Abstract
Pharmacy could serve as a model for the health informationist profession proposed by Davidoff and Florance in their 2000 editorial in the Annals of Internal Medicine. The current training and practice roles for pharmacists suggest a way to prepare health sciences librarians for work with clinical health care teams. The influences that spurred the transformation of pharmacy parallel in many respects those suggesting the need for more information professionals prepared to practice in clinical health care settings. During the same decades that health sciences librarians have been debating and experimenting with new professional roles such as clinical medical librarians, pharmacy has undergone an intensive review of its core values, mission, practice roles, and educational preparation methods. Until recently, most pharmacists graduated from five-year baccalaureate programs preparing them to understand drug products, sources of supply, and effective ways to dispense them to patients as prescribed by physicians. Today, almost all pharmacy students graduate from six-year doctor of pharmacy programs that prepare them to be the primary providers of what their profession calls “pharmaceutical care.” The pharmaceutical care model suggests that health information professionals in clinical settings could be educated and trained to provide what we might call health information care.
Today medical care is provided in an increasingly electronic, Web-networked information environment, with a vast array of online information products and services. This environment suggests for many that a virtual library of resources and services could and should be designed to provide instant answers and solutions for almost every conceivable health care information dilemma. On the positive side, this tempting and apparently ubiquitous availability of all kinds of health information has helped to convince most physicians and other health professionals that their clinical decisions (as well as their research and continuing education) should be based on the “best evidence” from the current literature. To the extent that they view librarians as key health information professionals, most clinicians also recognize that the profession should have a central role in making this information accessible. On the negative side, these same health professionals are too often frustrated when they attempt to find useful answers to their clinical care questions in this information-rich environment. Working on their own, they discover that the best evidence is often widely scattered, poorly indexed in complex databases, and difficult to locate and use for a variety of technical, economic, or political reasons. Therefore, when these same clinicians view librarians as the primary managers of the print and electronic archives of medical literature, they experience the database structures, search engines, passwords, and other access policies and procedures managed by the library as barriers to their effective use of this information.
Thus, questions concerning the professional training and practice roles of medical librarians and other health information professionals in patient care settings have been and continue to be appropriately serious topics of debate and experimentation. Case study reports and more serious evaluative studies of service programs, like clinical medical librarians (CML) and literature attached to charts (LATCH), continue to appear regularly in the literature and are reported at professional conferences. These studies and reports date at least from the first CML service created by Lamb at the University of Missouri–Kansas City in the early 1970s [1, 2]. But despite this continuing strong interest, the number of active clinical librarian programs has remained very small in proportion to the number of hospitals and other clinical settings served by health sciences libraries. Davidoff and Florance's editorial effectively summarizes the challenges that have propelled that continuing interest, while also constraining widespread implementation [3]. Health sciences librarians still struggle to provide practicing clinicians with rapid access to the best information from the medical literature in ways that truly help improve decisions at the point of care.
Davidoff and Florance also acknowledge that their health “informationist” or “clinical knowledge worker” idea is not the first proposal for a new type of information professional, educated and trained to understand both information science and the clinical care environment. As one letter to the editor prompted by Davidoff and Florance's editorial notes with some passion, pharmacists, especially those more fully trained as doctors of pharmacy (PharmDs), already combine professional training in clinical health care with an in-depth knowledge of drug therapeutics and the retrieval of relevant biomedical literature [4]. Davidoff and Florance's response to this letter suggests that the training these PharmD drug-information specialists receive may serve as a model for the broader training and professional roles they envision for health informationists or clinical knowledge workers [5]. This paper will explore that possibility more thoroughly. How did the current model of pharmaceutical education and practice evolve from the previous baccalaureate-in-pharmacy training that prepared most pharmacists for their traditional dispensing roles in drug stores and hospital pharmacies? Can the process used to change the training for, and practice of, pharmacy suggest a way to bring more widespread recognition of, and credibility to, the new professional roles health sciences librarians have been experimenting with for the past thirty years? Also, how closely do the influences that spurred this transformation of professional pharmacy training and practice parallel the issues suggesting the need to educate more health information professionals for practice in clinical care settings?
