eberhart, & Brennan, 2009; Jolley, Elmore, Barnard, & Carr, 2007; Vreeburg et al., 2009). Nursing research utilizing a multi-system approach that includes biological, social and environmental factors has the potential to illuminate the complex factors underlying psychological distress vulnerability. This information can be used to improve public health interventions among vulnerable populations (Beckie, 2012).
In addition to biological vulnerability, it is well-established that socioeconomic disadvantage confers important risk factors for maternal psychological distress. For example, young maternal age, low socioeconomic status, poor social support and/or marital relationship, history of abuse and/or domestic violence, and food insecurity are associated with depression and anxiety in mothers (Beydoun, Beydoun, Kaufman, Lo, & Zonderman, 2012; Biaggi, Conroy, Pawlby, & Pariante, 2016; Chung et al., 2004; Dolbier et al., 2013; Field, 2017; Leung, Epel, Willett, Rimm, & Laraia, 2014; Norhayati, Hazlina, Asrenee, & Emilin, 2015; Sockol et al., 2014; Wu, Chen, & Xu, 2012). Additional risk factors for elevated anxiety symptoms include being employed and having a high level of education (Field, 2017) highlighting the inconsistencies in the field between predictors across individual psychological distress symptoms. Risk factors associated with increased perinatal maternal stress include young age, low-income, low educational attainment, history of sexual abuse, stressful life events in the last month, smoking, alcohol consumption, low social support, preterm birth, and pregnancy with complications (Graignic-Philippe, Dayan, Chokron, Jacquet, & Tordjman, 2014; Roy-Matton, Moutquin, Brown, Carrier, & Bell, 2011).
Current studies typically explore the relationship of risk factors to maternal psychological distress at a single time point (Guintivano, Manuck, & Meltzer-Brody, 2018; J Guintivano et al., 2018). Information on how risk factors relate to change in psychological distress over time is largely unexplored. Hence, there is a lack of consensus as to which factors are most relevant to understand longitudinal changes in prevalence of psychological distress (O’Campo et al., 2016). Additionally, few studies simultaneously explore biological and social determinants of health factors, which include economic stability, education, social and community context, health and healthcare, and neighborhood and built environment (Office of Disease and Health Promotion(Promotion, 2018). The relationship between allostatic load, as a marker of chronic stress, and psychological distress symptoms among low-income postpartum mothers is not well established (O’Campo et al., 2016; Tanner Stapleton et al., 2016). In this study, we address this important limitation in the field of perinatal mental health. Exploring the predictive role of allostatic load, in addition to social determinant factors, on psychological distress is important because allostatic load is one of few comprehensive biological measures of global wear and tear on the body. Such research is of great interest in health care pertaining to both physical and psychological health. This and future studies can inform whether allostatic load should be further tested as a biomarker of perinatal psychological distress as well as be targeted as a biological mechanism related to the stress response in future intervention research. This study has the potential to inform the development of public health nursing interventions aimed at psychosocial factors highly associated with the development of psychological distress symptoms.
The purpose of this study was to explore the extent to which social determinants of health (e.g., maternal hardship, socioeconomic status) and allostatic load score predict stress, depression, and anxiety symptoms among low-income mothers over the first year postpartum.
Method
For this study, we conducted a secondary data analysis of de-identified data from the CCHN study dataset, obtained via the National Institute of Child and Human Development Data and Specimen Hub. The Institutional Review Board of the University of North Carolina at Chapel Hill approved the current study (#17–1518).
The CCHN is a multi-site observational study aimed at exploring how community, family, and individual level stressors may influence and interact with biological factors and their impacts on maternal and child health (Ramey et al., 2015). Recruitment was conducted between 2008 and 2010, from North Carolina, Illinois, Maryland, California, and Washington, D.C. utilizing community-based participatory research methods. In order to study health inequalities, the CCHN investigators oversampled the target population of low-income mothers by purposively sampling in low-income neighborhoods as well as targeting mothers who experienced preterm birth. Women were enrolled in the study if they met the following eligibility criteria: self-identified as Black or African American, Hispanic or Latina, or White, between the ages of 18 and 40, resided for at least 6 months within data collection locations, had three or fewer children, and had no plans for future sterilization after the index birth. Data collection included multiple methods administered at baseline (T0), 1 (T1), 6 (T2), 12 (T3), 18, and 24 months postpartum. Trained community-based research staff conducted interviews through in person home visits. These individuals were also trained to collect biologic data for measures of allostatic load at T2 and T3 including blood pressure, height, weight, waist and hip circumference, blood and saliva samples. Additional data regarding birth and pregnancy outcomes were collected via chart review from the pregnancy-related hospitalization. For further information on the CCHN, refer to: https://www.nichd.nih.gov/research/supported/cchn.
Participants
For this secondary data analysis, demographic data was utilized from the hospital chart review (T0) and the initial in-home interview (T1). Women meeting inclusion criteria were included in a cohort of 2,510 participants who completed T1 (approximately 1 month postpartum), T2 (24- to 29-week postpartum) and T3 (50- to 65-week postpartum) study visits. We did not include later time points because the CCHN did not utilize the same measures of psychological distress after T3. Our study included mothers with full data in all our predictor and outcome measures, resulting in the following sample sizes: stress (n = 842), depression (n = 845), and anxiety (n = 846) (see Figure 1).
Figure 1.
Study flowchart for sample size
Measures
Predictors
Social Determinants of Health:
At T0, a set of demographic risk factors was utilized, including ethnicity, percent poverty level, education, employment, health insurance status, marital status, nativity, and cohabitation. In order to measure public assistance, multiple survey questions were asked, i.e.: “In the past year, have you or any member of your family living with you received any income from the following sources? Temporary Assistance for Needy Families, Temporary Cash Assistance, or welfare cash assistance;” “Food stamps?”. Additionally, perceived food security was measured through the survey question: “In the last 12 months, were you ever hungry but didn’t eat because you couldn’t afford enough food?”.
Interpersonal Violence:
At T0, the Hurt, Insult, Threaten, Scream (HITS) screening tool was used to measure interpersonal violence. This tool utilizes four questions asking how often your partner does the following: “physically hurt you”, “insult or talk down to you”, “threaten you with harm”, and “scream or curse at you”. Each item is scored with a 1–5 Likert scale for the frequency of the behavior, with one being “never” and five being “frequently.” The sum score of the responses ranges from 5 – 25 with higher scores indicating higher interpersonal violence (Sherin, Sinacore, Li, Zitter, & Shakil, 1998). The HITS screening tool has undergone psychometric testing and according to a systematic review Cronbach Alpha is reported as .61-.80 (Rabin, Jennings, Campbell, & Bair-Merritt, 2009). For our data Cronbach Alpha was .87.
