Abstract
Background
Hypertension is assumed to be asymptomatic. Yet, clinically significant nocturia (≥2 nightly voids) constitutes a putative symptom of uncontrolled hypertension. Black men with hypertension may be prone to nocturia because of blunted nocturnal blood pressure (BP) dipping, diuretic drug use for hypertension, and comorbidity that predisposes to nocturia. Here, we test the hypothesis that nocturia is a common and potentially reversible symptom of uncontrolled hypertension in black men.
Methods and Results
We determined the strength of association between nocturia (≥2 nightly voids) and high BP (≥135/85 mm Hg) by conducting in‐person health interviews and measuring BP with an automated monitor in a large community‐based sample of black men in their barbershops. Because nocturia is prevalent and steeply age‐dependent after age 50 years, we studied men aged 35 to 49 years. Among 1673 black men (mean age, 43±4 years [SD]), those with hypertension were 56% more likely than men with normotension to have nocturia after adjustment for diabetes mellitus and sleep apnea (adjusted odds ratio, 1.56; 95% CI, 1.25–1.94 [P<0.0001]). Nocturia prevalence varied by hypertension status, ranging from 24% in men with normotension to 49% in men whose hypertension was medically treated but uncontrolled. Men with untreated hypertension were 39% more likely than men with normotension to report nocturia (P=0.02), whereas men whose hypertension was treated and controlled were no more likely than men with normotension to report nocturia (P=0.69).
Conclusions
Uncontrolled hypertension was an independent determinant of clinically important nocturia in a large cross‐sectional community‐based study of non‐Hispanic black men aged 35 to 49 years.
Clinical Trial Registration
URL: http://www.clinicaltrials.gov. Unqiue identifier: NCT 02321618.
Keywords: high blood pressure, hypertension, nocturia
Subject Categories: Hypertension, High Blood Pressure, Race and Ethnicity
Clinical Perspective
What Is New?
Uncontrolled hypertension was an independent determinant of clinically significant nocturia (≥2 voids per night) in a large cross‐sectional cohort of non‐Hispanic black men, which calls into question the asymptomatic nature of hypertension.
What Are the Clinical Implications?
If tight control of blood pressure could alleviate a bothersome symptom such as nocturia, it would prove a powerful public health message to increase medication adherence.
A randomized controlled trial is warranted to test whether pharmacologic reduction of nighttime blood pressure can reduce or altogether eliminate nocturia in young black men.
Introduction
Non‐Hispanic black men have the highest hypertension‐attributable death rate of any race, ethnic, or sex group in the United States.1, 2 Black men have less physician interaction than black women and thus lower rates of hypertension treatment and control.1, 2, 3 In the absence of bothersome symptoms, men in general—but especially underserved black men—are less likely than women to see the need for routine medical checkups, where hypertension typically is diagnosed and managed.3 A long‐held tenet is that the asymptomatic nature of hypertension reduces risk perception, thus hindering treatment‐seeking behavior and use of prescription blood pressure (BP) medication. But, is hypertension truly asymptomatic?
Nocturia—awakening at night to void—constitutes a putative, but understudied, symptom of uncontrolled hypertension.4 High BP induces natriuresis with diuresis (the main renal defense against surges in BP). This “pressure‐natriuresis” relationship is reset in hypertension, causing higher urine output at night than during the day (nocturnal polyuria).4 Nocturia, the most common cause of disturbed sleep, becomes clinically important when it occurs ≥2 times per night.5, 6, 7 Repeated arousal from sleep further increases BP and nocturia,8, 9, 10 creating a vicious cycle. The resulting sleep fragmentation promotes daytime sleepiness, napping, impaired quality of life, depression, falls, and absenteeism from work. It is associated with increased risk of the same cardiovascular disease events as hypertension, suggesting a common mechanistic link.6
Both nocturia and hypertension are more prevalent in non‐Hispanic black men than in men of other races/ethnicities.11, 12 Black men with hypertension may be especially prone to nocturia for several reasons. These include a high‐sodium/low‐potassium diet and blunted nocturnal dipping of BP, both of which drive nocturnal pressure‐natriuresis13, 14, 15, 16, 17; treatment with diuretics that are often recommended as first‐line BP drugs for black patients with hypertension2; and common comorbid conditions that are known determinants of nocturia including prostate disease, diabetes mellitus, sleep apnea, and salt‐retaining/edema‐forming states including venous insufficiency, heart failure, and kidney failure.18 Observational studies that enrolled few or no black people have found nocturia to be more prevalent in men and women with hypertension than with normotension; however, the strength of the association—typically based on a self‐reported history of hypertension rather than BP measurement—varied considerably and some studies found no association.4, 11, 19, 20, 21, 22, 23, 24
Thus, the goal of this study was to test the hypothesis that nocturia is a common and potentially reversible symptom of uncontrolled hypertension in black men. To test this hypothesis, we determined the strength of association between clinically important nocturia—defined as ≥2 nightly voids—and high BP by conducting in‐person health interviews and measuring BP in a large community‐based sample of black men in their barbershops, a uniquely relaxed and popular social setting for engaging black men in clinical research and obtaining accurate out‐of‐office BP measurements.25 Because nocturia prevalence rises steeply after age 50 years (as a result of prostate disease in men, cardiovascular comorbidity, and an age‐dependent reversal of the normal circadian rhythm in arginine vasopressin secretion),5 we focused our study on men aged 35 to 49 years in whom clinically important nocturia should be relatively uncommon. To examine the influence of BP level and of antihypertensive drug therapy alone and in combination, we studied the association of nocturia with hypertension that was medically untreated, treated but uncontrolled, or treated and controlled.