THE EMERGENCE OF PHARMACEUTICAL CARE
During roughly the same thirty years that health sciences librarians have been debating and experimenting with new professional roles in health care settings, the profession of pharmacy has undergone an intensive review of its core values, mission, practice roles, and educational preparation methods. Throughout this review, pharmacy professionals have continued to view themselves as “a major part of the system that discovers, develops, produces and distributes drug entities and drug products.” This system creates and disseminates knowledge related to drug entities, drug products, and drug distribution systems [6].
Over the course of the past century, pharmacy training evolved from a four- to a five-year baccalaureate program. This training prepared pharmacists to understand the composition and therapeutic properties of drug products, the sources of supply for those products, and the most effective ways to dispense those products to patients as prescribed by physicians. Graduate training in pharmacy was research oriented, with master's of science and doctor of philosophy paths taken by relatively few students. In 1950, the “Elliott Survey” of the American Council on Education's Committee on the Pharmaceutical Survey first recommended the development and establishment of a six-year advanced clinical degree, the doctor of pharmacy, to prepare some practitioners for advanced clinical practice [7]. Over time, the widespread value that such training could provide to patients and other health care providers began to emerge, as holders of the degree developed advanced clinical practices and engaged in clinical research activities. Recognizing the evolving nature of pharmacy practice, some pharmacy schools, beginning in the 1960s with programs on the West Coast, began to convert their curricula or add an additional track for six-year, entry-level degrees that graduated pharmacists with the PharmD degree [8].
Looking back, it is now clear that, while preserving its core professional values, pharmacy practice and education have been transformed in some fundamental ways. Today, almost all students entering pharmacy schools graduate from a six-year PharmD program that prepares them to be the primary providers of what their profession calls “pharmaceutical care,” in addition to providing the traditional knowledge and skills about the composition and dispensing of drug entities and products. Pharmaceutical care (also sometimes called pharmacotherapy) involves “judgments and decisions to avoid, initiate, maintain or discontinue drug therapy.” This care is provided in collaboration with patients, physicians, nurses, and other care providers, and pharmacists are expected to take direct responsibility for the cost, quality, and results of the pharmaceutical care provided to their patients. As core members of the clinical health care team, pharmacists are expected to be activists on behalf of their patients, helping them achieve the desired outcomes of their therapy and working as consultants to physicians, nurses, and other care providers to help them make appropriate drug treatment choices. In academic medical centers, they also collaborate actively on a variety of clinical research projects involving drug therapies [9].
Studies and reports
A key component of this move towards pharmaceutical care as the standard of pharmacy practice was the recognition that pharmaceutical education would need to be more extensive and intensive. A series of studies and reports starting in the 1940s suggested the need for major changes in the education of pharmacists to meet these new demands of the profession and to better serve the health care system and society as a whole [10–16]. In 1989, the American Association of Colleges of Pharmacy (AACP) charged the Commission to Implement Change in Pharmaceutical Education, and, starting in 1992, the commission's recommendations were adopted by the AACP as policy guidelines [17]. In 1997, the American Council on Pharmaceutical Education, the accreditation board for schools of pharmacy, formally adopted new accreditation standards and guidelines for a new PharmD curriculum as the sole professional training program for the profession. This standard became effective July 1, 2000, with a provision to allow the remaining baccalaureate programs until June 30, 2004, to move their last undergraduate students to graduation [18]. This decade-long process led to a steady increase in the number of pharmacy schools offering the PharmD as the sole first professional degree. In 1990/91, only eleven of seventy-four schools limited enrollments to PharmD candidates, but, by 1999/2000, fifty of eighty-two schools were only admitting PharmD students and another twenty-nine were enrolling both bachelor of science (BS) and PharmD students [19].