Allostatic Load Score:
At T2 and T3, the allostatic load score was derived from a composite measure of 10 biomarkers, including body mass index, high density lipoprotein cholesterol, total cholesterol/high density lipoprotein ratio, pulse, systolic blood pressure, diastolic blood pressure, waist hip ratio, hemoglobin A1c, C-reactive protein, and cortisol (Juster et al., 2010). There is variation in the selection and scoring of the biologic measures selected to create the allostatic load score in previous research studies (Beckie, 2012). Originally the allostatic load score was calculated using cut off values for each of the measures using the top quartile of the sample data (Beckie, 2012; Juster et al., 2010; McEwen, 1998; Seeman et al., 1997). For the CCHN study, the allostatic load score was derived by utilizing clinically relevant cut off points instead of the upper quartile (O’Campo et al., 2016). Specifically, the 10 biomarker measures used for allostatic load in the CCHN data collection were categorized using clinical cut offs as follows: body mass of ≥ 30 kg/m2, high density lipoprotein ≤ 40 mg/dL, total cholesterol/high density lipoprotein ratio ≥ 5.9%, pulse ≥ 100 beats per minute, systolic blood pressure ≥ 125 mmHg, diastolic blood pressure ≥ 80 mmHg, waist hip ratio of ≥ .85, hemoglobin A1C of ≥ 5.4, c-reactive protein of ≥ 3 mg/L, and the top quartile of the sample for diurnal cortisol. A sum score was created based on these 10 clinical cut off values in order to get a final composite allostatic load score. Participants with missing allostatic load data were included if three or fewer values out of the 10 biomarkers were missing, and an average was taken based on the remaining measures to get a final composite allostatic load score (for further details refer to (O’Campo et al., 2016; Ramey et al., 2015). Although the clinical cut off points method of calculating allostatic load deviates from the originally proposed calculation (Beckie, 2012), evidence suggests that there is not a significant difference between this method and the original one based on quartiles (O’Campo et al., 2016). This clinically based score has been used in a previous publication by the CCHN team, which showed that household poverty as well as psychological, economic, neighborhood and medical factors explained the racial and ethnic differences in allostatic load (O’Campo et al., 2016).
Outcomes
Stress Symptoms:
At T1, T2 and T3, the Perceived Stress Scale (PSS) was utilized to measure stress symptoms (Cohen, Kamarck, & Mermelstein, 1983). This scale includes 10 questions assessing the frequency of specific feelings and thoughts over the last month, using a Likert scale of 1 – 5, with one being “never” and five “almost always”. The sum score ranges from 10 – 50 with higher scores indicating more perceived stress. For this analysis, the sum score was dichotomized into low chronic stress (bottom 75% of the distribution) and high chronic stress (top 25% of the distribution). Reliability was calculated using the Cronbach Alpha statistic to assess internal consistency of the PSS items at T1, T2, and T3 with scores of 0.83, 0.85, and 0.76, respectively.
Depressive Symptoms:
At T1, T2 and T3, the Edinburgh Postnatal Depression Scale (EPDS) was utilized to measure depressive symptoms. This scale consists of 10 questions assessing depressed mood for the last seven days. Responses are given on a 0 – 3 Likert scale. The sum of scores ranges from 0 – 30 with higher scores indicating worse depressive symptoms (Cox, Holden, & Sagovsky, 1987). For this analysis, the EPDS was dichotomized into no-to-low (scores ≤ 9) and moderate-to-high (scores ≥ 10) depressive symptoms. Previous studies have shown that EPDS scores of ≥ 10 were clinically significant (Lagerberg, Magnusson, & Sundelin, 2011; Wisner, Parry, & Piontek, 2002). Cronbach Alpha of the EPDS at T1, T2, and T3 were 0.83, 0.82, and 0.83, respectively.
Anxiety Symptoms:
At T2 and T3, the Mini International Neuropsychiatric Interview (MINI) - Anxiety subscale, a clinical interview tool, was utilized to measure anxiety symptoms. This subscale includes six Yes or No questions, asking about anxiety symptoms over the last six months (Hergueta, Baker, & Dunbar, 1998). A sum of the yes responses (1) is calculated to get a score between 0–6. For this analysis, we used the CCHN dichotomization: No Generalized Anxiety Disorder (GAD) (sum score ≤ 2) and probable GAD (score of ≥ 3). Cronbach Alpha statistic of the MINI at T2 and T3 were 0.96 and 0.96, respectively.
Analysis
Descriptive statistics were calculated to determine baseline information about the full cohort in comparison to the subsamples for each outcome: stress, depression, and anxiety. Independent t tests were used to assess group differences. All predictors were collected at baseline or T1 and were considered constant fixed effects within the model, except for allostatic load score which was collected at T2 and T3. For allostatic load score, missing data were entered for T1. The outcome variables of psychological distress included data from all available time points to reflect longitudinal psychological distress symptoms across the first postpartum year (T1, T2, T3 for stress and anxiety and T2 and T3 for anxiety). Generalized linear mixed modeling was utilized to conduct a logistic regression for each psychological distress outcome on each predictor in bivariate models. As the basis for statistical significance, we selected an alpha level of < .05, and thus predictors with this threshold were entered into a multivariate logistic model. Beta estimates, parameter-likelihood odds ratio (OR), 95% confidence intervals (CI) for OR and p-values are reported for the bivariate and multivariate model results.
Results
Our sample derived from the original CCHN cohort (n = 2,510) and consisted of 842, 845 and 846 women in the stress, depression and anxiety outcome subsamples, respectively. The samples utilized for the longitudinal analysis had similar demographic and clinical characteristics as the original cohort (Table 1). Women had a mean age of 25.6 years (standard deviation [SD] = 5.67). Most of the women (53.8%) were self-reported African American, along with 24.2% Hispanic, and 22% Caucasian. The plurality of participants (43%) had an income of < 100% federal poverty level (FPL) and a high school diploma (43.8%). The cohort consisted of 57% unemployed women; 31.6% were non-married; 40.9% were non-cohabitating with the biological father; 53.1% were on Medicaid, and 51.4% expressed that they did not have food security. Regarding interpersonal violence as measured by HITS, the average score was 6.45 (SD = 2.40) out of 25. In terms of allostatic load score, the average scores were 2.62 (SD = 1.95) and 2.58 (SD = 1.97) out of 10 at T2 and T3, respectively. For summary statistics of each individual allostatic load measure see Supplementary Table S1.
Table 1.