Methods
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Study Population
This cross‐sectional study was a prespecified substudy of a recently published cluster‐randomized trial of BP reduction in 52 black‐owned barbershops in Los Angeles County, California (Clinicaltrials.gov, NCT02321618).25 Field interviewers screened the clientele at participating barbershops to recruit self‐identified regular patrons (≥1 haircut every 6 weeks for ≥6 months) who were non‐Hispanic black men aged 35 to 79 years with systolic BP ≥140 mm Hg on 2 screening days. Women and patients undergoing dialysis and chemotherapy were excluded. Our analyses in this report are derived from the men who completed the first screening visit, which included: (1) a brief in‐person computer‐based health questionnaire that provided structured response data on nocturia frequency, known determinants of nocturia, and other relevant baseline characteristics; and (2) BP measurements. The study was approved by institutional review boards at Cedars‐Sinai Medical Center, Kaiser‐Permanente, and Westat (the survey research company that conducted the screening and collected the data reported in this article). For the first screening visit only, the institutional review boards waived written consent, which was replaced by informed verbal consent.
Study Measurements
Nocturia and covariates
Self‐reported data on nocturia frequency were obtained using the same question and structured response items used in NHANES (National Health and Nutrition Examination Survey): “During the past 30 days, how many times per night did you most typically get up to urinate from the time you went to bed at night until the time you got up in the morning: Would you say: 0, 1, 2, 3, 4, 5, or more?” Self‐reported data on potential covariates (including age, body mass index, diabetes mellitus, enlarged prostate, prostate cancer, sleep apnea, kidney disease, stroke, heart attack, and heart failure) were obtained using standard NHANES questions. To assess hypertension treatment status, men were asked whether they were now taking prescription BP pills. Men were also asked whether they were currently taking any of the following prescription medication: water pills, insulin or pills for diabetes mellitus, or pills for enlarged prostate.
BP Measurement
All BPs were measured in the barbershops using a validated oscillometric monitor (AccutorrV, Mindray).26 To automate measurement, minimize operator dependence, and eliminate human transcription error, monitor readings were directly uploaded to a computer that electronically transmitted data to a secure website. The protocol required 5 sequential readings, and discarded the first 2 and averaged the last 3 readings.27 Field interviewers were trained in proper measurement technique (5 minutes of rest, arm at heart level, back supported, legs not crossed, no urinary urgency, and no conversation with participants). The correct arm cuff size was determined for each participant.
Statistical Analysis
In accordance with current urologic standards,6 nocturia was defined as ≥2 nightly voids, which is clinically important. Absence of nocturia was defined as 0 or 1 nightly void. To assess the external validity of our convenience sample, we compared age‐specific prevalence rates of nocturia in our barbershop patrons with weighted estimates of US population prevalence for non‐Hispanic black men from the NHANES 2013–2014 (the last NHANES to address nocturia). Also, we compared hypertension prevalence, hypertension treatment, and hypertension control rates in our study sample with weighted estimates from NHANES 2013–2016. The statistical package of SAS procedure SURVEYFREQ was used for analyzing NHANES data. WTMEC2YR sample weights and design variables SDMVSTRA and SDMVPSU were applied in estimating the nocturia and hypertension‐related rates, standard errors, and 95% CIs. Missing data were rare and thus assumed to occur at random.
To minimize confounding by prostate disease, we focused our analyses on men younger than 50 years, above which prostate disease becomes prevalent and the dominant determinant of nocturia. We examined the prevalence by decade of self‐reported enlarged prostate, current use of prescription medications of enlarged prostate, prostate cancer, and the aggregate of these prostate conditions.
Hypertension was defined as systolic BP ≥135 mm Hg or diastolic BP ≥85 mm Hg (conventional cutoff values for out‐of‐office BP)28 or current use of prescription BP medication. Hypertension treatment rate was calculated as the percentage of patients with hypertension currently using prescription BP medication. Hypertension control rate was calculated as the percentage of patients with hypertension with systolic BP <135 mm Hg and diastolic BP <85 mm Hg.
Summary statistics were generated to describe patient characteristics for the whole cohort and by the nocturia status (≥2 nightly voids, yes/no). In the analysis for the association of nocturia with hypertension, men aged 35 to 49 years with prostate disease, heart attack, heart failure, stroke, or kidney disease were excluded because the numbers were small (Table S1). The association of nocturia with hypertension was evaluated using logistic regression that included hypertension (yes/no) as the primary predictor and diabetes mellitus and sleep apnea as covariates. We also classified hypertension into categories “untreated,” “treated and controlled,” and “treated but uncontrolled,” and evaluated the association of nocturia with these categories (normotension as the reference) using logistic regression while adjusting for diabetes mellitus and sleep apnea. We further evaluated the effect of diuretic use on the odds of nocturia by classifying “treatment and controlled” and “treated but uncontrolled” into subgroups with and without diuretic use. An additional logistic regression analysis was performed to determine whether nocturia is a predictor of uncontrolled hypertension in treated patients. In this analysis, we adjusted for age, diabetes mellitus, and sleep apnea.