The studies and reports that led to this transformation to a new standard of education for the practice of pharmaceutical care were grounded in reflections on the basic mission of the pharmacy profession and the societal and individual patient needs it serves. The roles and responsibilities for pharmaceutical care professionals developed “in response to the increasing effectiveness, potency, precision, risk and cost of drug therapy and the increasing use of drugs in diagnosis” [20]. They also evolved in an environment of dramatic change and stress in academic health sciences centers and in health care generally.
Until recently, individual, independent care providers have characterized our health care system. Their work has been focused on curing acute diseases using specialized, technologically driven interventions in hospitals and other institutional settings, all with little attention to the costs covered by third-party payors. Health system–managed teams of professional providers more accurately characterize the rapidly emerging new health care environment. These teams work to ameliorate chronic conditions with primary interventions that balance the use of technologies and humane care in community-based settings, all with a much greater concern for costs. Similarly, professional education in the health sciences has been characterized by fixed curricula of discipline-based faculty lecture courses taught to undergraduates in campus classrooms relatively isolated from practicing professionals. The less rapidly emerging new health education environment recognizes the need to create more flexible, integrated curricula, structured around learning outcomes and using electronic media or distance-learning technologies for delivery to graduate-level students in off-campus settings, in partnership with practicing professionals [21].
A new mission and curriculum
Given this analysis of the health care and education environment for pharmaceutical care, the profession outlined and approved a new mission for pharmaceutical education encompassing the following key elements:
preparing students to function as pharmaceutical care professionals and informed citizens in a changing health care system
generating and disseminating new knowledge, through research, about drugs and about pharmaceutical care systems
inculcating students with the values necessary to serve society as caring, ethical, learning professionals and enlightened citizens
providing students with scientific fundamentals and the attitudes needed to adapt their careers to changes in health care over time
encouraging students to take active roles in shaping the policies, practices, and future directions of the profession [22]
The core PharmD curriculum for pharmaceutical care, now approved as a guideline for faculty at schools of pharmacy, includes the following components:
general education (including the humanities, social and behavioral sciences, oral and written communication, and computer and information technologies)
basic physical and biological sciences and mathematics
biomedical sciences (anatomy, physiology, biochemistry or molecular biology, immunology, and biostatistics)
pharmaceutical sciences
clinical sciences (epidemiology, pathophysiology, clinical laboratory medicine, physical assessment, health promotion, and disease prevention)
practice experiences (in ambulatory, inpatient, and managed-care environments; in ethical principle applications and legal issues; and in drug information management) [23]
Challenges and barriers
The implementation of these far-reaching changes in pharmacy education and practice were not accomplished without overcoming some significant challenges and perceived barriers. These included the need to find and organize the additional budget and faculty personnel resources to implement an entirely new curriculum in dozens of schools. The new curricula have also required new classroom and laboratory facilities and new preceptor roles, as well as new experiential practice training sites. The need to restructure some research and graduate training programs and the opportunities to develop new post-PharmD residency and fellowship programs have also posed challenges. The most significant perceived barrier has been the anxiety felt among practicing pharmacists who earned the traditional BS degree. Most schools have made plans to provide nontraditional paths for practicing professionals to earn PharmD degrees and have strengthened their continuing-education programs [24].
As this process of change moves forward, strategies to maintain the profession's commitment to change have become increasingly important topics of study and debate. The continuing rapid changes in the health care environment have presented new challenges and opportunities. These have included: managing drug therapies for large populations of patients in managed-care settings (a challenge for a profession historically oriented to serving individual patients); taking full advantage of new information technologies to gather, store, analyze, and use data on drug use and outcomes; developing new strategies and partnerships for experiential education; determining ways to provide the most cost-effective and ethical therapeutic plans; and understanding and appreciating cultural diversity as it affects pharmaceutical care. The pharmacy profession has come to understand that the implementation of these changes in pharmacy education and practice will not be finished in 2004, when the last students in baccalaureate programs graduate. Instead, the process is ongoing and will require regular reviews and the maintenance of momentum in a climate of constant change [25].