Descriptive Statistics for Predictor Variables of Full CCHN Cohort and Stress, Depression, and Anxiety Subsamples
| Full Cohort N = 2510 | Stress N = 842 | Depression N = 845 | Anxiety N = 846 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| % or Mean | Standard Deviation | % or Mean | Standard Deviation | % or Mean | Standard Deviation | % or Mean | Standard Deviation | ||
| Age | 2510 | 25.68 | 5.76 | 25.98 | 5.81 | 25.99 | 5.83 | 26.0 | 5.83 |
| Ethnicity | 2454 | ||||||||
| Caucasian | 540 | 22% | - | 25.3%* | - | 25.2%* | - | 25.2%* | - |
| African American | 1320 | 53.8% | - | 48.2%** | - | 47.9%** | - | 48%** | - |
| Hispanic | 594 | 24.2% | - | 26.5% | - | 26.9% | - | 26.8% | - |
| FPL | 2510 | ||||||||
| <100% | 1079 | 43% | - | 40.4% | - | 40.4% | - | 40.3% | - |
| 100–200% | 688 | 27.4% | - | 27.9% | - | 28.0% | - | 28% | - |
| >200% | 743 | 29.6% | - | 31.7% | - | 31.6% | - | 31.7% | - |
| Maternal Education | 2443 | ||||||||
| <HS | 464 | 19% | - | 17.3% | - | 17.4% | - | 17.4% | - |
| HS | 1070 | 43.8% | - | 43.1% | - | 43.1% | - | 43% | - |
| Some Higher | 557 | 22.8% | - | 21.4% | - | 21.4% | - | 21.4% | - |
| 4 Year College Degree | 352 | 14.4% | - | 18.2%** | - | 18.1%** | - | 18.2%** | - |
| Employment | 2422 | ||||||||
| Unemployed | 1380 | 57% | - | 56.7% | - | 56.7% | - | 56.6% | - |
| Employed | 1042 | 43% | - | 43.3% | - | 43.3% | - | 43.4% | - |
| Marital Status T1 | 2509 | ||||||||
| Married | 1717 | 68.4% | - | 64.6%** | - | 64.4%** | - | 64.5%** | - |
| Non Married | 792 | 31.6% | - | 35.4%** | - | 35.4%** | - | 35.5%** | - |
| Cohabitation T1 | 2406 | ||||||||
| Cohabitating | 1421 | 59.1 % | - | 61.9% | - | 61.8% | - | 61.8% | - |
| Non-Cohabitating | 985 | 40.9% | - | 38.1% | - | 38.2% | - | 38.2% | - |
| Interpersonal Violence (HITS) | 2064 | 6.45 | 2.40 | 6.38 | 2.39 | 6.39 | 2.40 | 6.39 | 2.40 |
| US vs Foreign Born | 2507 | ||||||||
| US Born | 1991 | 79.4% | - | 76.2% | - | 75.9%* | - | 75.9%* | - |
| Foreign Born | 516 | 20.6% | - | 23.8% | - | 24.1%* | - | 24.1%* | - |
| Health Insurance | 2473 | ||||||||
| No Insurance | 115 | 4.7% | - | 5.9% | - | 6% | - | 6% | - |
| Medicaid | 1312 | 53.1% | - | 52.9% | - | 53% | - | 53% | - |
| Private Insurance | 1046 | 42.3% | - | 41.2% | - | 40.9% | - | 41% | - |
| Past Year TANF, TCA, Welfare | 2502 | ||||||||
| yes | 486 | 19.4% | - | 17.7% | - | 17.5% | - | 17.5% | - |
| no | 2016 | 80.6% | - | 82.3% | - | 82.5% | - | 82.5% | - |
| Food Stamps Past Year | 2505 | ||||||||
| yes | 1214 | 48.5% | - | 34.2%** | - | 42.5%** | - | 42.4%** | - |
| no | 1291 | 51.5% | - | 65.8%** | - | 57.5%** | - | 57.6%** | - |
| Public Assistance since 18 | 2506 | ||||||||
| yes | 926 | 37% | - | 34.2% | - | 34.1% | - | 34% | - |
| no | 1580 | 63% | - | 65.8% | - | 65.9% | - | 66% | - |
| Perceived Food Security | 2504 | ||||||||
| yes | 157 | 6.3% | - | 5.8% | - | 5.8% | - | 5.8% | - |
| no | 2347 | 93.7% | - | 94.2% | - | 94.2% | - | 94.2% | - |
| Allostatic Load T2 | 1535 | 2.62 | 1.95 | 2.52 | 1.91 | 2.52 | 1.91 | 2.52 | 1.91 |
| Allostatic Load T3 | 1552 | 2.58 | 1.97 | 2.50 | 1.92 | 2.50 | 1.91 | 2.50 | 1.91 |
Note. CCHN = Child Community Health Research Network; Federal Poverty Level (FPL), High School (HS), United States (US), Temporary Assistance for Needy Families (TANF), Temporary Cash Assistance (TCA), Hurts Insult Threaten Scream (HITS). T-tests were conducted to evaluate mean differences between CCHN cohort and subsamples with significant differences denoted as
p= <0.05
p= <0.01.
We noted differences between the complete CCHN cohort and the stress subsample regarding ethnicity, education, marital status, and food stamp usage. The stress subsample included more Caucasian and college-educated women, fewer married women, and fewer women receiving food stamps. For the depression and anxiety subsamples there were significant differences from the complete cohort in ethnicity, education, marital status, nativity, and food stamp usage. The depression and anxiety subsamples had the same demographic differences as the stress sample, but additionally included more foreign-born women compared to the CCHN total sample (Table 1).
The prevalence of psychological distress symptoms between the original cohort and the longitudinal subsamples was largely similar (Table 2). The prevalence of elevated stress symptoms was 27.7%, 27.4%, and 29.3% from T1 to T3 in the stress subsample. The prevalence of depressive symptoms (EPDS ≥ 10) was 16.2%, 16.4%, 16.4% in the depression subsample. The prevalence of GAD (MINI ≥ 3) was 9% and 7.7% in the anxiety subsample.
Table 2.
Prevalence of Psychological Distress Symptoms over Time in Full CCHN Cohort and Psychological Distress Subsamples
| Psychological Distress1 | Full Cohort T1 | Subsample T1 | Full Cohort T2 | Subsample T2 | Full Cohort T3 | Subsample T3 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | N | % | N | % | |
| Stress Symptoms | ||||||||||||
| PPS < top quartile (low) | 1752 | 72.9% | 609 | 72.3% | 1188 | 71.0% | 611 | 72.6% | 1204 | 69.8% | 595 | 70.7% |
| PSS ≥ top quartile (high) | 651 | 27.1% | 233 | 27.7% | 486 | 29.0% | 231 | 27.4% | 522 | 30.2% | 247 | 29.3% |
| Depressive Symptoms | ||||||||||||
| EPDS ≤ 9 no-to-low | 2028 | 84.3% | 708 | 83.8% | 1409 | 83.6% | 706 | 83.6% | 1449 | 84.0% | 706 | 83.6% |
| EPDS ≥ 10 moderate-to-high | 378 | 15.7% | 137 | 16.2% | 277 | 16.4% | 139 | 16.4% | 227 | 16.0% | 139 | 16.4% |
| Anxiety Symptoms | ||||||||||||
| MINI ≤ 2 no GAD | -- | -- | -- | -- | 1552 | 92.0% | 770 | 91% | 1592 | 92.1% | 781 | 92.3% |
| MINI ≥ probable GAD | -- | -- | -- | -- | 135 | 8.0% | 76 | 9% | 136 | 7.9% | 65 | 7.7% |
Note. CCHN = Child Community Health Research Network; Perceived Stress Score (PSS), Edinburgh Postnatal Depression Scale, Mini International Neuropsychiatric Interview (MINI), Generalized Anxiety Disorder (GAD).
T-tests to evaluate mean differences between full CCHN cohort and subsamples showed no significant difference for psychological distress.
Risk Factors for Stress Symptoms
In the multivariate model (Table 3) the odds of experiencing elevated stress symptoms in women with an income less than 100% the FPL was 1.65 (CI 1.09–2.51, p = .018) that of women with an income greater than 200% FPL. The odds of elevated stress symptoms were 1.18 (CI 1.12–1.25; p < .001) for a one-point increase in the HITS interpersonal violence screening tool. Women who used food stamps showed reduced odds 0.72 (CI: .53-.98, p = .036) of experiencing elevated stress symptoms as compared to women not using food stamp, reflecting a protective factor. Allostatic load score (Odds Ratio [OR]: 1.06, CI: 1.00–1.12, p= 0.070) and the remaining demographic and social determinant of health predictors (e.g. being Hispanic, nativity, and no insurance) were not significantly predictive of elevated stress symptomology and thus were not included in the multivariate model.
Table 3.