Analyses were conducted using SAS (version 9.4 for Windows, SAS Institute). All tests were 2‐sided. P<0.05 was considered statistically significant.
Results
Sample Selection and Validation
As expected, nocturia prevalence increased with age. At each decade of life, the percentage of black male barbershop patrons reporting ≥2 nightly voids corresponded closely with weighted US population prevalence estimates from NHANES and were well within the 95% CIs (Figure 1). Among our participants, the prevalence of reported aggregate prostate disease, and its individual components, increased exponentially after age 49 years (Figure 2). Thus, to study the association of nocturia with hypertension, we focused our analyses on younger men aged 35 to 49 years.
Figure 1.
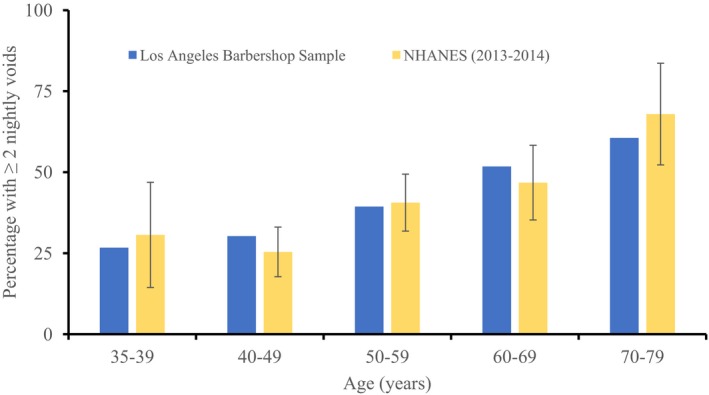
Age‐specific prevalence of nocturia (≥2 nightly voids) in non‐Hispanic black men aged 35 to 79 years: Los Angeles Barbershop Sample (blue bars) vs NHANES (National Health and Nutrition Examination Survey) data weighted to the US population (yellow bars). Weighted data are from the 2013–2014 survey, which was the most recent survey that asked about nocturia. Error bars represent 95% CIs.
Figure 2.
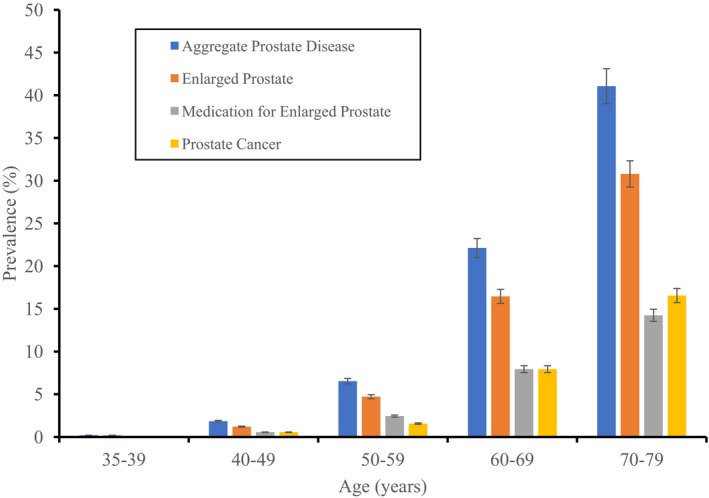
Age‐specific prevalence of prostate disease in the Los Angeles Barbershop Sample. Data are by participant self‐report. Error bars represent standard error.
Of 4027 black male barbershop patrons aged 35 to 79 years who completed all data collection for the initial screening visit, we excluded from analysis 2279 patrons aged 50 years and older (Figure S1). We excluded an additional 75 patrons with potentially confounding comorbidities because the number of patrons with each comorbid condition was too small to include in logistic regression. Thus, the primary analysis included 1673 men aged 35 to 49 years. Among these, hypertension prevalence (43.9%) and rates of hypertension treatment and control (15%) corresponded closely with NHANES data and were well within the 95% CIs (Table S2).
Hypertension is an Independent Determinant of Nocturia in Black Men Aged 35 to 49 Years
Overall, 29% of the final sample reported clinically significant nocturia. Compared with men reporting 0 or 1 nightly void, those with nocturia (≥2 nightly voids) had similar mean age and body mass index but, as expected, reported a higher prevalence of both diabetes mellitus and sleep apnea (Table 1). Hypertension was present in 53% of men with nocturia compared with 40% of men without nocturia. Men with hypertension were 56% more likely than men with normotension to have nocturia after adjustment for diabetes mellitus and sleep apnea (adjusted odds ratio [OR], 1.56; 95% CI, 1.25–1.94 [P<0.0001]) (Table 2).
Table 1.
Characteristics of Barbershop Patrons Aged 35 to 49 Years
| 0 or 1 Nightly Void | ≥2 Nightly Voids | All Patients | P Value (0 or 1 vs ≥2 Nightly Voids) | |
|---|---|---|---|---|
| No. (%) | 1196 (71) | 477 (29) | 1673 (100) | |
| Age, mean±SD, ya | 43±4 | 43±4 | 43±4 | 0.1704 |
| Body mass index, kg/m2 a | 30±6 | 31±7 | 30±6 | 0.0001 |
| Diabetes mellitusa | 68 (6) | 55 (12) | 123 (7) | <0.0001 |
| Sleep apneaa | 85 (7) | 56 (12) | 141 (8) | 0.0021 |
| Hypertension | 481 (40) | 254 (53) | 735 (44) | <0.0001 |
Values are expressed as number (percentage) or mean±SD.