THE DEVELOPMENT OF CLINICAL INFORMATION SPECIALISTS
Given this overview of the transformation of pharmacy education and practice to a new model of pharmaceutical care, what can health sciences librarians learn that may help our profession change the education and training of health information professionals for more effective practice in clinical health care settings? First, and perhaps most importantly, the experience of pharmacists suggests that this kind of fundamental change in health sciences librarianship requires a reexamination of our core values and mission. These values must be studied in the context of the changing environment of health care, of the education of health professionals, and of the health sciences research to which our services and resources are provided. While remaining committed to the system that discovers, develops, produces, and distributes drugs, pharmacy professionals have reshaped their world view from the provision of supporting expertise on drug formulation and distribution, to the direct provision of a new form of health care to patients as equal members of the health care team. Do the core professional values of health sciences librarians encompass the potential for members of the profession to provide expertise and services equivalent to pharmaceutical care?
Professional values
The 1987 mission statement of the Medical Library Association (MLA), written as part of a major strategic planning effort, strongly supported this potential. That mission stated, in part, that through professional excellence and leadership, health sciences librarians are committed to leadership in the system that designs, develops, and manages health information systems, while also creating and providing information services and educational programs for health information users. The statement of professional values included with that strategic plan emphasized service to “society by improving health through the provision of information for the delivery of health care” [26]. Since that plan was written, the MLA Board has revised the association's mission statement to read “professional achievement and leadership … to enhance the quality of health care” [27]. But surely, in clinical health care settings, both of these mission and values statements are at least somewhat analogous to the pharmacy profession's mission to provide pharmaceutical care. The pharmaceutical care model may even suggest that the mission of health information professionals in clinical settings could become the more direct provision of a service that could be called health information care.
In this view, a new professional practice standard would have librarians trained as health informationists, working as primary health care providers. They would be educated and prepared to make the judgments and decisions needed to avoid, initiate, maintain, or discontinue the application of appropriate knowledge-based information resources in clinical care decisions. Like pharmaceutical care, health information care would be provided in collaboration with patients, physicians, nurses, and other care providers. Health informationists would be expected to take direct responsibility for the cost, quality, and results of the health information care, provided either directly to their patients or through the other professional members of the health care team. As core members of the clinical health care team, health informationists would also be expected to be activists on behalf of their patients, helping them with appropriate information resources to understand and, thus, achieve the desired outcomes of their therapy. Like PharmDs, they would work as consultants to physicians, nurses, pharmacists, and other care providers to help them make appropriate information resource choices. In academic medical center settings, health informationists would also be core members of clinical research teams.
Thus, health informationists would be prepared to assume a much more active professional role than clinical librarians on patient care teams. Clinical librarians typically note observed or requested information gaps, return to the library to search the literature, and later deliver documents or annotated bibliographies to the other team members or to patients. Informationists would be educated and trained to actively contribute their information management expertise to each patient care issue or problem encountered, pointing out the relevant information resources and information management strategies needed to resolve the health care problems at hand. As providers of health information care, informationists would immediately turn to a clinical computer workstation, or their handheld computers, to locate relevant information resources, or they would draw on their personal information management expertise in team discussions about diagnosis and prognosis as well as treatment options for their patients.
Recent research has clearly demonstrated the positive impact hospital library services can have on clinical decision making, even when those services are limited to providing one-time responses to isolated questions [28]. When 80% of 208 physicians in fifteen different hospitals state that they would probably or definitely have handled some aspect of patient care differently as a result of reviewing information provide by the library [29], the potential for health information care to improve health care outcomes is very great indeed. Health informationists can also contribute their expertise about knowledge-based information resources to hospital committees reviewing policies and procedures concerning medications, safety, patient education, and a variety of other issues where current, relevant, and authoritative information would make a significant difference.
