Abstract
Introduction
The term “carotidynia” has been used to describe a symptom or a nosologic entity characterized by pain in the lateral neck region and over the carotid bifurcation. Recent advances in diagnostic imaging and the introduction of diagnostic criteria have led to the adoption of term “Transient perivascular inflammation of the carotid artery” (TIPIC) syndrome.
Method
A retrospective analysis of the Radiology Department’s database was performed to identify cases with the diagnosis of TIPIC syndrome. The purpose was to identify ultrasound images including B-mode technique, colour, power Doppler technique and contrast-enhanced ultrasound (CEUS).
Findings
In total, five patients with the diagnosis of TIPIC syndrome are presented in this review. TIPIC syndrome is a clinic-radiologic entity characterized by pain over the carotid area, a symptom referring to a wide differential diagnosis where imaging plays a crucial role for proper diagnosis and treatment. Characteristic imaging findings on conventional ultrasound and CEUS are presented in this review.
Discussion
TIPIC syndrome can be investigated with virtually any imaging modality. Ultrasound typically reveals perivascular infiltration and a hypoechoic intimal plaque, while no significant luminal narrowing is appreciated. Computed tomography angiography and magnetic resonance angiography also demonstrate these vascular wall changes primarily affecting the distal common carotid artery, the carotid bulb and possibly the internal carotid artery proximal part. Contrast enhancement is a very characteristic and constant finding of TIPIC lesions, suggestive of the inflammatory nature of the disease and can be appreciated on computed tomography angiography and magnetic resonance angiography. CEUS has been recently used and successfully observed contrast enhancement of the lesions, similar to computed tomography angiography and magnetic resonance angiography.
Conclusion
Ultrasound remains the first-line modality for the evaluation of TIPIC syndrome, capable of providing all the information needed, especially if supplemented with the administration of microbubbles so that the enhancement of lesions can be evaluated.
Keywords: Carotid, ultrasound, contrast-enhanced ultrasound, transient perivascular inflammation of the carotid artery syndrome
Introduction
A wide range of diseases can cause pain in the lateral neck area, including both vascular and non-vascular conditions such as carotid wall haematoma, dissection, inflammation of the salivary glands, lymphadenitis and many more. The entity of carotidynia is also one of them and has been originally described by Fay in 1927 as an idiopathic syndrome causing pain over the area of the carotid bifurcation. Later on, in 1988, it was included in the first International Classification of Headache Disorders, and in 2004, it was classified as a distinct entity.1–4 The entity of carotidynia was further complemented by the description of distinct imaging findings on every imaging modality, including ultrasound (US), computed tomography angiography (CTA) and magnetic resonance imaging or angiography (MRI/MRA). As a result, the condition of carotidynia is currently defined as the combination of pain and specific imaging findings, as it will be discussed later.3 Caution is needed regarding this entity, as it has been referred to with various terms such as carotidynia, carotidodynia, Fay syndrome, idiopathic carotiditis or carotid peri-arteritis, leading to confusion in the literature. Recently, the term “transient perivascular inflammation of the carotid artery” (TIPIC) syndrome was introduced in an attempt to describe the entity as thoroughly as possible and address the nomenclature issue. This term is also adopted and used in this review. The reader should also be cautious while reviewing the literature, as the term carotidynia has been used both to describe the symptom and a distinct disease.
US is deemed the primary imaging modality for the evaluation of the carotid arteries, thanks to the suitable superficial location of the examined vessels, the low cost and high repeatability and accuracy of the technique. Beyond the assessment of blood flow, US is also characterized by very good spatial and temporal resolution for the evaluation of vascular wall, being able to visualize subtle changes affecting any layer of the blood vessel. The technique’s role is significantly improved not only by the improvement and technological advance of modern ultrasonographic devices but also with the introduction of new technologies such as elastography and contrast-enhanced ultrasound (CEUS). As a consequence, US and CEUS are also perfectly suited for the initial investigation and follow-up of TIPIC syndrome, offering characteristic findings.5,6 In fact, the term multi-parametric ultrasound (MPUS) has been recently introduced to describe these many aspects of the ultrasonographic technique which combined provide the most diagnostic information regarding the organ examined.7
This paper reviews current literature on TIPC syndrome, presents characteristic imaging findings on conventional US and CEUS in correlation with other modalities and highlights the potential value of CEUS in the evaluation of this entity.