Bivariate and Multivariate Logistic Regression Models for Stress Symptoms (n = 842)
| Bivariate Model | Multivariate Model1 | |||||||
|---|---|---|---|---|---|---|---|---|
| Predictors | β | OR | 95% CI | p-value | β | OR | 95% CI | p |
| Age, years | −0.03 | 0.97 | 0.95–0.99 | 0.007 | 0.02 | 1.02 | 0.99–1.05 | 0.160 |
| Ethnicity (Reference Caucasian) | ||||||||
| African American | 0.55 | 1.73 | 1.27–2.36 | 0.001 | 0.24 | 1.27 | 1.09–2.51 | 0.136 |
| Hispanic | 0.27 | 1.31 | 0.92–1.86 | 0.134 | -- | -- | -- | -- |
| %FPL Group (Reference >200%) | ||||||||
| <100% | 0.79 | 2.92 | 1.64–2.94 | <0.001 | 0.50 | 1.65 | 1.09–2.51 | 0.018 |
| 100–200% | 0.39 | 1.40 | 1.02–1.94 | 0.040 | 0.19 | 1.21 | 0.82–1.80 | 0.338 |
| Education (Reference 4-year college degree) | ||||||||
| <HS | 1.02 | 2.77 | 1.81–4.24 | <0.001 | 0.50 | 1.65 | 0.96–2.82 | 0.070 |
| HS | 0.59 | 1.81 | 1.25–2.61 | 0.002 | 0.05 | 1.05 | 0.65–1.69 | 0.851 |
| Some Higher | 0.69 | 2.00 | 1.33–3.02 | 0.001 | 0.27 | 1.29 | 0.78–2.12 | 0.311 |
| Employment (Reference employed) | 0.43 | 1.54 | 1.21–1.97 | 0.001 | 0.14 | 1.16 | 0.88–1.52 | 0.300 |
| Marital Status (Reference married) | 0.55 | 1.73 | 1.34–2.24 | <0.001 | 0.15 | 1.16 | 0.83–1.64 | 0.384 |
| Cohabitation (Reference living together) | 0.47 | 1.59 | 1.25–2.04 | <0.001 | 0.09 | 1.09 | 0.80–1.48 | 0.573 |
| Foreign Born (Reference US Born) | −0.08 | 0.92 | 0.70–1.23 | 0.581 | -- | -- | -- | -- |
| Interpersonal Violence (HITS) | 0.19 | 1.20 | 1.14–1.28 | <0.001 | 0.17 | 1.18 | 1.12–1.25 | <0.001 |
| Health Insurance (Reference private insurance) | ||||||||
| No Insurance | 0.22 | 1.25 | 0.76–2.06 | 0.386 | -- | -- | -- | -- |
| Medicaid | 0.57 | 1.76 | 1.36–2.27 | <0.001 | 0.20 | 1.23 | 0.90–1.68 | 0.203 |
| Past Year TANF, TCA, Welfare (Reference no TANF, TCA, Welfare) | 0.57 | 0.1.77 | 1.31–2.39 | <0.001 | 0.15 | 1.16 | 0.80–1.67 | 0.440 |
| Food Stamps Past Year (Reference no food stamps) | 0.39 | 1.47 | 1.15–1.87 | 0.002 | −0.33 | 0.72 | 0.53–0.98 | 0.036 |
| Public Assistance since 18 (Reference no public assistance) | 0.43 | 1.54 | 1.20–1.97 | 0.001 | −0.01 | 1.00 | 0.72–1.37 | 0.979 |
| Perceived Food Security (Reference perceived food secure) | 0.64 | 1.90 | 1.19–3.02 | 0.007 | 0.41 | 1.51 | 0.95–2.40 | 0.085 |
| Allostatic Load | 0.06 | 1.06 | 1.00–1.12 | 0.070 | -- | -- | -- | -- |
Note. Perceived Stress Score (PSS), Federal Poverty Level (FPL), High School (HS), United States (US), Temporary Assistance for Needy Families (TANF), Temporary Cash Assistance (TCA), Hurts Insult Threaten Scream (HITS).
The multivariate model included all the statistically significant factors from the bivariate models.
Risk Factors for Depressive Symptoms
In the multivariate model (Table 4), regarding nativity, the odds of experiencing elevated depressive symptoms among women who were born outside of the United States was 1.77 (CI 1.13–2.77, p = .013) compared to women who were born in the United States. The odds of elevated depressive symptoms were 1.18 (CI 1.09–1.21, p < .001) for a one-point increase in the HITS screening tool for interpersonal violence. Compared to those women without perceived food insecurity, the odds of elevated depressive symptoms in women with food insecurity were 2.12 (CI: 1.33–3.37, p = .002). Allostatic load score (OR: 0.98, CI: 0.91–1.05, p= 0.563) and the remaining demographic and social determinant of health predictor variables were not significantly predictive of elevated depressive symptomology and thus were not included in the multivariate model.
Table 4.
Bivariate and Multivariate Logistic Regression Models for Depressive Symptoms (n = 845)
| Bivariate Model | Multivariate Model1 | |||||||
|---|---|---|---|---|---|---|---|---|
| Predictors | β | OR | 95% CI | p-value | β | OR | 95% CI | p |
| Age, years | −0.01 | 0.99 | 0.97–1.01 | 0.267 | -- | -- | -- | -- |
| Ethnicity (Reference Caucasian) | ||||||||
| African American | 0.33 | 1.40 | 0.99–1.95 | 0.051 | -- | -- | -- | -- |
| Hispanic | 0.52 | 1.68 | 1.17–2.43 | 0.005 | −0.22 | 0.80 | 0.51–1.27 | 0.346 |
| %FPL Group (Reference >200%) | ||||||||
| <100% | 0.76 | 2.13 | 1.54–2.93 | <0.001 | 0.29 | 1.33 | 0.86–2.06 | 0.194 |
| 100–200% | 0.48 | 1.62 | 1.14–2.31 | 0.007 | 0.08 | 1.08 | 0.70–1.66 | 0.732 |
| Education (Reference 4-year college degree) | ||||||||
| <HS | 1.12 | 3.08 | 1.95–4.87 | <0.001 | 0.47 | 1.60 | 0.91–2.80 | 0.102 |
| HS | 0.63 | 1.87 | 1.24–2.83 | 0.003 | 0.08 | 1.09 | 0.67–1.77 | 0.737 |
| Some Higher | 0.74 | 2.09 | 1.33–3.29 | 0.001 | 0.36 | 1.43 | 0.86–2.37 | 0.166 |
| Employment (Reference employed) | 0.46 | 1.59 | 1.22–2.07 | 0.001 | 0.17 | 1.18 | 0.87–1.60 | 0.280 |
| Marital Status (Reference married) | 0.24 | 1.27 | 0.97–1.68 | 0.088 | -- | -- | -- | -- |
| Cohabitation (Reference living together) | 0.23 | 1.26 | 0.97–1.64 | 0.088 | -- | -- | -- | -- |
| Foreign Born (Reference US Born) | 0.15 | 1.16 | 1.12–1.22 | <0.001 | 0.57 | 1.77 | 1.13–2.77 | 0.013 |
| Interpersonal Violence (HITS) | 0.40 | 1.49 | 1.11–1.99 | 0.007 | 0.14 | 1.18 | 1.09–1.21 | <0.001 |
| Health Insurance (Reference private insurance) | ||||||||
| No Insurance | 0.79 | 2.19 | 1.29–3.74 | 0.004 | 0.34 | 1.41 | 0.75–2.64 | 0.283 |
| Medicaid | 0.61 | 1.85 | 1.40–2.44 | <0.001 | 0.31 | 1.37 | 0.97–1.93 | 0.072 |
| Past Year TANF, TCA, Welfare (Reference no TANF, TCA, Welfare) | 0.31 | 1.36 | 0.98–1.88 | 0.066 | -- | -- | -- | -- |
| Food Stamps Past Year (Reference no food stamps) | 0.35 | 1.42 | 1.09–1.84 | 0.008 | −0.07 | 0.93 | 0.67–1.29 | 0.662 |
| Public Assistance since 18 (Reference no public assistance) | 0.14 | 1.15 | 0.87–1.50 | 0.324 | -- | -- | -- | -- |
| Perceived Food Security (Reference perceived food secure) | 0.95 | 2.59 | 1.60–4.17 | <0.001 | 0.75 | 2.12 | 1.33–3.37 | 0.002 |
| Allostatic Load | −0.02 | 0.98 | 0.91–1.05 | 0.563 | -- | -- | -- | -- |
Note. Perceived Stress Score (PSS), Federal Poverty Level (FPL), High School (HS), United States (US), Temporary Assistance for Needy Families (TANF), Temporary Cash Assistance (TCA), Hurts Insult Threaten Scream (HITS)
The multivariate model included all the statistically significant factors from the bivariate models.