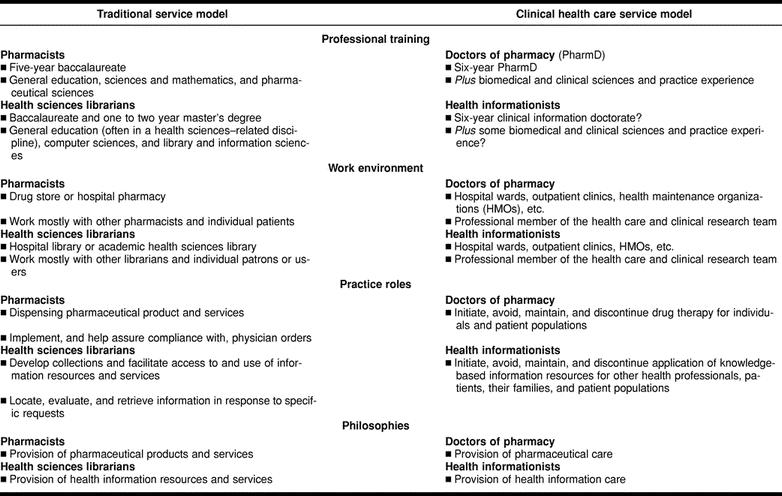
A close comparison of the characteristics of pharmacy training and practice, before and after its transition to the provision of pharmaceutical care, with health sciences librarianship, before and after its potential transition to health information care, reveals many striking parallels and analogies. Table 1 shows the key characteristics of the professional training, work environment, practice roles, and philosophies of these two professions prior to and after their actual, or potential, transition to new professional roles as care providers.
Table 1 Comparison of the traditional service model and the new clinical care service model as applied to pharmacy professionals and health information professionals
New education models
This new health informationist role in clinical health care settings would certainly require a more extensive and intensive level of professional training than the traditional one- to two-year post-baccalaureate master's degree in library or information science. The information science and clinical work curriculum components suggested by Davidoff and Florance imply more extensive training than would be possible in a one- or two-year master's degree program. Their editorial suggests a curriculum that includes, at a minimum, medical terminology, clinical epidemiology, biostatistics, and critical appraisal skills, as well as the traditional information science and management courses [30]. Such a curriculum would fit well in the framework of a six-year clinical information doctorate, modeled on the doctor of pharmacy, but substituting more extensive computer, library, and information sciences components for the pharmaceutical sciences portions of the six-year PharmD curriculum.
One current program, where some librarians receive more extensive on-the-job training in the clinical sciences along with practical experience as consultants to the health care team, is the Clinical Informatics Consult Service of the Eskind Biomedical Library at the Vanderbilt University Medical Center. These services have focused on the development of “gold standard” practices in searching and filtering the biomedical literature for members of the health care team. However, in that process, this consult service demonstrates the ability of health sciences librarians to learn enough about the biomedical and clinical sciences to become trusted professional colleagues in these clinical settings [31, 32]. The success of this consult service also suggests that a cadre of health informationists, educated and trained for six years to a clinical doctorate level, would be widely welcomed by other health professionals, especially in academic clinical health care settings.
Transition challenges
Moving librarians, educated and trained as health informationists, out of the library and into clinical care settings should not be overly difficult for two reasons. First, for the past thirty years, through a variety of clinical medical librarian programs, the profession has demonstrated that librarians learn quickly how to listen and contribute their expertise to the deliberations of health care teams. Second, a newly trained cadre of professionals would likely find a warm welcome from the other members of health care teams, who have struggled to make effective use of the best evidence in the medical literature. This welcome would also be facilitated by the teams' recognition that their new colleagues' doctoral degrees includes rigorous formal education and practical experiences focused on understanding and meeting the information needs of health professionals, patients, and their families.