Clinical/laboratory findings of TIPIC
A large study of 47 patients with TIPIC syndrome was published by Lecler et al., thoroughly reviewing the patients’ characteristics and imaging findings. Overall, TIPIC syndrome was a rather rare disease, as it was characterized by a prevalence of only 2.8% in patients with neck pain of acute onset.3 Based on a different estimation, the entity of TIPIC affects 0.002% of all patients attending a medical practice, although the latter represents a type of general and unselected population.8 Patients’ median age was 48 years with a range of 39 to 56 and a slight male predominance was detected (1.5:1). Clinical presentation included pain in the lateral neck region and over the carotid bifurcation, mostly unilateral and occasionally projecting to the ipsilateral ear. In 10% of cases, the complaint may be bilateral. The pain is described as a dull or throbbing sense of discomfort which may range from mild to severe and is worsened by palpation or head and neck movements. The pain may also be associated with oedema or fullness of the affected area. Less than 20% of patients reported had associated neurologic symptoms like episodes of dizziness, vertical diplopia with oculomotor cranial nerve palsy, sensory and motor deficits. These patients with transient neurological symptoms should be treated initially with antiplatelet drugs until the final diagnosis of a TIPIC syndrome is made after the two weeks follow-up exam. Fever and other symptoms resembling upper respiratory infection or constitutional symptoms such as fever, chills or malaise were only rarely reported by the patients. On clinical examination, cervical oedema or a palpable lesion over the bifurcation of the carotid system was evident in 13% of patients, while enlarged lymph nodes were detected in 17%. In the vast majority of patients, biologic examinations like erythrocyte sedimentation rate or C-reactive protein were unremarkable, leaving the diagnosis primarily relying on imaging findings.3,4,8 A clinical sign named after the physician who first described the entity (Fay sign) has also been proposed, referring to the pain elicited by the pressure applied with the thumbs over the bifurcation.9
In 1988, when physicians were not so familiar with imaging findings of TIPIC syndrome, the International Headache Society stipulated four main clinical criteria for the diagnosis of “idiopathic carotidynia,” a term equivalent to TIPIC syndrome. These criteria comprised (i) a clinical finding of tenderness, oedema or increased pulsations over the area of the carotid bifurcation, (ii) investigations excluding structural abnormality, (iii) pain over the affected side of the neck and (iv) a self-limiting course of the symptoms of up to two weeks. These clinical criteria have now been updated with the incorporation of imaging findings, as it will be discussed in the imaging section of this review.2,4
Throughout the literature, one can understand that there was a confusion regarding optimal treatment of “carotidynia,” deriving from the unclear use of the term and the variety of conditions that can cause this symptom. Currently, TIPIC syndrome can be successfully treated with anti-inflammatory drugs or steroids, showing full clinical recovery in all patients within a mean period of approximately two weeks. In some cases, the disease may be self-limiting without the use of any treatment. A relapse rate of about 20% was reported.3,4
Imaging findings of TIPIC
Imaging findings of TIPIC syndrome include both vascular and perivascular findings. The former correspond to lesions affecting the vascular wall itself. The latter have been described by the general term “perivascular infiltration,” referring to the presence of amorphous soft tissue replacing the adipose tissue normally surrounding the carotid system.3