Risk Factors for Anxiety Symptoms
In the multivariate model (Table 5), the odds of experiencing elevated anxiety symptoms were 1.12 (CI 1.06–1.19; p < .001) for a one-point increase in the HITS screen of interpersonal violence. The odds of elevated anxiety symptoms in women with perceived food insecurity was 2.53 (1.43–4.48, p = .001) in relation to food secure women. Allostatic load score (OR: 1.05, CI: 0.97–1.15, p= 0.248) and the remaining demographic and social determinants of health predictor variables were not significantly predictive of elevated anxiety symptomology and thus were not included in the multivariate model.
Table 5.
Bivariate and Multivariate Logistic Regression for Anxiety Symptoms (n = 846)
| Bivariate Model | Multivariate Model | |||||||
|---|---|---|---|---|---|---|---|---|
| Predictors | β | OR | 95% CI | p-value | β | OR | 95% CI | p |
| Age, years | −0.02 | 0.99 | 0.96–1.02 | 0.329 | -- | -- | -- | -- |
| Ethnicity (Reference Caucasian) | ||||||||
| African American | 0.04 | 1.05 | 0.69–1.58 | 0.836 | -- | -- | -- | -- |
| Hispanic | −0.03 | 0.97 | 0.60–1.56 | 0.896 | -- | -- | -- | -- |
| %FPL Group (Reference >200%) | ||||||||
| <100% | 0.57 | 1.76 | 1.17–2.65 | 0.007 | 0.31 | 1.37 | 0.93–2.02 | 0.115 |
| 100–200% | 0.02 | 1.02 | 0.63–1.66 | 0.932 | -- | -- | -- | -- |
| Education (Reference 4-year college degree) | ||||||||
| <HS | 0.52 | 1.68 | 0.94–3.01 | 0.080 | -- | -- | -- | -- |
| HS | 0.25 | 1.29 | 0.77–2.16 | 0.342 | -- | -- | -- | -- |
| Some Higher | 0.40 | 1.50 | 0.85–2.64 | 0.163 | -- | -- | -- | -- |
| Employment (Reference employed) | 0.30 | 1.35 | 0.95–1.91 | 0.096 | -- | -- | -- | -- |
| Marital Status (Reference married) | 0.26 | 1.30 | 0.90–1.87 | 0.166 | -- | -- | -- | -- |
| Cohabitation (Reference living together) | 0.30 | 1.35 | 0.96–1.90 | 0.084 | -- | -- | -- | -- |
| Foreign Born (Reference US Born) | −0.04 | 0.97 | 0.65–1.44 | 0.861 | -- | -- | -- | -- |
| Interpersonal Violence (HITS) | 0.13 | 1.14 | 1.08–1.20 | <0.001 | 0.11 | 1.12 | 1.06–1.19 | <0.001 |
| Health Insurance (Reference private insurance) | ||||||||
| No Insurance | 0.30 | 1.35 | 0.63–2.92 | 0.439 | -- | -- | -- | -- |
| Medicaid | 0.60 | 1.82 | 1.26–2.65 | 0.002 | 0.34 | 1.41 | 0.96–207 | 0.084 |
| Past Year TANF, TCA, Welfare (Reference no TANF, TCA, Welfare) | 0.35 | 1.42 | 0.95–2.14 | 0.091 | -- | -- | -- | -- |
| Food Stamps Past Year (Reference no food stamps) | 0.40 | 1.49 | 1.06–2.08 | 0.022 | −0.08 | 0.93 | 0.62–1.39 | 0.718 |
| Public Assistance since 18 (Reference no public assistance) | 0.28 | 1.33 | 0.94–1.87 | 0.111 | -- | -- | -- | -- |
| Perceived Food Security (Reference perceived food secure) | 1.14 | 3.13 | 1.87–5.24 | <0.001 | 0.93 | 2.53 | 1.43–4.48 | 0.001 |
| Allostatic Load | 0.05 | 1.05 | 0.97–1.15 | 0.248 | -- | -- | -- | -- |
Note. Perceived Stress Score (PSS), Federal Poverty Level (FPL), High School (HS), United States (US), Temporary Assistance for Needy Families (TANF), Temporary Cash Assistance (TCA), Hurts Insult Threaten Scream (HITS)
The multivariate model included all the statistically significant factors from the bivariate models.
Discussion
We set out to explore the extent to which social determinants of health factors and allostatic load score were predictive of elevated stress, depression, and anxiety symptoms over the first year postpartum. The results showed interpersonal violence, food security, poverty level and nativity as significant predictors of elevated psychological distress symptomatology.
Interpersonal violence as measured by the HITS tool was the most consistent predictor of all three psychological distress symptoms over time, with ORs of 1.18, 1.18, 1.12 in stress, depressive, and anxiety symptom models. Our findings add to the large body of knowledge on the link between experiencing interpersonal violence and developing psychological distress symptomatology (Beydoun et al., 2012; Biaggi et al., 2016; Wu et al., 2012). Studies suggest that between 3–9% of women in the general population experience abuse during pregnancy, and this rate goes up to as high as 50% when considering low-income women (Alhusen, Ray, Sharps, & Bullock, 2015). A previous study established that interpersonal violence was associated with an increased risk of stress and depression over the first-year postpartum; however, the study did not explore anxiety as an outcome (Velonis et al., 2017). These results highlight the importance of interventions that address prevention and screening for interpersonal violence in order to reduce its effects on maternal psychological distress and other related poor health outcomes.