Values are by participant self‐report, except for hypertension, which was determined by both blood pressure measurement and self‐report of current use of prescription blood pressure medication.
Table 2.
Logistic Regression for Nocturia (≥2 Nightly Voids vs 0 or 1 Nightly Void)
| Unadjusted OR (95% CI) | P Value | Adjusted OR (95% CI) | P Value | |
|---|---|---|---|---|
| Hypertension | 1.69 (1.37–2.10) | <0.0001 | 1.56 (1.25–1.94) | <0.0001 |
| Diabetes mellitus | 2.16 (1.49–3.14) | <0.0001 | 1.83 (1.25–2.68) | 0.0018 |
| Sleep apnea | 1.74 (1.22–2.48) | 0.0023 | 1.48 (1.03–2.13) | 0.0352 |
OR indicates odds ratio.
Treated But Uncontrolled Hypertension is a Particularly Strong Determinant of Nocturia
Nocturia varied by hypertension status, ranging from 24% of men with normotension to 49% of men whose hypertension was treated but uncontrolled (Table 3).
Table 3.
Prevalence and Odds of Nocturia (≥2 Nightly Voids) by Hypertension Status
| SBP, mean±SD, mm Hg | DBP, mean±SD, mm Hg | Nocturia | |||
|---|---|---|---|---|---|
| Percentage | OR (95% CI)a | P Value | |||
| Normotensionb | 120±9 | 71±7 | 24 | 1.00 | ··· |
| Hypertension | ··· | ··· | ··· | ··· | ··· |
| Treated, uncontrolled | 148±14 | 91±11 | 49 | 2.63 (1.85–3.74) | <0.0001 |
| Untreated | 144±12 | 87±10 | 31 | 1.39 (1.08–1.79) | 0.0097 |
| Treated, controlled | 123±8 | 74±7 | 29 | 1.10 (0.69–1.73) | 0.6969 |
DBP indicates diastolic blood pressure; OR, odds ratio; SBP, systolic blood pressure.
Adjusted for diabetes mellitus and sleep apnea.
Reference group.
Men with treated but uncontrolled hypertension were 2.63 times more likely than men with normotension to report ≥2 nightly voids (adjusted OR, 2.63; 95% CI, 1.85–3.74 [P<0.0001]) (Table 3 and Figure 3). Men with untreated hypertension were 39% more likely than men with normotension to report ≥2 nightly voids (P=0.0097), whereas men whose hypertension was treated and controlled were no more likely than men with normotension to report ≥2 nightly voids (Table 3 and Figure 3). The adjusted OR for nocturia was considerably higher for patients with hypertension that was treated but uncontrolled than for patients with untreated hypertension (P<0.0008, Figure 3).
Figure 3.
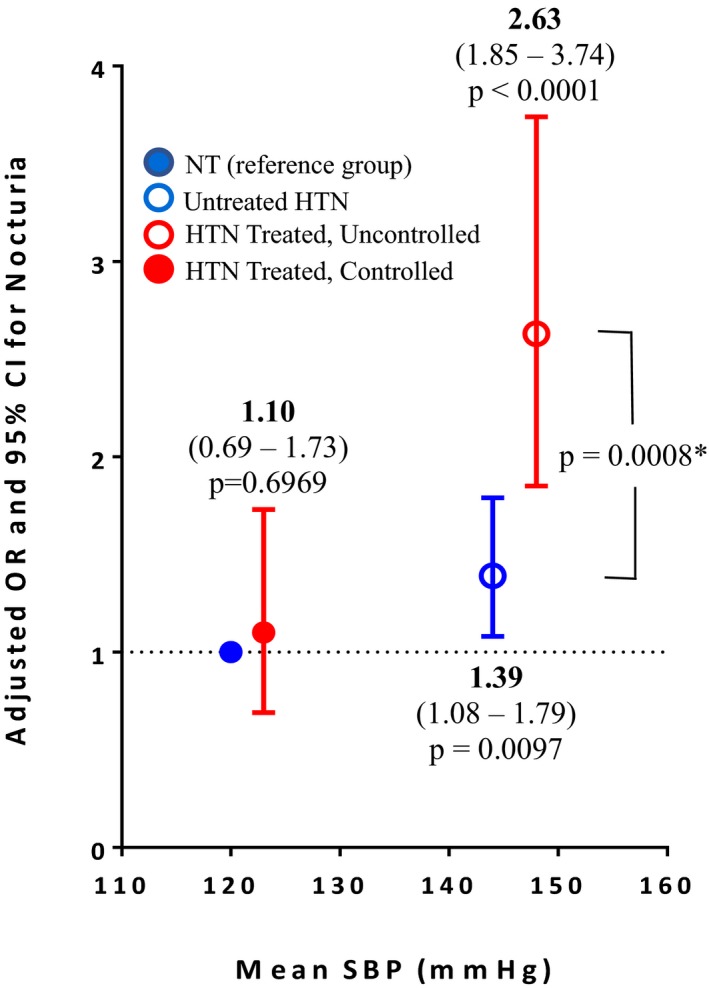
Adjusted odds ratios (ORs) and 95% CIs for nocturia plotted against group mean values for systolic blood pressure (SBP). *A statistically significant difference exists between the adjusted ORs for men with treated but uncontrolled hypertension (HTN) vs those with untreated hypertension (P=0.0008).