The vast majority of patients with TIPIC syndrome show some degree of perivascular infiltration affecting the carotid bifurcation, usually in its posterior or lateral aspect. The thickness of perivascular changes ranges from 4 to 5 mm, while its length was found to be between 15 and 28 mm. The confidence of investigators for the assessment and characterization of perivascular infiltration was invariably high for US and MRI, highlighting the value of US for the evaluation of fine structures of the vascular wall and adjacent tissues. Moreover, it was noted that these lesions do not affect the entire circumference of the carotid system but are usually limited to less than half of the perimeter, thus being characterized as eccentric. Also associated with perivascular infiltration, stranding of the adjacent adipose tissue was evidenced in all patients and with every modality (US, CTA or MRA). Enlarged lymph nodes were detected in a third of patients with US and less than 20% of patients with MRI. The tissue of perivascular infiltration showed enhancement in 85% of patients examined with CTA and 100% of MRI scans, suggesting the importance of this finding for establishing the diagnosis of TIPIC.3,4 Although imaging findings of TIPIC syndrome are primarily located in the bifurcation, there may be some extension towards the proximal internal or external carotid artery.4
Indeed, the demonstration of contrast enhancement within the abnormal tissue indicated the inflammatory nature of this lesion and is a significant finding helping to establish the diagnosis. Even though conventional ultrasonographic techniques such as colour Doppler and power Doppler technique do not have the potential to demonstrate the enhancement of tissues, the introduction of ultrasonographic contrast agents has now rendered possible to observe and quantify the enhancement pattern of normal and abnormal tissues, in real time and with a highly accurate pattern, using the technique of CEUS. The latter has gained widespread acceptance and growing indications, some of which also for the carotid arteries.10 El Nawar et al. were the first to report the use of CEUS for the evaluation of TIPIC syndrome. Similar to the literature, these authors detected a hypoechoic lesion situated in the medial-adventitial layer of the vascular wall and affecting the carotid bifurcation, which showed some contrast enhancement after the administration of microbubbles.11 This finding of contrast enhancement has also been documented in our cases (Figures 1 and 2). Moreover, it can be appreciated that the perivascular hypoechoic lesion on high-resolution B-mode US has usually an onionskin like appearance (Figure 3; also Figures 4 and 5 in the online supplemental material).
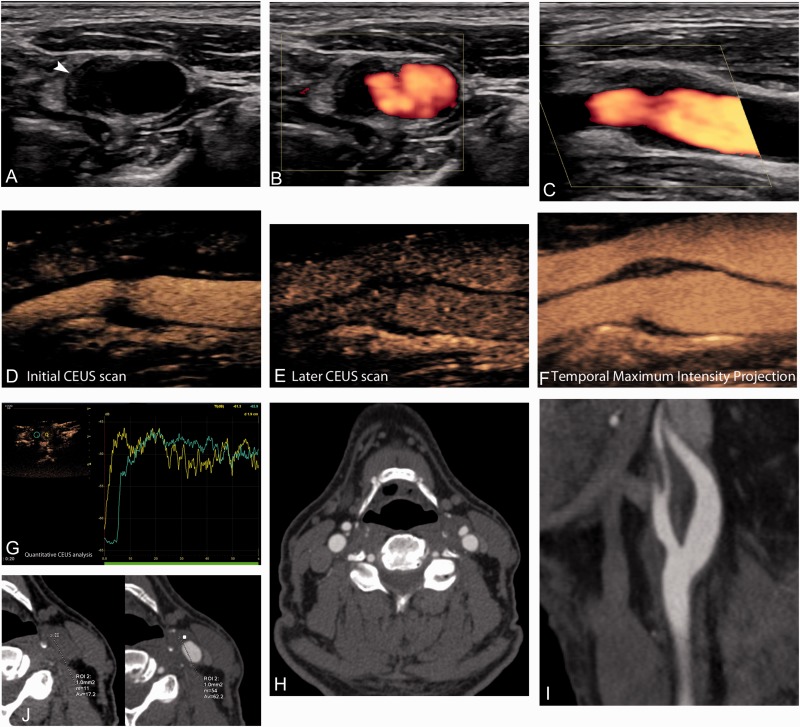
Figure 1.
A 52-year-old male patient presenting with pain over the carotid area and diagnosed with TIPIC syndrome. Axial B-mode image (a) showing perivascular infiltration in the form of hypoechoic mural thickening eccentrically affecting the external carotid artery (arrowhead). Axial (b) and longitudinal (c) power Doppler images showing only mild luminal narrowing. Longitudinal CEUS image after the administration of microbubbles (d) and a few seconds later (e) showing the presence of microbubbles within the hypoechoic lesions. Temporal maximum intensity projection CEUS image (f) showing the enhancement of lesions. CEUS also provides the possibility to quantify lesion enhancement (g) using time-intensity curves. Note that the lesion (green curve) enhances equally to the lumen (yellow curve) and a few seconds later than the latter. Axial (h) and sagittal (i) CTA images showing the eccentric mural thickening affecting the left proximal external carotid artery. Note the presence of mural thickening affecting the media and adventitia, adjacent fat stranding and the soft-tissue intimal component of the lesion causing mild luminal stenosis. Intense enhancement was demonstrated after the administration of contrast medium as it is demonstrated in the comparative image prior and after to the administration of contrast medium (j).