Within this study, food security was measured in two ways: (1) as perceived food security, and (2) whether participants had received food stamps in the past 12 months. We found that perceived food insecurity was associated with an increased risk of depressive (OR = 2.12) and anxiety (OR = 2.53) symptomatology. However, receiving food stamps was a significant protective factor for stress symptoms (OR = .72). This is an interesting finding, as it highlights the difference in the effect on psychological distress between perceived food security and receiving food stamps. Those individuals who received food stamps may have been more food secure, with access to such benefits, compared to those not receiving food stamps. Utilizing Supplemental Nutrition Assistance Program (SNAP) services among very low food secure individuals has been shown to decrease the risk of depression compared to non-SNAP recipients (Leung et al., 2014). Another study found that SNAP participation in itself is not associated with maternal depression, but perceptions of the usage of welfare programs moderate the relationship between SNAP programs and maternal depression, finding those with positive perceptions of welfare programs having lower odds of depressive symptoms (Bergmans et al., 2018).
On one hand, taken together, these findings can inform clinical nurses by highlighting the importance of food security as a potential risk factor for psychological distress. On the other hand, these results highlight the increased complexity of food security and psychological distress, and future studies should incorporate more comprehensive measures of food security. For example, the Four-Dimensional Food Insecurity Scale (4D-FIS) was created to measure the complex phenomena of food security; its four dimensions are quantitative (reduction in food intake), qualitative (reduction in dietary quality), psychological (worry), and social (alienation) (Johnson, 2017). Nursing research utilizing more comprehensive measures of food security, such as the 4D-FIS, may provide a more informative context for the phenomenological experience of food insecurity, rather than simple yes or no responses regarding perceived food security and food stamp participation in order reflect the complexity of food insecurity. Public policies designed to expand access to food and nutritional programs may also provide a protective effect on psychological distress in food insecure mothers. Also, programs that aim to address the negative stigma associated with utilizing welfare food and nutritional programs could be expanded to address the relationship between food security and psychological distress. These findings indicate that food and nutritional policies that aim to improve the perception and access of these programs could be tested as interventions among postpartum food insecure mothers to decrease the effect of food insecurity on psychological distress.
Our study also found that having low income (< 100% the FPL) was only associated with an increase in stress symptomology. Previous literature exploring low-income status suggested a strong link between income and stress, depressive, and anxiety symptoms (Chung et al., 2004; Field, 2017; Garfield et al., 2015; Graignic-Philippe et al., 2014; O’Campo et al., 2016). In our study we did not find low-income status to be a significant predictor for elevated depressive symptomology in the full model. This reflects the complex relationship between low-income status and psychological distress.
Additionally, nativity was a significant predictor in developing depressive symptomology. More specifically, being foreign born increasing the risk of developing depressive symptomology (OR = 1.77). This could reflect unique stressors for this population of postpartum mothers including acculturative factors (Sun, Hoyt, Brockberg, Lam, & Tiwari, 2016). However, there is a lack of consensus regarding nativity as a risk factor for psychological distress (Beck, Froman, & Bernal, 2005), where some studies suggest that being foreign born could be a protective factors for negative health outcomes (Ribble, PhD, & Keddie, 2001). Future research should explore the role of acculturation and acculturative stress in this patient population (Ayón, 2015).
Contrary to previous research (Hammen et al., 2009; McEwen & Seeman, 1999; Vreeburg et al., 2009), our study did not find allostatic load score to be a statistically significant predictor for psychological distress. Of the three psychological distress outcomes, allostatic load had the strongest relationship with stress symptoms ([OR]: 1.06, CI: 1.00–1.12, p= 0.070). We note that in our sample the allostatic load score was low, with a mean of 2.62 out of 10 at T2 and 2.58 at T3. The lack of variability in these scores could have affected our ability to observe potential effects in our sample. Furthermore, as we previously mentioned, there is great heterogeneity in operationalization of allostatic load score in the literature, thus direct comparison of scores across studies is problematic because there is no set of established normative scores (Beckie, 2012). Additional research should explore if allostatic load is a potential biological mechanism related to the stress response during the postpartum period in a more heterogeneous sample.
Some limitations need to be taken into consideration while interpreting the results of this study. First, interpersonal violence was measured at only one time point, although research suggests that there is an increased detection in prevalence when there are multiple measurements (Alhusen et al., 2015; Campbell, García-Moreno, & Sharps, 2004). Second, in the CCHN, food security was limited to yes or no responses from participants regarding perceived food security and food stamp utilization. Other comprehensive measures, such as the 4D-FIS, may better inform the phenomenological experience of food insecurity and provide more information in the development of future interventions and policies. Third, the CCHN chose to deviate from the original allostatic load index measurement with clinically relevant cut offs, and further research is needed to explore the strengths and limitations of this approach in establishing an allostatic load score. Lastly, we explored psychological distress outcomes separate from each other, because combined analysis would reduce sample size substantially resulting in inadequate power for analysis. Future studies should consider that psychological distress symptoms are comorbid and explore this aspect in their analysis. There were some differences in the demographics and the selected social determinants of health between the complete CCHN cohort and our final psychological distress outcome subsamples reflecting that they were not completely representative of the whole cohort. However, the CCHN cohort is not an epidemiologically representative sample of the U.S. population and our study was able to investigate the predictors of psychological distress symptomology over the first year postpartum within an ethnically diverse sample of low-income postpartum women.
Our findings have clinical implications related to maternal risk factors for psychological distress over the first year postpartum. These results indicate modifiable risk factors (e.g., interpersonal violence and food security) as potential targets for intervention research to improve a mother’s quality of life and decrease the prevalence of negative mental health outcomes. Few studies utilize a longitudinal design when exploring psychological distress in low-income mothers. This study highlights important risk factors for psychological distress over the first year postpartum. The longitudinal nature of this and future studies can be utilized clinically to inform the timing of important screening measures that aim to prevent the effects of these risk factors on psychological distress symptoms.
Conclusions
Our study is one of the first to explore how various social determinants of health factors and allostatic load score are associated with elevated stress, depression, and anxiety symptoms over time in mothers during the first year postpartum. Interpersonal violence and food security were consistently associated with increased psychological distress symptoms. This information is of great relevance for screening women at risk for psychological distress. A better understanding of these risk factors will likely lead to interventions as well as inform policy that aims to help reduce maternal risk of developing psychological distress and negative mental health outcomes.
Supplementary Material
Acknowledgements:
This article is a product of the Child Community Health Network (CCHN). The CCHN was supported through cooperative agreements with the Eunice Kennedy Shriver National Institute of Child Health and Human Development (U HD44207, U HD44219, U HD44226, U HD44245, U HD44253, U HD54791, U HD54019, U HD44226-05S1, U HD44245–06S1, R03 HD59584) and the National Institute for Nursing Research (U NR008929). We thank the CCHN Primary Investigator (PI) Vernon M. Chinchilli, PhD, and the multiple CCHN site PIs and co-investigators for conducting this study and making it available via the Eunice Kennedy Shriver National Institute of Child Health and Human Development, Data and Specimen Hub. The content is solely the responsibility of the authors and does not represent the official views of the original CCHN investigators or NIH.
Footnotes
Conflict of interest: The authors declare no conflict of interest.