Based on the above findings, additional logistic regressions were performed. The first was aimed at determining the effect of diuretic use on nocturia. Among patients with treated and controlled hypertension, diuretic use increased the odds of nocturia after adjustment for both diabetes mellitus and sleep apnea (P<0.03, Table S3). However, there was no statistically significant difference in the odds among patients with treated uncontrolled hypertension (P=0.39). The second analysis was performed to determine whether nocturia is a predictor (ie, a symptom) of uncontrolled hypertension in treated patients. Among patients with treated hypertension, men with nocturia were 2.47 times more likely to have elevated BP after adjustment for age, diabetes mellitus, and sleep apnea (adjusted OR, 2.47; 95% CI, 1.46–4.17 [P=0.0007]) (Table S4).
Discussion
In a large community‐based sample of non‐Hispanic black male barbershop patrons aged 35 to 49 years without known prostate disease or prior cardiovascular events or kidney disease, we found that clinically important nocturia was common and positively associated with both high BP per se and BP drug therapy. By far, the strongest association was in men who were using prescription BP medication but still had elevated BP. These men were 2.63 times more likely to have nocturia than men with normotension. Among patients with treated hypertension, those with nocturia were 2.47 times more likely to have uncontrolled high BP. Thus, these data implicate nocturia as a common symptom of uncontrolled hypertension—especially unsuccessfully treated hypertension—among relatively young middle‐aged black men.
The 29% overall prevalence rate of ≥2 nightly voids in our study (as in NHANES) is 2 to 3 times higher than what has been reported for men of this age group in white US and European population studies, as well as in Asian men.18, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32 Our data indicate that a major factor in this exceptionally high rate of nocturia in young black men is a high prevalence of hypertension (44%) combined with a low rate of hypertension control—only 15%. Men with untreated hypertension were 39% more likely to have nocturia than men with normotension, indicating that high BP per say constitutes an independent determinant of nocturia. On one hand, the adjusted OR of 1.39 seems modest given that mean systolic BP was 24 mm Hg higher in patients with untreated hypertension than in men with normotension. On the other hand, the strength of association may be underestimated, being based on daytime BP rather than nighttime BP, which is the putative proximate stimulus to nocturnal pressure‐natriuresis.
The seminal finding of this study is the striking association between high BP and nocturia in men who were under medical treatment for hypertension. That the adjusted OR for nocturia was almost 2 times higher for high BP in presence than absence of drug treatment suggests several plausible explanations. First, men with treated but uncontrolled hypertension likely had much higher BP before treatment. Also, they likely had longer‐standing hypertension, which is associated with dysregulation of renal sodium transporters and blunting or reversal of the normal nocturnal dip in BP.13, 33 Second, mean systolic BP was 4 mm Hg higher and diastolic BP 5 mm Hg in men with treated uncontrolled hypertension than those with untreated hypertension. The relationship between high BP and nocturia could be exponential rather than linear. Third, nocturia has been implicated as a potential side effect of diuretics and calcium channel blockers—2 classes of BP drugs that are recommended as first‐line treatment for hypertension in black patients2, 28; however, the existing evidence for this assertion is inconclusive.21, 34, 35, 36, 37, 38 While this study assessed diuretic usage, we did not collect drug‐specific data (ie, diuretic type and time of administration). Although diuretic use did increase the odds for significant nocturia among patients with hypertension with controlled hypertension, the magnitude of the increased odds was smaller than the odds associated with uncontrolled hypertension, both with and without diuretic use. This leads us to hypothesize that tighter control of BP may help overcome any propensity of BP drugs to cause nocturia.
Study Limitations
Our study has several limitations. The data are cross‐sectional and correlational and thus do not prove causal attribution. However, compared with prior observational studies that tested for an association between hypertension and nocturia, ours had the largest sample of black men and was the only one to measure BP.4, 11, 19, 20, 21, 22, 23 We may have overestimated the strength of association of nocturia with high BP relative to its association with diabetes mellitus and sleep apnea, which were based on self‐report and thus their prevalence was likely underestimated. Undiagnosed diabetes mellitus, undiagnosed sleep apnea, or undiagnosed prostate disease may have contributed in part to the unexplained 24% prevalence rate of nocturia in our participants with normotension. Nondipping of nocturnal BP (ie, isolated nocturnal hypertension), which is common in black people14, 39, 40, 41, 42, 43 but not assessed in our study, also may have contributed to nocturia in men who have normotension by in‐barbershop (daytime) BP. The BP was measured at a single point in time, which can overestimate BP levels and underestimate hypertension control rates. However, hypertension prevalence and control rates, as well as our age‐specific prevalence rates for self‐reported nocturia in our convenience sample, were comparable to nationally representative NHANES data. While we collected general information on BP medication and diuretic use, we did not collect drug‐specific data. Finally, our health questionnaire did not ask about insomnia, shift work, and alcohol use—all potential confounders that were not taken into account in the analysis. Future randomized controlled trials should exclude men with these conditions.