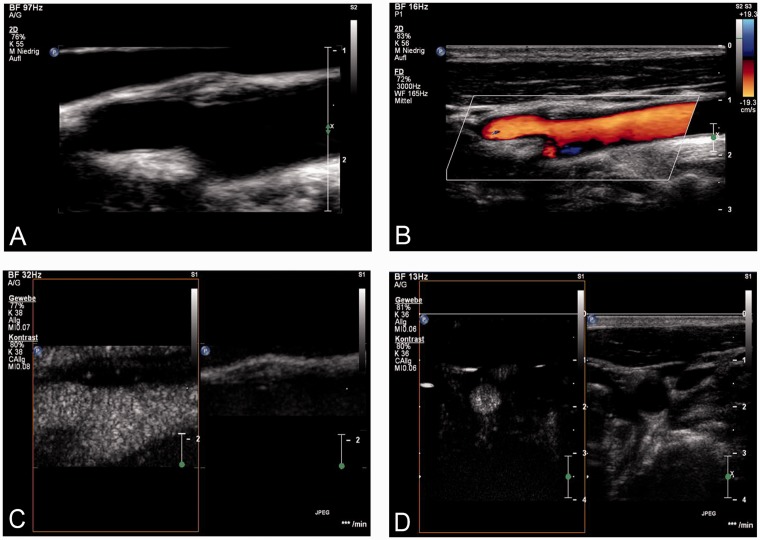
Figure 2.
A 40-year old male patient presented with recurrent short episodes of pain during the last weeks located at the region of the right carotid bifurcation. The pain increased by turning the head to the left side and occasionally the pain irradiated to the ipsilateral ear. It vanished within few days to a course of non-steroidal anti-inflammatory drug (ibuprofen). The patient was a cigarette smoker, but no other cardiovascular risk factors were known. He did not remember any previous trauma of the neck. Based on the clinical presentation and the results on standard and CEUS imaging, the diagnosis of TIPIC syndrome was made. B-mode US imaging using a 3–9 MHz linear probe revealed a perivascular hypoechogenic thickening at the origin of the right external carotid artery with outward extension of the vessel (a) but no relevant stenosis of the carotid artery on colour-Doppler US (b). The mass had an onionskin like appearance. After a bolus injection of 2.5 ml SonoVue™, the lesion in the longitudinal (c) and transversal view (d) revealed microbubbles within perivascular lesion on CEUS suggesting a vascularized and non-specific inflammatory process.
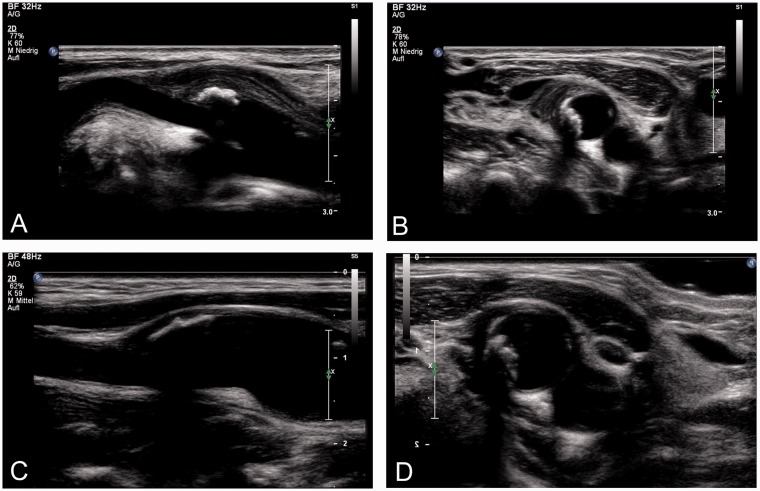
Figure 3.