The professional support network of other librarians and library staff and the physical, technical, and information resources infrastructure of a health sciences library building or space would probably be difficult to give up entirely. Doctors of pharmacy continue to rely on their pharmaceutical expertise and the resources and services of drug stores and hospital pharmacies. Similarly, health informationists would continue to use their information management and retrieval expertise and the resources and services of health sciences libraries, as well as the worldwide virtual library of electronic health information resources and services.
Perhaps the most challenging part of this potential transition from health sciences librarian training and practice to the clinical health care role of health informationists would be the assumption of professional responsibility for health information care. Health sciences librarians have traditionally worked hard to maintain some distance and neutrality about the value and applicability of specific information resources for specific patient-care decisions, leaving that final quality and applicability assessment to physicians or other health professionals. The philosophy of health information care implies a greater level of personal responsibility for assessing the value of health information resources in specific clinical care or patient compliance situations. In the clinical health care setting, the assumption of these responsibilities could also mean assuming a greater share of legal liability for the outcomes of the provided care.
The pharmaceutical care philosophy also implies a greater level of professional responsibility for the outcomes of drug therapy, but PharmDs are still not legally authorized to write prescriptions. Perhaps that fine line between professional and legal responsibility in the provision of pharmaceutical care could also serve as a model for the provision of health information care. The actual provision of health information resources to patients and their families would most appropriately involve some level of consultation with and approval by the physician or other health professional on the health care team.
FINAL THOUGHTS
This paper has outlined the case for using the profession of pharmacy as a model for how health sciences librarianship could work to transform its professional training and practice roles for more effective work in clinical health care settings. The PharmD training model is, of course, only one possibility for reaching the goal outlined by Davidoff and Florance. Most medical informatics training programs have emphasized the acquisition of additional specialized graduate training by librarians or other health professionals. Medical students interested in clinical research are often guided into medical doctor or doctor of philosophy training programs. The University at Buffalo has just announced the creation of a new doctor of jurisprudence/master's of library science dual program in legal information management and analysis offered by the School of Law and Department of Library and Information Studies to prepare a new cadre of legal information professionals [33]. Any of these approaches could help to prepare some librarians or other health professionals for the provision of health information care. However, the history and development of pharmacy and health sciences librarianship and the challenges the professions face in applying their knowledgebases and professional expertise to improve patient care have many similarities.
One important difference worth noting here is that, where almost all members of the pharmacy profession are necessarily concerned with pharmaceutical care, not all health sciences librarians need to be as directly concerned with health information care. All pharmacists are fundamentally concerned with the provision of effective drug therapies for individual patients and for populations, but not all health sciences librarians need to be concerned about the provision of effective health information resources for care providers, patients, or populations. Health information professionals also serve educators, students, and researchers. Their work and information resource needs are often only very indirectly connected to clinical health care decisions or the health information needs of specific patients, families, or populations. In addition to health informationists, there will continue to be a need for health information professionals with more general expertise in library and information science, in informatics and information systems development, in education technologies and strategies, and in the research process. Medical centers and health professions schools will continue to need these general types of expertise in nonclinical settings for the benefit of other users of health information resources.
Thus, health informationists, educated and trained to provide health information care, would likely become a specialization in the profession rather than the training and practice standard for all health sciences librarians. But the implementation of the education and training changes needed for the practice of health information care would certainly need to overcome some significant challenges and perceived barriers. As with the transition in pharmacy to the standard of pharmaceutical care, schools of library and information science or informatics would need to find and organize additional budget and faculty personnel resources to offer a more extensive and intensive curriculum. These new professional training programs would also require new classroom and laboratory facilities and new preceptor roles, as well as new experiential practice training sites.