The data herein confirm and extend prior studies implicating high BP as a cause for nocturia. Hypertension by self‐report was an independent determinant of ≥2 nightly voids in men in both NHANES11 and the Korean Community Health Survey.29 In an in‐patient study of older Danish men with intermittent nocturia, nocturnal BP (by ambulatory monitoring) averaged 12 mm Hg higher on nights when men experienced nocturia than on nights without nocturia.30 In older Japanese men, nocturnal polyuria was positively related to daytime BP31 and high nocturnal systolic BP and impaired nocturnal BP dipping by ambulatory BP monitoring.32, 44
Our findings call into question the assumption that uncomplicated hypertension is asymptomatic and thus have potential practical implications for both patients and providers. In young middle‐aged black men who are under medical treatment for hypertension, nocturia may be a common symptom of uncontrolled hypertension that merits further medical attention. Based on the strength of the BP‐nocturia associations reported here, we believe that a randomized controlled treatment trial is warranted to test whether pharmacologic reduction of nocturnal high BP can alleviate nocturia in young black men. If tight control of nocturnal as well as daytime hypertension were proven to eliminate bothersome nocturia and thus improve sleep in such patients, this would generate a powerful public health message to enhance BP medication compliance.
Conclusions
Uncontrolled hypertension—especially in medically treated patients—was an independent determinant of clinically important nocturia in a large cross‐sectional community‐based study of non‐Hispanic black men 35 to 49 years. A randomized treatment trial to demonstrate the effect of hypertension treatment and control on nocturia is warranted.
Sources of Funding
This work was supported by the National Institutes of Health (NIH) National Heart, Lung, and Blood Institute (R01HL117983 and 3R01HL117983‐01A1S1), the NIH National Center for Advancing Translational Sciences UCLA Clinical and Translational Science Institute (UL1TR001881), the California Endowment (grant 20131872 and 20162257), the Lincy Foundation, the Harriet and Steven Nichols Foundation, the Burns and Allen Chair in Cardiology Research at the Smidt Heart Institute, and the Division of Community Relations and Development at Cedars–Sinai Medical Center.
Disclosures
Dr Rader is a consultant of Recor Medical Inc. The remaining authors have no disclosures to report.
Supporting information
Table S1. Study Cohort Characteristics (N=4027, Aged 35–79 years)*
Table S2. Hypertension Status of Non‐Hispanic Black Men Aged 35 to 49 Years: Los Angeles Barbershop Sample vs NHANES (2013–2016)*
Table S3. Logistic Regression for Nocturia (≥2 Nightly Voids) With or Without Diuretics (n=1673)
Table S4. Logistic Regression for Nocturia (≥2 Nightly Voids) as a Determinant of Blood Pressure ≥135/85 mm Hg Among Patients With Treated Hypertension
Figure S1. Sample selection.
Acknowledgments
We wish to dedicate this article to Ronald G. Victor, MD, our beloved colleague, mentor, and friend who passed away shortly before publication. The authors thank the participants for taking part in the study, the barbers and barbershop owners for allowing us to conduct the study in their barbershops, and the Westat team for rigorous data collection.
(J Am Heart Assoc. 2019;8:e010794 DOI: 10.1161/JAHA.118.010794.)
References
- 1. Benjamin EJ, Blaha MJ, Chiuve SE, Cushman M, Das SR, Deo R, de Ferranti SD, Floyd J, Fornage M, Gillespie C, Isasi CR, Jiménez MC, Jordan LC, Judd SE, Lackland D, Lichtman JH, Lisabeth L, Liu S, Longenecker CT, Mackey RH, Matsushita K, Mozaffarian D, Mussolino ME, Nasir K, Neumar RW, Palaniappan L, Pandey DK, Thiagarajan RR, Reeves MJ, Ritchey M, Rodriguez CJ, Roth GA, Rosamond WD, Sasson C, Towfighi A, Tsao CW, Turner MB, Virani SS, Voeks JH, Willey JZ, Wilkins JT, Wu JH, Alger HM, Wong SS, Muntner P. Heart disease and stroke statistics—2017 update: a report from the American Heart Association. Circulation. 2017;135:e146–e603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, DePalma SM, Gidding S, Jamerson KA, Jones DW, MacLaughlin EJ, Muntner P, Ovbiagele B, Smith SC Jr, Spencer CC, Stafford RS, Taler SJ, Thomas RJ, Williams KA Sr, Williamson JD, Wright JT Jr. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2017;71:e13–e115. [DOI] [PubMed] [Google Scholar]
- 3. Victor RG, Leonard D, Hess P, Bhat DG, Jones J, Vaeth PA, Ravenell J, Freeman A, Wilson RP, Haley RW. Factors associated with hypertension awareness, treatment, and control in Dallas County, Texas. Arch Intern Med. 2008;168:1285–1293. [DOI] [PubMed] [Google Scholar]
- 4. Feldstein CA. Nocturia in arterial hypertension: a prevalent, underreported, and sometimes underestimated association. J Am Soc Hypertens. 2013;7:75–84. [DOI] [PubMed] [Google Scholar]