A 68-year-old female subject with arterial hypertension and smoking history. She had pain at the left carotid bifurcation without trauma and no neurological symptoms. The pain decreased after treatment with a non-steroidal anti-inflammatory drug (ibuprofen). B-mode US imaging using a 5–12 MHz linear probe a perivascular hypoechogenic thickening with a onionskin like appearance at the origin of the left carotid artery in the longitudinal view (a) and in the cross-section view (b) with outward extension of the vessel and subjacent a hyperechoic, calcified luminal plaque but no relevant stenosis of the carotid artery. After 10 days, the patient was spontaneously asymptomatic. B-mode US imaging revealed a complete disappearance of the previously documented perivascular thickening at the origin of the left carotid artery. In the longitudinal (c) and cross-section view (d), only the calcified non-stenotic carotid plaque was left. Based on the clinical presentation, the course with spontaneous clear resolution of the symptoms and morphological alteration on standard US imaging the diagnosis of TIPIC syndrome in the region of an arteriosclerotic carotid plaque was made.
Vascular findings of TIPIC include intimal plaques of low echogenicity consistent with soft composition, detectable in nearly 60% of US examinations, a little less than half (46%) of CTA examinations and a third of MRA scans. Mild luminal stenosis was appreciated in approximately a third of the patients in all imaging modalities. Importantly though, no haemodynamically significant changes were detected on colour Doppler technique, and no associated brain ischaemia was detected on MRI. The lack of haemodynamic disturbance justifies the absence of audible bruit during auscultation. The mean percentage of stenosis of the carotid lumen was 20–30% as documented with every modality. The identification of intimal lesions causing luminal narrowing showed good interobserver agreement on US and MRI but was lower with CTA, suggesting the superiority of US for the appreciation of fine mural changes.3,8
On MRI, the hallmark of TIPIC syndrome is increased contrast enhancement on T1-weighted images of the symptomatic carotid wall, while there is also high signal intensity on T2-weighted images, possibly attributable to oedema. The lesion usually shows intermediate signal intensity on unenhanced T1-weighted images. The degree of enhancement has been described as striking, while the enhancing rim of inflammatory tissue may measure up to 8 mm in thickness and 3.5 cm in length, although there is a report of a lesion extending as much as 7 cm in the cranio-caudal direction. Fat saturation is particularly useful for the T1-weighted images, as the enhancement may be more readily appreciated. Similar to US, luminal narrowing is usually absent and can be evaluated using some type of angiographic sequence or based on the presence of normal flow voids within the examined vessels. MRI is also particularly useful in differentiating TIPIC from an intramural haematoma or carotid dissection that are the principal vascular differential diagnoses.4,12–14 In a recent report, MRI revealed abnormal enhancement of the laryngeal tissue adjacent to the affected carotid system, possibly attributed to a history of prior upper respiratory infection.14 CTA can also be used to evaluate patients with TIPIC syndrome, revealing a soft-tissue density lesion which demonstrates contrast enhancement (Figure 1).4 This lesion is usually eccentric and affects the posterior wall of the carotid bifurcation, while consisting of an inner layer of low attenuation resembling to a lipid atherosclerotic plaque and an outer layer of slightly higher soft-tissue density. These changes demonstrate enhancement of about 30 HU. The adipose tissue surrounding the carotid arteries may be seen obliterated or even enhancing post contrast administration. In both MRA and CTA, the rest of the carotid system should appear normal, helping exclude other diagnoses such as atherosclerosis or vasculitis.12 It has been reported that US may miss subtle mural changes diagnosed on MRI. However, this may be explained by the fact that US was mainly done for evaluation of blood flow and did not focus on wall characteristics. As a consequence, physicians performing carotid US should focus both on Doppler interrogation and vascular wall evaluation for reaching the right diagnosis.12 An important finding of TIPIC is the resolution of findings on follow-up imaging. Indeed, it has been shown that both intimal plaques and perivascular infiltration may disappear on follow-up imaging performed with US, CTA or MRA15 (Figure 3; also Figure 4 in online supplemental material). Sometimes however, some residual wall thickening of soft-tissue density showing enhancement may be noted.16 On follow-up imaging, improvement of findings should be evident in keeping with clinical symptoms resolution. The perivascular infiltration decreased in size or completely resolved in all patients reported by Lecler et al. US and MRI were able to visualize only a mild degree of residual changes in 65% of patients. The presence of intimal lesions and luminal narrowing may also resolve or persist on serial follow-up imaging with US or MRI.3