References
- Alhusen JL, Ray E, Sharps P, & Bullock L (2015). Intimate Partner Violence During Pregnancy: Maternal and Neonatal Outcomes. Journal of Women’s Health (15409996), 24(1), 100–106. doi: 10.1089/jwh.2014.4872 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ayón C (2015). Economic, social, and health effects of discrimination on Latino immigrant families. Migration Policy Institute; www.migrationpolicy.org. [Google Scholar]
- Bauer A, Knapp M, & Parsonage M (2016). Lifetime costs of perinatal anxiety and depression. Journal of Affective Disorders, 192, 83–90. doi: 10.1016/j.jad.2015.12.005 [DOI] [PubMed] [Google Scholar]
- Beck CT, Froman RD, & Bernal H (2005). Acculturation level and postpartum depression in Hispanic mothers. MCN: The American Journal of Maternal/Child Nursing, 30(5), 299–304. [DOI] [PubMed] [Google Scholar]
- Beckie TM (2012). A systematic review of allostatic load, health, and health disparities. Biological research for nursing, 14(4), 311–346. [DOI] [PubMed] [Google Scholar]
- Bergmans RS, Berger LM, Palta M, Robert SA, Ehrenthal DB, & Malecki K (2018). Participation in the Supplemental Nutrition Assistance Program and maternal depressive symptoms: Moderation by program perception. Social Science & Medicine, 197, 1–8. doi: 10.1016/j.socscimed.2017.11.039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beydoun HA, Beydoun MA, Kaufman JS, Lo B, & Zonderman AB (2012). Intimate partner violence against adult women and its association with major depressive disorder, depressive symptoms and postpartum depression: a systematic review and meta-analysis. Social science & medicine, 75(6), 959–975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biaggi A, Conroy S, Pawlby S, & Pariante CM (2016). Identifying the women at risk of antenatal anxiety and depression: A systematic review. Journal of Affective Disorders, 191, 62–77. doi: 10.1016/j.jad.2015.11.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell J, García-Moreno C, & Sharps P (2004). Abuse during pregnancy in industrialized and developing countries. Violence Against Women, 10(7), 770–789. doi: 10.1177/1077801204265551 [DOI] [Google Scholar]
- Chung EK, McCollum KF, Elo IT, Lee HJ, & Culhane JF (2004). Maternal depressive symptoms and infant health practices among low-income women. Pediatrics, 113(6), e523–e529. [DOI] [PubMed] [Google Scholar]
- Cohen S, Kamarck T, & Mermelstein R (1983). A global measure of perceived stress. Journal of health and social behavior, 385–396. [PubMed] [Google Scholar]
- Cox JL, Holden JM, & Sagovsky R (1987). Detection of postnatal depression: development of the 10-item Edinburgh Postnatal Depression Scale. The British journal of psychiatry, 150(6), 782–786. [DOI] [PubMed] [Google Scholar]
- Dolbier CL, Rush TE, Sahadeo LS, Shaffer ML, Thorp J, & Investigators CCHN (2013). Relationships of race and socioeconomic status to postpartum depressive symptoms in rural African American and non-Hispanic white women. Maternal and child health journal, 17(7), 1277–1287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunkel Schetter C, Schafer P, Lanzi RG, Clark-Kauffman E, Raju TN, Hillemeier MM, & Network CCH (2013). Shedding light on the mechanisms underlying health disparities through community participatory methods: The stress pathway. Perspectives on Psychological Science, 8(6), 613–633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Falah-Hassani K, Shiri R, & Dennis C-L (2016). Prevalence and risk factors for comorbid postpartum depressive symptomatology and anxiety. Journal of affective disorders, 198, 142–147. [DOI] [PubMed] [Google Scholar]
- Field T (2017). Postpartum anxiety prevalence, predictors and effects on child development: A Review. Journal of Psychiatry and Psychiatric Disorders, 1(2), 86–102. [Google Scholar]
- Garfield L, Holditch-Davis D, Carter CS, McFarlin BL, Schwertz D, Seng JS, . . . White-Traut R. (2015). Risk factors for Postpartum Depressive Symptoms in Low-Income Women with Very Low Birth Weight Infants. Advances in neonatal care: official journal of the National Association of Neonatal Nurses, 15(1), E3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gavin NI, Gaynes BN, Lohr KN, Meltzer-Brody S, Gartlehner G, & Swinson T (2005). Perinatal depression: a systematic review of prevalence and incidence. Obstetrics & Gynecology, 106(5), 1071–1083. [DOI] [PubMed] [Google Scholar]
- Goodman JH, Watson GR, & Stubbs B (2016). Anxiety disorders in postpartum women: a systematic review and meta-analysis. Journal of Affective Disorders, 203, 292–331. [DOI] [PubMed] [Google Scholar]
- Graignic-Philippe R, Dayan J, Chokron S, Jacquet A, & Tordjman S (2014). Effects of prenatal stress on fetal and child development: a critical literature review. Neuroscience & biobehavioral reviews, 43, 137–162. [DOI] [PubMed] [Google Scholar]
- Guintivano J, Manuck T, & Meltzer-Brody S (2018). Predictors of Postpartum Depression: A Comprehensive Review of the Last Decade of Evidence. Clinical obstetrics and gynecology. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guintivano J, Sullivan P, Stuebe A, Penders T, Thorp J, Rubinow D, & Meltzer-Brody S (2018). Adverse life events, psychiatric history, and biological predictors of postpartum depression in an ethnically diverse sample of postpartum women. Psychological medicine, 48(7), 1190–1200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammen C, Kim EY, Eberhart NK, & Brennan PA (2009). Chronic and acute stress and the prediction of major depression in women. Depression and anxiety, 26(8), 718–723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hergueta T, Baker R, & Dunbar GC (1998). The Mini-International Neuropsychiatric Interview (MINI): the development and validation of a structured diagnostic psychiatric interview for DSM-IVand ICD-10. J clin psychiatry, 59(Suppl 20), 2233. [PubMed] [Google Scholar]
- Holditch-Davis D, Miles MS, Weaver MA, Black B, Beeber L, Thoyre S, & Engelke S (2009). Patterns of distress in African American mothers of preterm infants. Journal of developmental and behavioral pediatrics: JDBP, 30(3), 193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holditch-Davis D, Santos H, Levy J, White-Traut R, O’Shea TM, Geraldo V, & David R (2015). Patterns of psychological distress in mothers of preterm infants. Infant Behavior and Development, 41, 154–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hübner-Liebermann B, Hausner H, & Wittmann M (2012). Recognizing and treating peripartum depression. Deutsches Ärzteblatt International, 109(24), 419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson C (2017). Understanding how severity of food insecurity relates to dietary and health outcomes in women (PhD), University of North Carolina at Chapel Hill; Chapel Hill: Retrieved from https://cdr.lib.unc.edu/record/uuid:dc97c02c-0f77-4440-8108-c078beb036a5 [Google Scholar]
- Jolley SN, Elmore S, Barnard KE, & Carr DB (2007). Dysregulation of the hypothalamic-pituitary-adrenal axis in postpartum depression. Biological research for nursing, 8(3), 210–222. [DOI] [PubMed] [Google Scholar]
- Juster R-P, McEwen BS, & Lupien SJ (2010). Allostatic load biomarkers of chronic stress and impact on health and cognition. Neuroscience & Biobehavioral Reviews, 35(1), 2–16. [DOI] [PubMed] [Google Scholar]