- 5. Weiss JP, Marshall SD. Nocturia In: Wein AJ, Kavoussi LR, Partin AW, Peters CA, eds. Campbell‐Walsh Urology. 11th ed Philadelphia, PA: Elsevier; 2016:1821–1835. [Google Scholar]
- 6. Oelke M, De Wachter S, Drake MJ, Giannantoni A, Kirby M, Orme S, Rees J, van Kerrebroeck P, Everaert K. A practical approach to the management of nocturia. Int J Clin Pract. 2017;71:e13027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Weiss JP, Blaivas JG, Van Kerrebroeck PE, Wein AJ. Nocturia: Causes, Consequences, and Clinical Approaches. New York, NY: Springer; 2012:172. [Google Scholar]
- 8. Kamperis K, Hagstroem S, Radvanska E, Rittig S, Djurhuus JC. Excess diuresis and natriuresis during acute sleep deprivation in healthy adults. Am J Physiol Renal Physiol. 2010;299:F404–F411. [DOI] [PubMed] [Google Scholar]
- 9. Perk G, Ben‐Arie L, Mekler J, Bursztyn M. Dipping status may be determined by nocturnal urination. Hypertension. 2001;37:749–752. [DOI] [PubMed] [Google Scholar]
- 10. Agarwal R, Light RP, Bills JE, Hummel LA. Nocturia, nocturnal activity, and non‐dipping. Hypertension. 2009;54:646–651. [DOI] [PubMed] [Google Scholar]
- 11. Markland AD, Vaughan CP, Johnson TM II, Goode PS, Redden DT, Burgio KL. Prevalence of nocturia in United States men: results from the National Health and Nutrition Examination Survey. J Urol. 2011;185:998–1002. [DOI] [PubMed] [Google Scholar]
- 12. Kupelian V, Link CL, Hall SA, McKinlay JB. Are racial/ethnic disparities in the prevalence of nocturia due to socioeconomic status? Results of the BACH survey. J Urol. 2009;181:1756–1763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Bankir L, Perucca J, Weinberger MH. Ethnic differences in urine concentration: possible relationship to blood pressure. Clin J Am Soc Nephrol. 2007;2:304–312. [DOI] [PubMed] [Google Scholar]
- 14. Jehn ML, Brotman DJ, Appel LJ. Racial differences in diurnal blood pressure and heart rate patterns: results from the Dietary Approaches to Stop Hypertension (DASH) trial. Arch Intern Med. 2008;168:996–1002. [DOI] [PubMed] [Google Scholar]
- 15. McDonough AA, Veiras LC, Guevara CA, Ralph DL. Cardiovascular benefits associated with higher dietary K(+) vs. lower dietary Na(+): evidence from population and mechanistic studies. Am J Physiol Endocrinol Metab. 2017;312:E348–E356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. McDonough AA, Youn JH. Potassium homeostasis: the knowns, the unknowns, and the health benefits. Physiology. 2017;32:100–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Gumz ML, Rabinowitz L, Wingo CS. An integrated view of potassium homeostasis. N Engl J Med. 2015;373:60–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Tikkinen KAO. Epidemiology of nocturia: evaluation of prevalence, incidence, impact and risk factors In: Weiss JP, Blaivas JG, Kerrebroeck PE, Wein AJ, eds. Nocturia: Causes, Consequences and Clinical Approaches. New York, NY: Springer; 2012:77–107. [Google Scholar]
- 19. van Doorn B, Kok ET, Blanker MH, Westers P, Bosch JL. Determinants of nocturia: the Krimpen study. J Urol. 2014;191:1034–1039. [DOI] [PubMed] [Google Scholar]
- 20. Kupelian V, Rosen RC, Link CL, McVary KT, Aiyer LP, Mollon P, Kaplan SA, McKinlay JB. Association of urologic symptoms and chronic illnesses in men and women: contributions of symptom severity and duration. Results from the Boston Area Community Health (BACH) Survey. J Urol. 2009;181:694–700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Johnson TM II, Sattin RW, Parmlee P, Fultz N, Ouslander JG. Evaluating potentially modifiable risk factors for prevalent and incident nocturia in older adults. J Am Geriatr Soc. 2005;53:1011–1016. [DOI] [PubMed] [Google Scholar]
- 22. Bing HM, Moller LA, Jennum P, Mortensen S, Lose G. Prevalence and bother of nocturia, and causes of sleep interruption in a Danish population of men and women aged 60‐80 years. BJU Int. 2006;98:599–604. [DOI] [PubMed] [Google Scholar]
- 23. Yoshimura K, Terada N, Matsui Y, Terai A, Kinukawa N, Arai Y. Prevalence of and risk factors for nocturia: analysis of a health screening program. Int J Urol. 2004;11:282–287. [DOI] [PubMed] [Google Scholar]
- 24. Kosimaki J, Hakama M, Huhtala H, Tammela TL. Association of nonurological diseases with lower urinary tract symptoms. Scand J Urol Nephrol. 2001;35:377–381. [DOI] [PubMed] [Google Scholar]
- 25. Victor RG, Lynch K, Li N, Blyler C, Muhammad E, Handler J, Brettler J, Rashid M, Hsu B, Foxx‐Drew D, Moy N, Reid AE, Elashoff RM. A cluster‐randomized trial of blood‐pressure reduction in black barbershops. N Engl J Med. 2018;378:1291–1301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Anwar YA, Tendler BE, McCabe EJ, Mansoor GA, White WB. Evaluation of the Datascope Accutorr Plus according to the recommendations of the Association for the Advancement of Medical Instrumentation. Blood Press Monit. 1997;2:105–110. [PubMed] [Google Scholar]