18F-FDG positron emission tomography (PET) has also been used for the evaluation of patients with TIPIC syndrome, and as it would be expected based on the inflammatory nature of this process, the affected carotid bifurcation showed double maximum standardized uptake value compared to the contralateral unaffected carotid system (6.2 vs. 3.1), while no other area of abnormal tracer activity was detected in the patient’s body.17 In another report, 18F-FDG-PET performed two weeks after the occurrence of symptoms showed no increased uptake of the tracer, findings in keeping with the described self-limiting course of the disease.11
In view of the clinic-radiologic findings which constantly occur in patients with TIPIC, four diagnostic criteria have been proposed: (i) the occurrence of pain in the area of the carotid bifurcation, of acute onset, (ii) visualization of perivascular infiltrative tissue on imaging, (iii) exclusion of different vascular or non-vascular entities based on imaging findings and (iv) improvement of clinical and imaging findings within two weeks either spontaneously or with the use of anti-inflammatory medication. The identification of an intimal plaque of soft composition could also be used as an ancillary criterion.3 It is evident that imaging plays the primary role in the diagnosis of this syndrome, as three out of four criteria are relying on imaging findings. Examining a patient with unilateral neck pain leads to a wide differential diagnosis including both vascular (Figure 6 – online supplemental material) and non-vascular diseases, as listed in Table 1. Although high clinical suspicion is necessary for the accurate diagnosis of TIPIC syndrome, the radiologist performing an US examination or reviewing an angiographic study of the carotid arteries should carefully take into consideration the clinical history, think of TIPIC syndrome in the setting of appropriate imaging findings and suggest follow-up in order to document resolution of findings. Therefore, the clinical and imaging follow-up is essential to corroborate the initial diagnosis and to make the final diagnosis of TIPIC syndrome.
Table 1.
Differential diagnosis of diseases causing unilateral neck pain apart from TIPIC syndrome
| Non-vascular causes | Vascular causes |
|---|---|
| Infection of the pharynx, oral cavity, salivary glands | Carotid aneurysm |
| Deep neck abscess | Carotid body tumour |
| Lymphadenitis | Carotid dissection |
| Thyroiditis | Acute carotid occlusion |
| Migraine type of headache | Fibromuscular dysplasia |
| Neuralgia of the trigeminal nerve | Vessel wall or intraplaque haematoma |
| Tumours of the head and neck region | |
| Temporomandibular joint syndrome | |
| Cervical spondylosis | |
| Eagle syndrome |
Conclusion
The demonstration of contrast enhancement is a very important feature of TIPIC syndrome, is attributed to the postulated inflammatory nature of the disease and can be traditionally observed on CTA, MRA and nuclear medicine studies. However, all these modalities are limited by the increased cost, lower patient tolerability and use of ionizing radiation or potential nephrotoxic contrast agents. Nevertheless, the same observation can now be made both qualitatively and quantitatively using the CEUS technique in a patient-friendly, cost-effective and repeatable way characterized by real-time assessment with high spatial and temporal resolution. Thus, we believe that US remains the first-line modality for the evaluation of TIPIC syndrome, while CEUS could be incorporated in the diagnostic work-up for investigation of contrast enhancement at patient presentation and for follow-up after treatment. It is clear that thanks to the widespread availability of imaging modalities and the increased awareness of physicians for this entity, future studies will further elucidate the entity of TIPIC and all its clinical and imaging manifestations.
Supplemental Material
Supplemental Material for Role of multi-parametric ultrasound in transient perivascular inflammation of the carotid artery syndrome by Vasileios Rafailidis, Ioannis Chryssogonidis, Thomas Tegos, Sasan Partovi, Afroditi Charitanti-Kouridou and Daniel Staub in Ultrasound
Acknowledgements
The patients provided written informed consent.
Contributors
VR: conception of the idea, writing the paper, revising it and providing some of the figures IC: reviewing the paper, making revisions and supervision TT: reviewing the paper, making revisions and supervision SP: drafting and revising the paper, providing figures and overall supervision ACK: reviewing the paper, making revisions and overall supervision DS: drafting and revising the paper, providing figures and overall supervision
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethics Approval
The publication of this paper has been approved by the Bioethics and Deontology Committee of the Medical School of Aristotle University of Thessaloniki during its meeting on 2 June 2016 (Number 4/2.6.2016).
Funding
The author(s) declared receipt of the following financial support for the research, authorship, and/or publication of this article: VR has received a scholarship for his PhD studies on “Imaging of the carotid vulnerable plaque with contrast-enhanced US and multi-detector computed tomography angiography” from the Alexander S. Onassis Public Benefit Foundation.