As with pharmacy, many practicing health sciences librarians who earned the traditional American Library Association–accredited master's in library or information science would likely feel anxious. They may feel threatened by those who have earned the new doctoral degree and can command higher salaries to go along with their increased responsibilities. Thus, library or informatics schools would need to make plans to provide nontraditional paths for practicing professionals to earn the clinical information doctorate degree and to strengthen their continuing-education programs. Finally, and perhaps most importantly, those who lead and finance hospitals and other health care institutions will need to be convinced that these new doctorally trained health informationists will contribute significant value to the health care team. In business terminology, the profession will need to demonstrate the potential for clinical knowledge workers to provide real returns on investment by improving the quality of the care provided or reducing the costs of that care.
Acknowledgments
The author wishes to thank Edward M. Bednarczyk, Pharm.D., clinical assistant professor of pharmacy practice, School of Pharmacy, University at Buffalo, for his review of drafts of the manuscript and suggestions for the section on the emergence of pharmaceutical care.
REFERENCES
- Cimpl K. Clinical medical librarianship: a review of the literature. Bull Med Libr Assoc. 1985 Jan; 73(1):21–8. [PMC free article] [PubMed] [Google Scholar]
- Lipscomb CE. Clinical librarianship. Bull Med Libr Assoc. 2000 Oct; 88(4):393–5. [PMC free article] [PubMed] [Google Scholar]
- Davidoff F, Florance V. The informationist: a new health profession? Ann Int Med. 2000 Jun 20; 132(12):996–8. [DOI] [PubMed] [Google Scholar]
- Jorgenen DBR. The informationist [letter to editor]. Ann Int Med. 2001 Feb 6; 134(3):251. [Google Scholar]
- Davidoff F, Florance V. The informationist [response to letters to editor]. Ann Int Med. 2001 Feb 6; 134(3):253. 11177349 [Google Scholar]
- Commission to Implement Change in Pharmaceutical Education, American Association of Colleges of Pharmacy. Background paper I: what is the mission of pharmaceutical education? Am J Pharm Educ. 1993. Winter; 57(4):374–6. [Google Scholar]
- Elliott EC. The general report of the pharmaceutical survey, 1946–49. Washington, DC: American Council on Education, 1950:229–30. [Google Scholar]
- American Association of Colleges of Pharmacy, Study Commission on Pharmacy. Pharmacists for the future. Ann Arbor, MI: Health Administration Press, 1975:88–9. [Google Scholar]
- Commission to Implement Change in Pharmaceutical Education, American Association of Colleges of Pharmacy. Background paper I: what is the mission of pharmaceutical education? Am J Pharm Educ. 1993. Winter; 57(4):375–6. [Google Scholar]
- Elliott EC. The general report of the pharmaceutical survey, 1946–49. Washington, DC: American Council on Education, 1950:229–30. [Google Scholar]
- American Association of Colleges of Pharmacy, Study Commission on Pharmacy. Pharmacists for the future. Ann Arbor, MI: Health Administration Press, 1975:88–9. [Google Scholar]
- American Pharmaceutical Association. The final report of the task force on pharmacy education. Washington, DC: The Association, 1984. [Google Scholar]
- American Society of Hospital Pharmacists (ASHP). Directions for clinical practice in pharmacy: proceedings of an invitational conference conducted by the ASHP Research and Education Foundation and the American Society of Hospital Pharmacists (February 10–13, 1985). Am J Hosp Pharm. 1985 Jun; 42(6):1287–342. [PubMed] [Google Scholar]
- American Association of Colleges of Pharmacy. Pharmacy in the 21st century conference. Am J Pharm Educ. Winter 1989 53(suppl): 1S–78S. [Google Scholar]