- 27. Victor RG, Ravenell JE, Freeman A, Leonard D, Bhat DG, Shafiq M, Knowles P, Storm JS, Adhikari E, Bibbins‐Domingo K, Coxson PG, Pletcher MJ, Hannan P, Haley RW. Effectiveness of a barber‐based intervention for improving hypertension control in black men: the BARBER‐1 study: a cluster randomized trial. Arch Intern Med. 2011;171:342–350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. James PA, Oparil S, Carter BL, Cushman WC, Dennison‐Himmelfarb C, Handler J, Lackland DT, LeFevre ML, MacKenzie TD, Ogedegbe O, Smith SC, Svetkey LP, Taler SJ, Townsend RR, Wright JT Jr, Narva AS, Ortiz E. 2014 evidence‐based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311:507–520. [DOI] [PubMed] [Google Scholar]
- 29. Kim SY, Bang W, Kim MS, Park B, Kim JH, Choi HG. Analysis of the prevalence and factors associated with nocturia in adult Korean men. Sci Rep. 2017;7:41714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Graugaard‐Jensen C, Rittig S, Djurhuus JC. Nocturia and circadian blood pressure profile in healthy elderly male volunteers. J Urol. 2006;176:1034–1039; discussion 9. [DOI] [PubMed] [Google Scholar]
- 31. Natsume O. Diuretic pattern in adults with nocturnal polyuria: the possible contribution of blood pressure to the worsening of nocturnal polyuria. Int J Urol. 2007;14:822–827. [DOI] [PubMed] [Google Scholar]
- 32. Obayashi K, Saeki K, Kurumatani N. Independent associations between nocturia and nighttime blood pressure/dipping in elderly individuals: the HEIJO‐KYO cohort. J Am Geriatr Soc. 2015;63:733–738. [DOI] [PubMed] [Google Scholar]
- 33. McKeigue PM, Reynard JM. Relation of nocturnal polyuria of the elderly to essential hypertension. Lancet. 2000;355:486–488. [DOI] [PubMed] [Google Scholar]
- 34. Kojima T, Akishita M, Iijima K, Eto M, Ouchi Y. Nocturia in elderly people with hypertension—no influence of low‐dose thiazide added to losartan. J Am Geriatr Soc. 2008;56:2155–2156. [DOI] [PubMed] [Google Scholar]
- 35. Reynard JM, Cannon A, Yang Q, Abrams P. A novel therapy for nocturnal polyuria: a double‐blind randomized trial of furosemide against placebo. Br J Urol. 1998;81:215–218. [DOI] [PubMed] [Google Scholar]
- 36. Pedersen PA, Johansen PB. Prophylactic treatment of adult nocturia with bumetanide. Br J Urol. 1988;62:145–147. [DOI] [PubMed] [Google Scholar]
- 37. Salman M, Khan AH, Syed Sulaiman SA, Khan JH, Hussain K, Shehzadi N. Effect of calcium channel blockers on lower urinary tract symptoms: a systematic review. Biomed Res Int. 2017;2017:4269875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Fadayomi MO, Akinroye KK, Ajao RO, Awosika LA. Monotherapy with nifedipine for essential hypertension in adult blacks. J Cardiovasc Pharmacol. 1986;8:466–469. [DOI] [PubMed] [Google Scholar]
- 39. Abdalla M, Caughey MC, Tanner RM, Booth JN, Diaz KM, Anstey DE, Sims M, Ravenell J, Muntner P, Viera AJ, Shimbo D. Associations of blood pressure dipping patterns with left ventricular mass and left ventricular hypertrophy in blacks: the Jackson Heart Study. J Am Heart Assoc. 2017;6:e004847 DOI: 10.1161/JAHA.116.004847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Cooper DC, Ziegler MG, Nelesen RA, Dimsdale JE. Racial differences in the impact of social support on nocturnal blood pressure. Psychosom Med. 2009;71:524–531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Ogedegbe G, Spruill TM, Sarpong DF, Agyemang C, Chaplin W, Pastva A, Martins D, Ravenell J, Pickering TG. Correlates of isolated nocturnal hypertension and target organ damage in a population‐based cohort of African Americans: the Jackson Heart Study. Am J Hypertens. 2013;26:1011–1016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Hyman DJ, Ogbonnaya K, Taylor AA, Ho K, Pavlik VN. Ethnic differences in nocturnal blood pressure decline in treated hypertensives. Am J Hypertens. 2000;13:884–891. [DOI] [PubMed] [Google Scholar]
- 43. Ravenell J, Shimbo D, Booth JN III, Sarpong DF, Agyemang C, Beatty‐Moody DL, Abdalla M, Spruill TM, Shallcross AJ, Bress AP, Munter P, Ogedegbe G. Thresholds for ambulatory blood pressure among African Americans in the Jackson Heart Study. Circulation. 2017;135:2470–2480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Takayama M, Omori S, Iwasaki K, Shiomi E, Takata R, Sugimura J, Abe T, Obara W. Relationship between nocturnal polyuria and non‐dipping blood pressure in male patients with lower urinary tract symptoms. Low Urin Tract Symptoms. 2018. Available at: https://onlinelibrary.wiley.com/doi/full/10.1111/luts.12225. Accessed February 21, 2019. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Study Cohort Characteristics (N=4027, Aged 35–79 years)*
Table S2. Hypertension Status of Non‐Hispanic Black Men Aged 35 to 49 Years: Los Angeles Barbershop Sample vs NHANES (2013–2016)*
Table S3. Logistic Regression for Nocturia (≥2 Nightly Voids) With or Without Diuretics (n=1673)
Table S4. Logistic Regression for Nocturia (≥2 Nightly Voids) as a Determinant of Blood Pressure ≥135/85 mm Hg Among Patients With Treated Hypertension
Figure S1. Sample selection.