Guarantor
VR.
References
- 1.Headache Classification Subcommittee of the International Headache Society. The International Classification of Headache Disorders. 2nd edition. Cephalalgia 2004; 24(Suppl 1): 9–160. [DOI] [PubMed]
- 2.Headache Classification Committee of the International Headache Society. Classification and diagnostic criteria for headache disorders, cranial neuralgias and facial pain.. Cephalalgia 1988; 8(Suppl 7): 1–96. [PubMed] [Google Scholar]
- 3.Lecler A, Obadia M, Savatovsky J, et al. TIPIC syndrome: beyond the myth of carotidynia, a new distinct unclassified entity. AJNR Am J Neuroradiol 2017; 38: 1391–1398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stanbro M, Gray BH, Kellicut DC. Carotidynia: revisiting an unfamiliar entity. Ann Vasc Surg 2011; 25: 1144–1153. [DOI] [PubMed] [Google Scholar]
- 5.Rafailidis V and Sidhu PS. Vascular ultrasound, the potential of integration of multiparametric ultrasound into routine clinical practice. Ultrasound 2018; 26: 136–144. [DOI] [PMC free article] [PubMed]
- 6.Tahmasebpour HR, Buckley AR, Cooperberg PL, et al. Sonographic examination of the carotid arteries. RadioGraphics 2005; 25: 1561–1575. [DOI] [PubMed] [Google Scholar]
- 7.Sidhu PS. Multiparametric ultrasound (MPUS) imaging: terminology describing the many aspects of ultrasonography. Ultraschall Med 2015; 36: 315–317. [DOI] [PubMed] [Google Scholar]
- 8.Cannon CR. Carotidynia: an unusual pain in the neck. Otolaryngol Head Neck Surg 1994; 110: 387–390. [DOI] [PubMed] [Google Scholar]
- 9.Hill LM, Hastings G. Carotidynia: a pain syndrome. J Fam Pract 1994; 39: 71–75. [PubMed] [Google Scholar]
- 10.Sidhu PS, Cantisani V, Dietrich CF, et al. The EFSUMB Guidelines and Recommendations for the Clinical Practice of Contrast-Enhanced Ultrasound (CEUS) in Non-Hepatic Applications: update 2017 (Short Version). Ultraschall Med 2018; 39: 154–180. [DOI] [PubMed] [Google Scholar]
- 11.El Nawar R, Villain N, Baud JM, et al. Carotid contrast-enhanced ultrasonography and multimodal imaging in a case of TIPIC syndrome. Rev Neurol (Paris) 2018; 174: 304–307. [DOI] [PubMed] [Google Scholar]
- 12.Burton BS, Syms MJ, Petermann GW, et al. MR imaging of patients with carotidynia. AJNR Am J Neuroradiol 2000; 21: 766–769. [PMC free article] [PubMed] [Google Scholar]
- 13.Tardy J, Pariente J, Nasr N, et al. Carotidynia: a new case for an old controversy. Eur J Neurol 2007; 14: 704–705. [DOI] [PubMed] [Google Scholar]
- 14.Comacchio F, Bottin R, Brescia G, et al. Carotidynia: new aspects of a controversial entity. Acta Otorhinolaryngol Ital 2012; 32: 266–269. [PMC free article] [PubMed] [Google Scholar]
- 15.Woo JK, Jhamb A, Heran MK, et al. Resolution of existing intimal plaque in a patient with carotidynia. AJNR Am J Neuroradiol 2008; 29: 732–733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Park JK, Choi JC, Kim BS, et al. CT imaging features of carotidynia: a case report. J Neuroimaging 2009; 19: 84–85. [DOI] [PubMed] [Google Scholar]
- 17.Amaravadi RR, Behr SC, Kousoubris PD, et al. [18F] fluorodeoxyglucose positron-emission tomography-CT imaging of carotidynia. AJNR Am J Neuroradiol 2008; 29: 1197–1199. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material for Role of multi-parametric ultrasound in transient perivascular inflammation of the carotid artery syndrome by Vasileios Rafailidis, Ioannis Chryssogonidis, Thomas Tegos, Sasan Partovi, Afroditi Charitanti-Kouridou and Daniel Staub in Ultrasound