- Kingston D, McDonald S, Austin M-P, & Tough S (2015). Association between prenatal and postnatal psychological distress and toddler cognitive development: a systematic review. PLoS One, 10(5), e0126929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lagerberg D, Magnusson M, & Sundelin C (2011). Drawing the line in the Edinburgh Postnatal Depression Scale (EPDS): a vital decision. International journal of adolescent medicine and health, 23(1). [DOI] [PubMed] [Google Scholar]
- Lazarus RS, & Folkman S (1984). Coping and adaptation. The handbook of behavioral medicine, 282325. [Google Scholar]
- Leung CW, Epel ES, Willett WC, Rimm EB, & Laraia BA (2014). Household Food Insecurity Is Positively Associated with Depression among Low-Income Supplemental Nutrition Assistance Program Participants and Income-Eligible Nonparticipants1–3. The Journal of nutrition, 145(3), 622–627. [DOI] [PubMed] [Google Scholar]
- Marcus S, Lopez JF, McDonough S, MacKenzie MJ, Flynn H, Neal CR Jr, . . . Vazquez DM (2011). Depressive symptoms during pregnancy: impact on neuroendocrine and neonatal outcomes. Infant Behavior and Development, 34(1), 26–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marin M-F, Lord C, Andrews J, Juster R-P, Sindi S, Arsenault-Lapierre G, . . . Lupien SJ (2011). Chronic stress, cognitive functioning and mental health. Neurobiology of learning and memory, 96(4), 583–595. [DOI] [PubMed] [Google Scholar]
- McEwen BS (1998). Stress, adaptation, and disease: Allostasis and allostatic load. Annals of the New York academy of sciences, 840(1), 33–44. [DOI] [PubMed] [Google Scholar]
- McEwen BS, & Seeman T (1999). Protective and damaging effects of mediators of stress: elaborating and testing the concepts of allostasis and allostatic load. Annals of the New York Academy of Sciences, 896(1), 30–47. [DOI] [PubMed] [Google Scholar]
- McEwen BS, & Stellar E (1993). Stress and the individual: mechanisms leading to disease. Archives of internal medicine, 153(18), 2093–2101. [PubMed] [Google Scholar]
- Netsi E, Pearson R, Murray L, Cooper P, Craske M, & Stein A (2017). The long term course of persistent and severe postnatal depression and its impact on child development. [DOI] [PMC free article] [PubMed]
- Norhayati M, Hazlina NN, Asrenee A, & Emilin WW (2015). Magnitude and risk factors for postpartum symptoms: a literature review. Journal of affective Disorders, 175, 34–52. [DOI] [PubMed] [Google Scholar]
- O’Hara MW, & Wisner KL (2014). Perinatal mental illness: definition, description and aetiology. Best Practice & Research Clinical Obstetrics & Gynaecology, 28(1), 3–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Campo P, Schetter CD, Guardino CM, Vance MR, Hobel CJ, Ramey SL, & Shalowitz MU (2016). Explaining racial and ethnic inequalities in postpartum allostatic load: Results from a multisite study of low to middle income woment. SSM-population health, 2, 850–858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearson RM, Evans J, Kounali D, Lewis G, Heron J, Ramchandani PG, . . . Stein A (2013). Maternal depression during pregnancy and the postnatal period: risks and possible mechanisms for offspring depression at age 18 years. JAMA psychiatry, 70(12), 1312–1319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Promotion O. o. D. P. a. H. (2018). Healthy People 2020: Social Determinants of Health. Retrieved from https://www.healthypeople.gov/2020/topics-objectives/topic/social-determinants-of-health
- Rabin RF, Jennings JM, Campbell JC, & Bair-Merritt MH (2009). Intimate partner violence screening tools: a systematic review. American journal of preventive medicine, 36(5), 439–445. e434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramey SL, Schafer P, DeClerque JL, Lanzi RG, Hobel C, Shalowitz M, . . . Raju TN (2015). The preconception stress and resiliency pathways model: A multi-level framework on maternal, paternal, and child health disparities derived by community-based participatory research. Maternal and Child Health Journal, 19(4), 707–719. [DOI] [PubMed] [Google Scholar]
- Ribble F, PhD M, & Keddie M (2001). Understanding the Hispanic paradox. Ethn Dis, 11(3), 496–518. [PubMed] [Google Scholar]
- Roy-Matton N, Moutquin J-M, Brown C, Carrier N, & Bell L (2011). The impact of perceived maternal stress and other psychosocial risk factors on pregnancy complications. Journal of Obstetrics and Gynaecology Canada, 33(4), 344–352. [DOI] [PubMed] [Google Scholar]
- Schetter CD, & Tanner L (2012). Anxiety, depression and stress in pregnancy: implications for mothers, children, research, and practice. Current opinion in psychiatry, 25(2), 141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seeman TE, Singer BH, Rowe JW, Horwitz RI, & McEwen BS (1997). Price of adaptation—allostatic load and its health consequences: MacArthur studies of successful aging. Archives of internal medicine, 157(19), 2259–2268. [PubMed] [Google Scholar]
- Shapiro GD, Fraser WD, Frasch MG, & Séguin JR (2013). Psychosocial stress in pregnancy and preterm birth: associations and mechanisms. Journal of Perinatal Medicine, 41(6), 631–645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherin KM, Sinacore JM, Li X-Q, Zitter RE, & Shakil A (1998). HITS: a short domestic violence screening tool for use in a family practice setting. FAMILY MEDICINE-KANSAS CITY-, 30, 508–512. [PubMed] [Google Scholar]
- Sockol LE, Epperson CN, & Barber JP (2014). The relationship between maternal attitudes and symptoms of depression and anxiety among pregnant and postpartum first-time mothers. Archives of women’s mental health, 17(3), 199–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun S, Hoyt WT, Brockberg D, Lam J, & Tiwari D (2016). Acculturation and enculturation as predictors of psychological help-seeking attitudes (HSAs) among racial and ethnic minorities: A meta-analytic investigation. Journal of counseling psychology, 63(6), 617. [DOI] [PubMed] [Google Scholar]
- Tanner Stapleton LR, Dunkel Schetter C, Dooley LN, Guardino CM, Huynh J, Paek C, . . . Lanzi RG (2016). The Community Child Health Network Life Stress Interview: a brief chronic stress measure for community health research. Anxiety, Stress, & Coping, 29(4), 352–366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Velonis AJ, O’Campo P, Kaufman-Shriqui V, Kenny K, Schafer P, Vance M, . . . Chinchilli VM (2017). The Impact of Prenatal and Postpartum Partner Violence on Maternal Mental Health: Results from the Community Child Health Network Multisite Study. Journal of Women’s Health, 26(10), 1053–1061. [Google Scholar]
- Vreeburg SA, Hoogendijk WJ, van Pelt J, DeRijk RH, Verhagen JC, van Dyck R, . . . Penninx BW (2009). Major depressive disorder and hypothalamic-pituitary-adrenal axis activity: results from a large cohort study. Archives of general psychiatry, 66(6), 617–626. [DOI] [PubMed] [Google Scholar]
- Wisner KL, Parry BL, & Piontek CM (2002). Postpartum depression. New England Journal of Medicine, 347(3), 194–199. [DOI] [PubMed] [Google Scholar]
- Wu Q, Chen H-L, & Xu X-J (2012). Violence as a risk factor for postpartum depression in mothers: a meta-analysis. Archives of women’s mental health, 15(2), 107–114. [DOI] [PubMed] [Google Scholar]
- Yim IS, Stapleton LRT, Guardino CM, Hahn-Holbrook J, & Schetter CD (2015). Biological and psychosocial predictors of postpartum depression: systematic review and call for integration. Annual review of clinical psychology, 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.