- U.S. Department of Health and Human Services, Office of Inspector General. The clinical role of the community pharmacist. Washington, DC: The Department, 1990. [Google Scholar]
- SRI International. An assessment of future educational needs for community pharmacists. Menlo Park, CA: SRI International, 1990. [Google Scholar]
- Commission to Implement Change in Pharmaceutical Education, American Association of Colleges of Pharmacy. Papers from the Commission to Implement Change in Pharmaceutical Education. Am J Pharm Educ. 1993 Winter; 57(4):366–99. [Google Scholar]
- American Council on Pharmaceutical Education. Accredited professional programs of colleges and schools of pharmacy: annual directory 2000–2001. Chicago, IL: The Council, 2000:1. [Google Scholar]
- Patton JM. Profile of pharmacy students [unpublished spreadsheets and personal electronic mail report]. Alexandria, VA: American Association of Colleges of Pharmacy, 2001. [Google Scholar]
- Commission to Implement Change in Pharmaceutical Education, American Association of Colleges of Pharmacy. Papers from the Commission to Implement Change in Pharmaceutical Education. Am J Pharm Educ. 1993 Winter; 57(4):375. [Google Scholar]
- Ohvall RA, Knapp DA, Koda-Kimble MA, and Rutledge CO. Report of the 1997/98 AACP Argus Commission: doing right things right! Am J Pharm Educ. 1998 Winter; 62(suppl):5S. [Google Scholar]
- Commission to Implement Change in Pharmaceutical Education, American Association of Colleges of Pharmacy. Papers from the Commission to Implement Change in Pharmaceutical Education. Am J Pharm Educ. 1993 Winter; 57(4):376. [Google Scholar]
- Commission to Implement Change in Pharmaceutical Education, American Association of Colleges of Pharmacy. Papers from the Commission to Implement Change in Pharmaceutical Education. Am J Pharm Educ. 1993 Winter; 57(4):385. [Google Scholar]
- Commission to Implement Change in Pharmaceutical Education, American Association of Colleges of Pharmacy. Papers from the Commission to Implement Change in Pharmaceutical Education. Am J Pharm Educ. 1993 Winter; 57(4):370–371. [Google Scholar]
- Commission to Implement Change in Pharmaceutical Education. Maintaining our commitment to change. Am J Pharm Educ. 1996 Winter; 60(4):378–84. [Google Scholar]
- Medical Library Association. Shaping the future: the strategic plan of the Medical Library Association. MLA News. 1987 Apr; 194;(suppl): S1–S16. [Google Scholar]
- Medical Library Association. Our mission. [Web document]. Chicago, IL: The Association. [24 Oct 2000; cited 4 Jun 2001]. <http://www.mlanet.org/about/mission.html>. [Google Scholar]
- Marshall JG. The impact of the hospital library on clinical decision making: the Rochester study. Bull Med Libr Assoc. 1992 Apr; 80(2):169–78. [PMC free article] [PubMed] [Google Scholar]
- Marshall JG. The impact of the hospital library on clinical decision making: the Rochester study. Bull Med Libr Assoc. 1992 Apr; 80(2):169. [PMC free article] [PubMed] [Google Scholar]
- Davidoff F, Florance V. The informationist: a new health profession? Ann Int Med. 2000 Jun 20; 132(12):997. [DOI] [PubMed] [Google Scholar]
- Jerome RN, Gish KW, and Giuse NB. Evaluating the evidence: creation of gold standard practices for searching and filtering the biomedical literature. Paper presented at: 101st Annual Meeting of the Medical Library Association; Orlando, FL; May 30, 2001. [Google Scholar]
- Jerome RN, Giuse NB, Gish KW, Sathe NA, and Dietrich MS. Information needs of clinical teams: analysis of questions received by the Clinical Informatics Consult Service. Bull Med Libr Assoc. 2001 Apr; 89(2):177–84. [PMC free article] [PubMed] [Google Scholar]
- Milles J. JD/MLS dual degree program in legal information management and analysis. [Web document]. Buffalo, NY: Charles B. Sears Law Library, State University of New York at Buffalo. [15 May 2001; cited 7 Jun 2001]. <http://ublib.buffalo.edu/libraries/units/law/JDMLS_program.html>. [Google Scholar]


